7.2 Head and Neck Basic Concepts
Open Resources for Nursing (Open RN)
To perform and document an accurate assessment of the head and neck, it is important to understand their basic anatomy and physiology.
Anatomy
Skull
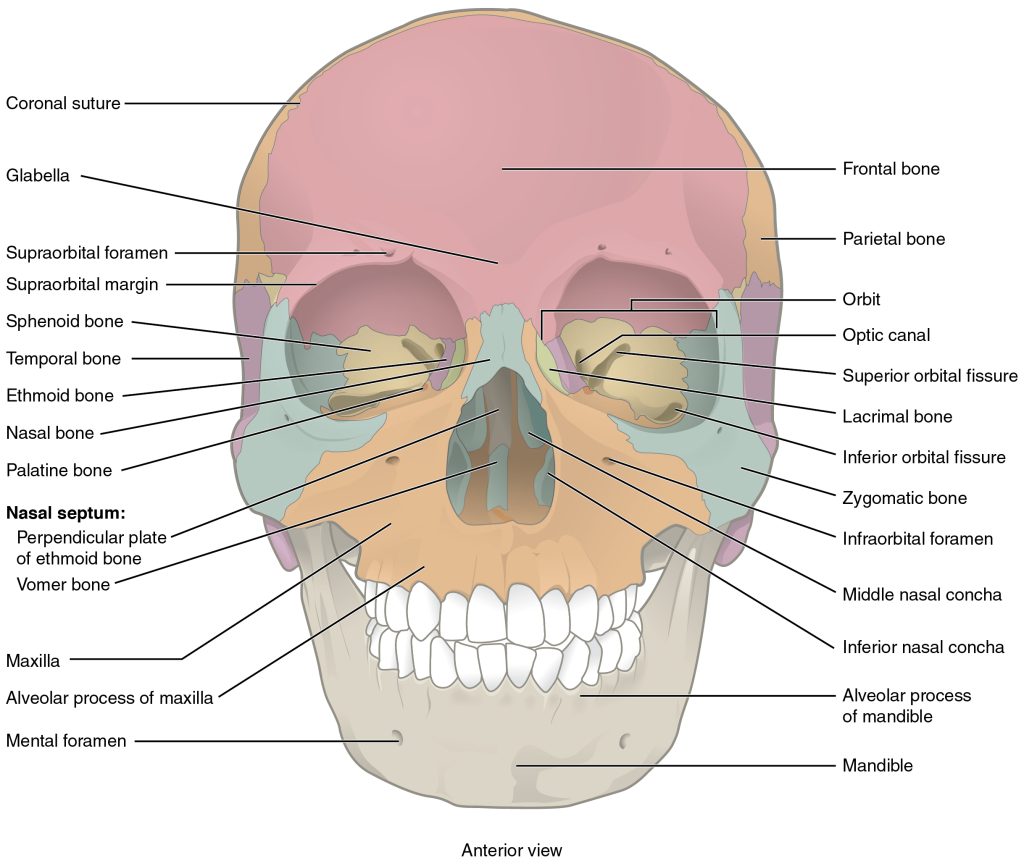
The anterior skull consists of facial bones that provide the bony support for the eyes and structures of the face. This anterior view of the skull is dominated by the openings of the orbits, the nasal cavity, and the upper and lower jaws. See Figure 7.1[1] for an illustration of the skull. The orbit is the bony socket that houses the eyeball and the muscles that move the eyeball. Inside the nasal area of the skull, the nasal cavity is divided into halves by the nasal septum that consists of both bone and cartilage components. The mandible forms the lower jaw and is the only movable bone in the skull. The maxilla forms the upper jaw and supports the upper teeth.[2]
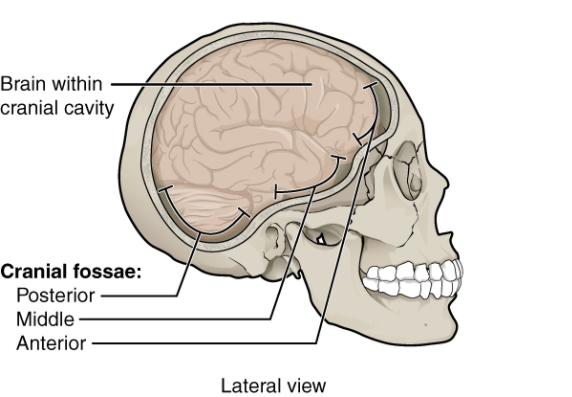
The cranium, or “brain case,” surrounds and protects the brain that occupies the cranial cavity. See Figure 7.2[3] for an image of the brain within the cranial cavity. The brain case consists of eight bones, including the paired parietal and temporal bones, plus the unpaired frontal, occipital, sphenoid, and ethmoid bones.[4]
A suture is an interlocking joint between adjacent bones of the skull and is filled with dense, fibrous connective tissue that unites the bones. In a newborn infant, the pressure from vaginal delivery compresses the head and causes the bony plates to overlap at the sutures, creating a small ridge. Over the next few days, the head expands, the overlapping disappears, and the edges of the bony plates meet edge to edge. This is the normal position for the remainder of the life span and the sutures become immobile.
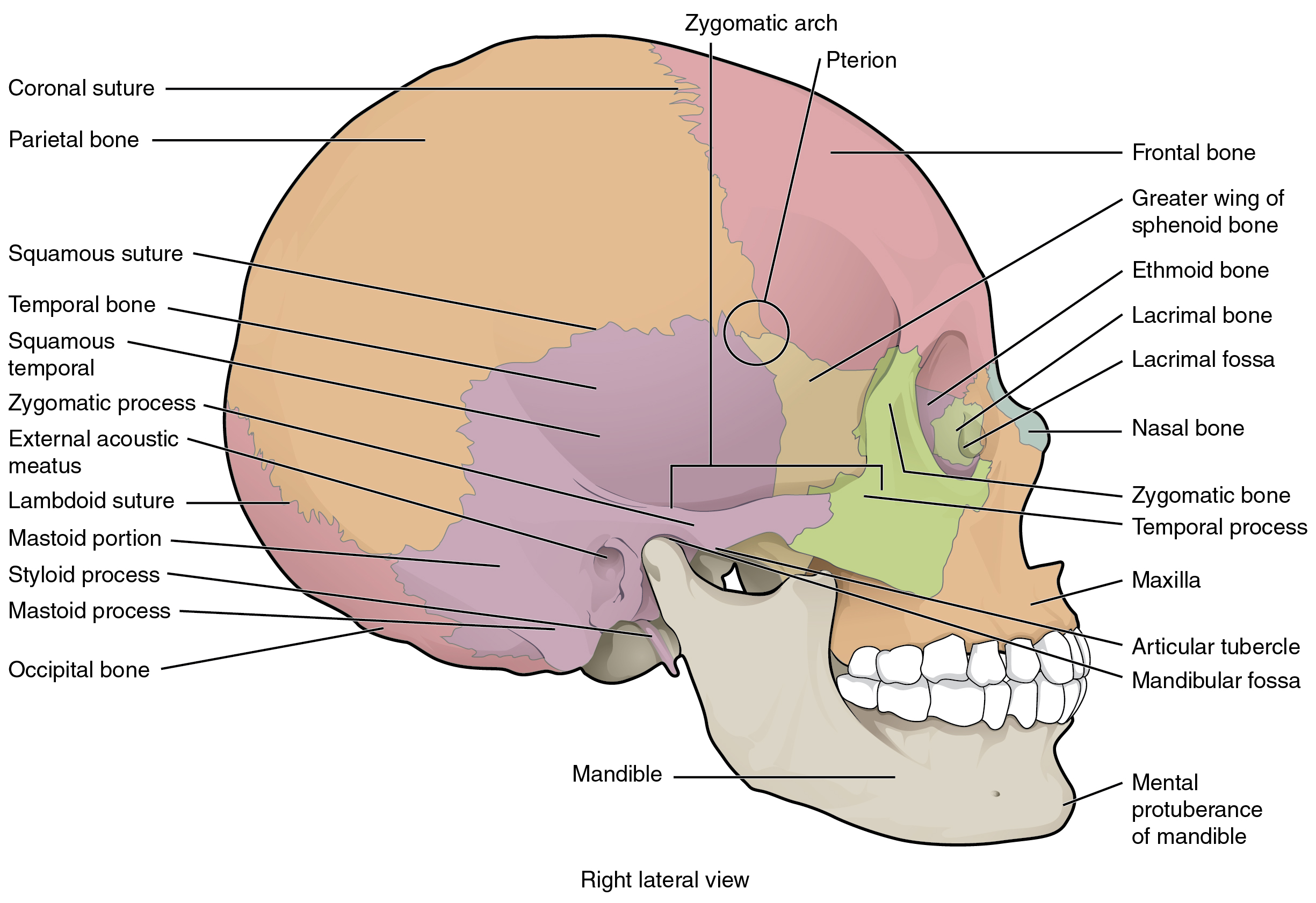
See Figure 7.3[5] for an illustration of two of the sutures, the coronal and squamous sutures, on the lateral view of the head. The coronal suture is seen on the top of the skull. It runs from side to side across the skull and joins the frontal bone to the right and left parietal bones. The squamous suture is located on the lateral side of the skull. It unites the squamous portion of the temporal bone with the parietal bone. At the intersection of the coronal and squamous sutures is the pterion, a small, capital H-shaped suture line region that unites the frontal bone, parietal bone, temporal bone, and greater wing of the sphenoid bone. The pterion is an important clinical landmark because located immediately under it, inside the skull, is a major branch of an artery that supplies the brain. A strong blow to this region can fracture the bones around the pterion. If the underlying artery is damaged, bleeding can cause the formation of a collection of blood, called a hematoma, between the brain and interior of the skull, which can be life-threatening.[6]
Paranasal Sinuses
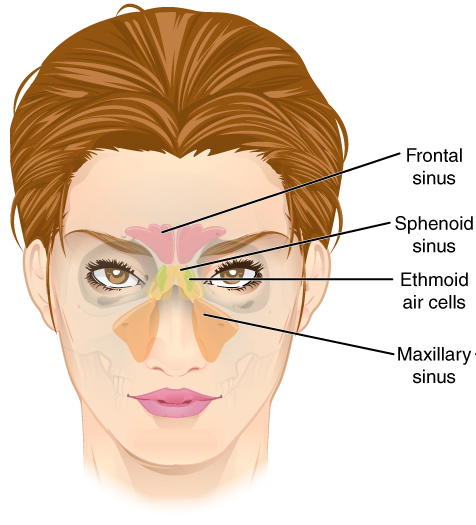
The paranasal sinuses are hollow, air-filled spaces located within the skull. See Figure 7.4[7] for an illustration of the sinuses. The sinuses connect with the nasal cavity and are lined with nasal mucosa. They reduce bone mass, lightening the skull, and also add resonance to the voice. When a person has a cold or sinus congestion, the mucosa swells and produces excess mucus that often obstructs the narrow passageways between the sinuses and the nasal cavity. The resulting pressure produces pain and discomfort.[8]
Each of the paranasal sinuses is named for the skull bone that it occupies. The frontal sinus is located just above the eyebrows within the frontal bone. The largest sinus, the maxillary sinus, is paired and located within the right and left maxillary bones just below the orbits. The maxillary sinuses are most commonly involved during sinus infections. The sphenoid sinus is a single, midline sinus located within the body of the sphenoid bone. The lateral aspects of the ethmoid bone contain multiple small spaces separated by very thin, bony walls. Each of these spaces is called an ethmoid air cell.
Anatomy of Nose, Pharynx, and Mouth
See Figure 7.5[9] to review the anatomy of the head and neck. The major entrance and exit for the respiratory system is through the nose. The bridge of the nose consists of bone, but the protruding portion of the nose is composed of cartilage. The nares are the nostril openings that open into the nasal cavity and are separated into left and right sections by the nasal septum. The floor of the nasal cavity is composed of the palate. The hard palate is located at the anterior region of the nasal cavity and is composed of bone. The soft palate is located at the posterior portion of the nasal cavity and consists of muscle tissue. The uvula is a small, teardrop-shaped structure located at the apex of the soft palate. Both the uvula and soft palate move like a pendulum during swallowing, swinging upward to close off the nasopharynx and prevent ingested materials from entering the nasal cavity.[10]
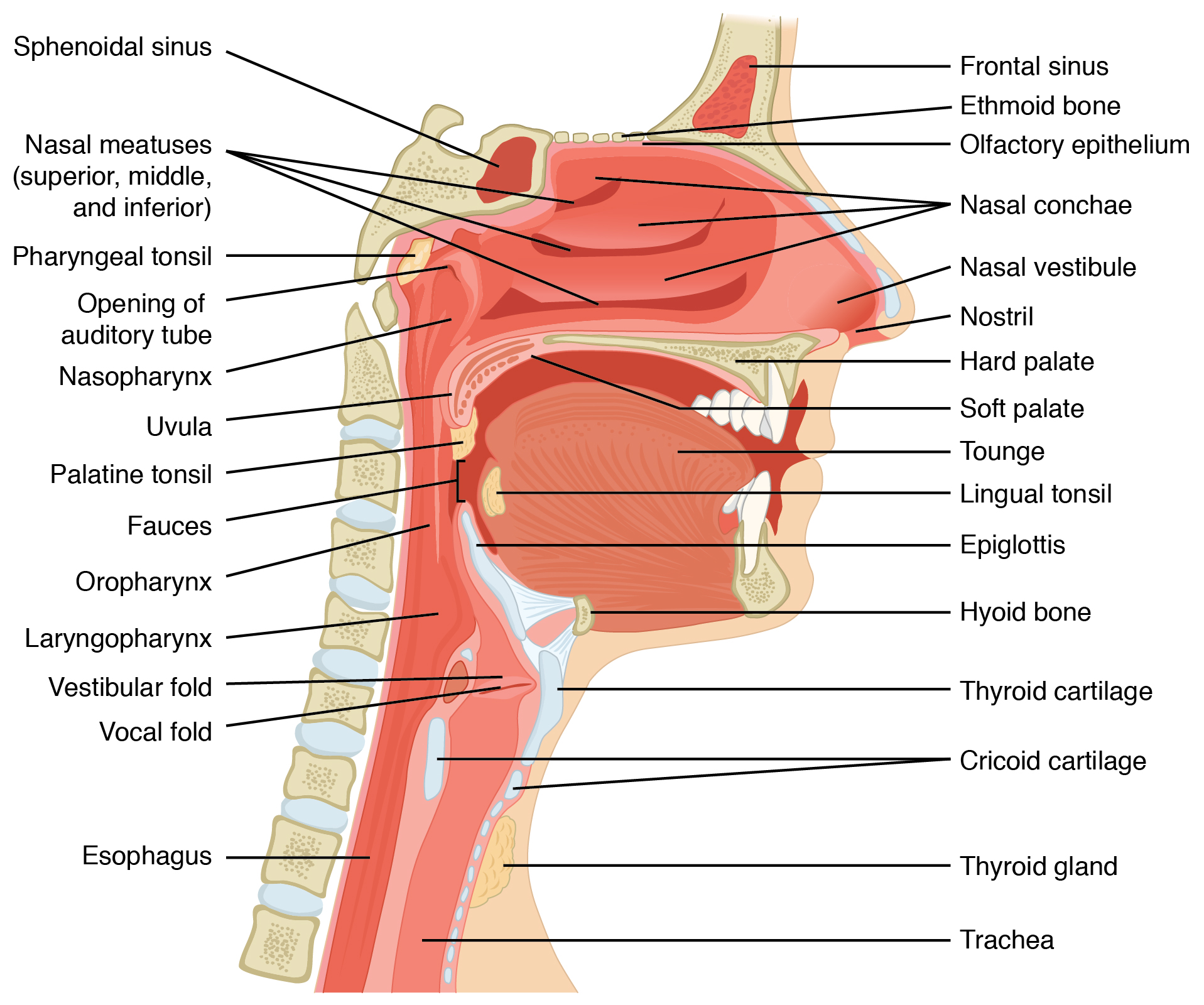
As air is inhaled through the nose, the paranasal sinuses warm and humidify the incoming air as it moves into the pharynx. The pharynx is a tube-lined mucous membrane that begins at the nasal cavity and is divided into three major regions: the nasopharynx, the oropharynx, and the laryngopharynx.[11]
The nasopharynx serves only as an airway. At the top of the nasopharynx is the pharyngeal tonsil, commonly referred to as the adenoids. Adenoids are lymphoid tissue that trap and destroy invading pathogens that enter during inhalation. They are large in children but tend to regress with age and may even disappear.[12]
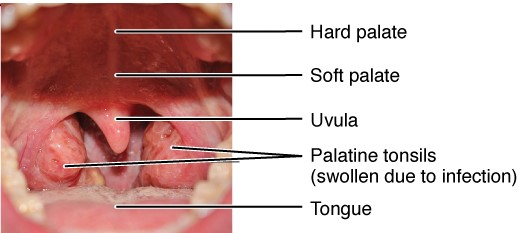
The oropharynx is a passageway for both air and food. The oropharynx is bordered superiorly by the nasopharynx and anteriorly by the oral cavity. The oropharynx contains two sets of tonsils, the palatine and lingual tonsils. The palatine tonsil is located laterally in the oropharynx, and the lingual tonsil is located at the base of the tongue. Similar to the pharyngeal tonsil, the palatine and lingual tonsils are composed of lymphoid tissue and trap and destroy pathogens entering the body through the oral or nasal cavities. See Figure 7.6[13] for an image of the oral cavity and oropharynx with enlarged palatine tonsils.
The laryngopharynx is inferior to the oropharynx and posterior to the larynx. It continues the route for ingested material and air until its inferior end where the digestive and respiratory systems diverge. Anteriorly, the laryngopharynx opens into the larynx, and posteriorly, it enters the esophagus that leads to the stomach. The larynx connects the pharynx to the trachea and helps regulate the volume of air that enters and leaves the lungs. It also contains the vocal cords that vibrate as air passes over them to produce the sound of a person’s voice. The trachea extends from the larynx to the lungs. The epiglottis is a flexible piece of cartilage that covers the opening of the trachea during swallowing to prevent ingested material from entering the trachea.[14]
Muscles and Nerves of the Head and Neck
Facial Muscles
Several nerves innervate the facial muscles to create facial expressions. See Figure 7.7[15] for an illustration of nerves innervating facial muscles. These nerves and muscles are tested during a cranial nerve exam. See more information about performing a cranial nerve exam in the “Neurological Assessment” chapter.
