21.7 Managing Ostomies
Open Resources for Nursing (Open RN)
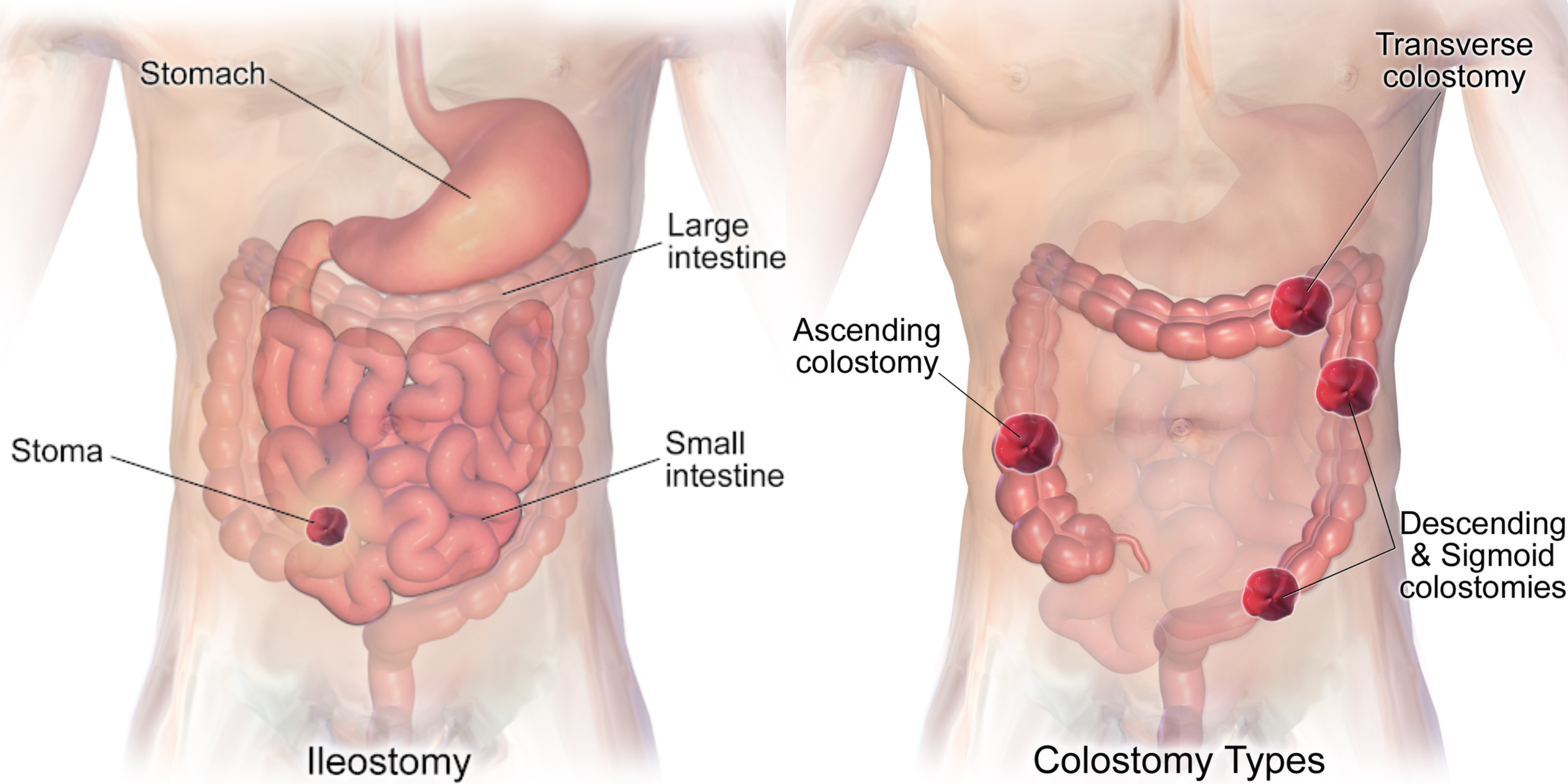
An ostomy is the surgical procedure that creates an opening (stoma) from an area inside the body to the outside of the body. In ostomies related to elimination, a stoma is an opening on the abdomen that is connected to the gastrointestinal or urinary system to allow waste (i.e., urine or feces) to be collected in a pouch. See Figure 21.14[1] for an image of a stoma. A stoma can be permanent, such as when an organ is removed, or temporary, such as when an organ requires time to heal. Ostomies are created for patients with conditions such as cancer of the bowel or bladder, inflammatory bowel diseases, or perforation of the colon.

