15.2 Basic Concepts of Administering Medications
Open Resources for Nursing (Open RN)
The scope of practice regarding a nurse’s ability to legally dispense and administer medication is based on each state’s Nurse Practice Act. Registered Nurses (RNs) and Licensed Practical Nurses (LPNs/LVNs) may legally administer medications that are prescribed by a health care provider, such as a physician, nurse practitioner, or physician’s assistant. Prescriptions are “orders, interventions, remedies, or treatments ordered or directed by an authorized primary health care provider.”[1]
For more information about the state Nurse Practice Act, visit the “Legal/Ethical” chapter in Open RN Nursing Pharmacology.
Types of Orders
Prescriptions are often referred to as orders in clinical practice. There are several types of orders, such as routine orders, PRN orders, standing orders, one-time orders, STAT orders, and titration orders.
- A routine order is a prescription that is followed until another order cancels it. An example of a routine order is “Lisinopril 10 mg PO daily.”
- A PRN order is a prescription for medication to be administered when it is requested by, or as needed, by the patient. PRN orders are typically administered based on patient symptoms, such as pain, nausea, or itching. An example of a PRN order for pain medication is “Acetaminophen 500 mg PO every 4-6 hours as needed for pain.”
- A standing order is also referred to in practice as an “order set” or a “protocol.” Standing orders are standardized prescriptions for nurses to implement to any patient in clearly defined circumstances without the need to initially notify a provider. An example of a standing order set/protocol for patients visiting an urgent care clinic reporting chest pain is to immediately administer four chewable aspirin, establish intravenous (IV) access, and obtain an electrocardiogram (ECG).
- A one-time order is a prescription for a medication to be administered only once. An example of a one-time order is a prescription for an IV dose of antibiotics to be administered immediately prior to surgery.
- A STAT order is a one-time order that is administered without delay due to the urgency of the circumstances. An example of a STAT order is “Benadryl 50 mg PO stat” for a patient having an allergic reaction.
- A titration order is an order in which the medication dose is either progressively increased or decreased by the nurse in response to the patient’s status. Titration orders are typically used for patients in critical care as defined by agency policy. The Joint Commission requires titration orders to include the medication name, medication route, initial rate of infusion (dose/unit of time), incremental units to which the rate or dose can be increased or decreased, how often the rate or dose can be changed, the maximum rate or dose of infusion, and the objective clinical measure to be used to guide changes. An example of a titration order is “Norepinephrine 2-12 micrograms/min, start at 2 mcg/min and titrate upward by 1 mcg/min every 5 minutes with continual blood pressure monitoring until systolic blood pressure >90 mm Hg.”
Components of a Medication Order
According to the Centers for Medicare & Medicaid Services, all orders for the administration of drugs and biologicals must contain the following information[2]:
- Name of the patient
- Age or date of birth
- Date and time of the order
- Drug name
- Dose, frequency, and route
- Name/Signature of the prescriber
- Weight of the patient to facilitate dose calculation when applicable. (Note that dose calculations are based on metric weight: kilograms for children/adults or grams for newborns)
- Dose calculation requirements, when applicable
- Exact strength or concentration, when applicable
- Quantity and/or duration of the prescription, when applicable
- Specific instructions for use, when applicable
When reviewing a medication order, the nurse must ensure these components are included in the prescription before administering the medication. If a pertinent piece of information is not included, the nurse must contact the prescribing provider to clarify and correct the order.
Drug Name
The name of the drug may be ordered by the generic name or brand name. The generic name is considered the safest method to use and allows for substitution of various brand medications by the pharmacist.
Dose
The dosage of a drug is prescribed using either the metric or the household system. The metric system is the most commonly accepted system internationally. Examples of standard dosage are 5 mL (milliliters) or 1 teaspoon. Standard abbreviations of metric measurement are frequently used regarding the dosage, such as mg (milligram), kg (kilogram), mL (milliliter), mcg (microgram), or L (liter). However, it is considered safe practice to avoid other abbreviations and include the full words in prescriptions to avoid errors. In fact, several abbreviations have been deemed unsafe by the Joint Commission and have been put on a “do not use” list. See the box below to view The Joint Commission’s “Do Not Use List” and the Institute of Safe Medication Practices’ (ISMP) list of abbreviations to avoid. If a dosage is unclear or written in a confusing manner in a prescription, it is always best to clarify the order with the prescribing provider before administering the medication.
Frequency
Frequency in prescriptions is indicated by how many times a day the medication is to be administered or how often it is to be administered in hours or minutes. Examples of frequency include verbiage such as once daily, twice daily, three times daily, four times daily, every 30 minutes, every hour, every four hours, or every eight hours. Medication times are typically indicated using military time (i.e., using a 24-hour clock). For example, 11 p.m. is indicated as “2300.” Read more about military time in the “Math Calculations” chapter.
Some types of medications may be ordered “around the clock (ATC).” An around-the-clock frequency order indicates they should be administered at regular time intervals, such as every six hours, to maintain consistent levels of the drug in the patient’s bloodstream. For example, pain medications administered at end of life are often prescribed ATC instead of PRN (as needed) to maintain optimal pain relief.
Route of Administration
Common routes of administration and standard abbreviations include the following:
- Oral (PO) – the patient swallows a tablet or capsule
- Sublingual (SL) – applied under the tongue
- Enteral (NG or PEG) – administered via a tube directly into the GI tract
- Rectal (PR) – administered via rectal suppository
- Inhalation (INH) – the patient breathes in medication from an inhaler
- Intramuscular (IM) – administered via an injection into a muscle
- Subcutaneous – administered via injection into the fat tissue beneath the skin (Note that “subcutaneous” is on ISMP’s recommended list of abbreviations to avoid due to common errors.)
- Transdermal (TD) – administered by applying a patch on the skin
For more information about routes of administration and considerations regarding absorption, visit the “Kinetics and Dynamics” chapter in Open RN Nursing Pharmacology.
Provider Name/Signature
The signature of the prescribing provider is required on the order and can be electronic or handwritten. Verbal orders from a prescriber are not recommended but may be permitted in some agencies for urgent situations. Verbal orders require the nurse to “repeat back” the order to the prescriber for confirmation.
Rights of Medication Administration
Each year in the United States, 7,000 to 9,000 people die as a result of a medication error. Hundreds of thousands of other patients experience adverse reactions or other complications related to a medication. The total cost of caring for patients with medication-associated errors exceeds $40 billion each year. In addition to the monetary cost, patients experience psychological and physical pain and suffering as a result of medication errors.[3] Nurses play a vital role in reducing the number of medication errors that occur by verifying several rights of medication.
The Centers for Medicare & Medicaid Services requires nurses to verify specific information prior to the administration of medication to avoid errors, referred to as verifying the rights of medication administration.[4] These rights of medication administration are the vital last safety check by nurses to prevent errors in the chain of medication administration that includes the prescribing provider, the pharmacist, the nurse, and the patient.
It is important to remember that if a medication error occurs resulting in harm to a patient, a nurse can be held liable even if “just following orders.” It is absolutely vital for nurses to use critical thinking and clinical judgment to ensure each medication is safe for each specific patient before administering it. The consequences of liability resulting from a medication error can range from being charged with negligence in a court of law, to losing one’s job, to losing one’s nursing license.
The six rights of medication administration must be verified by the nurse at least three times before administering a medication to a patient. These six rights include the following:
- Right Patient
- Right Drug
- Right Dose
- Right Time
- Right Route[5]
- Right Documentation
Recent literature indicates that up to ten rights should be completed as part of a safe medication administration process. These additional rights include Right History and Assessment, Right Drug Interactions, Right to Refuse, and Right Education and Information. Information for each of these rights is further described below.[6],[7]
Right Patient
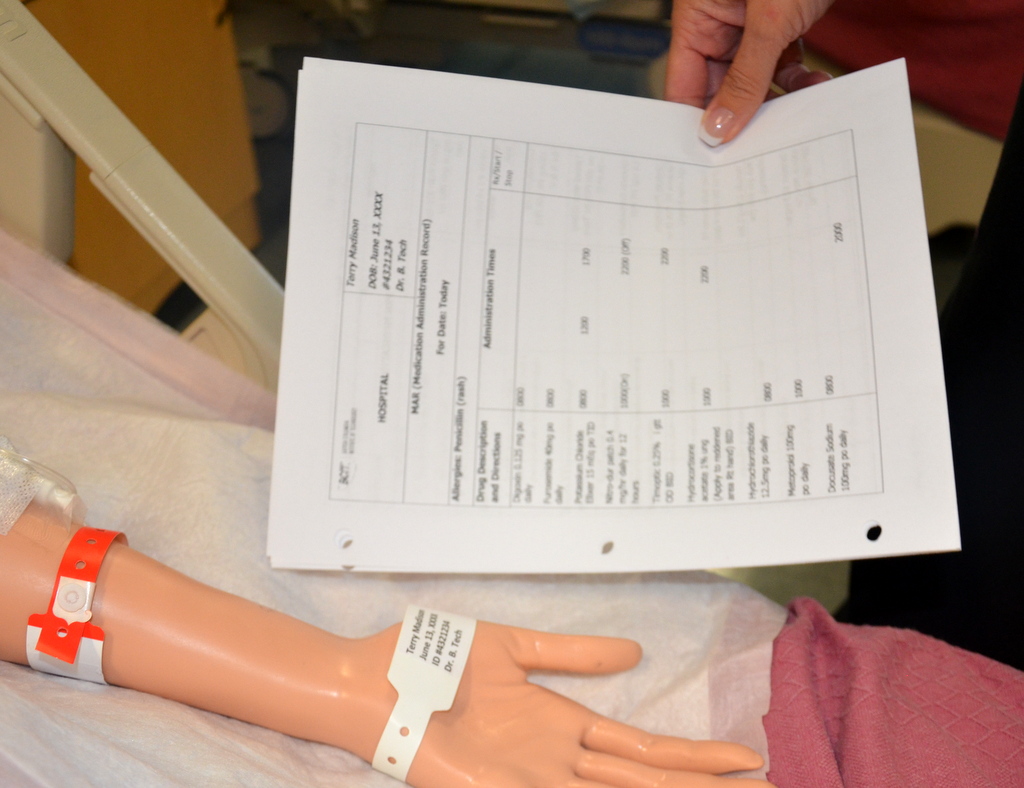
Acceptable patient identifiers include, but are not limited to, the patient’s full name, an identification number assigned by the hospital, or date of birth. A patient’s room number must never be used as an identifier because a patient may change rooms. Identifiers must be confirmed by the patient wristband, patient identification card, patient statement (when possible), or other means outlined in the agency policy such as a patient picture included on the MAR. The nurse must confirm the patient’s identification matches the medication administration record (MAR) and medication label prior to administration to ensure that the medication is being given to the correct patient.[8] See Figure 15.1[9] for an illustration of the nurse verifying the patient’s identify by scanning their identification band and asking for their date of birth. See Figure 15.2[10] for a close-up image of a patient identification wristband.
