3.7 Vitamin B12 and Folate Deficiency Anemia
Open Resources for Nursing (Open RN)
Vitamin B12 and folate are water-soluble vitamins required for the production of red blood cells, white blood cells, and platelets. A deficiency of either of these vitamins causes megaloblastic anemia (also called macrocytic anemia) because the red blood cells in these disorders are abnormally large when compared to a healthy red blood cell.
As water-soluble vitamins, vitamin B12 and folate are not stored in the body and adequate amounts must be consumed in a person’s daily diet. Vitamin B12 (also called cobalamin) is present in many animal products, such as meats, dairy products, and eggs. Most balanced diets contain sufficient amounts of B12 except for vegan diets. Folate (also called vitamin B9) is present in many animal products and plants, especially liver and dark leafy vegetables. Most diets contain sufficient folate because many countries have supplemented cereals, flours, and grains with folic acid since the late 1990s to reduce the risk of neural tube defects during fetal development that can occur due to folate deficiency.[1],[2],[3],[4]
There are three basic causes of vitamin B12 anemia, including dietary deficiency, decreased absorption of vitamin B12, and an autoimmune disorder called pernicious anemia. Populations at risk for these causes include the following[5],[6],[7]:
- Dietary Deficiency: Individuals who follow a strict vegetarian (vegan) diet and do not eat animal products are at risk for not consuming enough vitamin B12 in their daily diet and often require vitamin supplements. Additionally, people of low socioeconomic status may not be able to afford animal proteins that contain Vitamin B12.
- Decreased Absorption of Vitamin B12: Some people may consume adequate amounts of vitamin B12 but have issues with absorbing this vitamin. Risk factors for decreased absorption of vitamin B12 are a gastric bypass, Crohn’s disease or other inflammatory bowel disorder, chronic use of antacids or proton pump inhibitors (PPIs), chronic H. Pylori infection, gastric cancer, chronic use of metformin, and chronic excess alcohol intake.
- Autoimmune Disorder: Pernicious anemia is a specific type of vitamin B12 anemia. Pernicious anemia is an autoimmune disorder in which antibodies are formed that attack the stomach cells that produce intrinsic factor. Intrinsic factor is a protein produced by the parietal cells of the stomach that carry vitamin B12 into the small intestine. Without intrinsic factor, vitamin B12 cannot be absorbed by the gastrointestinal tract.
Folate deficiency has become less common because food has been routinely supplemented with folic acid, but risk factors are similar to vitamin B12 deficiency. People who do not consume a varied, nutrient-rich diet are at risk for folate deficiency. For example, people with restrictive diets, anorexia nervosa, or those with excessive chronic alcohol use and a limited diet are at risk. Gastric bypass and inflammatory bowel disorders, as well as chronic medications such as methotrexate, antiseizure medications, and certain antibiotics, can also impact the absorption of folate. Furthermore, there is an increased need for folate for DNA synthesis in people who are pregnant or lactating, have chronic hemolytic anemia or severe eczema, or are undergoing dialysis.[8]
Pathophysiology
In healthy clients, when food sources containing vitamin B12 are ingested, vitamin B12 binds to an intrinsic factor, which is released from the parietal cells in the stomach. The vitamin B12-intrinsic factor complex is then able to bind to receptors on the ileum of the small intestine, and vitamin B12 can be absorbed. If vitamin B12 is not absorbed, neurological and hematological impairments will be seen as this vitamin plays a role in many chemical reactions throughout the body.[9]
Vitamin B12 and folate play critical roles in DNA and RNA synthesis. Therefore, when these vitamins are not available, not only are typical signs of anemia seen due to impaired red blood cell formation, but also other rapidly dividing cells are also affected. This also leads to elevated homocysteine (an amino acid that is broken down in the process of DNA synthesis), which can be useful for diagnostic purposes.[10],[11]
Vitamin B12 is also needed as a cofactor for enzymes in the Kreb’s cycle (a complex cycle that regulates cellular energy production). When B12 is not present for this cycle, methylmalonic acid (MMA) accumulates, which can damage the myelin sheath that surrounds and insulates nerves. This can lead to the neurological symptoms that are seen with vitamin B12 deficiency. MMA levels are also useful as a diagnostic tool.[12]
Assessment
Physical Examination
Clinical manifestations of anemia caused by vitamin B12 and folate deficiencies are related to the body’s inability to form red blood cells and other rapidly dividing cells. Vitamin B12 deficiency is also more likely to affect the nervous system, although folate deficiency may also cause neurocognitive symptoms. See Table 3.7a for a summary of the clinical manifestations of vitamin B12 and folic acid anemia across body systems.
Table 3.7a. Clinical Manifestations of Vitamin B12 and Folate Anemia[13],[14],[15],[16]
| Body System | Clinical Manifestation |
|---|---|
| General | Fatigue, progressive weakness |
| Nervous | Vitamin B12 deficiency: Symmetrical paresthesia/peripheral neuropathy, especially in the legs causing gait problems; dizziness; headaches; and vision changes |
| Gastrointestinal | Loss of appetite, weight loss, diarrhea
Vitamin B12 deficiency: Glossitis (pain, swelling, and tenderness of the tongue) Folate deficiency: Oral ulcers and beefy, red tongue |
| Integumentary | Pallor |
| Cardiovascular | Tachycardia and lightheadedness |
| Respiratory | Shortness of breath and tachypnea |
| Behavioral/Psychological | Subtle cognitive or psychiatric changes, especially in older adults |
Diagnostic Testing
A variety of lab tests may be ordered by a provider to diagnose vitamin B12 or folate deficiency. See Table 3.7b for a summary of common diagnostic tests. Review normal reference ranges for common diagnostic tests in “Appendix A – Normal Reference Ranges.”
Table 3.7b. Common Diagnostic Tests for Vitamin B12 and Folate Deficiency Anemia[17],[18]
| Lab Test | Expected Findings |
|---|---|
| Complete Blood Count | Decreased RBCs, decreased hemoglobin and hematocrit, and increased MCV (measures size of red blood cells). |
| Serum B12 Level | Above 300 pg/mL is normal.
Between 200-300 pg/mL is borderline deficient.* Below 200 pg/mL is considered deficient.* *Additional testing is performed to determine the cause, which impacts the route of supplementation. |
| Folate Level | Above 4 ng/mL is normal.
