22.1 General Survey Introduction
Open Resources for Nursing (Open RN)
Learning Objectives
- Perform a general survey assessment, including vital signs, ability to communicate, appropriateness of behaviors and responses, general mobility, and basic nutritional and fluid status
- Modify assessment techniques to reflect variations across the life span, cultural values and beliefs, and gender expression
- Document actions and observations
- Recognize and report significant deviations from norms
“Learn to see, learn to hear, learn to feel, learn to smell, and know that by practice alone can you become expert.”[1]
This quote provides a good description of learning how to perform a general survey assessment. A general survey assessment is a component of a patient assessment that observes the entire patient as a whole. General surveys begin with the initial patient contact and continue throughout the helping relationship. In this instance, observation includes using all five senses to gather cues. Nurses begin assessing patients from the moment they meet them, noting their appearance, posture, gait, verbal communication, nonverbal communication, and behaviors. Cues obtained during a general survey assessment are used to guide additional focused assessments in areas of concern.
Introduction to the Nursing Process
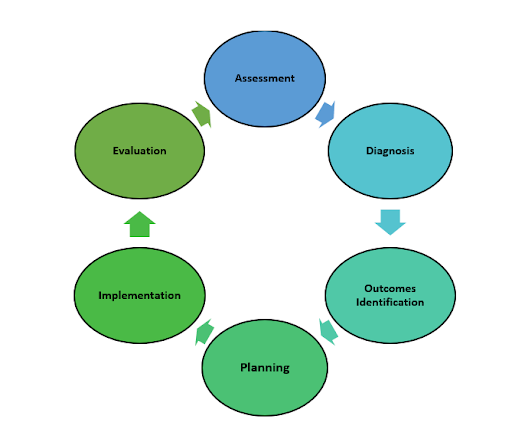
Before discussing the components of a general survey, it is important to understand how assessment fits under the standards for professional nursing practice established by the American Nurses Association (ANA). These standards are the foundation of the nursing profession and include duties that all registered nurses, regardless of role or specialty, are expected to perform competently.[2] There are six components of the nursing process: Assessment, Diagnosis, Outcomes Identification, Planning, Implementation, and Evaluation. See Figure 1.1[3] for an illustration of the nursing process. The mnemonic ADOPIE is an easy way to remember the ANA Standards and the nursing process. The nursing process is a continuous, cyclic process that is constantly adapting to the patient’s current health status. This textbook contains several chapters pertaining to techniques used during the assessment phase of the nursing process.
Read more about the “Nursing Process” in the Open RN Nursing Fundamentals textbook.
Assessment
According to the ANA, assessment includes collecting “pertinent data, including but not limited to, demographics, social determinants of health, health disparities, and physical, functional, psychosocial, emotional, cognitive, sexual, cultural, age-related, environmental, spiritual/transpersonal, and economic assessments in a systematic, ongoing process with compassion and respect for the inherent dignity, worth, and unique attributes of every person.”[4]
Patient data is considered either subjective or objective, and it can be collected from multiple sources.
Subjective Assessment Data
Subjective data is information obtained from the patient and/or family members and offers important cues from their perspectives. When documenting subjective data, it should be in quotation marks and start with verbiage such as, “The patient reports…” or “The patient’s wife states…” It is vital for the nurse to establish rapport with a patient to obtain accurate, valuable subjective data regarding the mental, emotional, and spiritual aspects of their condition.
Example. An example of documented subjective data obtained from a patient assessment is, “The patient reports pain severity of 2 on a 0-10 scale.” Additionally, if you create an inference, then that data is considered subjective. For example, documenting an inference, such as “The patient appears anxious,” is subjective data.
There are two types of subjective information, primary and secondary. Primary data is information provided directly by the patient. Patients are the best source of information about their bodies and feelings, and the nurse who actively listens to a patient will often learn valuable information while also promoting a sense of well-being. Information collected from a family member, chart, or other sources is known as secondary data. Family members can provide important information, especially for infants and children or when the patient is unable to speak for themselves.
Objective Assessment Data
Objective data is anything that you can observe through your senses of hearing, sight, smell, and touch while assessing the patient. Objective data is reproducible, meaning another person can easily obtain the same data. Examples of objective data are vital signs, physical examination findings, and laboratory results.
Example. An example of documented objective data is, “The patient’s radial pulse is 58 and regular, and their skin feels warm and dry.”
Sources of Assessment Data
Assessment data is collected in three ways: during a focused interview, during physical examination, or while reviewing laboratory and diagnostic test results.
Interviewing
Interviewing includes asking the patient questions, listening, and observing verbal and nonverbal communication. Reviewing the chart prior to interviewing the patient eliminates redundancy in the interview process and allows the nurse to hone in on the most significant areas of concern or need for clarification. However, if information in the chart does not make sense or is incomplete, the nurse should use the interview process to verify data with the patient.
When beginning an interview, it may be helpful to start with questions related to the patient’s medical diagnoses to gather information about how they have affected the patient’s functioning, relationships, and lifestyle. Listen carefully and ask for clarification when something isn’t clear to you. Patients may not volunteer important information because they don’t realize it is important for their care. By using critical thinking and active listening, you may discover valuable cues that are important to provide safe, quality nursing care. Sometimes nursing students can feel uncomfortable with having difficult conversations or asking personal questions because of generational or other differences. Don’t shy away from asking about information that is important to know for safe patient care. Most patients will be grateful that you cared enough to ask and listen.
Be alert and attentive to how the patient answers questions, as well as when they do not answer a question. Nonverbal communication and body language can be cues to important information that requires further investigation. A keen sense of observation is important. To avoid making inappropriate inferences, the nurse should validate any cues. For example, a nurse may make an inference that a patient is depressed when the patient avoids making eye contact during an interview. However, upon further questioning, the nurse may discover that the patient’s cultural background believes direct eye contact to be disrespectful and this is why they are avoiding eye contact.
Read more information about communicating with patients in the “Communication” chapter of the Open RN Nursing Fundamentals book.
Physical Examination
Physical examination is a systematic data collection method of the body that uses the techniques of inspection, auscultation, palpation, and percussion. Inspection is the observation of a patient’s anatomical structures. Auscultation is listening to sounds, such as heart, lung, and bowel sounds, created by organs using a stethoscope. Palpation is the use of touch to evaluate organs for size, location, or tenderness. Percussion is an advanced physical examination technique where body parts are tapped with fingers to determine their size and if fluid is present. See Figure 1.2[5] for an image of a nurse performing a physical examination.

Registered Nurses (RNs) complete a physical examination and analyze the findings as part of the nursing process. Collection of physical examination data can be delegated to Licensed Practical Nurses/Licensed Vocational Nurses (LPNs/LVNs), or measurements such as vital signs and weight may be delegated to Unlicensed Assistive Personnel (UAP) when it is appropriate to do so. However, the RN remains responsible for analyzing the findings.
Assessment data is documented in the patient’s electronic medical record (EMR), an electronic version of the patient’s paper medical chart.
Reviewing Laboratory and Diagnostic Test Results
Reviewing laboratory and diagnostic test results is an important component of the assessment phase of the nursing process and provides relevant and useful information related to the needs of the patient. Understanding how normal and abnormal results affect patient care is important when implementing the nursing care plan and administering prescriptions.
Read more about interpreting laboratory and diagnostic testing results based on nursing concepts in the Open RN Nursing Fundamentals textbook.
- Dallas Hall, W. (1990). Chapter 209: An overview of the general examination. In Walker, H. K., Hall, W. D., Hurst, J. W. (Eds.), Clinical methods: The history, physical, and laboratory examinations (3rd ed.). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK706/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- "The Nursing Process” by Kim Ernstmeyer at Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- “13394660711603.jpg” by CDC/Amanda Mills is in the Public Domain. ↵
Fluids found outside cells in the intravascular or interstitial spaces.
A localized pathogen that spreads to a secondary location.
Answer Key to Chapter 23 Critical Thinking Activities
1. Correct Order: 2 - Stop the IV infusion, 1 - Discontinue the IV, 3 - Elevate the affected side, 4 - Document the findings
Answers to interactive elements are given within the interactive element.
This is where you can add appendices or other back matter.
An infection that becomes disseminated throughout the body.
Checklists
Checklist for Handwashing
- Use the checklist below to review the steps for completion of "Hand Hygiene With Soap and Water."
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Remove jewelry according to agency policy; push your sleeves above your wrists.
- Turn on the water and adjust the flow so that the water is warm. Wet your hands thoroughly, keeping your hands and forearms lower than your elbows. Avoid splashing water on your uniform.
- Apply a palm-sized amount of hand soap.
- Perform hand hygiene using plenty of lather and friction for at least 15 seconds:
- Rub hands palm to palm
- Back of right and left hand (fingers interlaced)
- Palm to palm with fingers interlaced
- Rotational rubbing of left and right thumbs
- Rub your fingertips against the palm of your opposite hand
- Rub wrists
- Repeat sequence at least 2 times
- Keep fingertips pointing downward throughout
- Clean under your fingernails with disposable nail cleaner (if applicable).
- Wash for a minimum of 20 seconds.
- Keep your hands and forearms lower than your elbows during the entire washing.
- Rinse your hands with water, keeping your fingertips pointing down so water runs off your fingertips. Do not shake water from your hands.
- Do not lean against the sink or touch the inside of the sink during the hand-washing process.
- Dry your hands thoroughly from your fingers to wrists with a paper towel or air dryer.
- Dispose of the paper towel(s).
- Use a new paper towel to turn off the water.
- Dispose of the paper towel.
Checklist for using Hand Sanitizer
- Use the checklist below to review the steps for completion of "Hand Hygiene With Alcohol-Based Hand Sanitizer."
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
-
- Gather supplies (antiseptic hand rub).
- Remove jewelry according to agency policy; push your sleeves above your wrists.
- Apply enough product into the palm of one hand and enough to cover your hands thoroughly, per product directions.
- Rub your hands together, covering all surfaces of your hands and fingers with antiseptic until the alcohol is dry (a minimum of 20-30 seconds):
- Rub hands palm to palm
- Back of right and left hand (fingers interlaced)
- Palm to palm with fingers interlaced
- Rotational rubbing of left and right thumbs
- Rub your fingertips against the palm of your opposite hand
- Rub your wrists
- Repeat hand sanitizing sequence a minimum of two times.
- Repeat hand sanitizing sequence until the product is dry.
Checklist for Vital Signs
(See “Blood Pressure” chapter for Manual Blood Pressure Checklist)
- Knock, enter the room, greet the patient, and provide for privacy.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Perform hand hygiene and clean the stethoscope before approaching the patient.
- Ask the patient their name and date of birth for the first identifier and verify wristband while the patient is stating information. Then use one of the following for the second identifier:
- Scan wristband
- Compare name/DOB to MAR
- Ask staff to verify patient (LTC setting)
- Compare picture on MAR to patient
- Explain the procedure to the patient; ask if they have any questions.
- Obtain temperature using correct technique in Celsius. Inform instructor if temperature is out of range. Normal range: 98.6 F or 37 C.
- Obtain accurate pulse using radial artery. Inform instructor if pulse is out of range. Normal range for a pulse in an adult: 60-100 with regular rhythm.