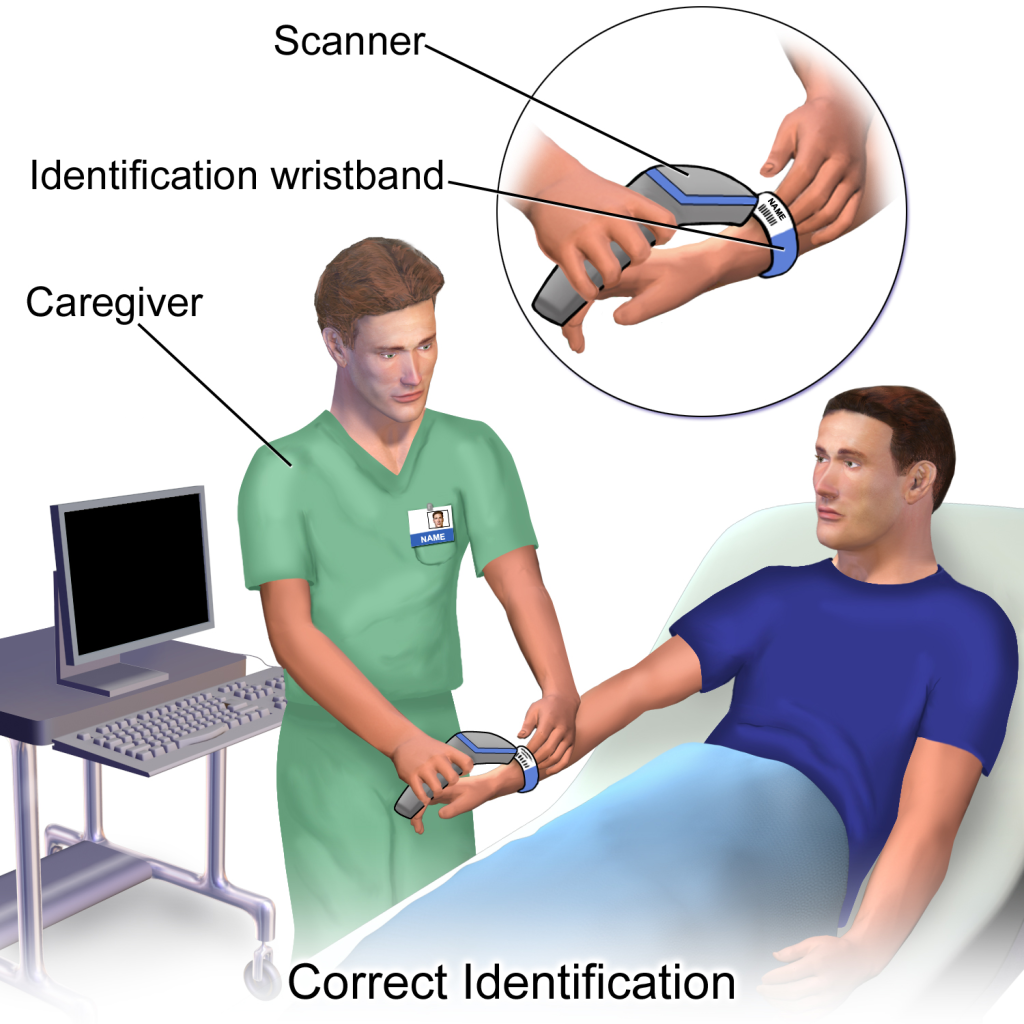

If barcode scanning is used in an agency, this scanning is not intended to take the place of confirming two patient identifiers but is intended to add another layer of safety to the medication administration process. The National Patient Safety Goals established by The Joint Commission state that whenever administering patient medications, at least two patient identifiers should be used.[11]
Right Drug
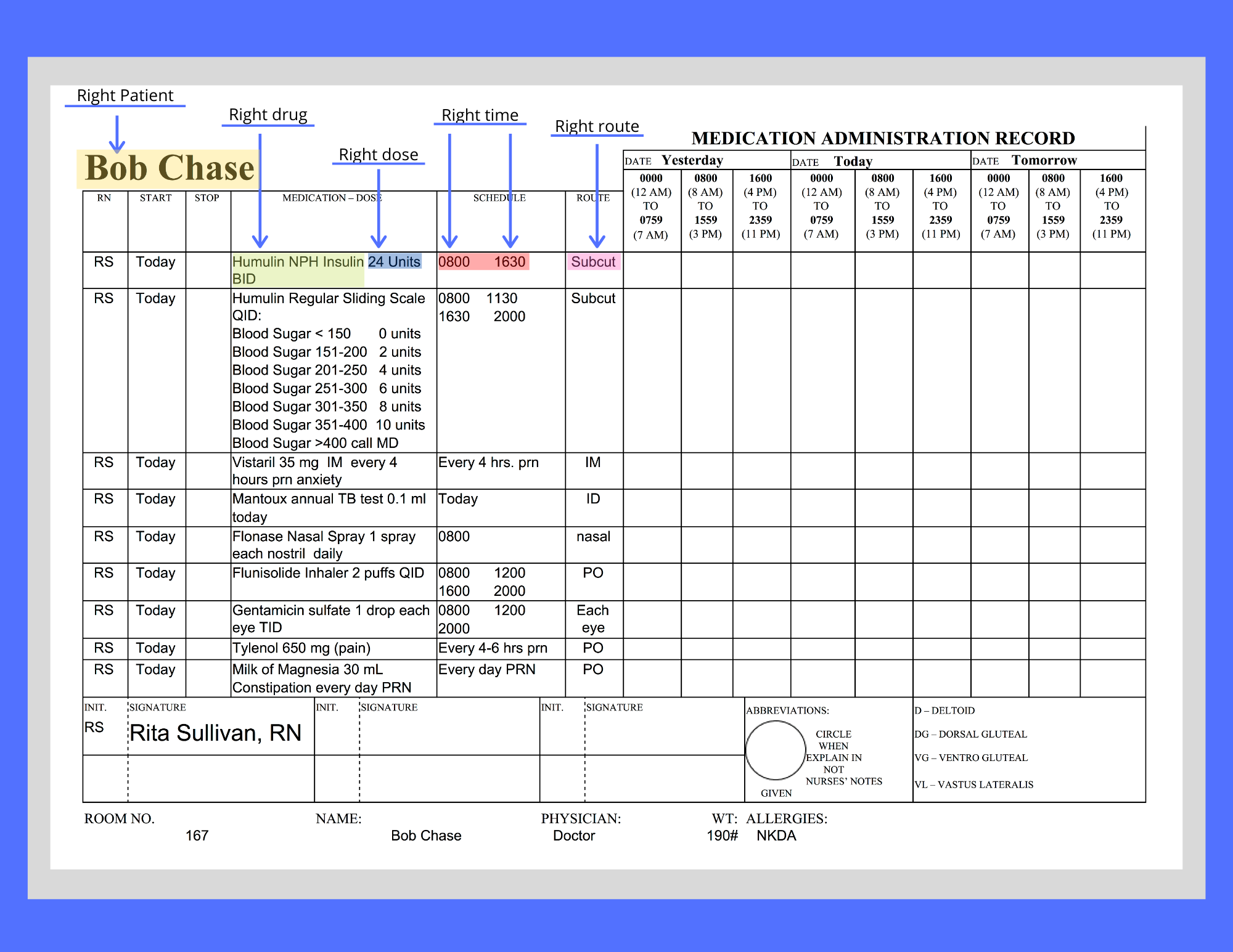
During this step, the nurse ensures the medication to be administered to the patient matches the order or Medication Administration Record (MAR) and that the patient does not have a documented allergy to it. Also, check the expiration date of the medication.[12] The Medication Administration Record (MAR), or eMAR, an electronic medical record, is a specific type of documentation found in a patient’s chart. See Figure 15.3[13] for an image of an MAR and its components. Beware of look-alike and sound-alike medication names, as well as high-alert medications that bear a heightened risk of causing significant patient harm if they are used in error. The nurse should also be aware of what medication can be crushed and those that cannot be crushed. Read more information about these concerns using the box below.
View the ISMP Frequently Confused Medication List.
View a PDF of the ISMP High-Alert Medications List.
View the ISMP Do Not Crush List.
Right Dose
During this step, the nurse ensures the dosage of the medication matches the prescribed dose, verifies the correct dosage range for the age and medical status of the patient, and also confirms that the prescription itself does not reflect an unsafe dosage level (i.e., a dose that is too high or too low).[14] For example, medication errors commonly occur in children, who typically receive a lower dose of medication than an adult. Medication errors also commonly occur in older patients who have existing kidney or liver disease and are unable to metabolize or excrete typical doses of medications.
Right Time and Frequency
During this step, the nurse verifies adherence to the prescribed frequency and scheduled time of administration of the medication.[15] This step is especially important when PRN medications are administered because it is up to the nurse to verify the time of the previous dose and compare it to the ordered frequency.
Medications should be administered on time whenever possible. However, when multiple patients are scheduled to receive multiple medications at the same time, this goal of timeliness can be challenging. Most facilities have a policy that medications can be given within a range of 30 minutes before or 30 minutes after the medication is scheduled. For example, a medication ordered for 0800 could be administered anytime between 0730 and 0830. However, some medications must be given at their specific ordered time due to pharmacokinetics of the drug. For example, if an antibiotic is scheduled every eight hours, this time frame must be upheld to maintain effective bioavailability of the drug, but a medication scheduled daily has more flexibility with time of actual administration.
Right Route
During this step, the nurse ensures the route of administration is appropriate for the specific medication and also for the patient.[16] Many medications can potentially be administered via multiple routes, whereas other medications can only be given safely via one route. Nurses must administer medications via the route indicated in the order. If a nurse discovers an error in the order or believes the route is unsafe for a particular patient, the route must be clarified with the prescribing provider before administration. For example, a patient may have a PEG tube in place, but the nurse notices the medication order indicates the route of administration as PO. If the nurse believes this medication should be administered via the PEG tube and the route indicated in the order is an error, the prescribing provider must be notified, and the order must be revised indicating via PEG tube before the medication is administered.
Right Documentation
After administering medication, it is important to immediately document the administration to avoid potential errors from an unintended repeat dose.
In addition to checking the basic rights of medication administration and documenting the administration, it is also important for nurses to verify the following information to prevent medication errors.
Right History and Assessment
The nurse should be aware of the patient’s allergies, as well as any history of any drug interactions. Additionally, nurses collect appropriate assessment data regarding the patient’s history, current status, and recent lab results to identify any contraindications for the patients to receive the prescribed medication.[17]
Right Drug Interactions
The patient’s history should be reviewed for any potential interactions with medications previously given or with the patient’s diet. It is also important to verify the medication’s expiration date before administration.
Right Education and Information
Information should be provided to the patient about the medication, including the expected therapeutic effects, as well as the potential adverse effects. The patient should be encouraged to report suspected side effects to the nurse and/or prescribing provider. If the patient is a minor, the parent may also have a right to know about the medication in many states, depending upon the circumstances.
Right of Refusal
After providing education about the medication, the patient has the right to refuse to take medication in accordance with the nursing Code of Ethics and respect for individual patient autonomy. If a patient refuses to take the medication after proper education has been performed, the event should be documented in the patient chart and the prescribing provider notified.
Medication Dispensing
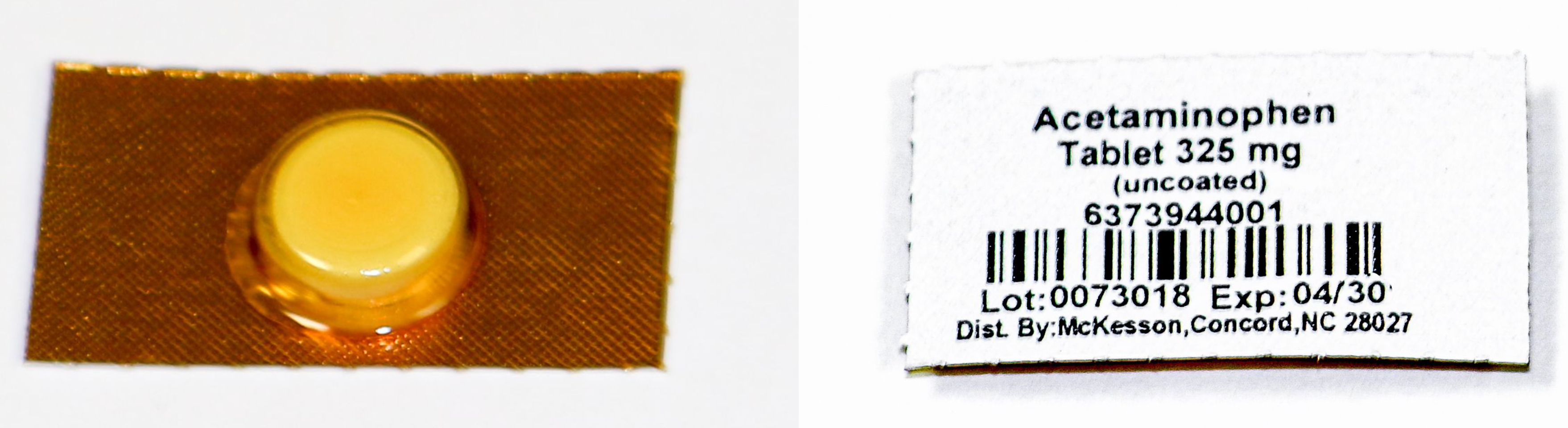
Medications are dispensed for patients in a variety of methods. During inpatient care, unit dose packaging is a common method for dispensing medications. See Figure 15.4[18] for an image of unit dose packaging.
Unit dose dispensing is typically used in association with a medication dispensing system, sometimes referred to in practice with brand names such as “Pyxis” or “Omnicell.” Medication dispensing systems help keep medications secure by requiring a user sign-in and password. They also reduce medication errors by only allowing medications prescribed for a specific patient to be removed unless additional actions are taken. However, it is important to remember that medication errors can still occur when using a medication dispensing system if the incorrect medication is erroneously stocked in a compartment. See Figure 15.5[19] for an image of a medication dispensing system.

Barcodes are often incorporated with unit dose medication dispensing as an additional layer of safety to prevent medication errors. Each patient and medication is identified with a unique bar code. The nurse scans the patient’s identification wristband with a bedside portable device and then scans each medication to be administered. The portable device will display error messages if an incorrect medication is scanned or if medication is scanned at an incorrect time. It is vital for nurses to stop and investigate the medication administration process when an error is received. The scanning device is typically linked to an electronic MAR and the medication administered is documented immediately in the patient’s chart.
In long-term care agencies, weekly blister cards may be used that contain a specific patient’s medications for each day of the week. See Figure 15.6[20] for an image of a blister pack.

Agencies using blister cards or pill bags typically store medications in a locked medication cart to keep them secure. Supplies used to administer medications are also stored on the cart. The MAR is available in printed format or electronically with a laptop computer. See Figure 15.7[21] for an image of a medication cart.

Process of Medication Administration
No matter what method of medication storage and dispensing is used in a facility, the nurse must continue to verify the rights of medication administration to perform an accurate and safe medication pass. Using a medication dispensing system or barcoding does not substitute for verifying the rights but is used to add an additional layer of safety to medication administration. Nurses can also avoid medication errors by creating a habitual process of performing medication checks when administering medication. The rights of medication administration should be done in the following order:
- Perform the first check as the unit dose package, blister pack, or pill bag is removed from the dispensing machine or medication cart. Also, check the expiration date of the medication.
- A second check should be performed after the medication is removed from the dispensing machine or medication cart. This step should be performed prior to pouring or removing from a multidose container. Note: Some high-alert medications, such as insulin, require a second nurse to perform a medication check at this step due to potentially life-threatening adverse effects that can occur if an error is made.
- The third check should be performed immediately before administering the medication to the patient at the bedside or when replacing the multidose container back into the drawer.
See Figure 15.8[22] for an image of a nurse comparing medication information on the medication packet to information on the patient’s MAR.
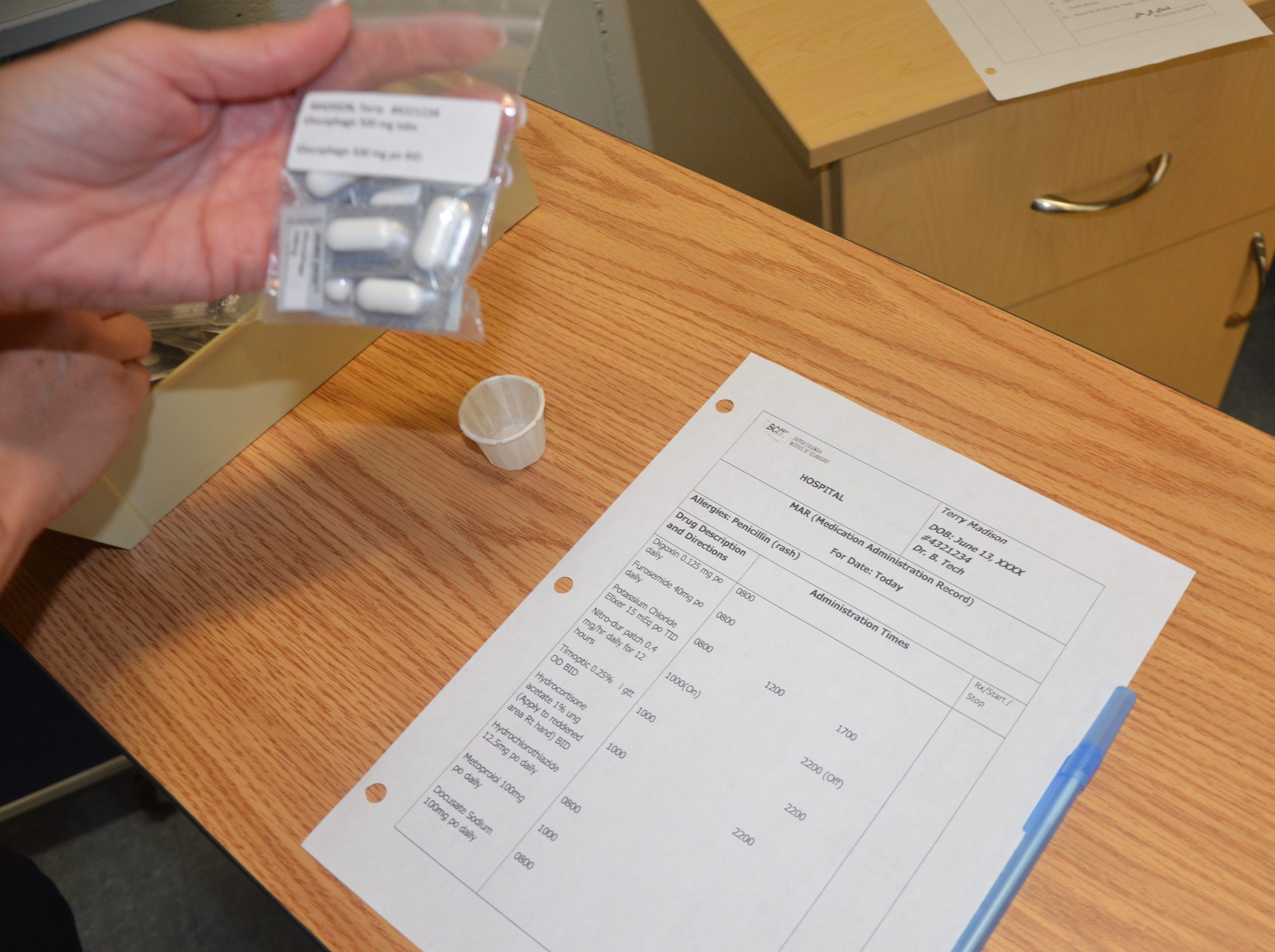
When performing these three checks, the nurse should ensure this is the right medication, right patient, right dosage, right route, and right time. See Figure 15.9[23] for an image of the nurse performing patient identification prior to administering the medication. The sixth right, correct documentation, should be done immediately after the medication is administered to the patient to avoid an error from another nurse inadvertently administering the dose a second time. These six rights completed three times have greatly reduced medication errors.
