3.2 Blood Pressure Basics
Open Resources for Nursing (Open RN)
What is Blood Pressure?
A blood pressure reading is the measurement of the force of blood against the walls of the arteries as the heart pumps blood through the body. It is reported in millimeters of mercury (mmHg). This pressure changes in the arteries when the heart is contracting compared to when it is resting and filling with blood. Blood pressure is typically expressed as the reflection of two numbers, systolic pressure and diastolic pressure. The systolic blood pressure is the maximum pressure on the arteries during systole, the phase of the heartbeat when the ventricles contract. This is the top number of a blood pressure reading. Systole causes the ejection of blood out of the ventricles and into the aorta and pulmonary arteries. The diastolic blood pressure is the resting pressure on the arteries during diastole, the phase between each contraction of the heart when the ventricles are filling with blood. This is the bottom number of the blood pressure reading.[1] Therefore, 120/80 indicates the systolic blood pressure is 120 mm Hg and the diastolic blood pressure is 80 mm Hg.
Blood pressure measurements are obtained using a stethoscope and a sphygmomanometer, also called a blood pressure cuff. To obtain a manual blood pressure reading, the blood pressure cuff is placed around a patient’s extremity, and a stethoscope is placed over an artery. For most blood pressure readings, the cuff is usually placed around the upper arm, and the stethoscope is placed over the brachial artery. The cuff is inflated to constrict the artery until the pulse is no longer palpable, and then it is deflated slowly. The American Heart Association (AHA) recommends that the blood pressure cuff be inflated at least 30 mmHg above the point at which the radial pulse is no longer palpable. The first appearance of sounds, called Korotkoff sounds, are noted as the systolic blood pressure reading. Korotkoff sounds are named after Dr. Korotkoff, who first discovered the audible sounds of blood pressure when the arm is constricted.[2] The blood pressure cuff continues to be deflated until Korotkoff sounds disappear. The last Korotkoff sounds reflect the diastolic blood pressure reading.[3] It is important to deflate the cuff slowly at no more than 2-3 mmHg per second to ensure that the absence of pulse is noted promptly and that the reading is accurate. Blood pressure readings are documented as systolic blood pressure/diastolic pressure, for example, 120/80 mmHg.
Abnormal blood pressure readings can signify an area of concern and a need for intervention. Normal adult blood pressure is less than 120/80 mmHg. Hypertension is the medical term for elevated blood pressure readings of 130/80 mmHg or higher. See Table 3.2 for blood pressure categories according to the 2017 American College of Cardiology and American Heart Association Blood Pressure Guidelines.[4] Prior to diagnosing a person with hypertension, the health care provider will calculate an average blood pressure based on two or more blood pressure readings obtained on two or more occasions.
For more information about hypertension and blood pressure medications, visit the “Cardiovascular and Renal System” chapter in Open RN Nursing Pharmacology.
Hypotension is the medical term for low blood pressure readings less than 90/60 mmHg.[5] Hypotension can be caused by dehydration, bleeding, cardiac conditions, and the side effects of many medications. Hypotension can be of significant concern because of the potential lack of perfusion to critical organs when blood pressures are low. Orthostatic hypotension is a drop in blood pressure that occurs when moving from a lying down (supine) or seated position to a standing (upright) position. When measuring blood pressure, orthostatic hypotension is defined as a decrease in blood pressure by at least 20 mmHg systolic or 10 mmHg diastolic within three minutes of standing. When a person stands, gravity moves blood from the upper body to the lower limbs. As a result, there is a temporary reduction in the amount of blood in the upper body for the heart to pump, which decreases blood pressure. Normally, the body quickly counteracts the force of gravity and maintains stable blood pressure and blood flow. In most people, this transient drop in blood pressure goes unnoticed. However, some patients with orthostatic hypotension can experience light-headedness, dizziness, or fainting. This is a significant safety concern because of the increased risk of falls and injury, particularly in older adults.[6] Orthostatic hypotension is also commonly referred to a postural hypotension. When obtaining orthostatic vital signs, the pulse rate may also be collected. If the pulse increases by 30 beats/minute or more while the patient stands (or sits if unable to stand), this indicates a significant change.