Between 2- 4 ng/mL is borderline deficient. Below 2 ng/mL is considered deficient. |
| Homocysteine Level | Elevated in vitamin B12 and folate deficiencies. |
| MMA Levels | Elevated in vitamin B12 deficiency. A normal MMA with elevated homocysteine levels indicates folate deficiency. |
| Anti-intrinsic Factor Antibodies | Positive in pernicious anemia. |
| Various Tests to Ascertain Etiology | If surgical or dietary history is not a causative factor, other tests may be ordered to determine the etiology of the vitamin B12 deficiency. For example, GI tests may be ordered to detect malabsorption issues. |
Nursing Diagnoses
Nursing priorities for clients with vitamin B12 anemia include promoting adequate tissue perfusion and oxygenation, providing adequate pain relief, preventing long-term neurological damage, preventing injury, enhancing nutrition (if applicable), improving fatigue and activity tolerance, and providing health teaching to help the client self-manage their disease.
Nursing diagnoses for clients with vitamin B12 anemia are created based on the specific needs of the client, their signs and symptoms, and their etiology of the disorder. These nursing diagnoses guide the creation of client specific care plans that encompass client outcomes and nursing interventions, as well the evaluation of those outcomes. These individualized care plans then serve as a guide for client treatment.
Common nursing diagnoses for clients with vitamin B12 anemia include the following[19],[20],[21]:
- Inadequate Tissue Perfusion
- Acute Pain
- Chronic Pain
- Risk for Falls
- Disturbed Sensory Perception
- Imbalanced Nutrition: Less Than Body Requirements
- Fatigue
- Decreased Activity Intolerance
- Readiness for Enhanced Knowledge
Outcome Identification
Outcome identification encompasses the creation of short- and long-term goals for the client. These goals are used to create expected outcome statements that are based on the specific needs of the client. Expected outcomes should be specific, measurable, and realistic. These outcomes should be achievable within a set time frame based on the application of appropriate nursing interventions.
Sample expected outcomes related to the previous nursing diagnoses are as follows[22]:
- The client will demonstrate adequate perfusion as demonstrated by appropriate urine output, skin color appropriate for race, palpable peripheral pulses, and vital signs within normal limits for age.
- The client will engage in fall prevention activities as specified by the care plan.
- The client will accurately verbalize the presence of sharp and dull sensations on hands and feet.
- The client will include food sources high in vitamin B12 with every meal.
- The client will describe two methods of energy conservation to manage fatigue.
Interventions
Medical Interventions
Medical Interventions for vitamin B12 deficiency depend on the cause, as well as the severity of the disorder. Common medical treatments include the following[23],[24],[25],[26]:
- Vitamin B12 Supplements (Cyanocobalamin): Supplements are administered orally or parenterally, with the prescribed route determined by the severity and the cause of the deficiency. For example, individuals with pernicious anemia must receive lifelong vitamin B12 parenteral (IM) supplements because they cannot absorb oral vitamin B12 due to the lack of intrinsic factor. Clients with severe vitamin B12 deficiency may also be initially treated with parenteral B12. Vitamin B12 is also available in oral, sublingual, subcutaneous, and intranasal forms. Clients should also be urged to increase their dietary intake of vitamin B12 with food sources such as meat and dairy. For those who follow a vegan diet, fortified cereals and fortified vegan milk substitutes are good sources of vitamin B12.
- Routine Monitoring of Vitamin B12 Levels: Monitoring is especially important in those who are at risk due to malabsorption such as those with Crohn’s disease.
- Blood Transfusions: Blood transfusions may be necessary in severe cases of vitamin B12 anemia. When clients have extreme symptoms or their hemoglobin levels fall below 7 g/dL, a transfusion may be prescribed.
Folate deficiency is treated with oral or parenteral administration of folic acid. Parental administration may be prescribed for severe, symptomatic anemia and then switched to oral therapy after symptoms resolve.[27]
Nursing Interventions
Common nursing interventions for clients with vitamin B12 deficiency anemia include the following[28],[29],[30],[31]:
- Monitor vitals because anemia can cause tachycardia and tachypnea.
- Perform comprehensive neurological assessments due to the neurological effects of vitamin B12 deficiency. If the client has been deficient in vitamin B12 for a prolonged amount of time, neurological symptoms may not be completely reversed even with adequate treatment.
- Administer vitamin B12 via enteral or parenteral routes per provider order and provide related health teaching. The RN should also monitor for potential side effects and allergic reactions. Hypokalemia is a common side effect of cyanocobalamin and would manifest as muscle cramping/weakness and/or irregular heartbeat. Cyanocobalamin contains cobalt and may need to be avoided in those with a cobalt sensitivity/allergy.
- Encourage a diet rich in vitamin B12. The recommended daily intake for vitamin B12 for adults is 2.4 mcg and more for those who are pregnant or breastfeeding.
- Initiate fall precautions such as a bed/chair alarm and a low height bed. Those with vitamin B12 anemia frequently exhibit dizziness, lightheadedness, paresthesia, vision changes, or confusion. Any of these symptoms put the client at increased risk for falls.
- Monitor input and output. Due to the potential for glossitis and impaired taste, the client may have a decreased appetite. Decreased appetite could also worsen the dietary intake of vitamin B12. Diarrhea can also put the client at risk for dehydration. Decreased urine output can also indicate ineffective peripheral tissue perfusion due to decreased red blood cell production.
- Assess pain because paresthesia and peripheral neuropathy may be painful.
- Teach energy management techniques such as setting priorities, assigning tasks to others, and balancing rest with activity.
Nurses provide preventative interventions by providing health teaching about the importance of folic acid supplements to prevent neural tube defects to female clients who are pregnant or trying to get pregnant. The recommended daily allowance of folic acid for adults is 400 mcg per day. For pregnant and lactating women, the dietary guideline is 600 mcg per day. Treatment of folate deficiency is typically 1-5 mg daily.[32]
Evaluation
During the evaluation stage, nurses determine the effectiveness of nursing interventions for a specific client. Lab results showing improvement of anemia resulting from vitamin B12 or folate deficiency should improve within one to two weeks and normalize within one to two months.[33] The previously identified expected outcomes are reviewed to determine if they were met, partially met, or not met by the time frames indicated. If outcomes are not met or only partially met by the time frame indicated, the nursing care plan is revised. Evaluation should occur every time the nurse implements interventions with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with other members of the interprofessional team.
