6.9 Tuberculosis
Open Resources for Nursing (Open RN)
Overview
Tuberculosis (TB) is a contagious bacterial infection caused by Mycobacterium tuberculosis. It primarily affects the lungs but can also target other parts of the body. TB spreads through the air when an infected person coughs or sneezes, releasing small infectious droplets into the environment. It is a serious public health concern worldwide.[1]
Pathophysiology
TB is caused by an organism called a bacillus that enters the lung. Over the course of 2 to 12 weeks, the bacillus replicates and the immune response becomes activated. The immune response involves macrophages and lymphocytes migrating to the site of inflammation and walling off the bacillus, forming a tubercle. Over time, cheese-like material develops in the center of the tubercle, called caseous necrosis. Individuals with healthy immune systems may heal this initial lesion and develop latent TB before any signs or symptoms of the illness occur. However, the tubercle may calcify and remain dormant for many years, but over time, or in immunocompromised states, spread to other areas of the lung or to other organs.
There are several risk factors for TB. Primary risk factors include close contact with an TB-infected person, HIV infection or otherwise weakened immune system, and substance abuse. TB is a common disease around the world, so individuals who travel or live in regions with high TB prevalence such as Africa, Asia, or parts of Latin America have increased risk. Individuals who immigrate from high-incidence countries or experience homelessness are also at increased risk. Additionally, individuals who live in overcrowded conditions are at increased risk for TB transmission, including individuals who work or live in long-term health care settings or prisons.[2]
In regions of the world with high TB prevalence, a Bacillus Calmette-Guérin (BCG) vaccine is commonly administered. Receiving a BCG vaccine has a substantial effect on tuberculin skin test reactivity, with individuals who received BCG after infancy having tuberculin skin test reactions up to 55 years post-immunization.[3] Nurses must be aware of an individual’s history of receiving a BCG vaccine when interpreting the results of a tuberculin skin test. Anyone who has received the BCG vaccine within the last ten years will have a positive test result for their skin test.
Mycobacterium tuberculosis has developed drug resistance in many areas of the world, causing a significant treatment problem. Multidrug-resistant TB (MDR TB) is caused by an organism that is resistant to at least isoniazid and rifampin, the two most potent TB drugs used to treat all persons with TB disease. Extensively drug-resistant TB (XDR TB) is a rare type of MDR TB that is resistant to isoniazid and rifampin, plus any fluoroquinolone and at least one of the second-line drugs. XDR TB is of special concern for persons with HIV infection or other conditions that weaken the immune system. These persons are more likely to develop TB disease once they are infected, and they also have a higher risk of death once they develop TB. Resistance to anti-TB medications can occur when these drugs are mismanaged. Examples of mismanagement include when individuals do not complete their full course of treatment; when health care providers prescribe the wrong treatment, the wrong dose, or length of time for taking the drugs; when the supply of drugs is not always available; or when the drugs are of poor quality. The most important thing a person can do to prevent the spread of MDR TB is to take all of their medications exactly as prescribed by their health care provider. No doses should be missed, and treatment should not be stopped early.[4]
Assessment
Tuberculosis (TB) can affect various body systems, but it primarily targets the respiratory system. TB can mimic other diseases, and its presentation can vary widely among individuals. Identifying TB through clinical manifestations and diagnostic tests is crucial for early diagnosis and treatment. TB is a contagious disease, and timely intervention helps prevent its spread to others. It is important to note that some forms of tuberculosis may present with minimal or no symptoms, known as latent tuberculosis infection (LTBI). In LTBI, the individual carries the TB bacteria but does not exhibit active disease. See Table 6.9 for a summary of potential clinical manifestations of tuberculosis across body systems.
