6.2 Review of Anatomy and Physiology of the Respiratory System
Open Resources for Nursing (Open RN)
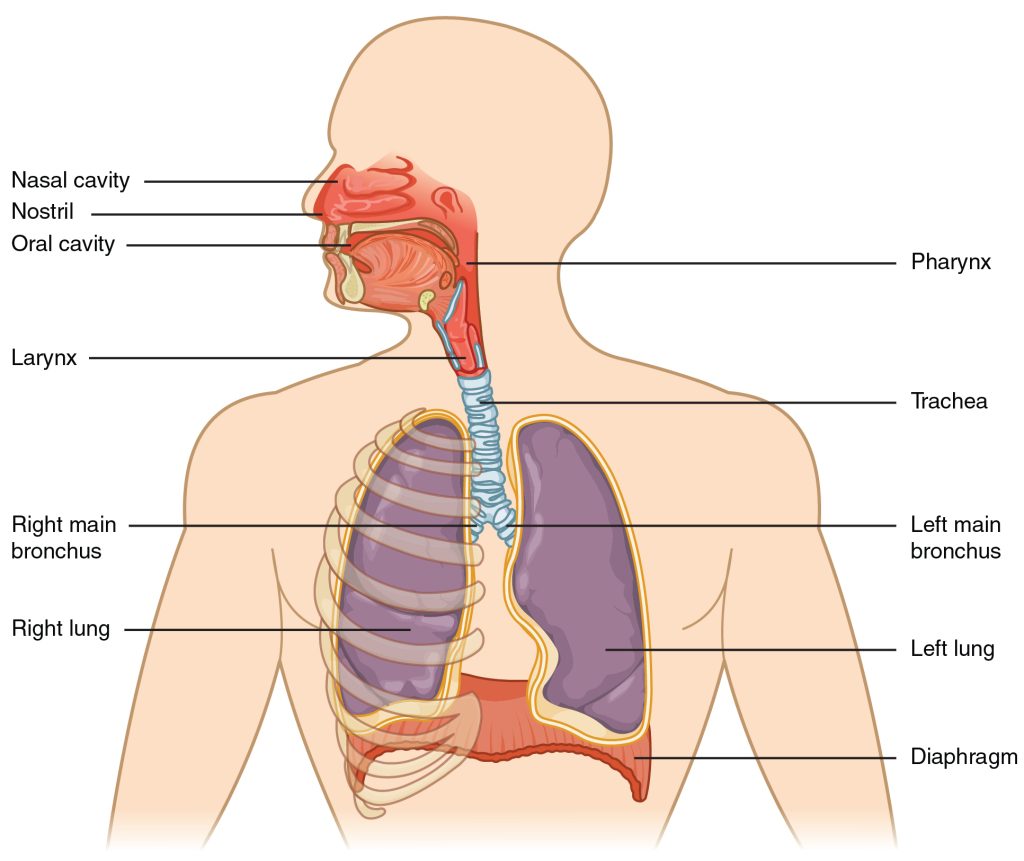
This section will review the anatomy and physiology of the respiratory system. Common disorders affecting these anatomic structures are also introduced. See Figure 6.1[1] for an illustration of the major structures of the respiratory system.
Nose, Nasal Cavity, and Sinuses
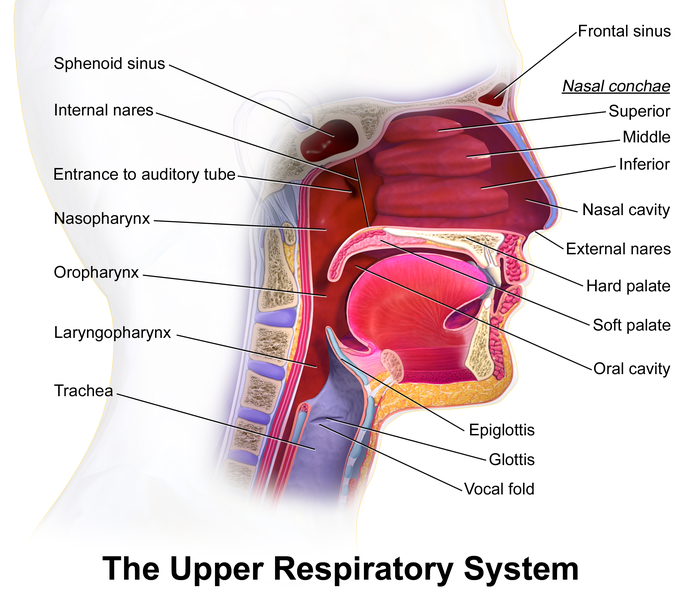
The upper respiratory system refers to the nose, nasal cavities, sinuses, pharynx, and larynx. See Figure 6.2[2] for an illustration of anatomic structures of the upper respiratory system. An upper respiratory infection (URI) refers to a viral infection of one or more of these structures.
The entrance and exit for the respiratory system are through the nose. The nostrils are the opening to the nose, also referred to as nares. The nares and nasal cavities are lined with mucous membranes, containing sebaceous glands and hair follicles that serve to prevent the passage of large debris, such as dirt, through the nasal cavity. Rhinorrhagia refers to bleeding from the nose, also called epistaxis. Rhinitis refers to inflammation of the nasal mucosa.
The nares open into the nasal cavity, which is separated into left and right sections by the nasal septum. The floor of the nasal cavity is composed of the hard palate and the soft palate. The nasal cavities are lined with mucous membranes that produce mucus, a substance created for lubrication and protection. Rhinorrhea, commonly referred to as a “runny nose,” is a medical term for excess mucus production by the nasal cavities.
Adjacent to the nasal cavity are the sinuses that serve to warm and humidify incoming air. There are four sinuses named for their adjacent bones: frontal sinus, maxillary sinus, sphenoidal sinus, and ethmoidal sinus. Air moves from the nasal cavities and sinuses into the pharynx. Sinusitis refers to inflammation of the sinus cavities.[3]
Pharynx
The pharynx, commonly known as the throat, is divided into three major regions: the nasopharynx, the oropharynx, and the laryngopharynx. See Figure 6.3[4] for an illustration of the regions of the pharynx.[5]
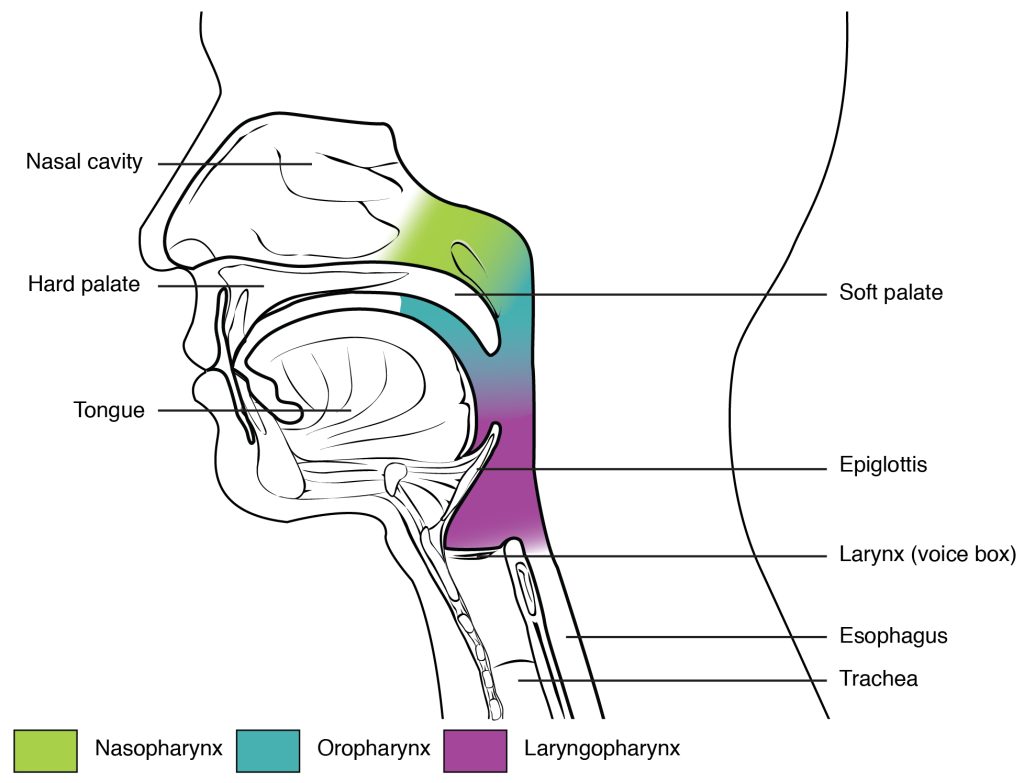
At the top of the nasopharynx is the pharyngeal tonsil, also called adenoid. The function of the pharyngeal tonsil is to trap and destroy invading pathogens that enter the airway during inhalation. Pharyngitis is inflammation of the pharynx, and tonsillitis is inflammation of the tonsils.[6]
The soft palate and a bulbous structure called the uvula swing upward during swallowing to close off the nasopharynx to prevent ingested materials from entering the nasal cavity. Eustachian tubes connect the middle ear cavities with the nasopharynx. This connection is why upper respiratory infections often lead to ear infections.[7]
The oropharynx is bordered superiorly by the nasopharynx and anteriorly by the oral cavity. The oropharynx contains two distinct sets of tonsils called the palatine tonsils and lingual tonsils that also trap and destroy pathogens entering the body through the oral or nasal cavities. Adenoids are lymphatic tissue between the back of the nasal cavity and the pharynx. Adenoiditis refers to inflammation of the adenoids, a common medical condition in young children that can hinder speaking and breathing.[8]
The laryngopharynx is just below the oropharynx. It is part of the pharynx (throat) located behind the larynx. The laryngopharynx separates into the trachea (the tube going into the larynx) and the esophagus (the tube going into the stomach). The epiglottis prevents food and fluid from entering the trachea while swallowing.[9]
Larynx
The structure of the larynx is formed by several pieces of cartilage, as shown in Figure 6.4.[10] Three large cartilage pieces form the major structure of the larynx called the thyroid cartilage (the larger piece of cartilage on the anterior side), epiglottis (at the top of the larynx), and cricoid cartilage (just inferior to the thyroid cartilage). Laryngitis refers to inflammation of the larynx, specifically the vocal cords, typically resulting in huskiness or loss of one’s voice and a cough.[11]
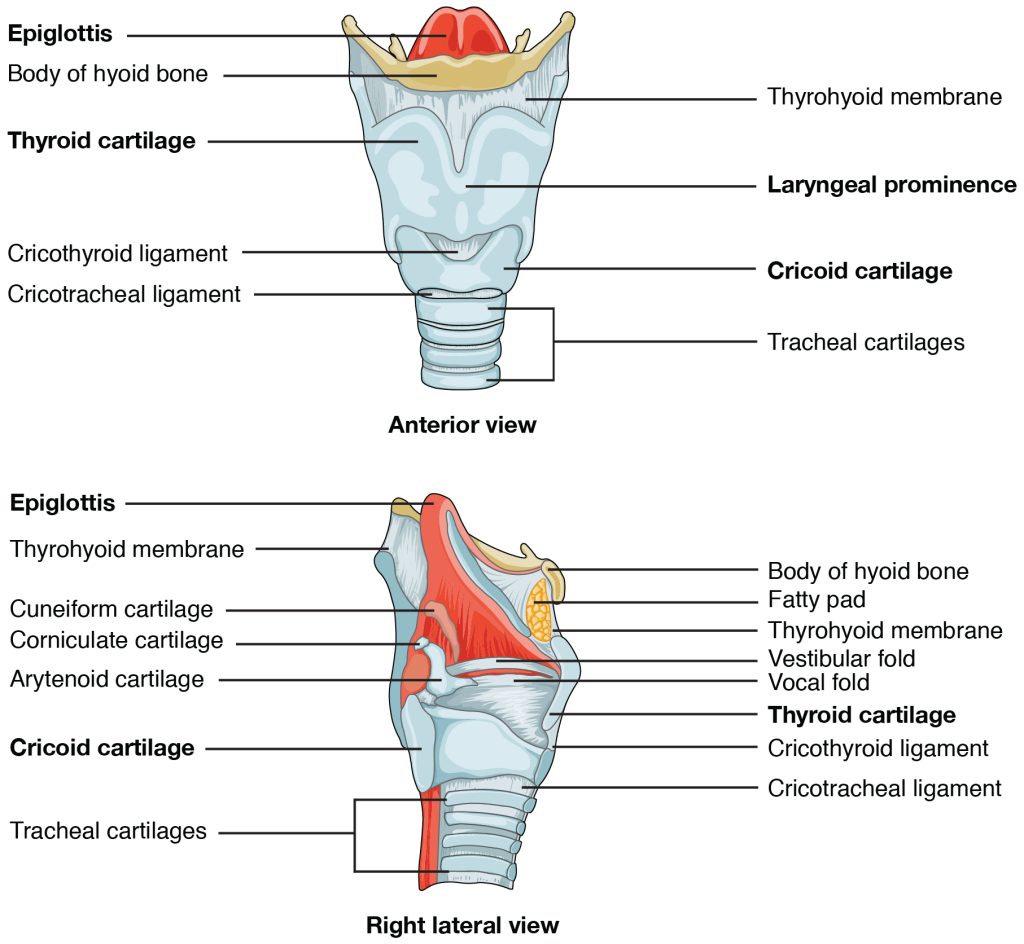
The epiglottis is a flap of tissue that covers the trachea during swallowing to prevent aspiration, the inhalation of food or fluids into the trachea and lower respiratory tract. The act of swallowing causes the pharynx and larynx to lift upward, allowing the pharynx to expand and the epiglottis of the larynx to swing downward, closing the opening to the trachea.[12]
Vocal cords are white, membranous folds attached by muscle to the cartilages of the larynx on their outer edges. The inner edges of the vocal cords are free, allowing oscillation as air passes through to produce sound for speaking.[13]
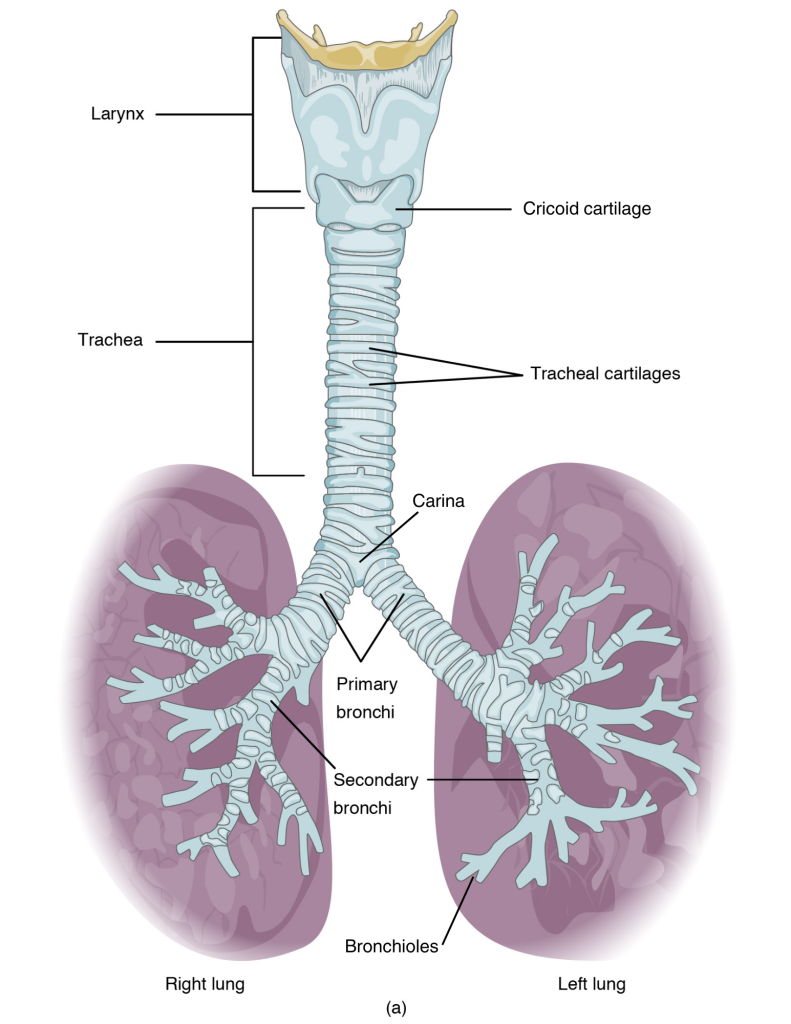
The lower respiratory tract consists of the trachea, bronchi, alveoli, and lungs.[14]
Trachea
The trachea is formed by stacked, C-shaped pieces of cartilage that are connected by dense connective tissue. See Figure 6.5[15] for an illustration of the trachea. The trachea stretches and expands slightly during inhalation and exhalation, whereas the rings of cartilage provide structural support and prevent the trachea from collapsing. The trachea is lined with cilia and mucus-secreting cells to trap debris and move it towards the pharynx to be swallowed or spit out.[16]
If the upper respiratory tract becomes blocked with mucus, inflammation, or a foreign object, no air can pass to the lungs, causing a life-threatening emergency requiring a tracheostomy. A tracheostomy is an incision created in the trachea to create an artificial opening to allow breathing when an obstruction is present.[17]
Bronchi and Bronchioles
Bronchi are the main air passageways of the lungs. The trachea branches into the right and left primary bronchi at the carina. The carina is a raised structure that contains specialized nervous system tissue that induces violent coughing if a foreign body, such as food, is present. Rings of cartilage, similar to those of the trachea, support the structure of the bronchi and prevent their collapse. The bronchi of each lung continue to branch up to 26 times creating the bronchial tree, which looks similar to the branching of an actual tree. The main function of the bronchi is to provide a passageway for air to move into and out of each lung.[18]
Bronchioles are the smallest branches of the bronchi that lead to the alveolar sacs. The muscular walls of these tiny bronchioles do not contain cartilage like those of the bronchi, so the muscular wall can change the size of the bronchioles to increase or decrease airflow to the alveoli. Bronchospasm is a symptom of many respiratory conditions that refers to a sudden constriction of the muscles in the walls of the bronchioles. Bronchitis refers to inflammation of the bronchi.[19]
The trachea, bronchi, and bronchioles are lined with mucous membranes that create mucus secretions that can be expelled through the mouth, also referred to as sputum.[20]
Alveoli
Alveoli are small, grape-like sacs where gas exchange occurs. See Figure 6.6[21] for an illustration of one alveolus surrounded by capillaries. The blue capillaries refer to deoxygenated blood transported to the lungs from the pulmonary artery, and the red capillaries refer to oxygenated blood that is being transported back to the heart via the pulmonary vein. Note in this case that a vein is carrying oxygenated blood. Veins always carry blood back to the heart, but most of the time, it is deoxygenated. However, in this case, the pulmonary vein is transporting blood that is oxygenated back to the heart because it is being transported from the lungs.[22]
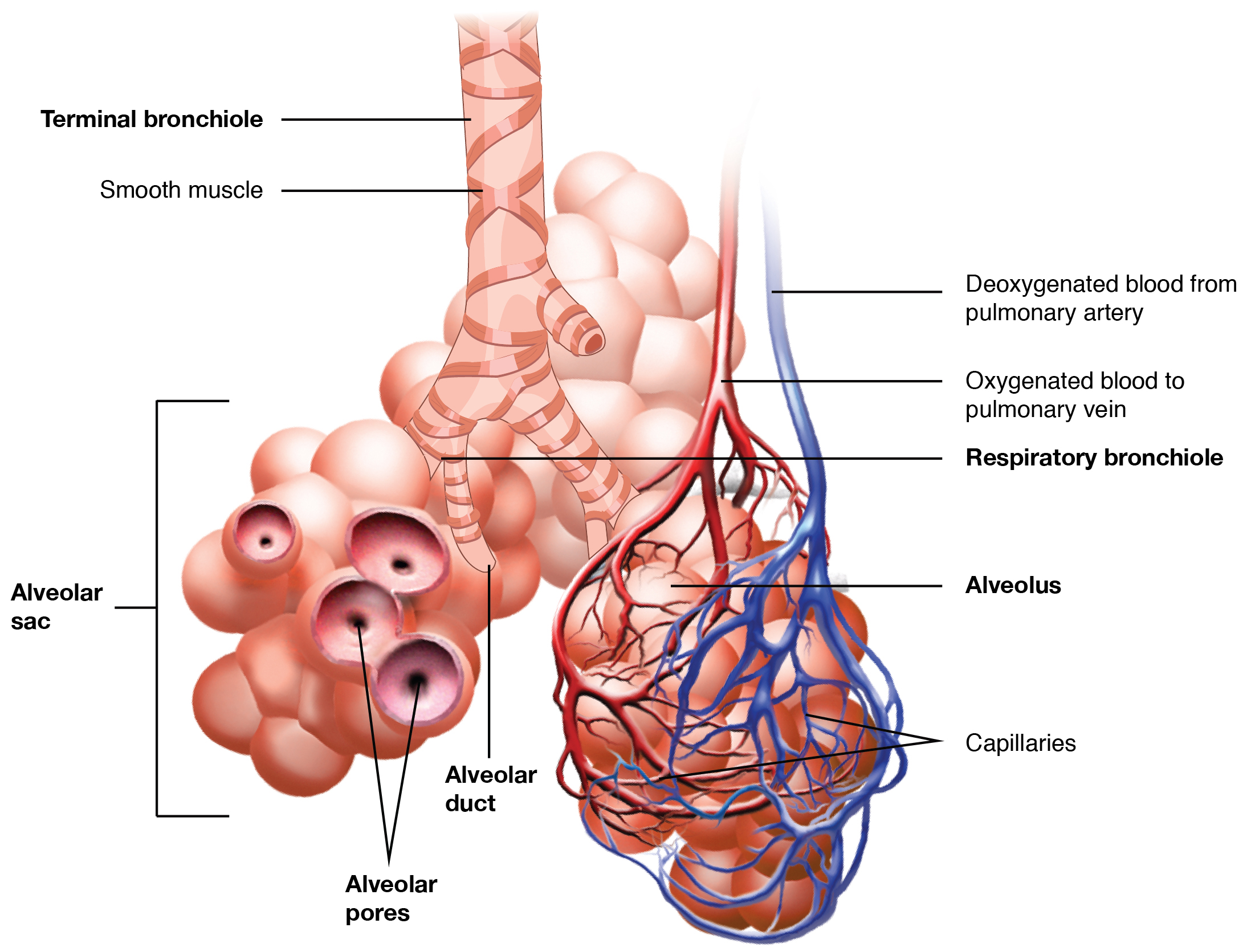
Alveoli have elastic walls that allow the alveolus to stretch during air intake, which greatly increases the surface area available for gas exchange. Alveoli secrete surfactant, a slippery substance that keeps the lungs from collapsing. Atelectasis is a medical term that refers to the collapse of alveoli and/or small passageways of the lungs that can result in a partially or completely collapsed lung.[23]
Lungs
The lungs are connected to the trachea by the main (primary) bronchi that branches into the right and left bronchi. See Figure 6.7[24] for an illustration of the lungs. On the inferior surface, the lungs are bordered by the diaphragm. The cardiac notch, a medial indentation found only on the left lung, allows space for the heart. The apex of the lung is the superior region, whereas the base is the distal region near the diaphragm.[25]
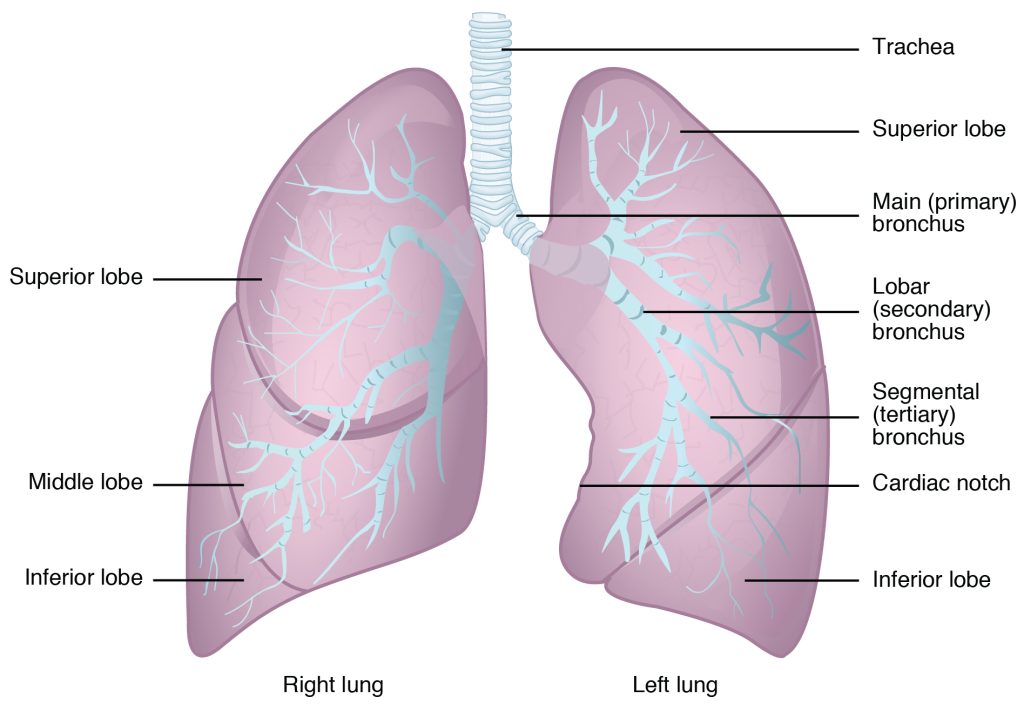
Each lung is composed of smaller units called lobes. The right lung consists of three lobes: the superior, middle, and inferior lobes. The left lung is smaller and only contains two lobes, superior and inferior, as it shares space with the heart. Each lobe receives its own large bronchus that has multiple branches. A lobectomy refers to surgical removal of a lobe of the lung.[26]
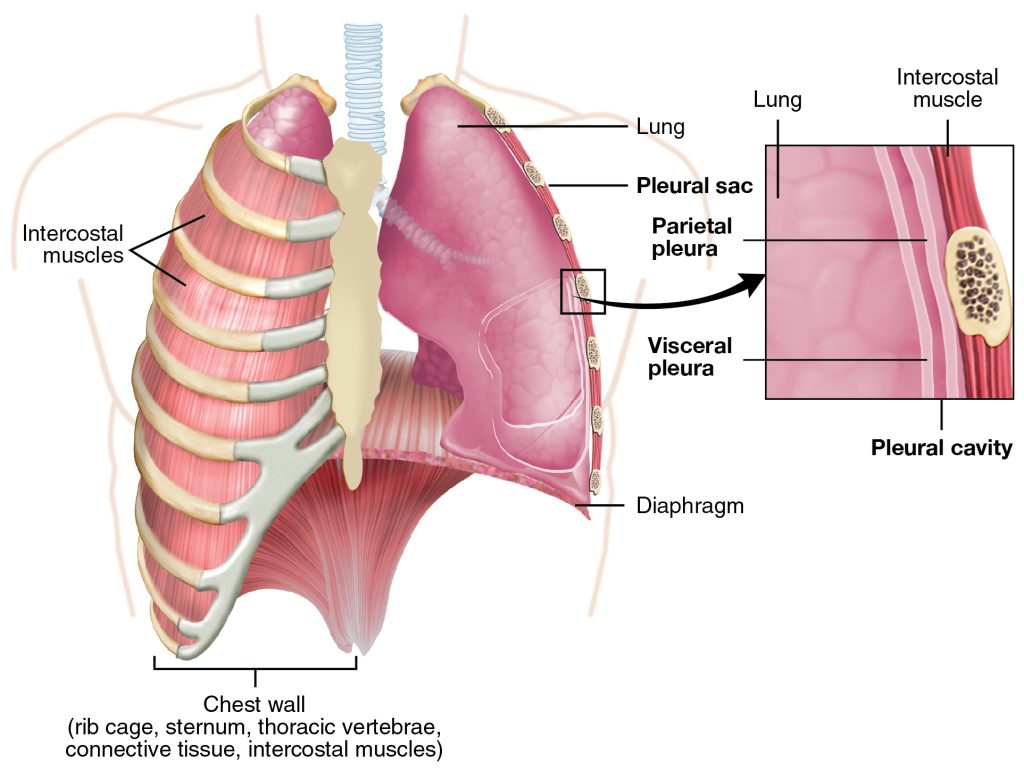
There are two pleural membranes in the lungs. The visceral pleura is a thin membrane on the outer surface of the lungs. The parietal pleura lines the inside of the thoracic cavity. Between these two membranes is the pleural cavity that contains pleural fluid to reduce friction and also sticks to the lungs to help keep them inflated. See Figure 6.8[27] for an illustration of the pleural membranes and the pleural cavity. Pleural effusion refers to excessive fluid between the pleural membranes that is commonly caused by disease or trauma.[28]
The main function of the respiratory system is gas exchange, meaning providing the body with a constant supply of oxygen to the body and removing carbon dioxide. To achieve gas exchange, the structures of the respiratory system create the mechanical movement of air into and out of the lungs called ventilation.[29]
Ventilation and the Mechanics of Breathing
The lungs bring oxygen to the cells of our body through inhalation and exhalation. Inhalation, also called inspiration, is the act of breathing air inward. During inhalation, the diaphragm contracts and flattens, creating a larger lung cavity, which decreases the pressure inside the lungs. At the same time, the intercostal muscles (the muscles between the ribs) pull downward, also causing the thoracic cavity to expand. The thoracic cavity is the space inside the chest that contains the heart, lungs, and other organs. As the thoracic cavity expands, a negative pressure (i.e., vacuum) is created inside the chest cavity, causing air to rush into the lungs (because air always moves from high pressure to low pressure).[30]
During exhalation, also called expiration or the act of breathing out, the diaphragm relaxes and the thoracic cavity springs back to its original position. This causes the volume of the thoracic cavity to decrease and pressure to increase, causing air to leave the lungs.
Lung sounds are caused by the movement of air from the trachea to the bronchioles to the alveoli and can be impacted by the presence of sputum, bronchoconstriction, or fluid in the alveoli. These sounds are referred to as rhonchi (coarse crackles), rales (fine crackles), wheezes, stridor, and pleural rub[31]:
- Rhonchi, also referred to as coarse crackles, are low-pitched, continuous sounds heard on expiration that are a sign of turbulent airflow through mucus in the large airways.
- Rales, also called fine crackles, are popping or crackling sounds heard on inspiration. They are associated with medical conditions that cause fluid accumulation within the alveolar and interstitial spaces, such as heart failure or pneumonia. The sound is similar to that produced by rubbing strands of hair together close to your ear.
- Wheezes are whistling noises produced when air is forced through airways narrowed by bronchoconstriction or mucosal edema. For example, clients with asthma commonly have wheezing.
- Stridor is heard only on inspiration. It is associated with obstruction of the trachea/upper airway.
- Pleural rub sounds like the rubbing together of leather and can be heard on inspiration and expiration. It is caused by inflammation of the pleura membranes that results in friction as the surfaces rub against each other.
Listen to lungs sounds in the “Respiratory Assessment” section of the “Respiratory Assessment” chapter of Open RN Nursing Skills, 2e.
Forced breathing is a type of breathing that can occur during exercise, singing, or playing a musical instrument. During forced breathing, inspiration and expiration both occur due to muscle contractions. In addition to the contraction of the diaphragm and intercostal muscles, other accessory muscles must also contract. Muscles of the neck contract and lift the thoracic wall, increasing lung volume, and accessory muscles of the abdomen contract, forcing abdominal organs upward against the diaphragm. This helps to push the diaphragm farther into the thorax, pushing out more air. In addition, accessory muscles help to compress the rib cage, which also reduces the volume of the thoracic cavity. These additional muscle contractions during inspiration also occur during labored breathing, a symptom of many respiratory disorders.[32]
Control of Breathing
Respiratory rate is the number of breaths taken per minute. The normal respiratory rate for adults is 12-20 breaths per minute. A child under 1 year of age has a normal respiratory rate between 30 and 60 breaths per minute. By the time a child is about eleven years old, the normal rate is closer to 14 to 22.
Respiratory rate may increase or decrease during illness or disease. Medical terms related to breathing include tachypnea (rapid breathing), bradypnea (slow breathing), and apnea (episodes of the absence of breathing). Dyspnea is a common symptom of respiratory disorders and refers to shortness of breath or a feeling of breathlessness.[33]
The respiratory rate is controlled by the respiratory center located within the medulla oblongata and pons in the brain stem, which responds primarily to changes in carbon dioxide, oxygen, and pH levels in the blood. These changes are sensed by central chemoreceptors, which are located in the brain, and peripheral chemoreceptors, which are located in the aortic arch and carotid arteries.
The major factor that drives breathing is not hypoxemia (a decreased amount of dissolved oxygen in the blood), but rather the concentration of carbon dioxide. Carbon dioxide is a waste product of cellular respiration and is toxic at high levels in the blood. Elevated levels of carbon dioxide are called hypercapnia. As carbon dioxide levels increase, the central chemoreceptors stimulate the contraction of the diaphragm and intercostal muscles, increasing the rate and depth of respirations to help rid the body of carbon dioxide. Hyperventilation refers to rapid and deep breathing. It can occur for many reasons such as anxiety and pain, but it can also be a sign the body is trying to compensate for acidosis and increasing the pH level by eliminating excess carbon dioxide.
In contrast, low levels of carbon dioxide in the blood stimulate shallow, slow breathing to help the body retain carbon dioxide. Hypoventilation refers to slow and shallow breathing.[34] Hypoventilation can occur for several reasons, such as oversedation by opioids and exhaustion from hyperventilation. It can also be a sign the body is trying to compensate for alkalosis by retaining carbon dioxide and decreasing the pH level.
Gas Exchange
Ventilation (i.e., the mechanics of breathing) provides air to the alveoli for gas exchange. Respiration refers to the exchange of gases in the lungs between the alveoli and the pulmonary capillaries or in the tissues between the systemic capillaries and cells/tissues.
Gas exchange refers to the exchange of oxygen and carbon dioxide through capillary walls of the alveoli and the pulmonary capillaries, called external respiration. During external respiration, oxygen from the air we breathe diffuses into the blood. Carbon dioxide (waste) diffuses out of the blood and into the alveoli where it can be exhaled. Throughout the rest of the body, gas exchange also occurs between the systemic capillaries and body cells/tissues, called internal respiration. During internal respiration, oxygen diffuses out of the systemic capillaries and body cells/tissues, and carbon dioxide diffuses from the cells/tissues into the systemic capillaries where it is carried to the lungs. It is through this process that cells in the body are oxygenated and carbon dioxide, the waste product of cellular respiration, is removed from the body.[35]
Perfusion
In addition to adequate ventilation, the second important aspect of gas exchange is perfusion. Perfusion refers to the flow of blood. In the lungs, perfusion occurs in the pulmonary circulation as it moves from the heart into the lungs and then back to the heart for distribution to the body. The pulmonary arteries carry deoxygenated blood from the heart into the lungs, where they branch and eventually become the capillary network composed of pulmonary capillaries. These pulmonary capillaries create the respiratory membrane with the alveoli. As the blood is pumped through this capillary network, gas exchange occurs.[36]
Although a small amount of the oxygen is able to dissolve directly into the blood from the alveoli, most of the oxygen binds to hemoglobin within the red blood cells. The more oxygen the hemoglobin in the red blood cells carry, the brighter red the color of the blood. Oxygenated blood returns to the heart through the pulmonary veins to the left atrium and ventricle, where it is pumped out to the body via the aorta. The hemoglobin on the red blood cells transports the oxygen to the tissues throughout the body.[37]
Hypoxia and Hypoxemia
Diseases and disorders affecting the respiratory system can cause hypoxia, defined as reduced tissue oxygenation. Hypoxia can occur due to inadequate ventilation or impaired perfusion, also referred to as V-Q mismatch, where the ratio of air ventilating the lungs’ alveoli (V) to blood perfusing through the surrounding capillaries (Q) is not properly matched.
Pulmonary edema is an example of hypoxia caused by inadequate ventilation due to fluid accumulation in alveoli, often caused by heart failure or kidney failure. As a result of the fluid accumulation, oxygen cannot move across the alveolar membrane into the blood, and carbon dioxide cannot be removed from the blood. As a result, hypoxia and hypercapnia (high levels of carbon dioxide) may occur, requiring urgent medical interventions to sustain life by decreasing carbon dioxide levels and increasing oxygen levels.[38]
Another example of hypoxia caused by impaired perfusion is a pulmonary embolism. Let’s take a closer look at pulmonary embolism in the box below.
Pulmonary Embolism
A pulmonary embolism (PE) can occur when a clot from elsewhere in the body travels through venous circulation and gets lodged in the blood vessels of the lungs. This impedes blood flow, and impacted lung tissue dies. PEs are medical emergencies that require emergent treatment. Diagnosis of pulmonary embolism involves various tests:
- CT pulmonary angiography (CTPA): Visualizes blood flow in the pulmonary arteries.
- D-dimer test: Detects the presence of a substance that may indicate the presence of a blood clot.
- Ultrasound: Checks for DVT in the legs.
- Ventilation-perfusion (V/Q) scan: Detects blood flow and air movement in the lungs.
Signs and symptoms of PE include sudden shortness of breath, sudden anxiety or feeling of “impending doom,” chest pain, rapid heart rate, coughing up blood, sweating, feeling lightheaded or dizzy, or leg swelling or pain if a DVT is present. Read more about DVT in the “Cardiovascular Alterations” chapter. Complications of PE include death of lung tissue, increased pulmonary pressure in the arteries of the lungs, and cardiac arrest. Rapid intervention is required if PE is suspected. Treatment includes blood thinners to prevent additional clotting, thrombolytic therapy to dissolve clots, inferior vena cava (IVC) filter to prevent clots traveling to the lungs, oxygen therapy, and supportive measures such as pain management and breathing exercises.[39]
The term hypoxia and hypoxemia are not synonymous. Whereas hypoxia refers to reduced tissue oxygenation, hypoxemia is defined as a decrease in the partial pressure of oxygen in the blood (PaO2). Hypoxemia can be caused by impaired delivery of oxygen to the tissues or defective utilization of oxygen by tissues. Additionally, hypoxemia and hypoxia do not always coexist. For example, clients can develop hypoxemia without hypoxia if there is a compensatory increase in their hemoglobin levels and/or cardiac output (CO).[40]
- “2301_Major_Respiratory_Organs.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- “Blausen_0872_UpperRespiratorySystem.png” by Blausen.com staff (2014). Medical gallery of Blausen Medical 2014 is licensed under CC BY 3.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- "2305_Divisions_of_the_Pharynx.jpg" by OpenStax College is licensed under CC BY 3.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- “2306_The_Larynx.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- “Trachea” by Meredith Pomietlo is a derivative of "File:2308a_The Trachea" by OpenStax Anatomy and Physiology and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- “2309_The_Respiratory_Zone” by OpenStax College is licensed under CC BY 3.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- “2312_Gross_Anatomy_of_the_Lungs.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- "2313_The_Lung_Pleurea.jpg" by OpenStax College is licensed under CC BY 3.0. ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Open RN Nursing Skills 2e by Chippewa Valley Technical College with CC BY 4.0 licensing. ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of Medical Terminology - 2e by Open RN and is licensed under CC BY 4.0 ↵
- Centers for Disease Control and Prevention. (2023, June 28). Venous thromboembolism. https://www.cdc.gov/ncbddd/dvt/facts.html ↵
- Sarkar, M., Niranjan, N., & Banyal, P. K. (2017). Mechanisms of hypoxemia. Lung India, 34(1), 47–60. https://doi.org/10.4103/0970-2113.197116 ↵
This textbook discusses professional and management concepts related to the role of a registered nurse (RN) as defined by the American Nurses Association (ANA). The ANA publishes two resources that set standards and guide professional nursing practice in the United States: The Code of Ethics for Nurses With Interpretive Statements and Nursing: Scope and Standards of Practice. The Code of Ethics for Nurses With Interpretive Statements establishes an ethical framework for nursing practice across all roles, levels, and settings and is discussed in greater detail in the “Ethical Practice” chapter of this book. The Nursing: Scope and Standards of Practice resource defines the “who, what, where, when, why, and how of nursing” and sets the standards for practice that all registered nurses are expected to perform competently.[1]
The ANA defines the “who” of nursing practice as the nurses who have been educated, titled, and maintain active licensure to practice nursing. The “what” of nursing is the recently revised ANA definition of nursing: “Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in recognition of the connection of all humanity.”[2] Simply put, nurses treat human responses to health problems and life processes and advocate for the care of others.
Nursing practice occurs “when'' there is a need for nursing knowledge, wisdom, caring, leadership, practice, or education, anytime, anywhere. Nursing practice occurs in any environment “where'' there is a health care consumer in need of care, information, or advocacy. The “why” of nursing practice is described as nursing’s response to the changing needs of society to achieve positive health care consumer outcomes in keeping with nursing’s social contract and obligation to society. The “how” of nursing practice is defined as the ways, means, methods, and manners that nurses use to practice professionally.[3] The “how” of nursing, also referred to as a nurse’s “scope and standards of practice,” is further defined by each state’s Nurse Practice Act; agency policies, procedures, and protocols; and federal regulations and ANA’s Standards of Practice.
State Boards of Nursing and Nurse Practice Acts
RNs must legally follow regulations set by the Nurse Practice Act by the state in which they are caring for patients with their nursing license. The Board of Nursing is the state-specific licensing and regulatory body that sets standards for safe nursing care and issues nursing licenses to qualified candidates based on the Nurse Practice Act. The Nurse Practice Act is enacted by that state’s legislature and defines the scope of nursing practice and establishes regulations for nursing practice within that state. If nurses do not follow the standards and scope of practice set forth by the Nurse Practice Act, they may be disciplined by the Board of Nursing in the form of reprimand, probation, suspension, or revocation of their nursing license. Investigations and discipline actions are reportable among states participating in the Nurse Licensure Compact (that allows nurses to practice across state lines) or when a nurse applies for licensure in a different state. The scope and standards of practice set forth in the Nurse Practice Act can also be used as evidence if a nurse is sued for malpractice.
Find your state's Nurse Practice Act on the National Council of State Board of Nursing (NCSBN) website.
Agency Policies, Procedures, and Protocols
In addition to practicing according to the Nurse Practice Act in the state they are employed, nurses must also practice according to agency policies, procedures, and protocols.
A policy is an expected course of action set by an agency. For example, hospitals set a policy requiring a thorough skin assessment to be completed when a patient is admitted and then reassessed and documented daily.
Agencies also establish their own set of procedures. A procedure is the method or defined steps for completing a task. For example, each agency has specific procedural steps for inserting a urinary catheter.
A protocol is a detailed, written plan for performing a regimen of therapy. For example, agencies typically establish a hypoglycemia protocol that nurses can independently and quickly implement when a patient’s blood sugar falls below a specific number without first calling a provider. A hypoglycemia protocol typically includes actions such as providing orange juice and rechecking the blood sugar and then reporting the incident to the provider.
Agency-specific policies, procedures, and protocols supersede the information taught in nursing school, and nurses can be held legally liable if they don’t follow them. It is vital for nurses to review and follow current agency-specific procedures, policies, and protocols while also practicing according to that state's nursing scope of practice. Malpractice cases have occurred when a nurse was asked by their employer to do something outside their legal scope of practice, impacting their nursing license. It is up to you to protect your nursing license and follow the Nurse Practice Act when providing patient care. If you have a concern about an agency’s policy, procedure, or protocol, follow the agency’s chain of command to report your concern.
Federal Regulations
Nursing practice is impacted by regulations enacted by federal agencies. Two examples of federal agencies setting standards of care are The Joint Commission and the Centers for Medicare and Medicaid Services.
The Joint Commission accredits and certifies over 20,000 health care organizations in the United States. The Joint Commission’s standards help health care organizations measure, assess, and improve performance on functions that are essential to providing safe, high-quality care. The standards are updated regularly to reflect the rapid advances in health care and address topics such as patient rights and education, infection control, medication management, and prevention of medical errors. The annual National Patient Safety Goals are also set by The Joint Commission after reviewing emerging patient safety issues.[4]
The Centers for Medicare & Medicaid Services (CMS) is an example of another federal agency that establishes regulations affecting nursing care. CMS is a part of the U.S. Department of Health and Human Services (HHS) that administers the Medicare program and works in partnership with state governments to administer Medicaid. The CMS establishes and enforces regulations to protect patient safety in hospitals that receive Medicare and Medicaid funding. For example, one CMS regulation often referred to as “checking the rights of medication administration” requires nurses to confirm specific information several times before medication is administered to a patient.[5]
Standards of Practice
The ANA defines Standards of Professional Nursing Practice as “authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently.”[6] These standards are classified into two categories: Standards of Practice and Standards of Professional Performance.
The ANA’s Standards of Practice describe a competent level of nursing practice as demonstrated by the critical thinking model known as the nursing process. The nursing process includes the components of assessment, diagnosis, outcomes identification, planning, implementation, and evaluation and forms the foundation of the nurse’s decision-making, practice, and provision of care.[7]
The ANA’s Standards of Professional Performance “describe a competent level of behavior in the professional role, including activities related to ethics, advocacy, respectful and equitable practice, communication, collaboration, leadership, education, scholarly inquiry, quality of practice, professional practice evaluation, resource stewardship, and environmental health. All registered nurses are expected to engage in professional role activities, including leadership, reflective of their education, position, and role.”[8] This book discusses content related to these professional practice standards. Each professional practice standard is defined in the following sections with information provided to related content in this book and the Open RN Nursing Fundamentals, 2e textbook.[9]
Ethics
The ANA’s Ethics standard states, “The registered nurse integrates ethics in all aspects of practice.”[10]
Advocacy
The ANA’s Advocacy standard states, “The registered nurse demonstrates advocacy in all roles and settings.”[11]
Respectful and Equitable Practice
The ANA’s Respectful and Equitable Practice standard states, “The registered nurse practices with cultural humility and inclusiveness.”
Communication
The ANA’s Communication standard states, “The registered nurse communicates effectively in all areas of professional practice.”[12]
Collaboration
The ANA’s Collaboration standard states, “The registered nurse collaborates with the health care consumer and other key stakeholders.”[13]
Leadership
The ANA’s Leadership standard states, “The registered nurse leads within the profession and practice setting.”[14]
Education
The ANA’s Education standard states, “The registered nurse seeks knowledge and competence that reflects current nursing practice and promotes futuristic thinking.”[15]
Scholarly Inquiry
The ANA’s Scholarly Inquiry standard states, “The registered nurse integrates scholarship, evidence, and research findings into practice.”[16]
Quality of Practice
The ANA’s Quality of Practice standard states, “The nurse contributes to quality nursing practice.”[17]
Professional Practice Evaluation
The ANA’s Professional Practice Evaluation standard states, “The registered nurse evaluates one’s own and others’ nursing practice.”[18]
Resource Stewardship
The ANA’s Resource Stewardship standard states, “The registered nurse utilizes appropriate resources to plan, provide, and sustain evidence-based nursing services that are safe, effective, financially responsible, and used judiciously.”[19]
Environmental Health
The ANA’s Environmental Health standard states, “The registered nurse practices in a manner that advances environmental safety and health.”[20]
This textbook discusses professional and management concepts related to the role of a registered nurse (RN) as defined by the American Nurses Association (ANA). The ANA publishes two resources that set standards and guide professional nursing practice in the United States: The Code of Ethics for Nurses With Interpretive Statements and Nursing: Scope and Standards of Practice. The Code of Ethics for Nurses With Interpretive Statements establishes an ethical framework for nursing practice across all roles, levels, and settings and is discussed in greater detail in the “Ethical Practice” chapter of this book. The Nursing: Scope and Standards of Practice resource defines the “who, what, where, when, why, and how of nursing” and sets the standards for practice that all registered nurses are expected to perform competently.[21]
The ANA defines the “who” of nursing practice as the nurses who have been educated, titled, and maintain active licensure to practice nursing. The “what” of nursing is the recently revised ANA definition of nursing: “Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in recognition of the connection of all humanity.”[22] Simply put, nurses treat human responses to health problems and life processes and advocate for the care of others.
Nursing practice occurs “when'' there is a need for nursing knowledge, wisdom, caring, leadership, practice, or education, anytime, anywhere. Nursing practice occurs in any environment “where'' there is a health care consumer in need of care, information, or advocacy. The “why” of nursing practice is described as nursing’s response to the changing needs of society to achieve positive health care consumer outcomes in keeping with nursing’s social contract and obligation to society. The “how” of nursing practice is defined as the ways, means, methods, and manners that nurses use to practice professionally.[23] The “how” of nursing, also referred to as a nurse’s “scope and standards of practice,” is further defined by each state’s Nurse Practice Act; agency policies, procedures, and protocols; and federal regulations and ANA’s Standards of Practice.
State Boards of Nursing and Nurse Practice Acts
RNs must legally follow regulations set by the Nurse Practice Act by the state in which they are caring for patients with their nursing license. The Board of Nursing is the state-specific licensing and regulatory body that sets standards for safe nursing care and issues nursing licenses to qualified candidates based on the Nurse Practice Act. The Nurse Practice Act is enacted by that state’s legislature and defines the scope of nursing practice and establishes regulations for nursing practice within that state. If nurses do not follow the standards and scope of practice set forth by the Nurse Practice Act, they may be disciplined by the Board of Nursing in the form of reprimand, probation, suspension, or revocation of their nursing license. Investigations and discipline actions are reportable among states participating in the Nurse Licensure Compact (that allows nurses to practice across state lines) or when a nurse applies for licensure in a different state. The scope and standards of practice set forth in the Nurse Practice Act can also be used as evidence if a nurse is sued for malpractice.
Find your state's Nurse Practice Act on the National Council of State Board of Nursing (NCSBN) website.
Read more about malpractice and protecting your nursing license in the “Legal Implications” chapter of this book.
Read Wisconsin’s Nurse Practice Act, Standards of Practice for Registered Nurses and Licensed Practical Nurses (Chapter N6) PDF, and Rules of Conduct (Chapter N7) PDF.
Agency Policies, Procedures, and Protocols
In addition to practicing according to the Nurse Practice Act in the state they are employed, nurses must also practice according to agency policies, procedures, and protocols.
A policy is an expected course of action set by an agency. For example, hospitals set a policy requiring a thorough skin assessment to be completed when a patient is admitted and then reassessed and documented daily.
Agencies also establish their own set of procedures. A procedure is the method or defined steps for completing a task. For example, each agency has specific procedural steps for inserting a urinary catheter.
A protocol is a detailed, written plan for performing a regimen of therapy. For example, agencies typically establish a hypoglycemia protocol that nurses can independently and quickly implement when a patient’s blood sugar falls below a specific number without first calling a provider. A hypoglycemia protocol typically includes actions such as providing orange juice and rechecking the blood sugar and then reporting the incident to the provider.
Agency-specific policies, procedures, and protocols supersede the information taught in nursing school, and nurses can be held legally liable if they don’t follow them. It is vital for nurses to review and follow current agency-specific procedures, policies, and protocols while also practicing according to that state's nursing scope of practice. Malpractice cases have occurred when a nurse was asked by their employer to do something outside their legal scope of practice, impacting their nursing license. It is up to you to protect your nursing license and follow the Nurse Practice Act when providing patient care. If you have a concern about an agency’s policy, procedure, or protocol, follow the agency’s chain of command to report your concern.
Federal Regulations
Nursing practice is impacted by regulations enacted by federal agencies. Two examples of federal agencies setting standards of care are The Joint Commission and the Centers for Medicare and Medicaid Services.
The Joint Commission accredits and certifies over 20,000 health care organizations in the United States. The Joint Commission’s standards help health care organizations measure, assess, and improve performance on functions that are essential to providing safe, high-quality care. The standards are updated regularly to reflect the rapid advances in health care and address topics such as patient rights and education, infection control, medication management, and prevention of medical errors. The annual National Patient Safety Goals are also set by The Joint Commission after reviewing emerging patient safety issues.[24]
The Centers for Medicare & Medicaid Services (CMS) is an example of another federal agency that establishes regulations affecting nursing care. CMS is a part of the U.S. Department of Health and Human Services (HHS) that administers the Medicare program and works in partnership with state governments to administer Medicaid. The CMS establishes and enforces regulations to protect patient safety in hospitals that receive Medicare and Medicaid funding. For example, one CMS regulation often referred to as “checking the rights of medication administration” requires nurses to confirm specific information several times before medication is administered to a patient.[25]
Standards of Practice
The ANA defines Standards of Professional Nursing Practice as “authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently.”[26] These standards are classified into two categories: Standards of Practice and Standards of Professional Performance.
The ANA’s Standards of Practice describe a competent level of nursing practice as demonstrated by the critical thinking model known as the nursing process. The nursing process includes the components of assessment, diagnosis, outcomes identification, planning, implementation, and evaluation and forms the foundation of the nurse’s decision-making, practice, and provision of care.[27]
Read more information about the nursing process in the “Nursing Process” chapter of Open RN Nursing Fundamentals, 2e.[28]
The ANA’s Standards of Professional Performance “describe a competent level of behavior in the professional role, including activities related to ethics, advocacy, respectful and equitable practice, communication, collaboration, leadership, education, scholarly inquiry, quality of practice, professional practice evaluation, resource stewardship, and environmental health. All registered nurses are expected to engage in professional role activities, including leadership, reflective of their education, position, and role.”[29] This book discusses content related to these professional practice standards. Each professional practice standard is defined in the following sections with information provided to related content in this book and the Open RN Nursing Fundamentals, 2e textbook.[30]
Ethics
The ANA’s Ethics standard states, “The registered nurse integrates ethics in all aspects of practice.”[31]
Read about ethical nursing practice in the “Ethical Practice” chapter of this book.
Advocacy
The ANA’s Advocacy standard states, “The registered nurse demonstrates advocacy in all roles and settings.”[32]
Read about nurse advocacy in the “Advocacy” chapter of this book.
Respectful and Equitable Practice
The ANA’s Respectful and Equitable Practice standard states, “The registered nurse practices with cultural humility and inclusiveness.”
Read about cultural humility and culturally responsive care in the “Diverse Patients” chapter in Open RN Nursing Fundamentals, 2e.[33]
Communication
The ANA’s Communication standard states, “The registered nurse communicates effectively in all areas of professional practice.”[34]
Read about communicating with clients and team members in the “Communication” chapter in Open RN Nursing Fundamentals, 2e.[35]
Read about interprofessional communication strategies that promote patient safety in the “Collaboration Within the Interprofessional Team” chapter of this book.
Collaboration
The ANA’s Collaboration standard states, “The registered nurse collaborates with the health care consumer and other key stakeholders.”[36]
Read about strategies to enhance the performance of the interprofessional team and manage conflict in the “Collaboration Within the Interprofessional Team” chapter of this book.
Leadership
The ANA’s Leadership standard states, “The registered nurse leads within the profession and practice setting.”[37]
Read about leadership, management, and implementing change in the “Leadership and Management” chapter of this book.
Read about assigning, delegating, and supervising patient care in the “Delegation and Supervision” chapter of this book.
Read about tools for prioritizing patient care and managing resources for the nursing team in the “Prioritization” chapter of this book.
Education
The ANA’s Education standard states, “The registered nurse seeks knowledge and competence that reflects current nursing practice and promotes futuristic thinking.”[38]
Read about professional development and specialty certification in the “Preparation for the RN Role” chapter of this book.
Scholarly Inquiry
The ANA’s Scholarly Inquiry standard states, “The registered nurse integrates scholarship, evidence, and research findings into practice.”[39]
Read about integrating evidence-based practice into one’s nursing practice in the “Quality and Evidence-Based Practice” chapter of this book.
Quality of Practice
The ANA’s Quality of Practice standard states, “The nurse contributes to quality nursing practice.”[40]
Read about improving quality patient care and participating in quality improvement initiatives in the “Quality and Evidence-Based Practice” chapter of this book.
Professional Practice Evaluation
The ANA’s Professional Practice Evaluation standard states, “The registered nurse evaluates one’s own and others’ nursing practice.”[41]
Read about nursing practice within the legal framework of health care, negligence, malpractice, and protecting your nursing license in the “Legal Implications” chapter of this book.
Read about reviewing the interprofessional team’s performance, providing constructive feedback, and advocating for patient safety with assertive statements in the “Collaboration Within the Interprofessional Team” chapter of this book.
Resource Stewardship
The ANA’s Resource Stewardship standard states, “The registered nurse utilizes appropriate resources to plan, provide, and sustain evidence-based nursing services that are safe, effective, financially responsible, and used judiciously.”[42]
Read more about health care funding, reimbursement models, budgets and staffing, and resource stewardship in the “Health Care Economics” chapter of this book.
Environmental Health
The ANA’s Environmental Health standard states, “The registered nurse practices in a manner that advances environmental safety and health.”[43]
Read about promoting workplace safety for nurses in the “Safety” chapter in Open RN Nursing Fundamentals, 2e.[44]
Read about fostering a professional environment that does not tolerate abusive behaviors in the “Collaboration Within the Interprofessional Team” chapter of this book.
Read about addressing the impacts of social determinants of health in the “Advocacy” chapter of this book.
“So much to do, so little time.” This is a common mantra of today’s practicing nurse in various health care settings. Whether practicing in acute inpatient care, long-term care, clinics, home care, or other agencies, nurses may feel there is "not enough of them to go around.”
The health care system faces a significant challenge in balancing the ever-expanding task of meeting patient care needs with scarce nursing resources that has even worsened as a result of the COVID-19 pandemic. Many health care organizations have seen exacerbation in nurse turnover post-pandemic as nurses struggle with increasing stress, burnout, and feeling of uncertainty within the profession.[45] A recent nursing survey done by the American Nurses Foundation found that 60% of nurses reported extremely stressful, violent, and traumatic events as a result of the COVID-19 pandemic.[46] Additionally, a staggering 89% of nurses reported that their organizations experience significant staffing shortages.[47]
With a limited supply of registered nurses, nurse managers are often challenged to implement creative staffing practices such as sending staff to units where they do not normally work (i.e., floating), implementing mandatory staffing and/or overtime, utilizing travel nurses, or using other practices to meet patient care demands.[48] Staffing strategies can result in nurses experiencing increased patient assignments and workloads, extended shifts, or temporary suspension of paid time off. Nurses may receive a barrage of calls and text messages offering “extra shifts” and bonus pay, and although the extra pay may be welcomed, they often eventually feel burnt out trying to meet the ever-expanding demands of the patient-care environment.
A novice nurse who is still learning how to navigate the complex health care environment and provide optimal patient care may feel overwhelmed by these conditions. Novice nurses frequently report increased levels of stress and disillusionment as they transition to the reality of the nursing role.[49] How can we address this professional dilemma and enhance the novice nurse's successful role transition to practice? The novice nurse must enter the profession with purposeful tools and strategies to help prioritize tasks and manage time so they can confidently address patient care needs, balance role demands, and manage day-to-day nursing activities.
Let’s take a closer look at the foundational concepts related to prioritization and time management in the nursing profession.
Assessment of reflexes is not typically performed by registered nurses as part of a routine nursing neurological assessment of adult patients, but it is used in nursing specialty units and in advanced practice. Spinal cord injuries, neuromuscular diseases, or diseases of the lower motor neuron tract can cause weak or absent reflexes. To perform deep reflex tendon testing, place the patient in a seated position. Use a reflex hammer in a quick striking motion by the wrist on various tendons to produce an involuntary response. Before classifying a reflex as absent or weak, the test should be repeated after the patient is encouraged to relax because voluntary tensing of the muscles can prevent an involuntary reflexive action.
Reflexes are graded from 0 to 4+, with "2+" considered normal:
- 0: Absent
- 1+: Hypoactive
- 2+: Normal
- 3+: Hyperactive without clonus
- 4+: Hyperactive with clonus (involuntary muscle contraction)
To observe assessment of deep tendon reflexes, view the following video.
View Stanford Medicine's Assessment of Deep Tendon Reflexes video on YouTube.[50]
Brachioradialis Reflex
The brachioradialis reflex is used to assess the cervical spine nerves C5 and C6. Ask the patient to support their arm on their thigh or on your hand. Identify the insertion of the brachioradialis tendon on the radius and briskly tap it with the reflex hammer. The reflex consists of flexion and supination of the forearm. See Figure 6.37[51] for an image of obtaining the brachioradialis reflex.