- Obtain accurate respiratory rate over 60 seconds. Inform instructor if respiratory rate is out of range. Normal range for respiratory rate in an adult: 12-20.
- Obtain oxygen saturation reading (SpO2) using a pulse oximeter. Inform instructor if SpO2 is out of range. Normal range for SpO2: 94-100%.
- Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Perform hand hygiene and clean the stethoscope.
- Follow the agency policy for following up on vital signs outside of normal range.
- Document vital signs.
| Name | Classification | Description | Indication for Use | Instruction for Use | Other |
|---|---|---|---|---|---|
| Duoderm | Hydrocolloid | Contains gel-forming agents, impermeable to outside contaminants, promotes autolysis, reduces pain, and promotes moist wound healing. | Partial or full-thickness wounds; may be used to hold other dressing in place; avoid use with infections or diabetes. | Cleanse wound. Select dressing 1-2 inches larger than wound, apply light pressure to allow body heat to promote adhesion, change 3-5 days and PRN. | Watch for moisture buildup and odor. |
| Tegaderm | Transparent film | Permeable to oxygen and water vapor, protects from environmental contaminants, nonabsorbent, “second skin.” | PICC/IV site covers, dry wounds, contains moisture in wound when desired. | Cleanse wound. Use skin sealant around edges to hold firm. Change 4-7 days. | Use adhesive remover to remove and protect from skin tears in the elderly. |
| Steri-Strip | Adhesive | Surgical tape. | May be used for linear wound closure or placement after removal of staples or sutures on surgical wounds. | Apply adhesive sealant prior to application.
Apply perpendicular to wound edges to promote closure. |
|
| Tubigrip | Compression wrap/skin cover | Woven elastic fabric. | May be used as compression wrap or protection of skin. | Sizes vary from infant to body wrap. | When used as compression, double layer provides low end compression 15-20mm Hg. |
| Vaseline Gauze | Occlusive gauze | Woven gauze impregnated with petroleum. | May be used as a nonadherent dressing or to keep wounds moist. | Frequent changes.
Cleanse wound prior to each application. |
Watch for bacteria buildup and odor. |
| Xeroform Gauze | Occlusive gauze | Petrolatum impregnated gauze dressing with 3% bismuth tribromophenate. | The bismuth tribromophenate works to reduce wound odor easily.
It also has a nonsticking surface and protects the wound from contamination. Used for surgical incisions, donor sites, skin grafts, and first- and second- degree burns. |
Cleanse wound prior to placement.
Place dressing directly over wound. Cover with appropriate cover/ secondary dressing. |
Helps minimize bacterial buildup. |
| Coban | Elastic wrap | Sticks to itself without need for adhesive, pins, or clips. Wrap stays in place and is lightweight, porous, and comfortable for patients. Reduces pain. | Can be used as compression wrap. Holds primary dressing in place. Can be used to protect skin or medical device. | If using wrap as compression, verify pulse first.
Do not apply compression to infected area or exposed bone/organ. |
Do not tape to skin.
If used as compression, check pulse regularly. May be left in place up to 7 days. |
| Iodosorb Gel | Fiber gel | Absorbing fluids; removing exudate slough, and debris; and forming a gel over the wound surface. As the gel absorbs exudate, iodine is released, killing bacteria and changing color as the iodine is used up. | For use in cleaning wet ulcers and wounds such as venous stasis ulcers, pressure injuries, diabetic foot ulcers, and infected traumatic and surgical wounds. | Cleanse wound. Squeeze gel in shape of wound onto sterile gauze, apply to wound, and hold with secondary dressing. | May be used to eliminate pseudomonas bacteria.
Verify allergies prior to use. |
| 2"x2" Gauze | Gauze | Wound cover. | Cleaning and coverage. | Apply to wound and tape. | Avoid applying tape to skin. |
| 3"x3” 4-ply Nonwoven | Gauze | Wound cover. | Cleaning and coverage. | Apply to wound and tape. | Avoid applying tape to skin. |
| 4"x4” 8-ply Gauze Sponge | Gauze | Wound cover. | Cleaning, coverage, and wet-to-dry. | Apply to wound and tape. | Avoid applying tape to skin. |
| 4"x4” 6-ply Drain Sponge | Gauze | Wound cover, trachea, PEG tube, drain cover/protection. | Use to surround trachea, drain, and PEG tube for protection and drainage absorption. | Cleanse area surrounding tube; apply surrounding the drain site top and bottom. | If applying tape to hold, use minimal tape to protect skin upon removal. |
| 6"x6” Super Sponge (“fluff”) | Gauze | Woven-layered, super absorbent for moderate to large drainage. | Wound cover drainage collection and wet-to-dry. | Cleanse wound. Apply and change as prescribed and wound drainage dictates. | Do not allow drainage-filled gauze to remain on wound surface for extended periods. Promotes bacteria and infection. |
| Abdominal Pad | Gauze | Absorbent of a soft nonwoven outer layer that quickly wicks fluid to a cellulose center. Cellulose quickly absorbs and disperses fluids laterally to prevent pooling. | Wound cover and heavy drainage collection. Keeps moisture off skin. Similar to incontinent pad. | Cleanse wound. Apply as prescribed and wound drainage dictates. | Do not allow drainage-filled pad to remain on wound surface for extended periods. Promotes bacteria and infection. |
| Optilock | Polymer | Super-absorbent polymer core locks in drainage under compression.
Adjusts absorption to the amount of drainage. Protects skin from maceration. Nonadherent wound contact layer. |
Pressure injuries, partial and full-thickness wounds, leg ulcers, lacerations and abrasions, and wounds under compression. | Cleanse wound. Apply to wound bed, and hold in place with tape, wrap, etc.
May be left in place up to 7 days if drainage is minimal. |
Do not allow drainage-filled pad to remain on wound surface for extended periods. Promotes bacteria and infection. |
| Kerlix 4” 6-ply Gauze Roll | Gauze | Prewashed, fluff-dried 100% woven gauze with crinkle-weave pattern for loft and bulk. Provides fast-wicking action, aeration, and absorbency. Comes in large variety of sizes. | Wound cover, wound packing, skin wrap protection, and wet-to-dry. | Cleanse wound and apply. | Change as prescribed. Do not allow drainage-filled gauze to remain on wound surface for extended periods. Promotes bacteria and infection. |
| 4” Stretch Bandage (“Kling”) | Gauze | Nonsterile absorbent gauze roll and stretches and conforms to the body shape and clings to itself as it is wrapped. Conforms to the wound area and offers flexibility to allow for body movement. | May be used to hold dressings in place or wrap for skin protection. | Apply as needed. | Avoid applying tape to skin. Apply tape to Kling to hold.
Comes in large variety of sizes. |
| Adaptic | Contact layer | Nonadhering dressing, primary wound contact dressing designed to minimize wound adherence and prevent maceration. Mesh impregnated with a specially formulated petroleum emulsion, and easy to remove and minimizes pain. | Dry to heavily exuding wounds for which adherence of dressing and exudate is to be prevented. | Cleanse wound. Apply to wound, apply primary dressing, and hold with appropriate dressing or tape. | May be used as a contact layer with wound VAC foam or cover skin tears. |
| Telfa | Composite | Made of cotton fabric with a perforated seal of polyester resin. This perforated seal acts as a nonadherent, preventing the dressing from sticking to the wound and/or acting as a barrier between the wound and excretions. | Covers cuts and abrasions. It is also used to prevent infection to sutured wounds and as an absorbent dressing for wound secretions. | Cleanse wound and apply as primary or secondary (contact) layer.
May be used with topical medications. |
Change daily or when saturated. |
| ¼” Plain Packing Strip | Gauze | 100% cotton, fine mesh gauze ideal for wet-to-dry packing.
Available in plain and iodoform (antiseptic). |
Used for packing or as drainage conduits in nasal, sinus, or tunnel packing. | Cleanse wound. Apply as packing or filler in wound tunnel, nasal passage, or sinus cavity. | Change daily or as prescribed.
Do not cut in small pieces to avoid not being able to locate them for removal. |
| Aquacel Ag (also comes as plain hydrofiber with no additives) | Hydrofiber | Primary wound dressing made from sodium carboxymethylcellulose. Textile fiber and presented in the form of fleece held together by a needle bonding process and is available both as a "ribbon” for packing cavities and as a flat nonwoven pad for application to larger open wounds. Fiber turns to gel when moistened by drainage. | Primary wound dressing to absorb large amounts of drainage. Silver component is antimicrobial. The dressing is easy to remove without causing pain or trauma and leaves minimal residue on the surface of the wound. | Cleanse wound. Apply to surface or lightly pack into wound.
Cover with secondary dressing. |
Some patients may be sensitive to silver.
Silver must remain in place for at least 24 hours to be effective. Change frequency as prescribed by physician. |
| Hydrofera Blue | Antimicrobial foam | Pulls bacteria-laden exudate up and away from the wound, which may facilitate healing. Provides a protective antibacterial cover that inhibits the growth of microorganisms. Foam impregnated with methylene blue. | Pressure injuries, diabetic ulcers, venous stasis ulcers, arterial ulcers, superficial burns, donor sites, post-surgical incisions, trauma wounds, abrasions, and lacerations. | Cleanse wound.
Moisten foam with saline or sterile water. Ring out excess moisture. Apply to wound and hold with occlusive cover (Tegaderm, Duoder). |
Hydrofera Blue foam is effective against microorganisms commonly found in wounds, including MRSA, VRE, and Candida. |
| Polymem (Pink)
Polymem (Silver) |
Foam | Polymem contains a mild, nonionic, nontoxic, tissue-friendly cleansing agent, activated by moisture that is gradually released into the wound bed.
Built-in cleansing capabilities reduce the need to cleanse wounds during dressing changes, which can disrupt the growth of healthy tissue as the wounds heals. Wicks away up to ten times its weight in exudate. The absorption capability activates only if the material detects exudate. Nonstick surface to reduce pain and tissue loss during removal. |
Wounds with small to moderate drainage.
Pressure injuries, diabetic ulcers, venous stasis ulcers, arterial ulcers, superficial burns, donor sites, post-surgical incisions, trauma wounds, abrasions, and lacerations. |
Cleanse wound. Place uncut foam directly on wound. Hold with nonocclusive dressing to allow for moisture evaporation.
May use Kerlix, Kling, or Tubigrip to hold in place. |
May be changed daily or weekly depending on drainage amount.
Silver is most effective when left in place > 24 hours. Some patients complain of pain with use of silver. |
| Aquacel Ag Foam | Foam | Absorbs wound fluid and creates a soft gel, maintaining a moist wound environment. Locks in exudates through vertically wicking, reducing the risk of maceration. Helps minimize pain while in place and during dressing changes. | Wounds with small to moderate drainage. Pressure injuries, diabetic ulcers, venous stasis ulcers, arterial ulcers, superficial burns, donor sites, post-surgical incisions, trauma wounds abrasions, and lacerations. | Cleanse wound. Place uncut foam directly on wound. Hold with nonocclusive dressing to allow for moisture evaporation.
May use Kerlix, Kling, or Tubigrip to hold in place. |
May be changed daily or weekly depending on drainage amount.