There are several different kinds of ostomies related to elimination. Common types of ostomies include the following:
- Ileostomy: The lower end of the small intestine (ileum) is attached to a stoma to bypass the colon, rectum, and anus.
- Colostomy: The colon is attached to a stoma to bypass the rectum and the anus.
- Urostomy: The ureters (tubes that carry urine from the kidney to the bladder) are attached to a stoma to bypass the bladder.[2]
See Figure 21.15[3] comparing the anatomical locations of ileostomies and various sites of colostomies. It is important for the nurse to understand the site of a patient’s colostomy because the site impacts the characteristics of the waste. For example, due to the natural digestive process of the colon and absorption of water, waste from an ileostomy or a colostomy placed in the anterior ascending colon will be watery compared to waste from an ostomy placed in the descending colon.
The tissue of a stoma is very delicate. Immediately after surgery, a stoma is swollen, but it will shrink in size over several weeks. A healthy, healed stoma appears moist and dark red or pink in color. Stomas that are swollen; dry; have malodorous discharge; or are bluish, purple, black, or pale should be reported to the provider. The skin surrounding a stoma can easily become irritated from the pouch adhesive or leakage of fluid from the stoma, so the nurse must perform interventions to prevent skin breakdown. Any identified signs of skin breakdown should be reported to the provider.[4]
Stoma appliances are supplied as a one- or two-piece set. A two-piece set consists of an ostomy barrier (also called a wafer) and a pouch. The ostomy barrier is the part of the appliance that sticks to the skin with a hole that is fitted around the stoma. The pouch collects the waste and must be emptied regularly. It attaches to the ostomy barrier in a clicking motion to secure the two parts, similar to how a plastic storage container cover snaps to a container to create a seal. The pouching system must be completely sealed to prevent leaking of the waste and to protect the surrounding peristomal skin. The pouch has an end with an opening where the waste is drained and is closed using a plastic clip or VelcroTM strip.[5] In a one-piece stoma appliance set, the ostomy barrier and the pouch are one piece. See Figure 21.16[6] for an image of a stoma with an ostomy barrier in place. See Figure 21.17[7] for an image of a patient with an ileostomy appliance with a pouch attached.
Individuals with colostomies, ileostomies, and urostomies have no sensation and no control over the output of the stoma. Depending on the type of system, the ostomy appliance can last from four to seven days, but the pouch must be changed if there is leaking, odor, excessive skin exposure, or itching or burning under the skin barrier. Patients with pouches can swim and take showers with the pouching system on.[8]


When changing an ostomy appliance, the ostomy barrier is cut to fit closely around the stoma without impinging on it. See the “Checklist for Ostomy Appliance Change” for detailed instructions. The nurse measures the stoma with a template and then cuts and fits the ostomy barrier to a size that is 2 mm larger than the stoma.[9] See Figure 21.18[10] for an image of a nurse measuring and cutting the ostomy barrier to fit around a stoma.