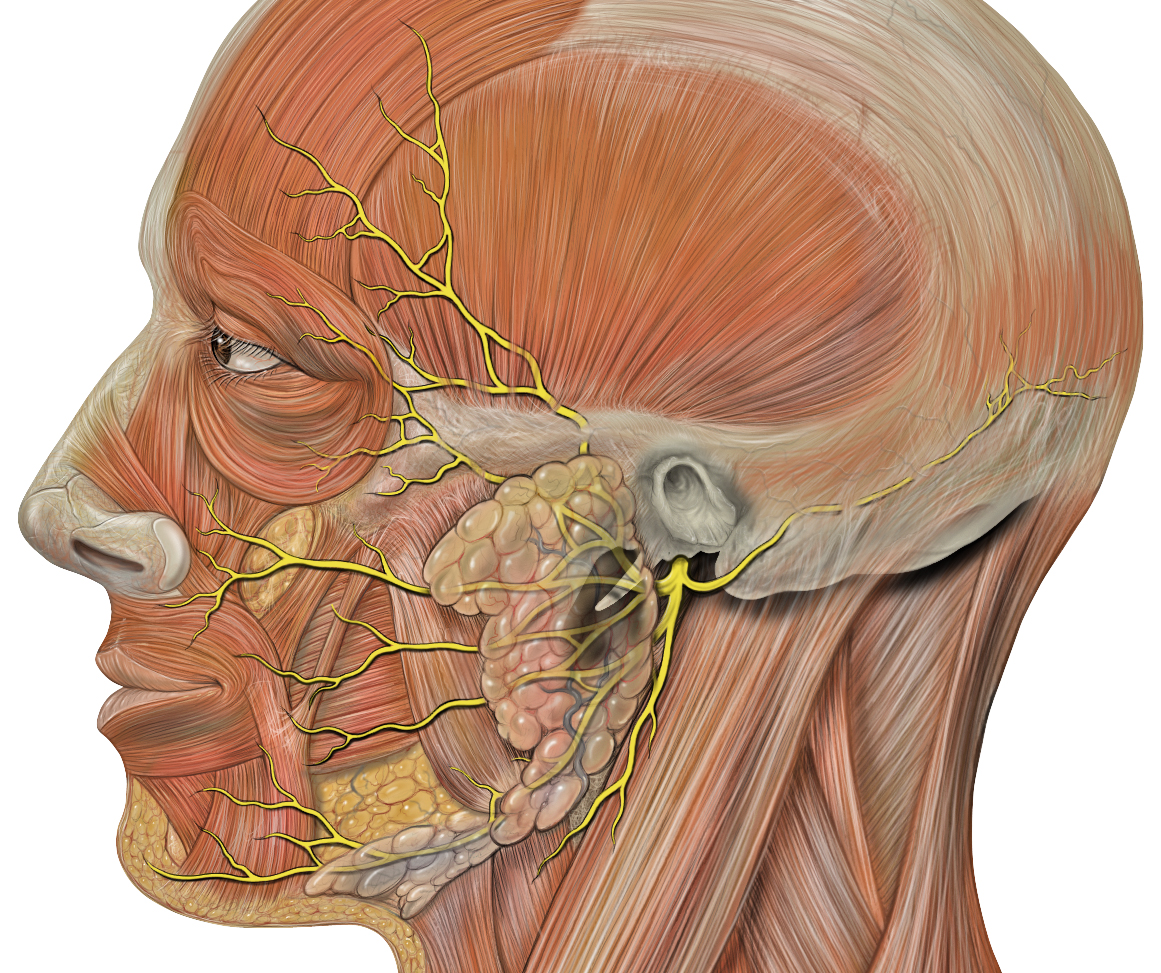
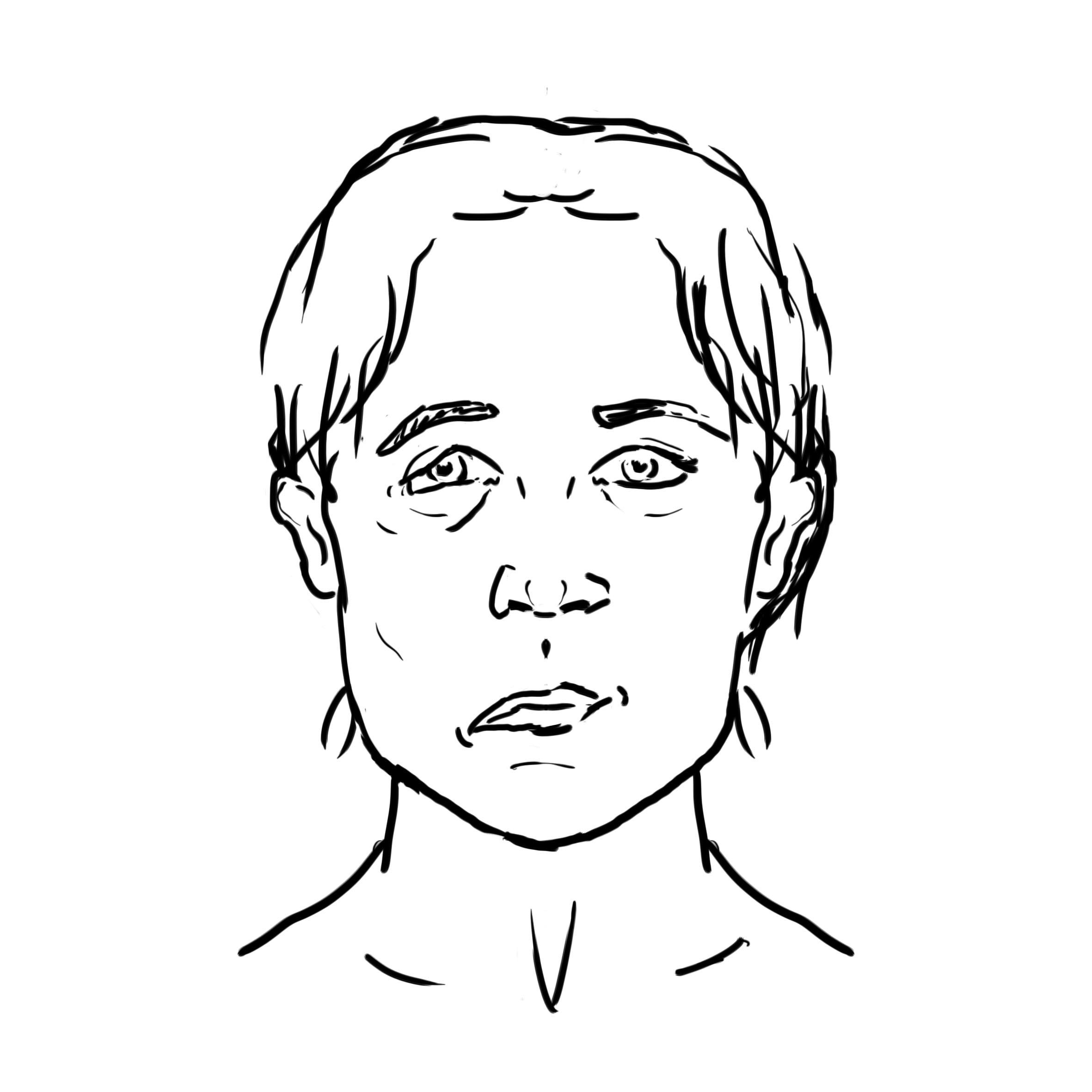
When a patient is experiencing a cerebrovascular accident (i.e., stroke), it is common for facial drooping to occur. Facial drooping is an asymmetrical facial expression that occurs due to damage of the nerve innervating a specific part of the face. See Figure 7.8[16] for an image of facial drooping occurring on the patient’s right side of their face.
Neck Muscles
The muscles of the anterior neck assist in swallowing and speech by controlling the positions of the larynx and the hyoid bone, a horseshoe-shaped bone that functions as a solid foundation on which the tongue can move. The head, attached to the top of the vertebral column, is balanced, moved, and rotated by the neck muscles. When these muscles act unilaterally, the head rotates. When they contract bilaterally, the head flexes or extends. The major muscle that laterally flexes and rotates the head is the sternocleidomastoid. The trapezius muscle elevates the shoulders (shrugging), pulls the shoulder blades together, and tilts the head backwards. See Figure 7.9[17] for an illustration of the sternocleidomastoid and trapezius muscles.[18] Both of these muscles are tested during a cranial nerve assessment. See more information about cranial nerve assessment in the “Neurological Assessment” chapter.

Jaw Muscles
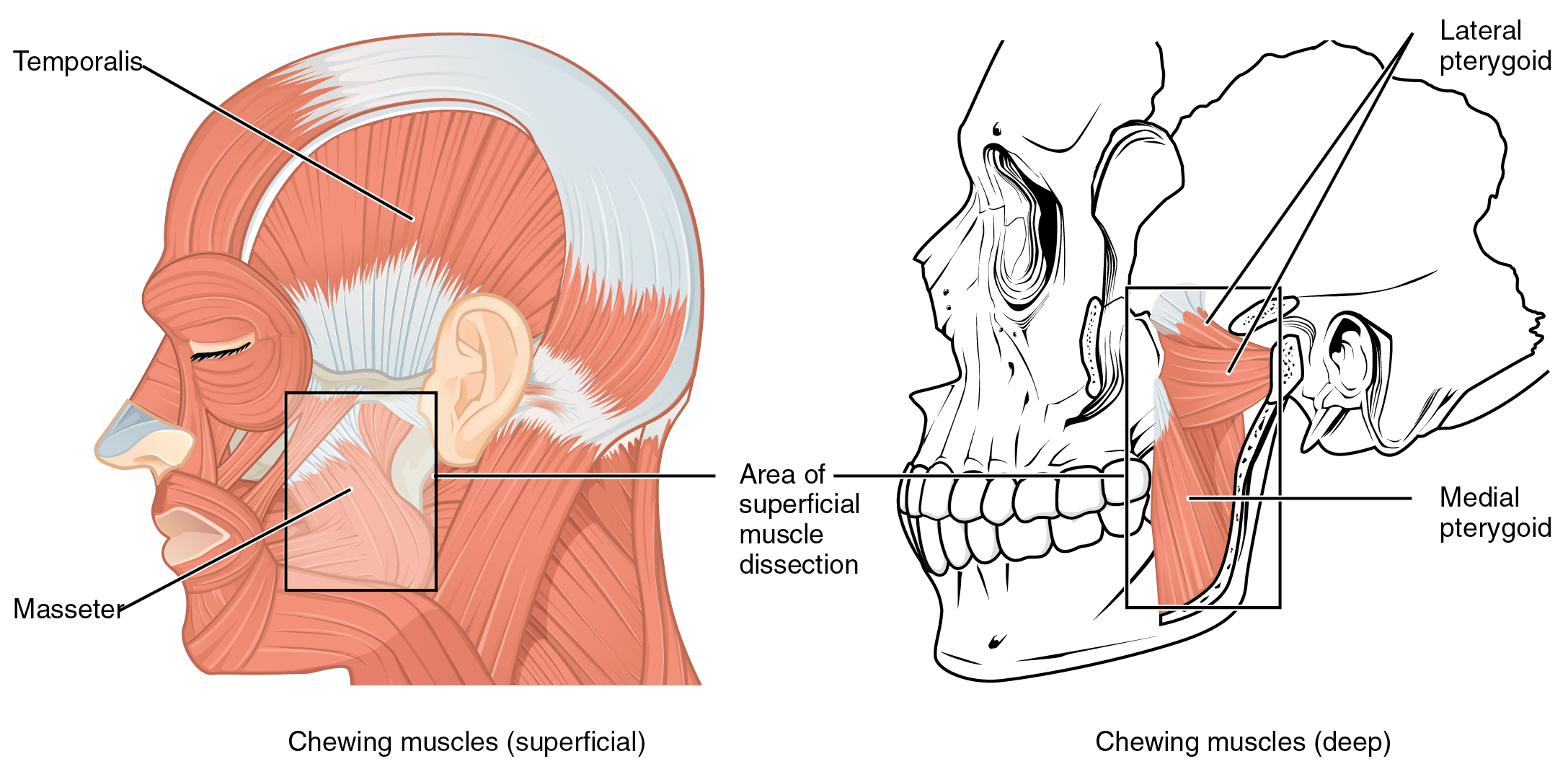
The masseter muscle is the main muscle used for chewing because it elevates the mandible (lower jaw) to close the mouth. It is assisted by the temporalis muscle that retracts the mandible. The temporalis muscle can be felt moving by placing fingers on the patient’s temple as they chew. See Figure 7.10[19] for an illustration of the masseter and temporalis muscles.[20]
Tongue Muscles
Muscles of the tongue are necessary for chewing, swallowing, and speech. Because it is so moveable, the tongue facilitates complex speech patterns and sounds.[21]
Airway and Unconsciousness
When a patient becomes unconscious and is lying supine, the tongue often moves backwards and blocks the airway. This is why it is important to open the airway when performing CPR by using a chin-thrust maneuver. See Figure 7.11[22] for an image of the tongue blocking the airway. In a similar manner, when a patient is administered general anesthesia during surgery, the tongue relaxes and can block the airway. For this reason, endotracheal intubation is performed during surgery with general anesthesia by placing a tube into the trachea to maintain an open airway to the lungs. After surgery, patients often report a sore or scratchy throat for a few days due to the endotracheal intubation.[23]

Swallowing
Swallowing is a complex process that uses 50 pairs of muscles and many nerves to receive food in the mouth, prepare it, and move it from the mouth to the stomach. Swallowing occurs in three stages. During the first stage, called the oral phase, the tongue collects the food or liquid and makes it ready for swallowing. The tongue and jaw move solid food around in the mouth so it can be chewed and made the right size and texture to swallow by mixing food with saliva. The second stage begins when the tongue pushes the food or liquid to the back of the mouth. This triggers a swallowing response that passes the food through the pharynx. During this phase, called the pharyngeal phase, the epiglottis closes off the larynx and breathing stops to prevent food or liquid from entering the airway and lungs. The third stage begins when food or liquid enters the esophagus, and it is carried to the stomach. The passage through the esophagus, called the esophageal phase, usually occurs in about three seconds.[24]
View the following video from Medline Plus on the swallowing process:
Dysphagia is the medical term for swallowing difficulties that occur when there is a problem with the nerves or structures involved in the swallowing process.[26] Nurses are often the first to notice signs of dysphagia in their patients that can occur due to a multitude of medical conditions such as a stroke, head injury, or dementia. For more information about the symptoms, screening, and treatment for dysphagia, go to the “Common Conditions of the Head and Neck” section.
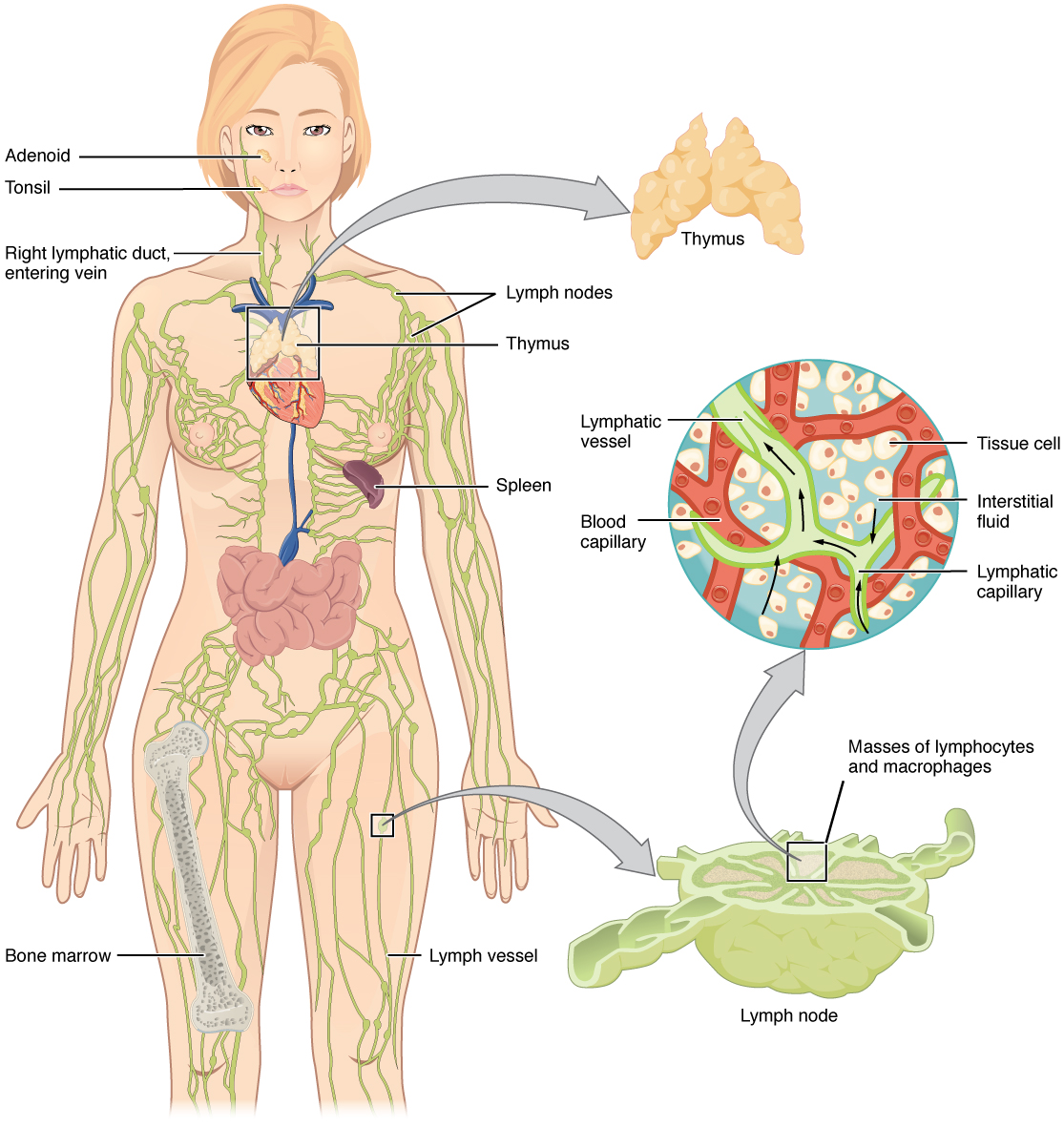
Lymphatic System
The lymphatic system is the system of vessels, cells, and organs that carries excess interstitial fluid to the bloodstream and filters pathogens from the blood through lymph nodes found near the neck, armpits, chest, abdomen, and groin. See Figure 7.12[27] and Figure 7.13[28] for an illustration of the lymph nodes found in the head and neck regions. When a person is fighting off an infection, the lymph nodes in that region become enlarged, indicating an active immune response to infection.[29]
![]“Cervical lymph nodes and level.png” by Mikael Häggström, M.D. is licensed under CC0 1.0 Illustration of lymph nodes in head and neck, with labels](https://opencontent.ccbcmd.edu/app/uploads/sites/32/2024/08/Cervical_lymph_nodes_and_levels-3.png)
- “704 Skull -01.jpg” by OpenStax College is licensed under CC BY 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/7-2-the-skull ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of “727_Cranial_Fossae.jpg” by OpenStax and is licensed under CC BY 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/7-2-the-skull ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “705 Lateral View of Skull-01.jpg” by OpenStax is licensed under CC BY 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/7-2-the-skull ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “Paranasal Sinuses ant.jpg” by OpenStax is licensed under CC BY-SA 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/7-2-the-skull ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- "2303 Anatomy of Nose-Pharynx-Mouth-Larynx.jpg” by OpenStax is licensed CC BY 3.0 ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of “2209 Location and Histology of Tonsils.jpg” by OpenStax and is licensed under CC BY 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/21-1-anatomy-of-the-lymphatic-and-immune-systems ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “Head facial nerve branches.jpg” by Patrick J. Lynch, medical illustrator is licensed under CC BY 2.5 ↵
- “Stroke-facial-droop.jpg” by Another-anon-artist-234 is licensed under CC0 1.0 ↵
- “1111 Posterior and Side Views of the Next.jpg” by OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/11-3-axial-muscles-of-the-head-neck-and-back. ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “1108 Muscle that Move the Lower Jaw.jpg” by OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/11-3-axial-muscles-of-the-head-neck-and-back ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “Airway closed in an unconscious patient because the head inflexed forward.jpg” by Dr. Lorimer is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- National Institute on Deafness and Other Communication Disorders. (2017, March 6). Dysphagia. https://www.nidcd.nih.gov/health/dysphagia ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M. Inc.; c1997-2021. Swallowing [Video]. [updated 2019, July 11]. https://medlineplus.gov/ency/anatomyvideos/000126.htm ↵
- National Institute on Deafness and Other Communication Disorders. (2017, March 6). Dysphagia. https://www.nidcd.nih.gov/health/dysphagia ↵
- “2201 Anatomy of the Lymphatic System.jpg” by OpenStax College is licensed under CC BY 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/21-1-anatomy-of-the-lymphatic-and-immune-systems ↵
- “Cervical lymph nodes and level.png” by Mikael Häggström, M.D. is licensed under CC0 1.0 ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
Prioritization of care for multiple patients while also performing daily nursing tasks can feel overwhelming in today’s fast-paced health care system. Because of the rapid and ever-changing conditions of patients and the structure of one’s workday, nurses must use organizational frameworks to prioritize actions and interventions. These frameworks can help ease anxiety, enhance personal organization and confidence, and ensure patient safety.
