5.2 Review of Anatomy & Physiology of the Cardiovascular System
Open Resources for Nursing (Open RN)
Heart
Location of the Heart
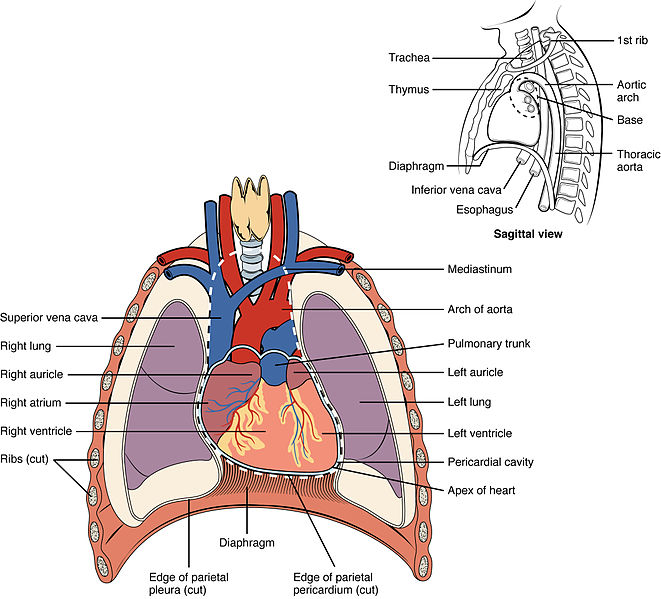
The human heart is located within the thoracic cavity, medially between the lungs in the space known as the mediastinum. The great veins, the superior and inferior venae cavae, and the great arteries, the aorta and pulmonary trunk, are attached to the superior surface of the heart, called the base. The base of the heart is located at the level of the third costal cartilage, as seen in Figure 5.1.[1] The inferior tip of the heart, the apex, lies just to the left of the sternum between the junction of the fourth and fifth ribs. It is important to remember the position of the heart when placing a stethoscope on the chest of a client and listening for heart sounds.[2]
Chambers and Circulation Through the Heart
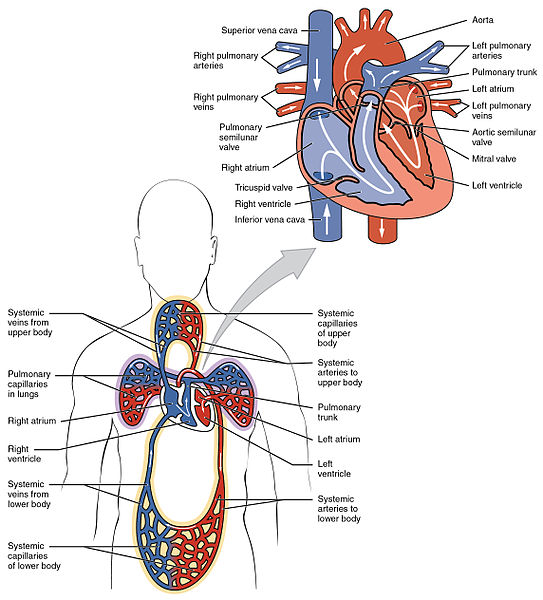
The heart consists of four chambers: two atria and two ventricles. The right atrium receives deoxygenated blood from the systemic circulation, and the left atrium receives oxygenated blood from the lungs. The atria contract to push blood into the lower chambers, the right ventricle and the left ventricle. The right ventricle contracts to push blood into the lungs, and the left ventricle is the primary pump that propels blood to the rest of the body.
There are two distinct but linked circuits in the human circulation called the pulmonary and systemic circuits. The pulmonary circuit transports blood to and from the lungs, where it picks up oxygen and delivers carbon dioxide for exhalation. The systemic circuit transports oxygenated blood to virtually all of the tissues of the body and returns deoxygenated blood and carbon dioxide to the heart to be sent back to the pulmonary circulation. See Figure 5.2[3] for an illustration of blood flow through the heart and blood circulation throughout the body.[4]
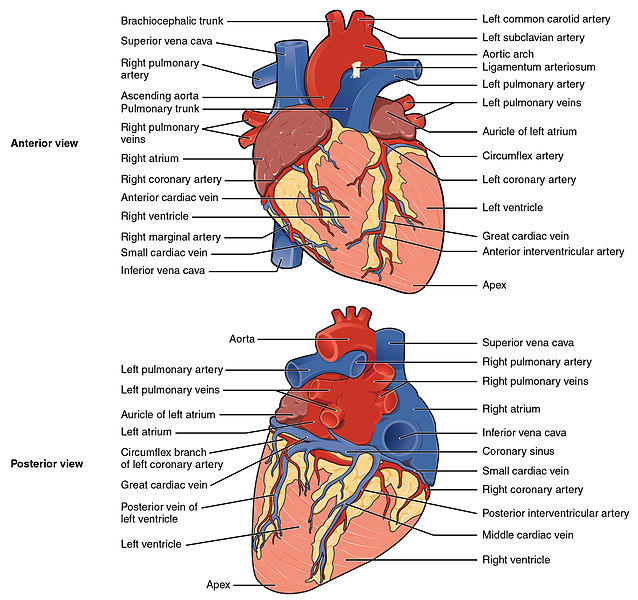
Blood also circulates through the coronary arteries with each beat of the heart. The left coronary artery distributes blood to the left side of the heart, and the right coronary distributes blood to the right atrium, portions of both ventricles, and the heart conduction system. See Figure 5.3[5] for an illustration of the coronary arteries. When a client has a myocardial infarction, a blood clot lodges in one of these coronary arteries that perfuse the heart tissue. If a significant area of muscle tissue dies from lack of perfusion, the heart is no longer able to pump.
Conduction System of the Heart
Contractions of the heart are stimulated by the electrical conduction system. The components of the cardiac conduction system include the sinoatrial (SA) node, the atrioventricular (AV) node, the bundle of His, the left and right bundle branches, and the Purkinje fibers. See Figure 5.4[6] for an image of the conduction system of the heart.