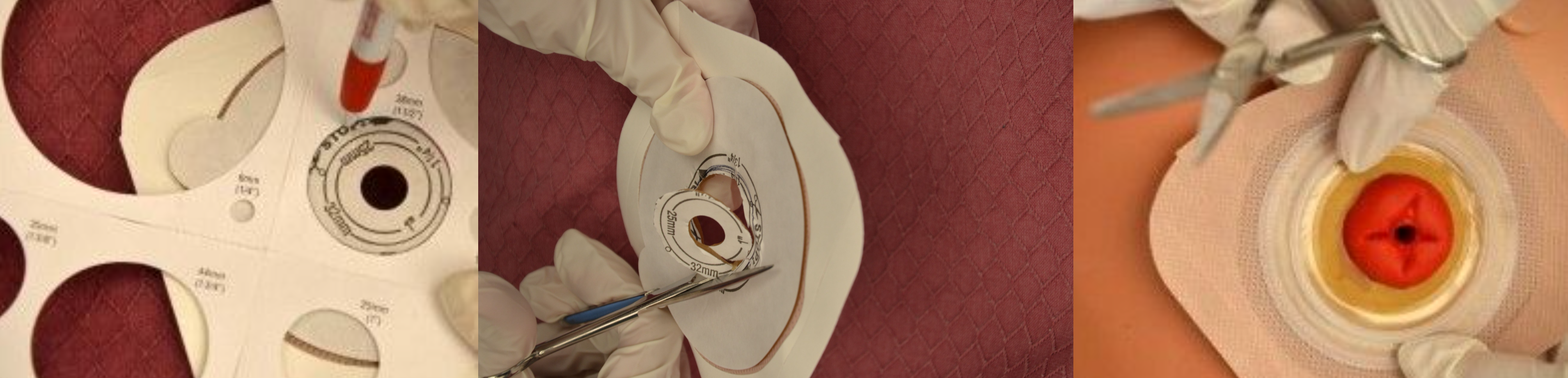
After the skin barrier is applied to the skin, the pouch is snapped to the barrier. See Figure 21.19[11] for an image of applying the pouch.

Physical and Emotional Assessment
Patients may have other medical conditions that affect their ability to manage their ostomy care. Conditions such as arthritis, vision changes, Parkinson’s disease, or post-stroke complications can hinder a patient’s coordination and ability to manage the ostomy. In addition, the emotional burden of coping with an ostomy may be devastating for some patients and may affect their self-esteem, body image, quality of life, and ability to be intimate. It is common for patients with ostomies to struggle with body image and their altered pattern of elimination. Nurses can promote healthy coping by ensuring the patient has appropriate referrals to a wound/ostomy nurse specialist, a social worker, and support groups. Nurses should also be aware of their nonverbal cues when assisting a patient with their appliance changes. It is vital not to show signs of disgust at the appearance of the ostomy or at the odor that may be present when changing an appliance or pouching system.[12]
View a supplementary YouTube video on Changing an Ostomy Pouch[13]
Urostomy Care
A urostomy is similar to a colostomy, but it is an artificial opening for passing urine. Urostomies are surgically created due to medical conditions such as bladder cancer, removal of the bladder, trauma, spinal cord injuries, or congenital abnormalities.
A urostomy patient has no voluntary control of urine, so the pouching system must be emptied regularly. Many patients empty their urostomy bag every two to four hours or when the pouch becomes one-third full. The pouch may also be attached to a drainage bag for overnight drainage. Patients with a urostomy are at risk for urinary tract infections (UTIs), so it is important to educate them regarding the signs and symptoms of an infection.
- “Ileostomy 2017-02-20 5351.jpg” by Salicyna is licensed under CC BY-SA 4.0 ↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2020, Apr 24]. Ostomy. [reviewed 2014, Jul 3; cited 2020, Nov 17]. https://medlineplus.gov/ostomy.html ↵
- “Ileostomy.png” by BruceBlaus is licensed under CC BY-SA 4.0 and “Blausen_0247_Colostomy.png” by CC BY 3.0 ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Ileostomy - caring for your stoma; [updated 2020, Nov 3]. https://medlineplus.gov/ency/patientinstructions/000071.htm ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Ileostomy - caring for your stoma; [updated 2020, Nov 3]. https://medlineplus.gov/ency/patientinstructions/000071.htm ↵
- “Ostomy_wafer_being_worn_by_an_ileostomy_patient.jpg” by Eric Polsinelli (VeganOstomy) is licensed under CC BY 4.0 ↵
- “Ileostomy_2016-09-09_4158.jpg” by Salicyna is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- “DSC_1284-e1442766479432.jpg” and “Assess-if-flange-is-the-correct-size-for-stoma-001.jpg” by British Columbia Institute of Technology are licensed under CC BY 4.0. Access for free at https://ecampusontario.pressbooks.pub/clinicalskills/chapter/10-6-ostomies/ ↵
- “Removing-ostomy-bag-from-flange-001.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://ecampusontario.pressbooks.pub/clinicalskills/chapter/10-6-ostomies/ ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- RegisteredNurseRN. (2017, February 14). Ostomy bag pouch change | Ostomy care nursing | Colostomy, ileostomy bag change [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/h8CtsPAaa5Y ↵
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
1. An older, frail patient is prescribed a flu vaccine that is an aqueous or water-based solution. The patient’s deltoid muscle is not very prominent, and the patient has very little fat over the deltoid. The needles available are 23 G 5⁄8-inch, 22 G 1-inch, and 20 G 1 1⁄2-inch. What needle size/length would work best for this particular medication and patient? Give the reason for your selection.