As discussed earlier, other rights to consider during this process are as follows:
- Is the patient receiving this medication for the right reason?
- Have the right assessments been performed prior to giving the medication?
- Has the patient also received the right education regarding the medications?
- Is the patient exhibiting the right response to the medication?
- Is the patient refusing to take the medication? Patients have the right to refuse medication. The patient’s refusal and any education or explanation provided related to the attempt to administer the medication should be documented by the nurse and the prescribing provider should be notified.
![]()
- Listen to the patient if they verbalize any concerns about medications. Explore their concerns, verify the order, and/or discuss their concerns with the prescribing provider before administering the medication to avoid a potential medication error.
- If a pill falls on the floor, it is contaminated and should not be administered. Dispose the medication according to agency policy.
- Be aware of absorption considerations of the medications you are administering. For example, certain medications such as levothyroxine should be administered on an empty stomach because food and other medications will affect its absorption.
- Nurses are often the first to notice when a patient has difficulty swallowing. If you notice a patient coughs immediately after swallowing water or has a “gurgling” sound to their voice, do not administer any medications, food, or fluid until you have reported your concerns to the heath care provider. A swallow evaluation may be needed, and the route of medication may need to be changed from oral to another route to avoid aspiration.
- If your patient has a nothing by mouth (NPO) order, verify if this includes all medications. This information may be included on the MAR or the orders, and if not, verify this information with the provider. Some medications, such as diabetes medication, may be given with a sip of water in some situations where the patient has NPO status.
- If the route of administration is not accurately listed on the MAR, contact the prescribing provider before administering the medication. For example, a patient may have a PEG tube, but the medication is erroneously listed as “PO” on the order.
For more information regarding classes of medications, administration considerations, and adverse effects to monitor, visit Open RN Nursing Pharmacology.
For information about specific medications, visit DailyMed, a current, evidence-based medication reference.
Special Considerations for Administering Controlled Substances
Controlled substances, also called Scheduled Medications, are kept in a locked system and accounted for using a checks and balance system. Removal of a controlled substance from a medication dispensing system must be verified and documented by a second nurse witness. Removal of a controlled substance from a medication cart needs to be documented on an additional controlled substance record with the patient’s name, the actual amount of substance given, the time it was given, associated pre-assessment data, and the name of the nurse administering the controlled substance.
Controlled substances stored in locked areas of medication carts must also be counted at every shift change by two nurses and then compared to the controlled substance administration record. If the count does not match the documentation record, the discrepancy must be reported immediately according to agency policy.
Additionally, if a partial dose of a controlled substance is administered, the remainder of the substance must be discarded in front of another nurse witness to document the event. This process is called “wasting.” Follow agency policy regarding wasting of controlled substances.
These additional safety measures help to prevent drug diversion, the use of a prescription medication for other than its intended purpose.
For more information about scheduled medications, drug diversion, and substance abuse in health care personnel, visit the “Legal/Ethical” chapter in Open RN Nursing Pharmacology.
Oral Medication Administration
Most medications are administered orally because it is the most convenient and least invasive route for the patient. Medication given orally has a slower onset, typically about 30-60 minutes. Prior to oral administration of medications, ensure the patient has no contraindications to receiving oral medication, is able to swallow, and is not on gastric suction. If the patient has difficulty swallowing (dysphagia), tablets are typically crushed and placed in a substance like applesauce or pudding for easier swallowing (based on the patient’s prescribed diet). However, it is important to verify that a tablet may be crushed by consulting a drug reference or a pharmacist. For example, medications such as enteric-coated tablets, capsules, and sustained-release or long-acting drugs should never be crushed because doing so will affect the intended action of the medication. In this event, the provider must be contacted for a change in route.[24]
View the ISMP Do Not Crush List.
Position the patient receiving oral medication in an upright position to decrease the risk of aspiration. Patients should remain in this position for 30 minutes after medication administration, if possible. If a patient is unable to sit, assist them into a side-lying position. See Figure 15.10[25] for an image of a nurse positioning the patient in an upright position prior to medication administration. Offer a glass of water or other oral fluid (that is not contraindicated with the medication) to ease swallowing and improve absorption and dissolution of the medication, taking any fluid restrictions into account.[26]
Remain with the patient until all medication has been swallowed before documenting to verify the medication has been administered.[27]
If any post-assessments are required, follow up in the appropriate time frame. For example, when administering oral pain medication, follow up approximately 30 minutes to an hour after medication is given to ensure effective pain relief.
If medication is given sublingual (under the tongue) or buccal (between the cheek and gum), the mouth should be moist. Offering the patient a drink of water prior to giving the medication can help with absorption. Instruct the patient to allow the medication to completely dissolve and reinforce the importance of not swallowing or chewing the medication.
Liquid medications are available in multidose vials or single-dose containers. It may be necessary to shake liquid medications if they are suspensions prior to pouring. Make sure the label is clearly written and easy to read. When pouring a liquid medication, it is ideal to place the label in the palm of your hand so if any liquid medication runs down the outside of the bottle it does not blur the writing and make the label unidentifiable. When pouring liquid medication, read the dose at eye level measuring at the meniscus of the poured fluid. Always follow specific agency policy and procedure when administering oral medications.

Rectal Medication Administration
Drugs administered rectally have a faster action than the oral route and a higher bioavailability, meaning a higher amount of effective drug in the bloodstream because it has not been influenced by upper gastrointestinal tract digestive processes. Rectal administration also reduces side effects of some drugs, such as gastric irritation, nausea, and vomiting. Rectal medications may also be prescribed for their local effects in the gastrointestinal system (e.g., laxatives) or their systemic effects (e.g., analgesics when oral route is contraindicated). Rectal medications are contraindicated after rectal or bowel surgery, with rectal bleeding or prolapse, and with low platelet counts.[28]
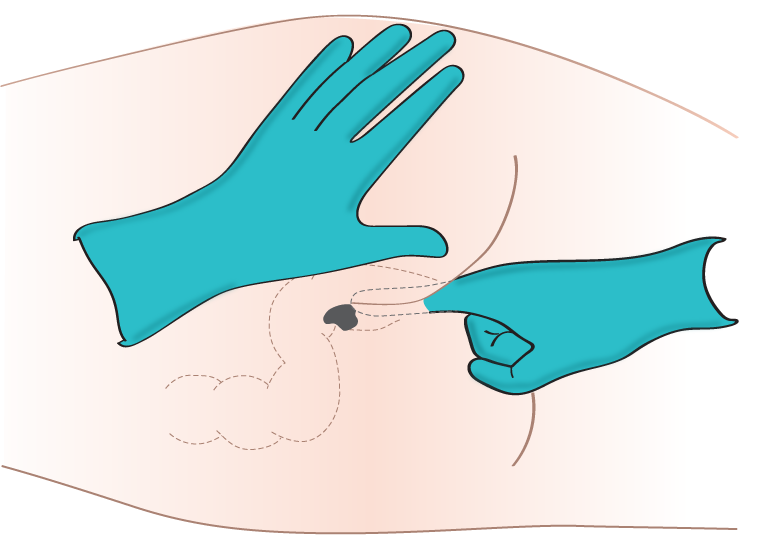
Rectal medications are often formulated as suppositories. Suppositories are small, cone-shaped objects that melt inside the body and release medication. When administering rectal suppositories, the patient should be placed on their left side in the Sims position. See Figure 15.11[29] for an image of patient positioning during rectal medication administration. The suppository and gloved index finger placing the suppository should be lubricated for ease of placement. Suppositories are conical and should be placed into the rectum rounded side first. The suppository should be inserted past the sphincter along the wall of the rectum. After placement, the patient should remain on their side while the medication takes effect. This time period is specific to each medication, but typically is at least 5 minutes. Make sure to avoid placing the suppository into stool. It is also important to monitor for a vasovagal response when placing medications rectally. A vasovagal response can occur when the vagus nerve is stimulated, causing the patient’s blood pressure and heart rate to drop, and creating symptoms of dizziness and perspiration. Sometimes the patient can faint or even have a seizure. Patients with a history of cardiac arrhythmias should not be administered rectal suppositories due to the potential for a vasovagal response. Always follow agency policy and procedure when administering rectal medications.[30],[31]
Another type of rectal medication is an enema. An enema is the administration of a substance in liquid form into the rectum. Many enemas are formulated in disposable plastic containers. Warming the solution to body temperature prior to administration may be beneficial because cold solution can cause cramping. It is also helpful to encourage the patient to empty their bladder prior to administration to reduce feelings of discomfort. Place an incontinence pad under the patient and position them on their left side in the Sims position. Lubricate the nozzle of the container and expel air. Insert the lubricated nozzle into the rectum slowly and gently expel the contents into the rectum. Ask the patient to retain the enema based on manufacturer’s recommendations.
Enteral Tube Medication Administration
Medication is administered via an enteral tube when the patient is unable to orally swallow medication. Medications given through an enteral feeding tube (nasogastric, nasointestinal, percutaneous endoscopic gastrostomy {PEG}, or jejunostomy {J} tube) should be in liquid form whenever possible to avoid clogging the tube. If a liquid form is not available, medications that are safe to crush should be crushed finely and dissolved in water to keep the tube from becoming clogged. If a medication is not safe to crush, the prescribing provider should be notified and a prescription for alternative medication obtained. Capsules should be opened and emptied into liquid as indicated prior to administration, and liquids should be administered at room temperature. Keep in mind that some capsules are time-released and should not be opened. In this case, contact the provider for a change in order.[32],[33]
As always, follow agency policy for this medication administration procedure. Position the patient to at least 30 degrees and in high Fowler’s position when feasible. If gastric suctioning is in place, turn off the suctioning. See Figure 15.12[34] for an image of a nurse positioning the patient prior to administration of medications via a PEG tube. Follow the tube to the point of entry into the patient to ensure you are accessing the correct tube.[35],[36]
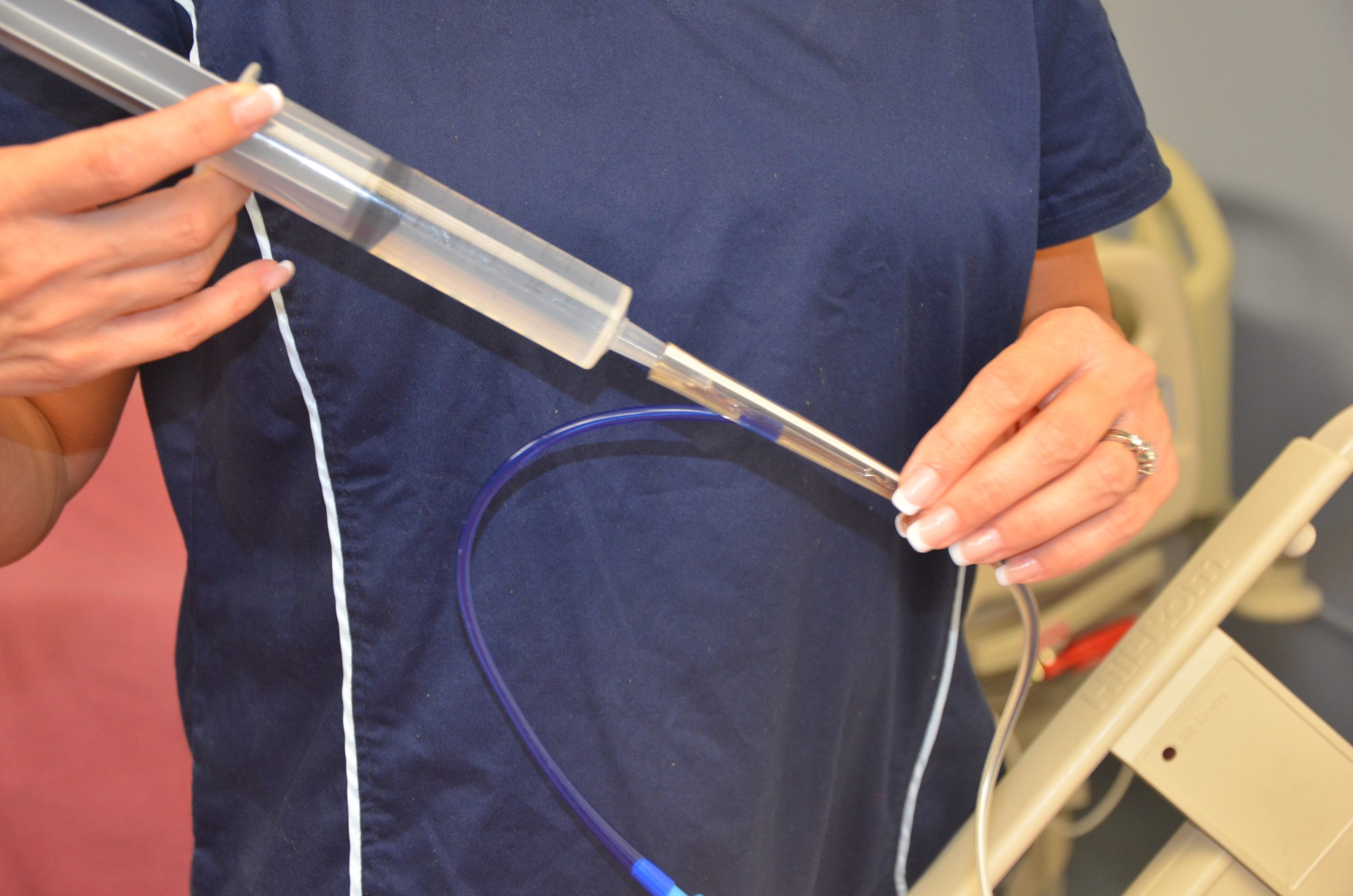
Prior to medication administration, verify tube placement. Placement is initially verified immediately after the tube is placed with an X-ray, and the nurse should verify these results. Additionally, bedside placement is verified by the nurse before every medication pass. There are multiple evidence-based methods used to check placement. One method includes aspirating tube contents with a 60-mL syringe and observing the fluid. Fasting gastric secretions appear grassy-green, brown, or clear and colorless, whereas secretions from a tube that has perforated the pleural space typically have a pale yellow serous appearance. A second method used to verify placement is to measure the pH of aspirate from the tube. Fasting gastric pH is usually 5 or less, even in patients receiving gastric acid inhibitors. Fluid aspirated from a tube in the pleural space typically has a pH of 7 or higher.[37],[38] Note that installation of air into the tube while listening over the stomach with a stethoscope is no longer considered a safe method to check tube placement according to evidence-based practices.[39]
After tube placement is checked, a clean 60-mL syringe is used to flush the tube with a minimum of 15 mL of water (5-10 mL for children) before administering the medication. Follow agency policy regarding flushing amount. Liquid medication, or appropriately crushed medication dissolved in water, is administered one medication at a time. Medication should not be mixed because of the risks of physical and chemical incompatibilities, tube obstruction, and altered therapeutic drug responses. Between each medication, the tube is flushed with 15 mL of water, keeping in mind the patient’s fluid volume status. After the final medication is administered, the tube is flushed with 15 mL of water. The tube is then clamped, or if the patient is receiving tube feeding, it can be restarted. If the patient is receiving gastric suctioning, it can be restarted 30 minutes after medication administration.[40],[41],[42] See Figure 15.13[43] for an image of a nurse administering medication via an enteral tube.