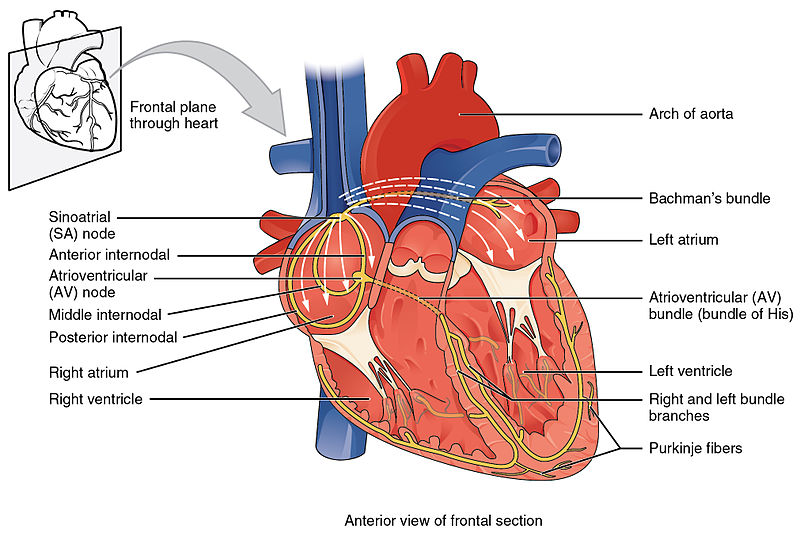
Normal cardiac rhythm is established by the sinoatrial (SA) node. The SA node has an intrinsic rate of 60-100 beats per minute and is known as the pacemaker of the heart. It initiates the sinus rhythm or normal electrical pattern followed by contraction of the heart. The SA node initiates the action potential, which sweeps across the atria through the AV node to the bundle branches and Purkinje fibers, and then spreads to the contractile fibers of the ventricle to stimulate the contraction of the ventricle.[7]
Cardiac Conductive Cells
Sodium (Na), potassium (K), and calcium (Ca2) ions play critical roles in cardiac conduction. Conductive cells contain a series of sodium ion channels that allow influx of sodium ions that cause the membrane potential to rise slowly and eventually cause spontaneous depolarization. Calcium ion channels open and Ca2 enters the cell, further depolarizing it. As the calcium ion channels then close, the K channels open, resulting in repolarization. When the membrane potential reaches approximately −60 mV, the K channels close and Na channels open, and the prepotential phase begins again. This phenomenon explains the autorhythmicity properties of cardiac muscle. Calcium ions play two critical roles in the physiology of cardiac muscle: conduction and contraction. In addition to depolarization, calcium ions also cause myosin to form cross bridges with the muscle cells that then provide the power stroke of contraction. Medications called calcium channel blockers thus affect both the conduction and contraction roles of calcium in the heart.[8]
Focus on Clinical Practice: The ECG
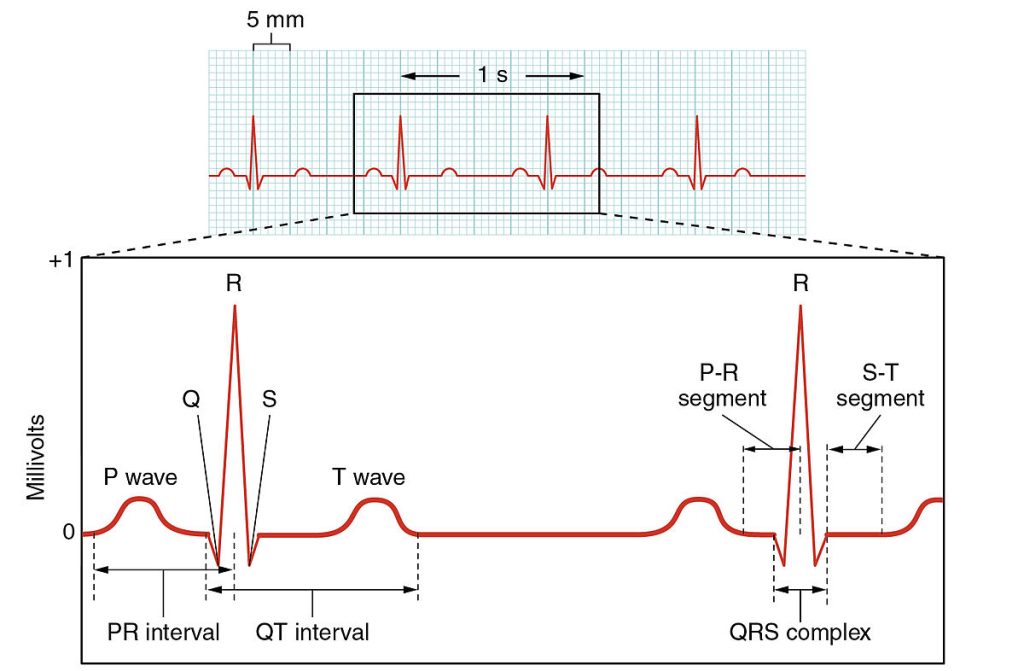
Surface electrodes placed on specific anatomical sites on the body can record the heart’s electrical signals. This tracing of the electrical signal is called an electrocardiogram (ECG), also historically abbreviated EKG. Careful analysis of an ECG reveals a detailed picture of both normal and abnormal heart function and is an indispensable clinical diagnostic tool. A normal ECG tracing is presented in Figure 5.5.[9] Each component, segment, and interval is labeled and corresponds to important electrical events.
There are five prominent components of the ECG: the P wave; the Q, R, and S components; and the T wave. The small P wave represents the depolarization of the atria. The large QRS complex represents the depolarization of the ventricles, which requires a much stronger impulse because of the larger size of the ventricular cardiac muscle. The ventricles begin to contract as the QRS reaches the peak of the R wave. Lastly, the T wave represents the repolarization of the ventricle. Several cardiac disorders can cause an altered conduction of the electrical signal through the heart, resulting in an abnormal rate or rhythm called dysrhythmia (also called arrhythmia).[10]
Cardiac Cycle
The period of time that begins with contraction of the atria and ends with ventricular relaxation is known as the cardiac cycle. The period of contraction that the heart undergoes while it pumps blood into circulation is called systole. The period of relaxation that occurs as the chambers fill with blood is called diastole.
Phases of the Cardiac Cycle
At the beginning of the cardiac cycle, both the atria and ventricles are relaxed, referred to as diastole. During diastole, blood flows into the right atrium from the superior and inferior venae cavae and into the left atrium from the four pulmonary veins. Contraction of the atria follows depolarization, which is represented by the P wave of the ECG. Just prior to atrial contraction, the ventricles contain approximately 130 mL of blood in a resting adult. This volume is known as the end diastolic volume or preload. As the atrial muscles contract, pressure rises within the atria, and blood is pumped into the ventricles.
Ventricular systole follows the depolarization of the ventricles and is represented by the QRS complex in the ECG. During the ventricular ejection phase, the contraction of the ventricular muscle causes blood to be pumped out of the heart. This quantity of blood is referred to as stroke volume (SV). Ventricular relaxation, or diastole, follows repolarization of the ventricles and is represented by the T wave of the ECG.[11]
Cardiac Output
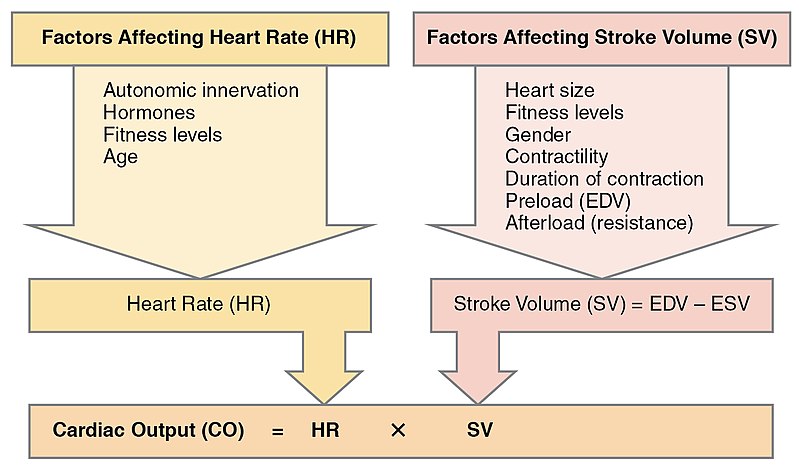
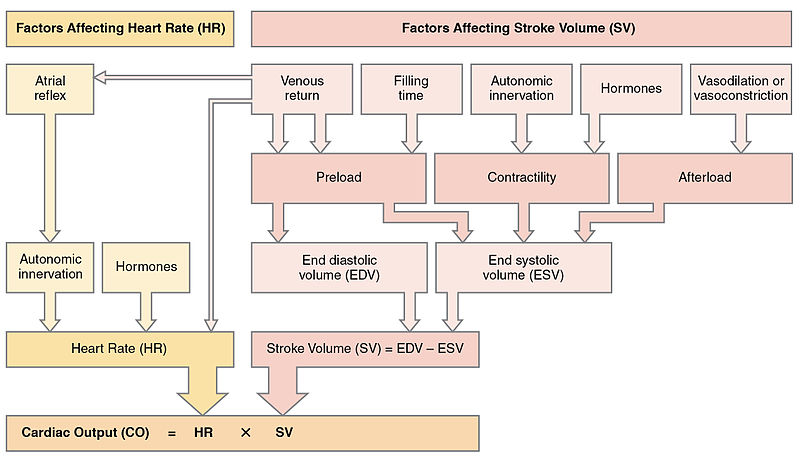
Cardiac output (CO) is a measurement of the amount of blood pumped by each ventricle in one minute. To calculate this value, multiply stroke volume (SV), the amount of blood pumped by the left ventricle, by the heart rate (HR) in beats per minute. It can be represented mathematically by the following equation: CO = HR × SV. Factors influencing CO are summarized in Figure 5.6[12] and include autonomic innervation by the sympathetic and parasympathetic nervous systems, hormones such as epinephrine, preload, contractility, and afterload. Each of these factors is further discussed below.[13] SV is also used to calculate ejection fraction, which is the portion of the blood that is pumped or ejected from the heart with each contraction.