Acuity
Acuity and intensity are foundational concepts for prioritizing nursing care and interventions. Acuity refers to the level of patient care that is required based on the severity of a patient’s illness or condition. For example, acuity may include characteristics such as unstable vital signs, oxygenation therapy, high-risk IV medications, multiple drainage devices, or uncontrolled pain. A "high-acuity" patient requires several nursing interventions and frequent nursing assessments.
Intensity addresses the time needed to complete nursing care and interventions such as providing assistance with activities of daily living (ADLs), performing wound care, or administering several medication passes. For example, a "high-intensity" patient generally requires frequent or long periods of psychosocial, educational, or hygiene care from nursing staff members. High-intensity patients may also have increased needs for safety monitoring, familial support, or other needs.[1]
Many health care organizations structure their staffing assignments based on acuity and intensity ratings to help provide equity in staff assignments. Acuity helps to ensure that nursing care is strategically divided among nursing staff. An equitable assignment of patients benefits both the nurse and patient by helping to ensure that patient care needs do not overwhelm individual staff and safe care is provided.
Organizations use a variety of systems when determining patient acuity with rating scales based on nursing care delivery, patient stability, and care needs. See an example of a patient acuity tool published in the American Nurse in Table 2.3.[2] In this example, ratings range from 1 to 4, with a rating of 1 indicating a relatively stable patient requiring minimal individualized nursing care and intervention. A rating of 2 reflects a patient with a moderate risk who may require more frequent intervention or assessment. A rating of 3 is attributed to a complex patient who requires frequent intervention and assessment. This patient might also be a new admission or someone who is confused and requires more direct observation. A rating of 4 reflects a high-risk patient. For example, this individual may be experiencing frequent changes in vital signs, may require complex interventions such as the administration of blood transfusions, or may be experiencing significant uncontrolled pain. An individual with a rating of 4 requires more direct nursing care and intervention than a patient with a rating of 1 or 2.[3]
Table 2.3. Example of a Patient Acuity Tool[4]
| 1: Stable Patient | 2: Moderate-Risk Patient | 3: Complex Patient | 4: High-Risk Patient | |
|---|---|---|---|---|
| Assessment |
|
|
|
|
| Respiratory |
|
|
|
|
| Cardiac |
|
|
|
|
| Medications |
|
|
|
|
| Drainage Devices |
|
|
|
|
| Pain Management |
|
|
|
|
| Admit/Transfer/Discharge |
|
|
|
|
| ADLs and Isolation |
|
|
|
|
| Patient Score | Most = 1 | Two or > = 2 | Any = 3 | Any = 4 |
Read more about using a patient acuity tool on a medical-surgical unit.
Rating scales may vary among institutions, but the principles of the rating system remain the same. Organizations include various patient care elements when constructing their staffing plans for each unit. Read more information about staffing models and acuity in the following box.
Staffing Models and Acuity
Organizations that base staffing on acuity systems attempt to evenly staff patient assignments according to their acuity ratings. This means that when comparing patient assignments across nurses on a unit, similar acuity team scores should be seen with the goal of achieving equitable and safe division of workload across the nursing team. For example, one nurse should not have a total acuity score of 6 for their patient assignments while another nurse has a score of 15. If this situation occurred, the variation in scoring reflects a discrepancy in workload balance and would likely be perceived by nursing peers as unfair. Using acuity-rating staffing models is helpful to reflect the individualized nursing care required by different patients.
Alternatively, nurse staffing models may be determined by staffing ratio. Ratio-based staffing models are more straightforward in nature, where each nurse is assigned care for a set number of patients during their shift. Ratio-based staffing models may be useful for administrators creating budget requests based on the number of staff required for patient care, but can lead to an inequitable division of work across the nursing team when patient acuity is not considered. Increasingly complex patients require more time and interventions than others, so a blend of both ratio and acuity-based staffing is helpful when determining staffing assignments.[5]
As a practicing nurse, you will be oriented to the elements of acuity ratings within your health care organization, but it is also important to understand how you can use these acuity ratings for your own prioritization and task delineation. Let’s consider the Scenario B in the following box to better understand how acuity ratings can be useful for prioritizing nursing care.
Scenario B
You report to work at 6 a.m. for your nursing shift on a busy medical-surgical unit. Prior to receiving the handoff report from your night shift nursing colleagues, you review the unit staffing grid and see that you have been assigned to four patients to start your day. The patients have the following acuity ratings:
Patient A: 45-year-old patient with paraplegia admitted for an infected sacral wound, with an acuity rating of 4.
Patient B: 87-year-old patient with pneumonia with a low-grade fever of 99.7 F and receiving oxygen at 2 L/minute via nasal cannula, with an acuity rating of 2.
Patient C: 63-year-old patient who is postoperative Day 1 from a right total hip replacement and is receiving pain management via a PCA pump, with an acuity rating of 2.
Patient D: 83-year-old patient admitted with a UTI who is finishing an IV antibiotic cycle and will be discharged home today, with an acuity rating of 1.
Based on the acuity rating system, your patient assignment load receives an overall acuity score of 9. Consider how you might use their acuity ratings to help you prioritize your care. Based on what is known about the patients related to their acuity rating, whom might you identify as your care priority? Although this can feel like a challenging question to answer because of the many unknown elements in the situation using acuity numbers alone, Patient A with an acuity rating of 4 would be identified as the care priority requiring assessment early in your shift.
Although acuity can a useful tool for determining care priorities, it is important to recognize the limitations of this tool and consider how other patient needs impact prioritization.
Maslow’s Hierarchy of Needs
When thinking back to your first nursing or psychology course, you may recall a historical theory of human motivation based on various levels of human needs called Maslow's Hierarchy of Needs. Maslow’s Hierarchy of Needs reflects foundational human needs with progressive steps moving towards higher levels of achievement. This hierarchy of needs is traditionally represented as a pyramid with the base of the pyramid serving as essential needs that must be addressed before one can progress to another area of need.[6] See Figure 2.1[7] for an illustration of Maslow’s Hierarchy of Needs.
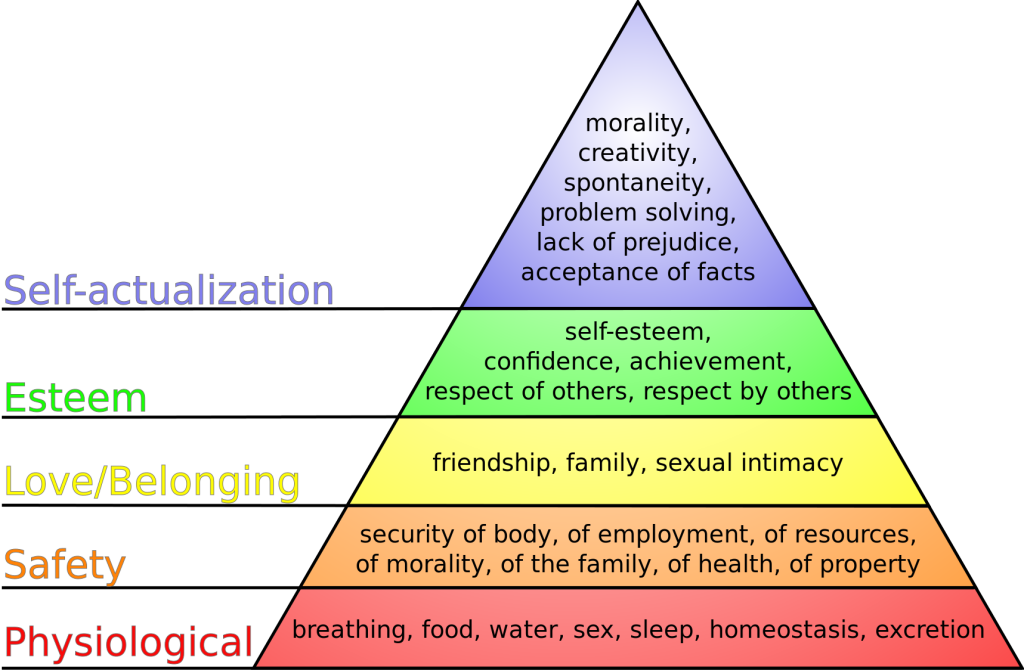
Maslow’s Hierarchy of Needs places physiological needs as the foundational base of the pyramid.[8] Physiological needs include oxygen, food, water, sex, sleep, homeostasis, and excretion. The second level of Maslow’s hierarchy reflects safety needs. Safety needs include elements that keep individuals safe from harm. Examples of safety needs in health care include fall precautions. The third level of Maslow’s hierarchy reflects emotional needs such as love and a sense of belonging. These needs are often reflected in an individual’s relationships with family members and friends. The top two levels of Maslow’s hierarchy include esteem and self-actualization. An example of addressing these needs in a health care setting is helping an individual build self-confidence in performing blood glucose checks that leads to improved self-management of their diabetes.
So how does Maslow’s theory impact prioritization? To better understand the application of Maslow’s theory to prioritization, consider Scenario C in the following box.
Scenario C
You are an emergency response nurse working at a local shelter in a community that has suffered a devastating hurricane. Many individuals have relocated to the shelter for safety in the aftermath of the hurricane. Much of the community is still without electricity and clean water, and many homes have been destroyed. You approach a young woman who has a laceration on her scalp that is bleeding through her gauze dressing. The woman is weeping as she describes the loss of her home stating, “I have lost everything! I just don’t know what I am going to do now. It has been a day since I have had water or anything to drink. I don’t know where my sister is, and I can’t reach any of my family to find out if they are okay!”
Despite this relatively brief interaction, this woman has shared with you a variety of needs. She has demonstrated a need for food, water, shelter, homeostasis, and family. As the nurse caring for her, it might be challenging to think about where to begin her care. These thoughts could be racing through your mind:
Should I begin to make phone calls to try and find her family? Maybe then she would be able to calm down.
Should I get her on the list for the homeless shelter so she wouldn’t have to worry about where she will sleep tonight?
She hasn’t eaten in a while; I should probably find her something to eat.
All these needs are important and should be addressed at some point, but Maslow’s hierarchy provides guidance on what needs must be addressed first. Use the foundational level of Maslow’s pyramid of physiological needs as the top priority for care. The woman is bleeding heavily from a head wound and has had limited fluid intake. As the nurse caring for this patient, it is important to immediately intervene to stop the bleeding and restore fluid volume. Stabilizing the patient by addressing her physiological needs is required before undertaking additional measures such as contacting her family. Imagine if instead you made phone calls to find the patient’s family and didn't address the bleeding or dehydration - you might return to a severely hypovolemic patient who has deteriorated and may be near death. In this example, prioritizing emotional needs above physiological needs can lead to significant harm to the patient.
Although this is a relatively straightforward example, the principles behind the application of Maslow’s hierarchy are essential. Addressing physiological needs before progressing toward additional need categories concentrates efforts on the most vital elements to enhance patient well-being. Maslow’s hierarchy provides the nurse with a helpful framework for identifying and prioritizing critical patient care needs.
ABCs
Airway, breathing, and circulation, otherwise known by the mnemonic “ABCs,” are another foundational element to assist the nurse in prioritization. Like Maslow’s hierarchy, using the ABCs to guide decision-making concentrates on the most critical needs for preserving human life. If a patient does not have a patent airway, is unable to breathe, or has inadequate circulation, very little of what else we do matters. The patient’s ABCs are reflected in Maslow’s foundational level of physiological needs and direct critical nursing actions and timely interventions. Let’s consider Scenario D in the following box regarding prioritization using the ABCs and the physiological base of Maslow’s hierarchy.
Scenario D
You are a nurse on a busy cardiac floor charting your morning assessments on a computer at the nurses’ station. Down the hall from where you are charting, two of your assigned patients are resting comfortably in Room 504 and Room 506. Suddenly, both call lights ring from the rooms, and you answer them via the intercom at the nurses’ station.
Room 504 has an 87-year-old male who has been admitted with heart failure, weakness, and confusion. He has a bed alarm for safety and has been ringing his call bell for assistance appropriately throughout the shift. He requires assistance to get out of bed to use the bathroom. He received his morning medications, which included a diuretic about 30 minutes previously, and now reports significant urge to void and needs assistance to the bathroom.
Room 506 has a 47-year-old woman who was hospitalized with new onset atrial fibrillation with rapid ventricular response. The patient underwent a cardioversion procedure yesterday that resulted in successful conversion of her heart back into normal sinus rhythm. She is reporting via the intercom that her "heart feels like it is doing that fluttering thing again” and she is having chest pain with breathlessness.
Based upon these two patient scenarios, it might be difficult to determine whom you should see first. Both patients are demonstrating needs in the foundational physiological level of Maslow’s hierarchy and require assistance. To prioritize between these patients' physiological needs, the nurse can apply the principles of the ABCs to determine intervention. The patient in Room 506 reports both breathing and circulation issues, warning indicators that action is needed immediately. Although the patient in Room 504 also has an urgent physiological elimination need, it does not overtake the critical one experienced by the patient in Room 506. The nurse should immediately assess the patient in Room 506 while also calling for assistance from a team member to assist the patient in Room 504.
CURE
Prioritizing what should be done and when it can be done can be a challenging task when several patients all have physiological needs. Recently, there has been professional acknowledgement of the cognitive challenge for novice nurses in differentiating physiological needs. To expand on the principles of prioritizing using the ABCs, the CURE hierarchy has been introduced to help novice nurses better understand how to manage competing patient needs. The CURE hierarchy uses the acronym “CURE” to guide prioritization based on identifying the differences among Critical needs, Urgent needs, Routine needs, and Extras.[9]
“Critical” patient needs require immediate action. Examples of critical needs align with the ABCs and Maslow’s physiological needs, such as symptoms of respiratory distress, chest pain, and airway compromise. No matter the complexity of their shift, nurses can be assured that addressing patients' critical needs is the correct prioritization of their time and energies.
After critical patient care needs have been addressed, nurses can then address “urgent” needs. Urgent needs are characterized as needs that cause patient discomfort or place the patient at a significant safety risk.[10]
The third part of the CURE hierarchy reflects “routine” patient needs. Routine patient needs can also be characterized as "typical daily nursing care" because the majority of a standard nursing shift is spent addressing routine patient needs. Examples of routine daily nursing care include actions such as administering medication and performing physical assessments.[11] Although a nurse’s typical shift in a hospital setting includes these routine patient needs, they do not supersede critical or urgent patient needs.
The final component of the CURE hierarchy is known as “extras.” Extras refer to activities performed in the care setting to facilitate patient comfort but are not essential.[12] Examples of extra activities include providing a massage for comfort or washing a patient’s hair. If a nurse has sufficient time to perform extra activities, they contribute to a patient’s feeling of satisfaction regarding their care, but these activities are not essential to achieve patient outcomes.
Let's apply the CURE mnemonic to patient care in the following box.
If we return to Scenario D regarding patients in Room 504 and 506, we can see the patient in Room 504 is having urgent needs. He is experiencing a physiological need to urgently use the restroom and may also have safety concerns if he does not receive assistance and attempts to get up on his own because of weakness. He is on a bed alarm, which reflects safety considerations related to his potential to get out of bed without assistance. Despite these urgent indicators, the patient in Room 506 is experiencing a critical need and takes priority. Recall that critical needs require immediate nursing action to prevent patient deterioration. The patient in Room 506 with a rapid, fluttering heartbeat and shortness of breath has a critical need because without prompt assessment and intervention, their condition could rapidly decline and become fatal.
Data Cues
In addition to using the identified frameworks and tools to assist with priority setting, nurses must also look at their patients’ data cues to help them identify care priorities. Data cues are pieces of significant clinical information that direct the nurse toward a potential clinical concern or a change in condition. For example, have the patient’s vital signs worsened over the last few hours? Is there a new laboratory result that is concerning? Data cues are used in conjunction with prioritization frameworks to help the nurse holistically understand the patient's current status and where nursing interventions should be directed. Common categories of data clues include acute versus chronic conditions, actual versus potential problems, unexpected versus expected conditions, information obtained from the review of a patient’s chart, and diagnostic information.
Acute Versus Chronic Conditions
A common data cue that nurses use to prioritize care is considering if a condition or symptom is acute or chronic. Acute conditions have a sudden and severe onset. These conditions occur due to a sudden illness or injury, and the body often has a significant response as it attempts to adapt. Chronic conditions have a slow onset and may gradually worsen over time. The difference between an acute versus a chronic condition relates to the body’s adaptation response. Individuals with chronic conditions often experience less symptom exacerbation because their body has had time to adjust to the illness or injury. Let’s consider an example of two patients admitted to the medical-surgical unit complaining of pain in Scenario E in the following box.
Scenario E
As part of your patient assignment on a medical-surgical unit, you are caring for two patients who both ring the call light and report pain at the start of the shift. Patient A was recently admitted with acute appendicitis, and Patient B was admitted for observation due to weakness. Not knowing any additional details about the patients' conditions or current symptoms, which patient would receive priority in your assessment? Based on using the data cue of acute versus chronic conditions, Patient A with a diagnosis of acute appendicitis would receive top priority for assessment over a patient with chronic pain due to osteoarthritis. Patients experiencing acute pain require immediate nursing assessment and intervention because it can indicate a change in condition. Acute pain also elicits physiological effects related to the stress response, such as elevated heart rate, blood pressure, and respiratory rate, and should be addressed quickly.
