7.3 Common Conditions of the Head and Neck
Open Resources for Nursing (Open RN)
Headache
A headache is a common type of pain that patients experience in everyday life and a major reason for missed time at work or school. Headaches range greatly in severity of pain and frequency of occurrence. For example, some patients experience mild headaches once or twice a year, whereas others experience disabling migraine headaches more than 15 days a month. Severe headaches such as migraines may be accompanied by symptoms of nausea or increased sensitivity to noise or light. Primary headaches occur independently and are not caused by another medical condition. Migraine, cluster, and tension-type headaches are types of primary headaches. Secondary headaches are symptoms of another health disorder that causes pain-sensitive nerve endings to be pressed on or pulled out of place. They may result from underlying conditions including fever, infection, medication overuse, stress or emotional conflict, high blood pressure, psychiatric disorders, head injury or trauma, stroke, tumors, and nerve disorders such as trigeminal neuralgia, a chronic pain condition that typically affects the trigeminal nerve on one side of the cheek.[1]
Not all headaches require medical attention, but some types of headaches can signify a serious disorder and require prompt medical care. Symptoms of headaches that require immediate medical attention include a sudden, severe headache unlike any the patient has ever had; a sudden headache associated with a stiff neck; a headache associated with convulsions, confusion, or loss of consciousness; a headache following a blow to the head; or a persistent headache in a person who was previously headache free.[2]
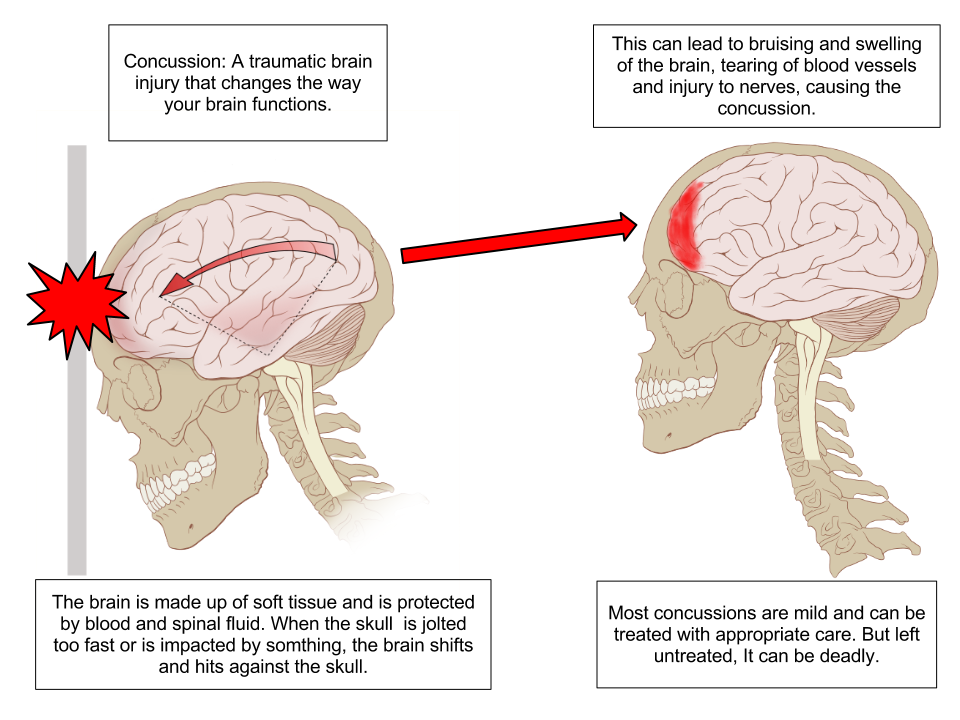
Concussion
A concussion is a type of traumatic brain injury caused by a blow to the head or by a hit to the body that causes the head and brain to move rapidly back and forth. This sudden movement causes the brain to bounce around in the skull, creating chemical changes in the brain and sometimes damaging brain cells.[3] See Figure 7.14[4] for an illustration of a concussion.
Review of Concussions on YouTube[5]
A person who has experienced a concussion may report the following symptoms:
- Headache or “pressure” in head
- Nausea or vomiting
- Balance problems or dizziness or double or blurry vision
- Light or noise sensitivity
- Feeling sluggish, hazy, foggy, or groggy
- Confusion, concentration, or memory problems
- Just not “feeling right” or “feeling down”[6]
The following signs may be observed in someone who has experienced a concussion:
- Can’t recall events prior to or after a hit or fall
- Appears dazed or stunned
- Forgets an instruction, is confused about an assignment or position, or is unsure of the game, score, or opponent
- Moves clumsily
- Answers questions slowly
- Loses consciousness (even briefly)
- Shows mood, behavior, or personality changes[7]
Anyone suspected of experiencing a concussion should immediately be seen by a health care provider or go to the emergency department for further testing.
Read more information about concussion signs and symptoms on the CDC’s Concussion Signs and Symptoms webpage.
Head Injury
Head and traumatic brain injuries are major causes of immediate death and disability. Falls are the most common cause of head injuries in young children (ages 0–4 years), adolescents (15–19 years), and the elderly (over 65 years). Strong blows to the brain case of the skull can produce fractures resulting in bleeding inside the skull. A blow to the lateral side of the head may fracture the bones of the pterion. If the underlying artery is damaged, bleeding can cause the formation of a hematoma (collection of blood) between the brain and interior of the skull. As blood accumulates, it will put pressure on the brain. Symptoms associated with a hematoma may not be apparent immediately following the injury, but if untreated, blood accumulation will continue to exert increasing pressure on the brain and can result in death within a few hours.[8]
See Figure 7.15[9] for an image of an epidural hematoma indicated by a red arrow associated with a skull fracture.

Sinusitis
Sinusitis is the medical diagnosis for inflamed sinuses that can be caused by a viral or bacterial infection. When the nasal membranes become swollen, the drainage of mucous is blocked and causes pain.
There are several types of sinusitis, including these types:
- Acute Sinusitis: Infection lasting up to 4 weeks
- Chronic Sinusitis: Infection lasting more than 12 weeks
- Recurrent Sinusitis: Several episodes of sinusitis within a year
Symptoms of sinusitis can include fever, weakness, fatigue, cough, and congestion. There may also be mucus drainage in the back of the throat, called postnasal drip. Health care providers diagnose sinusitis based on symptoms and an examination of the nose and face. Treatments include antibiotics, decongestants, and pain relievers.[10]
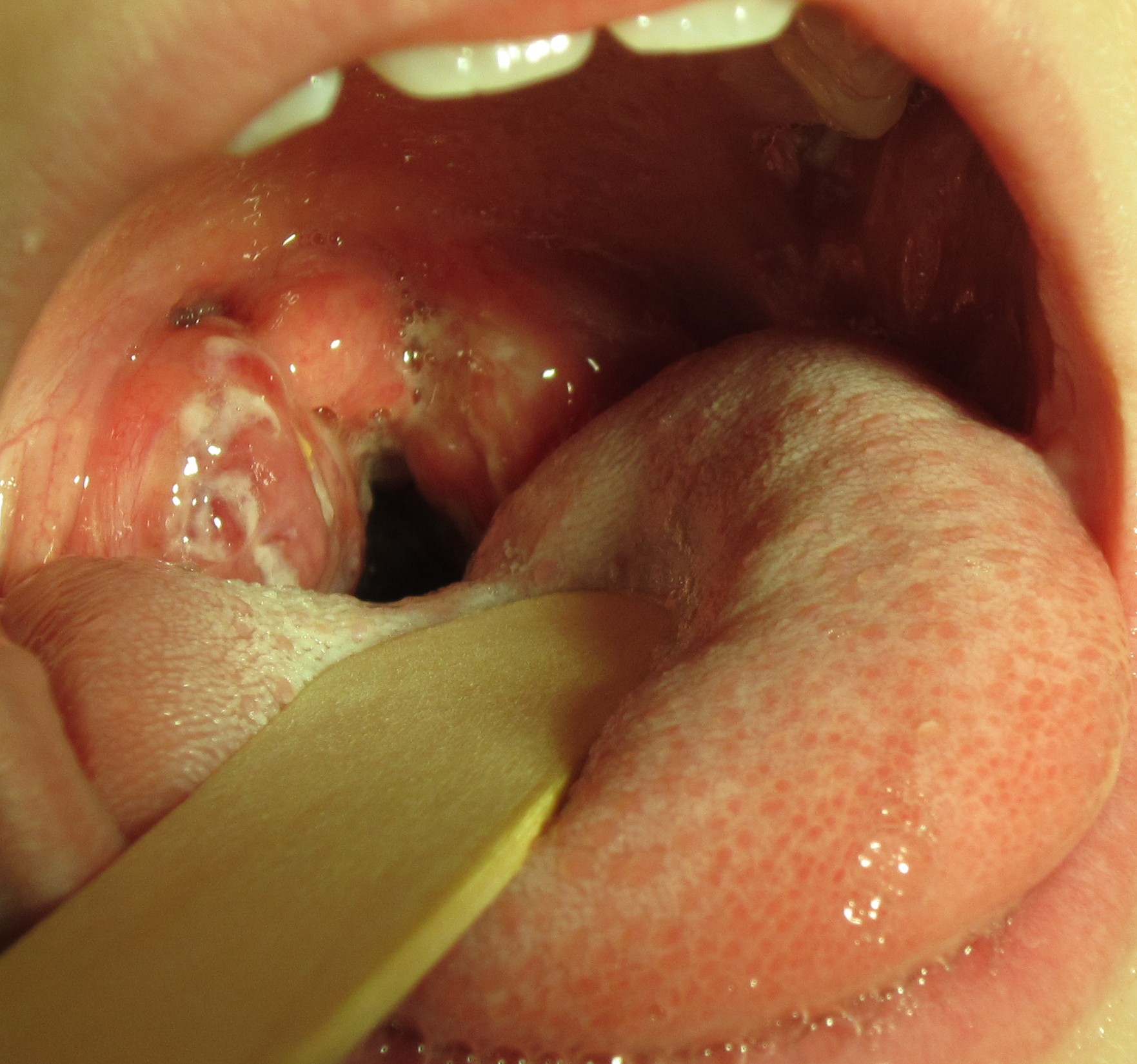
Pharyngitis
Pharyngitis is the medical term used for infection and/or inflammation in the back of the throat (pharynx). Common causes of pharyngitis are the cold viruses, influenza, strep throat caused by group A streptococcus, and mononucleosis. Strep throat typically causes white patches on the tonsils with a fever and enlarged lymph nodes. It must be treated with antibiotics to prevent potential complications in the heart and kidneys. See Figure 7.16[11] for an image of strep throat in a child.
If not diagnosed as strep throat, most cases of pharyngitis are caused by viruses, and the treatment is aimed at managing the symptoms. Nurses can teach patients the following ways to decrease the discomfort of a sore throat:
- Drink soothing liquids such as lemon tea with honey or ice water.
- Gargle several times a day with warm salt water made of 1/2 tsp. of salt in 1 cup of water.
- Suck on hard candies or throat lozenges.
- Use a cool-mist vaporizer or humidifier to moisten the air.
- Try over-the-counter pain medicines, such as acetaminophen.[12]
Epistaxis
Epistaxis, the medical term for a nosebleed, is a common problem affecting up to 60 million Americans each year. Although most cases of epistaxis are minor and manageable with conservative measures, severe cases can become life-threatening if the bleeding cannot be stopped.[13] See Figure 7.17[14] for an image of a severe case of epistaxis.

The most common cause of epistaxis is dry nasal membranes in winter months due to low temperatures and low humidity. Other common causes are picking inside the nose with fingers, trauma, anatomical deformity, high blood pressure, and clotting disorders. Medications associated with epistaxis are aspirin, clopidogrel, nonsteroidal anti-inflammatory drugs, and anticoagulants.[15]
To treat a nosebleed, have the victim lean forward at the waist and pinch the lateral sides of the nose with the thumb and index finger for up to 15 minutes while breathing through the mouth.[16] Continued bleeding despite this intervention requires urgent medical intervention such as nasal packing.
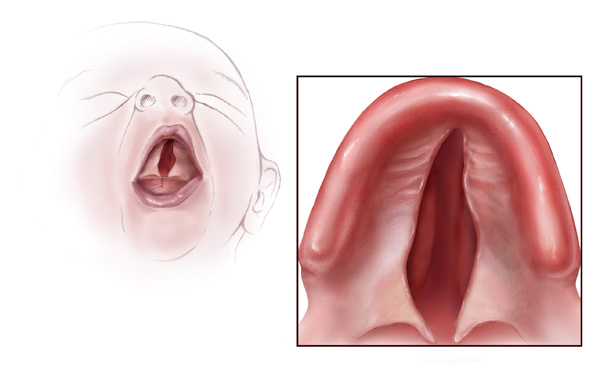
Cleft Lip and Palate
During embryonic development, the right and left maxilla bones come together at the midline to form the upper jaw. At the same time, the muscle and skin overlying these bones join together to form the upper lip. Inside the mouth, the palatine processes of the maxilla bones, along with the horizontal plates of the right and left palatine bones, join together to form the hard palate. If an error occurs in these developmental processes, a birth defect of cleft lip or cleft palate may result.
Cleft lip is a common developmental defect that affects approximately 1:1,000 births, most of which are male. This defect involves a partial or complete failure of the right and left portions of the upper lip to fuse together, leaving a cleft (gap). See Figure 7.18[17] for an image of an infant with a cleft lip.

A more severe developmental defect is a cleft palate that affects the hard palate, the bony structure that separates the nasal cavity from the oral cavity. See Figure 7.19[18] for an illustration of a cleft palate. Cleft palate affects approximately 1:2,500 births and is more common in females. It results from a failure of the two halves of the hard palate to completely come together and fuse at the midline, thus leaving a gap between the nasal and oral cavities. In severe cases, the bony gap continues into the anterior upper jaw where the alveolar processes of the maxilla bones also do not properly join together above the front teeth. If this occurs, a cleft lip will also be seen. Because of the communication between the oral and nasal cavities, a cleft palate makes it very difficult for an infant to generate the suckling needed for nursing, thus creating risk for malnutrition. Surgical repair is required to correct a cleft palate.[19]
Poor Oral Health
Despite major improvements in oral health for the population as a whole, oral health disparities continue to exist for many racial, ethnic, and socioeconomic groups in the United States. Healthy People 2020, a nationwide initiative geared to improve the health of Americans, identified improved oral health as a health care goal. A growing body of evidence has also shown that periodontal disease is associated with negative systemic health consequences. Periodontal diseases are infections and inflammation of the gums and bone that surround and support the teeth. Red, swollen, and bleeding gums are signs of periodontal disease. Other symptoms of periodontal disease include bad breath, loose teeth, and painful chewing.[20] In 2020, the Centers for Disease Control and Prevention (CDC) reported that 42% of U.S. adults have some form of periodontitis, and almost 60% of adults aged 65 and older have periodontitis. See Figure 7.20[21] for an image of a patient with periodontal disease. Nurses may encounter patients who complain of bleeding gums, or they may discover other signs of periodontal disease during a physical assessment.

