6.2 Basic Neurological Concepts
Open Resources for Nursing (Open RN)
When completing a neurological assessment, it is important to understand the functions performed by different parts of the nervous system while analyzing findings. For example, damage to specific areas of the brain, such as that caused by a head injury or cerebrovascular accidents (i.e., strokes), can cause specific deficits in speech, facial movements, or use of the extremities. Damage to the spinal cord, such as that caused by a motor vehicle accident or diving accident, will cause specific motor and sensory deficits according to the level where the spinal cord was damaged.
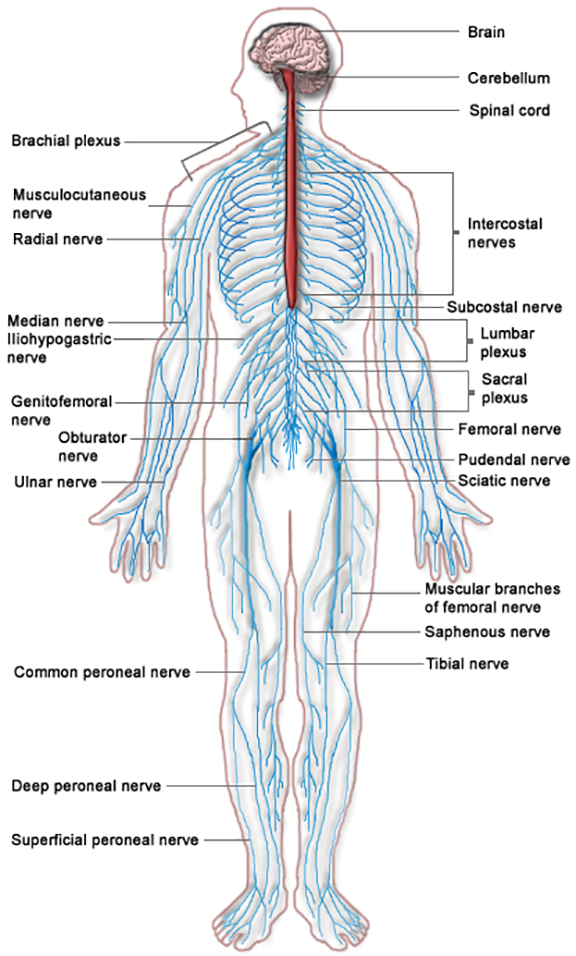
The nervous system is divided into two parts, the central nervous system and the peripheral nervous system. See Figure 6.1[1] for an image of the entire nervous system. The central nervous system (CNS) includes the brain and the spinal cord. The brain can be described as the interpretation center, and the spinal cord can be described as the transmission pathway. The peripheral nervous system (PNS) consists of the neurological system outside of the brain and spinal cord, including the cranial nerves that branch out from the brain and the spinal nerves that branch out from the spinal cord. The peripheral nervous system can be described as the communication network between the brain and the body parts. Both parts of the nervous system must work correctly for healthy body functioning.
Central Nervous System
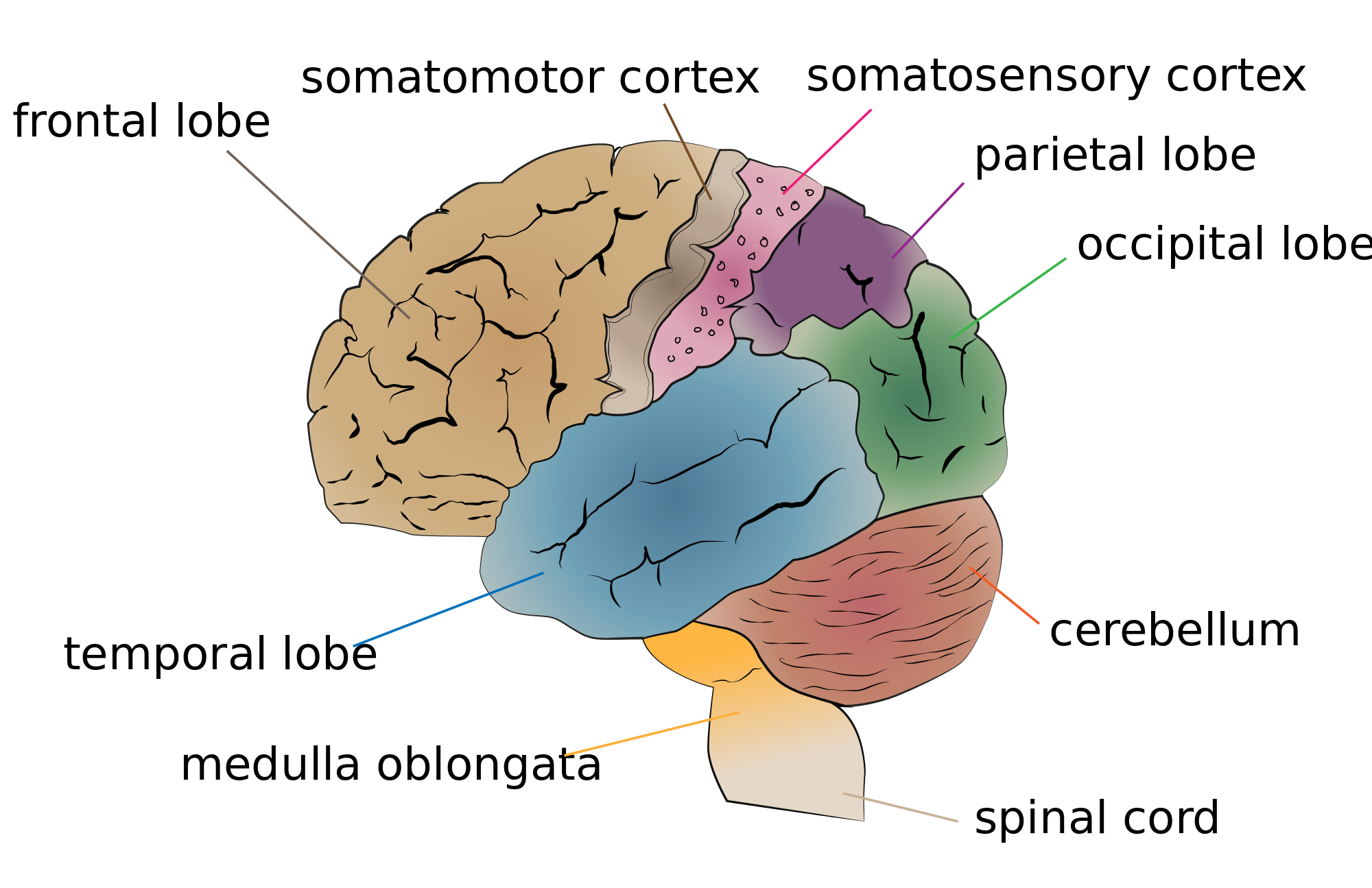
The major regions of the brain are the cerebrum and cerebral cortex, the diencephalon, the brain stem, and the cerebellum. See Figure 6.2[2] for an illustration of the cerebellum and the lobes of the cerebrum.
Cerebrum and Cerebral Cortex
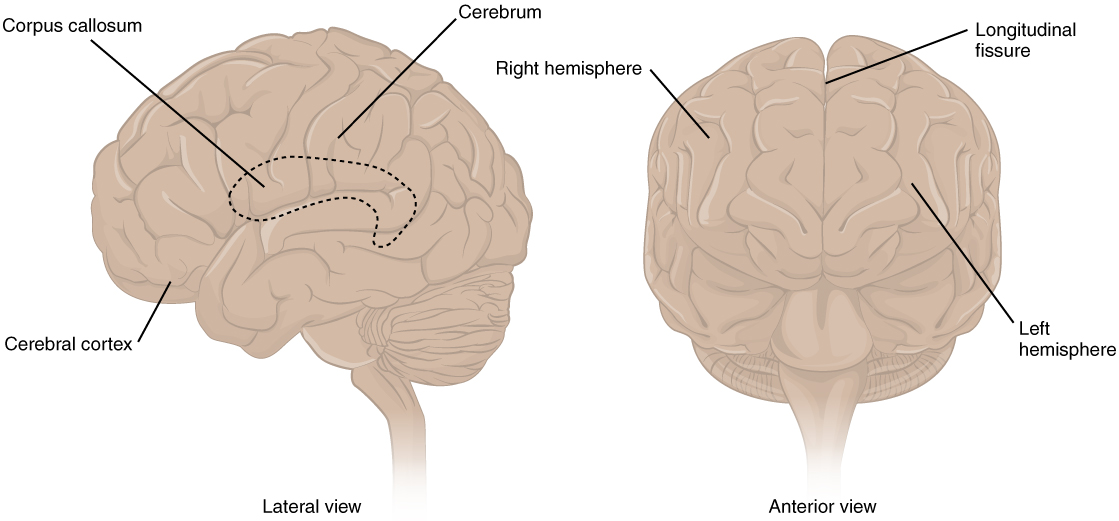
The largest portion of our brain is the cerebrum. The cerebrum is covered by a wrinkled outer layer of gray matter called the cerebral cortex. See Figure 6.3[3] for an image of the cerebral cortex. The cerebral cortex is responsible for the higher functions of the nervous system such as memory, emotion, and consciousness. The corpus callosum is the major pathway of communication between the right and left hemispheres of the cerebral cortex. The cerebral cortex is further divided into four lobes named the frontal, parietal, occipital, and temporal lobes.[4] Each lobe has specific functions.
Frontal Lobe
The frontal lobe is associated with movement because it contains neurons that instruct cells in the spinal cord to move skeletal muscles. The anterior portion of the frontal lobe is called the prefrontal lobe, and it provides cognitive functions such as planning and problem-solving that are the basis of our personality, short-term memory, and consciousness. Broca’s area is also located in the frontal lobe and is responsible for the production of language and controlling movements responsible for speech.[5]
Parietal Lobe
The parietal lobe processes general sensations from the body. All of the tactile senses are processed in this area, including touch, pressure, tickle, pain, itch, and vibration, as well as general senses of the body, such as proprioception (the sense of body position) and kinesthesia (the sense of movement).[6]
Temporal Lobe
The temporal lobe processes auditory information and is involved with language comprehension and production. Wernicke’s area and Broca’s area are located in the temporal lobe. Wernicke’s area is involved in the comprehension of written and spoken language, and Broca’s area is involved in the production of language. Because regions of the temporal lobe are part of the limbic system, memory is also an important function associated with the temporal lobe.[7] The limbic system is involved with our behavioral and emotional responses needed for survival, such as feeding, reproduction, and the fight – or – flight responses.
Occipital Lobe
The occipital lobe primarily processes visual information.[8]
Diencephalon
Information from the rest of the central and peripheral nervous system is sent to the cerebrum through the diencephalon, with the exception of the olfactory nerve that connects directly to the cerebrum.[9] See Figure 6.4[10] for an illustration of the diencephalon deep within the cerebrum. The diencephalon contains the hypothalamus and the thalamus.
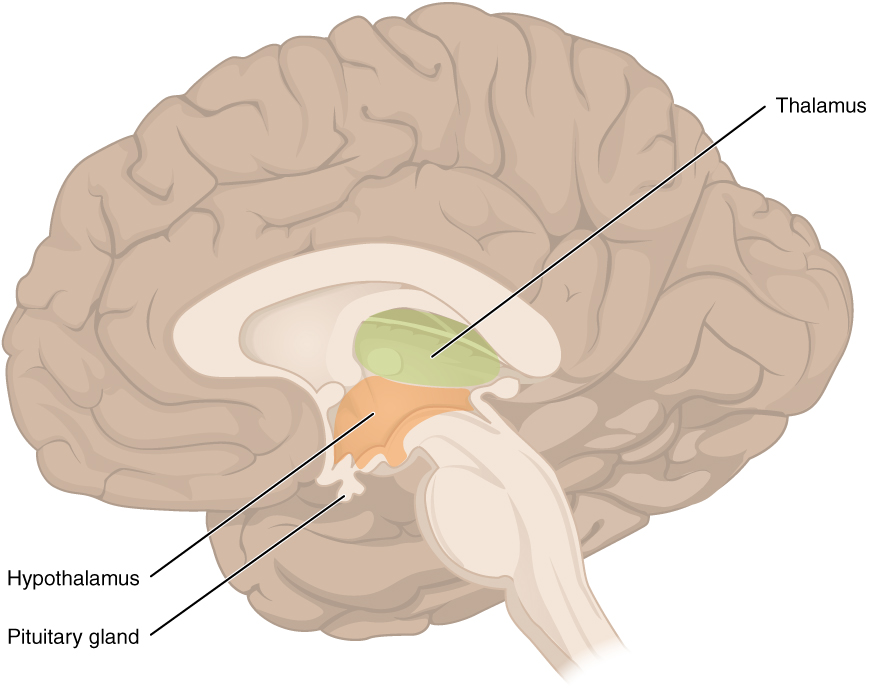
The hypothalamus helps regulate homeostasis such as body temperature, thirst, hunger, and sleep. The hypothalamus is also the executive region in charge of the autonomic nervous system and the endocrine system through its regulation of the anterior pituitary gland. Other parts of the hypothalamus are involved in memory and emotion as part of the limbic system.[11]
The thalamus relays sensory information and motor information in collaboration with the cerebellum. The thalamus does not just pass the information on, but it also processes and prioritizes that information. For example, the portion of the thalamus that receives visual information will influence what visual stimuli are considered important enough to receive further attention from the brain.[12]
Brain Stem
The brain stem is composed of the pons and the medulla. The pons and the medulla regulate several crucial autonomic functions in the body, including involuntary functions in the cardiovascular and respiratory systems, vasodilation, and reflexes like vomiting, coughing, sneezing, and swallowing. Cranial nerves also connect to the brain through the brain stem and provide sensory input and motor output.[13]
For more information about the functions of the autonomic nervous system, visit the “Autonomic Nervous System” chapter in the Open RN Nursing Pharmacology textbook.
Cerebellum
The cerebellum is located in the posterior part of the brain behind the brain stem and is responsible for fine motor movements and coordination. For example, when the motor neurons in the frontal lobe of the cerebral cortex send a command down the spinal cord to initiate walking, a copy of that instruction is also sent to the cerebellum. Sensory feedback from the muscles and joints, proprioceptive information about the movements of walking, and sensations of balance are sent back to the cerebellum. If the person becomes unbalanced while walking because the ground is uneven, the cerebellum sends out a corrective command to compensate for the difference between the original cerebral cortex command and the sensory feedback.[14]
Spinal Cord
The spinal cord is a continuation of the brain stem that transmits sensory and motor impulses. The length of the spinal cord is divided into regions that correspond to the level at which spinal nerves pass through the vertebrae. Immediately adjacent to the brain stem is the cervical region, followed by the thoracic, the lumbar, and finally the sacral region.[15] The spinal nerves in each of these regions innervate specific parts of the body. See more information under the “Spinal Nerves” subsection.
Review the anatomy of the brain using following supplementary video.
Review for Anatomy of the Brain on YouTube[16]
Peripheral Nervous System
The peripheral nervous system (PNS) consists of cranial nerves and spinal nerves that exist outside of the brain, spinal cord, and autonomic nervous system. The main function of the PNS is to connect the limbs and organs to the central nervous system (CNS). Sensory information from the body enters the CNS through cranial and spinal nerves. Cranial nerves are connected directly to the brain, whereas spinal nerves are connected to the brain via the spinal cord.
Peripheral nerves are classified as sensory nerves, motor nerves, or a combination of both. Sensory nerves carry impulses from the body to the brain for processing. Motor nerves transmit motor signals from the brain to the muscles to cause movement.
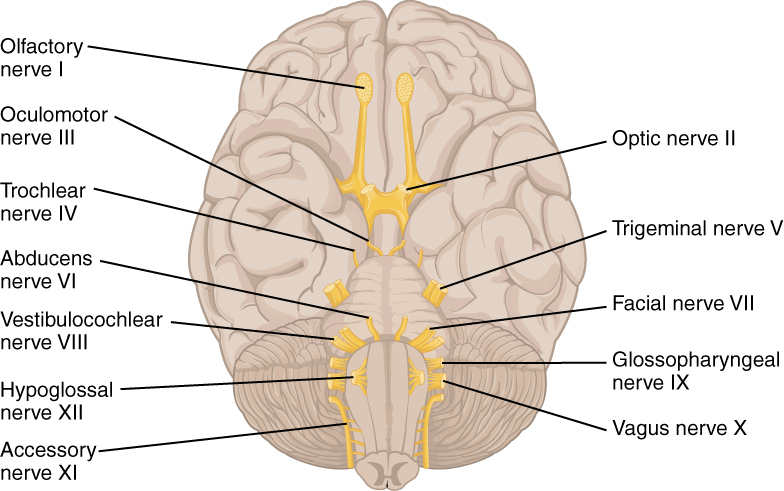
Cranial Nerves
Cranial nerves are directly connected from the periphery to the brain. They are primarily responsible for the sensory and motor functions of the head and neck. There are twelve cranial nerves that are designated by Roman numerals I through XII. See Figure 6.5[17] for an image of cranial nerves. Three cranial nerves are strictly sensory nerves; five are strictly motor nerves; and the remaining four are mixed nerves.[18] A traditional mnemonic for memorizing the names of the cranial nerves is “On Old Olympus Towering Tops A Finn And German Viewed Some Hops,” in which the initial letter of each word corresponds to the initial letter in the name of each nerve. A second popular mnemonic to assist with memorization is “Oh Once One Takes The Anatomy Final Very Good Vacations Are Heavenly”.
- The olfactory nerve is responsible for the sense of smell.
- The optic nerve is responsible for the sense of vision.
- The oculomotor nerve regulates eye movements by controlling four of the extraocular muscles, lifting the upper eyelid when the eyes point up and for constricting the pupils.
- The trochlear nerve and the abducens nerve are both responsible for eye movement but do so by controlling different extraocular muscles.
- The trigeminal nerve regulates skin sensations of the face and controls the muscles used for chewing.
- The facial nerve is responsible for the muscles involved in facial expressions, as well as part of the sense of taste and the production of saliva.
- The auditory/vestibulocochlear nerve manages hearing and balance.
- The glossopharyngeal nerve regulates the controlling muscles in the oral cavity and upper throat, as well as part of the sense of taste and the production of saliva.
- The vagus nerve is responsible for contributing to homeostatic control of the organs of the thoracic and upper abdominal cavities.
- The accessory nerve controls movements of the neck, along with cervical spinal nerves.
- The hypoglossal nerve manages the muscles of the lower throat and tongue.[19] Methods for assessing each of these nerves are described in the “Assessing Cranial Nerves” section.
Review of Cranial Nerves on YouTube[20]
Spinal Nerves
There are 31 spinal nerves that are named based on the level of the spinal cord where they emerge. See Figure 6.6[21] for an illustration of spinal nerves. There are eight pairs of cervical nerves designated C1 to C8, twelve thoracic nerves designated T1 to T12, five pairs of lumbar nerves designated L1 to L5, five pairs of sacral nerves designated S1 to S5, and one pair of coccygeal nerves. All spinal nerves are combined sensory and motor nerves. Spinal nerves extend outward from the vertebral column to innervate the periphery while also transmitting sensory information back to the CNS.[22]
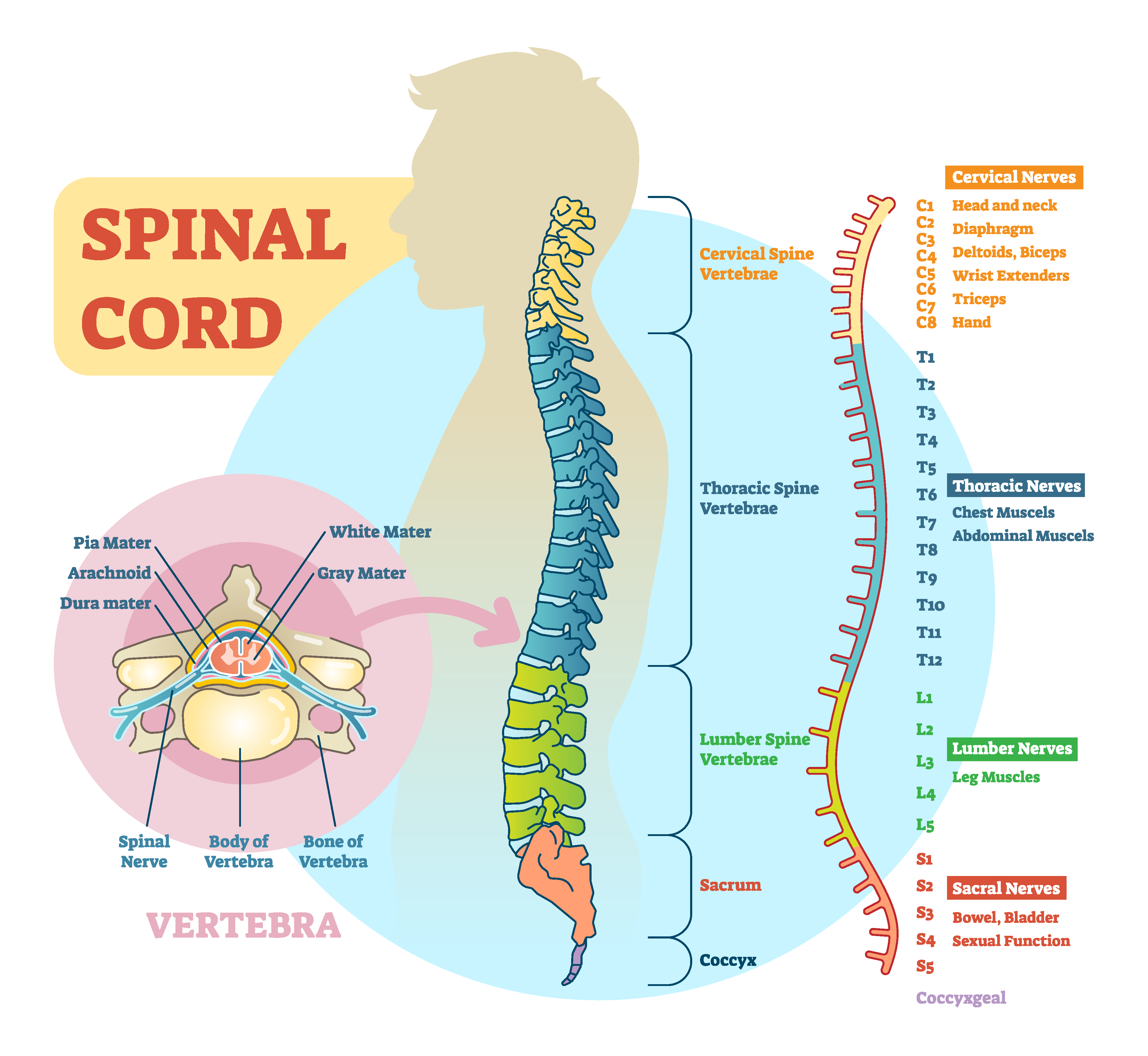
Functions of Spinal Nerves
Each spinal nerve innervates a specific region of the body:
- C1 provides motor innervation to muscles at the base of the skull.[23]
- C2 and C3 provide both sensory and motor control to the back of the head and behind the ears.[24]
- The phrenic nerve arises from nerve roots C3, C4, and C5. This is a vital nerve because it innervates the diaphragm to enable breathing. If a patient’s spinal cord is transected above C3 from an injury, then spontaneous breathing is not possible.[25]
- C5 through C8 and T1 combine to form the brachial plexus, a tangled array of nerves that serve the upper limbs and upper back.[26]
- The lumbar plexus arises from L1-L5 and innervates the pelvic region and the anterior leg.[27]
- The sacral plexus comes from the lower lumbar nerves L4 and L5 and the sacral nerves S1 to S4. The most significant systemic nerve to come from this plexus is the sciatic nerve. The sciatic nerve is associated with the painful medical condition sciatica, which is back and leg pain as a result of compression or irritation of the sciatic nerve.[28]
Functions of the Nervous System
The nervous system receives information about the environment around us (sensation) and generates responses to that information (motor responses). The process of integration combines sensory perceptions and higher cognitive functions such as memories, learning, and emotion while producing a response.
Sensation
Sensation is defined as receiving information about the environment. The major senses are taste, smell, touch, sight, and hearing. Additional sensory stimuli are also provided from inside the body, such as the stretch of an organ wall or the concentration of certain ions in the blood.[29]
Response
The nervous system produces a response based on the stimuli perceived by sensory nerves. For example, withdrawing a hand from a hot stove is an example of a response to a painfully hot stimulus. Responses can be classified by those that are voluntary (such as contraction of a skeletal muscle) and those that are involuntary (such as contraction of smooth muscle in the intestine). Voluntary responses are governed by the somatic nervous system, and involuntary responses are governed by the autonomic nervous system.[30]
Integration
Integration occurs when stimuli received by sensory nerves are communicated to the nervous system and the information is processed, leading to the generation of a conscious response. Consider this example of sensory integration. A batter in a baseball game does not automatically swing when they see the baseball thrown to them by the pitcher. First, the trajectory of the ball and its speed will need to be considered before creating the motor response of a swing. Then, integration will occur as the batter generates a conscious decision of whether to swing or not. Perhaps the count is three balls and one strike, and the batter decides to let this pitch go by in the hope of getting a walk to first base. Perhaps the batter is afraid to strike out and doesn’t swing, or maybe the batter learned the pitcher’s nonverbal cues the previous time at bat and is confident to take a swing at an anticipated fast ball. All of these considerations are included as part of the batter’s integration response and the higher-level functioning that occurs in the cerebral cortex.[31]
- “Nervous system diagram.png” by unknown is licensed under CC BY-NC-SA 3.0. Access for free at https://med.libretexts.org/Bookshelves/Nursing/Book%3A_Clinical_Procedures_for_Safer_Patient_Care_(Doyle_and_McCutcheon)/02%3A_Patient_Assessment/2.07%3A_Focused_Assessments ↵
- “Cerebrum lobes.svg” by Jkwchui is licensed under CC BY-SA 3.0 ↵
- “1305 CerebrumN.jpg” by OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/13-2-the-central-nervous-system ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “1310 Diencephalon.jpg” by OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/13-2-the-central-nervous-system ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- Forciea, B. (2015, May 12). Anatomy and physiology: Central nervous system: Brain anatomy v2.0 [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/DBRdInd2-Vg ↵
- “1320 The Cranial Nerves.jpg” by OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/13-4-the-peripheral-nervous-system ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- Forciea, B. (2015, May 12). Anatomy and physiology: Nervous system: Cranial nerves (v2.0) [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/JBEZh6CHogo ↵
- “1008694237-vector.png” by VectorMine on Shutterstock. All rights reserved. Imaged used with purchased permission. ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy and Physiology by Boundless.com and is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Anatomy and Physiology by Boundless.com and is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Anatomy and Physiology by Boundless.com and is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Anatomy and Physiology by Boundless.com and is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
Now that we have discussed various concepts related to oxygenation and hypoxia, we will explain how a nurse uses the nursing process to care for clients with alterations in oxygenation.
Assessment
When assessing a client’s oxygenation status, there are several subjective and objective assessments to include.
Subjective Assessment
The primary symptom to assess when a client is experiencing decreased oxygenation is their level of dyspnea, the medical term for the subjective feeling of shortness of breath or difficulty breathing. Clients can be asked to rate their dyspnea on a scale of 0-10, similar to using a pain rating scale.[1] The feeling of dyspnea can be very disabling for clients. There are many interventions that a nurse can implement to help improve the feeling of dyspnea and, thus, improve a client’s overall quality of life.
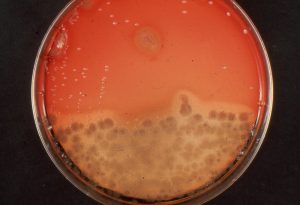
It is also important to ask clients if they are experiencing a cough. If a cough is present, determine if sputum is present, and if so, the color and amount of sputum. Sputum is mucus and other secretions that are coughed up and expelled from the mouth. The body always produces mucus to keep the delicate tissues of the respiratory tract moist so small particles of foreign matter can be trapped and forced out, but when there is an infection in the lungs, an excess of mucus is produced. The body attempts to get rid of this excess by coughing it up as sputum. The color of a client’s sputum can provide cues for underlying medical conditions. For example, sputum caused by a respiratory infection is often yellow, green, or brown and often referred to as purulent sputum.[2] See Figure 8.7[3] for an image of purulent sputum.