Perform the following actions when obtaining orthostatic vital signs:
- Have the patient stand upright for 1 minute if able.
- Obtain the blood pressure measurement while the patient stands using the same arm and the same equipment as the previous measurement that was taken with patient lying or sitting.
- Obtain the radial pulse again.
- Repeat the blood pressure and radial pulse measurements again at 3 minutes. Waiting several minutes before repeating the measurements allows time for the autonomic nervous system to compensate for blood volume shifts after position change in the patient without orthostatic hypotension.
- If the patient has symptoms that suggest orthostatic hypotension but doesn’t have documented orthostatic hypotension, repeat blood pressure measurement.
Tip: Some patients may not demonstrate significant decreases in blood pressure until they stand for more than 3 minutes.
Table 3.2 Blood Pressure Categories[7]
| Blood Pressure Category | Systolic mm Hg | Diastolic mm Hg |
|---|---|---|
| Normal | Less than 120 | Less than80 |
| Elevated | 120-129 | Less than 80 |
| Stage 1 | 130-139 | 80-89 |
| Stage 2 | 140 or higher | Greater or equal to 90 |
| Hypertensive Crisis | Greater than 180 | Greater than 120 |
View Ahmend Alzawi’s Korotkoff sounds video on YouTube.[8]
Equipment to Measure Blood Pressure
Manual Blood Pressure
A sphygmomanometer, commonly called a blood pressure cuff, is used to measure blood pressure while Korotkoff sounds are auscultated using a stethoscope. See Figure 3.1[9] for an image of a sphygmomanometer.
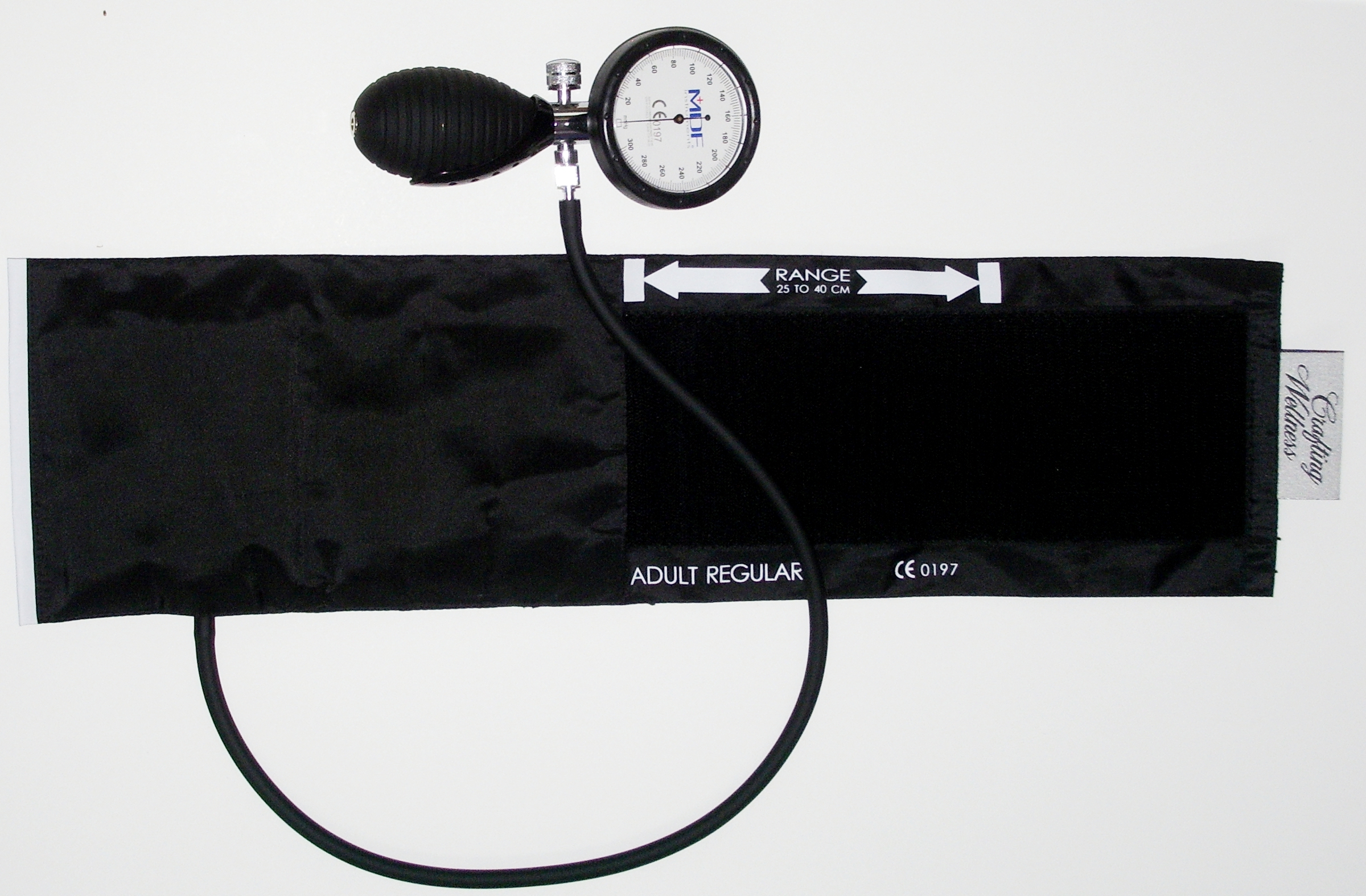