Triceps Reflex
The triceps reflex assesses cervical spine nerves C6 and C7. Support the patient’s arm underneath their bicep to maintain a position midway between flexion and extension. Ask the patient to relax their arm and allow it to fully be supported by your hand. Identify the triceps tendon posteriorly just above its insertion on the olecranon. Tap briskly on the tendon with the reflex hammer. Note extension of the forearm. See Figure 6.38[52] for an image of the triceps reflex exam.

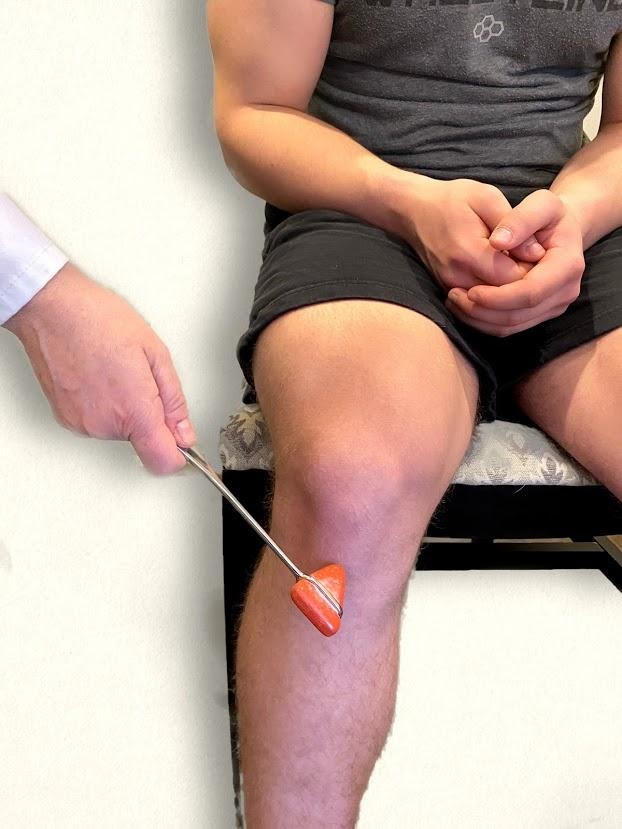
Patella (Knee Jerk) Reflex
The patellar reflex, commonly referred to as the knee jerk test, assesses lumbar spine nerves L2, L3, and L4. Ask the patient to relax the leg and allow it to swing freely at the knee. Tap the patella tendon briskly, looking for extension of the lower leg. See Figure 6.39[53] for an image of assessing a patellar reflex.
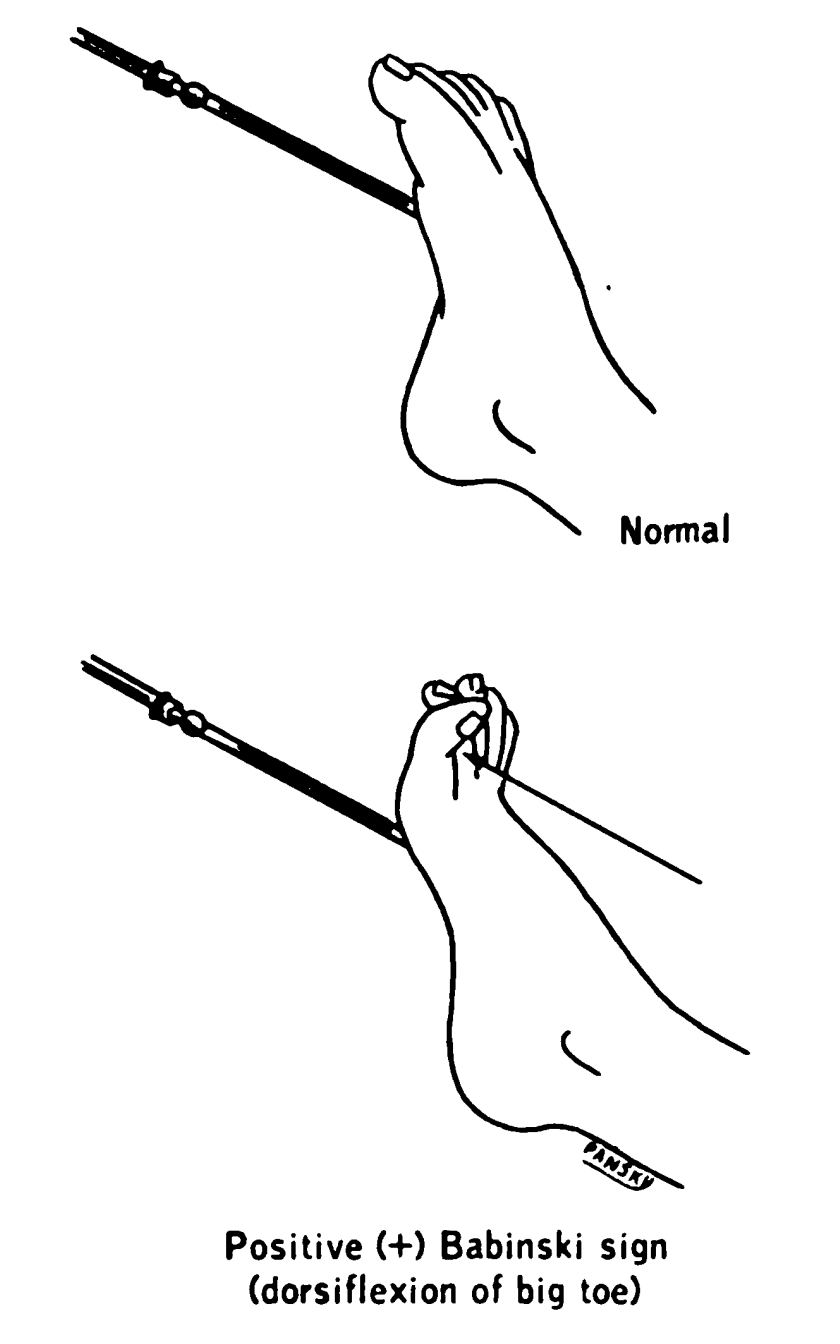
Plantar Reflex
The plantar reflex, or "Babinski reflex" assesses lumbar spine L5 and sacral spine S1. Ask the patient to extend their lower leg, and then stabilize their foot in the air with your hand. Slide the object along the lateral surface of the sole of the foot toward the toes. Many patients are ticklish and withdraw their foot, so it is sufficient to elicit the reflex by using your thumb to stroke lightly from the sole of the foot toward the toes. If there is no response, use a blunt object such as a key or pen. The expected reflex is flexion (i.e., bending) of the great toe. An abnormal response is toe extension (i.e., straightening), also known as the Babinski reflex. In a child younger than 2 years old, the big toe should bend up and backward toward the top of your foot while the other four toes fan out. This response is normal and doesn’t indicate any problems or abnormalities. In a child older than 2 years old or in a mature adult, the Babinski sign should be absent. All five toes should flex, or curl downward, as if they’re trying to grab something. If this test is conducted on a child older than 2 or an adult and the toes respond like those of a child under two years old, this can indicate an underlying neurological issue. See Figures 6.40 - 6.43[54],[55],[56],[57] for images of assessing the plantar reflex.



Newborn Reflexes
Newborn reflexes originate in the central nervous system and are exhibited by infants at birth but disappear as part of child development. Neurological disease or delayed development is indicated if these reflexes are not present at birth, do not spontaneously resolve, or reappear in adulthood. Common newborn reflexes include sucking, rooting, palmar grasp, plantar grasp, Babinski, Moro, and tonic neck reflexes.
Sucking Reflex
The sucking reflex is common to all mammals and is present at birth. It is linked with the rooting reflex and breastfeeding. It causes the child to instinctively suck anything that touches the roof of their mouth and simulates the way a child naturally eats. See Figure 6.44[60] for an image of the newborn sucking reflex.

Rooting Reflex
The rooting reflex assists in the act of breastfeeding. A newborn infant will turn its head toward anything that strokes its cheek or mouth, searching for the object by moving its head in steadily decreasing arcs until the object is found. See Figure 6.45[61] for an image of a newborn exhibiting the rooting reflex.

Palmar and Plantar Grasps
When an object is placed in an infant's hand and the palm of the child is stroked, the fingers will close reflexively, referred to as the palmar grasp reflex. A similar reflexive action occurs if an object is placed on the plantar surface of an infant’s foot, referred to as the plantar grasp reflex. See Figure 6.46[62] for an image of the palmar grasp reflex.

Moro Reflex
The Moro reflex is present at birth and is often stimulated by a loud noise. The Moro reflex occurs when the legs and head of the infant extend while the arms jerk up and out with the palms up. See Figure 6.47[63] for an image of an infant exhibiting the Moro reflex.

Tonic Neck Reflex
The asymmetrical tonic neck reflex, also known as the “fencing posture,” occurs when the child's head is turned to the side. The arm on the same side as the head is turned will straighten and the opposite arm will bend. See Figure 6.48[64] for an image of the tonic neck reflex.