Table 6.9. Clinical Manifestations of Tuberculosis Across Body Systems[5],[6]
| Body System | Clinical Manifestations |
|---|---|
| Respiratory | Persistent cough for more than two weeks, hemoptysis, purulent sputum, pleuritic chest pain, dyspnea, and adventitious lung sounds. |
| General | Fever, chills, night sweats, fatigue, malaise (general discomfort), weakness, unexplained weight loss, and loss of appetite. |
| Lymphatic | Lymphadenopathy (swelling of lymph nodes), especially in the neck. |
| Nervous | Tuberculous meningitis can lead to symptoms such as severe headache, confusion, stiffness of the neck, and neurological deficits. |
| Genitourinary | Renal tuberculosis can cause hematuria (blood in the urine) and flank pain. |
| Musculoskeletal | Tuberculous osteomyelitis may lead to bone pain, joint pain, and limited mobility of affected joints. |
| Skin and Soft Tissues | Cutaneous tuberculosis can result in skin lesions or ulcers. |
Diagnostic Testing
Diagnosing tuberculosis (TB) involves a combination of clinical assessment, imaging, and laboratory tests to confirm the presence of Mycobacterium tuberculosis. If diagnostic tests reveal a positive result, TB is a reportable disease to the public health department.
A combination of tests may be necessary to confirm a TB diagnosis, and prompt diagnosis and treatment are crucial to prevent the spread of TB and improve client outcomes. Diagnostic testing may include the following[7],[8]:
- Tuberculin Skin Test (Mantoux Test): A small amount of tuberculin protein is injected just beneath the skin, usually in the forearm. The test is read 48 to 72 hours later to check for induration at the injection site. A positive reaction indicates exposure to TB or the BCG vaccine, but it does not confirm active disease. Further testing is needed to determine if the infection is active or latent.
- Blood Tests (Interferon-Gamma Release Assays – IGRA): These tests measure the body’s immune response to TB by detecting the release of interferon-gamma when exposed to TB proteins. Common IGRA tests include the QuantiFERON-TB Gold In-Tube (QFT-GIT) and the T-SPOT TB tests. Blood tests are particularly useful when the tuberculin skin test results may be affected by prior BCG vaccination or other factors.
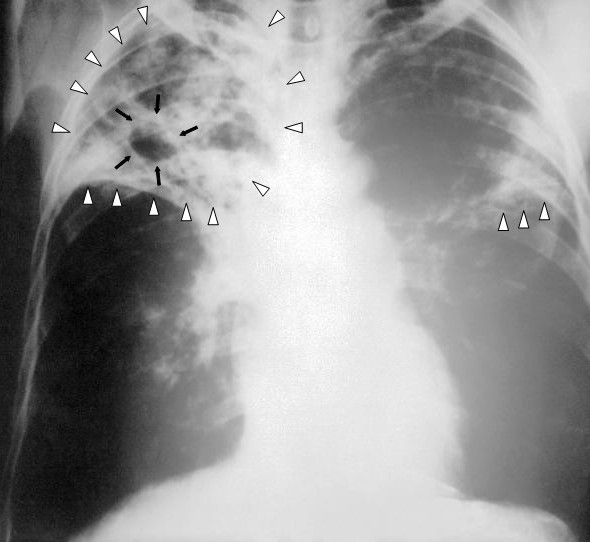
- Chest X-ray: A chest X-ray is used to detect pulmonary TB and assess the extent of lung involvement. However, active TB cannot be distinguished from inactive disease using only radiography. See Figure 6.26[9] for an image of a chest X-ray illustrating advanced active TB.
- Sputum Smear Microscopy: A sputum sample is examined in a lab under a microscope to detect acid-fast bacilli (AFB). It is a rapid method for diagnosing pulmonary TB. However, it may not always detect the Mycobacterium tuberculosis bacteria, particularly in early stages.
- Sputum Culture: A sputum sample is cultured to grow the Mycobacterium tuberculosis bacteria. A sputum culture confirms the diagnosis of active TB and is also used to evaluate the effectiveness of treatment. Culture allows for drug susceptibility testing to determine which antibiotics are effective against the specific strain. It is more sensitive than smear microscopy but takes several weeks to yield results.