Clients should be asked if they are experiencing chest pain. Chest pain can occur with several types of respiratory and cardiac conditions, some of which are emergent. If the client reports chest pain, first determine if it is an emergency by asking questions such as:
- “Does it feel like something is sitting on your chest?”
- “Is the pain radiating into your jaw or arm?”
- “Do you feel short of breath, dizzy, or nauseated?”
If any of these symptoms are occurring, seek emergency medical assistance according to agency policy. If it is not a medical emergency, perform a focused assessment on the chest pain, including onset, location, duration, characteristics, alleviating or aggravating factors, radiation, and if any treatment has been used for the pain.[4] Noncardiac chest pain tends to worsen with coughing and deep breathing.
Objective Assessment
Focused objective assessments for a client suspected of experiencing decreased oxygenation include assessing the airway; evaluating respiratory rate, effort, and quality; analyzing pulse oximetry readings; auscultating lung sounds for adventitious sounds; and evaluating the heart rate for tachycardia.
Signs of cyanosis or clubbing should be noted. Clubbing is the enlargement of the fingertips that occurs with chronic hypoxia such as in chronic obstructive pulmonary disease (COPD) or congenital deficits in pediatric clients. See Figure 8.8[5] for an image of clubbing.

Another sign of chronic hypoxia that often occurs in clients with chronic respiratory diseases like COPD includes an increased anterior-posterior chest diameter, often referred to as a barrel chest. A barrel chest results from air trapping in the alveoli. See Figure 8.9[6] for an image of a barrel chest.

Diagnostic Tests and Lab Work
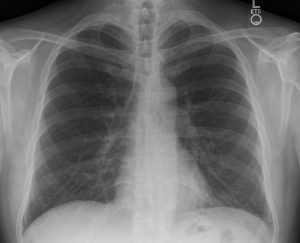
Diagnostic tests and lab work are based on the client’s medical condition that is causing the decreased oxygenation. For example, clients with a productive cough may have a chest X-ray or sputum culture ordered, and clients experiencing respiratory distress often have arterial blood gas (ABG) tests performed.
A chest X-ray is a fast and painless imaging test that uses certain electromagnetic waves to create pictures of the structures in and around the chest. This test can help diagnose and monitor conditions such as pneumonia, heart failure, lung cancer, and tuberculosis. Health care providers also use chest X-rays to see how well certain treatments are working and to check for complications after certain procedures or surgeries. Chest X-rays are contraindicated during pregnancy.[7],[8] See Figure 8.10[9] for an image of a chest X-ray.
A sputum culture is a diagnostic test that evaluates the type and number of bacteria present in sputum. The client is asked to cough deeply and spit any mucus that comes up into a sterile specimen container. The sample is sent to a lab where it is placed in a special dish and is watched for two to three days or longer to see if bacteria or other disease-causing germs grow. The data is used to determine appropriate antimicrobial therapy.[10] See Figure 8.11[11] for an image of a sputum culture.
For clients experiencing respiratory distress, arterial blood gas (ABG) tests are often ordered. Additional details about ABG tests are discussed in the “Oxygenation Basic Concepts” section of this chapter, as well as in the “Acid-Base Balance” section of the “Fluid and Electrolytes” chapter. See Table 8.3a for a summary of normal ranges of ABG values in adults.
Table 8.3a Normal Ranges of ABG Values in Adults
| Value | Description | Normal Range |
|---|---|---|
| pH | Acid-base balance of blood | 7.35-7.45 |
| PaO2 | Partial pressure of oxygen | 80-100 mmHg |
| PaCO2 | Partial pressure of carbon dioxide | 35-45 mmHg |
| HCO3 | Bicarbonate level | 22-26 mEq/L |
| SaO2 | Calculated oxygen saturation | 95-100% |
Diagnoses
Commonly used NANDA-I nursing diagnoses for clients experiencing decreased oxygenation and dyspnea include Impaired Gas Exchange, Ineffective Breathing Pattern, Ineffective Airway Clearance, Decreased Cardiac Output, and Activity Intolerance. See Table 8.3b for definitions and selected defining characteristics for these commonly used nursing diagnoses.[12] Use a current, evidence-based nursing care plan resource when creating a care plan for a client.
Table 8.3b NANDA-I Nursing Diagnoses Related to Decreased Oxygenation and Dyspnea
| NANDA-I Nursing Diagnoses | Definition | Selected Defining Characteristics |
|---|---|---|
| Impaired Gas Exchange | Excess or deficit in oxygenation and/or carbon dioxide elimination at the alveolar-capillary membrane. |
|
| Ineffective Breathing Pattern | Inspiration and/or expiration that does not provide adequate ventilation. | |
| Ineffective Airway Clearance | Inability to clear secretions or obstructions from the respiratory tract to maintain a clear airway. |
|
| Decreased Cardiac Output | Inadequate blood pumped by the heart to meet the metabolic demands of the body. |
|
| Activity Intolerance | Activity Intolerance: Insufficient physiological or psychological energy to endure or complete required or desired daily activities. |
|
For example, nurses commonly care for clients with chronic obstructive pulmonary disease (COPD). To select an accurate nursing diagnosis for a specific client with COPD, the nurse compares assessment findings with the defining characteristics of various nursing diagnoses. The nurse may select Ineffective Breathing Pattern after validating this client is demonstrating the associated signs and symptoms related to this nursing diagnosis:
- Dyspnea
- Increase in anterior-posterior chest diameter (e.g., barrel chest)
- Nasal flaring
- Orthopnea
- Prolonged expiration phase
- Pursed-lip breathing
- Tachypnea
- Use of accessory muscles to breathe
- Use of three-point position
Outcome Identification
A broad goal(s) for clients experiencing alterations in oxygenation is:
- The client will have adequate movement of air into and out of the lungs.[13]
A sample “SMART” outcome for a client experiencing dyspnea is:
- The client’s reported level of dyspnea will be within their stated desired range of 1-2 throughout their hospital stay.
Planning Interventions
According to NOC and NIC Linkages to NANDA-I and Clinical Conditions[14] and Nursing Interventions Classification (NIC),[15] Anxiety Reduction and Respiratory Monitoring are common categories of independent nursing interventions used to care for clients experiencing dyspnea and alterations in oxygenation. Anxiety Reduction is defined as, “Minimizing apprehension, dread, foreboding, or uneasiness related to an unidentified source of anticipated danger.”[16] Respiratory Monitoring is defined as, “Collection and analysis of client data to ensure airway patency and adequate gas exchange.”[17] Selected nursing interventions related to anxiety reduction and respiratory monitoring are listed in the following box.
Selected Nursing Interventions to Reduce Anxiety and Perform Respiratory Monitoring
Anxiety Reduction
- Use a calm, reassuring approach
- Explain all procedures, including sensations likely to be experienced during the procedure
- Provide factual information concerning diagnosis, treatment, and prognosis
- Stay with the client to promote safety and reduce fear
- Encourage the family to stay with the client, as appropriate
- Listen attentively
- Create an atmosphere of trust
- Encourage verbalization of feelings, perceptions, and fears
- Identify when level of anxiety changes
- Provide diversional activities geared toward the reduction of tension
- Instruct the client on the use of relaxation techniques
- Administer medications to reduce anxiety, as appropriate
Respiratory Monitoring
- Monitor rate, rhythm, depth, and effort of respirations
- Note chest movement, watching for symmetry and use of accessory muscles
- Monitor for noisy respirations such as snoring
- Monitor breathing patterns
- Monitor oxygen saturation levels in sedated clients
- Provide for noninvasive continuous oxygen sensors with appropriate alarm systems in clients with risk factors per agency policy and as indicated
- Auscultate lung sounds, noting areas of decreased or absent ventilation and presence of adventitious sounds
- Monitor client’s ability to cough effectively
- Note onset, characteristics, and duration of cough
- Monitor the client’s respiratory secretions
- Provide frequent intermittent monitoring of respiratory status in at-risk clients
- Monitor for dyspnea and events that improve and worsen it
- Monitor chest X-ray reports as appropriate
- Note changes in ABG values if ordered and notify provider as appropriate
- Institute resuscitation efforts as needed
- Institute respiratory therapy treatments as needed
In addition to the independent nursing interventions listed in the preceding box, several nursing interventions can be implemented to manage hypoxia, such as teaching enhanced breathing and coughing techniques, repositioning, managing oxygen therapy, administering medications, and providing suctioning. Refer to Table 8.2b in the “Oxygenation Basic Concepts” section earlier in this chapter for information about these interventions.
For additional details regarding managing oxygen therapy, see the “Oxygen Therapy” chapter in Open RN Nursing Skills, 2e.
Read more information about respiratory medications in the "Respiratory" chapter in Open RN Nursing Pharmacology, 2e.
Clients should also receive individualized health promotion teaching to enhance their respiratory status. Health promotion teaching includes encouraging activities such as the following:
- Receiving an annual influenza vaccine
- Receiving a pneumococcal vaccine every five years as indicated
- Stopping smoking
- Drinking adequate fluids to thin respiratory secretions
- Participating in physical activity as tolerated
Implementing Interventions
When implementing interventions that have been planned to enhance oxygenation, it is always important to assess the client’s current level of dyspnea and modify interventions based on the client’s current status. For example, if dyspnea has worsened, some interventions may no longer be appropriate (such as ambulating), and additional interventions may be needed (such as consulting with a respiratory therapist or administering additional medication).
Evaluation
After implementing interventions, the effectiveness of interventions should be documented, and the overall nursing care plan evaluated. Focused reassessments for evaluating improvement of oxygenation status include analyzing the client’s heart rate, respiratory rate, pulse oximetry reading, and lung sounds, in addition to asking the client to rate their level of dyspnea.
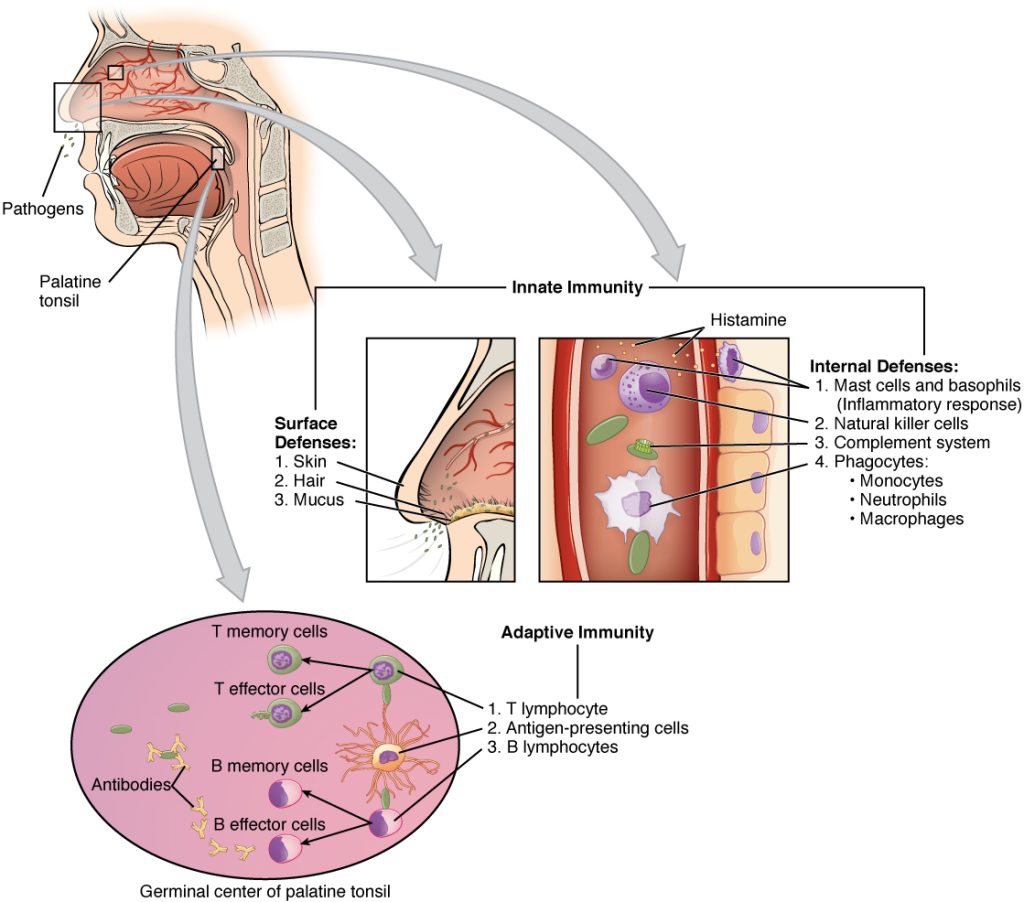
There are two basic ways the body defends against pathogens: nonspecific innate immunity and specific adaptive immunity.
Nonspecific Innate Immunity
Nonspecific innate immunity is a system of defenses in the body that targets invading pathogens in a nonspecific manner. It is called “innate” because it is present from the moment we are born. Nonspecific innate immunity includes physical defenses, chemical defenses, and cellular defenses.[18]
Physical Defenses
Physical defenses are the body’s most basic form of defense against infection. They include physical barriers to microbes, such as skin and mucous membranes, as well as mechanical defenses that physically remove microbes and debris from areas of the body where they might cause harm or infection. In addition, a person’s microbiome provides physical protection against disease as normal flora compete with pathogens for nutrients and cellular-binding sites.[19]
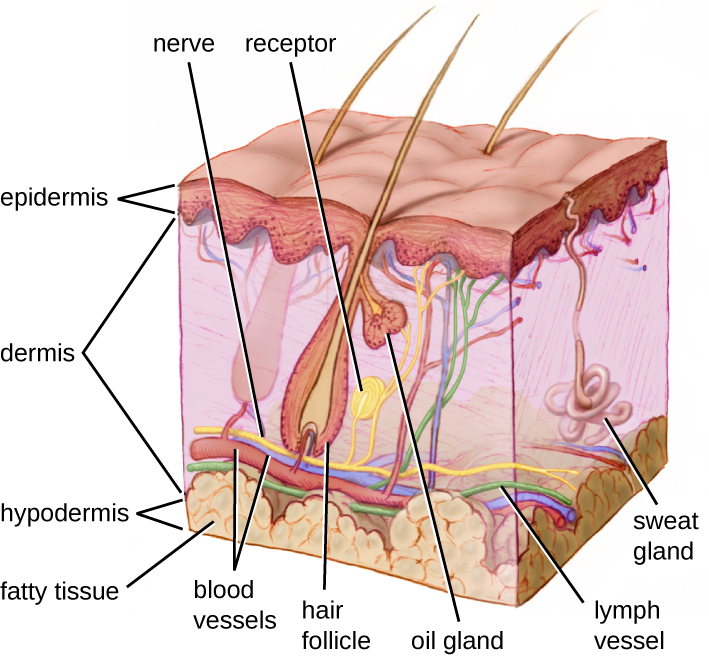
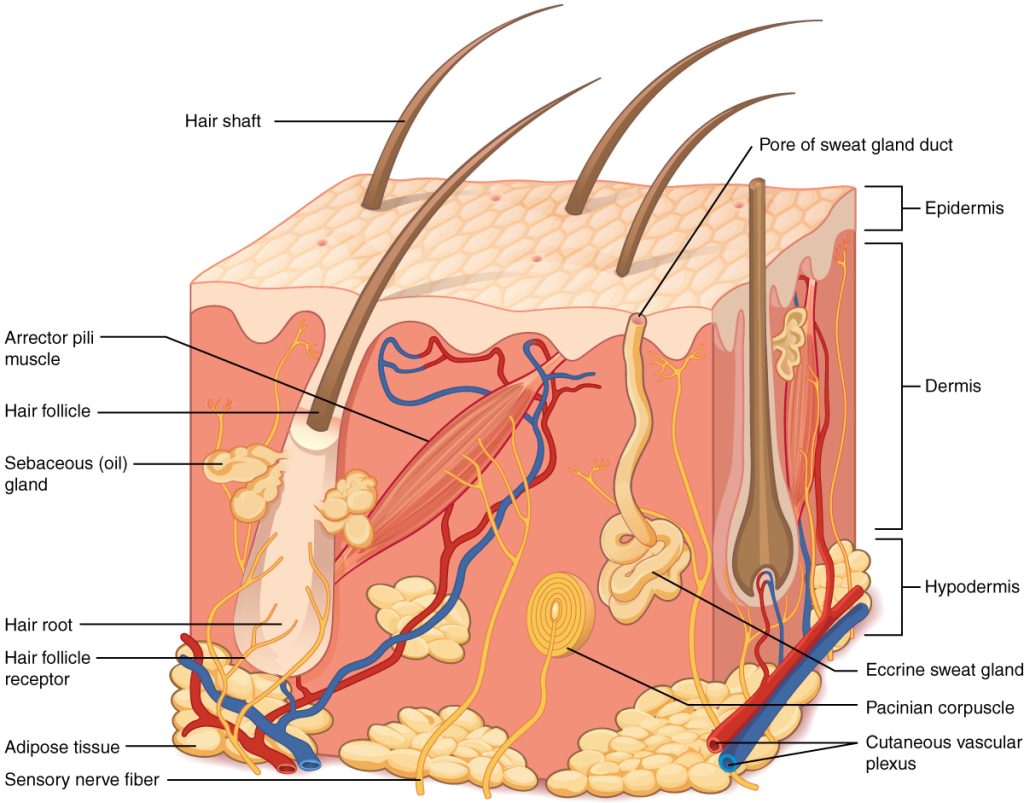
Skin
One of the body’s most important physical barriers is the skin barrier, which is composed of three layers of closely packed cells. See Figure 9.5[20] for an illustration of the layers of skin. The topmost layer of skin called the epidermis consists of cells that are packed with keratin. Keratin makes the skin’s surface mechanically tough and resistant to degradation by bacteria. Infections can occur when the skin barrier is broken, allowing the entry of opportunistic pathogens that infect the skin tissue surrounding the wound and possibly spread to deeper tissues.[21]
Mucus Membranes
The mucous membranes lining the nose, mouth, lungs, and urinary and digestive tracts provide another nonspecific barrier against potential pathogens. Mucous membranes consist of a layer of epithelial cells bound by tight junctions. The epithelial cells secrete a moist, sticky substance called mucous. Mucous covers and protects the fragile cell layers beneath it and also traps debris, including microbes. Mucus secretions also contain antimicrobial peptides.[22]
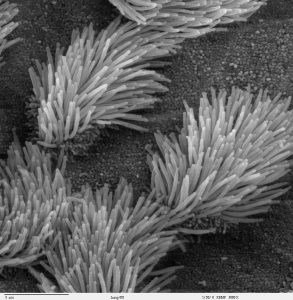
In many regions of the body, mechanical actions flush mucus (along with trapped or dead microbes) out of the body or away from potential sites of infection. For example, in the respiratory system, inhalation can bring microbes, dust, mold spores, and other small airborne debris into the body. This debris becomes trapped in the mucus lining the respiratory tract. The epithelial cells lining the upper parts of the respiratory tract have hair-like appendages known as cilia. Movement of the cilia propels debris-laden mucus out and away from the lungs. The expelled mucus is then swallowed and destroyed in the stomach, coughed up, or sneezed out. This system of removal is often called the mucociliary escalator. Disruption of the mucociliary escalator by the damaging effects of smoking can lead to increased colonization of bacteria in the lower respiratory tract and frequent infections, which highlights the importance of this physical barrier to host defenses.[23] See Figure 9.6[24] for an image of a magnified mucociliary escalator.
Like the respiratory tract, the digestive tract is a portal of entry through which microbes enter the body, and the mucous membranes lining the digestive tract provide a nonspecific physical barrier against ingested microbes. The intestinal tract is lined with epithelial cells, interspersed with mucus-secreting goblet cells. This mucus mixes with material received from the stomach, trapping foodborne microbes and debris, and is moved forward through the digestive tract via the mechanical action of peristalsis. Peristalsis refers to involuntary contraction and relaxation of the muscles of the intestine, creating wave-like movements that push digested content forward in the digestive tract.[25] For this reason, feces can contain microorganisms that can cause the spread of infection, making it essential to perform good hand hygiene to prevent transmission of disease through the fecal-oral route.
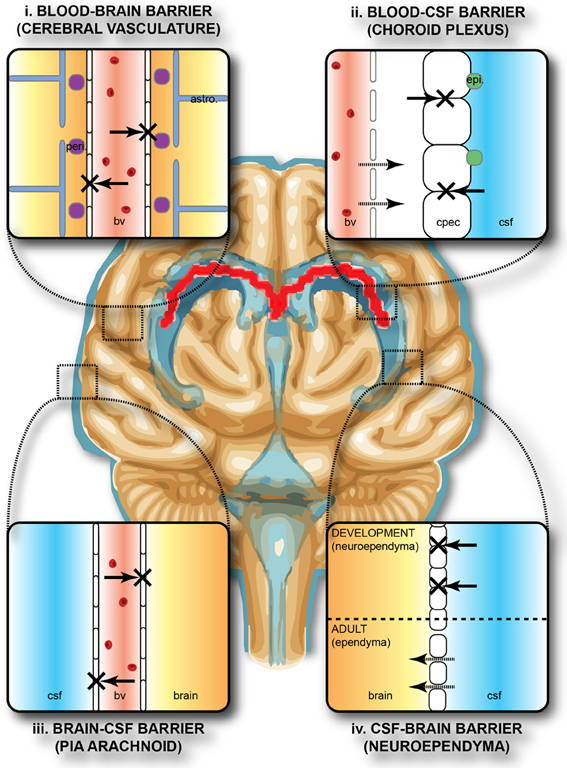
Endothelia
The epithelial cells lining the urogenital tract, blood vessels, lymphatic vessels, and other tissues are known as endothelia. These tightly packed cells provide an effective frontline barrier against invaders. The endothelia of the blood-brain barrier, for example, protects the central nervous system (CNS) from microorganisms. Infection of the CNS can quickly lead to serious and often fatal inflammation. The protection of the blood-brain barrier keeps the cerebrospinal fluid that surrounds the brain and spinal cord sterile.[26] See Figure 9.7[27] for an illustration of the blood-brain barrier.
Mechanical Defenses
In addition to physical barriers that keep microbes out, the body has several mechanical defenses that physically remove pathogens from the body and prevent them from taking up residence. For example, the flushing action of urine and tears serves to carry microbes away from the body. The flushing action of urine is responsible for the normally sterile environment of the urinary tract. The eyes have additional physical barriers and mechanical mechanisms for preventing infections. The eyelashes and eyelids prevent dust and airborne microorganisms from reaching the surface of the eye. Any microbes or debris that make it past these physical barriers is flushed out by the mechanical action of blinking, which bathes the eye in tears, washing debris away.[28] See Figure 9.8[29] for an image of an infant’s eyelashes that prevent dust from reaching the surface of the eye.

