10.10 Other Musculoskeletal Disorders
Open Resources for Nursing (Open RN)
Additional musculoskeletal disorders are briefly discussed in this section.
Bone Cancer
There are three types of primary bone cancers: osteosarcoma, Ewing sarcoma, and chondrosarcoma. These are considered primary cancers because they originate in the bones. Osteosarcoma and Ewing sarcomas are cancers found in children, teenagers, and young adults. Ewing sarcoma is considered to be the more aggressive of the two cancers because it tends to metastasize quickly. Osteosarcoma is the most common type of bone cancer, and it begins in the tissues of growing bones. Chondrosarcoma develops in cells that produce cartilage and affects adults.
Bone cancer can also be caused by cancer that has metastasized from other areas of the body. For example, breast, lung, and prostate cancer commonly cause bone metastasis.
Symptoms of bone cancer may include fatigue, unintended weight loss, bone pain, swelling, tenderness, and weakened bone leading to fractures. Diagnostic testing may include a bone scan, X-ray, CT scan, MRI, PET scan, and bone biopsy. Treatment is based on the type of cancer, the stage of the cancer, and the client’s overall health and preferences. For example, some bone cancers are treated with surgery; some are treated with surgery and chemotherapy; and others are treated with surgery, chemotherapy, and radiation therapy.[1]
Cerebral Palsy
Cerebral palsy (CP) is a group of disorders that affects the ability to move and maintain balance and posture. “Cerebral” means having to do with the brain, and “palsy” means weakness or problems with using the muscles. CP is caused by abnormal brain development or damage to the developing brain that affects the ability to control muscles.[2]
The symptoms of CP vary from person to person. A person with severe CP might require the use of special equipment to walk or might not be able to walk at all and need lifelong care. A person with mild CP, on the other hand, might walk a little awkwardly, but otherwise not require specialized care. Doctors classify CP according to the main type of movement disorder involved. Depending on which areas of the brain are affected, one or more of the following movement disorders can occur[3]:
- Spasticity: Stiff muscles
- Dyskinesia: Uncontrollable movements
- Ataxia: Poor balance and coordination
There is no cure for CP, but treatment can improve the quality of life for people who have the condition. After CP is diagnosed, a team of health professionals works with the child and family to develop a plan to help the child reach their optimal potential. Common treatments include medications; surgery; braces; and physical, occupational, and speech therapy.[4]
See Figure 10.39[5] for an image of David Smith who has cerebral palsy and is a Paralympian. Paralympians are athletes with a range of impairments who compete in the Paralympics, a competition similar to the Olympics. Paralympic athletes inspire people around the world with their performances and focus on moving forward and never giving up.[6]

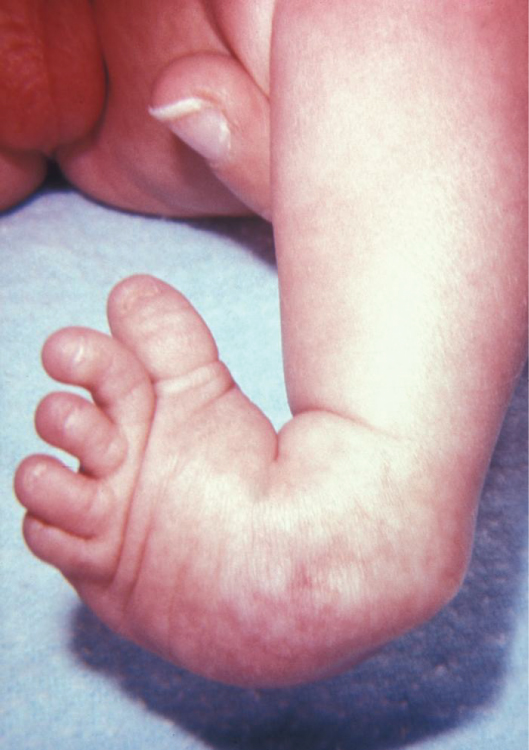
Clubfoot
Clubfoot is a congenital condition that causes the foot and lower leg to turn inward and downward. See Figure 10.40[7] for an image of an infant with a clubfoot. Clubfoot can range from mild and flexible to severe and rigid. Treatment by an orthopedic specialist involves using repeated applications of casts beginning soon after birth to gradually moving the foot into the correct position. Severe cases of clubfoot require surgery. After the foot is in the correct position, the child typically wears a special brace for up to three years.[8]
Contracture
A contracture is a condition of shortening and hardening of muscles, tendons, or other tissue, often leading to deformity and rigidity of joints. Contractures are caused by immobility and can happen in as little as two days if the joint remains immobile. It can be the result of several disorders such as a stroke, cerebral palsy, or muscular dystrophy. Contractures may be prevented and/or treated with braces, physical therapy, and range-of-motion exercises.[9] See Figure 10.41[10] for an image of a hand contracture.

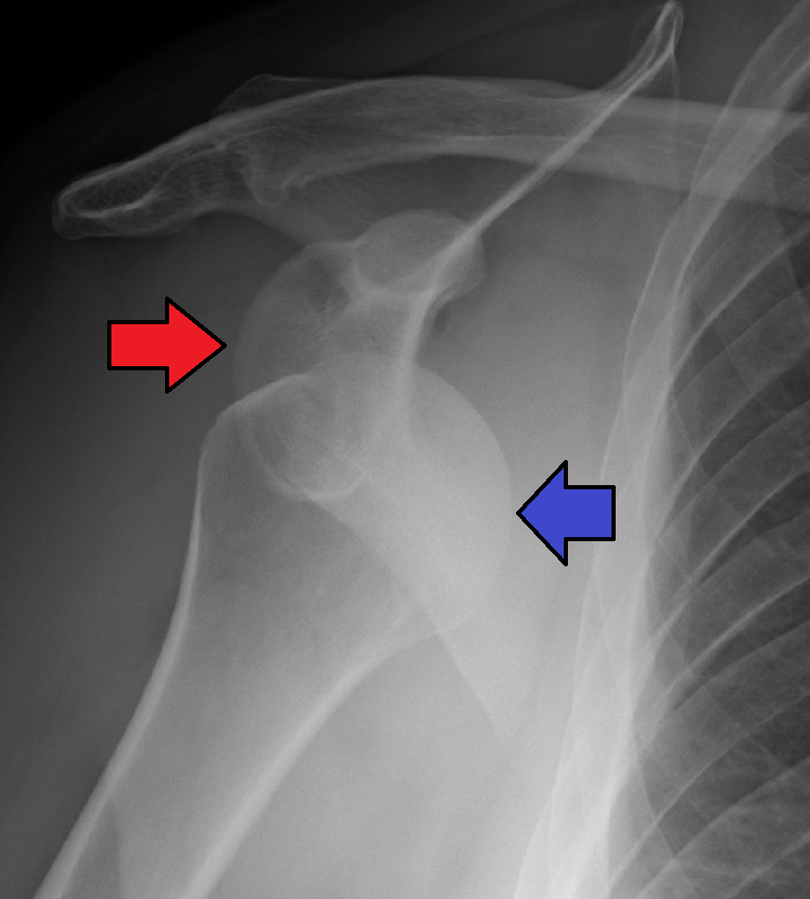
Dislocation and Subluxation
A dislocation is an injury, often caused by a fall or a blow to the joint, that forces the ends of bones out of position. Subluxation refers to partial dislocation of a joint, resulting in structural displacement. Dislocated joints are typically very painful, swollen, and visibly out of place. The client may not be able to move the affected extremity. See Figure 10.42[11] for an X-ray image of an anterior dislocation of the right shoulder where the ball (i.e., head of the humerus) has popped out of the socket (i.e., the glenoid cavity of the scapula). A dislocated joint requires immediate medical attention. Treatment depends on the joint and the severity of the injury and may include manipulation to reposition the bones, medication, a splint or sling, or rehabilitation. When properly repositioned, a joint will usually function and move normally again in a few weeks; however, once a joint is dislocated, it is more likely to become dislocated again. Instructing clients to wear protective gear during sports may help to prevent future dislocations.[12]
Fibromyalgia
Fibromyalgia is a condition that causes widespread pain, sleep problems, fatigue, and often emotional and mental distress. People with fibromyalgia may be more sensitive to pain than people without fibromyalgia, referred to as abnormal pain perception processing. The cause of fibromyalgia is not known, but it can be effectively treated and managed.[13]
Common symptoms of fibromyalgia include the following:
- Pain and stiffness all over the body
- Fatigue and tiredness
- Depression and anxiety
- Sleep problems
- Problems with thinking, memory, and concentration
- Headaches, including migraines
- Tingling or numbness in hands and feet
- Pain in the face or jaw, including disorders of the jaw known as temporomandibular joint syndrome (TMJ)
- Digestive problems, such as abdominal pain, bloating, constipation, and irritable bowel syndrome (IBS)
Fibromyalgia is treated by a doctor or team of health care professionals who specialize in the treatment of fibromyalgia. A combination of treatments is typically prescribed, which may include the following[14]:
- Medications, including prescription drugs and over-the-counter pain relievers
- Aerobic exercise and muscle strengthening exercise
- Client education classes
- Stress management techniques such as meditation, yoga, and massage
- Good sleep habits to improve the quality of sleep
- Cognitive behavioral therapy, a type of talk therapy that helps people change the way they think about their life circumstances
Foot Drop
Foot drop is the inability to raise the front part of the foot due to weakness or paralysis of the muscles that lift the foot. As a result, individuals with foot drop often scuff their toes along the ground when walking or bend their knees to lift their foot higher than usual to avoid the scuffing. Foot drop is a symptom of an underlying problem and can be temporary or permanent, depending on the cause. The prognosis for foot drop depends on the cause. Foot drop caused by trauma or nerve damage usually shows partial or complete recovery, but in progressive neurological disorders, foot drop will be a symptom that is likely to continue as a lifelong disability. Treatment depends on the specific cause of foot drop. The most common treatment is to support the foot with lightweight leg braces. See Figure 10.43[15] for an image of a client with foot drop treated with a leg brace. Exercise therapy to strengthen the muscles and maintain joint motion also helps to improve a client’s gait.[16]

Gout
Gout is a type of inflammatory arthritis that causes pain and swelling in the joints, usually as flares that last for one or two weeks and then resolve. Gout flares often begin in the big toe or a lower limb. Gout occurs when high levels of serum uric acid form needle-shaped crystals in and around the joint and cause inflammation. Uric acid is a waste product produced by the breakdown of purine, a type of molecule found in many foods we eat. Gout is diagnosed with blood tests for uric acid. It is commonly treated with medications like nonsteroidal anti-inflammatories (NSAIDs) and colchicine.[17] It is common for gout to reoccur. Clients with recurring gout are treated with allopurinol to decrease chronic uric acid levels. See Figure 10.44[18] for an illustration of gout.

Read additional information about medications used to treat gout in “Antigout Medications” in the “Analgesics and Musculoskeletal System” chapter in Open RN Nursing Pharmacology, 2e.
Osteomyelitis
Osteomyelitis is an infection in a bone. Infections can reach a bone by traveling through the bloodstream or spreading from nearby tissue. Infections can also begin in the bone itself if an injury exposes the bone to bacteria. Smokers and people with chronic health conditions, such as diabetes or kidney failure, are at higher risk of developing osteomyelitis. People who have diabetes may develop osteomyelitis in their feet if they develop foot ulcers. Although once considered incurable, osteomyelitis can now be successfully treated with surgery and intravenous antibiotics typically administered over a long period of time, such as four to six weeks.[19]
Muscular Dystrophy
Muscular dystrophy (MD) refers to a group of diseases caused by abnormal muscle development due to gene mutations. Muscular dystrophy can run in families, or a person can be the first in their family to have muscular dystrophy. Over time, muscle weakness decreases mobility and makes it difficult to perform everyday tasks. There are many types of muscular dystrophy, each affecting specific muscle groups. Each type has signs and symptoms that appear at different ages and vary in severity.[20]
An example of one type of MD is Duchenne muscular dystrophy (DMD), a genetic disorder characterized by progressive muscle degeneration and weakness due to the alterations of a muscle protein called dystrophin. DMD symptom onset is in early childhood, usually between the ages two and three. The disease primarily affects boys. Muscle weakness is the principal symptom of DMD and begins by first affecting the proximal muscles (those closest to the core of the body) and later affecting the distal limb muscles. The child with DMD might have difficulty jumping, running, and walking. Other symptoms include enlargement of the calves, a waddling gait, and lumbar lordosis (an inward curve of the spine). The heart and respiratory muscles are affected as well. Progressive weakness and scoliosis result in impaired pulmonary function, which can eventually cause acute respiratory failure. Treatment of DMD requires multidisciplinary care to coordinate specialized assessments and interventions needed to maximize function and quality of life. Due to recent advances in cardiology and pulmonology, people with DMD are living longer than ever and often well into adulthood.[21]
The impact of DMD can be significantly minimized by keeping the body as flexible, upright, and mobile as possible. As muscle deteriorates, a person with muscular dystrophy often develops contractures. If not treated, contractures can become severe, causing discomfort and restricting mobility and flexibility. Contractures can affect the knees, hips, feet, elbows, wrists, and fingers. However, there are many ways to minimize and postpone contractures. Range-of-motion exercises performed on a regular schedule help delay contractures by keeping tendons from shortening prematurely. Braces on the lower legs also can help keep the limbs stretched and flexible, delaying the onset of contractures. Eventually, a wheelchair is needed, typically by about age 12. Although a child and their parents may dread using a wheelchair, many people find that when they start to use one, they are more mobile, energetic, and independent than when trying to walk without assistance[22] See Figure 10.45[23] for an image of a child with MD using a specialized wheelchair called an “Easy Stand” that supports him while sitting and also allows him to stand for periods of time.

Myasthenia Gravis
Myasthenia gravis (MG) is a chronic, autoimmune, neuromuscular disease that causes weakness in voluntary muscles, including those required for breathing and swallowing. Onset of symptoms can be rapid.[24]
Paralysis
Paralysis occurs when an injury or medical condition disrupts the nerve signals to the muscles, resulting in being unable to make voluntary movements. Common causes of paralysis include spinal cord injuries and strokes. Paralysis can be localized, where it affects specific areas of the body, such as the face. For example, Bell’s palsy temporarily paralyzes facial muscles. Paralysis can also be generalized where it affects a larger area of the body. There are categories of generalized paralysis based on its extent. Common categories include hemiplegia, paraplegia, and quadriplegia/tetraplegia[25]:
- Hemiplegia: Paralysis affects one side of the body, for example, an arm and a leg on the same side.
- Paraplegia: Paralysis affects both legs and sometimes the torso.
- Quadriplegia or Tetraplegia: Cervical nerves are damaged, causing paralysis in all limbs, with little or no movement from the neck down.
See Figure 10.46[26] for an illustration of paraplegia, hemiplegia, and tetraplegia (quadriplegia), where pink indicates the area of muscle paralysis. Because muscle paralysis is caused by disruption of nerve signals, the cervical (C), thoracic (T), and lumbar (L) nerves are labeled in the image.

Paralysis is also classified by its effect on muscles in terms of being flaccid or spastic[27]:
- Flaccid: The muscles atrophy (i.e., shrink) due to loss of function.
- Spastic: The muscles tighten, causing uncontrollable jerks and spasms.
There is no cure for permanent paralysis caused by spinal nerve damage because the spinal cord can’t heal itself. However, rehabilitative services like physical and occupational therapy can help people with paralysis live independently and enjoy a quality life. Equipment used for rehabilitative/restorative care may include the following[28]:
- Adaptive equipment: Equipment that allows people to feed themselves or drive.
- Assistive equipment: Equipment that enhances mobility, such as wheelchairs, scooters, crutches, and canes.
- Orthotic/prosthetic devices: Devices that support the limbs and prevent contractures, such as braces.
- Voice-activated technology: Technology that doesn’t require the need for touch or movement, such as computers, lighting systems, and phones.
See Figure 10.47[29] for an image of Mark Manion, founder of “Mark Speaks Out.” Mark was permanently disabled during a cross-country biking trip when he was struck by a drunk driver. He travels the country educating and inspiring audiences on how he has effectively coped with his life circumstances.