There are various sizes of blood pressure cuffs. It is crucial to select the appropriate size for the patient to obtain an accurate reading. An undersized cuff will cause an artificially high blood pressure reading, and an oversized cuff will produce an artificially low reading. See Figure 3.2[10] for an image of various sizes of blood pressure cuffs ranging in size for a large adult to an infant.

The width of the cuff should be 40% of the person’s arm circumference, and the length of the cuff’s bladder should be 80–100% of the person’s arm circumference. Keep in mind that only about half of the blood pressure cuff is the bladder and the other half is cloth with a hook and loop fastener to secure it around the arm.
View Ryerson University’s accurate blood pressure cuff sizing video on YouTube.[11]
Automatic Blood Pressure Equipment
Automatic blood pressure monitors are often used in health care settings to efficiently measure blood pressure for multiple patients or to repeatedly measure a single patient’s blood pressure at a specific frequency such as every 15 minutes. See Figure 3.3[12] for an image of an automatic blood pressure monitor. To use an automatic blood pressure monitor, appropriately position the patient and place the correctly sized blood pressure cuff on their bare arm or other extremity. Press the start button on the monitor. The cuff will automatically inflate and then deflate at a rate of 2 mmHg per second. The monitor digitally displays the blood pressure reading when done. If the blood pressure reading is unexpected, it is important to follow up by obtaining a reading using a manual blood pressure cuff. Additionally, automatic blood pressure monitors should not be used if the patient has a rapid or irregular heart rhythm, such as atrial fibrillation, or has tremors as it may lead to an inaccurate reading.