![]() RN Recap: Vitamin B12 Deficiency Anemia
RN Recap: Vitamin B12 Deficiency Anemia
View a brief YouTube video overview of vitamin B deficiency anemia[34]:
- Means, R. T., & Fairifeld, K. M. (2023, October 18). Causes and physiology of vitamin B12 and folate deficiencies. In UpToDate. https://www.uptodate.com/contents/causes-and-pathophysiology-of-vitamin-b12-and-folate-deficiencies. ↵
- National Heart, Lung, and Blood Institute. (2022). Anemia - vitamin B12 deficiency. National Institutes of Health. https://www.nhlbi.nih.gov/health/anemia/vitamin-b12-deficiency-anemia ↵
- Ankar, A., & Kumar, A. (2022, Oct 22). Vitamin B12 Deficiency. In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441923 ↵
- Khan, K. M. & Jialal, I. (2023, June 26). Folic Acid Deficiency. In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK535377/ ↵
- National Heart, Lung, and Blood Institute. (2022). Anemia - vitamin B12 deficiency. National Institutes of Health. https://www.nhlbi.nih.gov/health/anemia/vitamin-b12-deficiency-anemia ↵
- Ankar, A., & Kumar, A. (2022, Oct 22). Vitamin B12 Deficiency. In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441923 ↵
- Means, R. T., & Fairifeld, K. M. (2023, October 18). Causes and physiology of vitamin B12 and folate deficiencies. In UpToDate. https://www.uptodate.com/contents/causes-and-pathophysiology-of-vitamin-b12-and-folate-deficiencies. ↵
- Means, R. T., & Fairifeld, K. M. (2023, October 18). Causes and physiology of vitamin B12 and folate deficiencies. In UpToDate. https://www.uptodate.com/contents/causes-and-pathophysiology-of-vitamin-b12-and-folate-deficiencies. ↵
- Ankar, A., & Kumar, A. (2022, Oct 22). Vitamin B12 Deficiency. In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441923 ↵
- Ankar, A., & Kumar, A. (2022, Oct 22). Vitamin B12 Deficiency. In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441923 ↵
- Means, R. T., & Fairifeld, K. M. (2023, October 18). Causes and physiology of vitamin B12 and folate deficiencies. In UpToDate. https://www.uptodate.com/contents/causes-and-pathophysiology-of-vitamin-b12-and-folate-deficiencies. ↵
- Ankar, A., & Kumar, A. (2022, Oct 22). Vitamin B12 Deficiency. In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441923 ↵
- National Heart, Lung, and Blood Institute. (2022). Anemia - vitamin B12 deficiency. National Institutes of Health. https://www.nhlbi.nih.gov/health/anemia/vitamin-b12-deficiency-anemia ↵
- Ankar, A., & Kumar, A. (2022, Oct 22). Vitamin B12 Deficiency. In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441923 ↵
- Vaqar, S., Shackelford, K., & Rudolph, S. (2023, May 8). Pernicious Anemia (Nursing). In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK568700 ↵
- Means, R. T., & Fairifeld, K. M. (2023, October 18). Causes and physiology of vitamin B12 and folate deficiencies. In UpToDate. https://www.uptodate.com/contents/causes-and-pathophysiology-of-vitamin-b12-and-folate-deficiencies. ↵
- Ankar, A., & Kumar, A. (2022, Oct 22). Vitamin B12 Deficiency. In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441923 ↵
- Means, R. T., & Fairifeld, K. M. (2023, October 18). Causes and physiology of vitamin B12 and folate deficiencies. In UpToDate. https://www.uptodate.com/contents/causes-and-pathophysiology-of-vitamin-b12-and-folate-deficiencies. ↵
- Ankar, A., & Kumar, A. (2022, Oct 22). Vitamin B12 Deficiency. In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441923 ↵
- Vaqar, S., Shackelford, K., & Rudolph, S. (2023, May 8). Pernicious Anemia (Nursing). In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK568700 ↵
- NursesLabs. (2023). 7 anemia nursing care plans. https://nurseslabs.com/anemia-nursing-care-plans/#h-nursing-diagnosis ↵
- NursesLabs. (2023). 7 anemia nursing care plans. https://nurseslabs.com/anemia-nursing-care-plans/#h-nursing-diagnosis ↵
- National Heart, Lung, and Blood Institute. (2022). Anemia - vitamin B12 deficiency. National Institutes of Health. https://www.nhlbi.nih.gov/health/anemia/vitamin-b12-deficiency-anemia ↵
- Ankar, A., & Kumar, A. (2022, Oct 22). Vitamin B12 Deficiency. In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441923 ↵
- Vaqar, S., Shackelford, K., & Rudolph, S. (2023, May 8). Pernicious Anemia (Nursing). In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK568700 ↵
- Vasavada, A. & Sanghavi, D. K. (2023, Apr 6). Cyanocobalamin. In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK555964 ↵
- Means, R. T., & Fairifeld, K. M. (2024, June 5). Treatment of vitamin B12 and folate deficiencies. In UpToDate. Treatment of vitamin B12 and folate deficiencies ↵
- National Heart, Lung, and Blood Institute. (2022). Anemia - vitamin B12 deficiency. National Institutes of Health. https://www.nhlbi.nih.gov/health/anemia/vitamin-b12-deficiency-anemia ↵
- Ankar, A., & Kumar, A. (2022, Oct 22). Vitamin B12 Deficiency. In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK441923 ↵
- Vaqar, S., Shackelford, K., & Rudolph, S. (2023, May 8). Pernicious Anemia (Nursing). In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK568700 ↵
- Vasavada, A. & Sanghavi, D. K. (2023, Apr 6). Cyanocobalamin. In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK555964 ↵
- Means, R. T., & Fairifeld, K. M. (2024, June 5). Treatment of vitamin B12 and folate deficiencies. In UpToDate. Treatment of vitamin B12 and folate deficiencies ↵
- Means, R. T., & Fairifeld, K. M. (2024, June 5). Treatment of vitamin B12 and folate deficiencies. In UpToDate. Treatment of vitamin B12 and folate deficiencies ↵
- Open RN Project. (2024, June 23). Health Alterations - Chapter 3 Hematological - Vitamin B12 deficiency anemia [Video]. YouTube. CC BY-NC 4.0https://youtu.be/sf7LS9eULyE?feature=shared ↵
When performing a comprehensive neurological exam, examiners may assess the functioning of the cranial nerves. When performing these tests, examiners compare responses of opposite sides of the face and neck. Instructions for assessing each cranial nerve are provided below.
Cranial Nerve I - Olfactory
Ask the patient to identify a common odor, such as coffee or peppermint, with their eyes closed. See Figure 6.11[1] for an image of a nurse performing an olfactory assessment.

Cranial Nerve II - Optic
Be sure to provide adequate lighting when performing a vision assessment.