Rhabdomyolysis
Rhabdomyolysis refers to the breakdown of muscles that causes damage to the kidney. When muscle is damaged, a protein called myoglobin is released into the bloodstream and is filtered out of the body by the kidneys. Myoglobin breaks down into substances that damage kidney cells.[30] See Figure 10.48[31] for an illustration of rhabdomyolysis.
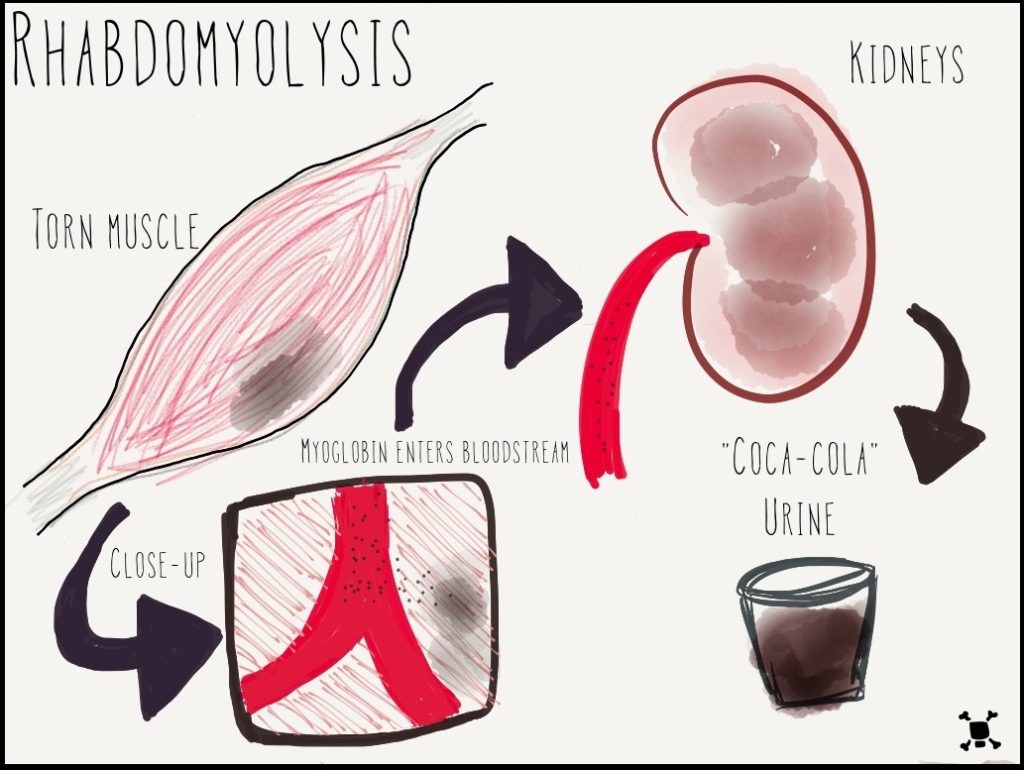
Rhabdomyolysis may be caused by injury or any other condition that damages skeletal muscle. Potential causes of rhabdomyolysis include the following conditions[32]:
- Trauma or crush injuries
- Use of drugs such as cocaine, amphetamines, statins, heroin, or phencyclidine (PCP)
- Genetic muscle diseases
- Extremes of body temperature
- Ischemia or death of muscle tissue
- Low phosphate levels
- Seizures or muscle tremors
- Severe exertion, such as marathon running or calisthenics
- Lengthy surgical procedures
- Severe dehydration
Symptoms of rhabdomyolysis include dark, red, or cola-colored urine; decreased urine output; weakness; and myalgia (i.e., muscle pain). Rhabdomyolysis is diagnosed with blood tests, including creatine kinase (CK), myoglobin, and creatinine, as well as urine tests such as urinalysis and urine myoglobin. Rhabdomyolysis is treated with intravenous fluids that contain bicarbonate. In cases causing severe kidney damage, dialysis may be required.[33]
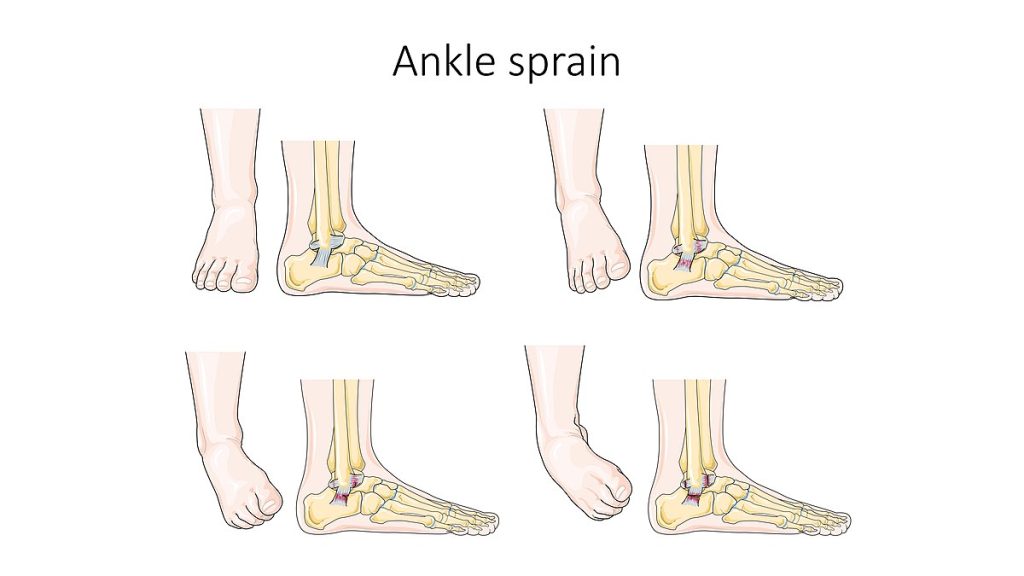
Strains and Sprains
A strain is an injury to a muscle or tendon from being overstretched or torn, causing pain. Strains can be caused by an injury, overusing a muscle, or using a muscle in the wrong way (such as twisting the back while lifting a heavy object). A sprain is an injury to a joint when a ligament is stretched or torn. See Figure 10.49[34] for an illustration of an ankle sprain.
Initial treatments for strains and sprains are similar and can be easily recalled by the mnemonic called RICE, which stands for the following[35]:
- Rest: Rest the strain or sprain for at least 24 hours. The health care provider may recommend not putting any weight on the injured area for 48 to 72 hours, so crutches may be needed for lower extremity injuries.
- Ice: Apply ice as soon as possible after the injury to reduce swelling. The ice should not be applied directly to the skin but should be wrapped in a cloth to avoid tissue injury. Ice should be applied for 5 to 20 minutes, four to eight times a day, for the first 48 hours or until swelling improves.
- Compression: Compress the area with an elastic wrap or bandage to reduce swelling.
- Elevate: Elevate the injured limb above the heart whenever possible to help prevent or limit swelling.
Tendonitis
Tendonitis refers to inflammation of a tendon, causing pain around a joint. Tendonitis usually happens after repeated injury to an area such as the wrist or ankle. Common forms of tendonitis are named after the sports that increase their risk, such as tennis elbow, golfer’s elbow, pitcher’s shoulder, swimmer’s shoulder, and jumper’s knee. Health care providers diagnose tendonitis based on medical history, a physical exam, and possible imaging tests. Initial treatment is focused on reducing pain and swelling with RICE (rest, ice, compression, and elevation). Other treatments may include ultrasound, physical therapy, steroid injections, and surgery in severe cases.[36]
Vertebral Disorders
The spine is composed of many vertebrae stacked on top of one another, forming the vertebral column. There are several disorders that can occur in the vertebral column causing abnormal curvature of the spine such as kyphosis, lordosis, and scoliosis. See Figure 10.50[37] for an illustration of kyphosis, lordosis, and scoliosis.