Sliver is most effective when left in place > 21 hours. Some patients complain of pain with use of silver. |
| Lyofoam | Foam | Management of moderately to highly exuding wounds. Its high absorbency and fluid-handling capacity, combined with the reduced risk of maceration and leakage, provide a longer wear time. Waterproof backing film acts as a barrier to bacterial and viral penetration. Works under compression. | Moderate to heavy draining wounds. Pressure injuries, diabetic ulcers, venous stasis ulcers, arterial ulcers, superficial burns, donor sites, post-surgical incisions, trauma wounds, abrasions, and lacerations. | Cleanse wound. Place uncut foam directly on wound. Hold with nonocclusive dressing to allow for moisture evaporation.
May use Kerlix, Kling, or Tubigrip to hold in place. |
Monitor dressing frequently and change when saturated with drainage. |
| Mepilex Border | Foam | Absorbs and retains exudate and maintains a moist wound environment. The Safetac® layer seals the wound edges, preventing the exudate from leaking onto the surrounding skin, which minimizes the risk for maceration. The Safetac® layer ensures that the dressing can be changed without damaging the wound or surrounding skin or exposing the patient to additional pain. | For moderate to high exuding wounds, such as pressure injuries, leg and foot ulcers, traumatic wounds, and other secondary healing wounds.
May also be used for skin and pressure injury protection/prevention. |
Clean the wound prior to applying a dressing.
The dressing should overlap the wound bed by at least 2 cm onto the surrounding skin. |
Adhesive border is designed to be peeled back to view wound and reseal multiple times. Monitor wound frequently.
Comes in a variety of sizes. |
| Mepilex Border Ag | Foam | Silver has been added. Silver kills bacteria and might be used both for preventing infection and also on wounds with signs of local infection. The Safetac® layer ensures that the dressing can be changed without damaging the wound or surrounding skin or exposing the patient to additional pain. | For moderate to high exuding wounds, such as pressure injuries, leg and foot ulcers, traumatic wounds, and other secondary healing wounds. | Clean the wound prior to applying a dressing.
The dressing should overlap the wound bed by at least 2 cm onto the surrounding skin. |
Adhesive border is designed to be peeled back to view wound and reseal multiple times. Monitor wound frequently.
Comes in a variety of sizes. Mepilex surgical dressing has a super adhesive border and remains in place for 7-10 days. Some patients complain of pain with use of silver. |
| KCI Granufoam Black | Negative Pressure Wound Therapy (NPWT) | Promotes wound healing through Negative Pressure Wound Therapy (NPWT). This helps draw wound edges together, remove infectious materials, and actively promote granulation. By MD order. | Do not place foam dressings directly in contact with exposed blood vessels, anastomotic sites, organs, or nerves. | Detailed instruction for use available online at the myKCI website. | Consider pain control prior to application and removal. |
Head-to-Toe Assessment Checklist
This checklist is intended as a guide for a routine, general, daily assessment performed by an entry-level nurse during inpatient care. Students should use a systematic approach and include these components in their assessment and documentation. Assessment techniques should be modified according to life span considerations. Focused assessments should be performed for abnormal findings and according to specialty unit guidelines. Unanticipated findings should be reported per agency protocol with emergency assistance obtained as indicated.
- Gather supplies: stethoscope, penlight, watch with second hand, gloves, hand sanitizer, and wound measurement tool.
- Perform hand hygiene before providing care and clean stethoscope.
- Perform safety steps:
- Knock before entering the room.
- Check the room for transmission-based precautions.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Explain the process to the patient and ask if they have any questions.
- Be organized and systematic.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure the patient’s privacy and dignity.
- Identify the patient using two patient identifiers (e.g., name and date of birth).
- Perform a primary survey to ensure medical stability. Obtain emergency assistance if needed.
- Airway: Is the airway open? Is suctioning needed?
- Breathing: Is the patient breathing normally?
- Circulation: Are there any abnormal findings in the overall color and moisture of the patient’s skin (cyanosis, diaphoresis)?
- Mental Status: Is the patient responsive and alert?
- Perform a general survey while completing the head-to-toe assessment. Include general appearance, behavior, mood, mobility (i.e., balance and coordination), communication, overall nutritional status, and overall fluid status.
- Address patient needs before starting assessment (toileting, glasses, hearing aids, etc.).
- Evaluate chief concern using PQRSTU (i.e., ask the patient their reason for seeking/receiving care). Ask, “Do you have any concerns or questions you’d like to talk about before we begin?”
- Obtain and/or analyze vital signs. (Initiate emergency assistance as needed.)
- Evaluate for the presence of pain or other type of discomfort. If pain or discomfort is present, perform comprehensive pain assessment using PQRSTU.
- Perform a neuromuscular assessment:
- Perform a subjective assessment. Ask if headache, dizziness, weakness, numbness, tingling, or tremors are present. Inquire if the patient has experienced loss of balance, decreased coordination, previous falls, or difficulty swallowing. Be aware of previously diagnosed neuromuscular conditions and currently prescribed medications and how these impact your assessment findings.
- Assess level of consciousness and orientation to person, place, and time.
- Assess PERRLA using penlight.
- Assess motor strength and sensation:
- Bilateral hand grasps
- Upper strength and resistance
- Lower strength and resistance
- Sensation in extremities
- Note unanticipated neurological findings in symmetrical facial expressions, extremity movement, and speech and obtain emergency assistance as needed.
- Assess fall assessment risk per agency policy.
- Perform a focused assessment if neurological or musculoskeletal condition is present.
- Perform a basic head, neck, eye, and ear assessment:
- Perform a subjective assessment. Be aware of previously diagnosed head, neck, eye, or ear conditions and associated medications and how these impact your assessment findings.
- Ask if they are having any problems with their teeth or gums, and if this has impacted their ability to eat.
- Ask if they use glasses, hearing aids, or dentures.
- Ask if they have any difficulty seeing or blurred vision.
- Ask if they have trouble hearing or experience ringing in their ears.
- Inspect the external eye and the external ear. Inspect the oral cavity for lesions, tongue position, moisture, and oral health. Ask the patient to swallow their saliva and note any difficulty swallowing.
- Palpate the lymph nodes (per agency policy).
- Perform a subjective assessment. Be aware of previously diagnosed head, neck, eye, or ear conditions and associated medications and how these impact your assessment findings.
- Perform a cardiovascular system assessment:
- Perform a subjective assessment. Ask if they are having chest pain, shortness of breath, edema, palpitations, calf pain, or pain in their feet or lower legs when exercising. Be aware of previously diagnosed cardiovascular conditions and currently prescribed medications and how these impact your assessment findings.
- Inspect:
- The face, lips, and extremities for pallor or cyanosis.
- The neck for JVD in upright position or with head of bed at 30-45-degree angle.
- The bilateral upper and lower extremities for color, warmth, and sensation.
- The lower extremities for hair distribution, edema, and signs of deep vein thrombosis (DVT).
- Palpate:
- Palpate and compare the radial, brachial, dorsalis pedis, and posterior tibial pulses bilaterally. Note the presence and amplitude of pulses.
- Palate the nail beds for capillary refill.
- Auscultate:
- Auscultate with both the bell and the diaphragm of the stethoscope over the five auscultation areas of the heart. Note the rate and rhythm. Identify S1 and S2 and any unexpected findings (i.e., extra sounds or irregular rhythm).
- Measure the apical pulse for one minute.
- Perform a respiratory assessment:
- Perform a subjective assessment. Ask if they have shortness of breath or a cough. Ask if the cough is dry or productive. Ask if they smoke, and if so, what products, how many a day, and if they are interested in quitting. Be aware of previously diagnosed respiratory conditions and currently prescribed medications or treatments and how these impact your assessment findings.
- Inspect:
- Level of consciousness and for signs of irritability, restlessness, anxiety, or confusion.
- Breathing pattern, including rate, rhythm, effort, and depth of breathing. Note signs of difficulty breathing such as nasal flaring, use of accessory muscles, or pursed-lip breathing.
- Skin color of lips, face, hands and feet for cyanosis and pallor.
- Trachea (midline).
- Symmetrical chest movement.
- Auscultate lung sounds using stethoscope directly on the skin over anterior and posterior auscultation areas. Compare sounds from side to side and note any adventitious sounds such as rhonchi, crackles, wheezing, stridor, or pleural rub.
- If oxygen equipment is prescribed:
- Note if the patient is using oxygenation devices during the exam or on room air.
- If the patient is using an oxygenation device, document the name of device and current flow rate and/or fraction of inspired oxygen (FiO2).
- Inspect for signs of skin breakdown due to the use of oxygenation devices.
- If a tracheostomy is present, document the condition of the tracheostomy site and characteristics of sputum present.
- Perform an abdominal assessment:
- Perform a subjective assessment:
- Ask if the patient is having any abdominal pain, cramping, nausea, vomiting, constipation, loss of appetite, or difficulty swallowing. Inquire about the date of the last bowel movement, if there have been any changes in the pattern or consistency of the stool, and if any blood is present or dark stool. Be aware of previously diagnosed gastrointestinal or genitourinary conditions and currently prescribed medications and how these impact your assessment findings.
- Ask if the patient has pain or problems with urination or leakage of urine.
- Inspect the general contour and symmetry of the abdomen and for distension.
- Auscultate for bowel sounds over four quadrants for one minute, note any hypoactive, high-pitched sounds.
- Palpate lightly for tenderness and masses.
- Analyze weight trend and 24-hour input and output, as appropriate for patient status.
- If enteral tube is present, assess tube insertion site, tube placement, and amount of enteral feeding/fluids administered during your shift per agency policy.
- If an indwelling urinary catheter is present, assess urine output and urine characteristics. Document continued need for indwelling catheter per agency policy.
- If an ostomy is present, document the condition of stoma and peristomal skin. Document amount and characteristics of output during your shift.
- Perform a subjective assessment:
- Perform an integumentary assessment:
- Perform a subjective assessment. Ask if the patient has any skin concerns such as itching, rashes, or an unusual mole or lump. Be aware of previously diagnosed integumentary conditions and currently prescribed medications or treatments and how these impact your assessment findings.
- Inspect:
- Assess overall skin color and note pallor, cyanosis, jaundice, erythema, bruising, moisture, and turgor.
- If an intravenous site is present, assess the insertion site for redness, warmth, tenderness, or induration. If intravenous fluids and/or medications are infusing, document the type and amount of fluids during your shift per agency policy.
- Assess for skin breakdown in pressure points (behind ears, occipital area, elbows, sacrum, and heels).
- If a pressure injury is present, stage from 1 to 4.
- If a wound is present, perform a wound assessment.
- Palpate for temperature, moisture, and texture. If erythema or rashes are present, assess for blanching. If edema is present, document the depth of indentation and the time it takes to rebound to original position and grade on a scale from 1 to 4.
- When the assessment is completed, assist the patient back to a comfortable position. Thank them and ask if anything is needed before you leave the room.
- Ensure safety measures when leaving room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Remove any PPE before leaving the room. Perform hand hygiene and clean stethoscope.
- Document assessment findings and report unanticipated findings according to agency policy.
On the NCLEX-PN Test Plan, some nursing skills are referenced in Activity Statements under various Client Need Categories that are not included in this OER textbook because of its alignment with a specific WTCS nursing course. View the information below on the related content in the Open RN Nursing Advanced Skills OER textbook.
