7.7 Adrenal Disorders
Open Resources for Nursing (Open RN)
The adrenal glands are a pair of small, triangular-shaped glands located on top of each kidney. See Figure 7.18[1] for an illustration of the location of the adrenal glands.
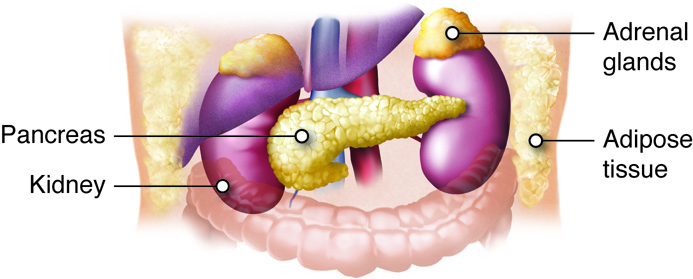
The adrenal glands are responsible for producing several hormones that are essential for maintaining overall health and regulating various body functions. The two primary parts of the adrenal glands are the adrenal cortex and the adrenal medulla, each of which produces different hormones. See Figure 7.19[2] for an illustration of adrenal cortex and adrenal medulla.
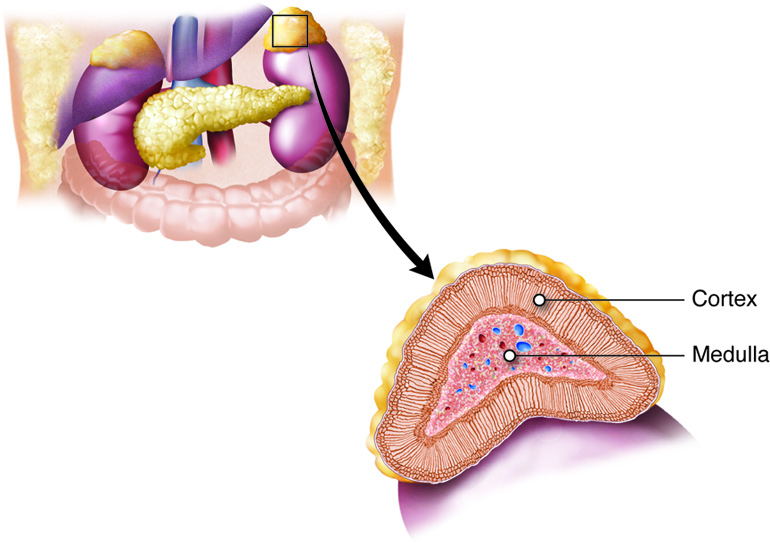
The adrenal cortex produces corticosteroids, including cortisol and aldosterone, which help to regulate metabolism, immune response, and salt and water balance. Cortisol is a glucocorticoid hormone produced by the adrenal glands that regulates physiological processes in the body. It is referred to as the “stress hormone” due to its involvement in the body’s stress response. Aldosterone is a mineralocorticoid hormone produced by the adrenal gland that regulates the salt and water balance of the body in the kidneys by increasing the retention of sodium and water and excreting potassium.
The adrenal medulla produces catecholamines, including epinephrine and norepinephrine. These hormones help induce the fight-or-flight response and play a critical role in elevating heart rate and blood pressure to prepare the body in times of stress or danger.[3]
Adrenal Insufficiency: Addison’s Disease
Addison’s disease refers to a specific type of adrenal gland insufficiency, resulting in inadequate production of cortisol and aldosterone. Addison’s disease is often the result of an autoimmune response and destruction of the adrenal glands. It can also occur as the result of tuberculosis; infection; or the sudden cessation of long-term, high-dose glucocorticoid treatment.[4]
Addisonian crisis is a life-threatening medical emergency that occurs when the body’s need for the hormones cortisol and aldosterone exceeds the available supply. This crisis is a severe complication of Addison’s disease, a condition in which the adrenal glands do not produce enough of these critical hormones. The crisis often occurs in response to a stressful event, such as an infection, surgery, trauma, or a significant physical or emotional stressor.[5],[6] Read additional information about Addisonian crisis in the following box.
A Closer Look: Emergency Care of Client in Addisonian Crisis[7]
An Addisonian crisis is a life-threatening situation, and prompt medical attention is crucial. In an Addisonian crisis there is a rapid shift in electrolytes. Sodium (Na) levels fall, leading to hyponatremia, while potassium (K) levels rise, causing hyperkalemia. These electrolyte imbalances can result in various life-threatening complications, including cardiac arrhythmias. Low blood pressure is another hallmark sign of an Addisonian crisis. It occurs due to the loss of aldosterone, which subsequently impairs the body’s ability to retain sodium.
Prompt intervention requires administration of intravenous fluids with saline to rapidly correct the dehydration, raise blood pressure, and correct electrolyte imbalances. These fluids help raise blood pressure and restore blood volume. Intravenous corticosteroids, such as hydrocortisone, are administered to rapidly replace the deficient cortisol. If hyperkalemia is present, medications may be given to lower potassium levels and reduce the risk of life-threatening cardiac arrhythmias.
Assessment
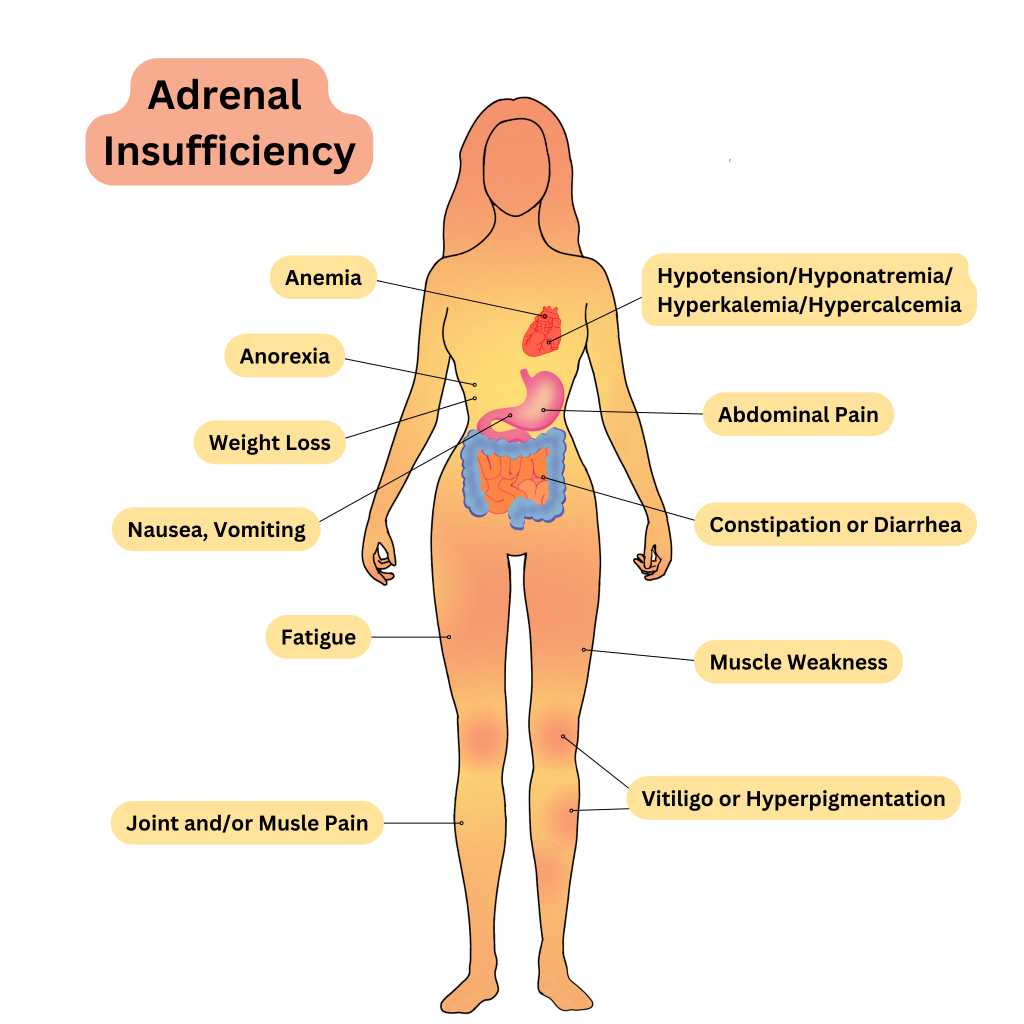
Common assessment findings for adrenal insufficiency can be seen in Table 7.7a.
Table 7.7a. Common Manifestations of Adrenal Insufficiency[8]
| Body System | Clinical Manifestations |
|---|---|
| General | Fatigue, weakness, weight loss, and salt cravings |
| Cardiovascular | Hypotension, dizziness, and fainting episodes |
| Gastrointestinal | Abdominal pain, diarrhea, nausea and vomiting, and anorexia (loss of appetite) |
| Musculoskeletal | Muscle weakness, joint pain and stiffness, and muscle and joint aches |
| Endocrine | Hypoglycemia, loss of pubic and axillary hair, amenorrhea (absence of menstrual periods in women), reduced libido and sexual dysfunction, infertility, and oligomenorrhea (infrequent or irregular menstrual periods) |
| Dermatological | Hyperpigmentation (darkening of the skin, especially in sun-exposed areas), skin thinning, easy bruising, vitiligo (loss of skin pigmentation), hyperhidrosis (excessive sweating), and slow wound healing |
| Neurological | Lethargy and apathy, depression and mood changes, difficulty concentrating, confusion and cognitive changes, headache, and irritability |
See Figure 7.20 [9]for an illustration of the clinical manifestations of adrenal insufficiency.
Diagnostic Testing
Diagnosing Addison’s disease involves a combination of clinical assessment, laboratory tests, and specialized tests to confirm adrenal insufficiency. Addison’s disease is characterized by the insufficient production of cortisol and often aldosterone by the adrenal glands, so serum cortisol and aldosterone levels are abnormally low. Additionally, as a result of abnormally low aldosterone levels, electrolyte imbalances can also be found, including hyponatremia (low sodium) and hyperkalemia (elevated potassium).[10] Review normal reference ranges for common diagnostic tests in “Appendix A – Normal Reference Ranges.”
Nursing Diagnoses
Nursing diagnoses for clients with adrenal gland hypofunction can help guide nursing care and address the specific needs of these individuals.
Common nursing diagnoses include the following:
- Risk for Imbalanced Fluid Volume
- Impaired Skin Integrity
- Fatigue
- Imbalanced Nutrition: Less Than Body Requirements
Outcome Identification
Outcome identification includes setting short- and long-term goals and creating expected outcome statements customized for the client’s specific needs. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions.
- The client will maintain adequate fluid balance as evidenced by stable vital signs and absence of signs and symptoms of dehydration or fluid overload.
- The client will exhibit intact skin without any signs of breakdown, ulceration, or infection.
- The client will demonstrate improved ability to perform activities of daily living without excessive fatigue.
- The client will achieve and maintain a stable and appropriate body weight.
Interventions
Medical Interventions
Medical interventions for adrenal insufficiency focus on medication therapy to replace the deficient hormones and effectively manage the condition to prevent adrenal crisis.
Medication Therapy
Clients with Addison’s disease are typically prescribed oral glucocorticoid medications, such as hydrocortisone, prednisone, or dexamethasone, to replace deficient cortisol levels. The dose is often divided into multiple daily doses to mimic the body’s natural cortisol release pattern.
Clients may also require mineralocorticoid replacement with medications like fludrocortisone to replace aldosterone and regulate salt and water balances in the body.
Clients with adrenal insufficiency often have abnormal electrolyte levels. Those presenting with hyperkalemia require urgent treatment to lower their potassium levels, along with close cardiac monitoring.
Review information about treatment of abnormal electrolyte levels in the “Electrolytes” section of the “Fluids and Electrolytes” chapter in Open RN Nursing Fundamentals, 2e.
Hormone Monitoring
Periodic blood tests are conducted to assess hormone levels and adjust medication doses as needed. Clients are educated about the need to increase their glucocorticoid medication during times of illness, injury, or stress to prevent an adrenal crisis.
Lifestyle Changes
Clients are advised to maintain a well-balanced diet and avoid excessive stress, which can exacerbate symptoms.[11]
Nursing Interventions
Nursing interventions for adrenal insufficiency focus on medication management, health teaching, and nutritional support.
Medication Management
Nurses administer prescribed glucocorticoid and mineralocorticoid replacement medications during inpatient care according to the health care provider’s orders. Health teaching is provided about proper medication administration techniques and adherence to the medication schedule.
Health Teaching
Nurses provide health teaching about several topics to clients with adrenal insufficiency:
- The disease process and the importance of medication adherence.
- Signs and symptoms of adrenal crises and when to immediately notify the health care provider. Additional doses of medications may be required during illness and stressful situations.
- Wearing a medical alert bracelet or necklace to inform health care professionals of their diagnosis if an emergency should occur.
Nutritional Support
Nurses advocate for multidisciplinary treatment with a registered dietician to develop a well-balanced diet plan and to ensure adequate sodium intake for clients on mineralocorticoid replacement therapy. The nurse also monitors the client’s dietary intake and hydration status.
Evaluation
Evaluation focuses on the effectiveness of the nursing interventions by reviewing the client’s expected outcomes to determine if they were met by the time frames indicated. During the evaluation phase, nurses use critical thinking to analyze reassessment data and determine if a client’s expected outcomes have been met, partially met, or not met by the time frames established. If outcomes are not met or only partially met by the time frame indicated, the care plan should be revised. Reassessment should occur every time the nurse interacts with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with others on the interprofessional team.
Nurses refer to the previously identified outcome statements and perform reassessments to determine if they have been met by the current nursing care plan or if additional interventions are required. For example, the nurse would perform assessments related to the previously established outcome criteria and determine if they were “met” or if additional interventions are required.
Cushing’s Disease & Cushing’s Syndrome
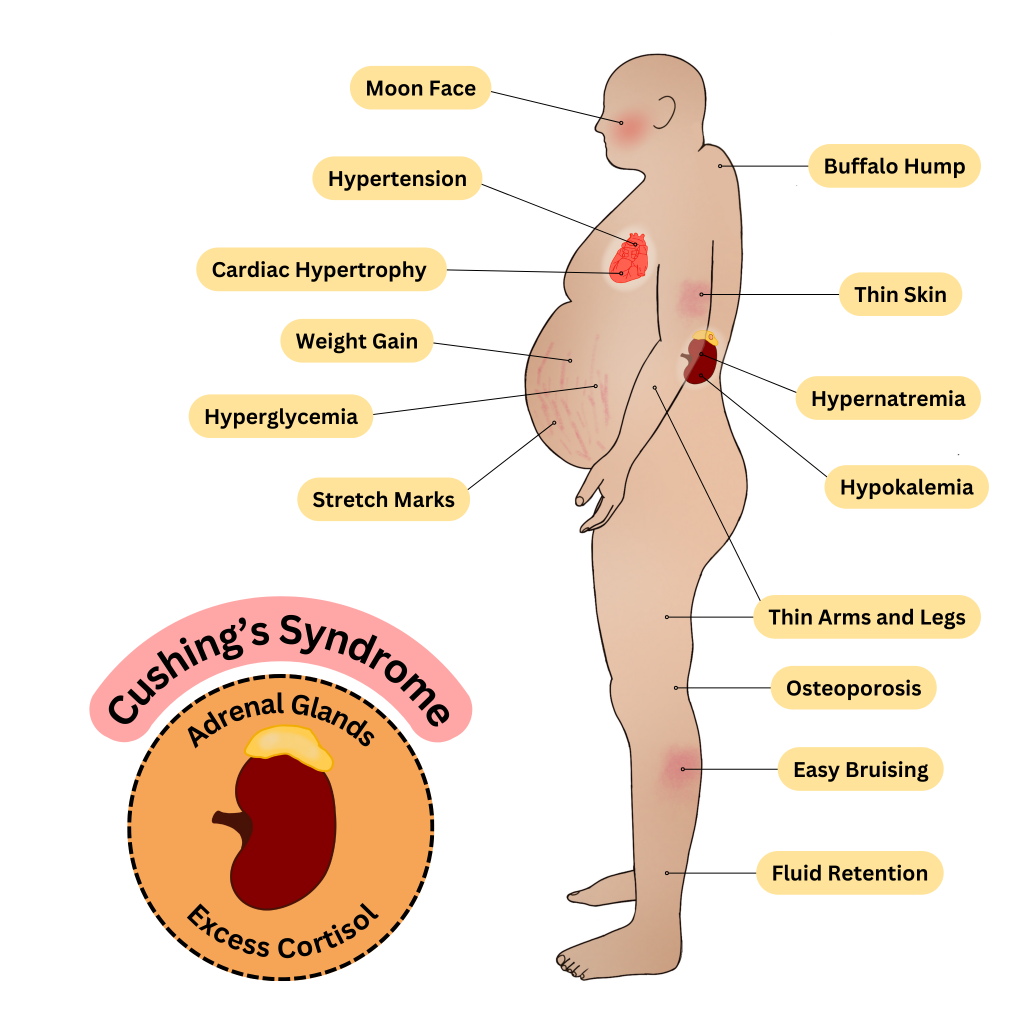
Excessive amounts of adrenal hormones, including glucocorticoids (cortisol), mineralocorticoids (aldosterone), and/or catecholamines (epinephrine and norepinephrine), can be caused by a medical condition or a side effect of other medications. Cushing’s disease is typically caused by a benign tumor in the adrenal gland that causes excess hormone production. Cushing’s syndrome is caused by excess glucocorticoid blood levels caused by medication therapy for another medical problem, such as COPD or immunosuppressive therapy after an organ transplant. In both cases, excessive glucocorticoids can cause widespread issues throughout the body.[12]
Assessment
Common assessment findings for Cushing’s disease and Cushing’s syndrome are summarized in Table 7.7b.
Table 7.7b. Common Manifestations of Cushing’s Disease and Cushing’s Syndrome[13]
| Body System | Clinical Manifestations |
|---|---|
| Endocrine | Elevated blood pressure, impaired glucose tolerance, and weight gain and obesity with classic signs such as a collection of fat on the back of the neck between the shoulder blades and a round face |
| Cardiovascular | Hypertension, palpitations, and rapid heart rate |
| Musculoskeletal | Muscle weakness and wasting and increased risk of fracture |
| Integumentary | Easy bruising and thinning of the skin and purple or red stretch marks (striae) |
| Gastrointestinal | Abdominal obesity and central weight gain, increased appetite, and overeating |
| Neurological | Mood changes, including anxiety and depression, irritability, headaches, and cognitive impairment |
| Immune | Increased susceptibility to infections, delayed wound healing, and poor scar formation |
| Reproductive | Irregular menstrual periods in women with PCOS, hirsutism (excessive hair growth) in women, and decreased libido and erectile dysfunction in men |
| Renal | Fluid retention and edema and increased urinary frequency and urgency |
| Ocular | Increased intraocular pressure and risk of glaucoma and visual disturbances, including blurry vision |
See Figure 7.21 [14] by for an illustration of common clinical manifestations of Cushing’s Disease and Cushing’s Syndrome.
Diagnostic Testing
Diagnostic testing includes blood tests of cortisol and aldosterone levels. Review information about cortisol testing under diagnostic testing in the “Adrenal Insufficiency” subsection. Electrolytes are commonly monitored because excessive aldosterone levels can cause hypernatremia (elevated sodium) and hypokalemia (decreased potassium).[15]
Nursing Diagnoses
Nursing diagnoses for clients with excessive adrenal hormones guide nursing care and address the specific needs of these individuals. Common nursing diagnoses include the following:
- Fluid Volume Excess
- Imbalanced Nutrition: More Than Body Requirements
- Disturbed Body Image
- Impaired Skin Integrity
- Risk for Infection
Outcome Identification
Outcome identification includes setting short- and long-term goals and creating expected outcome statements customized for the client’s specific needs. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions.
- The client will maintain optimal fluid balance as evidenced by normal blood pressure, no signs of edema, and balanced input and output within normal limits.
- The client will achieve and maintain a healthy body weight, with weight gain within recommended limits, while demonstrating knowledge of appropriate portion sizes and balanced dietary choices.
- The client will exhibit improved body image and self-esteem, as evidenced by positive self-talk, engagement in activities they enjoy, and verbalization of self-acceptance.
- The client will maintain intact skin and prevent skin breakdown, as evidenced by the absence of skin lesions, regular skin assessments, and adherence to recommended skin care routines.
Interventions
Medical Interventions
Medical interventions include surgery or radiation therapy, medication therapy, and lifestyle modifications.
Surgery/Radiation Therapy
Surgery may be used to remove a tumor or the affected area of the adrenal gland in cases of adrenal adenoma or pituitary adenoma. Radiation therapy may also be utilized following surgery.
Medication Therapy
If a client is experiencing Cushing’s disease as a result of glucocorticoid therapy for another condition, the medication may be stopped or reduced, if possible. Medications, such as aminoglutethimide and ketoconazole, may be prescribed to suppress cortisol production. Mineralocorticoid receptor antagonists such as spironolactone may also be prescribed to help control blood pressure and manage electrolytes. Beta-blockers may also be prescribed to help manage blood pressure and heart rate.
Read additional information about spironolactone and beta-blockers in the “Cardiovascular & Renal Systems” chapter of Open RN Nursing Pharmacology, 2e.
Lifestyle Modifications
Dietary modifications may be necessary to address weight gain or changes in appetite. Clients may also be advised to reduce sodium intake in conditions of excess aldosterone. Regular exercise, stress management, and healthy lifestyle choices can help manage symptoms and improve overall well-being.[16]
Nursing Interventions
Nursing interventions for Cushing’s disease and Cushing’s syndrome focus on promoting fluid and electrolyte balance, providing health teaching on diet and exercise, and psychological support.
Promoting Fluid and Electrolyte Balance
Nurses monitor for signs of electrolyte imbalances (e.g., potassium levels) and provide education on dietary changes and medications to address these imbalances. Health teaching about dietary sodium restrictions is provided, if necessary, to help manage fluid balance.