Because many Americans lack access to oral care, it is important for nurses to perform routine oral assessment and identify needs for follow-up. If signs and/or symptoms indicate potential periodontal disease, the patient should be referred to a dental health professional for a more thorough evaluation.[22]
Thrush/Candidiasis
Candidiasis is a fungal infection caused by Candida. Candida normally lives on the skin and inside the body without causing any problems, but it can multiply and cause an infection if the environment inside the mouth, throat, or esophagus changes in a way that encourages fungal growth.[23] See Figure 7.21[24] for an image of candidiasis.

Candidiasis in the mouth and throat can have many symptoms, including the following:
- White patches on the inner cheeks, tongue, roof of the mouth, and throat
- Redness or soreness
- Cotton-like feeling in the mouth
- Loss of taste
- Pain while eating or swallowing
- Cracking and redness at the corners of the mouth[25]
Candidiasis in the mouth or throat is common in babies but is uncommon in healthy adults. Risk factors for getting candidiasis as an adult include the following:
- Wearing dentures
- Diabetes
- Cancer
- HIV/AIDS
- Taking antibiotics or corticosteroids including inhaled corticosteroids for conditions like asthma
- Taking medications that cause dry mouth or have medical conditions that cause dry mouth
- Smoking
The treatment for mild to moderate cases of candidiasis infections in the mouth or throat is typically an antifungal medicine applied to the inside of the mouth for 7 to 14 days, such as clotrimazole, miconazole, or nystatin.
“Meth Mouth”
The use of methamphetamine (i.e., meth), a strong stimulant drug, has become an alarming public health issue in the United States. A common sign of meth abuse is extreme tooth and gum decay often referred to as “Meth Mouth.” See Figure 7.22[26] for an image of Meth Mouth.

Signs of Meth Mouth include the following:
- Dry Mouth. Methamphetamines dry out the salivary glands, and the acid content in the mouth will start to destroy the enamel on the teeth. Eventually this will lead to cavities.
- Cracked Teeth. Methamphetamine can make the user feel anxious, hyper, or nervous, so they clench or grind their teeth. You may see severe wear patterns on their teeth.
- Tooth Decay. Methamphetamine users crave beverages high in sugar while they are “high.” The bacteria that feed on the sugars in the mouth will secrete acid, which can lead to more tooth destruction. With methamphetamine users, tooth decay will start at the gum line and eventually spread throughout the tooth. The front teeth are usually destroyed first.
- Gum Disease. Methamphetamine users do not seek out regular dental treatment. Lack of oral health care can contribute to periodontal disease. Methamphetamines also cause the blood vessels that supply the oral tissues to shrink in size, reducing blood flow, causing the tissues to break down.
- Lesions. Users who smoke methamphetamine may present with lesions and/or burns on their lips or gingival inside the cheeks or on the hard palate. Users who snort may present with burns in the back of their throats.[27]
Nurses who notice possible signs of “Meth Mouth” should report their concerns to the health care provider, not only for a referral for dental care, but also for treatment of suspected substance abuse.
Dysphagia
Dysphagia is the medical term for difficulty swallowing that can be caused by many medical conditions. Nurses are often the first health care professionals to notice a patient’s difficulty swallowing as they administer medications or monitor food intake. Early identification of dysphagia, especially after a patient has experienced a cerebrovascular accident (i.e., stroke) or other head injury, helps to prevent aspiration pneumonia.[28] Aspiration pneumonia is a type of lung infection caused by material from the stomach or mouth entering the lungs and can be life-threatening.
Signs of dysphagia include the following:
- Coughing during or right after eating or drinking
- Wet or gurgly sounding voice during or after eating or drinking
- Extra effort or time required to chew or swallow
- Food or liquid leaking from mouth
- Food getting stuck in the mouth
- Difficulty breathing after meals[29]
The Barnes-Jewish Hospital-Stroke Dysphagia Screen (BJH-SDS) is an example of a simple, evidence-based bedside screening tool that can be used by nursing staff to efficiently identify swallowing impairments in patients who have experienced a stroke. See internet resource below for an image of the dysphagia screening tool. The result of the screening test is recorded as a “fail” if any of the five items tested are abnormal (Glasgow Coma Scale < 13, facial/tongue/palatal asymmetry or weakness, or signs of aspiration on the 3-ounce water test) or “pass” if all five items tested were normal. Patients with a failed screening result are placed on nothing-by-mouth (NPO) status until further evaluation is completed by a speech therapist. For more information about using the Glasgow Coma Scale, see the “Assessing Mental Status” section in the “Neurological Assessment” chapter.
View a PDF sample of a Nursing Bedside Swallow Screen.
Enlarged Lymph Nodes
Lymphadenopathy is the medical term for swollen lymph nodes. In a child, a node is considered enlarged if it is more than 1 centimeter (0.4 inch) wide. See Figure 7.23[30] for an image of an enlarged cervical lymph node.

Common infections such as a cold, pharyngitis, sinusitis, mononucleosis, strep throat, ear infection, or infected tooth often cause swollen lymph nodes. However, swollen lymph nodes can also signify more serious conditions. Notify the health care provider if the patient’s lymph nodes have the following characteristics:
- Do not decrease in size after several weeks or continue to get larger
- Are red and tender
- Feel hard, irregular, or fixed in place
- Are associated with night sweats or unexplained weight loss
- Are larger than 1 centimeter in diameter
The health care provider may order blood tests, a chest X-ray, or a biopsy of the lymph node if these signs occur.[31]
Thyroid
The thyroid is a butterfly-shaped gland located at the front of the neck that controls many of the body’s important functions. The thyroid gland makes hormones that affect breathing, heart rate, digestion, and body temperature. If the thyroid makes too much or not enough thyroid hormone, many body systems are affected. In hypothyroidism, the thyroid gland doesn’t produce enough hormone and many body functions slow down. When the thyroid makes too much hormone, a condition called hyperthyroidism, many body systems speed up.[32]
A goiter is an abnormal enlargement of the thyroid gland that can occur with hypothyroidism or hyperthyroidism. If you find a goiter when assessing a patient’s neck, notify the health care provider for additional testing and treatment. See Figure 7.24[33] for an image of a goiter.

- National Institute of Neurological Disorders and Stroke. (2019, December 31). Headache information page. https://www.ninds.nih.gov/Disorders/All-Disorders/Headache-Information-Page ↵
- National Institute of Neurological Disorders and Stroke. (2019, December 31). Headache information page. https://www.ninds.nih.gov/Disorders/All-Disorders/Headache-Information-Page ↵
- Centers for Disease Control and Prevention. (2019, February 12). Concussion signs and symptoms. https://www.cdc.gov/headsup/basics/concussion_symptoms.html ↵
- “Concussion Anatomy.png” by Max Andrews is licensed under CC BY-SA 3.0 ↵
- Centers for Disease Control and Prevention. (2013, October 24). What is a concussion? [Video]. YouTube. All rights reserved. https://youtu.be/Sno_0Jd8GuA ↵
- Centers for Disease Control and Prevention. (2019, February 12). Concussion signs and symptoms. https://www.cdc.gov/headsup/basics/concussion_symptoms.html ↵
- Centers for Disease Control and Prevention. (2019, February 12). Concussion signs and symptoms. https://www.cdc.gov/headsup/basics/concussion_symptoms.html ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “EpiduralHeatoma.jpg” by James Heilman, MD is licensed under CC BY-SA 4.0 ↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2020, Aug 17]. Sinusitis; [updated 2020, Jun 10; reviewed 2016, Oct 26]; [cited 2020, Sep 4]; https://medlineplus.gov/sinusitis.html ↵
- “Strep throat2010.JPG” by James Heilman, MD is licensed under CC BY-SA 3.0 ↵
- Centers for Disease Control and Prevention. (2020, May 1). Disparities in oral health. https://www.cdc.gov/OralHealth/oral_health_disparities/ ↵
- Fatakia, A., Winters, R., & Amedee, R. G. (2010). Epistaxis: A common problem. The Ochsner Journal, 10(3), 176–178. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3096213/ ↵
- “Epstaxis1.jpg” by Welleschik is licensed under CC BY-SA 3.0 ↵
- Fatakia, A., Winters, R., & Amedee, R. G. (2010). Epistaxis: A common problem. The Ochsner Journal, 10(3), 176–178. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3096213/ ↵
- American Heart Association. (2000). Part 5: New guidelines for first aid. Circulation, 102(supplement 1). https://www.ahajournals.org/doi/10.1161/circ.102.suppl_1.I-77 ↵
- “Cleftlipandpalate.JPG” by James Heilman, MD is licensed under CC BY-SA 3.0 ↵
- “Cleft palate.jpg” by Centers for Disease Control and Prevention is licensed under CC0 1.0 ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- Bencosme, J. (2018). Periodontal disease: What nurses need to know. Nursing, 48(7), 22-27. https://doi.org/10.1097/01.nurse.0000534088.56615.e4 ↵
- “Periodontal Disease.png” by Warren Schnider is licensed under CC BY-SA 4.0 ↵
- Bencosme, J. (2018). Periodontal disease: What nurses need to know. Nursing, 48(7), 22-27. https://doi.org/10.1097/01.nurse.0000534088.56615.e4. ↵
- Centers for Disease Control and Prevention. (2020, June 15). Candida infections of the mouth, throat, and esophagus. https://www.cdc.gov/fungal/diseases/candidiasis/thrush/index.html ↵
- “Human tongue infected with oral candidiasis.jpg” by James Heilman, MD is licensed under CC BY-SA 3.0 ↵
- Centers for Disease Control and Prevention. (2020, June 15). Candida infections of the mouth, throat, and esophagus. https://www.cdc.gov/fungal/diseases/candidiasis/thrush/index.html ↵
- “Suspectedmethmouth09-19-05closeup.jpg” by Dozenist is licensed under CC BY-SA 3.0 ↵
- Maine Center for Disease Control and Prevention. (n.d.). Meth mouth. https://www.maine.gov/dhhs/mecdc/population-health/odh/documents/meth-mouth.pdf ↵
- Edmiaston, J., Connor, L. T., Steger-May, K., & Ford, A. L. (2014). A simple bedside stroke dysphagia screen, validated against videofluoroscopy, detects dysphagia and aspiration with high sensitivity. Journal of Stroke and Cerebrovascular Diseases: The Official Journal of National Stroke Association, 23(4), 712–716. https://doi.org/10.1016/j.jstrokecerebrovasdis.2013.06.030 ↵
- American Speech-Language-Hearing Association. (n.d.). Swallowing disorders in adults. https://www.asha.org/public/speech/swallowing/Swallowing-Disorders-in-Adults/ ↵
- “Cervical lymphadenopathy right neck.png” by Coronation Dental Specialty Group is licensed under CC BY-SA 4.0 ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Johns Creek (GA): Ebix, Inc., A.D.A.M.; c1997-2020. Swollen lymph nodes; [updated 2020, Aug 25; cited 2020, Sep 4]; https://medlineplus.gov/ency/article/003097.htm ↵
- National Institutes of Health. (2015). Thinking about your thyroid. https://newsinhealth.nih.gov/2015/09/thinking-about-your-thyroid ↵
- “Struma 00a.jpg” by Drahreg01 is licensed under CC BY-SA 3.0 ↵
Change is constant in the health care environment. Change is defined as the process of altering or replacing existing knowledge, skills, attitudes, systems, policies, or procedures.[1] The outcomes of change must be consistent with an organization’s mission, vision, and values. Although change is a dynamic process that requires alterations in behavior and can cause conflict and resistance, change can also stimulate positive behaviors and attitudes and improve organizational outcomes and employee performance. Change can result from identified problems or from the incorporation of new knowledge, technology, management, or leadership. Problems may be identified from many sources, such as quality improvement initiatives, employee performance evaluations, or accreditation survey results.[2]
Nurse managers must deal with the fears and concerns triggered by change. They should recognize that change may not be easy and may be met with enthusiasm by some and resistance by others. Leaders should identify individuals who will be enthusiastic about the change (referred to as “early adopters”), as well as those who will be resisters (referred to as "laggers"). Early adopters should be involved to build momentum, and the concerns of resisters should be considered to identify barriers. Data should be collected, analyzed, and communicated so the need for change (and its projected consequences) can be clearly articulated. Managers should articulate the reasons for change, the way(s) the change will affect employees, the way(s) the change will benefit the organization, and the desired outcomes of the change process.[3] See Figure 4.5[4] for an illustration of communicating upcoming change.

Change Theories
There are several change theories that nurse leaders may adopt when implementing change. Two traditional change theories are known as Lewin’s Unfreeze-Change-Refreeze Model and Lippitt’s Seven-Step Change Theory.[5]
Lewin’s Change Model
Kurt Lewin, the father of social psychology, introduced the classic three-step model of change known as Unfreeze-Change-Refreeze Model that requires prior learning to be rejected and replaced. Lewin’s model has three major concepts: driving forces, restraining forces, and equilibrium. Driving forces are those that push in a direction and cause change to occur. They facilitate change because they push the person in a desired direction. They cause a shift in the equilibrium towards change. Restraining forces are those forces that counter the driving forces. They hinder change because they push the person in the opposite direction. They cause a shift in the equilibrium that opposes change. Equilibrium is a state of being where driving forces equal restraining forces, and no change occurs. It can be raised or lowered by changes that occur between the driving and restraining forces.[6],[7]
- Step 1: Unfreeze the status quo. Unfreezing is the process of altering behavior to agitate the equilibrium of the current state. This step is necessary if resistance is to be overcome and conformity achieved. Unfreezing can be achieved by increasing the driving forces that direct behavior away from the existing situation or status quo while decreasing the restraining forces that negatively affect the movement from the existing equilibrium. Nurse leaders can initiate activities that can assist in the unfreezing step, such as motivating participants by preparing them for change, building trust and recognition for the need to change, and encouraging active participation in recognizing problems and brainstorming solutions within a group.[8]
- Step 2: Change. Change is the process of moving to a new equilibrium. Nurse leaders can implement actions that assist in movement to a new equilibrium by persuading employees to agree that the status quo is not beneficial to them; encouraging them to view the problem from a fresh perspective; working together to search for new, relevant information; and connecting the views of the group to well-respected, powerful leaders who also support the change.[9]
- Step 3: Refreeze. Refreezing refers to attaining equilibrium with the newly desired behaviors. This step must take place after the change has been implemented for it to be sustained over time. If this step does not occur, it is very likely the change will be short-lived and employees will revert to the old equilibrium. Refreezing integrates new values into community values and traditions. Nursing leaders can reinforce new patterns of behavior and institutionalize them by adopting new policies and procedures.[10]
Example Using Lewin’s Change Theory
A new nurse working in a rural medical-surgical unit identifies that bedside handoff reports are not currently being used during shift reports.