- Nucleic Acid Amplification Tests (NAAT): NAAT tests can rapidly detect TB and simultaneously assess resistance to rifampin, an important anti-TB drug. These tests are particularly valuable in diagnosing drug-resistant TB. This type of test is performed by obtaining a swab of respiratory material.
- Bronchoscopy and Bronchoalveolar Lavage (BAL): These procedures involve inserting a thin, flexible tube into the airways and collecting samples for testing. They are used when sputum samples are not obtainable or when there is a need for a definitive diagnosis.
- Biopsy: A biopsy may be necessary if there is suspicion of extrapulmonary TB, affecting organs outside the lungs. Biopsies are performed to examine tissue samples for the presence of TB.
- Molecular Diagnostic Tests: These tests are highly sensitive and provide rapid results. They can identify Mycobacterium tuberculosis and determine rifampin resistance.
Nursing Diagnoses
Nursing care for clients with TB focuses on promoting adherence to treatment, preventing the spread of the disease, and addressing the physical and psychosocial challenges associated with TB. Common nursing diagnoses for clients with TB include the following[10]:
- Ineffective Airway Clearance
- Fatigue
- Impaired Gas Exchange
- Readiness for Enhanced Health Self-Management
- Social Isolation
Outcome Identification
Outcome identification includes setting short- and long-term goals and creating expected outcome statements customized for the client’s specific needs. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions.
Sample expected outcomes for common nursing diagnoses related to tuberculosis are as follows:
- The client will effectively clear airway secretions as evidenced by improved breath sounds and productive coughing.
- The client will maintain adequate oxygenation with oxygen saturation levels above 92%.
- The client will verbalize the importance of adhering to prescribed therapy for the full treatment plan.
- The client will verbalize three positive coping strategies before discharge from the hospital.
Interventions
Medical Interventions
Medical interventions for tuberculosis (TB) are primarily aimed at treating the infection and preventing its spread. Treatment regimens for TB typically involve a combination of antibiotics taken for an extended period of time and the implementation of airborne transmission precautions when the disease is active.[11],[12]
Medication Therapy
The cornerstone of TB treatment involves a combination of antibiotics to effectively kill the Mycobacterium tuberculosis bacteria. The standard treatment includes four first-line drugs: isoniazid, rifampin, ethambutol, and pyrazinamide. Drug-sensitive TB is treated with a combination of these antibiotics over a period of four to nine months, with the initial phase lasting two months. Multi-drug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB) require more complex regimens with second-line drugs. Treatment for drug-resistant TB may last 18 to 24 months or longer. The selection of drugs and treatment duration depend on the type of TB and individual client factors. After medication therapy has been initiated, sputum cultures are obtained at specific intervals to monitor the presence of acid-fast bacilli (AFB) and to assess treatment response. Clients are considered infectious until three negative sputum samples have been obtained, typically after approximately three months of treatment.
To ensure medication adherence and reduce the risk of developing drug resistance, health care workers or trained observers may directly observe clients taking their medications, referred to as directly observed therapy (DOT). DOT is a crucial intervention to assist with medication compliance, prevent treatment failure, and control the spread of drug-resistant TB.
Infection Control
Clients who are diagnosed with active TB and are hospitalized have airborne transmission precautions in place, including placement in private rooms with special air venting. Health care workers wear N95 masks when caring for clients with active TB. Individuals in close contact with newly diagnosed clients are tested and monitored for TB infection. Prophylactic treatment may be offered to those exposed to TB to prevent the progression to active TB.
Nursing Interventions
Nursing interventions for tuberculosis (TB) include supporting adherence to treatment and preventing the spread of the disease.
Medication Management
For clients receiving inpatient care, nurses administer prescribed medications. During outpatient care, nurses may assist in providing directly observed therapy (DOT) to ensure clients take their medications as directed for the full course of treatment to help prevent the development of drug resistance. Nurses also monitor and teach clients about potential side effects of their medications, including when to notify their health care provider.