Additional Skills Addressed in NCLEX-PN Client Need Categories
Pharmacological Therapies
Reduction of Risk
- Perform an electrocardiogram (ECG)
- Perform venipuncture
- Maintain central venous catheter
- Insert, maintain, and remove nasogastric (NG) tubes
Physiological Adaptation
- Recognize abnormalities on client cardiac monitor strip
- Provide care for client drainage device (chest tube)
This section contains a master glossary of vocabulary terms used in this book and their location.
A
ABCDE: A mnemonic for assessing for melanoma developing in moles: Asymmetrical, Borders are irregular in shape, Color is various shades of brown or black, Diameter is larger than 6 mm., and the shape of the mole is Evolving. (Chapter 14.2)
Abduction: Joint movement away from the midline of the body. (Chapter 13.2)
Accessory muscles: Muscles other than the diaphragm and intercostal muscles that may be used for labored breathing. (Chapter 10.3)
Accommodation: The ability of the eye to adjust from near vision to far vision. Pupils constrict at near vision and dilate at far vision. (Chapter 6.5)
Acne: A skin disturbance that typically occurs on areas of the skin that are rich in sebaceous glands, such as the face and back. (Chapter 14.3)
Active range of motion: The degree of movement a patient can voluntarily achieve in a joint without assistance. (Chapter 13.4)
Activities of daily living: Daily basic tasks fundamental to everyday functioning (e.g., hygiene, elimination, dressing, eating, ambulating/moving). (Chapter 2.8)
Acute otitis media: The medical diagnosis for a middle ear infection. (Chapter 8.2)
Adduction: Joint movement toward the middle line of the body. (Chapter 13.2)
Affect: Outward display of one’s emotional state. A “flat” affect with little display of emotion is associated with depression. (Chapter 1.4)
AIDET: Mnemonic for introducing oneself in health care that includes Acknowledge, Introduce, Duration, Explanation, and Thank You. (Chapter 1.2)
Airborne precautions: Infection prevention and control interventions to be used in addition to standard precautions for diseases spread by airborne transmission, such as measles and tuberculosis. (Chapter 4.2)
Ampules: Small glass containers of liquid medication ranging from 1 mL to 10 mL sizes. (Chapter 18.2)
Angiogenesis: The development of new capillaries in a wound base. (Chapter 20.2)
Anosmia: Partial or complete loss of smell. This symptom can be related to underlying cranial nerve dysfunction or other nonpathological causes such as a common cold. (Chapter 6.5)
Apnea: Absence of respirations. (Chapter 10.3)
Apocrine sweat gland: Sweat glands associated with hair follicles in densely hairy areas that release organic compounds subject to bacterial decomposition causing odor. (Chapter 14.2)
Around the Clock (ATC) order: An order that reflects that medication should be administered at regular time intervals, such as every six hours, to maintain consistent levels of the drug in the patient’s bloodstream. (Chapter 15.2)
Arterial blood gas (ABG): A sample of arterial blood that measures the oxygen, carbon dioxide, and bicarbonate levels. (Chapter 11.2)
Arterial blood sampling: Blood is obtained via puncture into an artery by specially trained registered nurses and other health care personnel, such as respiratory therapists, physicians, nurse practitioners, and physician assistants. (Chapter 23.2)
Arterial ulcers: Ulcers caused by lack of blood flow and oxygenation to tissues and typically occur in the distal areas of the body such as the feet, heels, and toes. (Chapter 20.2)
Arthroplasty: Joint replacement surgery. (Chapter 13.3)
Arthroscopic surgery: A surgical procedure involving a small incision and the insertion of an arthroscope, a pencil-thin instrument that allows for visualization of the joint interior. Small surgical instruments are inserted via additional incisions to remove or repair ligaments and other joint structures. (Chapter 13.3)
Articular cartilage: Smooth, white tissue that covers the ends of bones where they come together at joints, allowing them to glide over each other with very little friction. Articular cartilage can be damaged by injury or normal wear and tear. (Chapter 13.2)
Asepsis: A state of being free of disease-causing microorganisms. (Chapter 4.3)
Aseptic non-touch technique: A standardized technique, supported by evidence, to maintain asepsis and standardize practice. (Chapter 4.3)
Aseptic technique (medical asepsis): The purposeful reduction of pathogen numbers while preventing microorganism transfer from one person or object to another. This technique is commonly used to perform invasive procedures, such as IV starts or urinary catheterization. (Chapter 4.3)
Aspiration pneumonia: A type of lung infection caused by material from the stomach or mouth inadvertently entering the lungs that can be life-threatening. (Chapter 7.3, Chapter 12.3)
Atelectasis: Alveoli or an entire lung is collapsed, allowing no air movement. (Chapter 10.3)
Atrial fibrillation: An irregular heartbeat that is often fast and increases the risk of heart attack or stroke. (Chapter 9.3)
Auricle: The large, fleshy structure of the ear on the lateral aspect of the head. (Chapter 8.2)
Auscultation: Listening to sounds, such as heart, lung, and bowel sounds, created by organs using a stethoscope. (Chapter 1.1)
B
Babinski response: A reflex demonstrated as fanning of 4 toes with great toe bending towards top of foot when object slid along sole of foot. Normal in children under 2. Older than 2 through adulthood, all five toes should curl downward. (Chapter 6.9)
Barrel-chested: An equal AP-to-transverse diameter that often occurs in patients with COPD due to hyperinflation of the lungs. (Chapter 10.3)
Belief: Something accepted as true with a sense of certainty. (Chapter 2.8)
Bladder scan: A bedside test using a noninvasive tool used to measure the volume of urine in the bladder. (Chapter 21.6)
Blanching: To make white or pale by applying pressure. (Chapter 9.3, Chapter 14.4)
Bleb: A small, raised circle that appears after administration of an intradermal medication indicating correct placement into the dermis. (Chapter 18.4)
Body image: A mental picture of one’s body related to appearance and function. (Chapter 2.8)
Body Mass Index (BMI): A standardized reference range to gauge a patient’s weight status. (Chapter 1.4)
Borborygmus: Hyperperistalsis, often referred to as “stomach growling.” (Chapter 12.3)
Bradypnea: Decreased respiratory rate or slow breath less than normal range according to the patient’s age. (Chapter 10.3)
Broca’s area: An area located in the frontal lobe that is responsible for the production of language and controlling movements responsible for speech. (Chapter 6.2)
Bronchial breath sounds: High-pitched hollow sounds heard over trachea and the larynx. (Chapter 10.3)
Bronchovesicular sounds: Mixture of low- and high-pitched sounds heard over major bronchi. (Chapter 10.3)
Bruit: A swishing sound heard upon auscultation. (Chapter 6.10, Chapter 9.3)
C
Candidiasis: A fungal infection often referred to as “thrush” when it occurs in the oral cavity in children. (Chapter 7.3)
Capillary blood testing: Blood collected from capillaries located near the surface of the skin. (Chapter 23.2)
Capillary refill: The time it takes for color to return after pressure is applied to tissue causing blanching. (Chapter 9.3)
Care partners: Family and friends who are involved in helping to care for the patient. (Chapter 2.2)
Catheter embolism: Occurs when a small part of the cannula breaks off and flows into the vascular system. (Chapter 23.4)
CAUTI: Catheter-associated urinary tract infection. (Chapter 21.3)
Central nervous system: The part of the nervous system that includes the brain (the interpretation center) and the spinal cord (the transmission pathway). (Chapter 6.2)
Central venous access device (CAVD): A type of vascular access that involves the insertion of a catheter into a large vein in the arm, neck, chest, or groin. (Chapter 23.2)
Cerebellum: The part of the brain that coordinates skeletal and smooth muscle movement and maintains equilibrium and balance. (Chapter 6.2)
Cerebral cortex: The cerebrum is covered by a wrinkled outer layer of gray matter. (Chapter 6.2)
Cerumen impaction: A buildup of earwax causing occlusion of the ear canal. (Chapter 8.2)
Chief complaint: The reason a patient is seeking health care during a visit to a clinic or on admission to a health care facility. (Chapter 2.5)
Cleft lip: A birth defect caused by a partial or complete failure of the right and left portions of the upper lip to fuse together, leaving a gap in the lip. (Chapter 7.3)
Cleft palate: A birth defect caused when two halves of the hard palate fail to completely come together and fuse at the midline, leaving a gap between them, and making it very difficult for an infant to generate the suckling needed for nursing. (Chapter 7.3)
Click: Clicking sound heard on auscultation of the precordium; often heard in patients with heart valve abnormalities. (Chapter 9.3)
Clubbing: A change in the configuration where the tips of the nails curve around the fingertips, usually caused by chronic low levels of oxygen in the blood. (Chapter 10.3, Chapter 11.2)
Clubfoot: A congenital condition that causes the foot and lower leg to turn inward and downward. (Chapter 13.3)
Colostomy: The colon is attached to a stoma to bypass the rectum and the anus. (Chapter 21.7)
Comatose: A decreased level of consciousness with a score of less than 8 on the Glasgow Coma Scale. (Chapter 6.4)
Concussion: A type of traumatic brain injury caused by a bump, blow, or jolt to the head or by a hit to the body that causes the head and brain to move rapidly back and forth. This sudden movement can cause the brain to bounce around or twist in the skull, creating chemical changes in the brain and damaging brain cells. (Chapter 7.3)
Conductive hearing loss: Hearing loss that occurs when something in the external or middle ear is obstructing the transmission of sound. (Chapter 8.2)
Congenital condition: A condition present at birth. (Chapter 13.3)
Conjunctiva: Inner surface of the eyelid. (Chapter 8.2)
Conjunctivitis: A viral or bacterial infection in the eye causing swelling and redness in the conjunctiva and sclera. (Chapter 8.2)
Contact precautions: Infection prevention and control interventions to be used, in addition to standard precautions, for diseases spread by contact with the patient, their body fluids, or their surroundings, such as C-diff, MRSA, VRE, and RSV. (Chapter 4.2)
Contracture: A fixed or permanent tightening of muscles, tendons, ligaments, or the skin that prevents normal movement of the body part. (Chapter 13.3)
Convergence: The action of both eyes moving inward as they focus on a close object using near vision. (Chapter 6.5)
Cornea: The transparent front part of the eye that covers the iris, pupil, and anterior chamber. (Chapter 8.2)
Coude catheter: A catheter specifically designed to maneuver around obstructions or blockages in the urethra such as with enlarged prostate glands in males. Coude originates from the French word that means “bend.” (Chapter 21.2)
Crackles: Also referred to as “rales”; sound like popping or crackling noises during inspiration. Associated with inflammation and fluid accumulation in the alveoli. (Chapter 10.3)
Cranium: Eight bones that protect the brain in the cranial cavity. (Chapter 7.2)
Crepitus: A crackling, popping noise heard on joint movement. It is considered normal when it is not associated with pain. (Chapter 10.3, Chapter 13.2)
Cultural safety: The creation of safe spaces for patients to interact with health professionals without judgment, racial reductionism, racialization, or discrimination. (Chapter 1.2, Chapter 2.2)