Step 1: Unfreeze: The new nurse recognizes a change is needed for improved patient safety and discusses the concern with the nurse manager. Current evidence-based practice is shared regarding bedside handoff reports between shifts for patient safety.[11] The nurse manager initiates activities such as scheduling unit meetings to discuss evidence-based practice and the need to incorporate bedside handoff reports.
Step 2: Change: The nurse manager gains support from the director of nursing to implement organizational change and plans staff education about bedside report checklists and the manner in which they are performed.
Step 3: Refreeze: The nurse manager adopts bedside handoff reports in a new unit policy and monitors staff for effectiveness.
Lippitt’s Seven-Step Change Theory
Lippitt’s Seven-Step Change Theory expands on Lewin’s change theory by focusing on the role of the change agent. A change agent is anyone who has the skill and power to stimulate, facilitate, and coordinate the change effort. Change agents can be internal, such as nurse managers or employees appointed to oversee the change process, or external, such as an outside consulting firm. External change agents are not bound by organizational culture, politics, or traditions, so they bring a different perspective to the situation and challenge the status quo. However, this can also be a disadvantage because external change agents lack an understanding of the agency's history, operating procedures, and personnel.[12] The seven-step model includes the following steps[13]:
- Step 1: Diagnose the problem. Examine possible consequences, determine who will be affected by the change, identify essential management personnel who will be responsible for fixing the problem, collect data from those who will be affected by the change, and ensure those affected by the change will be committed to its success.
- Step 2: Evaluate motivation and capability for change. Identify financial and human resources capacity and organizational structure.
- Step 3: Assess the change agent’s motivation and resources, experience, stamina, and dedication.
- Step 4: Select progressive change objectives. Define the change process and develop action plans and accompanying strategies.
- Step 5: Explain the role of the change agent to all employees and ensure the expectations are clear.
- Step 6: Maintain change. Facilitate feedback, enhance communication, and coordinate the effects of change.
- Step 7: Gradually terminate the helping relationship of the change agent.
Example Using Lippitt’s Seven-Step Change Theory
Refer to the previous example of using Lewin’s change theory on a medical-surgical unit to implement bedside handoff reporting. The nurse manager expands on the Unfreeze-Change-Refreeze Model by implementing additional steps based on Lippitt’s Seven-Step Change Theory:
- The nurse manager collects data from team members affected by the changes and ensures their commitment to success.
- Early adopters are identified as change agents on the unit who are committed to improving patient safety by implementing evidence-based practices such as bedside handoff reporting.
- Action plans (including staff education and mentoring), timelines, and expectations are clearly communicated to team members as progressive change objectives. Early adopters are trained as “super-users” to provide staff education and mentor other nurses in using bedside handoff checklists across all shifts.
- The nurse manager facilitates feedback and encourages two-way communication about challenges as change is implemented on the unit. Positive reinforcement is provided as team members effectively incorporate change.
- Bedside handoff reporting is implemented as a unit policy, and all team members are held accountable for performing accurate bedside handoff reporting.
Read more about additional change theories in the Current Theories of Change Management pdf.
Change Management
Change management is the process of making changes in a deliberate, planned, and systematic manner.[14] It is important for nurse leaders and nurse managers to remember a few key points about change management[15]:
- Employees will react differently to change, no matter how important or advantageous the change is purported to be. Recognizing this variability is crucial for effectively managing the transition process.
- Basic needs will influence reaction to change, such as the need to be part of the change process, the need to be able to express oneself openly and honestly, and the need to feel that one has some control over the impact of change. Ensuring these needs are met can significantly reduce resistance.
- Change often results in a feeling of loss due to changes in established routines. Employees may react with shock, anger, and resistance, but ideally will eventually accept and adopt change. Acknowledging these feelings and providing support can facilitate smoother transitions.
- Change must be managed realistically, without false hopes and expectations, yet with enthusiasm for the future. Employees should be provided information honestly and allowed to ask questions and express concerns. This transparency builds trust and helps in aligning everyone towards common goals.
Strategies for Effective Change Management
- Engage Stakeholders Early: Involve key stakeholders in the planning stages of the change process. Their input can provide valuable insights and help in identifying potential challenges early on.
- Communicate Clearly and Frequently: Clear and frequent communication is essential. Use multiple channels to disseminate information and ensure that the message is consistent and comprehensible to all staff members.
- Provide Training and Resources: Equip employees with the necessary skills and resources to adapt to the change. This might include training sessions, informational materials, or access to support personnel.
- Build a Supportive Culture: Create an environment where change is viewed positively. Encourage collaboration and create opportunities for employees to share their experiences and strategies for adapting to change.
- Monitor and Adjust: Continuously monitor the progress of the change initiative and be prepared to make adjustments as needed. Solicit feedback from employees and be responsive to their concerns.
There are multiple strategies that can employed to overcome resistance to change. First, it is important to understand the underlying reasons for resistance. Resistance is commonly aligned to feelings of fear, lack of trust in leadership, or logistical concerns regarding workload, seniority, etc. To implement change effectively, a leader should empower staff by making sure they feel that their voice is respected and valued. When individuals feel valued and hear, they are more likely to support change, even if they do not personally agree with all elements associated with the change. Leaders also must understand that change is stressful for individuals. Depending on the significance of change, a leader may take actions to ensure that employee assistance programs, support groups, or additional counseling services or resources are available. These additional resources can be beneficial for individuals as they work through the emotions associated with the proposed change. Additionally, the benefits for any change should be clearly described. It is important to highlight how the proposed change will help improve work processes and patient care quality. It is also helpful to acknowledge and demonstrate appreciation for early adopters of the change. This can provide motivation and encouragement for others to follow suit and fosters a positive attitude toward future changes.
When clients experience deficient fluid volume, intravenous (IV) fluids are often prescribed. IV fluid restores fluid to the intravascular compartment, and some IV fluids are also used to facilitate the movement of fluid between compartments due to osmosis. There are three types of IV fluids: isotonic, hypotonic, and hypertonic.
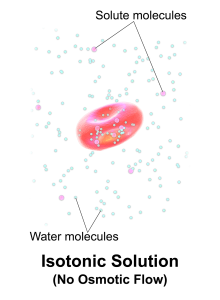
Isotonic Solutions
Isotonic solutions are IV fluids that have a similar concentration of dissolved particles as blood. An example of an isotonic IV solution is 0.9% Normal Saline (0.9% NaCl). Because the concentration of the IV fluid is similar to the blood, the fluid stays in the intravascular space and osmosis does not cause fluid movement between compartments. See Figure 15.8[16] for an illustration of isotonic IV solution administration with no osmotic movement of fluid with cells. Isotonic solutions are used for clients with fluid volume deficit (also called hypovolemia) to raise their blood pressure. However, infusion of too much isotonic fluid can cause excessive fluid volume (also referred to as hypervolemia).
Hypotonic Solutions
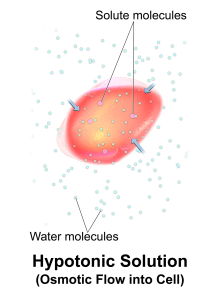
Hypotonic solutions have a lower concentration of dissolved solutes than blood. An example of a hypotonic IV solution is 0.45% sodium chloride (0.45% NaCl). When hypotonic IV solutions are infused, it results in a decreased concentration of dissolved solutes in the blood as compared to the intracellular space. This imbalance causes osmotic movement of water from the intravascular compartment into the intracellular space. For this reason, hypotonic fluids are used to treat cellular dehydration. See Figure 15.9[17] for an illustration of the osmotic movement of fluid into a cell when a hypotonic IV solution is administered, causing lower concentration of solutes (pink molecules) in the bloodstream compared to within the cell.
However, if too much fluid moves out of the intravascular compartment into cells, cerebral edema can occur. It is also possible to cause worsening hypovolemia and hypotension if too much fluid moves out of the intravascular space and into the cells. Therefore, client status should be monitored carefully when hypotonic solutions are infused.
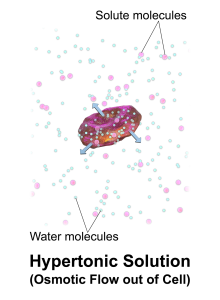
Hypertonic Solutions
Hypertonic solutions have a higher concentration of dissolved particles than blood. An example of hypertonic IV solution is 3% sodium chloride (3% NaCl). When infused, hypertonic fluids cause an increased concentration of dissolved solutes in the intravascular space compared to the cells. This causes the osmotic movement of water out of the cells and into the intravascular space to dilute the solutes in the blood. See Figure 15.10[18] for an illustration of osmotic movement of fluid out of a cell when hypertonic IV fluid is administered due to a higher concentration of solutes (pink molecules) in the bloodstream compared to the cell.
When administering hypertonic fluids, it is essential to monitor for signs of hypervolemia such as breathing difficulties and elevated blood pressure. Additionally, if hypertonic solutions with sodium are given, the client’s serum sodium level should be closely monitored.[19] See Table 15.3 for a comparison of types of IV solutions, their uses, and nursing considerations.
See Figure 15.11[20] for an illustration comparing how different types of IV solutions affect red blood cell size.
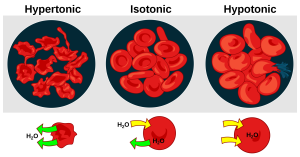
Table 15.3 Comparison of IV Solutions[21],[22],[23]
| Type | IV Solution | Uses | Nursing Considerations |
| Isotonic | 0.9% Normal Saline (0.9% NaCl) | Fluid resuscitation for hemorrhaging, severe vomiting, diarrhea, GI suctioning losses, wound drainage, mild hyponatremia, or blood transfusions. | Monitor closely for hypervolemia, especially with heart failure or renal failure. |
| Isotonic | Lactated Ringer’s Solution (LR) | Fluid resuscitation, GI tract fluid losses, burns, traumas, or metabolic acidosis. Often used during surgery. | Should not be used if serum pH is greater than 7.5 because it will worsen alkalosis. May elevate potassium levels if used with renal failure. |
| Isotonic | 5% Dextrose in Water (D5W) *starts as isotonic and then changes to hypotonic when dextrose is metabolized | Provides free water to help renal excretion of solutes, hypernatremia, and some dextrose supplementation. | Should not be used for fluid resuscitation because after dextrose is metabolized, it becomes hypotonic and leaves the intravascular space, causing brain swelling. Used to dilute plasma electrolyte concentrations. |
| Hypotonic | 0.45% Sodium Chloride (0.45% NaCl) | Used to treat intracellular dehydration and hypernatremia and to provide fluid for renal excretion of solutes. | Monitor closely for hypovolemia, hypotension, or confusion due to fluid shifting into the intracellular space, which can be life-threatening. Avoid use in clients with liver disease, trauma, and burns to prevent hypovolemia from worsening. Monitor closely for cerebral edema. |
| Hypotonic | 5% Dextrose in Water (D5W) | Provides free water to promote renal excretion of solutes and treat hypernatremia, as well as some dextrose supplementation. | Monitor closely for hypovolemia, hypotension, or confusion due to fluid shifting out of the intravascular space, which can be life-threatening. Avoid use in clients with liver disease, trauma, and burns to prevent hypovolemia from worsening. Monitor closely for cerebral edema. |
| Hypertonic | 3% Sodium Chloride (3% NaCl) | Used to treat severe hyponatremia and cerebral edema. | Monitor closely for hypervolemia, hypernatremia, and associated respiratory distress. Do not use it with clients experiencing heart failure, renal failure, or conditions caused by cellular dehydration because it will worsen these conditions. |
| Hypertonic | 5% Dextrose and 0.45% Sodium Chloride (D5 0.45% NaCl) | Replacement of fluid, minimal carbohydrate calories, and sodium chloride; hypoglycemia. | Monitor closely for hypervolemia, hypernatremia, and associated respiratory distress. Do not use it with clients experiencing heart failure, renal failure, or conditions caused by cellular dehydration because it will worsen these conditions. |
| Hypertonic | 5% Dextrose and Lactated Ringer’s (D5LR)
D10 |
Replacement of fluid, electrolyte, and calories; hypoglycemia. Lactated ringers provide some alkalizing action in the blood. | Monitor closely for hypervolemia, hypernatremia, and associated respiratory distress. Do not use it with clients experiencing heart failure, renal failure, or conditions caused by cellular dehydration because it will worsen these conditions. |
Osmolarity is defined as the proportion of dissolved particles in an amount of fluid and is generally the term used to describe body fluids. As the dissolved particles become more concentrated, the osmolarity increases. Osmolality refers to the proportion of dissolved particles in a specific weight of fluid. The terms osmolarity and osmolality are often used interchangeably in clinical practice.
Electrolytes play an important role in bodily functions and fluid regulation. There is a very narrow target range for normal electrolyte values, and slight abnormalities can have devastating consequences. For this reason, it is crucial to understand normal electrolyte ranges, causes of electrolyte imbalances, signs and symptoms of imbalances, and appropriate treatments.
Sodium
Sodium levels in the blood typically range from 136-145 mEq/L.[24] Refer to each agency's normal reference range on the lab report. Sodium is the most abundant electrolyte in the extracellular fluid (ECF) and is maintained by the sodium-potassium pump. Sodium plays an important role in maintaining adequate fluid balance in the intravascular and interstitial spaces. See the “Fluid and Electrolyte Regulation” subsection of this chapter for more information about how the body regulates sodium and water balance.