Kyphosis is a curving of the spine that causes a bowing or rounding of the back, often referred to as a “buffalo hump,” that can lead to a hunchback or slouching posture. Kyphosis can be caused by osteoarthritis, osteoporosis, or other conditions. Pain in the middle or lower back is the most common symptom. Treatment depends upon the cause, the severity of pain, and the presence of any neurological symptoms.[38]
Lordosis is the inward curve of the lumbar spine just above the buttocks. A small degree of lordosis is normal, especially during the third trimester of pregnancy. Too much curving of the lower back is often called swayback. Most of the time, lordosis is not treated if the back is flexible because it is not likely to progress or cause problems.[39]
Scoliosis causes a sideways curve of the spine. It commonly develops in late childhood and the early teens when children grow quickly. Symptoms of scoliosis include leaning to one side and having uneven shoulders and hips. Treatment depends on the client’s age, the amount of expected additional growth, the degree of curving, and whether the curve is temporary or permanent. Clients with mild scoliosis might only need checkups to monitor if the curve is getting worse, whereas others may require a brace or have surgery.[40]
- Mayo Clinic. (2023, May 11). Bone cancer. https://www.mayoclinic.org/diseases-conditions/bone-cancer/symptoms-causes/syc-20350217 ↵
- Centers for Disease Control and Prevention. (2023, October 6). What is cerebral palsy? https://www.cdc.gov/ncbddd/cp/facts.html ↵
- Centers for Disease Control and Prevention. (2023, October 6). What is cerebral palsy? https://www.cdc.gov/ncbddd/cp/facts.html ↵
- Centers for Disease Control and Prevention. (2023, October 6). What is cerebral palsy? https://www.cdc.gov/ncbddd/cp/facts.html ↵
- “David_Smith_and_his_Boccia_medals_(cropped).jpg” by Richard Gillin from St Albans, UK is licensed under CC BY-SA 2.0 ↵
- International Paralympic Committee. (n.d.). FAQ. https://www.paralympic.org/frequently-asked-questions ↵
- “813 Clubfoot.jpg” by OpenStax is licensed under CC BY 3.0 ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Club foot; [updated 2020, Sep 16; cited 2020, Sep 18]. https://medlineplus.gov/ency/article/001228.htm ↵
- Friedlander, T., Masterson, R., & Mahesh, K. (2023, July 20). Contractures. PM&R KnowledgeNow. https://now.aapmr.org/contractures/#:~:text=Soft%20tissue%20changes%20that%20contribute,fibers%20occurs%20within%2024%20hours ↵
- “Freeman-Sheldon_syndrome.JPG” by MI Poling at English Wikipedia is licensed under CC BY-SA 2.5 ↵
- “AnterDisAPMark.png” by James Heilman, MD is licensed under CC BY-SA 4.0 ↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2019, Feb 7]. Dislocations; [reviewed 2016, Oct 26; cited 2020, Sep 18]. https://medlineplus.gov/dislocations.html ↵
- Centers for Disease Control and Prevention. (2022). Fibromyalgia. https://www.cdc.gov/arthritis/basics/fibromyalgia.htm ↵
- Centers for Disease Control and Prevention. (2022). Fibromyalgia. https://www.cdc.gov/arthritis/basics/fibromyalgia.htm ↵
- “AFO brace for foot drop.JPG” by Pagemaker787 is licensed under CC BY-SA 4.0 ↵
- National Institute of Neurological Disorders and Stroke. (2019, March 27). Foot drop information page. https://www.ninds.nih.gov/Disorders/All-Disorders/Foot-Drop-Information-Page ↵
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. (2020, February). Gout. National Institutes of Health. https://www.niams.nih.gov/health-topics/gout ↵
- “Gout_Signs_and_Symptoms.jpg” by www.scientificanimations.com is licensed under CC BY-SA 4.0 ↵
- Mayo Clinic. (2022, November 8). Osteomyelitis. https://www.mayoclinic.org/diseases-conditions/osteomyelitis/symptoms-causes/syc-20375913 ↵
- Centers for Disease Control and Prevention. (2022, November 21). What is muscular dystrophy? https://www.cdc.gov/ncbddd/musculardystrophy/facts.html ↵
- Muscular Dystrophy Association. (n.d.). Duchenne muscular dystrophy. https://www.mda.org/disease/duchenne-muscular-dystrophy ↵
- Muscular Dystrophy Association. (n.d.). Duchenne muscular dystrophy. https://www.mda.org/disease/duchenne-muscular-dystrophy ↵
- “3576255511_4c36222845_b.jpg” by EasyStand is licensed under CC BY-NC-ND 2.0 ↵
- National Institute of Neurological Disorders and Stroke. (2023, November). Myasthenia gravis. National Institutes of Health. https://www.ninds.nih.gov/health-information/disorders/myasthenia-gravis ↵
- Cleveland Clinic. (2021, June 10). Paralysis. https://my.clevelandclinic.org/health/diseases/15345-paralysis ↵
- “Neurological_Levels_%26_Types_of_Paralysis.png” by Servier Medical Art is licensed under CC BY 2.0 ↵
- Cleveland Clinic. (2021, June 10). Paralysis. https://my.clevelandclinic.org/health/diseases/15345-paralysis ↵
- Cleveland Clinic. (2021, June 10). Paralysis. https://my.clevelandclinic.org/health/diseases/15345-paralysis ↵
- “USMC-100519-M-3215R-002.jpg” by unknown author for United States Marine Corps is licensed in the Public Domain ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2023. Rhabdomyolysis; [reviewed 2021, Jul 27; cited 2023, Nov 28). https://medlineplus.gov/ency/article/000473.htm ↵
- “Rhabdo.jpg” by AquapatMedia is licensed under CC BY-SA 3.0 ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2023. Rhabdomyolysis; [reviewed 2021, Jul 27; cited 2023, Nov 28). https://medlineplus.gov/ency/article/000473.htm ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2023. Rhabdomyolysis; [reviewed 2021, Jul 27; cited 2023, Nov 28). https://medlineplus.gov/ency/article/000473.htm ↵
- “Ankle_sprain_--_Smart-Servier.jpg” by SMART-Servier Medical Art, part of Laboratoires Servier is licensed under CC BY-SA 3.0 ↵
- Mayo Clinic. (2022, March 22). Sprain: First aid. https://www.mayoclinic.org/first-aid/first-aid-sprain/basics/art-20056622 ↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2022, Apr. 4]. Tendinitis; [cited 2017, Mar. 16]. https://medlineplus.gov/tendinitis.html ↵
- “Vertebral column disorders - Normal Scoliosis Lordosis Kyphosis -- Smart-Servier.jpg” by Laboratoires Servier is licensed under CC BY-SA 3.0 ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Kyphosis; [updated 2020, Sep 16; cited 2020, Sep 18]. https://medlineplus.gov/ency/article/001240.htm ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Lordosis - lumbar; [updated 2020, Sep 16; cited 2020, Sep 18]. https://medlineplus.gov/ency/article/003278.htm ↵
- MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US); [updated 2020, Apr 29]. Scoliosis; [reviewed 2016, Oct 18; cited 2020, Sep 18]. https://medlineplus.gov/scoliosis.html ↵
Standard Versus Transmission-Based Precautions
Standard Precautions
Standard precautions are used when caring for all patients to prevent health care associated infections. According to the Centers for Disease Control and Prevention (CDC), standard precautions are “the minimum infection prevention practices that apply to all patient care, regardless of suspected or confirmed infection status of the patient, in any setting where health care is delivered.”[1] They are based on the principle that all blood, body fluids (except sweat), nonintact skin, and mucous membranes may contain transmissible infectious agents. These standards reduce the risk of exposure for the health care worker and protect the patient from potential transmission of infectious organisms.
Current standard precautions according to the CDC (2019) include the following:
- Appropriate hand hygiene
- Use of personal protective equipment (e.g., gloves, gowns, masks, eyewear) whenever infectious material exposure may occur
- Appropriate patient placement and care using transmission-based precautions when indicated
- Respiratory hygiene/cough etiquette
- Proper handling and cleaning of environment, equipment, and devices
- Safe handling of laundry
- Sharps safety (i.e., engineering and work practice controls)
- Aseptic technique for invasive nursing procedures such as parenteral medication administration[2]
Each of these standard precautions is described in more detail in the following subsections.
Transmission-Based Precautions
In addition to standard precautions, transmission-based precautions are used for patients with documented or suspected infection, or colonization, of highly transmissible or epidemiologically important pathogens. Epidemiologically important pathogens include, but are not limited to, Coronavirus disease (COVID-19), Clostridium difficile (C-diff), Methicillin-resistant staphylococcus aureus (MRSA), Vancomycin-resistant enterococci (VRE), Respiratory syncytial sirus (RSV), measles, and tuberculosis (TB). For patients with these types of pathogens, standard precautions are used along with specific transmission-based precautions.
There are four categories of transmission-based precautions: contact precautions, enhanced barrier precautions, droplet precautions, and airborne precautions. Transmission-based precautions are used when the route(s) of transmission is (are) not completely interrupted using standard precautions alone. Some diseases, such as tuberculosis, have multiple routes of transmission so more than one transmission-based precautions category must be implemented. See Table 4.2 outlining the categories of transmission precautions with associated PPE and other precautions. When possible, patients with transmission-based precautions should be placed in a single occupancy room with dedicated patient care equipment (e.g., blood pressure cuffs, stethoscope, thermometer). Transport of the patient and unnecessary movement outside the patient room should be limited. However, when transmission-based precautions are implemented, it is also important for the nurse to make efforts to counteract possible adverse effects of these precautions on patients, such as anxiety, depression, perceptions of stigma, and reduced contact with clinical staff.
Table 4.2 Transmission-Based Precautions[3]
| Precaution | Implementation | PPE and Other Precautions |
|---|---|---|
| Contact | Known or suspected infections with increased risk for contact transmission (e.g., draining wounds, fecal incontinence) or with epidemiologically important organisms, such as C-diff, MRSA, VRE, or RSV |
Note: Use only soap and water for hand hygiene in patients with C. difficile infection. |
| Enhanced barrier | Used during high-contact resident care activities for individuals colonized or infected with a multidrug-resistant organism (MDRO), as well as those at increased risk of MDRO acquisition |
|
| Droplet | Known or suspected infection with pathogens transmitted by large respiratory droplets generated by coughing, sneezing, or talking, such as influenza, coronavirus, or pertussis |
|
| Airborne | Known or suspected infection with pathogens transmitted by small respiratory droplets, such as measles, tuberculosis, and disseminated herpes zoster | Fit-tested N-95 respirator or PAPR
|
View a list of transmission-based precautions used for specific medical conditions at the CDC Guideline for Isolation Precautions.
Patient Transport
Several principles are used to guide transport of patients requiring transmission-based precautions. In the inpatient and residential settings, these principles include the following:
- Limiting transport for essential purposes only, such as diagnostic and therapeutic procedures that cannot be performed in the patient’s room
- Using appropriate barriers on the patient consistent with the route and risk of transmission (e.g., mask, gown, covering the affected areas when infectious skin lesions or drainage is present)
- Notify other health care personnel involved in the care of the patient of the transmission-based precautions. For example, when transporting the patient to radiology, inform the radiology technician of the precautions.[4]
Appropriate Hand Hygiene
Hand hygiene is the single most important practice to reduce the transmission of infectious agents in health care settings and is an essential element of standard precautions.[5] Routine handwashing during appropriate moments is a simple and effective way to prevent infection. However, it is estimated that health care professionals, on average, properly clean their hands less than 50% of the time it is indicated.[6] The Joint Commission, the organization that sets evidence-based standards of care for hospitals, recently updated its hand hygiene standards in 2018 to promote enforcement. If a Joint Commission surveyor witnesses an individual failing to properly clean their hands when it is indicated, a deficiency will be cited requiring improvement by the agency. This deficiency could potentially jeopardize a hospital’s accreditation status and their ability to receive payment for patient services. Therefore, it is essential for all health care workers to ensure they are using proper hand hygiene at the appropriate times.[7]
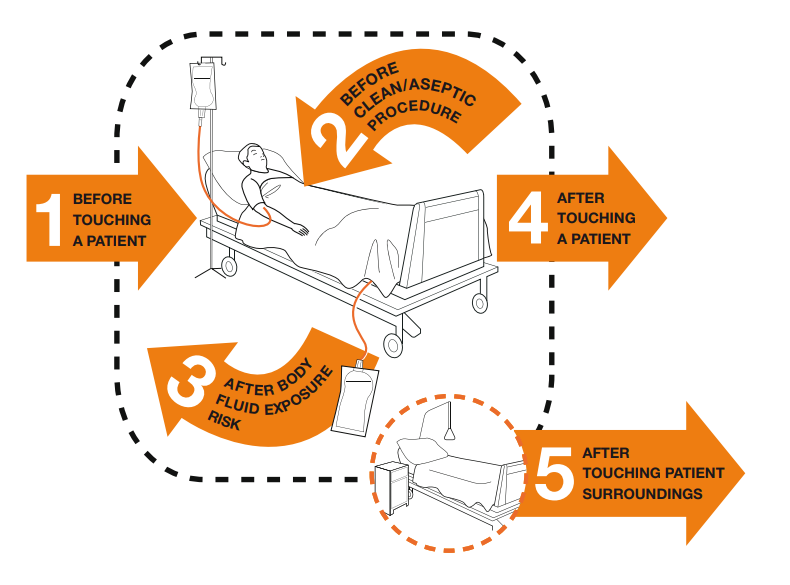
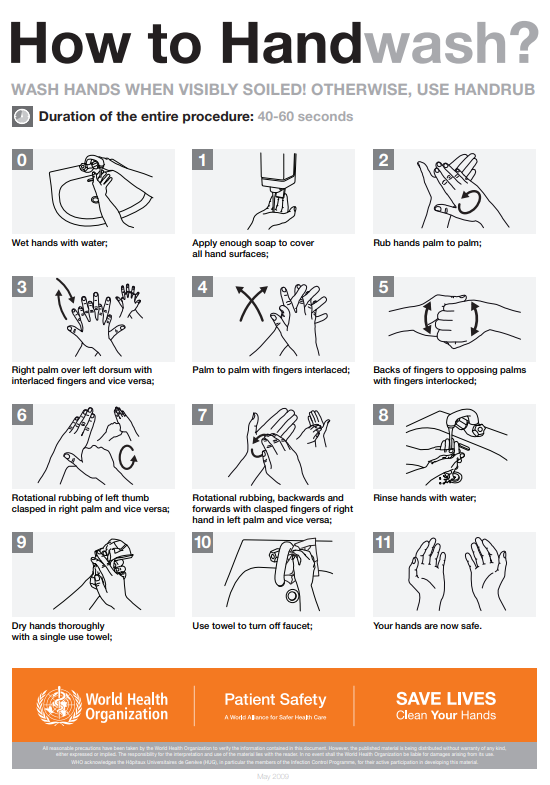
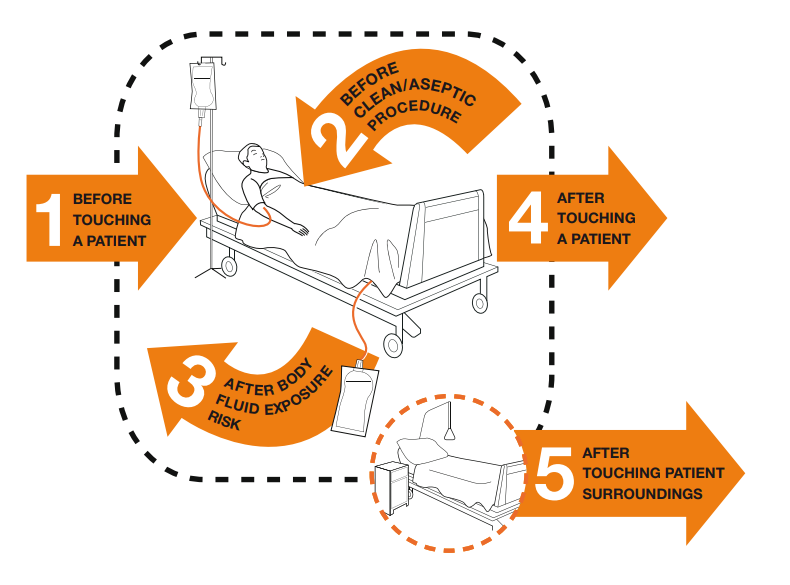
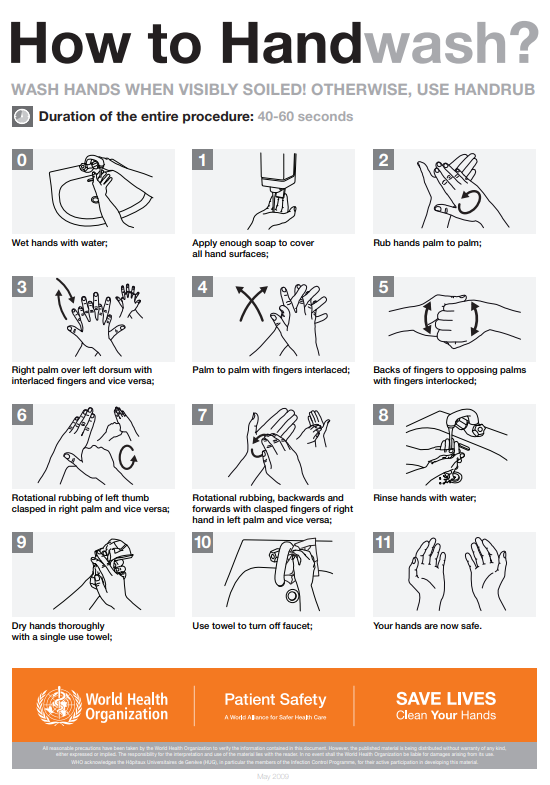
There are several evidence-based guidelines for performing appropriate hand hygiene. These guidelines include frequency of performing hand hygiene according to the care circumstances, solutions used, and technique performed. The Healthcare Infection Control Practices Advisory Committee (HICPAC) recommends health care personnel perform hand hygiene at specific times when providing care to patients. These moments are often referred to as the “Moments for Hand Hygiene.”[8] See Figures 4.1[9] and 4.2[10] for an illustration and application of the five moments of hand hygiene. The five moments of hand hygiene are as follows:
- Immediately before touching a patient
- Before performing an aseptic task or handling invasive devices
- Before moving from a soiled body site to a clean body site on a patient
- After touching a patient or their immediate environment
- After contact with blood, body fluids, or contaminated surfaces (with or without glove use)
When performing hand hygiene, washing with soap and water, or an approved alcohol-based hand rub solution that contains at least 60% alcohol, may be used. Unless hands are visibly soiled, an alcohol-based hand rub is preferred over soap and water in most clinical situations due to evidence of improved compliance. Handrubs are also preferred because they are generally less irritating to health care worker’s hands. However, it is important to recognize that alcohol-based rubs do not eliminate some types of germs, such as Clostridium difficile (C-diff).
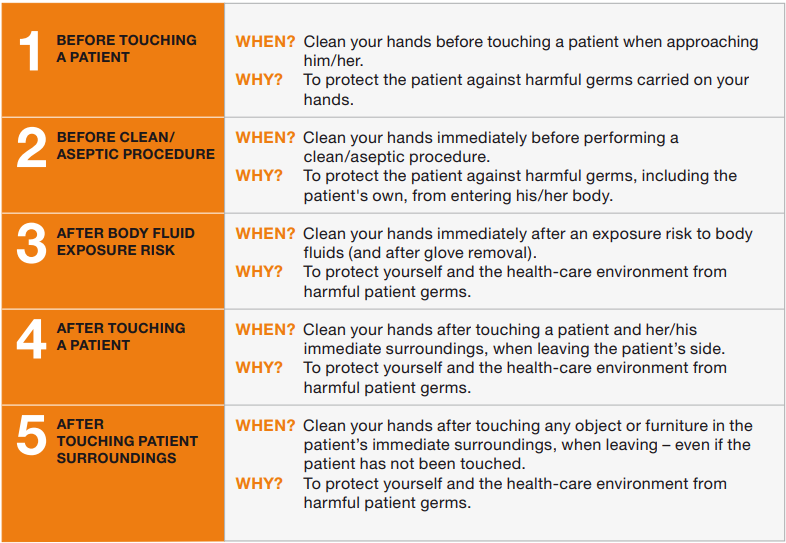
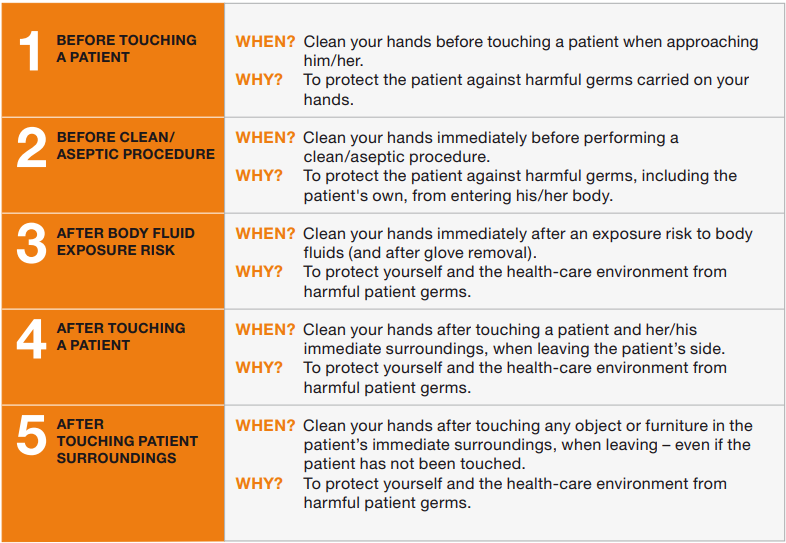
When using the alcohol-based handrub method, the CDC recommends the following steps. See Figure 4.3[11] for a handrub poster created by the World Health Organization.
- Apply product to the palm of one hand in an amount that will cover all surfaces.
- Rub hands together, covering all the surfaces of the hands, fingers, and wrists until the hands are dry. Surfaces include the palms and fingers, between the fingers, the backs of the hands and fingers, the fingertips, and the thumbs.
- The process should take about 20 seconds, and the solution should be dry.[12]
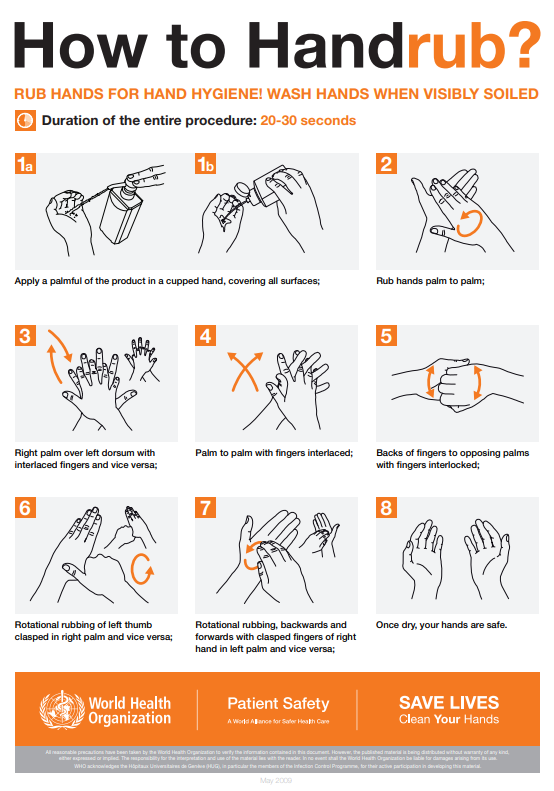
When washing with soap and water, the CDC recommends using the following steps. See Figure 4.4[13] for an image of a handwashing poster created by the World Health Organization.
- Wet hands with warm or cold running water and apply facility-approved soap.
- Lather hands by rubbing them together with the soap. Use the same technique as the handrub process to clean the palms and fingers, between the fingers, the backs of the hands and fingers, the fingertips, and the thumbs.
- Scrub thoroughly for at least 20 seconds.
- Rinse hands well under clean, running water.
- Dry the hands using a clean towel or disposable toweling.
- Use a clean paper towel to shut off the faucet.[14]
By performing hand hygiene at the proper moments and using appropriate techniques, you will ensure your hands are safe and you are not transmitting infectious organisms to yourself or others.
Hand Hygiene for Healthcare Workers on YouTube[15]
Personal Protective Equipment (PPE)
Personal protective equipment (PPE) includes gloves, gowns, face shields, goggles, and masks used to prevent the spread of infection to and from patients and health care providers. Depending on the anticipated exposure, PPE may include the use of gloves, a fluid-resistant gown, goggles or a face shield, and a mask or respirator. When used for a patient with transmission-based precautions, PPE supplies are typically stored in an isolation cart next to the patient’s room, and a card is posted on the door alerting staff and visitors to precautions needed before entering the room.
Gloves
Gloves protect both patients and health care personnel from exposure to infectious material that may be carried on the hands. Gloves are used to prevent contamination of health care personnel hands during activities such as the following:
- Anticipating direct contact with blood or body fluids, mucous membranes, nonintact skin, and other potentially infectious material
- Having direct contact with patients who are colonized or infected with pathogens transmitted by the contact route, such as Vancomycin-resistant enterococci (VRE), Methicillin-resistant staphylococcus aureus (MRSA), and Respiratory syncytial virus (RSV)
- Handling or touching visibly or potentially contaminated patient care equipment and environmental surfaces[16]
Nonsterile disposable medical gloves for routine patient care are made of a variety of materials, such as latex, vinyl, and nitrile. Many people are allergic to latex, so be sure to check for latex allergies for the patient and other health care professionals. See Figure 4.5[17] for an image of nonsterile medical gloves in various sizes in a health care setting. At times, gloves may need to be changed when providing care to a single patient to prevent cross-contamination of body sites. It is also necessary to change gloves if the patient interaction requires touching portable computer keyboards or other mobile equipment that is transported from room to room. Discarding gloves between patients is necessary to prevent transmission of infectious material. Gloves must not be washed for subsequent reuse because microorganisms cannot be reliably removed from glove surfaces, and continued glove integrity cannot be ensured.[18]