Health Teaching
Nurses provide health teaching to clients with Cushing’s disease on balanced nutrition and weight management. In collaboration with dieticians, meal plans are developed, and clients are taught about portion control and healthy food choices. Clients are encouraged to participate in regular physical activity to improve muscle strength and overall well-being. Exercise routines are planned that are aligned with their energy level and physical capabilities.
Psychological Support
Nurses provide emotional support and encourage open communication to help clients cope with the chronic nature of their condition and any body image changes. Resources are provided for support groups and counseling, as indicated.
Evaluation
Evaluation focuses on the effectiveness of the nursing interventions by reviewing the client’s expected outcomes to determine if they were met by the time frames indicated. During the evaluation phase, nurses use critical thinking to analyze reassessment data and determine if a client’s expected outcomes have been met, partially met, or not met by the time frames established. If outcomes are not met or only partially met by the time frame indicated, the care plan should be revised. Reassessment should occur every time the nurse interacts with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with others on the interprofessional team.
Nurses refer to the previously identified outcome statements and perform reassessments to determine if they have been met by the current nursing care plan or if additional interventions are required. For example, the nurse would perform assessments related to the previously established outcome criteria and determine if they were “met” or if additional interventions are required.
![]() RN Recap: Cushing’s Disease and Cushing’s Syndrome
RN Recap: Cushing’s Disease and Cushing’s Syndrome
View a brief YouTube video overview of Cushing’s disease and Cushing’s syndrome[17]:
![]() RN Recap: Adrenal Insufficiency
RN Recap: Adrenal Insufficiency
View a brief YouTube video overview of adrenal insufficiency[18]:
View a supplementary YouTube video[19] comparing Addison’s disease and Cushing’s disease:
- “E_M1_13.jpg” by SBCCOE is licensed under a CC BY-NC-SA 4.0. Access for free at https://pressbooks.ccconline.org/bio106/chapter/endocrine-structures-and-functions/. ↵
- “E_M1_14a.jpg” by SBCCOE is licensed under a CC BY-NC-SA 4.0. Access for free at https://pressbooks.ccconline.org/bio106/chapter/endocrine-structures-and-functions/. ↵
- Roman, S., & Wu, L. (2022). Surgical anatomy of the adrenal glands. UpToDate. Retrieved October 26, 2023, from www.uptodate.com ↵
- Niema, L., & DeSantis, A. (2023). Determining the etiology of adrenal insufficiency in adults. UpToDate. Retrieved October 26, 2023, from www.uptodate.com ↵
- Niema, L., & DeSantis, A. (2023). Determining the etiology of adrenal insufficiency in adults. UpToDate. Retrieved October 26, 2023, from www.uptodate.com ↵
- Nieman, L., & DeSantis, A. (2023). Treatment of adrenal insufficiency in adults. UpToDate. Retrieved October 27, 2023, from www.uptodate.com ↵
- Nieman, L., & DeSantis, A. (2023). Treatment of adrenal insufficiency in adults. UpToDate. Retrieved October 27, 2023, from www.uptodate.com ↵
- Nieman, L. K. (2022). Clinical manifestations of adrenal insufficiency in adults. UpToDate. Retrieved October 27, 2023, from www.uptodate.com ↵
- "Adrenal Insufficiency" by Meredith Pomietlo is licensed under CC BY-NC 4.0 ↵
- Nieman, L., & DeSantis, A. (2023). Treatment of adrenal insufficiency in adults. UpToDate. Retrieved October 27, 2023, from www.uptodate.com ↵
- Nieman, L., & DeSantis, A. (2023). Treatment of adrenal insufficiency in adults. UpToDate. Retrieved October 27, 2023, from www.uptodate.com ↵
- Nieman, L. K. (2022). Causes and pathophysiology of Cushing syndrome. UpToDate. Retrieved October 29, 2023, from www.uptodate.com ↵
- Nieman, L. K. (2023). Epidemiology and clinical manifestations of Cushing syndrome. UpToDate. Retrieved October 29, 2023, from www.uptodate.com ↵
- "Cushing's Syndrome by Meredith Pomietlo is licensed under CC BY-NC 4.0 ↵
- Nieman, L. K. (2023). Establishing the diagnosis of Cushing syndrome. UpToDate. Retrieved October 28, 2023, from www.uptodate.com ↵
- Nieman, L. K. (2023). Overview of the treatment of Cushing syndrome. UpToDate. Retrieved October 30, 2023, from www.uptodate.com ↵
- Open RN Project. (2024, April 24).Health Alterations - Chapter 7 Endocrine - Cushing’s syndrome and Cushing’s disease [Video]. YouTube. CC BY-NC 4.0 https://www.youtube.com/watch?v=u6To7kidkg0 ↵
- Open RN Project. (2024, June 23). Health Alterations - Chapter 7 - Adrenal insufficiency [Video]. You Tube. CC BY-NC 4.0 https://youtu.be/dYw0vwib4QU?si=p_VNu76TDiM9nKU- ↵
- RegisteredNurseRN.(2016, April 15). Cushings and Addisons nursing | Addison's disease vs Cushing's syndrome nursing | Endocrine NCLEX. [Video]. YouTube. All rights reserved. Reused with permission. https://www.youtube.com/watch?v=w_I-8aKaq68 ↵
National standards of care and treatment processes for common conditions. These processes are proven to reduce complications and lead to better patient outcomes.
Learning Objectives
- Explain principles of delegation
- Evaluate the criteria used for delegation
- Apply effective communication techniques when delegating care
- Determine specific barriers to delegation
- Evaluate team members' performance based on delegation and supervision principles
- Incorporate principles of supervision and evaluation in the delegation process
- Identify scope of practice of the RN, LPN/VN, and unlicensed assistive personnel roles
- Identify tasks that can and cannot be delegated to members of the nursing team
As health care technology continues to advance, clients require increasingly complex nursing care, and as staffing becomes more challenging, health care agencies respond with an evolving variety of nursing and assistive personnel roles and responsibilities to meet these demands. As an RN, you are on the front lines caring for ill or injured clients and their families, advocating for clients’ rights, creating nursing care plans, educating clients on how to self-manage their health, and providing leadership throughout the complex health care system. Delivering safe, effective, quality client care requires the RN to coordinate care by the nursing team as tasks are assigned, delegated, and supervised. Nursing team members include advanced practice registered nurses (APRN), registered nurses (RN), licensed practical/vocational nurses (LPN/VN), and assistive personnel (AP).[1]
Assistive personnel (AP) (formerly referred to as ‘‘unlicensed” assistive personnel [UAP]) are any assistive personnel trained to function in a supportive role, regardless of title, to whom a nursing responsibility may be delegated. This includes, but is not limited to, certified nursing assistants or aides (CNAs), patient-care technicians (PCTs), certified medical assistants (CMAs), certified medication aides, and home health aides.[2] Making assignments, delegating tasks, and supervising delegatees are essential components of the RN role and can also provide the RN more time to focus on the complex needs of clients. For example, an RN may delegate to AP the attainment of vital signs for clients who are stable, thus providing the nurse more time to closely monitor the effectiveness of interventions in maintaining complex clients' hemodynamics, thermoregulation, and oxygenation. Collaboration among the nursing care team members allows for the delivery of optimal care as various skill sets are implemented to care for the patient.
Properly assigning and delegating tasks to nursing team members can promote efficient client care. However, inappropriate assignments or delegation can compromise client safety and produce unsatisfactory client outcomes that may result in legal issues. How does the RN know what tasks can be assigned or delegated to nursing team members and assistive personnel? What steps should the RN follow when determining if care can be delegated? After assignments and delegations are established, what is the role and responsibility of the RN in supervising client care? This chapter will explore and define the fundamental concepts involved in assigning, delegating, and supervising client care according to the most recent joint national delegation guidelines published by the National Council of State Boards of Nursing (NCSBN) and the American Nurses Association (ANA).[3]
Effective communication is a vital component of proper assignment, delegation, and supervision. It is also one of the Standards of Professional Performance established by the American Nurses Association (ANA).[4] Research has identified that new graduate nurses are more susceptible to stress and isolation within their job roles due to poor communication and teamwork within the interdisciplinary team.[5] Strong communication skills foster a supportive work environment and colleagial relationships that benefit both patients and nursing staff.
Consider the fundamentals of good communication practices. Effective communication requires each interaction to include a sender of the message, a clear and concise message, and a receiver who can decode and interpret that message. The receiver also provides a feedback message back to the sender in response to the received message. See Figure 3.1[6] for an image of effective communication between a sender and receiver. This feedback message is referred to as closed-loop communication in health care settings. Closed-loop communication enables the person giving the instructions to hear what they said reflected back and to confirm that their message was received correctly. It also allows the person receiving the instructions to verify and confirm the actions to be taken. If closed-loop communication is not used, the receiver may nod or say “OK,” and the sender may assume the message has been effectively transmitted, but this may not be the case and can lead to errors and client harm.
An example of closed-loop communication can be found in the following exchange:
- RN: “Jane, can you get a set of vitals on Mr. Smith and let me know if the results are outside of normal range?”
- Jane, CNA: “OK, I’ll get a set of vitals on Mr. Smith and let you know if they are out of range.”
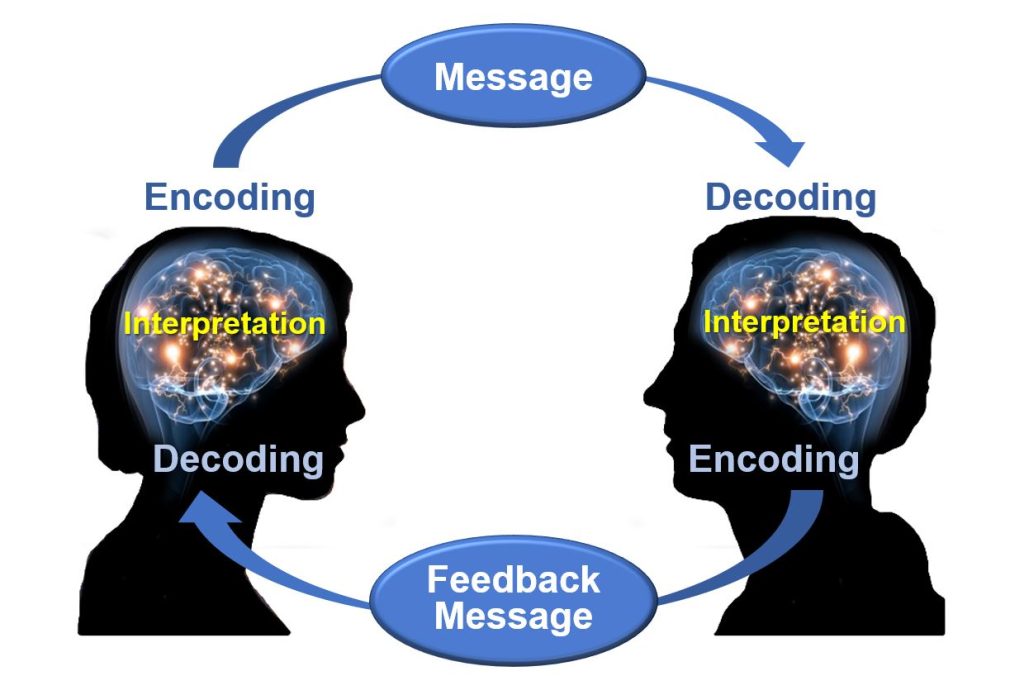
Closed-loop communication is vital for communication among health care team members to avoid misunderstandings that can cause unsafe client care. According to the HIPAA Journal, poor communication leads to a “reduction in the quality of care, poor client outcomes, wastage of resources, and high health care costs.”[7] Parameters for reporting results and the results that should be expected are often left unsaid rather than spelled out in sufficient detail. It is imperative for the RN to provide clear, complete, concise instructions when delegating. A lack of clarity can lead to misunderstanding, unfinished tasks, incomplete care, and/or medical errors.[8]
Effective communication is at the core of proper assignment, delegation, and supervision. With effective communication at the beginning of every shift, each nursing team member should have a clear plan for their shift, what to do and why, and what and when to report to the RN or team leader. Communication should continue throughout the shift as tasks are accomplished and patients’ needs change. Effective communication improves client outcomes and satisfaction scores, as well as improving team morale by enhancing the collaborative relationships of the health care team.
The RN is accountable for clear, concise, correct, and complete communication when making assignments and delegating, both initially and throughout the shift. These communication characteristics can be remembered by using the mnemonic the "4 Cs":
- Clear: Information is understood by the listener. Asking the listener to restate the instructions and the plan can be helpful to determine whether the communication is clear.
- Concise: Sufficient information should be provided to accurately perform the task, but excessive or irrelevant information should be avoided because it can confuse the listener and waste precious time.
- Correct: Correct communication is not vague or confusing. Accurate information is also aligned with agency policy and the team member’s scope of practice as defined by their state’s Nurse Practice Act and other state regulations.
- Complete: Complete instructions leave no room for doubt. Always ask if further information or clarification is needed, especially regarding tasks that are infrequently performed or include unique instructions.[9]
The use of closed-loop communication is the best method to achieve clear, concise, correct, and complete information exchanged among team members. Closed-loop communication allows team members the opportunity to verify and validate the exchange of information. By repeating back information, members confirm the exchange has occurred, understanding is clear, and expectations are heard.
Closed-loop communication should also be used when the RN is receiving a verbal order from a provider. For example, when the resuscitation team leader gives a verbal order of “Epinephrine 1 mg/mL IV push now,” the RN confirms correct understanding of the order by repeating back, “I will prepare Epinephrine 1 mg/mL to be given IV push now.” After the provider confirms the verbal order and the task is completed, the nurse confirms completion of the task by stating, “Epinephrine 1 mg/mL IV push was administered.”
In addition to using closed-loop communication, a common format used by health care team members to exchange client information is ISBARR, a mnemonic for the components of Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat Back. ISBARR and other communication strategies are discussed in more detail in the "Interprofessional Communication" section of the "Collaboration Within the Interprofessional Team" chapter.
Nursing team members working in inpatient or long-term care settings receive patient assignments at the start of their shift. Assignment refers to routine care, activities, and procedures that are within the legal scope of practice of registered nurses (RN), licensed practical/vocational nurses (LPN/VN), or assistive personnel (AP).[10] Scope of practice for RNs and LPNs is described in each state's Nurse Practice Act. Care tasks for AP vary by state; regulations are typically listed on sites for the state's Board of Nursing, Department of Health, Department of Aging, Department of Health Professions, Department of Commerce, or Office of Long-Term Care.[11]
See Table 3.3a for common tasks performed by members of the nursing team based on their scope of practice. These tasks are within the traditional role and training the team member has acquired through a basic educational program. They are also within the expectations of the health care agency during a shift of work. Agency policy can be more restrictive than federal or state regulations, but it cannot be less restrictive.
Patient assignments are typically made by the charge nurse (or nurse supervisor) from the previous shift. A charge nurse is an RN who provides leadership on a patient-care unit within a health care facility during their shift. Charge nurses perform many of the tasks that general nurses do, but also have some supervisory duties such as making assignments, delegating tasks, preparing schedules, monitoring admissions and discharges, and serving as a staff member resource.[12]
Table 3.3a. Nursing Team Members’ Scope of Practice and Common Tasks[13]
| Nursing Team Member | Scope of Practice | Common Tasks
|
|---|---|---|
| RN |
|
|
| LPN/VN |
|
Tasks That Potentially Can Be Delegated According to the Five Rights of Delegation:
|
| AP |
|
|
An example of a patient assignment is when an RN assigns an LPN/VN to care for a client with stable heart failure. The LPN/VN collects assessment data, monitors intake/output throughout the shift, and administers routine oral medication. The LPN/VN documents this information and reports information back to the RN. This is considered the LPN/VN’s “assignment” because the skills are taught within an LPN educational program and are consistent with the state’s Nurse Practice Act for LPN/VN scope of practice. They are also included in the unit’s job description for an LPN/VN. The RN may also assign some care for this client to AP. These tasks may include assistance with personal hygiene, toileting, and ambulation. The AP documents these tasks as they are completed and reports information back to the RN or LPN/VN. These tasks are considered the AP’s assignment because they are taught within a nursing aide's educational program, are consistent with the AP's scope of practice for that state, and are included in the job description for the nursing aide's role in this unit. The RN continues to be accountable for the care provided to this client despite the assignments made to other nursing team members.
Special consideration is required for AP with additional training. With increased staffing needs, skills such as administering medications, inserting Foley catheters, or performing injections are included in specialized training programs for AP. Due to the impact these skills can have on the outcome and safety of the client, the National Council of State Board of Nursing (NCSBN) recommends these activities be considered delegated tasks by the RN or nurse leader. By delegating these advanced skills when appropriate, the nurse validates competency, provides supervision, and maintains accountability for client outcomes. Read more about delegation in the “Delegation” section of this chapter.
When making assignments to other nursing team members, it is essential for the RN to keep in mind specific tasks that cannot be delegated to other nursing team members based on federal and/or state regulations. These tasks include, but are not limited to, those tasks described in Table 3.3b.
Table 3.3b. Examples of Tasks Outside the Scope of Practice of Nursing Assistive Personnel
| Nursing Team Member | Tasks That Cannot Be Delegated
|
|---|---|
| LPN/VN |
|
| Assistive Personnel (AP) |
|
As always, refer to each state’s Nurse Practice Act and other state regulations for specific details about nursing team members’ scope of practice when providing care in that state.
Find and review Nurse Practice Acts by state at https://www.ncsbn.org/policy/npa.page.
Read more about the Wisconsin's Nurse Practice Act and the standards and scope of practice for RNs and LPNs at Wisconsin's Legislative Code Chapter N6.
Read more about scope of practice, skills, and practices of nurse aides in Wisconsin at DHS 129.07 Standards for Nurse Aide Training Programs.
There has been significant national debate over the difference between assignment and delegation over the past few decades. In 2019 the National Council of State Boards of Nursing (NCSBN) and the American Nurses Association (ANA) published updated joint National Guidelines on Nursing Delegation (NGND).[15] These guidelines apply to all levels of nursing licensure (advanced practice registered nurses [APRN], registered nurses [RN], and licensed practical/vocational nurses [LPN/VN]) when delegating when there is no specific guidance provided by the state’s Nurse Practice Act (NPA).[16] It is important to note that states have different laws and rules/regulations regarding delegation, so it is the responsibility of all licensed nurses to know what is permitted in their jurisdiction.
The NGND defines a delegatee as an RN, LPN/VN, or AP who is delegated a nursing responsibility by either an APRN, RN, or LPN/VN, is competent to perform the task, and verbally accepts the responsibility.[17] Delegation is allowing a delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role and not routinely performed, but the individual has obtained additional training and validated their competence to perform the delegated responsibility.[18] However, the licensed nurse still maintains accountability for overall client care. Delegated responsibility is a nursing activity, skill, or procedure that is transferred from a licensed nurse to a delegatee.[19] Accountability is defined as being answerable to oneself and others for one’s own choices, decisions, and actions as measured against a standard. Therefore, if a nurse does not feel it is appropriate to delegate a certain responsibility to a delegatee, the delegating nurse should perform the activity themselves.[20]
Delegation is summarized in the NGND as the following[21]:
- A delegatee is allowed to perform a specific nursing activity, skill, or procedure that is outside the traditional role and basic responsibilities of the delegatee’s current job.
- The delegatee has obtained the additional education and training and validated competence to perform the care/delegated responsibility. The context and processes associated with competency validation will be different for each activity, skill, or procedure being delegated. Competency validation should be specific to the knowledge and skill needed to safely perform the delegated responsibility, as well as to the level of the practitioner (e.g., RN, LPN/VN, AP) to whom the activity, skill, or procedure has been delegated. The licensed nurse who delegates the “responsibility” maintains overall accountability for the client, but the delegatee bears the responsibility for completing the delegated activity, skill, or procedure.
- The licensed nurse cannot delegate nursing clinical judgment or any activity that will involve nursing clinical judgment or critical decision-making to AP.
- Nursing responsibilities are delegated by a licensed nurse who has the authority to delegate and the delegated responsibility is within the delegator’s scope of practice.
An example of delegation is medication administration that is delegated by a licensed nurse to AP with additional training in some agencies, according to agency policy. This task is outside the traditional role of AP, but the delegatee has received additional training for this delegated responsibility and has completed competency validation in completing this task accurately.
An example illustrating the difference between assignment and delegation is assisting patients with eating. Feeding patients is typically part of the routine role of AP. However, if a client has recently experienced a stroke (i.e., cerebrovascular accident) or is otherwise experiencing swallowing difficulties (e.g., dysphagia), this task cannot be assigned to AP because it is not considered routine care. Instead, the RN should perform this task themselves or delegate it to an AP who has received additional training on feeding assistance.