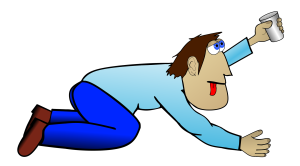
Hypernatremia refers to an elevated sodium level in the blood. Typically, hypernatremia is caused by excess water loss due to lack of fluid intake, vomiting, or diarrhea. As you recall, elevated sodium levels in the blood cause the osmotic movement of water out of the cells to dilute the blood. This causes the body’s cells to shrink, referred to as cellular dehydration. This fluid shift can have a significant impact on various organs within the body and is especially notable in the client’s neurological function. As fluid shifts out of the brain cells, the nurse may notice symptoms such as confusion, irritability, lethargy, and even seizures. Other signs and symptoms of hypernatremia include severe thirst and sticky mucous membranes. See Figure 15.12[25] for an illustration of a client with severe thirst due to hypernatremia. Treatment for hypernatremia includes decreasing sodium intake, increasing oral water intake, and rehydrating with a hypotonic IV solution.[26],[27]
Hyponatremia refers to a decreased sodium level in the blood. Hyponatremia can be caused by excess water intake or excessive administration of hypotonic IV solutions. For example, a marathon runner who only rehydrates with water instead of sports drinks (that include solutes as well as water) can develop hyponatremia. As with hypernatremia, altered sodium levels often cause neurological symptoms due to the movement of water into brain cells, causing them to swell. Symptoms of hyponatremia are headache, confusion, seizures, and coma. Treatment for hyponatremia depends on the cause and often consists of limiting water intake or discontinuing administration of hypotonic IV fluids. If hyponatremia is severe, a hypertonic IV saline solution may be prescribed to gradually raise the client’s sodium level.[28]
View helpful mnemonics related to hyponatremia and hypernatremia from RegisteredNurseRN.com.
Video Review of Fluids and Electrolytes: Sodium[29]
Potassium
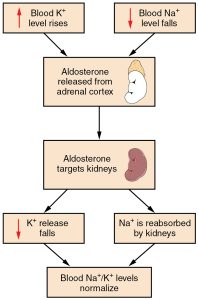
Potassium levels normally range from 3.5 to 5.1 mEq/L.[30] Refer to each agency's normal reference range on the lab report. Potassium is the most abundant electrolyte in intracellular fluid and is maintained inside the cell by the sodium-potassium pump. Potassium is regulated by aldosterone in the kidneys and is obtained in the diet through consumption of foods such as bananas, oranges, and tomatoes. See Figure 15.13[31] for an illustration of potassium regulation by aldosterone. Recall that aldosterone causes reabsorption of sodium and excretion of potassium in the distal tubule of the kidneys. In response to potassium levels rising or sodium levels falling in the bloodstream, the adrenal cortex releases aldosterone and targets the kidneys. In response, the kidneys excrete potassium and reabsorb sodium. Potassium is also impacted by the hormone insulin that moves potassium into the cells from the ECF.[32]
Potassium is necessary for normal cardiac function, neural function, and muscle contractility, including effective contractility of the cardiac muscles. Abnormal potassium levels can cause significantly abnormal heart rhythms and contractility. Potassium is poorly conserved by the body, and much is lost with urine output. For this reason, it is often necessary to provide potassium supplements when administering loop and thiazide diuretics because potassium is excreted from the kidneys along with water.[33] Potassium supplementation can be given orally or by IV infusion mixed with fluids. Potassium must NEVER be administered IV push because it can immediately stop the heart.
Hyperkalemia refers to increased potassium levels in the blood. Hyperkalemia can be caused by kidney failure, metabolic acidosis, and administration of potassium-sparing diuretics or oral/intravenous potassium supplements. Signs and symptoms of hyperkalemia are generally cardiac in nature and include irritability, cramping, diarrhea, and electrocardiogram (ECG) abnormalities. As hyperkalemia worsens, ECG abnormalities may progress to cardiac dysrhythmias and cardiac arrest.
Treatment for hyperkalemia depends on the severity of the hyperkalemia symptoms. For mild symptoms, decreased potassium intake in the diet is helpful. Adjustment to medications contributing to increased levels of potassium may be indicated. For severe symptoms, administration of sodium polystyrene sulfonate (Kayexalate) orally or rectally helps bind excess potassium, so it is excreted through the GI tract. Insulin may be administered to push potassium into cells and decrease serum potassium levels. When administering an insulin infusion, it is important to monitor blood glucose levels closely, often hourly per agency policy. The client often requires supplemental IV dextrose to prevent low blood sugar levels when insulin is used for potassium reduction. IV calcium gluconate may also be given to prevent excess potassium from affecting cardiac muscle. This is a temporary measure and wears off quickly but allows time for other treatments to take effect and lower potassium levels before cardiac arrest develops. For severe symptomatic hyperkalemia, temporary hemodialysis may also be used to quickly decrease potassium levels.[34]
Hypokalemia refers to decreased potassium level in the blood. Hypokalemia can be caused by excessive vomiting, diarrhea, potassium-wasting diuretics, and insulin use, as well as lack of potassium in the diet. Signs and symptoms of hypokalemia include weakness, arrhythmias, lethargy, and a thready pulse. Treatment for hypokalemia includes increasing oral intake of potassium in the diet and oral or IV potassium in fluids supplementation. It is important to remember that administering IV potassium too quickly can cause cardiac arrest. In fact, potassium is one of the ingredients used during lethal injection to stop the heart.
View helpful mnemonics for hypokalemia and hyperkalemia from RegisteredNurseRN.com.
Video Review About Potassium[35]
Calcium
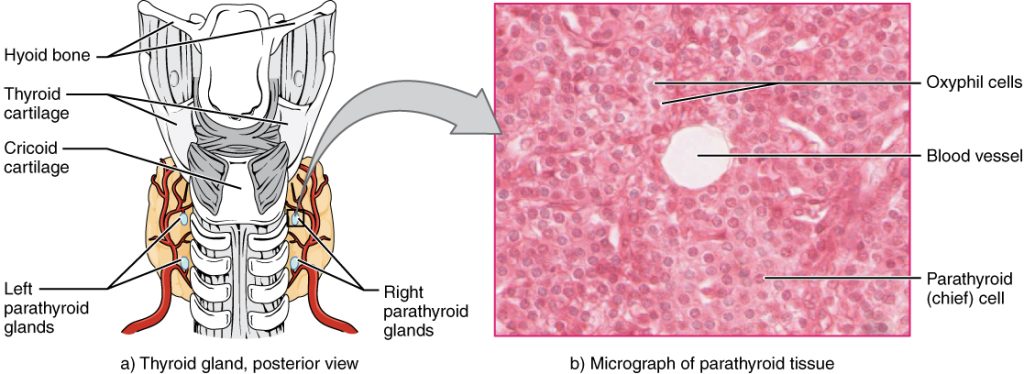
Calcium levels normally range from 8.6-10.2 mg/dL.[36] Refer to each agency's normal reference range on the lab report. Calcium circulates in the bloodstream, but the majority is stored in bones. Calcium is important for bone and teeth structure, nerve transmission, and muscle contraction. Calcium excretion and reabsorption are regulated by the parathyroid hormone (PTH) that is secreted from the parathyroid glands near the thyroid. See Figure 15.14[37] for an illustration of the parathyroid glands. As PTH is secreted in response to low calcium levels in the blood, calcium is reabsorbed in both the kidneys and the intestine and released from the bones to increase serum calcium levels. Calcium is also affected by dietary intake and physical activity. Activity causes calcium to move into bones whereas immobility causes the release of calcium from bones, which cases them to become weak. Dietary sources of calcium include dairy products, green leafy vegetables, sardines, and whole grains.[38]
Hypercalcemia refers to an increased calcium level. It can be caused by prolonged immobilization that allows calcium to leach out of the bones and into the serum. Additionally, there are many types of cancers that may cause excessive calcium release from bones. Hypercalcemia can also be caused by hyperparathyroidism and parathyroid tumors, which can cause too much PTH secretion, causing too much calcium to be reabsorbed in the kidneys and intestines and released from bone.
Signs and symptoms of hypercalcemia often impact the gastrointestinal and musculoskeletal systems. These symptoms include nausea, vomiting, constipation, increased thirst and/or urination, and skeletal muscle weakness. Treatment for hypercalcemia includes decreasing calcium intake in the diet, phosphate supplementation (which has an inverse relationship to calcium), hemodialysis, surgical removal of the parathyroid gland (if hyperparathyroidism is causing the hypercalcemia), and weight-bearing exercises as tolerated.[39]
Hypocalcemia refers to a decreased calcium level in the blood. Hypocalcemia can be caused by hypoparathyroidism where not enough PTH is excreted, causing a decreased reabsorption of calcium and decreased release of calcium from the bones. Hypocalcemia is also caused by vitamin D deficiency and renal disease. Because phosphorus is inversely related to calcium, an abnormally high phosphorus level as seen with renal failure can also result in hypocalcemia.
Signs and symptoms of hypocalcemia often impact the musculoskeletal and nervous systems. These include paresthesias (numbness and tingling) of the lips, tongue, hands and feet, muscle cramps, and tetany. Chvostek’s sign is a classic sign of acute hypocalcemia and is an involuntary twitching of facial muscles when the facial nerve is tapped. A second classic sign of acute hypocalcemia is Trousseau’s sign where a hand spasm is caused by inflating a blood pressure cuff to a level above the client's systolic pressure for three minutes. See a video of a client experiencing Chvostek’s and Trousseau’s signs below. Treatment of hypocalcemia includes increasing oral intake of dietary calcium and vitamin D and oral or IV calcium supplementation and decreasing the phosphorus level if it is elevated.[40]
View a video of a client exhibiting Chvostek's Sign and Trousseau's Sign of hypocalcemia.
View helpful mnemonics for hypercalcemia and hypocalcemia from RegisteredNurseRN.com.
Phosphorus
Phosphorus levels typically range from 2.5-4.0 mg/dL. Refer to each agency's normal reference range on the lab report. Phosphorus is stored in the bones and is predominantly found in the ICF with small amounts in the ECF. Phosphorus is important in energy metabolism, RNA and DNA formation, nerve function, muscle contraction, and for bone, teeth, and membrane building and repair. Phosphorus is excreted by the kidneys and absorbed by the intestines. Dietary phosphorus sources include dairy products, fruits, vegetables, meat, and cereal.[41]
Hyperphosphatemia refers to an increased phosphorus level in the blood and can be caused by kidney disease, crush injuries, or overuse of phosphate-containing enemas. Hyperphosphatemia itself is usually asymptomatic, but signs of associated hypocalcemia may be present due to the inverse relationship between phosphorus and calcium. Treatment for hyperphosphatemia includes decreasing intake of phosphorus, administration of phosphate-binder medications to help with excretion, and hemodialysis.[42]
Hypophosphatemia is a decreased phosphorus level in the blood. Acute hypophosphatemia can be caused by acute alcohol abuse, burns, diuretic use, respiratory alkalosis, resolving diabetic ketoacidosis, and starvation. Chronic hypophosphatemia is caused by hyperparathyroidism, vitamin D deficiency, prolonged use of phosphate binders, and hypomagnesemia or hypokalemia. Hypophosphatemia is usually asymptomatic, but in severe cases, it can cause muscle weakness, anorexia, encephalopathy, seizures, and death. Treatment for hypophosphatemia includes treating what is causing the imbalance, oral or IV phosphorus replacement, and increased phosphate-containing foods in the diet.[43]
Magnesium
Magnesium levels typically range from 1.5-2.4 mEq/L. Refer to each agency's reference range on the lab report. Magnesium is essential for normal cardiac, nerve, muscle, and immune system functioning. About half of the body’s magnesium is stored in the bones. About 1% is stored in ECF and the rest is found in ICF.[44] Dietary sources of magnesium include green leafy vegetables, citrus, peanut butter, almonds, legumes, and chocolate.
Hypermagnesemia refers to an elevated magnesium level in the blood. It is usually the result of renal failure, excess magnesium replacement, or use of magnesium containing laxatives or antacids. Signs and symptoms of hypermagnesemia include bradycardia, weak and thready pulse, lethargy, tremors, hyporeflexia, muscle weakness, and cardiac arrest. Treatment for hypermagnesemia involves increasing fluid intake, discontinuing magnesium-containing medications, and in severe cases, hemodialysis or peritoneal dialysis. Additionally, administration of calcium gluconate can be helpful to reduce the cardiac effects of hypermagnesemia until the magnesium level can be lowered.[45]
Hypomagnesemia refers to decreased magnesium level in the blood. It typically results from inadequate magnesium in the diet or from loop diuretics that excrete magnesium. Clients with alcohol use disorder often have hypomagnesemia due to concurrent poor diet and impaired nutrient absorption that occurs with alcohol consumption. Chronic proton pump inhibitor use can also cause hypomagnesemia due to impaired nutrient absorption.
Signs and symptoms of hypomagnesemia include nausea, vomiting, lethargy, weakness, leg cramps, tremor, dysrhythmias, and tetany that is associated with concurrent hypocalcemia that can occur with hypomagnesemia. Treatment for hypomagnesemia consists of increasing dietary intake of magnesium containing foods and oral or IV magnesium supplementation.[46]
View helpful mnemonics for hypermagnesemia and hypomagnesemia from RegisteredNurseRN.com.
See Table 15.4 for a comparison of causes, symptoms, and treatments of different electrolyte imbalances. As always, refer to agency lab reference ranges when providing client care.
Table 15.4 Comparison of Causes, Symptoms, and Treatments of Imbalanced Electrolyte Levels
| Elevated Level | Decreased Level | |
|---|---|---|
| Sodium (Na+)
Normal range 136-145 mEq/L |
Hypernatremia
Causes: Excessive salt intake Symptoms: Lethargy, irritability, seizures, and weakness Treatments: Rehydrate w/ D5W and increase water intake |
Hyponatremia
Causes: Excessive water intake and diuretics Symptoms: Headache, confusion, and coma Treatments: 3% NS and fluid restriction |
| Potassium (K+)
Normal range 3.5-5.1 mmol/L |
Hyperkalemia
Causes: Kidney dysfunction, excessive potassium intake, and ACE inhibitors Symptoms: Cardiac arrhythmias, cramping, diarrhea, and irritability Treatments: Limit potassium in diet, loop diuretic, insulin, dialysis, and kayexalate |
Hypokalemia
Causes: Deficient intake of potassium-rich foods, loop and thiazide diuretics, and IV administration of insulin Symptoms: Weakness, arrhythmias, lethargy, and thready pulse (WALT) Treatments: PO/IV potassium and increase K+ in diet |
| Calcium (Ca++)
Normal range 8.6 -10.2 mg/dL |
Hypercalcemia
Causes: Overactive parathyroid glands and cancer Symptoms: Nausea, vomiting, constipation, and thirst Treatments: Decrease calcium in diet, increase mobility, and administer phosphorous |
Hypocalcemia
Causes: Diuretic use and removal of parathyroid glands Symptoms: Numbness, tingling, Chvostek’s sign, and Trousseau's sign (tetany) Treatments: Increase Ca++ in diet and IV/PO calcium |
| Magnesium (Mg+)
Normal range 1.5-2.4 mg/dL |
Hypermagnesemia
Causes: Kidney disease and excessive magnesium intake (i.e., laxatives and antacids) Symptoms: Muscle weakness, bradycardia, asystole, tremors, and slow reflexes Treatments: Dialysis, increased fluid intake, and stopping medications containing Mg+ |
Hypomagnesemia
Causes: Diuretics, undernutrition, and long-term alcohol use disorder Symptoms: Nausea, vomiting, lethargy, weakness, tetany, leg cramps, tremors, and arrhythmias Treatments: Increase Mg+ in diet and PO/IV magnesium |
The nursing process is used continuously when caring for individuals who have fluid, electrolyte, or acid-base imbalances, or at risk for developing them because their condition can change rapidly. This systematic approach to nursing care ensures that subtle cues or changes are not overlooked and that appropriate outcomes and interventions are implemented according to the client’s current condition.