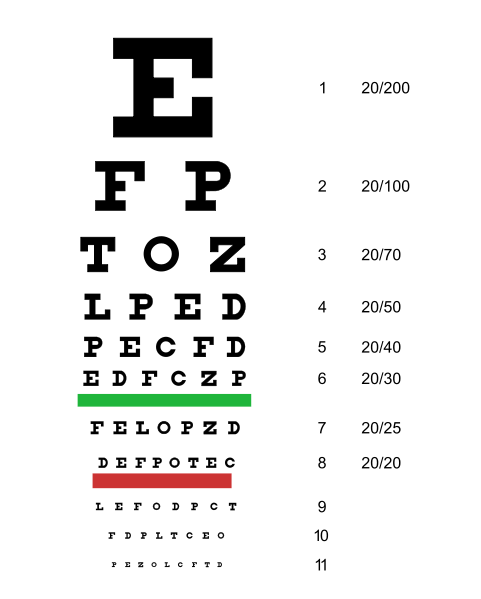
Far vision is tested using the Snellen chart. See Figure 6.12[2] for an image of a Snellen chart. The numerator of the fractions on the chart indicates what the individual can see at 20 feet, and the denominator indicates the distance at which someone with normal vision could see this line. For example, a result of 20/40 indicates this individual can see this line at 20 feet but someone with normal vision could see this line at 40 feet.
Test far vision by asking the patient to stand 20 feet away from a Snellen chart. Ask the patient to cover one eye and read the letters from the lowest line they can see.[3] Record the corresponding result in the furthermost right-hand column, such as 20/30. Repeat with the other eye. If the patient is wearing glasses or contact lens during this assessment, document the results as “corrected vision.” Repeat with each eye, having the patient cover the opposite eye. Alternative charts are available for children or adults who can’t read letters in English.
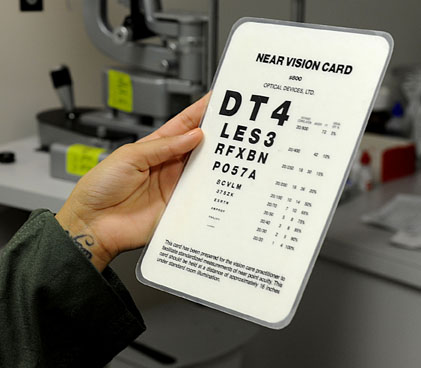
Near vision is assessed by having a patient read from a prepared card from 14 inches away. See Figure 6.13[4] for a card used to assess near vision.
Cranial Nerve III, IV, and VI - Oculomotor, Trochlear, Abducens
Cranial nerve III, IV, and VI (oculomotor, trochlear, abducens nerves) are tested together.
- Test eye movement by using a penlight. Stand 1 foot in front of the patient and ask them to follow the direction of the penlight with only their eyes. At eye level, move the penlight left to right, right to left, up and down, upper right to lower left, and upper left to lower right. Watch for smooth movement of the eyes in all fields. An unexpected finding is involuntary eye movement which may cause the eye to move rapidly from side to side, up and down, or in a circle, and may slightly blur vision referred to as nystagmus.
- Test bilateral pupils to ensure they are equally round and reactive to light and accommodation. Dim the lights of the room before performing this test.
- Pupils should be round and bilaterally equal in size. The diameter of the pupils usually ranges from two to five millimeters. Emergency clinicians often encounter patients with the triad of pinpoint pupils, respiratory depression, and coma related to opioid overuse.
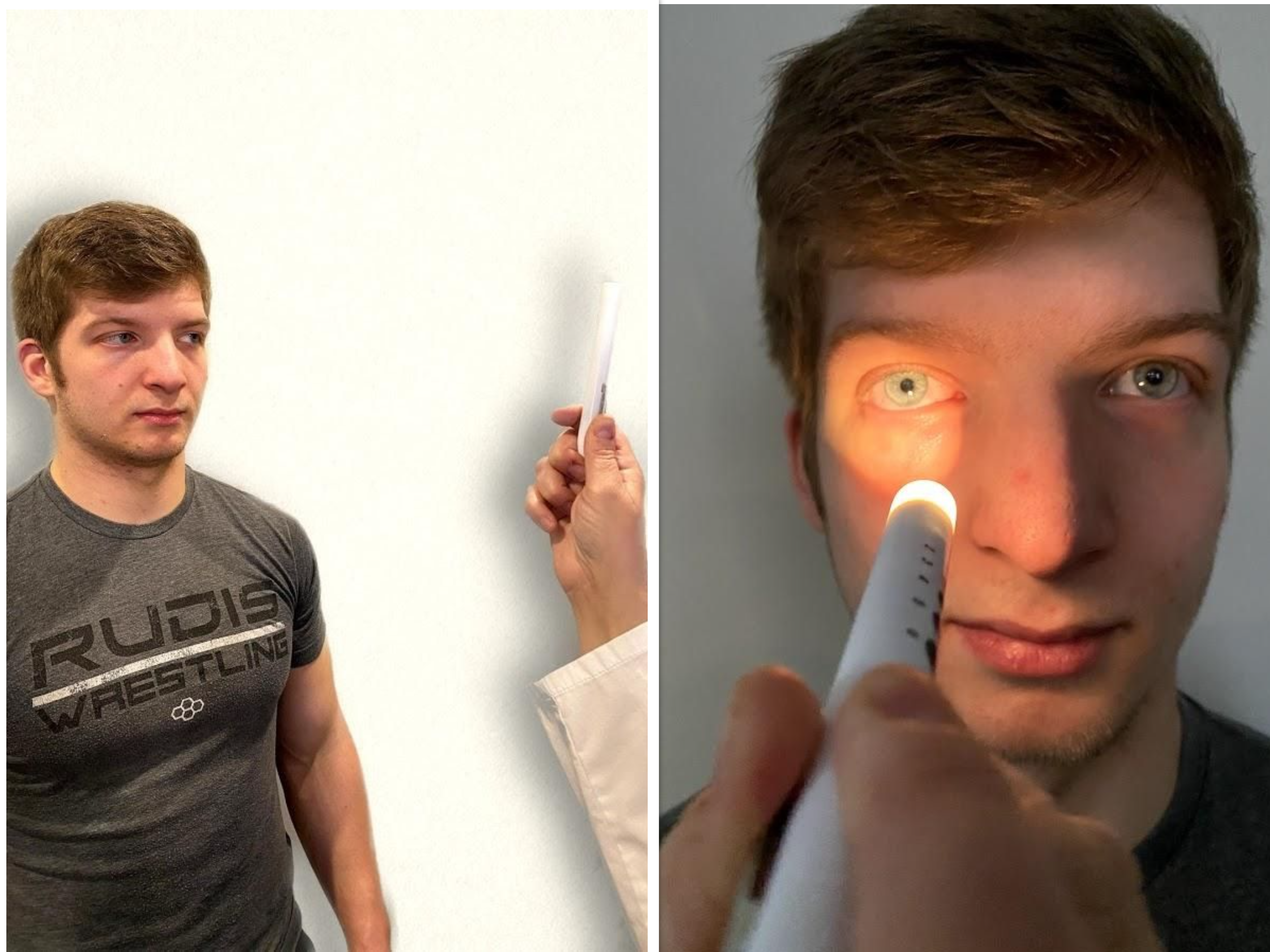
- Test pupillary reaction to light. Using a penlight, approach the patient from the side, and shine the penlight on one pupil. Observe the response of the lighted pupil, which is expected to quickly constrict. The pupil where you shine the light should constrict (direct reaction) and so should the other one (consensual reaction). Repeat by shining the light on the other pupil. Both pupils should react in the same manner to light. See Figure 6.14[5] for an image of a nurse assessing a patient’s pupillary reaction to light. An unexpected finding is when one pupil is larger than the other or one pupil responds more slowly than the other to light, which is often referred to as a “sluggish response.”