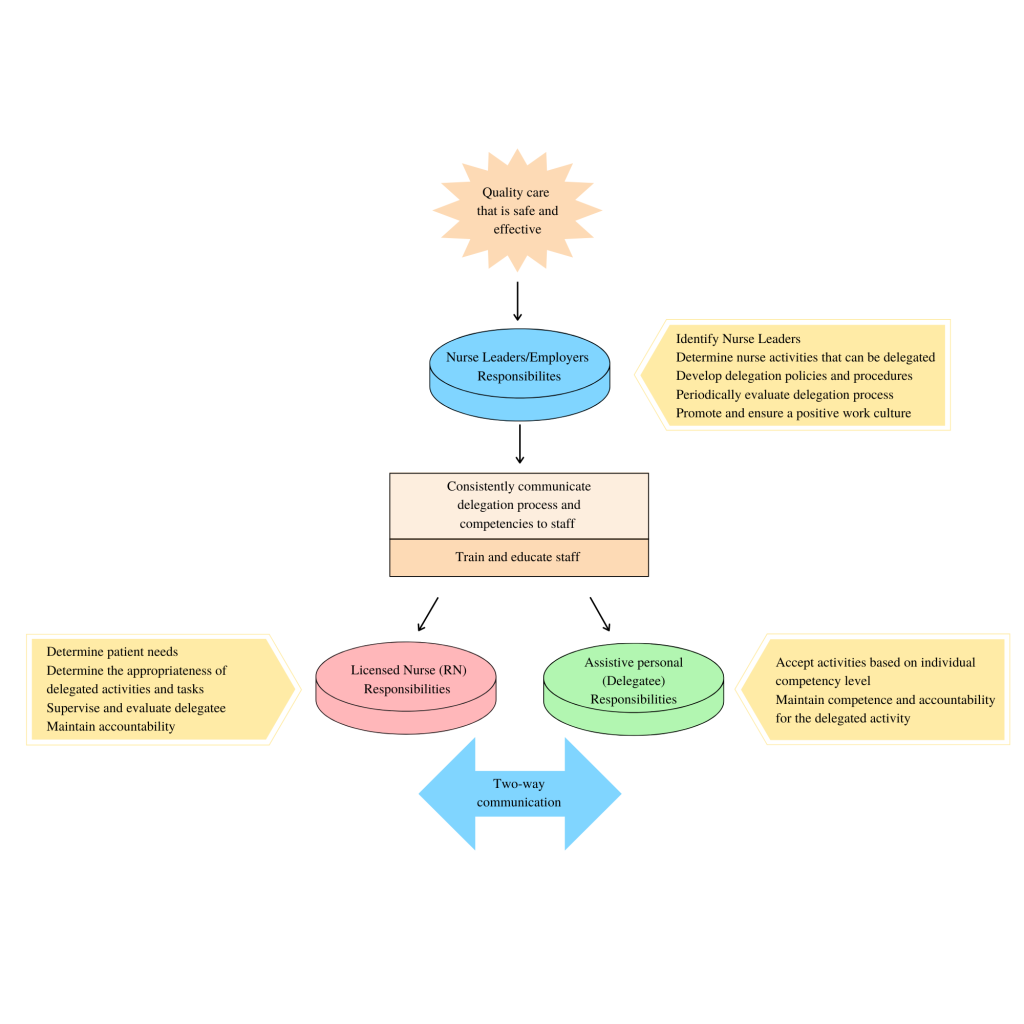
The delegation process is multifaceted. See Figure 3.2[22] for an illustration of the intersecting responsibilities of the employer/nurse leader, licensed nurse, and delegatee with two-way communication that protects the safety of the public. “Delegation begins at the administrative/nurse leader level of the organization and includes determining nursing responsibilities that can be delegated, to whom, and under what circumstances; developing delegation policies and procedures; periodically evaluating delegation processes; and promoting a positive culture/work environment. The licensed nurse is responsible for determining client needs and when to delegate, ensuring availability to the delegatee, evaluating outcomes, and maintaining accountability for delegated responsibility. Finally, the delegatee must accept activities based on their competency level, maintain competence for delegated responsibility, and maintain accountability for delegated activity.”[23]
Five Rights of Delegation
How does the RN determine what tasks can be delegated, when, and to whom? According to the National Council of State Boards of Nursing (NCSBN), RNs should use the five rights of delegation to ensure proper and appropriate delegation: right task, right circumstance, right person, right directions and communication, and right supervision and evaluation[24]:
- Right task: The activity falls within the delegatee’s job description or is included as part of the established policies and procedures of the nursing practice setting. The facility needs to ensure the policies and procedures describe the expectations and limits of the activity and provide any necessary competency training.
- Right circumstance: The health condition of the client must be stable. If the client’s condition changes, the delegatee must communicate this to the licensed nurse, and the licensed nurse must reassess the situation and the appropriateness of the delegation.[25]
- Right person: The licensed nurse, along with the employer and the delegatee, is responsible for ensuring that the delegatee possesses the appropriate skills and knowledge to perform the activity.[26]
- Right directions and communication: Each delegation situation should be specific to the client, the nurse, and the delegatee. The licensed nurse is expected to communicate specific instructions for the delegated activity to the delegatee; the delegatee, as part of two-way communication, should ask any clarifying questions. This communication includes any data that need to be collected, the method for collecting the data, the time frame for reporting the results to the licensed nurse, and additional information pertinent to the situation. The delegatee must understand the terms of the delegation and must agree to accept the delegated activity. The licensed nurse should ensure the delegatee understands they cannot make any decisions or modifications in carrying out the activity without first consulting the licensed nurse.[27]
- Right supervision and evaluation: The licensed nurse is responsible for monitoring the delegated activity, following up with the delegatee at the completion of the activity, and evaluating client outcomes. The delegatee is responsible for communicating client information to the licensed nurse during the delegation situation. The licensed nurse should be ready and available to intervene as necessary. The licensed nurse should ensure appropriate documentation of the activity is completed.[28]
Simply stated, the licensed nurse determines the right person is assigned the right tasks for the right clients under the right circumstances. When determining what aspects of care can be delegated, the licensed nurse uses clinical judgment while considering the client’s current clinical condition, as well as the abilities of the health care team member. The RN must also consider if the circumstances are appropriate for delegation. For example, although obtaining routine vital signs on stable clients may be appropriate to delegate to assistive personnel, obtaining vital signs on an unstable client is not appropriate to delegate.
After the decision has been made to delegate, the nurse assigning the tasks must communicate appropriately with the delegatee and provide the right directions and supervision. Communication is key to successful delegation. Clear, concise, and closed-loop communication is essential to ensure successful completion of the delegated task in a safe manner. During the final step of delegation, also referred to as supervision, the nurse verifies and evaluates that the task was performed correctly, appropriately, safely, and competently. Read more about supervision in the following section on “Supervision.” See Table 3.4 for additional questions to consider for each “right” of delegation.
Table 3.4. Rights of Delegation[29]
| Rights of Delegation | Description | Questions to Consider When Delegating |
|---|---|---|
| Right Task | A task that can be transferred to a member of the nursing team for a specific client. |
|
| Right Circumstances | The client is stable. |
|
| Right Person | The person delegating the task has the appropriate scope of practice to do so. The task is also appropriate for this delegatee’s skills and knowledge. |
|
| Right Directions and Communication | The task or activity is clearly defined and described. |
|
| Right Supervision and Evaluation | The RN appropriately monitors the delegated activity, evaluates client outcomes, and follows up with the delegatee at the completion of the activity. |
|
Keep in mind that any nursing intervention that requires specific nursing knowledge, clinical judgment, or use of the nursing process can only be delegated to another RN. Examples of these types of tasks include initial preoperative or admission assessments, client teaching, and creation and evaluation of a nursing care plan. See Figure 3.3[30] for an algorithm based on the 2019 National Guidelines for Nursing Delegation that can be used when deciding if a nursing task can be delegated.[31]
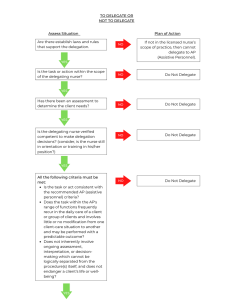
Responsibilities of the Licensed Nurse
The licensed nurse has several responsibilities as part of the delegation process. According to the NGND, any decision to delegate a nursing responsibility must be based on the needs of the client or population, the stability and predictability of the client’s condition, the documented training and competence of the delegatee, and the ability of the licensed nurse to supervise the delegated responsibility and its outcome with consideration to the available staff mix and client acuity. Additionally, the licensed nurse must consider the state Nurse Practice Act regarding delegation and the employer’s policies and procedures prior to making a final decision to delegate. Licensed nurses must be aware that delegation is at the nurse’s discretion, with consideration of the particular situation. The licensed nurse maintains accountability for the client, while the delegatee is responsible for the delegated activity, skill, or procedure. If, under the circumstances, a nurse does not feel it is appropriate to delegate a certain responsibility to a delegatee, the delegating nurse should perform the activity.[32]
1. The licensed nurse must determine when and what to delegate based on the practice setting, the client’s needs and condition, the state's/jurisdiction’s provisions for delegation, and the employer’s policies and procedures regarding delegating a specific responsibility. The licensed nurse must determine the needs of the client and whether those needs are matched by the knowledge, skills, and abilities of the delegatee and can be performed safely by the delegatee. The licensed nurse cannot delegate any activity that requires clinical reasoning, nursing judgment, or critical decision-making. The licensed nurse must ultimately make the final decision whether an activity is appropriate to delegate to the delegatee based on the “Five Rights of Delegation.”
- Rationale: The licensed nurse, who is present at the point of care, is in the best position to assess the needs of the client and what can or cannot be delegated in specific situations.[33]
2. The licensed nurse must communicate with the delegatee who will be assisting in providing client care. This should include reviewing the delegatee’s assignment and discussing delegated responsibilities, including information on the client’s condition/stability, any specific information pertaining to a certain client (e.g., no blood draws in the right arm), and any specific information about the client’s condition that should be communicated back to the licensed nurse by the delegatee.
- Rationale: Communication must be a two-way process involving both the licensed nurse delegating the activity and the delegatee being delegated the responsibility. Evidence shows that the better the communication between the nurse and the delegatee, the more optimal the outcome. The licensed nurse must provide information about the client and care requirements. This includes any specific issues related to any delegated responsibilities. These instructions should include any unique client requirements. The licensed nurse must instruct the delegatee to regularly communicate the status of the client.[34]
3. The licensed nurse must be available to the delegatee for guidance and questions, including assisting with the delegated responsibility, if necessary, or performing it themselves if the client’s condition or other circumstances warrant doing so.
- Rationale: Delegation calls for nursing judgment throughout the process. The final decision to delegate rests in the hands of the licensed nurse as they have overall accountability for the client.[35]
4. The licensed nurse must follow up with the delegatee and the client after the delegated responsibility has been completed.
- Rationale: The licensed nurse who delegates the “responsibility” maintains overall accountability for the client, while the delegatee is responsible for the delegated activity, skill, or procedure.[36]
5. The licensed nurse must provide feedback information about the delegation process and any issues regarding delegatee competence level to the nurse leader. Licensed nurses in the facility need to communicate to the nurse leader responsible for delegation any issues arising related to delegation and any individual whom they identify as not being competent in a specific responsibility or unable to use good judgment and decision-making.
- Rationale: This will allow the nurse leader responsible for delegation to develop a plan to address the situation.[37]
The decision of whether or not to delegate or assign is based on the RN’s judgment concerning the condition of the client, the competence of the nursing team member, and the degree of supervision that will be required of the RN if a task is delegated.[38]
Responsibilities of the Delegatee
Everyone is responsible for the well-being of clients. While the nurse is ultimately accountable for the overall care provided to a client, the delegatee shares the responsibility for the client and is fully responsible for the delegated activity, skill, or procedure.[39] The delegatee has the following responsibilities:
1. The delegatee must accept only the delegated responsibilities that they are appropriately trained and educated to perform and feel comfortable doing given the specific circumstances in the health care setting and client’s condition. The delegatee should confirm acceptance of the responsibility to carry out the delegated activity. If the delegatee does not believe they have the appropriate competency to complete the delegated responsibility, then the delegatee should not accept the delegated responsibility. This includes informing the nursing leadership if they do not feel they have received adequate training to perform the delegated responsibility, do not perform the procedure frequently enough to do it safely, or their knowledge and skills need updating.
- Rationale: The delegatee shares the responsibility to keep clients safe, and this includes only performing activities, skills, or procedures in which they are competent and comfortable doing.[40]
2. The delegatee must maintain competency for the delegated responsibility.
- Rationale: Competency is an ongoing process. Even if properly taught, the delegatee may become less competent if they do not frequently perform the procedure. Given that the delegatee shares the responsibility for the client, the delegatee also has a responsibility to maintain competency.[41]
3. The delegatee must communicate with the licensed nurse in charge of the client. This includes any questions related to the delegated responsibility and follow-up on any unusual incidents that may have occurred while the delegatee was performing the delegated responsibility, any concerns about a client’s condition, and any other information important to the client’s care.
- Rationale: The delegatee is a partner in providing client care. They are interacting with the client/family and caring for the client. This information and two-way communication are important for successful delegation and optimal outcomes for the client.[42]
4. Once the delegatee verifies acceptance of the delegated responsibility, the delegatee is accountable for carrying out the delegated responsibility correctly and completing timely and accurate documentation per facility policy.
- Rationale: The delegatee cannot delegate to another individual. If the delegatee is unable to complete the responsibility or feels as though they need assistance, the delegatee should inform the licensed nurse immediately so the licensed nurse can assess the situation and provide support. Only the licensed nurse can determine if it is appropriate to delegate the activity to another individual. If at any time the licensed nurse determines they need to perform the delegated responsibility, the delegatee must relinquish responsibility upon request of the licensed nurse.[43]
Responsibilities of the Employer/Nurse Leader
The employer and nurse leaders also have responsibilities related to safe delegation of client care:
1. The employer must identify a nurse leader responsible for oversight of delegated responsibilities for the facility. If there is only one licensed nurse within the practice setting, that licensed nurse must be responsible for oversight of delegated responsibilities for the facility.
- Rationale: The nurse leader has the ability to assess the needs of the facility, understand the type of knowledge and skill needed to perform a specific nursing responsibility, and be accountable for maintaining a safe environment for clients. They are also aware of the knowledge, skill level, and limitations of the licensed nurses and AP. Additionally, the nurse leader is positioned to develop appropriate staffing models that take into consideration the need for delegation. Therefore, the decision to delegate begins with a thorough assessment by a nurse leader designated by the institution to oversee the process.[44]
2. The designated nurse leader responsible for delegation, ideally with a committee (consisting of other nurse leaders) formed for the purposes of addressing delegation, must determine which nursing responsibilities may be delegated, to whom, and under what circumstances. The nurse leader must be aware of the state Nurse Practice Act and the laws/rules and regulations that affect the delegation process and ensure all institutional policies are in accordance with the law.
- Rationale: A systematic approach to the delegation process fosters communication and consistency of the process throughout the facility.[45]
3. Policies and procedures for delegation must be developed. The employer/nurse leader must outline specific responsibilities that can be delegated and to whom these responsibilities can be delegated. The policies and procedures should also indicate what may not be delegated. The employer must periodically review the policies and procedures for delegation to ensure they remain consistent with current nursing practice trends and that they are consistent with the state Nurse Practice Act. (Institution/employer policies can be more restrictive, but not less restrictive.)
- Rationale: Policies and procedures standardize the appropriate method of care and ensure safe practices. Having a policy and procedure specific to delegation and delegated responsibilities eliminates questions from licensed nurses and AP about what can be delegated and how they should be performed.[46]
4. The employer/nurse leader must communicate information about delegation to the licensed nurses and AP and educate them about what responsibilities can be delegated. This information should include the competencies of delegatees who can safely perform a specific nursing responsibility.
- Rationale: Licensed nurses must be aware of the competence level of staff and expectations for delegation (as described within the policies and procedures) to make informed decisions on whether or not delegation is appropriate for the given situahttps://www.nursingworld.org/content-hub/resources/nursing-leadership/delegation-in-nursing/tion. Licensed nurses maintain accountability for the client. However, the delegatee has responsibility for the delegated activity, skill, or procedure.
In summary, delegation is the transfer of the nurse’s responsibility for a task while retaining professional accountability for the client’s overall outcome. The decision to delegate is based on the nurse’s judgment, the act of delegation must be clearly defined by the nurse, and the outcomes of delegation are an extension of the nurse’s guidance and supervision. Delegation, when rooted in mutual respect and trust, is a key component to an effective health care team.
Delegation is an integral skill in the nursing profession to help manage the complexities of the dynamic and ever-changing health care environment. Delegation in nursing has been found to increase employee empowerment, decrease burnout, increase role commitment, and improve job satisfaction.[47] Cultivating delegation skills helps nurses better manage the complexities of their client care role, ensuring that their clients are safely cared for and outcomes are optimized. Delegation skills, like other nursing skills, require purposeful development and do not necessarily come easily when first transitioning into the nursing role. It is important that the new graduate nurse does not mistake delegation for pompous or arrogant behavior. Delegation requires mutual respect between the delegator and delegatee. Delegation is not seen as a sign or weakness and does not reflect one's desire to shirk their work responsibilities. Instead, delegation reflects strong leadership and organizational skills in which the nurse leader demonstrates that they understand how to leverage their team's strengths in order to achieve optimal care outcomes.
To help avoid any perception of arrogance in the delegation of an activity, it is important that the new graduate nurse approaches the task of delegation with humility. Clarity in the communication of the delegated responsibility is critical, and the rationale behind the delegation should be communicated to the delegatee. Within the task of delegation, the delegator should express appreciation for the delegatee and their contributions in the collaborative health care environment. Additionally, it is important to understand that no specific nurse delegated task is outside of the "nurse" role. For example, ambulating a client does not to an unlicensed assistive personnel simply because that individual is able to perform that task. Rather, nurses must be willing to perform delegated tasks themselves when necessary. This reflects a team-oriented mindset and helps to reinforce among the care team that all roles are critical to optimizing client care. For new graduate nurses who first transition into a specific health care setting, having the opportunity to shadow individuals in various work roles helps to foster a team mindset. Asking questions of various team members regarding their work role can help a new graduate nurse demonstrate respect and value for other roles.
Examples of helpful questions may include the following:
- "What is the biggest challenge in your typical workday?"
- "What do you most enjoy about your job?"
- "How is it best to communicate with you when the unit is busy?"
- "What do you think people misunderstand most about your role?"
It is important to ensure that the team understands that care is optimized when they function as one collective unit and not in siloed roles. Each team member must feel valued and competent in their role. By understanding and practicing strategic delegation, new graduate nurses can overcome any misconceptions of arrogance and contribute positively to the healthcare team.
Please review the example below to consider variation in approach to task delegation.
Scenario A: Nurse June, a newly graduated nurse, is working in a busy hospital unit. She needs an unlicensed assistive personnel (UAP), Alex, to take vital signs of a patient. Nurse June approaches Alex in the hallway and says in an abrupt tone, "Alex, I need you to take Mr. Smith's vital signs right now. I'm too busy to do it myself, and besides, that's what you're here for. Just get it done quickly."
Analysis: June’s tone and words suggest she sees Alex's role as less important and purely as a means to offload her tasks. June does not explain the urgency or importance of the task. June doesn’t acknowledge Alex's effort or capability, making the request seem like a command rather than a collaborative effort.
Scenario B: Nurse June, a newly graduated nurse, is working in a busy hospital unit. She needs an unlicensed assistive personnel (UAP), Alex, to take vital signs of a patient. Nurse June approaches Alex and says, "Hi Alex, could you please help me by taking Mr. Smith's vital signs? I'm handling a few urgent matters right now, and it would really help to have your support. I know you’re great at this, and your thoroughness really makes a difference in our patient care. Thank you so much!"
Analysis: June speaks to Alex with courtesy and acknowledges the value of his role. June clearly explains why she needs Alex's help and the importance of the task. June acknowledges Alex’s competence and expresses gratitude, fostering feelings of value and respect.
The licensed nurse has the responsibility to supervise, monitor, and evaluate the nursing team members who have received delegated tasks, activities, or procedures. As previously noted, the act of supervision requires the nurse to assess the staff member’s ability, competency, and experience prior to delegating. After the nurse has made the decision to delegate, supervision continues in terms of coaching, supporting, assisting, and educating as needed throughout the task to assure appropriate care is provided.
The nurse is accountable for client care delegated to other team members. Communication and supervision should be ongoing processes throughout the shift within the nursing care team. The nurse must ensure quality of care, appropriateness, timeliness, and completeness through direct and indirect supervision. For example, an RN may directly observe the AP reposition a client or assist them to the bathroom to assure both client and staff safety are maintained. An RN may also indirectly evaluate an LPN’s administration of medication by reviewing documentation in the client’s medical record for timeliness and accuracy. Through direct and indirect supervision of delegation, quality client care and compliance with standards of practice and facility policies can be assured.
Supervision also includes providing constructive feedback to the nursing team member. Constructive feedback is supportive and identifies solutions to areas needing improvement. It is provided with positive intentions to address specific issues or concerns as the person learns and grows in their role. Constructive feedback includes several key points:
- Was the task, activity, care, or procedure performed correctly?
- Were the expected outcomes involving delegation for that client achieved?
- Did the team member utilize effective and timely communication?
- What were the challenges of the activity and what aspects went well?
- Were there any problems or specific concerns that occurred and how were they managed?
After these questions have been addressed, the RN creates a plan for future delegation with the nursing team member. This plan typically includes the following:
- Recognizing difficulty of the nursing team member in initiating or completing the delegated activities.
- Observing the client’s responses to actions performed by the nursing team member.
- Following up in a timely manner on any problems, incidents, or concerns that arose.
- Creating a plan for providing additional training and monitoring outcomes of future delegated tasks, activities, or procedures.
- Consulting with appropriate nursing administrators per agency policy if the client’s safety was compromised.
Please review the following example regarding constructive feedback and task supervision
Nurse Sarah, an experienced RN, delegated a task to Peter, an unlicensed assistive personnel (UAP), to take the vital signs of a post-operative patient, Mrs. Johnson, and report any abnormalities immediately.
Sarah: "Hi Peter, I wanted to discuss the task you completed earlier with Mrs. Johnson's vital signs. Thank you for your help with that. Let’s review how it went."
Was the task, activity, care, or procedure performed correctly?
Sarah: "First, I noticed you recorded the vital signs accurately. Good job on that. However, there was a delay in reporting Mrs. Johnson's elevated blood pressure to me. Can you walk me through what happened?"
Peter: "I took her vital signs, and her blood pressure was high. I was going to inform you, but I got called to assist with another patient immediately after."
Were the expected outcomes involving delegation for that client achieved?
Sarah: "Ultimately, we did address the elevated blood pressure, but the delay could have impacted her care. It's crucial to report such abnormalities immediately."
Did the team member utilize effective and timely communication?
Sarah: "While you communicated the vital signs correctly, the timing was off. In future, if you can't find me immediately, please inform any available nurse or use the intercom system."
What were the challenges of the activity and what aspects went well?
Peter: "The challenge was managing multiple tasks at once. I did feel confident in taking and recording the vital signs accurately, though."