Microbiome
Normal flora that contributes to an individual’s microbiome serve as an important first-line defense against invading pathogens. Through their occupation of cellular binding sites and competition for available nutrients, normal flora prevents the early steps of pathogen attachment and proliferation required for the establishment of an infection. For example, in the vagina, normal flora competes with opportunistic pathogens like Candida albicans. This competition prevents yeast infection by limiting the availability of nutrients and inhibiting the growth of Candida, keeping its population in check. Similar competitions occur between normal flora and potential pathogens on the skin, in the upper respiratory tract, and in the gastrointestinal tract.[30]
The importance of the normal flora in host defenses is highlighted by a person’s increased susceptibility to infectious diseases when their microbiome is disrupted or eliminated. For example, treatment with antibiotics can significantly deplete the normal flora of the gastrointestinal tract, providing an advantage for pathogenic bacteria such as Clostridium difficile (C-diff) to colonize and cause diarrheal infection. Diarrhea caused by C-diff can be severe and potentially lethal. In fact, a recent strategy for treating recurrent C-diff infections is fecal transplantation that involves the transfer of fecal material from a donor into the intestines of the client as a method of restoring their normal flora.[31]
Chemical Defenses
In addition to physical defenses, our nonspecific innate immune system uses several chemical mediators that inhibit microbial invaders. The term chemical mediators encompass a wide array of substances found in various fluids and tissues throughout the body. For example, sebaceous glands in the dermis secrete an oil called sebum that is released onto the skin surface through hair follicles. Sebum provides an additional layer of defense by helping seal off the pore of the hair follicle and preventing bacteria on the skin’s surface from invading sweat glands and surrounding tissue. Environmental factors can affect these chemical defenses of the skin. For example, low humidity in the winter makes the skin drier and more susceptible to pathogens normally inhibited by the skin’s low pH. Application of skin moisturizer restores moisture and essential oils to the skin and helps prevent dry skin from becoming infected.[32]
Examples of other chemical defenses are enzymes, pH level, and chemical mediators. Enzymes in saliva and the digestive tract eliminate most pathogens that manage to survive the acidic environment of the stomach. In the urinary tract, the slight acidity of urine inhibits the growth of potential pathogens in the urinary tract. The respiratory tract also uses various chemical mediators in the nasal passages, trachea, and lungs that have antibacterial properties.[33]
Plasma Protein Mediators
In addition to physical, mechanical, and chemical defenses, there are also nonspecific innate immune factors in plasma, the fluid portion of blood, such as acute-phase proteins, complement proteins, and cytokines. These plasma protein mediators contribute to the inflammatory response.[34]
An example of an acute-phase protein is C-reactive protein. High levels of C-reactive protein indicate inflammation caused by a serious infection or other medical condition.[35]
Complement proteins are always present in the blood and tissue fluids, allowing them to be activated quickly. They aid in the destruction of pathogens by piercing their outer membranes (cell lysis) or by making them more attractive to phagocytic cells such as macrophages.[36]
Cytokines are proteins that affect interaction and communication between cells. When a pathogen enters the body, the first immune cell to notice the pathogen is like the conductor of an orchestra. That cell directs all the other immune cells by creating and sending out messages (cytokines) to the rest of the organs or cells in the body to respond to and initiate inflammation. Too many cytokines can have a negative effect and result in what's known as a cytokine storm.[37],[38] A cytokine storm is a severe immune reaction in which the body releases too many cytokines into the blood too quickly. A cytokine storm can occur as a result of an infection, autoimmune condition, or other disease. Signs and symptoms include high fever, inflammation, severe fatigue, and nausea. A cytokine storm can be severe or life-threatening and lead to multiple organ failure. For example, many COVID-19 complications and deaths were caused by a cytokine storm.[39],[40]
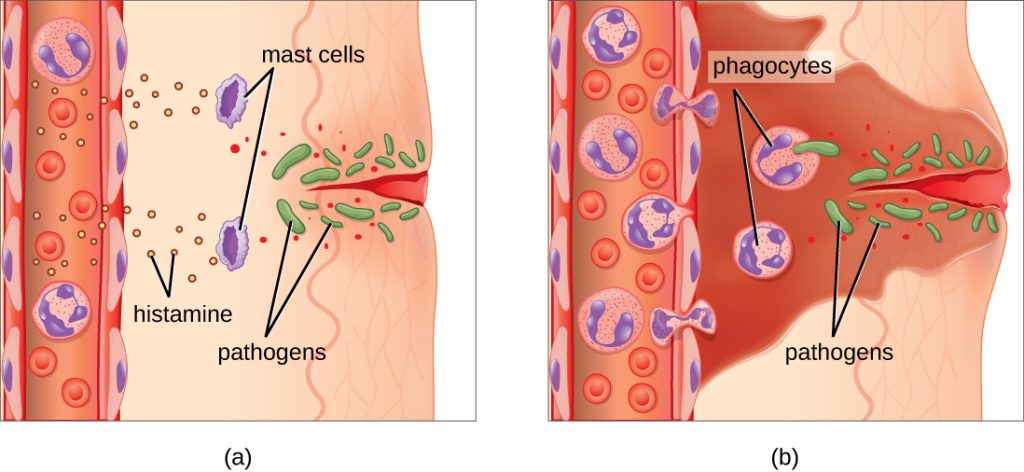
Inflammation
Inflammation is a response triggered by a cascade of chemical mediators and occurs when pathogens successfully breach the nonspecific innate immune system or when an injury occurs. Although inflammation is often perceived as a negative consequence of injury or disease, it is a necessary process that recruits cellular defenses needed to eliminate pathogens, remove damaged and dead cells, and initiate repair mechanisms. Excessive inflammation, however, can result in local tissue damage, and in severe cases, such as sepsis, it can become deadly.[41]
An immediate response to tissue injury is acute inflammation. Vasoconstriction occurs to minimize blood loss if injury has occurred. Vasoconstriction is followed by vasodilation with increased permeability of the blood vessels due to the release of histamine by mast cells. Histamine contributes to the five observable signs of the inflammatory response: erythema (redness), edema (swelling), heat, pain, and altered function. It is also associated with an influx of phagocytes at the site of injury and/or infection. See Figure 9.9[42] for an illustration of the inflammatory response, with (a) demonstrating when mast cells detect injury to nearby cells and release histamine, initiating an inflammatory response and (b) illustrating where histamine increases blood flow to the wound site and the associated increased vascular permeability allows fluid, proteins, phagocytes, and other immune cells to enter infected tissue. These events result in the swelling and reddening of the injured site. The increased blood flow to the injured site causes it to feel warm. Inflammation is also associated with pain due to these events stimulating nerve pain receptors in the tissue. Increasing numbers of neutrophils are then recruited to the area to fight pathogens. As the fight rages on, white blood cells are recruited to the area, and pus forms from the accumulation of neutrophils, dead cells, tissue fluids, and lymph. Typically, after a few days, macrophages clear out this pus.[43] During injury, if this nonspecific inflammatory process does not successfully kill the pathogens, infection occurs.
Fever
A fever is part of the inflammatory response that extends beyond the site of infection and affects the entire body, resulting in an overall increase in body temperature. Like other forms of inflammation, a fever enhances the nonspecific innate immune defenses by stimulating white blood cells to kill pathogens. The rise in body temperature also inhibits the growth of many pathogens. During fever, the client’s skin may appear pale due to vasoconstriction of the blood vessels in the skin to divert blood flow away from extremities, minimize the loss of heat, and raise the body’s core temperature. The hypothalamus also stimulates the shivering of muscles to generate heat and raise the core temperature.[44]
A low-level fever is thought to help an individual overcome an illness. However, in some instances, this immune response can be too strong, causing tissue and organ damage and, in severe cases, even death. For example, Staphylococcus aureus and Streptococcus pyogenes are capable of producing superantigens that cause toxic shock syndrome and scarlet fever, respectively. Both of these conditions are associated with extremely high fevers in excess of 42 °C (108 °F) that must be managed to prevent tissue injury and death.[45]
When a fever breaks, the hypothalamus stimulates vasodilation, resulting in a return of blood flow to the skin and a subsequent release of heat from the body. The hypothalamus also stimulates sweating, which cools the skin as the sweat evaporates.[46]
Specific Adaptive Immunity
Now that we have discussed several nonspecific innate defenses against a pathogen, let’s discuss specific adaptive immunity. Specific adaptive immunity is the immune response that is activated when the nonspecific innate immune response is insufficient to control an infection. There are two types of adaptive responses: the cell-mediated immune response, which is carried out by T cells, and the humoral immune response, which is controlled by activated B cells and antibodies.[47]
B cells mature in the bone marrow. B cells make Y-shaped proteins called antibodies that are specific to each pathogen and lock onto its surface and mark it for destruction by other immune cells. The five classes of antibodies are IgG, IgM, IgA, IgD, and IgE. They also turn into memory B cells. Memory B cells are stored and released in the event a specific antigen reappears in the future. This allows the immune system to mount a quick defense because of the previously created memory B cells.[48]
T cells mature in the thymus. T cells are categorized into three classes: helper T cells, regulatory T cells, and cytotoxic T cells. Helper T cells stimulate B cells to make antibodies and help killer cells develop. Killer T cells directly kill cells that have already been infected by a pathogen. T cells also use cytokines as messenger molecules to send chemical instructions to the rest of the immune system to ramp up its response.[49]
Specific adaptive immunity also creates memory cells for each specific pathogen that provides the host with long-term protection from reinfection with that pathogen. On reexposure, these memory cells facilitate an efficient and quick immune response. For example, when an individual recovers from chicken pox, the body develops a memory of the varicella-zoster virus that will specifically protect it from reinfection if it is exposed to the virus again. Vaccines are administered with the purpose of enhancing a person's specific adaptive immunity.[50]
See Figure 9.10[51] for an illustration of innate immunity and specific adaptive immunity that occur in response to a pathogen entering the body through the nose.
Skin
Skin is made up of three layers: epidermis, dermis, and hypodermis. See Figure 10.1[52] for an illustration of skin layers. The epidermis is the thin, topmost layer of the skin. It contains sweat gland duct openings and the visible part of hair known as the hair shaft. Underneath the epidermis lies the dermis where many essential components of skin function are located. The dermis contains hair follicles (the roots of hair shafts), sebaceous oil glands, blood vessels, endocrine sweat glands, and nerve endings. The bottommost layer of skin is the hypodermis (also referred to as the subcutaneous layer). It mostly consists of adipose tissue (fat), along with some blood vessels and nerve endings. Beneath the hypodermis layer lies bone, muscle, ligaments, and tendons.
Hair
Hair is a filament that grows from a hair follicle in the dermis of the skin. See Figure 10.2[53] for an illustration of a hair follicle. It consists mainly of tightly packed, keratin-filled cells called keratinocytes. The human body is covered with hair follicles except for the mucous membranes, lips, palms of the hands, and soles of the feet. The part of the hair that is located within the follicle is called the hair root, the only living part of the hair. The part of the hair that is visible above the surface of the skin is the hair shaft. The shaft of the hair has no biochemical activity and is considered dead.
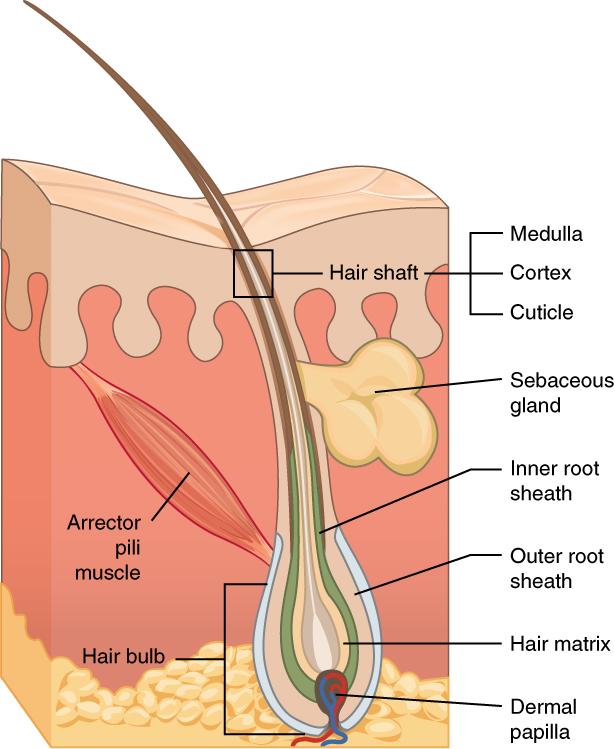
Functions of Hair
The functions of head hair are to provide insulation to retain heat and to protect the skin from damage by UV light. The function of hair in other locations on the body is debated. One idea is that body hair helps to keep us warm in cold weather. When the body is cold, the arrector pili muscles contract, causing hairs to stand up and trapping a layer of warm air above the epidermis. However, this action is more effective in mammals that have thick hair than it is in relatively hairless human beings.
Human hair has an important sensory function as well. Sensory receptors in the hair follicles can sense when the hair moves, whether it is because of a breeze or the touch of a physical object. Some hairs, such as the eyelashes, are especially sensitive to the presence of potentially harmful matter. The eyebrows protect the eyes from dirt, sweat, and rain. In addition, the eyebrows play a key role in nonverbal communication by expressing emotions such as sadness, anger, surprise, and excitement.[54]
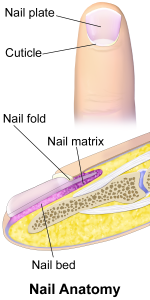
Nails
Nails are accessory organs of the skin. They are made of sheets of dead keratinocytes and are found on the distal ends of the fingers and toes. The keratin in nails makes them hard but flexible. Nails serve a number of purposes, including protecting the fingers, enhancing sensations, and acting like tools. A nail has three main parts: root, plate, and free margin. Other structures around or under the nail include the nail bed, cuticle, and nail fold. See Figure 10.3 for an illustration of the structure of a nail.[55],[56] The top diagram in this figure shows the external, visible part of the nail and the cuticle. The bottom diagram shows internal structures in a cross-section of the nail and nail bed.
Impaired Skin and Tissue Integrity
Skin integrity is a medical term that refers to skin health. Impaired skin integrity is a NANDA-I nursing diagnosis defined as, “Altered epidermis/or dermis.”[57] However, when deeper layers of the skin or integumentary structures are damaged, it is referred to as impaired tissue integrity. The NANDA-I definition of impaired tissue integrity is, “Damage to the mucous membrane, cornea, integumentary system, muscular fascia, muscle, tendon, bone, cartilage, joint capsule, and/or ligament.”[58]
Risk Factors Affecting Skin Health and Wound Healing
There are several risk factors that place a client at increased risk for altered skin health and delayed wound healing. Risk factors include impaired circulation and oxygenation, impaired immune function, diabetes, inadequate nutrition, obesity, exposure to moisture, smoking, and age. Each of these risk factors is discussed in more detail in the following subsections.
Impaired Circulation and Oxygenation
Skin, like every other organ in the body, depends on good blood perfusion to keep it healthy and functioning correctly. Cardiovascular circulation delivers important oxygen, nutrients, infection-fighting cells, and clotting factors to tissues. These elements are needed by skin, tissues, and nerves to properly grow, function, and repair damage. Without good cardiovascular circulation, skin becomes damaged. Damage can occur from poor blood perfusion from the arteries, as well as from poor return of blood through the veins to the heart. Common medical conditions that decrease cardiovascular circulation include cardiac disease, diabetes, and peripheral vascular disease (PVD). PVD includes two medical conditions called arterial insufficiency and venous insufficiency.
Arterial Insufficiency
Arterial insufficiency refers to a lack of adequately oxygenated blood movement in arteries to specific tissues. Arterial insufficiency can be a sudden, acute lack of oxygenated blood, such as when a blood clot in an artery blocks blood flow to a specific area. Arterial insufficiency can also be a chronic condition caused by peripheral vascular disease (PVD). As a person’s arteries become blocked with plaque due to atherosclerosis, there is decreased blood flow to the tissues. Signs of arterial insufficiency are cool skin temperature, pale skin color, pain that increases with exercise, and possible arterial ulcers.
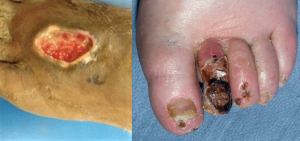
When oxygenated blood flow to tissues becomes inadequate, the tissue dies. This is called necrosis. Tissue death causes the skin and tissue to become necrotic (black). Necrotic tissue does not heal, so surgical debridement or amputation of the extremity becomes necessary for healing. See Figure 10.4[59] for images of an arterial insufficiency ulcer and necrotic toes.
Venous Insufficiency
Venous insufficiency occurs when the cardiovascular system cannot adequately return blood and fluid from the extremities to the heart. Venous insufficiency can cause stasis dermatitis when blood pools in the lower legs and leaks out into the skin and other tissues. Signs of venous insufficiency are edema, a brownish-leathery appearance to skin in the lower extremities, and venous ulcers that weep fluid.[60] See Figure 10.5[61] for an image of stasis dermatitis.