2. A patient is hospitalized on the surgical floor. Pain medication is prescribed to be given by intramuscular route. After calculating, the volume to be administered is 2 mL. The patient has a large amount of adipose tissue around her hips and buttocks region and weighs 253 pounds. The needle sizes available include 27 G 3⁄8-inch, 25 G 5⁄8-inch, 22 G 1-inch, 21 G 1 1⁄2-inch, and 20 G 2-inches. What needle size/length and injection site would work best for this particular medication and patient? Give the reason for your selection.
3. The nurse is teaching a patient how to mix 5 units of regular insulin and 15 units of NPH insulin in the same syringe. The nurse determines further instruction is needed if the patient does which of the following?
- Injects 5 units of air into the regular insulin vial first and withdraws 5 units of regular insulin
- Injects 15 units of air into the NPH insulin vial but does not withdraw the medication
- Withdraws 5 units of regular insulin before withdrawing 15 units of NPH insulin
- Calculates the combined total insulin dose as 20 units after withdrawing the regular insulin from the vial
![]()
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 18, Assignment 1.
![]()
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 18, Assignment 2.
![]()
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 18, Assignment 3.
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 18, Assignment 4.
Learning Activities
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
1. Your patient complains of pain while you are inflating the balloon during a urinary catheter insertion. Describe your next steps.
2. Your patient is admitted with a fractured head of the right femur and is scheduled for surgery in the next six hours. You have a prescription to insert a Foley catheter. After you assess the patient’s ability for the recommended position to insert the catheter, you note that the patient is unable to move the right leg and should not move the leg. Describe how you will proceed with the procedure.
3. A patient with a new colostomy refuses to look at the stoma or participate in changing the pouching system. What are some suggestions to help your patient adjust to the stoma?
4. The nurse is caring for a female patient who is experiencing inadequate bladder emptying. The nurse obtains an order to determine post-void residual. Which catheter type would the nurse use to evaluate post-void residual?
- Coude catheter
- Indwelling catheter
- Straight catheter
- Foley catheter
5. The nurse is caring for a patient who had a colostomy placed two days earlier. The nurse notes that the stoma is moist and beefy red. Which action should the nurse be expected to take based on these findings?
- Notify the physician of the findings immediately.
- Remove the bag and apply pressure to the stoma.
- Document the assessment findings of the stoma.
- Change the appliance pouch and clean the skin.
6. The nurse is providing patient education on the care of an ostomy. Which of the following statements by the patient would indicate that further education is necessary?
- “I should plan to replace the pouch system every 8-10 days.”
- “Wafer should be cut 1/16 to 1/8 an inch larger than the stoma.”
- “It is important to chew all foods completely and slowly.”
- “I will keep a diary of the foods I eat and my stool pattern.”
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 21, Assignment 1.
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 21, Assignment 2.
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 21, Assignment 3.
Learning Activities
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
The patient's IV site is cool to the touch and swollen. The patient states, “It hurts a little.” List in order the steps the nurse should take.
- Discontinue the IV
- Stop the IV infusion
- Elevate the affected site
- Document the findings
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 23, Assignment 1.
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 23, Assignment 2.
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 23, Assignment 3.