Sarah: "It sounds like you’re balancing a lot of responsibilities well, but prioritizing urgent communications is key. You handled the technical part perfectly."
Were there any problems or specific concerns that occurred and how were they managed?
Sarah: "The main concern was the delay in reporting the elevated blood pressure. Fortunately, there were no serious consequences, but it’s a potential risk we need to manage better. Let’s create a plan to support you moving forward."
Recognizing difficulty of the nursing team member in initiating or completing the delegated activities:
Sarah: "I recognize that you were busy with multiple tasks. It’s important to prioritize patient safety over other duties."
Observing the client’s responses to actions performed by the nursing team member:
Sarah: "I will check on Mrs. Johnson's response to ensure there are no ongoing issues, and I’ll keep exploring how we can improve this process."
Following up in a timely manner on any problems, incidents, or concerns that arose:
Sarah: "I’ll follow up with you soon to see how you’re managing your other tasks, and we can address any challenges you’re facing."
Creating a plan for providing additional training and monitoring outcomes of future delegated tasks, activities, or procedures:
Sarah: "We’ll arrange some additional training on prioritizing tasks and urgent communication. Let's monitor the outcomes of your delegated tasks over the next few weeks to ensure you’re supported."
Consulting with appropriate nursing administrators per agency policy if the client’s safety was compromised:
Sarah: "Fortunately, Mrs. Johnson is fine, but if there were any safety concerns, we’d need to report it according to our policy. Keep this in mind for the future."
Sarah: "Peter, you're doing a great job with your responsibilities, and with a bit more focus on communication priorities, I’m confident you’ll excel even more. Let’s touch base again in a week to see how things are going. Feel free to come to me with any questions or concerns in the meantime."
Peter: "Thank you, Sarah. I appreciate the feedback and will work on prioritizing urgent communications."
Sarah: "Great. Keep up the good work, and let’s keep improving together."
Organizational Culture
The formal leaders of an organization provide a sense of direction and overall guidance for their employees by establishing organizational vision, mission, and values statements. An organization’s vision statement defines why the organization exists, describes how the organization is unique from similar organizations, and specifies what the organization is striving to be. The mission statement describes how the organization will fulfill its vision and establishes a common course of action for future endeavors. See Figure 4.1[48] for an illustration of a mission statement. A values statement establishes the values of an organization that assist with the achievement of its vision and mission. A values statement also provides strategic guidelines for decision-making, both internally and externally, by members of the organization. A values statement may also be reflected as the organization's "core values," which are the foundational ideals that guide the organization's actions and decision-making processes. The vision, mission, and values statements are expressed in a concise and clear manner that is easily understood by members of the organization and the public.[49]

Organizational culture refers to the implicit values and beliefs that reflect the norms and traditions of an organization. An organization’s vision, mission, and values statements are the foundation of organizational culture. Because individual organizations have their own vision, mission, and values statements, each organization has a different culture.[50] Organizational culture helps reflect the expected norms and behaviors that are inherent to an organization. Expected conduct is comprised of the unwritten rules and standards that reflect how employees should behave in different situations. The culture also informs the common communication styles that are inherent to an organization, including both formal and informal channels. The culture may also be manifested outwardly through various symbols and artifacts that embedded within the organization. These may include specific logos, objects, or other physical manifestations of elements that represent the organization's culture. Some organizations may also reflect their cultural values through activities or ceremonies held within the community.
As health care continues to evolve and new models of care are introduced, nursing managers must develop innovative approaches that address change while aligning with that organization’s vision, mission, and values. Leaders embrace the organization’s mission, identify how individuals’ work contributes to it, and ensure that outcomes advance the organization’s mission and purpose. Leaders use vision, mission, and values statements for guidance when determining appropriate responses to critical events and unforeseen challenges that are common in a complex health care system. Successful organizations require employees to be committed to following these strategic guidelines during the course of their work activities. Employees who understand the relationship between their own work and the mission and purpose of the organization will contribute to a stronger health care system that excels in providing first-class patient care. The vision, mission, and values provide a common organization-wide frame of reference for decision-making for both leaders and staff.[51] It is important for employees in health care organizations to have understanding of how their roles and responsibilities connect to the broader mission and vision of the organization. This alignment fosters a cohesive work environment where each staff member is motivated by a shared purpose, leading to more effective and high-quality patient care. It is important that both the leader and employee have clarity in the underlying vision, mission, and values of an organization. This involves responsibility for both the leader and employee. Leaders must articulate the organization's vision, mission, and values clearly and consistently. This involves regular communication through meetings, written materials, etc. Employees share in the responsibility by being empowered to ask questions and seek clarification on how their daily tasks contribute to the organization's overarching goals.
Learning Activity
Investigate the mission, vision, and values of a potential employer, as you would do prior to an interview for a job position.
Reflective Questions
- How well do the organization’s vision and values align with your personal values regarding health care?
- How well does the organization’s mission align with your professional objective in your resume?
Followership
Followership is described as the upward influence of individuals on their leaders and their teams. The actions of followers have an important influence on staff performance and patient outcomes. Being an effective follower requires individuals to contribute to the team not only by doing as they are told, but also by being aware and raising relevant concerns. Effective followers realize that they can initiate change and disagree or challenge their leaders if they feel their organization or unit is failing to promote wellness and deliver safe, value-driven, and compassionate care. Leaders who gain the trust and dedication of followers are more effective in their leadership role. Everybody has a voice and a responsibility to take ownership of the workplace culture, and good followership contributes to the establishment of high-functioning and safety-conscious teams.[52] Key elements of effective followership include proactive engagement, constructive communication, collaboration, advocacy, continuous improvement, and a supportive leadership environment.
In order to demonstrate proactive engagement, followers must also be initiators. Effective followers do not passively wait for instruction by rather take initiative to address issues, propose solutions, and contribute to ideas. They recognize the importance of their voice in engaging in problem-solving and understand that being an effective follower does not mean being passive in their role. Effective followers also employ a keen situational awareness where they maintain vigilant assessment of the environment and potential risks, ensuring that they act in the best interests of clients. They must be confident that they can raise concerns if they identify potential problems or unsafe practices. This reflects a culture where followers feels that their feedback is welcomed and valued. Effective followership also involves communication practices in which the message is clearly conveyed, measures to confirm the message are employed, and the confirmation is received. To be an effective follower, support of the team's goals must be a central tenet of one's work. Collaboration with others involves supporting colleagues and working together toward the common goal even when viewpoints may differ. Identifying strategies that create a respectful opportunity to debate and explore different opinions is important to effective followership. Additionally, followers must take accountability for their own actions while understanding how their role and performance impacts the function of the team, as well as client outcomes. Effective followers also practice ethical advocacy, ensuring that the needs of clients are prioritized and respected. This advocacy also involves the ability to courageously challenge any decisions or actions that may jeopardize care or organizational values. Finally, effective followers engage in continuous learning to enhance their skills and knowledge. They seek feedback and use the feedback to contribute to their own performance and also the growth of the team. Effective followership is further cultivated when leaders and followers come together with mutual respect, trust, and work with a purposeful drive toward shared goals that reflect the organization's mission.
Team members impact patient safety by following teamwork guidelines for good followership. For example, strategies such as closed-loop communication are important tools to promote patient safety.
Read more about communication and teamwork strategies in the “Collaboration Within the Interprofessional Team” chapter.
Leadership and Management Characteristics
Leadership and management are terms often used interchangeably, but they are two different concepts with many overlapping characteristics. Leadership is the art of establishing direction and influencing and motivating others to achieve their maximum potential to accomplish tasks, objectives, or projects.[53],[54] See Figure 4.2[55] for an illustration of team leadership. There is no universally accepted definition or theory of nursing leadership, but there is increasing clarity about how it differs from management.[56] Management refers to roles that focus on tasks such as planning, organizing, prioritizing, budgeting, staffing, coordinating, and reporting.[57] The overriding function of management has been described as providing order and consistency to organizations, whereas the primary function of leadership is to produce change and movement.[58] View a comparison of the characteristics of management and leadership in Table 4.2a.

Table 4.2a. Management and Leadership Characteristics[59]
| MANAGEMENT | LEADERSHIP |
|---|---|
Planning, Organizing, and Prioritizing
|
Establishing Direction
|
Budgeting and Staffing
|
Influencing Others
|
Coordinating and Problem-Solving
|
Motivating
|
Leader Vs. Manager Case Activity
Utilizing the information from the table above, review the following cases and identify whether the individual is serving as a leader or manager based upon the actions taken within the case scenario. Include supportive rationale for your decision regarding the role.
Case 1: Sima, the head nurse, reviews the upcoming schedule and allocates resources to ensure each shift is adequately staffed. She also makes assignments for the nursing staff based on their skills and patient needs. Additionally, she is responsible for hiring new staff and, when necessary, terminating employees who do not meet performance standards.
Case 2: Juan, a senior nurse, is passionate about improving patient care. He identifies an issue with the current handoff process between shifts and proposes a new strategy that incorporates evidence-based practices to enhance communication and reduce errors. He reaches out to his team at their monthly department meetings in order to develop a shared vision for this change and encourages them to partner with him on the new process.
Case 3: Maria, a unit supervisor, holds a meeting to set specific goals and time frames for the department’s upcoming projects. She prioritizes tasks for the team and establishes policies and procedures to ensure these tasks are completed efficiently and within the given deadlines.
Case 4: Emily, the nurse director, is tasked with preparing the budget for the upcoming fiscal year. She allocates resources effectively to ensure all departments are adequately funded. Emily also manages the staffing needs, ensuring that the hiring and termination processes are handled efficiently.
Case 5: Rachel, an experienced nurse, takes the time to build effective teamwork within her unit. She advocates for her patients, their families, and the nursing profession as a whole. Rachel communicates openly and listens to her team’s concerns, ensuring everyone feels valued and heard.
Not all nurses are managers, but all nurses are leaders because they encourage individuals to achieve their goals. The American Nurses Association (ANA) established Leadership as a Standard of Professional Performance for all registered nurses. Standards of Professional Performance are “authoritative statements of action and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently.”[60] See the competencies of the ANA Leadership standard in the following box and additional content in other chapters of this book.
Competencies of ANA’s Leadership Standard of Professional Performance
- Promotes effective relationships to achieve quality outcomes and a culture of safety
- Leads decision-making groups
- Engages in creating an interprofessional environment that promotes respect, trust, and integrity
- Embraces practice innovations and role performance to achieve lifelong personal and professional goals
- Communicates to lead change, influence others, and resolve conflict
- Implements evidence-based practices for safe, quality health care and health care consumer satisfaction
- Demonstrates authority, ownership, accountability, and responsibility for appropriate delegation of nursing care
- Mentors colleagues and others to embrace their knowledge, skills, and abilities
- Participates in professional activities and organizations for professional growth and influence
- Advocates for all aspects of human and environmental health in practice and policy
Read additional content related to leadership and management activities in corresponding chapters of this book:
- Read about the culture of safety in the “Legal Implications” chapter.
- Read about effective interprofessional teamwork and resolving conflict in the “Collaboration Within the Interprofessional Team” chapter.
- Read about quality improvement and implementing evidence-based practices in the “Quality and Evidence-Based Practice” chapter.
- Read more about delegation, supervision, and accountability in the “Delegation and Supervision” chapter.
- Read about professional organizations and advocating for patients, communities, and their environments in the “Advocacy” chapter.
- Read about budgets and staffing in the “Health Care Economics” chapter.
- Read about prioritization in the “Prioritization” chapter.
Leadership Theories and Styles
In the 1930s Kurt Lewin, the father of social psychology, originally identified three leadership styles: authoritarian, democratic, and laissez-faire.[61],[62]
Authoritarian leadership means the leader has full power. Authoritarian leaders tell team members what to do and expect team members to execute their plans. When fast decisions must be made in emergency situations, such as when a patient “codes,” the authoritarian leader makes quick decisions and provides the group with direct instructions. However, there are disadvantages to authoritarian leadership. Authoritarian leaders are more likely to disregard creative ideas of other team members, causing resentment and stress.[63]
Democratic leadership balances decision-making responsibility between team members and the leader. Democratic leaders actively participate in discussions, but also make sure to listen to the views of others. For example, a nurse supervisor may hold a meeting regarding an increased incidence of patient falls on the unit and ask team members to share their observations regarding causes and potential solutions. The democratic leadership style often leads to positive, inclusive, and collaborative work environments that encourage team members’ creativity. Under this style, the leader still retains responsibility for the final decision.[64]
Laissez-faire is a French word that translates to English as, “leave alone.” Laissez-faire leadership gives team members total freedom to perform as they please. Laissez-faire leaders do not participate in decision-making processes and rarely offer opinions. The laissez-faire leadership style can work well if team members are highly skilled and highly motivated to perform quality work. However, without the leader’s input, conflict and a culture of blame may occur as team members disagree on roles, responsibilities, and policies. By not contributing to the decision-making process, the leader forfeits control of team performance.[65]
Over the decades, Lewin’s original leadership styles have evolved into many styles of leadership in health care, such as passive-avoidant, transactional, transformational, servant, resonant, and authentic.[66],[67] Many of these leadership styles have overlapping characteristics. See Figure 4.3[68] for a comparison of various leadership styles in terms of engagement.

Passive-avoidant leadership is similar to laissez-faire leadership and is characterized by a leader who avoids taking responsibility and confronting others. Employees perceive the lack of control over the environment resulting from the absence of clear directives. Organizations with this type of leader have high staff turnover and low retention of employees. These types of leaders tend to react and take corrective action only after problems have become serious and often avoid making any decisions at all.[69]
Transactional leadership involves both the leader and the follower receiving something for their efforts; the leader gets the job done and the follower receives pay, recognition, rewards, or punishment based on how well they perform the tasks assigned to them.[70] Staff generally work independently with no focus on cooperation among employees or commitment to the organization.[71]
Transformational leadership involves leaders motivating followers to perform beyond expectations by creating a sense of ownership in reaching a shared vision.[72] It is characterized by a leader’s charismatic influence over team members and includes effective communication, valued relationships, and consideration of team member input. Transformational leaders know how to convey a sense of loyalty through shared goals, resulting in increased productivity, improved morale, and increased employees’ job satisfaction.[73] They often motivate others to do more than originally intended by inspiring them to look past individual self-interest and perform to promote team and organizational interests.[74]
Servant leadership focuses on the professional growth of employees while simultaneously promoting improved quality care through a combination of interprofessional teamwork and shared decision-making. Servant leaders assist team members to achieve their personal goals by listening with empathy and committing to individual growth and community-building. They share power, put the needs of others first, and help individuals optimize performance while forsaking their own personal advancement and rewards.[75]
Visit the Greenleaf Center site to learn more about What is Servant Leadership?
Resonant leaders are in tune with the emotions of those around them, use empathy, and manage their own emotions effectively. Resonant leaders build strong, trusting relationships and create a climate of optimism that inspires commitment even in the face of adversity. They create an environment where employees are highly engaged, making them willing and able to contribute with their full potential.[76]
Authentic leaders have an honest and direct approach with employees, demonstrating self-awareness, internalized moral perspective, and relationship transparency. They strive for trusting, symmetrical, and close leader–follower relationships; promote the open sharing of information; and consider others’ viewpoints.[77]
Table 4.2b. Characteristics of Leadership Styles
| Authoritarian | Democratic | Laissez-Faire or Passive-Avoidant |
|---|---|---|
|
|
|
| Transactional | Transformational | Servant |
|---|---|---|
|
|
|
| Resonant Leaders | Authentic Leaders |
|---|---|
|
|
Outcomes of Various Leadership Styles
Leadership styles affect team members, patient outcomes, and the organization. A systematic review of the literature published in 2021 showed significant correlations between leadership styles and nurses’ job satisfaction. Transformational leadership style had the greatest positive correlation with nurses’ job satisfaction, followed by authentic, resonant, and servant leadership styles. Passive-avoidant and laissez-faire leadership styles showed a negative correlation with nurses’ job satisfaction.[78] In this challenging health care environment, managers and nurse leaders must promote technical and professional competencies of their staff, but they must also act to improve staff satisfaction and morale by using appropriate leadership styles with their team.[79]
Systems Theory
Systems theory is based on the concept that systems do not function in isolation but rather there is an interdependence that exists between their parts. Systems theory assumes that most individuals strive to do good work but are affected by diverse influences within the system. Efficient and functional systems account for these diverse influences and improve outcomes by studying patterns and behaviors across the system.[80]
Many health care agencies have adopted a culture of safety based on systems theory. A culture of safety is an organizational culture that embraces error reporting by employees with the goal of identifying systemic causes of problems that can be addressed to improve patient safety. According to The Joint Commission, a culture of safety includes the following components[81]:
- Just Culture: A culture where people feel safe raising questions and concerns and report safety events in an environment that emphasizes a nonpunitive response to errors and near misses. Clear lines are drawn by managers between human error, at-risk, and reckless employee behaviors. See Figure 4.4[82] for an illustration of Just Culture.
- Reporting Culture: People realize errors are inevitable and are encouraged to speak up for patient safety by reporting errors and near misses. For example, nurses complete an “incident report” according to agency policy when a medication error occurs, or a client falls. Error reporting helps the agency manage risk and reduce potential liability.
- Learning Culture: People regularly collect information and learn from errors and successes while openly sharing data and information and applying best evidence to improve work processes and patient outcomes.
Just Culture
The American Nurses Association (ANA) officially endorses the Just Culture model. In 2019 the ANA published a position statement on Just Culture, stating, “Traditionally, healthcare’s culture has held individuals accountable for all errors or mishaps that befall patients under their care. By contrast, a Just Culture recognizes that individual practitioners should not be held accountable for system failings over which they have no control. A Just Culture also recognizes many individual or ‘active’ errors represent predictable interactions between human operators and the systems in which they work. However, in contrast to a culture that touts ‘no blame’ as its governing principle, a Just Culture does not tolerate conscious disregard of clear risks to patients or gross misconduct (e.g., falsifying a record or performing professional duties while intoxicated).”
The Just Culture model categorizes human behavior into three causes of errors. Consequences of errors are based on whether the error is a simple human error or caused by at-risk or reckless behavior.
- Simple human error: A simple human error occurs when an individual inadvertently does something other than what should have been done. Most medical errors are the result of human error due to poor processes, programs, education, environmental issues, or situations. These errors are managed by correcting the cause, looking at the process, and fixing the deviation. For example, a nurse appropriately checks the rights of medication administration three times, but due to the similar appearance and names of two different medications stored next to each other in the medication dispensing system, administers the incorrect medication to a patient. In this example, a root cause analysis reveals a system issue that must be modified to prevent future patient errors (e.g., change the labelling and storage of look alike-sound alike medication).
- At-risk behavior: An error due to at-risk behavior occurs when a behavioral choice is made that increases risk where the risk is not recognized or is mistakenly believed to be justified. For example, a nurse scans a patient’s medication with a barcode scanner prior to administration, but an error message appears on the scanner. The nurse mistakenly interprets the error to be a technology problem and proceeds to administer the medication instead of stopping the process and further investigating the error message, resulting in the wrong dosage of a medication being administered to the patient. In this case, ignoring the error message on the scanner can be considered “at-risk behavior” because the behavioral choice was considered justified by the nurse at the time.
- Reckless behavior: Reckless behavior is an error that occurs when an action is taken with conscious disregard for a substantial and unjustifiable risk.[83] For example, a nurse arrives at work intoxicated and administers the wrong medication to the wrong patient. This error is considered due to reckless behavior because the decision to arrive intoxicated was made with conscious disregard for substantial risk.
These examples show three different causes of medication errors that would result in different consequences to the employee based on the Just Culture model. Under the Just Culture model, after root cause analysis is completed, system-wide changes are made to decrease factors that contributed to the error. Managers appropriately hold individuals accountable for errors if they were due to simple human error, at-risk behavior, or reckless behaviors.
If an individual commits a simple human error, managers console the individual and consider changes in training, procedures, and processes. In the “simple human error” above, system-wide changes would be made to change the label and location of the medication to prevent future errors from occurring with the same medication.
Individuals committing at-risk behavior are held accountable for their behavioral choice and often require coaching with incentives for less risky behaviors and situational awareness. In the “at-risk behavior” example above where the nurse ignored an error message on the barcode scanner, mandatory training on using a barcode scanner and responding to errors would be implemented, and the manager would track the employee’s correct usage of the barcode scanner for several months following training.
If an individual demonstrates reckless behavior, remedial action and/or punitive action is taken.[84] In the “reckless behavior” example above, the manager would report the nurse’s behavior to the state's Board of Nursing with mandatory substance abuse counseling to maintain their nursing license. Employment may be terminated with consideration of patterns of behavior.
A Just Culture in which employees aren't afraid to report errors is a highly successful way to enhance patient safety, increase staff and patient satisfaction, and improve outcomes. Success is achieved through good communication, effective management of resources, and an openness to changing processes to ensure the safety of patients and employees. The infographic in Figure 4.4[85] illustrates the components of a culture of safety and Just Culture.