Walking-Stepping Reflex
Although infants cannot support their own weight, when the soles of their feet touch a surface, it appears as if they are attempting to walk by placing one foot in front of the other foot.
Prioritization
As new nurses begin their career, they look forward to caring for others, promoting health, and saving lives. However, when entering the health care environment, they often discover there are numerous and competing demands for their time and attention. Patient care is often interrupted by call lights, rounding physicians, and phone calls from the laboratory department or other interprofessional team members. Even individuals who are strategic and energized in their planning can feel frustrated as their task lists and planned patient-care activities build into a long collection of “to dos.”
Without utilization of appropriate prioritization strategies, nurses can experience time scarcity, a feeling of racing against a clock that is continually working against them. Functioning under the burden of time scarcity can cause feelings of frustration, inadequacy, and eventually burnout. Time scarcity can also impact patient safety, resulting in adverse events and increased mortality.[65] Additionally, missed or rushed nursing activities can negatively impact patient satisfaction scores that ultimately affect an institution's reimbursement levels.
It is vital for nurses to plan patient care and implement their task lists while ensuring that critical interventions are safely implemented first. Identifying priority patient problems and implementing priority interventions are skills that require ongoing cultivation as one gains experience in the practice environment.[66] To develop these skills, students must develop an understanding of organizing frameworks and prioritization processes for delineating care needs. These frameworks provide structure and guidance for meeting the multiple and ever-changing demands in the complex health care environment.
Let’s consider a clinical scenario in the following box to better understand the implications of prioritization and outcomes.
Scenario A
Imagine you are beginning your shift on a busy medical-surgical unit. You receive a handoff report on four medical-surgical patients from the night shift nurse:
- Patient A is a 34-year-old total knee replacement patient, post-op Day 1, who had an uneventful night. It is anticipated that she will be discharged today and needs patient education for self-care at home.
- Patient B is a 67-year-old male admitted with weakness, confusion, and a suspected urinary tract infection. He has been restless and attempting to get out of bed throughout the night. He has a bed alarm in place.
- Patient C is a 49-year-old male, post-op Day 1 for a total hip replacement. He has been frequently using his patient-controlled analgesia (PCA) pump and last rated his pain as a "6."
- Patient D is a 73-year-old male admitted for pneumonia. He has been hospitalized for three days and receiving intravenous (IV) antibiotics. His next dose is due in an hour. His oxygen requirements have decreased from 4 L/minute of oxygen by nasal cannula to 2 L/minute by nasal cannula.
Based on the handoff report you received, you ask the nursing assistant to check on Patient B while you do an initial assessment on Patient D. As you are assessing Patient D's oxygenation status, you receive a phone call from the laboratory department relating a critical lab value on Patient C, indicating his hemoglobin is low. The provider calls and orders a STAT blood transfusion for Patient C. Patient A rings the call light and states she and her husband have questions about her discharge and are ready to go home. The nursing assistant finds you and reports that Patient B got out of bed and experienced a fall during the handoff reports.
It is common for nurses to manage multiple and ever-changing tasks and activities like this scenario, illustrating the importance of self-organization and priority setting. This chapter will further discuss the tools nurses can use for prioritization.
Prioritization of care for multiple patients while also performing daily nursing tasks can feel overwhelming in today’s fast-paced health care system. Because of the rapid and ever-changing conditions of patients and the structure of one’s workday, nurses must use organizational frameworks to prioritize actions and interventions. These frameworks can help ease anxiety, enhance personal organization and confidence, and ensure patient safety.
Acuity
Acuity and intensity are foundational concepts for prioritizing nursing care and interventions. Acuity refers to the level of patient care that is required based on the severity of a patient’s illness or condition. For example, acuity may include characteristics such as unstable vital signs, oxygenation therapy, high-risk IV medications, multiple drainage devices, or uncontrolled pain. A "high-acuity" patient requires several nursing interventions and frequent nursing assessments.
Intensity addresses the time needed to complete nursing care and interventions such as providing assistance with activities of daily living (ADLs), performing wound care, or administering several medication passes. For example, a "high-intensity" patient generally requires frequent or long periods of psychosocial, educational, or hygiene care from nursing staff members. High-intensity patients may also have increased needs for safety monitoring, familial support, or other needs.[67]
Many health care organizations structure their staffing assignments based on acuity and intensity ratings to help provide equity in staff assignments. Acuity helps to ensure that nursing care is strategically divided among nursing staff. An equitable assignment of patients benefits both the nurse and patient by helping to ensure that patient care needs do not overwhelm individual staff and safe care is provided.
Organizations use a variety of systems when determining patient acuity with rating scales based on nursing care delivery, patient stability, and care needs. See an example of a patient acuity tool published in the American Nurse in Table 2.3.[68] In this example, ratings range from 1 to 4, with a rating of 1 indicating a relatively stable patient requiring minimal individualized nursing care and intervention. A rating of 2 reflects a patient with a moderate risk who may require more frequent intervention or assessment. A rating of 3 is attributed to a complex patient who requires frequent intervention and assessment. This patient might also be a new admission or someone who is confused and requires more direct observation. A rating of 4 reflects a high-risk patient. For example, this individual may be experiencing frequent changes in vital signs, may require complex interventions such as the administration of blood transfusions, or may be experiencing significant uncontrolled pain. An individual with a rating of 4 requires more direct nursing care and intervention than a patient with a rating of 1 or 2.[69]
Table 2.3. Example of a Patient Acuity Tool[70]
| 1: Stable Patient | 2: Moderate-Risk Patient | 3: Complex Patient | 4: High-Risk Patient | |
|---|---|---|---|---|
| Assessment |
|
|
|
|
| Respiratory |
|
|
|
|
| Cardiac |
|
|
|
|
| Medications |
|
|
|
|
| Drainage Devices |
|
|
|
|
| Pain Management |
|
|
|
|
| Admit/Transfer/Discharge |
|
|
|
|
| ADLs and Isolation |
|
|
|
|
| Patient Score | Most = 1 | Two or > = 2 | Any = 3 | Any = 4 |
Read more about using a patient acuity tool on a medical-surgical unit.
Rating scales may vary among institutions, but the principles of the rating system remain the same. Organizations include various patient care elements when constructing their staffing plans for each unit. Read more information about staffing models and acuity in the following box.
Staffing Models and Acuity
Organizations that base staffing on acuity systems attempt to evenly staff patient assignments according to their acuity ratings. This means that when comparing patient assignments across nurses on a unit, similar acuity team scores should be seen with the goal of achieving equitable and safe division of workload across the nursing team. For example, one nurse should not have a total acuity score of 6 for their patient assignments while another nurse has a score of 15. If this situation occurred, the variation in scoring reflects a discrepancy in workload balance and would likely be perceived by nursing peers as unfair. Using acuity-rating staffing models is helpful to reflect the individualized nursing care required by different patients.
Alternatively, nurse staffing models may be determined by staffing ratio. Ratio-based staffing models are more straightforward in nature, where each nurse is assigned care for a set number of patients during their shift. Ratio-based staffing models may be useful for administrators creating budget requests based on the number of staff required for patient care, but can lead to an inequitable division of work across the nursing team when patient acuity is not considered. Increasingly complex patients require more time and interventions than others, so a blend of both ratio and acuity-based staffing is helpful when determining staffing assignments.[71]
As a practicing nurse, you will be oriented to the elements of acuity ratings within your health care organization, but it is also important to understand how you can use these acuity ratings for your own prioritization and task delineation. Let’s consider the Scenario B in the following box to better understand how acuity ratings can be useful for prioritizing nursing care.
Scenario B
You report to work at 6 a.m. for your nursing shift on a busy medical-surgical unit. Prior to receiving the handoff report from your night shift nursing colleagues, you review the unit staffing grid and see that you have been assigned to four patients to start your day. The patients have the following acuity ratings:
Patient A: 45-year-old patient with paraplegia admitted for an infected sacral wound, with an acuity rating of 4.
Patient B: 87-year-old patient with pneumonia with a low-grade fever of 99.7 F and receiving oxygen at 2 L/minute via nasal cannula, with an acuity rating of 2.
Patient C: 63-year-old patient who is postoperative Day 1 from a right total hip replacement and is receiving pain management via a PCA pump, with an acuity rating of 2.
Patient D: 83-year-old patient admitted with a UTI who is finishing an IV antibiotic cycle and will be discharged home today, with an acuity rating of 1.
Based on the acuity rating system, your patient assignment load receives an overall acuity score of 9. Consider how you might use their acuity ratings to help you prioritize your care. Based on what is known about the patients related to their acuity rating, whom might you identify as your care priority? Although this can feel like a challenging question to answer because of the many unknown elements in the situation using acuity numbers alone, Patient A with an acuity rating of 4 would be identified as the care priority requiring assessment early in your shift.
Although acuity can a useful tool for determining care priorities, it is important to recognize the limitations of this tool and consider how other patient needs impact prioritization.
Maslow’s Hierarchy of Needs
When thinking back to your first nursing or psychology course, you may recall a historical theory of human motivation based on various levels of human needs called Maslow's Hierarchy of Needs. Maslow’s Hierarchy of Needs reflects foundational human needs with progressive steps moving towards higher levels of achievement. This hierarchy of needs is traditionally represented as a pyramid with the base of the pyramid serving as essential needs that must be addressed before one can progress to another area of need.[72] See Figure 2.1[73] for an illustration of Maslow’s Hierarchy of Needs.
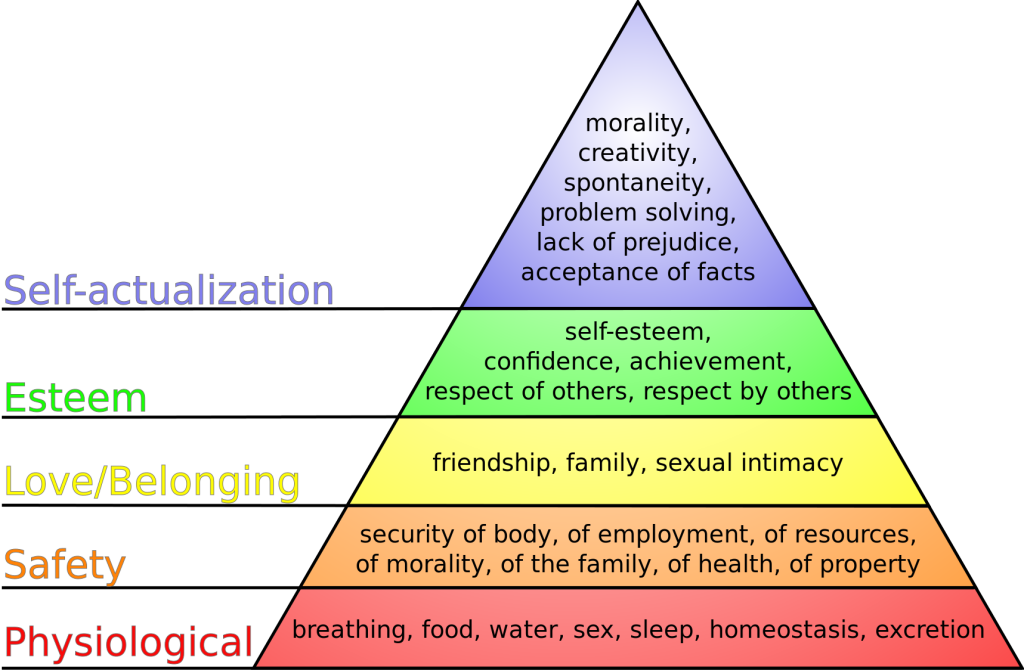
Maslow’s Hierarchy of Needs places physiological needs as the foundational base of the pyramid.[74] Physiological needs include oxygen, food, water, sex, sleep, homeostasis, and excretion. The second level of Maslow’s hierarchy reflects safety needs. Safety needs include elements that keep individuals safe from harm. Examples of safety needs in health care include fall precautions. The third level of Maslow’s hierarchy reflects emotional needs such as love and a sense of belonging. These needs are often reflected in an individual’s relationships with family members and friends. The top two levels of Maslow’s hierarchy include esteem and self-actualization. An example of addressing these needs in a health care setting is helping an individual build self-confidence in performing blood glucose checks that leads to improved self-management of their diabetes.
So how does Maslow’s theory impact prioritization? To better understand the application of Maslow’s theory to prioritization, consider Scenario C in the following box.
Scenario C
You are an emergency response nurse working at a local shelter in a community that has suffered a devastating hurricane. Many individuals have relocated to the shelter for safety in the aftermath of the hurricane. Much of the community is still without electricity and clean water, and many homes have been destroyed. You approach a young woman who has a laceration on her scalp that is bleeding through her gauze dressing. The woman is weeping as she describes the loss of her home stating, “I have lost everything! I just don’t know what I am going to do now. It has been a day since I have had water or anything to drink. I don’t know where my sister is, and I can’t reach any of my family to find out if they are okay!”
Despite this relatively brief interaction, this woman has shared with you a variety of needs. She has demonstrated a need for food, water, shelter, homeostasis, and family. As the nurse caring for her, it might be challenging to think about where to begin her care. These thoughts could be racing through your mind:
Should I begin to make phone calls to try and find her family? Maybe then she would be able to calm down.
Should I get her on the list for the homeless shelter so she wouldn’t have to worry about where she will sleep tonight?
She hasn’t eaten in a while; I should probably find her something to eat.
All these needs are important and should be addressed at some point, but Maslow’s hierarchy provides guidance on what needs must be addressed first. Use the foundational level of Maslow’s pyramid of physiological needs as the top priority for care. The woman is bleeding heavily from a head wound and has had limited fluid intake. As the nurse caring for this patient, it is important to immediately intervene to stop the bleeding and restore fluid volume. Stabilizing the patient by addressing her physiological needs is required before undertaking additional measures such as contacting her family. Imagine if instead you made phone calls to find the patient’s family and didn't address the bleeding or dehydration - you might return to a severely hypovolemic patient who has deteriorated and may be near death. In this example, prioritizing emotional needs above physiological needs can lead to significant harm to the patient.
Although this is a relatively straightforward example, the principles behind the application of Maslow’s hierarchy are essential. Addressing physiological needs before progressing toward additional need categories concentrates efforts on the most vital elements to enhance patient well-being. Maslow’s hierarchy provides the nurse with a helpful framework for identifying and prioritizing critical patient care needs.
ABCs
Airway, breathing, and circulation, otherwise known by the mnemonic “ABCs,” are another foundational element to assist the nurse in prioritization. Like Maslow’s hierarchy, using the ABCs to guide decision-making concentrates on the most critical needs for preserving human life. If a patient does not have a patent airway, is unable to breathe, or has inadequate circulation, very little of what else we do matters. The patient’s ABCs are reflected in Maslow’s foundational level of physiological needs and direct critical nursing actions and timely interventions. Let’s consider Scenario D in the following box regarding prioritization using the ABCs and the physiological base of Maslow’s hierarchy.
Scenario D
You are a nurse on a busy cardiac floor charting your morning assessments on a computer at the nurses’ station. Down the hall from where you are charting, two of your assigned patients are resting comfortably in Room 504 and Room 506. Suddenly, both call lights ring from the rooms, and you answer them via the intercom at the nurses’ station.
Room 504 has an 87-year-old male who has been admitted with heart failure, weakness, and confusion. He has a bed alarm for safety and has been ringing his call bell for assistance appropriately throughout the shift. He requires assistance to get out of bed to use the bathroom. He received his morning medications, which included a diuretic about 30 minutes previously, and now reports significant urge to void and needs assistance to the bathroom.
Room 506 has a 47-year-old woman who was hospitalized with new onset atrial fibrillation with rapid ventricular response. The patient underwent a cardioversion procedure yesterday that resulted in successful conversion of her heart back into normal sinus rhythm. She is reporting via the intercom that her "heart feels like it is doing that fluttering thing again” and she is having chest pain with breathlessness.
Based upon these two patient scenarios, it might be difficult to determine whom you should see first. Both patients are demonstrating needs in the foundational physiological level of Maslow’s hierarchy and require assistance. To prioritize between these patients' physiological needs, the nurse can apply the principles of the ABCs to determine intervention. The patient in Room 506 reports both breathing and circulation issues, warning indicators that action is needed immediately. Although the patient in Room 504 also has an urgent physiological elimination need, it does not overtake the critical one experienced by the patient in Room 506. The nurse should immediately assess the patient in Room 506 while also calling for assistance from a team member to assist the patient in Room 504.
CURE
Prioritizing what should be done and when it can be done can be a challenging task when several patients all have physiological needs. Recently, there has been professional acknowledgement of the cognitive challenge for novice nurses in differentiating physiological needs. To expand on the principles of prioritizing using the ABCs, the CURE hierarchy has been introduced to help novice nurses better understand how to manage competing patient needs. The CURE hierarchy uses the acronym “CURE” to guide prioritization based on identifying the differences among Critical needs, Urgent needs, Routine needs, and Extras.[75]
“Critical” patient needs require immediate action. Examples of critical needs align with the ABCs and Maslow’s physiological needs, such as symptoms of respiratory distress, chest pain, and airway compromise. No matter the complexity of their shift, nurses can be assured that addressing patients' critical needs is the correct prioritization of their time and energies.
After critical patient care needs have been addressed, nurses can then address “urgent” needs. Urgent needs are characterized as needs that cause patient discomfort or place the patient at a significant safety risk.[76]
The third part of the CURE hierarchy reflects “routine” patient needs. Routine patient needs can also be characterized as "typical daily nursing care" because the majority of a standard nursing shift is spent addressing routine patient needs. Examples of routine daily nursing care include actions such as administering medication and performing physical assessments.[77] Although a nurse’s typical shift in a hospital setting includes these routine patient needs, they do not supersede critical or urgent patient needs.
The final component of the CURE hierarchy is known as “extras.” Extras refer to activities performed in the care setting to facilitate patient comfort but are not essential.[78] Examples of extra activities include providing a massage for comfort or washing a patient’s hair. If a nurse has sufficient time to perform extra activities, they contribute to a patient’s feeling of satisfaction regarding their care, but these activities are not essential to achieve patient outcomes.
Let's apply the CURE mnemonic to patient care in the following box.
If we return to Scenario D regarding patients in Room 504 and 506, we can see the patient in Room 504 is having urgent needs. He is experiencing a physiological need to urgently use the restroom and may also have safety concerns if he does not receive assistance and attempts to get up on his own because of weakness. He is on a bed alarm, which reflects safety considerations related to his potential to get out of bed without assistance. Despite these urgent indicators, the patient in Room 506 is experiencing a critical need and takes priority. Recall that critical needs require immediate nursing action to prevent patient deterioration. The patient in Room 506 with a rapid, fluttering heartbeat and shortness of breath has a critical need because without prompt assessment and intervention, their condition could rapidly decline and become fatal.
Data Cues
In addition to using the identified frameworks and tools to assist with priority setting, nurses must also look at their patients’ data cues to help them identify care priorities. Data cues are pieces of significant clinical information that direct the nurse toward a potential clinical concern or a change in condition. For example, have the patient’s vital signs worsened over the last few hours? Is there a new laboratory result that is concerning? Data cues are used in conjunction with prioritization frameworks to help the nurse holistically understand the patient's current status and where nursing interventions should be directed. Common categories of data clues include acute versus chronic conditions, actual versus potential problems, unexpected versus expected conditions, information obtained from the review of a patient’s chart, and diagnostic information.
Acute Versus Chronic Conditions
A common data cue that nurses use to prioritize care is considering if a condition or symptom is acute or chronic. Acute conditions have a sudden and severe onset. These conditions occur due to a sudden illness or injury, and the body often has a significant response as it attempts to adapt. Chronic conditions have a slow onset and may gradually worsen over time. The difference between an acute versus a chronic condition relates to the body’s adaptation response. Individuals with chronic conditions often experience less symptom exacerbation because their body has had time to adjust to the illness or injury. Let’s consider an example of two patients admitted to the medical-surgical unit complaining of pain in Scenario E in the following box.
Scenario E
As part of your patient assignment on a medical-surgical unit, you are caring for two patients who both ring the call light and report pain at the start of the shift. Patient A was recently admitted with acute appendicitis, and Patient B was admitted for observation due to weakness. Not knowing any additional details about the patients' conditions or current symptoms, which patient would receive priority in your assessment? Based on using the data cue of acute versus chronic conditions, Patient A with a diagnosis of acute appendicitis would receive top priority for assessment over a patient with chronic pain due to osteoarthritis. Patients experiencing acute pain require immediate nursing assessment and intervention because it can indicate a change in condition. Acute pain also elicits physiological effects related to the stress response, such as elevated heart rate, blood pressure, and respiratory rate, and should be addressed quickly.
Actual Versus Potential Problems
Nursing diagnoses and the nursing care plan have significant roles in directing prioritization when interpreting assessment data cues. Actual problems refer to a clinical problem that is actively occurring with the patient. A risk problem indicates the patient may potentially experience a problem but they do not have current signs or symptoms of the problem actively occurring.
Consider an example of prioritizing actual and potential problems in Scenario F in the following box.
Scenario F
A 74-year-old woman with a previous history of chronic obstructive pulmonary disease (COPD) is admitted to the hospital for pneumonia. She has generalized weakness, a weak cough, and crackles in the bases of her lungs. She is receiving IV antibiotics, fluids, and oxygen therapy. The patient can sit at the side of the bed and ambulate with the assistance of staff, although she requires significant encouragement to ambulate.
Nursing diagnoses are established for this patient as part of the care planning process. One nursing diagnosis for this patient is Ineffective Airway Clearance. This nursing diagnosis is an actual problem because the patient is currently exhibiting signs of poor airway clearance with an ineffective cough and crackles in the lungs. Nursing interventions related to this diagnosis include coughing and deep breathing, administering nebulizer treatment, and evaluating the effectiveness of oxygen therapy. The patient also has the nursing diagnosis Risk for Skin Breakdown based on her weakness and lack of motivation to ambulate. Nursing interventions related to this diagnosis include repositioning every two hours and assisting with ambulation twice daily.
The established nursing diagnoses provide cues for prioritizing care. For example, if the nurse enters the patient’s room and discovers the patient is experiencing increased shortness of breath, nursing interventions to improve the patient’s respiratory status receive top priority before attempting to get the patient to ambulate.
Although there may be times when risk problems may supersede actual problems, looking to the “actual” nursing problems can provide clues to assist with prioritization.
Unexpected Versus Expected Conditions
In a similar manner to using acute versus chronic conditions as a cue for prioritization, it is also important to consider if a client's signs and symptoms are "expected" or "unexpected" based on their overall condition. Unexpected conditions are findings that are not likely to occur in the normal progression of an illness, disease, or injury. Expected conditions are findings that are likely to occur or are anticipated in the course of an illness, disease, or injury. Unexpected findings often require immediate action by the nurse.
Let’s apply this tool to the two patients previously discussed in Scenario E. As you recall, both Patient A (with acute appendicitis) and Patient B (with weakness and diagnosed with osteoarthritis) are reporting pain. Acute pain typically receives priority over chronic pain. But what if both patients are also reporting nausea and have an elevated temperature? Although these symptoms must be addressed in both patients, they are "expected" symptoms with acute appendicitis (and typically addressed in the treatment plan) but are "unexpected" for the patient with osteoarthritis. Critical thinking alerts you to the unexpected nature of these symptoms in Patient B, so they receive priority for assessment and nursing interventions.
Handoff Report/Chart Review
Additional data cues that are helpful in guiding prioritization come from information obtained during a handoff nursing report and review of the patient chart. These data cues can be used to establish a patient's baseline status and prioritize new clinical concerns based on abnormal assessment findings. Let’s consider Scenario G in the following box based on cues from a handoff report and how it might be used to help prioritize nursing care.
Scenario G
Imagine you are receiving the following handoff report from the night shift nurse for a patient admitted to the medical-surgical unit with pneumonia:
At the beginning of my shift, the patient was on room air with an oxygen saturation of 93%. She had slight crackles in both bases of her posterior lungs. At 0530, the patient rang the call light to go to the bathroom. As I escorted her to the bathroom, she appeared slightly short of breath. Upon returning the patient to bed, I rechecked her vital signs and found her oxygen saturation at 88% on room air and respiratory rate of 20. I listened to her lung sounds and noticed more persistent crackles and coarseness than at bedtime. I placed the patient on 2 L/minute of oxygen via nasal cannula. Within five minutes, her oxygen saturation increased to 92%, and she reported increased ease in respiration.
Based on the handoff report, the night shift nurse provided substantial clinical evidence that the patient may be experiencing a change in condition. Although these changes could be attributed to lack of lung expansion that occurred while the patient was sleeping, there is enough information to indicate to the oncoming nurse that follow-up assessment and interventions should be prioritized for this patient because of potentially worsening respiratory status. In this manner, identifying data cues from a handoff report can assist with prioritization.
Now imagine the night shift nurse had not reported this information during the handoff report. Is there another method for identifying potential changes in patient condition? Many nurses develop a habit of reviewing their patients’ charts at the start of every shift to identify trends and “baselines” in patient condition. For example, a chart review reveals a patient’s heart rate on admission was 105 beats per minute. If the patient continues to have a heart rate in the low 100s, the nurse is not likely to be concerned if today’s vital signs reveal a heart rate in the low 100s. Conversely, if a patient’s heart rate on admission was in the 60s and has remained in the 60s throughout their hospitalization, but it is now in the 100s, this finding is an important cue requiring prioritized assessment and intervention.
Diagnostic Information
Diagnostic results are also important when prioritizing care. In fact, the National Patient Safety Goals from The Joint Commission include prompt reporting of important test results. New abnormal laboratory results are typically flagged in a patient’s chart or are reported directly by phone to the nurse by the laboratory as they become available. Newly reported abnormal results, such as elevated blood levels or changes on a chest X-ray, may indicate a patient’s change in condition and require additional interventions. For example, consider Scenario H in which you are the nurse providing care for five medical-surgical patients.
Scenario H
You completed morning assessments on your assigned five patients. Patient A previously underwent a total right knee replacement and will be discharged home today. You are about to enter Patient A’s room to begin discharge teaching when you receive a phone call from the laboratory department, reporting a critical hemoglobin of 6.9 gm/dL on Patient B. Rather than enter Patient A’s room to perform discharge teaching, you immediately reprioritize your care. You call the primary provider to report Patient B’s critical hemoglobin level and determine if additional intervention, such as a blood transfusion, is required.
Prioritization Principles & Staffing Considerations[79]
With the complexity of different staffing variables in health care settings, it can be challenging to identify a method and solution that will offer a resolution to every challenge. The American Nurses Association has identified five critical principles that should be considered for nurse staffing. These principles are as follows:
- Health Care Consumer: Nurse staffing decisions are influenced by the specific number and needs of the health care consumer. The health care consumer includes not only the client, but also families, groups, and populations served. Staffing guidelines must always consider the patient safety indicators, clinical, and operational outcomes that are specific to a practice setting. What is appropriate for the consumer in one setting, may be quite different in another. Additionally, it is important to ensure that there is resource allocation for care coordination and health education in each setting.
- Interprofessional Teams: As organizations identify what constitutes appropriate staffing in various settings, they must also consider the appropriate credentials and qualifications of the nursing staff within a specific setting. This involves utilizing an interprofessional care team that allows each individual to practice to the full extent of their educational, training, scope of practice as defined by their state Nurse Practice Act, and licensure. Staffing plans must include an appropriate skill mix and acknowledge the impact of more experienced nurses to help serve in mentoring and precepting roles.
- Workplace culture: Staffing considerations must also account for the importance of balance between costs associated with best practice and the optimization of care outcomes. Health care leaders and organizations must strive to ensure a balance between quality, safety, and health care cost. Organizations are responsible for creating work environments, which develop policies allowing for nurses to practice to the full extent of their licensure in accordance with their documented competence. Leaders must foster a culture of trust, collaboration, and respect among all members of the health care team, which will create environments that engage and retain health care staff.
- Practice environment: Staffing structures must be founded in a culture of safety where appropriate staffing is integral to achieve patient safety and quality goals. An optimal practice environment encourages nurses to report unsafe conditions or poor staffing that may impact safe care. Organizations should ensure that nurses have autonomy in reporting and concerns and may do so without threat of retaliation. The ANA has also taken the position to state that mandatory overtime is an unacceptable solution to achieve appropriate staffing. Organizations must ensure that they have clear policies delineating length of shifts, meal breaks, and rest period to help ensure safety in patient care.
- Evaluation: Staffing plans should be consistently evaluated and changed based upon evidence and client outcomes. Environmental factors and issues such as work-related illness, injury, and turnover are important elements of determining the success of need for modification within a staffing plan.[80]
Prioritization of patient care should be grounded in critical thinking rather than just a checklist of items to be done. Critical thinking is a broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow."[81] Certainly, there are many actions that nurses must complete during their shift, but nursing requires adaptation and flexibility to meet emerging patient needs. It can be challenging for a novice nurse to change their mindset regarding their established “plan” for the day, but the sooner a nurse recognizes prioritization is dictated by their patients’ needs, the less frustration the nurse might experience. Prioritization strategies include collection of information and utilization of clinical reasoning to determine the best course of action. Clinical reasoning is defined as, “A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions.”[82] Clinical reasoning is fostered within nurses when they are challenged to integrate data in various contexts. The clinical reasoning cycle begins when nurses first consider a client situation and progress to collecting cues and information. As nurses process the information, they begin to identify problems and establish realistic goals. They then take appropriate actions and evaluate outcomes. Finally, they reflect upon the process and the learning that has occurred. The reflection piece is critical for solidifying or changing future actions and developing knowledge.
When nurses use critical thinking and clinical reasoning skills, they set forth on a purposeful course of intervention to best meet patient-care needs. Rather than focusing on one’s own priorities, nurses utilizing critical thinking and reasoning skills recognize their actions must be responsive to their patients. For example, a nurse using critical thinking skills understands that scheduled morning medications for their patients may be late if one of the patients on their care team suddenly develops chest pain. Many actions may be added or removed from planned activities throughout the shift based on what is occurring holistically on the patient-care team.
Additionally, in today’s complex health care environment, it is important for the novice nurse to recognize the realities of the current health care environment. Patients have become increasingly complex in their health care needs, and organizations are often challenged to meet these care needs with limited staffing resources. It can become easy to slip into the mindset of disenchantment with the nursing profession when first assuming the reality of patient-care assignments as a novice nurse. The workload of a nurse in practice often looks and feels quite different than that experienced as a nursing student. As a nursing student, there may have been time for lengthy conversations with patients and their family members, ample time to chart, and opportunities to offer personal cares, such as a massage or hair wash. Unfortunately, in the time-constrained realities of today's health care environment, novice nurses should recognize that even though these “extra” tasks are not always possible, they can still provide quality, safe patient care using the “CURE” prioritization framework. Rather than feeling frustrated about “extras” that cannot be accomplished in time-constrained environments, it is vital to use prioritization strategies to ensure appropriate actions are taken to complete what must be done. With increased clinical experience, a novice nurse typically becomes more comfortable with prioritizing and reprioritizing care.
Prioritization of patient care should be grounded in critical thinking rather than just a checklist of items to be done. Critical thinking is a broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow."[83] Certainly, there are many actions that nurses must complete during their shift, but nursing requires adaptation and flexibility to meet emerging patient needs. It can be challenging for a novice nurse to change their mindset regarding their established “plan” for the day, but the sooner a nurse recognizes prioritization is dictated by their patients’ needs, the less frustration the nurse might experience. Prioritization strategies include collection of information and utilization of clinical reasoning to determine the best course of action. Clinical reasoning is defined as, “A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions.”[84] Clinical reasoning is fostered within nurses when they are challenged to integrate data in various contexts. The clinical reasoning cycle begins when nurses first consider a client situation and progress to collecting cues and information. As nurses process the information, they begin to identify problems and establish realistic goals. They then take appropriate actions and evaluate outcomes. Finally, they reflect upon the process and the learning that has occurred. The reflection piece is critical for solidifying or changing future actions and developing knowledge.
When nurses use critical thinking and clinical reasoning skills, they set forth on a purposeful course of intervention to best meet patient-care needs. Rather than focusing on one’s own priorities, nurses utilizing critical thinking and reasoning skills recognize their actions must be responsive to their patients. For example, a nurse using critical thinking skills understands that scheduled morning medications for their patients may be late if one of the patients on their care team suddenly develops chest pain. Many actions may be added or removed from planned activities throughout the shift based on what is occurring holistically on the patient-care team.
Additionally, in today’s complex health care environment, it is important for the novice nurse to recognize the realities of the current health care environment. Patients have become increasingly complex in their health care needs, and organizations are often challenged to meet these care needs with limited staffing resources. It can become easy to slip into the mindset of disenchantment with the nursing profession when first assuming the reality of patient-care assignments as a novice nurse. The workload of a nurse in practice often looks and feels quite different than that experienced as a nursing student. As a nursing student, there may have been time for lengthy conversations with patients and their family members, ample time to chart, and opportunities to offer personal cares, such as a massage or hair wash. Unfortunately, in the time-constrained realities of today's health care environment, novice nurses should recognize that even though these “extra” tasks are not always possible, they can still provide quality, safe patient care using the “CURE” prioritization framework. Rather than feeling frustrated about “extras” that cannot be accomplished in time-constrained environments, it is vital to use prioritization strategies to ensure appropriate actions are taken to complete what must be done. With increased clinical experience, a novice nurse typically becomes more comfortable with prioritizing and reprioritizing care.
Time management is not an unfamiliar concept to nursing students because many students are balancing time demands related to work, family, and school obligations. To determine where time should be allocated, prioritization processes emerge. Although the prioritization frameworks of nursing may be different than those used as a student, the concept of prioritization remains the same. Despite the context, prioritization is essentially using a structure to organize tasks to ensure the most critical tasks are completed first and then identify what to move onto next. To truly maximize time management, in addition to prioritization, individuals should be organized, strive for accuracy, minimize waste, mobilize resources, and delegate when appropriate.
Time management is one of the greatest challenges that nurses face in their busy workday. As novice nurses develop their practice, it is important to identify organizational strategies to ensure priority tasks are completed and time is optimized. Each nurse develops a personal process for organizing information and structuring the timing of their assessments, documentation, medication administration, interventions, and patient education. However, one must always remember that this process and structure must be flexible because in a moment’s time, a patient’s condition can change, requiring a reprioritization of care. An organizational tool is important to guide a nurse’s daily task progression. Organizational tools may be developed individually by the nurse or may be recommended by the organization. Tools can be rudimentary in nature, such as a simple time column format outlining care activities planned throughout the shift, or more complex and integrated within an organization’s electronic medical record. No matter the format, an organizational tool is helpful to provide structure and guide progression toward task achievement.
In addition to using an organizational tool, novice nurses should utilize other time management strategies to optimize their time. For example, assessments can start during bedside handoff report, such as what fluids and medications are running and what will need to be replaced soon. Take a moment after handoff reports to prioritize which patients you will see first during your shift. Other strategies such as grouping tasks, gathering appropriate equipment prior to initiating nursing procedures, and gathering assessment information while performing tasks are helpful in minimizing redundancy and increasing efficiency. For example, observe an experienced nurse providing care and note the efficient processes they use. They may conduct an assessment, bring in morning medications, flush an IV line, collect a morning blood glucose level, and provide patient education about medications all during one patient encounter. Efficiency becomes especially important if the patient has transmission-based precautions and the time spent donning and doffing PPE are considered. The realities of the time-constrained health care environments often necessitate clustering tasks to ensure that all patient-care tasks are completed. Furthermore, nurses who do not manage their time effectively may inadvertently place their patients at risk as a result of delayed care.[85] Effective time management benefits both the patient and the nursing staff.
Time estimation is an additional helpful strategy to facilitate time management. Time estimation involves the review of planned tasks for the day and allocating time estimated to complete the task. Time estimation is especially helpful for novice nurses as they begin to structure and prioritize their shift based on the list of tasks that are required.[86] For example, estimating the time it will take to perform an assessment and administer morning medications to one patient allows the nurse to better plan when to complete the dressing change on another patient. Without using time estimation, the nurse may attempt to group all care tasks with the morning assessments and not leave themselves enough time to administer morning medications within the desired administration time window. Additionally, working in a time-constrained environment without using time estimation strategies increases the likelihood of performing tasks “in a rush” and subsequently increasing the potential for error.
Who’s On My Team?
One of the most critical strategies to enhance time management is to mobilize the resources of the nursing team. The nursing care team includes advanced practice registered nurses (APRN), registered nurses (RN), licensed practical/vocational nurses (LPN/VN), and assistive personnel (AP). AP (formerly referred to as unlicensed assistive personnel [UAP]) include, but are not limited to, certified nursing assistants or aides (CNA), patient-care technicians (PCT), certified medical assistants (CMA), certified medication aides, and home health aides.[87] Each care environment may have a blend of staff, and it is important to understand the legalities associated with the scope and role of each member and what can be safely and appropriately delegated to other members of the team. For example, assistive personnel may be able to assist with ambulating a patient in the hallway, but they would not be able to help administer morning medications. Dividing tasks appropriately among nursing team members can help ensure that the required tasks are completed and individual energies are best allocated to meet patient needs. The nursing care team and requirements around the process of delegation are explored in detail in the "Delegation and Supervision" chapter.
Time management is not an unfamiliar concept to nursing students because many students are balancing time demands related to work, family, and school obligations. To determine where time should be allocated, prioritization processes emerge. Although the prioritization frameworks of nursing may be different than those used as a student, the concept of prioritization remains the same. Despite the context, prioritization is essentially using a structure to organize tasks to ensure the most critical tasks are completed first and then identify what to move onto next. To truly maximize time management, in addition to prioritization, individuals should be organized, strive for accuracy, minimize waste, mobilize resources, and delegate when appropriate.
Time management is one of the greatest challenges that nurses face in their busy workday. As novice nurses develop their practice, it is important to identify organizational strategies to ensure priority tasks are completed and time is optimized. Each nurse develops a personal process for organizing information and structuring the timing of their assessments, documentation, medication administration, interventions, and patient education. However, one must always remember that this process and structure must be flexible because in a moment’s time, a patient’s condition can change, requiring a reprioritization of care. An organizational tool is important to guide a nurse’s daily task progression. Organizational tools may be developed individually by the nurse or may be recommended by the organization. Tools can be rudimentary in nature, such as a simple time column format outlining care activities planned throughout the shift, or more complex and integrated within an organization’s electronic medical record. No matter the format, an organizational tool is helpful to provide structure and guide progression toward task achievement.
In addition to using an organizational tool, novice nurses should utilize other time management strategies to optimize their time. For example, assessments can start during bedside handoff report, such as what fluids and medications are running and what will need to be replaced soon. Take a moment after handoff reports to prioritize which patients you will see first during your shift. Other strategies such as grouping tasks, gathering appropriate equipment prior to initiating nursing procedures, and gathering assessment information while performing tasks are helpful in minimizing redundancy and increasing efficiency. For example, observe an experienced nurse providing care and note the efficient processes they use. They may conduct an assessment, bring in morning medications, flush an IV line, collect a morning blood glucose level, and provide patient education about medications all during one patient encounter. Efficiency becomes especially important if the patient has transmission-based precautions and the time spent donning and doffing PPE are considered. The realities of the time-constrained health care environments often necessitate clustering tasks to ensure that all patient-care tasks are completed. Furthermore, nurses who do not manage their time effectively may inadvertently place their patients at risk as a result of delayed care.[88] Effective time management benefits both the patient and the nursing staff.
Time estimation is an additional helpful strategy to facilitate time management. Time estimation involves the review of planned tasks for the day and allocating time estimated to complete the task. Time estimation is especially helpful for novice nurses as they begin to structure and prioritize their shift based on the list of tasks that are required.[89] For example, estimating the time it will take to perform an assessment and administer morning medications to one patient allows the nurse to better plan when to complete the dressing change on another patient. Without using time estimation, the nurse may attempt to group all care tasks with the morning assessments and not leave themselves enough time to administer morning medications within the desired administration time window. Additionally, working in a time-constrained environment without using time estimation strategies increases the likelihood of performing tasks “in a rush” and subsequently increasing the potential for error.
Who’s On My Team?
One of the most critical strategies to enhance time management is to mobilize the resources of the nursing team. The nursing care team includes advanced practice registered nurses (APRN), registered nurses (RN), licensed practical/vocational nurses (LPN/VN), and assistive personnel (AP). AP (formerly referred to as unlicensed assistive personnel [UAP]) include, but are not limited to, certified nursing assistants or aides (CNA), patient-care technicians (PCT), certified medical assistants (CMA), certified medication aides, and home health aides.[90] Each care environment may have a blend of staff, and it is important to understand the legalities associated with the scope and role of each member and what can be safely and appropriately delegated to other members of the team. For example, assistive personnel may be able to assist with ambulating a patient in the hallway, but they would not be able to help administer morning medications. Dividing tasks appropriately among nursing team members can help ensure that the required tasks are completed and individual energies are best allocated to meet patient needs. The nursing care team and requirements around the process of delegation are explored in detail in the "Delegation and Supervision" chapter.
Sam is a novice nurse who is reporting to work for his 0600 shift on the medical telemetry/progressive care floor. He is waiting to receive handoff report from the night shift nurse for his assigned patients. The information that he has received thus far regarding his patient assignment includes the following:
- Room 501: 64-year-old patient admitted last night with heart failure exacerbation. Patient received furosemide 80mg IV push at 2000 with 1600 mL urine output. He is receiving oxygen via nasal cannula at 2L/minute. According to the night shift aide, he has been resting comfortably overnight.
- Room 507: 74-year-old patient admitted yesterday for possible cardioversion due to new onset of atrial fibrillation with rapid ventricular response and is scheduled for transesophageal echocardiogram and possible cardioversion at 1000.
- Room 512: 82-year-old patient who is scheduled for coronary artery bypass graft (CABG) surgery today at 0700 and is receiving an insulin infusion.
- Room 536: 72-year-old patient who had a negative heart catheterization yesterday but experienced a groin bleed; plans for discharge this morning.
Based on the limited information Sam has thus far, he begins to prioritize his activities for the morning. With what is known thus far regarding his patient assignment, whom might Sam plan to see first and why? What principles of prioritization might be applied?
Although Sam would benefit from hearing a full report on his patients and reviewing the patient charts, he can already begin to engage in strategies for prioritization. Based on the information that has been shared thus far, Sam determines that none of the patients assigned to him are experiencing critical or urgent needs. All the patients' basic physiological needs are being met, but many have actual clinical concerns. Based on the time constraint with scheduled surgery and the insulin infusion for the patient in Room 512, this patient should take priority in Sam's assessments. It is important for Sam to ensure that this patient's pre-op checklist is complete, and he is stable with the infusion prior to transferring him for surgery. Although Sam may later receive information that alters this priority setting, based on the information he has thus far, he has utilized prioritization principles to make an informed decision.
Sam is a novice nurse who is reporting to work for his 0600 shift on the medical telemetry/progressive care floor. He is waiting to receive handoff report from the night shift nurse for his assigned patients. The information that he has received thus far regarding his patient assignment includes the following:
- Room 501: 64-year-old patient admitted last night with heart failure exacerbation. Patient received furosemide 80mg IV push at 2000 with 1600 mL urine output. He is receiving oxygen via nasal cannula at 2L/minute. According to the night shift aide, he has been resting comfortably overnight.
- Room 507: 74-year-old patient admitted yesterday for possible cardioversion due to new onset of atrial fibrillation with rapid ventricular response and is scheduled for transesophageal echocardiogram and possible cardioversion at 1000.
- Room 512: 82-year-old patient who is scheduled for coronary artery bypass graft (CABG) surgery today at 0700 and is receiving an insulin infusion.
- Room 536: 72-year-old patient who had a negative heart catheterization yesterday but experienced a groin bleed; plans for discharge this morning.
Based on the limited information Sam has thus far, he begins to prioritize his activities for the morning. With what is known thus far regarding his patient assignment, whom might Sam plan to see first and why? What principles of prioritization might be applied?
Although Sam would benefit from hearing a full report on his patients and reviewing the patient charts, he can already begin to engage in strategies for prioritization. Based on the information that has been shared thus far, Sam determines that none of the patients assigned to him are experiencing critical or urgent needs. All the patients' basic physiological needs are being met, but many have actual clinical concerns. Based on the time constraint with scheduled surgery and the insulin infusion for the patient in Room 512, this patient should take priority in Sam's assessments. It is important for Sam to ensure that this patient's pre-op checklist is complete, and he is stable with the infusion prior to transferring him for surgery. Although Sam may later receive information that alters this priority setting, based on the information he has thus far, he has utilized prioritization principles to make an informed decision.
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activities are provided as immediate feedback.)
- The nurse is conducting an assessment on a 70-year-old male client who was admitted with atrial fibrillation. The client has a history of hypertension and Stage 2 chronic kidney disease. The nurse begins the head-to-toe assessment and notes the patient is having difficulty breathing and is complaining about chest discomfort. The client states, “It feels as if my heart is going to pound out of my chest and I feel dizzy.” The nurse begins the head-to-toe assessment and documents the findings. Client assessment findings are presented in the table below. Select the assessment findings requiring immediate follow-up by the nurse.
Vital Signs
| Temperature | 98.9 °F (37.2°C) |
|---|---|
| Heart Rate | 182 beats/min |
| Respirations | 36 breaths/min |
| Blood Pressure | 152/90 mm Hg |
| Oxygen Saturation | 88% on room air |
| Capillary Refill Time | >3 |
| Pain | 9/10 chest discomfort |
| Physical Assessment Findings | |
|---|---|
| Glasgow Coma Scale Score | 14 |
| Level of Consciousness | Alert |
| Heart Sounds | Irregularly regular |
| Lung Sounds | Clear bilaterally anterior/posterior |
| Pulses-Radial | Rapid/bounding |
| Pulses-Pedal | Weak |
| Bowel Sounds | Present and active x 4 |
| Edema | Trace bilateral lower extremities |
| Skin | Cool, clammy |
2. The following nursing actions may or may not be required at this time based on the assessment findings. Indicate whether the actions are "Indicated" (i.e., appropriate or necessary), "Contraindicated" (i.e., could be harmful), or "Nonessential" (i.e., makes no difference or are not necessary).
| Nursing Action | Indicated | Contraindicated | Nonessential |
|---|---|---|---|
| Apply oxygen at 2 liters per nasal cannula. | |||
| Call imaging for a STAT lung CT. | |||
| Perform the National Institutes of Health (NIH) Stroke Scale Neurologic Exam. | |||
| Obtain a comprehensive metabolic panel (CMP). | |||
| Obtain a STAT EKG. | |||
| Raise the head-of-bed to less than 10 degrees. | |||
| Establish patent IV access. | |||
| Administer potassium 20 mEq IV push STAT. |
3. The CURE hierarchy has been introduced to help novice nurses better understand how to manage competing patient needs. The CURE hierarchy uses the acronym “CURE” to help guide prioritization based on identifying the differences among Critical needs, Urgent needs, Routine needs, and Extras.
You are the nurse caring for the patients in the following table. For each patient, indicate if this is a "critical," "urgent," "routine," or "extra" need.
<td">
| Critical | Urgent | Routine | Extra | |
|---|---|---|---|---|
| Patient exhibits new left-sided facial droop | ||||
| Patient reports 9/10 acute pain and requests PRN pain medication | ||||
| Patient with BP 120/80 and regular heart rate of 68 has scheduled dose of oral amlodipine | ||||
| Patient with insomnia requests a back rub before bedtime | ||||
| Patient has a scheduled dressing change for a pressure ulcer on their coccyx |
||||
| Patient is exhibiting new shortness of breath and altered mental status | ||||
| Patient with fall risk precautions ringing call light for assistance to the restroom for a bowel movement |

