6.7 Pneumonia
Open Resources for Nursing (Open RN)
Overview
Pathophysiology
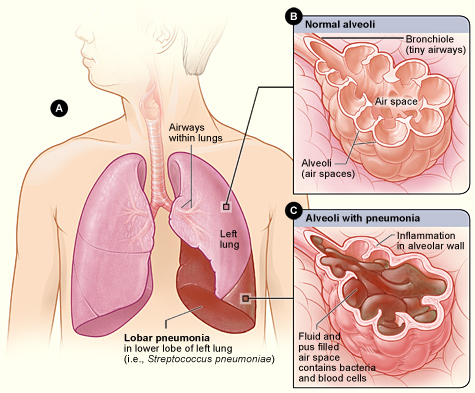
Pneumonia is a common respiratory infection that can affect people of all ages. It is characterized by inflammation and infection within the alveoli, causing them to fill with fluid or purulent material, resulting in a productive cough, fever, chills, and difficulty breathing. Pneumonia differs from chronic conditions like asthma and COPD in that it is an acute infection. Pneumonia can range in seriousness from mild to life-threatening. It is most serious for infants and young children, people older than age 65, and people with chronic health problems like COPD or weakened immune systems.[1],[2]
Pneumonia can be caused by a variety of microorganisms, including bacteria, viruses, and fungi. Common bacteria that cause pneumonia include Streptococcus pneumoniae and Mycoplasma pneumoniae. A variety of respiratory viruses such as rhinovirus, influenza, respiratory syncytial virus (RSV), and COVID-19 also cause pneumonia. Fungi can also cause pneumonia, especially in individuals with weakened immune systems.[3] See Figure 6.23[4] for an illustration of pneumonia.
Classifications of Pneumonia
Pneumonia is classified according to the type of microorganism that caused it and the location where the individual developed the infection. This classification affects the medical treatment plan and the antibiotics used to treat it. Classifications of pneumonia include the following[5]:
- Community-acquired pneumonia (CAP) refers to pneumonia that began in the community (not in a hospital).
- Hospital-acquired pneumonia (HAP) refers to pneumonia that began during or immediately following a stay in a health care setting. Health care settings include hospitals, long-term care facilities, and dialysis centers.
- Ventilator-associated pneumonia (VAP) refers to when someone gets pneumonia during or after being on a ventilator.
- Aspiration pneumonia refers to when someone inhales food, drink, vomit, saliva, or medication into the lungs instead of swallowing it. Risk factors for aspiration pneumonia include difficulty swallowing, a brain injury that causes an impaired gag reflex, oversedation by medications, or excessive alcohol or drug use.[6]
Assessment
Clinical manifestations of pneumonia vary in severity and can be influenced by factors such as the causative pathogen, as well as the individual’s age, overall health, and underlying medical conditions. See Table 6.7 for a summary of clinical manifestations of pneumonia across body systems. It is essential for nurses to recognize these symptoms early and notify the health care provider of suspected pneumonia.
Table 6.7. Clinical Manifestations of Pneumonia[7],[8]
| Body System | Clinical Manifestations |
|---|---|
| Respiratory | Cough (nonproductive or productive of purulent sputum), dyspnea, pleuritic chest pain (worse with deep breathing or coughing), labored breathing, tachypnea, fine crackles on auscultation, and decreased pulse oximetry readings |
| Cardiovascular | Tachycardia |
| Nervous | New onset confusion or altered mental status |
| Gastrointestinal | Decreased appetite |
| Musculoskeletal | Muscle aches and joint pain, especially for viral causes, fatigue, and weakness |
| Integumentary | Diaphoresis and cyanosis (bluish or grayish skin due to lack of oxygen) |
| General | Fever, shaking chills (most often with high temperature), malaise (general discomfort or uneasiness), and weight loss (often due to reduced appetite) |
Diagnostic Testing
Pneumonia is typically diagnosed through a combination of clinical assessment, medical history, and diagnostic tests. Common diagnostic tests used to diagnose pneumonia are as follows:
- Chest X-Ray: A chest X-ray identifies areas of the lung that are inflamed or filled with fluid, called “consolidation.” The X-ray provides a visual confirmation of the infection and its extent in the lungs.
- Complete Blood Count (CBC): An elevated white blood cell count is often an indicator of an infection.
- Sputum Culture: A sputum sample (mucus coughed up from the lungs) may be collected for laboratory testing to identify the causative microorganism. This is especially important for selecting appropriate antibiotic treatment.
In serious cases of pneumonia, especially for hospitalized clients, additional diagnostic testing may be performed[9],[10]:
- Arterial Blood Gas (ABG): ABG testing assesses the amount of dissolved oxygen and carbon dioxide levels in the blood and determines the severity of hypoxemia and hypercapnia.
- Bronchoscopy: In cases where the diagnosis is uncertain or when there is a need to examine the airways directly, a bronchoscopy may be performed. This involves passing a thin, flexible tube with a camera through the airways to visualize the lungs and collect samples.