Heart Rate
Heart rate (HR) can vary considerably, not only with exercise and fitness levels, but also with age. Newborn resting HRs may be 120 -160 bpm. HR gradually decreases until young adulthood and then gradually increases again with age. For an adult, normal resting HR will be in the range of 60–100 bpm. Bradycardia is the condition in which resting rate drops below 60 bpm, and tachycardia is the condition in which the resting rate is above 100 bpm.
Correlation Between Heart Rate and Cardiac Output
Conditions that cause increased HR also trigger an initial increase in SV. However, as the HR rises, there is less time spent in diastole and, consequently, less time for the ventricles to fill with blood. As HR continues to increase, SV gradually decreases due to less filling time. In this manner, tachycardia will eventually cause decreased cardiac output.
Autonomic Nervous Stimulation
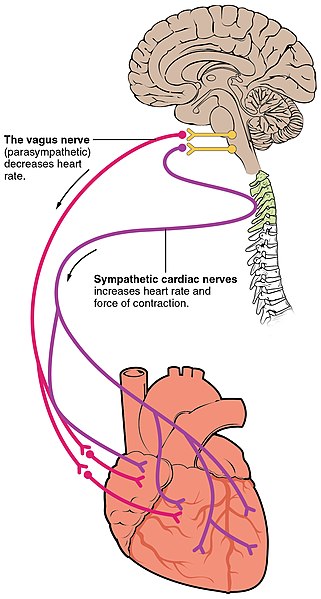
Sympathetic stimulation increases the heart rate and contractility, whereas parasympathetic stimulation decreases the heart rate. See Figure 5.7 for an illustration of the ANS stimulation of the heart.[14] Sympathetic stimulation causes the release of the neurotransmitter norepinephrine (NE), which shortens the repolarization period, thus speeding the rate of depolarization and contraction and increasing the HR. It also opens sodium and calcium ion channels, allowing an influx of positively charged ions.
NE binds to the Beta-1 receptor. Some cardiac medications (for example, beta-blockers) work by blocking these receptors, thereby slowing HR and lowering blood pressure. However, an overdose of beta-blockers can lead to bradycardia and even stop the heart.[15]
Stroke Volume
Many of the same factors that regulate HR also impact cardiac function by altering SV. Three primary factors that affect stroke volume are preload, or the stretch on the ventricles prior to contraction; contractility, or the force or strength of the contraction itself; and afterload, the force the ventricles must generate to pump blood against the resistance in the vessels. Many cardiovascular medications affect cardiac output by affecting preload, contractility, or afterload.[16]
Preload
Preload reflects the degree of myocardial stretch of muscle tissue at the end of diastole and before contraction. Preload is another way of describing end diastolic volume (EDV). Therefore, the greater the EDV is, the greater the preload is. One of the primary factors to consider is filling time, the duration of ventricular diastole during which filling occurs. Any sympathetic stimulation to the venous system will also increase venous return to the heart, which contributes to ventricular filling and preload. Medications such as diuretics decrease preload by causing the kidneys to excrete more water, thus decreasing blood volume.
Contractility
Contractility refers to the force of the contraction of the heart muscle, which controls SV. Factors that increase contractility are described as positive inotropic factors, and those that decrease contractility are described as negative inotropic factors.
Not surprisingly, sympathetic stimulation is a positive inotrope, whereas parasympathetic stimulation is a negative inotrope. The drug digoxin is used to lower HR and increase the strength of the contraction. It works by inhibiting the activity of an enzyme (ATPase) that controls movement of calcium, sodium, and potassium into heart muscle. Inhibiting ATPase increases calcium in heart muscle and, therefore, increases the force of heart contractions.
Negative inotropic agents include hypoxia, acidosis, hyperkalemia, and a variety of medications such as beta-blockers and calcium channel blockers.
Afterload
Afterload refers to the force that the ventricles must develop to pump blood effectively against the resistance in the vascular system. Any condition that increases resistance requires a greater afterload to force open the semilunar valves and pump the blood, which decreases cardiac output. On the other hand, any decrease in resistance reduces the afterload and then increases cardiac output. Figure 5.8[17] summarizes the major factors influencing cardiac output. Calcium channel blockers such as amlodipine, verapamil, nifedipine, and diltiazem can be used to reduce afterload and increase cardiac output.[18]
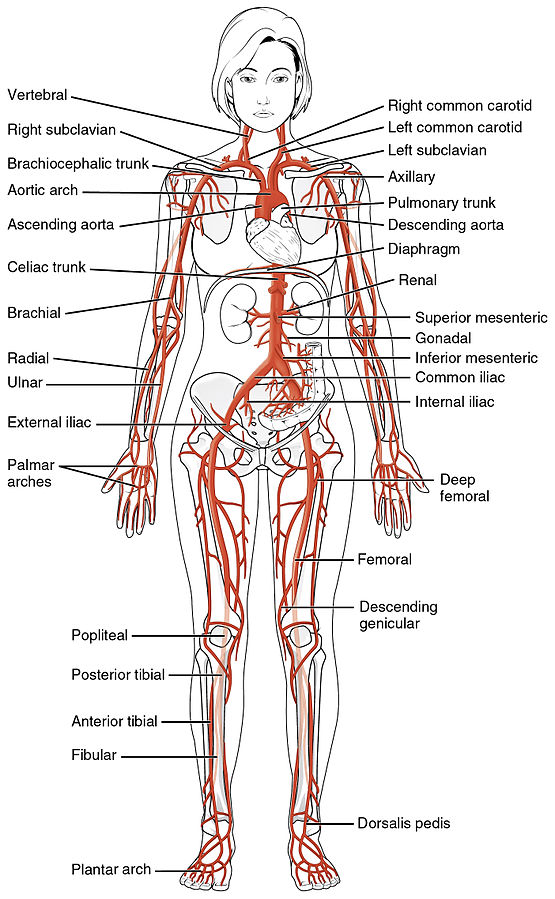
After blood is pumped out of the left ventricle into the aorta, it is carried through the body via the systemic arteries. An artery is a blood vessel that carries blood away from the heart, where it branches into ever-smaller arterioles and eventually into tiny capillaries. See Figure 5.9[19] for an illustration of the systemic arteries that carry oxygenated blood throughout the body to organs and tissues, as indicated by the red color.
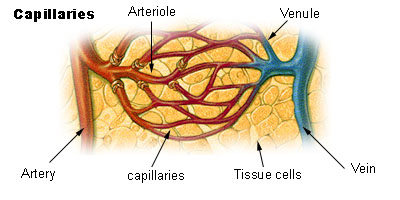
Oxygen and nutrients are exchanged with cells at the capillary level. A capillary is a microscopic channel that supplies blood to the tissue cells where nutrients and wastes are exchanged at the cellular level. Capillaries connect arterioles and venules, small veins. See Figure 5.10[20] for an illustration of capillaries supplying blood to tissue cells.
Venules carry blood to veins, a larger blood vessel that returns blood to the heart. Compared to arteries, veins are thin-walled, low-pressure vessels. Larger veins are also equipped with valves that promote the unidirectional flow of blood toward the heart and prevent backflow caused by the inherent low blood pressure in veins, as well as the pull of gravity. See Figure 5.11[21] for an illustration of the systemic veins.