Health Teaching
Nurses teach clients cough etiquette, respiratory hygiene, and proper disposal of tissues to prevent the spread of infection. Airborne transmission precautions, including the use of N95 masks, are explained to hospitalized clients and their family members.
Malnutrition is common in clients with TB. Nurses monitor for signs of malnutrition and advocate for referrals to dieticians for meal plans and supplements to support weight gain and overall health.
Psychosocial Support
Nurses assess the psychosocial impact of TB, considering the potential stigma and anxiety associated with the disease. They provide emotional support to clients and their family members to help them cope with the diagnosis. They also advocate for client access to health care services and help them navigate the health care system and connect with appropriate resources.
Evaluation
During the evaluation stage, nurses determine the effectiveness of nursing interventions for a specific client. The previously identified expected outcomes are reviewed to determine if they were met, partially met, or not met by the time frames indicated. If outcomes are not met or only partially met by the time frame indicated, the nursing care plan is revised. Evaluation should occur every time the nurse implements interventions with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with other members of the interprofessional team.
![]() RN Recap: Tuberculosis
RN Recap: Tuberculosis
View a brief YouTube video overview of tuberculosis[13]:
- Menzies, D. (2023). Tuberculosis infection (latent tuberculosis) in adults: Approach to diagnosis (screening). UpToDate. Retrieved October 5, 2023, from https://www.uptodate.com/ ↵
- Menzies, D. (2023). Tuberculosis infection (latent tuberculosis) in adults: Approach to diagnosis (screening). UpToDate. Retrieved October 5, 2023, from https://www.uptodate.com/ ↵
- This work is a derivative of StatPearls by Okafor, Rewane, & Momodu and is licensed under CC BY 4.0 ↵
- Centers for Disease Control and Prevention. (2023, August 29). Tuberculosis (TB). https://www.cdc.gov/tb/default.htm ↵
- Menzies, D. (2023). Tuberculosis infection (latent tuberculosis) in adults: Approach to diagnosis (screening). UpToDate. Retrieved October 5, 2023, from https://www.uptodate.com/ ↵
- Bernardo, J. (2022). Diagnosis of pulmonary tuberculosis in adults. UpToDate. Retrieved October 5, 2023, from https://www.uptodate.com/ ↵
- Menzies, D. (2023). Tuberculosis infection (latent tuberculosis) in adults: Approach to diagnosis (screening). UpToDate. Retrieved October 5, 2023, from https://www.uptodate.com/ ↵
- Bernardo, J. (2022). Diagnosis of pulmonary tuberculosis in adults. UpToDate. Retrieved October 5, 2023, from https://www.uptodate.com/ ↵
- “Tuberculosis-x-ray-1.jpg” by Unknown author, for the Centers for Disease Control and Prevention, is licensed in the Public Domain. ↵
- Flynn Makic, M. B., & Martinez-Kratz, M. R. (2023). Ackley and Ladwig’s Nursing diagnosis handbook: An evidence-based guide to planning care (13th ed.). Elsevier. ↵
- Menzies, D. (2023). Tuberculosis infection (latent tuberculosis) in adults: Approach to diagnosis (screening). UpToDate. Retrieved October 5, 2023, from https://www.uptodate.com/ ↵
- Bernardo, J. (2022). Diagnosis of pulmonary tuberculosis in adults. UpToDate. Retrieved October 5, 2023, from https://www.uptodate.com/ ↵
- Open RN Project. (2024, June 23). Health Alterations - Chapter 6 - Tuberculosis [Video]. You Tube. CC BY-NC 4.0 https://youtu.be/LpH6ql_MENo?si=Zm6-gcGXC364lAAO ↵
The cost of health care in the United States is higher than any other country in the world and has a significant financial impact on our economy.[1] U.S. health care spending grew 4.1 percent in 2022, reaching $ 4.5 trillion or $13,493 per person. Health care spending accounts for 17.3 percent of our Gross Domestic Product (GDP), the total value of goods produced and services provided annually.[2] See Figure 8.1[3] for a graph of health care cost as a percentage of GDP in the United States compared to other countries around the world.