When gloves are worn in combination with other PPE, they are put on last. Gloves that fit snugly around the wrist should be used in combination with isolation gowns because they will cover the gown cuff and provide a more reliable continuous barrier for the arms, wrists, and hands.
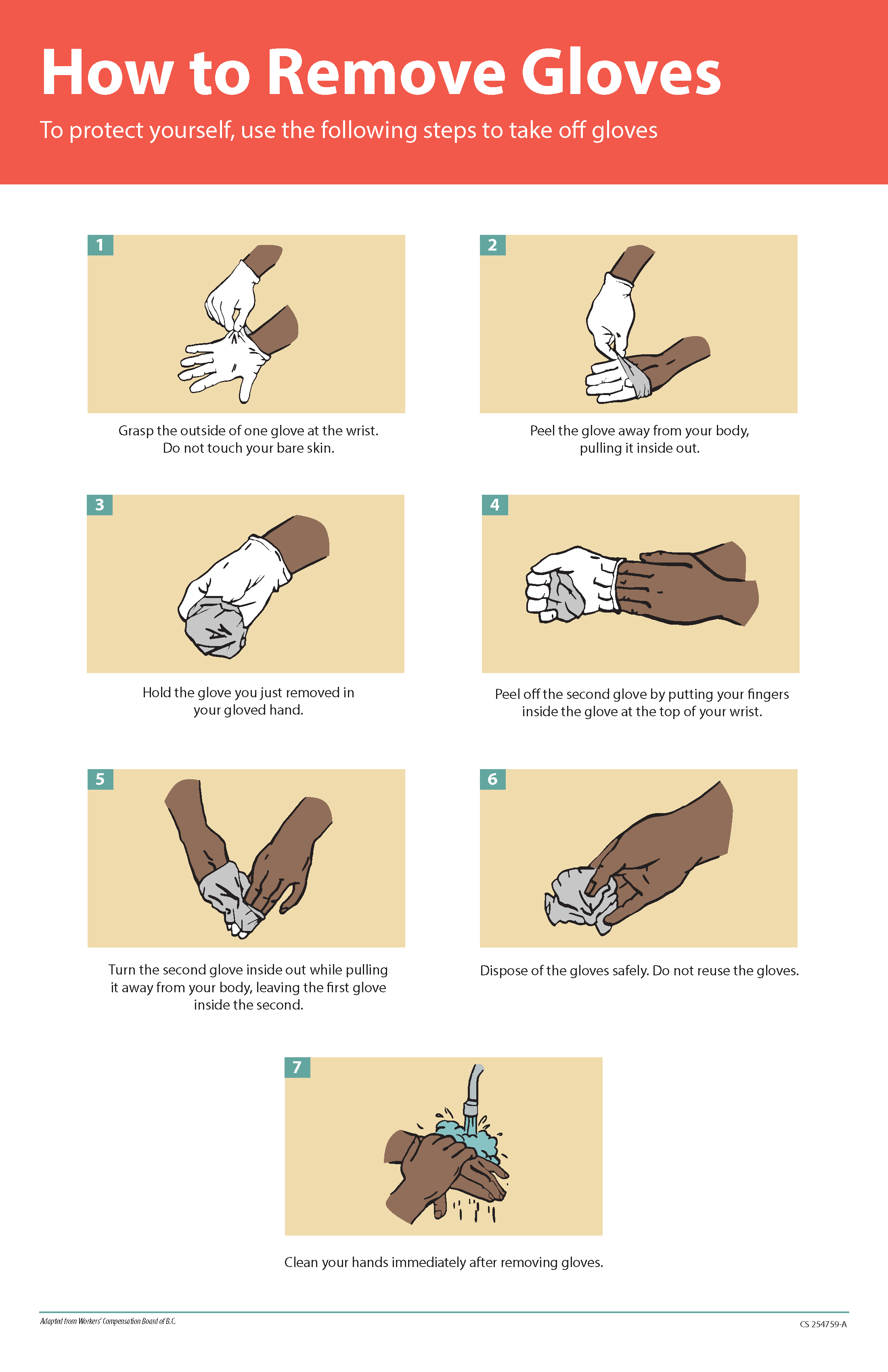
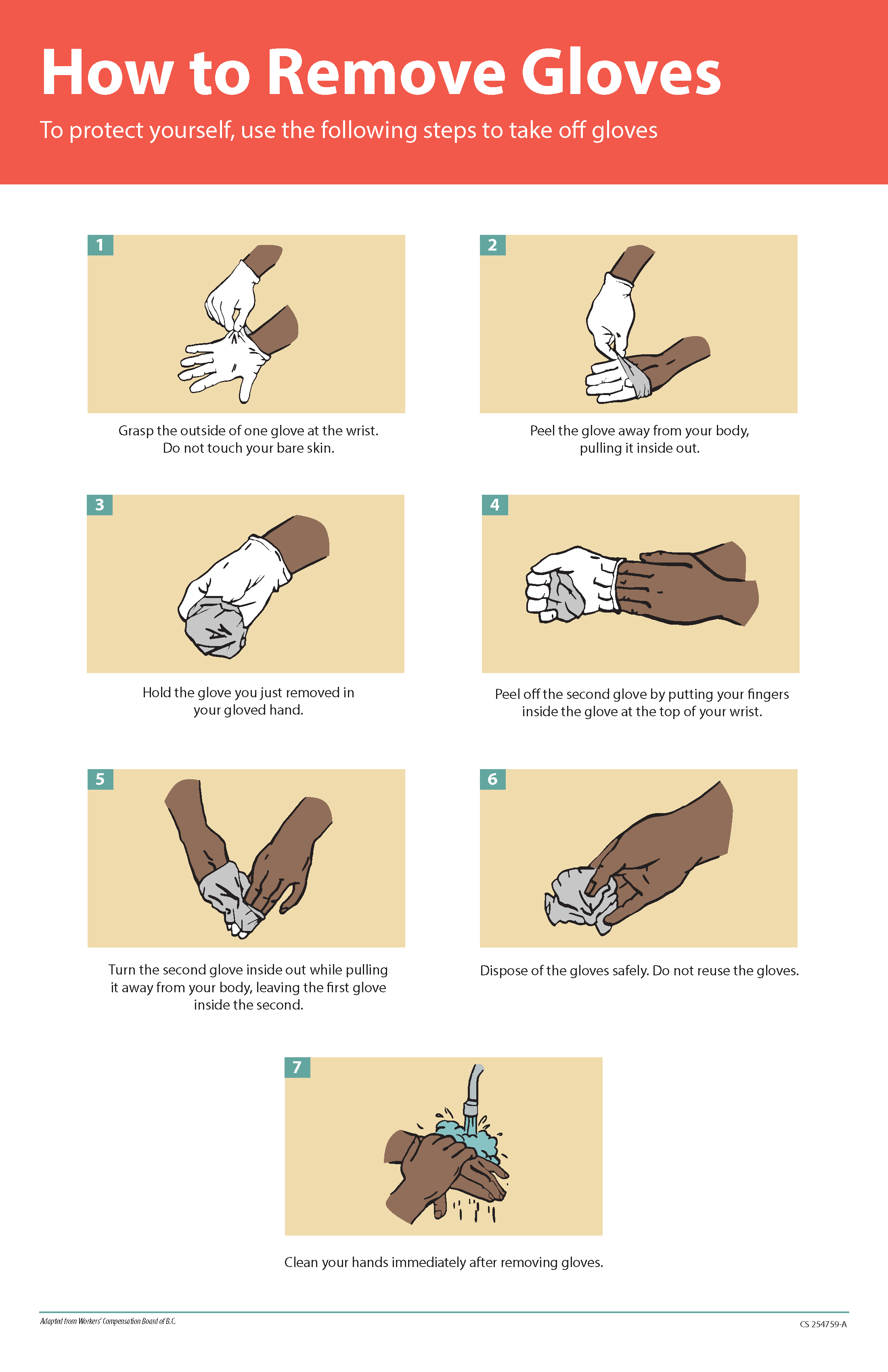
Gloves should be removed properly to prevent contamination. See Figure 4.6[19] for an illustration of properly removing gloves. Hand hygiene should be performed following glove removal to ensure the hands will not carry potentially infectious material that might have penetrated through unrecognized tears or contaminated the hands during glove removal. One method for properly removing gloves includes the following steps:
- Grasp the outside of one glove near the wrist. Do not touch your skin.
- Peel the glove away from your body, pulling it inside out.
- Hold the removed glove in your gloved hand.
- Put your fingers inside the glove at the top of your wrist and peel off the second glove.
- Turn the second glove inside out while pulling it away from your body, leaving the first glove inside the second.
- Dispose of the gloves safely. Do not reuse.
- Perform hand hygiene immediately after removing the gloves.[20]
Gowns
Isolation gowns are used to protect the health care worker’s arms and exposed body areas and to prevent contamination of their clothing with blood, body fluids, and other potentially infectious material. Isolation gowns may be disposable or washable/reusable. See Figure 4.7[21] for an image of a nurse wearing an isolation gown along with goggles and a respirator. When using standard precautions, an isolation gown is worn only if contact with blood or body fluid is anticipated. However, when contact transmission-based precautions are in place, donning of both gown and gloves upon room entry is indicated to prevent unintentional contact of clothing with contaminated environmental surfaces.
Gowns are usually the first piece of PPE to be donned. Isolation gowns should be removed before leaving the patient room to prevent possible contamination of the environment outside the patient’s room. Isolation gowns should be removed in a manner that prevents contamination of clothing or skin. The outer, “contaminated,” side of the gown is turned inward and rolled into a bundle, and then it is discarded into a designated container to contain contamination. See more information about putting on and removing PPE in the subsection below.[22]

Masks
The mucous membranes of the mouth, nose, and eyes are susceptible portals of entry for infectious agents. Masks are used to protect these sites from entry of large infectious droplets. See Figure 4.8[23] for an image of nurse wearing a surgical mask. Masks have three primary purposes in health care settings:
- Used by health care personnel to protect them from contact with infectious material from patients (e.g., respiratory secretions and sprays of blood or body fluids), consistent with standard precautions and droplet transmission precautions
- Used by health care personnel when engaged in procedures requiring sterile technique to protect patients from exposure to infectious agents potentially carried in a health care worker’s mouth or nose
- Placed on coughing patients to limit potential dissemination of infectious respiratory secretions from the patient to others in public areas (i.e., respiratory hygiene)[24]
Masks may be used in combination with goggles or a face shield to provide more complete protection for the face. Masks should not be confused with respirators used during airborne transmission-based precautions to prevent inhalation of small, aerosolized infectious droplets.[25]

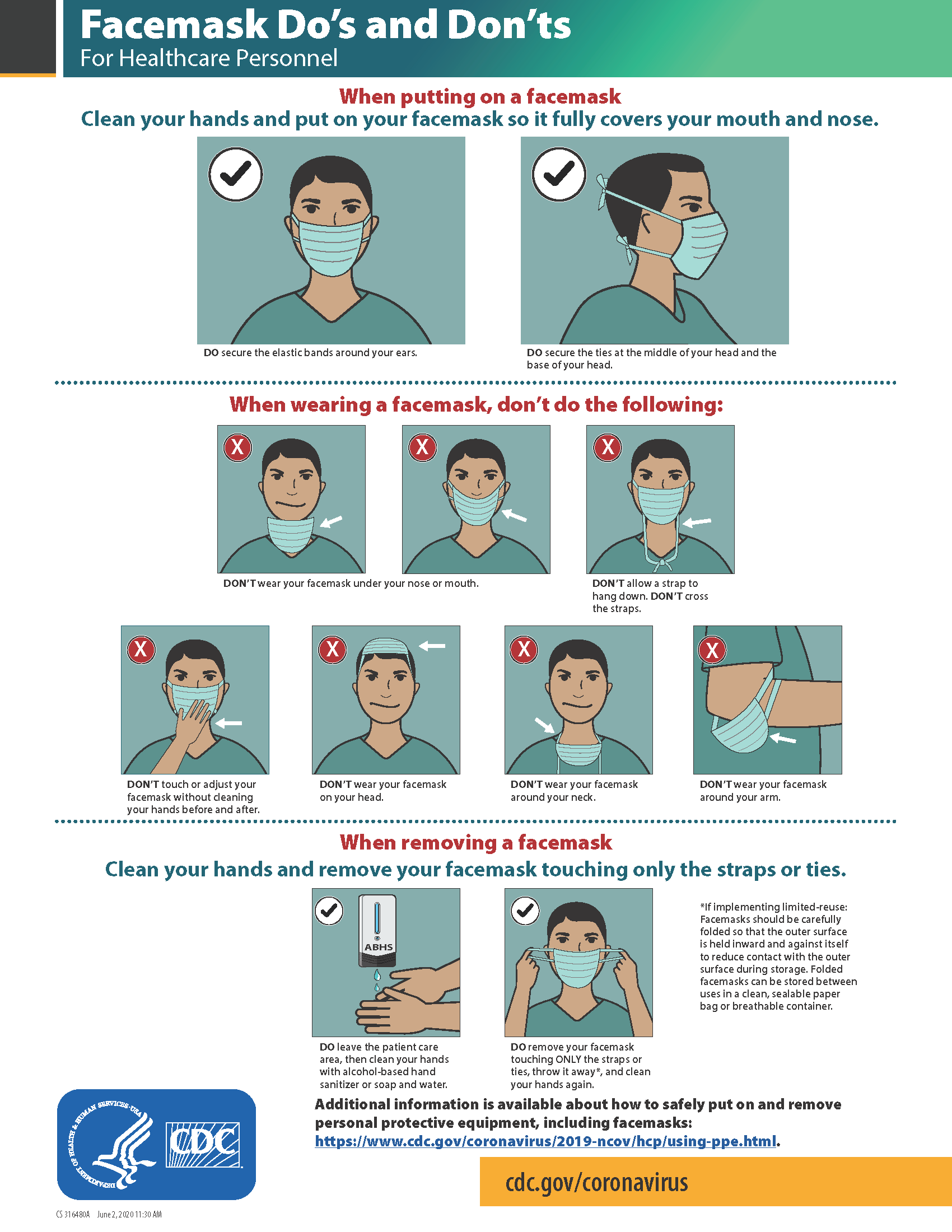
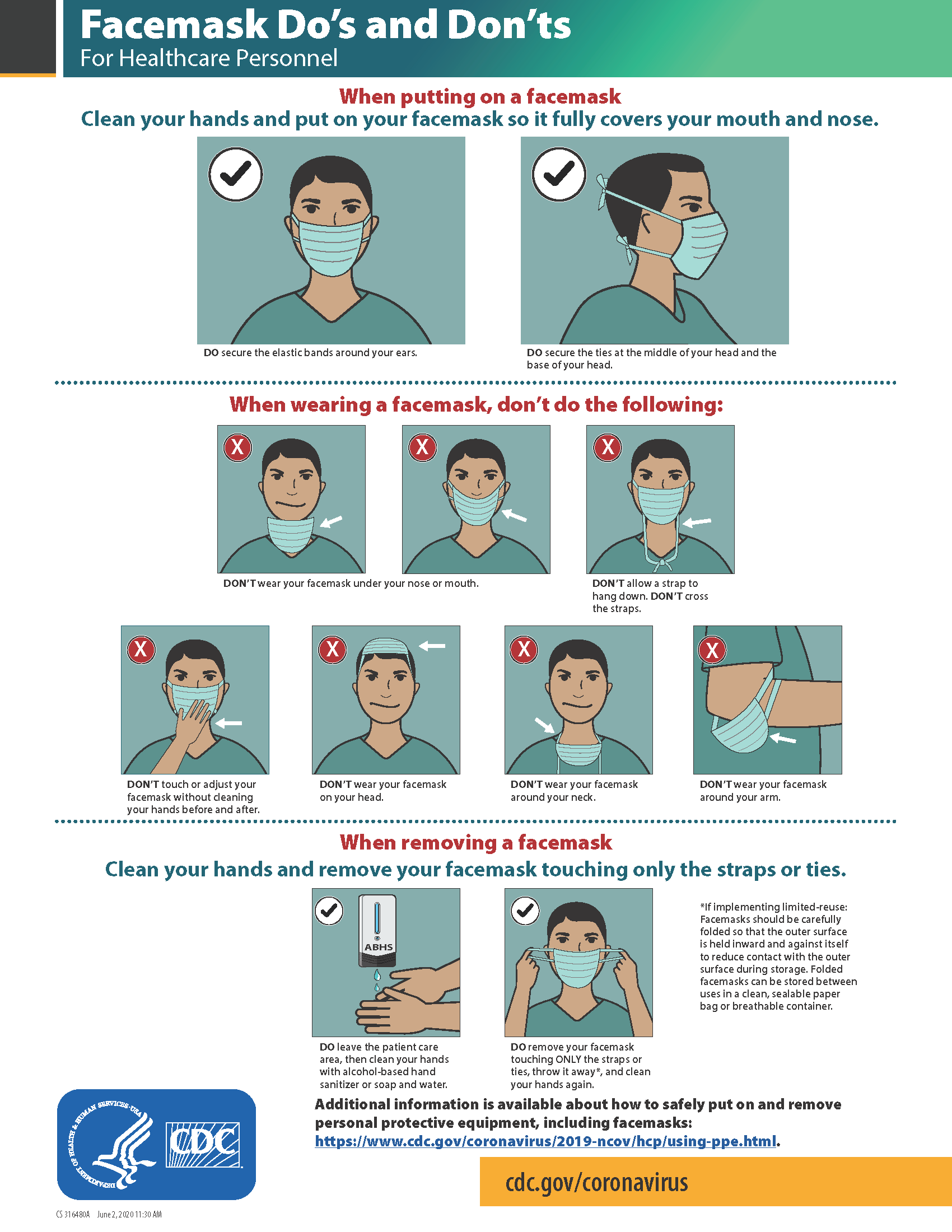
It is important to properly wear and remove masks to avoid contamination. See Figure 4.9[26] for CDC face mask recommendations for health care personnel.
Goggles/Face Shields
Eye protection chosen for specific work situations (e.g., goggles or face shields) depends upon the circumstances of exposure, other PPE used, and personal vision needs. Personal eyeglasses are not considered adequate eye protection. See Figure 4.10[27] for an image of a health care professional wearing a face shield along with a N95 respirator.

Respirators and PAPRs
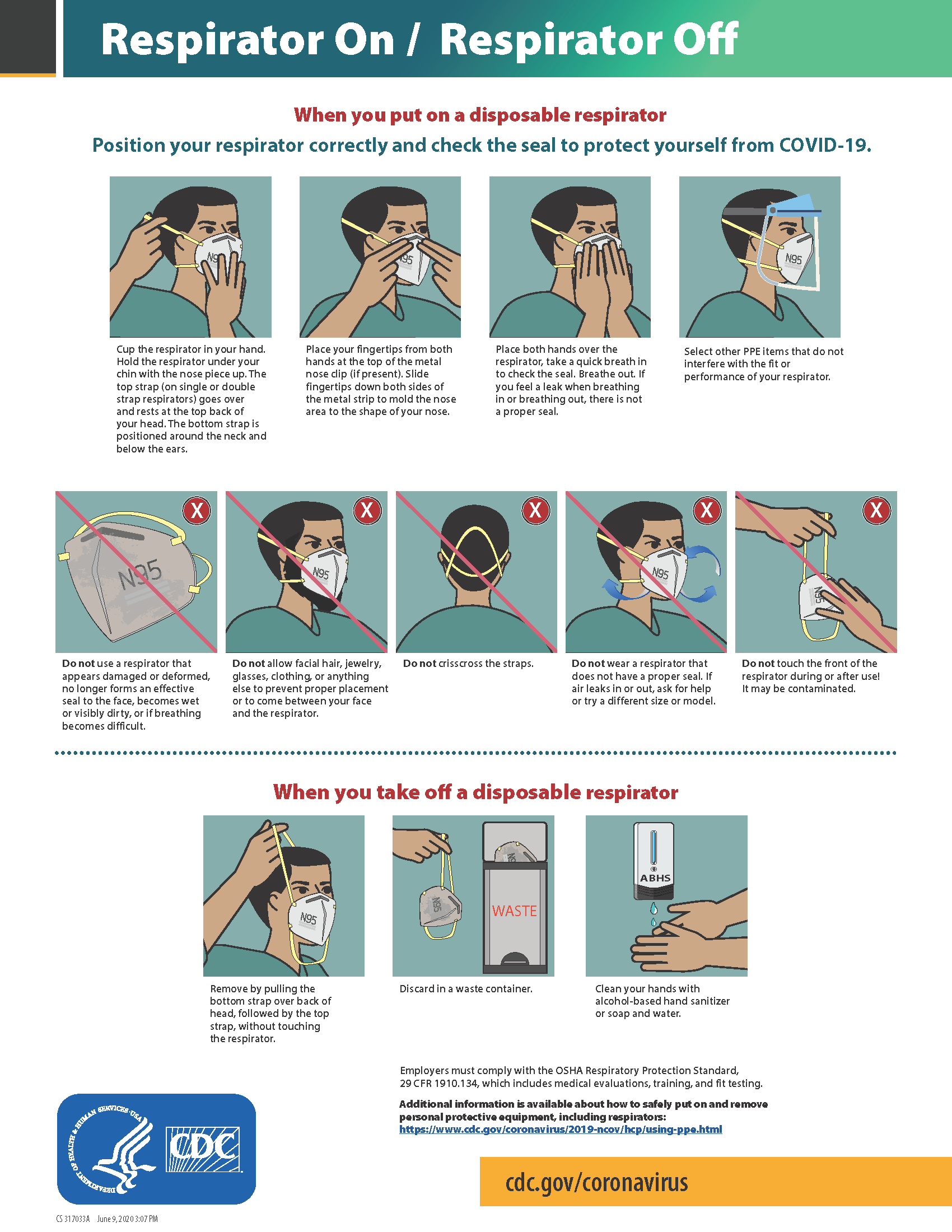
Respiratory protection used during airborne transmission precautions requires the use of special equipment. Traditionally, a fitted respirator mask with N95 or higher filtration has been worn by health care professionals to prevent inhalation of small airborne infectious particles. A user-seal check (formerly called a “fit check”) should be performed by the wearer of a respirator each time a respirator is donned to minimize air leakage around the facepiece.
A newer piece of equipment used for respiratory protection is the powered air-purifying respirator (PAPR). A PAPR is an air-purifying respirator that uses a blower to force air through filter cartridges or canisters into the breathing zone of the wearer. This process creates an air flow inside either a tight-fitting facepiece or loose-fitting hood or helmet, providing a higher level of protection against aerosolized pathogens, such as COVID-19, than a N95 respirator. See Figure 4.11[28] for an example of PAPR in use.