- CT Scan: A computed tomography (CT) scan may be performed to provide more detailed images of the lungs.
- Blood Cultures: Blood cultures may be performed to determine if bacterial pneumonia has spread to the blood.
- Pleural Fluid Culture: A pleural fluid culture may be taken using a procedure called thoracentesis, which is a procedure where a health care provider uses a needle to take a sample of fluid from the pleural space between the lungs and chest wall.
Review normal reference ranges for common diagnostic tests in “Appendix A – Normal Reference Ranges.”
Nursing Diagnoses
Nursing priorities for clients with pneumonia are focused on improving respiratory function, alleviating symptoms, and supporting recovery while preventing complications.
Nursing diagnoses for clients with pneumonia are formulated based on the client’s assessment data, medical history, and specific needs. Common nursing diagnoses include the following[11]:
- Ineffective Airway Clearance
- Impaired Gas Exchange
- Ineffective Thermoregulation
- Decreased Activity Intolerance
- Risk for Deficient Fluid Volume
Outcome Identification
Outcome identification includes setting short- and long-term goals and creating expected outcome statements customized for the client’s specific needs. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions.
Sample expected outcomes for common nursing diagnoses related to pneumonia are as follows:
- The client will maintain oxygen saturation within the target range, typically above 92%.
- The client’s signs of infection, such as fever above 101 degrees Fahrenheit and elevated white blood cell count, will improve with treatment.
- The client’s reported level of dyspnea at rest and with activity will decrease with treatment.
Interventions
Medical Interventions
Medical interventions for pneumonia aim to treat the underlying infection, alleviate symptoms, and support the client’s recovery.
Medication Therapy
A variety of medications may be prescribed for clients with pneumonia[12],[13]:
- Antibiotic Therapy: Antibiotics are prescribed if the suspected or confirmed causative agent is bacteria. The choice of antibiotic by the health care provider is based on the classification of pneumonia (i.e., CAP, HAP, VAP, or aspiration pneumonia). The antibiotic may be adjusted based on sputum or blood culture and sensitivity results. Duration of treatment is determined by the type of pneumonia and the client’s clinical response.
- Antiviral Medications: If pneumonia is caused by a viral infection, antiviral medications may be prescribed. These medications aim to reduce viral replication and severity of symptoms.
- Antifungal Medications: If pneumonia is caused by a fungal infection, antifungal medications are utilized to target and eliminate fungal pathogens, disrupting their ability to grow and reproduce.
- Bronchodilators: Bronchodilators, such as albuterol, may be administered to alleviate bronchoconstriction and improve airflow, especially in clients with concurrent obstructive lung diseases like asthma or COPD.
- Corticosteroids: Corticosteroids may be prescribed in specific cases to reduce inflammation in the airways and improve breathing.
- Antipyretics: Antipyretic medications (e.g., acetaminophen or ibuprofen) may be prescribed to reduce fever and discomfort.
- Pneumococcal and Influenza Vaccinations: To prevent future episodes of pneumonia, clients are encouraged to receive influenza, COVID, and pneumococcal vaccines.
- Oxygen Therapy: Supplemental oxygen is prescribed to maintain adequate oxygen saturation levels. Oxygen delivery methods vary based on the client’s needs and severity of respiratory distress.
- Fluid Intake: Clients are encouraged to increase fluid intake to maintain hydration and thin secretions, if not contraindicated. For hospitalized clients, IV fluids may be prescribed, especially if the client has a high fever, reduced oral intake, or difficulty swallowing.
Read additional information about oxygen equipment and safety measures in the “Oxygenation Therapy” chapter of Open RN Nursing Skills, 2e.
Respiratory Therapies
Chest physiotherapy techniques, such as postural drainage and percussion, may be used to assist in clearing mucus and secretions from the airways. Vibratory positive expiratory pressure (PEP) therapy (i.e., flutter valves) may be prescribed for clients who need assistance in clearing mucus from their airways. Clients are encouraged to cough and deep breathe, and incentive spirometry devices may be prescribed to treat/prevent atelectasis. Review information about vibratory positive expiratory pressure therapy, coughing and deep breathing, and incentive spirometers in the “General Nursing Interventions Related to Respiratory Alterations” subsection earlier in this chapter.
Ventilation Support
In severe cases of pneumonia, noninvasive positive pressure ventilation, commonly referred to as CPAP or BiPAP, or intubation and mechanical ventilation may be necessary to provide respiratory support.[14],[15] See Figure 6.24[16] for an image of a simulated client with a BiPAP mask in place.

Read more about CPAP, BiPAP, and mechanical ventilation in the “Oxygen Equipment” section of the “Oxygen Therapy” chapter of Open RN Nursing Skills, 2e.
Pleural Procedures
In cases of pleural effusion (accumulation of fluid in the pleural cavity), procedures such as thoracentesis or chest tube insertion may be required.[17],[18]
Nursing Interventions
Nursing interventions for pneumonia focus on promoting recovery, preventing complications, and preventing future illness.