Actual Versus Potential Problems
Nursing diagnoses and the nursing care plan have significant roles in directing prioritization when interpreting assessment data cues. Actual problems refer to a clinical problem that is actively occurring with the patient. A risk problem indicates the patient may potentially experience a problem but they do not have current signs or symptoms of the problem actively occurring.
Consider an example of prioritizing actual and potential problems in Scenario F in the following box.
Scenario F
A 74-year-old woman with a previous history of chronic obstructive pulmonary disease (COPD) is admitted to the hospital for pneumonia. She has generalized weakness, a weak cough, and crackles in the bases of her lungs. She is receiving IV antibiotics, fluids, and oxygen therapy. The patient can sit at the side of the bed and ambulate with the assistance of staff, although she requires significant encouragement to ambulate.
Nursing diagnoses are established for this patient as part of the care planning process. One nursing diagnosis for this patient is Ineffective Airway Clearance. This nursing diagnosis is an actual problem because the patient is currently exhibiting signs of poor airway clearance with an ineffective cough and crackles in the lungs. Nursing interventions related to this diagnosis include coughing and deep breathing, administering nebulizer treatment, and evaluating the effectiveness of oxygen therapy. The patient also has the nursing diagnosis Risk for Skin Breakdown based on her weakness and lack of motivation to ambulate. Nursing interventions related to this diagnosis include repositioning every two hours and assisting with ambulation twice daily.
The established nursing diagnoses provide cues for prioritizing care. For example, if the nurse enters the patient’s room and discovers the patient is experiencing increased shortness of breath, nursing interventions to improve the patient’s respiratory status receive top priority before attempting to get the patient to ambulate.
Although there may be times when risk problems may supersede actual problems, looking to the “actual” nursing problems can provide clues to assist with prioritization.
Unexpected Versus Expected Conditions
In a similar manner to using acute versus chronic conditions as a cue for prioritization, it is also important to consider if a client's signs and symptoms are "expected" or "unexpected" based on their overall condition. Unexpected conditions are findings that are not likely to occur in the normal progression of an illness, disease, or injury. Expected conditions are findings that are likely to occur or are anticipated in the course of an illness, disease, or injury. Unexpected findings often require immediate action by the nurse.
Let’s apply this tool to the two patients previously discussed in Scenario E. As you recall, both Patient A (with acute appendicitis) and Patient B (with weakness and diagnosed with osteoarthritis) are reporting pain. Acute pain typically receives priority over chronic pain. But what if both patients are also reporting nausea and have an elevated temperature? Although these symptoms must be addressed in both patients, they are "expected" symptoms with acute appendicitis (and typically addressed in the treatment plan) but are "unexpected" for the patient with osteoarthritis. Critical thinking alerts you to the unexpected nature of these symptoms in Patient B, so they receive priority for assessment and nursing interventions.
Handoff Report/Chart Review
Additional data cues that are helpful in guiding prioritization come from information obtained during a handoff nursing report and review of the patient chart. These data cues can be used to establish a patient's baseline status and prioritize new clinical concerns based on abnormal assessment findings. Let’s consider Scenario G in the following box based on cues from a handoff report and how it might be used to help prioritize nursing care.
Scenario G
Imagine you are receiving the following handoff report from the night shift nurse for a patient admitted to the medical-surgical unit with pneumonia:
At the beginning of my shift, the patient was on room air with an oxygen saturation of 93%. She had slight crackles in both bases of her posterior lungs. At 0530, the patient rang the call light to go to the bathroom. As I escorted her to the bathroom, she appeared slightly short of breath. Upon returning the patient to bed, I rechecked her vital signs and found her oxygen saturation at 88% on room air and respiratory rate of 20. I listened to her lung sounds and noticed more persistent crackles and coarseness than at bedtime. I placed the patient on 2 L/minute of oxygen via nasal cannula. Within five minutes, her oxygen saturation increased to 92%, and she reported increased ease in respiration.
Based on the handoff report, the night shift nurse provided substantial clinical evidence that the patient may be experiencing a change in condition. Although these changes could be attributed to lack of lung expansion that occurred while the patient was sleeping, there is enough information to indicate to the oncoming nurse that follow-up assessment and interventions should be prioritized for this patient because of potentially worsening respiratory status. In this manner, identifying data cues from a handoff report can assist with prioritization.
Now imagine the night shift nurse had not reported this information during the handoff report. Is there another method for identifying potential changes in patient condition? Many nurses develop a habit of reviewing their patients’ charts at the start of every shift to identify trends and “baselines” in patient condition. For example, a chart review reveals a patient’s heart rate on admission was 105 beats per minute. If the patient continues to have a heart rate in the low 100s, the nurse is not likely to be concerned if today’s vital signs reveal a heart rate in the low 100s. Conversely, if a patient’s heart rate on admission was in the 60s and has remained in the 60s throughout their hospitalization, but it is now in the 100s, this finding is an important cue requiring prioritized assessment and intervention.
Diagnostic Information
Diagnostic results are also important when prioritizing care. In fact, the National Patient Safety Goals from The Joint Commission include prompt reporting of important test results. New abnormal laboratory results are typically flagged in a patient’s chart or are reported directly by phone to the nurse by the laboratory as they become available. Newly reported abnormal results, such as elevated blood levels or changes on a chest X-ray, may indicate a patient’s change in condition and require additional interventions. For example, consider Scenario H in which you are the nurse providing care for five medical-surgical patients.
Scenario H
You completed morning assessments on your assigned five patients. Patient A previously underwent a total right knee replacement and will be discharged home today. You are about to enter Patient A’s room to begin discharge teaching when you receive a phone call from the laboratory department, reporting a critical hemoglobin of 6.9 gm/dL on Patient B. Rather than enter Patient A’s room to perform discharge teaching, you immediately reprioritize your care. You call the primary provider to report Patient B’s critical hemoglobin level and determine if additional intervention, such as a blood transfusion, is required.
Prioritization Principles & Staffing Considerations[13]
With the complexity of different staffing variables in health care settings, it can be challenging to identify a method and solution that will offer a resolution to every challenge. The American Nurses Association has identified five critical principles that should be considered for nurse staffing. These principles are as follows:
- Health Care Consumer: Nurse staffing decisions are influenced by the specific number and needs of the health care consumer. The health care consumer includes not only the client, but also families, groups, and populations served. Staffing guidelines must always consider the patient safety indicators, clinical, and operational outcomes that are specific to a practice setting. What is appropriate for the consumer in one setting, may be quite different in another. Additionally, it is important to ensure that there is resource allocation for care coordination and health education in each setting.
- Interprofessional Teams: As organizations identify what constitutes appropriate staffing in various settings, they must also consider the appropriate credentials and qualifications of the nursing staff within a specific setting. This involves utilizing an interprofessional care team that allows each individual to practice to the full extent of their educational, training, scope of practice as defined by their state Nurse Practice Act, and licensure. Staffing plans must include an appropriate skill mix and acknowledge the impact of more experienced nurses to help serve in mentoring and precepting roles.
- Workplace culture: Staffing considerations must also account for the importance of balance between costs associated with best practice and the optimization of care outcomes. Health care leaders and organizations must strive to ensure a balance between quality, safety, and health care cost. Organizations are responsible for creating work environments, which develop policies allowing for nurses to practice to the full extent of their licensure in accordance with their documented competence. Leaders must foster a culture of trust, collaboration, and respect among all members of the health care team, which will create environments that engage and retain health care staff.
- Practice environment: Staffing structures must be founded in a culture of safety where appropriate staffing is integral to achieve patient safety and quality goals. An optimal practice environment encourages nurses to report unsafe conditions or poor staffing that may impact safe care. Organizations should ensure that nurses have autonomy in reporting and concerns and may do so without threat of retaliation. The ANA has also taken the position to state that mandatory overtime is an unacceptable solution to achieve appropriate staffing. Organizations must ensure that they have clear policies delineating length of shifts, meal breaks, and rest period to help ensure safety in patient care.
- Evaluation: Staffing plans should be consistently evaluated and changed based upon evidence and client outcomes. Environmental factors and issues such as work-related illness, injury, and turnover are important elements of determining the success of need for modification within a staffing plan.[14]
Prioritization of patient care should be grounded in critical thinking rather than just a checklist of items to be done. Critical thinking is a broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow."[15] Certainly, there are many actions that nurses must complete during their shift, but nursing requires adaptation and flexibility to meet emerging patient needs. It can be challenging for a novice nurse to change their mindset regarding their established “plan” for the day, but the sooner a nurse recognizes prioritization is dictated by their patients’ needs, the less frustration the nurse might experience. Prioritization strategies include collection of information and utilization of clinical reasoning to determine the best course of action. Clinical reasoning is defined as, “A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions.”[16] Clinical reasoning is fostered within nurses when they are challenged to integrate data in various contexts. The clinical reasoning cycle begins when nurses first consider a client situation and progress to collecting cues and information. As nurses process the information, they begin to identify problems and establish realistic goals. They then take appropriate actions and evaluate outcomes. Finally, they reflect upon the process and the learning that has occurred. The reflection piece is critical for solidifying or changing future actions and developing knowledge.
When nurses use critical thinking and clinical reasoning skills, they set forth on a purposeful course of intervention to best meet patient-care needs. Rather than focusing on one’s own priorities, nurses utilizing critical thinking and reasoning skills recognize their actions must be responsive to their patients. For example, a nurse using critical thinking skills understands that scheduled morning medications for their patients may be late if one of the patients on their care team suddenly develops chest pain. Many actions may be added or removed from planned activities throughout the shift based on what is occurring holistically on the patient-care team.
Additionally, in today’s complex health care environment, it is important for the novice nurse to recognize the realities of the current health care environment. Patients have become increasingly complex in their health care needs, and organizations are often challenged to meet these care needs with limited staffing resources. It can become easy to slip into the mindset of disenchantment with the nursing profession when first assuming the reality of patient-care assignments as a novice nurse. The workload of a nurse in practice often looks and feels quite different than that experienced as a nursing student. As a nursing student, there may have been time for lengthy conversations with patients and their family members, ample time to chart, and opportunities to offer personal cares, such as a massage or hair wash. Unfortunately, in the time-constrained realities of today's health care environment, novice nurses should recognize that even though these “extra” tasks are not always possible, they can still provide quality, safe patient care using the “CURE” prioritization framework. Rather than feeling frustrated about “extras” that cannot be accomplished in time-constrained environments, it is vital to use prioritization strategies to ensure appropriate actions are taken to complete what must be done. With increased clinical experience, a novice nurse typically becomes more comfortable with prioritizing and reprioritizing care.
Time management is not an unfamiliar concept to nursing students because many students are balancing time demands related to work, family, and school obligations. To determine where time should be allocated, prioritization processes emerge. Although the prioritization frameworks of nursing may be different than those used as a student, the concept of prioritization remains the same. Despite the context, prioritization is essentially using a structure to organize tasks to ensure the most critical tasks are completed first and then identify what to move onto next. To truly maximize time management, in addition to prioritization, individuals should be organized, strive for accuracy, minimize waste, mobilize resources, and delegate when appropriate.
Time management is one of the greatest challenges that nurses face in their busy workday. As novice nurses develop their practice, it is important to identify organizational strategies to ensure priority tasks are completed and time is optimized. Each nurse develops a personal process for organizing information and structuring the timing of their assessments, documentation, medication administration, interventions, and patient education. However, one must always remember that this process and structure must be flexible because in a moment’s time, a patient’s condition can change, requiring a reprioritization of care. An organizational tool is important to guide a nurse’s daily task progression. Organizational tools may be developed individually by the nurse or may be recommended by the organization. Tools can be rudimentary in nature, such as a simple time column format outlining care activities planned throughout the shift, or more complex and integrated within an organization’s electronic medical record. No matter the format, an organizational tool is helpful to provide structure and guide progression toward task achievement.
In addition to using an organizational tool, novice nurses should utilize other time management strategies to optimize their time. For example, assessments can start during bedside handoff report, such as what fluids and medications are running and what will need to be replaced soon. Take a moment after handoff reports to prioritize which patients you will see first during your shift. Other strategies such as grouping tasks, gathering appropriate equipment prior to initiating nursing procedures, and gathering assessment information while performing tasks are helpful in minimizing redundancy and increasing efficiency. For example, observe an experienced nurse providing care and note the efficient processes they use. They may conduct an assessment, bring in morning medications, flush an IV line, collect a morning blood glucose level, and provide patient education about medications all during one patient encounter. Efficiency becomes especially important if the patient has transmission-based precautions and the time spent donning and doffing PPE are considered. The realities of the time-constrained health care environments often necessitate clustering tasks to ensure that all patient-care tasks are completed. Furthermore, nurses who do not manage their time effectively may inadvertently place their patients at risk as a result of delayed care.[17] Effective time management benefits both the patient and the nursing staff.
Time estimation is an additional helpful strategy to facilitate time management. Time estimation involves the review of planned tasks for the day and allocating time estimated to complete the task. Time estimation is especially helpful for novice nurses as they begin to structure and prioritize their shift based on the list of tasks that are required.[18] For example, estimating the time it will take to perform an assessment and administer morning medications to one patient allows the nurse to better plan when to complete the dressing change on another patient. Without using time estimation, the nurse may attempt to group all care tasks with the morning assessments and not leave themselves enough time to administer morning medications within the desired administration time window. Additionally, working in a time-constrained environment without using time estimation strategies increases the likelihood of performing tasks “in a rush” and subsequently increasing the potential for error.
Who’s On My Team?
One of the most critical strategies to enhance time management is to mobilize the resources of the nursing team. The nursing care team includes advanced practice registered nurses (APRN), registered nurses (RN), licensed practical/vocational nurses (LPN/VN), and assistive personnel (AP). AP (formerly referred to as unlicensed assistive personnel [UAP]) include, but are not limited to, certified nursing assistants or aides (CNA), patient-care technicians (PCT), certified medical assistants (CMA), certified medication aides, and home health aides.[19] Each care environment may have a blend of staff, and it is important to understand the legalities associated with the scope and role of each member and what can be safely and appropriately delegated to other members of the team. For example, assistive personnel may be able to assist with ambulating a patient in the hallway, but they would not be able to help administer morning medications. Dividing tasks appropriately among nursing team members can help ensure that the required tasks are completed and individual energies are best allocated to meet patient needs. The nursing care team and requirements around the process of delegation are explored in detail in the "Delegation and Supervision" chapter.
Sam is a novice nurse who is reporting to work for his 0600 shift on the medical telemetry/progressive care floor. He is waiting to receive handoff report from the night shift nurse for his assigned patients. The information that he has received thus far regarding his patient assignment includes the following:
- Room 501: 64-year-old patient admitted last night with heart failure exacerbation. Patient received furosemide 80mg IV push at 2000 with 1600 mL urine output. He is receiving oxygen via nasal cannula at 2L/minute. According to the night shift aide, he has been resting comfortably overnight.
- Room 507: 74-year-old patient admitted yesterday for possible cardioversion due to new onset of atrial fibrillation with rapid ventricular response and is scheduled for transesophageal echocardiogram and possible cardioversion at 1000.
- Room 512: 82-year-old patient who is scheduled for coronary artery bypass graft (CABG) surgery today at 0700 and is receiving an insulin infusion.
- Room 536: 72-year-old patient who had a negative heart catheterization yesterday but experienced a groin bleed; plans for discharge this morning.
Based on the limited information Sam has thus far, he begins to prioritize his activities for the morning. With what is known thus far regarding his patient assignment, whom might Sam plan to see first and why? What principles of prioritization might be applied?
Although Sam would benefit from hearing a full report on his patients and reviewing the patient charts, he can already begin to engage in strategies for prioritization. Based on the information that has been shared thus far, Sam determines that none of the patients assigned to him are experiencing critical or urgent needs. All the patients' basic physiological needs are being met, but many have actual clinical concerns. Based on the time constraint with scheduled surgery and the insulin infusion for the patient in Room 512, this patient should take priority in Sam's assessments. It is important for Sam to ensure that this patient's pre-op checklist is complete, and he is stable with the infusion prior to transferring him for surgery. Although Sam may later receive information that alters this priority setting, based on the information he has thus far, he has utilized prioritization principles to make an informed decision.
You are an RN and are reporting to work on a 16-bed medical/renal unit in a county hospital for the 0700 - 1500 shift today. The client population is primarily socioeconomically disadvantaged. Staff for the shift includes four RNs, one LPN/VN, and two AP.
You are a new RN graduate on the unit, and your orientation was completed two weeks ago. The LPN/VN has been working on the unit for ten years. Both AP have been on the unit for six months and are certified nursing assistants after completing basic nurse aide training. You, as one of four RNs on the unit, have been assigned four clients. You share the LPN with the other RNs, and there is one AP for every two RNs.
The charge nurse has assigned you the following four clients. Scheduled morning medications are due at 0800 and all four require some assistance with their ADLs.
- Client A: An obese 52-year-old male with hypertension and diabetes requiring insulin therapy. He has been depressed since recently being diagnosed with end-stage renal disease requiring hemodialysis. He needs his morning medications and assistance getting dressed for transport to hemodialysis in 30 minutes.
- Client B: A 83-year-old female client with acute pyelonephritis admitted two days ago. She has a PICC line in place and is receiving IV vancomycin every 12 hours. The next dose is due at 0830 after a trough level is drawn.
- Client C: A 78-year-old male recently diagnosed with bladder cancer. He has bright red urine today but reports it is painless. He has surgery scheduled at 0900 and the pre-op checklist has not yet been completed.
- Client D: A malnourished 80-year-old male client admitted with dehydration and imbalanced electrolyte levels. He is being discharged home today and requires patient education.
Reflective Questions
- At the start of the shift, you determine which tasks, cares, activities, and/or procedures you will delegate to the LPN and AP. What factors must you consider prior to delegation?
- What tasks will you delegate to the LPN/VN?
- What tasks will you delegate to the AP?
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activities are provided as immediate feedback.)
- The nurse is conducting an assessment on a 70-year-old male client who was admitted with atrial fibrillation. The client has a history of hypertension and Stage 2 chronic kidney disease. The nurse begins the head-to-toe assessment and notes the patient is having difficulty breathing and is complaining about chest discomfort. The client states, “It feels as if my heart is going to pound out of my chest and I feel dizzy.” The nurse begins the head-to-toe assessment and documents the findings. Client assessment findings are presented in the table below. Select the assessment findings requiring immediate follow-up by the nurse.