- This work is a derivative of Vital Sign Measurement Across the Lifespan - 1st Canadian Edition by Ryerson University licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Campbell and Pillarisetty licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology licensed under CC BY 4.0 ↵
- American College of Cardiology. Whelton, P. K., Carey, R. M., Aronow, W. S.., et al. (2018, May 7). 2017 guidelines for high blood pressure in adults. https://www.acc.org/latest-in-cardiology/ten-points-to-remember/2017/11/09/11/41/2017-guideline-for-high-blood-pressure-in-adults ↵
- National Heart, Lung, and Blood Institute. (n.d.). Low blood pressure. https://www.nhlbi.nih.gov/health-topics/low-blood-pressure ↵
- U.S. National Library of Medicine. (2020, June 23). Orthostatic hypotension. https://ghr.nlm.nih.gov/condition/orthostatic-hypotension ↵
- American College of Cardiology. Whelton, P. K., Carey, R. M., Aronow, W. S.., et al. (2018, May 7). 2017 guidelines for high blood pressure in adults. https://www.acc.org/latest-in-cardiology/ten-points-to-remember/2017/11/09/11/41/2017-guideline-for-high-blood-pressure-in-adults ↵
- Alzawi, A. (2015, November 19). Korotkoff+blood+pressure+sights+and+sounds SD [Video]. YouTube. All rights reserved. https://youtu.be/UfCr_wUepxo ↵
- “Sphygmomanometer&Cuff.JPG” by ML5 is in the Public Domain. ↵
- “BP-Multiple-Cuff-Sizes.jpg” by British Columbia Institute of Technology (BCIT) is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/vitalsign/chapter/how-is-blood-pressure-measured/ ↵
- Ryerson University. (2018, March 21). Blood pressure - Accurate cuff sizing [Video]. YouTube. All rights reserved. https://youtu.be/uNTMwoJTfFE ↵
- “Automatische bloeddrukmeter (0).jpg” by Harmid is in the Public Domain. ↵
Client Scenario
Mr. Hernandez is a 54-year-old client admitted to the medical telemetry floor with a diagnosis of heart failure exacerbation. He tells the nurse, "My breathing has gotten worse the past last three days and I have a lot of swelling in my feet."
Applying the Nursing Process
Assessment: Vital signs at the start of shift were blood pressure 154/94, heart rate 88, respiratory rate 24, and oxygen saturation 88%. On assessment, the nurse finds fine crackles in bilateral posterior lower lung bases, an S3 heart sound, and 2+ pitting edema in bilateral lower extremities midway to the knee. The nurse reviews the client's chart and discovers Mr. Hernandez has gained ten pounds since his previous office visit last week.
Based on the assessment information that has been gathered, the nurse creates the following nursing care plan for Mr. Hernandez:
Nursing Diagnosis: Excess Fluid Volume related to compromised regulatory mechanism as evidenced by fine crackles in bilateral posterior lung bases, S3 heart sound, weight gain of 10 pounds in the past week, and the client states, "My breathing has gotten worse the past last three days and I have a lot of swelling in my feet."
Overall Goal: The client will demonstrate stabilization in fluid volume.
SMART Expected Outcomes:
- Mr. Hernandez's vital signs and weight will return to his baseline in the next 48 hours.
- Mr. Hernandez will verbalize three rules of dietary and fluid restriction to follow at home following his educational session.
Planning and Implementing Nursing Interventions:
The nurse will weigh the client daily and analyze weight trends and 24-hour intake and output. The nurse will closely monitor lung sounds, respiratory rate, and oxygenation status. The nurse will establish a 24-hour schedule for fluid intake and educate the client regarding fluid restriction. The nurse will closely monitor lab results, especially sodium and potassium, and monitor for symptoms of fluid shifts. The nurse will provide health teaching regarding fluid and sodium restrictions.
Sample Documentation:
The client was admitted with acute heart failure exacerbation and stated, "My breathing has gotten worse the past last three days and I have a lot of swelling in my feet." On admission to the unit at 0900, vital signs were blood pressure 154/94, heart rate 88, respiratory rate 24, and oxygen saturation 88%. Fine crackles were present in bilateral posterior lower lung bases, an S3 heart sound was present, and there was 2+ pitting edema in bilateral lower extremities midway to the knee. The chart indicates he has gained ten pounds since his previous office visit last week. Provider orders and fluid restrictions were implemented. Lab results are within normal ranges. Client education regarding fluid and sodium restrictions and a handout were provided. At the end of the session, Mr. Hernandez was able to report back three rules of dietary and fluid restrictions to follow at home when discharged.
Evaluation:
By the end of the shift, the second SMART outcome was "met" when Mr. Hernandez was able to report back three rules of dietary and fluid restrictions after the client education session. The first SMART outcome was not yet met but will be reevaluated every shift for the next 24 hours.