Medication Management
Nurses safely administer prescribed antibiotics, antivirals, or antifungals that target the specific pathogen causing pneumonia. Antipyretic medications (e.g., acetaminophen or ibuprofen) are administered as needed to reduce fever and discomfort. Bronchodilators may be administered to alleviate bronchoconstriction and improve airflow, especially in clients with preexisting lung conditions. Nurses teach clients about the purpose of prescribed medications and the importance of taking the full course of antibiotics as directed.
Maintain Hydration
Nurses monitor fluid intake and output and for signs of fluid volume deficit. Clients are encouraged to maintain adequate hydration, especially if they have a fever, productive cough, or increased respiratory rate that can contribute to fluid loss. Clients are encouraged to drink at least two liters of water daily to loosen secretions, unless they are on a fluid restriction.
Assist With Respiratory Therapy
Nurses assist clients with techniques such as postural drainage, coughing and deep breathing, incentive spirometry, and/or vibratory pressure therapy, as prescribed. Effective coughing techniques are demonstrated and encouraged. Review enhanced breathing and coughing techniques in the “General Nursing Interventions Related to Respiratory Alterations” subsection earlier in this chapter.
Infection Control
Nurses implement appropriate infection control measures, including hand hygiene, personal protective equipment, and transmission-based precautions based on the infectious organism to prevent the spread of infection.
Immunizations
Nurses encourage clients to remain up-to-date on recommended vaccinations, including the pneumococcal vaccine for adults at risk and all those over age 65.
Review current information about “Recommended Vaccines By Age” from the Centers for Disease Control and Prevention (CDC).
Evaluation
During the evaluation stage, nurses determine the effectiveness of nursing interventions for a specific client. The previously identified expected outcomes are reviewed to determine if they were met, partially met, or not met by the time frames indicated. If outcomes are not met or only partially met by the time frame indicated, the nursing care plan is revised. Evaluation should occur every time the nurse implements interventions with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with other members of the interprofessional team.
![]() RN Recap: Pneumonia
RN Recap: Pneumonia
View a brief YouTube video overview of pneumonia[19]:
- Ramirez, J. A. (2023). Overview of community-acquired pneumonia in adults. UpToDate. Retrieved October 4, 2023, from https://www.uptodate.com/ ↵
- National Heart, Lung, and Blood Institute. (2022, March 24). What is pneumonia? https://www.nhlbi.nih.gov/health/pneumonia#:~:text=Pneumonia%20is%20an%20infection%20that,or%20fungi%20may%20cause%20pneumonia ↵
- Centers for Disease Control and Prevention. (2022, September 30). Pneumonia. https://www.cdc.gov/pneumonia/index.html ↵
- “Lobar_pneumonia_illustrated.jpg” by Heart, Lung and Blood Institute is licensed in the Public Domain. ↵
- Centers for Disease Control and Prevention. (2022, September 30). Pneumonia. https://www.cdc.gov/pneumonia/index.html ↵
- Mayo Clinic. (2020, June 13). Pneumonia. https://www.mayoclinic.org/diseases-conditions/pneumonia/symptoms-causes/syc-20354204 ↵
- Ramirez, J. A. (2023). Overview of community-acquired pneumonia in adults. UpToDate. Retrieved October 4, 2023, from https://www.uptodate.com/ ↵
- National Heart, Lung, and Blood Institute. (2022, March 24). What is pneumonia? https://www.nhlbi.nih.gov/health/pneumonia#:~:text=Pneumonia%20is%20an%20infection%20that,or%20fungi%20may%20cause%20pneumonia ↵
- Ramirez, J. A. (2023). Overview of community-acquired pneumonia in adults. UpToDate. Retrieved October 4, 2023, from https://www.uptodate.com/ ↵
- National Heart, Lung, and Blood Institute. (2022, March 24). What is pneumonia? https://www.nhlbi.nih.gov/health/pneumonia#:~:text=Pneumonia%20is%20an%20infection%20that,or%20fungi%20may%20cause%20pneumonia ↵
- Flynn Makic, M. B., & Martinez-Kratz, M. R. (2023). Ackley and Ladwig’s Nursing diagnosis handbook: An evidence-based guide to planning care (13th ed.). Elsevier. ↵
- Ramirez, J. A. (2023). Overview of community-acquired pneumonia in adults. UpToDate. Retrieved October 4, 2023, from https://www.uptodate.com/ ↵
- National Heart, Lung, and Blood Institute. (2022, March 24). What is pneumonia? https://www.nhlbi.nih.gov/health/pneumonia#:~:text=Pneumonia%20is%20an%20infection%20that,or%20fungi%20may%20cause%20pneumonia ↵
- Ramirez, J. A. (2023). Overview of community-acquired pneumonia in adults. UpToDate. Retrieved October 4, 2023, from https://www.uptodate.com/ ↵
- National Heart, Lung, and Blood Institute. (2022, March 24). What is pneumonia? https://www.nhlbi.nih.gov/health/pneumonia#:~:text=Pneumonia%20is%20an%20infection%20that,or%20fungi%20may%20cause%20pneumonia ↵
- “Simulated patient wearing a BiPAP mask” by Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- Ramirez, J. A. (2023). Overview of community-acquired pneumonia in adults. UpToDate. Retrieved October 4, 2023, from https://www.uptodate.com/ ↵
- National Heart, Lung, and Blood Institute. (2022, March 24). What is pneumonia? https://www.nhlbi.nih.gov/health/pneumonia#:~:text=Pneumonia%20is%20an%20infection%20that,or%20fungi%20may%20cause%20pneumonia ↵
- Open RN Project. (2024, June 23). Health Alterations - Chapter 6 - Pneumonia [Video]. You Tube. CC BY-NC 4.0 https://youtu.be/PDbrPS3X50I?si=BGo8htPvDJIqfW82 ↵
Allison is a new graduate nurse who is recently transitioned from her orientation period to her scheduled night shift work on a medical telemetry unit. She has a patient care assignment of six patients. Her patient, Mr. Daniels, was admitted from the ER at 2200 shortly before her shift began. He was transferred to the floor with a diagnosis of Heart Failure exacerbation. The patient was prescribed IV push furosemide for diuresis. It is now 0500 and the patient’s morning potassium level is reported from the lab to be 2.9 mmol/L. Allison understands that this level needs to be reported to the admitting physician. Utilizing an ISBARR format, what information should Allison be prepared to phone the physician?