Cyanosis: Bluish discoloration of the skin, lips, and nail beds. It is an indication of decreased perfusion and oxygenation. (Chapter 9.3, Chapter 10.3, Chapter 11.2, Chapter 14.4)
D
Debridement: The removal of nonviable tissue in a wound. (Chapter 20.4)
Deep Vein Thrombosis (DVT): A blood clot that forms in a vein deep in the body. (Chapter 9.3)
Dehiscence: The separation of the edges of a surgical wound. (Chapter 20.2)
Deltoid: Commonly used for intramuscular vaccinations in adults because it has a triangular shape and is easy to locate and access. The injection site is in the middle of the deltoid muscle, about 1 to 2 inches below the acromion process. (Chapter 18.6)
Dermatome: An area of the skin that is supplied by a single spinal nerve. (Chapter 6.6)
Dermis: The inner layer of skin with connective tissue, blood vessels, sweat glands, nerves, hair follicles, and other structures. (Chapter 14.2)
Developmental stages: A person’s life span can be classified into nine categories of development, including Prenatal Development, Infancy and Toddlerhood, Early Childhood, Middle Childhood, Adolescence, Early Adulthood, Middle Adulthood, Late Adulthood, and Death and Dying. (Chapter 1.2)
Diabetic ulcers: Ulcers that typically develop on the plantar aspect of the feet and toes of patients with diabetes due to lack of sensation of pressure or injury. (Chapter 20.2)
Diaphoretic: Excessive, abnormal sweating. (Chapter 14.4)
Diastole: The phase between each contraction of the heart when the ventricles are filling with blood. (Chapter 3.2)
Diastolic blood pressure: The resting pressure of blood on the arteries between each cardiac contraction. (Chapter 3.2)
Dimensional analysis: Dimensional analysis is a problem-solving technique where measurements are converted to a different (but equivalent) unit of measure by multiplying with a fractional form of 1 to obtain a desired unit of administration. (Chapter 5.6)
Diplopia: Double vision (i.e., seeing two images of a single object). (Chapter 6.5)
Dislocation: A joint injury that forces the ends of bones out of position; often caused by a fall or a blow to the joint. (Chapter 13.3)
Distention: An expansion of the abdomen caused by the accumulation of air or fluid. Patients often report “feeling bloated.” (Chapter 12.3)
Doff: To take off or remove personal protective equipment, such as gloves or a gown. (Chapter 4.2)
Don: To put on equipment for personal protection, such as gloves or a gown. (Chapter 4.2)
Drop factor: The number of drops in one mL of solution when fluids or medications are administered using gravity IV tubing. (Chapter 5.14)
Droplet precautions: Infection prevention and control interventions to be used in addition to standard precautions; used for diseases spread by large respiratory droplets such as influenza, COVID-19, or pertussis. (Chapter 4.2)
Dry powder inhaler (DPI): An inhaler with medication provided in a powder form that is inhaled from the mouth into the lungs using a quick breath to activate the medication and move it into the lungs. An example of a DPI is tiotropium (Spiriva). (Chapter 16.2)
Ductus arteriosus: Shunt that connects the pulmonary artery and aorta in the developing fetus. (Chapter 9.3)
Dysphagia: Difficulty swallowing. (Chapter 6.10, Chapter 7.2, Chapter 7.3, Chapter 12.3, Chapter 15.2)
Dyspnea: A feeling of shortness of breath. (Chapter 9.3, Chapter 10.3, Chapter 11.2)
Dysuria: Painful urination. (Chapter 2.8, Chapter 12.3)
E
Ecchymosis: Bruising that occurs when small veins and capillaries under the skin break. (Chapter 14.4, Chapter 20.2)
Eccrine sweat gland: Sweat gland that produces hypotonic sweat for thermoregulation. (Chapter 14.2)
Edema: Swelling in tissues caused by fluid retention. (Chapter 9.3, Chapter 20.2)
Elimination: Refers to the removal of waste products through the urine and stool. (Chapter 2.8)
eMAR: Electronic medication administration record contained in a patient’s electronic chart. (Chapter 15.2)
Enhanced barrier precautions: An infection control intervention designed to reduce transmission of multidrug-resistant organisms (MDRO’S) in nursing homes. (Chapter 4.2)
Enteral medications: Medications that are administered directly into the gastrointestinal tract orally, rectally, or through a tube such as a nasogastric (NG) tube, nasointestinal (NI) tube, or percutaneous endoscopic gastrostomy (PEG) tube. (Chapter 15.1)
Enteral nutrition (EN): Nutrition provided directly into the gastrointestinal (GI) tract through an enteral tube that bypasses the oral cavity. (Chapter 17.2)
Epidermis: The thin, uppermost layer of skin. (Chapter 14.2)
Epiglottis: A flexible piece of cartilage that covers the opening of the trachea during swallowing to prevent ingested material from entering the trachea. (Chapter 7.2)
Epistaxis: Nosebleed. (Chapter 7.3)
Epithelialization: The development of new epidermis and granulation tissue. (Chapter 20.2)
Equivalency: Two values or quantities that are the same amount. For example, one cup is equivalent to eight ounces. (Chapter 5.4)
Erythema: Redness. (Chapter 14.4, Chapter 20.2, Chapter 20.3)
Eschar: Dark brown/black, dry, thick, and leathery dead tissue in a wound base that must be removed for healing to occur. (Chapter 20.2)
Eustachian tube: The tube connecting the middle ear to the pharynx that helps equilibrate air pressure across the tympanic membrane. (Chapter 8.2)
Extension: Joint movement causing the straightening of limbs (increase in angle) at a joint. (Chapter 13.2)
Extraocular muscles: Six muscles that control the movement of the eye within the orbit. Extraocular muscles are innervated by three cranial nerves, the abducens nerve, the trochlear nerve, and the oculomotor nerve. (Chapter 8.2)
Extravasation: The infiltration of damaging intravenous medications, such as chemotherapy, into the extravascular tissue around the site of infusion, causing tissue injury and possible necrosis. (Chapter 23.4)
Exudate: Fluid that oozes out of a wound; also commonly called pus. (Chapter 20.2)
F
Facial drooping: An asymmetrical facial expression that occurs due to damage of the nerve innervating a particular part of the face. (Chapter 7.2)
Family dynamics: Patterns of interactions between family members that influence family structure, hierarchy, roles, values, and behaviors. (Chapter 1.4)
Fenestrated cannula: Type of tracheostomy tube that contains holes so the patient can speak if the cuff is deflated and the inner cannula is removed. (Chapter 22.2)
15-15 Rule: A rule in an agency’s hypoglycemia protocols that includes providing 15 grams of carbohydrate, and then repeating the blood glucose reading in 15 minutes, and then repeating as needed until the patient’s blood glucose reading is above 70. (Chapter 19.2)
FiO2: Fraction of inspired oxygen (i.e., the concentration of oxygen inhaled). Room air contains 21% oxygen levels, and oxygenation devices can increase the inhaled concentration of oxygen up to 100%. However, FiO2 levels should be decreased as soon as feasible to do so to prevent lung injury. (Chapter 11.2)
First-degree burn: A superficial burn that affects only the epidermis. (Chapter 14.3)
Five moments of hand hygiene: Hand hygiene should be performed during the five moments of patient care: immediately before touching a patient; before performing an aseptic task or handling invasive devices; before moving from a soiled body site to a clean body site on a patient; after touching a patient or their immediate environment; after contact with blood, body fluids, or contaminated surfaces (with or without glove use); and immediately after glove removal. (Chapter 4.2)
Flange: The end of the tracheostomy tube that is placed securely against the patient’s neck. (Chapter 22.2)
Flexion: Joint movement causing the bending of the limbs (reduction of angle) at a joint. (Chapter 13.2)
Fluid volume overload (hypervolemia): A condition when there is too much fluid in the blood. Patients may present with shortness of breath, edema to the extremities, and weight gain. (Chapter 23.2)
Foot drop: The inability to raise the front part of the foot due to weakness or paralysis of the muscles that lift the foot. (Chapter 13.3)
Fourth-degree burn: Severe burn damaging the dermis and the underlying muscle and bone. (Chapter 14.3)
Fracture: A broken bone. (Chapter 13.3)
Functional health: The patient’s physical and mental capacity to participate in activities of daily living (ADLs) and instrumental activities of daily living (IADLs). (Chapter 2.8)
G
Gastric residual volume (GRV): Stomach contents aspirated with a 60-mL syringe, typically performed for patients receiving enteral feeding to assess aspiration risk with associated interventions such as slowing or stopping tube feeding. GRVs in the range of 200–500 mL should raise concern and lead to the implementation of measures to reduce risk of aspiration. (Chapter 17.2)
Gauge: Refers to the diameter of a needle. Gauges can vary from very small diameter (25 to 29 gauge) to large diameter (18 to 22 gauge). (Chapter 18.2)
Gender expression: Characteristics in appearance, personality, and behavior, culturally defined as masculine or feminine. (Chapter 2.8)
Gender identity: One’s basic sense of being male, female, or other gender. (Chapter 2.8)
General survey assessment: A component of a patient assessment that observes the entire patient as a whole. Observation includes using all five senses to gather cues that provide a guideline for additional focused assessments in areas of concern. (Chapter 1.1)
Goiter: An abnormal enlargement of the thyroid gland that can occur with hypothyroidism or hyperthyroidism. (Chapter 7.3)
Gout: A type of arthritis that causes swollen, red, hot, and stiff joints due to the buildup of uric acid, commonly starting in the big toe. (Chapter 13.3)
Granulation tissue: New connective tissue in a wound base with fragile, thin-walled capillaries that must be protected. (Chapter 20.2)
Guarding: Voluntary contraction of abdominal wall musculature; may be related to fear, anxiety, or presence of cold hands. (Chapter 12.3)
H
Hand hygiene: A way of cleaning one’s hands to substantially reduce the number of pathogens and other contaminants (e.g., dirt, body fluids, chemicals, or other unwanted substances) to prevent disease transmission or integumentary harm, typically using soap, water, and friction. An alcohol-based hand rub solution may be appropriate hand hygiene for hands not visibly soiled. (Chapter 4.1)
HCO3: Bicarbonate level reflected in arterial blood gas results. Normal range is 22-26 meq/L. (Chapter 11.2)
Healthcare-Associated Infections (HAIs): Unintended infections caused by care received in a health care setting. (Chapter 4.1)
Health history: The process of using directed interview questions to obtain symptoms and perceptions about a patient’s illness or life condition. The purpose of obtaining a health history is to gather subjective data from the patient and/or the patient’s family so that the health care team and the patient can collaboratively create a plan that will promote health, address acute health problems, and minimize chronic health conditions. (Chapter 2.1)
Heave or lift: Palpable lifting sensation under the sternum and anterior chest wall to the left of the sternum; it suggests severe right ventricular hypertrophy. (Chapter 9.3)
Hematemesis: Blood-tinged mucus secretions from the lungs. (Chapter 12.3)
Hematochezia: Passage of bloody stool. (Chapter 12.3)
Hematoma: An area of blood that collects outside of larger blood vessels. (Chapter 7.2, Chapter 20.2)
Hemoptysis: Blood-tinged mucus secretions from the lungs. (Chapter 10.3)
Hemosiderin staining: Dark-colored discoloration of the lower legs due to blood pooling. (Chapter 20.2)
Hemostasis phase: The first phase of wound healing that occurs immediately after skin injury. Blood vessels constrict and clotting factors are activated. (Chapter 20.2)