Impaired Immune Function
Skin contributes to the body’s immune function and is also affected by the immune system. Intact skin provides an excellent first line of defense against microorganisms entering the body. This is why it is essential to keep skin intact. If skin does break down, the next line of defense is a strong immune system that attacks harmful invading organisms. However, if the immune system is not working well, the body is much more susceptible to infections. This is why maintaining intact skin, especially in the presence of an impaired immune system, is imperative to decrease the risk of infections.
Stress can cause an impaired immune response that results in delayed wound healing.[62] Being hospitalized or undergoing surgery triggers the stress response in many clients. Medications, such as corticosteroids, also affect a client’s immune function and can impair wound healing.[63] When assessing a chronic wound that is not healing as expected, it is important to consider the potential effects of stress and medications.
Diabetes
Diabetes can cause wounds to develop, as well as delayed healing of wounds. This is due to elevated blood glucose causing stiffening of arterial walls, resulting in decreased circulation and tissue hypoxia. Elevated blood glucose also reduces leukocyte function, directly affecting wound healing and risk for infection. Additionally, if clients with diabetes also have diabetic neuropathy, they do not feel pain associated with skin injuries, resulting in delayed treatment and further risk of infection.[64] Nurses provide vital health teaching to clients with diabetes to help them effectively manage the disease and prevent complications.
Read more about diabetes in the “Antidiabetics” section of the “Endocrine” chapter in Open RN Nursing Pharmacology, 2e.
Inadequate Nutrition
A healthy diet is essential for maintaining healthy skin, as well as maintaining an appropriate weight. Nutrients that are particularly important for skin health include protein; vitamins A, C, D, and E; and minerals such as selenium, copper, and zinc.[65]
Nutritional deficiencies can have a profound impact on wound healing and must be addressed for chronic wounds to heal. Protein is one of the most important nutritional factors affecting wound healing. For example, in clients with pressure injuries, 30 to 35 kcal/kg of calorie intake with 1.25 to 1.5g/kg of protein and micronutrients supplementation are recommended daily.[66] In addition, vitamin C and zinc have many roles in wound healing. It is important to collaborate with a dietician to identify and manage nutritional deficiencies when a client is experiencing poor wound healing.[67]
Obesity
In the same way a balanced diet is vital for healthy skin, a healthy weight is also imperative. Obese individuals are at increased risk for fungal and yeast infections in skin folds caused by increased moisture and friction. See Figure 10.6[68] for an image of a fungal infection in the groin.[69] Symptoms of yeast and fungal infection include redness and scaliness of the skin associated with itching.

Obese clients also are at higher risk for wound complications due to a decreased supply of oxygenated blood flow to adipose tissue. Potential complications include infection, dehiscence (separation of the edges of a surgical wound), hematoma formation, pressure injuries, and venous ulcers.[70] Evisceration is a rare but severe complication when an abdominal surgical incision separates and the abdominal organs protrude or come out of the incision. Nurses can educate clients about making healthy lifestyle choices to reduce obesity and the risk of dehiscence. See Figure 10.7[71] for an image of a dehiscence in an abdominal surgical wound of an obese client.

Exposure to Moisture
Healthy skin needs good moisture balance. If too much moisture (i.e., sweat, urine, or water) is left on the skin for extended periods of time, the skin will become soggy, wrinkly, and turn whiter than usual and is called maceration. A simple example of maceration is when you spend too much time in a bathtub and your fingers and toes turn white and get “pruny.” See Figure 10.8[72] for an image of maceration. If healthy skin is exposed to moisture for an extended period of time, such as when a moist wound dressing is incorrectly applied on healthy skin, the skin will break down. This type of skin breakdown is called excoriation. Excoriation refers to removal of the topmost surface of the skin, which results in redness and abrasions. See Figure 10.9[73] for an image of excoriation.


The opposite occurs when skin lacks proper moisture. Skin becomes flaky, itchy, and cracked when it becomes too dry. Conditions such as decreased moisture in the air during cold winter months or bathing in hot water can worsen skin dryness. Dry skin, especially when accompanied with cracking, breaks the protective barrier and increases the risk of infection. It is important for nurses to apply emollient cream to clients’ areas of dry skin to maintain the protective skin barrier.
Smoking
Smoking impacts the inflammatory phase of the wound healing process, which can result in poor wound healing and an increased risk of infection, wound dehiscence, and necrosis. This is likely due to tissue hypoxia caused by toxins in tobacco smoke such as carbon monoxide and hydrogen cyanide, as well as vasoconstriction caused by nicotine.[74],[75] Clients who smoke should be encouraged to stop smoking.
Age
Older adults have thin, less elastic skin that puts them at increased risk for injury. They also have an altered inflammatory response that can impair wound healing. Additionally, the elderly are at risk for poor nutrition that contributes to poor wound healing. Nurses teach older clients about the importance of exercise for skin health and improved wound healing as appropriate.[76]
The remainder of this chapter will focus on applying the nursing process to a specific type of wound called a pressure injury. Pressure injuries are defined as, “Localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.” (Note that the 2016 NPUAP Pressure Injury Staging System now uses the term “pressure injury” instead of the historic term “pressure ulcer” because a pressure injury can occur without an ulcer present.) Pressure injuries commonly occur on the sacrum, heels, ischia, and coccyx and form when the skin layer of tissue gets caught between an external hard surface, such as a bed or chair, and the internal hard surface of a bone.
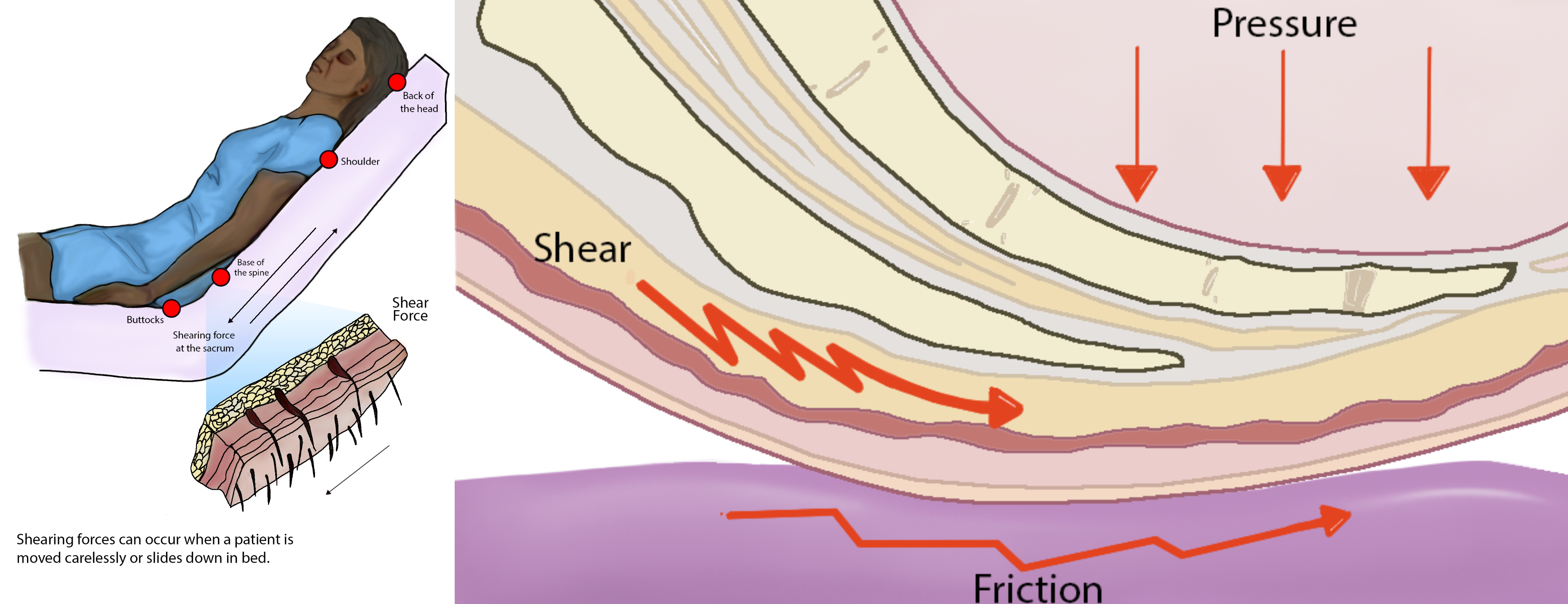
Shear occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue. For example, when a client slides down in bed, the outer layer of skin remains immobile because it remains attached to the sheets due to friction. However, the deeper layer of tissue (attached to bone) moves as the client slides down. This opposing movement of the outer layer of skin and the underlying tissues causes the capillaries to stretch and tear, which then causes decreased blood flow and oxygenation of the surrounding tissues resulting in a pressure injury.[77]
Friction refers to rubbing the skin against a hard object, such as the bed or the arm of a wheelchair. This rubbing causes heat, which can remove the top layer of skin and often results in skin damage. See Figure 10.13[78] for an illustration of shear and friction forces in the development of pressure injuries.
Hospital-acquired or worsening pressure injuries during hospitalization are considered "never events," meaning they are a serious, preventable medical errors that should never occur and require reporting to The Joint Commission. Additionally, the Centers for Medicare and Medicaid Services (CMS) and many private insurers will no longer pay for additional costs associated with "never events."[79],[80] Pressure injuries can be prevented with diligent assessment and nursing interventions such as frequent repositioning and providing good skin care.
Staging
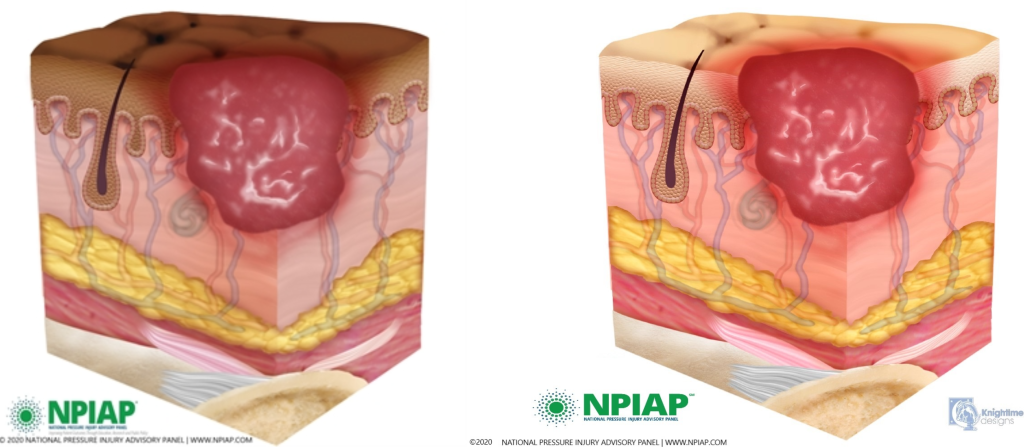
When assessed, pressure injuries are staged from 1 through 4 based on the extent of tissue damage. For example, Stage 1 pressure injuries have the least amount of tissue damage as evidenced by reddened, intact skin, whereas Stage 4 pressure injuries have the greatest amount of damage with deep, open ulcers affecting underlying tissue, muscle, ligaments, or tendons. See Figure 10.14[81] for images of four stages of pressure injuries.[82] Each stage is further described in the following subsections.
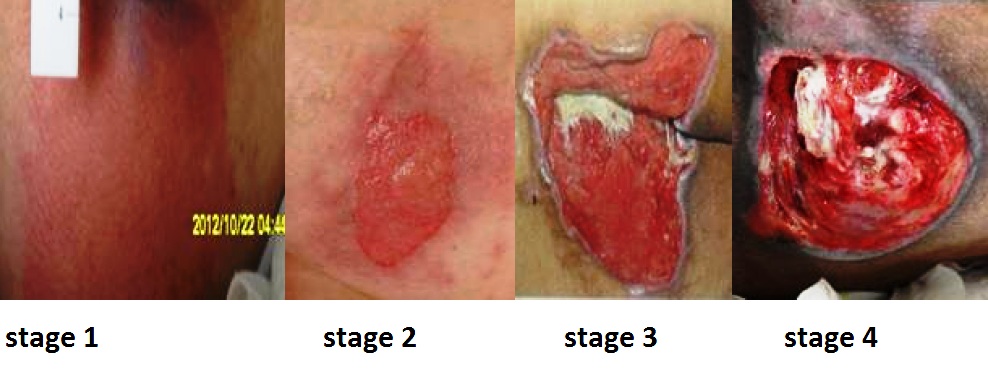
Stage 1 Pressure Injuries
Stage 1 pressure injuries are intact skin with a localized area of nonblanchable erythema where prolonged pressure has occurred. Nonblanchable erythema is a medical term used to describe an area of reddened skin that does not turn white when pressed. Nonblanchable erythema is an early sign of damage to underlying tissue caused by poor blood flow, ischemia, and damage to blood vessels in the area. Because damage is already present, there is a greater risk for Stage 1 pressure injuries to develop into worse pressure injuries if interventions to relieve pressure and not implemented. Skin with dark pigmentation may not demonstrate visible blanching, so it can be challenging to detect Stage 1 pressure injuries. For clients with dark pigmentation, nurses should assess for pain, firmness, softness, changes in temperature, or changes in color compared to surrounding areas.[83],[84]
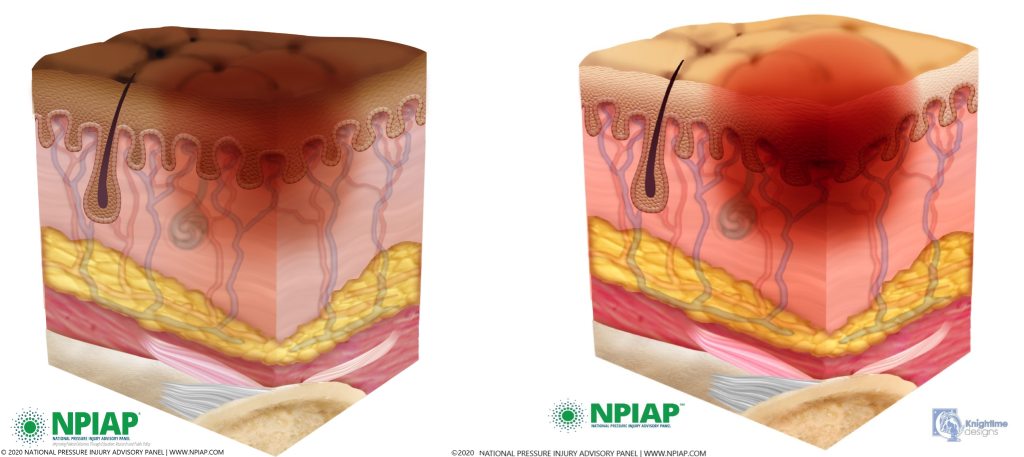
See Figure 10.15[85] for an illustration of a Stage 1 pressure injury.
Stage 2 Pressure Injuries
Stage 2 pressure injuries are partial-thickness loss of skin with exposed dermis. The wound has completely broken through the top layer of skin, and partly through the second layer, resulting in a shallow wound. The wound is shallow and generally open. The wound bed is viable and may appear like an intact or ruptured blister.[86] The wound area may be painful and the surrounding tissue may be swollen or discolored.[87] See Figure 10.16[88] for an illustration of a Stage 2 pressure injury.
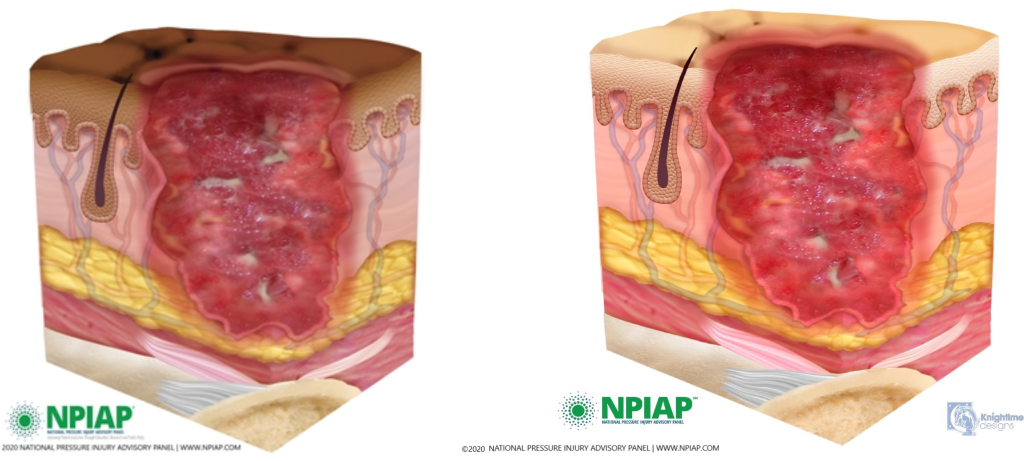
Stage 3 Pressure Injuries
Stage 3 pressure injuries are full-thickness tissue loss in which fat is visible, but cartilage, tendon, ligament, muscle, and bone are not exposed. The depth of tissue damage varies by anatomical location. Because the wound extends through all skin layers, there is increased risk of infection in Stage 3 pressure injuries. There may be pus draining from the wound, tissue necrosis, pain, or fever, especially in the presence of an infection.[89] See Figure 10.17[90] for an illustration of a Stage 3 pressure injury.
Undermining and tunneling may occur in Stage 3 and 4 pressure injuries. Undermining occurs when the tissue under the wound edge becomes eroded, resulting in a pocket beneath the skin. Tunneling refers to passageways underneath the skin surface that extend from a wound and can take twists and turns.
Slough and eschar may also be present in Stage 3 and 4 pressure injuries. Slough is inflammatory exudate that is usually light yellow, soft, and moist. Eschar is dark brown/black, dry, thick, and leathery dead tissue. If slough or eschar obscures the wound so that tissue loss cannot be assessed, the pressure injury is referred to as unstageable.[91] In most wounds, slough and eschar must be removed by debridement for accurate wound staging and for healing to occur. Removed of slough or eschar is surgically performed by specially trained health care providers. Nurses may apply prescribed chemical debridement agents or wet-to-dry dressings for mechanical debridement per provider orders.
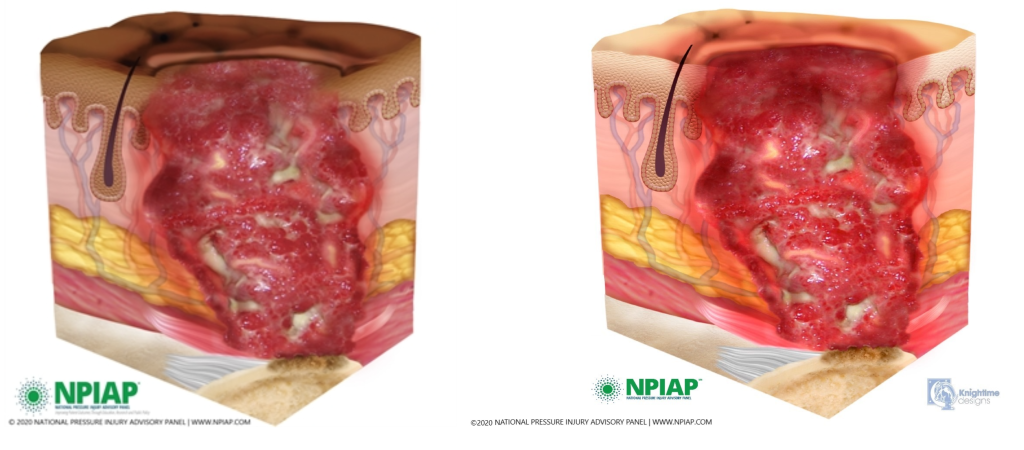
Stage 4 Pressure Injuries
Stage 4 pressure injuries are full-thickness tissue loss, like in Stage 3 pressure injuries, but also have exposed cartilage, tendon, ligament, muscle, or bone. Stage 4 pressure injuries are at an increased risk of infection because their depth goes through all skin layers. There may be pain associated with Stage 4 pressure ulcers, although they are often less painful because the wound damages nerve endings. There also at be firm or mushy texture at the site, discoloration, or necrosis to the wound. Because the wound often extends to the bone, thus exposing the bone to infectious agents in the environment, osteomyelitis (bone infection) may also be present. Osteomyelitis is a serious bone infection that may require amputation or cause death if not promptly treated aggressively with antibiotics.[92],[93]
See Figure 10.18[94] for an illustration of a Stage 4 pressure injury.
View images of different stages of pressure injuries on people with dark skin tones on the PPPIA Pressure Ulcers in People With Dark Skin Tones poster.
Unstageable Pressure Injuries
Unstageable pressure injuries are full-thickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If slough or eschar were to be removed, a Stage 3 or Stage 4 pressure injury would likely be revealed. However, dry and adherent eschar on the heel or ischemic limb is not typically removed.[95] See Figure 10.19[96] for an illustration of an unstageable pressure ulcer due to the presence of eschar (on the left side of the wound) and slough (on the right side of the wound).
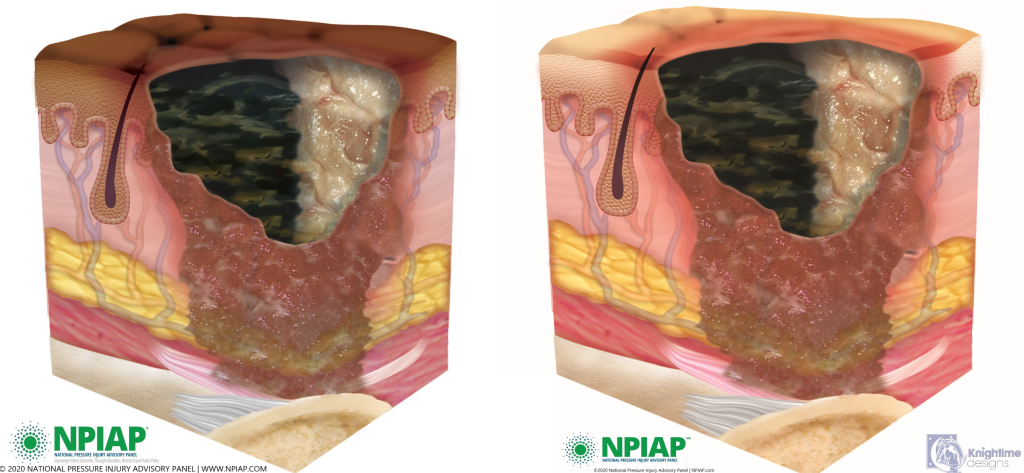
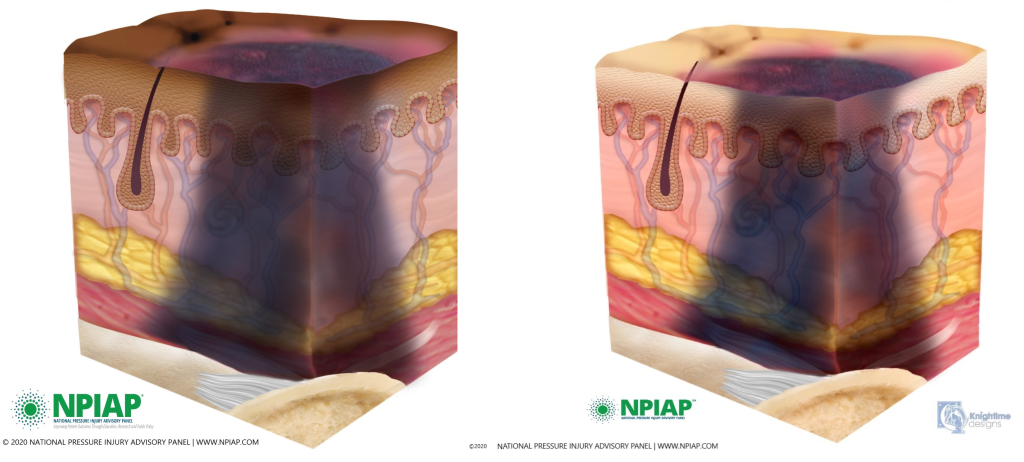
Deep Tissue Pressure Injuries
Deep tissue pressure injuries consist of persistent nonblanchable and deep red, maroon, or purple discoloration of an area. These discolorations typically reveal a dark wound bed or blood-filled blister. Be aware that the discoloration may appear differently in darkly pigmented skin. Deep tissue injury results from intense and/or prolonged pressure, as well as shear forces at the bone-muscle interface. The wound may evolve rapidly to reveal the actual extent of tissue injury, or it may resolve without tissue loss.[97],[98] See Figure 10.20 for an illustration of a deep tissue injury.
Video Review of Assessing Pressure Injuries[99]
Assessment
Subjective Assessment
During a subjective assessment of a client’s integumentary system, begin by asking about current symptoms such as itching, rashes, or wounds. If a client has a wound, it is important to determine if a client has pain associated with the wound so that pain management can be implemented. For clients with chronic wounds, it is also important to identify factors that delay wound healing, such as nutrition, decreased oxygenation, infection, stress, diabetes, obesity, medications, alcohol use, and smoking.[100] See Table 10.6a for a list of suggested interview questions to use when assessing a client with a wound.
If a client has a chronic wound or is experiencing delayed wound healing, it is important for the nurse to assess the impact of the wound on their quality of life. Reasons for this may include the frequency and regularity of dressing changes, which affect daily routine; a feeling of continued fatigue due to lack of sleep; restricted mobility; pain; odor; and the side effects of multiple medications. The loss of independence associated with functional decline can also lead to changes in overall health and well-being. These changes include altered eating habits, depression, social isolation, and a gradual reduction in activity levels.
Table 10.6a Interview Questions Related to Integumentary Disorders
| Symptoms | Questions | Follow-up Questions |
|---|---|---|
| Current Symptoms | Are you currently experiencing any skin symptoms such as itching, rashes, or an unusual mole? | Please describe. |
| Wounds | Do you have any current wounds such as a surgical incision, skin tear, arterial ulcer, venous ulcer, diabetic or neuropathic ulcer, or a pressure injury?
If a wound is present:
|
Please describe.
Use the PQRSTU method to comprehensively assess pain. Read more about the PQRSTU method in the "Pain Assessment Methods" section of the "Comfort" chapter. |
| Medical History | Have you ever been diagnosed with a wound related to diabetes, heart disease, or peripheral vascular disease? | Please describe. |
| If chronic wounds or wounds with delayed healing are present: | ||
| Medications | Are you taking any medications that can affect wound healing, such as oral steroids to treat inflammation or help you breathe? | Please describe. |
| Treatments | What have you used to try to treat this wound? | What was successful? Unsuccessful? |
| Symptoms of Infection (pain, purulent drainage, etc.) | Are you experiencing any symptoms of infection related to this wound such as increased pain or yellow/green drainage? | Please describe. |
| Stress | Have you experienced any recent stressors such as surgery, hospitalization, or a change in life circumstances? | How do you cope with stress in your life? |
| Smoking | Do you smoke? | How many cigarettes do you smoke a day? How long have you smoked? Have you considered quitting smoking? |
| Quality of Life | Has this wound impacted your quality of life? | Have you had any changes in eating habits, feelings of depression or social isolation, or a reduction in your usual activity levels? |
Objective Assessment
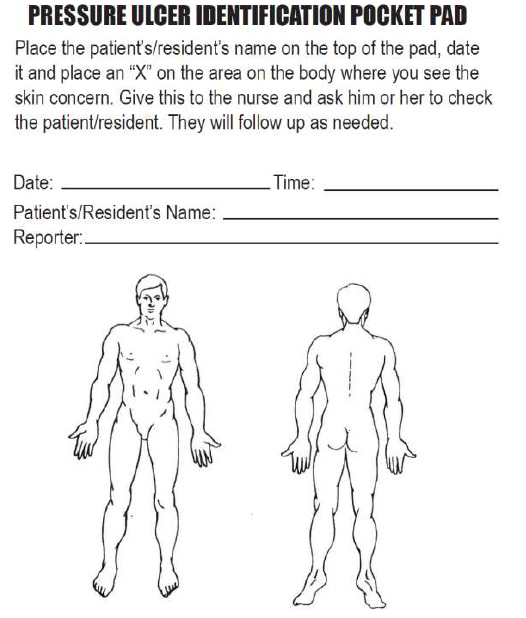
When performing an objective integumentary assessment on a client receiving inpatient care, it is important to perform a thorough exam on admission to check for existing wounds, as well as to evaluate their risk of skin breakdown using the Braden Scale. Agencies are not reimbursed for care of pressure injuries received during a client’s stay, so existing wounds on admission must be well-documented. Routine skin assessment should continue throughout a client’s stay, usually on a daily or shift-by-shift basis based on the client’s condition. If a wound is present, it is assessed during every dressing change for signs of healing. See Table 10.6b for components to include in a wound assessment. See Figure 10.22[101] for an image of a common tool used to document the location of a skin concern found during assessment.
Read more information about performing an overall integumentary assessment in the “Integumentary Assessment” chapter in Open RN Nursing Skills, 2e.
For additional discussion regarding assessing wounds, go to the “Assessing Wounds” section of the “Wound Care” chapter in Open RN Nursing Skills, 2e.
There are many common skin disorders that a nurse may find during assessment. Read more about common skin disorders in the “Common Integumentary Conditions” section of the “Integumentary Assessment” chapter in Open RN Nursing Skills, 2e.
Table 10.6b Wound Assessment
| Wound Assessment | |
|---|---|
| Type | Types of wounds may include abrasions, lacerations, burns, surgical incisions, pressure injuries, skin tears, arterial ulcers, or venous ulcers. It is important to understand the type of wound present to select appropriate interventions. |
| Location | The location of the wound should be documented precisely. A body diagram template is helpful to demonstrate exactly where the wound is located. |
| Size | Wound size should be measured regularly to determine if the wound is increasing or decreasing in size. Length is measured using the head-to-toe axis, and width is measured laterally. If tunneling or undermining is present, their depth should be assessed using a sterile, cotton-tipped applicator and documented using the clock method. |
| Degree of Tissue Injury | Wounds are classified as partial-thickness (meaning the epidermis and dermis are affected) or full-thickness (meaning the subcutaneous and deeper layers are affected). See Figure 10.1 in the “Basic Concepts” section for an image of the layers of skin.
For pressure injuries, it is important to assess the stage of the injury (see information on staging in the “Pressure Injuries” section). |
| Color of Wound Base | Assess the base of the wound for the presence of healthy, pink/red granulation tissue. Note the unhealthy appearance of dark red granulation tissue, white or yellow slough, or brown or black necrotic tissue. |
| Drainage | The color, consistency, and amount of exudate (drainage) should be assessed and documented at every dressing change. Drainage from wounds is often described as scant, small/minimal, moderate, and large/copious amounts. Use the following descriptions to select the appropriate terms:[102]
The type of wound drainage should be described using medical terms such as serosanguinous, sanguineous, serous, or purulent:
|
| Tubes or Drains | Check for patency and if they are attached correctly. |
| Signs and Symptoms of Infection | Assess for signs and symptoms of infection, which include the following:
|
| Wound Edges and Periwound | Assess the surrounding skin for maceration or signs of infection. |
| Pain | Assess for pain in the wound or during dressing changes. If pain is present, use the PQRSTU or OLDCARTES method to obtain a comprehensive pain assessment. |