Allison should be prepared to tell the physician her role on the unit and that she is calling to relate information on a critical lab value. She should describe information about the patient, including Mr. Daniel’s name, position on the unit, and a reminder of when the patient was admitted. She should provide a brief synopsis of the stability of the patient. If there is relevant information regarding allergies, this should be related at this time as well. The concern related to the lab value and any accompanying symptoms should also be described. Allison should provide insight into the current intake and output status, weight, cardiac rhythm, signs of edema, respiratory status, etc. Allison should outline her request related to orders for potassium replacement. When these orders are received from the provider, she must be sure to repeat back the order to confirm accuracy.
Allison is a new graduate nurse who is recently transitioned from her orientation period to her scheduled night shift work on a medical telemetry unit. She has a patient care assignment of six patients. Her patient, Mr. Daniels, was admitted from the ER at 2200 shortly before her shift began. He was transferred to the floor with a diagnosis of Heart Failure exacerbation. The patient was prescribed IV push furosemide for diuresis. It is now 0500 and the patient’s morning potassium level is reported from the lab to be 2.9 mmol/L. Allison understands that this level needs to be reported to the admitting physician. Utilizing an ISBARR format, what information should Allison be prepared to phone the physician?
Allison should be prepared to tell the physician her role on the unit and that she is calling to relate information on a critical lab value. She should describe information about the patient, including Mr. Daniel’s name, position on the unit, and a reminder of when the patient was admitted. She should provide a brief synopsis of the stability of the patient. If there is relevant information regarding allergies, this should be related at this time as well. The concern related to the lab value and any accompanying symptoms should also be described. Allison should provide insight into the current intake and output status, weight, cardiac rhythm, signs of edema, respiratory status, etc. Allison should outline her request related to orders for potassium replacement. When these orders are received from the provider, she must be sure to repeat back the order to confirm accuracy.
Learning Activities
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activities are provided as immediate feedback.)
Visit the TeamSTEPPS® Instructor Manual: Specialty Scenarios for multiple AHRQ scenarios requiring application of TeamSTEPPS® to patient scenarios.
Scenario 1
Read this scenario and answer the following questions.
Jill and Neil are both nurses working the same shift. Jill is responsible for patients in Rooms 1–6, and Neil is responsible for patients in Rooms 7–12. Over the course of their shift, both nurses routinely visit their patients’ rooms to take vitals and deliver medication.
On one of his rounds, Neil attends to his patient in Room 8. He reads the chart and notices Jill’s initials signaling that she had already checked on this patient. A bit confused, he continues on to his next patient. After another hour goes by, Neil returns to Room 8 and again notices Jill’s initials on the chart. Neil thinks to himself, “What is she doing? I’ve got it covered. She’s checking my work. She must think I’m incompetent.” Neil decides to approach Jill and see what is going on.
Questions:
a) What might have been the initial cause of the conflict?
b) What kind of conflict did it turn into?
c) If Neil provides Jill with a copy of the room assignments, would that resolve the conflict?
Scenario 2
Read this scenario and answer the following questions.
A nursing team is having a routine meeting. One of the nurses, Stephen, is at the end of a 12-hour shift, and another nurse, Tanya, is just beginning hers. Tanya is a senior nurse in the unit with over ten years’ experience on this specific unit. Stephen is new to the unit with fewer than three years’ experience in nursing. Tanya has been asked to present information to the team about effective time management on the unit. During Tanya’s presentation, Stephen is seen rolling his eyes and talking to other members of the team. Tanya breaks from her presentation and asks, “Stephen, do you have anything to add?” Stephen replies, “No, I just don’t know why we need to talk about this again.” Tanya chooses to avoid engaging with Stephen further and finishes her presentation. Stephen continues to be disruptive throughout the presentation.