Learning Activities
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Scenario A
Mr. Smith, a 60-year-old male, was admitted to the general medical floor with a diagnosis of an exacerbation of heart failure. See Figure 15.17 for an image of Mr. Smith.[1] He has a past medical history of hypertension and coronary artery disease. His admitting weight was 225 pounds. His baseline weight from a previous clinic visit was 210 pounds. On admission, he had fine crackles throughout his lower posterior lobes and 4+ pitting edema in his lower extremities. His ABG results on admission were pH 7.30, PaCO2 50 mmHg, PaO2 80 mm Hg, HCO3- 27 mEq/L, and SaO2 85%.

Questions
1. Interpret Mr. Smith's ABG results on admission.
2. Explain the likely cause of the ABG results.
3. Create a nursing diagnosis for Mr. Smith's fluid status in PES format based on his admission data.
Mr. Smith has received multiple doses of IV diuretics over the past three days since admission. During your morning assessment, Mr. Smith tells you he very thirsty and feels dizzy. You notice he is irritable and is becoming increasingly confused. You quickly obtain his vital signs: BP 85/45, HR 110, RR 24/minute, O2 saturation 98% on 2L/min per nasal cannula, and temperature 37.2 degrees Celsius. His lung sounds are clear, and his heart sounds are regular sinus rhythm. You notice his weight this morning was 205 pounds. You call the provider and receive orders for STAT basic metabolic panel and to initiate 0.9% Normal Saline IV fluids at 250 mL/hour until the provider arrives to evaluate the client.
The basic metabolic panel results (with the lab's normal reference range in parentheses) are as follows:
Sodium: 155 mEq/L (135-145)
Potassium: 3.3 mEq/L (3.5-5.3)
Chloride: 103 mEq/L (98-108)
Carbon dioxide: 25 mEq/L (23-27)
Blood urea nitrogen (BUN): 30 mg/dL (10-25)
Creatinine: 1.9 mg/dL (0.5-1.5)
Glucose: 100 mg/dL (fasting 70-99)
Questions
4. What is Mr. Smith’s fluid balance this morning? Support your answer with data.
5. What is the probable cause of his fluid balance?
6. Interpret Mr. Smith's lab results. What are the potential causes of these results?
7. Create a nursing diagnosis statement in PES format for Mr. Smith's current fluid status.
8. Create a new expected outcome in SMART format for Mr. Smith.
9. In addition to providing intravenous fluids, what additional interventions will you implement for Mr. Smith?
10. How will you evaluate if the nursing interventions are effective?
Scenario B
A 74-year-old male, Mr. M., was admitted to the general medical floor during the night shift with a diagnosis of pneumonia. See Figure 15.18 for an image of Mr. M.[2] He has a past medical history of alcohol abuse and coronary artery disease. You are the day shift nurse, and during your morning assessment, you notice that Mr. M. becomes increasingly lethargic and is not following commands consistently. You obtain the following vital signs: BP 80/45, HR 110, RR 8 and labored, O2 saturation 80% on 3L per nasal cannula, and temperature 38.1 degrees Celsius. His lung sounds reveal coarse crackles throughout, and you notice he is using accessory muscles with breathing. You notify the provider using an SBAR report and receive orders to increase oxygen to 10L per non-rebreather mask.

Lab results are ordered with the following results:
ABGs: pH 7.30, PaCO2 50, PaO2 59, HCO3 24, SaO2 80
Potassium: 5.9 mEq/L
Magnesium: 1.0 mEq/L
Calcium: 10.2 mg/dL
Sodium: 137 mEq/L
Hematocrit: 55%
Serum Osmolarity: 305 mmol/kg
BUN: 30 mg/dL
Urine Specific Gravity: 1.025
Questions
1. What is Mr. M.’s fluid balance? Provide data supporting the imbalance.
2. What is your interpretation of Mr. M.’s ABGs?
3. What is your interpretation of Mr. M.’s electrolyte studies?
4. Is Mr. M. stable or unstable? Why?
5. For what complications will you monitor?
6. Write an SBAR communication you would have with the health care provider to notify them about Mr. M.’s condition.
7. Create a NANDA-I diagnosis for Mr. M. in PES format.
8. Identify an expected outcome for Mr. M. in SMART format.
9. What interventions will you plan for Mr. M.?
10. How will you evaluate if your interventions are effective?
11. Write a nursing note about Mr. M.’s condition and your actions taken. This can be in the form of a DAR, SOAP, or summary nursing note.