Special considerations during this procedure include the following:
- If the patient has fluid restrictions, the amount of fluid used to flush the tube between each medication may need to be modified to avoid excess fluid intake.
- If the tube is attached to suctioning, the suctioning should be left off for 20 to 30 minutes after the medication is given to promote absorption of the medication.
- If the patient is receiving tube feedings, review information about the drugs that are being administered. If they cannot be taken with food or need to be taken on an empty stomach, the tube feeding running time will need to be adjusted.
- Be sure to document the amount of water used to flush the tube during the medication pass on the fluid intake record.
- If the patient has a chronic illness or is immunosuppressed, sterile water is suggested for use of mixing and flushing instead of tap water.
- Enteric-coated medications and other medications on the “Do Not Crush List” should not be crushed for this procedure. Instead, the prescribing provider must be notified and an order for a different form of the medication must be obtained.
- If the tube becomes clogged, attempt to flush it with water. If unsuccessful, notify the provider and a pancreatic enzyme solution or kit may be ordered before a new tube is placed.[44]

View a supplementary YouTube video on Crushing Medications[45]
Preventing Medication Errors
Medication errors can occur at various stages of the medication administration process, beginning with the prescribing provider, to the pharmacist preparing the medication, to the pharmacy technician stocking the medication, to the nurse administering the medication. Medication errors are most common at the ordering or prescribing stage. Typical errors include the prescribing provider writing the wrong medication, wrong route or dose, or the wrong frequency. These ordering errors account for almost 50% of medication errors. Data shows that nurses and pharmacists identify anywhere from 30% to 70% of medication-ordering errors.[46]
One of the major causes for medication errors is a distraction. Nearly 75% of medication errors have been attributed to this cause.[47] To minimize distractions, hospitals have introduced measures to reduce medication errors. For example, some hospitals set a “no-interruption zone policy” during medication dispensing and preparation and ask health care team members to only disrupt the medication administration process for emergencies. To reduce medication errors, agencies are also adopting many initiatives developed by the World Health Organization (WHO),[48] Institute for Safe Medication Practices (ISMP), Institute of Medicine (IOM),[49] and several other organizations. Initiatives include measures such as avoiding error-prone abbreviations, being aware of commonly confused medication names, and instituting additional safeguards for high-alert medications. Student nurses must also be aware of conditions that may contribute to making a medication error during their clinical courses. Read more about initiatives to prevent medication errors in the boxes and videos provided below.
For more information about preventing medication errors as a student nurse, visit IMSP’s Error-Prone Conditions that Lead to Student Nurse-Related Errors.
When you prepare to administer medications to your patients during clinical, your instructor will ask you questions to ensure safe medication administration. View a supplementary YouTube video of a nursing instructor asking a student typical medication questions.
View a supplementary YouTube video from the WHO on Administering Medications Without Harm[50]
Reporting Medication Errors
Despite multiple initiatives that have been instituted to prevent medication errors, including properly checking the rights of medication administration, medication errors happen. Examples of common errors include administering the wrong dose or an unsafe dose, giving medication to the wrong patient, administering medication by the wrong route or at the incorrect rate, and giving a drug that is expired. If a medication error occurs, the nurse must follow specific steps of reporting according to agency policy. In the past when medication errors occurred, the individual who caused it was usually blamed for the mishap and disciplinary action resulted. However, this culture of blame has shifted, and many medication errors by well-trained and careful nurses and other health care professions are viewed as potential symptoms of a system-wide problem. This philosophy is referred to as an institution’s safety culture. Thus, rather than focusing on disciplinary action, agencies are now trying to understand how the system failed causing the error to occur. This approach is designed to introduce safeguards at every level so that a mistake can be caught before the drug is given to the patient, which is often referred to as a “near miss.” For an agency to effectively institute a safety culture, all medication errors and near misses must be reported.
When a medication error occurs, the nurse’s first response should be to immediately monitor the patient’s condition and watch for any side effects from the medication. Secondly, the nurse must notify the nurse manager and prescribing provider of the error. The provider may provide additional orders to counteract the medication’s effects or to monitor for potential adverse reactions. In some situations, family members of the patient who are legal guardians or powers of attorney should also be notified. Lastly, a written report should be submitted documenting the incident, often referred to as an incident report. Incident reports are intended to identify if patterns of errors are occurring due to system-wide processes that can be modified to prevent future errors.
For more information about safety culture, visit the following section of the “Legal/Ethical” chapter in Open RN Nursing Pharmacology.
Life Span Considerations
Children
It can be difficult to persuade children to take medications. It is often helpful for medications to be prescribed in liquid or chewable form. For example, droppers are used for infants or very young children; the medication should be placed between the gum and cheek to prevent aspiration. Mixing medication with soft foods can also be helpful to encourage the child to swallow medications, but it is best to avoid mixing the medication with a staple food in the child’s diet because of potential later refusal of the food associated with medication administration. It can be helpful to offer the child a cool item, such as a popsicle or frozen fruit bar, prior to medication administration to numb the child’s tongue and decrease the taste of the medication. Other clinical tips for medication administration include asking the caregiver how the child takes medications at home and mimicking this method or asking the caregiver to administer the medication if the child trusts them more than the nurse. Oral syringes (without needles attached) may be used to administer precise dosages of medication to children. See Figure 15.14[51] of a nurse administering oral medication to a child with an oral syringe. When administering medication with an oral syringe, remember to remove the cap prior to administration because this could be a choking hazard. It is also important to educate the caregiver of the child how to properly administer the medication at the correct dosage at home.

Older Adults
Many older adults have a “polypharmacy,” meaning many medications to keep track of and multiple times these medications need to be taken per day. Nurses should help patients set up a schedule to remember when to take the medications. Organizing medications in medication boxes by day and time is a very helpful strategy. See Figure 15.15[52] of a medication box. Nurses can suggest to patients to have all medications filled at the same pharmacy to avoid drug-drug interactions that can occur when multiple providers are prescribing medications.
Older adults often have difficulty swallowing, so obtaining a prescription for liquid medication or crushing the medication when applicable and placing it in applesauce or pudding is helpful. Allow extra time when administering medication to an older adult to give them time to ask questions and to swallow multiple pills. Monitor for adverse effects and drug interactions in older adults, who are often taking multiple medications and may have preexisting kidney or liver dysfunction.
Be sure to address the economic needs of an older adult as it relates to their medications. Medications can be expensive, and many older adults live on a strict budget. Nurses often advocate for less expensive alternatives for patients, such as using a generic brand instead of a name brand or a less expensive class of medication. Be aware that an older adult with financial concerns may try to save money by not taking medications as frequently as prescribed. Also, the older adult may “feel good” on their medications and think they don’t need to monitor or take medications because they are “cured.” Reinforce that “feeling good” usually means the medication is working as prescribed and should continue to be taken. Finally, empower patients to take control of managing their health by providing education and ongoing support.

- NCSBN.(2018). 2019 NCLEX-RN test plan. https://www.ncsbn.org/2019_RN_TestPlan-English.pdf ↵
- Centers for Medicare & Medicaid Services. (2014, March 14). Memo: Requirements for hospital medication administration, particularly intravenous (IV) medications and post-operative care of patients receiving IV opioids. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-14-15.pdf ↵
- This work is a derivative of StatPearls by Tariq, Vashisht, Sinha, and Scherbak and is licensed under CC BY 4.0 ↵
- Centers for Medicare & Medicaid Services. (2014, March 14). Memo: Requirements for hospital medication administration, particularly intravenous (IV) medications and post-operative care of patients receiving IV opioids. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-14-15.pdf ↵
- Centers for Medicare & Medicaid Services. (2014, March 14). Memo: Requirements for hospital medication administration, particularly intravenous (IV) medications and post-operative care of patients receiving IV opioids. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-14-15.pdf ↵
- Vera, M. (2020, June 30). The 10 rights of drug administration. Nurselabs. https://nurseslabs.com/10-rs-rights-of-drug-administration/ ↵
- Butcher, H., Bulechek, G., Dochterman, J., & Wagner, C. (2018). Nursing interventions classification (NIC). Elsevier, pp.250-251,257-258. ↵
- Centers for Medicare & Medicaid Services. (2014, March 14). Memo: Requirements for hospital medication administration, particularly intravenous (IV) medications and post-operative care of patients receiving IV opioids. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-14-15.pdf ↵
- “Patient Identification.png” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- “Wrist Identification Band.jpg” by Whoisjohngalt is licensed under CC BY-SA 4.0 ↵
- The Joint Commission. (n.d.). National patient safety goals. https://www.jointcommission.org/standards/national-patient-safety-goals/ ↵
- Centers for Medicare & Medicaid Services. (2014, March 14). Memo: Requirements for hospital medication administration, particularly intravenous (IV) medications and post-operative care of patients receiving IV opioids. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-14-15.pdf ↵
- “MAR.png” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- Centers for Medicare & Medicaid Services. (2014, March 14). Memo: Requirements for hospital medication administration, particularly intravenous (IV) medications and post-operative care of patients receiving IV opioids. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-14-15.pdf ↵
- Centers for Medicare & Medicaid Services. (2014, March 14). Memo: Requirements for hospital medication administration, particularly intravenous (IV) medications and post-operative care of patients receiving IV opioids. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-14-15.pdf ↵
- Centers for Medicare & Medicaid Services. (2014, March 14). Memo: Requirements for hospital medication administration, particularly intravenous (IV) medications and post-operative care of patients receiving IV opioids. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-14-15.pdf ↵
- NCSBN. (2018). 2019 NCLEX-RN test plan. https://www.ncsbn.org/2019_RN_TestPlan-English.pdf ↵
- “Unit Dose Packaging.jpg” and “Unit Dose Label.jpg” by Deanna Hoyord, Chippewa Valley Technical College are licensed under CC BY 4.0 ↵
- “Med Cart 1_313A0209.jpg” and “Med Cart Drawer._313A0224.jpg” by Deanna Hoyord, Chippewa Valley Technical College are licensed under CC BY 4.0 ↵
- “Medication_blister_pack_2.jpg” by Sprinno is licensed under CC BY-SA 3.0 ↵
- “MMI medication cart.JPG” by BrokenSphere is licensed under CC BY-SA 3.0 ↵
- “DSC_17601-150x150.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/6-1-safe-medication-adminstration/ ↵
- “Book-pictures-2015-430-150x150.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0.. Access for free at https://opentextbc.ca/clinicalskills/chapter/6-1-safe-medication-adminstration/ ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- “DSC_17631-150x150.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/6-1-safe-medication-adminstration/ ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- “Administering-med-rectally-2.png” by British Columbia Institute of Technology is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- Butcher, H., Bulechek, G., Dochterman, J., & Wagner, C. (2018). Nursing interventions classification (NIC). Elsevier, pp.250-251, 257-258. ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053 ↵
- “degreeLow.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/3-4-positioning-a-patient-in-bed/ ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053 ↵
- ABoullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T.J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053 ↵
- Butcher, H., Bulechek, G., Dochterman, J., & Wagner, C. (2018). Nursing interventions classification (NIC). Elsevier, pp. 250-251, 257-258. ↵
- “Administering medication into a gastric tube.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053 ↵
- RegisteredNurseRN. (2017, March 22). Crushing medications for tube feeding and oral administration [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/86RzAgHu75U ↵
- This work is a derivative of StatPearls by Tariq, Vashisht, Sinha, and Scherbak and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Tariq, Vashisht, Sinha, and Scherbak and is licensed under CC BY 4.0 ↵
- World Health Organization (n.d.). Patient safety. https://www.who.int/patientsafety/medication-safety/technical-reports/en/ ↵
- IOM. Institute of Medicine. (2007). Preventing medication errors. The National Academies Press. https://doi.org/10.17226/11623 ↵
- World Health Organization (WHO). (2017, October 6). WHO: Medication without harm [Video]. YouTube. All rights reserved. https://youtu.be/MWUM7LIXDeA ↵
- “USMC-080623-M-9467O-024.jpg” by Lance Cpl. Regina A. Ochoa for the United States Marine Corps is in the Public Domain. ↵
- “pills-4005382_960_720.jpg” by Nemo73 is licensed under CC0 ↵
Health care costs impact both macroeconomics (affecting the entire country and society as a whole) and microeconomics (affecting the financial decisions of businesses and individuals). Health care services are funded by several payment models, including federal government programs (e.g., Medicare and Medicaid), private health insurance (typically provided by employers), and self-pay. Payment models also impact services provided by health care agencies, as well as the services and medications available to consumers. Nurses must be aware of these payment models because of the impact on the allocation of resources they need to provide patient care.