- Test eye convergence and accommodation. Recall that accommodation refers to the ability of the eye to adjust from near to far vision, with pupils constricting for near vision and dilating for far vision. Convergence refers to the action of both eyes moving inward as they focus on a close object using near vision. Ask the patient to look at a near object (4-6 inches away from the eyes), and then move the object out to a distance of 12 inches. Pupils should constrict while viewing a near object and then dilate while looking at a distant object, and both eyes should move together. See Figure 6.15[6] for an image of a nurse assessing convergence and accommodation.
- The acronym PERRLA is commonly used in medical documentation and refers to, "pupils are equal, round and reactive to light and accommodation."

Visit the National Library of Medicine's webpage for more details about assessing the Pupillary Light Reflex.
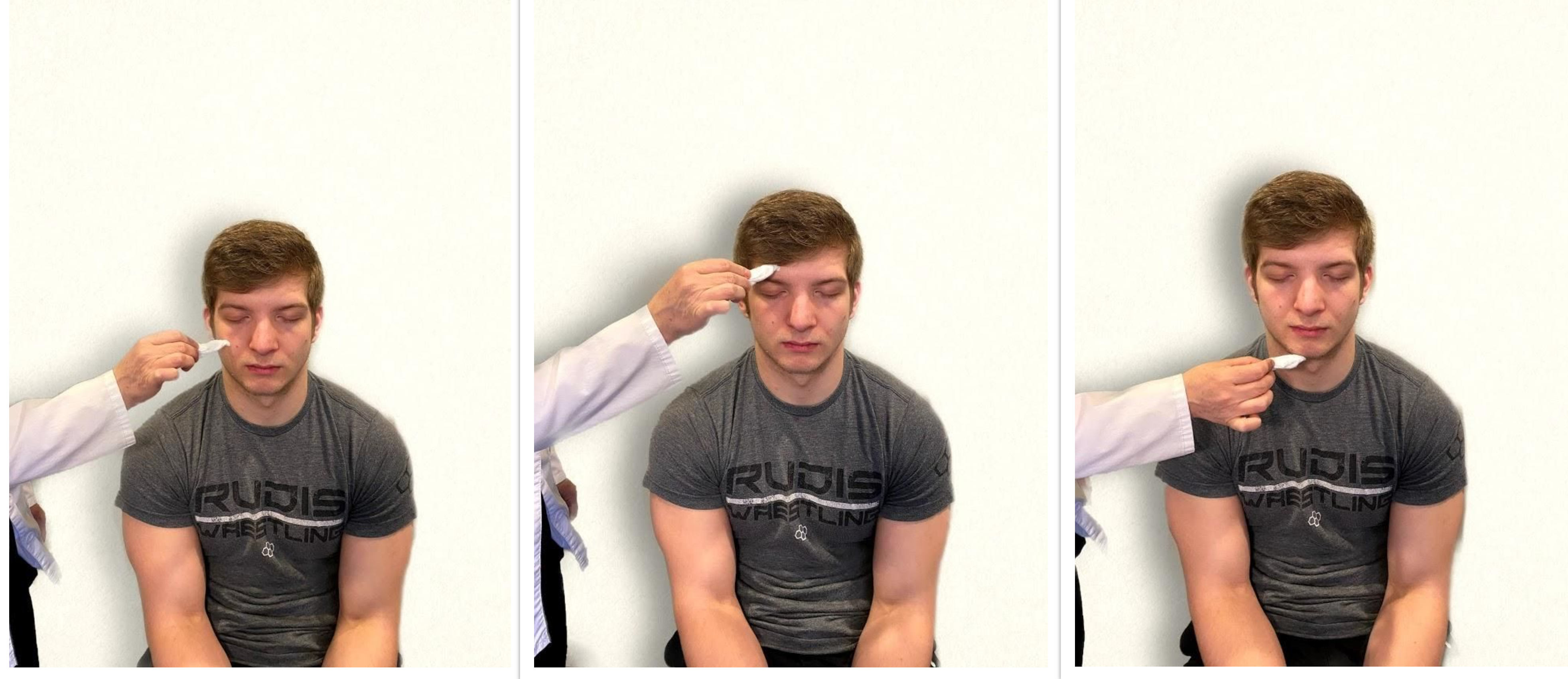
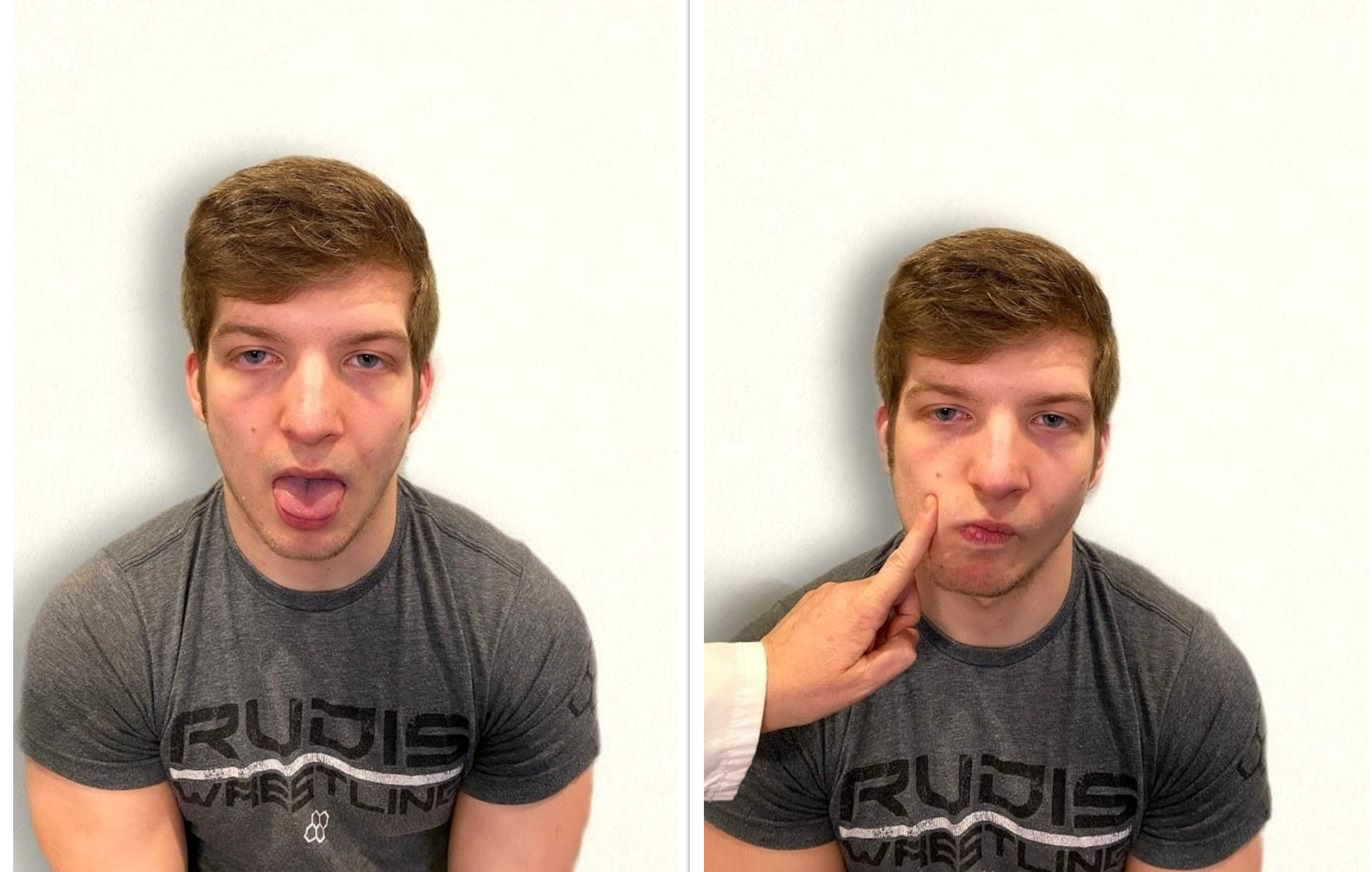
Cranial Nerve V - Trigeminal