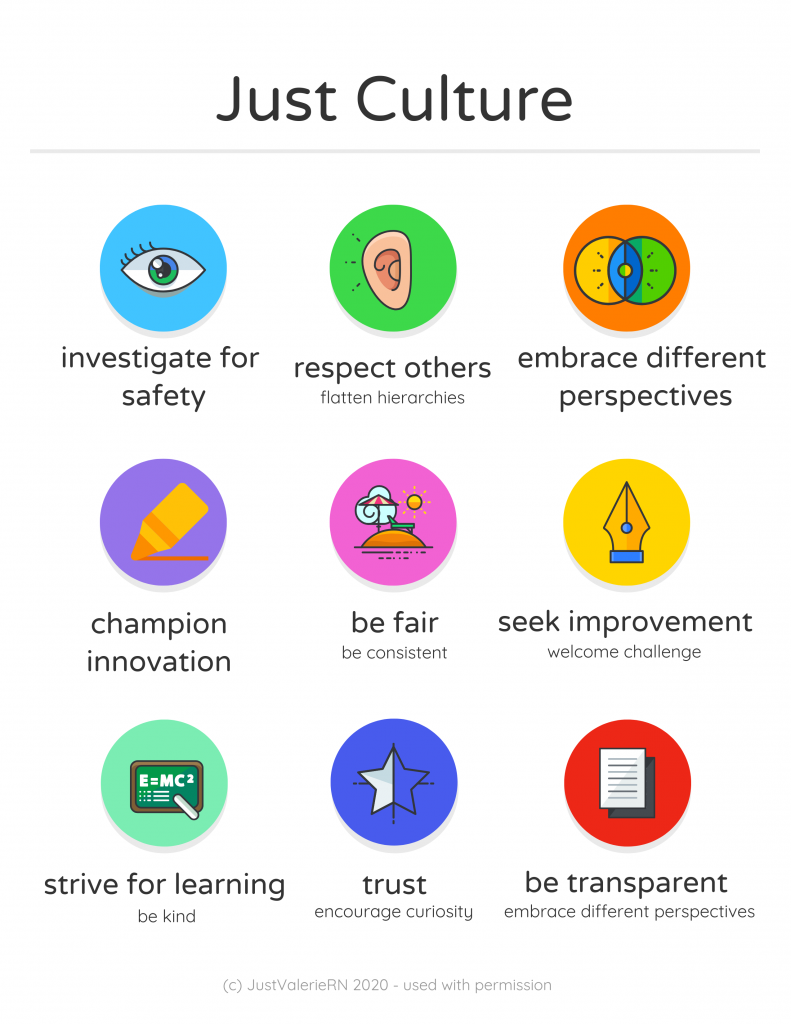
The principles of culture of safety, including Just Culture, Reporting Culture, and Learning Culture are also being adopted in nursing education. It’s understood that mistakes are part of learning and that a shared accountability model promotes individual- and system-level learning for improved patient safety. Under a shared accountability model, students are responsible for the following[86]:
- Being fully prepared for clinical experiences, including laboratory and simulation assignments
- Being rested and mentally ready for a challenging learning environment
- Accepting accountability for their part in contributing to a safe learning environment
- Behaving professionally
- Reporting their own errors and near mistakes
- Keeping up-to-date with current evidence-based practice
- Adhering to ethical and legal standards
Students know they will be held accountable for their actions but will not be blamed for system faults that lie beyond their control. They can trust that a fair process will be used to determine what went wrong if a patient care error or near miss occurs. Student errors and near misses are addressed based on an investigation determining if it was simple human error, an at-risk behavior, or reckless behavior. For example, a simple human error by a student can be addressed with coaching and additional learning opportunities to remedy the knowledge deficit. However, if a student acts with recklessness (for example, repeatedly arrives to clinical unprepared despite previous faculty feedback or falsely documents an assessment or procedure), they are appropriately and fairly disciplined, which may include dismissal from the program.[87]
See Table 4.2c describing classifications of errors using the Just Culture model.
Table 4.2c. Classification of Errors Using the Just Culture Model
| Human Error | At-Risk Behavior | Reckless Behavior |
|---|---|---|
| The caregiver made an error while working appropriately and focusing on the patient’s best interests. | The caregiver made a potentially unsafe choice resulting from faulty or self-serving decision-making. | The caregiver knowingly violated a rule and/or made a dangerous or unsafe choice. |
| Investigation reveals system factors contributing to similar errors by others with similar knowledge and skills. | Investigation reveals the system supports risky action and the caregiver requires coaching. | Investigation reveals the caregiver is accountable and needs retraining. |
| Manage by fixing system errors in processes, procedures, training, design, or environment. | Manage by coaching the caregiver and fixing any system issues:
|
Manage by disciplining the caregiver. If the system supports reckless behavior, it requires fixing. |
| CONSOLE | COACH | PUNISH |
Systems leadership refers to a set of skills used to catalyze, enable, and support the process of systems-level change that is encouraged by the Just Culture Model. Systems leadership is comprised of three interconnected elements:[88]
- The Individual: The skills of collaborative leadership to enable learning, trust-building, and empowered action among stakeholders who share a common goal
- The Community: The tactics of coalition building and advocacy to develop alignment and mobilize action among stakeholders in the system, both within and between organizations
- The System: An understanding of the complex systems shaping the challenge to be addressed
Just Culture Case Review
Review the following case descriptions. Identify the classification of error that has occurred and the recommended actions that should occur.
A chief nursing officer receives a daily report of organization incident reports and reviews the following incident:
Incident Description
Patient Mr. Joe Doden, Room 13067, Medical-Surgical floor
On the afternoon of May 15, 2024, Nurse Sarah was responsible for administering Mr. Joe Doden's insulin dose. The insulin vials used by the hospital had recently been redesigned by the manufacturer, which led to changes in the labeling. The patient was scheduled to receive ten units of regular insulin at 14:30. However, at 1450 the patient turns on his call light, reports feeling unwell. He is shaky, confused, and sweating profusely. The patient's glucose is checked, and he is found to be hypoglycemic. He is treated based upon the hypoglycemia protocol and recovers without further complication.
Case Investigation A
Action: Sarah RN who administered the insulin was following the protocol but mistakenly read the dosage due to a poorly designed label on the insulin vial. The nurse was focused on the patient’s best interests and followed all required steps.
Findings: The investigation revealed that the labeling on the insulin vials was confusing and had led to similar errors by other nurses in the past. The system's design flaw contributed significantly to the error.
How would you classify this error? What actions should be taken?
Case Investigation B
Action: Sarah RN, due to time pressure and a high patient load, decided to skip the double-check protocol for administering the same insulin dose, believing it would save time without causing harm.
Findings: The investigation revealed that the hospital’s workload and time pressures often led to shortcuts in following safety protocols.
How would you classify this error? What actions should be taken?
Case Investigation C
Action: Sarah RN, is familiar with the protocol and knowingly bypassed the double check system, dismissing its importance and administering a medication dose on her own.
Findings: The investigation found that the nurse had a history of disregarding safety protocols, showing a pattern of reckless behavior. This behavior was not supported by the hospital’s policies or environment.
How would you classify this error? What actions should be taken?
Change is constant in the health care environment. Change is defined as the process of altering or replacing existing knowledge, skills, attitudes, systems, policies, or procedures.[89] The outcomes of change must be consistent with an organization’s mission, vision, and values. Although change is a dynamic process that requires alterations in behavior and can cause conflict and resistance, change can also stimulate positive behaviors and attitudes and improve organizational outcomes and employee performance. Change can result from identified problems or from the incorporation of new knowledge, technology, management, or leadership. Problems may be identified from many sources, such as quality improvement initiatives, employee performance evaluations, or accreditation survey results.[90]
Nurse managers must deal with the fears and concerns triggered by change. They should recognize that change may not be easy and may be met with enthusiasm by some and resistance by others. Leaders should identify individuals who will be enthusiastic about the change (referred to as “early adopters”), as well as those who will be resisters (referred to as "laggers"). Early adopters should be involved to build momentum, and the concerns of resisters should be considered to identify barriers. Data should be collected, analyzed, and communicated so the need for change (and its projected consequences) can be clearly articulated. Managers should articulate the reasons for change, the way(s) the change will affect employees, the way(s) the change will benefit the organization, and the desired outcomes of the change process.[91] See Figure 4.5[92] for an illustration of communicating upcoming change.

Change Theories
There are several change theories that nurse leaders may adopt when implementing change. Two traditional change theories are known as Lewin’s Unfreeze-Change-Refreeze Model and Lippitt’s Seven-Step Change Theory.[93]
Lewin’s Change Model
Kurt Lewin, the father of social psychology, introduced the classic three-step model of change known as Unfreeze-Change-Refreeze Model that requires prior learning to be rejected and replaced. Lewin’s model has three major concepts: driving forces, restraining forces, and equilibrium. Driving forces are those that push in a direction and cause change to occur. They facilitate change because they push the person in a desired direction. They cause a shift in the equilibrium towards change. Restraining forces are those forces that counter the driving forces. They hinder change because they push the person in the opposite direction. They cause a shift in the equilibrium that opposes change. Equilibrium is a state of being where driving forces equal restraining forces, and no change occurs. It can be raised or lowered by changes that occur between the driving and restraining forces.[94],[95]
- Step 1: Unfreeze the status quo. Unfreezing is the process of altering behavior to agitate the equilibrium of the current state. This step is necessary if resistance is to be overcome and conformity achieved. Unfreezing can be achieved by increasing the driving forces that direct behavior away from the existing situation or status quo while decreasing the restraining forces that negatively affect the movement from the existing equilibrium. Nurse leaders can initiate activities that can assist in the unfreezing step, such as motivating participants by preparing them for change, building trust and recognition for the need to change, and encouraging active participation in recognizing problems and brainstorming solutions within a group.[96]
- Step 2: Change. Change is the process of moving to a new equilibrium. Nurse leaders can implement actions that assist in movement to a new equilibrium by persuading employees to agree that the status quo is not beneficial to them; encouraging them to view the problem from a fresh perspective; working together to search for new, relevant information; and connecting the views of the group to well-respected, powerful leaders who also support the change.[97]
- Step 3: Refreeze. Refreezing refers to attaining equilibrium with the newly desired behaviors. This step must take place after the change has been implemented for it to be sustained over time. If this step does not occur, it is very likely the change will be short-lived and employees will revert to the old equilibrium. Refreezing integrates new values into community values and traditions. Nursing leaders can reinforce new patterns of behavior and institutionalize them by adopting new policies and procedures.[98]
Example Using Lewin’s Change Theory
A new nurse working in a rural medical-surgical unit identifies that bedside handoff reports are not currently being used during shift reports.
Step 1: Unfreeze: The new nurse recognizes a change is needed for improved patient safety and discusses the concern with the nurse manager. Current evidence-based practice is shared regarding bedside handoff reports between shifts for patient safety.[99] The nurse manager initiates activities such as scheduling unit meetings to discuss evidence-based practice and the need to incorporate bedside handoff reports.
Step 2: Change: The nurse manager gains support from the director of nursing to implement organizational change and plans staff education about bedside report checklists and the manner in which they are performed.
Step 3: Refreeze: The nurse manager adopts bedside handoff reports in a new unit policy and monitors staff for effectiveness.
Lippitt’s Seven-Step Change Theory
Lippitt’s Seven-Step Change Theory expands on Lewin’s change theory by focusing on the role of the change agent. A change agent is anyone who has the skill and power to stimulate, facilitate, and coordinate the change effort. Change agents can be internal, such as nurse managers or employees appointed to oversee the change process, or external, such as an outside consulting firm. External change agents are not bound by organizational culture, politics, or traditions, so they bring a different perspective to the situation and challenge the status quo. However, this can also be a disadvantage because external change agents lack an understanding of the agency's history, operating procedures, and personnel.[100] The seven-step model includes the following steps[101]:
- Step 1: Diagnose the problem. Examine possible consequences, determine who will be affected by the change, identify essential management personnel who will be responsible for fixing the problem, collect data from those who will be affected by the change, and ensure those affected by the change will be committed to its success.
- Step 2: Evaluate motivation and capability for change. Identify financial and human resources capacity and organizational structure.
- Step 3: Assess the change agent’s motivation and resources, experience, stamina, and dedication.
- Step 4: Select progressive change objectives. Define the change process and develop action plans and accompanying strategies.
- Step 5: Explain the role of the change agent to all employees and ensure the expectations are clear.
- Step 6: Maintain change. Facilitate feedback, enhance communication, and coordinate the effects of change.
- Step 7: Gradually terminate the helping relationship of the change agent.
Example Using Lippitt’s Seven-Step Change Theory
Refer to the previous example of using Lewin’s change theory on a medical-surgical unit to implement bedside handoff reporting. The nurse manager expands on the Unfreeze-Change-Refreeze Model by implementing additional steps based on Lippitt’s Seven-Step Change Theory:
- The nurse manager collects data from team members affected by the changes and ensures their commitment to success.
- Early adopters are identified as change agents on the unit who are committed to improving patient safety by implementing evidence-based practices such as bedside handoff reporting.
- Action plans (including staff education and mentoring), timelines, and expectations are clearly communicated to team members as progressive change objectives. Early adopters are trained as “super-users” to provide staff education and mentor other nurses in using bedside handoff checklists across all shifts.
- The nurse manager facilitates feedback and encourages two-way communication about challenges as change is implemented on the unit. Positive reinforcement is provided as team members effectively incorporate change.
- Bedside handoff reporting is implemented as a unit policy, and all team members are held accountable for performing accurate bedside handoff reporting.
Read more about additional change theories in the Current Theories of Change Management pdf.
Change Management
Change management is the process of making changes in a deliberate, planned, and systematic manner.[102] It is important for nurse leaders and nurse managers to remember a few key points about change management[103]:
- Employees will react differently to change, no matter how important or advantageous the change is purported to be. Recognizing this variability is crucial for effectively managing the transition process.
- Basic needs will influence reaction to change, such as the need to be part of the change process, the need to be able to express oneself openly and honestly, and the need to feel that one has some control over the impact of change. Ensuring these needs are met can significantly reduce resistance.
- Change often results in a feeling of loss due to changes in established routines. Employees may react with shock, anger, and resistance, but ideally will eventually accept and adopt change. Acknowledging these feelings and providing support can facilitate smoother transitions.
- Change must be managed realistically, without false hopes and expectations, yet with enthusiasm for the future. Employees should be provided information honestly and allowed to ask questions and express concerns. This transparency builds trust and helps in aligning everyone towards common goals.
Strategies for Effective Change Management
- Engage Stakeholders Early: Involve key stakeholders in the planning stages of the change process. Their input can provide valuable insights and help in identifying potential challenges early on.
- Communicate Clearly and Frequently: Clear and frequent communication is essential. Use multiple channels to disseminate information and ensure that the message is consistent and comprehensible to all staff members.
- Provide Training and Resources: Equip employees with the necessary skills and resources to adapt to the change. This might include training sessions, informational materials, or access to support personnel.
- Build a Supportive Culture: Create an environment where change is viewed positively. Encourage collaboration and create opportunities for employees to share their experiences and strategies for adapting to change.
- Monitor and Adjust: Continuously monitor the progress of the change initiative and be prepared to make adjustments as needed. Solicit feedback from employees and be responsive to their concerns.
There are multiple strategies that can employed to overcome resistance to change. First, it is important to understand the underlying reasons for resistance. Resistance is commonly aligned to feelings of fear, lack of trust in leadership, or logistical concerns regarding workload, seniority, etc. To implement change effectively, a leader should empower staff by making sure they feel that their voice is respected and valued. When individuals feel valued and hear, they are more likely to support change, even if they do not personally agree with all elements associated with the change. Leaders also must understand that change is stressful for individuals. Depending on the significance of change, a leader may take actions to ensure that employee assistance programs, support groups, or additional counseling services or resources are available. These additional resources can be beneficial for individuals as they work through the emotions associated with the proposed change. Additionally, the benefits for any change should be clearly described. It is important to highlight how the proposed change will help improve work processes and patient care quality. It is also helpful to acknowledge and demonstrate appreciation for early adopters of the change. This can provide motivation and encouragement for others to follow suit and fosters a positive attitude toward future changes.
Understanding the Legal System
There are several types of laws and regulations that affect nursing practice. Laws are rules and regulations created by a society and enforced by courts and professional licensure boards. Nurses are responsible for being aware of public and private laws that affect client care, as well as legal actions that can result when these laws are broken.
Laws are generally classified as public or private law. Public law regulates relations of individuals with the government or institutions, whereas private law governs the relationships between private parties.
Public Law
There are several types of public law, including constitutional, statutory, administrative, and criminal law.
- Constitutional law refers to the rights, privileges, and responsibilities established by the U.S. Constitution.[104] The right to privacy is an example of a patient right based on constitutional law.
- Statutory law refers to written laws enacted by the federal or state legislature. For example, the Nurse Practice Act in each state is an example of statutory law enacted by that state’s legislature. The Health Insurance Portability and Accountability Act (HIPAA) is an example of a federal statutory law. HIPAA required the creation of national standards to protect sensitive client health information from being disclosed without the client's consent or knowledge.
- Administrative law is law created by government agencies that have been granted the authority to establish rules and regulations to protect the public.[105] An example of federal administrative law is the regulations set by the Occupational Safety and Health Administration (OSHA). OSHA was established by Congress to ensure safe and healthy working conditions for employees by setting and enforcing federal standards. An example of administrative law at the state level is the State Board of Nursing (SBON). The SBON is a group of individuals in each state, established by that state’s legislature, to develop, review, and enforce the Nurse Practice Act. The SBON also issues nursing licenses to qualified candidates, investigates reports of nursing misconduct, and implements consequences for nurses who have violated the Nurse Practice Act.
- Criminal law is a system of laws concerned with punishment of individuals who commit crimes.[106] A crime is a behavior defined by Congress or state legislature as deserving of punishment. Crimes are classified as felonies, misdemeanors, and infractions. Conviction for a crime requires evidence to show the defendant is guilty beyond a shadow of doubt. This means the prosecution must convince a jury there is no reasonable explanation other than guilty that can come from the evidence presented at trial. In the United States, an individual is considered innocent until proven guilty. See Figure 5.1[107] for an illustration of a trial with a jury.

Serious crimes that can result in imprisonment for longer than one year are called felonies. Felony convictions can also result in the loss of voting rights, the ability to own or use guns, and the loss of one’s nursing license. An example of a felony committed by some nurses is drug diversion of controlled substances.
Misdemeanors are less serious crimes resulting in penalties of fines and/or imprisonment for less than one year. For example, in Wisconsin, misdemeanors are categorized as Class A, B, or C based on their sentencing. Class A misdemeanors are sentenced to a fine not to exceed $10,000 or imprisonment not to exceed nine months, or both. Class B misdemeanors are sentenced to a fine not to exceed $1,000 or imprisonment not to exceed 90 days, or both. Class C misdemeanors are sentenced to a fine not to exceed $500 or imprisonment not to exceed 30 days, or both.[108] Examples of misdemeanors include battery, possession of controlled substances, petty theft, disorderly conduct, and driving under the influence (DUI) charges. Although considered less serious crimes, misdemeanors can impact an individual’s ability to obtain or maintain a nursing license.
Nurses who are found guilty of misdemeanors or felonies, regardless if the violation is related to the practice of nursing, must typically report these violations to their state’s Board of Nursing.
Infractions are minor offenses, such as speeding tickets, that result in fines but not jail time. Infractions do not generally impact nursing licensure unless there is a significant quantity of them over a short period of time.
Sample Case
An LPN working for a hospice agency was accused of stealing a patient’s pain medications and substituting them with anti-seizure medication. The family asserted the actions of the LPN prolonged the patient’s suffering. The LPN served time in prison for diverting the patient’s medications.[109]
Private Law
Private law, also referred to as civil law, focuses on the rights, responsibilities, and legal relationships between private citizens. Civil law typically involves compensation to the injured party. Unlike criminal law that requires a jury to determine a defendant is guilty beyond reasonable doubt, civil law only requires a certainty of guilt of greater than 50 percent.[110] See Figure 5.2[111] illustrating balancing the evidence to determine the certainty of guilt. Any nurse can be impacted by civil law based on actions occurring in daily nursing practice.

Civil law includes contract law and tort law. Contracts are binding written, verbal, or implied agreements. A tort is an act of commission or omission that gives rise to injury or harm to another and amounts to a civil wrong for which courts impose liability. In the context of torts, "injury" describes the invasion of any legal right, whereas "harm" describes a loss or detriment that an individual suffers.[112]
Two categories of torts affect nursing practice: intentional torts, such as intentionally hitting a person, and unintentional torts (also referred to as negligent torts), such as making an error by failing to follow agency policy.
Intentional Torts
Intentional torts are wrongs that the defendant knew (or should have known) would be caused by their actions. Examples of intentional torts include assault, battery, false imprisonment, slander, libel, and breach of privacy or client confidentiality.
Unintentional Torts
Unintentional torts occur when the defendant's actions or inactions were unreasonably unsafe. Unintentional torts can result from acts of commission (i.e., doing something a reasonable nurse would not have done) or omission (i.e., failing to do something a reasonable nurse would do).[113]
Negligence and malpractice are examples of unintentional torts. Tort law exists to compensate clients injured by negligent practice, provide corrective judgement, and deter negligence with visible consequences of action or inaction.[114],[115] Examples of common torts affecting nursing practice are discussed in further detail in the following subsections. See Table 5.2 for a comparison of public and private law.
Table 5.2 Comparison of Public and Private Law
| Type of Law | Subtypes of Law and Examples |
|---|---|
| Public Law |
|
| Private Law (Civil Law) |
|
Examples of Intentional and Unintentional Torts
Assault and Battery
Assault and battery are intentional torts. Assault is defined as intentionally putting another person in reasonable apprehension of an imminent harmful or offensive contact.[116] Battery is defined as intentional causation of harmful or offensive contact with another person without that person's consent.[117] Physical harm does not need to occur to be charged with assault or battery. Battery convictions are often misdemeanors but can be felonies if serious bodily harm occurs. To avoid the risk of being charged with assault or battery, nurses must obtain consent from clients to provide hands-on care.
False Imprisonment
False imprisonment is an intentional tort. False imprisonment is defined as an act of restraining another person and causing that person to be confined in a bounded area.[118] In nursing practice, restraints can be physical, chemical, or verbal. Nurses must strictly follow agency policies related to the use of restraints. Physical restraints typically require a provider order and documentation according to strict guidelines within specific time frames. See Figure 5.3[119] for an image of a simulated client in full physical medical restraints.
Chemical restraints include administering medications such as benzodiazepines and require clear documentation supporting their use. Verbal threats to keep an individual in an inpatient environment can also qualify as false imprisonment and should be avoided.