Vital Signs
| Temperature | 98.9 °F (37.2°C) |
|---|---|
| Heart Rate | 182 beats/min |
| Respirations | 36 breaths/min |
| Blood Pressure | 152/90 mm Hg |
| Oxygen Saturation | 88% on room air |
| Capillary Refill Time | >3 |
| Pain | 9/10 chest discomfort |
| Physical Assessment Findings | |
|---|---|
| Glasgow Coma Scale Score | 14 |
| Level of Consciousness | Alert |
| Heart Sounds | Irregularly regular |
| Lung Sounds | Clear bilaterally anterior/posterior |
| Pulses-Radial | Rapid/bounding |
| Pulses-Pedal | Weak |
| Bowel Sounds | Present and active x 4 |
| Edema | Trace bilateral lower extremities |
| Skin | Cool, clammy |
2. The following nursing actions may or may not be required at this time based on the assessment findings. Indicate whether the actions are "Indicated" (i.e., appropriate or necessary), "Contraindicated" (i.e., could be harmful), or "Nonessential" (i.e., makes no difference or are not necessary).
| Nursing Action | Indicated | Contraindicated | Nonessential |
|---|---|---|---|
| Apply oxygen at 2 liters per nasal cannula. | |||
| Call imaging for a STAT lung CT. | |||
| Perform the National Institutes of Health (NIH) Stroke Scale Neurologic Exam. | |||
| Obtain a comprehensive metabolic panel (CMP). | |||
| Obtain a STAT EKG. | |||
| Raise the head-of-bed to less than 10 degrees. | |||
| Establish patent IV access. | |||
| Administer potassium 20 mEq IV push STAT. |
3. The CURE hierarchy has been introduced to help novice nurses better understand how to manage competing patient needs. The CURE hierarchy uses the acronym “CURE” to help guide prioritization based on identifying the differences among Critical needs, Urgent needs, Routine needs, and Extras.
You are the nurse caring for the patients in the following table. For each patient, indicate if this is a "critical," "urgent," "routine," or "extra" need.
<td">
| Critical | Urgent | Routine | Extra | |
|---|---|---|---|---|
| Patient exhibits new left-sided facial droop | ||||
| Patient reports 9/10 acute pain and requests PRN pain medication | ||||
| Patient with BP 120/80 and regular heart rate of 68 has scheduled dose of oral amlodipine | ||||
| Patient with insomnia requests a back rub before bedtime | ||||
| Patient has a scheduled dressing change for a pressure ulcer on their coccyx |
||||
| Patient is exhibiting new shortness of breath and altered mental status | ||||
| Patient with fall risk precautions ringing call light for assistance to the restroom for a bowel movement |

Test your knowledge using this NCLEX Next Generation-style Case Study. You may reset and resubmit your answers to this question an unlimited number of times.[20]
ABCs: Airway, breathing, and circulation.
Actual problems: Nursing problems currently occurring with the patient.
Acuity: The level of patient care that is required based on the severity of a patient’s illness or condition.
Acuity-rating staffing models: A staffing model used to make patient assignments that reflects the individualized nursing care required for different types of patients.
Acute conditions: Conditions having a sudden onset.
Chronic conditions: Conditions that have a slow onset and may gradually worsen over time.
Clinical reasoning: “A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions.”[21]
Critical thinking: A broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.”[22]
CURE hierarchy: A strategy for prioritization based on identifying “critical” needs, “urgent” needs, “routine” needs, and “extras.”
Data cues: Pieces of significant clinical information that direct the nurse toward a potential clinical concern or a change in condition.
Expected conditions: Conditions that are likely to occur or anticipated in the course of an illness, disease, or injury.
Maslow’s Hierarchy of Needs: Prioritization strategies often reflect the foundational elements of physiological needs and safety and progress toward higher levels.
Ratio-based staffing models: A staffing model used to make patient assignments in terms of one nurse caring for a set number of patients.
Risk problem: A nursing problem that reflects that a patient may experience a problem but does not currently have signs reflecting the problem is actively occurring.
Time estimation: A prioritization strategy including the review of planned tasks and allocation of time believed to be required to complete each task.
Time scarcity: A feeling of racing against a clock that is continually working against you.
Unexpected conditions: Conditions that are not likely to occur in the normal progression of an illness, disease, or injury.
Learning Objectives
- Explain principles of delegation
- Evaluate the criteria used for delegation
- Apply effective communication techniques when delegating care
- Determine specific barriers to delegation
- Evaluate team members' performance based on delegation and supervision principles
- Incorporate principles of supervision and evaluation in the delegation process
- Identify scope of practice of the RN, LPN/VN, and unlicensed assistive personnel roles
- Identify tasks that can and cannot be delegated to members of the nursing team
As health care technology continues to advance, clients require increasingly complex nursing care, and as staffing becomes more challenging, health care agencies respond with an evolving variety of nursing and assistive personnel roles and responsibilities to meet these demands. As an RN, you are on the front lines caring for ill or injured clients and their families, advocating for clients’ rights, creating nursing care plans, educating clients on how to self-manage their health, and providing leadership throughout the complex health care system. Delivering safe, effective, quality client care requires the RN to coordinate care by the nursing team as tasks are assigned, delegated, and supervised. Nursing team members include advanced practice registered nurses (APRN), registered nurses (RN), licensed practical/vocational nurses (LPN/VN), and assistive personnel (AP).[23]
Assistive personnel (AP) (formerly referred to as ‘‘unlicensed” assistive personnel [UAP]) are any assistive personnel trained to function in a supportive role, regardless of title, to whom a nursing responsibility may be delegated. This includes, but is not limited to, certified nursing assistants or aides (CNAs), patient-care technicians (PCTs), certified medical assistants (CMAs), certified medication aides, and home health aides.[24] Making assignments, delegating tasks, and supervising delegatees are essential components of the RN role and can also provide the RN more time to focus on the complex needs of clients. For example, an RN may delegate to AP the attainment of vital signs for clients who are stable, thus providing the nurse more time to closely monitor the effectiveness of interventions in maintaining complex clients' hemodynamics, thermoregulation, and oxygenation. Collaboration among the nursing care team members allows for the delivery of optimal care as various skill sets are implemented to care for the patient.
Properly assigning and delegating tasks to nursing team members can promote efficient client care. However, inappropriate assignments or delegation can compromise client safety and produce unsatisfactory client outcomes that may result in legal issues. How does the RN know what tasks can be assigned or delegated to nursing team members and assistive personnel? What steps should the RN follow when determining if care can be delegated? After assignments and delegations are established, what is the role and responsibility of the RN in supervising client care? This chapter will explore and define the fundamental concepts involved in assigning, delegating, and supervising client care according to the most recent joint national delegation guidelines published by the National Council of State Boards of Nursing (NCSBN) and the American Nurses Association (ANA).[25]
Effective communication is a vital component of proper assignment, delegation, and supervision. It is also one of the Standards of Professional Performance established by the American Nurses Association (ANA).[26] Research has identified that new graduate nurses are more susceptible to stress and isolation within their job roles due to poor communication and teamwork within the interdisciplinary team.[27] Strong communication skills foster a supportive work environment and colleagial relationships that benefit both patients and nursing staff.
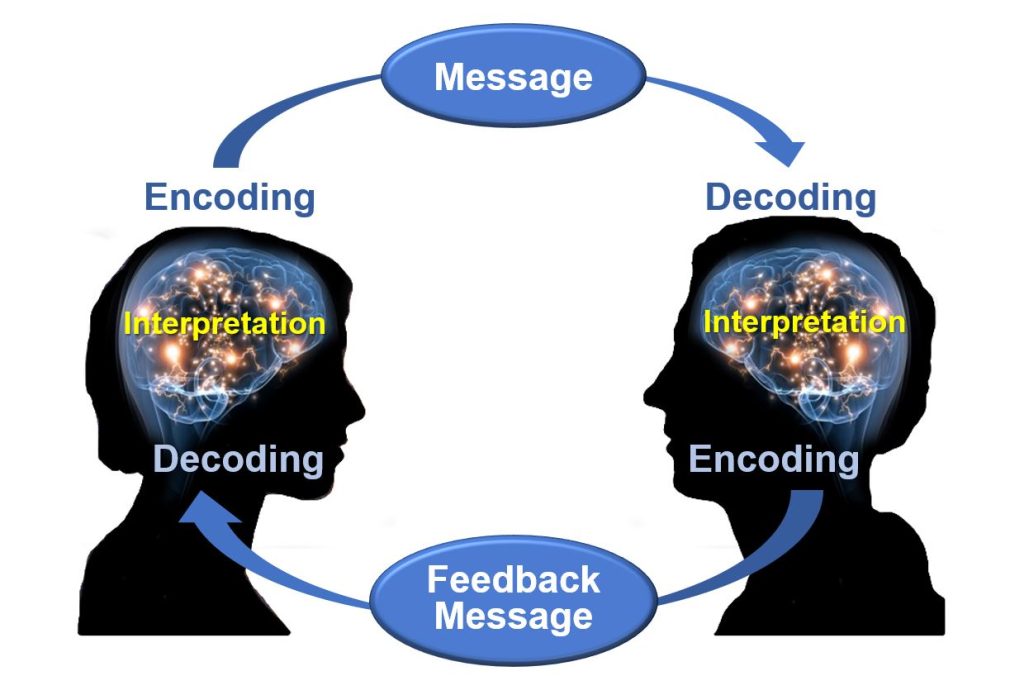
Consider the fundamentals of good communication practices. Effective communication requires each interaction to include a sender of the message, a clear and concise message, and a receiver who can decode and interpret that message. The receiver also provides a feedback message back to the sender in response to the received message. See Figure 3.1[28] for an image of effective communication between a sender and receiver. This feedback message is referred to as closed-loop communication in health care settings. Closed-loop communication enables the person giving the instructions to hear what they said reflected back and to confirm that their message was received correctly. It also allows the person receiving the instructions to verify and confirm the actions to be taken. If closed-loop communication is not used, the receiver may nod or say “OK,” and the sender may assume the message has been effectively transmitted, but this may not be the case and can lead to errors and client harm.
An example of closed-loop communication can be found in the following exchange:
- RN: “Jane, can you get a set of vitals on Mr. Smith and let me know if the results are outside of normal range?”
- Jane, CNA: “OK, I’ll get a set of vitals on Mr. Smith and let you know if they are out of range.”
Closed-loop communication is vital for communication among health care team members to avoid misunderstandings that can cause unsafe client care. According to the HIPAA Journal, poor communication leads to a “reduction in the quality of care, poor client outcomes, wastage of resources, and high health care costs.”[29] Parameters for reporting results and the results that should be expected are often left unsaid rather than spelled out in sufficient detail. It is imperative for the RN to provide clear, complete, concise instructions when delegating. A lack of clarity can lead to misunderstanding, unfinished tasks, incomplete care, and/or medical errors.[30]
Effective communication is at the core of proper assignment, delegation, and supervision. With effective communication at the beginning of every shift, each nursing team member should have a clear plan for their shift, what to do and why, and what and when to report to the RN or team leader. Communication should continue throughout the shift as tasks are accomplished and patients’ needs change. Effective communication improves client outcomes and satisfaction scores, as well as improving team morale by enhancing the collaborative relationships of the health care team.
The RN is accountable for clear, concise, correct, and complete communication when making assignments and delegating, both initially and throughout the shift. These communication characteristics can be remembered by using the mnemonic the "4 Cs":
- Clear: Information is understood by the listener. Asking the listener to restate the instructions and the plan can be helpful to determine whether the communication is clear.
- Concise: Sufficient information should be provided to accurately perform the task, but excessive or irrelevant information should be avoided because it can confuse the listener and waste precious time.
- Correct: Correct communication is not vague or confusing. Accurate information is also aligned with agency policy and the team member’s scope of practice as defined by their state’s Nurse Practice Act and other state regulations.
- Complete: Complete instructions leave no room for doubt. Always ask if further information or clarification is needed, especially regarding tasks that are infrequently performed or include unique instructions.[31]
The use of closed-loop communication is the best method to achieve clear, concise, correct, and complete information exchanged among team members. Closed-loop communication allows team members the opportunity to verify and validate the exchange of information. By repeating back information, members confirm the exchange has occurred, understanding is clear, and expectations are heard.
Closed-loop communication should also be used when the RN is receiving a verbal order from a provider. For example, when the resuscitation team leader gives a verbal order of “Epinephrine 1 mg/mL IV push now,” the RN confirms correct understanding of the order by repeating back, “I will prepare Epinephrine 1 mg/mL to be given IV push now.” After the provider confirms the verbal order and the task is completed, the nurse confirms completion of the task by stating, “Epinephrine 1 mg/mL IV push was administered.”
In addition to using closed-loop communication, a common format used by health care team members to exchange client information is ISBARR, a mnemonic for the components of Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat Back. ISBARR and other communication strategies are discussed in more detail in the "Interprofessional Communication" section of the "Collaboration Within the Interprofessional Team" chapter.
Nursing team members working in inpatient or long-term care settings receive patient assignments at the start of their shift. Assignment refers to routine care, activities, and procedures that are within the legal scope of practice of registered nurses (RN), licensed practical/vocational nurses (LPN/VN), or assistive personnel (AP).[32] Scope of practice for RNs and LPNs is described in each state's Nurse Practice Act. Care tasks for AP vary by state; regulations are typically listed on sites for the state's Board of Nursing, Department of Health, Department of Aging, Department of Health Professions, Department of Commerce, or Office of Long-Term Care.[33]
See Table 3.3a for common tasks performed by members of the nursing team based on their scope of practice. These tasks are within the traditional role and training the team member has acquired through a basic educational program. They are also within the expectations of the health care agency during a shift of work. Agency policy can be more restrictive than federal or state regulations, but it cannot be less restrictive.
Patient assignments are typically made by the charge nurse (or nurse supervisor) from the previous shift. A charge nurse is an RN who provides leadership on a patient-care unit within a health care facility during their shift. Charge nurses perform many of the tasks that general nurses do, but also have some supervisory duties such as making assignments, delegating tasks, preparing schedules, monitoring admissions and discharges, and serving as a staff member resource.[34]
Table 3.3a. Nursing Team Members’ Scope of Practice and Common Tasks[35]
| Nursing Team Member | Scope of Practice | Common Tasks
|
|---|---|---|
| RN |
|
|
| LPN/VN |
|
Tasks That Potentially Can Be Delegated According to the Five Rights of Delegation:
|
| AP |
|
|
An example of a patient assignment is when an RN assigns an LPN/VN to care for a client with stable heart failure. The LPN/VN collects assessment data, monitors intake/output throughout the shift, and administers routine oral medication. The LPN/VN documents this information and reports information back to the RN. This is considered the LPN/VN’s “assignment” because the skills are taught within an LPN educational program and are consistent with the state’s Nurse Practice Act for LPN/VN scope of practice. They are also included in the unit’s job description for an LPN/VN. The RN may also assign some care for this client to AP. These tasks may include assistance with personal hygiene, toileting, and ambulation. The AP documents these tasks as they are completed and reports information back to the RN or LPN/VN. These tasks are considered the AP’s assignment because they are taught within a nursing aide's educational program, are consistent with the AP's scope of practice for that state, and are included in the job description for the nursing aide's role in this unit. The RN continues to be accountable for the care provided to this client despite the assignments made to other nursing team members.
Special consideration is required for AP with additional training. With increased staffing needs, skills such as administering medications, inserting Foley catheters, or performing injections are included in specialized training programs for AP. Due to the impact these skills can have on the outcome and safety of the client, the National Council of State Board of Nursing (NCSBN) recommends these activities be considered delegated tasks by the RN or nurse leader. By delegating these advanced skills when appropriate, the nurse validates competency, provides supervision, and maintains accountability for client outcomes. Read more about delegation in the “Delegation” section of this chapter.
When making assignments to other nursing team members, it is essential for the RN to keep in mind specific tasks that cannot be delegated to other nursing team members based on federal and/or state regulations. These tasks include, but are not limited to, those tasks described in Table 3.3b.
Table 3.3b. Examples of Tasks Outside the Scope of Practice of Nursing Assistive Personnel
| Nursing Team Member | Tasks That Cannot Be Delegated
|
|---|---|
| LPN/VN |
|
| Assistive Personnel (AP) |
|
As always, refer to each state’s Nurse Practice Act and other state regulations for specific details about nursing team members’ scope of practice when providing care in that state.
Find and review Nurse Practice Acts by state at https://www.ncsbn.org/policy/npa.page.
Read more about the Wisconsin's Nurse Practice Act and the standards and scope of practice for RNs and LPNs at Wisconsin's Legislative Code Chapter N6.
Read more about scope of practice, skills, and practices of nurse aides in Wisconsin at DHS 129.07 Standards for Nurse Aide Training Programs.
The licensed nurse has the responsibility to supervise, monitor, and evaluate the nursing team members who have received delegated tasks, activities, or procedures. As previously noted, the act of supervision requires the nurse to assess the staff member’s ability, competency, and experience prior to delegating. After the nurse has made the decision to delegate, supervision continues in terms of coaching, supporting, assisting, and educating as needed throughout the task to assure appropriate care is provided.
The nurse is accountable for client care delegated to other team members. Communication and supervision should be ongoing processes throughout the shift within the nursing care team. The nurse must ensure quality of care, appropriateness, timeliness, and completeness through direct and indirect supervision. For example, an RN may directly observe the AP reposition a client or assist them to the bathroom to assure both client and staff safety are maintained. An RN may also indirectly evaluate an LPN’s administration of medication by reviewing documentation in the client’s medical record for timeliness and accuracy. Through direct and indirect supervision of delegation, quality client care and compliance with standards of practice and facility policies can be assured.
Supervision also includes providing constructive feedback to the nursing team member. Constructive feedback is supportive and identifies solutions to areas needing improvement. It is provided with positive intentions to address specific issues or concerns as the person learns and grows in their role. Constructive feedback includes several key points:
- Was the task, activity, care, or procedure performed correctly?
- Were the expected outcomes involving delegation for that client achieved?
- Did the team member utilize effective and timely communication?
- What were the challenges of the activity and what aspects went well?
- Were there any problems or specific concerns that occurred and how were they managed?
After these questions have been addressed, the RN creates a plan for future delegation with the nursing team member. This plan typically includes the following:
- Recognizing difficulty of the nursing team member in initiating or completing the delegated activities.
- Observing the client’s responses to actions performed by the nursing team member.
- Following up in a timely manner on any problems, incidents, or concerns that arose.
- Creating a plan for providing additional training and monitoring outcomes of future delegated tasks, activities, or procedures.
- Consulting with appropriate nursing administrators per agency policy if the client’s safety was compromised.
Please review the following example regarding constructive feedback and task supervision
Nurse Sarah, an experienced RN, delegated a task to Peter, an unlicensed assistive personnel (UAP), to take the vital signs of a post-operative patient, Mrs. Johnson, and report any abnormalities immediately.
Sarah: "Hi Peter, I wanted to discuss the task you completed earlier with Mrs. Johnson's vital signs. Thank you for your help with that. Let’s review how it went."
Was the task, activity, care, or procedure performed correctly?
Sarah: "First, I noticed you recorded the vital signs accurately. Good job on that. However, there was a delay in reporting Mrs. Johnson's elevated blood pressure to me. Can you walk me through what happened?"
Peter: "I took her vital signs, and her blood pressure was high. I was going to inform you, but I got called to assist with another patient immediately after."