After the meeting concludes, Tanya approaches Stephen and asks if he had anything to add from the meeting. Stephen replies, “No, I don’t have anything. I just think we all know what the procedure is because we just learned it all during orientation training. Maybe if you don’t remember the training, you should take it again.” Tanya is shocked by his reply and quickly composes herself. She states, “Stephen, I have worked on this unit for over ten years. I was asked to present that information because there are current issues going on among the staff. Next time please respect my authority and listen to those who come before you.”
Questions:
a) What types of conflict are present?
b) What will need to happen to resolve this issue between Tanya and Stephen?
c) Take a moment to think about what your preferred approach to conflict may be. How might you adapt your approach to conflict when working with others?
Scenario 3
Read this scenario and answer the following questions.
Connie, the head nurse on Unit 7, is a respected member of the team. She has been working on this unit for a number of years and is seen by the other nurses as the “go to” person for questions and guidance. Connie is always thorough with patients and demonstrates excellence and quality in her work. Dr. Smith is a well-respected member of the medical profession and an expert in his field of medicine. He has a reputation for excellent bedside manner and is thorough in his approach with patients.
Connie is four hours into her 12-hour shift when she is approached by Dr. Smith. He asks, “Connie, why has the patient in Room 2 not received his blood pressure medication over the past few days? I was not notified about this!”
Connie, trying to find a quick solution, replies, “I didn’t know that patient had been missing medication. I’ll go check on it and get back to you.”
Dr. Smith is persistent, saying, “You don’t need to go check anything. I know this patient and should have been informed about the withholding of medication and the reasons why.”
Connie, again attempting to find a resolution, states, “Well, there must be some communication about this change somewhere . . .”
“There isn’t!” Dr. Smith interrupts.
Connie becomes upset and decides to leave the conversation after declaring, “Fine, if you know everything, then you figure it out; you’re the one with the medical degree, aren’t you?” She storms off.
Connie makes her way to the nurses’ station where Dan and Elise are assessing charts and says to them, “You will not believe what Dr. Smith just said to me!”
Dan and Elise look shocked and ask “What?”
Connie explains, “Well, he thinks I don’t do my job, when really we nurses are the ones that keep this unit going. Who is he to question my ability to look after patients? I am the most knowledgeable person on this unit!”
Dan and Elise don’t know how to reply and decide to avoid the interaction with a simple, “Oh yeah.”
Meanwhile, Dr. Smith has made his way to the doctor’s lounge and finds his colleague Dr. Lee. Dr. Smith tells him, “That head nurse on Unit 7 is useless. She doesn’t know what she is doing and doesn’t understand that we must be informed about changes to our patients’ medications, does she?” Dr. Lee nods quickly and returns to reviewing his file.
About three hours later, Connie and Dr. Smith have each spoken to several people about the interaction. Connie bumps into another nurse, Jessie, one of her best friends. Connie pulls Jessie aside and says, “You will not believe what I just saw. I was going into the admin office to file my holiday requests and out of the corner of my eye, I saw Dr. Smith lurking around the corner, pretending to look at a chart, spying on me!”
“What? Are you serious? That’s not safe,” replies Jessie.
Connie is relieved that Jessie is taking her side—it makes her feel as if she is not going crazy. “Yeah, I’m really getting worried about this. First, that creep is accusing me of not doing my job, and then he is wasting his time spying on me. What a loser! Maybe what I should do is file a complaint. That’ll show the ‘big man’ that he isn’t that big around here and maybe take him down a notch.”
When Jessie gives her an apprehensive look, Connie continues, “Oh Jessie, don’t worry. I have a perfect record and this won’t affect me. Even if it does, I will have done something good for all the other nurses around here. It is the principle of the matter at this point.”
Meanwhile, Dr. Smith has run into an old classmate of his, Dr. Drucker, and says, “Wow! You got hired! So happy to have you in the hospital. I do need to tell you though to be careful of the head nurse on Unit 7 . . .” Dr. Smith describes his troubles with Connie and adds, “She’s a real snitch! She makes trouble out of nothing. I was reviewing a chart down the corridor from the admin office, minding my own business and actually getting my work done, when I saw her slip into the admin office to squeal about me to the top bosses! This is something that needs to be watched! We can’t have people reporting doctors to administration over nothing. I think I’m going to write her up and get a black mark on that perfect record of hers. I will be fine—everyone knows I’m right. There will be consequences for her.”
Questions:
a) Using the scenario above, identify the stages of the conflict escalation.
b) What suggestions might you give to Dan, Elise, Jessie, Dr. Lee, and Dr. Drucker about how to respond to Connie and Dr. Smith?
c) How do you think this conflict will be resolved?

Test your knowledge using this NCLEX Next Generation-style Case Study. You may reset and resubmit your answers to this question an unlimited number of times.[1]
Learning Activities
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activities are provided as immediate feedback.)