See Table 10.6c for a comparison of expected versus unexpected findings on integumentary assessment.
Table 10.6c Expected Versus Unexpected Findings
| Assessment | Expected Findings | Unexpected Findings |
|---|---|---|
| Skin | Color: appropriate for ethnicity
Temperature: warm to touch Texture: smooth, soft, and supple Turgor: resilient Integrity: no wounds or lesions noted Sensory: no pain or itching noted |
Color: pale, white, red, yellow, purple, black and blue
Temperature: cool or hot to touch Texture: rough, scaly or thick; thin and easily torn; dry and cracked Turgor: tenting noted Integrity: rashes, lesions, abrasions, burns, lacerations, surgical wounds, pressure injuries noted Pain or pruritus (itching) present |
| Hair | Full distribution of hair on the head, axilla, and genitalia | Alopecia (hair loss), hirsutism (excessive hair growth over body), lice and/or nits, or lesions under hair |
| Nails | Smooth, well-shaped, and firm but flexible | Cracked, chipped, or splitting nail; excessively thick; presence of clubbing; ingrown nails |
| Skin Integrity | Skin intact with no wounds or pressure injuries. Braden Scale is 23 | A wound or pressure injury is present, or there is risk of developing a pressure injury with a Braden scale score of less than 23 |
Diagnostic and Lab Work
When a chronic wound is not healing as expected, laboratory test results can provide additional clues for the delayed healing. See Table 10.6d for a summary of lab results that offer clues to systemic issues causing delayed wound healing.
Table 10.6d Lab Values Associated with Delayed Wound Healing[108]
| Abnormal Lab Value | Rationale |
|---|---|
| Low hemoglobin | Low hemoglobin indicates less oxygen is transported to the wound site. |
| Elevated white blood cells (WBC) | Increased WBC indicates infection is occurring. |
| Low platelets | Platelets have an important role in the creation of granulation tissue. |
| Low albumin | Low albumin indicates decreased protein levels. Protein is required for effective wound healing. |
| Elevated blood glucose or hemoglobin A1C | Elevated blood glucose and hemoglobin A1C levels indicate poor management of diabetes mellitus, a disease that negatively impacts wound healing. |
| Elevated serum BUN and creatinine | BUN and creatinine levels are indicators of kidney function, with elevated levels indicating worsening kidney function. Elevated BUN (blood urea nitrogen) levels impact wound healing because it can indicate increased breakdown of the body's protein stores due to deficient protein in the diet. |
| Positive wound culture | Positive wound cultures indicate an infection is present and provide additional information including the type and number of bacteria present, as well as identifying antibiotics the bacteria is susceptible to. The nurse reviews this information when administering antibiotics to ensure the prescribed therapy is effective for the type of bacteria present. |
Life Span and Cultural Considerations
Newborns and Infants
Newborn skin is thin and sensitive. It tends to be easy to scratch and bruise and is susceptible to rashes and irritation. Common rashes seen in newborns and infants include diaper rash (contact dermatitis), cradle cap (seborrheic dermatitis), newborn acne, and prickly heat.
Toddlers and Preschoolers
Because of high levels of activity and increasing mobility, this age group is more prone to accidents. Issues like lacerations, abrasions, burns, and sunburns can occur frequently. It is important to be highly aware of the potential for accidents and implement safety precautions as needed.
School-Aged Children and Adolescents
Skin rashes tend to affect skin within this age group. Impetigo, scabies, and head lice are commonly seen and may keep children home from school. Acne vulgaris typically begins during adolescence and can alter physical appearance, which can be very upsetting to this age group. Another change during adolescence is the appearance of axillary, pubic, and other body hair. Also, as these children spend more time out of doors, sunburns are more common, and care should be given to encourage sunscreen and discourage the use of tanning beds.
Adults and Older Adults
As skin ages, many changes take place. Because aging increases the loss of subcutaneous fat and collagen breakdown, skin becomes thinner and wrinkles deepen. Decreased sweat gland activity leads to drier skin and pruritus (itching). Wound healing is slowed because of reduced circulation and the inability of proteins and proper nutrients to arrive at injury sites. Hair loses pigmentation and turns gray or white. Nails become thicker and are more difficult to cut. Age or liver spots become darker and more noticeable. The number of skin growths increases and includes skin tags and keratoses.
Diagnoses
There are several NANDA-I nursing diagnoses related to clients experiencing skin alterations or those at risk of developing a skin injury. See Table 10.6e for common NANDA-I nursing diagnoses and their definitions.[109]
Table 10.6e Common NANDA-I Nursing Diagnoses Related to Integumentary Disorders[110]
| Risk for Pressure Injury: “Susceptible to localized injury to the skin and/or underlying tissue usually over a bony prominence as a result of pressure, or pressure in combination with shear.” |
| Impaired Skin Integrity: “Altered epidermis and/or dermis.” |
| Risk for Impaired Skin Integrity: “Susceptible to alteration in epidermis and/or dermis, which may compromise health.” |
| Impaired Tissue Integrity: “Damage to the mucous membrane, cornea, integumentary system, muscular fascia, muscle, tendon, bone, cartilage, joint capsule, and/or ligament.” |
| Risk for Impaired Tissue Integrity: “Susceptible to damage to the mucous membrane, cornea, integumentary system, muscular fascia, muscle, tendon, bone, cartilage, joint capsule, and/or ligament, which may compromise health.” |
A commonly used NANDA-I nursing diagnosis for clients experiencing alterations in the integumentary system is Impaired Tissue Integrity, defined as, “Damage to the mucous membrane, cornea, integumentary system, muscular fascia, muscle, tendon, bone, cartilage, joint capsule, and/or ligament.”
To verify accuracy of this diagnosis for a client, the nurse compares assessment findings with defining characteristics of that diagnosis. Defining characteristics for Impaired Tissue Integrity include the following:
- Acute pain
- Bleeding
- Destroyed tissue
- Hematoma
- Localized area hot to touch
- Redness
- Tissue damage
A sample NANDA-I diagnosis in current PES format would be: “Impaired Tissue Integrity related to insufficient knowledge about protecting tissue integrity as evidenced by redness and tissue damage.”
Outcome Identification
An example of a broad goal for a client experiencing alterations in tissue integrity is:
- The client will experience tissue healing.
A sample SMART expected outcome for a client with a wound is:
- The client’s wound will decrease in size and have increased granulation tissue within two weeks.
Planning Interventions
In addition to the interventions outlined under the “Braden Scale” section to prevent and treat pressure injury, see the following box for a list of interventions to prevent and treat impaired skin integrity. As always, consult a current, evidence-based nurse care planning resource for additional interventions when planning client care.
Selected Interventions to Prevent and Treat Impaired Skin Integrity [111],[112],[113]
- Assess and document the client’s skin status routinely. (Frequency is determined based on the client’s status.)
- Use the Braden Scale to identify clients at risk for skin breakdown. Customize interventions to prevent and treat skin breakdown according to client needs.
- If a wound is present, evaluate the healing process at every dressing change. Note and document characteristics of the wound, including size, appearance, staging (if applicable), and drainage. Notify the provider of new signs of infection or lack of progress in healing.
- Provide wound care treatments, as prescribed by the provider or wound care specialist, and monitor the client's response toward expected outcomes.
- Cleanse the wound per facility protocol or as ordered.
- Maintain non-touch or aseptic technique when performing wound dressing changes, as indicated. (Read more details about using aseptic technique and the non-touch method in the "Aseptic Technique" chapter of the Open RN Nursing Skills,2e textbook.)
- Change wound dressings as needed to keep them clean and dry and prevent bacterial reservoir.
- Monitor for signs of infection in an existing wound (as indicated by redness, warmth, edema, increased pain, reddened appearance of surrounding skin, fever, increased white blood cell count, changes in wound drainage, or sudden change in client’s level of consciousness).
- Apply lotion to dry areas to prevent cracking.
- Apply lubricant to moisten lips and oral mucosa, as needed.
- Keep skin free of excess moisture. Use moisture barrier ointments (protective skin barriers) or incontinence products in skin areas subject to increased moisture and risk of skin breakdown.
- Educate the client and/or family caregivers on caring for the wound and request return demonstrations, as appropriate.
- Administer medications, as prescribed, and monitor for expected effects.
- Consult with a wound specialist, as needed.
- Obtain specimens of wound drainage for wound culture, as indicated, and monitor results.
- Advocate for pressure-relieving devices in clients at risk for pressure injuries, such as elbow protectors, heel protectors, chair cushions, and specialized mattresses and monitor the client's response.
- Promote adequate nutrition and hydration intake, unless contraindicated.
- Use a minimum of two-person assistance and a draw sheet to pull a client up in bed to minimize shear and friction.
- Reposition the client frequently to prevent skin breakdown and to promote healing. Turn the immobilized client at least every two hours, according to a specific schedule.
- Maintain a client’s position at 30 degrees or less, as appropriate, to prevent shear.
- Keep bed linens clean, dry, and wrinkle free.
Implementation
Before implementing interventions, it is important to assess the current status of the skin and risk factors present for skin breakdown and modify interventions based on the client’s current status. For example, if a client's rash has resolved, some interventions may no longer be appropriate (such as applying topical creams). However, if a wound is showing signs of worsening or delayed healing, additional interventions may be required. As always, if the client demonstrates new signs of localized or systemic infection, the provider should be notified.
Evaluation
It is important to evaluate for healing when performing wound care. Use the following expected outcomes when evaluating wound healing:
- Resolution of periwound redness in 1 week
- 50% reduction in wound dimensions in 2 weeks
- Reduction in volume of exudate
- 25% reduction in amount of necrotic tissue/eschar in 1 week
- Decreased pain intensity during dressing changes[114]
If a client is experiencing delayed wound healing or has a chronic wound, it is helpful to advocate for a referral to a wound care nurse specialist.
Read a sample nursing care plan for a client with impaired skin integrity.
Before discussing assessments and interventions related to promoting good nutrition, let’s review the structure and function of the digestive system, essential nutrients, and nutritional guidelines.
Digestive System
The digestive system breaks down food and then absorbs nutrients into the bloodstream via the small intestine and large intestine. Because good health depends on good nutrition, any disorder affecting the functioning of the digestive system can significantly impact overall health and well-being and increase the risk of chronic health conditions.
Structure and Function
The gastrointestinal system (also referred to as the digestive system) is responsible for several functions, including digestion, absorption, and immune response. Digestion begins in the upper gastrointestinal tract at the mouth, where chewing of food occurs, called mastication. Mastication results in mechanical digestion when food is broken down into small chunks and swallowed. Masticated food is formed into a bolus as it moves toward the pharynx in the back of the throat and then into the esophagus. Coordinated muscle movements in the esophagus called peristalsis move the food bolus into the stomach where it is mixed with acidic gastric juices and further broken down into chyme through a chemical digestion process. As chyme is moved out of the stomach and into the duodenum of the small intestine, it is mixed with bile from the gallbladder and pancreatic enzymes from the pancreas for further digestion.[115]
Absorption is a second gastrointestinal function. After chyme enters the small intestine, it comes into contact with tiny fingerlike projections along the inside of the intestine called villi. Villi increase the surface area of the small intestine and allow nutrients, such as protein, carbohydrates, fat, vitamins, and minerals, to absorb through the intestinal wall and into the bloodstream. Absorption of nutrients is essential for metabolism to occur because nutrients fuel bodily functions and create energy. Peristalsis moves leftover liquid from the small intestine into the large intestine, where additional water and minerals are absorbed. Waste products are condensed into feces and excreted from the body through the anus.[116] See Figure 14.1[117] for labeled parts of the gastrointestinal system.
In addition to digestion and absorption, the gastrointestinal system is also involved in immune function. Good bacteria in the stomach create a person’s gut biome. Gut biome contributes to a person’s immune response through antibody production in response to foreign materials, chemicals, bacteria, and other substances.[118] For example, clients may develop Clostridium difficile (C-diff) after taking antibiotics that kill these beneficial bacteria in the gut. Read additional details about our microbiome and immune response in the “Infection” chapter of this book.
Essential Nutrients
Nutrients from food and fluids are used by the body for growth, energy, and bodily processes. Essential nutrients refer to nutrients that are necessary for bodily functions but must come from dietary intake because the body is unable to synthesize them. Essential nutrients include vitamins, minerals, some amino acids, and some fatty acids.[119] Essential nutrients can be further divided into macronutrients and micronutrients.
Macronutrients
Macronutrients make up most of a person’s diet and provide energy, as well as essential nutrient intake. Macronutrients include carbohydrates, proteins, and fats. However, too many macronutrients without associated physical activity cause excess nutrition that can lead to obesity, cardiovascular disease, diabetes mellitus, kidney disease, and other chronic diseases. Too few macronutrients result in undernutrition, which contributes to nutrient deficiencies and malnourishment.[120]
Carbohydrates
Carbohydrates are sugars and starches and are an important energy source that provides 4 kcal/g of energy. Simple carbohydrates are small molecules (called monosaccharides or disaccharides) and break down quickly. As a result, simple carbohydrates are easily digested and absorbed into the bloodstream, so they raise blood glucose levels quickly. Examples of simple carbohydrates include table sugar, syrup, soda, and fruit juice. Complex carbohydrates are larger molecules (called polysaccharides) that break down more slowly, which causes slower release into the bloodstream and a slower increase in blood sugar over a longer period of time. Examples of complex carbohydrates include whole grains, beans, and vegetables.[121]
Foods can also be categorized according to their glycemic index, a measure of how quickly glucose levels increase in the bloodstream after carbohydrates are consumed. The glycemic index was initially introduced as a way for people with diabetes mellitus to control their blood glucose levels. For example, processed foods, white bread, white rice, and white potatoes have a high glycemic index. They quickly raise blood glucose levels after being consumed and also cause the release of insulin, which can result in more hunger and overeating. However, foods such as fruit, green leafy vegetables, raw carrots, kidney beans, chickpeas, lentils, and bran breakfast cereals have a low glycemic index. These foods minimize blood sugar spikes and insulin release after eating, which leads to less hunger and overeating. Eating a diet of low glycemic foods has been linked to a decreased risk of obesity and diabetes mellitus.[122] See Figure 14.2[123] for an image of the glycemic index of various foods.