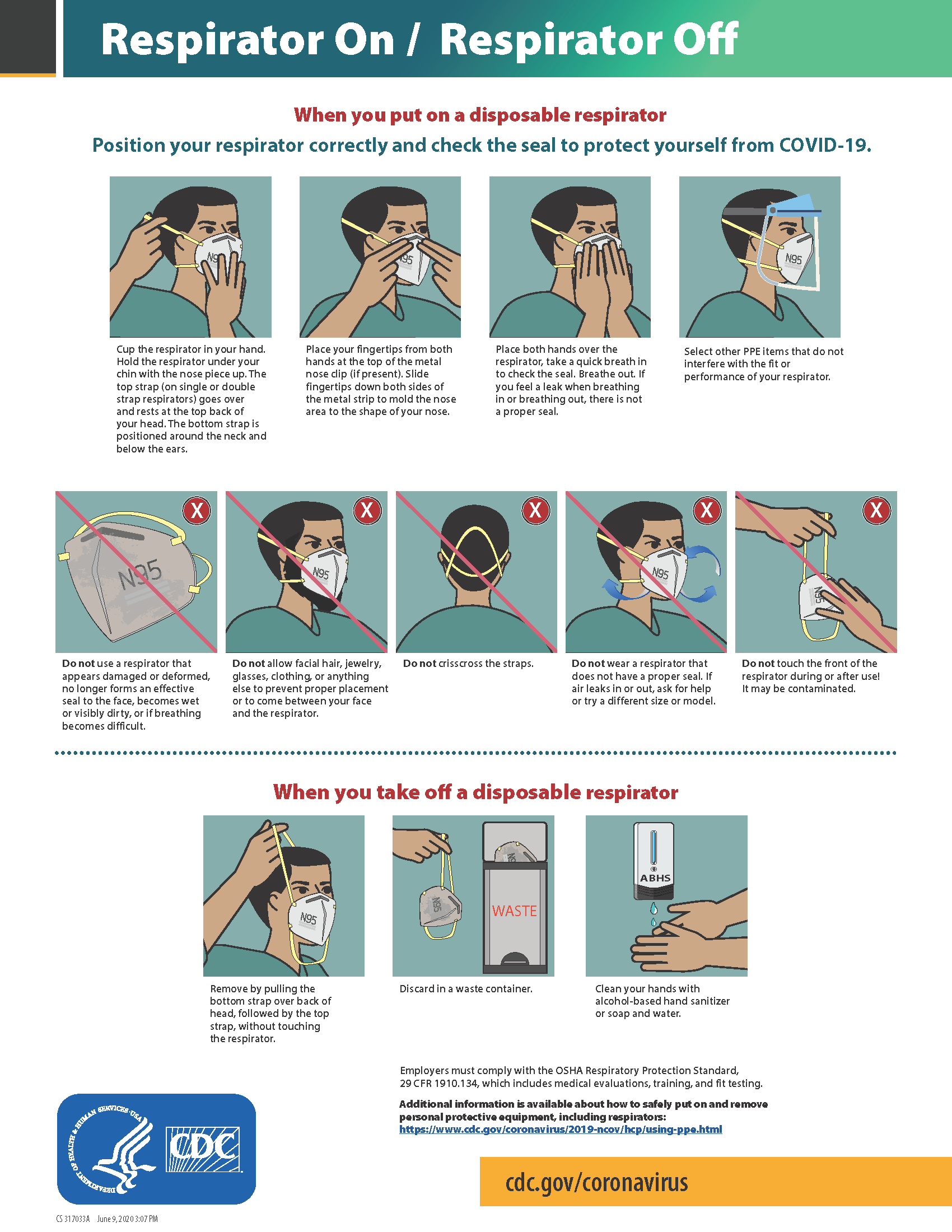
The CDC currently recommends N95 or higher level respirators for personnel exposed to patients with suspected or confirmed tuberculosis and other airborne diseases, especially during aerosol-generating procedures such as respiratory-tract suctioning.[29] It is important to apply, wear, and remove respirators appropriately to avoid contamination. See Figure 4.12[30] for CDC recommendations when wearing disposable respirators.
How to Put On (Don) PPE Gear
Follow agency policy for donning PPE according to transmission-based precautions. More than one donning method for putting on PPE may be acceptable. The CDC recommends the following steps for donning PPE[31]:
- Identify and gather the proper PPE to don. Ensure the gown size is correct.
- Perform hand hygiene using hand sanitizer or wash hands with soap and water.
- Put on the isolation gown. Tie all of the ties on the gown. Assistance may be needed by other health care personnel to tie back ties.
- Based on specific transmission-based precautions and agency policy, put on a mask or N95 respirator. The top strap should be placed on the crown (top) of the head, and the bottom strap should be at the base of the neck. If the mask has loops, hook them appropriately around your ears. Masks and respirators should extend under the chin, and both your mouth and nose should be protected. Perform a user-seal check each time you put on a respirator. If the respirator has a nosepiece, it should be fitted to the nose with both hands, but it should not be bent or tented. Masks typically require the nosepiece to be pinched to fit around the nose, but do not pinch the nosepiece of a respirator with one hand. Do not wear a respirator or mask under your chin or store it in the pocket of your scrubs between patients.
- Put on a face shield or goggles when indicated. When wearing an N95 respirator with eye protection, select eye protection that does not affect the fit or seal of the respirator and one that does not affect the position of the respirator. Goggles provide excellent protection for the eyes, but fogging is common. Face shields provide full-face coverage.
- Put on gloves. Gloves should cover the cuff (wrist) of the gown.
- You may now enter the patient’s room.
How to Take Off (Doff) PPE Gear
More than one doffing method for removing PPE may be acceptable. Train using your agency’s procedure, and practice until you have successfully mastered the steps to avoid contamination of yourself and others. There are established cases of nurses dying from disease transmitted during incorrect removal of PPE. Below are sample steps of doffing established by the CDC[34]:
- Remove the gloves. Ensure glove removal does not cause additional contamination of the hands. Gloves can be removed using more than one technique (e.g., glove-in-glove or bird beak).
- Remove the gown. Untie all ties (or unsnap all buttons). Some gown ties can be broken rather than untied; do so in a gentle manner and avoid a forceful movement. Reach up to the front of your shoulders and carefully pull the gown down and away from your body. Rolling the gown down is also an acceptable approach. Dispose of the gown in a trash receptacle. If it is a washable gown, place it in the specified laundry bin for PPE in the room.
- Health care personnel may now exit the patient room.
- Perform hand hygiene.
- Remove the face shield or goggles. Carefully remove the face shield or goggles by grabbing the strap and pulling upwards and away from head. Do not touch the front of the face shield or goggles.
- Remove and discard the respirator or face mask. Do not touch the front of the respirator or face mask. Remove the bottom strap by touching only the strap and bringing it carefully over the head. Grasp the top strap and bring it carefully over the head, and then pull the respirator away from the face without touching the front of the respirator. For masks, carefully untie (or unhook ties from the ears) and pull the mask away from your face without touching the front.
- Perform hand hygiene after removing the respirator/mask. If your workplace is practicing reuse, perform hand hygiene before putting it on again.
View a YouTube Video from the CDC on Putting on PPE[35]
View a YouTube Video from the CDC on Removing PPE[36]
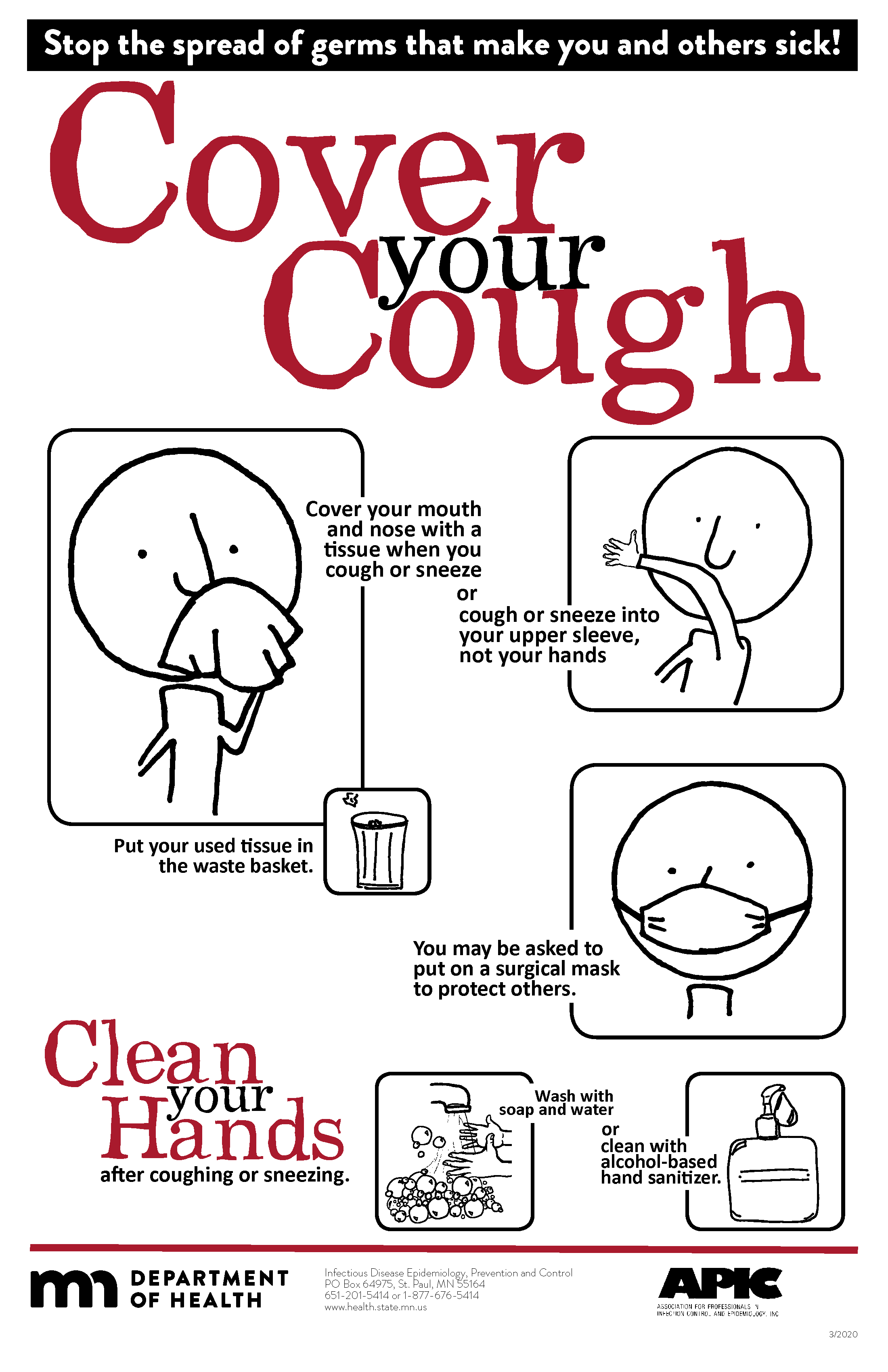
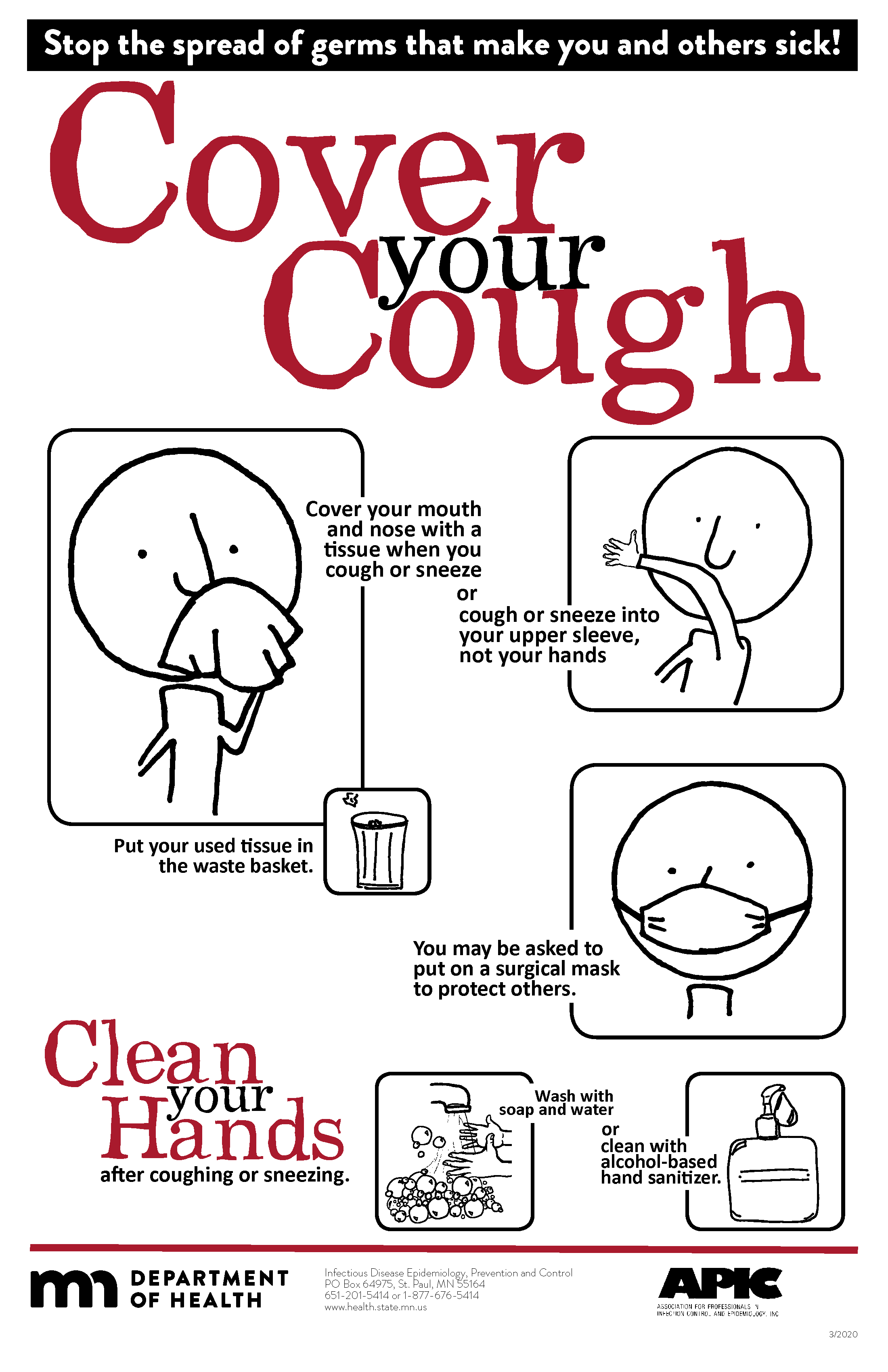
Respiratory Hygiene
Respiratory hygiene is targeted at patients, accompanying family members and friends, and health care workers with undiagnosed transmissible respiratory infections. It applies to any person with signs of illness, including cough, congestion, rhinorrhea, or increased production of respiratory secretions when entering a health care facility. See Figure 4.13[37] for an example of a “Cover Your Cough” poster used in public areas to promote respiratory hygiene. The elements of respiratory hygiene include the following:
- Education of health care facility staff, patients, and visitors
- Posted signs, in language(s) appropriate to the population served, with instructions to patients and accompanying family members or friends
- Source control measures for a coughing person (e.g., covering the mouth/nose with a tissue when coughing and prompt disposal of used tissues, or applying surgical masks on the coughing person to contain secretions)
- Hand hygiene after contact with one’s respiratory secretions
- Spatial separation, ideally greater than 3 feet, of persons with respiratory infections in common waiting areas when possible.[38]
Health care personnel are advised to wear a mask and use frequent hand hygiene when examining and caring for patients with signs and symptoms of a respiratory infection. Health care personnel who have a respiratory infection are advised to avoid direct patient contact, especially with high-risk patients. If this is not possible, then a mask should be worn while providing patient care.[39]
Environmental Measures
Routine cleaning and disinfecting surfaces in patient-care areas are part of standard precautions. The cleaning and disinfecting of all patient-care areas are important for frequently touched surfaces, especially those closest to the patient that are most likely to be contaminated (e.g., bedrails, bedside tables, commodes, doorknobs, sinks, surfaces, and equipment in close proximity to the patient).
Medical equipment and instruments/devices must also be cleaned to prevent patient-to-patient transmission of infectious agents. For example, stethoscopes should be cleaned before and after use for all patients. Patients who have transmission-based precautions should have dedicated medical equipment that remains in their room (e.g., stethoscope, blood pressure cuff, thermometer). When dedicated equipment is not possible, such as a unit-wide bedside blood glucose monitor, disinfection after each patient’s use should be performed according to agency policy.[40]
Disposal of Contaminated Waste
Medical waste requires careful disposal according to agency policy. The Occupational Safety and Health Administration (OSHA) has established measures for discarding regulated medical waste items to protect the workers who generate medical waste, as well as those who manage the waste from point of generation to disposal. Contaminated waste is placed in a leak-resistant biohazard bag, securely closed, and placed in a labeled, leakproof, puncture-resistant container in a storage area. Sharps containers are used to dispose of sharp items such as discarded tubes with small amounts of blood, scalpel blades, needles, and syringes.[41]
Sharps Safety
Injuries due to needles and other sharps have been associated with transmission of blood-borne pathogens (BBP), including hepatitis B, hepatitis C, and HIV to health care personnel. The prevention of sharps injuries is an essential element of standard precautions and includes measures to handle needles and other sharp devices in a manner that will prevent injury to the user and to others who may encounter the device during or after a procedure. The Bloodborne Pathogens Standard is a regulation that prescribes safeguards to protect workers against health hazards related to blood-borne pathogens. It includes work practice controls, hepatitis B vaccinations, hazard communication and training, plans for when an employee is exposed to a BBP, and recordkeeping.
When performing procedures that include needles or other sharps, dispose of these items immediately in FDA-cleared sharps disposal containers. Additionally, to prevent needlestick injuries, needles and other contaminated sharps should not be recapped. See Figure 4.14[42] for an image of a sharps disposal container. FDA-cleared sharps disposal containers are made from rigid plastic and come marked with a line that indicates when the container should be considered full, which means it’s time to dispose of the container. When a sharps disposal container is about three-quarters full, follow agency policy for proper disposal of the container.
If you are stuck by a needle or other sharps or are exposed to blood or other potentially infectious materials in your eyes, nose, mouth, or on broken skin, immediately flood the exposed area with water and clean any wound with soap and water. Report the incident immediately to your instructor or employer and seek immediate medical attention according to agency and school policy.