Despite spending more money on health care than other high-income countries, the United States has some of the poorest health outcomes, such as the lowest life expectancy, the highest infant mortality rate, and a higher prevalence of chronic diseases.[4] The increasing costs of health care also have several negative impacts on society, employers, and individuals, including the following effects[5]:
- When the government spends more on health care, the national debt increases and funds available for other programs decrease.
- When people spend more on health care, they have less money to spend on other items.
- When health insurance is paid by employers, employees are paid less.
- When employers spend more on health care, the costs of their products and services increase. Jobs may be moved to countries with lower health care costs.
- An increasing number of people cannot afford health care insurance. When people without health care insurance receive health care, they often cannot pay for it. As a result of unpaid bills, this care is indirectly paid for by other people paying increased insurance premiums and taxes.
- People without health care insurance may not seek preventative care and develop a more costly, serious medical disorder that could have been prevented.
- Medical bills that are not covered by health insurance can cause bankruptcy.
There are several national trends affecting the cost of health care and related impacts, including the aging population, increased costs of medical technology, increased prescription medication cost, the Affordable Care Act, social determinants of health, etc. These trends can be further classified as intrinsic or extrinsic factors. Intrinsic factors related to increased health care costs are inherent to the characteristics and needs of the population. One significant intrinsic factor is the demographics of the population, such as age, gender, and overall health status. An aging population, for example, typically requires more medical care due to the prevalence of chronic conditions and the natural decline in health associated with aging. Another intrinsic factor is the demand for health care services. As people become more health-conscious, the demand for preventive care, regular check-ups, and advanced treatments rises, leading to increased overall health care spending. Additionally, the extent and nature of health insurance coverage play a crucial role. Comprehensive insurance plans often lead to higher utilization of health care services, as insured individuals are more likely to seek medical care, knowing that a significant portion of the costs will be covered by their insurance.
Extrinsic factors are external elements that impact health care costs. One of the most prominent extrinsic factors is the availability and adoption of medical technology. Advanced diagnostic tools, treatment methods, and surgical techniques can drive up costs due to their high development, implementation, and maintenance expenses. While these technologies can significantly improve patient outcomes, they also contribute to rising health care expenditures. Another critical extrinsic factor is the cost of prescription drugs. Pharmaceutical pricing strategies, including research and development costs, marketing, and profit margins, often lead to high prices for medications, especially for new and specialized drugs. Workforce costs are also a significant extrinsic factor. The salaries and benefits of health care professionals, including doctors, nurses, and administrative staff, constitute a substantial portion of health care expenses. These costs are influenced by factors such as education and training requirements, labor market conditions, and regulatory policies. Addressing these extrinsic factors requires strategic planning and policy interventions to balance cost containment with the quality and accessibility of health care services.