Proteins
Proteins are peptides and amino acids that provide 4 kcal/g of energy. Proteins are necessary for tissue repair and function, growth, energy, fluid balance, clotting, and the production of white blood cells. Protein status is also referred to as nitrogen balance. Nitrogen is consumed in dietary intake and excreted in the urine and feces. If the body excretes more nitrogen than it takes in through the diet, this is referred to as a negative nitrogen balance. Negative nitrogen balance is seen in clients with starvation or severe infection. Conversely, if the body takes in more nitrogen through the diet than what is excreted, this is referred to as a positive nitrogen balance.[124] During positive nitrogen balance, excess protein is converted to fat tissue for storage.
Proteins are classified as complete, incomplete, or partially complete. Complete proteins must be ingested in the diet. They have enough amino acids to perform necessary bodily functions, such as growth and tissue maintenance. Examples of foods containing complete proteins are soy, quinoa, eggs, fish, meat, and dairy products. Incomplete proteins do not contain enough amino acids to sustain life. Examples of incomplete proteins include most plants, such as beans, peanut butter, seeds, grains, and grain products. Incomplete proteins must be combined with other types of proteins to add to amino acids and form complete protein combinations.[125] For example, vegetarians must be careful to eat complementary proteins, such as grains and legumes, or nuts and seeds and legumes, to create complete protein combinations during their daily food intake. Partially complete proteins have enough amino acids to sustain life, but not enough for tissue growth and maintenance. Because of the similarities, most sources consider partially complete proteins to be in the same category as incomplete proteins. See Figure 14.3[126] for an image of protein-rich foods.

Fats
Fats consist of fatty acids and glycerol and are essential for tissue growth, insulation, energy, energy storage, and hormone production. Fats provide 9 kcal/g of energy.[127] While some fat intake is necessary for energy and uptake of fat-soluble vitamins, excess fat intake contributes to heart disease and obesity. Due to its high-energy content, a little fat goes a long way.
Fats are classified as saturated, unsaturated, and trans fatty acids. Saturated fats come from animal products, such as butter and red meat (e.g., steak). Saturated fats are solid at room temperature. Recommended intake of saturated fats is less than 10% of daily calories because saturated fat raises cholesterol and contributes to heart disease.[128]
Unsaturated fats come from oils and plants, although chicken and fish also contain some unsaturated fats. Unsaturated fats are healthier than saturated fats. Examples of unsaturated fats include olive oil, canola oil, avocados, almonds, and pumpkin seeds. Fats containing omega-3 fatty acids are considered polyunsaturated fats and help lower LDL cholesterol levels. Fish and other seafood are excellent sources of omega-3 fatty acids.
Trans fats are fats that have been altered through a hydrogenation process, so they are not in their natural state. During the hydrogenation process, fat is changed to make it harder at room temperature and have a longer shelf life. Trans fats are found in processed foods, such as chips, crackers, and cookies, as well as in some margarines and salad dressings. Minimal trans-fat intake is recommended because it increases cholesterol and contributes to heart disease.[129]
Micronutrients
Micronutrients include vitamins and minerals.
Vitamins
Vitamins are necessary for many bodily functions, including growth, development, healing, vision, and reproduction. Most vitamins are considered essential because they are not manufactured by the body and must be ingested in the diet. Vitamin D is also manufactured through exposure to sunlight.[130]
Vitamin toxicity can be caused by overconsumption of certain vitamins, such as vitamins A, D, C, B6, and niacin. Conversely, vitamin deficiencies can be caused by various factors, including poor food intake due to poverty, malabsorption problems with the gastrointestinal tract, drug and alcohol abuse, proton pump inhibitors, and prolonged parenteral nutrition. Deficiencies can take years to develop, so it is usually a long-term problem for clients.[131]
Vitamins are classified as water soluble or fat soluble. Water-soluble vitamins are not stored in the body and include vitamin C and B-complex vitamins: B1 (thiamine), B2 (riboflavin), B3 (niacin), B6 (pyridoxine), B12 (cyanocobalamin), and B9 (folic acid). Additional water-soluble vitamins include biotin and pantothenic acid. Excess amounts of these vitamins are excreted through the kidneys in urine, so toxicity is rarely an issue, though excess intake of vitamin B6, C, or niacin can result in toxicity.[132] See Table 14.2a for a list of selected water-soluble vitamins, their sources, and their function.[133],[134],[135],[136],[137],[138],[139],[140],[141]
Table 14.2a Selected Water-Soluble Vitamins
| Water-Soluble Vitamin | Sources | Functions | Deficiency |
|---|---|---|---|
| C (Ascorbic Acid) | Citrus fruits, broccoli, greens, sweet peppers, tomatoes, lettuce, potatoes, tropical fruits, and strawberries | Infection prevention, wound healing, collagen formation, iron absorption, amino acid metabolism, antioxidant, and bone growth in children. | Early Signs: weakness, weight loss, myalgias, and irritability. Late Signs: scurvy; swollen, spongy gums; loose teeth; bleeding gums and skin; poor wound healing; edema; leg pain; anorexia; irritability; and poor growth in children. |
| B1 (Thiamine) | Nuts, liver, whole grains, pork, and legumes | Nerve function; metabolism of carbohydrates, fat, amino acids, glucose, and alcohol; appetite and digestion. | Fatigue, memory deficits, insomnia, chest pain, abdominal pain, anorexia, numbness of extremities, muscle wasting, heart failure, and shock in severe cases. |
| B2 (Riboflavin) | Eggs, liver, leafy greens, milk, and whole grains | Protein and carbohydrate metabolism, healthy skin, and normal vision. | Pallor, lip fissures, and seborrheic dermatitis. |
| B3 (Niacin) | Fish, chicken, eggs, dairy, mushrooms, peanut butter, whole grains, and red meat | Glycogen metabolism, cell metabolism, tissue regeneration, fat synthesis, nerve function, digestion, and skin health. | Pellagra characterized by skin lesions at pressure points/sun exposed skin, glossitis (swollen tongue), constipation progressing to bloody diarrhea, abdominal pain, abdominal distention, nausea, psychosis, and encephalopathy. |
| B6 (Pyridoxine) | Organ meats, fish, and various fruits and vegetables | Protein metabolism and red blood cell formation. | Rare due to presence in most foods. Peripheral neuropathy, seizures refractory to antiseizure medications, anemia, glossitis (swollen tongue), seborrheic dermatitis, depression, and confusion. |
| B9 (Folic Acid) | Liver, legumes, leafy greens, seeds, orange juice, and enriched refined grains | Coenzyme in protein metabolism and cell growth, red blood cell formation, and prevention of fetal neural tube defects in utero. | Glossitis (swollen tongue), confusion, depression, diarrhea, anemia, and fetal neural tube defects. |
| B12 (Cyanocobalamin) | Meat, organ meat, dairy, seafood, poultry, and eggs | Mature red blood cell formation, DNA/RNA synthesis, new cell formation, and nerve function. | Pernicious anemia from lack of intrinsic factor in intestines. Early Signs: weight loss, abdominal pain, peripheral neuropathy, weakness, hyporeflexia, and ataxia. Late Signs: irritability, depression, paranoia, and confusion. |
Fat-soluble vitamins are absorbed with fats in the diet and include vitamins A, D, E, and K. They are stored in fat tissue and can build up in the liver. They are not excreted easily by the kidneys due to storage in fatty tissue and the liver, so overconsumption can cause toxicity, especially with vitamins A and D.[142] See Table 14.2b for a list of selected fat-soluble vitamins, their sources, their function, and manifestations of deficiencies and toxicities.[143],[144],[145],[146],[147],[148],[149],[150],[151]
Table 14.2b Selected Fat-Soluble Vitamins
| Fat-Soluble Vitamin | Source | Function | Deficiency | Toxicity |
|---|---|---|---|---|
| A (Retinol)
|
Retinol: fortified milk and dairy, egg yolks, and fish liver oil
Beta carotene: green leafy vegetables, and dark orange fruits and vegetables |
Eyesight, epithelial, bone and tooth development, normal cellular proliferation, and immunity. | Night blindness, rough scaly skin, dry eyes, and poor tooth/ bone development. Causes poor growth and infections common with mortality >50%. | Dry, itchy skin; headache; nausea; blurred vision; and yellowing skin (carotenosis). |
| D | Milk, dairy, sun exposure, egg yolks, fatty fish, and liver | Changed to active form with sun exposure. Needed for calcium/ phosphorus absorption, immunity, and bone strength. | Rickets, poor dentition, tetany, osteomalacia, muscle aches and weakness, bone pain, poor calcium absorption leading to hypocalcemia and subsequent hyperparathyroidism and tetany. | Hypercalcemia resulting in nausea, vomiting, anorexia, renal failure, weakness, pruritus, and polyuria. |
| E | Green leafy vegetables, whole grains, liver, egg yolks, nuts, and plant oils | Anticoagulant, antioxidant, and cellular protection. | Red blood cell breakdown leading to anemia, neuron degeneration, neuropathy, and retinopathy. | Rare. Occasionally muscle weakness, fatigue, GI upset with diarrhea, and hemorrhagic stroke. |
| K | Green leafy vegetables and green vegetables
*Produced by bacteria in intestines |
Needed for producing clotting factors in the liver. | Rare in adults. Prolonged clotting times, hemorrhaging (especially in newborns causing morbidity & mortality), and jaundice. | Rare, but can interfere with effectiveness of certain anticoagulant medications (Warfarin). |
Minerals
Minerals are inorganic materials essential for hormone and enzyme production, as well as for bone, muscle, neurological, and cardiac function. Minerals are needed in varying amounts and are obtained from a well-rounded diet. In some cases of deficiencies, mineral supplements may be prescribed by a health care provider. Deficiencies can be caused by malnutrition, malabsorption, or certain medications, such as diuretics.
Minerals are classified as either macrominerals or trace minerals. Macrominerals are needed in larger amounts and are typically measured in milligrams, grams, or milliequivalents. Macrominerals include sodium, potassium, calcium, magnesium, chloride, and phosphorus. Macrominerals are discussed in further detail in the "Electrolytes" section of the “Fluids and Electrolytes” chapter of this book.
Trace minerals are needed in tiny amounts. Trace minerals include zinc, iron, chromium, copper, fluorine, iodine, manganese, molybdenum, and selenium.[152] See Table 14.2c for a list of selected macrominerals and Table 14.2d for a list of trace minerals.[153],[154],[155],[156]
Table 14.2c Macrominerals
| Macromineral | Source | Function |
|---|---|---|
| Sodium | Table salt, spinach, and milk | Water balance |
| Potassium | Legumes, potatoes, bananas, and whole grains | Muscle contraction, cardiac muscle function, and nerve function |
| Calcium | Dairy, eggs, and green leafy vegetables | Bone and teeth development, nerve function, muscle contraction, immunity, and blood clotting |
| Magnesium | Raw nuts, spinach (cooked has higher magnesium content), tomatoes, and beans | Cell energy, muscle function, cardiac function, and glucose metabolism |
| Chloride | Table salt | Fluid and electrolyte balance and digestion |
| Phosphorus | Red meat, poultry, rice, oats, dairy, and fish | Bone strength and cellular function |
Table 14.2d Trace Minerals
| Trace Mineral | Source | Function |
|---|---|---|
| Zinc | Eggs, spinach, yogurt, whole grains, fish, and brewer’s yeast | Immune function, healing, and vision |
| Iron | Red meat, organ meats, spinach, shrimp, tuna, salmon, kidney beans, peas, and lentils (nonanimal forms are harder to absorb, so need more!) | Hemoglobin production and collagen production |
| Chromium | Whole grains, meat, and brewer’s yeast | Glucose metabolism |
| Copper | Shellfish, fruits, nuts, and organ meats | Hemoglobin production, collagen, elastin, neurotransmitter production, and melanin production |
| Fluorine | Fluoridated water and toothpaste | Retention of calcium in bones and teeth |
| Iodine | Iodized salt and seafood | Energy production and thyroid function |
| Manganese | Whole grain and nuts | Not fully understood |
| Molybdenum | Organ meats, green leafy vegetables, legumes, whole grains, and dairy | Not fully understood; detoxification |
| Selenium | Broccoli, cabbage, garlic, whole grains, brewer’s yeast, celery, onions, and organ meats | Not fully understood |
Nutritional Guidelines
Nutritional guidelines are developed by governmental agencies to provide guidance to the population on how to best meet nutritional needs. These guidelines may vary by country. The National Academies of Sciences, Engineering, and Medicine set the Dietary Reference Intakes (DRIs) for the United States and Canada. Dietary Reference Intakes (DRIs) are a set of reference values used to plan and assess nutrient intakes of healthy people, including proteins, carbohydrates, fats, vitamins, minerals, and fiber. Nutrients included in the DRIs are obtained through a typical diet, although some foods may be fortified with certain nutrients that are commonly deficient in diets.[157]
Choose MyPlate Food Guide
The U.S. Department of Agriculture (USDA) issues dietary guidelines for appropriate serving sizes of each food group and number of servings recommended each day. The “Choose MyPlate” food guide is an easy-to-understand visual representation of how a healthy plate of food should be divided based on food groups. See Figure 14.4[158] for a Choose MyPlate image. A little more than half of the plate should be grains and vegetables, with a focus on whole grains and a variety of vegetables. About one quarter of the plate should be fruits, with an emphasis on whole fruits. About one quarter of the plate should be protein, with an emphasis on consuming a variety of low-fat protein sources. All of these groups combined should make up no more than 85% of daily caloric intake based on a 2,000-calorie diet. Fats, oils, and added sugars are not included, but should make up no more than 15% of daily caloric intake. Foods should be selected that are as nutrient-dense as possible. Nutrient-dense foods mean there is a high proportion of nutritional value relative to calories contained in the food, such as fruits and vegetables. Conversely, calorie-dense foods should be minimized because they have a large amount of calories with few nutrients. For example, candy and soda are calorie-dense with few nutrients and should be minimized.[159],[160] See Figure 14.5 for an image of MyPlate [161]
Figure 14.4 MyPlate Food Guide
Read more about USDA MyPlate guidelines at https://www.myplate.gov/.
MyPlate information and images are also available in several other languages so that education can be tailored to the client’s preferred language. For example, Figure 14.5[162] shows MyPlate in Vietnamese. This image would be accompanied with written information about food groups that include the client’s typical dietary choices.
Vegetable Group
For a well-rounded diet, a variety of vegetables should be consumed, including vegetables from all five vegetable groups: dark green leafy vegetables; red and orange vegetables; beans, peas, and lentils (formerly called the legumes group); starchy vegetables; and other vegetables. Vegetables can be fresh, frozen, canned, or dried. Dark green leafy vegetables include kale, Swiss chard, spinach, broccoli, and salad greens. Red and orange vegetables include carrots, bell peppers, sweet potatoes, tomatoes, tomato juice, and squash. The beans, peas, and lentils group includes dried beans, black beans, chickpeas, kidney beans, split peas, and black-eyed peas. (Note that this group does not include green beans or green peas.) This vegetable group also supplies some protein and can be included in the protein group as well. Starchy vegetables include root vegetables, such as potatoes, as well as corn. The “other vegetables” category includes any vegetable that doesn’t fit in the other four categories, such as asparagus, avocados, brussels sprouts, cabbage, cucumbers, snow peas, and mushrooms, and a variety of others.
Daily serving suggestions of vegetables for individuals with a 2,000 calorie diet are 2 ½ cup equivalents of vegetables per day. For example, a “one cup equivalent” equals 1 cup raw or cooked vegetables, one cup 100% vegetable juice, ½ cup of dried vegetables, or 2 cups of leafy green vegetables. Approximately 90% of Americans do not meet the recommended daily intake of vegetables.[163] See Figure 14.6[164] for an image of vegetables.

Grain Group
Grains are classified as whole grains or refined grains. Whole grains include the entire grain kernel and supply more fiber than refined grains. Examples of whole grains include amaranth, whole barley, popcorn, oats, whole grain cornmeal, brown or wild rice, and whole grain cereal or crackers. Refined grains have been processed to remove parts of the grain kernel and supply little fiber. As a result, they quickly increase blood glucose levels. Examples of refined grains include white bread, white rice, Cream of Wheat, pearled barley, white pasta, and refined-grain cereals or crackers. Some grains are fortified to ensure adequate intake of folic acid. See Figure 14.7[165] for an image of whole grain whole wheat bread.
The daily serving suggestions of grains for an individual with a 2,000-calorie diet are six-ounce equivalents per day, split equally between whole and refined grains. For example, a “one ounce equivalent” of grains equals ½ cup of cooked rice, pasta, or cereal or 1 cup of flaked cereal. Most Americans consume adequate amounts of total grains, although roughly 98% are deficient in recommended whole grain amounts, and 74% consume more than the recommended refined grain amounts.[166]
Fruit Group
Fruits can be frozen, canned, or dried, in addition to 100% fruit juice. A few examples of fruits include apples, oranges, bananas, melons, peaches, apricots, pineapples, and rhubarb. Daily serving suggestions of fruits for an individual with a 2,000-calorie diet are 2 cup equivalents per day. For example, “one cup equivalent” equals 1 cup of raw or cooked fruit, 8 ounces of 100% fruit juice, or ½ cup of dried fruit. Approximately 80% of Americans do not consume the recommended daily intake of fruits.[167] See Figure 14.8[168] for an image of fruits.

Dairy Group
Dairy products can be liquid, dried, semi-solid, or solid depending on the type of product. Dairy products include milk, lactose-free milk, fortified soy milk, buttermilk, cheese, yogurt, and kefir. Sour cream and cream cheese are not considered dairy items in terms of nutritional benefits. Daily serving suggestions of dairy products for an individual with a 2,000-calorie diet are 3 cup equivalents per day. For example, “one cup equivalent” equals 1 cup of milk, soy milk, or yogurt; 1 ½ ounces of natural cheese, or 2 ounces of processed cheese. Approximately 90% of Americans consume less than the recommended daily intake of dairy products.[169] See Figure 14.9[170] for an image of dairy products.

Protein Group
Proteins are categorized by the type of protein source. The meats, poultry, and eggs category consists of any type of animal or poultry meat, organ meat, or poultry egg. Lean meats should be selected to minimize fat and calorie intake from high-fat meats.
The seafood category includes any type of fish, clams, crab, lobster, oyster, and scallops. It is important to choose fish with low mercury levels to prevent negative effects of a buildup of mercury in the body. In general, large, fatty ocean fish, such as tuna, have higher levels of mercury due to their diet and storage of mercury in their fatty tissues.
The nuts, seeds, and soy products category includes tree nuts, peanuts, nut butters, seeds, or seed butters. Soy products include tofu and any other products made from soy. Unsalted nuts should be selected to avoid excess salt intake.
Protein is also contained in other food groups, such as dairy or the vegetable category of peas, beans, and lentils. Daily serving suggestions of proteins for individuals with a 2,000-calorie diet are 5 ½ ounce equivalents per day. Servings should total up to 26-ounce equivalents per week of meats, eggs, and poultry; 8-ounce equivalents per week of seafood; and 5-ounce equivalents per week of nuts, seeds, or soy products. A “one ounce equivalent” of protein equals 1 ounce of lean meat, one egg, ¼ cup cooked beans, or 1 tablespoon of peanut butter. Most Americans consume adequate amounts of protein, but many consume proteins high in saturated fat and sodium that contribute to diseases such as coronary artery disease.[171]
Oil/Fat Group
Examples of oils are vegetable oil, canola oil, olive oil, butter, lard, and coconut oil. Daily serving suggestions of fats or oils for individuals with a 2,000-calorie diet are 27 grams per day. While it is important to limit oils and fats due to their calorie-dense nature, some fat and oil intake is essential for nutrient absorption and overall health. It is best to select healthy unsaturated fats, such as avocados, nuts, or olive oil.[172]
Gender
A person’s gender affects their calorie and nutrient requirements. Males typically have higher calorie and protein needs related to increased muscle mass. Females typically require fewer calories to maintain their body weight due to a higher proportion of adipose (fat tissue) than muscle. Menstruating females also have higher iron requirements to offset losses that occur during menstruation.
Read Nutrition and Food Safety Information and Resources for Healthcare Professionals from the U.S. Food and Drug Administration.
Factors Affecting Nutritional Status
Now that we have discussed basic nutritional concepts and dietary guidelines, let’s discuss factors that can affect a person’s nutritional status. Many things that can cause altered nutrition, such as physiological factors, cultural and religious beliefs, economic resources, drug and nutrient disorders, surgery, altered metabolic states, alcohol and drug abuse, and psychological states.
Physiological Factors
Nutritional intake is affected by several physiological factors. Appetite is controlled by the hypothalamus, a tiny gland deep within the brain that triggers feelings of hunger or fullness depending on hormone and neural signals being sent and received. See Figure 14.10[173] for an image of the hypothalamus indicated by the red arrow. Hunger causes a feeling of emptiness in the abdomen and is often accompanied by audible noises coming from the abdomen as the stomach contracts due to emptiness. Hunger can cause feelings of discomfort, nausea, and tiredness. Satiety is a feeling of fullness that often comes after eating, although it can also be caused by impairments of the hypothalamus. Electrolyte imbalances and fluid volume imbalances can also trigger hunger and thirst by sending signals to the hypothalamus.[174]