Test your knowledge using this NCLEX Next Generation-style bowtie question. You may reset and resubmit your answers to this question an unlimited number of times.[3]

Test your knowledge using these NCLEX Next Generation-style questions. You may reset and resubmit your answers to the questions in this assignment an unlimited number of times.[4]
Learning Activities
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Scenario A
Mr. Smith, a 60-year-old male, was admitted to the general medical floor with a diagnosis of an exacerbation of heart failure. See Figure 15.17 for an image of Mr. Smith.[5] He has a past medical history of hypertension and coronary artery disease. His admitting weight was 225 pounds. His baseline weight from a previous clinic visit was 210 pounds. On admission, he had fine crackles throughout his lower posterior lobes and 4+ pitting edema in his lower extremities. His ABG results on admission were pH 7.30, PaCO2 50 mmHg, PaO2 80 mm Hg, HCO3- 27 mEq/L, and SaO2 85%.

Questions
1. Interpret Mr. Smith's ABG results on admission.
2. Explain the likely cause of the ABG results.
3. Create a nursing diagnosis for Mr. Smith's fluid status in PES format based on his admission data.
Mr. Smith has received multiple doses of IV diuretics over the past three days since admission. During your morning assessment, Mr. Smith tells you he very thirsty and feels dizzy. You notice he is irritable and is becoming increasingly confused. You quickly obtain his vital signs: BP 85/45, HR 110, RR 24/minute, O2 saturation 98% on 2L/min per nasal cannula, and temperature 37.2 degrees Celsius. His lung sounds are clear, and his heart sounds are regular sinus rhythm. You notice his weight this morning was 205 pounds. You call the provider and receive orders for STAT basic metabolic panel and to initiate 0.9% Normal Saline IV fluids at 250 mL/hour until the provider arrives to evaluate the client.
The basic metabolic panel results (with the lab's normal reference range in parentheses) are as follows:
Sodium: 155 mEq/L (135-145)
Potassium: 3.3 mEq/L (3.5-5.3)
Chloride: 103 mEq/L (98-108)
Carbon dioxide: 25 mEq/L (23-27)
Blood urea nitrogen (BUN): 30 mg/dL (10-25)
Creatinine: 1.9 mg/dL (0.5-1.5)
Glucose: 100 mg/dL (fasting 70-99)
Questions
4. What is Mr. Smith’s fluid balance this morning? Support your answer with data.
5. What is the probable cause of his fluid balance?
6. Interpret Mr. Smith's lab results. What are the potential causes of these results?
7. Create a nursing diagnosis statement in PES format for Mr. Smith's current fluid status.
8. Create a new expected outcome in SMART format for Mr. Smith.
9. In addition to providing intravenous fluids, what additional interventions will you implement for Mr. Smith?
10. How will you evaluate if the nursing interventions are effective?
Scenario B
A 74-year-old male, Mr. M., was admitted to the general medical floor during the night shift with a diagnosis of pneumonia. See Figure 15.18 for an image of Mr. M.[6] He has a past medical history of alcohol abuse and coronary artery disease. You are the day shift nurse, and during your morning assessment, you notice that Mr. M. becomes increasingly lethargic and is not following commands consistently. You obtain the following vital signs: BP 80/45, HR 110, RR 8 and labored, O2 saturation 80% on 3L per nasal cannula, and temperature 38.1 degrees Celsius. His lung sounds reveal coarse crackles throughout, and you notice he is using accessory muscles with breathing. You notify the provider using an SBAR report and receive orders to increase oxygen to 10L per non-rebreather mask.