- Test sensory function. Ask the patient to close their eyes, and then use a wisp from a cotton ball to lightly touch their face, forehead, and chin. Instruct the patient to say “Now” every time they feel the placement of the cotton wisp. See Figure 6.16[8] for an image of assessing trigeminal sensory function. The expected finding is that the patient will report every instance the cotton wisp is placed. An advanced technique is to assess the corneal reflex in comatose patients by touching the cotton wisp to the cornea of the eye to elicit a blinking response.
- Test motor function. Ask the patient to clench their teeth tightly while bilaterally palpating the temporalis and masseter muscles for strength. Ask the patient to open and close their mouth several times while observing muscle symmetry. See Figure 6.17[9] for an image of assessing trigeminal motor strength. The expected finding is the patient is able to clench their teeth and symmetrically open and close their mouth.

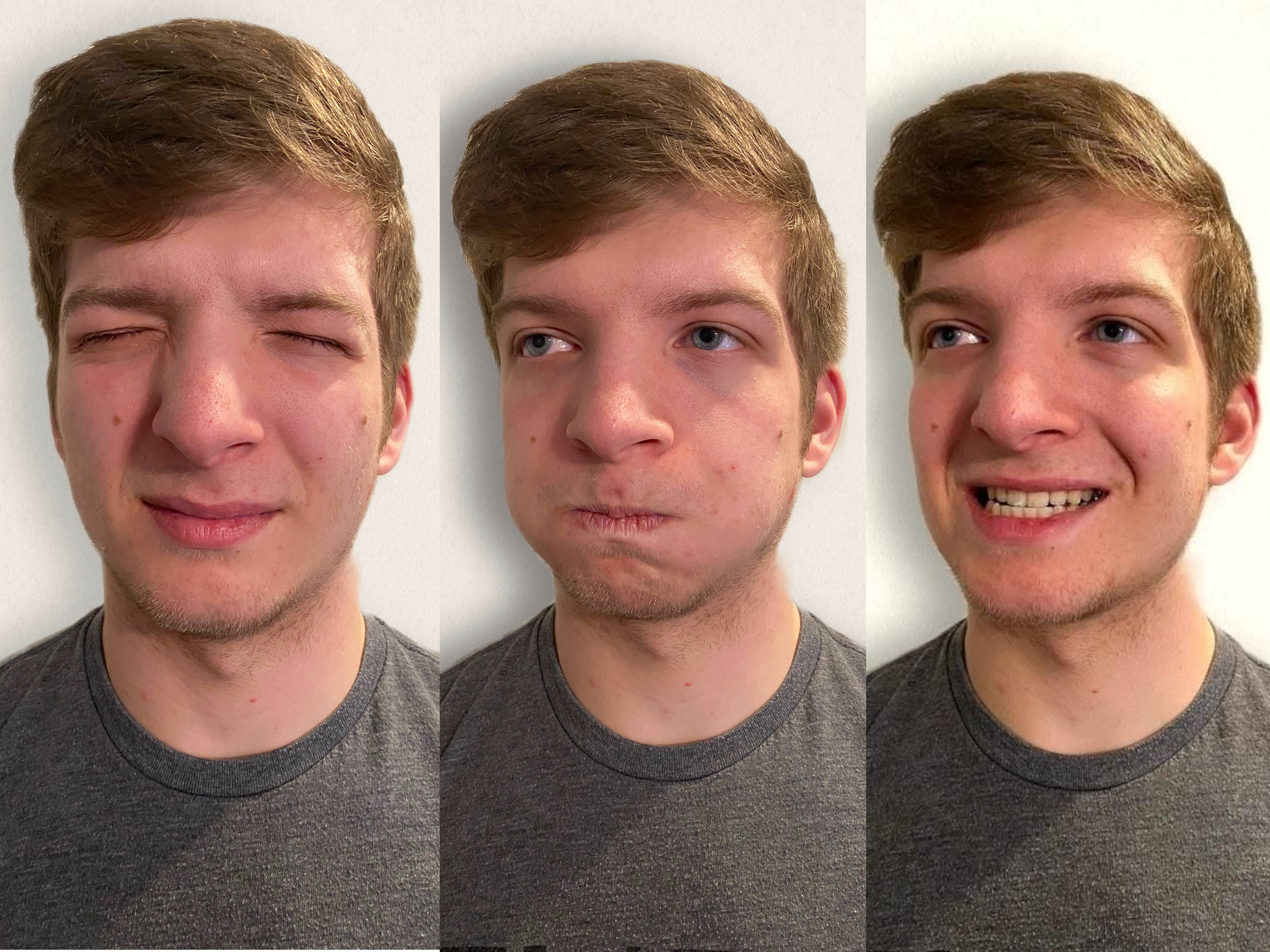
Cranial Nerve VII - Facial Nerve
- Test motor function. Ask the patient to smile, show teeth, close both eyes, puff cheeks, frown, and raise eyebrows. Look for symmetry and strength of facial muscles. See Figure 6.18[10] for an image of assessing motor function of the facial nerve.