Assessment
A thorough assessment provides valuable information about a client’s current fluid, electrolyte, and acid-base balance, as well as risk factors for developing imbalances. Performing a chart review or focused health history is a good place to start collecting data, with any identified gaps or discrepancies verified during the physical assessment. It is also important to consider pertinent life span or cultural considerations that impact a client’s fluid and electrolyte status.
Subjective Assessment
Subjective assessment data is information obtained from the client as a primary source or family members or friends as a secondary source. This information must be obtained by interviewing the client or someone accompanying the client. Some of this information can be obtained through a chart review but should be verified with the client or family member for accuracy.
Subjective data to obtain includes age; history of chronic disease, surgeries, or traumas; dietary intake; activity level; prescribed medications and compliance with taking medications; pain; and bowel and bladder functioning. Subjective assessment data is helpful to determine normal pattern identification and risk identification. For example, a history of kidney disease or heart failure places the client at risk for fluid volume excess, whereas diuretic use places the client at risk for fluid volume deficit and electrolyte and acid-base imbalances. A history of diabetes mellitus also places a client at risk for fluid, electrolyte, and acid-base imbalances. Recognizing these risks helps nurses be prepared for complications that may arise and allows the nurse to recognize subtle cues as problems develop.
Objective Assessment
Objective assessment data is information that the nurse directly observes. This data is obtained through a physical examination using inspection, auscultation, and palpation. A complete head-to-toe assessment should be performed to avoid missing clues to the client’s condition.
Focused assessments such as trends in weight, 24-hour intake and output, vital signs, pulses, lung sounds, skin, and mental status are used to determine fluid balance, electrolyte, and acid-base status.
- Accurate daily weights can provide important clues to fluid balance. Weights must be taken on the same scale, at the same time of day, with the client wearing similar clothing in order to be accurate. A one-kilogram change in weight in 24 hours is considered significant because this represents a one-liter fluid gain or loss and should be reported to the provider.
- Accurate measurement of 24-hour intake and output helps validate weight findings. Averaged urine output of less than 30 mL/hour or 0.5mL/kg/hr should be reported to the provider.
- Vital signs should be analyzed. An elevated blood pressure and bounding pulses are often seen with fluid volume excess. Decreased blood pressure with an elevated heart rate and a weak or thready pulse are hallmark signs of fluid volume deficit. Systolic blood pressure less than 100 mm Hg in adults, unless other parameters are provided, should be reported to the health care provider.
- Lung crackles can signify fluid volume excess and are often first auscultated in the lower posterior lung fields.
- Tight, edematous, shiny skin can indicate fluid volume excess. See Figure 15.15[47] for an image of edema. Conversely, skin tenting, dry mucous membranes, or dry skin indicate fluid volume deficit. Keep in mind that clients with edema may also be experiencing intravascular fluid volume deficit if too much fluid has leaked into the interstitial space, resulting in signs of hypotension, tachycardia, and weak, thready pulses.
- New mental status changes such as confusion or decreased level of consciousness can indicate fluid, electrolyte, or acid-base imbalance, especially hypo- or hypernatremia, acid-base imbalances, or fluid volume deficit.
- Cardiac arrhythmias can be seen with acid-base imbalances and electrolyte imbalances, especially with hypo- or hyperkalemia and alkalosis. See Table 15.6a for a comparison of expected and unexpected findings and those that require notification of a health care provider.

Table 15.6a Expected Findings Versus Unexpected Findings Indicating a Fluid Imbalance[48]
| Assessment | Expected Findings | Unexpected Findings Indicating Excessive Fluid Volume
*Bolded items are critical conditions that require immediate health care provider notification. |
Unexpected Findings Indicating Deficient Fluid Volume
*Bolded items are critical conditions that require immediate health care provider notification. |
|---|---|---|---|
| Vital signs | Blood pressure, heart rate, and oxygen saturation levels within normal limits | Elevated blood pressure, increased respiratory rate, or decreased oxygen saturation | Decreased blood pressure or elevated heart rate |
| Neurological | Alert and oriented | Headache | Headache, confusion, decreased level of consciousness, dizziness, or weakness |
| Cardiac | Normal heart rate and rhythm, capillary refill <3 seconds, and normal pulses | Bounding pulses, S3 heart sound, or jugular venous distention | Weak, thready pulses; sluggish capillary refill; or chest pain |
| Respiratory | Clear lung sounds throughout, normal respiratory rate, and no shortness of breath | Crackles in lung fields, pink frothy sputum, shortness of breath, or respiratory distress | Shortness of breath possible |
| Gastrointestinal | Bowel sounds present x4 quadrants and normal stool consistency and frequency for the client | Constipation with dry, hard stools | |
| Urinary | Clear urine, normal urine specific gravity, and urine output greater than 30 ml/hr | Decreased urine output <30 mL/hr or < 0.5 mL/kg/hr concentrated urine | Decreased urine output <30 mL/hr or <0.5 mL/kg/hr concentrated urine, or elevated urine specific gravity |
| Integumentary | Normal skin turgor and moist mucous membranes | Tight, edematous, or shiny skin | Tenting (poor skin turgor); dry, sticky mucous membranes; or dry skin |
| Weight | <1kg change in weight over 24 hours | >1kg increase over 24 hours | >1kg decrease over 24 hours |
Diagnostic and Lab Work
Diagnostic tests and lab work provide important information about fluid status, electrolyte, and acid-base balance and should be used in conjunction with a thorough subjective and objective assessment to form a complete picture of the client’s overall status. It is important to cluster diagnostic and lab assessment data with subjective and objective assessment data to ensure a complete assessment picture. This will help ensure correct information is reported to the provider as necessary.
Lab work provides important clues to overall fluid status. Common lab tests used to evaluate fluid status include serum osmolarity, urine specific gravity, hematocrit, and blood urea nitrogen (BUN).
Serum osmolarity (often interchanged with the term serum osmolality) measures the concentration of particles in the blood with a normal range of 275 to 295 mmol/kg. Normal value ranges may vary slightly among different laboratories. In healthy people, when serum osmolality in the blood becomes high, the body releases antidiuretic hormone (ADH). This hormone causes the kidneys to reabsorb water, resulting in dilution of the blood and the return of serum osmolarity to normal range. An elevated serum osmolarity level means the blood is more concentrated than normal and often indicates deficient fluid volume deficit. A decreased serum osmolarity means the blood is more dilute than normal and may indicate a fluid volume excess.[49]
Urine osmolarity measures the concentration of particles in the urine. An increased urine osmolarity result means the urine is concentrated and can indicate fluid volume deficit. A decreased urine osmolarity result means the urine is dilute and can indicate excess fluid intake.[50] Urine specific gravity is a urine test that commonly measures hydration status by measuring the concentration of particles in urine. Normal urine specific gravity levels are between 1.010 and 1.020. A urine specific gravity above 1.020 indicates concentrated urine and can indicate a fluid volume deficit, similarly to an elevated urine osmolarity. A urine specific gravity below 1.010 indicates dilute urine, which can occur with excessive fluid intake.[51]
When a condition called “Excessive Fluid Volume” occurs, it is often the result of altered physiological mechanisms, which impact the kidney’s ability to increase urine output to eliminate excessive fluid volume, causing urine output to decrease. As a result, the serum osmolarity decreases as fluid is retained but the urine specific gravity is elevated because urine is concentrated.
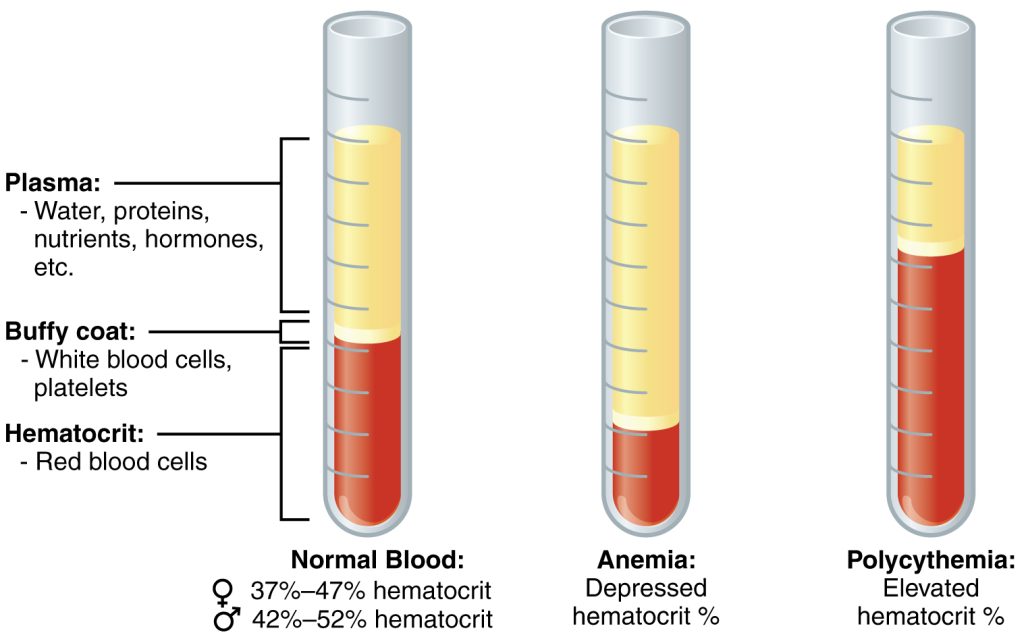
Hematocrit (HCT) is a blood test that measures how much of your blood is made up of red blood cells compared to the liquid component of blood called plasma. It is often part of a complete blood count (CBC), a routine test that measures different components of your blood. The normal hematocrit for men is 42 to 52%; for women it is 37 to 47%, but these ranges may vary slightly across laboratories.
In addition to measuring red blood cells, hematocrit levels can also be used to evaluate fluid balance. When deficient fluid volume is occurring, the plasma component of the blood also decreases, causing an elevated concentration of red blood cells (and an elevated hematocrit). In this case, drinking more fluid or receiving intravenous fluids will bring the hematocrit level back to normal range. Conversely, if a client is experiencing “Excessive Fluid Volume,” the plasma component of the blood is increased, causing dilution of the red blood cells and a decreased hematocrit level.[52],[53] See Figure 15.16[54] for an illustration of normal hematocrit, elevated hematocrit, and decreased hematocrit due to fluid imbalance.
Blood Urea Nitrogen (BUN) measures the amount of urea nitrogen in your blood. BUN and serum creatinine levels are used to evaluate kidney function, with increased levels indicating worsening kidney function. In general, the normal BUN range is 7 to 20 mg/dL, but normal ranges vary depending on the reference range used by the lab and the client’s age. Clients with “Deficient Fluid Volume” can also have elevated BUN levels for the same reason that hematocrit is affected; as plasma levels decrease, the blood becomes more concentrated.
In addition to monitoring lab work for results indicating fluid imbalance, electrolytes, specifically sodium, potassium, calcium, phosphorus, and magnesium, should be monitored closely for clients at risk. Refer to Table 15.4 in the "Electrolytes" section for an overview of electrolyte imbalances, common symptoms, and common treatments.
Additional diagnostic tests used to evaluate for signs of fluid and electrolyte imbalances are the chest X-ray and the electrocardiogram. A chest X-ray evaluates for fluid in the lungs, a common complication of excessive fluid volume. An electrocardiogram (ECG) evaluates for arrhythmias (e.g., electrical conduction disturbances) in the heart resulting from electrolyte imbalances.
Arterial blood gases (ABGs) are used to closely monitor critically ill clients, such as clients in diabetic ketoacidosis or in severe respiratory distress. ABG results provide important clues about respiratory status, oxygenation, and metabolic processes occurring in the body. See Table 15.6b for a summary of laboratory findings associated with fluid, electrolyte, and acid-base imbalances.
Table 15.6b Lab Values Associated with Fluid and Electrolyte Imbalances
| Lab Value | Normal Ranges |
|---|---|
| Serum osmolarity | 275 to 295 mmol/kg |
| Urine specific gravity | 1.010 and 1.020 |
| Hematocrit | Men: 42 to 52%
Women: 37 to 47% |
| BUN | 7 to 20 mg/dL |
| Serum sodium | 135-145 mEq/L |
| Serum potassium | 3.5-5 mEq/L |
| Serum magnesium | 1.5-2.4 mEq/L |
| Serum calcium | 8.5-10.3 mg/dL |
| Serum phosphorus | 2.5-4 mg/dL |
| ABG | pH: 7.35 and 7.45
PaO2: 80-100 mm Hg HCO3: 22-26 mEq/L PaO2: 35-45 mm Hg |
Life Span Considerations
There are several life span considerations when assessing for fluid, electrolyte, and acid-base balance.
Newborns and Infants
Newborns and infants have a large proportion of water weight compared to adults, with approximately 75% of weight being water. During the first week after birth, a newborn's weight decreases partly because extracellular fluid is lost in urine along with sodium. Additionally, compensatory mechanisms such as the Renin-Angiotensin-Aldosterone System are less developed, and newborn kidneys are less able to concentrate urine, resulting in a decreased ability to retain sodium. Newborns and infants also have a greater body surface area, making them more susceptible to insensible fluid losses through the skin and lungs via evaporation. This causes increased risk of developing hyponatremia and fluid volume deficit. In contrast, newborns are less able to excrete potassium, placing them at risk for hyperkalemia.[55] Episodes of vomiting and diarrhea also place infants at an increased risk of quickly developing fluid and electrolyte disturbances.
When monitoring urine output in infants, parents are often asked about the number of wet diapers in a day. Nurses may also weigh diapers for hospitalized infants for more accurate measurement of urine output.