Test your knowledge using this NCLEX Next Generation-style Case Study. You may reset and resubmit your answers to this question an unlimited number of times.[91]
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activities are provided as immediate feedback.)
- The nurse is conducting an assessment on a 70-year-old male client who was admitted with atrial fibrillation. The client has a history of hypertension and Stage 2 chronic kidney disease. The nurse begins the head-to-toe assessment and notes the patient is having difficulty breathing and is complaining about chest discomfort. The client states, “It feels as if my heart is going to pound out of my chest and I feel dizzy.” The nurse begins the head-to-toe assessment and documents the findings. Client assessment findings are presented in the table below. Select the assessment findings requiring immediate follow-up by the nurse.
Vital Signs
| Temperature | 98.9 °F (37.2°C) |
|---|---|
| Heart Rate | 182 beats/min |
| Respirations | 36 breaths/min |
| Blood Pressure | 152/90 mm Hg |
| Oxygen Saturation | 88% on room air |
| Capillary Refill Time | >3 |
| Pain | 9/10 chest discomfort |
| Physical Assessment Findings | |
|---|---|
| Glasgow Coma Scale Score | 14 |
| Level of Consciousness | Alert |
| Heart Sounds | Irregularly regular |
| Lung Sounds | Clear bilaterally anterior/posterior |
| Pulses-Radial | Rapid/bounding |
| Pulses-Pedal | Weak |
| Bowel Sounds | Present and active x 4 |
| Edema | Trace bilateral lower extremities |
| Skin | Cool, clammy |
2. The following nursing actions may or may not be required at this time based on the assessment findings. Indicate whether the actions are "Indicated" (i.e., appropriate or necessary), "Contraindicated" (i.e., could be harmful), or "Nonessential" (i.e., makes no difference or are not necessary).
| Nursing Action | Indicated | Contraindicated | Nonessential |
|---|---|---|---|
| Apply oxygen at 2 liters per nasal cannula. | |||
| Call imaging for a STAT lung CT. | |||
| Perform the National Institutes of Health (NIH) Stroke Scale Neurologic Exam. | |||
| Obtain a comprehensive metabolic panel (CMP). | |||
| Obtain a STAT EKG. | |||
| Raise the head-of-bed to less than 10 degrees. | |||
| Establish patent IV access. | |||
| Administer potassium 20 mEq IV push STAT. |
3. The CURE hierarchy has been introduced to help novice nurses better understand how to manage competing patient needs. The CURE hierarchy uses the acronym “CURE” to help guide prioritization based on identifying the differences among Critical needs, Urgent needs, Routine needs, and Extras.
You are the nurse caring for the patients in the following table. For each patient, indicate if this is a "critical," "urgent," "routine," or "extra" need.
<td">
| Critical | Urgent | Routine | Extra | |
|---|---|---|---|---|
| Patient exhibits new left-sided facial droop | ||||
| Patient reports 9/10 acute pain and requests PRN pain medication | ||||
| Patient with BP 120/80 and regular heart rate of 68 has scheduled dose of oral amlodipine | ||||
| Patient with insomnia requests a back rub before bedtime | ||||
| Patient has a scheduled dressing change for a pressure ulcer on their coccyx |
||||
| Patient is exhibiting new shortness of breath and altered mental status | ||||
| Patient with fall risk precautions ringing call light for assistance to the restroom for a bowel movement |