Textiles and Laundry
Soiled textiles, including bedding, towels, and patient or resident clothing may be contaminated with pathogenic microorganisms. However, the risk of disease transmission is negligible if they are handled, transported, and laundered in a safe manner. Follow agency policy for handling soiled laundry using standard precautions. Key principles for handling soiled laundry are as follows:
- Do not shake items or handle them in any way that may aerosolize infectious agents.
- Avoid contact of one’s body and personal clothing with the soiled items being handled.
- Place soiled items in a laundry bag or designated bin in the patient’s room before transporting to a laundry area. When laundry chutes are used, they must be maintained to minimize dispersion of aerosols from contaminated items.[43]
Standard Versus Transmission-Based Precautions
Standard Precautions
Standard precautions are used when caring for all patients to prevent health care associated infections. According to the Centers for Disease Control and Prevention (CDC), standard precautions are “the minimum infection prevention practices that apply to all patient care, regardless of suspected or confirmed infection status of the patient, in any setting where health care is delivered.”[44] They are based on the principle that all blood, body fluids (except sweat), nonintact skin, and mucous membranes may contain transmissible infectious agents. These standards reduce the risk of exposure for the health care worker and protect the patient from potential transmission of infectious organisms.
Current standard precautions according to the CDC (2019) include the following:
- Appropriate hand hygiene
- Use of personal protective equipment (e.g., gloves, gowns, masks, eyewear) whenever infectious material exposure may occur
- Appropriate patient placement and care using transmission-based precautions when indicated
- Respiratory hygiene/cough etiquette
- Proper handling and cleaning of environment, equipment, and devices
- Safe handling of laundry
- Sharps safety (i.e., engineering and work practice controls)
- Aseptic technique for invasive nursing procedures such as parenteral medication administration[45]
Each of these standard precautions is described in more detail in the following subsections.
Transmission-Based Precautions
In addition to standard precautions, transmission-based precautions are used for patients with documented or suspected infection, or colonization, of highly transmissible or epidemiologically important pathogens. Epidemiologically important pathogens include, but are not limited to, Coronavirus disease (COVID-19), Clostridium difficile (C-diff), Methicillin-resistant staphylococcus aureus (MRSA), Vancomycin-resistant enterococci (VRE), Respiratory syncytial sirus (RSV), measles, and tuberculosis (TB). For patients with these types of pathogens, standard precautions are used along with specific transmission-based precautions.
There are four categories of transmission-based precautions: contact precautions, enhanced barrier precautions, droplet precautions, and airborne precautions. Transmission-based precautions are used when the route(s) of transmission is (are) not completely interrupted using standard precautions alone. Some diseases, such as tuberculosis, have multiple routes of transmission so more than one transmission-based precautions category must be implemented. See Table 4.2 outlining the categories of transmission precautions with associated PPE and other precautions. When possible, patients with transmission-based precautions should be placed in a single occupancy room with dedicated patient care equipment (e.g., blood pressure cuffs, stethoscope, thermometer). Transport of the patient and unnecessary movement outside the patient room should be limited. However, when transmission-based precautions are implemented, it is also important for the nurse to make efforts to counteract possible adverse effects of these precautions on patients, such as anxiety, depression, perceptions of stigma, and reduced contact with clinical staff.
Table 4.2 Transmission-Based Precautions[46]
| Precaution | Implementation | PPE and Other Precautions |
|---|---|---|
| Contact | Known or suspected infections with increased risk for contact transmission (e.g., draining wounds, fecal incontinence) or with epidemiologically important organisms, such as C-diff, MRSA, VRE, or RSV |
Note: Use only soap and water for hand hygiene in patients with C. difficile infection. |
| Enhanced barrier | Used during high-contact resident care activities for individuals colonized or infected with a multidrug-resistant organism (MDRO), as well as those at increased risk of MDRO acquisition |
|
| Droplet | Known or suspected infection with pathogens transmitted by large respiratory droplets generated by coughing, sneezing, or talking, such as influenza, coronavirus, or pertussis |
|
| Airborne | Known or suspected infection with pathogens transmitted by small respiratory droplets, such as measles, tuberculosis, and disseminated herpes zoster | Fit-tested N-95 respirator or PAPR
|
View a list of transmission-based precautions used for specific medical conditions at the CDC Guideline for Isolation Precautions.
Patient Transport
Several principles are used to guide transport of patients requiring transmission-based precautions. In the inpatient and residential settings, these principles include the following:
- Limiting transport for essential purposes only, such as diagnostic and therapeutic procedures that cannot be performed in the patient’s room
- Using appropriate barriers on the patient consistent with the route and risk of transmission (e.g., mask, gown, covering the affected areas when infectious skin lesions or drainage is present)
- Notify other health care personnel involved in the care of the patient of the transmission-based precautions. For example, when transporting the patient to radiology, inform the radiology technician of the precautions.[47]
Appropriate Hand Hygiene
Hand hygiene is the single most important practice to reduce the transmission of infectious agents in health care settings and is an essential element of standard precautions.[48] Routine handwashing during appropriate moments is a simple and effective way to prevent infection. However, it is estimated that health care professionals, on average, properly clean their hands less than 50% of the time it is indicated.[49] The Joint Commission, the organization that sets evidence-based standards of care for hospitals, recently updated its hand hygiene standards in 2018 to promote enforcement. If a Joint Commission surveyor witnesses an individual failing to properly clean their hands when it is indicated, a deficiency will be cited requiring improvement by the agency. This deficiency could potentially jeopardize a hospital’s accreditation status and their ability to receive payment for patient services. Therefore, it is essential for all health care workers to ensure they are using proper hand hygiene at the appropriate times.[50]
There are several evidence-based guidelines for performing appropriate hand hygiene. These guidelines include frequency of performing hand hygiene according to the care circumstances, solutions used, and technique performed. The Healthcare Infection Control Practices Advisory Committee (HICPAC) recommends health care personnel perform hand hygiene at specific times when providing care to patients. These moments are often referred to as the “Moments for Hand Hygiene.”[51] See Figures 4.1[52] and 4.2[53] for an illustration and application of the five moments of hand hygiene. The five moments of hand hygiene are as follows:
- Immediately before touching a patient
- Before performing an aseptic task or handling invasive devices
- Before moving from a soiled body site to a clean body site on a patient
- After touching a patient or their immediate environment
- After contact with blood, body fluids, or contaminated surfaces (with or without glove use)
When performing hand hygiene, washing with soap and water, or an approved alcohol-based hand rub solution that contains at least 60% alcohol, may be used. Unless hands are visibly soiled, an alcohol-based hand rub is preferred over soap and water in most clinical situations due to evidence of improved compliance. Handrubs are also preferred because they are generally less irritating to health care worker’s hands. However, it is important to recognize that alcohol-based rubs do not eliminate some types of germs, such as Clostridium difficile (C-diff).
When using the alcohol-based handrub method, the CDC recommends the following steps. See Figure 4.3[54] for a handrub poster created by the World Health Organization.
- Apply product to the palm of one hand in an amount that will cover all surfaces.
- Rub hands together, covering all the surfaces of the hands, fingers, and wrists until the hands are dry. Surfaces include the palms and fingers, between the fingers, the backs of the hands and fingers, the fingertips, and the thumbs.
- The process should take about 20 seconds, and the solution should be dry.[55]
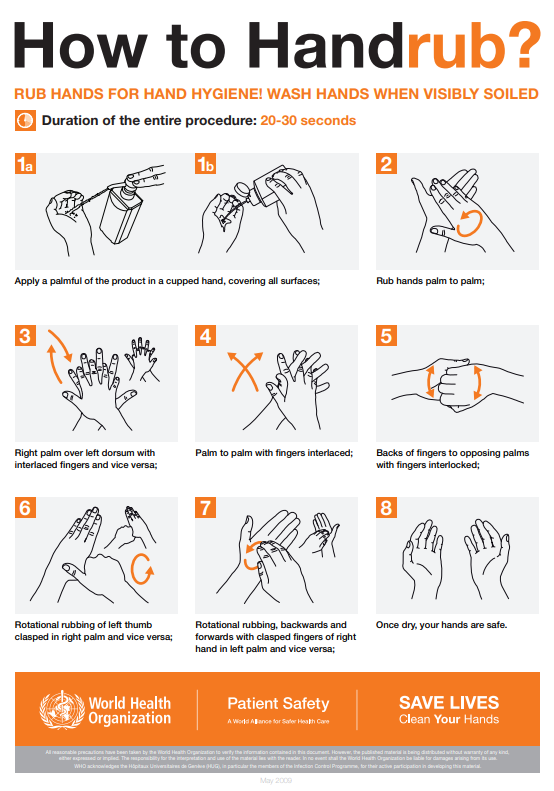
When washing with soap and water, the CDC recommends using the following steps. See Figure 4.4[56] for an image of a handwashing poster created by the World Health Organization.
- Wet hands with warm or cold running water and apply facility-approved soap.
- Lather hands by rubbing them together with the soap. Use the same technique as the handrub process to clean the palms and fingers, between the fingers, the backs of the hands and fingers, the fingertips, and the thumbs.
- Scrub thoroughly for at least 20 seconds.
- Rinse hands well under clean, running water.
- Dry the hands using a clean towel or disposable toweling.
- Use a clean paper towel to shut off the faucet.[57]
By performing hand hygiene at the proper moments and using appropriate techniques, you will ensure your hands are safe and you are not transmitting infectious organisms to yourself or others.
Hand Hygiene for Healthcare Workers on YouTube[58]
Personal Protective Equipment (PPE)
Personal protective equipment (PPE) includes gloves, gowns, face shields, goggles, and masks used to prevent the spread of infection to and from patients and health care providers. Depending on the anticipated exposure, PPE may include the use of gloves, a fluid-resistant gown, goggles or a face shield, and a mask or respirator. When used for a patient with transmission-based precautions, PPE supplies are typically stored in an isolation cart next to the patient’s room, and a card is posted on the door alerting staff and visitors to precautions needed before entering the room.
Gloves
Gloves protect both patients and health care personnel from exposure to infectious material that may be carried on the hands. Gloves are used to prevent contamination of health care personnel hands during activities such as the following:
- Anticipating direct contact with blood or body fluids, mucous membranes, nonintact skin, and other potentially infectious material
- Having direct contact with patients who are colonized or infected with pathogens transmitted by the contact route, such as Vancomycin-resistant enterococci (VRE), Methicillin-resistant staphylococcus aureus (MRSA), and Respiratory syncytial virus (RSV)
- Handling or touching visibly or potentially contaminated patient care equipment and environmental surfaces[59]
Nonsterile disposable medical gloves for routine patient care are made of a variety of materials, such as latex, vinyl, and nitrile. Many people are allergic to latex, so be sure to check for latex allergies for the patient and other health care professionals. See Figure 4.5[60] for an image of nonsterile medical gloves in various sizes in a health care setting. At times, gloves may need to be changed when providing care to a single patient to prevent cross-contamination of body sites. It is also necessary to change gloves if the patient interaction requires touching portable computer keyboards or other mobile equipment that is transported from room to room. Discarding gloves between patients is necessary to prevent transmission of infectious material. Gloves must not be washed for subsequent reuse because microorganisms cannot be reliably removed from glove surfaces, and continued glove integrity cannot be ensured.[61]

When gloves are worn in combination with other PPE, they are put on last. Gloves that fit snugly around the wrist should be used in combination with isolation gowns because they will cover the gown cuff and provide a more reliable continuous barrier for the arms, wrists, and hands.
Gloves should be removed properly to prevent contamination. See Figure 4.6[62] for an illustration of properly removing gloves. Hand hygiene should be performed following glove removal to ensure the hands will not carry potentially infectious material that might have penetrated through unrecognized tears or contaminated the hands during glove removal. One method for properly removing gloves includes the following steps:
- Grasp the outside of one glove near the wrist. Do not touch your skin.
- Peel the glove away from your body, pulling it inside out.
- Hold the removed glove in your gloved hand.
- Put your fingers inside the glove at the top of your wrist and peel off the second glove.
- Turn the second glove inside out while pulling it away from your body, leaving the first glove inside the second.
- Dispose of the gloves safely. Do not reuse.
- Perform hand hygiene immediately after removing the gloves.[63]
Gowns
Isolation gowns are used to protect the health care worker’s arms and exposed body areas and to prevent contamination of their clothing with blood, body fluids, and other potentially infectious material. Isolation gowns may be disposable or washable/reusable. See Figure 4.7[64] for an image of a nurse wearing an isolation gown along with goggles and a respirator. When using standard precautions, an isolation gown is worn only if contact with blood or body fluid is anticipated. However, when contact transmission-based precautions are in place, donning of both gown and gloves upon room entry is indicated to prevent unintentional contact of clothing with contaminated environmental surfaces.
Gowns are usually the first piece of PPE to be donned. Isolation gowns should be removed before leaving the patient room to prevent possible contamination of the environment outside the patient’s room. Isolation gowns should be removed in a manner that prevents contamination of clothing or skin. The outer, “contaminated,” side of the gown is turned inward and rolled into a bundle, and then it is discarded into a designated container to contain contamination. See more information about putting on and removing PPE in the subsection below.[65]

Masks
The mucous membranes of the mouth, nose, and eyes are susceptible portals of entry for infectious agents. Masks are used to protect these sites from entry of large infectious droplets. See Figure 4.8[66] for an image of nurse wearing a surgical mask. Masks have three primary purposes in health care settings:
- Used by health care personnel to protect them from contact with infectious material from patients (e.g., respiratory secretions and sprays of blood or body fluids), consistent with standard precautions and droplet transmission precautions
- Used by health care personnel when engaged in procedures requiring sterile technique to protect patients from exposure to infectious agents potentially carried in a health care worker’s mouth or nose
- Placed on coughing patients to limit potential dissemination of infectious respiratory secretions from the patient to others in public areas (i.e., respiratory hygiene)[67]
Masks may be used in combination with goggles or a face shield to provide more complete protection for the face. Masks should not be confused with respirators used during airborne transmission-based precautions to prevent inhalation of small, aerosolized infectious droplets.[68]

It is important to properly wear and remove masks to avoid contamination. See Figure 4.9[69] for CDC face mask recommendations for health care personnel.
Goggles/Face Shields
Eye protection chosen for specific work situations (e.g., goggles or face shields) depends upon the circumstances of exposure, other PPE used, and personal vision needs. Personal eyeglasses are not considered adequate eye protection. See Figure 4.10[70] for an image of a health care professional wearing a face shield along with a N95 respirator.

Respirators and PAPRs
Respiratory protection used during airborne transmission precautions requires the use of special equipment. Traditionally, a fitted respirator mask with N95 or higher filtration has been worn by health care professionals to prevent inhalation of small airborne infectious particles. A user-seal check (formerly called a “fit check”) should be performed by the wearer of a respirator each time a respirator is donned to minimize air leakage around the facepiece.
A newer piece of equipment used for respiratory protection is the powered air-purifying respirator (PAPR). A PAPR is an air-purifying respirator that uses a blower to force air through filter cartridges or canisters into the breathing zone of the wearer. This process creates an air flow inside either a tight-fitting facepiece or loose-fitting hood or helmet, providing a higher level of protection against aerosolized pathogens, such as COVID-19, than a N95 respirator. See Figure 4.11[71] for an example of PAPR in use.