Visit the TeamSTEPPS® Instructor Manual: Specialty Scenarios for multiple AHRQ scenarios requiring application of TeamSTEPPS® to patient scenarios.
Scenario 1
Read this scenario and answer the following questions.
Jill and Neil are both nurses working the same shift. Jill is responsible for patients in Rooms 1–6, and Neil is responsible for patients in Rooms 7–12. Over the course of their shift, both nurses routinely visit their patients’ rooms to take vitals and deliver medication.
On one of his rounds, Neil attends to his patient in Room 8. He reads the chart and notices Jill’s initials signaling that she had already checked on this patient. A bit confused, he continues on to his next patient. After another hour goes by, Neil returns to Room 8 and again notices Jill’s initials on the chart. Neil thinks to himself, “What is she doing? I’ve got it covered. She’s checking my work. She must think I’m incompetent.” Neil decides to approach Jill and see what is going on.
Questions:
a) What might have been the initial cause of the conflict?
b) What kind of conflict did it turn into?
c) If Neil provides Jill with a copy of the room assignments, would that resolve the conflict?
Scenario 2
Read this scenario and answer the following questions.
A nursing team is having a routine meeting. One of the nurses, Stephen, is at the end of a 12-hour shift, and another nurse, Tanya, is just beginning hers. Tanya is a senior nurse in the unit with over ten years’ experience on this specific unit. Stephen is new to the unit with fewer than three years’ experience in nursing. Tanya has been asked to present information to the team about effective time management on the unit. During Tanya’s presentation, Stephen is seen rolling his eyes and talking to other members of the team. Tanya breaks from her presentation and asks, “Stephen, do you have anything to add?” Stephen replies, “No, I just don’t know why we need to talk about this again.” Tanya chooses to avoid engaging with Stephen further and finishes her presentation. Stephen continues to be disruptive throughout the presentation.
After the meeting concludes, Tanya approaches Stephen and asks if he had anything to add from the meeting. Stephen replies, “No, I don’t have anything. I just think we all know what the procedure is because we just learned it all during orientation training. Maybe if you don’t remember the training, you should take it again.” Tanya is shocked by his reply and quickly composes herself. She states, “Stephen, I have worked on this unit for over ten years. I was asked to present that information because there are current issues going on among the staff. Next time please respect my authority and listen to those who come before you.”
Questions:
a) What types of conflict are present?
b) What will need to happen to resolve this issue between Tanya and Stephen?
c) Take a moment to think about what your preferred approach to conflict may be. How might you adapt your approach to conflict when working with others?
Scenario 3
Read this scenario and answer the following questions.
Connie, the head nurse on Unit 7, is a respected member of the team. She has been working on this unit for a number of years and is seen by the other nurses as the “go to” person for questions and guidance. Connie is always thorough with patients and demonstrates excellence and quality in her work. Dr. Smith is a well-respected member of the medical profession and an expert in his field of medicine. He has a reputation for excellent bedside manner and is thorough in his approach with patients.
Connie is four hours into her 12-hour shift when she is approached by Dr. Smith. He asks, “Connie, why has the patient in Room 2 not received his blood pressure medication over the past few days? I was not notified about this!”
Connie, trying to find a quick solution, replies, “I didn’t know that patient had been missing medication. I’ll go check on it and get back to you.”
Dr. Smith is persistent, saying, “You don’t need to go check anything. I know this patient and should have been informed about the withholding of medication and the reasons why.”
Connie, again attempting to find a resolution, states, “Well, there must be some communication about this change somewhere . . .”
“There isn’t!” Dr. Smith interrupts.
Connie becomes upset and decides to leave the conversation after declaring, “Fine, if you know everything, then you figure it out; you’re the one with the medical degree, aren’t you?” She storms off.
Connie makes her way to the nurses’ station where Dan and Elise are assessing charts and says to them, “You will not believe what Dr. Smith just said to me!”
Dan and Elise look shocked and ask “What?”
Connie explains, “Well, he thinks I don’t do my job, when really we nurses are the ones that keep this unit going. Who is he to question my ability to look after patients? I am the most knowledgeable person on this unit!”
Dan and Elise don’t know how to reply and decide to avoid the interaction with a simple, “Oh yeah.”
Meanwhile, Dr. Smith has made his way to the doctor’s lounge and finds his colleague Dr. Lee. Dr. Smith tells him, “That head nurse on Unit 7 is useless. She doesn’t know what she is doing and doesn’t understand that we must be informed about changes to our patients’ medications, does she?” Dr. Lee nods quickly and returns to reviewing his file.
About three hours later, Connie and Dr. Smith have each spoken to several people about the interaction. Connie bumps into another nurse, Jessie, one of her best friends. Connie pulls Jessie aside and says, “You will not believe what I just saw. I was going into the admin office to file my holiday requests and out of the corner of my eye, I saw Dr. Smith lurking around the corner, pretending to look at a chart, spying on me!”
“What? Are you serious? That’s not safe,” replies Jessie.