Government Funding
Medicare and Medicaid were signed into law in 1965. These programs provide eligible Americans support for their health care needs with taxpayer funding.
Medicare
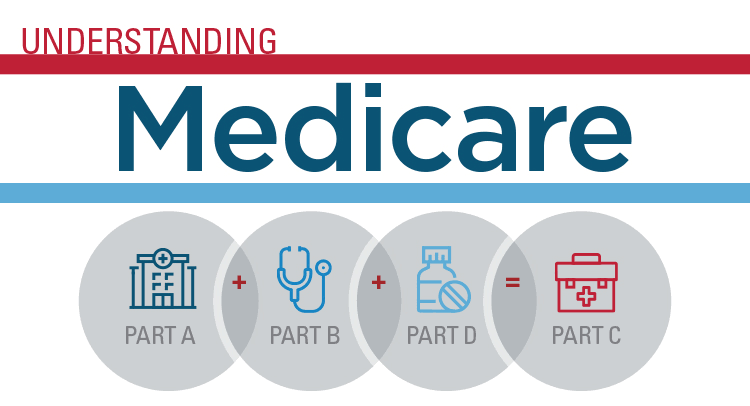
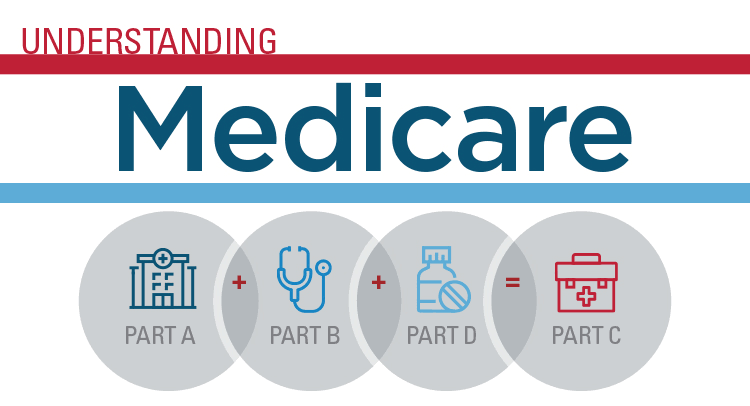
Medicare is a federal health insurance program used by people aged 65 and older, younger individuals with permanent disabilities, and people with end-stage renal disease requiring dialysis or kidney transplantation. Medicare coverage has four possible components: Part A, Part B, Part C, and Part D.[1] See Figure 8.5[2] for an infographic illustrating Medicare Parts A, B, C, and D.
- Part A (Hospital Insurance): Part A covers patients’ hospital stays, skilled nursing facility care, hospice care, and some home health care. Part A is free for clients if they or their spouse paid Medicare taxes for a specific amount of time while working. If clients are not eligible for free coverage, they can buy it with premiums based on the number of months they paid Medicare taxes.
- Part B (Medical Insurance): Part B covers doctors’ services, outpatient care, medical supplies, and preventative care services. Most people pay a standard premium for Part B.
- Part C (Medicare Advantage Plan): A Medicare Advantage Plan is a health plan choice offered by private companies approved by Medicare, also referred to as "Part C." These plans provide Part A and Part B coverage, and most also include Part D coverage. Medicare Advantage Plans may offer extra coverage, such as vision, hearing, dental, and/or health and wellness programs.
- Part D (Prescription Drug Coverage): Part D helps cover the cost of prescription drugs and vaccinations. To get Medicare drug coverage, clients must enroll in a Medicare-approved plan that offers drug coverage. Different plans vary in cost and what prescription medications they cover, also referred to as a formulary.
Read more about Medicare at medicare.gov.
Medicaid
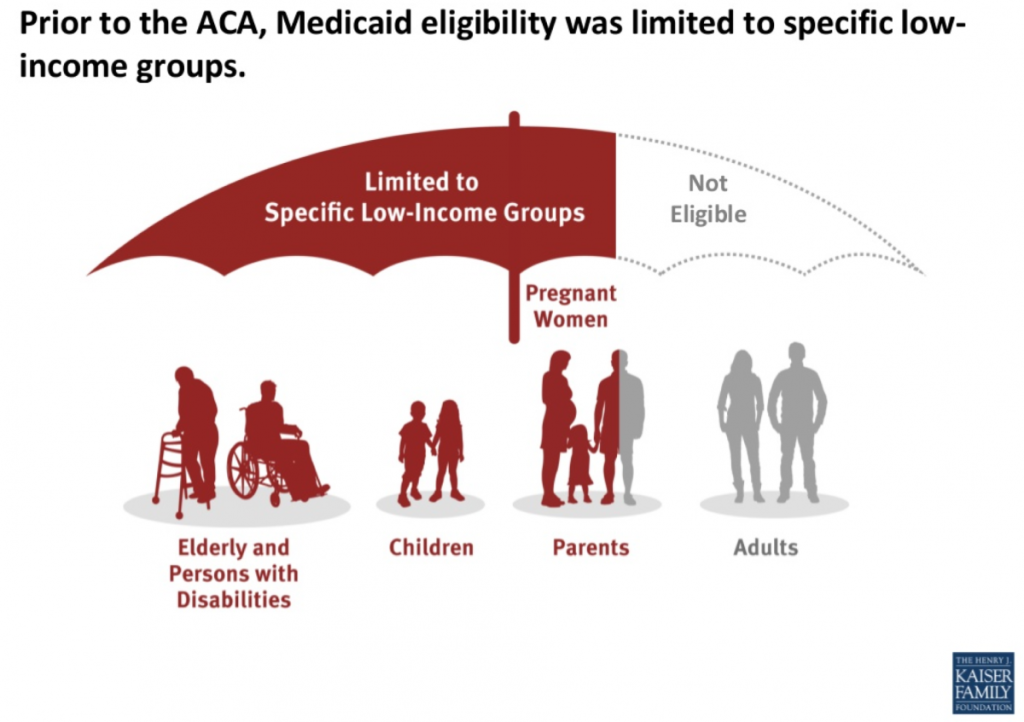
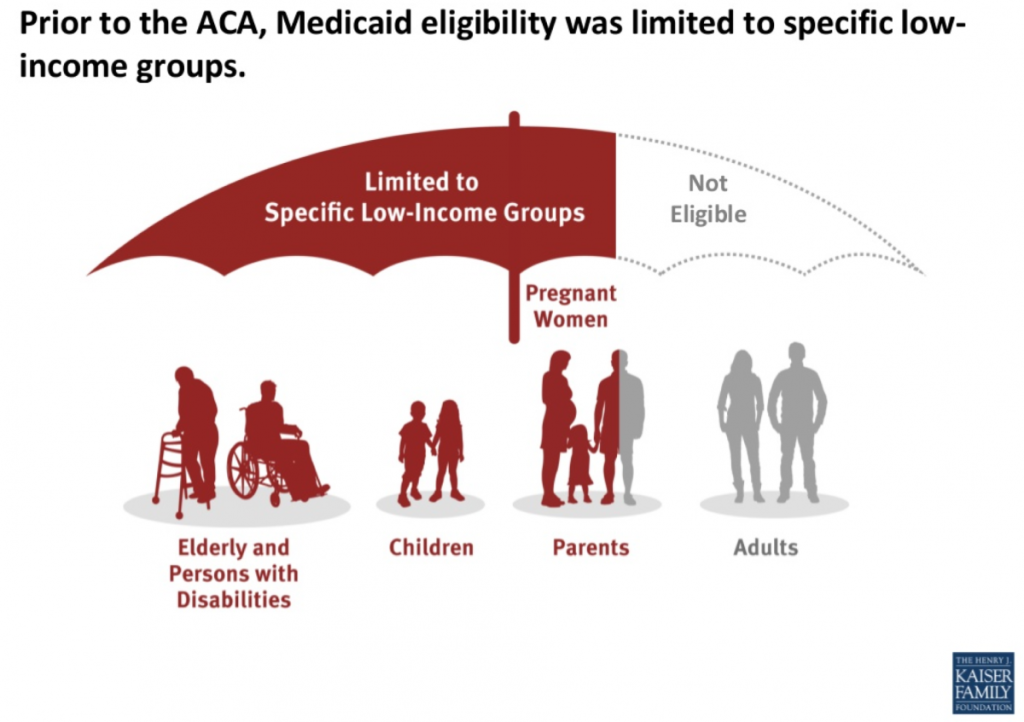
Medicaid is the largest source of health coverage in the United States. It is a joint federal and state program covering eligible individuals with taxpayer funding. To participate in Medicaid, federal law requires states to cover certain groups of individuals, such as low-income families, qualified pregnant women and children, and individuals receiving Supplemental Security Income (SSI). States may choose to cover additional groups, such as individuals receiving home and community-based services and children in foster care who are not otherwise eligible.[3]
In 2014 the Affordable Care Act expanded Medicaid to cover all low-income Americans under the age of 65 years and also expanded coverage for children. Due to the individual states’ involvement in Medicaid, coverage of services varies from state to state.[4] See Figure 8.6[5] for an illustration of Medicaid-eligible populations.
Individuals with Medicaid plans have support in paying for a variety of health services, including hospital care, laboratory and diagnostic testing, skilled nursing care, home health services, preventative care, and regular outpatient provider visits.
Other Government Health Funding
There are several other types of health coverage provided by federal and state programs. Read more about these programs in the following box.
Other Federal and State Health Care Funding Programs[6]
- State Children’s Health Insurance Program (CHIP): A program designed to help provide coverage for uninsured children whose family income is below average but too high to qualify for Medicaid. The federal government provides matching funds to states for health insurance for these families.
Read more details at InsuredKidsNow.gov.
- Children and Youth With Special Health Care Needs: This program coordinates funding and resources to provide care to people with special health needs.
Read more details at Children With Special Health Care Needs.
- Tricare: This program covers about 9 million active duty and retired military personnel and their families.
Read more details at TRICARE.
- Veterans Health Administration (VHA): This government-operated health care system provides comprehensive health services to eligible military veterans. About 9 million veterans are enrolled.
Read more details at Veterans Health Administration.
- Indian Health Service: This system of government hospitals and clinics provides health services to about 2 million Native Americans living on or near a reservation.
Read more details at Indian Health Service.
- Federal Employee Health Benefits (FEHB) Program: This program allows private insurers to offer insurance plans within guidelines set by the government for the benefit of active and retired federal employees and their survivors.
Read more details at The Federal Employees Health Benefits (FEHB) Program.
- Refugee Health Promotion Program: This program provides short-term health insurance to newly arrived refugees.
Read more details at Refugee Health Promotion Program (RHP).
Private Insurance
Individuals who are not eligible for government-funded health programs like Medicare or Medicaid can purchase private health insurance. Many individuals with private insurance obtain coverage through their employers’ benefit packages, where the costs for coverage are shared between the employer and the employee. If an individual does not receive health insurance through their employer, they may purchase it from the Marketplace established by the Affordable Care Act.
Read more about obtaining health insurance through the ACA Marketplace at healthcare.gov.
Self-Pay
Some individuals do not have health care coverage provided by their employer, do not qualify for Medicare or Medicaid, and do not elect to purchase health insurance coverage. Instead, these individuals go without coverage and pay health care costs as they arise. See Figure 8.7[7] for a graph illustrating the decreasing numbers of uninsured consumers in the United States over the past several decades. Unfortunately, due to the skyrocketing cost of health care services, significant bills can accrue from a single serious illness or traumatic injury that can put consumers without health care coverage in jeopardy of bankruptcy. Nurses can assist uninsured individuals to better understand coverage options by referring them to a case manager or social worker.

Types of Insurance Coverage
Health insurance plans have different types of coverage. Common types of health insurance plans are HMO, PPO, POS, HDHP, or HSA.
- Health Maintenance Organization (HMO): HMO plans usually have the lowest monthly cost for coverage (i.e., premium) but also have a smaller network of providers and hospitals where the consumer may receive insured care. This means the consumer is restricted to receive care only from specific providers and health facilities. Many HMOs also require the consumer to see their primary care provider to request a referral to see a specialist, which may or may not be approved by the HMO. Additionally, many tests, procedures, surgeries, and medications require “preauthorization” by the HMO, which may or may not be approved. Due to these restrictions, consumers may find they sacrifice flexibility and choice for lower cost of coverage.[8]
- Preferred Provider Organization (PPO): PPO plans are typically less restrictive than HMOs. PPOs typically include “in-network” providers and hospitals where costs are lower if care is received in-network, but consumers also have a choice to receive “out-of-network” care at a higher cost. Referrals from a primary care provider are not generally required in a PPO. The monthly premium for a PPO plan is typically higher than an HMO plan, but PPOs allow more consumer flexibility in choosing their health care providers.[9]
- Point of Service (POS): POS plans are a combination of HMO and PPO plans, where the insured consumer has a preferred provider network to receive health care services at a lower cost, but also has the flexibility to receive care outside of their network. When consumers venture outside of the network, they often have to pay a significant share of the cost.[10]
- High Deductible Health Plan (HDHP): HDHP plans are often popular for younger individuals without chronic health care needs who spend little on health care but require coverage in the event a high-cost injury or illness occurs. HDHPs typically have lower monthly premiums but require the individual to pay more upfront for health care services before the coverage kicks in (referred to as a “deductible”). Individuals with an HDHP often have an associated Health Savings Account (HSA). HDHPs have grown in popularity as more employers offer these plans in an attempt to contain health care costs by shifting more cost-sharing to the consumer.
- Health Savings Account (HSA): An HSA is a special account reserved for eligible medical expenses with strict usage rules. Money placed in an HSA can often be deducted from a consumer’s pretaxed pay, resulting in tax savings. In addition to purchasing items like glasses, contacts, and over-the-counter medications, HSAs can often be used to pay for deductibles. Some employers deposit a specified amount of money into an employee’s HSA every year to help reimburse high deductibles.