The CDC currently recommends N95 or higher level respirators for personnel exposed to patients with suspected or confirmed tuberculosis and other airborne diseases, especially during aerosol-generating procedures such as respiratory-tract suctioning.[72] It is important to apply, wear, and remove respirators appropriately to avoid contamination. See Figure 4.12[73] for CDC recommendations when wearing disposable respirators.
How to Put On (Don) PPE Gear
Follow agency policy for donning PPE according to transmission-based precautions. More than one donning method for putting on PPE may be acceptable. The CDC recommends the following steps for donning PPE[74]:
- Identify and gather the proper PPE to don. Ensure the gown size is correct.
- Perform hand hygiene using hand sanitizer or wash hands with soap and water.
- Put on the isolation gown. Tie all of the ties on the gown. Assistance may be needed by other health care personnel to tie back ties.
- Based on specific transmission-based precautions and agency policy, put on a mask or N95 respirator. The top strap should be placed on the crown (top) of the head, and the bottom strap should be at the base of the neck. If the mask has loops, hook them appropriately around your ears. Masks and respirators should extend under the chin, and both your mouth and nose should be protected. Perform a user-seal check each time you put on a respirator. If the respirator has a nosepiece, it should be fitted to the nose with both hands, but it should not be bent or tented. Masks typically require the nosepiece to be pinched to fit around the nose, but do not pinch the nosepiece of a respirator with one hand. Do not wear a respirator or mask under your chin or store it in the pocket of your scrubs between patients.
- Put on a face shield or goggles when indicated. When wearing an N95 respirator with eye protection, select eye protection that does not affect the fit or seal of the respirator and one that does not affect the position of the respirator. Goggles provide excellent protection for the eyes, but fogging is common. Face shields provide full-face coverage.
- Put on gloves. Gloves should cover the cuff (wrist) of the gown.
- You may now enter the patient’s room.
How to Take Off (Doff) PPE Gear
More than one doffing method for removing PPE may be acceptable. Train using your agency’s procedure, and practice until you have successfully mastered the steps to avoid contamination of yourself and others. There are established cases of nurses dying from disease transmitted during incorrect removal of PPE. Below are sample steps of doffing established by the CDC[77]:
- Remove the gloves. Ensure glove removal does not cause additional contamination of the hands. Gloves can be removed using more than one technique (e.g., glove-in-glove or bird beak).
- Remove the gown. Untie all ties (or unsnap all buttons). Some gown ties can be broken rather than untied; do so in a gentle manner and avoid a forceful movement. Reach up to the front of your shoulders and carefully pull the gown down and away from your body. Rolling the gown down is also an acceptable approach. Dispose of the gown in a trash receptacle. If it is a washable gown, place it in the specified laundry bin for PPE in the room.
- Health care personnel may now exit the patient room.
- Perform hand hygiene.
- Remove the face shield or goggles. Carefully remove the face shield or goggles by grabbing the strap and pulling upwards and away from head. Do not touch the front of the face shield or goggles.
- Remove and discard the respirator or face mask. Do not touch the front of the respirator or face mask. Remove the bottom strap by touching only the strap and bringing it carefully over the head. Grasp the top strap and bring it carefully over the head, and then pull the respirator away from the face without touching the front of the respirator. For masks, carefully untie (or unhook ties from the ears) and pull the mask away from your face without touching the front.
- Perform hand hygiene after removing the respirator/mask. If your workplace is practicing reuse, perform hand hygiene before putting it on again.
View a YouTube Video from the CDC on Putting on PPE[78]
View a YouTube Video from the CDC on Removing PPE[79]
Respiratory Hygiene
Respiratory hygiene is targeted at patients, accompanying family members and friends, and health care workers with undiagnosed transmissible respiratory infections. It applies to any person with signs of illness, including cough, congestion, rhinorrhea, or increased production of respiratory secretions when entering a health care facility. See Figure 4.13[80] for an example of a “Cover Your Cough” poster used in public areas to promote respiratory hygiene. The elements of respiratory hygiene include the following:
- Education of health care facility staff, patients, and visitors
- Posted signs, in language(s) appropriate to the population served, with instructions to patients and accompanying family members or friends
- Source control measures for a coughing person (e.g., covering the mouth/nose with a tissue when coughing and prompt disposal of used tissues, or applying surgical masks on the coughing person to contain secretions)
- Hand hygiene after contact with one’s respiratory secretions
- Spatial separation, ideally greater than 3 feet, of persons with respiratory infections in common waiting areas when possible.[81]
Health care personnel are advised to wear a mask and use frequent hand hygiene when examining and caring for patients with signs and symptoms of a respiratory infection. Health care personnel who have a respiratory infection are advised to avoid direct patient contact, especially with high-risk patients. If this is not possible, then a mask should be worn while providing patient care.[82]
Environmental Measures
Routine cleaning and disinfecting surfaces in patient-care areas are part of standard precautions. The cleaning and disinfecting of all patient-care areas are important for frequently touched surfaces, especially those closest to the patient that are most likely to be contaminated (e.g., bedrails, bedside tables, commodes, doorknobs, sinks, surfaces, and equipment in close proximity to the patient).
Medical equipment and instruments/devices must also be cleaned to prevent patient-to-patient transmission of infectious agents. For example, stethoscopes should be cleaned before and after use for all patients. Patients who have transmission-based precautions should have dedicated medical equipment that remains in their room (e.g., stethoscope, blood pressure cuff, thermometer). When dedicated equipment is not possible, such as a unit-wide bedside blood glucose monitor, disinfection after each patient’s use should be performed according to agency policy.[83]
Disposal of Contaminated Waste
Medical waste requires careful disposal according to agency policy. The Occupational Safety and Health Administration (OSHA) has established measures for discarding regulated medical waste items to protect the workers who generate medical waste, as well as those who manage the waste from point of generation to disposal. Contaminated waste is placed in a leak-resistant biohazard bag, securely closed, and placed in a labeled, leakproof, puncture-resistant container in a storage area. Sharps containers are used to dispose of sharp items such as discarded tubes with small amounts of blood, scalpel blades, needles, and syringes.[84]
Sharps Safety
Injuries due to needles and other sharps have been associated with transmission of blood-borne pathogens (BBP), including hepatitis B, hepatitis C, and HIV to health care personnel. The prevention of sharps injuries is an essential element of standard precautions and includes measures to handle needles and other sharp devices in a manner that will prevent injury to the user and to others who may encounter the device during or after a procedure. The Bloodborne Pathogens Standard is a regulation that prescribes safeguards to protect workers against health hazards related to blood-borne pathogens. It includes work practice controls, hepatitis B vaccinations, hazard communication and training, plans for when an employee is exposed to a BBP, and recordkeeping.
When performing procedures that include needles or other sharps, dispose of these items immediately in FDA-cleared sharps disposal containers. Additionally, to prevent needlestick injuries, needles and other contaminated sharps should not be recapped. See Figure 4.14[85] for an image of a sharps disposal container. FDA-cleared sharps disposal containers are made from rigid plastic and come marked with a line that indicates when the container should be considered full, which means it’s time to dispose of the container. When a sharps disposal container is about three-quarters full, follow agency policy for proper disposal of the container.
If you are stuck by a needle or other sharps or are exposed to blood or other potentially infectious materials in your eyes, nose, mouth, or on broken skin, immediately flood the exposed area with water and clean any wound with soap and water. Report the incident immediately to your instructor or employer and seek immediate medical attention according to agency and school policy.

Textiles and Laundry
Soiled textiles, including bedding, towels, and patient or resident clothing may be contaminated with pathogenic microorganisms. However, the risk of disease transmission is negligible if they are handled, transported, and laundered in a safe manner. Follow agency policy for handling soiled laundry using standard precautions. Key principles for handling soiled laundry are as follows:
- Do not shake items or handle them in any way that may aerosolize infectious agents.
- Avoid contact of one’s body and personal clothing with the soiled items being handled.
- Place soiled items in a laundry bag or designated bin in the patient’s room before transporting to a laundry area. When laundry chutes are used, they must be maintained to minimize dispersion of aerosols from contaminated items.[86]
In addition to using standard precautions and transmission-based precautions, aseptic technique (also called medical asepsis) is the purposeful reduction of pathogens to prevent the transfer of microorganisms from one person or object to another during a medical procedure. For example, a nurse administering parenteral medication or performing urinary catheterization uses aseptic technique. When performed properly, aseptic technique prevents contamination and transfer of pathogens to the patient from caregiver hands, surfaces, and equipment during routine care or procedures. The word “aseptic” literally means an absence of disease-causing microbes and pathogens. In the clinical setting, aseptic technique refers to the purposeful prevention of microbe contamination from one person or object to another. These potentially infectious, microscopic organisms can be present in the environment, on an instrument, in liquids, on skin surfaces, or within a wound.
There is often misunderstanding between the terms aseptic technique and sterile technique in the health care setting. Both asepsis and sterility are closely related, and the shared concept between the two terms is removal of harmful microorganisms that can cause infection. In the most simplistic terms, asepsis is creating a protective barrier from pathogens, whereas sterile technique is a purposeful attack on microorganisms. Sterile technique (also called surgical asepsis) seeks to eliminate every potential microorganism in and around a sterile field while also maintaining objects as free from microorganisms as possible. It is the standard of care for surgical procedures, invasive wound management, and central line care. Sterile technique requires a combination of meticulous hand washing, creation of a sterile field, using long-lasting antimicrobial cleansing agents such as betadine, donning sterile gloves, and using sterile devices and instruments.
Principles of Aseptic Non-Touch Technique
Aseptic non-touch technique (ANTT) is the most commonly used aseptic technique framework in the health care setting and is considered a global standard. There are two types of ANTT: surgical-ANTT (sterile technique) and standard-ANTT.
Aseptic non-touch technique starts with a few concepts that must be understood before it can be applied. For all invasive procedures, the “ANTT-approach” identifies key parts and key sites throughout the preparation and implementation of the procedure. A key part is any sterile part of equipment used during an aseptic procedure, such as needle hubs, syringe tips, needles, and dressings. A key site is any nonintact skin, potential insertion site, or access site used for medical devices connected to the patients. Examples of key sites include open wounds and insertion sites for intravenous (IV) devices and urinary catheters.
ANTT includes four underlying principles to keep in mind while performing invasive procedures:
- Always wash hands effectively.
- Never contaminate key parts.
- Touch non-key parts with confidence.
- Take appropriate infective precautions.
Preparing and Preventing Infections Using Aseptic Technique
When planning for any procedure, careful thought and preparation of many infection control factors must be considered beforehand. While keeping standard precautions in mind, identify anticipated key sites and key parts to the procedure. Consider the degree to which the environment must be managed to reduce the risk of infection, including the expected degree of contamination and hazardous exposure to the clinician. Finally, review the expected equipment needed to perform the procedure and the level of key part or key site handling. See Table 4.3 for an outline of infection control measures when performing a procedure.
Table 4.3 Infection Control Measures When Performing Procedures
| Infection Control Measure | Key Considerations | Examples |
|---|---|---|
| Environmental control |
|
|
| Hand hygiene |
|
|
| Personal protective equipment (PPE) |
|
|
| Aseptic field management | Determine level of aseptic field needed and how it will be managed before the procedure begins:
|
General aseptic field:
IV irrigation Dry dressing changes Critical aseptic field: Urinary catheter placement Central line dressing change Sterile dressing change |
| Non-touch technique |
|
|
| Sequencing |
|
|
Use of Gloves and Sterile Gloves
There are two different levels of medical-grade gloves available to health care providers: clean (exam) gloves and sterile (surgical) gloves. Generally speaking, clean gloves are used whenever there is a risk of contact with body fluids or contaminated surfaces or objects. Examples include starting an intravenous access device or emptying a urinary catheter collection bag. Alternatively, sterile gloves meet FDA requirements for sterilization and are used for invasive procedures or when contact with a sterile site, tissue, or body cavity is anticipated. Sterile gloves are used in these instances to prevent transient flora and reduce resident flora contamination during a procedure, thus preventing the introduction of pathogens. For example, sterile gloves are required when performing central line dressing changes, insertion of urinary catheters, and during invasive surgical procedures. See Figure 4.15[87] for images of a nurse opening and removing sterile gloves from packaging.
See the “Checklist for Applying and Removing Sterile Gloves” for details on how to apply sterile gloves.
Applying Sterile Gloves on YouTube[88]
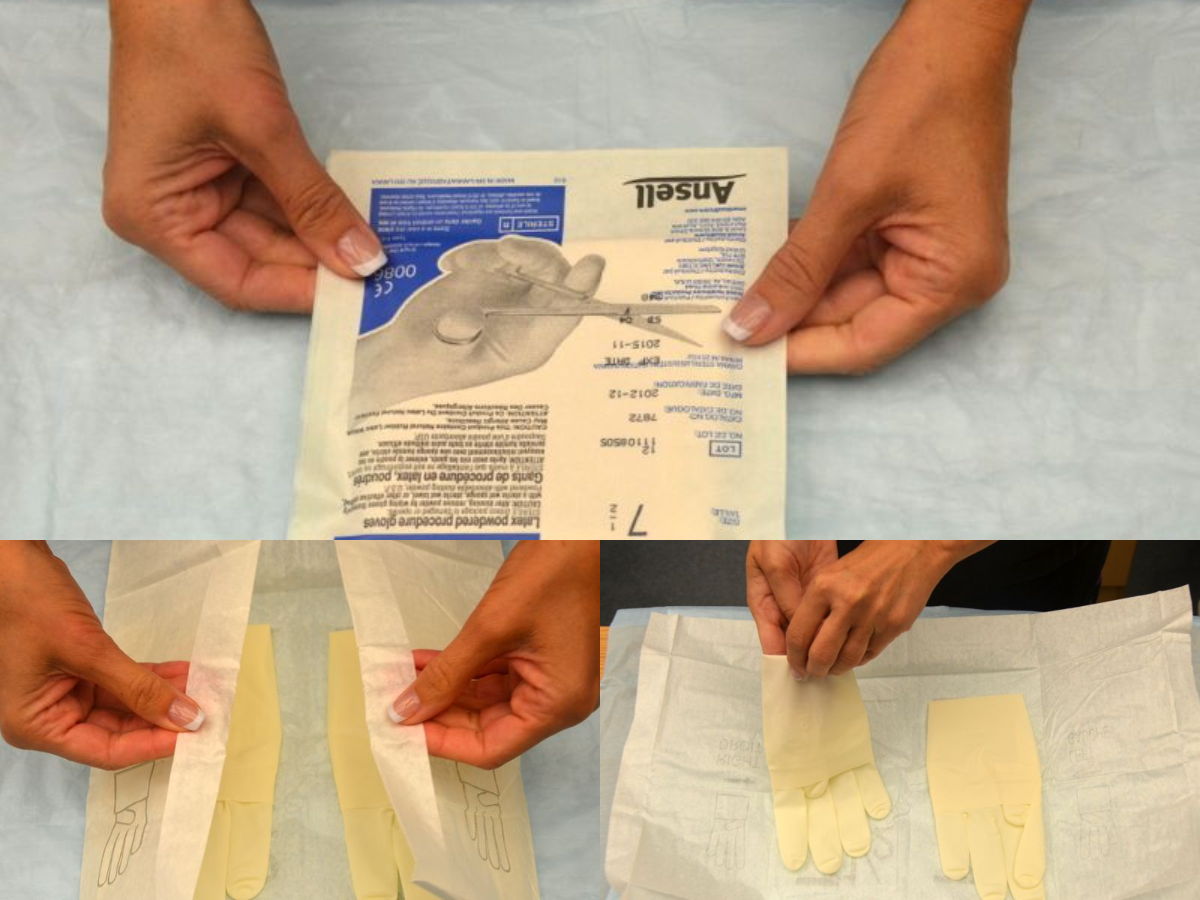
A sterile field is established whenever a patient’s skin is intentionally punctured or incised, during procedures involving entry into a body cavity, or when contact with nonintact skin is possible (e.g., surgery or trauma). Surgical asepsis requires adherence to strict principles and intentional actions to prevent contamination and to maintain the sterility of specific parts of a sterile field during invasive procedures. Creating and maintaining a sterile field is foundational to aseptic technique and encompasses practice standards that are performed immediately prior to and during a procedure to reduce the risk of infection, including the following:
- Handwashing
- Using sterile barriers, including drapes and appropriate personal protective equipment
- Preparing the patient using an approved antimicrobial product
- Maintaining a sterile field
- Using aseptically safe techniques
There are basic principles of asepsis that are critical to understand and follow when creating and maintaining a sterile field. The most basic principle is to allow only sterile supplies within the sterile field once it is established. This means that prior to using any supplies, exterior packaging must be checked for any signs of damage, such as previous exposure to moisture, holes, or tears. Packages should not be used if they are expired or if sterilization indicators are not the appropriate color. Sterile contents inside packages are dispensed onto the sterile field using the methods outlined below. See Figure 4.16[89] for an image of a nurse dispensing sterile supplies from packaging onto an established sterile field.
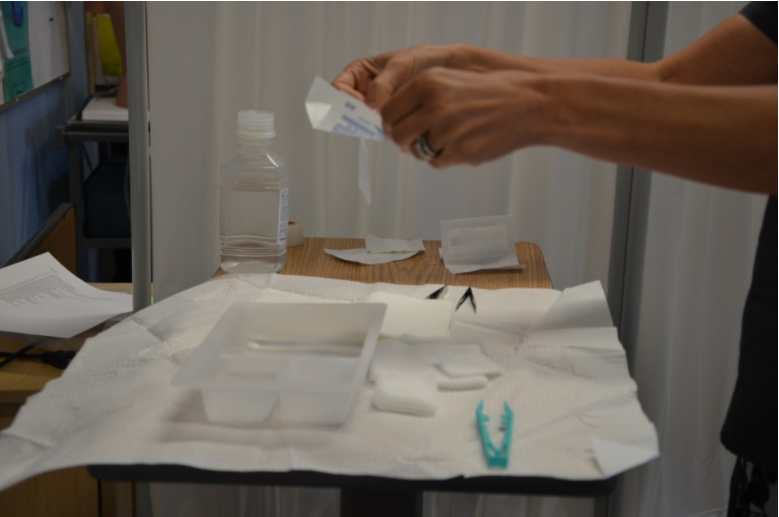
When establishing and maintaining a sterile field, there are other important principles to strictly follow:
- Disinfect any work surfaces and allow to them thoroughly dry before placing any sterile supplies on the surface.
- Be aware of areas of sterile fields that are considered contaminated:
- Any part of the field within 1 inch from the edge.
- Any part of the field that extends below the planar surface (i.e., a drape hanging down below the tray tabletop).
- Any part of the field below waist level or above shoulder level.
- Any supplies or field that you have not directly monitored (i.e., turned away from the sterile field or walked out of the room).
- Within 1 inch of any visible holes, tears, or moisture wicked from an unsterile area.
- When handling sterile kits and trays:
- Sterile kits and trays generally have an outer protective wrapper and four inner flaps that must be opened aseptically.
- Open sterile kits away from your body first, touching only the very edge of the opening flap.
- Using the same technique, open each of the side flaps one at a time using only one hand, being careful not to allow your body or arms to be directly above the opened drape. Take care not to allow already-opened corners to flip back into the sterile area again.
- Open the final flap toward you, being careful to not allow any part of your body to be directly over the field. See Figure 4.17[90] for images of opening the flaps of a sterile kit.
- If you must remove parts of the sterile kit (i.e., sterile gloves), reach into the sterile field with the elbow raised, using only the tips of the fingers before extracting. Pay close attention to where your body and clothing are in relationship to the sterile field to avoid inadvertent contamination.
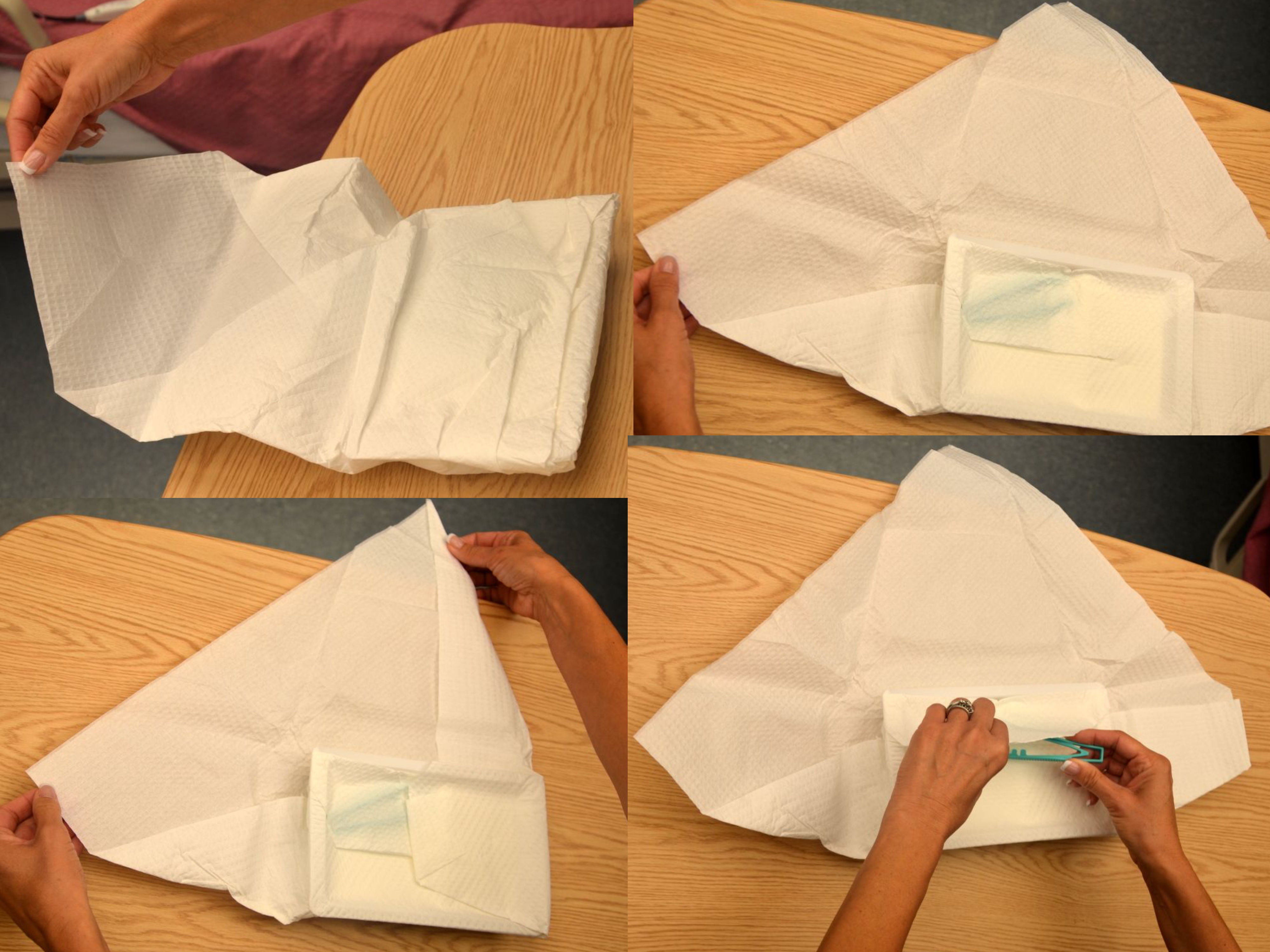
- When dispensing sterile supplies onto a sterile field:
- Before dispensing sterile supplies to a sterile field, do not allow sterile items to touch any part of the outer packaging once it is opened, including the former package seal.
- Heavy or irregular items should be opened and held, allowing a second person with sterile gloves to transfer them to the sterile field.
- Wrapped sterile items should be opened similarly to a sterile kit. Tuck each flap securely within your palm, and then open the flap away from your body first. Then open each side flap; secure the flap in the palm one at a time and open. Finally, open the flap (closest to you) toward you, while also protecting the other opened flaps from springing back onto the wrapped item.
- Peel pouches (i.e., gloves, gauze, syringes, etc.) can be opened by firmly grasping each side of the sealed edge with the thumb side of each hand parallel to the seal and pulling carefully apart.
- Drop items from six inches away from the sterile field.
- Sterile solutions should be poured into a sterile bowl or tray from the side of the sterile field and not directly over it. Use only sealed, sterile, unexpired solutions when pouring onto a sterile field. Solution should be held six inches away from the field as it is being poured. Avoid splashing solutions because this allows wicking and transfer of microbes. After pouring of solution stops, it should not be restarted because the edge is considered contaminated. See Figure 4.18[91] of an image of a nurse pouring sterile solution into a receptacle in a sterile field before the procedure begins.
- Don sterile gloves away from the sterile field to avoid contaminating the sterile field.