- Test sensory function. Test the sense of taste by moistening three different cotton applicators with salt, sugar, and lemon. Touch the patient's anterior tongue with each swab separately, and ask the patient to identify the taste. See Figure 6.19[11] for an image of assessing taste.

Cranial Nerve VIII - Vestibulocochlear
- Test auditory function. Perform the whispered voice test. The whispered voice test is a simple test for detecting hearing impairment if done accurately. See Figure 6.20[12] for an image assessing hearing using the whispered voice test. Complete the following steps to accurately perform this test:
- Stand at arm's length behind the seated patient to prevent lip reading.
- Each ear is tested individually. The patient should be instructed to occlude the non-test ear with their finger.
- Exhale before whispering and use as quiet a voice as possible.
- Whisper a combination of numbers and letters (for example, 4-K-2), and then ask the patient to repeat the sequence.
- If the patient responds correctly, hearing is considered normal; if the patient responds incorrectly, the test is repeated using a different number/letter combination.
- The patient is considered to have passed the screening test if they repeat at least three out of a possible six numbers or letters correctly.
- The other ear is assessed similarly with a different combination of numbers and letters.
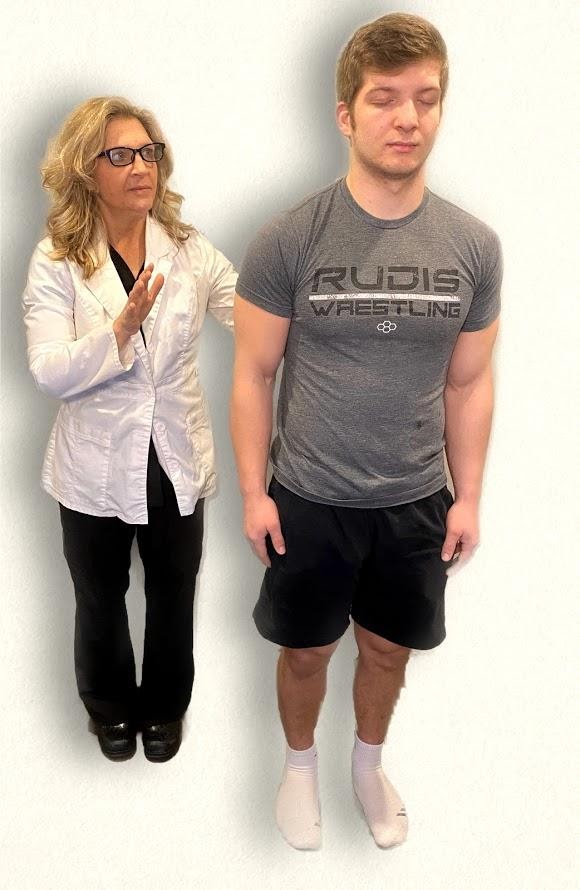
- Test balance. The Romberg test is used to test balance and is also used as a test for driving under the influence of an intoxicant. See Figure 6.21[13] for an image of the Romberg test. Ask the patient to stand with their feet together and eyes closed. Stand nearby and be prepared to assist if the patient begins to fall. It is expected that the patient will maintain balance and stand erect. A positive Romberg test occurs if the patient sways or is unable to maintain balance. The Romberg test is also a test of the body's sense of positioning (proprioception), which requires healthy functioning of the spinal cord.

Cranial Nerve IX - Glossopharyngeal
Ask the patient to open their mouth and say “Ah” and note symmetry of the upper palate. The uvula and tongue should be in a midline position and the uvula should rise symmetrically when the patient says "Ah." (See Figure 6.22.[14])

Cranial Nerve X - Vagus
Use a cotton swab or tongue blade to touch the patient’s posterior pharynx and observe for a gag reflex followed by a swallow. The glossopharyngeal and vagus nerves work together for integration of gag and swallowing. See Figure 6.23[15] for an image of assessing the gag reflex.

Cranial Nerve XI - Spinal Accessory
Test the right sternocleidomastoid muscle. Face the patient and place your right palm laterally on the patient's left cheek. Ask the patient to turn their head to the left while resisting the pressure you are exerting in the opposite direction. At the same time, observe and palpate the right sternocleidomastoid with your left hand. Then reverse the procedure to test the left sternocleidomastoid.
Continue to test the sternocleidomastoid by placing your hand on the patient's forehead and pushing backward as the patient pushes forward. Observe and palpate the sternocleidomastoid muscles.
Test the trapezius muscle. Ask the patient to face away from you and observe the shoulder contour for hollowing, displacement, or winging of the scapula and observe for drooping of the shoulder. Place your hands on the patient's shoulders and press down as the patient elevates or shrugs the shoulders and then retracts the shoulders.[16] See Figure 6.24[17] for an image of assessing the trapezius muscle.

Cranial Nerve XII - Hypoglossal
Ask the patient to protrude the tongue. If there is unilateral weakness present, the tongue will point to the affected side due to unopposed action of the normal muscle. An alternative technique is to ask the patient to press their tongue against their cheek while providing resistance with a finger placed on the outside of the cheek. See Figure 6.25[18] for an image of assessing the hypoglossal nerve.
Review of Cranial Nerve Assessment on YouTube[19]
Expected Versus Unexpected Findings
See Table 6.5 for a comparison of expected versus unexpected findings when assessing the cranial nerves.