Deductible and Copays
Costs paid by an insured individual are commonly referred to as “out-of-pocket expenses.” Out-of-pocket expenses include deductibles and co-pays. A deductible is the amount of money a consumer pays before the health care plan pays anything. Deductibles generally apply per person per calendar year. Typically, a PPO has higher premiums but lower deductibles than a HDHP.
A co-pay is a flat fee the consumer pays at the time of the health care service. For example, when visiting a primary provider, the consumer may pay $20 to the provider at each visit as a co-pay. Some health care plans require co-pays in addition to deductibles.
Nursing Considerations
Understanding a client’s health insurance coverage is important because it may impact their choice of health services and their ability to purchase medications and other supplies. Additionally, if a client is self-pay, it is helpful to refer them to resources such as case managers, social workers, or the financial department of the agency. These resources can assist them in obtaining affordable health care coverage through the ACA Marketplace or other government programs.
Health care costs impact both macroeconomics (affecting the entire country and society as a whole) and microeconomics (affecting the financial decisions of businesses and individuals). Health care services are funded by several payment models, including federal government programs (e.g., Medicare and Medicaid), private health insurance (typically provided by employers), and self-pay. Payment models also impact services provided by health care agencies, as well as the services and medications available to consumers. Nurses must be aware of these payment models because of the impact on the allocation of resources they need to provide patient care.
Government Funding
Medicare and Medicaid were signed into law in 1965. These programs provide eligible Americans support for their health care needs with taxpayer funding.
Medicare
Medicare is a federal health insurance program used by people aged 65 and older, younger individuals with permanent disabilities, and people with end-stage renal disease requiring dialysis or kidney transplantation. Medicare coverage has four possible components: Part A, Part B, Part C, and Part D.[11] See Figure 8.5[12] for an infographic illustrating Medicare Parts A, B, C, and D.
- Part A (Hospital Insurance): Part A covers patients’ hospital stays, skilled nursing facility care, hospice care, and some home health care. Part A is free for clients if they or their spouse paid Medicare taxes for a specific amount of time while working. If clients are not eligible for free coverage, they can buy it with premiums based on the number of months they paid Medicare taxes.
- Part B (Medical Insurance): Part B covers doctors’ services, outpatient care, medical supplies, and preventative care services. Most people pay a standard premium for Part B.
- Part C (Medicare Advantage Plan): A Medicare Advantage Plan is a health plan choice offered by private companies approved by Medicare, also referred to as "Part C." These plans provide Part A and Part B coverage, and most also include Part D coverage. Medicare Advantage Plans may offer extra coverage, such as vision, hearing, dental, and/or health and wellness programs.
- Part D (Prescription Drug Coverage): Part D helps cover the cost of prescription drugs and vaccinations. To get Medicare drug coverage, clients must enroll in a Medicare-approved plan that offers drug coverage. Different plans vary in cost and what prescription medications they cover, also referred to as a formulary.
Read more about Medicare at medicare.gov.
Medicaid
Medicaid is the largest source of health coverage in the United States. It is a joint federal and state program covering eligible individuals with taxpayer funding. To participate in Medicaid, federal law requires states to cover certain groups of individuals, such as low-income families, qualified pregnant women and children, and individuals receiving Supplemental Security Income (SSI). States may choose to cover additional groups, such as individuals receiving home and community-based services and children in foster care who are not otherwise eligible.[13]
In 2014 the Affordable Care Act expanded Medicaid to cover all low-income Americans under the age of 65 years and also expanded coverage for children. Due to the individual states’ involvement in Medicaid, coverage of services varies from state to state.[14] See Figure 8.6[15] for an illustration of Medicaid-eligible populations.
Individuals with Medicaid plans have support in paying for a variety of health services, including hospital care, laboratory and diagnostic testing, skilled nursing care, home health services, preventative care, and regular outpatient provider visits.
Other Government Health Funding
There are several other types of health coverage provided by federal and state programs. Read more about these programs in the following box.
Other Federal and State Health Care Funding Programs[16]
- State Children’s Health Insurance Program (CHIP): A program designed to help provide coverage for uninsured children whose family income is below average but too high to qualify for Medicaid. The federal government provides matching funds to states for health insurance for these families.
Read more details at InsuredKidsNow.gov.
- Children and Youth With Special Health Care Needs: This program coordinates funding and resources to provide care to people with special health needs.
Read more details at Children With Special Health Care Needs.
- Tricare: This program covers about 9 million active duty and retired military personnel and their families.
Read more details at TRICARE.
- Veterans Health Administration (VHA): This government-operated health care system provides comprehensive health services to eligible military veterans. About 9 million veterans are enrolled.
Read more details at Veterans Health Administration.
- Indian Health Service: This system of government hospitals and clinics provides health services to about 2 million Native Americans living on or near a reservation.
Read more details at Indian Health Service.
- Federal Employee Health Benefits (FEHB) Program: This program allows private insurers to offer insurance plans within guidelines set by the government for the benefit of active and retired federal employees and their survivors.
Read more details at The Federal Employees Health Benefits (FEHB) Program.
- Refugee Health Promotion Program: This program provides short-term health insurance to newly arrived refugees.
Read more details at Refugee Health Promotion Program (RHP).
Private Insurance
Individuals who are not eligible for government-funded health programs like Medicare or Medicaid can purchase private health insurance. Many individuals with private insurance obtain coverage through their employers’ benefit packages, where the costs for coverage are shared between the employer and the employee. If an individual does not receive health insurance through their employer, they may purchase it from the Marketplace established by the Affordable Care Act.
Read more about obtaining health insurance through the ACA Marketplace at healthcare.gov.
Self-Pay
Some individuals do not have health care coverage provided by their employer, do not qualify for Medicare or Medicaid, and do not elect to purchase health insurance coverage. Instead, these individuals go without coverage and pay health care costs as they arise. See Figure 8.7[17] for a graph illustrating the decreasing numbers of uninsured consumers in the United States over the past several decades. Unfortunately, due to the skyrocketing cost of health care services, significant bills can accrue from a single serious illness or traumatic injury that can put consumers without health care coverage in jeopardy of bankruptcy. Nurses can assist uninsured individuals to better understand coverage options by referring them to a case manager or social worker.

Types of Insurance Coverage
Health insurance plans have different types of coverage. Common types of health insurance plans are HMO, PPO, POS, HDHP, or HSA.
- Health Maintenance Organization (HMO): HMO plans usually have the lowest monthly cost for coverage (i.e., premium) but also have a smaller network of providers and hospitals where the consumer may receive insured care. This means the consumer is restricted to receive care only from specific providers and health facilities. Many HMOs also require the consumer to see their primary care provider to request a referral to see a specialist, which may or may not be approved by the HMO. Additionally, many tests, procedures, surgeries, and medications require “preauthorization” by the HMO, which may or may not be approved. Due to these restrictions, consumers may find they sacrifice flexibility and choice for lower cost of coverage.[18]
- Preferred Provider Organization (PPO): PPO plans are typically less restrictive than HMOs. PPOs typically include “in-network” providers and hospitals where costs are lower if care is received in-network, but consumers also have a choice to receive “out-of-network” care at a higher cost. Referrals from a primary care provider are not generally required in a PPO. The monthly premium for a PPO plan is typically higher than an HMO plan, but PPOs allow more consumer flexibility in choosing their health care providers.[19]
- Point of Service (POS): POS plans are a combination of HMO and PPO plans, where the insured consumer has a preferred provider network to receive health care services at a lower cost, but also has the flexibility to receive care outside of their network. When consumers venture outside of the network, they often have to pay a significant share of the cost.[20]
- High Deductible Health Plan (HDHP): HDHP plans are often popular for younger individuals without chronic health care needs who spend little on health care but require coverage in the event a high-cost injury or illness occurs. HDHPs typically have lower monthly premiums but require the individual to pay more upfront for health care services before the coverage kicks in (referred to as a “deductible”). Individuals with an HDHP often have an associated Health Savings Account (HSA). HDHPs have grown in popularity as more employers offer these plans in an attempt to contain health care costs by shifting more cost-sharing to the consumer.
- Health Savings Account (HSA): An HSA is a special account reserved for eligible medical expenses with strict usage rules. Money placed in an HSA can often be deducted from a consumer’s pretaxed pay, resulting in tax savings. In addition to purchasing items like glasses, contacts, and over-the-counter medications, HSAs can often be used to pay for deductibles. Some employers deposit a specified amount of money into an employee’s HSA every year to help reimburse high deductibles.
Deductible and Copays
Costs paid by an insured individual are commonly referred to as “out-of-pocket expenses.” Out-of-pocket expenses include deductibles and co-pays. A deductible is the amount of money a consumer pays before the health care plan pays anything. Deductibles generally apply per person per calendar year. Typically, a PPO has higher premiums but lower deductibles than a HDHP.
A co-pay is a flat fee the consumer pays at the time of the health care service. For example, when visiting a primary provider, the consumer may pay $20 to the provider at each visit as a co-pay. Some health care plans require co-pays in addition to deductibles.
Nursing Considerations
Understanding a client’s health insurance coverage is important because it may impact their choice of health services and their ability to purchase medications and other supplies. Additionally, if a client is self-pay, it is helpful to refer them to resources such as case managers, social workers, or the financial department of the agency. These resources can assist them in obtaining affordable health care coverage through the ACA Marketplace or other government programs.
Sample Documentation of Expected Findings
3 cm x 2 cm Stage 3 pressure injury on the patient’s sacrum. Dark pink wound base with no signs of infection. Cleansed with normal saline spray and hydrocolloid dressing applied.
Sample Documentation of Unexpected Findings
3 cm x 2 cm x 1 cm Stage 3 pressure injury on sacrum. Wound base dark red with yellow-green drainage present. Removed 4 x 4 dressing has 5 cm diameter ring of drainage present. Periwound skin red, warm, tender to palpation. Temperature 36.8⁰ C. Dr. Smith notified of all the above. Wound culture order received. Wound cleansed with normal saline spray, wound culture collected, hydrocolloid dressing applied.
Wound therapy is often prescribed by a multidisciplinary team that can include the provider, a wound care nurse, a dietician, and the bedside nurse who performs dressing changes. Topical dressings should be selected that create an environment conducive to healing the specific type of wound and its causes. It is important to perform the following actions when providing wound care:
- Prevent and manage infection
- Cleanse the wound
- Debride the wound
- Maintain appropriate moisture in the wound
- Control odor
- Manage wound pain
- Consider the big picture[21]
Each of these objectives is further discussed in the following subsections.
Prevent and Manage Infection
One of the primary goals of wound dressings is to protect the wound base from bacteria and contaminants (i.e., urine and feces). If new signs of infection are present during a wound dressing change, wound swabs should be taken according to agency policy and the need for a wound culture and possible antibiotic therapy discussed with the primary provider.[22]
Silver sulfadiazine is an example of a common topical antibiotic prescribed for wounds. Topical antibiotics are covered with a secondary dressing.[23]
Cleanse the Wound
Routine cleansing should be performed at each dressing change with products that are physiologically compatible with wound tissue. Normal saline is the most gentle solution and is typically delivered using a syringe or commercial cleansers. See Figure 20.20[24] for an image of wound irrigation with a syringe. Commercial cleansers may be used, but hydrogen peroxide, betadine, and acetic acid should be avoided because these agents can be cytotoxic.[25]

Debride the Wound
Debridement is the removal of nonviable tissue in a wound. If necrotic (black) tissue is present in the wound bed, it must be removed in most circumstances for the wound to heal. However, one exception is stable, dry eschar on a patient’s heel that should be left in place until the patient’s vascular status is determined.[26]
Wound debridement can be accomplished using several methods, such as autolytic, enzymatic, or sharp wound debridement. Autolytic debridement occurs when moist topical dressings foster the breakdown of necrotic tissue. Enzymatic debridement occurs when prescribed topical agents are directly applied to the wound bed.[27] Collagenase ointment is an example of a topical enzymatic debridement ointment that is applied daily (or more frequently if the dressing becomes soiled) and covered with sterile gauze or a foam dressing.[28] Sharp wound debridement is performed by a trained health care provider and may be at the bedside or in the operating room. Sharp debridement is an invasive procedure using a scalpel or scissors to remove necrotic tissue so that only viable tissue remains. See Figure 20.21[29] for an image of a wound that has been surgically debrided of necrotic tissue.

Maintain Appropriate Moisture in the Wound
Wound dressings should maintain a moist wound environment to facilitate the development of granulation tissue. However, excessive exudate must be managed with dressings that absorb excess moisture to avoid maceration of the surrounding tissue.[30] For example, dressings such as alginate or hydrofiber are used in wounds with large amounts of exudate to maintain an appropriate moisture level but also prevent maceration of tissue. Frequent dressing changes may also be required in wounds with heavy drainage.
Eliminate Dead Space
Deep wounds and tunneling should be packed with dressings to keep the wound bed moist. Sterile gauze dressings moistened with normal saline or hydrogel-impregnated dressings are examples of packing agents used to keep the wound bed moist. Packing material should be easy to remove from the wound base during each dressing change to avoid injuring the fragile granulation tissue. Keep in mind that dressings made of alginate have a slight greenish tint when removed and should not be confused with purulent drainage.
Control Odor
If odor is present in a wound, the nurse should consult with the health care provider about the frequency of dressing changes, wound cleansing agents, and the possible need for topical antimicrobial therapy or debridement. Room deodorants can be obtained for use after dressing changes.[31]
Manage Wound Pain
Wounds that are becoming increasingly painful should be assessed for potential infection or dehiscence. The nurse should plan on administering medication to the patient before performing dressing changes on wounds that are painful. If pain medication is not ordered, then the nurse should contact the health care provider for a prescription before performing the dressing change.[32]
Protect Periwound Skin
Heavily draining wounds or the improper use of moist dressings can cause maceration of the periwound skin. The nurse should apply dressings carefully to maintain wound bed moisture yet also protect the periwound skin. Skin barrier creams, skin protective wipes, or skin barrier wafers can also be used to protect the periwound skin.[33]
Consider the Big Picture
Most wounds do not occur in isolation but also have other systemic or local factors that impact wound healing. Be sure to consider the following points when caring for patients with wounds with delayed wound healing:
- Minimize pressure and shear for patients with pressure injuries. For example, a patient with a pressure injury should be repositioned at least every two hours to minimize pressure.
- Educate patients with neuropathy and decreased sensation about preventing further injury. For example, a patient with diabetes should wear well-fitting shoes and never go barefoot to prevent injuries.