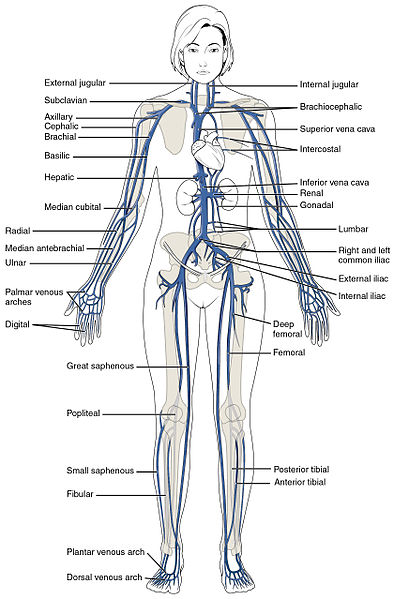
In addition to their primary function of returning blood to the heart, veins may be considered blood reservoirs because systemic veins contain approximately 64 percent of the blood volume at any given time. Approximately 21 percent of the venous blood is located in venous networks within the liver, bone marrow, and integument. This volume of blood is referred to as venous reserve. Through venoconstriction, this reserve volume of blood can get back to the heart more quickly for redistribution to other parts of the circulation. Nitroglycerin is an example of a medication that causes arterial and venous vasodilation. It is used for clients with angina to decrease cardiac workload and increase the amount of oxygen available to the heart. By causing vasodilation of the veins, nitroglycerin decreases the amount of blood returned to the heart, which then decreases preload. It also reduces afterload by causing vasodilation of the arteries and reducing peripheral vascular resistance.[22]
Transportation
The systemic circulation transports blood and its components for physiological processes that occur throughout the body:
- The right ventricle pumps deoxygenated blood through the pulmonary arteries away from the heart to the lungs. Note this is the only place where arteries carry deoxygenated blood. Oxygen from the air breathed into the lungs diffuses into the pulmonary circulation in the alveoli. The pulmonary veins return oxygenated blood to the left atria of the heart, which moves into the left ventricle where it is pumped out to the rest of the body via the aorta to the systemic arteries.
- Nutrients from the foods eaten are absorbed in the digestive tract, where they diffuse into the systemic circulation and are transported throughout the body.
- Systemic arteries carry blood to the liver, where wastes are filtered out of the blood in the form of bile and nutrients and medications are metabolized.
- Systemic arteries carry blood to the kidneys, where wastes are filtered out and urine is created.
- Endocrine glands scattered throughout the body release hormones into the bloodstream, where they are transported to distant target cells.
Pulse
Each time the heart ejects blood forcefully into the circulation, the arteries expand and recoil to accommodate the surge of blood moving through them. This expansion and recoiling of the arterial wall is called the pulse and allows us to measure heart rate. The pulse can be palpated manually by placing the tips of the fingers across an artery that runs close to the body surface, such as the radial artery or the common carotid artery. Common pulse sites are shown in the Figure 5.12[23] below.
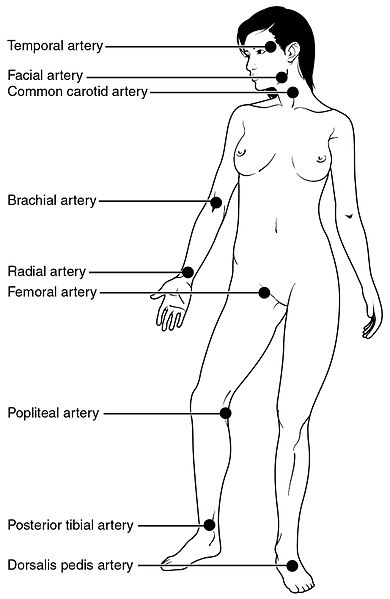
Both the rate and the strength of the pulse are important clinically. A high pulse rate can be temporarily caused by physical activity, but an extended fast or irregular pulse indicates a cardiac condition. The pulse strength indicates the strength of ventricular contraction, cardiac output, and perfusion. Recall that cardiac output is the amount of blood pumped by the heart per minute, and perfusion is the passage of blood through the blood vessels. If the pulse is strong, then cardiac output is high and perfusion to that site is good. If the pulse is weak, cardiac output is low or perfusion is impaired, and medical intervention may be warranted.
Blood Flow and Blood Pressure
Blood flow refers to the movement of blood through a vessel, tissue, or organ. Blood pressure is the force exerted by blood on the walls of the blood vessels. In clinical practice, this pressure is measured in mm Hg and is typically obtained using a sphygmomanometer (a blood pressure cuff) on the brachial artery of the arm. When systemic arterial blood pressure is measured, it is recorded as a ratio of two numbers expressed as systolic pressure over diastolic pressure (e.g., 120/80 is a normal adult blood pressure). The systolic pressure is the higher value (typically around 120 mm Hg) and reflects the arterial pressure resulting from the ejection of blood during ventricular contraction or systole. The diastolic pressure is the lower value (usually about 80 mm Hg) and represents the arterial pressure of blood during ventricular relaxation or diastole.
Three primary variables influence blood flow and blood pressure:
- Cardiac output
- Compliance of vessels
- Volume of the blood
Any factor that causes cardiac output to increase will elevate blood pressure and promote blood flow. Conversely, any factor that decreases cardiac output will decrease blood flow and blood pressure. See the previous “Cardiac Output” subsection for more information about factors that affect cardiac output.
Compliance is the ability of any compartment to expand to accommodate increased content. A metal pipe, for example, is not compliant, whereas a balloon is. The greater the compliance of an artery, the more effectively it is able to expand to accommodate surges in blood flow without increased resistance or blood pressure. When vascular disease causes arteriosclerosis (i.e., stiffening of arteries), compliance is reduced and resistance to blood flow is increased. The result is higher blood pressure within the vessel and reduced blood flow.
There is a relationship between blood volume, blood pressure, and blood flow. As an example, water may merely trickle along a creek bed in a dry season but rush quickly and under great pressure after a heavy rain. Similarly, as blood volume decreases, blood pressure and flow decrease, but when blood volume increases, blood pressure and flow increase.
Low blood volume, called hypovolemia, may be caused by bleeding, dehydration, vomiting, severe burns, or by diuretics used to treat hypertension. Treatment typically includes intravenous fluid replacement. Excessive fluid volume, called hypervolemia, is caused by retention of water and sodium, as seen in clients with heart failure, liver cirrhosis, and some forms of kidney disease. Treatment may include the use of diuretics that cause the kidneys to eliminate sodium and water.[24]
Edema
Despite the presence of valves within larger veins, over the course of a day, some blood will inevitably pool in the lower limbs, due to the pull of gravity. Any blood that accumulates in a vein will increase the pressure within it. Increased pressure will promote the flow of fluids out of the capillaries and into the interstitial fluid. The presence of excess fluid around the cells leads to a condition called edema. See Figure 5.13[25] for an image of a client with pitting edema. Edema can also be generalized and non-pitting.

Most people experience a daily accumulation of fluid in their tissues, especially if they spend much of their time on their feet. However, clinical edema goes beyond normal swelling and requires medical treatment. Edema has many potential causes, including heart failure, severe protein deficiency, and renal failure. Diuretics such as furosemide are used to treat edema by causing the kidneys to eliminate sodium and water.[26] Read additional information about how to assess and document pitting edema in the “Assessment” subsection of the “General Cardiovascular System Assessment” section of this chapter.
Homeostatic Regulation of the Cardiovascular System
To maintain homeostasis in the cardiovascular system and provide adequate blood to the tissues, blood flow must be redirected continually to the tissues as they become more active. For example, when an individual is exercising, more blood will be directed to skeletal muscles, the heart, and the lungs. On the other hand, following a meal, more blood is directed to the digestive system. Only the brain receives a constant supply of blood regardless of rest or activity. Three homeostatic mechanisms ensure adequate blood flow and ultimately perfusion of tissues: autonomic nervous system, endocrine system, and autoregulatory mechanisms.
Baroreceptors and Chemoreceptors
The autonomic nervous system plays a critical role in the regulation of vascular homeostasis based on baroreceptors and chemoreceptors. Baroreceptors are specialized stretch receptors located within the aorta and carotid arteries that respond to the degree of stretch caused by the presence of blood and then send impulses to the cardiovascular center to regulate blood pressure. Baroreceptors sense changes in the level of pressure within the vessels. In addition to the baroreceptors, chemoreceptors monitor levels of oxygen, carbon dioxide, and hydrogen ions (pH). Chemoreceptors sense changes in the level of oxygen within the blood. When the cardiovascular center in the brain receives this input, it triggers a reflex that maintains homeostasis.