Table 6.5 Expected Versus Unexpected Findings of an Adult Cranial Nerve Assessment
| Cranial Nerve | Expected Finding | Unexpected Finding (Dysfunction) |
|---|---|---|
| I. Olfactory | Patient is able to describe odor. | Patient has inability to identify odors (anosmia). |
| II. Optic | Patient has 20/20 near and far vision. | Patient has decreased visual acuity and visual fields. |
| III. Oculomotor | Pupils are equal, round, and reactive to light and accommodation. | Patient has different sized or reactive pupils bilaterally. |
| IV. Trochlear | Both eyes move in the direction indicated as they follow the examiner’s penlight. | Patient has inability to look up, down, inward, outward, or diagonally. Ptosis refers to drooping of the eyelid and may be a sign of dysfunction. |
| V. Trigeminal | Patient feels touch on forehead, maxillary, and mandibular areas of face and chews without difficulty. | Patient has weakened muscles responsible for chewing; absent corneal reflex; and decreased sensation of forehead, maxillary, or mandibular area. |
| VI. Abducens | Both eyes move in coordination. | Patient has inability to look side to side (lateral); patient reports diplopia (double vision). |
| VII. Facial | Patient smiles, raises eyebrows, puffs out cheeks, and closes eyes without difficulty; patient can distinguish different tastes. | Patient has decreased ability to taste. Patient has facial paralysis or asymmetry of face such as facial droop. |
| VIII. Vestibulocochlear (Acoustic) | Patient hears whispered words or finger snaps in both ears; patient can walk upright and maintain balance. | Patient has decreased hearing in one or both ears and decreased ability to walk upright or maintain balance. |
| IX. Glossopharyngeal | Gag reflex is present. | Gag reflex is not present; patient has dysphagia. |
| X. Vagus | Patient swallows and speaks without difficulty. | Slurred speech or difficulty swallowing is present. |
| XI. Spinal Accessory | Patient shrugs shoulders and turns head side to side against resistance. | Patient has inability to shrug shoulders or turn head against resistance. |
| XII. Hypoglossal | Tongue is midline and can be moved without difficulty. | Tongue is not midline or is weak. |
The Open RN Nursing Skills OER textbook was developed based on several external standards and uses a conceptual approach across all chapters.
External Standards
American Nurses Association (ANA):
The ANA provides standards for professional nursing practice, including nursing standards and a code of ethics for nurses.
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. https://www.nursingworld.org/ana/about-ana/standards/
- American Nurses Association. (2015). Code of ethics for nurses with interpretive statements. American Nurses Association. https://www.nursingworld.org/practice-policy/nursing-excellence/ethics/code-of-ethics-for-nurses
The National Council Licensure Examination for Registered Nurses: NCLEX-PN and NCLEX-RN Test Plans
The NCLEX-RN and NCLEX-PN test plans are updated every three years to reflect fair, comprehensive, current, and entry-level nursing competency measurement. Multiple resources are used to create the test plans, including recent practice analysis of nurses and expert opinions of the NEC, NCSBN staff, and boards of nursing/regulatory bodies, to ensure that the test plan is consistent with nurse practice acts.
The National League of Nursing (NLN): Competencies for Graduates of Nursing Programs
NLN competencies guide nursing curricula to position graduates in a dynamic health care arena with practice that is informed by a body of knowledge and ensures that all members of the public receive safe, quality care.
American Association of Colleges of Nursing (AACN): The Essentials: Competencies for Professional Nursing Education
The AACN provides a framework for preparing individuals as members of the discipline of nursing, reflecting expectations across
the trajectory of nursing education and applied experience.
Quality and Safety Education for Nurses (QSEN) Institute: Pre-licensure Competencies
Quality and safety competencies include knowledge, skills, and attitudes to be developed in nursing pre-licensure programs. QSEN competencies include patient-centered care, teamwork and collaboration, evidence-based practice, quality improvement, safety, and informatics.
Wisconsin State Legislature, Administrative Code Chapter N6
The Wisconsin Administrative Code governs the Registered Nursing and Practical Nursing professions in Wisconsin.
Healthy People 2030
Healthy People 2030 envisions a society in which all people can achieve their full potential for health and well-being across the life span. Healthy People provides objectives based on national data and includes social determinants of health.
Conceptual Approach
The Open RN Nursing Skills textbook incorporates the following concepts across all chapters.
- Holism. Florence Nightingale taught nurses to focus on the principles of holism, including wellness and the interrelationship of human beings and their environment. This textbook encourages the application of holism by assessing the impact of developmental, emotional, cultural, religious, and spiritual influences on a patient’s health status.
- Evidence Based Practice (EBP). Textbook content is based on current, evidence-based practices that are referenced by footnotes. To promote digital literacy, hyperlinks are provided to credible, free, online resources that supplement content. The Open RN textbooks will be updated as new EBP is established and with the release of updated NCLEX Test Plans every three years.
- Cultural Competency. Nurses have an ethical and moral obligation to provide culturally competent care to the patients they serve based on the ANA Code of Ethics.[20] Cultural considerations are included throughout this textbook.
- Care Across the Life Span. Developmental stages are addressed regarding patient assessments and procedures.
- Health Promotion. Focused interview questions and patient education topics are included to promote patient well-being and encourage self-care behaviors.
- Scope of Practice. Assessment techniques are included that have been identified as frequently performed by entry-level nurse generalists.[21],[22],[23],[24]
- Patient Safety. Expected and unexpected findings on assessment are highlighted in tables to promote patient safety by encouraging notification of health care providers when changes in condition occur.
- Clear and Inclusive Language. Content is written using clear language preferred by entry-level pre-licensure nursing students to enhance understanding of complex concepts.[25] "They" is used as a singular pronoun to refer to a person whose gender is unknown or irrelevant to the context of the usage, as endorsed by APA style. It is inclusive of all people and helps writers avoid making assumptions about gender.[26]
- Open-Source Images and Fair Use. Images are included to promote visual learning. Students and faculty can reuse open-source images by following the terms of their associated Creative Commons licensing. Some images are included based on Fair Use as described in the "Code of Best Practices for Fair Use and Fair Dealing in Open Education" presented at the OpenEd20 conference. Refer to the footnotes of images for source and licensing information throughout the text.
- Open Pedagogy. Students are encouraged to contribute to the Open RN textbooks in meaningful ways. In this textbook, students assisted in reviewing content for clarity for an entry-level learner and also assisted in creating open-source images.[27]
Supplementary Material Provided
Several supplementary resources are provided with this textbook.
- Supplementary, free videos to promote student understanding of concepts and procedures
- Sample documentation for assessments and procedures
- Online learning activities with formative feedback
- Critical thinking questions that encourage application of content to patient scenarios and the development of clinical judgment
- Free downloadable versions for offline use
Calculated oxygen saturation level in an ABG result. Normal range is 95-100%.