Test your knowledge using this NCLEX Next Generation-style Case Study. You may reset and resubmit your answers to this question an unlimited number of times.[92]
ABCs: Airway, breathing, and circulation.
Actual problems: Nursing problems currently occurring with the patient.
Acuity: The level of patient care that is required based on the severity of a patient’s illness or condition.
Acuity-rating staffing models: A staffing model used to make patient assignments that reflects the individualized nursing care required for different types of patients.
Acute conditions: Conditions having a sudden onset.
Chronic conditions: Conditions that have a slow onset and may gradually worsen over time.
Clinical reasoning: “A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions.”[93]
Critical thinking: A broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.”[94]
CURE hierarchy: A strategy for prioritization based on identifying “critical” needs, “urgent” needs, “routine” needs, and “extras.”
Data cues: Pieces of significant clinical information that direct the nurse toward a potential clinical concern or a change in condition.
Expected conditions: Conditions that are likely to occur or anticipated in the course of an illness, disease, or injury.
Maslow’s Hierarchy of Needs: Prioritization strategies often reflect the foundational elements of physiological needs and safety and progress toward higher levels.
Ratio-based staffing models: A staffing model used to make patient assignments in terms of one nurse caring for a set number of patients.
Risk problem: A nursing problem that reflects that a patient may experience a problem but does not currently have signs reflecting the problem is actively occurring.
Time estimation: A prioritization strategy including the review of planned tasks and allocation of time believed to be required to complete each task.
Time scarcity: A feeling of racing against a clock that is continually working against you.
Unexpected conditions: Conditions that are not likely to occur in the normal progression of an illness, disease, or injury.
Learning Objectives
- Explain principles of delegation
- Evaluate the criteria used for delegation
- Apply effective communication techniques when delegating care
- Determine specific barriers to delegation
- Evaluate team members' performance based on delegation and supervision principles
- Incorporate principles of supervision and evaluation in the delegation process
- Identify scope of practice of the RN, LPN/VN, and unlicensed assistive personnel roles
- Identify tasks that can and cannot be delegated to members of the nursing team
As health care technology continues to advance, clients require increasingly complex nursing care, and as staffing becomes more challenging, health care agencies respond with an evolving variety of nursing and assistive personnel roles and responsibilities to meet these demands. As an RN, you are on the front lines caring for ill or injured clients and their families, advocating for clients’ rights, creating nursing care plans, educating clients on how to self-manage their health, and providing leadership throughout the complex health care system. Delivering safe, effective, quality client care requires the RN to coordinate care by the nursing team as tasks are assigned, delegated, and supervised. Nursing team members include advanced practice registered nurses (APRN), registered nurses (RN), licensed practical/vocational nurses (LPN/VN), and assistive personnel (AP).[95]
Assistive personnel (AP) (formerly referred to as ‘‘unlicensed” assistive personnel [UAP]) are any assistive personnel trained to function in a supportive role, regardless of title, to whom a nursing responsibility may be delegated. This includes, but is not limited to, certified nursing assistants or aides (CNAs), patient-care technicians (PCTs), certified medical assistants (CMAs), certified medication aides, and home health aides.[96] Making assignments, delegating tasks, and supervising delegatees are essential components of the RN role and can also provide the RN more time to focus on the complex needs of clients. For example, an RN may delegate to AP the attainment of vital signs for clients who are stable, thus providing the nurse more time to closely monitor the effectiveness of interventions in maintaining complex clients' hemodynamics, thermoregulation, and oxygenation. Collaboration among the nursing care team members allows for the delivery of optimal care as various skill sets are implemented to care for the patient.
Properly assigning and delegating tasks to nursing team members can promote efficient client care. However, inappropriate assignments or delegation can compromise client safety and produce unsatisfactory client outcomes that may result in legal issues. How does the RN know what tasks can be assigned or delegated to nursing team members and assistive personnel? What steps should the RN follow when determining if care can be delegated? After assignments and delegations are established, what is the role and responsibility of the RN in supervising client care? This chapter will explore and define the fundamental concepts involved in assigning, delegating, and supervising client care according to the most recent joint national delegation guidelines published by the National Council of State Boards of Nursing (NCSBN) and the American Nurses Association (ANA).[97]
Learning Objectives
- Explain principles of delegation
- Evaluate the criteria used for delegation
- Apply effective communication techniques when delegating care
- Determine specific barriers to delegation
- Evaluate team members' performance based on delegation and supervision principles
- Incorporate principles of supervision and evaluation in the delegation process
- Identify scope of practice of the RN, LPN/VN, and unlicensed assistive personnel roles
- Identify tasks that can and cannot be delegated to members of the nursing team
As health care technology continues to advance, clients require increasingly complex nursing care, and as staffing becomes more challenging, health care agencies respond with an evolving variety of nursing and assistive personnel roles and responsibilities to meet these demands. As an RN, you are on the front lines caring for ill or injured clients and their families, advocating for clients’ rights, creating nursing care plans, educating clients on how to self-manage their health, and providing leadership throughout the complex health care system. Delivering safe, effective, quality client care requires the RN to coordinate care by the nursing team as tasks are assigned, delegated, and supervised. Nursing team members include advanced practice registered nurses (APRN), registered nurses (RN), licensed practical/vocational nurses (LPN/VN), and assistive personnel (AP).[98]
Assistive personnel (AP) (formerly referred to as ‘‘unlicensed” assistive personnel [UAP]) are any assistive personnel trained to function in a supportive role, regardless of title, to whom a nursing responsibility may be delegated. This includes, but is not limited to, certified nursing assistants or aides (CNAs), patient-care technicians (PCTs), certified medical assistants (CMAs), certified medication aides, and home health aides.[99] Making assignments, delegating tasks, and supervising delegatees are essential components of the RN role and can also provide the RN more time to focus on the complex needs of clients. For example, an RN may delegate to AP the attainment of vital signs for clients who are stable, thus providing the nurse more time to closely monitor the effectiveness of interventions in maintaining complex clients' hemodynamics, thermoregulation, and oxygenation. Collaboration among the nursing care team members allows for the delivery of optimal care as various skill sets are implemented to care for the patient.
Properly assigning and delegating tasks to nursing team members can promote efficient client care. However, inappropriate assignments or delegation can compromise client safety and produce unsatisfactory client outcomes that may result in legal issues. How does the RN know what tasks can be assigned or delegated to nursing team members and assistive personnel? What steps should the RN follow when determining if care can be delegated? After assignments and delegations are established, what is the role and responsibility of the RN in supervising client care? This chapter will explore and define the fundamental concepts involved in assigning, delegating, and supervising client care according to the most recent joint national delegation guidelines published by the National Council of State Boards of Nursing (NCSBN) and the American Nurses Association (ANA).[100]
Effective communication is a vital component of proper assignment, delegation, and supervision. It is also one of the Standards of Professional Performance established by the American Nurses Association (ANA).[101] Research has identified that new graduate nurses are more susceptible to stress and isolation within their job roles due to poor communication and teamwork within the interdisciplinary team.[102] Strong communication skills foster a supportive work environment and colleagial relationships that benefit both patients and nursing staff.
Consider the fundamentals of good communication practices. Effective communication requires each interaction to include a sender of the message, a clear and concise message, and a receiver who can decode and interpret that message. The receiver also provides a feedback message back to the sender in response to the received message. See Figure 3.1[103] for an image of effective communication between a sender and receiver. This feedback message is referred to as closed-loop communication in health care settings. Closed-loop communication enables the person giving the instructions to hear what they said reflected back and to confirm that their message was received correctly. It also allows the person receiving the instructions to verify and confirm the actions to be taken. If closed-loop communication is not used, the receiver may nod or say “OK,” and the sender may assume the message has been effectively transmitted, but this may not be the case and can lead to errors and client harm.
An example of closed-loop communication can be found in the following exchange:
- RN: “Jane, can you get a set of vitals on Mr. Smith and let me know if the results are outside of normal range?”
- Jane, CNA: “OK, I’ll get a set of vitals on Mr. Smith and let you know if they are out of range.”
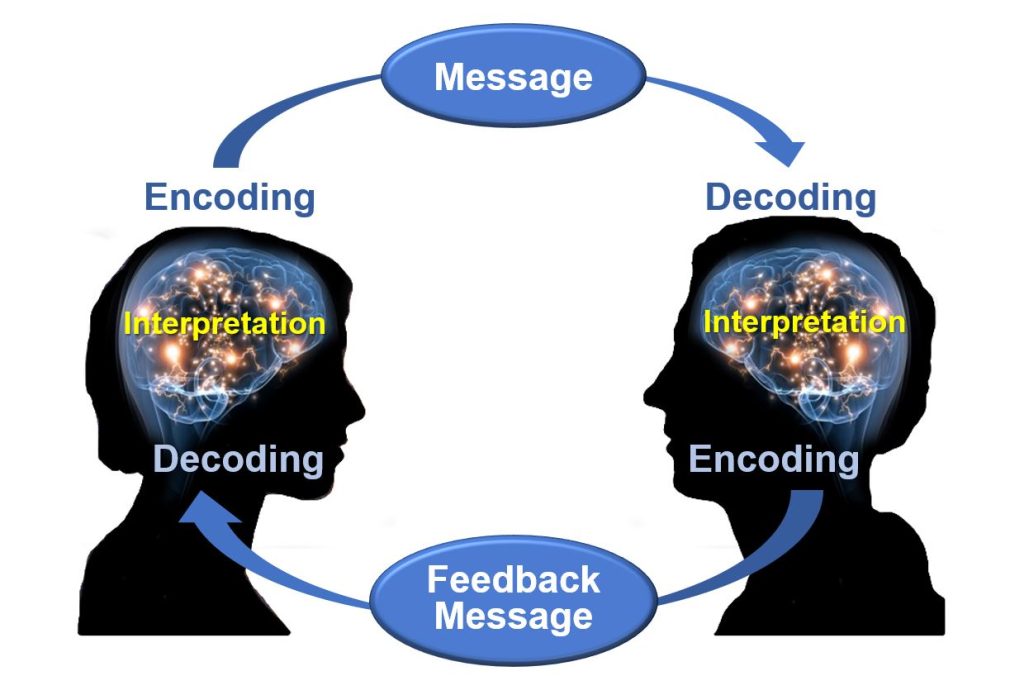
Closed-loop communication is vital for communication among health care team members to avoid misunderstandings that can cause unsafe client care. According to the HIPAA Journal, poor communication leads to a “reduction in the quality of care, poor client outcomes, wastage of resources, and high health care costs.”[104] Parameters for reporting results and the results that should be expected are often left unsaid rather than spelled out in sufficient detail. It is imperative for the RN to provide clear, complete, concise instructions when delegating. A lack of clarity can lead to misunderstanding, unfinished tasks, incomplete care, and/or medical errors.[105]
Effective communication is at the core of proper assignment, delegation, and supervision. With effective communication at the beginning of every shift, each nursing team member should have a clear plan for their shift, what to do and why, and what and when to report to the RN or team leader. Communication should continue throughout the shift as tasks are accomplished and patients’ needs change. Effective communication improves client outcomes and satisfaction scores, as well as improving team morale by enhancing the collaborative relationships of the health care team.
The RN is accountable for clear, concise, correct, and complete communication when making assignments and delegating, both initially and throughout the shift. These communication characteristics can be remembered by using the mnemonic the "4 Cs":
- Clear: Information is understood by the listener. Asking the listener to restate the instructions and the plan can be helpful to determine whether the communication is clear.
- Concise: Sufficient information should be provided to accurately perform the task, but excessive or irrelevant information should be avoided because it can confuse the listener and waste precious time.
- Correct: Correct communication is not vague or confusing. Accurate information is also aligned with agency policy and the team member’s scope of practice as defined by their state’s Nurse Practice Act and other state regulations.
- Complete: Complete instructions leave no room for doubt. Always ask if further information or clarification is needed, especially regarding tasks that are infrequently performed or include unique instructions.[106]
The use of closed-loop communication is the best method to achieve clear, concise, correct, and complete information exchanged among team members. Closed-loop communication allows team members the opportunity to verify and validate the exchange of information. By repeating back information, members confirm the exchange has occurred, understanding is clear, and expectations are heard.
Closed-loop communication should also be used when the RN is receiving a verbal order from a provider. For example, when the resuscitation team leader gives a verbal order of “Epinephrine 1 mg/mL IV push now,” the RN confirms correct understanding of the order by repeating back, “I will prepare Epinephrine 1 mg/mL to be given IV push now.” After the provider confirms the verbal order and the task is completed, the nurse confirms completion of the task by stating, “Epinephrine 1 mg/mL IV push was administered.”
In addition to using closed-loop communication, a common format used by health care team members to exchange client information is ISBARR, a mnemonic for the components of Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat Back. ISBARR and other communication strategies are discussed in more detail in the "Interprofessional Communication" section of the "Collaboration Within the Interprofessional Team" chapter.
The observed outcome of critical thinking and decision-making. It is an iterative process that uses nursing knowledge to observe and access presenting situations, identify a prioritized client concern, and generate the best possible evidence-based solutions in order to deliver safe client care.
Effective communication is a vital component of proper assignment, delegation, and supervision. It is also one of the Standards of Professional Performance established by the American Nurses Association (ANA).[107] Research has identified that new graduate nurses are more susceptible to stress and isolation within their job roles due to poor communication and teamwork within the interdisciplinary team.[108] Strong communication skills foster a supportive work environment and colleagial relationships that benefit both patients and nursing staff.
Consider the fundamentals of good communication practices. Effective communication requires each interaction to include a sender of the message, a clear and concise message, and a receiver who can decode and interpret that message. The receiver also provides a feedback message back to the sender in response to the received message. See Figure 3.1[109] for an image of effective communication between a sender and receiver. This feedback message is referred to as closed-loop communication in health care settings. Closed-loop communication enables the person giving the instructions to hear what they said reflected back and to confirm that their message was received correctly. It also allows the person receiving the instructions to verify and confirm the actions to be taken. If closed-loop communication is not used, the receiver may nod or say “OK,” and the sender may assume the message has been effectively transmitted, but this may not be the case and can lead to errors and client harm.
An example of closed-loop communication can be found in the following exchange:
- RN: “Jane, can you get a set of vitals on Mr. Smith and let me know if the results are outside of normal range?”
- Jane, CNA: “OK, I’ll get a set of vitals on Mr. Smith and let you know if they are out of range.”
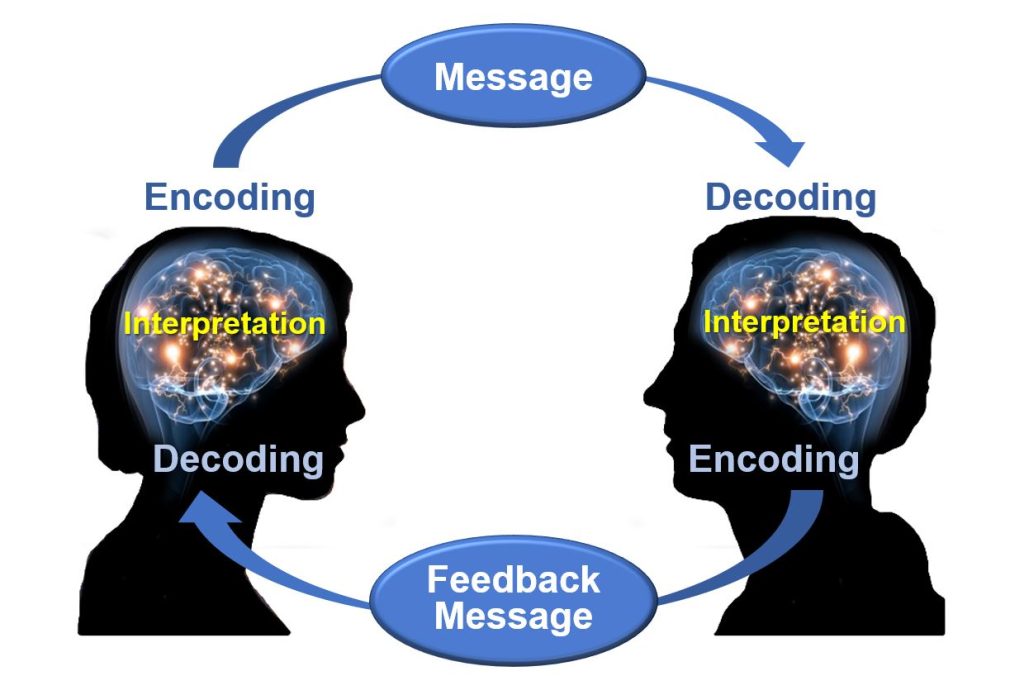
Closed-loop communication is vital for communication among health care team members to avoid misunderstandings that can cause unsafe client care. According to the HIPAA Journal, poor communication leads to a “reduction in the quality of care, poor client outcomes, wastage of resources, and high health care costs.”[110] Parameters for reporting results and the results that should be expected are often left unsaid rather than spelled out in sufficient detail. It is imperative for the RN to provide clear, complete, concise instructions when delegating. A lack of clarity can lead to misunderstanding, unfinished tasks, incomplete care, and/or medical errors.[111]
Effective communication is at the core of proper assignment, delegation, and supervision. With effective communication at the beginning of every shift, each nursing team member should have a clear plan for their shift, what to do and why, and what and when to report to the RN or team leader. Communication should continue throughout the shift as tasks are accomplished and patients’ needs change. Effective communication improves client outcomes and satisfaction scores, as well as improving team morale by enhancing the collaborative relationships of the health care team.
The RN is accountable for clear, concise, correct, and complete communication when making assignments and delegating, both initially and throughout the shift. These communication characteristics can be remembered by using the mnemonic the "4 Cs":
- Clear: Information is understood by the listener. Asking the listener to restate the instructions and the plan can be helpful to determine whether the communication is clear.
- Concise: Sufficient information should be provided to accurately perform the task, but excessive or irrelevant information should be avoided because it can confuse the listener and waste precious time.
- Correct: Correct communication is not vague or confusing. Accurate information is also aligned with agency policy and the team member’s scope of practice as defined by their state’s Nurse Practice Act and other state regulations.
- Complete: Complete instructions leave no room for doubt. Always ask if further information or clarification is needed, especially regarding tasks that are infrequently performed or include unique instructions.[112]
The use of closed-loop communication is the best method to achieve clear, concise, correct, and complete information exchanged among team members. Closed-loop communication allows team members the opportunity to verify and validate the exchange of information. By repeating back information, members confirm the exchange has occurred, understanding is clear, and expectations are heard.
Closed-loop communication should also be used when the RN is receiving a verbal order from a provider. For example, when the resuscitation team leader gives a verbal order of “Epinephrine 1 mg/mL IV push now,” the RN confirms correct understanding of the order by repeating back, “I will prepare Epinephrine 1 mg/mL to be given IV push now.” After the provider confirms the verbal order and the task is completed, the nurse confirms completion of the task by stating, “Epinephrine 1 mg/mL IV push was administered.”
In addition to using closed-loop communication, a common format used by health care team members to exchange client information is ISBARR, a mnemonic for the components of Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat Back. ISBARR and other communication strategies are discussed in more detail in the "Interprofessional Communication" section of the "Collaboration Within the Interprofessional Team" chapter.
Nursing team members working in inpatient or long-term care settings receive patient assignments at the start of their shift. Assignment refers to routine care, activities, and procedures that are within the legal scope of practice of registered nurses (RN), licensed practical/vocational nurses (LPN/VN), or assistive personnel (AP).[113] Scope of practice for RNs and LPNs is described in each state's Nurse Practice Act. Care tasks for AP vary by state; regulations are typically listed on sites for the state's Board of Nursing, Department of Health, Department of Aging, Department of Health Professions, Department of Commerce, or Office of Long-Term Care.[114]
See Table 3.3a for common tasks performed by members of the nursing team based on their scope of practice. These tasks are within the traditional role and training the team member has acquired through a basic educational program. They are also within the expectations of the health care agency during a shift of work. Agency policy can be more restrictive than federal or state regulations, but it cannot be less restrictive.
Patient assignments are typically made by the charge nurse (or nurse supervisor) from the previous shift. A charge nurse is an RN who provides leadership on a patient-care unit within a health care facility during their shift. Charge nurses perform many of the tasks that general nurses do, but also have some supervisory duties such as making assignments, delegating tasks, preparing schedules, monitoring admissions and discharges, and serving as a staff member resource.[115]
Table 3.3a. Nursing Team Members’ Scope of Practice and Common Tasks[116]
| Nursing Team Member | Scope of Practice | Common Tasks
|
|---|---|---|
| RN |
|
|
| LPN/VN |
|
Tasks That Potentially Can Be Delegated According to the Five Rights of Delegation:
|
| AP |
|
|
An example of a patient assignment is when an RN assigns an LPN/VN to care for a client with stable heart failure. The LPN/VN collects assessment data, monitors intake/output throughout the shift, and administers routine oral medication. The LPN/VN documents this information and reports information back to the RN. This is considered the LPN/VN’s “assignment” because the skills are taught within an LPN educational program and are consistent with the state’s Nurse Practice Act for LPN/VN scope of practice. They are also included in the unit’s job description for an LPN/VN. The RN may also assign some care for this client to AP. These tasks may include assistance with personal hygiene, toileting, and ambulation. The AP documents these tasks as they are completed and reports information back to the RN or LPN/VN. These tasks are considered the AP’s assignment because they are taught within a nursing aide's educational program, are consistent with the AP's scope of practice for that state, and are included in the job description for the nursing aide's role in this unit. The RN continues to be accountable for the care provided to this client despite the assignments made to other nursing team members.
Special consideration is required for AP with additional training. With increased staffing needs, skills such as administering medications, inserting Foley catheters, or performing injections are included in specialized training programs for AP. Due to the impact these skills can have on the outcome and safety of the client, the National Council of State Board of Nursing (NCSBN) recommends these activities be considered delegated tasks by the RN or nurse leader. By delegating these advanced skills when appropriate, the nurse validates competency, provides supervision, and maintains accountability for client outcomes. Read more about delegation in the “Delegation” section of this chapter.
When making assignments to other nursing team members, it is essential for the RN to keep in mind specific tasks that cannot be delegated to other nursing team members based on federal and/or state regulations. These tasks include, but are not limited to, those tasks described in Table 3.3b.
Table 3.3b. Examples of Tasks Outside the Scope of Practice of Nursing Assistive Personnel
| Nursing Team Member | Tasks That Cannot Be Delegated
|
|---|---|
| LPN/VN |
|
| Assistive Personnel (AP) |
|
As always, refer to each state’s Nurse Practice Act and other state regulations for specific details about nursing team members’ scope of practice when providing care in that state.
Find and review Nurse Practice Acts by state at https://www.ncsbn.org/policy/npa.page.
Read more about the Wisconsin's Nurse Practice Act and the standards and scope of practice for RNs and LPNs at Wisconsin's Legislative Code Chapter N6.
Read more about scope of practice, skills, and practices of nurse aides in Wisconsin at DHS 129.07 Standards for Nurse Aide Training Programs.
Nursing team members working in inpatient or long-term care settings receive patient assignments at the start of their shift. Assignment refers to routine care, activities, and procedures that are within the legal scope of practice of registered nurses (RN), licensed practical/vocational nurses (LPN/VN), or assistive personnel (AP).[118] Scope of practice for RNs and LPNs is described in each state's Nurse Practice Act. Care tasks for AP vary by state; regulations are typically listed on sites for the state's Board of Nursing, Department of Health, Department of Aging, Department of Health Professions, Department of Commerce, or Office of Long-Term Care.[119]
See Table 3.3a for common tasks performed by members of the nursing team based on their scope of practice. These tasks are within the traditional role and training the team member has acquired through a basic educational program. They are also within the expectations of the health care agency during a shift of work. Agency policy can be more restrictive than federal or state regulations, but it cannot be less restrictive.
Patient assignments are typically made by the charge nurse (or nurse supervisor) from the previous shift. A charge nurse is an RN who provides leadership on a patient-care unit within a health care facility during their shift. Charge nurses perform many of the tasks that general nurses do, but also have some supervisory duties such as making assignments, delegating tasks, preparing schedules, monitoring admissions and discharges, and serving as a staff member resource.[120]
Table 3.3a. Nursing Team Members’ Scope of Practice and Common Tasks[121]
| Nursing Team Member | Scope of Practice | Common Tasks
|
|---|---|---|
| RN |
|
|
| LPN/VN |
|
Tasks That Potentially Can Be Delegated According to the Five Rights of Delegation:
|
| AP |
|
|
An example of a patient assignment is when an RN assigns an LPN/VN to care for a client with stable heart failure. The LPN/VN collects assessment data, monitors intake/output throughout the shift, and administers routine oral medication. The LPN/VN documents this information and reports information back to the RN. This is considered the LPN/VN’s “assignment” because the skills are taught within an LPN educational program and are consistent with the state’s Nurse Practice Act for LPN/VN scope of practice. They are also included in the unit’s job description for an LPN/VN. The RN may also assign some care for this client to AP. These tasks may include assistance with personal hygiene, toileting, and ambulation. The AP documents these tasks as they are completed and reports information back to the RN or LPN/VN. These tasks are considered the AP’s assignment because they are taught within a nursing aide's educational program, are consistent with the AP's scope of practice for that state, and are included in the job description for the nursing aide's role in this unit. The RN continues to be accountable for the care provided to this client despite the assignments made to other nursing team members.
Special consideration is required for AP with additional training. With increased staffing needs, skills such as administering medications, inserting Foley catheters, or performing injections are included in specialized training programs for AP. Due to the impact these skills can have on the outcome and safety of the client, the National Council of State Board of Nursing (NCSBN) recommends these activities be considered delegated tasks by the RN or nurse leader. By delegating these advanced skills when appropriate, the nurse validates competency, provides supervision, and maintains accountability for client outcomes. Read more about delegation in the “Delegation” section of this chapter.
When making assignments to other nursing team members, it is essential for the RN to keep in mind specific tasks that cannot be delegated to other nursing team members based on federal and/or state regulations. These tasks include, but are not limited to, those tasks described in Table 3.3b.
Table 3.3b. Examples of Tasks Outside the Scope of Practice of Nursing Assistive Personnel
| Nursing Team Member | Tasks That Cannot Be Delegated
|
|---|---|
| LPN/VN |
|
| Assistive Personnel (AP) |
|
As always, refer to each state’s Nurse Practice Act and other state regulations for specific details about nursing team members’ scope of practice when providing care in that state.
Find and review Nurse Practice Acts by state at https://www.ncsbn.org/policy/npa.page.
Read more about the Wisconsin's Nurse Practice Act and the standards and scope of practice for RNs and LPNs at Wisconsin's Legislative Code Chapter N6.
Read more about scope of practice, skills, and practices of nurse aides in Wisconsin at DHS 129.07 Standards for Nurse Aide Training Programs.
There has been significant national debate over the difference between assignment and delegation over the past few decades. In 2019 the National Council of State Boards of Nursing (NCSBN) and the American Nurses Association (ANA) published updated joint National Guidelines on Nursing Delegation (NGND).[123] These guidelines apply to all levels of nursing licensure (advanced practice registered nurses [APRN], registered nurses [RN], and licensed practical/vocational nurses [LPN/VN]) when delegating when there is no specific guidance provided by the state’s Nurse Practice Act (NPA).[124] It is important to note that states have different laws and rules/regulations regarding delegation, so it is the responsibility of all licensed nurses to know what is permitted in their jurisdiction.
The NGND defines a delegatee as an RN, LPN/VN, or AP who is delegated a nursing responsibility by either an APRN, RN, or LPN/VN, is competent to perform the task, and verbally accepts the responsibility.[125] Delegation is allowing a delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role and not routinely performed, but the individual has obtained additional training and validated their competence to perform the delegated responsibility.[126] However, the licensed nurse still maintains accountability for overall client care. Delegated responsibility is a nursing activity, skill, or procedure that is transferred from a licensed nurse to a delegatee.[127] Accountability is defined as being answerable to oneself and others for one’s own choices, decisions, and actions as measured against a standard. Therefore, if a nurse does not feel it is appropriate to delegate a certain responsibility to a delegatee, the delegating nurse should perform the activity themselves.[128]
Delegation is summarized in the NGND as the following[129]:
- A delegatee is allowed to perform a specific nursing activity, skill, or procedure that is outside the traditional role and basic responsibilities of the delegatee’s current job.
- The delegatee has obtained the additional education and training and validated competence to perform the care/delegated responsibility. The context and processes associated with competency validation will be different for each activity, skill, or procedure being delegated. Competency validation should be specific to the knowledge and skill needed to safely perform the delegated responsibility, as well as to the level of the practitioner (e.g., RN, LPN/VN, AP) to whom the activity, skill, or procedure has been delegated. The licensed nurse who delegates the “responsibility” maintains overall accountability for the client, but the delegatee bears the responsibility for completing the delegated activity, skill, or procedure.
- The licensed nurse cannot delegate nursing clinical judgment or any activity that will involve nursing clinical judgment or critical decision-making to AP.
- Nursing responsibilities are delegated by a licensed nurse who has the authority to delegate and the delegated responsibility is within the delegator’s scope of practice.
An example of delegation is medication administration that is delegated by a licensed nurse to AP with additional training in some agencies, according to agency policy. This task is outside the traditional role of AP, but the delegatee has received additional training for this delegated responsibility and has completed competency validation in completing this task accurately.
An example illustrating the difference between assignment and delegation is assisting patients with eating. Feeding patients is typically part of the routine role of AP. However, if a client has recently experienced a stroke (i.e., cerebrovascular accident) or is otherwise experiencing swallowing difficulties (e.g., dysphagia), this task cannot be assigned to AP because it is not considered routine care. Instead, the RN should perform this task themselves or delegate it to an AP who has received additional training on feeding assistance.
The delegation process is multifaceted. See Figure 3.2[130] for an illustration of the intersecting responsibilities of the employer/nurse leader, licensed nurse, and delegatee with two-way communication that protects the safety of the public. “Delegation begins at the administrative/nurse leader level of the organization and includes determining nursing responsibilities that can be delegated, to whom, and under what circumstances; developing delegation policies and procedures; periodically evaluating delegation processes; and promoting a positive culture/work environment. The licensed nurse is responsible for determining client needs and when to delegate, ensuring availability to the delegatee, evaluating outcomes, and maintaining accountability for delegated responsibility. Finally, the delegatee must accept activities based on their competency level, maintain competence for delegated responsibility, and maintain accountability for delegated activity.”[131]
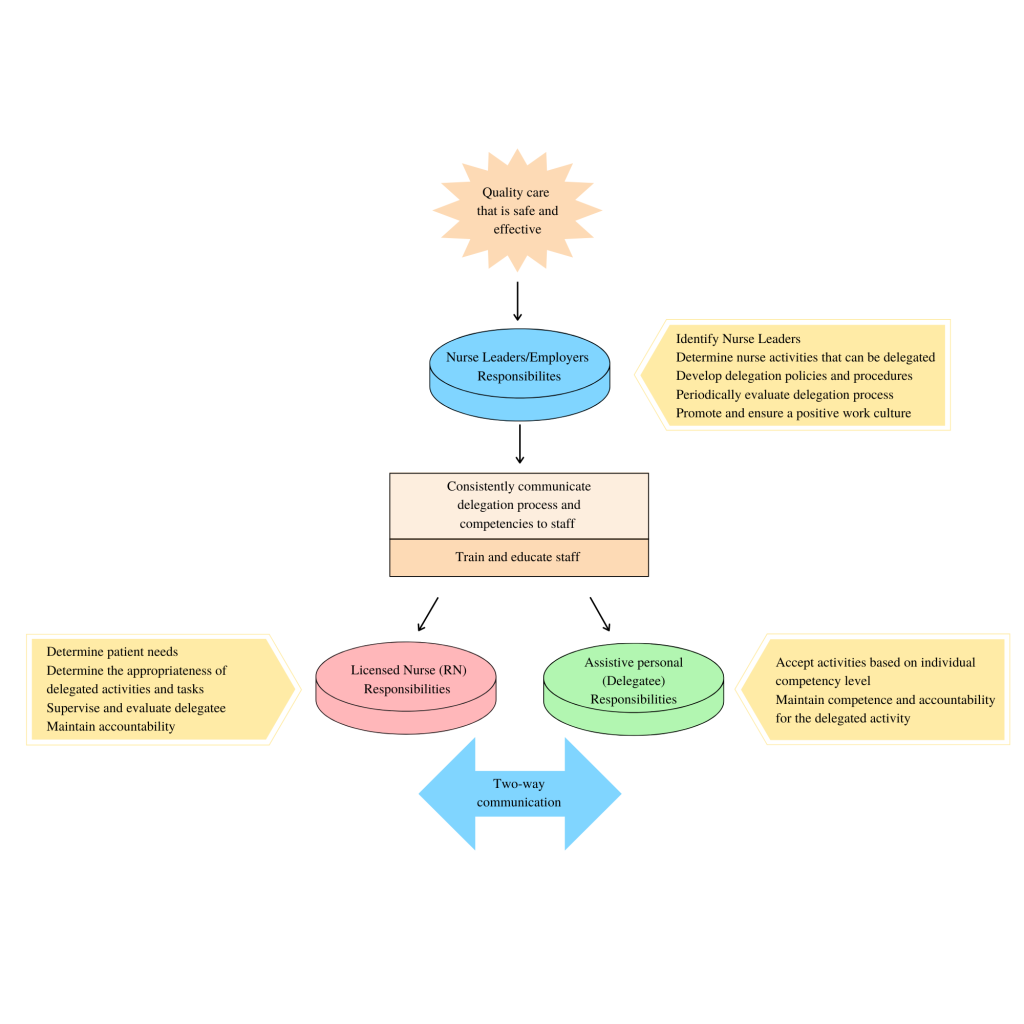
Five Rights of Delegation
How does the RN determine what tasks can be delegated, when, and to whom? According to the National Council of State Boards of Nursing (NCSBN), RNs should use the five rights of delegation to ensure proper and appropriate delegation: right task, right circumstance, right person, right directions and communication, and right supervision and evaluation[132]:
- Right task: The activity falls within the delegatee’s job description or is included as part of the established policies and procedures of the nursing practice setting. The facility needs to ensure the policies and procedures describe the expectations and limits of the activity and provide any necessary competency training.
- Right circumstance: The health condition of the client must be stable. If the client’s condition changes, the delegatee must communicate this to the licensed nurse, and the licensed nurse must reassess the situation and the appropriateness of the delegation.[133]
- Right person: The licensed nurse, along with the employer and the delegatee, is responsible for ensuring that the delegatee possesses the appropriate skills and knowledge to perform the activity.[134]
- Right directions and communication: Each delegation situation should be specific to the client, the nurse, and the delegatee. The licensed nurse is expected to communicate specific instructions for the delegated activity to the delegatee; the delegatee, as part of two-way communication, should ask any clarifying questions. This communication includes any data that need to be collected, the method for collecting the data, the time frame for reporting the results to the licensed nurse, and additional information pertinent to the situation. The delegatee must understand the terms of the delegation and must agree to accept the delegated activity. The licensed nurse should ensure the delegatee understands they cannot make any decisions or modifications in carrying out the activity without first consulting the licensed nurse.[135]
- Right supervision and evaluation: The licensed nurse is responsible for monitoring the delegated activity, following up with the delegatee at the completion of the activity, and evaluating client outcomes. The delegatee is responsible for communicating client information to the licensed nurse during the delegation situation. The licensed nurse should be ready and available to intervene as necessary. The licensed nurse should ensure appropriate documentation of the activity is completed.[136]
Simply stated, the licensed nurse determines the right person is assigned the right tasks for the right clients under the right circumstances. When determining what aspects of care can be delegated, the licensed nurse uses clinical judgment while considering the client’s current clinical condition, as well as the abilities of the health care team member. The RN must also consider if the circumstances are appropriate for delegation. For example, although obtaining routine vital signs on stable clients may be appropriate to delegate to assistive personnel, obtaining vital signs on an unstable client is not appropriate to delegate.
After the decision has been made to delegate, the nurse assigning the tasks must communicate appropriately with the delegatee and provide the right directions and supervision. Communication is key to successful delegation. Clear, concise, and closed-loop communication is essential to ensure successful completion of the delegated task in a safe manner. During the final step of delegation, also referred to as supervision, the nurse verifies and evaluates that the task was performed correctly, appropriately, safely, and competently. Read more about supervision in the following section on “Supervision.” See Table 3.4 for additional questions to consider for each “right” of delegation.
Table 3.4. Rights of Delegation[137]
| Rights of Delegation | Description | Questions to Consider When Delegating |
|---|---|---|
| Right Task | A task that can be transferred to a member of the nursing team for a specific client. |
|
| Right Circumstances | The client is stable. |
|
| Right Person | The person delegating the task has the appropriate scope of practice to do so. The task is also appropriate for this delegatee’s skills and knowledge. |
|
| Right Directions and Communication | The task or activity is clearly defined and described. |
|
| Right Supervision and Evaluation | The RN appropriately monitors the delegated activity, evaluates client outcomes, and follows up with the delegatee at the completion of the activity. |
|
Keep in mind that any nursing intervention that requires specific nursing knowledge, clinical judgment, or use of the nursing process can only be delegated to another RN. Examples of these types of tasks include initial preoperative or admission assessments, client teaching, and creation and evaluation of a nursing care plan. See Figure 3.3[138] for an algorithm based on the 2019 National Guidelines for Nursing Delegation that can be used when deciding if a nursing task can be delegated.[139]
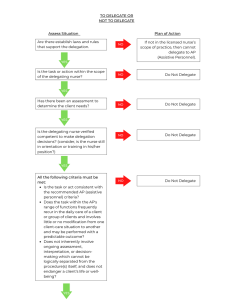
Responsibilities of the Licensed Nurse
The licensed nurse has several responsibilities as part of the delegation process. According to the NGND, any decision to delegate a nursing responsibility must be based on the needs of the client or population, the stability and predictability of the client’s condition, the documented training and competence of the delegatee, and the ability of the licensed nurse to supervise the delegated responsibility and its outcome with consideration to the available staff mix and client acuity. Additionally, the licensed nurse must consider the state Nurse Practice Act regarding delegation and the employer’s policies and procedures prior to making a final decision to delegate. Licensed nurses must be aware that delegation is at the nurse’s discretion, with consideration of the particular situation. The licensed nurse maintains accountability for the client, while the delegatee is responsible for the delegated activity, skill, or procedure. If, under the circumstances, a nurse does not feel it is appropriate to delegate a certain responsibility to a delegatee, the delegating nurse should perform the activity.[140]
1. The licensed nurse must determine when and what to delegate based on the practice setting, the client’s needs and condition, the state's/jurisdiction’s provisions for delegation, and the employer’s policies and procedures regarding delegating a specific responsibility. The licensed nurse must determine the needs of the client and whether those needs are matched by the knowledge, skills, and abilities of the delegatee and can be performed safely by the delegatee. The licensed nurse cannot delegate any activity that requires clinical reasoning, nursing judgment, or critical decision-making. The licensed nurse must ultimately make the final decision whether an activity is appropriate to delegate to the delegatee based on the “Five Rights of Delegation.”
- Rationale: The licensed nurse, who is present at the point of care, is in the best position to assess the needs of the client and what can or cannot be delegated in specific situations.[141]
2. The licensed nurse must communicate with the delegatee who will be assisting in providing client care. This should include reviewing the delegatee’s assignment and discussing delegated responsibilities, including information on the client’s condition/stability, any specific information pertaining to a certain client (e.g., no blood draws in the right arm), and any specific information about the client’s condition that should be communicated back to the licensed nurse by the delegatee.
- Rationale: Communication must be a two-way process involving both the licensed nurse delegating the activity and the delegatee being delegated the responsibility. Evidence shows that the better the communication between the nurse and the delegatee, the more optimal the outcome. The licensed nurse must provide information about the client and care requirements. This includes any specific issues related to any delegated responsibilities. These instructions should include any unique client requirements. The licensed nurse must instruct the delegatee to regularly communicate the status of the client.[142]
3. The licensed nurse must be available to the delegatee for guidance and questions, including assisting with the delegated responsibility, if necessary, or performing it themselves if the client’s condition or other circumstances warrant doing so.
- Rationale: Delegation calls for nursing judgment throughout the process. The final decision to delegate rests in the hands of the licensed nurse as they have overall accountability for the client.[143]
4. The licensed nurse must follow up with the delegatee and the client after the delegated responsibility has been completed.
- Rationale: The licensed nurse who delegates the “responsibility” maintains overall accountability for the client, while the delegatee is responsible for the delegated activity, skill, or procedure.[144]
5. The licensed nurse must provide feedback information about the delegation process and any issues regarding delegatee competence level to the nurse leader. Licensed nurses in the facility need to communicate to the nurse leader responsible for delegation any issues arising related to delegation and any individual whom they identify as not being competent in a specific responsibility or unable to use good judgment and decision-making.
- Rationale: This will allow the nurse leader responsible for delegation to develop a plan to address the situation.[145]
The decision of whether or not to delegate or assign is based on the RN’s judgment concerning the condition of the client, the competence of the nursing team member, and the degree of supervision that will be required of the RN if a task is delegated.[146]
Responsibilities of the Delegatee
Everyone is responsible for the well-being of clients. While the nurse is ultimately accountable for the overall care provided to a client, the delegatee shares the responsibility for the client and is fully responsible for the delegated activity, skill, or procedure.[147] The delegatee has the following responsibilities:
1. The delegatee must accept only the delegated responsibilities that they are appropriately trained and educated to perform and feel comfortable doing given the specific circumstances in the health care setting and client’s condition. The delegatee should confirm acceptance of the responsibility to carry out the delegated activity. If the delegatee does not believe they have the appropriate competency to complete the delegated responsibility, then the delegatee should not accept the delegated responsibility. This includes informing the nursing leadership if they do not feel they have received adequate training to perform the delegated responsibility, do not perform the procedure frequently enough to do it safely, or their knowledge and skills need updating.
- Rationale: The delegatee shares the responsibility to keep clients safe, and this includes only performing activities, skills, or procedures in which they are competent and comfortable doing.[148]
2. The delegatee must maintain competency for the delegated responsibility.
- Rationale: Competency is an ongoing process. Even if properly taught, the delegatee may become less competent if they do not frequently perform the procedure. Given that the delegatee shares the responsibility for the client, the delegatee also has a responsibility to maintain competency.[149]
3. The delegatee must communicate with the licensed nurse in charge of the client. This includes any questions related to the delegated responsibility and follow-up on any unusual incidents that may have occurred while the delegatee was performing the delegated responsibility, any concerns about a client’s condition, and any other information important to the client’s care.
- Rationale: The delegatee is a partner in providing client care. They are interacting with the client/family and caring for the client. This information and two-way communication are important for successful delegation and optimal outcomes for the client.[150]
4. Once the delegatee verifies acceptance of the delegated responsibility, the delegatee is accountable for carrying out the delegated responsibility correctly and completing timely and accurate documentation per facility policy.
- Rationale: The delegatee cannot delegate to another individual. If the delegatee is unable to complete the responsibility or feels as though they need assistance, the delegatee should inform the licensed nurse immediately so the licensed nurse can assess the situation and provide support. Only the licensed nurse can determine if it is appropriate to delegate the activity to another individual. If at any time the licensed nurse determines they need to perform the delegated responsibility, the delegatee must relinquish responsibility upon request of the licensed nurse.[151]
Responsibilities of the Employer/Nurse Leader
The employer and nurse leaders also have responsibilities related to safe delegation of client care:
1. The employer must identify a nurse leader responsible for oversight of delegated responsibilities for the facility. If there is only one licensed nurse within the practice setting, that licensed nurse must be responsible for oversight of delegated responsibilities for the facility.
- Rationale: The nurse leader has the ability to assess the needs of the facility, understand the type of knowledge and skill needed to perform a specific nursing responsibility, and be accountable for maintaining a safe environment for clients. They are also aware of the knowledge, skill level, and limitations of the licensed nurses and AP. Additionally, the nurse leader is positioned to develop appropriate staffing models that take into consideration the need for delegation. Therefore, the decision to delegate begins with a thorough assessment by a nurse leader designated by the institution to oversee the process.[152]
2. The designated nurse leader responsible for delegation, ideally with a committee (consisting of other nurse leaders) formed for the purposes of addressing delegation, must determine which nursing responsibilities may be delegated, to whom, and under what circumstances. The nurse leader must be aware of the state Nurse Practice Act and the laws/rules and regulations that affect the delegation process and ensure all institutional policies are in accordance with the law.
- Rationale: A systematic approach to the delegation process fosters communication and consistency of the process throughout the facility.[153]
3. Policies and procedures for delegation must be developed. The employer/nurse leader must outline specific responsibilities that can be delegated and to whom these responsibilities can be delegated. The policies and procedures should also indicate what may not be delegated. The employer must periodically review the policies and procedures for delegation to ensure they remain consistent with current nursing practice trends and that they are consistent with the state Nurse Practice Act. (Institution/employer policies can be more restrictive, but not less restrictive.)
- Rationale: Policies and procedures standardize the appropriate method of care and ensure safe practices. Having a policy and procedure specific to delegation and delegated responsibilities eliminates questions from licensed nurses and AP about what can be delegated and how they should be performed.[154]
4. The employer/nurse leader must communicate information about delegation to the licensed nurses and AP and educate them about what responsibilities can be delegated. This information should include the competencies of delegatees who can safely perform a specific nursing responsibility.
- Rationale: Licensed nurses must be aware of the competence level of staff and expectations for delegation (as described within the policies and procedures) to make informed decisions on whether or not delegation is appropriate for the given situahttps://www.nursingworld.org/content-hub/resources/nursing-leadership/delegation-in-nursing/tion. Licensed nurses maintain accountability for the client. However, the delegatee has responsibility for the delegated activity, skill, or procedure.
In summary, delegation is the transfer of the nurse’s responsibility for a task while retaining professional accountability for the client’s overall outcome. The decision to delegate is based on the nurse’s judgment, the act of delegation must be clearly defined by the nurse, and the outcomes of delegation are an extension of the nurse’s guidance and supervision. Delegation, when rooted in mutual respect and trust, is a key component to an effective health care team.
Delegation is an integral skill in the nursing profession to help manage the complexities of the dynamic and ever-changing health care environment. Delegation in nursing has been found to increase employee empowerment, decrease burnout, increase role commitment, and improve job satisfaction.[155] Cultivating delegation skills helps nurses better manage the complexities of their client care role, ensuring that their clients are safely cared for and outcomes are optimized. Delegation skills, like other nursing skills, require purposeful development and do not necessarily come easily when first transitioning into the nursing role. It is important that the new graduate nurse does not mistake delegation for pompous or arrogant behavior. Delegation requires mutual respect between the delegator and delegatee. Delegation is not seen as a sign or weakness and does not reflect one's desire to shirk their work responsibilities. Instead, delegation reflects strong leadership and organizational skills in which the nurse leader demonstrates that they understand how to leverage their team's strengths in order to achieve optimal care outcomes.
To help avoid any perception of arrogance in the delegation of an activity, it is important that the new graduate nurse approaches the task of delegation with humility. Clarity in the communication of the delegated responsibility is critical, and the rationale behind the delegation should be communicated to the delegatee. Within the task of delegation, the delegator should express appreciation for the delegatee and their contributions in the collaborative health care environment. Additionally, it is important to understand that no specific nurse delegated task is outside of the "nurse" role. For example, ambulating a client does not to an unlicensed assistive personnel simply because that individual is able to perform that task. Rather, nurses must be willing to perform delegated tasks themselves when necessary. This reflects a team-oriented mindset and helps to reinforce among the care team that all roles are critical to optimizing client care. For new graduate nurses who first transition into a specific health care setting, having the opportunity to shadow individuals in various work roles helps to foster a team mindset. Asking questions of various team members regarding their work role can help a new graduate nurse demonstrate respect and value for other roles.
Examples of helpful questions may include the following:
- "What is the biggest challenge in your typical workday?"
- "What do you most enjoy about your job?"
- "How is it best to communicate with you when the unit is busy?"
- "What do you think people misunderstand most about your role?"
It is important to ensure that the team understands that care is optimized when they function as one collective unit and not in siloed roles. Each team member must feel valued and competent in their role. By understanding and practicing strategic delegation, new graduate nurses can overcome any misconceptions of arrogance and contribute positively to the healthcare team.
Please review the example below to consider variation in approach to task delegation.
Scenario A: Nurse June, a newly graduated nurse, is working in a busy hospital unit. She needs an unlicensed assistive personnel (UAP), Alex, to take vital signs of a patient. Nurse June approaches Alex in the hallway and says in an abrupt tone, "Alex, I need you to take Mr. Smith's vital signs right now. I'm too busy to do it myself, and besides, that's what you're here for. Just get it done quickly."
Analysis: June’s tone and words suggest she sees Alex's role as less important and purely as a means to offload her tasks. June does not explain the urgency or importance of the task. June doesn’t acknowledge Alex's effort or capability, making the request seem like a command rather than a collaborative effort.
Scenario B: Nurse June, a newly graduated nurse, is working in a busy hospital unit. She needs an unlicensed assistive personnel (UAP), Alex, to take vital signs of a patient. Nurse June approaches Alex and says, "Hi Alex, could you please help me by taking Mr. Smith's vital signs? I'm handling a few urgent matters right now, and it would really help to have your support. I know you’re great at this, and your thoroughness really makes a difference in our patient care. Thank you so much!"
Analysis: June speaks to Alex with courtesy and acknowledges the value of his role. June clearly explains why she needs Alex's help and the importance of the task. June acknowledges Alex’s competence and expresses gratitude, fostering feelings of value and respect.
There has been significant national debate over the difference between assignment and delegation over the past few decades. In 2019 the National Council of State Boards of Nursing (NCSBN) and the American Nurses Association (ANA) published updated joint National Guidelines on Nursing Delegation (NGND).[156] These guidelines apply to all levels of nursing licensure (advanced practice registered nurses [APRN], registered nurses [RN], and licensed practical/vocational nurses [LPN/VN]) when delegating when there is no specific guidance provided by the state’s Nurse Practice Act (NPA).[157] It is important to note that states have different laws and rules/regulations regarding delegation, so it is the responsibility of all licensed nurses to know what is permitted in their jurisdiction.
The NGND defines a delegatee as an RN, LPN/VN, or AP who is delegated a nursing responsibility by either an APRN, RN, or LPN/VN, is competent to perform the task, and verbally accepts the responsibility.[158] Delegation is allowing a delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role and not routinely performed, but the individual has obtained additional training and validated their competence to perform the delegated responsibility.[159] However, the licensed nurse still maintains accountability for overall client care. Delegated responsibility is a nursing activity, skill, or procedure that is transferred from a licensed nurse to a delegatee.[160] Accountability is defined as being answerable to oneself and others for one’s own choices, decisions, and actions as measured against a standard. Therefore, if a nurse does not feel it is appropriate to delegate a certain responsibility to a delegatee, the delegating nurse should perform the activity themselves.[161]
Delegation is summarized in the NGND as the following[162]:
- A delegatee is allowed to perform a specific nursing activity, skill, or procedure that is outside the traditional role and basic responsibilities of the delegatee’s current job.
- The delegatee has obtained the additional education and training and validated competence to perform the care/delegated responsibility. The context and processes associated with competency validation will be different for each activity, skill, or procedure being delegated. Competency validation should be specific to the knowledge and skill needed to safely perform the delegated responsibility, as well as to the level of the practitioner (e.g., RN, LPN/VN, AP) to whom the activity, skill, or procedure has been delegated. The licensed nurse who delegates the “responsibility” maintains overall accountability for the client, but the delegatee bears the responsibility for completing the delegated activity, skill, or procedure.
- The licensed nurse cannot delegate nursing clinical judgment or any activity that will involve nursing clinical judgment or critical decision-making to AP.
- Nursing responsibilities are delegated by a licensed nurse who has the authority to delegate and the delegated responsibility is within the delegator’s scope of practice.
An example of delegation is medication administration that is delegated by a licensed nurse to AP with additional training in some agencies, according to agency policy. This task is outside the traditional role of AP, but the delegatee has received additional training for this delegated responsibility and has completed competency validation in completing this task accurately.
An example illustrating the difference between assignment and delegation is assisting patients with eating. Feeding patients is typically part of the routine role of AP. However, if a client has recently experienced a stroke (i.e., cerebrovascular accident) or is otherwise experiencing swallowing difficulties (e.g., dysphagia), this task cannot be assigned to AP because it is not considered routine care. Instead, the RN should perform this task themselves or delegate it to an AP who has received additional training on feeding assistance.
The delegation process is multifaceted. See Figure 3.2[163] for an illustration of the intersecting responsibilities of the employer/nurse leader, licensed nurse, and delegatee with two-way communication that protects the safety of the public. “Delegation begins at the administrative/nurse leader level of the organization and includes determining nursing responsibilities that can be delegated, to whom, and under what circumstances; developing delegation policies and procedures; periodically evaluating delegation processes; and promoting a positive culture/work environment. The licensed nurse is responsible for determining client needs and when to delegate, ensuring availability to the delegatee, evaluating outcomes, and maintaining accountability for delegated responsibility. Finally, the delegatee must accept activities based on their competency level, maintain competence for delegated responsibility, and maintain accountability for delegated activity.”[164]
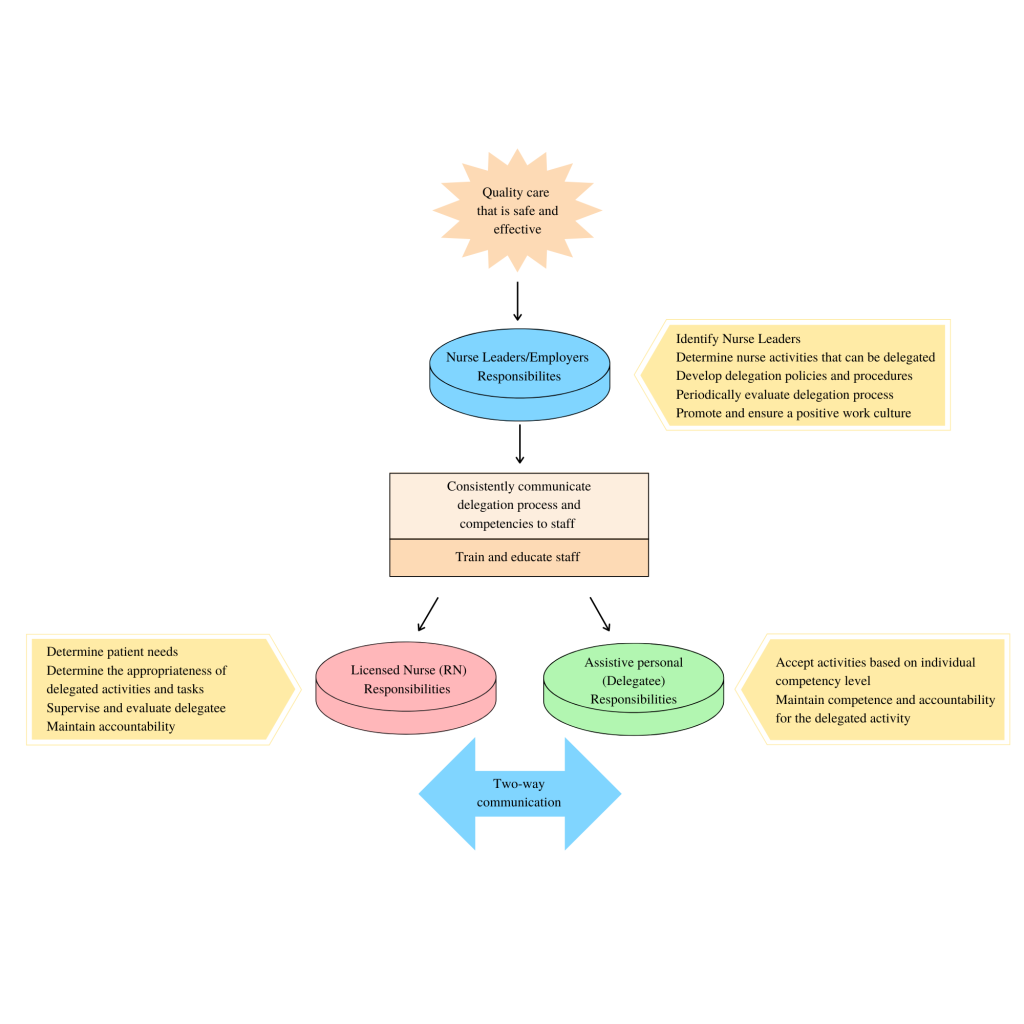
Five Rights of Delegation
How does the RN determine what tasks can be delegated, when, and to whom? According to the National Council of State Boards of Nursing (NCSBN), RNs should use the five rights of delegation to ensure proper and appropriate delegation: right task, right circumstance, right person, right directions and communication, and right supervision and evaluation[165]:
- Right task: The activity falls within the delegatee’s job description or is included as part of the established policies and procedures of the nursing practice setting. The facility needs to ensure the policies and procedures describe the expectations and limits of the activity and provide any necessary competency training.
- Right circumstance: The health condition of the client must be stable. If the client’s condition changes, the delegatee must communicate this to the licensed nurse, and the licensed nurse must reassess the situation and the appropriateness of the delegation.[166]
- Right person: The licensed nurse, along with the employer and the delegatee, is responsible for ensuring that the delegatee possesses the appropriate skills and knowledge to perform the activity.[167]
- Right directions and communication: Each delegation situation should be specific to the client, the nurse, and the delegatee. The licensed nurse is expected to communicate specific instructions for the delegated activity to the delegatee; the delegatee, as part of two-way communication, should ask any clarifying questions. This communication includes any data that need to be collected, the method for collecting the data, the time frame for reporting the results to the licensed nurse, and additional information pertinent to the situation. The delegatee must understand the terms of the delegation and must agree to accept the delegated activity. The licensed nurse should ensure the delegatee understands they cannot make any decisions or modifications in carrying out the activity without first consulting the licensed nurse.[168]
- Right supervision and evaluation: The licensed nurse is responsible for monitoring the delegated activity, following up with the delegatee at the completion of the activity, and evaluating client outcomes. The delegatee is responsible for communicating client information to the licensed nurse during the delegation situation. The licensed nurse should be ready and available to intervene as necessary. The licensed nurse should ensure appropriate documentation of the activity is completed.[169]
Simply stated, the licensed nurse determines the right person is assigned the right tasks for the right clients under the right circumstances. When determining what aspects of care can be delegated, the licensed nurse uses clinical judgment while considering the client’s current clinical condition, as well as the abilities of the health care team member. The RN must also consider if the circumstances are appropriate for delegation. For example, although obtaining routine vital signs on stable clients may be appropriate to delegate to assistive personnel, obtaining vital signs on an unstable client is not appropriate to delegate.
After the decision has been made to delegate, the nurse assigning the tasks must communicate appropriately with the delegatee and provide the right directions and supervision. Communication is key to successful delegation. Clear, concise, and closed-loop communication is essential to ensure successful completion of the delegated task in a safe manner. During the final step of delegation, also referred to as supervision, the nurse verifies and evaluates that the task was performed correctly, appropriately, safely, and competently. Read more about supervision in the following section on “Supervision.” See Table 3.4 for additional questions to consider for each “right” of delegation.
Table 3.4. Rights of Delegation[170]
| Rights of Delegation | Description | Questions to Consider When Delegating |
|---|---|---|
| Right Task | A task that can be transferred to a member of the nursing team for a specific client. |
|
| Right Circumstances | The client is stable. |
|
| Right Person | The person delegating the task has the appropriate scope of practice to do so. The task is also appropriate for this delegatee’s skills and knowledge. |
|
| Right Directions and Communication | The task or activity is clearly defined and described. |
|
| Right Supervision and Evaluation | The RN appropriately monitors the delegated activity, evaluates client outcomes, and follows up with the delegatee at the completion of the activity. |
|
Keep in mind that any nursing intervention that requires specific nursing knowledge, clinical judgment, or use of the nursing process can only be delegated to another RN. Examples of these types of tasks include initial preoperative or admission assessments, client teaching, and creation and evaluation of a nursing care plan. See Figure 3.3[171] for an algorithm based on the 2019 National Guidelines for Nursing Delegation that can be used when deciding if a nursing task can be delegated.[172]
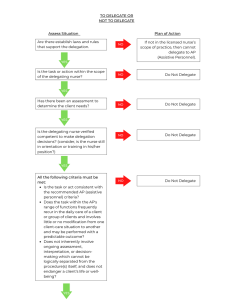
Responsibilities of the Licensed Nurse
The licensed nurse has several responsibilities as part of the delegation process. According to the NGND, any decision to delegate a nursing responsibility must be based on the needs of the client or population, the stability and predictability of the client’s condition, the documented training and competence of the delegatee, and the ability of the licensed nurse to supervise the delegated responsibility and its outcome with consideration to the available staff mix and client acuity. Additionally, the licensed nurse must consider the state Nurse Practice Act regarding delegation and the employer’s policies and procedures prior to making a final decision to delegate. Licensed nurses must be aware that delegation is at the nurse’s discretion, with consideration of the particular situation. The licensed nurse maintains accountability for the client, while the delegatee is responsible for the delegated activity, skill, or procedure. If, under the circumstances, a nurse does not feel it is appropriate to delegate a certain responsibility to a delegatee, the delegating nurse should perform the activity.[173]
1. The licensed nurse must determine when and what to delegate based on the practice setting, the client’s needs and condition, the state's/jurisdiction’s provisions for delegation, and the employer’s policies and procedures regarding delegating a specific responsibility. The licensed nurse must determine the needs of the client and whether those needs are matched by the knowledge, skills, and abilities of the delegatee and can be performed safely by the delegatee. The licensed nurse cannot delegate any activity that requires clinical reasoning, nursing judgment, or critical decision-making. The licensed nurse must ultimately make the final decision whether an activity is appropriate to delegate to the delegatee based on the “Five Rights of Delegation.”
- Rationale: The licensed nurse, who is present at the point of care, is in the best position to assess the needs of the client and what can or cannot be delegated in specific situations.[174]
2. The licensed nurse must communicate with the delegatee who will be assisting in providing client care. This should include reviewing the delegatee’s assignment and discussing delegated responsibilities, including information on the client’s condition/stability, any specific information pertaining to a certain client (e.g., no blood draws in the right arm), and any specific information about the client’s condition that should be communicated back to the licensed nurse by the delegatee.
- Rationale: Communication must be a two-way process involving both the licensed nurse delegating the activity and the delegatee being delegated the responsibility. Evidence shows that the better the communication between the nurse and the delegatee, the more optimal the outcome. The licensed nurse must provide information about the client and care requirements. This includes any specific issues related to any delegated responsibilities. These instructions should include any unique client requirements. The licensed nurse must instruct the delegatee to regularly communicate the status of the client.[175]
3. The licensed nurse must be available to the delegatee for guidance and questions, including assisting with the delegated responsibility, if necessary, or performing it themselves if the client’s condition or other circumstances warrant doing so.
- Rationale: Delegation calls for nursing judgment throughout the process. The final decision to delegate rests in the hands of the licensed nurse as they have overall accountability for the client.[176]
4. The licensed nurse must follow up with the delegatee and the client after the delegated responsibility has been completed.
- Rationale: The licensed nurse who delegates the “responsibility” maintains overall accountability for the client, while the delegatee is responsible for the delegated activity, skill, or procedure.[177]
5. The licensed nurse must provide feedback information about the delegation process and any issues regarding delegatee competence level to the nurse leader. Licensed nurses in the facility need to communicate to the nurse leader responsible for delegation any issues arising related to delegation and any individual whom they identify as not being competent in a specific responsibility or unable to use good judgment and decision-making.
- Rationale: This will allow the nurse leader responsible for delegation to develop a plan to address the situation.[178]
The decision of whether or not to delegate or assign is based on the RN’s judgment concerning the condition of the client, the competence of the nursing team member, and the degree of supervision that will be required of the RN if a task is delegated.[179]
Responsibilities of the Delegatee
Everyone is responsible for the well-being of clients. While the nurse is ultimately accountable for the overall care provided to a client, the delegatee shares the responsibility for the client and is fully responsible for the delegated activity, skill, or procedure.[180] The delegatee has the following responsibilities:
1. The delegatee must accept only the delegated responsibilities that they are appropriately trained and educated to perform and feel comfortable doing given the specific circumstances in the health care setting and client’s condition. The delegatee should confirm acceptance of the responsibility to carry out the delegated activity. If the delegatee does not believe they have the appropriate competency to complete the delegated responsibility, then the delegatee should not accept the delegated responsibility. This includes informing the nursing leadership if they do not feel they have received adequate training to perform the delegated responsibility, do not perform the procedure frequently enough to do it safely, or their knowledge and skills need updating.
- Rationale: The delegatee shares the responsibility to keep clients safe, and this includes only performing activities, skills, or procedures in which they are competent and comfortable doing.[181]
2. The delegatee must maintain competency for the delegated responsibility.
- Rationale: Competency is an ongoing process. Even if properly taught, the delegatee may become less competent if they do not frequently perform the procedure. Given that the delegatee shares the responsibility for the client, the delegatee also has a responsibility to maintain competency.[182]
3. The delegatee must communicate with the licensed nurse in charge of the client. This includes any questions related to the delegated responsibility and follow-up on any unusual incidents that may have occurred while the delegatee was performing the delegated responsibility, any concerns about a client’s condition, and any other information important to the client’s care.
- Rationale: The delegatee is a partner in providing client care. They are interacting with the client/family and caring for the client. This information and two-way communication are important for successful delegation and optimal outcomes for the client.[183]
4. Once the delegatee verifies acceptance of the delegated responsibility, the delegatee is accountable for carrying out the delegated responsibility correctly and completing timely and accurate documentation per facility policy.
- Rationale: The delegatee cannot delegate to another individual. If the delegatee is unable to complete the responsibility or feels as though they need assistance, the delegatee should inform the licensed nurse immediately so the licensed nurse can assess the situation and provide support. Only the licensed nurse can determine if it is appropriate to delegate the activity to another individual. If at any time the licensed nurse determines they need to perform the delegated responsibility, the delegatee must relinquish responsibility upon request of the licensed nurse.[184]
Responsibilities of the Employer/Nurse Leader
The employer and nurse leaders also have responsibilities related to safe delegation of client care:
1. The employer must identify a nurse leader responsible for oversight of delegated responsibilities for the facility. If there is only one licensed nurse within the practice setting, that licensed nurse must be responsible for oversight of delegated responsibilities for the facility.
- Rationale: The nurse leader has the ability to assess the needs of the facility, understand the type of knowledge and skill needed to perform a specific nursing responsibility, and be accountable for maintaining a safe environment for clients. They are also aware of the knowledge, skill level, and limitations of the licensed nurses and AP. Additionally, the nurse leader is positioned to develop appropriate staffing models that take into consideration the need for delegation. Therefore, the decision to delegate begins with a thorough assessment by a nurse leader designated by the institution to oversee the process.[185]
2. The designated nurse leader responsible for delegation, ideally with a committee (consisting of other nurse leaders) formed for the purposes of addressing delegation, must determine which nursing responsibilities may be delegated, to whom, and under what circumstances. The nurse leader must be aware of the state Nurse Practice Act and the laws/rules and regulations that affect the delegation process and ensure all institutional policies are in accordance with the law.
- Rationale: A systematic approach to the delegation process fosters communication and consistency of the process throughout the facility.[186]
3. Policies and procedures for delegation must be developed. The employer/nurse leader must outline specific responsibilities that can be delegated and to whom these responsibilities can be delegated. The policies and procedures should also indicate what may not be delegated. The employer must periodically review the policies and procedures for delegation to ensure they remain consistent with current nursing practice trends and that they are consistent with the state Nurse Practice Act. (Institution/employer policies can be more restrictive, but not less restrictive.)
- Rationale: Policies and procedures standardize the appropriate method of care and ensure safe practices. Having a policy and procedure specific to delegation and delegated responsibilities eliminates questions from licensed nurses and AP about what can be delegated and how they should be performed.[187]
4. The employer/nurse leader must communicate information about delegation to the licensed nurses and AP and educate them about what responsibilities can be delegated. This information should include the competencies of delegatees who can safely perform a specific nursing responsibility.
- Rationale: Licensed nurses must be aware of the competence level of staff and expectations for delegation (as described within the policies and procedures) to make informed decisions on whether or not delegation is appropriate for the given situahttps://www.nursingworld.org/content-hub/resources/nursing-leadership/delegation-in-nursing/tion. Licensed nurses maintain accountability for the client. However, the delegatee has responsibility for the delegated activity, skill, or procedure.
In summary, delegation is the transfer of the nurse’s responsibility for a task while retaining professional accountability for the client’s overall outcome. The decision to delegate is based on the nurse’s judgment, the act of delegation must be clearly defined by the nurse, and the outcomes of delegation are an extension of the nurse’s guidance and supervision. Delegation, when rooted in mutual respect and trust, is a key component to an effective health care team.
Delegation is an integral skill in the nursing profession to help manage the complexities of the dynamic and ever-changing health care environment. Delegation in nursing has been found to increase employee empowerment, decrease burnout, increase role commitment, and improve job satisfaction.[188] Cultivating delegation skills helps nurses better manage the complexities of their client care role, ensuring that their clients are safely cared for and outcomes are optimized. Delegation skills, like other nursing skills, require purposeful development and do not necessarily come easily when first transitioning into the nursing role. It is important that the new graduate nurse does not mistake delegation for pompous or arrogant behavior. Delegation requires mutual respect between the delegator and delegatee. Delegation is not seen as a sign or weakness and does not reflect one's desire to shirk their work responsibilities. Instead, delegation reflects strong leadership and organizational skills in which the nurse leader demonstrates that they understand how to leverage their team's strengths in order to achieve optimal care outcomes.
To help avoid any perception of arrogance in the delegation of an activity, it is important that the new graduate nurse approaches the task of delegation with humility. Clarity in the communication of the delegated responsibility is critical, and the rationale behind the delegation should be communicated to the delegatee. Within the task of delegation, the delegator should express appreciation for the delegatee and their contributions in the collaborative health care environment. Additionally, it is important to understand that no specific nurse delegated task is outside of the "nurse" role. For example, ambulating a client does not to an unlicensed assistive personnel simply because that individual is able to perform that task. Rather, nurses must be willing to perform delegated tasks themselves when necessary. This reflects a team-oriented mindset and helps to reinforce among the care team that all roles are critical to optimizing client care. For new graduate nurses who first transition into a specific health care setting, having the opportunity to shadow individuals in various work roles helps to foster a team mindset. Asking questions of various team members regarding their work role can help a new graduate nurse demonstrate respect and value for other roles.
Examples of helpful questions may include the following:
- "What is the biggest challenge in your typical workday?"
- "What do you most enjoy about your job?"
- "How is it best to communicate with you when the unit is busy?"
- "What do you think people misunderstand most about your role?"
It is important to ensure that the team understands that care is optimized when they function as one collective unit and not in siloed roles. Each team member must feel valued and competent in their role. By understanding and practicing strategic delegation, new graduate nurses can overcome any misconceptions of arrogance and contribute positively to the healthcare team.
Please review the example below to consider variation in approach to task delegation.
Scenario A: Nurse June, a newly graduated nurse, is working in a busy hospital unit. She needs an unlicensed assistive personnel (UAP), Alex, to take vital signs of a patient. Nurse June approaches Alex in the hallway and says in an abrupt tone, "Alex, I need you to take Mr. Smith's vital signs right now. I'm too busy to do it myself, and besides, that's what you're here for. Just get it done quickly."
Analysis: June’s tone and words suggest she sees Alex's role as less important and purely as a means to offload her tasks. June does not explain the urgency or importance of the task. June doesn’t acknowledge Alex's effort or capability, making the request seem like a command rather than a collaborative effort.
Scenario B: Nurse June, a newly graduated nurse, is working in a busy hospital unit. She needs an unlicensed assistive personnel (UAP), Alex, to take vital signs of a patient. Nurse June approaches Alex and says, "Hi Alex, could you please help me by taking Mr. Smith's vital signs? I'm handling a few urgent matters right now, and it would really help to have your support. I know you’re great at this, and your thoroughness really makes a difference in our patient care. Thank you so much!"
Analysis: June speaks to Alex with courtesy and acknowledges the value of his role. June clearly explains why she needs Alex's help and the importance of the task. June acknowledges Alex’s competence and expresses gratitude, fostering feelings of value and respect.
The licensed nurse has the responsibility to supervise, monitor, and evaluate the nursing team members who have received delegated tasks, activities, or procedures. As previously noted, the act of supervision requires the nurse to assess the staff member’s ability, competency, and experience prior to delegating. After the nurse has made the decision to delegate, supervision continues in terms of coaching, supporting, assisting, and educating as needed throughout the task to assure appropriate care is provided.
The nurse is accountable for client care delegated to other team members. Communication and supervision should be ongoing processes throughout the shift within the nursing care team. The nurse must ensure quality of care, appropriateness, timeliness, and completeness through direct and indirect supervision. For example, an RN may directly observe the AP reposition a client or assist them to the bathroom to assure both client and staff safety are maintained. An RN may also indirectly evaluate an LPN’s administration of medication by reviewing documentation in the client’s medical record for timeliness and accuracy. Through direct and indirect supervision of delegation, quality client care and compliance with standards of practice and facility policies can be assured.
Supervision also includes providing constructive feedback to the nursing team member. Constructive feedback is supportive and identifies solutions to areas needing improvement. It is provided with positive intentions to address specific issues or concerns as the person learns and grows in their role. Constructive feedback includes several key points:
- Was the task, activity, care, or procedure performed correctly?
- Were the expected outcomes involving delegation for that client achieved?
- Did the team member utilize effective and timely communication?
- What were the challenges of the activity and what aspects went well?
- Were there any problems or specific concerns that occurred and how were they managed?
After these questions have been addressed, the RN creates a plan for future delegation with the nursing team member. This plan typically includes the following:
- Recognizing difficulty of the nursing team member in initiating or completing the delegated activities.
- Observing the client’s responses to actions performed by the nursing team member.
- Following up in a timely manner on any problems, incidents, or concerns that arose.
- Creating a plan for providing additional training and monitoring outcomes of future delegated tasks, activities, or procedures.
- Consulting with appropriate nursing administrators per agency policy if the client’s safety was compromised.
Please review the following example regarding constructive feedback and task supervision
Nurse Sarah, an experienced RN, delegated a task to Peter, an unlicensed assistive personnel (UAP), to take the vital signs of a post-operative patient, Mrs. Johnson, and report any abnormalities immediately.
Sarah: "Hi Peter, I wanted to discuss the task you completed earlier with Mrs. Johnson's vital signs. Thank you for your help with that. Let’s review how it went."
Was the task, activity, care, or procedure performed correctly?
Sarah: "First, I noticed you recorded the vital signs accurately. Good job on that. However, there was a delay in reporting Mrs. Johnson's elevated blood pressure to me. Can you walk me through what happened?"
Peter: "I took her vital signs, and her blood pressure was high. I was going to inform you, but I got called to assist with another patient immediately after."
Were the expected outcomes involving delegation for that client achieved?
Sarah: "Ultimately, we did address the elevated blood pressure, but the delay could have impacted her care. It's crucial to report such abnormalities immediately."
Did the team member utilize effective and timely communication?
Sarah: "While you communicated the vital signs correctly, the timing was off. In future, if you can't find me immediately, please inform any available nurse or use the intercom system."
What were the challenges of the activity and what aspects went well?
Peter: "The challenge was managing multiple tasks at once. I did feel confident in taking and recording the vital signs accurately, though."
Sarah: "It sounds like you’re balancing a lot of responsibilities well, but prioritizing urgent communications is key. You handled the technical part perfectly."
Were there any problems or specific concerns that occurred and how were they managed?
Sarah: "The main concern was the delay in reporting the elevated blood pressure. Fortunately, there were no serious consequences, but it’s a potential risk we need to manage better. Let’s create a plan to support you moving forward."
Recognizing difficulty of the nursing team member in initiating or completing the delegated activities:
Sarah: "I recognize that you were busy with multiple tasks. It’s important to prioritize patient safety over other duties."
Observing the client’s responses to actions performed by the nursing team member:
Sarah: "I will check on Mrs. Johnson's response to ensure there are no ongoing issues, and I’ll keep exploring how we can improve this process."
Following up in a timely manner on any problems, incidents, or concerns that arose:
Sarah: "I’ll follow up with you soon to see how you’re managing your other tasks, and we can address any challenges you’re facing."
Creating a plan for providing additional training and monitoring outcomes of future delegated tasks, activities, or procedures:
Sarah: "We’ll arrange some additional training on prioritizing tasks and urgent communication. Let's monitor the outcomes of your delegated tasks over the next few weeks to ensure you’re supported."
Consulting with appropriate nursing administrators per agency policy if the client’s safety was compromised:
Sarah: "Fortunately, Mrs. Johnson is fine, but if there were any safety concerns, we’d need to report it according to our policy. Keep this in mind for the future."
Sarah: "Peter, you're doing a great job with your responsibilities, and with a bit more focus on communication priorities, I’m confident you’ll excel even more. Let’s touch base again in a week to see how things are going. Feel free to come to me with any questions or concerns in the meantime."
Peter: "Thank you, Sarah. I appreciate the feedback and will work on prioritizing urgent communications."
Sarah: "Great. Keep up the good work, and let’s keep improving together."
The licensed nurse has the responsibility to supervise, monitor, and evaluate the nursing team members who have received delegated tasks, activities, or procedures. As previously noted, the act of supervision requires the nurse to assess the staff member’s ability, competency, and experience prior to delegating. After the nurse has made the decision to delegate, supervision continues in terms of coaching, supporting, assisting, and educating as needed throughout the task to assure appropriate care is provided.
The nurse is accountable for client care delegated to other team members. Communication and supervision should be ongoing processes throughout the shift within the nursing care team. The nurse must ensure quality of care, appropriateness, timeliness, and completeness through direct and indirect supervision. For example, an RN may directly observe the AP reposition a client or assist them to the bathroom to assure both client and staff safety are maintained. An RN may also indirectly evaluate an LPN’s administration of medication by reviewing documentation in the client’s medical record for timeliness and accuracy. Through direct and indirect supervision of delegation, quality client care and compliance with standards of practice and facility policies can be assured.
Supervision also includes providing constructive feedback to the nursing team member. Constructive feedback is supportive and identifies solutions to areas needing improvement. It is provided with positive intentions to address specific issues or concerns as the person learns and grows in their role. Constructive feedback includes several key points:
- Was the task, activity, care, or procedure performed correctly?
- Were the expected outcomes involving delegation for that client achieved?
- Did the team member utilize effective and timely communication?
- What were the challenges of the activity and what aspects went well?
- Were there any problems or specific concerns that occurred and how were they managed?
After these questions have been addressed, the RN creates a plan for future delegation with the nursing team member. This plan typically includes the following:
- Recognizing difficulty of the nursing team member in initiating or completing the delegated activities.
- Observing the client’s responses to actions performed by the nursing team member.
- Following up in a timely manner on any problems, incidents, or concerns that arose.
- Creating a plan for providing additional training and monitoring outcomes of future delegated tasks, activities, or procedures.
- Consulting with appropriate nursing administrators per agency policy if the client’s safety was compromised.
Please review the following example regarding constructive feedback and task supervision
Nurse Sarah, an experienced RN, delegated a task to Peter, an unlicensed assistive personnel (UAP), to take the vital signs of a post-operative patient, Mrs. Johnson, and report any abnormalities immediately.
Sarah: "Hi Peter, I wanted to discuss the task you completed earlier with Mrs. Johnson's vital signs. Thank you for your help with that. Let’s review how it went."
Was the task, activity, care, or procedure performed correctly?
Sarah: "First, I noticed you recorded the vital signs accurately. Good job on that. However, there was a delay in reporting Mrs. Johnson's elevated blood pressure to me. Can you walk me through what happened?"
Peter: "I took her vital signs, and her blood pressure was high. I was going to inform you, but I got called to assist with another patient immediately after."
Were the expected outcomes involving delegation for that client achieved?
Sarah: "Ultimately, we did address the elevated blood pressure, but the delay could have impacted her care. It's crucial to report such abnormalities immediately."
Did the team member utilize effective and timely communication?
Sarah: "While you communicated the vital signs correctly, the timing was off. In future, if you can't find me immediately, please inform any available nurse or use the intercom system."
What were the challenges of the activity and what aspects went well?
Peter: "The challenge was managing multiple tasks at once. I did feel confident in taking and recording the vital signs accurately, though."
Sarah: "It sounds like you’re balancing a lot of responsibilities well, but prioritizing urgent communications is key. You handled the technical part perfectly."
Were there any problems or specific concerns that occurred and how were they managed?
Sarah: "The main concern was the delay in reporting the elevated blood pressure. Fortunately, there were no serious consequences, but it’s a potential risk we need to manage better. Let’s create a plan to support you moving forward."
Recognizing difficulty of the nursing team member in initiating or completing the delegated activities:
Sarah: "I recognize that you were busy with multiple tasks. It’s important to prioritize patient safety over other duties."
Observing the client’s responses to actions performed by the nursing team member:
Sarah: "I will check on Mrs. Johnson's response to ensure there are no ongoing issues, and I’ll keep exploring how we can improve this process."
Following up in a timely manner on any problems, incidents, or concerns that arose:
Sarah: "I’ll follow up with you soon to see how you’re managing your other tasks, and we can address any challenges you’re facing."
Creating a plan for providing additional training and monitoring outcomes of future delegated tasks, activities, or procedures:
Sarah: "We’ll arrange some additional training on prioritizing tasks and urgent communication. Let's monitor the outcomes of your delegated tasks over the next few weeks to ensure you’re supported."
Consulting with appropriate nursing administrators per agency policy if the client’s safety was compromised:
Sarah: "Fortunately, Mrs. Johnson is fine, but if there were any safety concerns, we’d need to report it according to our policy. Keep this in mind for the future."
Sarah: "Peter, you're doing a great job with your responsibilities, and with a bit more focus on communication priorities, I’m confident you’ll excel even more. Let’s touch base again in a week to see how things are going. Feel free to come to me with any questions or concerns in the meantime."
Peter: "Thank you, Sarah. I appreciate the feedback and will work on prioritizing urgent communications."
Sarah: "Great. Keep up the good work, and let’s keep improving together."
You are an RN and are reporting to work on a 16-bed medical/renal unit in a county hospital for the 0700 - 1500 shift today. The client population is primarily socioeconomically disadvantaged. Staff for the shift includes four RNs, one LPN/VN, and two AP.
You are a new RN graduate on the unit, and your orientation was completed two weeks ago. The LPN/VN has been working on the unit for ten years. Both AP have been on the unit for six months and are certified nursing assistants after completing basic nurse aide training. You, as one of four RNs on the unit, have been assigned four clients. You share the LPN with the other RNs, and there is one AP for every two RNs.
The charge nurse has assigned you the following four clients. Scheduled morning medications are due at 0800 and all four require some assistance with their ADLs.
- Client A: An obese 52-year-old male with hypertension and diabetes requiring insulin therapy. He has been depressed since recently being diagnosed with end-stage renal disease requiring hemodialysis. He needs his morning medications and assistance getting dressed for transport to hemodialysis in 30 minutes.
- Client B: A 83-year-old female client with acute pyelonephritis admitted two days ago. She has a PICC line in place and is receiving IV vancomycin every 12 hours. The next dose is due at 0830 after a trough level is drawn.
- Client C: A 78-year-old male recently diagnosed with bladder cancer. He has bright red urine today but reports it is painless. He has surgery scheduled at 0900 and the pre-op checklist has not yet been completed.
- Client D: A malnourished 80-year-old male client admitted with dehydration and imbalanced electrolyte levels. He is being discharged home today and requires patient education.
Reflective Questions
- At the start of the shift, you determine which tasks, cares, activities, and/or procedures you will delegate to the LPN and AP. What factors must you consider prior to delegation?
- What tasks will you delegate to the LPN/VN?
- What tasks will you delegate to the AP?
You are an RN and are reporting to work on a 16-bed medical/renal unit in a county hospital for the 0700 - 1500 shift today. The client population is primarily socioeconomically disadvantaged. Staff for the shift includes four RNs, one LPN/VN, and two AP.
You are a new RN graduate on the unit, and your orientation was completed two weeks ago. The LPN/VN has been working on the unit for ten years. Both AP have been on the unit for six months and are certified nursing assistants after completing basic nurse aide training. You, as one of four RNs on the unit, have been assigned four clients. You share the LPN with the other RNs, and there is one AP for every two RNs.
The charge nurse has assigned you the following four clients. Scheduled morning medications are due at 0800 and all four require some assistance with their ADLs.
- Client A: An obese 52-year-old male with hypertension and diabetes requiring insulin therapy. He has been depressed since recently being diagnosed with end-stage renal disease requiring hemodialysis. He needs his morning medications and assistance getting dressed for transport to hemodialysis in 30 minutes.
- Client B: A 83-year-old female client with acute pyelonephritis admitted two days ago. She has a PICC line in place and is receiving IV vancomycin every 12 hours. The next dose is due at 0830 after a trough level is drawn.
- Client C: A 78-year-old male recently diagnosed with bladder cancer. He has bright red urine today but reports it is painless. He has surgery scheduled at 0900 and the pre-op checklist has not yet been completed.
- Client D: A malnourished 80-year-old male client admitted with dehydration and imbalanced electrolyte levels. He is being discharged home today and requires patient education.
Reflective Questions
- At the start of the shift, you determine which tasks, cares, activities, and/or procedures you will delegate to the LPN and AP. What factors must you consider prior to delegation?
- What tasks will you delegate to the LPN/VN?
- What tasks will you delegate to the AP?
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activities are provided as immediate feedback.)
1. Review the following case studies regarding nurse liability associated with inappropriate delegation:
- Nurse Case Study: Wrongful delegation of patient care to unlicensed assistive personnel
- Nurse Video Case Study: Failure to assess and monitor
Reflective Questions: What delegation errors occurred in each of these scenarios and what were the repercussions of these errors for the nurses involved?
2. The RN is delegating tasks to the LPN/VN and AP on a medical-surgical unit. Using the columns as reference, indicate where delegation errors occurred using the 5 Rs of delegation.
| Right Person | Right Task | Right Circumstance | Right Direction and Communication | Right Supervision and Evaluation | |
|---|---|---|---|---|---|
| Directs the AP to assess the pain level of a client who is post-op Day 3 after a hip replacement and report back the finding. | |||||
| Directs the LPN to give 1 mg IV push morphine to a patient who is 2-hours post total left knee replacement and ensure documentation. | |||||
| Assigns the AP to collect blood pressures on all clients on the unit by 0800. Assumes the AP will report back any abnormal blood pressures. | |||||
| Directs a new AP to ambulate a patient who is post-op Day 2 from a shoulder replacement who needs the assistance of one person and an adaptive walker. The AP voices concerns about never having used an adaptive walker before. The RN directs the AP to get another AP to help. |