Children and Adolescents
Children and adolescents are at risk for dehydration when physically active in hot environments due to excessive sweating. Illnesses causing diarrhea, vomiting, or fever can also quickly cause fluid deficit if there is little fluid intake to replace the water and sodium lost. For this reason, it is important to educate parents regarding the importance of fluid intake when their child is sweating or ill.[56]
Older Adults
Older adults are at risk for fluid and electrolyte imbalances for a variety of reasons, including surgery, chronic diseases such as heart and kidney disease, diuretic use, and decreased mobility that limits the ability to obtain hydration. They also have a decreased thirst reflex, which contributes to decreased fluid consumption. Kidney function naturally decreases with age, resulting in decreased sodium and water retention, as well as decreased potassium excretion. These factors place older clients at risk for fluid volume deficit and electrolyte abnormalities.[57]
Diagnoses
There are many nursing diagnoses applicable to fluid, electrolyte, and acid-base imbalances. Review a nursing care planning resource for current NANDA-I approved nursing diagnoses, related factors, and defining characteristics. See Table 15.6c for commonly used NANDA-I diagnoses associated with clients with fluid and electrolyte imbalances.[58]
Table 15.6c Common NANDA-I Nursing Diagnoses Related to Fluid and Electrolyte Imbalances[59]
| NANDA-I Diagnosis | Definition | Defining Characteristics |
|---|---|---|
| Excess Fluid Volume | Surplus intake and/or retention of fluid. | Adventitious breath sounds
Elevated blood pressure Altered mental status Anxiety Decreased hematocrit, serum osmolarity, and BUN Dyspnea Edema Fluid intake exceeds output Jugular vein distension Restlessness Weight gain >1 kg/24 hours |
| Deficient Fluid Volume | Decreased intravascular, interstitial, and/or intracellular fluid. This refers to dehydration, water loss alone without change in sodium. | Altered mental status
Decreased skin turgor Decreased blood pressure Decreased urine output Dry skin and mucous membranes Increased heart rate Increased serum osmolarity, hematocrit, and BUN Increased urine concentration Sudden weight loss Thirst Weakness |
| Risk for Imbalanced Fluid Volume | Susceptible to a decrease, increase, or rapid shift from one to the other of intravascular, interstitial, and/or intracellular fluid, which may compromise health. This refers to body fluid loss, gain, or both. | Diarrhea
Vomiting
|
| Risk for Electrolyte Imbalance | Susceptible to changes in serum electrolyte levels, which may compromise health. | Diarrhea
Vomiting Excessive fluid volume Insufficient fluid volume |
Excess Fluid Volume Example
A client with heart failure has been hospitalized with an acute exacerbation with dyspnea and increased edema in the lower extremities. A sample PES statement is, "Fluid Volume Excess related to a compromised regulatory mechanism as evidenced by edema, crackles in lower posterior lungs, and weight gain of 2 kg in 24 hours."
Deficient Fluid Volume Example
An elderly client develops severe diarrhea due to food poisoning and is admitted to the hospital with dehydration. A sample PES statement is, "Deficient Fluid Volume related to insufficient fluid intake as evidenced by blood pressure 90/60, dry mucous membranes, decreased urine output, and an increase in hematocrit."
Risk for Imbalanced Fluid Volume Example
A client who is ten weeks pregnant has developed severe vomiting due to severe morning sickness. A sample PES statement is, "Risk for Imbalanced Fluid Volume as evidenced by vomiting." The nurse plans to educate the client about tips to stay hydrated despite vomiting, as well as when to contact the provider if signs of dehydration develop.
Risk for Electrolyte Imbalance Example
A client with chronic kidney disease is prescribed a diuretic to control fluid retention. A sample PES statement is, "Risk for Electrolyte Imbalance as evidenced by insufficient knowledge about modifiable risk factors related to diuretic use." The nurse plans to educate the client about signs and symptoms of fluid and electrolyte imbalance and when to contact the provider.
Note: Recall that risk diagnoses do not contain related factors in PES statements because a vulnerability for a potential problem is being identified for the client. Instead, the phrase “as evidenced by” is used to refer to the evidence of risk that exists. Read more about formulating PES statements in the “Nursing Process” chapter.
Outcome Identification
Goals for a client experiencing fluid, electrolyte, or acid-base imbalances depend on the chosen nursing diagnosis and specific client situation. Typically, goals should relate to resolution of the imbalance. For example, if the nursing diagnosis is Excess Fluid Volume, then an appropriate goal would pertain to resolution of the fluid volume excess. Remember that goals are broad, and outcomes should be narrowly focused and written in SMART format (Specific, Measurable, Achievable, Realistic, and Time Oriented).
For the nursing diagnosis of Excess Fluid Volume, an overall goal is, “The client will achieve fluid balance.” Fluid balance for a client with Excess Fluid Volume is indicated by body weight returning to baseline with no peripheral edema, neck vein distention, or adventitious breath sounds.[60] An example of a SMART outcome is, “The client will maintain clear lung sounds with no evidence of dyspnea over the next 24 hours.”
For clients experiencing Electrolyte Imbalances, an appropriate goal is, “The client will maintain serum sodium, potassium, calcium, phosphorus, magnesium, and/or pH levels within normal range.” An additional goal is, “The client will maintain a normal sinus heart rhythm with regular rate,” because many electrolyte imbalances impact the electrical conduction system of the heart, and this is a life-threatening complication.
Planning Interventions
Evidence-based interventions should be planned according to the client’s history and specific fluid, electrolyte, or acid-base imbalance present. Refer to a nursing care planning resource for evidence-based interventions for specific nursing diagnoses. Table 15.6d lists selected interventions for key imbalances.[61],[62],[63],[64]
Table 15.6d Interventions for Imbalances
| Nursing Diagnosis | Interventions |
|---|---|
| Excess Fluid Volume |
|
| Deficient Fluid Volume |
|
| Risk for Electrolyte Imbalance |
|
Read more about diuretic medications that affecting fluid and electrolyte balance in the “Cardiovascular and Renal System” chapter in Open RN Nursing Pharmacology, 2e.
Read about intravenous fluids used to treat Fluid Volume Deficit in the “IV Therapy Management” chapter in Open RN Nursing Skills, 2e.
Implement Interventions Safely
Clients with fluid and electrolyte imbalances can quickly move from one imbalance to another based on treatments received. It is vital to reassess a client before implementing interventions to ensure current status warrants the prescribed intervention. For example, a client admitted with Fluid Volume Deficit received intravenous fluids (IV) over the past 24 hours. When the nurse prepares to administer the next bag of IV fluids, she notices the client has developed pitting edema in his lower extremities. She listens to his lungs and discovers crackles. The nurse notifies the prescribing provider, and the order for intravenous fluids is discontinued and a new order for diuretic medication is received.
Assessments for new or worsening imbalances should be performed prior to implementing interventions[66]:
- Monitor daily weights for sudden changes. A weight change of greater than 1 kg in 24 hours (using the same scale and type of clothing) should be reported to the provider.
- Monitor location and extent of edema using the 1+ to 4+ scale to quantify edema.
- Monitor intake and output over a 24-hour period; note trends of decreasing urine output in relation to fluid intake indicating potential development of Fluid Volume Excess.
- Monitor lab work such as serum osmolarity, serum sodium, BUN, and hematocrit for abnormalities. (For example, a client receiving IV fluids may develop Fluid Volume Excess, resulting in decreased levels of serum osmolarity, serum sodium, BUN, and hematocrit. Conversely, a client receiving IV diuretics can quickly become dehydrated, resulting in elevated levels of serum osmolarity, serum sodium, BUN, and hematocrit.)
- For clients receiving intravenous fluids, monitor for the development of excessive fluid volume. Monitor lung sounds for crackles and ask about the presence of dyspnea. Report new abnormal findings to the provider.
- For clients receiving diuretic therapy, monitor for fluid volume deficit and electrolyte imbalances such as hypokalemia and hyponatremia.
Implement fall precautions for clients with orthostatic hypotension, restlessness, anxiety, or confusion related to fluid imbalances.
Evaluation
The effectiveness of interventions implemented to maintain fluid balance must be continuously evaluated. Evaluation helps the nurse determine whether goals and outcomes are met and if interventions are still appropriate for the client. If outcomes and goals are met, the plan of care can likely be discontinued. If outcomes and goals are not met, they may need to be revised. It is also possible that interventions may need to be added or revised to help the client meet their goals and outcomes. Table 15.6e provides a list of assessment findings indicating imbalances are improved.
Table 15.6e Evaluating for Improvement of Imbalances
| Imbalance | Signs and Symptoms of Improvement |
|---|---|
| Fluid Volume Excess | Decreased crackles, decreased edema, decreased shortness of breath, and/or improved jugular venous distention |
| Fluid Volume Deficit | Increased blood pressure, decreased heart rate, normal skin turgor, and/or moist mucous membranes |
| Electrolyte Imbalances | Electrolyte levels return to normal and/or absence of signs or symptoms of deficit or excess |
| Acid-Base Imbalance | ABGs return to normal or baseline, resolution of vomiting or diarrhea, and/or no respiratory distress |
Legal Considerations
As discussed earlier in this chapter, nurses can be reprimanded or have their licenses revoked for not appropriately following the Nurse Practice Act in the state they are practicing. Nurses can also be held legally liable for negligence, malpractice, or breach of client confidentiality when providing client care.
Negligence and Malpractice
Negligence is a general term that denotes conduct lacking in due care, carelessness, and a deviation from the standard of care that a reasonable person would use in a particular set of circumstances.[67] Malpractice is a more specific term that looks at a standard of care, as well as the professional status of the caregiver. [68]
To prove negligence or malpractice, the following elements must be established in a court of law[69]:
- Duty owed the client
- Breach of duty owed the client
- Foreseeability
- Causation
- Injury
- Damages
To avoid being sued for negligence or malpractice, it is essential for nurses and nursing students to follow the scope and standards of practice care set forth by their state’s Nurse Practice Act; the American Nurses Association; and employer policies, procedures, and protocols to avoid the risk of losing their nursing license. Examples of a nurse's breach of duty that can be viewed as negligence includes the following:[70]
- Failure to Assess: Nurses should assess for all potential nursing problems/diagnoses, not just those directly affected by the medical disease. For example, all clients should be assessed for fall risk and appropriate fall precautions implemented.
- Insufficient monitoring: Some conditions require frequent monitoring by the nurse, such as risk for falls, suicide risk, confusion, and self-injury.
- Failure to Communicate:
- Lack of documentation: A basic rule of thumb in a court of law is that if an assessment or action was not documented, it is considered not done. Nurses must document all assessments and interventions, in addition to the specific type of client documentation called a nursing care plan.
- Lack of provider notification: Changes in client condition should be urgently communicated to the health care provider based on client status. Documentation of provider notification should include the date, time, and person notified and follow-up actions taken by the nurse.
- Failure to Follow Protocols: Agencies and states have rules for reporting certain behaviors or concerns. For example, a nurse is considered a mandatory reporter by law and required to report suspicion of abuse or neglect of a child based on data gathered during an assessment.
Patient Self Determination Act
The Patient Self Determination Act (PSDA) of 1990 is an amendment made to the Social Security Act that requires health care facilities to inform clients of their right to be involved in their medical care decisions. This law specifically applies to facilities accepting Medicare or Medicaid funding but is considered a right of all clients regardless of their method of reimbursement.
Under the PSDA, clients must also be asked about their advance directives and care wishes. Clients must be provided with teaching about advance directives, appointment of an agent or surrogate in the event they become incapacitated, and their right to self-determination. Conversations about these topics and clients wishes must be documented in the medical record. It is considered an ethical duty of nurses and other health care professionals to ensure clients are aware and understand these healthcare-associated rights.[71]
Informed Consent
Informed consent is written consent voluntarily signed by a client who is competent and understands the terms of the consent without any form of coercion. In the event the client is a minor or deemed incompetent to make their own decisions, a parent or legal guardian signs the informed consent.[72]
Informed consent is crucial for upholding the client's right for self-determination. Informed consent provides documentation signed by the client of their understanding of health care being provided; its benefits, risks, potential complications; reasonable alternatives to treatment; and the right to withdraw consent. It is the health care provider's responsibility to fully discuss the treatment, procedure, or other health care action being proposed that requires consent. The nurse often signs as a witness to the client's signature on the form, affirming that person signed the form. However, it is not the nurse's responsibility or role to provide information. If the client (or their parent/legal guardian) expresses questions, concerns, or lack of understanding, the nurse has an ethical responsibility to notify the provider and advocate for further discussion before signing the form.[73]
In emergency situations where the delay to obtain consent would cause undue harm to the client, verbal or telephone consent may be temporarily obtained that is valid for no more than ten days. Verbal consent and the reason for verbal consent must be documented in the medical record by the provider.[74]
See the following box for examples of situations requiring informed consent in the state of Wisconsin according to the Wisconsin Department of Health Services.
Examples of Situations Requiring Informed Consent[75]
- Receipt of medications and/or treatment, including psychotropic medications (unless court-ordered)
- Undergoing customary treatment techniques and procedures
- Participation in experimental research
- Undergoing psychosurgery or other psychological treatment procedures
- Release of treatment records
- Videorecording
- Performance of labor beneficial to the facility
Confidentiality
In addition to negligence and malpractice, confidentiality is a major legal consideration for nurses and nursing students. Patient confidentiality is the right of an individual to have personal, identifiable medical information, referred to as their protected health information (PHI), protected and known only by those health care team members directly providing care to them. This right is protected by federal regulations called the Health Insurance Portability and Accountability Act (HIPAA). HIPAA was enacted in 1996 and was prompted by the need to ensure privacy and protection of personal health records and data in an environment of electronic medical records and third-party insurance payers. There are two main sections of HIPAA law, the Privacy Rule and the Security Rule. The Privacy Rule addresses the use and disclosure of individuals' health information. The Security Rule sets national standards for protecting the confidentiality, integrity, and availability of electronically protected health information. HIPAA regulations extend beyond medical records and apply to client information shared with others. Therefore, all types of client information should only be shared with health care team members who are actively providing care to them.
How do HIPAA regulations affect you as a student nurse? You are required to adhere to HIPAA guidelines from the moment you begin to provide client care. Nursing students may be disciplined or expelled by their nursing program for violating HIPAA. Nurses who violate HIPAA rules may be fired from their jobs or face lawsuits. See the following box for common types of HIPAA violations and ways to avoid them.
Common HIPAA Violations and Ways to Avoid Them[76]
- Gossiping in the hallways or otherwise talking about clients where other people can hear you. It is understandable that you will be excited about what is happening when you begin working with clients and your desire to discuss interesting things that occur. As a student, you will be able to discuss client care in a confidential manner behind closed doors with your instructor. However, as a health care professional, do not talk about clients in the hallways, elevator, breakroom, or with others who are not directly involved with that client’s care because it is too easy for others to overhear what you are saying.
- Mishandling medical records or leaving medical records unsecured. You can breach HIPAA rules by leaving your computer unlocked for anyone to access or by leaving written client charts in unsecured locations. You should never share your password with anyone else. Make sure that computers are always locked with a password when you step away from them and paper charts are closed and secured in an area where unauthorized people don’t have easy access to them. NEVER take records from a facility or include a client's name on paperwork that leaves the facility.