- Control edema in patients with venous ulcers through the use of compression dressings.
- Promote adequate perfusion to patients with arterial ulcers. For example, in most cases, the extremity of a patient with an arterial ulcer should not be elevated.
- Protect fragile skin in patients with skin tears to prevent further injury.
- Manage blood sugar levels in patients with diabetes mellitus for optimal healing.
- Promote good nutrition and hydration for all patients with wounds. Consult a registered dietician to assess the patient’s nutritional status and develop a nutrition plan if needed.[34]
- Document ongoing assessment findings and wound interventions for good communication and continuity of care across the multidisciplinary health care team.
- Concerns about the healing of a chronic wound or the dressings ordered should be communicated to the health care provider. Referral to a specialized wound care nurse is often helpful.
Quality is defined in a variety of ways that impact nursing practice.
ANA Definition of Quality
The American Nurses Association (ANA) defines quality as, “The degree to which nursing services for health care consumers, families, groups, communities, and populations increase the likelihood of desirable outcomes and are consistent with evolving nursing knowledge.”[35] The phrases in this definition focus on three aspects of quality: services (nursing interventions), desirable outcomes, and consistency with evolving nursing knowledge (evidence-based practice). Alignment of nursing interventions with current evidence-based practice is a key component for quality care.[36] Evidence-based practice (EBP) will be further discussed later in this chapter.
Quality of Practice is one of the ANA’s Standards of Professional Performance. ANA Standards of Professional Performance are “authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting are expected to perform competently." See the competencies for the ANA’s Quality of Practice Standard of Professional Performance in the following box.[37]
Competencies of ANA’s Quality of Practice Standard of Professional Performance[38]
- Ensures that nursing practice is safe, effective, efficient, equitable, timely, and person-centered.
- Incorporates evidence into nursing practice to improve outcomes.
- Uses creativity and innovation to enhance nursing care.
- Recommends strategies to improve nursing care quality.
- Collects data to monitor the quality of nursing practice.
- Contributes to efforts to improve health care efficiency.
- Provides critical review and evaluation of policies, procedures, and guidelines to improve the quality of health care.
- Engages in formal and informal peer review processes of the interprofessional team.
- Participates in quality improvement initiatives.
- Collaborates with the interprofessional team to implement quality improvement plans and interventions.
- Documents nursing practice in a manner that supports quality and performance improvement initiatives.
- Recognizes the value of professional and specialty certification.
Reflective Questions
- What Quality of Practice competencies have you already demonstrated during your nursing education?
- What Quality of Practice competencies are you most interested in mastering?
- What questions do you have about the ANA’s Quality of Practice competencies? Where could you find answers to those questions (e.g., instructors, preceptors, health care team members, guidelines, or core measures)?
This chapter will review content related to the competencies of the ANA’s Quality of Practice Standard of Professional Performance. Additional information about peer review is discussed in the “Leadership and Management” chapter, and specialty certification is discussed in the “Preparation for the RN Role” chapter.
Quality and Safety Education for Nurses
The Quality and Safety Education for Nurses (QSEN) project advocates for safe, quality patient care by defining six competencies for prelicensure nursing students: Patient-Centered Care, Teamwork and Collaboration, Evidence-Based Practice, Quality Improvement, Safety, and Informatics. These competencies are further discussed in the "Advocacy" chapter.
Framework of Quality Health Care
A definition of quality that has historically guided the measurement of quality initiatives in health care systems is based on the framework for improvement originally created by the Institute of Medicine (IOM). The IOM name changed to the National Academy of Medicine in 2015. The IOM framework includes the following six criteria for defining quality health care[39],[40]:
- Safe: Avoiding harm to patients from the care that is intended to help them.
- Effective: Providing services based on scientific knowledge to all who could benefit and refraining from providing services to those not likely to benefit (i.e., avoiding underuse and misuse).
- Patient-centered: Providing care that is respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions.
- Timely: Reducing waits and sometimes harmful delays for both those who receive and those who provide care.
- Efficient: Avoiding waste, including waste of equipment, supplies, ideas, and energy.
- Equitable: Providing care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status.
This framework continues to guide quality improvement initiatives across America’s health care system. The evidence-based practice (EBP) movement began with the public acknowledgement of unacceptable patient outcomes resulting from a gap between research findings and actual health care practices. For EBP to be successfully adopted and sustained, it must be adopted by nurses and other health care team members, system leaders, and policy makers. Regulations and recognitions are also necessary to promote the adoption of EBP. For example, the Magnet Recognition Program promotes nursing as a leader in catalyzing adoption of EBP and using it as a marker of excellence.[41]
Magnet Recognition Program
The Magnet Recognition Program is an award from the American Nurses Credentialing Center (ANCC) that recognizes organizational commitment to nursing excellence. The award recognizes organizations worldwide where nursing leaders have successfully aligned their nursing strategic goals to improve the organization’s patient outcomes. To nurses, Magnet Recognition means education and development are available through every stage of their career. To patients, it means quality care is delivered by nurses who are supported to be the best that they can be.[42] See Figure 9.2[43] for an image related to the Magnet Recognition Program.

Reimbursement Models
Quality health care is also defined by value-based reimbursement models used by Medicare, Medicaid, and private insurance companies paying for health services. As discussed in the “Health Care Reimbursement Models” section of the “Health Care Economics” chapter, value-based payment reimbursement models use financial incentives to reward quality health care and positive patient outcomes. For example, Medicare no longer reimburses hospitals to treat patients who acquire certain preventable conditions during their hospital stay, such as pressure injuries or urinary tract infections associated with use of catheters.[44] These reimbursement models directly impact the evidence-based care nurses provide at the bedside and the associated documentation of assessments, interventions, and nursing care plans to ensure quality performance criteria are met.
CMS Quality Initiatives
The Centers for Medicare & Medicaid Services (CMS) establishes quality initiatives that focus on several key quality measures of health care. These quality measures provide a comprehensive understanding and evaluation of the care an organization delivers, as well as patients’ responses to the care provided. These quality measures evaluate many areas of health care, including the following:[45]
- Health outcomes
- Clinical processes
- Patient safety
- Efficient use of health care resources
- Care coordination
- Patient engagement in their own care
- Patient perceptions of their care
These measures of quality focus on providing the care the patient needs when the patient needs it, in an affordable, safe, effective manner. It also means engaging and involving the patient, so they take ownership in managing their care at home.
Visit the CMS What is a Quality Measure web page.
Accreditation
Accreditation is a review process that determines if an agency is meeting the defined standards of quality determined by the accrediting body. The main accrediting organizations for health care are as follows:
- The Joint Commission
- National Committee for Quality Assurance
- American Medical Accreditation Program
- American Accreditation Healthcare Commission
The standards of quality vary depending on the accrediting organization, but they all share common goals to improve efficiency, equity, and delivery of high-quality care. Two terms commonly associated with accreditation that are directly related to quality nursing care are core measures and patient safety goals. Please see Table 9.2 for more information on accrediting organizations.
Table 9.2. Accrediting Organizations [46], [47], [48] [49]
| Organization | Overview | History | Accreditation Process | Standards | Impact |
| The Joint Commission | Non-profit organization accrediting and certifying health care organizations and programs in the U.S. | Founded in 1951, aims to improve public health care quality and safety | Conducts rigorous on-site surveys to assess compliance with standards covering patient care, medication safety, infection control, and overall performance | Developed with input from health care professionals, providers, and consumers and designed to help measure, assess, and improve performance | Recognized as a symbol of quality, reflecting commitment to high performance standards |
| National Committee for Quality Assurance (NCQA) | Private, non-profit organization improving health care quality through evidence-based standards, measures, programs, and accreditation | Established in 1990, provides quality information for health care decision-making | Comprehensive review of policies and procedures, including quality management, utilization management, credentialing, and member rights | Widely regarded standards used by CMS and state governments for quality oversight | Demonstrates commitment to improving health care quality and adhering to high performance standards |
| American Medical Accreditation Program (AMAP) | Program by AMA aimed at improving medical care quality by setting high standards for physicians | Launched in the late 1990s, assesses physicians' qualifications and ethical standards | Detailed review process, including verification of credentials, practice history assessment, and compliance with CME requirements | Ensures physicians provide high-quality care, maintain competency, and adhere to ethical practices | Recognizes physicians' commitment to high-quality care and medical practice standards |
| American Accreditation Healthcare Commission (AAHC) / URAC | Independent, non-profit organization promoting health care quality through accreditation, certification, and measurement | Founded in 1990, expanded from utilization review to a wide range of health care services | Thorough review of policies, procedures, and performance, including on-site visits and compliance assessment | Developed by a broad array of stakeholders to promote evidence-based practices, patient safety, and continuous improvement | Recognized as a mark of excellence, demonstrating commitment to quality and accountability |
Core Measures
Core measures are national standards of care and treatment processes for common conditions. These processes are proven to reduce complications and lead to better patient outcomes. Core measure compliance reports show how often a hospital successfully provides recommended treatment for certain medical conditions. In the United States, hospitals must report their compliance with core measures to The Joint Commission, CMS, and other agencies.[50]
In November 2003, The Joint Commission and CMS began work to align common core measures, so they are identical. This work resulted in the creation of one common set of measures known as the Specifications Manual for National Hospital Inpatient Quality Measures. These core measures are used by both organizations to improve the health care delivery process. Examples of core measures include guidelines regarding immunizations, tobacco treatment, substance use, hip and knee replacements, cardiac care, strokes, treatment of high blood pressure, and the use of high-risk medications in the elderly. Nurses must be aware of core measures and ensure the care they provide aligns with these recommendations.[51]
Read more about the National Hospital Inpatient Quality Measures.
Patient Safety Goals
Patient safety goals are guidelines specific to organizations accredited by The Joint Commission that focus on health care safety problems and ways to solve them. The National Patient Safety Goals (NPSG) were first established in 2003 and are updated annually to address areas of national concern related to patient safety, as well as to promote high-quality care. The NPSG provide guidance for specific health care settings, including hospitals, ambulatory clinics, behavioral health, critical access hospitals, home care, laboratory, skilled nursing care, and surgery.
The following goals are some examples of NPSG for hospitals[52]:
- Identify patients correctly
- Improve staff communication
- Use medicines safely
- Use alarms safely
- Prevent infection
- Identify patient safety risks
- Prevent mistakes in surgery
Nurses must be aware of the current NPSG for their health care setting, implement appropriate interventions, and document their assessments and interventions. Documentation in the electronic medical record is primarily used as evidence that an organization is meeting these goals.
Read the current agency-specific National Patient Safety Goals.
Localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.
As discussed in the previous section, hospitals and health care providers are paid for services provided to individuals by government insurance programs (such as Medicare and Medicaid), private insurance companies, or people using their out-of-pocket funds. Traditionally, health care institutions were paid based on a “fee-for-service” model. For example, if a patient was admitted to a hospital with pneumonia, the hospital billed that individual's insurance program for the cost of care.
However, as part of a recent national strategy to reduce health care costs, insurance providers have transitioned to "Pay for Performance" reimbursement models that are based on overall agency performance and patient outcomes.
Pay for Performance
Pay for Performance, also known as value-based payment, refers to reimbursement models that attach financial incentives to the performance of health care agencies and providers. Pay for Performance models tie higher reimbursement payments to positive patient outcomes, best practices, and patient satisfaction, thus aligning payment with value and quality.[53] Nurses support higher reimbursement levels to their employers based on their documentation related to nursing care plans and achievement of expected patient outcomes.
There are two Pay for Performance models. The first model rewards hospitals and providers with higher reimbursement payments based on how well they perform on process, quality, and efficiency measures. The second model penalizes hospitals and providers for subpar performance by reducing reimbursement amounts.[54] For example, Medicare no longer reimburses hospitals to treat patients who acquire certain preventable conditions during their hospital stay, such as pressure injuries or urinary tract infections associated with use of catheters.[55]
The Centers for Medicare and Medicaid Services (CMS), spurred by the Affordable Care Act, has led the way in value-based payment with a variety of payment models. CMS is the largest health care funder in the United States with almost 40% of overall health care spending for Medicare and Medicaid. CMS developed three Pay for Performance models that impact hospitals’ reimbursement by Medicare. These models are called the Hospital Value-Based Purchasing Program, the Hospital Readmissions Reduction Program, and the Hospital-Acquired Condition Reduction Program. Private insurers are also committed to performance-based payment models. In 2017 Forbes reported that almost 50% of insurers’ reimbursements were in the form of value-based care models.[56]
Hospital Value-Based Purchasing Program
The Hospital Value-Based Purchasing Program (VBP) was designed to improve health care quality and patient experience by using financial incentives that encourage hospitals to follow established best clinical practices and improve patient satisfaction scores via patient satisfaction surveys. Reimbursement is based on hospital performance on measures divided into four quality domains: safety, clinical care, efficiency and cost reduction, and patient and caregiver-centered experience.[57] The VBP program rewards hospitals based on the quality of care provided to Medicare patients and not just the quantity of services that are provided. Hospitals may have their Medicaid payments reduced by up to 2% if not meeting the quality metrics.
Read more about patient satisfaction surveys.
Hospital Readmissions Reduction Program
The Hospital Readmissions Reduction Program (HRRP) penalizes hospitals with higher rates of patient readmissions compared to other hospitals. HRRP was established by the Affordable Care Act and applies to patients with specific conditions, such as heart attacks, heart failure, pneumonia, chronic obstructive pulmonary disease (COPD), hip or knee replacements, and coronary bypass surgery. Hospitals with poor performance receive a 3% reduction of their Medicare payments. However, it was discovered that hospitals with higher proportions of low-income patients were penalized the most, so Congress passed legislation in 2019 that divided hospitals into groups for comparison based on the socioeconomic status of their patient populations.[58]
Hospital-Acquired Condition Reduction Program
The Hospital-Acquired Condition Reduction Program (HACRP) was established by the Affordable Care Act. This Pay for Performance model reduces payments to hospitals based on poor performance regarding patient safety and hospital-acquired conditions, such as surgical site infections, hip fractures resulting from falls, and pressure injuries. This model has saved Medicare approximately $350 million per year.[59]
The HACRP model measures the incidence of hospital-acquired conditions, including central line-associated bloodstream infections (CLABSI), catheter-associated urinary tract infections (CAUTI), surgical site infections (SSI), Methicillin-Resistant Staphylococcus Aureus (MRSA), and Clostridium Difficile (C. diff).[60] As a result, nurses have seen changes in daily practices based on evidence-based practices related to these conditions. For example, stringent documentation is now required for clients with Foley catheters that indicates continued need and associated infection control measures.