Were the expected outcomes involving delegation for that client achieved?
Sarah: "Ultimately, we did address the elevated blood pressure, but the delay could have impacted her care. It's crucial to report such abnormalities immediately."
Did the team member utilize effective and timely communication?
Sarah: "While you communicated the vital signs correctly, the timing was off. In future, if you can't find me immediately, please inform any available nurse or use the intercom system."
What were the challenges of the activity and what aspects went well?
Peter: "The challenge was managing multiple tasks at once. I did feel confident in taking and recording the vital signs accurately, though."
Sarah: "It sounds like you’re balancing a lot of responsibilities well, but prioritizing urgent communications is key. You handled the technical part perfectly."
Were there any problems or specific concerns that occurred and how were they managed?
Sarah: "The main concern was the delay in reporting the elevated blood pressure. Fortunately, there were no serious consequences, but it’s a potential risk we need to manage better. Let’s create a plan to support you moving forward."
Recognizing difficulty of the nursing team member in initiating or completing the delegated activities:
Sarah: "I recognize that you were busy with multiple tasks. It’s important to prioritize patient safety over other duties."
Observing the client’s responses to actions performed by the nursing team member:
Sarah: "I will check on Mrs. Johnson's response to ensure there are no ongoing issues, and I’ll keep exploring how we can improve this process."
Following up in a timely manner on any problems, incidents, or concerns that arose:
Sarah: "I’ll follow up with you soon to see how you’re managing your other tasks, and we can address any challenges you’re facing."
Creating a plan for providing additional training and monitoring outcomes of future delegated tasks, activities, or procedures:
Sarah: "We’ll arrange some additional training on prioritizing tasks and urgent communication. Let's monitor the outcomes of your delegated tasks over the next few weeks to ensure you’re supported."
Consulting with appropriate nursing administrators per agency policy if the client’s safety was compromised:
Sarah: "Fortunately, Mrs. Johnson is fine, but if there were any safety concerns, we’d need to report it according to our policy. Keep this in mind for the future."
Sarah: "Peter, you're doing a great job with your responsibilities, and with a bit more focus on communication priorities, I’m confident you’ll excel even more. Let’s touch base again in a week to see how things are going. Feel free to come to me with any questions or concerns in the meantime."
Peter: "Thank you, Sarah. I appreciate the feedback and will work on prioritizing urgent communications."
Sarah: "Great. Keep up the good work, and let’s keep improving together."
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activities are provided as immediate feedback.)
1. Review the following case studies regarding nurse liability associated with inappropriate delegation:
- Nurse Case Study: Wrongful delegation of patient care to unlicensed assistive personnel
- Nurse Video Case Study: Failure to assess and monitor
Reflective Questions: What delegation errors occurred in each of these scenarios and what were the repercussions of these errors for the nurses involved?
2. The RN is delegating tasks to the LPN/VN and AP on a medical-surgical unit. Using the columns as reference, indicate where delegation errors occurred using the 5 Rs of delegation.
| Right Person | Right Task | Right Circumstance | Right Direction and Communication | Right Supervision and Evaluation | |
|---|---|---|---|---|---|
| Directs the AP to assess the pain level of a client who is post-op Day 3 after a hip replacement and report back the finding. | |||||
| Directs the LPN to give 1 mg IV push morphine to a patient who is 2-hours post total left knee replacement and ensure documentation. | |||||
| Assigns the AP to collect blood pressures on all clients on the unit by 0800. Assumes the AP will report back any abnormal blood pressures. | |||||
| Directs a new AP to ambulate a patient who is post-op Day 2 from a shoulder replacement who needs the assistance of one person and an adaptive walker. The AP voices concerns about never having used an adaptive walker before. The RN directs the AP to get another AP to help. |

Test your knowledge using this NCLEX Next Generation-style Case Study. You may reset and resubmit your answers to this question an unlimited number of times.[37]
There has been significant national debate over the difference between assignment and delegation over the past few decades. In 2019 the National Council of State Boards of Nursing (NCSBN) and the American Nurses Association (ANA) published updated joint National Guidelines on Nursing Delegation (NGND).[38] These guidelines apply to all levels of nursing licensure (advanced practice registered nurses [APRN], registered nurses [RN], and licensed practical/vocational nurses [LPN/VN]) when delegating when there is no specific guidance provided by the state’s Nurse Practice Act (NPA).[39] It is important to note that states have different laws and rules/regulations regarding delegation, so it is the responsibility of all licensed nurses to know what is permitted in their jurisdiction.
The NGND defines a delegatee as an RN, LPN/VN, or AP who is delegated a nursing responsibility by either an APRN, RN, or LPN/VN, is competent to perform the task, and verbally accepts the responsibility.[40] Delegation is allowing a delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role and not routinely performed, but the individual has obtained additional training and validated their competence to perform the delegated responsibility.[41] However, the licensed nurse still maintains accountability for overall client care. Delegated responsibility is a nursing activity, skill, or procedure that is transferred from a licensed nurse to a delegatee.[42] Accountability is defined as being answerable to oneself and others for one’s own choices, decisions, and actions as measured against a standard. Therefore, if a nurse does not feel it is appropriate to delegate a certain responsibility to a delegatee, the delegating nurse should perform the activity themselves.[43]
Delegation is summarized in the NGND as the following[44]:
- A delegatee is allowed to perform a specific nursing activity, skill, or procedure that is outside the traditional role and basic responsibilities of the delegatee’s current job.
- The delegatee has obtained the additional education and training and validated competence to perform the care/delegated responsibility. The context and processes associated with competency validation will be different for each activity, skill, or procedure being delegated. Competency validation should be specific to the knowledge and skill needed to safely perform the delegated responsibility, as well as to the level of the practitioner (e.g., RN, LPN/VN, AP) to whom the activity, skill, or procedure has been delegated. The licensed nurse who delegates the “responsibility” maintains overall accountability for the client, but the delegatee bears the responsibility for completing the delegated activity, skill, or procedure.
- The licensed nurse cannot delegate nursing clinical judgment or any activity that will involve nursing clinical judgment or critical decision-making to AP.
- Nursing responsibilities are delegated by a licensed nurse who has the authority to delegate and the delegated responsibility is within the delegator’s scope of practice.
An example of delegation is medication administration that is delegated by a licensed nurse to AP with additional training in some agencies, according to agency policy. This task is outside the traditional role of AP, but the delegatee has received additional training for this delegated responsibility and has completed competency validation in completing this task accurately.
An example illustrating the difference between assignment and delegation is assisting patients with eating. Feeding patients is typically part of the routine role of AP. However, if a client has recently experienced a stroke (i.e., cerebrovascular accident) or is otherwise experiencing swallowing difficulties (e.g., dysphagia), this task cannot be assigned to AP because it is not considered routine care. Instead, the RN should perform this task themselves or delegate it to an AP who has received additional training on feeding assistance.
The delegation process is multifaceted. See Figure 3.2[45] for an illustration of the intersecting responsibilities of the employer/nurse leader, licensed nurse, and delegatee with two-way communication that protects the safety of the public. “Delegation begins at the administrative/nurse leader level of the organization and includes determining nursing responsibilities that can be delegated, to whom, and under what circumstances; developing delegation policies and procedures; periodically evaluating delegation processes; and promoting a positive culture/work environment. The licensed nurse is responsible for determining client needs and when to delegate, ensuring availability to the delegatee, evaluating outcomes, and maintaining accountability for delegated responsibility. Finally, the delegatee must accept activities based on their competency level, maintain competence for delegated responsibility, and maintain accountability for delegated activity.”[46]
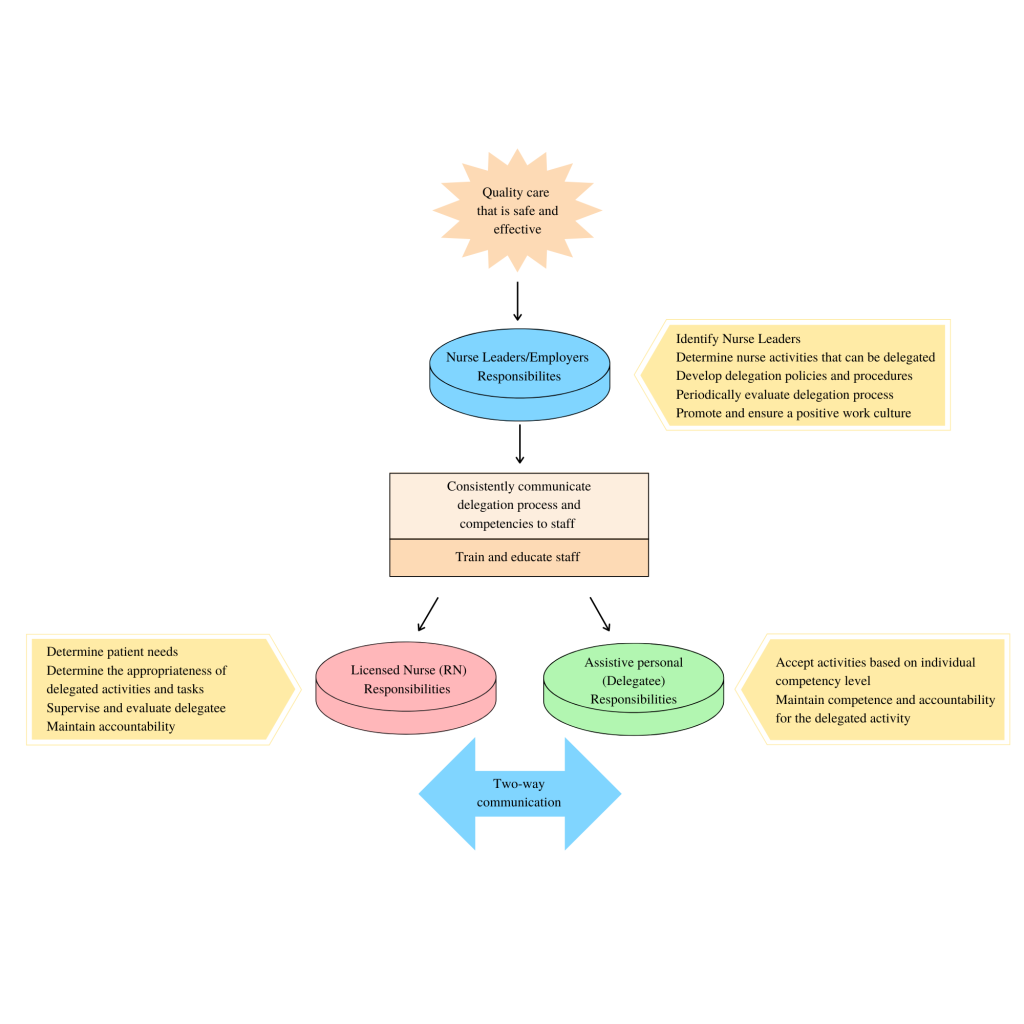
Five Rights of Delegation
How does the RN determine what tasks can be delegated, when, and to whom? According to the National Council of State Boards of Nursing (NCSBN), RNs should use the five rights of delegation to ensure proper and appropriate delegation: right task, right circumstance, right person, right directions and communication, and right supervision and evaluation[47]:
- Right task: The activity falls within the delegatee’s job description or is included as part of the established policies and procedures of the nursing practice setting. The facility needs to ensure the policies and procedures describe the expectations and limits of the activity and provide any necessary competency training.
- Right circumstance: The health condition of the client must be stable. If the client’s condition changes, the delegatee must communicate this to the licensed nurse, and the licensed nurse must reassess the situation and the appropriateness of the delegation.[48]
- Right person: The licensed nurse, along with the employer and the delegatee, is responsible for ensuring that the delegatee possesses the appropriate skills and knowledge to perform the activity.[49]
- Right directions and communication: Each delegation situation should be specific to the client, the nurse, and the delegatee. The licensed nurse is expected to communicate specific instructions for the delegated activity to the delegatee; the delegatee, as part of two-way communication, should ask any clarifying questions. This communication includes any data that need to be collected, the method for collecting the data, the time frame for reporting the results to the licensed nurse, and additional information pertinent to the situation. The delegatee must understand the terms of the delegation and must agree to accept the delegated activity. The licensed nurse should ensure the delegatee understands they cannot make any decisions or modifications in carrying out the activity without first consulting the licensed nurse.[50]
- Right supervision and evaluation: The licensed nurse is responsible for monitoring the delegated activity, following up with the delegatee at the completion of the activity, and evaluating client outcomes. The delegatee is responsible for communicating client information to the licensed nurse during the delegation situation. The licensed nurse should be ready and available to intervene as necessary. The licensed nurse should ensure appropriate documentation of the activity is completed.[51]
Simply stated, the licensed nurse determines the right person is assigned the right tasks for the right clients under the right circumstances. When determining what aspects of care can be delegated, the licensed nurse uses clinical judgment while considering the client’s current clinical condition, as well as the abilities of the health care team member. The RN must also consider if the circumstances are appropriate for delegation. For example, although obtaining routine vital signs on stable clients may be appropriate to delegate to assistive personnel, obtaining vital signs on an unstable client is not appropriate to delegate.
After the decision has been made to delegate, the nurse assigning the tasks must communicate appropriately with the delegatee and provide the right directions and supervision. Communication is key to successful delegation. Clear, concise, and closed-loop communication is essential to ensure successful completion of the delegated task in a safe manner. During the final step of delegation, also referred to as supervision, the nurse verifies and evaluates that the task was performed correctly, appropriately, safely, and competently. Read more about supervision in the following section on “Supervision.” See Table 3.4 for additional questions to consider for each “right” of delegation.
Table 3.4. Rights of Delegation[52]
| Rights of Delegation | Description | Questions to Consider When Delegating |
|---|---|---|
| Right Task | A task that can be transferred to a member of the nursing team for a specific client. |
|
| Right Circumstances | The client is stable. |
|
| Right Person | The person delegating the task has the appropriate scope of practice to do so. The task is also appropriate for this delegatee’s skills and knowledge. |
|
| Right Directions and Communication | The task or activity is clearly defined and described. |
|
| Right Supervision and Evaluation | The RN appropriately monitors the delegated activity, evaluates client outcomes, and follows up with the delegatee at the completion of the activity. |
|
Keep in mind that any nursing intervention that requires specific nursing knowledge, clinical judgment, or use of the nursing process can only be delegated to another RN. Examples of these types of tasks include initial preoperative or admission assessments, client teaching, and creation and evaluation of a nursing care plan. See Figure 3.3[53] for an algorithm based on the 2019 National Guidelines for Nursing Delegation that can be used when deciding if a nursing task can be delegated.[54]
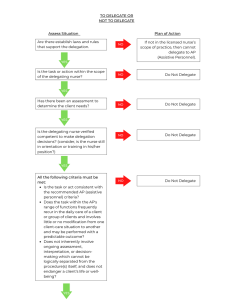
Responsibilities of the Licensed Nurse
The licensed nurse has several responsibilities as part of the delegation process. According to the NGND, any decision to delegate a nursing responsibility must be based on the needs of the client or population, the stability and predictability of the client’s condition, the documented training and competence of the delegatee, and the ability of the licensed nurse to supervise the delegated responsibility and its outcome with consideration to the available staff mix and client acuity. Additionally, the licensed nurse must consider the state Nurse Practice Act regarding delegation and the employer’s policies and procedures prior to making a final decision to delegate. Licensed nurses must be aware that delegation is at the nurse’s discretion, with consideration of the particular situation. The licensed nurse maintains accountability for the client, while the delegatee is responsible for the delegated activity, skill, or procedure. If, under the circumstances, a nurse does not feel it is appropriate to delegate a certain responsibility to a delegatee, the delegating nurse should perform the activity.[55]
1. The licensed nurse must determine when and what to delegate based on the practice setting, the client’s needs and condition, the state's/jurisdiction’s provisions for delegation, and the employer’s policies and procedures regarding delegating a specific responsibility. The licensed nurse must determine the needs of the client and whether those needs are matched by the knowledge, skills, and abilities of the delegatee and can be performed safely by the delegatee. The licensed nurse cannot delegate any activity that requires clinical reasoning, nursing judgment, or critical decision-making. The licensed nurse must ultimately make the final decision whether an activity is appropriate to delegate to the delegatee based on the “Five Rights of Delegation.”
- Rationale: The licensed nurse, who is present at the point of care, is in the best position to assess the needs of the client and what can or cannot be delegated in specific situations.[56]
2. The licensed nurse must communicate with the delegatee who will be assisting in providing client care. This should include reviewing the delegatee’s assignment and discussing delegated responsibilities, including information on the client’s condition/stability, any specific information pertaining to a certain client (e.g., no blood draws in the right arm), and any specific information about the client’s condition that should be communicated back to the licensed nurse by the delegatee.
- Rationale: Communication must be a two-way process involving both the licensed nurse delegating the activity and the delegatee being delegated the responsibility. Evidence shows that the better the communication between the nurse and the delegatee, the more optimal the outcome. The licensed nurse must provide information about the client and care requirements. This includes any specific issues related to any delegated responsibilities. These instructions should include any unique client requirements. The licensed nurse must instruct the delegatee to regularly communicate the status of the client.[57]
3. The licensed nurse must be available to the delegatee for guidance and questions, including assisting with the delegated responsibility, if necessary, or performing it themselves if the client’s condition or other circumstances warrant doing so.
- Rationale: Delegation calls for nursing judgment throughout the process. The final decision to delegate rests in the hands of the licensed nurse as they have overall accountability for the client.[58]
4. The licensed nurse must follow up with the delegatee and the client after the delegated responsibility has been completed.
- Rationale: The licensed nurse who delegates the “responsibility” maintains overall accountability for the client, while the delegatee is responsible for the delegated activity, skill, or procedure.[59]
5. The licensed nurse must provide feedback information about the delegation process and any issues regarding delegatee competence level to the nurse leader. Licensed nurses in the facility need to communicate to the nurse leader responsible for delegation any issues arising related to delegation and any individual whom they identify as not being competent in a specific responsibility or unable to use good judgment and decision-making.
- Rationale: This will allow the nurse leader responsible for delegation to develop a plan to address the situation.[60]
The decision of whether or not to delegate or assign is based on the RN’s judgment concerning the condition of the client, the competence of the nursing team member, and the degree of supervision that will be required of the RN if a task is delegated.[61]
Responsibilities of the Delegatee
Everyone is responsible for the well-being of clients. While the nurse is ultimately accountable for the overall care provided to a client, the delegatee shares the responsibility for the client and is fully responsible for the delegated activity, skill, or procedure.[62] The delegatee has the following responsibilities:
1. The delegatee must accept only the delegated responsibilities that they are appropriately trained and educated to perform and feel comfortable doing given the specific circumstances in the health care setting and client’s condition. The delegatee should confirm acceptance of the responsibility to carry out the delegated activity. If the delegatee does not believe they have the appropriate competency to complete the delegated responsibility, then the delegatee should not accept the delegated responsibility. This includes informing the nursing leadership if they do not feel they have received adequate training to perform the delegated responsibility, do not perform the procedure frequently enough to do it safely, or their knowledge and skills need updating.