Aging Population
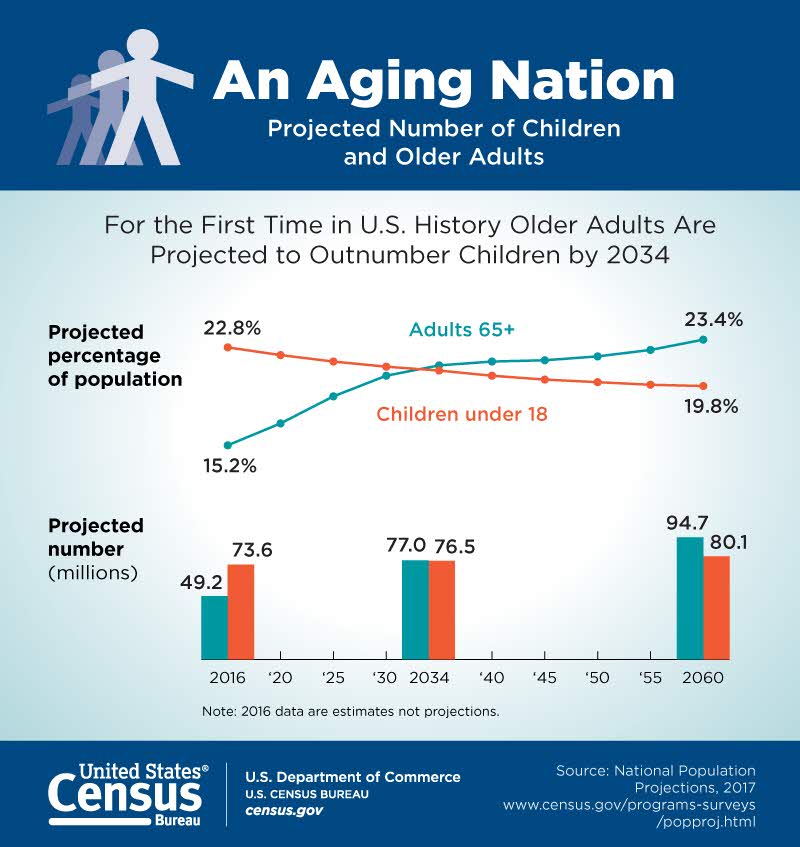
According to the Agency for Healthcare Research and Quality (AHRQ), the United States has a growing number of older adults (age 65 years or older) who are living longer than previous generations. It is anticipated that older adults will make up more than 20 percent of the U.S. population by 2030.[6] See Figure 8.2[7] for an illustration of the aging population from the U.S. Census Bureau. This change in demographics will result in increased national health care costs because older adults typically experience more chronic conditions than younger populations, requiring expensive specialty and long-term care.[8]
Increased Costs of Medical Technology
Highly visible medical technologies, such as organ transplantation, diagnostic imaging systems, and biotechnology products, attract both praise and blame. Evolving medical technologies may save lives and improve a client’s health status, but they are also viewed as a dominant cause of continued escalation of medical costs. Research suggests that medical technology accounts for about 10 to 40 percent of the increase in health care expenditures over time.[9] These costs also lead to further ethical dilemmas as decisions regarding what scarce resources are provided to which patients are made. See Figure 8.3[10] for an image of common technology used in health care.

Medical technologies, especially new ones, must justify their costs in a climate of competing claims on limited resources. Resource allocation follows American society's objective of cost effectiveness: if a new technology improves health outcomes at a lower cost than existing technologies, it should be adopted; otherwise, it should not.[11]
Increased Prescription Medication Costs
Retail prices for commonly-used prescription medications continue to increase twice as much as inflation, contributing to increased health care costs and making these life-sustaining medicines potentially unaffordable to many Americans. According to a recent AARP Rx Price Watch report, in 2020 prices for 260 commonly used medications increased 2.9 percent while the general rate of inflation was 1.3 percent.[12] For example, the cost of Symbicort, a medication used to treat asthma and COPD, increased 46 percent, from $2,940 to $4,282.[13] See Figure 8.4[14] for an illustration related to prescription medication costs.