Lab results are ordered with the following results:
ABGs: pH 7.30, PaCO2 50, PaO2 59, HCO3 24, SaO2 80
Potassium: 5.9 mEq/L
Magnesium: 1.0 mEq/L
Calcium: 10.2 mg/dL
Sodium: 137 mEq/L
Hematocrit: 55%
Serum Osmolarity: 305 mmol/kg
BUN: 30 mg/dL
Urine Specific Gravity: 1.025
Questions
1. What is Mr. M.’s fluid balance? Provide data supporting the imbalance.
2. What is your interpretation of Mr. M.’s ABGs?
3. What is your interpretation of Mr. M.’s electrolyte studies?
4. Is Mr. M. stable or unstable? Why?
5. For what complications will you monitor?
6. Write an SBAR communication you would have with the health care provider to notify them about Mr. M.’s condition.
7. Create a NANDA-I diagnosis for Mr. M. in PES format.
8. Identify an expected outcome for Mr. M. in SMART format.
9. What interventions will you plan for Mr. M.?
10. How will you evaluate if your interventions are effective?
11. Write a nursing note about Mr. M.’s condition and your actions taken. This can be in the form of a DAR, SOAP, or summary nursing note.

Test your knowledge using this NCLEX Next Generation-style bowtie question. You may reset and resubmit your answers to this question an unlimited number of times.[7]

Test your knowledge using these NCLEX Next Generation-style questions. You may reset and resubmit your answers to the questions in this assignment an unlimited number of times.[8]
Active transport: Movement of solutes and ions across a cell membrane against a concentration gradient from an area of lower concentration to an area of higher concentration using energy during the process. (Chapter 15.2)
Chvostek’s sign: An assessment sign of acute hypocalcemia characterized by involuntary facial muscle twitching when the facial nerve is tapped. (Chapter 15.4)
Diffusion: The movement of solute particles from an area of higher concentration to an area of lower concentration. (Chapter 15.2)
Edema: Swelling caused by excessive interstitial fluid retention. (Chapter 15.2)
Extracellular fluids (ECF): Fluids found outside cells in the intravascular or interstitial spaces. (Chapter 15.2)
Filtration: Movement of fluids through a permeable membrane utilizing hydrostatic pressure. (Chapter 15.2)
Hydrostatic pressure: The pressure that a contained fluid exerts on what is confining it. (Chapter 15.2)
Hypercapnia: Elevated levels of retained carbon dioxide in the body. (Chapter 15.5)
Hypertonic solution: Intravenous fluids with a higher concentration of dissolved particles than blood plasma. (Chapter 15.3)
Hypervolemia: Excess intravascular fluid. Used interchangeably with “excessive fluid volume.” (Chapter 15.3)
Hypotonic solution: Intravenous fluids with a lower concentration of dissolved particles than blood plasma. (Chapter 15.3)
Hypovolemia: Intravascular fluid loss. Used interchangeably with “deficient fluid volume” and “dehydration.” (Chapter 15.2)
Interstitial fluids: Fluids found between the cells and outside of the vascular system. (Chapter 15.2)
Intracellular fluids (ICF): Fluids found inside cells consisting of protein, water, and electrolytes. (Chapter 15.2)
Intravascular fluids: Fluids found in the vascular system consisting of the body’s arteries, veins, and capillary networks. (Chapter 15.2)
Isotonic solution: Intravenous fluids with a similar concentration of dissolved particles as blood plasma. (Chapter 15.3)
Oncotic pressure: Pressure inside the vascular compartment created by protein content of the blood (in the form of albumin) that holds water inside the blood vessels. (Chapter 15.2)
Osmolality: Proportion of dissolved particles in a specific weight of fluid. (Chapter 15.2)
Osmolarity: Proportion of dissolved particles or solutes in a specific volume of fluid. (Chapter 15.2, Chapter 15.3)
Osmosis: Movement of fluid through a semipermeable membrane from an area of lesser solute concentration to an area of greater solute concentration. (Chapter 15.2)