Endocrine Regulation
Endocrine control over the cardiovascular system involves catecholamines, epinephrine, and norepinephrine, as well as several hormones that interact with the kidneys in the regulation of blood volume.
Epinephrine and Norepinephrine
The catecholamines epinephrine and norepinephrine are released by the adrenal medulla and are a part of the body’s sympathetic or fight-or-flight response. They increase heart rate and force of contraction, while temporarily constricting blood vessels to organs not essential for flight-or-fight responses and redirecting blood flow to the liver, muscles, and heart.
Antidiuretic Hormone
Antidiuretic hormone (ADH), also known as vasopressin, is secreted by the hypothalamus. The primary trigger prompting the hypothalamus to release ADH is increasing osmolarity of tissue fluid, usually in response to significant loss of blood volume. ADH signals its target cells in the kidneys to reabsorb more water, thus preventing the loss of additional fluid in the urine. This will increase overall fluid levels and help restore blood volume and pressure.
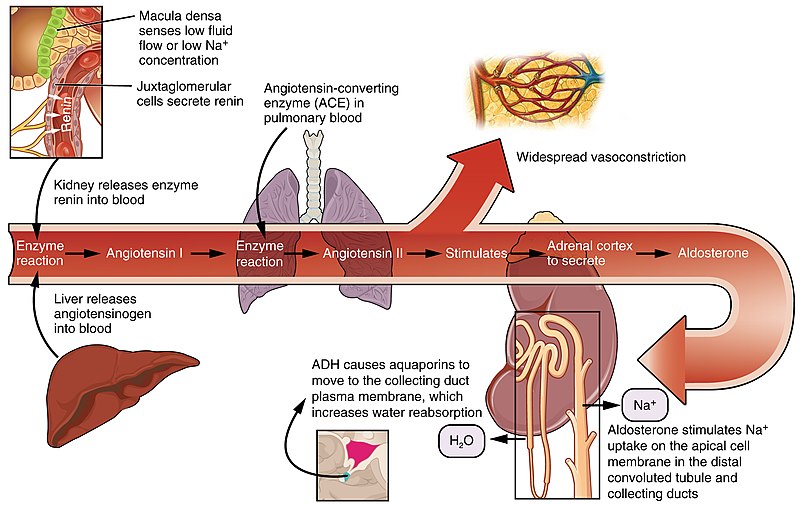
Renin-Angiotensin-Aldosterone System
The renin-angiotensin-aldosterone system (RAAS) also has a major effect on the cardiovascular system. Specialized cells in the kidneys respond to decreased blood flow by secreting renin into the blood. Renin converts the plasma protein angiotensinogen into its active form—Angiotensin I. Angiotensin I circulates in the blood and is then converted into Angiotensin II in the lungs. This reaction is catalyzed by the enzyme called angiotensin-converting enzyme (ACE). Medications that impact angiotensin, such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) target this step in the RAAS in an effort to decrease blood pressure.
Angiotensin II is a powerful vasoconstrictor that greatly increases blood pressure. It also stimulates the release of ADH and aldosterone, a hormone produced by the adrenal cortex. Aldosterone then increases the reabsorption of sodium into the blood by the kidneys. Because water follows sodium, there is an increase in the reabsorption of water, which increases blood volume and blood pressure. See Figure 5.14[27] for an illustration of the renin-angiotensin-aldosterone system. See Figure 5.15 [28] for a summary of the effect of hormones involved in renal control of blood pressure.
Autoregulation of Perfusion
Local, self-regulatory mechanisms allow each region of tissue to adjust its blood flow—and thus its perfusion. These mechanisms are affected by sympathetic and parasympathetic stimulation, as well as endocrine factors. See Table 5.2 for a summary of these factors and their effects.[29]
Table 5.2. Effects of Nervous System, Endocrine, and Local Controls on the Vasoconstriction and Vasodilation of Arterioles
| Control | Factor | Vasoconstriction | Vasodilation |
|---|---|---|---|
| Autonomic Nervous System | Sympathetic stimulation | Arterioles within integument, abdominal viscera, and mucosa membrane; skeletal muscles (at high levels); varied in veins and venules | Arterioles within heart; skeletal muscles at low to moderate levels |
| Parasympathetic | No known innervation for most | Arterioles in external genitalia; no known innervation for most other arterioles or veins | |
| Endocrine | Epinephrine | Similar to sympathetic stimulation for extended flight-or-fight responses; at high levels, binds to specialized alpha (α)-receptors | Similar to sympathetic stimulation for extended fight-or-flight responses; at low to moderate levels, binds to specialized beta (β)-receptors |
| Norepinephrine | Similar to epinephrine | Similar to epinephrine | |
| Angiotensin II | Powerful generalized vasoconstrictor; also stimulates release of aldosterone and ADH | N/A | |
| ADH | Moderately strong generalized vasoconstrictor; also causes body to retain more fluid via kidneys, increasing blood volume and pressure | N/A |
- “Position of the Heart in the Thorax” by OpenStax College is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/19-1-heart-anatomy ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “Dual System of the Human Blood Circulation” by OpenStax College is licensed under CC By 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/19-1-heart-anatomy ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “Surface Anatomy of the Heart” by OpenStax College is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/19-1-heart-anatom ↵
- “2018 Conduction System of the Heart” by OpenStax College is licensed under CC BY 4.0. Access it for free at https://openstax.org/books/anatomy-and-physiology/pages/19-2-cardiac-muscle-and-electrical-activity ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “2022_Electrocardiogram.jpg” by OpenStax College is licensed under CC BY 3.0. ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “2031 Factors in Cardiac Output.jpg” by OpenStax College is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/19-4-cardiac-physiology ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “2032 Automatic Innervation.jpg” by OpenStax College is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/19-4-cardiac-physiology ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “2036 Summary of Factors in Cardiac Output.jpg” by OpenStax College is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/19-4-cardiac-physiology ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “2120_Major_Systemic_Artery.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- “Illu_capillary_en.jpg” by Unknown author is licensed in the Public Domain ↵
- “2131_Major_S” by ystematic_Veins.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “2110_Pulse_Sites.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “Combinpedal.jpg” by James Heilman, MD is licensed under CC BY-SA 3.0 ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “2626 Renin Aldosterone Angiotensin.jpg” by OpenStax College is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/25-4-microscopic-anatomy-of-the-kidney ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy and Physiology by OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
A type of wound that is sutured, stapled, glued, or otherwise closed so the wound heals beneath the closure.
A type of healing that occurs when the edges of a wound cannot be brought together, so the wound fills in from the bottom up by the production of granulation tissue. An example of a wound healing by secondary intention is a pressure injury.
There has been significant national debate over the difference between assignment and delegation over the past few decades. In 2019 the National Council of State Boards of Nursing (NCSBN) and the American Nurses Association (ANA) published updated joint National Guidelines on Nursing Delegation (NGND).[1] These guidelines apply to all levels of nursing licensure (advanced practice registered nurses [APRN], registered nurses [RN], and licensed practical/vocational nurses [LPN/VN]) when delegating when there is no specific guidance provided by the state’s Nurse Practice Act (NPA).[2] It is important to note that states have different laws and rules/regulations regarding delegation, so it is the responsibility of all licensed nurses to know what is permitted in their jurisdiction.
The NGND defines a delegatee as an RN, LPN/VN, or AP who is delegated a nursing responsibility by either an APRN, RN, or LPN/VN, is competent to perform the task, and verbally accepts the responsibility.[3] Delegation is allowing a delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role and not routinely performed, but the individual has obtained additional training and validated their competence to perform the delegated responsibility.[4] However, the licensed nurse still maintains accountability for overall client care. Delegated responsibility is a nursing activity, skill, or procedure that is transferred from a licensed nurse to a delegatee.[5] Accountability is defined as being answerable to oneself and others for one’s own choices, decisions, and actions as measured against a standard. Therefore, if a nurse does not feel it is appropriate to delegate a certain responsibility to a delegatee, the delegating nurse should perform the activity themselves.[6]
Delegation is summarized in the NGND as the following[7]:
- A delegatee is allowed to perform a specific nursing activity, skill, or procedure that is outside the traditional role and basic responsibilities of the delegatee’s current job.