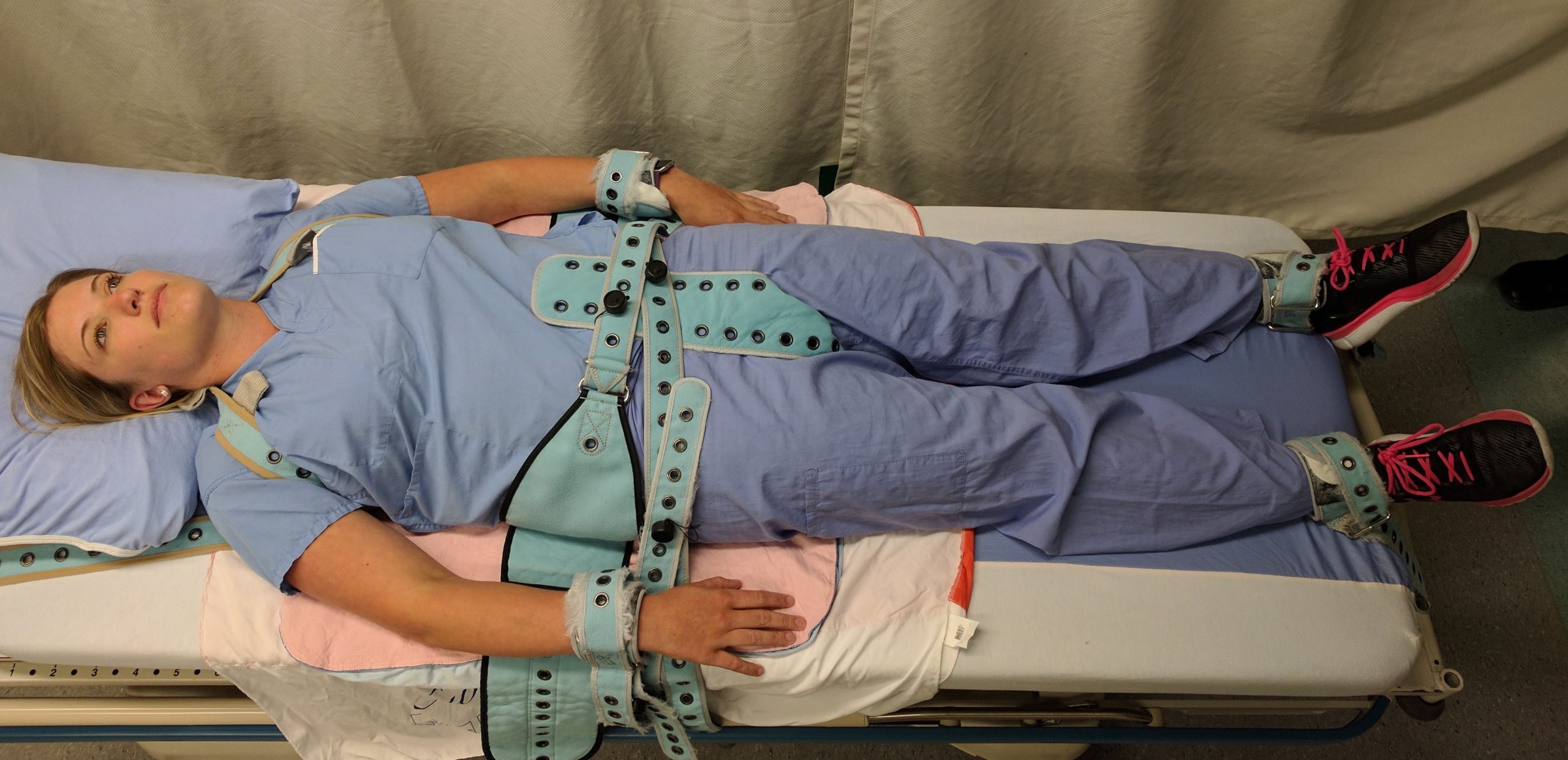
Breach of Privacy and Confidentiality
Breaching privacy and confidentiality are intentional torts. Confidentiality is the right of an individual to have personal, identifiable medical information, referred to as protected health information (PHI), kept private. Protected Health Information (PHI) is defined as individually identifiable health information, including demographic data, that relates to the individual’s past, present, or future physical or mental health or condition[120]; the provision of health care to the individual; and the past, present, or future payment for the provision of health care to the individual.
This right is protected by federal regulations called the Health Insurance Portability and Accountability Act (HIPAA). HIPAA was enacted in 1996 and was prompted by the need to ensure privacy and protection of personal health records and data in an environment of electronic medical records and third-party insurance payers. There are two main sections of HIPAA law: the Privacy Rule and the Security Rule. The Privacy Rule addresses the use and disclosure of individuals’ health information. The Security Rule sets national standards for protecting the confidentiality, integrity, and availability of electronically protected health information. HIPAA regulations extend beyond medical records and apply to client information shared with others. Therefore, all types of client information should be shared only with health care team members who are actively providing care to them.[121],[122]
HIPAA violations may result in fines from $100 for an individual violation to $1.5 million for organizational violations. Criminal penalties, including jail time of up to ten years, may be imposed for violations involving the use of PHI for personal gain or malicious intent. Nursing students are also required to adhere to HIPAA guidelines from the moment they enter the clinical setting or risk being disciplined or expelled by their nursing program.
Sample Case
An RN accessed a patient’s medical records, as well as the records of the newborn son, although she was not assigned to their care because she believed the newborn was her biological grandchild. Although the chart was accessed for less than five seconds, it was unauthorized. The nurse was publicly reprimanded by the state’s Board of Nursing, and her multistate licensure privileges were revoked. Expenses to defend the nurse exceeded $2,800.[123]
Read more about the HIPAA Privacy Rule.
Slander and Libel
Slander and libel are intentional torts. Defamation of character occurs when an individual makes negative, malicious, and false remarks about another person to damage their reputation. Slander is spoken defamation and libel is written defamation. Nurses must take care to communicate and document facts regarding patient care without defamation in their oral and written communications with clients and coworkers.
Fraud
Fraud is an intentional tort occurring when an individual is deceived for personal gain. An example of fraud is financial exploitation perpetrated by individuals who are in positions of trust.[124],[125] A nurse may be charged with fraud for documenting interventions not performed or altering documentation to cover up an error. Fraud can result in civil and criminal charges and also suspension or revocation of a nurse’s license.
Negligence and Malpractice
Negligence and malpractice are types of unintentional torts. Negligence is the failure to exercise the ordinary care a reasonable person would use in similar circumstances. Wisconsin civil jury instruction states, “A person is not using ordinary care and is negligent, if the person, without intending to do harm, does something (or fails to do something) that a reasonable person would recognize as creating an unreasonable risk of injury or damage to a person or property.”[126] Malpractice is a specific term used for negligence committed by a professional with a license. See Figure 5.4[127] for an illustration related to malpractice.
Elements of Nursing Malpractice
Nurses and nursing students don’t often get sued for malpractice, but when they do, it is important to understand the elements required to prove malpractice. All the following elements must be established in a court of law to prove malpractice[128]:
- Duty: A nurse-client relationship exists.
- Breach: The standard of care was not met and harm was a foreseeable consequence of the action or inaction.
- Cause: Injury was caused by the nurse’s breach.
- Harm: Injury resulted in damages.
Parties bringing a lawsuit must be able to demonstrate their interests were harmed, providing a reason to stand before the court. The person bringing the lawsuit is called the plaintiff. The parties named in the lawsuit are called defendants. Most malpractice lawsuits name physicians or hospitals, although nurses can be individually named. Employers can be held liable for the actions of their employees.[129]
Malpractice lawsuits are concerned with the legal obligations nurses have to their patients to adhere to current standards of practice. These legal obligations are referred to as the duty of reasonable care. Nurses are required to adhere to standards of practice when providing care to patients they have been assigned. This includes following organizational policies and procedures, maintaining clinical competency, and confining their activities to the authorized scope of practice as defined by their state’s Nurse Practice Act. Nurses also have a legal duty to be physically, mentally, and morally fit for practice. When nurses do not meet these professional obligations, they are said to have breached their duties to patients.[130]
Duty
In the work environment, a duty is created when the nurse accepts responsibility for a patient and establishes a nurse-patient relationship. This generally occurs during inpatient care upon acceptance of a handoff report from another nurse. Outside the work environment, a nurse-patient relationship is created when the nurse volunteers services. Some states have statutes requiring notification of authorities (also referred to as mandatory reporting) or summoning assistance.[131]
Good Samaritan Law
The Good Samaritan Law provides protections against negligence claims to individuals who render aid to people experiencing medical emergencies outside of clinical environments. All 50 states in the United States have a version of a Good Samaritan Law. See Figure 5.5[132] for historical artwork depicting a Good Samaritan. Differences exist in state laws regarding protection of bystanders who provide aid. For example, in Wisconsin, the law states, "Any person who renders emergency care at the scene of any emergency or accident in good faith is immune from civil liability for the person’s acts or omissions in rendering such emergency care."[133] There are a few states that require some emergency bystander action, so nurses should review the law in states they are visiting. It is also important to keep in mind that although anyone can file a lawsuit against someone who provides bystander aid, the Good Samaritan laws typically negate any penalty to the person rendering aid.
Although the majority of Good Samaritan laws are at the state level, the federal Aviation Medical Assistance Act (AMAA) provides liability protection for aid given on aircraft. The most common in-flight medical emergencies involve syncope, as well as gastrointestinal, respiratory, and cardiac events.[134] Note that consent for care by an unconscious person is implied, but consent must be obtained from alert individuals.

Mandatory Reporting
Nurses are legally responsible for reporting certain crimes. Mandatory reporting requirements vary based on the state of practice, but there are some commonalities. For example, nurses are mandated to report suspected abuse of children, the elderly, and the disabled (if they have been deemed as incompetent by a court of law or as incapacitated by qualified health care providers).
Nurses are also mandated to report gunshot wounds, dog bites, some communicable diseases, and unsafe or illegal practices of other health care team members. Reporting responsibility often begins at the organizational level. The nurse may also need to identify the appropriate local, state, or federal authorities to submit the report and pursue it to its resolution.
Sample Statute Regarding Duty to Assist
A Minnesota statute states that a person at the scene of an emergency who knows that another person is exposed to or has suffered grave physical harm shall, to the extent that the person can do so without danger or peril to self or others, give reasonable assistance to the exposed person. Reasonable assistance may include obtaining or attempting to obtain aid from law enforcement or medical personnel. A person who violates this is guilty of a petty misdemeanor.[135]
Implications for Nurses
Duty can be established in many ways. Nurses have a duty of reasonable care for a patient they have been assigned. They may also have a duty in other circumstances. Therefore, nurses should understand the following[136]:
- Recognize that a nurse-patient relationship is established upon acceptance of responsibility for a patient, whether after a handoff report in the workplace or during volunteered services.
- Assume that on-call or supervisory responsibilities create a duty to patients, even in the absence of an expressed nurse-patient relationship.
- Know if there is a duty to rescue statute in their state, and if so, what it demands.
Breach of Duty
The second element of malpractice is breach of duty. After a plaintiff has established the first element in a malpractice suit, that the nurse owed a duty to the plaintiff, the plaintiff must then demonstrate that the nurse breached that duty by failing to comply with the duty of reasonable care.[137]
To demonstrate that a nurse breached their duty to a patient, the plaintiff must prove the nurse departed from acceptable standards of practice. The plaintiff must establish how a reasonably prudent nurse in the same or similar circumstances would act and then show that the defendant nurse departed from that standard of practice. The plaintiff must claim the nurse did something a reasonably prudent nurse would not have done (an act of commission) or failed to do something a reasonable nurse would have done (an act of omission).[138]
Experts are needed during court hearings to explain things outside the knowledge of non-nurse jurors. In reaching their opinions, experts review many materials, including the state’s Nurse Practice Act and organizational policies, to determine whether the nurse adhered to them. To qualify as a nurse expert, the person testifying must have relevant experience, education, skill, and knowledge. They typically have advanced degrees, are published in nursing literature, have spoken at professional conferences, and belong to professional organizations. Medical malpractice trials take place primarily in state courts, so experts are deemed qualified based on state requirements.
Sample Case Regarding Breach of Duty[139]
Mary Jones was an 87-year-old woman who presented to the hospital with dizziness, nausea, intermittent slurred speech, an unsteady gait, and a history of four falls at home that day. Significant medical history included heart disease and multiple medications. The admitting nurse assessed her as being at risk for falls and placed her on universal fall precautions. The fall precautions included keeping the bed in the lowest position, instructing her on the use of the call light and ensuring the call light was within her reach, providing a bedside commode, and placing her in a room close to the nurses’ station where she could be observed. However, the nurse did not use a formal scoring system for fall risk assessment that was set forth in a nursing procedures textbook. Additionally, bed alarms had not been working at this agency for a year.
Five days later, a nurse responded to a sound coming from Mrs. Jones’s room and found her lying on the bathroom floor. She was conscious and able to move all extremities but complained of left knee and elbow pain. The physician was notified, and Mrs. Jones was sent for X-rays and a CT scan. When Mrs. Jones returned to her room, the nurse observed she was diaphoretic and deteriorating. The nurse took Mrs. Jones to the emergency department, where she lost consciousness. She was evaluated by a neurosurgeon, intubated, and airlifted to a different hospital for a higher level of care. She never regained consciousness and died the next day from intracranial bleeding that was aggravated by anticoagulant therapy.
Mrs. Jones’s estate brought a lawsuit alleging nursing malpractice. The estate’s nursing expert stated the universal fall precautions had been inadequate for a high-risk patient and additional measures should have been instituted. The expert testified that not only had the admitting nurse not adhered to the formal scoring system for fall risk assessment in the nursing procedures textbook, but also the standard of care required nurses to use bed alarms, institute 15-minute rounds, or place a sitter in the room.
A defense expert used The Joint Commission’s National Patient Safety Goals to define the standard of care and testified it was her opinion the nurse had met that standard. The organizational policy did not require bed alarms as part of its fall prevention plan. Although the nurses did not use the formal scoring system in a textbook to assess the patient’s risk, they clearly identified her as being at risk for falling; assessed her frequently; maintained her bed in the lowest position; kept the wheels of her bed locked and her side rails up; and kept the call light within her reach. They instructed her on the use of the call light and placed her in a room where she could be readily observed.
The court entered the judgment for the defendant hospital, noting that “under the circumstances, it is a close call on whether the hospital, by not having functioning bed alarms and staff not checking on Mary more frequently, breached the standard of care.”[140] In this case, the plaintiff's expert had not demonstrated the standard of care was breached.
Implications for Nurses
Nurses defending themselves against allegations of professional malpractice must demonstrate their actions conformed with accepted standards of practice. They must convince a jury they acted as a reasonably prudent nurse would have in the same or similar circumstances. Nurses should always follow these practices[141]:
- Adhere to organizational policies and procedures. Work-arounds can create liability. The standard of practice is to adhere to agency policy. Failing to do so creates an assumption of departure from standards.
- Document in a manner that permits accurate reconstruction of patient assessments and the sequence of events, especially when notifying providers regarding clinical concerns.
- Maintain competence through continuing education, participation in professional conferences, membership in professional organizations, and subscriptions to professional journals.
- When using an interpreter, ensure that properly trained interpreters are used and document the name of the interpreter. The use of family, friends, or other untrained interpreters is unsafe practice and is not consistent with acceptable standards of practice.
- Maintain professional boundaries. Personal relationships with patients or their families can be red flags for juries and can be viewed as evidence of departure from professional standards.
Cause
The third element of malpractice is cause. After the plaintiff has established the nurse owed a duty to a patient and then breached that duty, they must then demonstrate that damages or harm were caused by that breach. Plaintiffs cannot prevail by only demonstrating the nurse departed from acceptable standards of practice but must also prove that such departures were the cause of any injuries.[142] Additionally, nurses are held accountable for foreseeability, meaning a nurse of ordinary skill, care, and diligence could anticipate the risk of harm of departing from standards of practice in similar circumstances.[143]
Plaintiffs must be able to link the defendant’s acts or omissions to the harm for which they are seeking compensation. This requires expert testimony from a physician because it requires a medical diagnosis. Unlike in criminal cases, in which the standard of proof is that elements of prosecution must be proven “beyond reasonable doubt,” the elements of a malpractice lawsuit must be proven by a “preponderance of evidence.” Expert testimony is required to demonstrate “medical certainty” that the nurse’s breach was the cause of an actual injury.
Sample Cases Regarding Causation
Case 1
Janusz Osiecki was admitted to a subacute nursing facility to recover from Guillain-Barre syndrome. The standard of nursing care for this client included respiratory assessments and tracheostomy care. One morning, three weeks into his stay, he was found unresponsive, without pulse or respirations. His wife brought a wrongful death lawsuit, and expert witnesses testified the nurses breached the standard of care in not performing respiratory and tracheostomy assessments every two hours. Their rationale was that the purpose of the assessments was to detect and report pulmonary congestion, and if the nurses had done so in a timely manner, Mr. Osiecki could have received medical care that would have saved his life. A jury awarded the widow $577,005 for wrongful death and $250,000 for harm to family relationships.[144]
Case 2
A psychiatric patient identified as “C” was locked in a seclusion room after presenting to a hospital with psychosis and continuing bizarre behavior, hallucinations, irrationality, lack of contact with reality, and agitation. She was in the seclusion room undergoing treatment for over a week when she suffered a grand mal seizure. A psychiatrist ordered antipsychotic medication. The medication order was not noted by nursing staff until the next day, at which point it was discovered the medication was unavailable at the pharmacy. The psychiatrist was not made aware the medication was unavailable, and the patient went without the prescribed medication for three days. The nurses also did not notify the psychiatrist during those three days that C was becoming increasingly more agitated and hallucinating. On the fourth day, C attempted to leave the unit and told staff she was hearing voices instructing her to harm herself. She was returned to seclusion and remained there without being assessed or treated. Four hours later, she was found unconscious with her head wedged between the side rail and the mattress. She suffered brain damage that left her in a permanent semicomatose state.
C’s estate brought a lawsuit alleging it was negligent to leave C in a steel bed in a seclusion room without constant observation. The jury awarded $3.6 million. The hospital appealed, but the appellate court upheld the jury verdict and explained that particular injuries do not need to be foreseen, only the general harm that can occur. The court stated, “It is not extraordinary that a psychotic patient who is delusional…might wedge herself between a mattress and side rail in an attempt to hurt herself.”[145]
Implications for Nurses
Nurses can reduce their liability by adhering to professional standards and documenting their observations and communications. Nurses should always follow these standards[146]:
- Follow the chain of command when there are concerns about unclear or potentially unsafe orders. Pursue concerns to resolution, documenting precisely who is notified and at what times.
- Document observations to justify clinical decisions. Variance charting (i.e., only charting things that vary from the norm) does not provide sufficient evidence of compliance with the standards of care.
- Adhere to organizational policies and procedures with an understanding that a failure to do so creates foreseeable harm to patients.
Harm
The fourth element of malpractice is harm. In a civil lawsuit, after a plaintiff has established the nurse owed a duty to the patient and breached that duty and injury was caused by the nurse's breach, they must prove the injury resulted in damages. They request repayment for what they have lost.[147]
There are several types of injuries for which patients or their representatives seek compensation. Injuries can be physical, emotional, financial, professional, marital, or any combination of these. Physical injuries include loss of function, disfigurement, physical or mental impairment, exacerbation of prior medical problems, the need for additional medical care, and death. Economic injuries can include lost wages, additional medical expenses, rehabilitation, durable medical expenses, the need for architectural changes to one’s home, the loss of earning capacity, the need to hire people to do things the plaintiff can no longer do, and the loss of financial support. Emotional injuries can include psychological damage, emotional distress, or other forms of mental suffering.[148]
Determining the specific amount a plaintiff needs can require expert witness testimony from a person known as a life care planner who is trained in analyzing and evaluating medical costs, as well as the subjective determination of a jury. Damages fall into several categories, including compensatory (economic) damages, noneconomic damages, and punitive damages.[149] See Figure 5.6[150] for an illustration of damages.

Economic damages (also referred to as actual damages) can be quantified. They are intended to restore the plaintiff to the position they were in before being injured. Compensatory damages are objectively calculated to provide the plaintiff with the amount of money necessary to replace what was lost.[151]
Noneconomic damages are subjective and can include things such as emotional distress, pain and suffering, loss of enjoyment of life, reputation damage, loss of companionship, or loss of parental guidance. They are more difficult to quantify than economic damages.[152]
Punitive damages are awards not related to the actual injury but are intended to punish the defendant(s) and deter others from engaging in similar conduct. In professional malpractice cases, punitive damages are difficult for plaintiffs to obtain because they must be related to outrageous conduct, such as gross negligence, recklessness, willful actions, or fraud.[153]
Sample Case Related to Damages[154]
Betty Shiflett fell out of bed in the recovery room after undergoing knee surgery. Three days later, she reported a clicking sound and pain in her knee to one of the nurses. Although the nurse documented these symptoms, she did not convey the information to the physician. A physical therapist reported these symptoms to the physician a week later. The physician then identified a previously undiagnosed nondisplaced left tibial fracture that was now avulsed. Two additional surgeries were unsuccessful, and Betty remained disabled, confined to a wheelchair, and in chronic pain.
Betty and her husband filed a lawsuit alleging negligence for the fall and the nurse’s failure to report the symptoms to the physician. They also asserted a claim for a loss of consortium, meaning the spouse or family had also been harmed. The harm suffered is a loss of companionship, conjugal relations, support and services, or marital quality. The jury awarded total damages of $2,391,620 with the following breakdown:
- $791,620 for future medical expenses
- $800,000 for past noneconomic damages
- $500,000 for future noneconomic damages
- $300,000 for loss of consortium with spouse
Implications for Nurses
Nurses can reduce their liability exposure by following these principles[155]:
- Practicing according to current standards of practice.
- Maintaining professional liability insurance to provide coverage for events and licensure defense.
- Avoiding work-arounds or deviations from organizational policies and procedures.
- Maintaining clinical competency, including awareness of standard-of-practice changes.
- Engaging the chain of command with patient concerns and pursuing concerns to resolution.
- Documenting in a manner that permits accurate reconstruction of patient assessments, notification of others, and the sequence of events.