- Rationale: The delegatee shares the responsibility to keep clients safe, and this includes only performing activities, skills, or procedures in which they are competent and comfortable doing.[63]
2. The delegatee must maintain competency for the delegated responsibility.
- Rationale: Competency is an ongoing process. Even if properly taught, the delegatee may become less competent if they do not frequently perform the procedure. Given that the delegatee shares the responsibility for the client, the delegatee also has a responsibility to maintain competency.[64]
3. The delegatee must communicate with the licensed nurse in charge of the client. This includes any questions related to the delegated responsibility and follow-up on any unusual incidents that may have occurred while the delegatee was performing the delegated responsibility, any concerns about a client’s condition, and any other information important to the client’s care.
- Rationale: The delegatee is a partner in providing client care. They are interacting with the client/family and caring for the client. This information and two-way communication are important for successful delegation and optimal outcomes for the client.[65]
4. Once the delegatee verifies acceptance of the delegated responsibility, the delegatee is accountable for carrying out the delegated responsibility correctly and completing timely and accurate documentation per facility policy.
- Rationale: The delegatee cannot delegate to another individual. If the delegatee is unable to complete the responsibility or feels as though they need assistance, the delegatee should inform the licensed nurse immediately so the licensed nurse can assess the situation and provide support. Only the licensed nurse can determine if it is appropriate to delegate the activity to another individual. If at any time the licensed nurse determines they need to perform the delegated responsibility, the delegatee must relinquish responsibility upon request of the licensed nurse.[66]
Responsibilities of the Employer/Nurse Leader
The employer and nurse leaders also have responsibilities related to safe delegation of client care:
1. The employer must identify a nurse leader responsible for oversight of delegated responsibilities for the facility. If there is only one licensed nurse within the practice setting, that licensed nurse must be responsible for oversight of delegated responsibilities for the facility.
- Rationale: The nurse leader has the ability to assess the needs of the facility, understand the type of knowledge and skill needed to perform a specific nursing responsibility, and be accountable for maintaining a safe environment for clients. They are also aware of the knowledge, skill level, and limitations of the licensed nurses and AP. Additionally, the nurse leader is positioned to develop appropriate staffing models that take into consideration the need for delegation. Therefore, the decision to delegate begins with a thorough assessment by a nurse leader designated by the institution to oversee the process.[67]
2. The designated nurse leader responsible for delegation, ideally with a committee (consisting of other nurse leaders) formed for the purposes of addressing delegation, must determine which nursing responsibilities may be delegated, to whom, and under what circumstances. The nurse leader must be aware of the state Nurse Practice Act and the laws/rules and regulations that affect the delegation process and ensure all institutional policies are in accordance with the law.
- Rationale: A systematic approach to the delegation process fosters communication and consistency of the process throughout the facility.[68]
3. Policies and procedures for delegation must be developed. The employer/nurse leader must outline specific responsibilities that can be delegated and to whom these responsibilities can be delegated. The policies and procedures should also indicate what may not be delegated. The employer must periodically review the policies and procedures for delegation to ensure they remain consistent with current nursing practice trends and that they are consistent with the state Nurse Practice Act. (Institution/employer policies can be more restrictive, but not less restrictive.)
- Rationale: Policies and procedures standardize the appropriate method of care and ensure safe practices. Having a policy and procedure specific to delegation and delegated responsibilities eliminates questions from licensed nurses and AP about what can be delegated and how they should be performed.[69]
4. The employer/nurse leader must communicate information about delegation to the licensed nurses and AP and educate them about what responsibilities can be delegated. This information should include the competencies of delegatees who can safely perform a specific nursing responsibility.
- Rationale: Licensed nurses must be aware of the competence level of staff and expectations for delegation (as described within the policies and procedures) to make informed decisions on whether or not delegation is appropriate for the given situahttps://www.nursingworld.org/content-hub/resources/nursing-leadership/delegation-in-nursing/tion. Licensed nurses maintain accountability for the client. However, the delegatee has responsibility for the delegated activity, skill, or procedure.
In summary, delegation is the transfer of the nurse’s responsibility for a task while retaining professional accountability for the client’s overall outcome. The decision to delegate is based on the nurse’s judgment, the act of delegation must be clearly defined by the nurse, and the outcomes of delegation are an extension of the nurse’s guidance and supervision. Delegation, when rooted in mutual respect and trust, is a key component to an effective health care team.
Delegation is an integral skill in the nursing profession to help manage the complexities of the dynamic and ever-changing health care environment. Delegation in nursing has been found to increase employee empowerment, decrease burnout, increase role commitment, and improve job satisfaction.[70] Cultivating delegation skills helps nurses better manage the complexities of their client care role, ensuring that their clients are safely cared for and outcomes are optimized. Delegation skills, like other nursing skills, require purposeful development and do not necessarily come easily when first transitioning into the nursing role. It is important that the new graduate nurse does not mistake delegation for pompous or arrogant behavior. Delegation requires mutual respect between the delegator and delegatee. Delegation is not seen as a sign or weakness and does not reflect one's desire to shirk their work responsibilities. Instead, delegation reflects strong leadership and organizational skills in which the nurse leader demonstrates that they understand how to leverage their team's strengths in order to achieve optimal care outcomes.
To help avoid any perception of arrogance in the delegation of an activity, it is important that the new graduate nurse approaches the task of delegation with humility. Clarity in the communication of the delegated responsibility is critical, and the rationale behind the delegation should be communicated to the delegatee. Within the task of delegation, the delegator should express appreciation for the delegatee and their contributions in the collaborative health care environment. Additionally, it is important to understand that no specific nurse delegated task is outside of the "nurse" role. For example, ambulating a client does not to an unlicensed assistive personnel simply because that individual is able to perform that task. Rather, nurses must be willing to perform delegated tasks themselves when necessary. This reflects a team-oriented mindset and helps to reinforce among the care team that all roles are critical to optimizing client care. For new graduate nurses who first transition into a specific health care setting, having the opportunity to shadow individuals in various work roles helps to foster a team mindset. Asking questions of various team members regarding their work role can help a new graduate nurse demonstrate respect and value for other roles.
Examples of helpful questions may include the following:
- "What is the biggest challenge in your typical workday?"
- "What do you most enjoy about your job?"
- "How is it best to communicate with you when the unit is busy?"
- "What do you think people misunderstand most about your role?"
It is important to ensure that the team understands that care is optimized when they function as one collective unit and not in siloed roles. Each team member must feel valued and competent in their role. By understanding and practicing strategic delegation, new graduate nurses can overcome any misconceptions of arrogance and contribute positively to the healthcare team.
Please review the example below to consider variation in approach to task delegation.
Scenario A: Nurse June, a newly graduated nurse, is working in a busy hospital unit. She needs an unlicensed assistive personnel (UAP), Alex, to take vital signs of a patient. Nurse June approaches Alex in the hallway and says in an abrupt tone, "Alex, I need you to take Mr. Smith's vital signs right now. I'm too busy to do it myself, and besides, that's what you're here for. Just get it done quickly."
Analysis: June’s tone and words suggest she sees Alex's role as less important and purely as a means to offload her tasks. June does not explain the urgency or importance of the task. June doesn’t acknowledge Alex's effort or capability, making the request seem like a command rather than a collaborative effort.
Scenario B: Nurse June, a newly graduated nurse, is working in a busy hospital unit. She needs an unlicensed assistive personnel (UAP), Alex, to take vital signs of a patient. Nurse June approaches Alex and says, "Hi Alex, could you please help me by taking Mr. Smith's vital signs? I'm handling a few urgent matters right now, and it would really help to have your support. I know you’re great at this, and your thoroughness really makes a difference in our patient care. Thank you so much!"
Analysis: June speaks to Alex with courtesy and acknowledges the value of his role. June clearly explains why she needs Alex's help and the importance of the task. June acknowledges Alex’s competence and expresses gratitude, fostering feelings of value and respect.
Accountability: Being answerable to oneself and others for one’s own choices, decisions, and actions as measured against a standard.
Assignment: Routine care, activities, and procedures that are within the authorized scope of practice of the RN, LPN/VN, or routine functions of the assistive personnel.
Assistive Personnel (AP): Any assistive personnel (formerly referred to as ‘‘unlicensed” assistive personnel [UAP]) trained to function in a supportive role, regardless of title, to whom a nursing responsibility may be delegated. This includes, but is not limited to, certified nursing assistants or aides (CNAs), patient-care technicians (PCTs), certified medical assistants (CMAs), certified medication aides, and home health aides.[71]
Closed-loop communication: A process that enables the person giving the instructions to hear what they said reflected back and to confirm that their message was, in fact, received correctly.
Constructive feedback: Supportive feedback that offers solutions to areas of weakness.
Delegated responsibility: A nursing activity, skill, or procedure that is transferred from a license nurse to a delegatee.
Delegatee: An RN, LPN/VN, or AP who is delegated a nursing responsibility by either an APRN, RN, or LPN/VN who is competent to perform the task and verbally accepts the responsibility.
Delegation: Allowing a delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role but in which they have received additional training.
Delegator: An APRN, RN, or LPN/VN who requests a specially trained delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role.
Five rights of delegation: Right task, right circumstance, right person, right directions and communication, and right supervision and evaluation.
Nursing team members: Advanced practice registered nurses (APRN), registered nurses (RN), licensed practical/vocational nurses (LPN/VN), and assistive personnel (AP).
Scope of practice: Procedures, actions, and processes that a health care practitioner is permitted to undertake in keeping with the terms of their professional license.
Supervision: Appropriate monitoring of the delegated activity, evaluation of patient outcomes, and follow-up with the delegatee at the completion of the activity.
Titrate: Making adjustments to medication dosage per an established protocol to obtain a desired therapeutic outcome.
Learning Objectives
- Differentiate the role of leader and manager
- Examine the roles of team members
- Identify steps in the management process and activities that managers perform
- Describe the role of the RN as a leader and change agent
- Discuss effects of power, empowerment, and motivation in leading and managing a nursing team
As a nursing student preparing to graduate, you have spent countless hours on developing clinical skills, analyzing disease processes, creating care plans, and cultivating clinical judgment. In comparison, you have likely spent much less time on developing management and leadership skills. Yet, soon after beginning your first job as a registered nurse, you will become involved in numerous situations requiring nursing leadership and management skills. Some of these situations include the following:
- Prioritizing care for a group of assigned clients
- Collaborating with interprofessional team members regarding client care
- Participating in an interdisciplinary team conference
- Acting as a liaison when establishing community resources for a patient being discharged home
- Serving on a unit committee
- Investigating and implementing a new evidence-based best practice
- Mentoring nursing students
Delivering safe, quality client care often requires registered nurses (RN) to manage care provided by the nursing team. Making assignments, delegating tasks, and supervising nursing team members are essential managerial components of an entry-level staff RN role. As previously discussed, nursing team members include RNs, licensed practical/vocational nurses (LPN/VN), and assistive personnel (AP).[72]
Read more about assigning, delegating, and supervising in the “Delegation and Supervision” chapter.
An RN is expected to demonstrate leadership and management skills in many facets of the role. Nurses manage care for high-acuity patients as they are admitted, transferred, and discharged; coordinate care among a variety of diverse health professionals; advocate for clients’ needs; and manage limited resources with shrinking budgets.[73]
Read more about collaborating and communicating with the interprofessional team; advocating for clients; and admitting, transferring, and discharging clients in the “Collaboration Within the Interprofessional Team” chapter.
An article published in the Online Journal of Issues in Nursing states, "With the growing complexity of healthcare practice environments and pending nurse leader retirements, the development of future nurse leaders is increasingly important."[74] This chapter will explore leadership and management responsibilities of an RN. Leadership styles are introduced, and change theories are discussed as a means for implementing change in the health care system.
Localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.
Organizational Culture
The formal leaders of an organization provide a sense of direction and overall guidance for their employees by establishing organizational vision, mission, and values statements. An organization’s vision statement defines why the organization exists, describes how the organization is unique from similar organizations, and specifies what the organization is striving to be. The mission statement describes how the organization will fulfill its vision and establishes a common course of action for future endeavors. See Figure 4.1[75] for an illustration of a mission statement. A values statement establishes the values of an organization that assist with the achievement of its vision and mission. A values statement also provides strategic guidelines for decision-making, both internally and externally, by members of the organization. A values statement may also be reflected as the organization's "core values," which are the foundational ideals that guide the organization's actions and decision-making processes. The vision, mission, and values statements are expressed in a concise and clear manner that is easily understood by members of the organization and the public.[76]

Organizational culture refers to the implicit values and beliefs that reflect the norms and traditions of an organization. An organization’s vision, mission, and values statements are the foundation of organizational culture. Because individual organizations have their own vision, mission, and values statements, each organization has a different culture.[77] Organizational culture helps reflect the expected norms and behaviors that are inherent to an organization. Expected conduct is comprised of the unwritten rules and standards that reflect how employees should behave in different situations. The culture also informs the common communication styles that are inherent to an organization, including both formal and informal channels. The culture may also be manifested outwardly through various symbols and artifacts that embedded within the organization. These may include specific logos, objects, or other physical manifestations of elements that represent the organization's culture. Some organizations may also reflect their cultural values through activities or ceremonies held within the community.
As health care continues to evolve and new models of care are introduced, nursing managers must develop innovative approaches that address change while aligning with that organization’s vision, mission, and values. Leaders embrace the organization’s mission, identify how individuals’ work contributes to it, and ensure that outcomes advance the organization’s mission and purpose. Leaders use vision, mission, and values statements for guidance when determining appropriate responses to critical events and unforeseen challenges that are common in a complex health care system. Successful organizations require employees to be committed to following these strategic guidelines during the course of their work activities. Employees who understand the relationship between their own work and the mission and purpose of the organization will contribute to a stronger health care system that excels in providing first-class patient care. The vision, mission, and values provide a common organization-wide frame of reference for decision-making for both leaders and staff.[78] It is important for employees in health care organizations to have understanding of how their roles and responsibilities connect to the broader mission and vision of the organization. This alignment fosters a cohesive work environment where each staff member is motivated by a shared purpose, leading to more effective and high-quality patient care. It is important that both the leader and employee have clarity in the underlying vision, mission, and values of an organization. This involves responsibility for both the leader and employee. Leaders must articulate the organization's vision, mission, and values clearly and consistently. This involves regular communication through meetings, written materials, etc. Employees share in the responsibility by being empowered to ask questions and seek clarification on how their daily tasks contribute to the organization's overarching goals.
Learning Activity
Investigate the mission, vision, and values of a potential employer, as you would do prior to an interview for a job position.
Reflective Questions
- How well do the organization’s vision and values align with your personal values regarding health care?
- How well does the organization’s mission align with your professional objective in your resume?
Followership
Followership is described as the upward influence of individuals on their leaders and their teams. The actions of followers have an important influence on staff performance and patient outcomes. Being an effective follower requires individuals to contribute to the team not only by doing as they are told, but also by being aware and raising relevant concerns. Effective followers realize that they can initiate change and disagree or challenge their leaders if they feel their organization or unit is failing to promote wellness and deliver safe, value-driven, and compassionate care. Leaders who gain the trust and dedication of followers are more effective in their leadership role. Everybody has a voice and a responsibility to take ownership of the workplace culture, and good followership contributes to the establishment of high-functioning and safety-conscious teams.[79] Key elements of effective followership include proactive engagement, constructive communication, collaboration, advocacy, continuous improvement, and a supportive leadership environment.
In order to demonstrate proactive engagement, followers must also be initiators. Effective followers do not passively wait for instruction by rather take initiative to address issues, propose solutions, and contribute to ideas. They recognize the importance of their voice in engaging in problem-solving and understand that being an effective follower does not mean being passive in their role. Effective followers also employ a keen situational awareness where they maintain vigilant assessment of the environment and potential risks, ensuring that they act in the best interests of clients. They must be confident that they can raise concerns if they identify potential problems or unsafe practices. This reflects a culture where followers feels that their feedback is welcomed and valued. Effective followership also involves communication practices in which the message is clearly conveyed, measures to confirm the message are employed, and the confirmation is received. To be an effective follower, support of the team's goals must be a central tenet of one's work. Collaboration with others involves supporting colleagues and working together toward the common goal even when viewpoints may differ. Identifying strategies that create a respectful opportunity to debate and explore different opinions is important to effective followership. Additionally, followers must take accountability for their own actions while understanding how their role and performance impacts the function of the team, as well as client outcomes. Effective followers also practice ethical advocacy, ensuring that the needs of clients are prioritized and respected. This advocacy also involves the ability to courageously challenge any decisions or actions that may jeopardize care or organizational values. Finally, effective followers engage in continuous learning to enhance their skills and knowledge. They seek feedback and use the feedback to contribute to their own performance and also the growth of the team. Effective followership is further cultivated when leaders and followers come together with mutual respect, trust, and work with a purposeful drive toward shared goals that reflect the organization's mission.
Team members impact patient safety by following teamwork guidelines for good followership. For example, strategies such as closed-loop communication are important tools to promote patient safety.
Read more about communication and teamwork strategies in the “Collaboration Within the Interprofessional Team” chapter.
Leadership and Management Characteristics
Leadership and management are terms often used interchangeably, but they are two different concepts with many overlapping characteristics. Leadership is the art of establishing direction and influencing and motivating others to achieve their maximum potential to accomplish tasks, objectives, or projects.[80],[81] See Figure 4.2[82] for an illustration of team leadership. There is no universally accepted definition or theory of nursing leadership, but there is increasing clarity about how it differs from management.[83] Management refers to roles that focus on tasks such as planning, organizing, prioritizing, budgeting, staffing, coordinating, and reporting.[84] The overriding function of management has been described as providing order and consistency to organizations, whereas the primary function of leadership is to produce change and movement.[85] View a comparison of the characteristics of management and leadership in Table 4.2a.

Table 4.2a. Management and Leadership Characteristics[86]
| MANAGEMENT | LEADERSHIP |
|---|---|
Planning, Organizing, and Prioritizing
|
Establishing Direction
|
Budgeting and Staffing
|
Influencing Others
|
Coordinating and Problem-Solving
|
Motivating
|
Leader Vs. Manager Case Activity
Utilizing the information from the table above, review the following cases and identify whether the individual is serving as a leader or manager based upon the actions taken within the case scenario. Include supportive rationale for your decision regarding the role.
Case 1: Sima, the head nurse, reviews the upcoming schedule and allocates resources to ensure each shift is adequately staffed. She also makes assignments for the nursing staff based on their skills and patient needs. Additionally, she is responsible for hiring new staff and, when necessary, terminating employees who do not meet performance standards.
Case 2: Juan, a senior nurse, is passionate about improving patient care. He identifies an issue with the current handoff process between shifts and proposes a new strategy that incorporates evidence-based practices to enhance communication and reduce errors. He reaches out to his team at their monthly department meetings in order to develop a shared vision for this change and encourages them to partner with him on the new process.