- The delegatee has obtained the additional education and training and validated competence to perform the care/delegated responsibility. The context and processes associated with competency validation will be different for each activity, skill, or procedure being delegated. Competency validation should be specific to the knowledge and skill needed to safely perform the delegated responsibility, as well as to the level of the practitioner (e.g., RN, LPN/VN, AP) to whom the activity, skill, or procedure has been delegated. The licensed nurse who delegates the “responsibility” maintains overall accountability for the client, but the delegatee bears the responsibility for completing the delegated activity, skill, or procedure.
- The licensed nurse cannot delegate nursing clinical judgment or any activity that will involve nursing clinical judgment or critical decision-making to AP.
- Nursing responsibilities are delegated by a licensed nurse who has the authority to delegate and the delegated responsibility is within the delegator’s scope of practice.
An example of delegation is medication administration that is delegated by a licensed nurse to AP with additional training in some agencies, according to agency policy. This task is outside the traditional role of AP, but the delegatee has received additional training for this delegated responsibility and has completed competency validation in completing this task accurately.
An example illustrating the difference between assignment and delegation is assisting patients with eating. Feeding patients is typically part of the routine role of AP. However, if a client has recently experienced a stroke (i.e., cerebrovascular accident) or is otherwise experiencing swallowing difficulties (e.g., dysphagia), this task cannot be assigned to AP because it is not considered routine care. Instead, the RN should perform this task themselves or delegate it to an AP who has received additional training on feeding assistance.
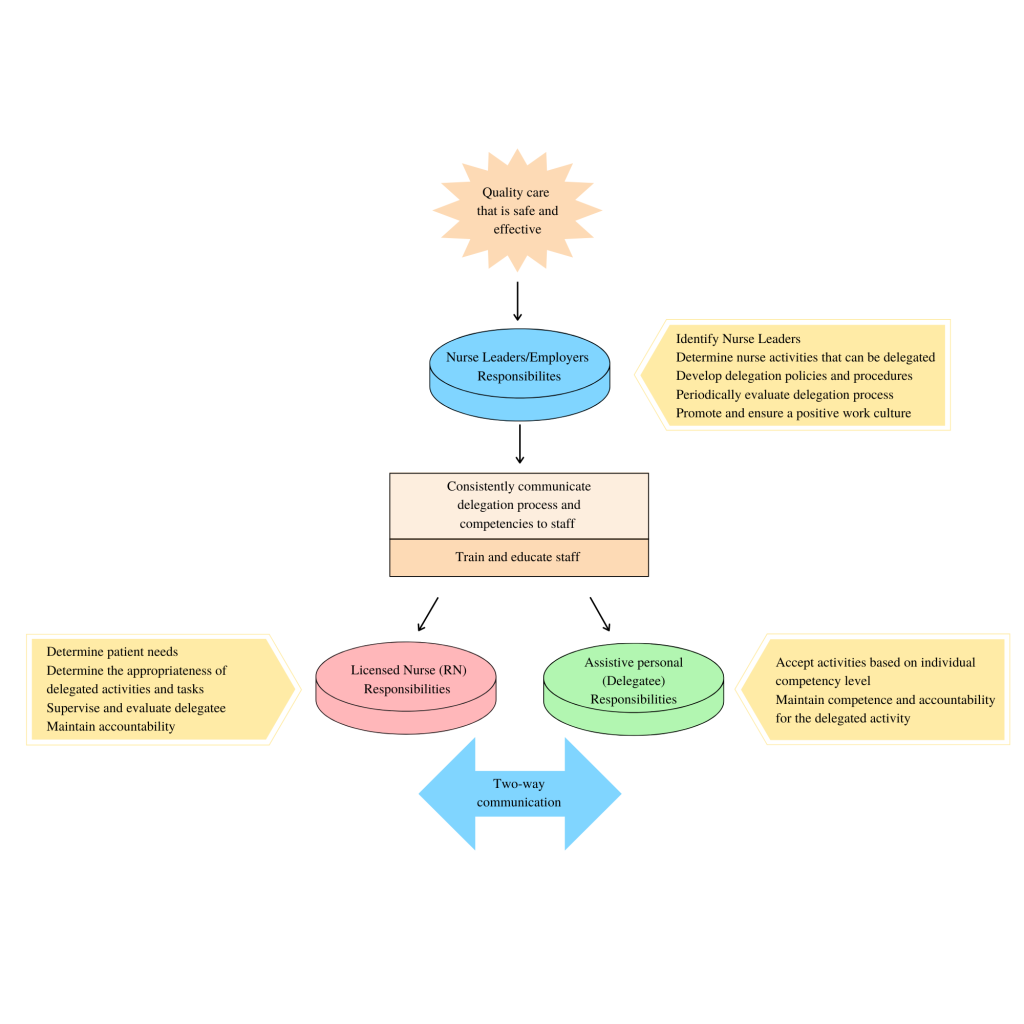
The delegation process is multifaceted. See Figure 3.2[8] for an illustration of the intersecting responsibilities of the employer/nurse leader, licensed nurse, and delegatee with two-way communication that protects the safety of the public. “Delegation begins at the administrative/nurse leader level of the organization and includes determining nursing responsibilities that can be delegated, to whom, and under what circumstances; developing delegation policies and procedures; periodically evaluating delegation processes; and promoting a positive culture/work environment. The licensed nurse is responsible for determining client needs and when to delegate, ensuring availability to the delegatee, evaluating outcomes, and maintaining accountability for delegated responsibility. Finally, the delegatee must accept activities based on their competency level, maintain competence for delegated responsibility, and maintain accountability for delegated activity.”[9]
Five Rights of Delegation
How does the RN determine what tasks can be delegated, when, and to whom? According to the National Council of State Boards of Nursing (NCSBN), RNs should use the five rights of delegation to ensure proper and appropriate delegation: right task, right circumstance, right person, right directions and communication, and right supervision and evaluation[10]:
- Right task: The activity falls within the delegatee’s job description or is included as part of the established policies and procedures of the nursing practice setting. The facility needs to ensure the policies and procedures describe the expectations and limits of the activity and provide any necessary competency training.
- Right circumstance: The health condition of the client must be stable. If the client’s condition changes, the delegatee must communicate this to the licensed nurse, and the licensed nurse must reassess the situation and the appropriateness of the delegation.[11]
- Right person: The licensed nurse, along with the employer and the delegatee, is responsible for ensuring that the delegatee possesses the appropriate skills and knowledge to perform the activity.[12]
- Right directions and communication: Each delegation situation should be specific to the client, the nurse, and the delegatee. The licensed nurse is expected to communicate specific instructions for the delegated activity to the delegatee; the delegatee, as part of two-way communication, should ask any clarifying questions. This communication includes any data that need to be collected, the method for collecting the data, the time frame for reporting the results to the licensed nurse, and additional information pertinent to the situation. The delegatee must understand the terms of the delegation and must agree to accept the delegated activity. The licensed nurse should ensure the delegatee understands they cannot make any decisions or modifications in carrying out the activity without first consulting the licensed nurse.[13]
- Right supervision and evaluation: The licensed nurse is responsible for monitoring the delegated activity, following up with the delegatee at the completion of the activity, and evaluating client outcomes. The delegatee is responsible for communicating client information to the licensed nurse during the delegation situation. The licensed nurse should be ready and available to intervene as necessary. The licensed nurse should ensure appropriate documentation of the activity is completed.[14]
Simply stated, the licensed nurse determines the right person is assigned the right tasks for the right clients under the right circumstances. When determining what aspects of care can be delegated, the licensed nurse uses clinical judgment while considering the client’s current clinical condition, as well as the abilities of the health care team member. The RN must also consider if the circumstances are appropriate for delegation. For example, although obtaining routine vital signs on stable clients may be appropriate to delegate to assistive personnel, obtaining vital signs on an unstable client is not appropriate to delegate.