As discussed in the previous sections, professional liability occurs when a civil lawsuit compensates patients who allege they have suffered injury or damage as a result of professional negligence. Many nurses elect to purchase malpractice insurance to protect themselves from professional liability, especially if working in specialty areas that experience a high number of claims, such as in obstetrics or post-anesthesia care units (PACUs). The Nursing Service Organization (NSO) works in association with the American Nurses Association to provide malpractice insurance for nurses interested in purchasing it.
Read more about malpractice insurance available for nurses at https://www.nso.com/.
The civil justice system cannot make rulings regarding your nursing license. It is the responsibility of the State Board of Nursing to suspend or revoke an individual’s nursing license based on a disciplinary process.
The State Board of Nursing (SBON) governs nursing practice according to that state’s Nurse Practice Act. The purpose of the SBON is to protect the public through licensure, education, legislation, and discipline. A nursing license is a contract between the state and licensee in which the licensee agrees to provide nursing care according to that state's Nurse Practice Act. Deviation from the Nurse Practice Act is a breach of contract that can lead to limited or revoked licensure. The SBON can suspend or revoke an individual’s nursing license to protect the public from unsafe nursing practice. Nursing scope of practice and standards of nursing care are defined in the Nurse Practice Act that is enacted by the state legislature and enforced by the SBON. Nurses must practice according to the Nurse Practice Act of the state in which they are providing client care.
A nurse may be named in a board licensing complaint, also called an allegation. Allegations can be directly related to a nurse’s clinical responsibilities, or they can be nonclinical (such as substance abuse, unprofessional behavior, or billing fraud). A complaint can be filed against a nurse by anyone, such as a patient, a patient's family member, a colleague, or an employer. It can be filed anonymously. After a complaint is filed, the SBON follows a disciplinary process that includes investigation, proceedings, board actions, and enforcement. The process can take months or years to resolve, and it can be costly to hire legal representation.[156]
During the investigation process, investigators use various methods to determine the facts, such as interviewing parties who were present, reviewing documentation and records, performing drug screens (if impairment is alleged), and compiling pertinent facts related to the events and circumstances surrounding the complaint. Nurses being investigated may receive a letter, email, or phone call from the SBON, or they may be required to appear at a certain date and time for an interview with an investigator. It is recommended that nurses consult with an attorney before responding to the SBON within the deadline provided. Nurses should be cooperative but should be aware that whatever is shared will be provided to a prosecuting attorney and/or the SBON.[157]
After completion of the investigation, the prosecuting attorney will determine how to proceed. A conference may be scheduled where the nurse will be interviewed by a member of the SBON and possibly the prosecuting attorney. It is recommended for the nurse to have an attorney present during proceedings. The nurse has the opportunity to present evidence supporting their case. A resolution may be offered after the conference that ends the matter.[158]
However, if the SBON believes there is significant evidence, a formal hearing is held where a disciplinary action is proposed. This formal hearing is similar to a civil trial. The hearing panel may include some or all of the SBON members. A court reporter records the entire proceeding and a transcript is created. Witnesses may be called to testify and the nurse undergoes cross-examination. When both sides have presented their cases, the hearing is concluded. The outcome of the formal hearing is a ruling by the administrative law judge and the SBON. The nurse may face disciplinary action such as a reprimand, limitation, suspension, or revocation of their license. Nondisciplinary actions, such as a warning or a remedial education order, may be set. See a description of possible disciplinary actions enforced by the Wisconsin State Board of Nursing in Table 5.3a.
Table 5.3a. Potential Disciplinary and Nondisciplinary Actions of the Wisconsin State Board of Nursing[159]
| Disciplinary Options
|
Reprimand: The licensee receives a public warning for a violation.
Limitation of License: The licensee has conditions or requirements imposed upon their license, their scope of practice, or both. Suspension: The license is completely and absolutely withdrawn and withheld for a period of time, including all rights, privileges, and authority previously conferred by the credential. Revocation: The license is completely and absolutely terminated, as well as all rights, privileges, and authority previously conferred by the credential. |
|---|---|
| Nondisciplinary Options | Administrative Warning: A warning is issued if the violation is of a minor nature or a first occurrence, and the warning will adequately protect the public. The issuance of an administrative warning is public information; however, the reason for issuance is not.
Remedial Education Order: A remedial education order is issued when there is reason to believe that the deficiency can be corrected with remedial education, while sufficiently protecting the public. |
Find and review your state's Nurse Practice Act at https://www.ncsbn.org/policy/npa.page.
Read more about Wisconsin’s Board of Nursing and Administrative Code.
Liability considerations does not only apply when working in your professional nursing role, but also within your student nurse role. As you work as a student nurse, there are other role considerations which may impact the decision regarding professional liability. Please see Table 5.3b for a comparison of different types of liability.
5.3b. Types of Liability
| Type of Liability | Definition | Example |
| Supervisory Liability[160] | When a clinical supervisor or preceptor is held responsible for the actions of the student nurse or for failing to properly supervise them. | A clinical supervisor fails to provide proper guidance during a procedure, resulting in the student nurse administering the wrong medication to a patient. The supervisor could be held liable for inadequate supervision. |
| Institutional Liability[161] | When the health care institution (e.g., hospital, clinic) is held responsible for the actions of its employees or for failing to implement adequate policies and procedures to prevent harm. | A hospital does not provide proper orientation or training programs for student nurses, leading to a student nurse making a critical error. The hospital could be held liable for not ensuring adequate training. |
| Student Liability[162] | When the student nurse is held responsible for their own actions that cause harm to patients or violate protocols. | A student nurse neglects to follow infection control protocols, resulting in a patient's condition worsening. The student nurse could be held liable for their negligence. |
You have worked hard to obtain a nursing license and it will be your livelihood. See Figure 5.7[163] for an illustration of a nursing license. Protecting your nursing license is vital.
Actions to Protect Your License
There are several actions that nurses can take to protect their nursing license, avoid liability, and promote patient safety. See Table 5.5 for a summary of recommendations.
Table 5.5 Risk Management Recommendations to Protect Your Nursing License
| Legal Issues | Recommendations to Protect Your License |
|---|---|
| Practicing outside one’s scope of practice |
|
| Failure to assess & monitor |
|
| Documentation |
|
| Medication errors |
|
| Substance abuse and drug diversion |
|
| Acts that may result in potential or actual client harm |
|
| Safe-guarding client possessions & valuables |
|
| Adherence to mandatory reporting responsibilities |
|
Culture of Safety
It can be frightening to think about entering the nursing profession after becoming aware of potential legal actions and risks to your nursing license, especially when realizing even an unintentional error could result in disciplinary or legal action. When seeking employment, it is helpful for nurses to ask questions during the interview process regarding organizational commitment to a culture of safety to reduce errors and enhance patient safety.
Many health care agencies have adopted a culture of safety that embraces error reporting by employees with the goal of identifying root causes of problems so they may be addressed to improve patient safety. One component of a culture of safety is "Just Culture." Just Culture is culture where people feel safe raising questions and concerns and report safety events in an environment that emphasizes a nonpunitive response to errors and near misses. Clear lines are drawn between human error, at-risk, and reckless behaviors. [170]
The American Nurses Association (ANA) officially endorses the Just Culture model. In 2019 the ANA published a position statement on Just Culture. They stated that while our traditional health care culture held individuals accountable for all errors and accidents that happened to patients under their care, the Just Culture model recognizes that individual practitioners should not be held accountable for system failings over which they have no control. The Just Culture model also recognizes that many errors represent predictable interactions between human operators and the systems in which they work. However, the Just Culture model does not tolerate conscious disregard of clear risks to patients or gross misconduct (e.g., falsifying a record or performing professional duties while intoxicated).[171]
The Just Culture model categorizes human behavior into three categories of errors: simple human error, at-risk behavior, or reckless behavior. Consequences of errors are based on these categories.[172] When seeking employment, it is helpful for nurses to determine how an agency implements a culture of safety because of its potential impact on one’s professional liability and licensure.
Read more about the Just Culture model in the "Basic Concepts" section of the "Leadership and Management" chapter.
In addition to being aware of the legal and regulatory frameworks in which one practices nursing, it is also important for nurses to understand the legal concepts of informed consent and advance directives.
Informed Consent
Informed consent is the fundamental right of a client to accept or reject health care. Nurses have a legal responsibility to provide verbal and/or written information and obtain verbal or written consent for performing nursing care such as bathing, medication administration, and urinary or intravenous catheter insertion. While physicians have the responsibility to provide information and obtain informed consent related to medical procedures, nurses are typically required to verify the presence of a valid, signed informed consent before the procedure is performed. Additionally, if nurses do not believe the patient has adequate understanding of a procedure, its risks, benefits, or alternatives to treatment, they should request the provider return to clarify unclear information with the client. Nurses must remain within their scope of practice related to informed consent beyond nursing acts.
Two legal concepts related to informed consent are competence and capacity. Competence is a legal term defined as the ability of an individual to participate in legal proceedings. A judge decides if an individual is “competent” or “incompetent.” In contrast, capacity is “a functional determination that an individual is or is not capable of making a medical decision within a given situation.”[173] It is outside the scope of practice for nurses to formally assess capacity, but nurses may initiate the evaluation of client capacity and contribute assessment information. States typically require two health care providers to identify an individual as “incapacitated” and unable to make their own health care decisions. Capacity may be a temporary or permanent state.
The following box outlines situations where the nurse may question a client's decision-making capacity.
| Triggers for Questioning Capacity and Decision-Making[174] |
|---|
|
If an individual has an advance directive in place, their designated power of attorney for health care may step in and make medical decisions when the client is deemed incapacitated. In the absence of advance directives, the legal system may take over and appoint a guardian to make medical decisions for an individual. The guardian is often a family member or friend but may be completely unrelated to the incapacitated individual. Nurses are instrumental in encouraging a client to complete an advance directive while they have capacity to do so.
Advance Directives
The Patient Self-Determination Act (PSDA) is a federal law passed by Congress in 1990 following highly publicized cases involving the withdrawal of life-supporting care for incompetent individuals. (Read more about the Karen Quinlan, Nancy Cruzan, and Terri Shaivo cases in the boxes at the end of this section.) The PSDA requires health care institutions, such as hospitals and long-term care facilities, to offer adults written information that advises them "to make decisions concerning their medical care, including the right to accept or refuse medical or surgical treatment and the right to formulate, at the individual's option, advance directives.”[175] Advanced directives are defined as written instructions, such as a living will or durable power of attorney for health care, recognized under state law, relating to the provision of health care when the individual is incapacitated. The PSDA allows clients to record their preferences about do-not-resuscitate (DNR) orders and withdrawing life-sustaining treatment. In the absence of a client’s advance directives, the court may assert an “unqualified interest in the preservation of human life to be weighed against the constitutionally protected interests of the individual.”[176] For this reason, nurses must educate and support the communities they serve regarding the creation of advanced directives.
Advanced directives vary by state. For example, some states allow lay witness signatures whereas some require a notary signature. Some states place restrictions on family members, doctors, or nurses serving as witnesses. It is important for individuals creating advance directives to follow instructions for state-specific documents to ensure they are legally binding and honored.
Advance directives do not require an attorney to complete. In many organizations, social workers or chaplains assist individuals to complete advance directives following referral from physicians or nurses. Clients should review and update their documents every 10-15 years, as well as with changes in relationship status or if new medical conditions are diagnosed.
Although advanced directive documents vary by state, they generally fall into two categories, referred to as a living will or durable power of attorney for healthcare.
Living Will
A living will is a type of advance directive in which an individual identifies what treatments they would like to receive or refuse if they become incapacitated and unable to make decisions. In most states, a living will only goes into effect if an individual meets specific medical criteria.[177] The living will often includes instructions regarding life-sustaining measures, such as cardiopulmonary resuscitation (CPR), mechanical ventilation, and tube feeding.
Durable Power of Attorney for Healthcare
It is impossible for an individual to document their preferences in a living will for every conceivable medical scenario that may occur. For this reason, it is essential for individuals to complete a durable power of attorney for healthcare. A durable power of attorney for healthcare (DPOAHC) is a person chosen to speak on one’s behalf if one becomes incapacitated. Typically, a primary health care power of attorney (POA) is identified with an alternative individual designated if the primary POA is unable or unwilling to do so. The health care POA is expected to make health care decisions for an individual they believe the person would make for themselves, based on wishes expressed in a living will or during previous conversations.[178]
It is essential for nurses to encourage clients to complete advance directives and have conversations with their designated POA about health care preferences, especially related to possible traumatic or end-of-life events that could require medical treatment decisions. Nurses can also dispel common misconceptions, such as these documents give the health care POA power to manage an individual’s finances. (A financial POA performs different functions than a health care POA and should be discussed with an attorney.)
After the advance directives are completed and included in the client’s medical record, the nurse has the responsibility to ensure they are appropriately incorporated into their care if they should become incapacitated.
View state-specific advance directives at the American Association of Retired Persons website.
Karen Ann Quinlan is an important figure in the United States’ history of defining life and death, a client’s privacy, and the state’s interest in preserving life and preventing murder. In April 1975, Karen Quinlan was 21 years old and became unresponsive after ingesting a combination of valium and alcohol while celebrating a friend’s birthday. She experienced respiratory failure, and although resuscitation efforts were successful, she suffered irreversible brain damage. She remained in a persistent vegetative state and became ventilator dependent. Her parents requested her physicians discontinue the ventilator because they believed it constituted extraordinary means to prolong her life. Her physicians denied their request out of concern of possible homicide charges based on New Jersey’s law. The Quinlans filed the first “right to die” lawsuit in September of 1975 but were denied by the New Jersey Superior Court in November. In March of 1976, the New Jersey Supreme Court determined the parent’s right to determine Karen’s medical treatment exceeded that of the state. Karen was discontinued from the ventilator six weeks later. When taken off the ventilator, Karen shocked many by continuing to breathe on her own. She lived in a coma for nine more years and succumbed to pneumonia on June 11, 1985.
-
- Sample Case: Nancy Beth Cruzan[180]
Nancy Cruzan is another important figure in the history of US “right to die” legal cases. At the age of 25, Nancy Cruzan was in a car accident on January 11, 1983. She never regained consciousness. After three years in a rehabilitation hospital, her parents began an eight-year battle in the courts to remove Nancy’s feeding tube. Nancy’s case was the first “right to die" case heard by the United States Supreme Court. Beyond allowing for the discontinuation of Nancy’s feeding tube, the U.S. Supreme Court ruled that all adults have the right to the following:1) Choose or refuse any medical or surgical intervention, including artificial nutrition and hydration.
2) Make advance directives and name a surrogate to make decisions on their behalf.
3) Surrogates can decide on treatment options even when all concerned are aware that such measures will hasten death, as long as causing death is not their intent.Nancy died nine days after removal of her feeding tube in December 1990. As a result of the Cruzan decision, the Patient Self-Determination Act (PSDA) was passed and took effect December 1, 1991. The act requires facilities to inform clients about their right to refuse treatment and to ask if they would like to prepare an advance directive.
- Sample Case: Nancy Beth Cruzan[180]
Sample Case: Terri Schaivo[181]
The Terri Schaivo case is a key case in history of advance directives in the United States because of its focus on the importance of having written advance directives to prevent family animosity, pain, and suffering. In 1990 Terri Schaivo was 26 years old. In her Florida home, she experienced a cardiac arrest thought to be a function of a low potassium level resulting from an eating disorder. She experienced severe anoxic brain injury and entered a persistent vegetative state. A PEG tube was inserted to provide medications, nutrition, and hydration. After three years, her husband refused further life-sustaining measures on her behalf, based on a statement Terri had once made, stating, “I don't want to be kept alive on a machine.” He expressed interest in obtaining a DNR order, withholding antibiotics for a urinary tract infection, and ultimately requested removal of the PEG tube. However, Terri’s parents never accepted the diagnosis of persistent vegetative state and vigorously opposed their son-in-law's decision and requests. Seven years of litigation generated 30 legal opinions, all supporting Michael Schiavo's right to make a decision on his wife's behalf. Terri died on March 31, 2005, following removal of her feeding tube.
The American Nurses Association (ANA) defines morality as “personal values, character, or conduct of individuals or groups within communities and societies,” whereas ethics is the formal study of morality from a wide range of perspectives.[182] Ethical behavior is considered to be such an important aspect of nursing the ANA has designated Ethics as the first Standard of Professional Performance. The ANA Standards of Professional Performance are "authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently." See the following box for the competencies associated with the ANA Ethics Standard of Professional Performance[183]:
Competencies of ANA's Ethics Standard of Professional Performance[184]
- Uses the Code of Ethics for Nurses With Interpretive Statements as a moral foundation to guide nursing practice and decision-making.
- Demonstrates that every person is worthy of nursing care through the provision of respectful, person-centered, compassionate care, regardless of personal history or characteristics (Beneficence).
- Advocates for health care consumer perspectives, preferences, and rights to informed decision-making and self-determination (Respect for autonomy).
- Demonstrates a primary commitment to the recipients of nursing and health care services in all settings and situations (Fidelity).
- Maintains therapeutic relationships and professional boundaries.
- Safeguards sensitive information within ethical, legal, and regulatory parameters (Nonmaleficence).
- Identifies ethics resources within the practice setting to assist and collaborate in addressing ethical issues.
- Integrates principles of social justice in all aspects of nursing practice (Justice).
- Refines ethical competence through continued professional education and personal self-development activities.
- Depicts one's professional nursing identity through demonstrated values and ethics, knowledge, leadership, and professional comportment.
- Engages in self-care and self-reflection practices to support and preserve personal health, well-being, and integrity.
- Contributes to the establishment and maintenance of an ethical environment that is conducive to safe, quality health care.
- Collaborates with other health professionals and the public to protect human rights, promote health diplomacy, enhance cultural sensitivity and congruence, and reduce health disparities.
- Represents the nursing perspective in clinic, institutional, community, or professional association ethics discussions.
Reflective Questions
- What Ethics competencies have you already demonstrated during your nursing education?
- What Ethics competencies are you most interested in mastering?
- What questions do you have about the ANA’s Ethics competencies?
The ANA's Code of Ethics for Nurses With Interpretive Statements is an ethical standard that guides nursing practice and ethical decision-making.[185] This section will review several basic ethical concepts related to the ANA's Ethics Standard of Professional Performance, such as values, morals, ethical theories, ethical principles, and the ANA Code of Ethics for Nurses.
Values
Values are individual beliefs that motivate people to act one way or another and serve as guides for behavior considered “right” and “wrong.” People tend to adopt the values with which they were raised and believe those values are “right” because they are the values of their culture. Some personal values are considered sacred and moral imperatives based on an individual’s religious beliefs.[186] See Figure 6.1[187] for an image depicting choosing right from wrong actions.

In addition to personal values, organizations also establish values. The American Nurses Association (ANA) Professional Nursing Model states that nursing is based on values such as caring, compassion, presence, trustworthiness, diversity, acceptance, and accountability. These values emerge from nursing practice beliefs, such as the importance of relationships, service, respect, willingness to bear witness, self-determination, and the pursuit of health.[188] As a result of these traditional values and beliefs by nurses, Americans have ranked nursing as the most ethical and honest profession in Gallup polls since 1999, with the exception of 2001, when firefighters earned the honor after the attacks on September 11.[189]
The National League of Nursing (NLN) has also established four core values for nursing education: caring, integrity, diversity, and excellence[190]:
- Caring: Promoting health, healing, and hope in response to the human condition.
- Integrity: Respecting the dignity and moral wholeness of every person without conditions or limitations.
- Diversity: Affirming the uniqueness of and differences among persons, ideas, values, and ethnicities.
- Excellence: Cocreating and implementing transformative strategies with daring ingenuity.
Morals
Morals are the prevailing standards of behavior of a society that enable people to live cooperatively in groups. “Moral” refers to what societies sanction as right and acceptable. Most people tend to act morally and follow societal guidelines, and most laws are based on the morals of a society. Morality often requires that people sacrifice their own short-term interests for the benefit of society. People or entities that are indifferent to right and wrong are considered “amoral,” while those who do evil acts are considered “immoral.”[192]
Ethical Theories
There are two major types of ethical theories that guide values and moral behavior referred to as deontology and consequentialism.
Deontology is an ethical theory based on rules that distinguish right from wrong. See Figure 6.2[193] for a word cloud illustration of deontology. Deontology is based on the word deon that refers to “duty.” It is associated with philosopher Immanuel Kant. Kant believed that ethical actions follow universal moral laws, such as, “Don’t lie. Don’t steal. Don’t cheat.”[194] Deontology is simple to apply because it just requires people to follow the rules and do their duty. It doesn’t require weighing the costs and benefits of a situation, thus avoiding subjectivity and uncertainty.[195],[196],[197]
The nurse-patient relationship is deontological in nature because it is based on the ethical principles of beneficence and maleficence that drive clinicians to “do good” and “avoid harm.”[198] Ethical principles will be discussed further in this chapter.
Consequentialism is an ethical theory used to determine whether or not an action is right by the consequences of the action. See Figure 6.3[200] for an illustration of weighing the consequences of an action in consequentialism. For example, most people agree that lying is wrong, but if telling a lie would help save a person’s life, consequentialism says it’s the right thing to do. One type of consequentialism is utilitarianism. Utilitarianism determines whether or not actions are right based on their consequences with the standard being achieving the greatest good for the greatest number of people.[201],[202],[203] For this reason, utilitarianism tends to be society-centered. When applying utilitarian ethics to health care resources, money, time, and clinician energy are considered finite resources that should be appropriately allocated to achieve the best health care for society.[204]

Utilitarianism can be complicated when accounting for values such as justice and individual rights. For example, assume a hospital has four patients whose lives depend upon receiving four organ transplant surgeries for a heart, lung, kidney, and liver. If a healthy person without health insurance or family support experiences a life-threatening accident and is considered brain dead but is kept alive on life-sustaining equipment in the ICU, the utilitarian framework might suggest the organs be harvested to save four lives at the expense of one life.[205] This action could arguably produce the greatest good for the greatest number of people, but the deontological approach could argue this action would be unethical because it does not follow the rule of “do no harm.”
Read more about Decision making on organ donation: The dilemmas of relatives of potential brain dead donors.