The five senses play an important role in food intake. For example, food with a pleasing aroma may induce mouth watering and hunger, whereas food or environments with displeasing aromas often suppress the appetite. Texture and taste of foods also play a role in stimulation of appetite.
Poor dentition or poor oral care has a negative effect on appetite, so adequate oral care is crucial for clients prior to eating.[175] Additionally, the condition of a client’s teeth and gums, the fit of dentures, and gastrointestinal function also play an important role in nutrition. Loose teeth, swollen gums, or poor-fitting dentures can make eating difficult.
Difficulty swallowing, called dysphagia, can make it dangerous for the client to swallow food because it can result in pneumonia from aspiration of food into the lungs. Special soft diets or enteral or parenteral nutrition are typically prescribed for clients with dysphagia. Nurses collaborate with speech therapists when assessing and managing dysphagia.
A poorly functioning gastrointestinal tract makes nutrient absorption difficult and can result in malnourishment. Diseases that cause inflammation of the gastrointestinal tract impair absorption of nutrients. Examples of these conditions include esophagitis, gastritis, inflammatory bowel disease, and cholecystitis. Clients with these disorders should select nutrient-dense foods and may require prescribed supplements to increase nutrient intake.
Cultural and Religious Beliefs
Cultural and religious beliefs often influence food selection and food intake. It is important for nurses to conduct a thorough client assessment, including food preferences, to ensure adequate nutritional intake during hospitalization. The nurse should not assume a particular diet based on a client’s culture or religion, but instead should determine their individual preferences through the assessment interview.
Cultural beliefs affect types of food eaten and when they are eaten. Some foods may be restricted due to beliefs or religious rituals, whereas other foods may be viewed as part of the healing process. For example, some cultures do not eat pork because it is considered unclean, and others eat “kosher” food that prescribes how food is prepared. Some religions fast during religious holidays from sunrise to sunset, where others avoid eating meat during the time of Lent.[176],[177]
Read more about the impact of religious and cultural beliefs on food intake in the “Spirituality” chapter of this book.
Economic Resources
If a client has inadequate financial resources, food security and food choices are often greatly impacted. Healthy, nutrient-dense, fresh foods typically cost more than prepackaged, heavily processed foods. Poor economic status is correlated with the consumption of calorie-dense, nutrient-poor food choices, putting these individuals at risk for inadequate nutrition and obesity.[178] Social programs such as Meals on Wheels, free or reduced-cost school breakfast and lunch programs, and government subsidies based on income help reduce food insecurity and promote the consumption of healthy, nutrient-dense foods. Nurses refer at-risk clients to social workers and case managers for assistance in applying for these social programs.
Drug and Nutrient Interactions
Some prescription drugs affect nutrient absorption. For example, some medications such as proton pump inhibitors (omeprazole) alter the pH of stomach acid, resulting in poor absorption of nutrients. Other medications, such as opioids, often decrease a person’s appetite or cause nausea, resulting in decreased calorie and nutrient intake.
Surgery
Surgery can affect a client’s nutritional status due to several factors. Food and drink are typically withheld for a period of time prior to surgery to prevent aspiration of fluid into the lungs during anesthesia. Anesthesia and pain medication used during surgery slow peristalsis, and it often takes time to return to normal. Slow peristalsis can cause nausea, vomiting, and constipation. Until the client is able to pass gas and bowel sounds return, the client is typically ordered to have nothing by mouth (NPO). If a client experiences prolonged NPO status, such as after significant abdominal surgery, intravenous fluids and nutrition may be required.
Surgery also stimulates the physiological stress response and increases metabolic demands, causing the need for increased calories. The stress response can also cause elevated blood glucose levels due to the release of corticosteroids, even if the client has not been previously diagnosed with diabetes mellitus. For this reason, nurses often monitor post-op clients’ bedside blood glucose levels carefully.
Bowel resection surgery in particular has a negative impact on nutrient absorption. Because all or parts of the intestine are removed, there is decreased absorption of nutrients, which can result in nutrient deficiencies. Many clients who have experienced bowel resection require nutrient supplementation.
Bariatric surgery is used to treat obesity and reduce obesity-related cardiovascular risk factors. Bariatric procedures alter the anatomy and physiology of the gastrointestinal tract, which makes clients susceptible to nutritional deficiencies.[179] Read more about bariatric surgery and long-term nutritional issues in the following box.
Read more about bariatric surgery and long-term nutritional issues.[180]
Altered Metabolic States
Metabolic demands impact nutrient intake. In conditions where metabolic demands are increased, such as during growth spurts in childhood or adolescence, nutritional intake should be increased. Disease states, such as cancer, hyperthyroidism, and AIDS, can increase metabolism and require an increased amount of nutrients. However, cancer treatment, such as radiation and chemotherapy, often causes nausea, vomiting, and decreased appetite, making it difficult for clients to obtain adequate nutrients at a time when they are needed in high amounts due to increased metabolic demand.
Other diseases like diabetes mellitus cause complications with nutrient absorption due to insulin. Insulin is necessary for the metabolism of fats, proteins, and carbohydrates, but in clients with diabetes mellitus, insulin production is insufficient or their body is not able to effectively use circulating insulin. This lack of insulin can result in impaired nutrient metabolism.
Alcohol and Drug Misuse
Alcohol and drug misuse can affect nutritional status. Alcohol is calorie-dense and nutrient-poor. With alcohol use, the consumption of water, food, and other nutrients often decreases as clients “drink their calories.” This may result in decreased protein intake and body protein deficiency. Nutrient digestion and absorption can also decrease with alcohol consumption if the stomach lining becomes eroded or scarred. This can cause hemoglobin, hematocrit, albumin, folate, thiamine, vitamin B12, and vitamin C deficiencies, as well as decreased calcium, magnesium, and phosphorus levels.[181]
Misuse of stimulants, such as methamphetamine and cocaine, causes an increased metabolic rate and decreased appetite and contributes to weight loss and malnourishment.
Psychological State
Various psychological states have a direct effect on appetite and a client’s desire to eat. Acute and chronic stress stimulates the hypothalamus and increases production of glucocorticoids and glucose. This can increase the person’s appetite, causing increased calorie intake, fat storage, and subsequent weight gain. When a person feels stressed, their food choices are often nutrient-poor and calorie-dense, which further increases weight gain and nutrient deficiencies. In other individuals, the stress response causes loss of appetite, weight loss, and nutrient deficiencies.[182]
Depression can cause loss of appetite or overeating. Many people eat calorie-dense “comfort foods” as a coping mechanism. Additionally, many antidepressants can cause weight gain as a side effect.
When clients experience deficient fluid volume, intravenous (IV) fluids are often prescribed. IV fluid restores fluid to the intravascular compartment, and some IV fluids are also used to facilitate the movement of fluid between compartments due to osmosis. There are three types of IV fluids: isotonic, hypotonic, and hypertonic.
Isotonic Solutions
Isotonic solutions are IV fluids that have a similar concentration of dissolved particles as blood. An example of an isotonic IV solution is 0.9% Normal Saline (0.9% NaCl). Because the concentration of the IV fluid is similar to the blood, the fluid stays in the intravascular space and osmosis does not cause fluid movement between compartments. See Figure 15.8[183] for an illustration of isotonic IV solution administration with no osmotic movement of fluid with cells. Isotonic solutions are used for clients with fluid volume deficit (also called hypovolemia) to raise their blood pressure. However, infusion of too much isotonic fluid can cause excessive fluid volume (also referred to as hypervolemia).
Hypotonic Solutions
Hypotonic solutions have a lower concentration of dissolved solutes than blood. An example of a hypotonic IV solution is 0.45% sodium chloride (0.45% NaCl). When hypotonic IV solutions are infused, it results in a decreased concentration of dissolved solutes in the blood as compared to the intracellular space. This imbalance causes osmotic movement of water from the intravascular compartment into the intracellular space. For this reason, hypotonic fluids are used to treat cellular dehydration. See Figure 15.9[184] for an illustration of the osmotic movement of fluid into a cell when a hypotonic IV solution is administered, causing lower concentration of solutes (pink molecules) in the bloodstream compared to within the cell.
However, if too much fluid moves out of the intravascular compartment into cells, cerebral edema can occur. It is also possible to cause worsening hypovolemia and hypotension if too much fluid moves out of the intravascular space and into the cells. Therefore, client status should be monitored carefully when hypotonic solutions are infused.
Hypertonic Solutions
Hypertonic solutions have a higher concentration of dissolved particles than blood. An example of hypertonic IV solution is 3% sodium chloride (3% NaCl). When infused, hypertonic fluids cause an increased concentration of dissolved solutes in the intravascular space compared to the cells. This causes the osmotic movement of water out of the cells and into the intravascular space to dilute the solutes in the blood. See Figure 15.10[185] for an illustration of osmotic movement of fluid out of a cell when hypertonic IV fluid is administered due to a higher concentration of solutes (pink molecules) in the bloodstream compared to the cell.
When administering hypertonic fluids, it is essential to monitor for signs of hypervolemia such as breathing difficulties and elevated blood pressure. Additionally, if hypertonic solutions with sodium are given, the client’s serum sodium level should be closely monitored.[186] See Table 15.3 for a comparison of types of IV solutions, their uses, and nursing considerations.
See Figure 15.11[187] for an illustration comparing how different types of IV solutions affect red blood cell size.
Table 15.3 Comparison of IV Solutions[188],[189],[190]
| Type | IV Solution | Uses | Nursing Considerations |
| Isotonic | 0.9% Normal Saline (0.9% NaCl) | Fluid resuscitation for hemorrhaging, severe vomiting, diarrhea, GI suctioning losses, wound drainage, mild hyponatremia, or blood transfusions. | Monitor closely for hypervolemia, especially with heart failure or renal failure. |
| Isotonic | Lactated Ringer’s Solution (LR) | Fluid resuscitation, GI tract fluid losses, burns, traumas, or metabolic acidosis. Often used during surgery. | Should not be used if serum pH is greater than 7.5 because it will worsen alkalosis. May elevate potassium levels if used with renal failure. |
| Isotonic | 5% Dextrose in Water (D5W) *starts as isotonic and then changes to hypotonic when dextrose is metabolized | Provides free water to help renal excretion of solutes, hypernatremia, and some dextrose supplementation. | Should not be used for fluid resuscitation because after dextrose is metabolized, it becomes hypotonic and leaves the intravascular space, causing brain swelling. Used to dilute plasma electrolyte concentrations. |
| Hypotonic | 0.45% Sodium Chloride (0.45% NaCl) | Used to treat intracellular dehydration and hypernatremia and to provide fluid for renal excretion of solutes. | Monitor closely for hypovolemia, hypotension, or confusion due to fluid shifting into the intracellular space, which can be life-threatening. Avoid use in clients with liver disease, trauma, and burns to prevent hypovolemia from worsening. Monitor closely for cerebral edema. |
| Hypotonic | 5% Dextrose in Water (D5W) | Provides free water to promote renal excretion of solutes and treat hypernatremia, as well as some dextrose supplementation. | Monitor closely for hypovolemia, hypotension, or confusion due to fluid shifting out of the intravascular space, which can be life-threatening. Avoid use in clients with liver disease, trauma, and burns to prevent hypovolemia from worsening. Monitor closely for cerebral edema. |
| Hypertonic | 3% Sodium Chloride (3% NaCl) | Used to treat severe hyponatremia and cerebral edema. | Monitor closely for hypervolemia, hypernatremia, and associated respiratory distress. Do not use it with clients experiencing heart failure, renal failure, or conditions caused by cellular dehydration because it will worsen these conditions. |
| Hypertonic | 5% Dextrose and 0.45% Sodium Chloride (D5 0.45% NaCl) | Replacement of fluid, minimal carbohydrate calories, and sodium chloride; hypoglycemia. | Monitor closely for hypervolemia, hypernatremia, and associated respiratory distress. Do not use it with clients experiencing heart failure, renal failure, or conditions caused by cellular dehydration because it will worsen these conditions. |
| Hypertonic | 5% Dextrose and Lactated Ringer’s (D5LR)
D10 |
Replacement of fluid, electrolyte, and calories; hypoglycemia. Lactated ringers provide some alkalizing action in the blood. | Monitor closely for hypervolemia, hypernatremia, and associated respiratory distress. Do not use it with clients experiencing heart failure, renal failure, or conditions caused by cellular dehydration because it will worsen these conditions. |
Osmolarity is defined as the proportion of dissolved particles in an amount of fluid and is generally the term used to describe body fluids. As the dissolved particles become more concentrated, the osmolarity increases. Osmolality refers to the proportion of dissolved particles in a specific weight of fluid. The terms osmolarity and osmolality are often used interchangeably in clinical practice.
As with electrolytes, correct balance of acids and bases in the body is essential to proper body functioning. Even a slight variance outside of normal can be life-threatening, so it is important to understand normal acid-base values, as well their causes and how to correct them. The kidneys and lungs work together to correct slight imbalances as they occur. As a result, the kidneys compensate for shortcomings of the lungs, and the lungs compensate for shortcomings of the kidneys.
Arterial Blood Gases
Arterial blood gases (ABG) are measured by collecting blood from an artery, rather than a vein, and are most commonly collected via the radial artery. ABGs measure the pH level of the blood, the partial pressure of arterial oxygen (PaO2), the partial pressure of arterial carbon dioxide (PaCO2), the bicarbonate level (HCO3), and the oxygen saturation level (SaO2).
![]() Prior to collecting blood gases, it is important to ensure the client has appropriate arterial blood flow to the hand. This is done by performing the Allen test. When performing the Allen test, pressure is held on both the radial and ulnar artery below the wrist. Pressure is released from the ulnar artery to check if blood flow is adequate. If arterial blood flow is adequate, warmth and color should return to the hand.
Prior to collecting blood gases, it is important to ensure the client has appropriate arterial blood flow to the hand. This is done by performing the Allen test. When performing the Allen test, pressure is held on both the radial and ulnar artery below the wrist. Pressure is released from the ulnar artery to check if blood flow is adequate. If arterial blood flow is adequate, warmth and color should return to the hand.
pH
pH is a scale from 0-14 used to determine the acidity or alkalinity of a substance. A neutral pH is 7, which is the same pH as water. Normally, the blood has a pH between 7.35 and 7.45. A blood pH of less than 7.35 is considered acidic, and a blood pH of more than 7.45 is considered alkaline.
The pH of blood is a measure of hydrogen ion concentration. A low pH, less than 7.35, occurs in acidosis when the blood has a high hydrogen ion concentration. A high pH, greater than 7.45, occurs in alkalosis when the blood has a low hydrogen ion concentration. Hydrogen ions are by-products of the metabolism of substances such as proteins, fats, and carbohydrates. These by-products create extra hydrogen ions (H+) in the blood that need to be balanced and kept within normal range as described earlier.
The body has several mechanisms for maintaining blood pH. The lungs are essential for maintaining pH, and the kidneys also play a role. For example, when the pH is too low (i.e., during acidosis), the respiratory rate quickly increases to eliminate acid in the form of carbon dioxide (CO2). The kidneys excrete additional hydrogen ions (acid) in the urine and retain bicarbonate (base). Conversely, when the pH is too high (i.e., during alkalosis), the respiratory rate decreases to retain acid in the form of CO2. The kidneys excrete bicarbonate (base) in the urine and retain hydrogen ions (acid).
PaCO2
PaCO2 is the partial pressure of arterial carbon dioxide in the blood. The normal PaCO2 level is 35-45 mmHg. CO2 forms an acid in the blood that is regulated by the lungs by changing the rate or depth of respirations.
As the respiratory rate increases or becomes deeper, additional CO2 is removed, causing decreased acid (H+) levels in the blood and increased pH (i.e., the blood becomes more alkaline). As the respiratory rate decreases or becomes shallower, less CO2 is removed, causing increased acid (H+) levels in the blood and decreased pH (i.e., the blood becomes more acidic).
Generally, the lungs work quickly to regulate the PaCO2 levels and cause a quick change in the pH. Therefore, an acid-base problem caused by hypoventilation can be quickly corrected by increasing ventilation, and a problem caused by hyperventilation can be quickly corrected by decreasing ventilation. For example, if an anxious client is hyperventilating, they may be asked to breathe into a paper bag to rebreathe some of the CO2 they are blowing off. Conversely, a postoperative client who is experiencing hypoventilation due to the sedative effects of receiving morphine is asked to cough and deep breathe to blow off more CO2.
HCO3
HCO3 is the bicarbonate level of the blood and the normal range is 22-26. HCO3 is a base managed by the kidneys and helps to make the blood more alkaline. The kidneys take longer than the lungs to adjust the acidity or alkalinity of the blood, and the response is not visible upon assessment. As the kidneys sense an alteration in pH, they begin to retain or excrete HCO3, depending on what is needed. If the pH becomes acidic, the kidneys retain HCO3 to increase the amount of bases present in the blood to increase the pH (i.e., the blood becomes alkaline). Conversely, if the pH becomes alkalotic, the kidneys excrete more HCO3, causing the pH to decrease (i.e., the blood becomes more acidic).
PaO2
PaO2 is the partial pressure of arterial oxygen in the blood. It more accurately measures a client’s oxygenation status than SaO2 (the measurement of hemoglobin saturation with oxygen). Therefore, ABG results are also used to manage clients in respiratory distress.
See Table 15.5a for a review of ABG components, normal values, and key critical values. A critical ABG value means there is a greater risk of serious complications and even death if not corrected rapidly. For example, a pH of 7.10, a shift of only 0.25 below normal, is often fatal because this level of acidosis can cause cardiac or respiratory arrest or significant hyperkalemia.[191] As you can see, failure to recognize ABG abnormalities can have serious consequences for your clients.
Table 15.5a ABG Components, Descriptions, Adult Normal Values, and Critical Values[192]
| ABG Component | Description | Adult Normal Value | Critical Value |
|---|---|---|---|
| pH |
|
7.35-7.45 | Less than 7.25
Greater than 7.60 |
| PaO2 |
|
80-100 mmHg | Less than 60 mmHg |
| PaCO2 |
|
35-45 mmHg | Less than 25 mmHg
Greater than 60 mmHg |
| HCO3 |
|
22-26 mEq/L | Less than 10 mEq/L
Greater than 40 mEq/L |
| SaO2 |
|
95-100% | Less than 88% |
Video Review of Acid-Base Balance[193]
Interpreting Arterial Blood Gases
After the ABG results are received, it is important to understand how to interpret them. A variety of respiratory, metabolic, electrolyte, or circulatory problems can cause acid-base imbalances. Correct interpretation helps the nurse and other health care providers determine the appropriate treatment and evaluate the effectiveness of interventions.
Arterial blood gasses can be interpreted as one of four conditions: respiratory acidosis, respiratory alkalosis, metabolic acidosis, or metabolic alkalosis. Once this interpretation is made, conditions can further be classified as compensated, partially compensated, or uncompensated. A simple way to remember how to interpret ABGs is by using the ROME method of interpretation, which stands for Respiratory Opposite, Metabolic Equal. This means that the respiratory component (PaCO2) moves in the opposite direction of the pH if the respiratory system is causing the imbalance. If the metabolic system is causing the imbalance, the metabolic component (HCO3) moves in the same direction as the pH. Some nurses find the Tic-Tac-Toe method of interpretation helpful. If you would like to learn more about this method, watch the video below.
Review of Tic-Tac-Toe Method of ABG Interpretation[194]
Respiratory Acidosis
Respiratory acidosis develops when carbon dioxide (CO2) builds up in the body (referred to as hypercapnia), causing the blood to become increasingly acidic. Respiratory acidosis is identified when reviewing ABGs and the pH level is below 7.35 and the PaCO2 level is above 45, indicating the cause of the acidosis is respiratory. Note that in respiratory acidosis, as the PaCO2 level increases, the pH level decreases. Respiratory acidosis is typically caused by a medical condition that decreases the exchange of oxygen and carbon dioxide at the alveolar level, such as an acute asthma exacerbation, chronic obstructive pulmonary disease (COPD), or an acute heart failure exacerbation causing pulmonary edema. It can also be caused by decreased ventilation from anesthesia, alcohol, or administration of medications such as opioids and sedatives.
Chronic respiratory diseases, such as COPD, often cause chronic respiratory acidosis that is fully compensated by the kidneys retaining HCO3. Because the carbon dioxide levels build up over time, the body adapts to elevated PaCO2 levels, so they are better tolerated. However, in acute respiratory acidosis, the body has not had time to adapt to elevated carbon dioxide levels, causing mental status changes associated with hypercapnia. Acute respiratory acidosis is caused by acute respiratory conditions, such as an asthma attack or heart failure exacerbation with pulmonary edema when the lungs suddenly are not able to ventilate adequately. As breathing slows and respirations become shallow, less CO2 is excreted by the lungs and PaCO2 levels quickly rise.
Signs of symptoms of hypercapnia vary depending upon the level and rate of CO2 accumulation in arterial blood:
- Clients with mild to moderate hypercapnia may be anxious and/or complain of mild dyspnea, daytime sluggishness, headaches, or hypersomnolence.
- Clients with higher levels of CO2 or rapidly developing hypercapnia develop delirium, paranoia, depression, confusion, or decreased level of consciousness that can progress to seizures and coma as levels continue to rise.
Individuals with normal lung function typically exhibit a depressed level of consciousness when the PaCO2 is greater than 75 to 80 mmHg, whereas clients with chronic hypercapnia may not develop symptoms until the PaCO2 rises above 90 to 100 mmHg.[195]
When a client demonstrates signs of potential hypercapnia, the nurse should assess airway, breathing, and circulation. It is important to note that SaO2 levels may be normal with hypercapnia, and as such should not be the determining factor in further assessing acid-base issues. Urgent assistance should be sought, especially if the client is in respiratory distress. The provider will order an ABG and prescribe treatments based on assessment findings and potential causes. Treatment for respiratory acidosis typically involves improving ventilation and respiration by removing airway restrictions, reversing oversedation, administering nebulizer treatments, or increasing the rate and depth of respiration by using a BiPAP or CPAP devices. BiPAP and CPAP devices provide noninvasive positive pressure ventilation to increase the depth of respirations, remove carbon dioxide, and oxygenate the client. If these noninvasive interventions are not successful, the client will need to be intubated and placed on mechanical ventilation.[196],[197]
Read more details about oxygenation equipment in “Oxygen Therapy” in Open RN Nursing Skills, 2e.
Respiratory Alkalosis
Respiratory alkalosis develops when the body removes too much carbon dioxide through respiration, resulting in increased pH and an alkalotic state. When reviewing ABGs, respiratory alkalosis is identified when pH levels are above 7.45 and the PaCO2 level is below 35. With respiratory alkalosis, notice that as the PaCO2 level decreases, the pH level increases.
Respiratory alkalosis is caused by hyperventilation that can occur due to anxiety, panic attacks, pain, fear, head injuries, or mechanical ventilation. Overdoses of salicylates and other toxins can also cause respiratory alkalosis initially and then often progress to metabolic acidosis in later stages. Acute asthma exacerbations, pulmonary embolisms, or other respiratory disorders can initially cause respiratory alkalosis as the lungs breathe faster in an attempt to increase oxygenation, which decreases the PaCO2. After a while, however, these hypoxic disorders cause respiratory acidosis as respiratory muscles tire, breathing slows, and CO2 builds up in the blood.
Clients experiencing respiratory alkalosis often report feelings of shortness of breath, dizziness or light-headedness, chest pain or tightness, paresthesias, and palpitations as a result of decreased carbon dioxide levels.[198] Respiratory alkalosis is not fatal, but it is important to recognize that underlying conditions such as an asthma exacerbation or pulmonary embolism can be life-threatening, so treatment of these underlying conditions is essential. As the pH level increases, the kidneys will attempt to compensate for the shortage of H+ ions by reabsorbing HCO3 before it can be excreted in the urine. This is a slow process, so additional treatment may be necessary.
Treatment of respiratory alkalosis involves treating the underlying cause of the hyperventilation. Acute management of clients who are hyperventilating should focus on client reassurance, an explanation of the symptoms the client is experiencing, removal of any stressors, and initiation of breathing retraining. Breathing retraining attempts to focus the client on abdominal (diaphragmatic) breathing. Read more about breathing retraining in the following box.
Breathing Retraining
While sitting or lying supine, the client should place one hand on their abdomen and the other on the chest, and then be asked to observe which hand moves with greater excursion. In hyperventilating clients, this will almost always be the hand on the chest. Ask the client to adjust their breathing so that the hand on the abdomen moves with greater excursion and the hand on the chest barely moves at all. Assure the client that this is hard to learn and will take some practice to fully master. Ask the client to breathe in slowly over four seconds, pause for a few seconds, and then breathe out over a period of eight seconds. After 5 to 10 such breathing cycles, the client should begin to feel a sense of calmness with a reduction in anxiety and an improvement in hyperventilation. Symptoms should ideally resolve with continuation of this breathing exercise.
If the breathing retraining technique is not successful in resolving a hyperventilation episode and severe symptoms persist, the client may be prescribed a small dose of a short-acting benzodiazepine (e.g., lorazepam 0.5 to 1 mg orally or 0.5 to 1 mg intravenously). Current research indicates that instructing clients who are hyperventilating to rebreathe carbon dioxide (CO2) by breathing into a paper bag can cause significant hypoxemia with significant complications, so this intervention is no longer recommended. If rebreathing is used, oxygen saturation levels should be continuously monitored.[199]
Metabolic Acidosis
Metabolic acidosis occurs when there is an accumulation of acids (hydrogen ions) and not enough bases (HCO3) in the body. Under normal conditions, the kidneys work to excrete acids through urine and neutralize excess acids by increasing bicarbonate (HCO3) reabsorption from the urine to maintain a normal pH. When the kidneys are not able to perform this buffering function to the level required to excrete and neutralize the excess acid, metabolic acidosis results.
Metabolic acidosis is characterized by a pH level below 7.35 and an HCO3 level below 22 when reviewing ABGs. It is important to notice that both the pH and HCO3 decrease with metabolic acidosis (i.e., the pH and HCO3 move in the same downward direction). A common cause of metabolic acidosis is diabetic ketoacidosis, where acids called ketones build up in the blood when blood sugar is extremely elevated. Another common cause of metabolic acidosis in hospitalized clients is lactic acidosis, which can be caused by impaired tissue oxygenation. Metabolic acidosis can also be caused by increased loss of bicarbonate due to severe diarrhea or from renal disease that causes decreased acid elimination. Additionally, toxins such as salicylate excess can cause metabolic acidosis.[200]
Nurses may first suspect that a client has metabolic acidosis due to rapid breathing that occurs as the lungs try to remove excess CO2 in an attempt to resolve the acidosis. Other symptoms of metabolic acidosis include confusion, decreased level of consciousness, hypotension, and electrolyte disturbances that can progress to circulatory collapse and death if not treated promptly. It is important to quickly notify the provider of suspected metabolic acidosis so that an ABG can be drawn, and treatment prescribed (based on the cause of the metabolic acidosis) to allow acid levels to improve. Treatment includes IV fluids to improve hydration status, glucose management, and circulatory support. When pH drops below 7.1, IV sodium bicarbonate is often prescribed to help neutralize the acids in the blood.[201],[202]
Metabolic Alkalosis
Metabolic alkalosis occurs when there is too much bicarbonate (HCO3) in the body or an excessive loss of acid (H+ ions). Metabolic alkalosis is defined by a pH above 7.45 and an HCO3 level above 26 on ABG results. Note that both pH and HCO3 are elevated in metabolic alkalosis.
Metabolic alkalosis can be caused by gastrointestinal loss of hydrogen ions, excessive urine loss, excessive levels of bicarbonate, or a shift of hydrogen ions from the bloodstream into cells.
Prolonged vomiting or nasogastric suctioning can also cause metabolic alkalosis. Gastric secretions have high levels of hydrogen ions (H+), so as acid is lost, the pH level of the bloodstream increases.
Excessive urinary loss (due to diuretics or excessive mineralocorticoids) can cause metabolic alkalosis due to loss of hydrogen ions in the urine. Intravenous administration of sodium bicarbonate can also cause metabolic alkalosis due to increased levels of bases introduced into the body. Although it was once thought that excessive intake of calcium antacids could cause metabolic alkalosis, it has been found that this only occurs if they are administered concurrently with Kayexelate.[203]
Hydrogen ions may shift into cells due to hypokalemia, causing metabolic alkalosis. When hypokalemia occurs (i.e., low levels of potassium in the bloodstream), potassium shifts out of cells and into the bloodstream in an attempt to maintain a normal level of serum potassium for optimal cardiac function. However, as the potassium (K+) molecules move out of the cells, hydrogen (H+) ions then move into the cells from the bloodstream to maintain electrical neutrality. This transfer of ions causes the pH in the bloodstream to drop, causing metabolic alkalosis.[204]
A nurse may first suspect that a client has metabolic alkalosis due to a decreased respiratory rate (as the lungs try to retain additional CO2 to increase the acidity of the blood and resolve the alkalosis). The client may also be confused due to the altered pH level. The nurse should report signs of suspected metabolic alkalosis because uncorrected metabolic alkalosis can result in hypotension and cardiac dysfunction.[205]
Treatment is prescribed based on the ABG results and the suspected cause. For example, treat the cause of the vomiting, stop the gastrointestinal suctioning, or stop the administration of diuretics. If hypokalemia is present, it should be treated. If bicarbonate is being administered, it should be stopped. Clients with kidney disease may require dialysis.[206]
Analyzing ABG Results
Now that we’ve discussed the differences between the various acid-base imbalances, let’s review the steps to systematically interpret ABG results. Table 15.5b outlines the steps of ABG interpretation.
Table 15.5b Analyzing ABG Results[207],[208]
| Step | Action |
|---|---|
| Step 1: pH (normal 7.35-7.45) | If pH is out of range, determine if it is acidosis or alkalosis:
|
| Step 2: PaCO2 (normal 35-45 mmHg) |
**If the imbalance does not appear to be caused by a respiratory problem, move on to evaluate the HCO3. |
| Step 3: HCO3 (normal 22-26) |
|
| Step 4: Determine level of compensation | After determining the cause of the pH imbalance, determine if compensation is occurring.
|
Legal Considerations
As discussed earlier in this chapter, nurses can be reprimanded or have their licenses revoked for not appropriately following the Nurse Practice Act in the state they are practicing. Nurses can also be held legally liable for negligence, malpractice, or breach of client confidentiality when providing client care.
Negligence and Malpractice
Negligence is a general term that denotes conduct lacking in due care, carelessness, and a deviation from the standard of care that a reasonable person would use in a particular set of circumstances.[209] Malpractice is a more specific term that looks at a standard of care, as well as the professional status of the caregiver. [210]
To prove negligence or malpractice, the following elements must be established in a court of law[211]:
- Duty owed the client
- Breach of duty owed the client
- Foreseeability
- Causation
- Injury
- Damages
To avoid being sued for negligence or malpractice, it is essential for nurses and nursing students to follow the scope and standards of practice care set forth by their state’s Nurse Practice Act; the American Nurses Association; and employer policies, procedures, and protocols to avoid the risk of losing their nursing license. Examples of a nurse's breach of duty that can be viewed as negligence includes the following:[212]
- Failure to Assess: Nurses should assess for all potential nursing problems/diagnoses, not just those directly affected by the medical disease. For example, all clients should be assessed for fall risk and appropriate fall precautions implemented.
- Insufficient monitoring: Some conditions require frequent monitoring by the nurse, such as risk for falls, suicide risk, confusion, and self-injury.
- Failure to Communicate:
- Lack of documentation: A basic rule of thumb in a court of law is that if an assessment or action was not documented, it is considered not done. Nurses must document all assessments and interventions, in addition to the specific type of client documentation called a nursing care plan.
- Lack of provider notification: Changes in client condition should be urgently communicated to the health care provider based on client status. Documentation of provider notification should include the date, time, and person notified and follow-up actions taken by the nurse.
- Failure to Follow Protocols: Agencies and states have rules for reporting certain behaviors or concerns. For example, a nurse is considered a mandatory reporter by law and required to report suspicion of abuse or neglect of a child based on data gathered during an assessment.
Patient Self Determination Act
The Patient Self Determination Act (PSDA) of 1990 is an amendment made to the Social Security Act that requires health care facilities to inform clients of their right to be involved in their medical care decisions. This law specifically applies to facilities accepting Medicare or Medicaid funding but is considered a right of all clients regardless of their method of reimbursement.
Under the PSDA, clients must also be asked about their advance directives and care wishes. Clients must be provided with teaching about advance directives, appointment of an agent or surrogate in the event they become incapacitated, and their right to self-determination. Conversations about these topics and clients wishes must be documented in the medical record. It is considered an ethical duty of nurses and other health care professionals to ensure clients are aware and understand these healthcare-associated rights.[213]
Informed Consent
Informed consent is written consent voluntarily signed by a client who is competent and understands the terms of the consent without any form of coercion. In the event the client is a minor or deemed incompetent to make their own decisions, a parent or legal guardian signs the informed consent.[214]
Informed consent is crucial for upholding the client's right for self-determination. Informed consent provides documentation signed by the client of their understanding of health care being provided; its benefits, risks, potential complications; reasonable alternatives to treatment; and the right to withdraw consent. It is the health care provider's responsibility to fully discuss the treatment, procedure, or other health care action being proposed that requires consent. The nurse often signs as a witness to the client's signature on the form, affirming that person signed the form. However, it is not the nurse's responsibility or role to provide information. If the client (or their parent/legal guardian) expresses questions, concerns, or lack of understanding, the nurse has an ethical responsibility to notify the provider and advocate for further discussion before signing the form.[215]
In emergency situations where the delay to obtain consent would cause undue harm to the client, verbal or telephone consent may be temporarily obtained that is valid for no more than ten days. Verbal consent and the reason for verbal consent must be documented in the medical record by the provider.[216]
See the following box for examples of situations requiring informed consent in the state of Wisconsin according to the Wisconsin Department of Health Services.
Examples of Situations Requiring Informed Consent[217]
- Receipt of medications and/or treatment, including psychotropic medications (unless court-ordered)
- Undergoing customary treatment techniques and procedures
- Participation in experimental research
- Undergoing psychosurgery or other psychological treatment procedures
- Release of treatment records
- Videorecording
- Performance of labor beneficial to the facility
Confidentiality
In addition to negligence and malpractice, confidentiality is a major legal consideration for nurses and nursing students. Patient confidentiality is the right of an individual to have personal, identifiable medical information, referred to as their protected health information (PHI), protected and known only by those health care team members directly providing care to them. This right is protected by federal regulations called the Health Insurance Portability and Accountability Act (HIPAA). HIPAA was enacted in 1996 and was prompted by the need to ensure privacy and protection of personal health records and data in an environment of electronic medical records and third-party insurance payers. There are two main sections of HIPAA law, the Privacy Rule and the Security Rule. The Privacy Rule addresses the use and disclosure of individuals' health information. The Security Rule sets national standards for protecting the confidentiality, integrity, and availability of electronically protected health information. HIPAA regulations extend beyond medical records and apply to client information shared with others. Therefore, all types of client information should only be shared with health care team members who are actively providing care to them.
How do HIPAA regulations affect you as a student nurse? You are required to adhere to HIPAA guidelines from the moment you begin to provide client care. Nursing students may be disciplined or expelled by their nursing program for violating HIPAA. Nurses who violate HIPAA rules may be fired from their jobs or face lawsuits. See the following box for common types of HIPAA violations and ways to avoid them.
Common HIPAA Violations and Ways to Avoid Them[218]
- Gossiping in the hallways or otherwise talking about clients where other people can hear you. It is understandable that you will be excited about what is happening when you begin working with clients and your desire to discuss interesting things that occur. As a student, you will be able to discuss client care in a confidential manner behind closed doors with your instructor. However, as a health care professional, do not talk about clients in the hallways, elevator, breakroom, or with others who are not directly involved with that client’s care because it is too easy for others to overhear what you are saying.
- Mishandling medical records or leaving medical records unsecured. You can breach HIPAA rules by leaving your computer unlocked for anyone to access or by leaving written client charts in unsecured locations. You should never share your password with anyone else. Make sure that computers are always locked with a password when you step away from them and paper charts are closed and secured in an area where unauthorized people don’t have easy access to them. NEVER take records from a facility or include a client's name on paperwork that leaves the facility.
- Illegally or unauthorized accessing of client files. If someone you know, like a neighbor, coworker, or family member is admitted to the unit you are working on, do not access their medical record unless you are directly caring for them. Facilities have the capability of tracing everything you access within the electronic medical record and holding you accountable. This rule holds true for employees who previously cared for a client as a student; once your shift is over as a student, you should no longer access that client’s medical records.
- Sharing information with unauthorized people. Anytime you share medical information with anyone but the client themselves, you must have written permission to do so. For instance, if a husband comes to you and wants to know his spouse’s lab results, you must have permission from his spouse before you can share that information with him. Just confirming or denying that a client has been admitted to a unit or agency can be considered a breach of confidentiality. Furthermore, voicemails should not be left regarding protected client information.
- Information can generally be shared with the parents of children until they turn 18, although there are exceptions to this rule if the minor child seeks birth control, an abortion, or becomes pregnant. After a child turns 18, information can no longer be shared with the parent unless written permission is provided, even if the minor is living at home and/or the parents are paying for their insurance or health care. As a general rule, any time you are asked for client information, check first to see if the client has granted permission.
- Texting or e-mailing regarding client information on an unencrypted device. Only use properly encrypted devices that have been approved by your health care facility for e-mailing or faxing protected client information. Also, ensure that the information is being sent to the correct person, address, or phone number.
- Sharing information on social media. Never post anything on social media that has anything to do with your clients, the facility where you are working or have clinical, or even how your day went at the agency. Nurses and other professionals have been fired for violating HIPAA rules on social media.[219],[220],[221]
Social Media Guidelines
Nursing students, nurses, and other health care team members must use extreme caution when posting to Facebook, Instagram, Twitter, Snapchat, and other social media sites. Information related to clients, client care, and/or health care agencies should never be posted on social media; health care team members who violate this guideline can lose their jobs and may face legal action and students can be disciplined or expelled from their nursing program. Be aware that even if you think you are posting in a private group, the information can become public.
The American Nurses Association (ANA) has established the following principles for nurses using social media:[222]
- Nurses must not transmit or place online individually identifiable client information.
- Nurses must observe ethically prescribed professional client-nurse boundaries.
- Nurses should understand that clients, colleagues, organizations, and employers may view postings.
- Nurses should take advantage of privacy settings and seek to separate personal and professional information online.
- Nurses should bring content that could harm a client’s privacy, rights, or welfare to the attention of appropriate authorities.
- Nurses should participate in developing organizational policies governing online conduct.
In addition to these principles, the ANA has also provided these tips for nurses and nursing students using social media:[223]
- Remember that standards of professionalism are the same online as in any other circumstance.
- Do not share or post information or photos gained through the nurse-client relationship.
- Maintain professional boundaries in the use of electronic media. Online contact with clients blurs this boundary.
- Do not make disparaging remarks about clients, employers, or coworkers, even if they are not identified.
- Do not take photos or videos of clients on personal devices, including cell phones.
- Promptly report a breach of confidentiality or privacy.
Read more about the ANA's Social Media Principles.
Code of Ethics
In addition to legal considerations, there are also several ethical guidelines for nursing care.
There is a difference between morality, ethical principles, and a code of ethics. Morality refers to “personal values, character, or conduct of individuals within communities and societies.”[224] An ethical principle is a general guide, basic truth, or assumption that can be used with clinical judgment to determine a course of action. Four common ethical principles are beneficence (do good), nonmaleficence (do no harm), autonomy (control by the individual), and justice (fairness). A code of ethics is set for a profession and makes their primary obligations, values, and ideals explicit.
The American Nursing Association (ANA) guides nursing practice with the Code of Ethics for Nurses.[225] This code provides a framework for ethical nursing care and a guide for decision-making. The Code of Ethics for Nurses serves the following purposes:
- It is a succinct statement of the ethical values, obligations, duties, and professional ideals of nurses individually and collectively.
- It is the profession’s nonnegotiable ethical standard.
- It is an expression of nursing’s own understanding of its commitment to society.[226]
The ANA Code of Ethics contains nine provisions. See a brief description of each provision in the following box.
Provisions of the ANA Code of Ethics[227]
The nine provisions of the ANA Code of Ethics are briefly described below. The full code is available to read for free at Nursingworld.org.
Provision 1: The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person.
Provision 2: The nurse’s primary commitment is to the patient, whether an individual, family, group, community, or population.
Provision 3: The nurse promotes, advocates for, and protects the rights, health, and safety of the patient.
Provision 4: The nurse has authority, accountability, and responsibility for nursing practice; makes decisions; and takes action consistent with the obligation to promote health and to provide optimal care.
Provision 5: The nurse owes the same duties to self as to others, including the responsibility to promote health and safety, preserve wholeness of character and integrity, maintain competence, and continue personal and professional growth.
Provision 6: The nurse, through individual and collective effort, establishes, maintains, and improves the ethical environment of the work setting and conditions of employment that are conducive to safe, quality health care.
Provision 7: The nurse, in all roles and settings, advances the profession through research and scholarly inquiry, professional standards development, and the generation of both nursing and health policy.
Provision 8: The nurse collaborates with other health professionals and the public to protect human rights, promote health diplomacy, and reduce health disparities.
Provision 9: The profession of nursing, collectively through its professional organizations, must articulate nursing values, maintain the integrity of the profession, and integrate principles of social justice into nursing and health policy.
The ANA Center for Ethics and Human Rights
In addition to publishing the Code of Ethics, the ANA Center for Ethics and Human Rights was established to help nurses navigate ethical and value conflicts and life-and-death decisions, many of which are common to everyday practice.
Check your knowledge with the following questions:
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Practice what you have learned in this chapter by completing these learning activities. When accessing the online activities that contain videos, it is best to use Google Chrome or Firefox browsers.
1. To test your understanding of therapeutic and nontherapeutic terms, complete this online quiz:
Therapeutic Communication Techniques vs. Non-therapeutic Communication Techniques Quizlet
2. Consider the following scenario and describe actions that you might take to facilitate the communication experience.
You are caring for Mr. Curtis, an 87-year-old client newly admitted to the medical surgical floor with a hip fracture. You are preparing to complete his admission history and need to collect relevant health information and complete a physical exam. You approach the room, knock at the door, complete hand hygiene, and enter. Upon entry, you see Mr. Curtis is in bed surrounded by multiple family members. The television is on in the background, and you also note the sound of meal trays being delivered in the hallway.
Based on the described scenario, what actions might be implemented to aid in your communication with Mr. Curtis?