Test your knowledge using this NCLEX Next Generation-style Case Study. You may reset and resubmit your answers to this question an unlimited number of times.[189]
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activities are provided as immediate feedback.)
1. Review the following case studies regarding nurse liability associated with inappropriate delegation:
- Nurse Case Study: Wrongful delegation of patient care to unlicensed assistive personnel
- Nurse Video Case Study: Failure to assess and monitor
Reflective Questions: What delegation errors occurred in each of these scenarios and what were the repercussions of these errors for the nurses involved?
2. The RN is delegating tasks to the LPN/VN and AP on a medical-surgical unit. Using the columns as reference, indicate where delegation errors occurred using the 5 Rs of delegation.
| Right Person | Right Task | Right Circumstance | Right Direction and Communication | Right Supervision and Evaluation | |
|---|---|---|---|---|---|
| Directs the AP to assess the pain level of a client who is post-op Day 3 after a hip replacement and report back the finding. | |||||
| Directs the LPN to give 1 mg IV push morphine to a patient who is 2-hours post total left knee replacement and ensure documentation. | |||||
| Assigns the AP to collect blood pressures on all clients on the unit by 0800. Assumes the AP will report back any abnormal blood pressures. | |||||
| Directs a new AP to ambulate a patient who is post-op Day 2 from a shoulder replacement who needs the assistance of one person and an adaptive walker. The AP voices concerns about never having used an adaptive walker before. The RN directs the AP to get another AP to help. |