- Illegally or unauthorized accessing of client files. If someone you know, like a neighbor, coworker, or family member is admitted to the unit you are working on, do not access their medical record unless you are directly caring for them. Facilities have the capability of tracing everything you access within the electronic medical record and holding you accountable. This rule holds true for employees who previously cared for a client as a student; once your shift is over as a student, you should no longer access that client’s medical records.
- Sharing information with unauthorized people. Anytime you share medical information with anyone but the client themselves, you must have written permission to do so. For instance, if a husband comes to you and wants to know his spouse’s lab results, you must have permission from his spouse before you can share that information with him. Just confirming or denying that a client has been admitted to a unit or agency can be considered a breach of confidentiality. Furthermore, voicemails should not be left regarding protected client information.
- Information can generally be shared with the parents of children until they turn 18, although there are exceptions to this rule if the minor child seeks birth control, an abortion, or becomes pregnant. After a child turns 18, information can no longer be shared with the parent unless written permission is provided, even if the minor is living at home and/or the parents are paying for their insurance or health care. As a general rule, any time you are asked for client information, check first to see if the client has granted permission.
- Texting or e-mailing regarding client information on an unencrypted device. Only use properly encrypted devices that have been approved by your health care facility for e-mailing or faxing protected client information. Also, ensure that the information is being sent to the correct person, address, or phone number.
- Sharing information on social media. Never post anything on social media that has anything to do with your clients, the facility where you are working or have clinical, or even how your day went at the agency. Nurses and other professionals have been fired for violating HIPAA rules on social media.[77],[78],[79]
Social Media Guidelines
Nursing students, nurses, and other health care team members must use extreme caution when posting to Facebook, Instagram, Twitter, Snapchat, and other social media sites. Information related to clients, client care, and/or health care agencies should never be posted on social media; health care team members who violate this guideline can lose their jobs and may face legal action and students can be disciplined or expelled from their nursing program. Be aware that even if you think you are posting in a private group, the information can become public.
The American Nurses Association (ANA) has established the following principles for nurses using social media:[80]
- Nurses must not transmit or place online individually identifiable client information.
- Nurses must observe ethically prescribed professional client-nurse boundaries.
- Nurses should understand that clients, colleagues, organizations, and employers may view postings.
- Nurses should take advantage of privacy settings and seek to separate personal and professional information online.
- Nurses should bring content that could harm a client’s privacy, rights, or welfare to the attention of appropriate authorities.
- Nurses should participate in developing organizational policies governing online conduct.
In addition to these principles, the ANA has also provided these tips for nurses and nursing students using social media:[81]
- Remember that standards of professionalism are the same online as in any other circumstance.
- Do not share or post information or photos gained through the nurse-client relationship.
- Maintain professional boundaries in the use of electronic media. Online contact with clients blurs this boundary.
- Do not make disparaging remarks about clients, employers, or coworkers, even if they are not identified.
- Do not take photos or videos of clients on personal devices, including cell phones.
- Promptly report a breach of confidentiality or privacy.
Read more about the ANA's Social Media Principles.
Code of Ethics
In addition to legal considerations, there are also several ethical guidelines for nursing care.
There is a difference between morality, ethical principles, and a code of ethics. Morality refers to “personal values, character, or conduct of individuals within communities and societies.”[82] An ethical principle is a general guide, basic truth, or assumption that can be used with clinical judgment to determine a course of action. Four common ethical principles are beneficence (do good), nonmaleficence (do no harm), autonomy (control by the individual), and justice (fairness). A code of ethics is set for a profession and makes their primary obligations, values, and ideals explicit.
The American Nursing Association (ANA) guides nursing practice with the Code of Ethics for Nurses.[83] This code provides a framework for ethical nursing care and a guide for decision-making. The Code of Ethics for Nurses serves the following purposes:
- It is a succinct statement of the ethical values, obligations, duties, and professional ideals of nurses individually and collectively.
- It is the profession’s nonnegotiable ethical standard.
- It is an expression of nursing’s own understanding of its commitment to society.[84]
The ANA Code of Ethics contains nine provisions. See a brief description of each provision in the following box.
Provisions of the ANA Code of Ethics[85]
The nine provisions of the ANA Code of Ethics are briefly described below. The full code is available to read for free at Nursingworld.org.
Provision 1: The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person.
Provision 2: The nurse’s primary commitment is to the patient, whether an individual, family, group, community, or population.
Provision 3: The nurse promotes, advocates for, and protects the rights, health, and safety of the patient.
Provision 4: The nurse has authority, accountability, and responsibility for nursing practice; makes decisions; and takes action consistent with the obligation to promote health and to provide optimal care.
Provision 5: The nurse owes the same duties to self as to others, including the responsibility to promote health and safety, preserve wholeness of character and integrity, maintain competence, and continue personal and professional growth.
Provision 6: The nurse, through individual and collective effort, establishes, maintains, and improves the ethical environment of the work setting and conditions of employment that are conducive to safe, quality health care.
Provision 7: The nurse, in all roles and settings, advances the profession through research and scholarly inquiry, professional standards development, and the generation of both nursing and health policy.
Provision 8: The nurse collaborates with other health professionals and the public to protect human rights, promote health diplomacy, and reduce health disparities.
Provision 9: The profession of nursing, collectively through its professional organizations, must articulate nursing values, maintain the integrity of the profession, and integrate principles of social justice into nursing and health policy.
The ANA Center for Ethics and Human Rights
In addition to publishing the Code of Ethics, the ANA Center for Ethics and Human Rights was established to help nurses navigate ethical and value conflicts and life-and-death decisions, many of which are common to everyday practice.
Check your knowledge with the following questions:
As with electrolytes, correct balance of acids and bases in the body is essential to proper body functioning. Even a slight variance outside of normal can be life-threatening, so it is important to understand normal acid-base values, as well their causes and how to correct them. The kidneys and lungs work together to correct slight imbalances as they occur. As a result, the kidneys compensate for shortcomings of the lungs, and the lungs compensate for shortcomings of the kidneys.
Arterial Blood Gases
Arterial blood gases (ABG) are measured by collecting blood from an artery, rather than a vein, and are most commonly collected via the radial artery. ABGs measure the pH level of the blood, the partial pressure of arterial oxygen (PaO2), the partial pressure of arterial carbon dioxide (PaCO2), the bicarbonate level (HCO3), and the oxygen saturation level (SaO2).
![]() Prior to collecting blood gases, it is important to ensure the client has appropriate arterial blood flow to the hand. This is done by performing the Allen test. When performing the Allen test, pressure is held on both the radial and ulnar artery below the wrist. Pressure is released from the ulnar artery to check if blood flow is adequate. If arterial blood flow is adequate, warmth and color should return to the hand.
Prior to collecting blood gases, it is important to ensure the client has appropriate arterial blood flow to the hand. This is done by performing the Allen test. When performing the Allen test, pressure is held on both the radial and ulnar artery below the wrist. Pressure is released from the ulnar artery to check if blood flow is adequate. If arterial blood flow is adequate, warmth and color should return to the hand.
pH
pH is a scale from 0-14 used to determine the acidity or alkalinity of a substance. A neutral pH is 7, which is the same pH as water. Normally, the blood has a pH between 7.35 and 7.45. A blood pH of less than 7.35 is considered acidic, and a blood pH of more than 7.45 is considered alkaline.
The pH of blood is a measure of hydrogen ion concentration. A low pH, less than 7.35, occurs in acidosis when the blood has a high hydrogen ion concentration. A high pH, greater than 7.45, occurs in alkalosis when the blood has a low hydrogen ion concentration. Hydrogen ions are by-products of the metabolism of substances such as proteins, fats, and carbohydrates. These by-products create extra hydrogen ions (H+) in the blood that need to be balanced and kept within normal range as described earlier.
The body has several mechanisms for maintaining blood pH. The lungs are essential for maintaining pH, and the kidneys also play a role. For example, when the pH is too low (i.e., during acidosis), the respiratory rate quickly increases to eliminate acid in the form of carbon dioxide (CO2). The kidneys excrete additional hydrogen ions (acid) in the urine and retain bicarbonate (base). Conversely, when the pH is too high (i.e., during alkalosis), the respiratory rate decreases to retain acid in the form of CO2. The kidneys excrete bicarbonate (base) in the urine and retain hydrogen ions (acid).
PaCO2
PaCO2 is the partial pressure of arterial carbon dioxide in the blood. The normal PaCO2 level is 35-45 mmHg. CO2 forms an acid in the blood that is regulated by the lungs by changing the rate or depth of respirations.
As the respiratory rate increases or becomes deeper, additional CO2 is removed, causing decreased acid (H+) levels in the blood and increased pH (i.e., the blood becomes more alkaline). As the respiratory rate decreases or becomes shallower, less CO2 is removed, causing increased acid (H+) levels in the blood and decreased pH (i.e., the blood becomes more acidic).
Generally, the lungs work quickly to regulate the PaCO2 levels and cause a quick change in the pH. Therefore, an acid-base problem caused by hypoventilation can be quickly corrected by increasing ventilation, and a problem caused by hyperventilation can be quickly corrected by decreasing ventilation. For example, if an anxious client is hyperventilating, they may be asked to breathe into a paper bag to rebreathe some of the CO2 they are blowing off. Conversely, a postoperative client who is experiencing hypoventilation due to the sedative effects of receiving morphine is asked to cough and deep breathe to blow off more CO2.
HCO3
HCO3 is the bicarbonate level of the blood and the normal range is 22-26. HCO3 is a base managed by the kidneys and helps to make the blood more alkaline. The kidneys take longer than the lungs to adjust the acidity or alkalinity of the blood, and the response is not visible upon assessment. As the kidneys sense an alteration in pH, they begin to retain or excrete HCO3, depending on what is needed. If the pH becomes acidic, the kidneys retain HCO3 to increase the amount of bases present in the blood to increase the pH (i.e., the blood becomes alkaline). Conversely, if the pH becomes alkalotic, the kidneys excrete more HCO3, causing the pH to decrease (i.e., the blood becomes more acidic).
PaO2
PaO2 is the partial pressure of arterial oxygen in the blood. It more accurately measures a client’s oxygenation status than SaO2 (the measurement of hemoglobin saturation with oxygen). Therefore, ABG results are also used to manage clients in respiratory distress.
See Table 15.5a for a review of ABG components, normal values, and key critical values. A critical ABG value means there is a greater risk of serious complications and even death if not corrected rapidly. For example, a pH of 7.10, a shift of only 0.25 below normal, is often fatal because this level of acidosis can cause cardiac or respiratory arrest or significant hyperkalemia.[86] As you can see, failure to recognize ABG abnormalities can have serious consequences for your clients.
Table 15.5a ABG Components, Descriptions, Adult Normal Values, and Critical Values[87]
| ABG Component | Description | Adult Normal Value | Critical Value |
|---|---|---|---|
| pH |
|
7.35-7.45 | Less than 7.25
Greater than 7.60 |
| PaO2 |
|
80-100 mmHg | Less than 60 mmHg |
| PaCO2 |
|
35-45 mmHg | Less than 25 mmHg
Greater than 60 mmHg |
| HCO3 |
|
22-26 mEq/L | Less than 10 mEq/L
Greater than 40 mEq/L |
| SaO2 |
|
95-100% | Less than 88% |
Video Review of Acid-Base Balance[88]
Interpreting Arterial Blood Gases
After the ABG results are received, it is important to understand how to interpret them. A variety of respiratory, metabolic, electrolyte, or circulatory problems can cause acid-base imbalances. Correct interpretation helps the nurse and other health care providers determine the appropriate treatment and evaluate the effectiveness of interventions.
Arterial blood gasses can be interpreted as one of four conditions: respiratory acidosis, respiratory alkalosis, metabolic acidosis, or metabolic alkalosis. Once this interpretation is made, conditions can further be classified as compensated, partially compensated, or uncompensated. A simple way to remember how to interpret ABGs is by using the ROME method of interpretation, which stands for Respiratory Opposite, Metabolic Equal. This means that the respiratory component (PaCO2) moves in the opposite direction of the pH if the respiratory system is causing the imbalance. If the metabolic system is causing the imbalance, the metabolic component (HCO3) moves in the same direction as the pH. Some nurses find the Tic-Tac-Toe method of interpretation helpful. If you would like to learn more about this method, watch the video below.
Review of Tic-Tac-Toe Method of ABG Interpretation[89]
Respiratory Acidosis
Respiratory acidosis develops when carbon dioxide (CO2) builds up in the body (referred to as hypercapnia), causing the blood to become increasingly acidic. Respiratory acidosis is identified when reviewing ABGs and the pH level is below 7.35 and the PaCO2 level is above 45, indicating the cause of the acidosis is respiratory. Note that in respiratory acidosis, as the PaCO2 level increases, the pH level decreases. Respiratory acidosis is typically caused by a medical condition that decreases the exchange of oxygen and carbon dioxide at the alveolar level, such as an acute asthma exacerbation, chronic obstructive pulmonary disease (COPD), or an acute heart failure exacerbation causing pulmonary edema. It can also be caused by decreased ventilation from anesthesia, alcohol, or administration of medications such as opioids and sedatives.
Chronic respiratory diseases, such as COPD, often cause chronic respiratory acidosis that is fully compensated by the kidneys retaining HCO3. Because the carbon dioxide levels build up over time, the body adapts to elevated PaCO2 levels, so they are better tolerated. However, in acute respiratory acidosis, the body has not had time to adapt to elevated carbon dioxide levels, causing mental status changes associated with hypercapnia. Acute respiratory acidosis is caused by acute respiratory conditions, such as an asthma attack or heart failure exacerbation with pulmonary edema when the lungs suddenly are not able to ventilate adequately. As breathing slows and respirations become shallow, less CO2 is excreted by the lungs and PaCO2 levels quickly rise.
Signs of symptoms of hypercapnia vary depending upon the level and rate of CO2 accumulation in arterial blood:
- Clients with mild to moderate hypercapnia may be anxious and/or complain of mild dyspnea, daytime sluggishness, headaches, or hypersomnolence.
- Clients with higher levels of CO2 or rapidly developing hypercapnia develop delirium, paranoia, depression, confusion, or decreased level of consciousness that can progress to seizures and coma as levels continue to rise.