Connie is relieved that Jessie is taking her side—it makes her feel as if she is not going crazy. “Yeah, I’m really getting worried about this. First, that creep is accusing me of not doing my job, and then he is wasting his time spying on me. What a loser! Maybe what I should do is file a complaint. That’ll show the ‘big man’ that he isn’t that big around here and maybe take him down a notch.”
When Jessie gives her an apprehensive look, Connie continues, “Oh Jessie, don’t worry. I have a perfect record and this won’t affect me. Even if it does, I will have done something good for all the other nurses around here. It is the principle of the matter at this point.”
Meanwhile, Dr. Smith has run into an old classmate of his, Dr. Drucker, and says, “Wow! You got hired! So happy to have you in the hospital. I do need to tell you though to be careful of the head nurse on Unit 7 . . .” Dr. Smith describes his troubles with Connie and adds, “She’s a real snitch! She makes trouble out of nothing. I was reviewing a chart down the corridor from the admin office, minding my own business and actually getting my work done, when I saw her slip into the admin office to squeal about me to the top bosses! This is something that needs to be watched! We can’t have people reporting doctors to administration over nothing. I think I’m going to write her up and get a black mark on that perfect record of hers. I will be fine—everyone knows I’m right. There will be consequences for her.”
Questions:
a) Using the scenario above, identify the stages of the conflict escalation.
b) What suggestions might you give to Dan, Elise, Jessie, Dr. Lee, and Dr. Drucker about how to respond to Connie and Dr. Smith?
c) How do you think this conflict will be resolved?

Test your knowledge using this NCLEX Next Generation-style Case Study. You may reset and resubmit your answers to this question an unlimited number of times.[2]
Admission: Refers to an initial visit or contact with a client.
Brief: A short session to share a plan, discuss team formation, assign roles and responsibilities, establish expectations and climate, and anticipate outcomes and contingencies.
Closed-loop communication: A communication strategy used to ensure that information conveyed by the sender is heard by the receiver and completed.
Communication conflict: Occurs when there is a failure in the exchange of information.
Continuity of care: The use of information on past events and personal circumstances to make current care appropriate for each individual.[3]
Cultural diversity: A term used to describe cultural differences among clients, family members, and health care team members.
Cultural humility: A humble and respectful attitude toward individuals of other cultures that pushes one to challenge their own cultural biases, realize they cannot possibly know everything about other cultures, and approach learning about other cultures as a lifelong goal and process.[4]
CUS statements: Assertive statements that are well-recognized by all staff across a health care agency as implementation of the two-challenge rule. These assertive statements are “I am Concerned - I am Uncomfortable - This is a Safety issue!”[5]
Debrief: An informal information exchange session designed to improve team performance and effectiveness through reinforcement of positive behaviors and reflecting on lessons learned after a significant event occurs.
DESC: A tool used to help resolve conflict. DESC is a mnemonic that stands for Describe the specific situation or behavior and provide concrete data, Express how the situation makes you feel/what your concerns are using “I” messages, Suggest other alternatives and seek agreement, and Consequences are stated in terms of impact on established team goals while striving for consensus.
Discharge: The completion of care and services in a health care facility and the client is sent home (or to another health care facility).
Ethical conflict: Occurs when individuals or groups have fundamentally different beliefs and values.
Feedback: Information is provided to a team member for the purpose of improving team performance. Feedback should be timely, respectful, specific, directed towards improvement, and considerate.[6]
Goal conflict: Happens when the objectives of individuals or groups are incompatible.
Handoff reports: A transfer and acceptance of patient care responsibility achieved through effective communication. It is a real-time process of passing patient specific information from one caregiver to another, or from one team of caregivers to another, for the purpose of ensuring the continuity and safety of the patient’s care.[7]
Horizontal aggression: Hostile behavior among one’s peers.
Huddle: A brief meeting during a shift to reestablish situational awareness, reinforce plans already in place, and adjust the teamwork plan as needed.
I’M SAFE: A tool used to assess one’s own safety status, as well as that of other team members in their ability to provide safe patient care. It is a mnemonic standing for personal safety risks as a result of Illness, Medication, Stress, Alcohol and Drugs, Fatigue, and Eating and Elimination.
Interdisciplinary care conferences: Meetings where interprofessional team members professionally collaborate, share their expertise, and plan collaborative interventions to meet client needs.
Interprofessional collaborative practice: Multiple health workers from different professional backgrounds working together with patients, families, caregivers, and communities to deliver the highest quality of care.
I-PASS: A mnemonic used as a structured communication tool among interprofessional team members. I-PASS stands for Illness severity, Patient summary, Action list, Situation awareness, and Synthesis by the receiver.
ISBARR: A mnemonic for the components of Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat back.[8],[9]
Mutual support: The ability to anticipate and support team members' needs through accurate knowledge about their responsibilities and workload.
Personality conflict: Arises from differences in individual temperaments, attitudes, and behaviors.
Role conflict: Arises when individuals have multiple, often conflicting, expectations associated with their roles.