Test your knowledge using this NCLEX Next Generation-style Case Study. You may reset and resubmit your answers to this question an unlimited number of times.[190]
Accountability: Being answerable to oneself and others for one’s own choices, decisions, and actions as measured against a standard.
Assignment: Routine care, activities, and procedures that are within the authorized scope of practice of the RN, LPN/VN, or routine functions of the assistive personnel.
Assistive Personnel (AP): Any assistive personnel (formerly referred to as ‘‘unlicensed” assistive personnel [UAP]) trained to function in a supportive role, regardless of title, to whom a nursing responsibility may be delegated. This includes, but is not limited to, certified nursing assistants or aides (CNAs), patient-care technicians (PCTs), certified medical assistants (CMAs), certified medication aides, and home health aides.[191]
Closed-loop communication: A process that enables the person giving the instructions to hear what they said reflected back and to confirm that their message was, in fact, received correctly.
Constructive feedback: Supportive feedback that offers solutions to areas of weakness.
Delegated responsibility: A nursing activity, skill, or procedure that is transferred from a license nurse to a delegatee.
Delegatee: An RN, LPN/VN, or AP who is delegated a nursing responsibility by either an APRN, RN, or LPN/VN who is competent to perform the task and verbally accepts the responsibility.
Delegation: Allowing a delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role but in which they have received additional training.
Delegator: An APRN, RN, or LPN/VN who requests a specially trained delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role.
Five rights of delegation: Right task, right circumstance, right person, right directions and communication, and right supervision and evaluation.
Nursing team members: Advanced practice registered nurses (APRN), registered nurses (RN), licensed practical/vocational nurses (LPN/VN), and assistive personnel (AP).
Scope of practice: Procedures, actions, and processes that a health care practitioner is permitted to undertake in keeping with the terms of their professional license.
Supervision: Appropriate monitoring of the delegated activity, evaluation of patient outcomes, and follow-up with the delegatee at the completion of the activity.
Titrate: Making adjustments to medication dosage per an established protocol to obtain a desired therapeutic outcome.
Accountability: Being answerable to oneself and others for one’s own choices, decisions, and actions as measured against a standard.
Assignment: Routine care, activities, and procedures that are within the authorized scope of practice of the RN, LPN/VN, or routine functions of the assistive personnel.
Assistive Personnel (AP): Any assistive personnel (formerly referred to as ‘‘unlicensed” assistive personnel [UAP]) trained to function in a supportive role, regardless of title, to whom a nursing responsibility may be delegated. This includes, but is not limited to, certified nursing assistants or aides (CNAs), patient-care technicians (PCTs), certified medical assistants (CMAs), certified medication aides, and home health aides.[192]
Closed-loop communication: A process that enables the person giving the instructions to hear what they said reflected back and to confirm that their message was, in fact, received correctly.
Constructive feedback: Supportive feedback that offers solutions to areas of weakness.
Delegated responsibility: A nursing activity, skill, or procedure that is transferred from a license nurse to a delegatee.
Delegatee: An RN, LPN/VN, or AP who is delegated a nursing responsibility by either an APRN, RN, or LPN/VN who is competent to perform the task and verbally accepts the responsibility.
Delegation: Allowing a delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role but in which they have received additional training.
Delegator: An APRN, RN, or LPN/VN who requests a specially trained delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role.
Five rights of delegation: Right task, right circumstance, right person, right directions and communication, and right supervision and evaluation.
Nursing team members: Advanced practice registered nurses (APRN), registered nurses (RN), licensed practical/vocational nurses (LPN/VN), and assistive personnel (AP).
Scope of practice: Procedures, actions, and processes that a health care practitioner is permitted to undertake in keeping with the terms of their professional license.
Supervision: Appropriate monitoring of the delegated activity, evaluation of patient outcomes, and follow-up with the delegatee at the completion of the activity.
Titrate: Making adjustments to medication dosage per an established protocol to obtain a desired therapeutic outcome.
Partial pressure of carbon dioxide level in arterial blood indicated in an ABG result. Normal range is 35-45 mmHg.
Learning Objectives
- Differentiate the role of leader and manager
- Examine the roles of team members
- Identify steps in the management process and activities that managers perform
- Describe the role of the RN as a leader and change agent
- Discuss effects of power, empowerment, and motivation in leading and managing a nursing team
As a nursing student preparing to graduate, you have spent countless hours on developing clinical skills, analyzing disease processes, creating care plans, and cultivating clinical judgment. In comparison, you have likely spent much less time on developing management and leadership skills. Yet, soon after beginning your first job as a registered nurse, you will become involved in numerous situations requiring nursing leadership and management skills. Some of these situations include the following:
- Prioritizing care for a group of assigned clients
- Collaborating with interprofessional team members regarding client care
- Participating in an interdisciplinary team conference
- Acting as a liaison when establishing community resources for a patient being discharged home
- Serving on a unit committee
- Investigating and implementing a new evidence-based best practice
- Mentoring nursing students
Delivering safe, quality client care often requires registered nurses (RN) to manage care provided by the nursing team. Making assignments, delegating tasks, and supervising nursing team members are essential managerial components of an entry-level staff RN role. As previously discussed, nursing team members include RNs, licensed practical/vocational nurses (LPN/VN), and assistive personnel (AP).[193]
Read more about assigning, delegating, and supervising in the “Delegation and Supervision” chapter.
An RN is expected to demonstrate leadership and management skills in many facets of the role. Nurses manage care for high-acuity patients as they are admitted, transferred, and discharged; coordinate care among a variety of diverse health professionals; advocate for clients’ needs; and manage limited resources with shrinking budgets.[194]
Read more about collaborating and communicating with the interprofessional team; advocating for clients; and admitting, transferring, and discharging clients in the “Collaboration Within the Interprofessional Team” chapter.
An article published in the Online Journal of Issues in Nursing states, "With the growing complexity of healthcare practice environments and pending nurse leader retirements, the development of future nurse leaders is increasingly important."[195] This chapter will explore leadership and management responsibilities of an RN. Leadership styles are introduced, and change theories are discussed as a means for implementing change in the health care system.
Learning Objectives
- Differentiate the role of leader and manager
- Examine the roles of team members
- Identify steps in the management process and activities that managers perform
- Describe the role of the RN as a leader and change agent
- Discuss effects of power, empowerment, and motivation in leading and managing a nursing team
As a nursing student preparing to graduate, you have spent countless hours on developing clinical skills, analyzing disease processes, creating care plans, and cultivating clinical judgment. In comparison, you have likely spent much less time on developing management and leadership skills. Yet, soon after beginning your first job as a registered nurse, you will become involved in numerous situations requiring nursing leadership and management skills. Some of these situations include the following:
- Prioritizing care for a group of assigned clients
- Collaborating with interprofessional team members regarding client care
- Participating in an interdisciplinary team conference
- Acting as a liaison when establishing community resources for a patient being discharged home
- Serving on a unit committee
- Investigating and implementing a new evidence-based best practice
- Mentoring nursing students
Delivering safe, quality client care often requires registered nurses (RN) to manage care provided by the nursing team. Making assignments, delegating tasks, and supervising nursing team members are essential managerial components of an entry-level staff RN role. As previously discussed, nursing team members include RNs, licensed practical/vocational nurses (LPN/VN), and assistive personnel (AP).[196]
Read more about assigning, delegating, and supervising in the “Delegation and Supervision” chapter.
An RN is expected to demonstrate leadership and management skills in many facets of the role. Nurses manage care for high-acuity patients as they are admitted, transferred, and discharged; coordinate care among a variety of diverse health professionals; advocate for clients’ needs; and manage limited resources with shrinking budgets.[197]
Read more about collaborating and communicating with the interprofessional team; advocating for clients; and admitting, transferring, and discharging clients in the “Collaboration Within the Interprofessional Team” chapter.
An article published in the Online Journal of Issues in Nursing states, "With the growing complexity of healthcare practice environments and pending nurse leader retirements, the development of future nurse leaders is increasingly important."[198] This chapter will explore leadership and management responsibilities of an RN. Leadership styles are introduced, and change theories are discussed as a means for implementing change in the health care system.
Interpretations or conclusions based on cues, personal experiences, preferences, or generalizations.
Full-thickness tissue loss like Stage 3 pressure injuries but also have exposed cartilage, tendon, ligament, muscle, or bone.
Organizational Culture
The formal leaders of an organization provide a sense of direction and overall guidance for their employees by establishing organizational vision, mission, and values statements. An organization’s vision statement defines why the organization exists, describes how the organization is unique from similar organizations, and specifies what the organization is striving to be. The mission statement describes how the organization will fulfill its vision and establishes a common course of action for future endeavors. See Figure 4.1[199] for an illustration of a mission statement. A values statement establishes the values of an organization that assist with the achievement of its vision and mission. A values statement also provides strategic guidelines for decision-making, both internally and externally, by members of the organization. A values statement may also be reflected as the organization's "core values," which are the foundational ideals that guide the organization's actions and decision-making processes. The vision, mission, and values statements are expressed in a concise and clear manner that is easily understood by members of the organization and the public.[200]

Organizational culture refers to the implicit values and beliefs that reflect the norms and traditions of an organization. An organization’s vision, mission, and values statements are the foundation of organizational culture. Because individual organizations have their own vision, mission, and values statements, each organization has a different culture.[201] Organizational culture helps reflect the expected norms and behaviors that are inherent to an organization. Expected conduct is comprised of the unwritten rules and standards that reflect how employees should behave in different situations. The culture also informs the common communication styles that are inherent to an organization, including both formal and informal channels. The culture may also be manifested outwardly through various symbols and artifacts that embedded within the organization. These may include specific logos, objects, or other physical manifestations of elements that represent the organization's culture. Some organizations may also reflect their cultural values through activities or ceremonies held within the community.
As health care continues to evolve and new models of care are introduced, nursing managers must develop innovative approaches that address change while aligning with that organization’s vision, mission, and values. Leaders embrace the organization’s mission, identify how individuals’ work contributes to it, and ensure that outcomes advance the organization’s mission and purpose. Leaders use vision, mission, and values statements for guidance when determining appropriate responses to critical events and unforeseen challenges that are common in a complex health care system. Successful organizations require employees to be committed to following these strategic guidelines during the course of their work activities. Employees who understand the relationship between their own work and the mission and purpose of the organization will contribute to a stronger health care system that excels in providing first-class patient care. The vision, mission, and values provide a common organization-wide frame of reference for decision-making for both leaders and staff.[202] It is important for employees in health care organizations to have understanding of how their roles and responsibilities connect to the broader mission and vision of the organization. This alignment fosters a cohesive work environment where each staff member is motivated by a shared purpose, leading to more effective and high-quality patient care. It is important that both the leader and employee have clarity in the underlying vision, mission, and values of an organization. This involves responsibility for both the leader and employee. Leaders must articulate the organization's vision, mission, and values clearly and consistently. This involves regular communication through meetings, written materials, etc. Employees share in the responsibility by being empowered to ask questions and seek clarification on how their daily tasks contribute to the organization's overarching goals.
Learning Activity
Investigate the mission, vision, and values of a potential employer, as you would do prior to an interview for a job position.
Reflective Questions
- How well do the organization’s vision and values align with your personal values regarding health care?
- How well does the organization’s mission align with your professional objective in your resume?
Followership
Followership is described as the upward influence of individuals on their leaders and their teams. The actions of followers have an important influence on staff performance and patient outcomes. Being an effective follower requires individuals to contribute to the team not only by doing as they are told, but also by being aware and raising relevant concerns. Effective followers realize that they can initiate change and disagree or challenge their leaders if they feel their organization or unit is failing to promote wellness and deliver safe, value-driven, and compassionate care. Leaders who gain the trust and dedication of followers are more effective in their leadership role. Everybody has a voice and a responsibility to take ownership of the workplace culture, and good followership contributes to the establishment of high-functioning and safety-conscious teams.[203] Key elements of effective followership include proactive engagement, constructive communication, collaboration, advocacy, continuous improvement, and a supportive leadership environment.
In order to demonstrate proactive engagement, followers must also be initiators. Effective followers do not passively wait for instruction by rather take initiative to address issues, propose solutions, and contribute to ideas. They recognize the importance of their voice in engaging in problem-solving and understand that being an effective follower does not mean being passive in their role. Effective followers also employ a keen situational awareness where they maintain vigilant assessment of the environment and potential risks, ensuring that they act in the best interests of clients. They must be confident that they can raise concerns if they identify potential problems or unsafe practices. This reflects a culture where followers feels that their feedback is welcomed and valued. Effective followership also involves communication practices in which the message is clearly conveyed, measures to confirm the message are employed, and the confirmation is received. To be an effective follower, support of the team's goals must be a central tenet of one's work. Collaboration with others involves supporting colleagues and working together toward the common goal even when viewpoints may differ. Identifying strategies that create a respectful opportunity to debate and explore different opinions is important to effective followership. Additionally, followers must take accountability for their own actions while understanding how their role and performance impacts the function of the team, as well as client outcomes. Effective followers also practice ethical advocacy, ensuring that the needs of clients are prioritized and respected. This advocacy also involves the ability to courageously challenge any decisions or actions that may jeopardize care or organizational values. Finally, effective followers engage in continuous learning to enhance their skills and knowledge. They seek feedback and use the feedback to contribute to their own performance and also the growth of the team. Effective followership is further cultivated when leaders and followers come together with mutual respect, trust, and work with a purposeful drive toward shared goals that reflect the organization's mission.
Team members impact patient safety by following teamwork guidelines for good followership. For example, strategies such as closed-loop communication are important tools to promote patient safety.
Read more about communication and teamwork strategies in the “Collaboration Within the Interprofessional Team” chapter.
Leadership and Management Characteristics
Leadership and management are terms often used interchangeably, but they are two different concepts with many overlapping characteristics. Leadership is the art of establishing direction and influencing and motivating others to achieve their maximum potential to accomplish tasks, objectives, or projects.[204],[205] See Figure 4.2[206] for an illustration of team leadership. There is no universally accepted definition or theory of nursing leadership, but there is increasing clarity about how it differs from management.[207] Management refers to roles that focus on tasks such as planning, organizing, prioritizing, budgeting, staffing, coordinating, and reporting.[208] The overriding function of management has been described as providing order and consistency to organizations, whereas the primary function of leadership is to produce change and movement.[209] View a comparison of the characteristics of management and leadership in Table 4.2a.

Table 4.2a. Management and Leadership Characteristics[210]
| MANAGEMENT | LEADERSHIP |
|---|---|
Planning, Organizing, and Prioritizing
|
Establishing Direction
|
Budgeting and Staffing
|
Influencing Others
|
Coordinating and Problem-Solving
|
Motivating
|
Leader Vs. Manager Case Activity
Utilizing the information from the table above, review the following cases and identify whether the individual is serving as a leader or manager based upon the actions taken within the case scenario. Include supportive rationale for your decision regarding the role.
Case 1: Sima, the head nurse, reviews the upcoming schedule and allocates resources to ensure each shift is adequately staffed. She also makes assignments for the nursing staff based on their skills and patient needs. Additionally, she is responsible for hiring new staff and, when necessary, terminating employees who do not meet performance standards.
Case 2: Juan, a senior nurse, is passionate about improving patient care. He identifies an issue with the current handoff process between shifts and proposes a new strategy that incorporates evidence-based practices to enhance communication and reduce errors. He reaches out to his team at their monthly department meetings in order to develop a shared vision for this change and encourages them to partner with him on the new process.
Case 3: Maria, a unit supervisor, holds a meeting to set specific goals and time frames for the department’s upcoming projects. She prioritizes tasks for the team and establishes policies and procedures to ensure these tasks are completed efficiently and within the given deadlines.
Case 4: Emily, the nurse director, is tasked with preparing the budget for the upcoming fiscal year. She allocates resources effectively to ensure all departments are adequately funded. Emily also manages the staffing needs, ensuring that the hiring and termination processes are handled efficiently.
Case 5: Rachel, an experienced nurse, takes the time to build effective teamwork within her unit. She advocates for her patients, their families, and the nursing profession as a whole. Rachel communicates openly and listens to her team’s concerns, ensuring everyone feels valued and heard.
Not all nurses are managers, but all nurses are leaders because they encourage individuals to achieve their goals. The American Nurses Association (ANA) established Leadership as a Standard of Professional Performance for all registered nurses. Standards of Professional Performance are “authoritative statements of action and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently.”[211] See the competencies of the ANA Leadership standard in the following box and additional content in other chapters of this book.
Competencies of ANA’s Leadership Standard of Professional Performance
- Promotes effective relationships to achieve quality outcomes and a culture of safety
- Leads decision-making groups
- Engages in creating an interprofessional environment that promotes respect, trust, and integrity
- Embraces practice innovations and role performance to achieve lifelong personal and professional goals
- Communicates to lead change, influence others, and resolve conflict
- Implements evidence-based practices for safe, quality health care and health care consumer satisfaction
- Demonstrates authority, ownership, accountability, and responsibility for appropriate delegation of nursing care
- Mentors colleagues and others to embrace their knowledge, skills, and abilities
- Participates in professional activities and organizations for professional growth and influence
- Advocates for all aspects of human and environmental health in practice and policy
Read additional content related to leadership and management activities in corresponding chapters of this book:
- Read about the culture of safety in the “Legal Implications” chapter.
- Read about effective interprofessional teamwork and resolving conflict in the “Collaboration Within the Interprofessional Team” chapter.
- Read about quality improvement and implementing evidence-based practices in the “Quality and Evidence-Based Practice” chapter.
- Read more about delegation, supervision, and accountability in the “Delegation and Supervision” chapter.
- Read about professional organizations and advocating for patients, communities, and their environments in the “Advocacy” chapter.
- Read about budgets and staffing in the “Health Care Economics” chapter.
- Read about prioritization in the “Prioritization” chapter.
Leadership Theories and Styles
In the 1930s Kurt Lewin, the father of social psychology, originally identified three leadership styles: authoritarian, democratic, and laissez-faire.[212],[213]
Authoritarian leadership means the leader has full power. Authoritarian leaders tell team members what to do and expect team members to execute their plans. When fast decisions must be made in emergency situations, such as when a patient “codes,” the authoritarian leader makes quick decisions and provides the group with direct instructions. However, there are disadvantages to authoritarian leadership. Authoritarian leaders are more likely to disregard creative ideas of other team members, causing resentment and stress.[214]
Democratic leadership balances decision-making responsibility between team members and the leader. Democratic leaders actively participate in discussions, but also make sure to listen to the views of others. For example, a nurse supervisor may hold a meeting regarding an increased incidence of patient falls on the unit and ask team members to share their observations regarding causes and potential solutions. The democratic leadership style often leads to positive, inclusive, and collaborative work environments that encourage team members’ creativity. Under this style, the leader still retains responsibility for the final decision.[215]
Laissez-faire is a French word that translates to English as, “leave alone.” Laissez-faire leadership gives team members total freedom to perform as they please. Laissez-faire leaders do not participate in decision-making processes and rarely offer opinions. The laissez-faire leadership style can work well if team members are highly skilled and highly motivated to perform quality work. However, without the leader’s input, conflict and a culture of blame may occur as team members disagree on roles, responsibilities, and policies. By not contributing to the decision-making process, the leader forfeits control of team performance.[216]
Over the decades, Lewin’s original leadership styles have evolved into many styles of leadership in health care, such as passive-avoidant, transactional, transformational, servant, resonant, and authentic.[217],[218] Many of these leadership styles have overlapping characteristics. See Figure 4.3[219] for a comparison of various leadership styles in terms of engagement.

Passive-avoidant leadership is similar to laissez-faire leadership and is characterized by a leader who avoids taking responsibility and confronting others. Employees perceive the lack of control over the environment resulting from the absence of clear directives. Organizations with this type of leader have high staff turnover and low retention of employees. These types of leaders tend to react and take corrective action only after problems have become serious and often avoid making any decisions at all.[220]
Transactional leadership involves both the leader and the follower receiving something for their efforts; the leader gets the job done and the follower receives pay, recognition, rewards, or punishment based on how well they perform the tasks assigned to them.[221] Staff generally work independently with no focus on cooperation among employees or commitment to the organization.[222]
Transformational leadership involves leaders motivating followers to perform beyond expectations by creating a sense of ownership in reaching a shared vision.[223] It is characterized by a leader’s charismatic influence over team members and includes effective communication, valued relationships, and consideration of team member input. Transformational leaders know how to convey a sense of loyalty through shared goals, resulting in increased productivity, improved morale, and increased employees’ job satisfaction.[224] They often motivate others to do more than originally intended by inspiring them to look past individual self-interest and perform to promote team and organizational interests.[225]
Servant leadership focuses on the professional growth of employees while simultaneously promoting improved quality care through a combination of interprofessional teamwork and shared decision-making. Servant leaders assist team members to achieve their personal goals by listening with empathy and committing to individual growth and community-building. They share power, put the needs of others first, and help individuals optimize performance while forsaking their own personal advancement and rewards.[226]
Visit the Greenleaf Center site to learn more about What is Servant Leadership?
Resonant leaders are in tune with the emotions of those around them, use empathy, and manage their own emotions effectively. Resonant leaders build strong, trusting relationships and create a climate of optimism that inspires commitment even in the face of adversity. They create an environment where employees are highly engaged, making them willing and able to contribute with their full potential.[227]
Authentic leaders have an honest and direct approach with employees, demonstrating self-awareness, internalized moral perspective, and relationship transparency. They strive for trusting, symmetrical, and close leader–follower relationships; promote the open sharing of information; and consider others’ viewpoints.[228]
Table 4.2b. Characteristics of Leadership Styles
| Authoritarian | Democratic | Laissez-Faire or Passive-Avoidant |
|---|---|---|
|
|
|
| Transactional | Transformational | Servant |
|---|---|---|
|
|
|
| Resonant Leaders | Authentic Leaders |
|---|---|
|
|
Outcomes of Various Leadership Styles
Leadership styles affect team members, patient outcomes, and the organization. A systematic review of the literature published in 2021 showed significant correlations between leadership styles and nurses’ job satisfaction. Transformational leadership style had the greatest positive correlation with nurses’ job satisfaction, followed by authentic, resonant, and servant leadership styles. Passive-avoidant and laissez-faire leadership styles showed a negative correlation with nurses’ job satisfaction.[229] In this challenging health care environment, managers and nurse leaders must promote technical and professional competencies of their staff, but they must also act to improve staff satisfaction and morale by using appropriate leadership styles with their team.[230]
Systems Theory
Systems theory is based on the concept that systems do not function in isolation but rather there is an interdependence that exists between their parts. Systems theory assumes that most individuals strive to do good work but are affected by diverse influences within the system. Efficient and functional systems account for these diverse influences and improve outcomes by studying patterns and behaviors across the system.[231]
Many health care agencies have adopted a culture of safety based on systems theory. A culture of safety is an organizational culture that embraces error reporting by employees with the goal of identifying systemic causes of problems that can be addressed to improve patient safety. According to The Joint Commission, a culture of safety includes the following components[232]:
- Just Culture: A culture where people feel safe raising questions and concerns and report safety events in an environment that emphasizes a nonpunitive response to errors and near misses. Clear lines are drawn by managers between human error, at-risk, and reckless employee behaviors. See Figure 4.4[233] for an illustration of Just Culture.
- Reporting Culture: People realize errors are inevitable and are encouraged to speak up for patient safety by reporting errors and near misses. For example, nurses complete an “incident report” according to agency policy when a medication error occurs, or a client falls. Error reporting helps the agency manage risk and reduce potential liability.
- Learning Culture: People regularly collect information and learn from errors and successes while openly sharing data and information and applying best evidence to improve work processes and patient outcomes.
Just Culture
The American Nurses Association (ANA) officially endorses the Just Culture model. In 2019 the ANA published a position statement on Just Culture, stating, “Traditionally, healthcare’s culture has held individuals accountable for all errors or mishaps that befall patients under their care. By contrast, a Just Culture recognizes that individual practitioners should not be held accountable for system failings over which they have no control. A Just Culture also recognizes many individual or ‘active’ errors represent predictable interactions between human operators and the systems in which they work. However, in contrast to a culture that touts ‘no blame’ as its governing principle, a Just Culture does not tolerate conscious disregard of clear risks to patients or gross misconduct (e.g., falsifying a record or performing professional duties while intoxicated).”
The Just Culture model categorizes human behavior into three causes of errors. Consequences of errors are based on whether the error is a simple human error or caused by at-risk or reckless behavior.
- Simple human error: A simple human error occurs when an individual inadvertently does something other than what should have been done. Most medical errors are the result of human error due to poor processes, programs, education, environmental issues, or situations. These errors are managed by correcting the cause, looking at the process, and fixing the deviation. For example, a nurse appropriately checks the rights of medication administration three times, but due to the similar appearance and names of two different medications stored next to each other in the medication dispensing system, administers the incorrect medication to a patient. In this example, a root cause analysis reveals a system issue that must be modified to prevent future patient errors (e.g., change the labelling and storage of look alike-sound alike medication).
- At-risk behavior: An error due to at-risk behavior occurs when a behavioral choice is made that increases risk where the risk is not recognized or is mistakenly believed to be justified. For example, a nurse scans a patient’s medication with a barcode scanner prior to administration, but an error message appears on the scanner. The nurse mistakenly interprets the error to be a technology problem and proceeds to administer the medication instead of stopping the process and further investigating the error message, resulting in the wrong dosage of a medication being administered to the patient. In this case, ignoring the error message on the scanner can be considered “at-risk behavior” because the behavioral choice was considered justified by the nurse at the time.
- Reckless behavior: Reckless behavior is an error that occurs when an action is taken with conscious disregard for a substantial and unjustifiable risk.[234] For example, a nurse arrives at work intoxicated and administers the wrong medication to the wrong patient. This error is considered due to reckless behavior because the decision to arrive intoxicated was made with conscious disregard for substantial risk.
These examples show three different causes of medication errors that would result in different consequences to the employee based on the Just Culture model. Under the Just Culture model, after root cause analysis is completed, system-wide changes are made to decrease factors that contributed to the error. Managers appropriately hold individuals accountable for errors if they were due to simple human error, at-risk behavior, or reckless behaviors.
If an individual commits a simple human error, managers console the individual and consider changes in training, procedures, and processes. In the “simple human error” above, system-wide changes would be made to change the label and location of the medication to prevent future errors from occurring with the same medication.
Individuals committing at-risk behavior are held accountable for their behavioral choice and often require coaching with incentives for less risky behaviors and situational awareness. In the “at-risk behavior” example above where the nurse ignored an error message on the barcode scanner, mandatory training on using a barcode scanner and responding to errors would be implemented, and the manager would track the employee’s correct usage of the barcode scanner for several months following training.
If an individual demonstrates reckless behavior, remedial action and/or punitive action is taken.[235] In the “reckless behavior” example above, the manager would report the nurse’s behavior to the state's Board of Nursing with mandatory substance abuse counseling to maintain their nursing license. Employment may be terminated with consideration of patterns of behavior.
A Just Culture in which employees aren't afraid to report errors is a highly successful way to enhance patient safety, increase staff and patient satisfaction, and improve outcomes. Success is achieved through good communication, effective management of resources, and an openness to changing processes to ensure the safety of patients and employees. The infographic in Figure 4.4[236] illustrates the components of a culture of safety and Just Culture.
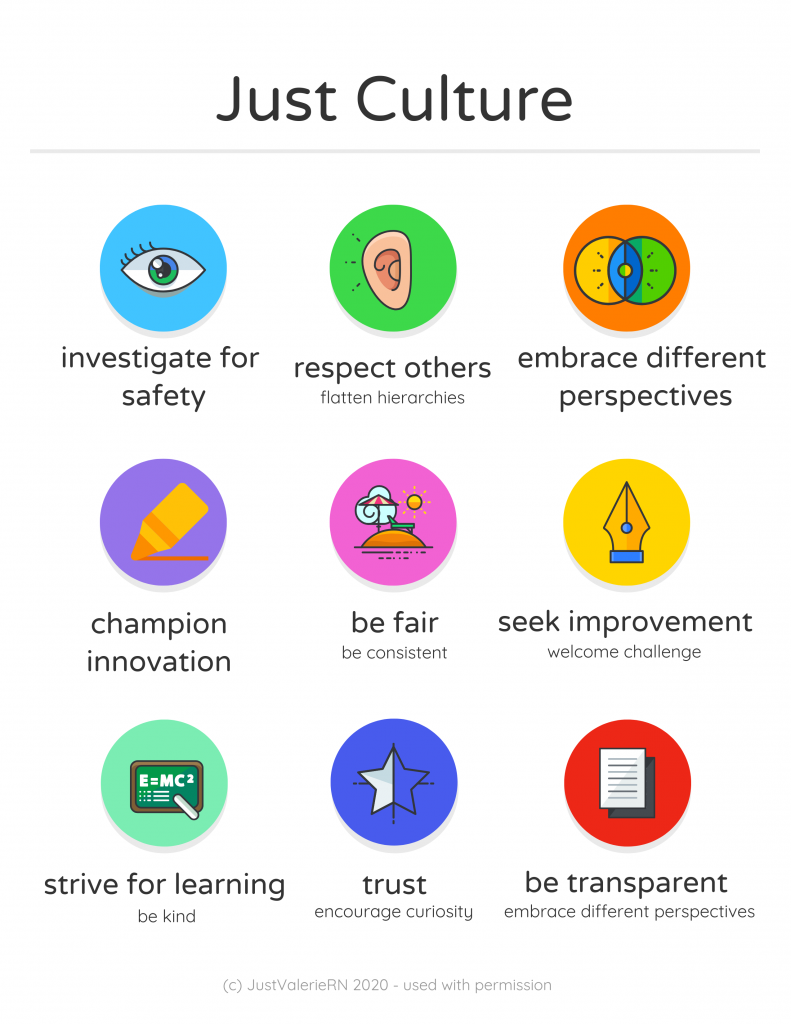
The principles of culture of safety, including Just Culture, Reporting Culture, and Learning Culture are also being adopted in nursing education. It’s understood that mistakes are part of learning and that a shared accountability model promotes individual- and system-level learning for improved patient safety. Under a shared accountability model, students are responsible for the following[237]:
- Being fully prepared for clinical experiences, including laboratory and simulation assignments
- Being rested and mentally ready for a challenging learning environment
- Accepting accountability for their part in contributing to a safe learning environment
- Behaving professionally
- Reporting their own errors and near mistakes
- Keeping up-to-date with current evidence-based practice
- Adhering to ethical and legal standards
Students know they will be held accountable for their actions but will not be blamed for system faults that lie beyond their control. They can trust that a fair process will be used to determine what went wrong if a patient care error or near miss occurs. Student errors and near misses are addressed based on an investigation determining if it was simple human error, an at-risk behavior, or reckless behavior. For example, a simple human error by a student can be addressed with coaching and additional learning opportunities to remedy the knowledge deficit. However, if a student acts with recklessness (for example, repeatedly arrives to clinical unprepared despite previous faculty feedback or falsely documents an assessment or procedure), they are appropriately and fairly disciplined, which may include dismissal from the program.[238]
See Table 4.2c describing classifications of errors using the Just Culture model.
Table 4.2c. Classification of Errors Using the Just Culture Model
| Human Error | At-Risk Behavior | Reckless Behavior |
|---|---|---|
| The caregiver made an error while working appropriately and focusing on the patient’s best interests. | The caregiver made a potentially unsafe choice resulting from faulty or self-serving decision-making. | The caregiver knowingly violated a rule and/or made a dangerous or unsafe choice. |
| Investigation reveals system factors contributing to similar errors by others with similar knowledge and skills. | Investigation reveals the system supports risky action and the caregiver requires coaching. | Investigation reveals the caregiver is accountable and needs retraining. |
| Manage by fixing system errors in processes, procedures, training, design, or environment. | Manage by coaching the caregiver and fixing any system issues:
|
Manage by disciplining the caregiver. If the system supports reckless behavior, it requires fixing. |
| CONSOLE | COACH | PUNISH |
Systems leadership refers to a set of skills used to catalyze, enable, and support the process of systems-level change that is encouraged by the Just Culture Model. Systems leadership is comprised of three interconnected elements:[239]
- The Individual: The skills of collaborative leadership to enable learning, trust-building, and empowered action among stakeholders who share a common goal
- The Community: The tactics of coalition building and advocacy to develop alignment and mobilize action among stakeholders in the system, both within and between organizations
- The System: An understanding of the complex systems shaping the challenge to be addressed
Just Culture Case Review
Review the following case descriptions. Identify the classification of error that has occurred and the recommended actions that should occur.
A chief nursing officer receives a daily report of organization incident reports and reviews the following incident:
Incident Description
Patient Mr. Joe Doden, Room 13067, Medical-Surgical floor
On the afternoon of May 15, 2024, Nurse Sarah was responsible for administering Mr. Joe Doden's insulin dose. The insulin vials used by the hospital had recently been redesigned by the manufacturer, which led to changes in the labeling. The patient was scheduled to receive ten units of regular insulin at 14:30. However, at 1450 the patient turns on his call light, reports feeling unwell. He is shaky, confused, and sweating profusely. The patient's glucose is checked, and he is found to be hypoglycemic. He is treated based upon the hypoglycemia protocol and recovers without further complication.
Case Investigation A
Action: Sarah RN who administered the insulin was following the protocol but mistakenly read the dosage due to a poorly designed label on the insulin vial. The nurse was focused on the patient’s best interests and followed all required steps.
Findings: The investigation revealed that the labeling on the insulin vials was confusing and had led to similar errors by other nurses in the past. The system's design flaw contributed significantly to the error.
How would you classify this error? What actions should be taken?
Case Investigation B
Action: Sarah RN, due to time pressure and a high patient load, decided to skip the double-check protocol for administering the same insulin dose, believing it would save time without causing harm.
Findings: The investigation revealed that the hospital’s workload and time pressures often led to shortcuts in following safety protocols.
How would you classify this error? What actions should be taken?
Case Investigation C
Action: Sarah RN, is familiar with the protocol and knowingly bypassed the double check system, dismissing its importance and administering a medication dose on her own.
Findings: The investigation found that the nurse had a history of disregarding safety protocols, showing a pattern of reckless behavior. This behavior was not supported by the hospital’s policies or environment.
How would you classify this error? What actions should be taken?
Organizational Culture
The formal leaders of an organization provide a sense of direction and overall guidance for their employees by establishing organizational vision, mission, and values statements. An organization’s vision statement defines why the organization exists, describes how the organization is unique from similar organizations, and specifies what the organization is striving to be. The mission statement describes how the organization will fulfill its vision and establishes a common course of action for future endeavors. See Figure 4.1[240] for an illustration of a mission statement. A values statement establishes the values of an organization that assist with the achievement of its vision and mission. A values statement also provides strategic guidelines for decision-making, both internally and externally, by members of the organization. A values statement may also be reflected as the organization's "core values," which are the foundational ideals that guide the organization's actions and decision-making processes. The vision, mission, and values statements are expressed in a concise and clear manner that is easily understood by members of the organization and the public.[241]