Hyperactive bowel sounds: Increased peristaltic activity; may be related to diarrhea, obstruction, or digestion of a meal. (Chapter 12.3)
Hypercapnia: Elevated carbon dioxide levels in the blood, indicated by PaCO2 level greater than 45 in an ABG test. (Chapter 10.3, Chapter 11.2)
Hyperglycemia: Elevated blood glucose reading with associated signs and symptoms such as frequent urination and increased thirst. (Chapter 19.2)
Hypertension: Elevated blood pressure over 130/80 mmHg in an adult. (Chapter 3.2)
Hypertonic solutions: Solutions that have a higher concentration of dissolved particles than blood. (Chapter 23.2)
Hypoactive bowel sounds: Decreased peristaltic activity; may be related to constipation following abdominal surgery or with an ileus. (Chapter 12.3)
Hypodermis: The layer of skin beneath the dermis composed of connective tissue and used for fat storage. (Chapter 14.2)
Hypoglycemia: A blood glucose reading less than 70 associated with symptoms such as irritability, shakiness, hunger, weakness, or confusion. If not rapidly treated, hypoglycemia can cause seizures and a coma. (Chapter 19.2)
Hypotension: Decreased blood pressure less than 90/60 mmHg in an adult. (Chapter 3.2)
Hypothalamus: The autonomic control center of the brain that controls functions such as blood pressure, heart rate, digestive movement, and pain perception. (Chapter 6.2)
Hypotonic solutions: Solutions that have a lower concentration of dissolved solutes than blood. (Chapter 23.2)
Hypoxemia: Decreased dissolved oxygen in the arterial blood, indicated by a PaO2 level less than 80 mmHg in an ABG test. (Chapter 10.3, Chapter 11.2)
Hypoxia: A reduced level of tissue oxygenation. (Chapter 11.2)
I
Ileostomy: The lower end of the small intestine (ileum) is attached to a stoma to bypass the colon, rectum, and anus. (Chapter 21.7)
Incident report: A report submitted per agency policy used to document the events surrounding a medication error. (Chapter 15.2)
Induration: Area of hardened tissue. (Chapter 20.3)
Indwelling catheter: A device often referred to as a “Foley catheter” that is inserted into the neck of the bladder and remains in place for continual collection of urine into a collection bag. (Chapter 21.2)
Infiltration: Infiltration occurs when the tip of the IV catheter slips out of the vein, the catheter passes through the wall of the vein, or the blood vessel wall allows part of the fluid to infuse into the surrounding tissue, resulting in the leakage of IV fluids into the surrounding tissue. (Chapter 23.4)
Inflammatory phase: The second phase of wound healing when vasodilation occurs so that white blood cells in the bloodstream can move into the wound to start cleaning the wound bed. (Chapter 20.2)
Inner cannula: The cannula inside the outer cannula that is removed during tracheostomy care by the nurse. Inner cannulas can be disposable or reusable with appropriate cleaning. (Chapter 22.2)
Inspection: The observation of a patient’s anatomical structures. (Chapter 1.1)
Instrumental activities of daily living: Complex daily tasks that allow patients to function independently such as managing finances, paying bills, purchasing and preparing meals, managing one’s household, taking medications, and facilitating transportation. (Chapter 2.8)
Intermittent catheterization: The insertion and removal of a straight catheter for relief of urinary retention. (Chapter 21.2)
Intradermal injection: Medication administered in the dermis just below the epidermis. (Chapter 18.1)
Intramuscular injection: Medication administered into a muscle. (Chapter 18.1)
Intravenous injection: Medication administered directly into the bloodstream. (Chapter 18.1)
Intravenous therapy (IV therapy): Involves the administration of substances such as fluids, electrolytes, blood products, nutrition, or medications directly into a client's vein. (Chapter 23.2)
Inunction: A medication that is massaged or rubbed into the skin. (Chapter 16.2)
Involuntary guarding: The reflexive contraction of overlying abdominal muscles as the result of peritoneal inflammation. (Chapter 12.3)
Iris: Colored part of the eye. (Chapter 8.2)
Isotonic solutions: IV fluids that have a similar concentration of dissolved particles as found in the blood. (Chapter 23.2)
J
Jaundice: A yellowing of the skin or sclera caused by underlying medical conditions. (Chapter 14.3, Chapter 14.4)
Joints: The location where bones come together. (Chapter 13.2)
Jugular Vein Distension (JVD): Occurs when the increased pressure of the superior vena cava causes the jugular vein to bulge, making it most visible on the right side of a person’s neck. (Chapter 9.3)
K
Keloid: A raised scar caused by overproduction of scar tissue. (Chapter 14.3)
Ketoacidosis: A life-threatening complication of hyperglycemia that can occur in patients with type 1 diabetes mellitus that is associated with symptoms such as fruity-smelling breath, nausea, vomiting, severe thirst, and shortness of breath. (Chapter 19.2)
Key part: Any sterile part of equipment used during an aseptic procedure, such as needle hubs, syringe tips, dressings, etc. (Chapter 4.3)
Key site: The site contacted during an aseptic procedure, such as nonintact skin, a potential insertion site, or an access site used for medical devices connected to the patients. Examples of key sites include the insertion or access site for intravenous (IV) devices, urinary catheters, and open wounds. (Chapter 4.3)
Kinesthesia: A person’s sense of movement. (Chapter 6.2)
Korotkoff sounds: The audible sounds of blood pressure named after Dr. Korotkoff who discovered them. (Chapter 3.2)
Kyphosis: Outward curvature of the back; often described as “hunchback.” (Chapter 10.3, Chapter 13.3)
L
Lacrimal duct: Tears produced by the lacrimal gland flow through this duct to the medial corner of the eye. (Chapter 8.2)
Laryngopharynx: The portion of the pharynx inferior to the oropharynx and posterior to the larynx that is a passageway for ingested material and air until its inferior end where the digestive and respiratory systems diverge into the esophagus and the larynx. (Chapter 7.2)
Larynx: The structure connecting the pharynx to the trachea that helps regulate the volume of air that enters and leaves the lungs and contains the vocal cords. (Chapter 7.2)
Lens: An inner part of the eye that helps the eye focus. (Chapter 8.2)
Lesion: An area of abnormal tissue. (Chapter 14.2)
Level of consciousness: A patient’s level of arousal and alertness, commonly assessed by asking them to report their name, current location, and time. (Chapter 6.4)
LGBTQ: An acronym standing for lesbian, gay, bisexual, transgender, and queer is an umbrella term that generally refers to a group of people who are diverse with regard to their gender identity and sexual orientation. There are expanded versions of this acronym. (Chapter 2.8)
Ligaments: Strong bands of fibrous connective tissue that connect bones and strengthen and support joints by anchoring bones together and preventing their separation. (Chapter 13.2)
Lordosis: An inward curve of the lumbar spine just above the buttocks. A small degree of lordosis is normal, but too much curving is called swayback. (Chapter 13.3)
Lymphadenopathy: Enlarged lymph nodes. (Chapter 7.3)
Lymphedema: A type of swelling that occurs when lymph fluid builds up in the body’s soft tissues due to damage to the lymph system. (Chapter 14.3)
Lymph nodes: Structures in the lymphatic system that filter pathogens. (Chapter 7.2)
M
Maceration: The softening and wasting away of skin due to excess fluid. (Chapter 20.2)
Macrodrip tubing: Gravity IV tubing with drop factors of 10, 15, or 20 drops per milliliter that are typically used to deliver general IV solutions for adults. (Chapter 5.14)
Main health care needs: Term used to classify what needs the patient feels are most important to address after admission to a health care agency. (Chapter 2.5)
Mandible: Lower jawbone. (Chapter 7.2)
MAR: Medication administration record contained in a patient’s chart. (Chapter 15.2)
Masseter: Main muscle used for chewing because it elevates the mandible to close the mouth. (Chapter 7.2)
Maturation phase: The final phase of wound healing as collagen continues to be created to strengthen the wound, causing scar tissue. (Chapter 20.2)
Maxilla: Bone that forms the upper jaw and supports the upper teeth. (Chapter 7.2)
Medical asepsis: Measures to prevent the spread of infection in health care agencies. (Chapter 1.2)
Medication cup: A small plastic or paper cup used to dispense oral medications. Some plastic medication cups have calibration marks for measuring medication amounts. (Chapter 5.2)
Medication reconciliation: A comparison of a list of current medications with a previous list and is completed at every hospitalization and clinic visit. (Chapter 2.6)
Melanin: Skin pigment produced by melanocytes scattered throughout the epidermis. (Chapter 14.2)
Melanoma: Skin cancer characterized by the uncontrolled growth of melanocytes that commonly develops from a mole. Melanoma is the most fatal of all skin cancers because it is highly metastatic. Melanomas usually appear as asymmetrical brown and black patches with uneven borders and a raised surface. (Chapter 14.3)
Melena: Dark, tarry-looking stool due to the presence of digested blood. (Chapter 2.8, Chapter 12.3)
Mental health: A state of well-being in which every individual realizes their own potential, can cope with normal stresses of life, can work productively and fruitfully, and is able to make a contribution to their community. (Chapter 2.8)
Metered dose inhaler (MDI): An inhaler that provides a mist of medication that is inhaled through the mouth into the lungs. An example of an MDI is albuterol. Optimal administration is achieved with a spacer attached to the inhaler. (Chapter 16.2)
Microdrip tubing: Gravity IV tubing with a drop factor of 60 drops per milliliter. (Chapter 5.14)
Midline peripheral catheters: A larger catheter (i.e., 16-18 gauge) that allow for rapid infusions but does not terminate in the central vasculature. (Chapter 23.2)
Military time: A method of measuring the time based on the full 24 hours of the day rather than two groups of 12 hours indicated by AM and PM. (Chapter 5.3)
Mobility: A patient’s ability to move around (e.g., sit up, sit down, stand up, walk). (Chapter 2.8)
Motor nerves: Nerves in the peripheral nervous system that transmit motor signals from the brain to the muscles to cause movement. (Chapter 6.2)
Murmur: A blowing or whooshing sound heard on auscultation of the precordium that signifies turbulent blood flow in the heart often caused by a valvular defect. (Chapter 9.3)
Muscle atrophy: The thinning or loss of muscle tissue that can be caused by disuse, aging, or neurological damage. (Chapter 13.2)
Myopia: Impaired vision, also known as nearsightedness, that makes far-away objects look blurry. (Chapter 8.2)
N
Nares: Nostril openings into the nasal cavity. (Chapter 7.2)
Nasal septum: Bone and cartilage that separate the nasal cavity into two compartments. (Chapter 7.2)
Nasopharynx: The upper region of the pharynx that connects to the nasal cavity and is a passageway for air. (Chapter 7.2)
Necrosis: Tissue death. (Chapter 23.2)
Necrotic: Black tissue color due to tissue death from lack of oxygenation to the area. (Chapter 20.2)
Nonblanchable erythema: Skin redness that does not turn white when pressure is applied. (Chapter 20.2)
Nursing: Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in recognition of the connection of all humanity. (Chapter 2.1)
Nystagmus: Involuntary, shaky eye movements. (Chapter 6.5)
O
Objective data: Information observed through your sense of hearing, sight, smell, and touch while assessing the patient. (Chapter 1.1, Chapter 2.2)
Obstructive sleep apnea (OSA): Characterized by repeated occurrences of complete or partial obstructions of the upper airway during sleep, resulting in apneic episodes. (Chapter 11.2)