Shared mental model: The actions of a team leader that ensure all team members have situation awareness and are "on the same page" as situations evolve on the unit.[10]
Situation awareness: The awareness of a team member knowing what is going on around them.[11]
Situation monitoring: The process of continually scanning and assessing the situation to gain and maintain an understanding of what is going on around you.[12]
STEP tool: A situation monitoring tool used to know what is going on with you, your patients, your team, and your environment. STEP stands for Status of the patients, Team members, Environment, and Progress Toward Goal.[13]
TeamSTEPPS®: An evidence-based framework used to optimize team performance across the health care system. It is a mnemonic standing for Team Strategies and Tools to Enhance Performance and Patient Safety.[14]
Two-challenge rule: A strategy for advocating for patient safety that includes a team member assertively voicing their concern at least two times to ensure that it has been heard by the decision-maker.
Admission: Refers to an initial visit or contact with a client.
Brief: A short session to share a plan, discuss team formation, assign roles and responsibilities, establish expectations and climate, and anticipate outcomes and contingencies.
Closed-loop communication: A communication strategy used to ensure that information conveyed by the sender is heard by the receiver and completed.
Communication conflict: Occurs when there is a failure in the exchange of information.
Continuity of care: The use of information on past events and personal circumstances to make current care appropriate for each individual.[15]
Cultural diversity: A term used to describe cultural differences among clients, family members, and health care team members.
Cultural humility: A humble and respectful attitude toward individuals of other cultures that pushes one to challenge their own cultural biases, realize they cannot possibly know everything about other cultures, and approach learning about other cultures as a lifelong goal and process.[16]
CUS statements: Assertive statements that are well-recognized by all staff across a health care agency as implementation of the two-challenge rule. These assertive statements are “I am Concerned - I am Uncomfortable - This is a Safety issue!”[17]
Debrief: An informal information exchange session designed to improve team performance and effectiveness through reinforcement of positive behaviors and reflecting on lessons learned after a significant event occurs.
DESC: A tool used to help resolve conflict. DESC is a mnemonic that stands for Describe the specific situation or behavior and provide concrete data, Express how the situation makes you feel/what your concerns are using “I” messages, Suggest other alternatives and seek agreement, and Consequences are stated in terms of impact on established team goals while striving for consensus.
Discharge: The completion of care and services in a health care facility and the client is sent home (or to another health care facility).
Ethical conflict: Occurs when individuals or groups have fundamentally different beliefs and values.
Feedback: Information is provided to a team member for the purpose of improving team performance. Feedback should be timely, respectful, specific, directed towards improvement, and considerate.[18]
Goal conflict: Happens when the objectives of individuals or groups are incompatible.
Handoff reports: A transfer and acceptance of patient care responsibility achieved through effective communication. It is a real-time process of passing patient specific information from one caregiver to another, or from one team of caregivers to another, for the purpose of ensuring the continuity and safety of the patient’s care.[19]
Horizontal aggression: Hostile behavior among one’s peers.
Huddle: A brief meeting during a shift to reestablish situational awareness, reinforce plans already in place, and adjust the teamwork plan as needed.
I’M SAFE: A tool used to assess one’s own safety status, as well as that of other team members in their ability to provide safe patient care. It is a mnemonic standing for personal safety risks as a result of Illness, Medication, Stress, Alcohol and Drugs, Fatigue, and Eating and Elimination.
Interdisciplinary care conferences: Meetings where interprofessional team members professionally collaborate, share their expertise, and plan collaborative interventions to meet client needs.
Interprofessional collaborative practice: Multiple health workers from different professional backgrounds working together with patients, families, caregivers, and communities to deliver the highest quality of care.
I-PASS: A mnemonic used as a structured communication tool among interprofessional team members. I-PASS stands for Illness severity, Patient summary, Action list, Situation awareness, and Synthesis by the receiver.
ISBARR: A mnemonic for the components of Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat back.[20],[21]
Mutual support: The ability to anticipate and support team members' needs through accurate knowledge about their responsibilities and workload.
Personality conflict: Arises from differences in individual temperaments, attitudes, and behaviors.
Role conflict: Arises when individuals have multiple, often conflicting, expectations associated with their roles.
Shared mental model: The actions of a team leader that ensure all team members have situation awareness and are "on the same page" as situations evolve on the unit.[22]
Situation awareness: The awareness of a team member knowing what is going on around them.[23]
Situation monitoring: The process of continually scanning and assessing the situation to gain and maintain an understanding of what is going on around you.[24]
STEP tool: A situation monitoring tool used to know what is going on with you, your patients, your team, and your environment. STEP stands for Status of the patients, Team members, Environment, and Progress Toward Goal.[25]
TeamSTEPPS®: An evidence-based framework used to optimize team performance across the health care system. It is a mnemonic standing for Team Strategies and Tools to Enhance Performance and Patient Safety.[26]
Two-challenge rule: A strategy for advocating for patient safety that includes a team member assertively voicing their concern at least two times to ensure that it has been heard by the decision-maker.