Interestingly, deontological and utilitarian approaches to ethical issues may result in the same outcome, but the rationale for the outcome or decision is different because it is focused on duty (deontologic) versus consequences (utilitarian).
Societies and cultures have unique ethical frameworks that may be based upon either deontological or consequentialist ethical theory. Culturally derived deontological rules may apply to ethical issues in health care. For example, a traditional Chinese philosophy based on Confucianism results in a culturally acceptable practice of family members (rather than the client) receiving information from health care providers about life-threatening medical conditions and making treatment decisions. As a result, cancer diagnoses and end-of-life treatment options may not be disclosed to the client in an effort to alleviate the suffering that may arise from knowledge of their diagnosis. In this manner, a client’s family and the health care provider may ethically prioritize a client’s psychological well-being over their autonomy and self-determination.[207] However, in the United States, this ethical decision may conflict with HIPAA Privacy Rules and the ethical principle of patient autonomy. As a result, a nurse providing patient care in this type of situation may experience an ethical dilemma. Ethical dilemmas are further discussed in the "Ethical Dilemmas" section of this chapter.
See Table 6.2 comparing common ethical issues in health care viewed through the lens of deontological and consequential ethical frameworks.
Table 6.2. Ethical Issues Through the Lens of Deontological or Consequential Ethical Frameworks
| Ethical Issue | Deontological View | Consequential View |
|---|---|---|
| Abortion | Abortion is unacceptable based on the rule of preserving life. | Abortion may be acceptable in cases of an unwanted pregnancy, rape, incest, or risk to the mother. |
| Bombing an area with known civilians | Killing civilians is not acceptable due to the loss of innocent lives. | The loss of innocent lives may be acceptable if the bombing stops a war that could result in significantly more deaths than the civilian casualties. |
| Stealing | Taking something that is not yours is wrong. | Taking something to redistribute resources to others in need may be acceptable. |
| Killing | It is never acceptable to take another human being’s life. | It may be acceptable to take another human life in self-defense or to prevent additional harm they could cause others. |
| Euthanasia/physician- assisted suicide | It is never acceptable to assist another human to end their life prematurely. | End-of-life care can be expensive and emotionally upsetting for family members. If a competent, capable adult wishes to end their life, medically supported options should be available. |
| Vaccines | Vaccination is a personal choice based on religious practices or other beliefs. | Recommended vaccines should be mandatory for everyone (without a medical contraindication) because of its greater good for all of society. |
Ethical Principles and Obligations
Ethical principles are used to define nurses’ moral duties and aid in ethical analysis and decision-making.[208] Although there are many ethical principles that guide nursing practice, foundational ethical principles include autonomy (self-determination), beneficence (do good), nonmaleficence (do no harm), justice (fairness), fidelity (keep promises), and veracity (tell the truth).
Autonomy
The ethical principle of autonomy recognizes each individual’s right to self-determination and decision-making based on their unique values, beliefs, and preferences. See Figure 6.4[209] for an illustration of autonomy. The American Nurses Association (ANA) defines autonomy as the “capacity to determine one’s own actions through independent choice, including demonstration of competence.”[210] The nurse’s primary ethical obligation is client autonomy.[211] Based on autonomy, clients have the right to refuse nursing care and medical treatment. An example of autonomy in health care is advance directives. Advance directives allow clients to specify health care decisions if they become incapacitated and unable to do so.
Read more about advance directives and determining capacity and competency in the “Legal Implications” chapter.
Nurses as Advocates: Supporting Autonomy
Nurses have a responsibility to act in the interest of those under their care, referred to as advocacy. The American Nurses Association (ANA) defines advocacy as “the act or process of pleading for, supporting, or recommending a cause or course of action. Advocacy may be for persons (whether an individual, group, population, or society) or for an issue, such as potable water or global health.”[212] See Figure 6.5[213] for an illustration of advocacy.
Advocacy includes providing education regarding client rights, supporting autonomy and self-determination, and advocating for client preferences to health care team members and family members. Nurses do not make decisions for clients, but instead support them in making their own informed choices. At the core of making informed decisions is knowledge. Nurses serve an integral role in patient education. Clarifying unclear information, translating medical terminology, and making referrals to other health care team members (within their scope of practice) ensures that clients have the information needed to make treatment decisions aligned with their personal values.
At times, nurses may find themselves in a position of supporting a client’s decision they do not agree with and would not make for themselves or for the people they love. However, self-determination is a human right that honors the dignity and well-being of individuals. The nursing profession, rooted in caring relationships, demands that nurses have nonjudgmental attitudes and reflect “unconditional positive regard” for every client. Nurses must suspend personal judgement and beliefs when advocating for their clients’ preferences and decision-making.[214]
Beneficence
Beneficence is defined by the ANA as “the bioethical principle of benefiting others by preventing harm, removing harmful conditions, or affirmatively acting to benefit another or others, often going beyond what is required by law.”[215] See Figure 6.6[216] for an illustration of beneficence. Put simply, beneficence is acting for the good and welfare of others, guided by compassion. An example of beneficence in daily nursing care is when a nurse sits with a dying patient and holds their hand to provide presence.

Nursing advocacy extends beyond direct patient care to advocating for beneficence in communities. Vulnerable populations such as children, older adults, cultural minorities, and the homeless often benefit from nurse advocacy in promoting health equity. Cultural humility is a humble and respectful attitude towards individuals of other cultures and an approach to learning about other cultures as a lifelong goal and process.[217] Nurses, the largest segment of the health care community, have a powerful voice when addressing community beneficence issues, such as health disparities and social determinants of health, and can serve as the conduit for advocating for change.
Nonmaleficence
Nonmaleficence is defined by the ANA as “the bioethical principle that specifies a duty to do no harm and balances avoidable harm with benefits of good achieved.”[218] An example of doing no harm in nursing practice is reflected by nurses checking medication rights three times before administering medications. In this manner, medication errors can be avoided, and the duty to do no harm is met. Another example of nonmaleficence is when a nurse assists a client with a serious, life-threatening condition to participate in decision-making regarding their treatment plan. By balancing the potential harm with potential benefits of various treatment options, while also considering quality of life and comfort, the client can effectively make decisions based on their values and preferences.
Justice
Justice is defined by the ANA as “a moral obligation to act on the basis of equality and equity and a standard linked to fairness for all in society.”[219] The principle of justice requires health care to be provided in a fair and equitable way. Nurses provide quality care for all individuals with the same level of fairness despite many characteristics, such as the individual's financial status, culture, religion, gender, or sexual orientation. Nurses have a social contract to “provide compassionate care that addresses the individual’s needs for protection, advocacy, empowerment, optimization of health, prevention of illness and injury, alleviation of suffering, comfort, and well-being.”[220] An example of a nurse using the principle of justice in daily nursing practice is effective prioritization based on client needs.
Read more about prioritization models in the “Prioritization” chapter.
Other Ethical Principles
Additional ethical principles commonly applied to health care include fidelity (keeping promises) and veracity (telling the truth). An example of fidelity in daily nursing practice is when a nurse tells a client, “I will be back in an hour to check on your pain level.” This promise is kept. An example of veracity in nursing practice is when a nurse honestly explains potentially uncomfortable side effects of prescribed medications. Determining how truthfulness will benefit the client and support their autonomy is dependent on a nurse’s clinical judgment, self-reflection, knowledge of the patient and their cultural beliefs, and other factors.[221]
A principle historically associated with health care is paternalism. Paternalism is defined as the interference by the state or an individual with another person, defended by the claim that the person interfered with will be better off or protected from harm.[222] Paternalism is the basis for legislation related to drug enforcement and compulsory wearing of seatbelts.
In health care, paternalism has been used as rationale for performing treatment based on what the provider believes is in the client’s best interest. In some situations, paternalism may be appropriate for individuals who are unable to comprehend information in a way that supports their informed decision-making, but it must be used cautiously to ensure vulnerable individuals are not misused and their autonomy is not violated.
Nurses may find themselves acting paternalistically when performing nursing care to ensure client health and safety. For example, repositioning clients to prevent skin breakdown is a preventative intervention commonly declined by clients when they prefer a specific position for comfort. In this situation, the nurse should explain the benefits of the preventative intervention and the risks if the intervention is not completed. If the client continues to decline the intervention despite receiving this information, the nurse should document the education provided and the client’s decision to decline the intervention. The process of reeducating the client and reminding them of the importance of the preventative intervention should be continued at regular intervals and documented.
Care-Based Ethics
Nurses use a client-centered, care-based ethical approach to patient care that focuses on the specific circumstances of each situation. This approach aligns with nursing concepts such as caring, holism, and a nurse-client relationship rooted in dignity and respect through virtues such as kindness and compassion.[223],[224] This care-based approach to ethics uses a holistic, individualized analysis of situations rather than the prescriptive application of ethical principles to define ethical nursing practice. This care-based approach asserts that ethical issues cannot be handled deductively by applying concrete and prefabricated rules, but instead require social processes that respect the multidimensionality of problems.[225] Frameworks for resolving ethical situations are discussed in the “Ethical Dilemmas” section of this chapter.
Nursing Code of Ethics
Many professions and institutions have their own set of ethical principles, referred to as a code of ethics, designed to govern decision-making and assist individuals to distinguish right from wrong. The American Nurses Association (ANA) provides a framework for ethical nursing care and guides nurses during decision-making in its formal document titled Code of Ethics for Nurses With Interpretive Statements (Nursing Code of Ethics). The Nursing Code of Ethics serves the following purposes[226]:
- It is a succinct statement of the ethical values, obligations, duties, and professional ideals of nurses individually and collectively.
- It is the profession’s nonnegotiable ethical standard.
- It is an expression of nursing’s own understanding of its commitment to society.
The preface of the ANA’s Nursing Code of Ethics states, “Individuals who become nurses are expected to adhere to the ideals and moral norms of the profession and also to embrace them as a part of what it means to be a nurse. The ethical tradition of nursing is self-reflective, enduring, and distinctive. A code of ethics makes explicit the primary goals, values, and obligations of the profession.”[227]
The Nursing Code of Ethics contains nine provisions. Each provision contains several clarifying or “interpretive” statements. Read a summary of the nine provisions in the following box.
Nine Provisions of the ANA Nursing Code of Ethics
- Provision 1: The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person.
- Provision 2: The nurse’s primary commitment is to the patient, whether an individual, family, group, community, or population.
- Provision 3: The nurse promotes, advocates for, and protects the rights, health, and safety of the patient.
- Provision 4: The nurse has authority, accountability, and responsibility for nursing practice; makes decisions; and takes action consistent with the obligation to promote health and to provide optimal care.
- Provision 5: The nurse owes the same duties to self as to others, including the responsibility to promote health and safety, preserve wholeness of character and integrity, maintain competence, and continue personal and professional growth.
- Provision 6: The nurse, through individual and collective effort, establishes, maintains, and improves the ethical environment of the work setting and conditions of employment that are conducive to safe, quality health care.
- Provision 7: The nurse, in all roles and settings, advances the profession through research and scholarly inquiry, professional standards development, and the generation of both nursing and health policy.
- Provision 8: The nurse collaborates with other health professionals and the public to protect human rights, promote health diplomacy, and reduce health disparities.
- Provision 9: The profession of nursing, collectively through its professional organizations, must articulate nursing values, maintain the integrity of the profession, and integrate principles of social justice into nursing and health policy.
Read the free, online full version of the ANA's Code of Ethics for Nurses With Interpretive Statements.
In addition to the Nursing Code of Ethics, the ANA established the Center for Ethics and Human Rights to help nurses navigate ethical conflicts and life-and-death decisions common to everyday nursing practice.
Read more about the ANA Center for Ethics and Human Rights.
Specialty Organization Code of Ethics
Many specialty nursing organizations have additional codes of ethics to guide nurses practicing in settings such as the emergency department, home care, or hospice care. These documents are unique to the specialty discipline but mirror the statements from the ANA’s Nursing Code of Ethics. View ethical statements of various specialty nursing organizations using the information in the following box.
Ethical Statements of Selected Specialty Nursing Organizations
External elements that impact healthcare costs.
This textbook discusses professional and management concepts related to the role of a registered nurse (RN) as defined by the American Nurses Association (ANA). The ANA publishes two resources that set standards and guide professional nursing practice in the United States: The Code of Ethics for Nurses With Interpretive Statements and Nursing: Scope and Standards of Practice. The Code of Ethics for Nurses With Interpretive Statements establishes an ethical framework for nursing practice across all roles, levels, and settings and is discussed in greater detail in the “Ethical Practice” chapter of this book. The Nursing: Scope and Standards of Practice resource defines the “who, what, where, when, why, and how of nursing” and sets the standards for practice that all registered nurses are expected to perform competently.[228]
The ANA defines the “who” of nursing practice as the nurses who have been educated, titled, and maintain active licensure to practice nursing. The “what” of nursing is the recently revised ANA definition of nursing: “Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in recognition of the connection of all humanity.”[229] Simply put, nurses treat human responses to health problems and life processes and advocate for the care of others.
Nursing practice occurs “when'' there is a need for nursing knowledge, wisdom, caring, leadership, practice, or education, anytime, anywhere. Nursing practice occurs in any environment “where'' there is a health care consumer in need of care, information, or advocacy. The “why” of nursing practice is described as nursing’s response to the changing needs of society to achieve positive health care consumer outcomes in keeping with nursing’s social contract and obligation to society. The “how” of nursing practice is defined as the ways, means, methods, and manners that nurses use to practice professionally.[230] The “how” of nursing, also referred to as a nurse’s “scope and standards of practice,” is further defined by each state’s Nurse Practice Act; agency policies, procedures, and protocols; and federal regulations and ANA’s Standards of Practice.
State Boards of Nursing and Nurse Practice Acts
RNs must legally follow regulations set by the Nurse Practice Act by the state in which they are caring for patients with their nursing license. The Board of Nursing is the state-specific licensing and regulatory body that sets standards for safe nursing care and issues nursing licenses to qualified candidates based on the Nurse Practice Act. The Nurse Practice Act is enacted by that state’s legislature and defines the scope of nursing practice and establishes regulations for nursing practice within that state. If nurses do not follow the standards and scope of practice set forth by the Nurse Practice Act, they may be disciplined by the Board of Nursing in the form of reprimand, probation, suspension, or revocation of their nursing license. Investigations and discipline actions are reportable among states participating in the Nurse Licensure Compact (that allows nurses to practice across state lines) or when a nurse applies for licensure in a different state. The scope and standards of practice set forth in the Nurse Practice Act can also be used as evidence if a nurse is sued for malpractice.
Find your state's Nurse Practice Act on the National Council of State Board of Nursing (NCSBN) website.
Read more about malpractice and protecting your nursing license in the “Legal Implications” chapter of this book.
Read Wisconsin’s Nurse Practice Act, Standards of Practice for Registered Nurses and Licensed Practical Nurses (Chapter N6) PDF, and Rules of Conduct (Chapter N7) PDF.
Agency Policies, Procedures, and Protocols
In addition to practicing according to the Nurse Practice Act in the state they are employed, nurses must also practice according to agency policies, procedures, and protocols.
A policy is an expected course of action set by an agency. For example, hospitals set a policy requiring a thorough skin assessment to be completed when a patient is admitted and then reassessed and documented daily.
Agencies also establish their own set of procedures. A procedure is the method or defined steps for completing a task. For example, each agency has specific procedural steps for inserting a urinary catheter.
A protocol is a detailed, written plan for performing a regimen of therapy. For example, agencies typically establish a hypoglycemia protocol that nurses can independently and quickly implement when a patient’s blood sugar falls below a specific number without first calling a provider. A hypoglycemia protocol typically includes actions such as providing orange juice and rechecking the blood sugar and then reporting the incident to the provider.
Agency-specific policies, procedures, and protocols supersede the information taught in nursing school, and nurses can be held legally liable if they don’t follow them. It is vital for nurses to review and follow current agency-specific procedures, policies, and protocols while also practicing according to that state's nursing scope of practice. Malpractice cases have occurred when a nurse was asked by their employer to do something outside their legal scope of practice, impacting their nursing license. It is up to you to protect your nursing license and follow the Nurse Practice Act when providing patient care. If you have a concern about an agency’s policy, procedure, or protocol, follow the agency’s chain of command to report your concern.
Federal Regulations
Nursing practice is impacted by regulations enacted by federal agencies. Two examples of federal agencies setting standards of care are The Joint Commission and the Centers for Medicare and Medicaid Services.
The Joint Commission accredits and certifies over 20,000 health care organizations in the United States. The Joint Commission’s standards help health care organizations measure, assess, and improve performance on functions that are essential to providing safe, high-quality care. The standards are updated regularly to reflect the rapid advances in health care and address topics such as patient rights and education, infection control, medication management, and prevention of medical errors. The annual National Patient Safety Goals are also set by The Joint Commission after reviewing emerging patient safety issues.[231]
The Centers for Medicare & Medicaid Services (CMS) is an example of another federal agency that establishes regulations affecting nursing care. CMS is a part of the U.S. Department of Health and Human Services (HHS) that administers the Medicare program and works in partnership with state governments to administer Medicaid. The CMS establishes and enforces regulations to protect patient safety in hospitals that receive Medicare and Medicaid funding. For example, one CMS regulation often referred to as “checking the rights of medication administration” requires nurses to confirm specific information several times before medication is administered to a patient.[232]
Standards of Practice
The ANA defines Standards of Professional Nursing Practice as “authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently.”[233] These standards are classified into two categories: Standards of Practice and Standards of Professional Performance.
The ANA’s Standards of Practice describe a competent level of nursing practice as demonstrated by the critical thinking model known as the nursing process. The nursing process includes the components of assessment, diagnosis, outcomes identification, planning, implementation, and evaluation and forms the foundation of the nurse’s decision-making, practice, and provision of care.[234]
Read more information about the nursing process in the “Nursing Process” chapter of Open RN Nursing Fundamentals, 2e.[235]
The ANA’s Standards of Professional Performance “describe a competent level of behavior in the professional role, including activities related to ethics, advocacy, respectful and equitable practice, communication, collaboration, leadership, education, scholarly inquiry, quality of practice, professional practice evaluation, resource stewardship, and environmental health. All registered nurses are expected to engage in professional role activities, including leadership, reflective of their education, position, and role.”[236] This book discusses content related to these professional practice standards. Each professional practice standard is defined in the following sections with information provided to related content in this book and the Open RN Nursing Fundamentals, 2e textbook.[237]
Ethics
The ANA’s Ethics standard states, “The registered nurse integrates ethics in all aspects of practice.”[238]
Read about ethical nursing practice in the “Ethical Practice” chapter of this book.
Advocacy
The ANA’s Advocacy standard states, “The registered nurse demonstrates advocacy in all roles and settings.”[239]
Read about nurse advocacy in the “Advocacy” chapter of this book.
Respectful and Equitable Practice
The ANA’s Respectful and Equitable Practice standard states, “The registered nurse practices with cultural humility and inclusiveness.”
Read about cultural humility and culturally responsive care in the “Diverse Patients” chapter in Open RN Nursing Fundamentals, 2e.[240]
Communication
The ANA’s Communication standard states, “The registered nurse communicates effectively in all areas of professional practice.”[241]
Read about communicating with clients and team members in the “Communication” chapter in Open RN Nursing Fundamentals, 2e.[242]
Read about interprofessional communication strategies that promote patient safety in the “Collaboration Within the Interprofessional Team” chapter of this book.
Collaboration
The ANA’s Collaboration standard states, “The registered nurse collaborates with the health care consumer and other key stakeholders.”[243]
Read about strategies to enhance the performance of the interprofessional team and manage conflict in the “Collaboration Within the Interprofessional Team” chapter of this book.
Leadership
The ANA’s Leadership standard states, “The registered nurse leads within the profession and practice setting.”[244]
Read about leadership, management, and implementing change in the “Leadership and Management” chapter of this book.
Read about assigning, delegating, and supervising patient care in the “Delegation and Supervision” chapter of this book.
Read about tools for prioritizing patient care and managing resources for the nursing team in the “Prioritization” chapter of this book.
Education
The ANA’s Education standard states, “The registered nurse seeks knowledge and competence that reflects current nursing practice and promotes futuristic thinking.”[245]
Read about professional development and specialty certification in the “Preparation for the RN Role” chapter of this book.
Scholarly Inquiry
The ANA’s Scholarly Inquiry standard states, “The registered nurse integrates scholarship, evidence, and research findings into practice.”[246]
Read about integrating evidence-based practice into one’s nursing practice in the “Quality and Evidence-Based Practice” chapter of this book.
Quality of Practice
The ANA’s Quality of Practice standard states, “The nurse contributes to quality nursing practice.”[247]
Read about improving quality patient care and participating in quality improvement initiatives in the “Quality and Evidence-Based Practice” chapter of this book.
Professional Practice Evaluation
The ANA’s Professional Practice Evaluation standard states, “The registered nurse evaluates one’s own and others’ nursing practice.”[248]
Read about nursing practice within the legal framework of health care, negligence, malpractice, and protecting your nursing license in the “Legal Implications” chapter of this book.
Read about reviewing the interprofessional team’s performance, providing constructive feedback, and advocating for patient safety with assertive statements in the “Collaboration Within the Interprofessional Team” chapter of this book.
Resource Stewardship
The ANA’s Resource Stewardship standard states, “The registered nurse utilizes appropriate resources to plan, provide, and sustain evidence-based nursing services that are safe, effective, financially responsible, and used judiciously.”[249]
Read more about health care funding, reimbursement models, budgets and staffing, and resource stewardship in the “Health Care Economics” chapter of this book.
Environmental Health
The ANA’s Environmental Health standard states, “The registered nurse practices in a manner that advances environmental safety and health.”[250]
Read about promoting workplace safety for nurses in the “Safety” chapter in Open RN Nursing Fundamentals, 2e.[251]
Read about fostering a professional environment that does not tolerate abusive behaviors in the “Collaboration Within the Interprofessional Team” chapter of this book.
Read about addressing the impacts of social determinants of health in the “Advocacy” chapter of this book.