After the decision has been made to delegate, the nurse assigning the tasks must communicate appropriately with the delegatee and provide the right directions and supervision. Communication is key to successful delegation. Clear, concise, and closed-loop communication is essential to ensure successful completion of the delegated task in a safe manner. During the final step of delegation, also referred to as supervision, the nurse verifies and evaluates that the task was performed correctly, appropriately, safely, and competently. Read more about supervision in the following section on “Supervision.” See Table 3.4 for additional questions to consider for each “right” of delegation.
Table 3.4. Rights of Delegation[15]
| Rights of Delegation | Description | Questions to Consider When Delegating |
|---|---|---|
| Right Task | A task that can be transferred to a member of the nursing team for a specific client. |
|
| Right Circumstances | The client is stable. |
|
| Right Person | The person delegating the task has the appropriate scope of practice to do so. The task is also appropriate for this delegatee’s skills and knowledge. |
|
| Right Directions and Communication | The task or activity is clearly defined and described. |
|
| Right Supervision and Evaluation | The RN appropriately monitors the delegated activity, evaluates client outcomes, and follows up with the delegatee at the completion of the activity. |
|
Keep in mind that any nursing intervention that requires specific nursing knowledge, clinical judgment, or use of the nursing process can only be delegated to another RN. Examples of these types of tasks include initial preoperative or admission assessments, client teaching, and creation and evaluation of a nursing care plan. See Figure 3.3[16] for an algorithm based on the 2019 National Guidelines for Nursing Delegation that can be used when deciding if a nursing task can be delegated.[17]
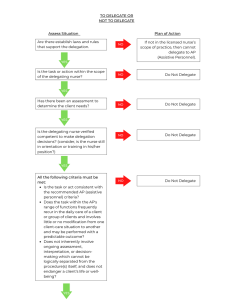
Responsibilities of the Licensed Nurse
The licensed nurse has several responsibilities as part of the delegation process. According to the NGND, any decision to delegate a nursing responsibility must be based on the needs of the client or population, the stability and predictability of the client’s condition, the documented training and competence of the delegatee, and the ability of the licensed nurse to supervise the delegated responsibility and its outcome with consideration to the available staff mix and client acuity. Additionally, the licensed nurse must consider the state Nurse Practice Act regarding delegation and the employer’s policies and procedures prior to making a final decision to delegate. Licensed nurses must be aware that delegation is at the nurse’s discretion, with consideration of the particular situation. The licensed nurse maintains accountability for the client, while the delegatee is responsible for the delegated activity, skill, or procedure. If, under the circumstances, a nurse does not feel it is appropriate to delegate a certain responsibility to a delegatee, the delegating nurse should perform the activity.[18]
1. The licensed nurse must determine when and what to delegate based on the practice setting, the client’s needs and condition, the state's/jurisdiction’s provisions for delegation, and the employer’s policies and procedures regarding delegating a specific responsibility. The licensed nurse must determine the needs of the client and whether those needs are matched by the knowledge, skills, and abilities of the delegatee and can be performed safely by the delegatee. The licensed nurse cannot delegate any activity that requires clinical reasoning, nursing judgment, or critical decision-making. The licensed nurse must ultimately make the final decision whether an activity is appropriate to delegate to the delegatee based on the “Five Rights of Delegation.”
- Rationale: The licensed nurse, who is present at the point of care, is in the best position to assess the needs of the client and what can or cannot be delegated in specific situations.[19]
2. The licensed nurse must communicate with the delegatee who will be assisting in providing client care. This should include reviewing the delegatee’s assignment and discussing delegated responsibilities, including information on the client’s condition/stability, any specific information pertaining to a certain client (e.g., no blood draws in the right arm), and any specific information about the client’s condition that should be communicated back to the licensed nurse by the delegatee.
- Rationale: Communication must be a two-way process involving both the licensed nurse delegating the activity and the delegatee being delegated the responsibility. Evidence shows that the better the communication between the nurse and the delegatee, the more optimal the outcome. The licensed nurse must provide information about the client and care requirements. This includes any specific issues related to any delegated responsibilities. These instructions should include any unique client requirements. The licensed nurse must instruct the delegatee to regularly communicate the status of the client.[20]
3. The licensed nurse must be available to the delegatee for guidance and questions, including assisting with the delegated responsibility, if necessary, or performing it themselves if the client’s condition or other circumstances warrant doing so.
- Rationale: Delegation calls for nursing judgment throughout the process. The final decision to delegate rests in the hands of the licensed nurse as they have overall accountability for the client.[21]
4. The licensed nurse must follow up with the delegatee and the client after the delegated responsibility has been completed.
- Rationale: The licensed nurse who delegates the “responsibility” maintains overall accountability for the client, while the delegatee is responsible for the delegated activity, skill, or procedure.[22]
5. The licensed nurse must provide feedback information about the delegation process and any issues regarding delegatee competence level to the nurse leader. Licensed nurses in the facility need to communicate to the nurse leader responsible for delegation any issues arising related to delegation and any individual whom they identify as not being competent in a specific responsibility or unable to use good judgment and decision-making.
- Rationale: This will allow the nurse leader responsible for delegation to develop a plan to address the situation.[23]
The decision of whether or not to delegate or assign is based on the RN’s judgment concerning the condition of the client, the competence of the nursing team member, and the degree of supervision that will be required of the RN if a task is delegated.[24]
Responsibilities of the Delegatee
Everyone is responsible for the well-being of clients. While the nurse is ultimately accountable for the overall care provided to a client, the delegatee shares the responsibility for the client and is fully responsible for the delegated activity, skill, or procedure.[25] The delegatee has the following responsibilities:
1. The delegatee must accept only the delegated responsibilities that they are appropriately trained and educated to perform and feel comfortable doing given the specific circumstances in the health care setting and client’s condition. The delegatee should confirm acceptance of the responsibility to carry out the delegated activity. If the delegatee does not believe they have the appropriate competency to complete the delegated responsibility, then the delegatee should not accept the delegated responsibility. This includes informing the nursing leadership if they do not feel they have received adequate training to perform the delegated responsibility, do not perform the procedure frequently enough to do it safely, or their knowledge and skills need updating.
- Rationale: The delegatee shares the responsibility to keep clients safe, and this includes only performing activities, skills, or procedures in which they are competent and comfortable doing.[26]
2. The delegatee must maintain competency for the delegated responsibility.
- Rationale: Competency is an ongoing process. Even if properly taught, the delegatee may become less competent if they do not frequently perform the procedure. Given that the delegatee shares the responsibility for the client, the delegatee also has a responsibility to maintain competency.[27]
3. The delegatee must communicate with the licensed nurse in charge of the client. This includes any questions related to the delegated responsibility and follow-up on any unusual incidents that may have occurred while the delegatee was performing the delegated responsibility, any concerns about a client’s condition, and any other information important to the client’s care.
- Rationale: The delegatee is a partner in providing client care. They are interacting with the client/family and caring for the client. This information and two-way communication are important for successful delegation and optimal outcomes for the client.[28]
4. Once the delegatee verifies acceptance of the delegated responsibility, the delegatee is accountable for carrying out the delegated responsibility correctly and completing timely and accurate documentation per facility policy.
- Rationale: The delegatee cannot delegate to another individual. If the delegatee is unable to complete the responsibility or feels as though they need assistance, the delegatee should inform the licensed nurse immediately so the licensed nurse can assess the situation and provide support. Only the licensed nurse can determine if it is appropriate to delegate the activity to another individual. If at any time the licensed nurse determines they need to perform the delegated responsibility, the delegatee must relinquish responsibility upon request of the licensed nurse.[29]
Responsibilities of the Employer/Nurse Leader
The employer and nurse leaders also have responsibilities related to safe delegation of client care:
1. The employer must identify a nurse leader responsible for oversight of delegated responsibilities for the facility. If there is only one licensed nurse within the practice setting, that licensed nurse must be responsible for oversight of delegated responsibilities for the facility.