Case 3: Maria, a unit supervisor, holds a meeting to set specific goals and time frames for the department’s upcoming projects. She prioritizes tasks for the team and establishes policies and procedures to ensure these tasks are completed efficiently and within the given deadlines.
Case 4: Emily, the nurse director, is tasked with preparing the budget for the upcoming fiscal year. She allocates resources effectively to ensure all departments are adequately funded. Emily also manages the staffing needs, ensuring that the hiring and termination processes are handled efficiently.
Case 5: Rachel, an experienced nurse, takes the time to build effective teamwork within her unit. She advocates for her patients, their families, and the nursing profession as a whole. Rachel communicates openly and listens to her team’s concerns, ensuring everyone feels valued and heard.
Not all nurses are managers, but all nurses are leaders because they encourage individuals to achieve their goals. The American Nurses Association (ANA) established Leadership as a Standard of Professional Performance for all registered nurses. Standards of Professional Performance are “authoritative statements of action and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently.”[87] See the competencies of the ANA Leadership standard in the following box and additional content in other chapters of this book.
Competencies of ANA’s Leadership Standard of Professional Performance
- Promotes effective relationships to achieve quality outcomes and a culture of safety
- Leads decision-making groups
- Engages in creating an interprofessional environment that promotes respect, trust, and integrity
- Embraces practice innovations and role performance to achieve lifelong personal and professional goals
- Communicates to lead change, influence others, and resolve conflict
- Implements evidence-based practices for safe, quality health care and health care consumer satisfaction
- Demonstrates authority, ownership, accountability, and responsibility for appropriate delegation of nursing care
- Mentors colleagues and others to embrace their knowledge, skills, and abilities
- Participates in professional activities and organizations for professional growth and influence
- Advocates for all aspects of human and environmental health in practice and policy
Read additional content related to leadership and management activities in corresponding chapters of this book:
- Read about the culture of safety in the “Legal Implications” chapter.
- Read about effective interprofessional teamwork and resolving conflict in the “Collaboration Within the Interprofessional Team” chapter.
- Read about quality improvement and implementing evidence-based practices in the “Quality and Evidence-Based Practice” chapter.
- Read more about delegation, supervision, and accountability in the “Delegation and Supervision” chapter.
- Read about professional organizations and advocating for patients, communities, and their environments in the “Advocacy” chapter.
- Read about budgets and staffing in the “Health Care Economics” chapter.
- Read about prioritization in the “Prioritization” chapter.
Leadership Theories and Styles
In the 1930s Kurt Lewin, the father of social psychology, originally identified three leadership styles: authoritarian, democratic, and laissez-faire.[88],[89]
Authoritarian leadership means the leader has full power. Authoritarian leaders tell team members what to do and expect team members to execute their plans. When fast decisions must be made in emergency situations, such as when a patient “codes,” the authoritarian leader makes quick decisions and provides the group with direct instructions. However, there are disadvantages to authoritarian leadership. Authoritarian leaders are more likely to disregard creative ideas of other team members, causing resentment and stress.[90]
Democratic leadership balances decision-making responsibility between team members and the leader. Democratic leaders actively participate in discussions, but also make sure to listen to the views of others. For example, a nurse supervisor may hold a meeting regarding an increased incidence of patient falls on the unit and ask team members to share their observations regarding causes and potential solutions. The democratic leadership style often leads to positive, inclusive, and collaborative work environments that encourage team members’ creativity. Under this style, the leader still retains responsibility for the final decision.[91]
Laissez-faire is a French word that translates to English as, “leave alone.” Laissez-faire leadership gives team members total freedom to perform as they please. Laissez-faire leaders do not participate in decision-making processes and rarely offer opinions. The laissez-faire leadership style can work well if team members are highly skilled and highly motivated to perform quality work. However, without the leader’s input, conflict and a culture of blame may occur as team members disagree on roles, responsibilities, and policies. By not contributing to the decision-making process, the leader forfeits control of team performance.[92]
Over the decades, Lewin’s original leadership styles have evolved into many styles of leadership in health care, such as passive-avoidant, transactional, transformational, servant, resonant, and authentic.[93],[94] Many of these leadership styles have overlapping characteristics. See Figure 4.3[95] for a comparison of various leadership styles in terms of engagement.

Passive-avoidant leadership is similar to laissez-faire leadership and is characterized by a leader who avoids taking responsibility and confronting others. Employees perceive the lack of control over the environment resulting from the absence of clear directives. Organizations with this type of leader have high staff turnover and low retention of employees. These types of leaders tend to react and take corrective action only after problems have become serious and often avoid making any decisions at all.[96]
Transactional leadership involves both the leader and the follower receiving something for their efforts; the leader gets the job done and the follower receives pay, recognition, rewards, or punishment based on how well they perform the tasks assigned to them.[97] Staff generally work independently with no focus on cooperation among employees or commitment to the organization.[98]
Transformational leadership involves leaders motivating followers to perform beyond expectations by creating a sense of ownership in reaching a shared vision.[99] It is characterized by a leader’s charismatic influence over team members and includes effective communication, valued relationships, and consideration of team member input. Transformational leaders know how to convey a sense of loyalty through shared goals, resulting in increased productivity, improved morale, and increased employees’ job satisfaction.[100] They often motivate others to do more than originally intended by inspiring them to look past individual self-interest and perform to promote team and organizational interests.[101]
Servant leadership focuses on the professional growth of employees while simultaneously promoting improved quality care through a combination of interprofessional teamwork and shared decision-making. Servant leaders assist team members to achieve their personal goals by listening with empathy and committing to individual growth and community-building. They share power, put the needs of others first, and help individuals optimize performance while forsaking their own personal advancement and rewards.[102]
Visit the Greenleaf Center site to learn more about What is Servant Leadership?
Resonant leaders are in tune with the emotions of those around them, use empathy, and manage their own emotions effectively. Resonant leaders build strong, trusting relationships and create a climate of optimism that inspires commitment even in the face of adversity. They create an environment where employees are highly engaged, making them willing and able to contribute with their full potential.[103]
Authentic leaders have an honest and direct approach with employees, demonstrating self-awareness, internalized moral perspective, and relationship transparency. They strive for trusting, symmetrical, and close leader–follower relationships; promote the open sharing of information; and consider others’ viewpoints.[104]
Table 4.2b. Characteristics of Leadership Styles
| Authoritarian | Democratic | Laissez-Faire or Passive-Avoidant |
|---|---|---|
|
|
|
| Transactional | Transformational | Servant |
|---|---|---|
|
|
|
| Resonant Leaders | Authentic Leaders |
|---|---|
|
|
Outcomes of Various Leadership Styles
Leadership styles affect team members, patient outcomes, and the organization. A systematic review of the literature published in 2021 showed significant correlations between leadership styles and nurses’ job satisfaction. Transformational leadership style had the greatest positive correlation with nurses’ job satisfaction, followed by authentic, resonant, and servant leadership styles. Passive-avoidant and laissez-faire leadership styles showed a negative correlation with nurses’ job satisfaction.[105] In this challenging health care environment, managers and nurse leaders must promote technical and professional competencies of their staff, but they must also act to improve staff satisfaction and morale by using appropriate leadership styles with their team.[106]
Systems Theory
Systems theory is based on the concept that systems do not function in isolation but rather there is an interdependence that exists between their parts. Systems theory assumes that most individuals strive to do good work but are affected by diverse influences within the system. Efficient and functional systems account for these diverse influences and improve outcomes by studying patterns and behaviors across the system.[107]
Many health care agencies have adopted a culture of safety based on systems theory. A culture of safety is an organizational culture that embraces error reporting by employees with the goal of identifying systemic causes of problems that can be addressed to improve patient safety. According to The Joint Commission, a culture of safety includes the following components[108]:
- Just Culture: A culture where people feel safe raising questions and concerns and report safety events in an environment that emphasizes a nonpunitive response to errors and near misses. Clear lines are drawn by managers between human error, at-risk, and reckless employee behaviors. See Figure 4.4[109] for an illustration of Just Culture.
- Reporting Culture: People realize errors are inevitable and are encouraged to speak up for patient safety by reporting errors and near misses. For example, nurses complete an “incident report” according to agency policy when a medication error occurs, or a client falls. Error reporting helps the agency manage risk and reduce potential liability.
- Learning Culture: People regularly collect information and learn from errors and successes while openly sharing data and information and applying best evidence to improve work processes and patient outcomes.
Just Culture
The American Nurses Association (ANA) officially endorses the Just Culture model. In 2019 the ANA published a position statement on Just Culture, stating, “Traditionally, healthcare’s culture has held individuals accountable for all errors or mishaps that befall patients under their care. By contrast, a Just Culture recognizes that individual practitioners should not be held accountable for system failings over which they have no control. A Just Culture also recognizes many individual or ‘active’ errors represent predictable interactions between human operators and the systems in which they work. However, in contrast to a culture that touts ‘no blame’ as its governing principle, a Just Culture does not tolerate conscious disregard of clear risks to patients or gross misconduct (e.g., falsifying a record or performing professional duties while intoxicated).”
The Just Culture model categorizes human behavior into three causes of errors. Consequences of errors are based on whether the error is a simple human error or caused by at-risk or reckless behavior.
- Simple human error: A simple human error occurs when an individual inadvertently does something other than what should have been done. Most medical errors are the result of human error due to poor processes, programs, education, environmental issues, or situations. These errors are managed by correcting the cause, looking at the process, and fixing the deviation. For example, a nurse appropriately checks the rights of medication administration three times, but due to the similar appearance and names of two different medications stored next to each other in the medication dispensing system, administers the incorrect medication to a patient. In this example, a root cause analysis reveals a system issue that must be modified to prevent future patient errors (e.g., change the labelling and storage of look alike-sound alike medication).
- At-risk behavior: An error due to at-risk behavior occurs when a behavioral choice is made that increases risk where the risk is not recognized or is mistakenly believed to be justified. For example, a nurse scans a patient’s medication with a barcode scanner prior to administration, but an error message appears on the scanner. The nurse mistakenly interprets the error to be a technology problem and proceeds to administer the medication instead of stopping the process and further investigating the error message, resulting in the wrong dosage of a medication being administered to the patient. In this case, ignoring the error message on the scanner can be considered “at-risk behavior” because the behavioral choice was considered justified by the nurse at the time.
- Reckless behavior: Reckless behavior is an error that occurs when an action is taken with conscious disregard for a substantial and unjustifiable risk.[110] For example, a nurse arrives at work intoxicated and administers the wrong medication to the wrong patient. This error is considered due to reckless behavior because the decision to arrive intoxicated was made with conscious disregard for substantial risk.
These examples show three different causes of medication errors that would result in different consequences to the employee based on the Just Culture model. Under the Just Culture model, after root cause analysis is completed, system-wide changes are made to decrease factors that contributed to the error. Managers appropriately hold individuals accountable for errors if they were due to simple human error, at-risk behavior, or reckless behaviors.
If an individual commits a simple human error, managers console the individual and consider changes in training, procedures, and processes. In the “simple human error” above, system-wide changes would be made to change the label and location of the medication to prevent future errors from occurring with the same medication.
Individuals committing at-risk behavior are held accountable for their behavioral choice and often require coaching with incentives for less risky behaviors and situational awareness. In the “at-risk behavior” example above where the nurse ignored an error message on the barcode scanner, mandatory training on using a barcode scanner and responding to errors would be implemented, and the manager would track the employee’s correct usage of the barcode scanner for several months following training.
If an individual demonstrates reckless behavior, remedial action and/or punitive action is taken.[111] In the “reckless behavior” example above, the manager would report the nurse’s behavior to the state's Board of Nursing with mandatory substance abuse counseling to maintain their nursing license. Employment may be terminated with consideration of patterns of behavior.
A Just Culture in which employees aren't afraid to report errors is a highly successful way to enhance patient safety, increase staff and patient satisfaction, and improve outcomes. Success is achieved through good communication, effective management of resources, and an openness to changing processes to ensure the safety of patients and employees. The infographic in Figure 4.4[112] illustrates the components of a culture of safety and Just Culture.
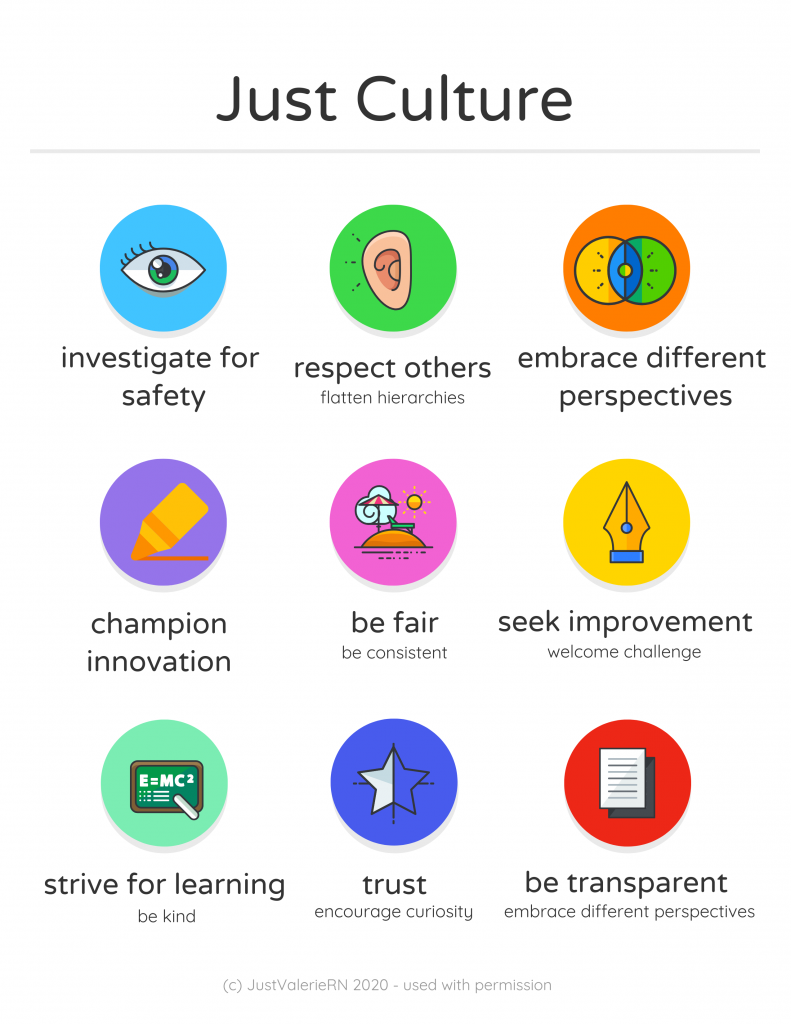
The principles of culture of safety, including Just Culture, Reporting Culture, and Learning Culture are also being adopted in nursing education. It’s understood that mistakes are part of learning and that a shared accountability model promotes individual- and system-level learning for improved patient safety. Under a shared accountability model, students are responsible for the following[113]:
- Being fully prepared for clinical experiences, including laboratory and simulation assignments
- Being rested and mentally ready for a challenging learning environment
- Accepting accountability for their part in contributing to a safe learning environment
- Behaving professionally
- Reporting their own errors and near mistakes
- Keeping up-to-date with current evidence-based practice
- Adhering to ethical and legal standards
Students know they will be held accountable for their actions but will not be blamed for system faults that lie beyond their control. They can trust that a fair process will be used to determine what went wrong if a patient care error or near miss occurs. Student errors and near misses are addressed based on an investigation determining if it was simple human error, an at-risk behavior, or reckless behavior. For example, a simple human error by a student can be addressed with coaching and additional learning opportunities to remedy the knowledge deficit. However, if a student acts with recklessness (for example, repeatedly arrives to clinical unprepared despite previous faculty feedback or falsely documents an assessment or procedure), they are appropriately and fairly disciplined, which may include dismissal from the program.[114]
See Table 4.2c describing classifications of errors using the Just Culture model.
Table 4.2c. Classification of Errors Using the Just Culture Model
| Human Error | At-Risk Behavior | Reckless Behavior |
|---|---|---|
| The caregiver made an error while working appropriately and focusing on the patient’s best interests. | The caregiver made a potentially unsafe choice resulting from faulty or self-serving decision-making. | The caregiver knowingly violated a rule and/or made a dangerous or unsafe choice. |
| Investigation reveals system factors contributing to similar errors by others with similar knowledge and skills. | Investigation reveals the system supports risky action and the caregiver requires coaching. | Investigation reveals the caregiver is accountable and needs retraining. |
| Manage by fixing system errors in processes, procedures, training, design, or environment. | Manage by coaching the caregiver and fixing any system issues:
|
Manage by disciplining the caregiver. If the system supports reckless behavior, it requires fixing. |
| CONSOLE | COACH | PUNISH |
Systems leadership refers to a set of skills used to catalyze, enable, and support the process of systems-level change that is encouraged by the Just Culture Model. Systems leadership is comprised of three interconnected elements:[115]
- The Individual: The skills of collaborative leadership to enable learning, trust-building, and empowered action among stakeholders who share a common goal
- The Community: The tactics of coalition building and advocacy to develop alignment and mobilize action among stakeholders in the system, both within and between organizations
- The System: An understanding of the complex systems shaping the challenge to be addressed
Just Culture Case Review
Review the following case descriptions. Identify the classification of error that has occurred and the recommended actions that should occur.
A chief nursing officer receives a daily report of organization incident reports and reviews the following incident:
Incident Description
Patient Mr. Joe Doden, Room 13067, Medical-Surgical floor
On the afternoon of May 15, 2024, Nurse Sarah was responsible for administering Mr. Joe Doden's insulin dose. The insulin vials used by the hospital had recently been redesigned by the manufacturer, which led to changes in the labeling. The patient was scheduled to receive ten units of regular insulin at 14:30. However, at 1450 the patient turns on his call light, reports feeling unwell. He is shaky, confused, and sweating profusely. The patient's glucose is checked, and he is found to be hypoglycemic. He is treated based upon the hypoglycemia protocol and recovers without further complication.
Case Investigation A
Action: Sarah RN who administered the insulin was following the protocol but mistakenly read the dosage due to a poorly designed label on the insulin vial. The nurse was focused on the patient’s best interests and followed all required steps.
Findings: The investigation revealed that the labeling on the insulin vials was confusing and had led to similar errors by other nurses in the past. The system's design flaw contributed significantly to the error.
How would you classify this error? What actions should be taken?
Case Investigation B
Action: Sarah RN, due to time pressure and a high patient load, decided to skip the double-check protocol for administering the same insulin dose, believing it would save time without causing harm.
Findings: The investigation revealed that the hospital’s workload and time pressures often led to shortcuts in following safety protocols.
How would you classify this error? What actions should be taken?
Case Investigation C
Action: Sarah RN, is familiar with the protocol and knowingly bypassed the double check system, dismissing its importance and administering a medication dose on her own.
Findings: The investigation found that the nurse had a history of disregarding safety protocols, showing a pattern of reckless behavior. This behavior was not supported by the hospital’s policies or environment.
How would you classify this error? What actions should be taken?