Passive transport: Movement of fluids or solutes down a concentration gradient where no energy is used during the process. (Chapter 15.2)
Renin-Angiotensin-Aldosterone System (RAAS): A body system that regulates extracellular fluids and blood pressure by regulating fluid output and electrolyte excretion. (Chapter 15.2)
Transcellular fluid: Fluid in areas such as cerebrospinal, synovial, intrapleural, and gastrointestinal system. (Chapter 15.2)
Trousseau’s sign: A sign associated with hypocalcemia that causes a spasm of the hand when a blood pressure cuff is inflated. (Chapter 15.4)
Urine specific gravity: A measurement of hydration status that measures the concentration of particles in urine. (Chapter 15.6)
Active transport: Movement of solutes and ions across a cell membrane against a concentration gradient from an area of lower concentration to an area of higher concentration using energy during the process. (Chapter 15.2)
Chvostek’s sign: An assessment sign of acute hypocalcemia characterized by involuntary facial muscle twitching when the facial nerve is tapped. (Chapter 15.4)
Diffusion: The movement of solute particles from an area of higher concentration to an area of lower concentration. (Chapter 15.2)
Edema: Swelling caused by excessive interstitial fluid retention. (Chapter 15.2)
Extracellular fluids (ECF): Fluids found outside cells in the intravascular or interstitial spaces. (Chapter 15.2)
Filtration: Movement of fluids through a permeable membrane utilizing hydrostatic pressure. (Chapter 15.2)
Hydrostatic pressure: The pressure that a contained fluid exerts on what is confining it. (Chapter 15.2)
Hypercapnia: Elevated levels of retained carbon dioxide in the body. (Chapter 15.5)
Hypertonic solution: Intravenous fluids with a higher concentration of dissolved particles than blood plasma. (Chapter 15.3)
Hypervolemia: Excess intravascular fluid. Used interchangeably with “excessive fluid volume.” (Chapter 15.3)
Hypotonic solution: Intravenous fluids with a lower concentration of dissolved particles than blood plasma. (Chapter 15.3)
Hypovolemia: Intravascular fluid loss. Used interchangeably with “deficient fluid volume” and “dehydration.” (Chapter 15.2)
Interstitial fluids: Fluids found between the cells and outside of the vascular system. (Chapter 15.2)
Intracellular fluids (ICF): Fluids found inside cells consisting of protein, water, and electrolytes. (Chapter 15.2)
Intravascular fluids: Fluids found in the vascular system consisting of the body’s arteries, veins, and capillary networks. (Chapter 15.2)
Isotonic solution: Intravenous fluids with a similar concentration of dissolved particles as blood plasma. (Chapter 15.3)
Oncotic pressure: Pressure inside the vascular compartment created by protein content of the blood (in the form of albumin) that holds water inside the blood vessels. (Chapter 15.2)
Osmolality: Proportion of dissolved particles in a specific weight of fluid. (Chapter 15.2)
Osmolarity: Proportion of dissolved particles or solutes in a specific volume of fluid. (Chapter 15.2, Chapter 15.3)
Osmosis: Movement of fluid through a semipermeable membrane from an area of lesser solute concentration to an area of greater solute concentration. (Chapter 15.2)
Passive transport: Movement of fluids or solutes down a concentration gradient where no energy is used during the process. (Chapter 15.2)
Renin-Angiotensin-Aldosterone System (RAAS): A body system that regulates extracellular fluids and blood pressure by regulating fluid output and electrolyte excretion. (Chapter 15.2)
Transcellular fluid: Fluid in areas such as cerebrospinal, synovial, intrapleural, and gastrointestinal system. (Chapter 15.2)
Trousseau’s sign: A sign associated with hypocalcemia that causes a spasm of the hand when a blood pressure cuff is inflated. (Chapter 15.4)
Urine specific gravity: A measurement of hydration status that measures the concentration of particles in urine. (Chapter 15.6)