Older adults: People over the age of 65. (Chapter 1.2)
One-time order: A prescription for a medication to be administered only once. An example of a one-time order is a prescription for an IV dose of antibiotics to be administered immediately prior to surgery. (Chapter 15.2)
Open fracture: A type of fracture when the broken bone punctures the skin. (Chapter 13.3)
Optic nerve: Cranial nerve II that conducts visual information from the retina to the brain. (Chapter 8.2)
Oral syringe: A specific type of syringe used to measure and/or administer medications via the oral route. (Chapter 5.2)
Orbit: The bony socket that houses the eyeball and muscles that move the eyeball. (Chapter 7.2)
Oropharyngeal suctioning: Suction of secretions through the mouth, often using a Yankauer device. (Chapter 22.4)
Oropharynx: The part of the throat at the back of the mouth behind the oral cavity. It includes the back third of the tongue, the soft palate, the side and back walls of the throat, and the tonsils. (Chapter 7.2, Chapter 19.4)
Orthopnea: Breathlessness or a feeling of shortness of breath when lying in a reclined position. (Chapter 9.3, Chapter 10.3)
Orthostatic hypotension: A decrease in blood pressure by at least 20 mmHg systolic or 10 mmHg diastolic within three minutes of standing from a seated or lying position. (Chapter 3.2)
Osteoarthritis: The most common type of arthritis associated with aging and wear and tear of the articular cartilage that covers the surfaces of bones at the synovial joint. (Chapter 13.3)
Osteomyelitis: Bone infection. (Chapter 20.2)
Osteoporosis: A disease that thins and weakens bones, especially in the hip, spine, and wrist, causing them to become fragile and break easily. (Chapter 13.3)
Ostomy: The surgical procedure that creates the opening from the stoma outside the body to an organ such as the small intestine, colon, rectum, or bladder. A stoma can be permanent, such as when an organ is removed, or temporary, such as when an organ requires time to heal. (Chapter 21.7)
Otitis externa: The medical diagnosis for external ear inflammation and/or infection. (Chapter 8.2)
Ototoxic medications: Medications that cause the adverse effect of sensorineural hearing loss by affecting the hair cells in the cochlea. (Chapter 8.2)
Outer cannula: The outer cannula placed by the provider through the tracheostomy stoma and continuously remains in place. (Chapter 22.2)
P
Pallor: A reduced amount of oxyhemoglobin in the skin or mucous membranes. Skin and mucous membranes present with a pale skin color. (Chapter 9.3, Chapter 10.3, Chapter 14.4)
PaO2: The partial pressure of dissolved oxygen in the blood measured by arterial blood gas samples. (Chapter 11.2)
Paralysis: The partial or complete loss of strength, movement, or control of a muscle or group of muscles within a body part that can be caused by brain or spinal injury. (Chapter 6.5)
Paroxysmal nocturnal dyspnea: An attack of severe shortness of breath that generally occurs at night. (Chapter 9.3)
Passive range of motion: The degree of range of motion a patient demonstrates in a joint when the examiner is providing the movement. (Chapter 13.4)
Percussion: An advanced physical examination technique where body parts are tapped with fingers to determine their size and if fluid is present. (Chapter 1.1)
Perfusion: The amount of blood flow to tissue. (Chapter 9.3)
Pericardial friction rub: Uncommon heart sounds produced when the parietal and visceral pericardium become inflamed, generating a creaky-scratchy noise as they rub together. (Chapter 9.3)
Peripheral edema: Swelling due to an accumulation of fluid in tissues perfused by the peripheral vascular system. (Chapter 9.3)
Peripheral inserted central catheter: A thin, flexible tube inserted into a vein in the upper arm and guided into the superior vena cava. (Chapter 23.2)
Peripheral IV: An intravenous catheter inserted by percutaneous venipuncture into a peripheral vein and held in place with a sterile transparent dressing. (Chapter 23.2)
Peripheral nervous system: The part of the nervous system that includes the cranial and spinal nerves. (Chapter 6.2)
Peripheral neuropathy: A condition that causes decreased sensation of pain and pressure, typically in the lower extremities. (Chapter 20.2)
Periwound: The skin around the outer edges of a wound. (Chapter 20.3)
Personal Protective Equipment (PPE): Includes gloves, gowns, goggles, face shields, and masks, along with environmental controls, to prevent the transmission of infection for patients who are diagnosed or suspected of having an infectious disease. (Chapter 1.2, Chapter 4.1)
Petechiae: Tiny red dots caused by bleeding under the skin. (Chapter 14.3)
Pharyngitis: Infection and/or inflammation in the back of the throat (pharynx). (Chapter 7.3)
Pharynx: A tube lined with mucous membrane that begins at the nasal cavity and is divided into three major regions: the nasopharynx, the oropharynx, and the laryngopharynx. (Chapter 7.2)
Phlebitis: Inflammation of a vein. (Chapter 23.4)
Physical examination: A systematic data collection method of the body that uses the techniques of inspection, auscultation, palpation, and percussion. (Chapter 1.1)
Pitting edema: An accumulation of fluid in tissue and causes an indentation when the area is pressed. (Chapter 9.3)
Pleural rub: Uncommon sound heard when there is inflammation of the lung pleura, resulting in friction as the surfaces rub against each other. (Chapter 10.3)
Precordium: The region of the thorax in front of the heart. (Chapter 9.3)
Presbycusis: Sensorineural hearing loss that occurs with aging due to gradual nerve degeneration. (Chapter 8.2)
Presbyopia: Impaired near vision that commonly occurs in middle-aged and older adults. (Chapter 8.2)
Prescriptions: Orders, interventions, remedies, or treatments ordered or directed by an authorized primary health care provider. (Chapter 15.2)
Pressure injury: Skin breakdown caused when a patient’s skin and soft tissue press against a hard surface for a prolonged period of time, causing reduced blood supply and resulting in damaged tissue. (Chapter 14.3, Chapter 20.2)
Primary intention: Wound healing that occurs with surgical incisions or clean-edged lacerations that are closed with sutures, staples, or surgical glue. (Chapter 20.2)
Primary source of data: Information obtained directly from the patient. (Chapter 1.1, Chapter 2.2)
Primary survey: A brief observation at the start of a shift or visit to verify the patient is stable by assessing mental status, airway, breathing, and circulation. (Chapter 1.4)
PRN order: A prescription for medication to be administered when it is requested by, or as needed by, the patient. PRN orders are usually administered based on patient symptoms such as pain medications. An example of a PRN order is a prescription for pain medication, such as “Acetaminophen 500 mg PO every 4-6 hours as needed for pain.” (Chapter 15.2)
Proliferative phase: The third phase of wound healing that includes epithelialization, angiogenesis, collagen formation, and contraction. (Chapter 20.2)
Proprioception: A person’s sense of their body position. (Chapter 6.2, Chapter 6.8)
Prostate hypertrophy: A common medical condition of the enlargement of the prostate gland in males as they age, causing uncomfortable urinary symptoms such as urgency and frequency. (Chapter 12.3)
Protuberant: Convex or bulging appearance. (Chapter 12.3)
Ptosis: Drooping of the eyelid. (Chapter 6.5)
Pulmonary embolism: A blood clot that lodges in one of the arteries that go from the heart to the lung. (Chapter 9.3)
Pupil: The hole at the center of the eye that allows light to enter. (Chapter 8.2)
Purulent drainage: Wound exudate that is thick and opaque and can be tan, yellow, green, or brown in color. It is never considered normal in a wound, and new purulent drainage should always be reported to the health care provider. (Chapter 20.3)
R
Rales: Another term used for crackles. (Chapter 10.3)
Rebound tenderness: Pain when hand is withdrawn during palpation. (Chapter 12.3)
Reconstitution: The process of adding a liquid diluent to a dry ingredient to make a liquid in a specific concentration. (Chapter 5.10)
Respiration: Includes ventilation and gas exchange at the alveolar level where blood is oxygenated and carbon dioxide is removed. (Chapter 10.2)
Retina: The nervous tissue and photoreceptors in the eye that initially process visual stimuli. (Chapter 8.2)
Retractions: The “pulling in” of muscles between the ribs or in the neck when breathing, indicating difficulty breathing or respiratory distress. (Chapter 10.3)
Rheumatoid arthritis: A type of arthritis that causes pain, swelling, stiffness, and loss of function in joints due to inflammation caused by an autoimmune disease. (Chapter 13.3)
RICE: A mnemonic for treatment of sprains and strains that stands for: Resting the injured area, Icing the area, Compressing the area with an ACE bandage or other device, and Elevating the affected limb. (Chapter 13.3)
Rigidity: Involuntary contraction of the abdominal musculature in response to peritoneal inflammation. (Chapter 12.3)
Rotation: Circular movement of a joint around a fixed point. (Chapter 13.2)
Routine order: A written prescription that is followed until another order cancels it. An example of a routine order is a prescription for daily medication such as “Lisinopril 10 mg PO daily.” (Chapter 15.2)
Rule of Nines: A tool used in the emergency department to assess the total body surface area burned to quickly estimate intravenous fluid requirements. (Chapter 14.3)
S
Safety culture: A culture established in health care agencies to empower staff to speak up about risks to patients and to report errors and near misses, all of which drive improvement in patient care and reduce the incident of patient harm. (Chapter 15.2)
Saline lock: Refers to the use of a short extension set that allows IV access without requiring ongoing IV infusions. (Chapter 23.2)
Sanguineous drainage: Wound drainage that is fresh bleeding. (Chapter 20.3)
SaO2: Calculated arterial oxygen saturation level. (Chapter 11.2)
Scaphoid: Sunken appearance. (Chapter 12.3)
Sclera: White area of the eye. (Chapter 8.2)
Scoliosis: A sideways curve of the spine that commonly develops in late childhood and the early teens. (Chapter 13.3)
Secondary intention: Wound healing that occurs when the edges of a wound cannot be approximated (brought together), so the wound fills in from the bottom up by the production of granulation tissue. Examples of wounds that heal by secondary intention are pressure injuries and chainsaw injuries. (Chapter 20.2)
Secondary source of data: Information from the patient’s chart, family members, or other health care team members. (Chapter 1.1, Chapter 2.2)
Second-degree burn: Burn affecting both the epidermis and a portion of the dermis, resulting in swelling and a painful blistering of the skin. (Chapter 14.3)
Self-concept: Knowledge a person has about themselves that makes up who they are (i.e., their identity). (Chapter 2.8)
Self-esteem: A person’s self-evaluation of their self-concept as being worthy or unworthy. (Chapter 2.8)
Sensation: The function of receiving information about the environment. The major senses are taste, smell, touch, sight, and hearing. (Chapter 6.2)
Sensorineural hearing loss: Hearing loss caused by pathology of the inner ear, cranial nerve VIII, or auditory areas of the cerebral cortex. (Chapter 8.2)
Sensory nerves: Nerves in the peripheral nervous system that carry impulses from the body to the brain for processing. (Chapter 6.2)
Serosanguinous drainage: Wound exudate contains serous drainage with small amounts of blood present. (Chapter 20.3)
Serous drainage: Wound drainage that is clear, thin, watery plasma. It is considered normal in minimal amounts during the inflammatory stage of wound healing. (Chapter 20.3)