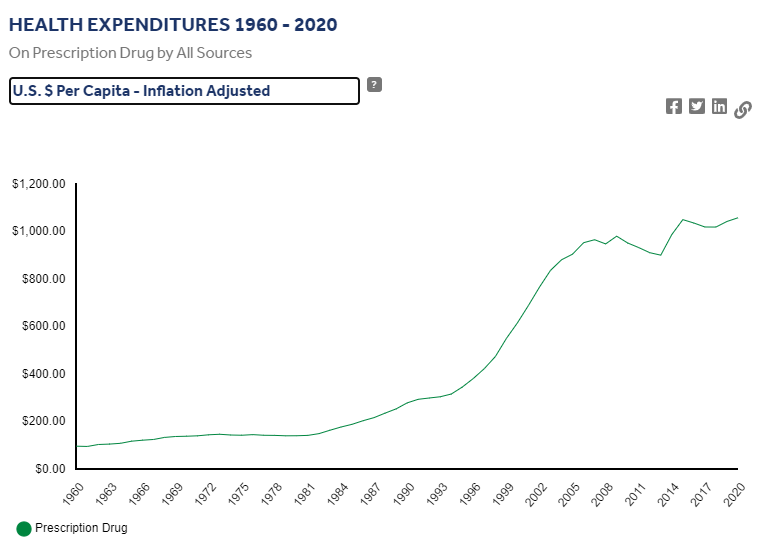
Although the majority of Americans have either public or private insurance that helps them pay for medications, increased medication prices result in higher health insurance premiums and higher taxpayer costs for the Medicare and Medicaid programs. Some insurance companies only cover approved formulary medications. As a result, national organizations like the American Association of Retired Persons (AARP) advocate for national policy changes, such as allowing Medicare to negotiate the prices of prescription medications with drug companies and allowing private insurance plans to have access to those lower prices.[15]
Many consumers find themselves tasked with the difficult decision of purchasing expensive medication or going without prescribed medication and paying for their families' housing and food. Nurses often become involved in case management activities when assisting clients to obtain medications they cannot afford. Nursing case management activities are discussed later in this chapter.
Affordable Care Act
The Patient Protection and Affordable Care Act (PPACA), also known as the Affordable Care Act (ACA) or Obamacare, was signed into law in 2010. The purpose of this legislation was to increase consumers' access to health care coverage and protect them from insurance practices that restricted care or significantly increased the cost of care. The ACA mandated health insurance coverage for employers and individuals. Employers were mandated to provide health care coverage based on the number of their employees, and individuals who were not covered through employer insurance plans were mandated to seek coverage through a newly created Marketplace. The Marketplace provides a central, website that offers three standard health insurance coverage levels to facilitate comparison by consumers. As a result of the ACA and associated Medicaid expansion, 32 million people had health care coverage in 2021.[16]
Key Provisions of the ACA
The ACA includes the following key provisions[17]:
- Insurers can no longer deny coverage or care for preexisting conditions like diabetes, asthma, and cancer.
- Young adults may remain on their parents’ insurance plans until they are 26 (even if they are married, financially independent, or not living with their parents).
- Health insurance plans cannot place annual or lifetime limits on coverage, except for nonessential exceptions, such as cosmetic procedures.
- Many preventive services must be provided, such as:
- Well-child visits, flu shots, and other common vaccines
- Screening tests for blood pressure and diabetes
- Diagnostic screening tests, such mammograms and colonoscopies
- Counseling services related to mental health and substance use
The ACA also provides an avenue for consumers to appeal insurance companies’ denials for care or payment of services and restricts situations in which an insurance carrier may cancel a policy.