Individuals with normal lung function typically exhibit a depressed level of consciousness when the PaCO2 is greater than 75 to 80 mmHg, whereas clients with chronic hypercapnia may not develop symptoms until the PaCO2 rises above 90 to 100 mmHg.[90]
When a client demonstrates signs of potential hypercapnia, the nurse should assess airway, breathing, and circulation. It is important to note that SaO2 levels may be normal with hypercapnia, and as such should not be the determining factor in further assessing acid-base issues. Urgent assistance should be sought, especially if the client is in respiratory distress. The provider will order an ABG and prescribe treatments based on assessment findings and potential causes. Treatment for respiratory acidosis typically involves improving ventilation and respiration by removing airway restrictions, reversing oversedation, administering nebulizer treatments, or increasing the rate and depth of respiration by using a BiPAP or CPAP devices. BiPAP and CPAP devices provide noninvasive positive pressure ventilation to increase the depth of respirations, remove carbon dioxide, and oxygenate the client. If these noninvasive interventions are not successful, the client will need to be intubated and placed on mechanical ventilation.[91],[92]
Read more details about oxygenation equipment in “Oxygen Therapy” in Open RN Nursing Skills, 2e.
Respiratory Alkalosis
Respiratory alkalosis develops when the body removes too much carbon dioxide through respiration, resulting in increased pH and an alkalotic state. When reviewing ABGs, respiratory alkalosis is identified when pH levels are above 7.45 and the PaCO2 level is below 35. With respiratory alkalosis, notice that as the PaCO2 level decreases, the pH level increases.
Respiratory alkalosis is caused by hyperventilation that can occur due to anxiety, panic attacks, pain, fear, head injuries, or mechanical ventilation. Overdoses of salicylates and other toxins can also cause respiratory alkalosis initially and then often progress to metabolic acidosis in later stages. Acute asthma exacerbations, pulmonary embolisms, or other respiratory disorders can initially cause respiratory alkalosis as the lungs breathe faster in an attempt to increase oxygenation, which decreases the PaCO2. After a while, however, these hypoxic disorders cause respiratory acidosis as respiratory muscles tire, breathing slows, and CO2 builds up in the blood.
Clients experiencing respiratory alkalosis often report feelings of shortness of breath, dizziness or light-headedness, chest pain or tightness, paresthesias, and palpitations as a result of decreased carbon dioxide levels.[93] Respiratory alkalosis is not fatal, but it is important to recognize that underlying conditions such as an asthma exacerbation or pulmonary embolism can be life-threatening, so treatment of these underlying conditions is essential. As the pH level increases, the kidneys will attempt to compensate for the shortage of H+ ions by reabsorbing HCO3 before it can be excreted in the urine. This is a slow process, so additional treatment may be necessary.
Treatment of respiratory alkalosis involves treating the underlying cause of the hyperventilation. Acute management of clients who are hyperventilating should focus on client reassurance, an explanation of the symptoms the client is experiencing, removal of any stressors, and initiation of breathing retraining. Breathing retraining attempts to focus the client on abdominal (diaphragmatic) breathing. Read more about breathing retraining in the following box.
Breathing Retraining
While sitting or lying supine, the client should place one hand on their abdomen and the other on the chest, and then be asked to observe which hand moves with greater excursion. In hyperventilating clients, this will almost always be the hand on the chest. Ask the client to adjust their breathing so that the hand on the abdomen moves with greater excursion and the hand on the chest barely moves at all. Assure the client that this is hard to learn and will take some practice to fully master. Ask the client to breathe in slowly over four seconds, pause for a few seconds, and then breathe out over a period of eight seconds. After 5 to 10 such breathing cycles, the client should begin to feel a sense of calmness with a reduction in anxiety and an improvement in hyperventilation. Symptoms should ideally resolve with continuation of this breathing exercise.
If the breathing retraining technique is not successful in resolving a hyperventilation episode and severe symptoms persist, the client may be prescribed a small dose of a short-acting benzodiazepine (e.g., lorazepam 0.5 to 1 mg orally or 0.5 to 1 mg intravenously). Current research indicates that instructing clients who are hyperventilating to rebreathe carbon dioxide (CO2) by breathing into a paper bag can cause significant hypoxemia with significant complications, so this intervention is no longer recommended. If rebreathing is used, oxygen saturation levels should be continuously monitored.[94]
Metabolic Acidosis
Metabolic acidosis occurs when there is an accumulation of acids (hydrogen ions) and not enough bases (HCO3) in the body. Under normal conditions, the kidneys work to excrete acids through urine and neutralize excess acids by increasing bicarbonate (HCO3) reabsorption from the urine to maintain a normal pH. When the kidneys are not able to perform this buffering function to the level required to excrete and neutralize the excess acid, metabolic acidosis results.
Metabolic acidosis is characterized by a pH level below 7.35 and an HCO3 level below 22 when reviewing ABGs. It is important to notice that both the pH and HCO3 decrease with metabolic acidosis (i.e., the pH and HCO3 move in the same downward direction). A common cause of metabolic acidosis is diabetic ketoacidosis, where acids called ketones build up in the blood when blood sugar is extremely elevated. Another common cause of metabolic acidosis in hospitalized clients is lactic acidosis, which can be caused by impaired tissue oxygenation. Metabolic acidosis can also be caused by increased loss of bicarbonate due to severe diarrhea or from renal disease that causes decreased acid elimination. Additionally, toxins such as salicylate excess can cause metabolic acidosis.[95]
Nurses may first suspect that a client has metabolic acidosis due to rapid breathing that occurs as the lungs try to remove excess CO2 in an attempt to resolve the acidosis. Other symptoms of metabolic acidosis include confusion, decreased level of consciousness, hypotension, and electrolyte disturbances that can progress to circulatory collapse and death if not treated promptly. It is important to quickly notify the provider of suspected metabolic acidosis so that an ABG can be drawn, and treatment prescribed (based on the cause of the metabolic acidosis) to allow acid levels to improve. Treatment includes IV fluids to improve hydration status, glucose management, and circulatory support. When pH drops below 7.1, IV sodium bicarbonate is often prescribed to help neutralize the acids in the blood.[96],[97]
Metabolic Alkalosis
Metabolic alkalosis occurs when there is too much bicarbonate (HCO3) in the body or an excessive loss of acid (H+ ions). Metabolic alkalosis is defined by a pH above 7.45 and an HCO3 level above 26 on ABG results. Note that both pH and HCO3 are elevated in metabolic alkalosis.
Metabolic alkalosis can be caused by gastrointestinal loss of hydrogen ions, excessive urine loss, excessive levels of bicarbonate, or a shift of hydrogen ions from the bloodstream into cells.
Prolonged vomiting or nasogastric suctioning can also cause metabolic alkalosis. Gastric secretions have high levels of hydrogen ions (H+), so as acid is lost, the pH level of the bloodstream increases.
Excessive urinary loss (due to diuretics or excessive mineralocorticoids) can cause metabolic alkalosis due to loss of hydrogen ions in the urine. Intravenous administration of sodium bicarbonate can also cause metabolic alkalosis due to increased levels of bases introduced into the body. Although it was once thought that excessive intake of calcium antacids could cause metabolic alkalosis, it has been found that this only occurs if they are administered concurrently with Kayexelate.[98]
Hydrogen ions may shift into cells due to hypokalemia, causing metabolic alkalosis. When hypokalemia occurs (i.e., low levels of potassium in the bloodstream), potassium shifts out of cells and into the bloodstream in an attempt to maintain a normal level of serum potassium for optimal cardiac function. However, as the potassium (K+) molecules move out of the cells, hydrogen (H+) ions then move into the cells from the bloodstream to maintain electrical neutrality. This transfer of ions causes the pH in the bloodstream to drop, causing metabolic alkalosis.[99]
A nurse may first suspect that a client has metabolic alkalosis due to a decreased respiratory rate (as the lungs try to retain additional CO2 to increase the acidity of the blood and resolve the alkalosis). The client may also be confused due to the altered pH level. The nurse should report signs of suspected metabolic alkalosis because uncorrected metabolic alkalosis can result in hypotension and cardiac dysfunction.[100]
Treatment is prescribed based on the ABG results and the suspected cause. For example, treat the cause of the vomiting, stop the gastrointestinal suctioning, or stop the administration of diuretics. If hypokalemia is present, it should be treated. If bicarbonate is being administered, it should be stopped. Clients with kidney disease may require dialysis.[101]
Analyzing ABG Results
Now that we’ve discussed the differences between the various acid-base imbalances, let’s review the steps to systematically interpret ABG results. Table 15.5b outlines the steps of ABG interpretation.
Table 15.5b Analyzing ABG Results[102],[103]
| Step | Action |
|---|---|
| Step 1: pH (normal 7.35-7.45) | If pH is out of range, determine if it is acidosis or alkalosis:
|
| Step 2: PaCO2 (normal 35-45 mmHg) |
**If the imbalance does not appear to be caused by a respiratory problem, move on to evaluate the HCO3. |
| Step 3: HCO3 (normal 22-26) |
|
| Step 4: Determine level of compensation | After determining the cause of the pH imbalance, determine if compensation is occurring.
|
Localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.
Learning Activities
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Ms. Curtis is a 67-year-old client admitted for a left total knee replacement. She is post-op Day 2 and is currently receiving care on the medical-surgical unit. Ms. Curtis has been complaining of pain and refused her previous two physical therapy appointments. She agrees to sitting up in the chair but declines walking.
- What focused assessments should the nurse perform and why?
- What complications could occur related to Ms. Curtis' immobility?
- What SMART outcomes should the nurse plan in collaboration with Ms. Curtis?
- List interventions the nurse should plan for Ms. Curtis and their rationale.
- How will the nurse evaluate if the interventions are successful?

Test your knowledge using this NCLEX Next Generation-style bowtie question. You may reset and resubmit your answers to this question an unlimited number of times.[104]
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Practice what you have learned in this chapter by completing these learning activities. When accessing the online activities that contain videos, it is best to use Google Chrome or Firefox browsers.
1. To test your understanding of therapeutic and nontherapeutic terms, complete this online quiz:
Therapeutic Communication Techniques vs. Non-therapeutic Communication Techniques Quizlet
2. Consider the following scenario and describe actions that you might take to facilitate the communication experience.
You are caring for Mr. Curtis, an 87-year-old client newly admitted to the medical surgical floor with a hip fracture. You are preparing to complete his admission history and need to collect relevant health information and complete a physical exam. You approach the room, knock at the door, complete hand hygiene, and enter. Upon entry, you see Mr. Curtis is in bed surrounded by multiple family members. The television is on in the background, and you also note the sound of meal trays being delivered in the hallway.
Based on the described scenario, what actions might be implemented to aid in your communication with Mr. Curtis?

Test your knowledge using this NCLEX Next Generation-style question. You may reset and resubmit your answers to this question an unlimited number of times.[106]

Test your knowledge using this NCLEX Next Generation-style question. You may reset and resubmit your answers to this question an unlimited number of times.[107]
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Assessing a client’s risk for falls and planning interventions to prevent falls are common safety strategies completed by nurses. This section uses a client scenario to demonstrate how to use the nursing process to assess a client and then create a nursing care plan to prevent falls. Begin by reading the Handoff Report received from the nurse on the previous shift.

Handoff Report
Mr. Moore is a 72-year-old widower recovering in the hospital after sustaining injuries he received from a fall at home. See Figure 5.15 for an image of Mr. Moore.[108] He fractured his right hip and underwent surgical repair two days ago. He is receiving IV fluids and morphine for pain control. He has a history of hypertension and cardiovascular disease. He wears glasses and hearing aids. Per recommendations from the physical therapist, he is able to transfer with one assist with a walker but is weak on his right side. He has an order to ambulate at least 100 feet four times daily with a wheeled walker. He is 6 feet tall and weighs 165 pounds. Prior to the fall, he lived at home alone independently, and he is looking forward to returning home.
Assessment
The nurse collects the following assessment findings:
- Vital Signs: Blood pressure 90/60, heart rate 56, respiratory rate 18, temperature 37 degrees Celsius, pulse oximetry reading 92%, current pain level 0
- Alert and oriented x 3 to person, place, and time
- Lungs clear
- Cardiovascular Assessment: Heart rate is regular, capillary refill less than 3 seconds in fingers and toes, pedal pulses 2+
- Right lower extremity strength is 1+ (weak)
- Ambulates with walker with assistance; gait is unsteady
Critical Thinking Questions
1. Describe the fall risk factors for Mr. Moore.
2. Use the Morse Fall Risk Scale to assess Mr. Moore’s risk for falling.
Diagnosis
The NANDA-I nursing diagnosis is established: Risk for Falls as evidenced by lower extremity weakness and difficulty with gait.
Outcome Identification
Overall Goal: Mr. Moore will remain free from falls during his hospitalization stay.
SMART Expected Outcomes:
- Mr. Moore will not experience a fall during hospitalization.
- Mr. Moore will correctly use his assistive device (walker) every time he ambulates during hospitalization.
Planning Interventions
The following interventions are planned based on Mr. Moore’s fall risk factors.
- Remove clutter from the floor.
- Provide adequate lighting with a night-light at the bedside.
- Use half side rails to prevent falls from the bed.
- Monitor gait, balance, and fatigue with ambulation and encourage resting as needed.
- Place personal items within easy reach of the client at the bedside.
- Provide an elevated toilet seat.
- Encourage the use of prescribed glasses and hearing aids when walking.
- Obtain orthostatic blood pressures daily and notify the provider as indicated.
- Ensure the client wears shoes that fit properly, are fastened securely, and have no-skid soles.
- Suggest home adaptations to improve safety after discharge, such as adjusting the toilet seat height, installing grab bars in the bathroom, and using a rubber mat in the shower.
Critical Thinking Question
3. What additional interventions could be implemented for Mr. Moore to reduce his risk of falls that target his specific risk factors?
Implementation of Interventions
The following day, upon entering the room, you find Mr. Moore has climbed out of bed and is on his way to the bathroom. He states, “I need to go to the bathroom for a bowel movement and didn’t have time to ring the call light and wait.” You assist him with his walker, but he seems unsteady on his feet as he walks toward the bathroom. You’re not sure if he will make it to the toilet without falling. He says, “We need to hurry or I’m not going to make it.”
Critical Thinking Question
4. What is the best response?
Evaluation
The nurse evaluates Mr. Moore’s progress based on the established expected outcomes:
- Mr. Moore will not experience a fall during hospitalization: Outcome Met.
- Mr. Moore will use his assistive device (walker) correctly during hospitalization: Outcome Partially Met.
Mr. Moore forgets to call for assistance and uses a walker when he needs to go to the bathroom. A “stop” sign has been placed within client view to remind him to use the call light before getting up. In addition to hourly rounding, toileting will be performed at scheduled intervals every two hours. An icon has been posted on the doorframe to alert staff that the client is at high risk for falls. In addition to the bed being kept low and locked, a mat will be placed next to the bed at night. If Mr. Moore continues to forget to call for assistance, a bed alarm will be placed to alert staff of movement so that quick assistance can be offered.