- Rationale: The nurse leader has the ability to assess the needs of the facility, understand the type of knowledge and skill needed to perform a specific nursing responsibility, and be accountable for maintaining a safe environment for clients. They are also aware of the knowledge, skill level, and limitations of the licensed nurses and AP. Additionally, the nurse leader is positioned to develop appropriate staffing models that take into consideration the need for delegation. Therefore, the decision to delegate begins with a thorough assessment by a nurse leader designated by the institution to oversee the process.[30]
2. The designated nurse leader responsible for delegation, ideally with a committee (consisting of other nurse leaders) formed for the purposes of addressing delegation, must determine which nursing responsibilities may be delegated, to whom, and under what circumstances. The nurse leader must be aware of the state Nurse Practice Act and the laws/rules and regulations that affect the delegation process and ensure all institutional policies are in accordance with the law.
- Rationale: A systematic approach to the delegation process fosters communication and consistency of the process throughout the facility.[31]
3. Policies and procedures for delegation must be developed. The employer/nurse leader must outline specific responsibilities that can be delegated and to whom these responsibilities can be delegated. The policies and procedures should also indicate what may not be delegated. The employer must periodically review the policies and procedures for delegation to ensure they remain consistent with current nursing practice trends and that they are consistent with the state Nurse Practice Act. (Institution/employer policies can be more restrictive, but not less restrictive.)
- Rationale: Policies and procedures standardize the appropriate method of care and ensure safe practices. Having a policy and procedure specific to delegation and delegated responsibilities eliminates questions from licensed nurses and AP about what can be delegated and how they should be performed.[32]
4. The employer/nurse leader must communicate information about delegation to the licensed nurses and AP and educate them about what responsibilities can be delegated. This information should include the competencies of delegatees who can safely perform a specific nursing responsibility.
- Rationale: Licensed nurses must be aware of the competence level of staff and expectations for delegation (as described within the policies and procedures) to make informed decisions on whether or not delegation is appropriate for the given situahttps://www.nursingworld.org/content-hub/resources/nursing-leadership/delegation-in-nursing/tion. Licensed nurses maintain accountability for the client. However, the delegatee has responsibility for the delegated activity, skill, or procedure.
In summary, delegation is the transfer of the nurse’s responsibility for a task while retaining professional accountability for the client’s overall outcome. The decision to delegate is based on the nurse’s judgment, the act of delegation must be clearly defined by the nurse, and the outcomes of delegation are an extension of the nurse’s guidance and supervision. Delegation, when rooted in mutual respect and trust, is a key component to an effective health care team.
Delegation is an integral skill in the nursing profession to help manage the complexities of the dynamic and ever-changing health care environment. Delegation in nursing has been found to increase employee empowerment, decrease burnout, increase role commitment, and improve job satisfaction.[33] Cultivating delegation skills helps nurses better manage the complexities of their client care role, ensuring that their clients are safely cared for and outcomes are optimized. Delegation skills, like other nursing skills, require purposeful development and do not necessarily come easily when first transitioning into the nursing role. It is important that the new graduate nurse does not mistake delegation for pompous or arrogant behavior. Delegation requires mutual respect between the delegator and delegatee. Delegation is not seen as a sign or weakness and does not reflect one's desire to shirk their work responsibilities. Instead, delegation reflects strong leadership and organizational skills in which the nurse leader demonstrates that they understand how to leverage their team's strengths in order to achieve optimal care outcomes.
To help avoid any perception of arrogance in the delegation of an activity, it is important that the new graduate nurse approaches the task of delegation with humility. Clarity in the communication of the delegated responsibility is critical, and the rationale behind the delegation should be communicated to the delegatee. Within the task of delegation, the delegator should express appreciation for the delegatee and their contributions in the collaborative health care environment. Additionally, it is important to understand that no specific nurse delegated task is outside of the "nurse" role. For example, ambulating a client does not to an unlicensed assistive personnel simply because that individual is able to perform that task. Rather, nurses must be willing to perform delegated tasks themselves when necessary. This reflects a team-oriented mindset and helps to reinforce among the care team that all roles are critical to optimizing client care. For new graduate nurses who first transition into a specific health care setting, having the opportunity to shadow individuals in various work roles helps to foster a team mindset. Asking questions of various team members regarding their work role can help a new graduate nurse demonstrate respect and value for other roles.
Examples of helpful questions may include the following:
- "What is the biggest challenge in your typical workday?"
- "What do you most enjoy about your job?"
- "How is it best to communicate with you when the unit is busy?"
- "What do you think people misunderstand most about your role?"
It is important to ensure that the team understands that care is optimized when they function as one collective unit and not in siloed roles. Each team member must feel valued and competent in their role. By understanding and practicing strategic delegation, new graduate nurses can overcome any misconceptions of arrogance and contribute positively to the healthcare team.
Please review the example below to consider variation in approach to task delegation.
Scenario A: Nurse June, a newly graduated nurse, is working in a busy hospital unit. She needs an unlicensed assistive personnel (UAP), Alex, to take vital signs of a patient. Nurse June approaches Alex in the hallway and says in an abrupt tone, "Alex, I need you to take Mr. Smith's vital signs right now. I'm too busy to do it myself, and besides, that's what you're here for. Just get it done quickly."
Analysis: June’s tone and words suggest she sees Alex's role as less important and purely as a means to offload her tasks. June does not explain the urgency or importance of the task. June doesn’t acknowledge Alex's effort or capability, making the request seem like a command rather than a collaborative effort.
Scenario B: Nurse June, a newly graduated nurse, is working in a busy hospital unit. She needs an unlicensed assistive personnel (UAP), Alex, to take vital signs of a patient. Nurse June approaches Alex and says, "Hi Alex, could you please help me by taking Mr. Smith's vital signs? I'm handling a few urgent matters right now, and it would really help to have your support. I know you’re great at this, and your thoroughness really makes a difference in our patient care. Thank you so much!"
Analysis: June speaks to Alex with courtesy and acknowledges the value of his role. June clearly explains why she needs Alex's help and the importance of the task. June acknowledges Alex’s competence and expresses gratitude, fostering feelings of value and respect.
A type of healing that occurs when the edges of a wound cannot be brought together, so the wound fills in from the bottom up by the production of granulation tissue. An example of a wound healing by secondary intention is a pressure injury.
The healing of a wound that has had to remain open or has been reopened, often due to severe infection.
The healing of a wound that has had to remain open or has been reopened, often due to severe infection.
The well-closed edges of a wound healing by primary intention.
The well-closed edges of a wound healing by primary intention.
Localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.
Localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.
Interpretations or conclusions based on cues, personal experiences, preferences, or generalizations.
Damage that occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue.
Damage that occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue.
The rubbing of skin against a hard object, such as the bed or the arm of a wheelchair. This rubbing causes heat that can remove the top layer of skin and often results in skin damage.
The rubbing of skin against a hard object, such as the bed or the arm of a wheelchair. This rubbing causes heat that can remove the top layer of skin and often results in skin damage.
Intact skin with a localized area of nonblanchable erythema where prolonged pressure has occurred.
Intact skin with a localized area of nonblanchable erythema where prolonged pressure has occurred.
Partial-thickness loss of skin with exposed dermis. The wound bed is viable and may appear like an intact or ruptured blister.
Partial-thickness loss of skin with exposed dermis. The wound bed is viable and may appear like an intact or ruptured blister.
Full-thickness tissue loss in which fat is visible, but cartilage, tendon, ligament, muscle, and bone are not exposed.
Full-thickness tissue loss in which fat is visible, but cartilage, tendon, ligament, muscle, and bone are not exposed.
Full-thickness tissue loss like Stage 3 pressure injuries but also have exposed cartilage, tendon, ligament, muscle, or bone.
Full-thickness tissue loss like Stage 3 pressure injuries but also have exposed cartilage, tendon, ligament, muscle, or bone.
Full-thickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar.
Full-thickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar.
Persistent; non-blanchable; deep red, maroon, or purple discoloration of intact or non-intact skin revealing a dark wound bed or blood filled blister.
Persistent; non-blanchable; deep red, maroon, or purple discoloration of intact or non-intact skin revealing a dark wound bed or blood filled blister.
Skin redness that does not turn white when pressed.