Other CMS Pay for Performance Models
CMS has created other value-based payment programs for agencies other than hospitals, including the End-Stage Renal Disease (ESRD) Quality Initiative Program, the Skilled Nursing Facility Value-Based Program (SNFVBP), the Home Health Value-Based Program (HHVBP), and the Value Modifier (VM) Program. The VM program is aimed at Medicare Part B providers who receive high, average, or low ratings based on quality and cost measurements as compared to peer agencies.
Impacts of Value-Based Payment
Pay for Performance (i.e., value-based payment) stresses quality over quantity of care and allows health care payers to use reimbursement to encourage best clinical practices and promote positive health outcomes. It focuses on transparency by using metrics that are publicly reported, thus incentivizing organizations to protect and strengthen their reputations. In this manner, Pay for Performance models encourage accountability and consumer-informed choice.[61] See Figure 8.8[62] for an illustration of Pay for Performance.
Pay for Performance models have reduced health care costs and decreased the incidence of poor patient outcomes. For example, 30-day hospital readmission rates have been falling since 2012, indicating HRRP and HACRP are having an impact.[63]
However, there are also disadvantages to value-based payment. As previously discussed, initial research indicated hospitals with higher proportions of low-income patients were being penalized the most, resulting in additional legislation to compare hospital performance in groups based on their clients’ socioeconomic status. Nursing leaders continue to emphasize strategies that further address social determinants of health and promote health equity.[64] Read more about equity and social determinants of health in the following subsection.
Nursing Considerations
Nurses have a direct impact on activities related to quality care and reimbursement rates received by their employer. There are several categories of actions nurses can take to improve quality patient care, reduce costs, and improve reimbursement. By incorporating these actions into their daily care, nurses can help ensure the funding they need to provide quality patient care is received by their employer and resources are allocated appropriately to their patients.
The following categories of actions to improve quality of care are based on the Institute of Medicine (IOM) report To Err Is Human: Building a Safer Health Care System and Crossing the Quality Chasm[65]:
- Effectiveness and Efficiency: Nurses support their institution's effectiveness and efficiency with individualized nursing care planning, good documentation, and care coordination. With accurate and timely documentation and care coordination, there is reduced care duplication and waste. Coordinating care also helps to reduce the risk of hospital readmissions.
- Timeliness: Nurses positively impact timeliness by prioritizing and delegating care. This helps reduce patient wait times and delays in care.
Read more about these concepts in the “Delegation and Supervision” and “Prioritization” chapters in this book.
- Safety: Nurses pay attention to their patients’ changing conditions and effectively communicate these changes with appropriate health care team members. They take any concerns about client care up the chain of command until their concerns are resolved.
- Patient-Centered Care: Nurses support this quality measure by ensuring nursing care plans are individualized for each patient. Effective care plans can improve patient compliance, resulting in improved patient outcomes.
- Evidence-Based Practice: Nurses provide care based on evidence-based practice. Evidence-Based Practice (EBP) is defined by the American Nurses Association as, “A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and patient, family, group, community, and population preferences and values.”[66] EBP is a component of Scholarly Inquiry, one of the ANA’s Standards of Professional Practice. Nurses’ implementation of EBP ensures proper resources are allocated to the appropriate clients. EBP promotes safe, efficient, and effective health care.[67],[68]
Read more information about EBP in the “Quality and Evidence-Based Practice” chapter of this book.
- Equity: Health care institutions care for all members of their community regardless of client demographics and their associated social determinants of health (SDOH). SDOH are conditions in the places where people live, learn, work, and play that affect a wide range of health risks and outcomes. Health disparities in communities with poor SDOH have been consistently documented in reports by the Agency for Healthcare Research and Quality (AHRQ).[69]
Nurses address negative determinants of health by advocating for interventions that reduce health disparities and promote the delivery of equitable health care resources. The term health disparities describes the differences in health outcomes that result from SDOH. Advocating for resources that enhance quality of life can significantly influence a community's health outcomes. Examples of resources that promote health include safe and affordable housing, access to education, public safety, availability of healthy foods, local emergency/health services, and environments free of life-threatening toxins.
A related term is health care disparity that refers to differences in access to health care and insurance coverage. Health disparities and health care disparities can lead to decreased quality of life, increased personal costs, and lower life expectancy. More broadly, these disparities also translate to greater societal costs, such as the financial burden of uncontrolled chronic illnesses. An example of nurses addressing health care disparities are nurse practitioners providing health care according to their scope of practice to underserved populations in rural communities.
The ANA promotes nurse advocacy in workplaces and local communities. There are many ways nurses can promote health and wellness within their communities through a variety of advocacy programs at the federal, state, and community level.[70] Read more about advocacy and reducing health disparities in the following boxes.
Read more about ANA Policy and Advocacy.
Read more information in the “Advocacy” chapter of this book.
Read more about addressing health disparities in the “Diverse Patients” chapter in Open RN Nursing Fundamentals, 2e.
Economics and health care reimbursement models impact health care institutional budgets that ultimately impact nurse staffing. A budget is an estimate of revenue and expenses over a specified period of time, usually over a year. There are two basic types of health care budgets that affect nursing: capital and operating budgets. Capital budgets are used to plan investments and upgrades to tangible assets that lose or gain value over time. Capital is something that can be touched, such as buildings or computers. Operating budgets include personnel costs and annual facility operating costs.[71] Typically 40% of the operating budgets of health care agencies are dedicated to nursing staffing. As a result, nursing is often targeted for reduced hours and other cutbacks.[72]
What is the value of a nurse? Nurses are priceless to the clients, families, and communities they serve, but health care organizations are tasked with calculating the cost of delivering safe, high-quality nursing care using affordable staffing models. All members of the health care team must understand the relationship between economics, resources, budgeting, and staffing, and how these issues affect their ability to provide safe, quality care to their patients.
As health care agencies continue to adapt to meet “Pay for Performance” reimbursement models and deliver cost-effective care to an aging population with complex health needs, many nurses are experiencing changes in staffing models.[73] Strategies implemented by agencies to facilitate cost-effective nurse staffing include acuity-based staffing, team nursing, mandatory overtime, floating, on call, and off with benefits. Agencies may also use agency nurses when nurse shortages occur.
Acuity-Based Staffing
Historically, inpatient staffing patterns focused on “nurse-to-patient ratios” where a specific number of patients were assigned to each registered nurse during a shift. Acuity-based staffing is a patient assignment model that takes into account the level of patient care required based on the severity of a patient’s illness or condition. As a result of acuity-based staffing, the number of clients a nurse cares for often varies from shift to shift as the needs of the patients change. Acuity-based staffing promotes efficient use of resources by ensuring nurses have adequate time to care for complex patients.
Read more information about acuity-based staffing in the “Prioritization” chapter.
Team Nursing
Team nursing is a common staffing pattern that uses a combination of Registered Nurses (RNs), Licensed Practical/Vocational Nurses (LPN/VNs), and Assistive Personnel (AP) to care for a group of patients. The RN is the leader of a nursing team, making assignments and delegating nursing care to other members of the team with appropriate supervision. Team nursing is an example of allocating human resources wisely to provide quality and cost-effective care. In order for team nursing to be successful, team members must use effective communication and organize their shift as a team.
Read more about team nursing in the “Delegation and Supervision” chapter of this book.
Mandatory Overtime
When client numbers and acuity levels exceed the number of staff scheduled for a shift, nurses may experience mandatory overtime as an agency staffing tool. Mandatory overtime requires a nurse to stay and care for patients beyond their scheduled shift when there is a lack of nursing staff (often referred to as short staffing). The American Nurses Association recognizes mandatory overtime as a dangerous staffing practice because of patient safety concerns related to overtired staff. Depending on state laws, nurses can be held liable for patient abandonment or neglect charges for refusing to stay when mandated. Nurses should be aware of state and organizational policies related to mandatory overtime.[74]
Read more about ANA’s advocacy for adequate nurse staffing.
Floating
Floating is a common agency staffing strategy that asks nurses to temporarily work on a different unit to help cover a short-staffed shift. Floating can reduce personnel costs by reducing overtime payments for staff. It can also reduce nurse burnout occurring from working in an environment without enough personnel.
Nurses must be aware of their rights and responsibilities when asked to float because they are still held accountable for providing safe patient care according to their state's Nurse Practice Act and professional standards of care. Before accepting a floating assignment, nurses should ensure the assignment is aligned with their skill set and they receive orientation to the new environment before caring for patients. If an error occurs and the nurse is held liable, the fact they received a floating assignment does not justify the error. As the ANA states, nurses don’t just have the right to refuse a floating patient assignment; they have the obligation to do so if it is unsafe.[75] The ANA has developed several questions to guide nurses through the decision process of accepting patient assignments. Review these questions in the following box.
ANA’s Suggested Questions When Deciding on Accepting a Patient Assignment[76]
- What is the assignment? Clarify what is expected; do not assume. Be certain about the details.
- What are the characteristics of the patients being assigned? Don’t just respond to the number of patients assigned. Make a critical assessment of the needs of each client and their complexity and stability. Be aware of the resources available to meet those needs.
- Do you have the expertise to care for the patients? Always ask yourself if you are familiar with caring for the types of patients assigned? If this is a “float assignment,” are you cross-trained to care for these patients? Is there a “buddy system” in place with staff who are familiar with the unit? If there is no cross-training or “buddy system,” has the patient load been modified accordingly?
- Do you have the experience and knowledge to manage the patients for whom you are being assigned care? If the answer to the question is “No,” you have an obligation to articulate your limitations. Limitations in experience and knowledge may not require refusal of the assignment, but rather an agreement regarding supervision or a modification of the assignment to ensure patient safety. If no accommodation for limitations is considered, the nurse has an obligation to refuse an assignment for which they lack education or experience.
- What is the geography of the assignment? Are you being asked to care for patients who are in close proximity for efficient management, or are the patients at opposite ends of the hall or in different units? If there are geographic difficulties, what resources are available to manage the situation? If the patients are in more than one unit and you must go to another unit to provide care, who will monitor patients out of your immediate attention?
- Is this a temporary assignment? When other staff are located for assistance, will you be relieved? If the assignment is temporary, it may be possible to accept a difficult assignment knowing that there will soon be reinforcements. Is there a pattern of short staffing at this agency, or is this truly an emergency?
- Is this a crisis or an ongoing staffing pattern? If the assignment is being made because of an immediate need or crisis in the unit, the decision to accept the assignment may be based on that immediate need. However, if the staffing pattern is an ongoing problem, you have the obligation to identify unmet standards of care that are occurring as a result of ongoing staffing inadequacies. This may result in a formal request for peer review using the appropriate channels.
- Can you take the assignment in good faith? If not, you will need to have the assignment modified or refuse the assignment. Consult your state’s Nurse Practice Act regarding clarification of accepting an assignment in good faith.
On Call and Off With Benefits
When staffing projected for a shift exceeds the number of clients admitted and their acuity, agencies often decrease staffing due to operating budget limitations. Two common approaches that agencies use to reduce staffing on a shift-to-shift basis are placing nurses “on call” or “off with benefits.”
On Call
On call is an agency staffing strategy when a nurse is not immediately needed for their scheduled shift. The nurse may have the options to report to work and do work-related education or stay home. When a nurse is on call, they typically receive a reduced hourly wage and have a required response time. A required response time means if a nurse who is on call is needed later in the shift, they need to be able to report and assume patient care in a designated amount of time.
Off With Benefits
A nurse may be placed “off with benefits” when not needed for their scheduled shift. When a nurse is placed off with benefits, they typically do not receive an hourly wage and are not expected to report to work or be on call, but still accrue benefits such as insurance and paid time off.
Agency Nursing
Agency nursing is an industry in health care that provides nurses to hospitals and health care facilities in need of staff. Nurse agencies employ nurses to work on an as-needed basis and place them in facilities that have staffing shortages.
Advocacy by the ANA for Appropriate Nurse Staffing
According to the ANA, there is significant evidence showing appropriate nurse staffing contributes to improved client outcomes and greater satisfaction for both clients and staff. Appropriate staffing levels have multiple client benefits, including the following[77]:
- Reduced mortality rates
- Reduced length of client stays
- Reduced number of preventable events, such as falls and infections
Nurses also benefit from appropriate staffing. Appropriate workload allows nurses to utilize their full expertise, without the pressure of fatigue. A recent report suggested that staff levels should depend on the following factors[78]:
- Patient complexity, acuity, or stability
- Number of admissions, discharges, and transfers
- Professional nurses’ and other staff members’ skill level and expertise
- Physical space and layout of the nursing unit
- Availability of technical support and other resources
Visit ANA's interactive Principles of Nurse Staffing infographic.
Read more information about patient acuity tools in the "Prioritization" chapter.
Cost-Effective Nursing Care
One of ANA's Standards of Professional Performance is Resource Stewardship. The Resource Stewardship standard states, “The registered nurse utilizes appropriate resources to plan, provide, and sustain evidence-based nursing services that are safe, effective, financially responsible, and used judiciously.”[79] Nurses have a fiscal responsibility to demonstrate resource stewardship to the employing organization and payer of care. This responsibility extends beyond direct patient care and encompasses a broader role in health care sustainability. By effectively managing resources, nurses help reduce unnecessary expenditures and ensure that funds are allocated where they are most needed. This can include everything from minimizing waste in the use of medical supplies to optimizing staffing levels to avoid both overworking and underutilizing nursing staff.
Nurses can help contain health care costs by advocating for patients and ensuring their care is received on time, the plan of care is appropriate and individualized to them, and clear documentation has been completed. These steps reduce waste, avoid repeated tests, and ensure timely treatments that promote positive patient outcomes and reduce unnecessary spending. Nurses routinely incorporate these practices to provide cost-effective nursing care in their daily practice:
- Keeping supplies near the client's room
- Preventing waste by only bringing needed supplies into a client’s room
- Avoiding prepackaged kits with unnecessary supplies
- Avoiding “Admission Bags” with unnecessary supplies
- Using financially-sound thinking
- Understanding health care costs and reimbursement models
- Charging out supplies and equipment according to agency policy
- Being Productive
- Organizing and prioritizing
- Using effective time management
- Grouping tasks when entering client rooms (i.e., clustering cares)
- Assigning and delegating nursing care to the nursing team according to the state Nurse Practice Act and agency policy
- Using effective team communication to avoid duplication of tasks and request assistance when needed
- Updating and individualizing clients’ nursing care plans according to their current needs
- Documenting for continuity of client care that avoids duplication and focuses on effective interventions based on identified outcomes and goals