Challenges to the ACA
Although the ACA has significantly increased the number of Americans with health insurance coverage, it continues to be debated. Debates focus on increased taxes, increased insurance premiums, and some people’s belief that mandated coverage is governmental intrusion on an individual’s rights. The Affordable Care Act has been challenged three times without success. In 2012 the U. S. Supreme Court upheld mandated coverage as a constitutional exercise of Congress’ taxing powers because it could be interpreted as an individual’s choice to maintain health insurance or pay a tax. However, in 2017 Congress set the penalty for failing to comply with the mandate at zero dollars after multiple attempts to repeal and replace the ACA. In June 2021 the U.S. Supreme Court rejected a third major challenge regarding the constitutionality of the ACA. In a 7-to-2 decision, the U.S. Supreme Court upheld the ACA based on the judgment that the states who brought forth the case did not prove damage to citizens because the fines for not having health coverage had been eliminated since the original legislation was passed.[18]
What to Expect Next
Given the Supreme Court’s recent decision regarding the ACA, it is expected the current administration will continue to advocate for the ACA and work towards making ACA tax credits permanent. Congress is also actively debating other legislative proposals to reduce health care costs, such as medication pricing reform and expanding Medicare eligibility age and benefits.[19]
Social Determinants of Health
Social Determinants of Health (SDOH) are the conditions in the environments where people live, learn, work, and play that affect a wide range of outcomes. SDOH include health care access and quality, neighborhood and environment, social and community context, economic stability, and education access and quality. These conditions have a major impact on people’s health and well-being, ultimately affecting national health care costs.[20]
SDOH directly impact individuals' health behaviors, their access to routine health care, and development of chronic disease. Yet, the United States spends a significantly lower percentage of its gross domestic product (GDP) on social services as compared to similar countries with better health outcomes.[21]
Healthy People 2030, established by the U.S. Department of Health and Human Services, identifies public health priorities to help individuals, organizations, and communities across the United States improve health and well-being over the next decade by addressing SDOH. One of Healthy People 2030’s goals states, “Create social, physical, and economic environments that promote attaining the full potential for health and well-being for all.”[22] Nurses act in many ways to address these priorities as they advocate for individuals, families, and communities.
Maria's Journey Through the Health Care System
Maria, a 45-year-old woman, lives in a low-income neighborhood in a large urban area. She works two part-time jobs to support her family of four and has limited access to health care due to financial constraints and transportation issues. Maria has been diagnosed with type 2 diabetes, and her health care outcomes are significantly influenced by various Social Determinants of Health (SDOH).
Maria's low income and unstable employment contribute to her inability to afford healthy food, medications, and regular medical check-ups. This economic instability exacerbates her diabetes, as she often skips doses of her medication to save money and cannot afford nutritious meals that would help manage her condition. The constant stress of making ends meet and providing for her family leads to increased cortisol levels, which can negatively impact her blood sugar control.
- How can Maria's financial stress impact her ability to manage her diabetes effectively?
2. What programs or policies could be implemented to assist individuals like Maria in managing their health care costs?
Maria has limited knowledge about diabetes management due to a lack of education and access to health information. This impacts her ability to understand and implement lifestyle changes or adhere to treatment plans. With limited education, Maria struggles to find better-paying jobs that could provide health insurance and more financial stability.
3. In what ways can improved health literacy impact Maria's diabetes management?
4. What community resources could be made available to enhance health education for individuals in Maria's situation?
The availability of health care services in Maria’s neighborhood is limited, with long wait times and fewer specialists. This results in delayed diagnoses and treatments for her diabetes-related complications. Maria lacks comprehensive health insurance, making it difficult for her to access primary and specialist care. High out-of-pocket costs deter her from seeking regular medical attention.
5. How does the lack of accessible health care services affect Maria's long-term health outcomes?
6. What are some potential solutions to improve health care access in underserved areas?
Maria lives in a food desert with limited access to fresh fruits and vegetables. She often relies on inexpensive, processed foods that worsen her diabetes. Public transportation in Maria’s area is unreliable, making it challenging for her to attend medical appointments. This lack of transportation contributes to missed check-ups and unmanaged diabetes.
7. How does living in a food desert affect Maria's ability to manage her diabetes?
8. What transportation initiatives could help individuals like Maria access healthcare services more easily?
Maria has a limited social network and lacks support from friends and family, which is crucial for managing a chronic condition like diabetes. This isolation can lead to depression and further neglect of her health. Living in a high-crime area, Maria feels unsafe walking outside for exercise, which is essential for diabetes management. This sedentary lifestyle negatively affects her health outcomes.
9. How does a lack of social support contribute to Maria's health challenges?
10. What community programs or interventions could be implemented to enhance social support and safety in high-crime areas?