Organizational culture refers to the implicit values and beliefs that reflect the norms and traditions of an organization. An organization’s vision, mission, and values statements are the foundation of organizational culture. Because individual organizations have their own vision, mission, and values statements, each organization has a different culture.[242] Organizational culture helps reflect the expected norms and behaviors that are inherent to an organization. Expected conduct is comprised of the unwritten rules and standards that reflect how employees should behave in different situations. The culture also informs the common communication styles that are inherent to an organization, including both formal and informal channels. The culture may also be manifested outwardly through various symbols and artifacts that embedded within the organization. These may include specific logos, objects, or other physical manifestations of elements that represent the organization's culture. Some organizations may also reflect their cultural values through activities or ceremonies held within the community.
As health care continues to evolve and new models of care are introduced, nursing managers must develop innovative approaches that address change while aligning with that organization’s vision, mission, and values. Leaders embrace the organization’s mission, identify how individuals’ work contributes to it, and ensure that outcomes advance the organization’s mission and purpose. Leaders use vision, mission, and values statements for guidance when determining appropriate responses to critical events and unforeseen challenges that are common in a complex health care system. Successful organizations require employees to be committed to following these strategic guidelines during the course of their work activities. Employees who understand the relationship between their own work and the mission and purpose of the organization will contribute to a stronger health care system that excels in providing first-class patient care. The vision, mission, and values provide a common organization-wide frame of reference for decision-making for both leaders and staff.[243] It is important for employees in health care organizations to have understanding of how their roles and responsibilities connect to the broader mission and vision of the organization. This alignment fosters a cohesive work environment where each staff member is motivated by a shared purpose, leading to more effective and high-quality patient care. It is important that both the leader and employee have clarity in the underlying vision, mission, and values of an organization. This involves responsibility for both the leader and employee. Leaders must articulate the organization's vision, mission, and values clearly and consistently. This involves regular communication through meetings, written materials, etc. Employees share in the responsibility by being empowered to ask questions and seek clarification on how their daily tasks contribute to the organization's overarching goals.
Learning Activity
Investigate the mission, vision, and values of a potential employer, as you would do prior to an interview for a job position.
Reflective Questions
- How well do the organization’s vision and values align with your personal values regarding health care?
- How well does the organization’s mission align with your professional objective in your resume?
Followership
Followership is described as the upward influence of individuals on their leaders and their teams. The actions of followers have an important influence on staff performance and patient outcomes. Being an effective follower requires individuals to contribute to the team not only by doing as they are told, but also by being aware and raising relevant concerns. Effective followers realize that they can initiate change and disagree or challenge their leaders if they feel their organization or unit is failing to promote wellness and deliver safe, value-driven, and compassionate care. Leaders who gain the trust and dedication of followers are more effective in their leadership role. Everybody has a voice and a responsibility to take ownership of the workplace culture, and good followership contributes to the establishment of high-functioning and safety-conscious teams.[244] Key elements of effective followership include proactive engagement, constructive communication, collaboration, advocacy, continuous improvement, and a supportive leadership environment.
In order to demonstrate proactive engagement, followers must also be initiators. Effective followers do not passively wait for instruction by rather take initiative to address issues, propose solutions, and contribute to ideas. They recognize the importance of their voice in engaging in problem-solving and understand that being an effective follower does not mean being passive in their role. Effective followers also employ a keen situational awareness where they maintain vigilant assessment of the environment and potential risks, ensuring that they act in the best interests of clients. They must be confident that they can raise concerns if they identify potential problems or unsafe practices. This reflects a culture where followers feels that their feedback is welcomed and valued. Effective followership also involves communication practices in which the message is clearly conveyed, measures to confirm the message are employed, and the confirmation is received. To be an effective follower, support of the team's goals must be a central tenet of one's work. Collaboration with others involves supporting colleagues and working together toward the common goal even when viewpoints may differ. Identifying strategies that create a respectful opportunity to debate and explore different opinions is important to effective followership. Additionally, followers must take accountability for their own actions while understanding how their role and performance impacts the function of the team, as well as client outcomes. Effective followers also practice ethical advocacy, ensuring that the needs of clients are prioritized and respected. This advocacy also involves the ability to courageously challenge any decisions or actions that may jeopardize care or organizational values. Finally, effective followers engage in continuous learning to enhance their skills and knowledge. They seek feedback and use the feedback to contribute to their own performance and also the growth of the team. Effective followership is further cultivated when leaders and followers come together with mutual respect, trust, and work with a purposeful drive toward shared goals that reflect the organization's mission.
Team members impact patient safety by following teamwork guidelines for good followership. For example, strategies such as closed-loop communication are important tools to promote patient safety.
Read more about communication and teamwork strategies in the “Collaboration Within the Interprofessional Team” chapter.
Leadership and Management Characteristics
Leadership and management are terms often used interchangeably, but they are two different concepts with many overlapping characteristics. Leadership is the art of establishing direction and influencing and motivating others to achieve their maximum potential to accomplish tasks, objectives, or projects.[245],[246] See Figure 4.2[247] for an illustration of team leadership. There is no universally accepted definition or theory of nursing leadership, but there is increasing clarity about how it differs from management.[248] Management refers to roles that focus on tasks such as planning, organizing, prioritizing, budgeting, staffing, coordinating, and reporting.[249] The overriding function of management has been described as providing order and consistency to organizations, whereas the primary function of leadership is to produce change and movement.[250] View a comparison of the characteristics of management and leadership in Table 4.2a.

Table 4.2a. Management and Leadership Characteristics[251]
| MANAGEMENT | LEADERSHIP |
|---|---|
Planning, Organizing, and Prioritizing
|
Establishing Direction
|
Budgeting and Staffing
|
Influencing Others
|
Coordinating and Problem-Solving
|
Motivating
|
Leader Vs. Manager Case Activity
Utilizing the information from the table above, review the following cases and identify whether the individual is serving as a leader or manager based upon the actions taken within the case scenario. Include supportive rationale for your decision regarding the role.
Case 1: Sima, the head nurse, reviews the upcoming schedule and allocates resources to ensure each shift is adequately staffed. She also makes assignments for the nursing staff based on their skills and patient needs. Additionally, she is responsible for hiring new staff and, when necessary, terminating employees who do not meet performance standards.
Case 2: Juan, a senior nurse, is passionate about improving patient care. He identifies an issue with the current handoff process between shifts and proposes a new strategy that incorporates evidence-based practices to enhance communication and reduce errors. He reaches out to his team at their monthly department meetings in order to develop a shared vision for this change and encourages them to partner with him on the new process.
Case 3: Maria, a unit supervisor, holds a meeting to set specific goals and time frames for the department’s upcoming projects. She prioritizes tasks for the team and establishes policies and procedures to ensure these tasks are completed efficiently and within the given deadlines.
Case 4: Emily, the nurse director, is tasked with preparing the budget for the upcoming fiscal year. She allocates resources effectively to ensure all departments are adequately funded. Emily also manages the staffing needs, ensuring that the hiring and termination processes are handled efficiently.
Case 5: Rachel, an experienced nurse, takes the time to build effective teamwork within her unit. She advocates for her patients, their families, and the nursing profession as a whole. Rachel communicates openly and listens to her team’s concerns, ensuring everyone feels valued and heard.
Not all nurses are managers, but all nurses are leaders because they encourage individuals to achieve their goals. The American Nurses Association (ANA) established Leadership as a Standard of Professional Performance for all registered nurses. Standards of Professional Performance are “authoritative statements of action and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently.”[252] See the competencies of the ANA Leadership standard in the following box and additional content in other chapters of this book.
Competencies of ANA’s Leadership Standard of Professional Performance
- Promotes effective relationships to achieve quality outcomes and a culture of safety
- Leads decision-making groups
- Engages in creating an interprofessional environment that promotes respect, trust, and integrity
- Embraces practice innovations and role performance to achieve lifelong personal and professional goals
- Communicates to lead change, influence others, and resolve conflict
- Implements evidence-based practices for safe, quality health care and health care consumer satisfaction
- Demonstrates authority, ownership, accountability, and responsibility for appropriate delegation of nursing care
- Mentors colleagues and others to embrace their knowledge, skills, and abilities
- Participates in professional activities and organizations for professional growth and influence
- Advocates for all aspects of human and environmental health in practice and policy
Read additional content related to leadership and management activities in corresponding chapters of this book:
- Read about the culture of safety in the “Legal Implications” chapter.
- Read about effective interprofessional teamwork and resolving conflict in the “Collaboration Within the Interprofessional Team” chapter.
- Read about quality improvement and implementing evidence-based practices in the “Quality and Evidence-Based Practice” chapter.
- Read more about delegation, supervision, and accountability in the “Delegation and Supervision” chapter.
- Read about professional organizations and advocating for patients, communities, and their environments in the “Advocacy” chapter.
- Read about budgets and staffing in the “Health Care Economics” chapter.
- Read about prioritization in the “Prioritization” chapter.
Leadership Theories and Styles
In the 1930s Kurt Lewin, the father of social psychology, originally identified three leadership styles: authoritarian, democratic, and laissez-faire.[253],[254]
Authoritarian leadership means the leader has full power. Authoritarian leaders tell team members what to do and expect team members to execute their plans. When fast decisions must be made in emergency situations, such as when a patient “codes,” the authoritarian leader makes quick decisions and provides the group with direct instructions. However, there are disadvantages to authoritarian leadership. Authoritarian leaders are more likely to disregard creative ideas of other team members, causing resentment and stress.[255]
Democratic leadership balances decision-making responsibility between team members and the leader. Democratic leaders actively participate in discussions, but also make sure to listen to the views of others. For example, a nurse supervisor may hold a meeting regarding an increased incidence of patient falls on the unit and ask team members to share their observations regarding causes and potential solutions. The democratic leadership style often leads to positive, inclusive, and collaborative work environments that encourage team members’ creativity. Under this style, the leader still retains responsibility for the final decision.[256]
Laissez-faire is a French word that translates to English as, “leave alone.” Laissez-faire leadership gives team members total freedom to perform as they please. Laissez-faire leaders do not participate in decision-making processes and rarely offer opinions. The laissez-faire leadership style can work well if team members are highly skilled and highly motivated to perform quality work. However, without the leader’s input, conflict and a culture of blame may occur as team members disagree on roles, responsibilities, and policies. By not contributing to the decision-making process, the leader forfeits control of team performance.[257]
Over the decades, Lewin’s original leadership styles have evolved into many styles of leadership in health care, such as passive-avoidant, transactional, transformational, servant, resonant, and authentic.[258],[259] Many of these leadership styles have overlapping characteristics. See Figure 4.3[260] for a comparison of various leadership styles in terms of engagement.

Passive-avoidant leadership is similar to laissez-faire leadership and is characterized by a leader who avoids taking responsibility and confronting others. Employees perceive the lack of control over the environment resulting from the absence of clear directives. Organizations with this type of leader have high staff turnover and low retention of employees. These types of leaders tend to react and take corrective action only after problems have become serious and often avoid making any decisions at all.[261]
Transactional leadership involves both the leader and the follower receiving something for their efforts; the leader gets the job done and the follower receives pay, recognition, rewards, or punishment based on how well they perform the tasks assigned to them.[262] Staff generally work independently with no focus on cooperation among employees or commitment to the organization.[263]
Transformational leadership involves leaders motivating followers to perform beyond expectations by creating a sense of ownership in reaching a shared vision.[264] It is characterized by a leader’s charismatic influence over team members and includes effective communication, valued relationships, and consideration of team member input. Transformational leaders know how to convey a sense of loyalty through shared goals, resulting in increased productivity, improved morale, and increased employees’ job satisfaction.[265] They often motivate others to do more than originally intended by inspiring them to look past individual self-interest and perform to promote team and organizational interests.[266]
Servant leadership focuses on the professional growth of employees while simultaneously promoting improved quality care through a combination of interprofessional teamwork and shared decision-making. Servant leaders assist team members to achieve their personal goals by listening with empathy and committing to individual growth and community-building. They share power, put the needs of others first, and help individuals optimize performance while forsaking their own personal advancement and rewards.[267]
Visit the Greenleaf Center site to learn more about What is Servant Leadership?
Resonant leaders are in tune with the emotions of those around them, use empathy, and manage their own emotions effectively. Resonant leaders build strong, trusting relationships and create a climate of optimism that inspires commitment even in the face of adversity. They create an environment where employees are highly engaged, making them willing and able to contribute with their full potential.[268]
Authentic leaders have an honest and direct approach with employees, demonstrating self-awareness, internalized moral perspective, and relationship transparency. They strive for trusting, symmetrical, and close leader–follower relationships; promote the open sharing of information; and consider others’ viewpoints.[269]
Table 4.2b. Characteristics of Leadership Styles
| Authoritarian | Democratic | Laissez-Faire or Passive-Avoidant |
|---|---|---|
|
|
|
| Transactional | Transformational | Servant |
|---|---|---|
|
|
|
| Resonant Leaders | Authentic Leaders |
|---|---|
|
|
Outcomes of Various Leadership Styles
Leadership styles affect team members, patient outcomes, and the organization. A systematic review of the literature published in 2021 showed significant correlations between leadership styles and nurses’ job satisfaction. Transformational leadership style had the greatest positive correlation with nurses’ job satisfaction, followed by authentic, resonant, and servant leadership styles. Passive-avoidant and laissez-faire leadership styles showed a negative correlation with nurses’ job satisfaction.[270] In this challenging health care environment, managers and nurse leaders must promote technical and professional competencies of their staff, but they must also act to improve staff satisfaction and morale by using appropriate leadership styles with their team.[271]
Systems Theory
Systems theory is based on the concept that systems do not function in isolation but rather there is an interdependence that exists between their parts. Systems theory assumes that most individuals strive to do good work but are affected by diverse influences within the system. Efficient and functional systems account for these diverse influences and improve outcomes by studying patterns and behaviors across the system.[272]
Many health care agencies have adopted a culture of safety based on systems theory. A culture of safety is an organizational culture that embraces error reporting by employees with the goal of identifying systemic causes of problems that can be addressed to improve patient safety. According to The Joint Commission, a culture of safety includes the following components[273]:
- Just Culture: A culture where people feel safe raising questions and concerns and report safety events in an environment that emphasizes a nonpunitive response to errors and near misses. Clear lines are drawn by managers between human error, at-risk, and reckless employee behaviors. See Figure 4.4[274] for an illustration of Just Culture.
- Reporting Culture: People realize errors are inevitable and are encouraged to speak up for patient safety by reporting errors and near misses. For example, nurses complete an “incident report” according to agency policy when a medication error occurs, or a client falls. Error reporting helps the agency manage risk and reduce potential liability.
- Learning Culture: People regularly collect information and learn from errors and successes while openly sharing data and information and applying best evidence to improve work processes and patient outcomes.
Just Culture
The American Nurses Association (ANA) officially endorses the Just Culture model. In 2019 the ANA published a position statement on Just Culture, stating, “Traditionally, healthcare’s culture has held individuals accountable for all errors or mishaps that befall patients under their care. By contrast, a Just Culture recognizes that individual practitioners should not be held accountable for system failings over which they have no control. A Just Culture also recognizes many individual or ‘active’ errors represent predictable interactions between human operators and the systems in which they work. However, in contrast to a culture that touts ‘no blame’ as its governing principle, a Just Culture does not tolerate conscious disregard of clear risks to patients or gross misconduct (e.g., falsifying a record or performing professional duties while intoxicated).”
The Just Culture model categorizes human behavior into three causes of errors. Consequences of errors are based on whether the error is a simple human error or caused by at-risk or reckless behavior.
- Simple human error: A simple human error occurs when an individual inadvertently does something other than what should have been done. Most medical errors are the result of human error due to poor processes, programs, education, environmental issues, or situations. These errors are managed by correcting the cause, looking at the process, and fixing the deviation. For example, a nurse appropriately checks the rights of medication administration three times, but due to the similar appearance and names of two different medications stored next to each other in the medication dispensing system, administers the incorrect medication to a patient. In this example, a root cause analysis reveals a system issue that must be modified to prevent future patient errors (e.g., change the labelling and storage of look alike-sound alike medication).
- At-risk behavior: An error due to at-risk behavior occurs when a behavioral choice is made that increases risk where the risk is not recognized or is mistakenly believed to be justified. For example, a nurse scans a patient’s medication with a barcode scanner prior to administration, but an error message appears on the scanner. The nurse mistakenly interprets the error to be a technology problem and proceeds to administer the medication instead of stopping the process and further investigating the error message, resulting in the wrong dosage of a medication being administered to the patient. In this case, ignoring the error message on the scanner can be considered “at-risk behavior” because the behavioral choice was considered justified by the nurse at the time.
- Reckless behavior: Reckless behavior is an error that occurs when an action is taken with conscious disregard for a substantial and unjustifiable risk.[275] For example, a nurse arrives at work intoxicated and administers the wrong medication to the wrong patient. This error is considered due to reckless behavior because the decision to arrive intoxicated was made with conscious disregard for substantial risk.
These examples show three different causes of medication errors that would result in different consequences to the employee based on the Just Culture model. Under the Just Culture model, after root cause analysis is completed, system-wide changes are made to decrease factors that contributed to the error. Managers appropriately hold individuals accountable for errors if they were due to simple human error, at-risk behavior, or reckless behaviors.
If an individual commits a simple human error, managers console the individual and consider changes in training, procedures, and processes. In the “simple human error” above, system-wide changes would be made to change the label and location of the medication to prevent future errors from occurring with the same medication.
Individuals committing at-risk behavior are held accountable for their behavioral choice and often require coaching with incentives for less risky behaviors and situational awareness. In the “at-risk behavior” example above where the nurse ignored an error message on the barcode scanner, mandatory training on using a barcode scanner and responding to errors would be implemented, and the manager would track the employee’s correct usage of the barcode scanner for several months following training.
If an individual demonstrates reckless behavior, remedial action and/or punitive action is taken.[276] In the “reckless behavior” example above, the manager would report the nurse’s behavior to the state's Board of Nursing with mandatory substance abuse counseling to maintain their nursing license. Employment may be terminated with consideration of patterns of behavior.
A Just Culture in which employees aren't afraid to report errors is a highly successful way to enhance patient safety, increase staff and patient satisfaction, and improve outcomes. Success is achieved through good communication, effective management of resources, and an openness to changing processes to ensure the safety of patients and employees. The infographic in Figure 4.4[277] illustrates the components of a culture of safety and Just Culture.
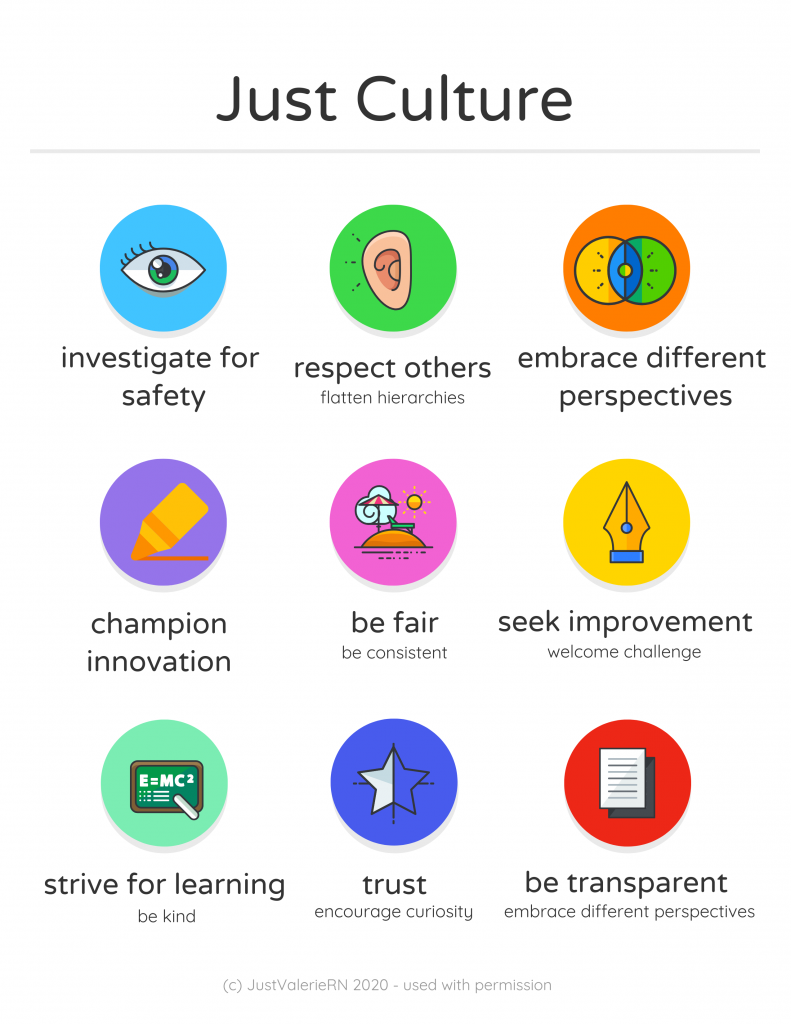
The principles of culture of safety, including Just Culture, Reporting Culture, and Learning Culture are also being adopted in nursing education. It’s understood that mistakes are part of learning and that a shared accountability model promotes individual- and system-level learning for improved patient safety. Under a shared accountability model, students are responsible for the following[278]:
- Being fully prepared for clinical experiences, including laboratory and simulation assignments
- Being rested and mentally ready for a challenging learning environment
- Accepting accountability for their part in contributing to a safe learning environment
- Behaving professionally
- Reporting their own errors and near mistakes
- Keeping up-to-date with current evidence-based practice
- Adhering to ethical and legal standards
Students know they will be held accountable for their actions but will not be blamed for system faults that lie beyond their control. They can trust that a fair process will be used to determine what went wrong if a patient care error or near miss occurs. Student errors and near misses are addressed based on an investigation determining if it was simple human error, an at-risk behavior, or reckless behavior. For example, a simple human error by a student can be addressed with coaching and additional learning opportunities to remedy the knowledge deficit. However, if a student acts with recklessness (for example, repeatedly arrives to clinical unprepared despite previous faculty feedback or falsely documents an assessment or procedure), they are appropriately and fairly disciplined, which may include dismissal from the program.[279]
See Table 4.2c describing classifications of errors using the Just Culture model.
Table 4.2c. Classification of Errors Using the Just Culture Model
| Human Error | At-Risk Behavior | Reckless Behavior |
|---|---|---|
| The caregiver made an error while working appropriately and focusing on the patient’s best interests. | The caregiver made a potentially unsafe choice resulting from faulty or self-serving decision-making. | The caregiver knowingly violated a rule and/or made a dangerous or unsafe choice. |
| Investigation reveals system factors contributing to similar errors by others with similar knowledge and skills. | Investigation reveals the system supports risky action and the caregiver requires coaching. | Investigation reveals the caregiver is accountable and needs retraining. |
| Manage by fixing system errors in processes, procedures, training, design, or environment. | Manage by coaching the caregiver and fixing any system issues:
|
Manage by disciplining the caregiver. If the system supports reckless behavior, it requires fixing. |
| CONSOLE | COACH | PUNISH |
Systems leadership refers to a set of skills used to catalyze, enable, and support the process of systems-level change that is encouraged by the Just Culture Model. Systems leadership is comprised of three interconnected elements:[280]
- The Individual: The skills of collaborative leadership to enable learning, trust-building, and empowered action among stakeholders who share a common goal
- The Community: The tactics of coalition building and advocacy to develop alignment and mobilize action among stakeholders in the system, both within and between organizations
- The System: An understanding of the complex systems shaping the challenge to be addressed
Just Culture Case Review
Review the following case descriptions. Identify the classification of error that has occurred and the recommended actions that should occur.
A chief nursing officer receives a daily report of organization incident reports and reviews the following incident:
Incident Description
Patient Mr. Joe Doden, Room 13067, Medical-Surgical floor
On the afternoon of May 15, 2024, Nurse Sarah was responsible for administering Mr. Joe Doden's insulin dose. The insulin vials used by the hospital had recently been redesigned by the manufacturer, which led to changes in the labeling. The patient was scheduled to receive ten units of regular insulin at 14:30. However, at 1450 the patient turns on his call light, reports feeling unwell. He is shaky, confused, and sweating profusely. The patient's glucose is checked, and he is found to be hypoglycemic. He is treated based upon the hypoglycemia protocol and recovers without further complication.
Case Investigation A
Action: Sarah RN who administered the insulin was following the protocol but mistakenly read the dosage due to a poorly designed label on the insulin vial. The nurse was focused on the patient’s best interests and followed all required steps.
Findings: The investigation revealed that the labeling on the insulin vials was confusing and had led to similar errors by other nurses in the past. The system's design flaw contributed significantly to the error.
How would you classify this error? What actions should be taken?
Case Investigation B
Action: Sarah RN, due to time pressure and a high patient load, decided to skip the double-check protocol for administering the same insulin dose, believing it would save time without causing harm.
Findings: The investigation revealed that the hospital’s workload and time pressures often led to shortcuts in following safety protocols.
How would you classify this error? What actions should be taken?
Case Investigation C
Action: Sarah RN, is familiar with the protocol and knowingly bypassed the double check system, dismissing its importance and administering a medication dose on her own.
Findings: The investigation found that the nurse had a history of disregarding safety protocols, showing a pattern of reckless behavior. This behavior was not supported by the hospital’s policies or environment.
How would you classify this error? What actions should be taken?
Change is constant in the health care environment. Change is defined as the process of altering or replacing existing knowledge, skills, attitudes, systems, policies, or procedures.[281] The outcomes of change must be consistent with an organization’s mission, vision, and values. Although change is a dynamic process that requires alterations in behavior and can cause conflict and resistance, change can also stimulate positive behaviors and attitudes and improve organizational outcomes and employee performance. Change can result from identified problems or from the incorporation of new knowledge, technology, management, or leadership. Problems may be identified from many sources, such as quality improvement initiatives, employee performance evaluations, or accreditation survey results.[282]
Nurse managers must deal with the fears and concerns triggered by change. They should recognize that change may not be easy and may be met with enthusiasm by some and resistance by others. Leaders should identify individuals who will be enthusiastic about the change (referred to as “early adopters”), as well as those who will be resisters (referred to as "laggers"). Early adopters should be involved to build momentum, and the concerns of resisters should be considered to identify barriers. Data should be collected, analyzed, and communicated so the need for change (and its projected consequences) can be clearly articulated. Managers should articulate the reasons for change, the way(s) the change will affect employees, the way(s) the change will benefit the organization, and the desired outcomes of the change process.[283] See Figure 4.5[284] for an illustration of communicating upcoming change.

Change Theories
There are several change theories that nurse leaders may adopt when implementing change. Two traditional change theories are known as Lewin’s Unfreeze-Change-Refreeze Model and Lippitt’s Seven-Step Change Theory.[285]
Lewin’s Change Model
Kurt Lewin, the father of social psychology, introduced the classic three-step model of change known as Unfreeze-Change-Refreeze Model that requires prior learning to be rejected and replaced. Lewin’s model has three major concepts: driving forces, restraining forces, and equilibrium. Driving forces are those that push in a direction and cause change to occur. They facilitate change because they push the person in a desired direction. They cause a shift in the equilibrium towards change. Restraining forces are those forces that counter the driving forces. They hinder change because they push the person in the opposite direction. They cause a shift in the equilibrium that opposes change. Equilibrium is a state of being where driving forces equal restraining forces, and no change occurs. It can be raised or lowered by changes that occur between the driving and restraining forces.[286],[287]
- Step 1: Unfreeze the status quo. Unfreezing is the process of altering behavior to agitate the equilibrium of the current state. This step is necessary if resistance is to be overcome and conformity achieved. Unfreezing can be achieved by increasing the driving forces that direct behavior away from the existing situation or status quo while decreasing the restraining forces that negatively affect the movement from the existing equilibrium. Nurse leaders can initiate activities that can assist in the unfreezing step, such as motivating participants by preparing them for change, building trust and recognition for the need to change, and encouraging active participation in recognizing problems and brainstorming solutions within a group.[288]
- Step 2: Change. Change is the process of moving to a new equilibrium. Nurse leaders can implement actions that assist in movement to a new equilibrium by persuading employees to agree that the status quo is not beneficial to them; encouraging them to view the problem from a fresh perspective; working together to search for new, relevant information; and connecting the views of the group to well-respected, powerful leaders who also support the change.[289]
- Step 3: Refreeze. Refreezing refers to attaining equilibrium with the newly desired behaviors. This step must take place after the change has been implemented for it to be sustained over time. If this step does not occur, it is very likely the change will be short-lived and employees will revert to the old equilibrium. Refreezing integrates new values into community values and traditions. Nursing leaders can reinforce new patterns of behavior and institutionalize them by adopting new policies and procedures.[290]
Example Using Lewin’s Change Theory
A new nurse working in a rural medical-surgical unit identifies that bedside handoff reports are not currently being used during shift reports.
Step 1: Unfreeze: The new nurse recognizes a change is needed for improved patient safety and discusses the concern with the nurse manager. Current evidence-based practice is shared regarding bedside handoff reports between shifts for patient safety.[291] The nurse manager initiates activities such as scheduling unit meetings to discuss evidence-based practice and the need to incorporate bedside handoff reports.
Step 2: Change: The nurse manager gains support from the director of nursing to implement organizational change and plans staff education about bedside report checklists and the manner in which they are performed.
Step 3: Refreeze: The nurse manager adopts bedside handoff reports in a new unit policy and monitors staff for effectiveness.
Lippitt’s Seven-Step Change Theory
Lippitt’s Seven-Step Change Theory expands on Lewin’s change theory by focusing on the role of the change agent. A change agent is anyone who has the skill and power to stimulate, facilitate, and coordinate the change effort. Change agents can be internal, such as nurse managers or employees appointed to oversee the change process, or external, such as an outside consulting firm. External change agents are not bound by organizational culture, politics, or traditions, so they bring a different perspective to the situation and challenge the status quo. However, this can also be a disadvantage because external change agents lack an understanding of the agency's history, operating procedures, and personnel.[292] The seven-step model includes the following steps[293]:
- Step 1: Diagnose the problem. Examine possible consequences, determine who will be affected by the change, identify essential management personnel who will be responsible for fixing the problem, collect data from those who will be affected by the change, and ensure those affected by the change will be committed to its success.
- Step 2: Evaluate motivation and capability for change. Identify financial and human resources capacity and organizational structure.
- Step 3: Assess the change agent’s motivation and resources, experience, stamina, and dedication.
- Step 4: Select progressive change objectives. Define the change process and develop action plans and accompanying strategies.
- Step 5: Explain the role of the change agent to all employees and ensure the expectations are clear.
- Step 6: Maintain change. Facilitate feedback, enhance communication, and coordinate the effects of change.
- Step 7: Gradually terminate the helping relationship of the change agent.
Example Using Lippitt’s Seven-Step Change Theory
Refer to the previous example of using Lewin’s change theory on a medical-surgical unit to implement bedside handoff reporting. The nurse manager expands on the Unfreeze-Change-Refreeze Model by implementing additional steps based on Lippitt’s Seven-Step Change Theory:
- The nurse manager collects data from team members affected by the changes and ensures their commitment to success.
- Early adopters are identified as change agents on the unit who are committed to improving patient safety by implementing evidence-based practices such as bedside handoff reporting.
- Action plans (including staff education and mentoring), timelines, and expectations are clearly communicated to team members as progressive change objectives. Early adopters are trained as “super-users” to provide staff education and mentor other nurses in using bedside handoff checklists across all shifts.
- The nurse manager facilitates feedback and encourages two-way communication about challenges as change is implemented on the unit. Positive reinforcement is provided as team members effectively incorporate change.
- Bedside handoff reporting is implemented as a unit policy, and all team members are held accountable for performing accurate bedside handoff reporting.
Read more about additional change theories in the Current Theories of Change Management pdf.
Change Management
Change management is the process of making changes in a deliberate, planned, and systematic manner.[294] It is important for nurse leaders and nurse managers to remember a few key points about change management[295]:
- Employees will react differently to change, no matter how important or advantageous the change is purported to be. Recognizing this variability is crucial for effectively managing the transition process.
- Basic needs will influence reaction to change, such as the need to be part of the change process, the need to be able to express oneself openly and honestly, and the need to feel that one has some control over the impact of change. Ensuring these needs are met can significantly reduce resistance.
- Change often results in a feeling of loss due to changes in established routines. Employees may react with shock, anger, and resistance, but ideally will eventually accept and adopt change. Acknowledging these feelings and providing support can facilitate smoother transitions.
- Change must be managed realistically, without false hopes and expectations, yet with enthusiasm for the future. Employees should be provided information honestly and allowed to ask questions and express concerns. This transparency builds trust and helps in aligning everyone towards common goals.
Strategies for Effective Change Management
- Engage Stakeholders Early: Involve key stakeholders in the planning stages of the change process. Their input can provide valuable insights and help in identifying potential challenges early on.
- Communicate Clearly and Frequently: Clear and frequent communication is essential. Use multiple channels to disseminate information and ensure that the message is consistent and comprehensible to all staff members.
- Provide Training and Resources: Equip employees with the necessary skills and resources to adapt to the change. This might include training sessions, informational materials, or access to support personnel.
- Build a Supportive Culture: Create an environment where change is viewed positively. Encourage collaboration and create opportunities for employees to share their experiences and strategies for adapting to change.
- Monitor and Adjust: Continuously monitor the progress of the change initiative and be prepared to make adjustments as needed. Solicit feedback from employees and be responsive to their concerns.
There are multiple strategies that can employed to overcome resistance to change. First, it is important to understand the underlying reasons for resistance. Resistance is commonly aligned to feelings of fear, lack of trust in leadership, or logistical concerns regarding workload, seniority, etc. To implement change effectively, a leader should empower staff by making sure they feel that their voice is respected and valued. When individuals feel valued and hear, they are more likely to support change, even if they do not personally agree with all elements associated with the change. Leaders also must understand that change is stressful for individuals. Depending on the significance of change, a leader may take actions to ensure that employee assistance programs, support groups, or additional counseling services or resources are available. These additional resources can be beneficial for individuals as they work through the emotions associated with the proposed change. Additionally, the benefits for any change should be clearly described. It is important to highlight how the proposed change will help improve work processes and patient care quality. It is also helpful to acknowledge and demonstrate appreciation for early adopters of the change. This can provide motivation and encouragement for others to follow suit and fosters a positive attitude toward future changes.