Test your knowledge using this NCLEX Next Generation-style question. You may reset and resubmit your answers to this question an unlimited number of times.[228]

Test your knowledge using this NCLEX Next Generation-style question. You may reset and resubmit your answers to this question an unlimited number of times.[229]
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Instructions: Apply what you’ve learned in this chapter by creating a nursing care plan using the following scenario. Use the template in Appendix B as a guide.
The client, Mark S., is a 57-year-old male who was admitted to the hospital with “severe” abdominal pain that was unable to be managed in the Emergency Department. The physician has informed Mark that he will need to undergo some diagnostic tests. The tests are scheduled for the morning.
After receiving the news about his condition and the need for diagnostic tests, Mark begins to pace the floor. He continues to pace constantly. He keeps asking the nurse the same question (“How long will the tests take?”) about his tests over and over again. The client also remarked, “I’m so uptight I will never be able to sleep tonight.” The nurse observes that the client avoids eye contact during their interactions and that he continually fidgets with the call light. His eyes keep darting around the room. He appears tense and has a strained expression on his face. He states, “My mouth is so dry.” The nurse observes his vital signs to be: T 98, P 104, R 30, BP 180/96. The nurse notes that his skin feels sweaty (diaphoretic) and cool to the touch.
Critical Thinking Activity:
-
- Group (cluster) the cues (subjective and objective data).
- Create a problem-focused nursing diagnosis (hypothesis).
- Develop a broad goal and then identify an expected outcome in “SMART” format.
- Outline three interventions for the nursing diagnosis to meet the goal and their rationale. Cite an evidence-based source for the interventions and rationale
- Imagine that you implemented the interventions that you identified. Evaluate the degree to which the expected outcome was achieved: Met - Partially Met - Not Met.

Test your knowledge using this NCLEX Next Generation-style question. You may reset and resubmit your answers to this question an unlimited number of times.[230]
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
- You are providing care for Mrs. Jones, an 83-year-old female client admitted to the medical-surgical floor with worsening pneumonia. Upon auscultation of the client's lung fields, you note scattered crackles and diminished breath sounds throughout all lung fields. Mrs. Jones requires 4L O2 via nasal cannula to maintain an oxygen saturation of 94%. You have constructed a nursing care diagnosis of Ineffective Breathing Pattern. What nursing interventions might you consider to help improve the client's breathing pattern?

Test your knowledge using these NCLEX Next Generation-style questions. You may reset and resubmit your answers to these questions an unlimited number of times.[232]

Test your knowledge using these NCLEX Next Generation-style questions. You may reset and resubmit your answers to the questions in this assignment an unlimited number of times.[233]