Sexual orientation: The preferred term used when referring to an individual’s physical and/or emotional attraction to the same and/or opposite gender. (Chapter 2.8)
Shear: A mechanical force that occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue. (Chapter 20.2)
Sign: Objective data found by the nurse or health care provider when assessing a patient. (Chapter 2.2)
Sinusitis: Inflamed sinuses caused by a viral or bacterial infection. (Chapter 7.3)
Skeletal muscle: Voluntary muscle that produces movement, assists in maintaining posture, protects internal organs, and generates body heat. (Chapter 13.2)
Skin tears: Wounds caused by mechanical forces, typically in the nonelastic skin of older adults. (Chapter 20.2)
Skin turgor: The skin’s elasticity and its ability to change shape and return to normal when gently grasped between two fingers. (Chapter 14.4)
Slough: Inflammatory exudate that is light yellow, soft, and moist and must be removed for wound healing to occur. (Chapter 20.2)
Small-volume nebulizers: Devices that provide a fine mist using oxygen or compressed air to transport the medication from a nebulizer cup into the mouth and into the lungs as the patient breathes normally through a mask or pipe device. (Chapter 16.2)
Snellen chart: A chart used to test far vision. (Chapter 8.2)
Sphygmomanometer: A device used to measure blood pressure and is commonly referred to as a blood pressure cuff. (Chapter 3.2, Chapter 9.3)
Spirituality: A way of living that comes from a set of meanings, values, and beliefs that are important to a person. (Chapter 2.8)
SpO2: An estimated oxygenation level based on the saturation level of hemoglobin measured by a pulse oximeter. (Chapter 11.2)
Sprain: A stretched or torn ligament caused by an injury. (Chapter 13.3)
Standardized sliding-scale insulin protocol: Standardized instructions for administration of adjustable insulin dosages based on a patient’s premeal blood glucose readings. (Chapter 19.2)
Standard precautions: The minimum infection prevention practices that apply to all patient care, regardless of suspected or confirmed infection status of the patient, in any setting where health care is delivered. (Chapter 4.2)
Standing order: Standing orders are standard prescriptions for nurses to implement for patients in clearly defined circumstances without the need to notify a provider. They may also be referred to as an “order set” or a “protocol.” An example of a standing order/protocol is a standard prescription for all patients coming into an urgent care reporting chest pain to immediately receive four chewable aspirin, the placement of an IV, and an electrocardiogram (ECG). (Chapter 15.2)
STAT order: A one-time prescription that is administered without delay. An example of a STAT order is the prescription for a dose of Benadryl to be administered to a patient having an allergic reaction. (Chapter 15.2)
Stereognosis: The ability to perceive the physical form and identity of an object based on tactile stimuli alone. (Chapter 6.6)
Sterile technique (surgical asepsis): Techniques used to eliminate every potential microorganism in and around a sterile field while maintaining objects and areas as free from microorganisms as possible. This technique is the standard of care for surgical procedures, invasive wound management, and central line care. (Chapter 4.3)
Sternocleidomastoid: The major muscle that laterally flexes and rotates the head. (Chapter 7.2)
Stoma: An opening on the abdomen that is connected to the gastrointestinal or urinary systems to allow waste (urine or feces) to be collected in a pouch. (Chapter 21.7)
Stomach decompression: Using suctioning through a nasogastric tube to remove the contents of the stomach. (Chapter 17.1)
Straight catheter: A catheter used for intermittent urinary catheterization; it does not have a balloon at the insertion end. (Chapter 21.2)
Strain: A stretched or torn muscle or tendon. (Chapter 13.3)
Striae: White or silver markings from stretching of the skin. (Chapter 12.3)
Stridor: High-pitched crowing sounds heard over the upper airway and larynx indicating obstruction. (Chapter 10.3)
Subcutaneous injection: Medication administered into the subcutaneous tissue just under the dermis. (Chapter 18.1)
Subjective data: Information obtained from the patient and/or family members that offers important cues from their perspectives. (Chapter 1.1, Chapter 2.2)
Suction canister: A container for collecting suctioned secretions that is attached to a suction source. (Chapter 22.4)
Suction catheter: A soft, flexible, sterile catheter used for nasopharyngeal and tracheostomy suctioning. (Chapter 22.4)
Suture: An interlocking joint between adjacent bones of the skull. (Chapter 7.2)
Symptom: Subjective data that the patient reports, such as “I feel dizzy.” (Chapter 2.2)
Syncope: A temporary loss of consciousness usually related to insufficient blood flow to the brain. (Chapter 9.3)
Synovial fluid: A thick fluid that provides lubrication in joints to reduce friction between the bones. (Chapter 13.2)
Synovial joints: A fluid-filled joint cavity where the articulating surfaces of the bones contact and move smoothly against each other. The elbow and knee are examples of synovial joints. (Chapter 13.2)
Syringe: A medical device used to administer parenteral medication into tissue or into the bloodstream. Syringes can also be used to withdraw blood or fluid. (Chapter 5.2)
Systole: The phase of the heartbeat when the left ventricle contracts and pumps blood into the arteries. (Chapter 3.2)
Systolic blood pressure: The maximum pressure of blood on the arteries during the contraction of the left ventricle of the heart referred to as systole. (Chapter 3.2)
T
Tachypnea: Rapid and often shallow breathing greater than normal range according to the patient’s age. (Chapter 10.3)
Temporalis: Muscle that assists in chewing by retracting the mandible. The temporalis muscle can be felt moving by placing fingers on the patient’s temple as they chew. (Chapter 7.2)
Tendons: Strong bands of dense, regular connective tissue that connect muscles to bones. (Chapter 13.2)
Tertiary intention: Wound healing that occurs when a wound must remain open or has been reopened, often due to severe infection. (Chapter 20.2)
Thalamus: Relays sensory information and motor information in collaboration with the cerebellum. (Chapter 6.2)
Third-degree burn: Severe burn that fully extends into the epidermis and dermis, destroying the tissue and affecting the nerve endings and sensory function. (Chapter 14.3)
Thrill: A vibration felt with palpation of the precordium. (Chapter 9.3)
Tinnitus: Ringing, buzzing, roaring, hissing, or whistling sound in the ears. (Chapter 8.2)
Titration order: An order in which the medication dose is either progressively increased or decreased by the nurse in response to the patient’s status. (Chapter 15.2)
Topical medications: Medications administered via the skin or mucous membranes for direct local action, as well as for systemic effects. (Chapter 16.2)
Total parenteral nutrition (TPN): A very concentrated solution that must be administered via a central line. (Chapter 23.2)
Trachea: A tube lined with mucus membrane that carries air from the larynx to the lungs. (Chapter 7.2)
Tracheostomy: A surgically created opening that goes from the front of the neck into the trachea. (Chapter 22.2)
Tracheostomy dressing: A manufactured dressing used with tracheostomies that does not shed fibers, which could potentially be inhaled by the patient. (Chapter 22.4)
Transdermal route: Patches or disks applied to the skin that deliver medication over an extended period of time. (Chapter 16.2)
Trapezius: The muscle that elevates the shoulders (shrugs), pulls the shoulder blades together, and tilts the head backwards. (Chapter 7.2)
Tunneling: Passageways underneath the surface of the skin that extend from a wound and can take twists and turns. (Chapter 20.2)
Tympanic membrane: The membrane at the end of the external ear canal, commonly called the eardrum, that vibrates after it is struck by sound waves. (Chapter 8.2)
U
Undermining: A condition that occurs in wounds when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound’s edge. (Chapter 20.2)
Unstageable: Occurs when slough or eschar obscures the wound so that tissue loss cannot be assessed. (Chapter 20.2)
Urinary catheterization: The insertion of a catheter tube into the urethral opening and placing it in the neck of the urinary bladder to drain urine. (Chapter 21.2)
Urinary frequency: Urination every hour or two. (Chapter 12.3)
Urinary incontinence: Involuntary leakage of urine. (Chapter 12.3)
Urinary tract infection (UTI): An infection in the urinary system causing symptoms such as burning on urination (dysuria), frequent urination, malodorous urine, fever, and change in level of consciousness. (Chapter 21.2)
Urinary urgency: An intense urge to urinate that can lead to urinary incontinence. (Chapter 12.3)
Urostomy: The ureters (tubes that carry urine from the kidney to the bladder) are attached to a stoma to bypass the bladder. (Chapter 21.7)
Uvula: A small, teardrop-shaped structure located at the apex of the soft palate that swings upward during swallowing to close off the nasopharynx and prevent ingested materials from entering the nasal cavity. (Chapter 7.2)
V
Value: An accepted principle or standard of an individual or group. (Chapter 2.8)
Vastus lateralis: A muscle located on the anterior lateral aspect of the thigh and extends from one hand’s breadth above the knee to one hand’s breadth below the greater trochanter. It is commonly used for immunizations in infants and toddlers because the muscle is thick and well-developed. (Chapter 18.6)
Venipuncture: The process of introducing a needle into a client’s vein to collect a blood sample or insert an IV catheter. (Chapter 23.2)
Venous insufficiency: A medical condition where the veins in the legs do not adequately send blood back to the heart, resulting in a pooling of fluids in the legs that can cause venous ulcers. (Chapter 20.2)
Venous ulcers: Ulcers caused by the pooling of fluid in the veins of the lower legs when the valves are not working properly, causing fluid to seep out, macerate the skin, and cause an ulcer. (Chapter 20.2)
Ventilation: The mechanical movement of air into and out of the lungs. (Chapter 10.2, Chapter 11.3)
Ventrogluteal: The safest intramuscular injection site for adults and children because it provides the greatest thickness of gluteal muscles, is free from penetrating nerves and blood vessels, and has a thin layer of fat. (Chapter 18.6)
Vertigo: A type of dizziness often described by patients as “the room feels as if it is spinning.” (Chapter 8.2)
Vesicular sounds: Low-pitched soft sounds like “rustling leaves” heard over alveoli and small bronchial airways. (Chapter 10.3)
Vestibulocochlear nerve: Cranial nerve VIII that transports neural signals from the cochlea and the vestibule to the brain stem regarding hearing and balance. (Chapter 8.2)
Voiding: Medical terminology used for urinating. (Chapter 2.8)
Voluntary guarding: Voluntary contraction of abdominal wall musculature; may be related to fear, anxiety, or presence of cold hands. (Chapter 12.3)
W
Wheeze: High-pitched sounds heard on expiration or inspiration associated with bronchoconstriction or bronchospasm. (Chapter 10.3)
Wound vac: A device used with special foam dressings and suctioning to remove fluid and decrease air pressure around a wound to assist in healing. (Chapter 20.5)
Y
Yankauer suction tip: Rigid device used to suction secretions from the mouth. (Chapter 22.4)
Z
Z-track method: A method for administering intramuscular injections that prevents the medication from leaking into the subcutaneous tissue, allows the medication to stay in the muscles, and minimizes irritation. (Chapter 18.6)