Use the checklist below to review the steps for completion of "Applying and Removing Personal Protective Equipment."[92]
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Check the provider's order for the type of precautions.
- Ensure that all supplies are available before check-off begins: isolation cart, gowns, gloves, mask, goggles/face shields, etc.
- Perform hand hygiene.
- Apply PPE in the correct order:
- 1st (GOWN): Gown should cover outer garments. Pull the sleeves down to the wrists, and tie at neck & waist.
- 2nd (MASK/RESPIRATOR): Apply surgical mask or N95 respirator if indicated by transmission-based precaution. Fit the mask around the nose and chin, securing bands around ears or tie straps at top of head and base of neck.
- 3rd (EYE PROTECTION): Apply goggles/face shield if indicated for patient condition or transmission-based precautions.
- 4th (CLEAN GLOVES): Pull on gloves to cover the wrist of the gown.
- Remove PPE in the correct order:
- 1st REMOVE GLOVES: REMEMBER: GLOVE TO GLOVE; SKIN TO SKIN. Do not touch contaminated gloves to your skin. Take off the contaminated glove with your gloved hand, wrapping the contaminated glove in the palm of your gloved hand. Take off the glove with your bare hand to the skin of your wrist, moving inside of the glove to remove the contaminated glove inside out over the other glove. Note: If the gown is tied in front, untie it prior to removing your glove.
- 2nd REMOVE GOWN: Untie all ties (or unsnap all buttons). Some gown ties can be broken rather than untied. Do so in a gentle manner, avoiding a forceful movement. Reach up to the shoulders and carefully pull the gown down and away from the body. Rolling the gown down is an acceptable approach. Dispose in trash receptacle.
- 3rd PERFORM HAND HYGIENE.
- 4th REMOVE FACE SHIELD or GOGGLES: Carefully remove face shield or goggles by grabbing the strap and pulling upwards and away from head. Do not touch the front of face shield or goggles.
- 5th REMOVE MASK or RESPIRATOR: Do not touch the front of the face shield or goggles.
- Respirator: Remove the bottom strap by touching only the strap and bringing it carefully over the head. Grasp the top strap and bring it carefully over the head, and then pull the respirator away from the face without touching the front of the respirator.
- Face mask: Carefully untie (or unhook from the ears) and pull it away from the face without touching the front.
- 6th PERFORM HAND HYGIENE after removing the mask.
A sterile field is established whenever a patient’s skin is intentionally punctured or incised, during procedures involving entry into a body cavity, or when contact with nonintact skin is possible (e.g., surgery or trauma). Surgical asepsis requires adherence to strict principles and intentional actions to prevent contamination and to maintain the sterility of specific parts of a sterile field during invasive procedures. Creating and maintaining a sterile field is foundational to aseptic technique and encompasses practice standards that are performed immediately prior to and during a procedure to reduce the risk of infection, including the following:
- Handwashing
- Using sterile barriers, including drapes and appropriate personal protective equipment
- Preparing the patient using an approved antimicrobial product
- Maintaining a sterile field
- Using aseptically safe techniques
There are basic principles of asepsis that are critical to understand and follow when creating and maintaining a sterile field. The most basic principle is to allow only sterile supplies within the sterile field once it is established. This means that prior to using any supplies, exterior packaging must be checked for any signs of damage, such as previous exposure to moisture, holes, or tears. Packages should not be used if they are expired or if sterilization indicators are not the appropriate color. Sterile contents inside packages are dispensed onto the sterile field using the methods outlined below. See Figure 4.16[93] for an image of a nurse dispensing sterile supplies from packaging onto an established sterile field.
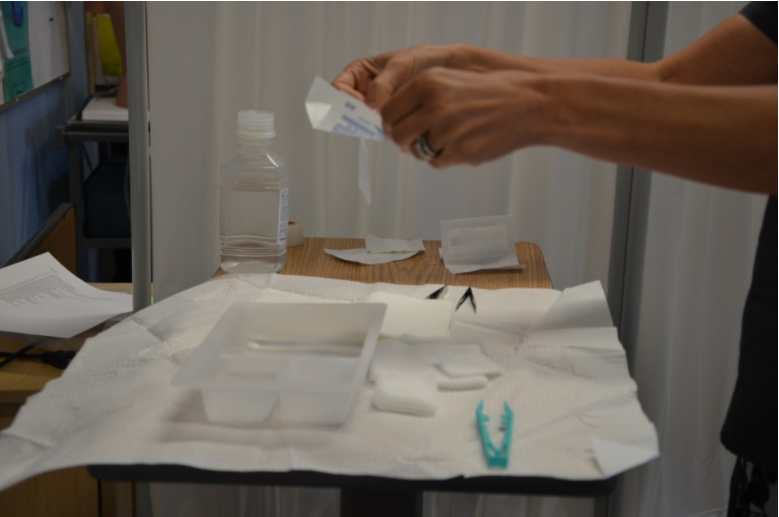
When establishing and maintaining a sterile field, there are other important principles to strictly follow:
- Disinfect any work surfaces and allow to them thoroughly dry before placing any sterile supplies on the surface.
- Be aware of areas of sterile fields that are considered contaminated:
- Any part of the field within 1 inch from the edge.
- Any part of the field that extends below the planar surface (i.e., a drape hanging down below the tray tabletop).
- Any part of the field below waist level or above shoulder level.
- Any supplies or field that you have not directly monitored (i.e., turned away from the sterile field or walked out of the room).
- Within 1 inch of any visible holes, tears, or moisture wicked from an unsterile area.
- When handling sterile kits and trays:
- Sterile kits and trays generally have an outer protective wrapper and four inner flaps that must be opened aseptically.
- Open sterile kits away from your body first, touching only the very edge of the opening flap.
- Using the same technique, open each of the side flaps one at a time using only one hand, being careful not to allow your body or arms to be directly above the opened drape. Take care not to allow already-opened corners to flip back into the sterile area again.
- Open the final flap toward you, being careful to not allow any part of your body to be directly over the field. See Figure 4.17[94] for images of opening the flaps of a sterile kit.
- If you must remove parts of the sterile kit (i.e., sterile gloves), reach into the sterile field with the elbow raised, using only the tips of the fingers before extracting. Pay close attention to where your body and clothing are in relationship to the sterile field to avoid inadvertent contamination.
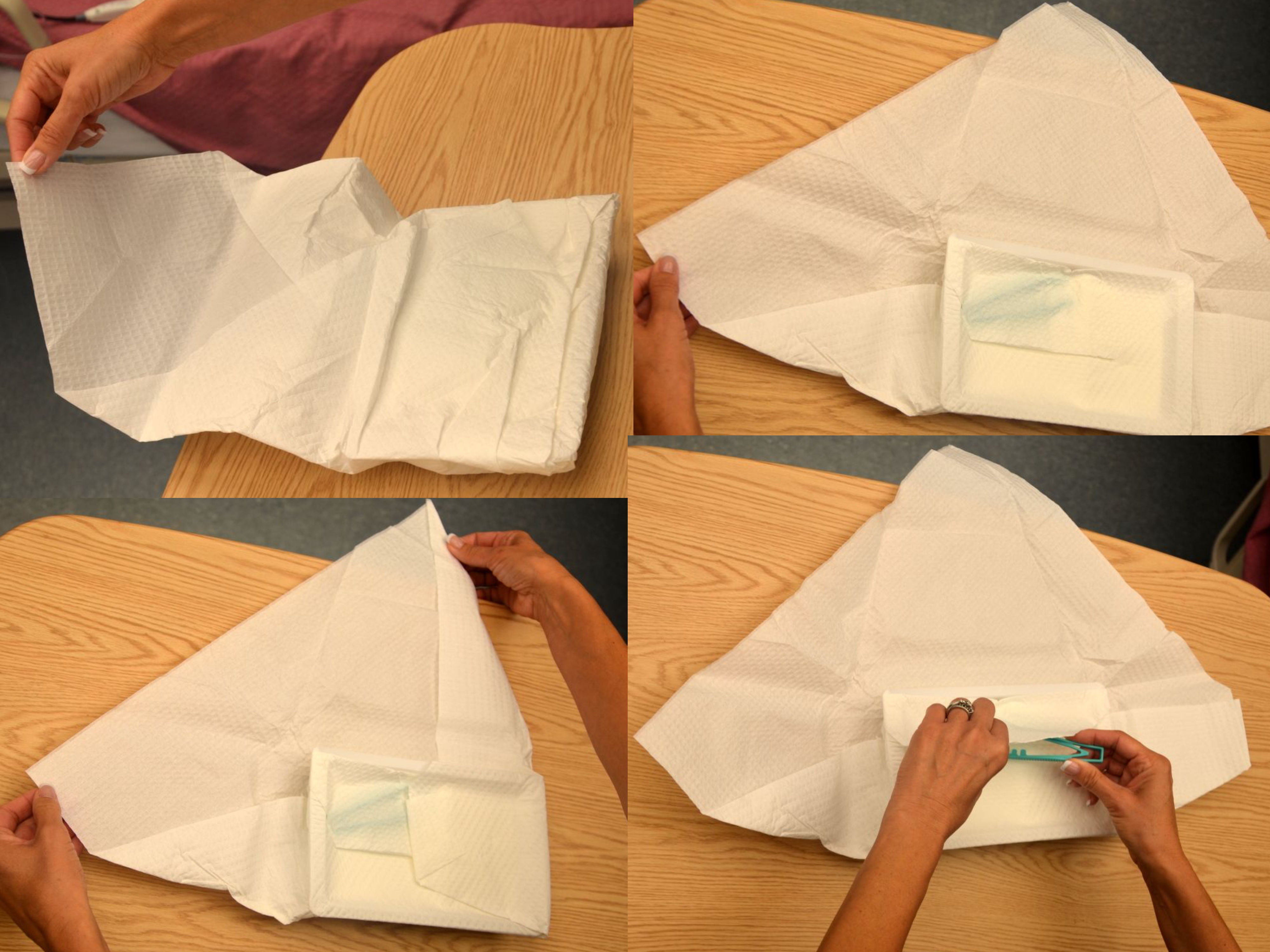
- When dispensing sterile supplies onto a sterile field:
- Before dispensing sterile supplies to a sterile field, do not allow sterile items to touch any part of the outer packaging once it is opened, including the former package seal.
- Heavy or irregular items should be opened and held, allowing a second person with sterile gloves to transfer them to the sterile field.
- Wrapped sterile items should be opened similarly to a sterile kit. Tuck each flap securely within your palm, and then open the flap away from your body first. Then open each side flap; secure the flap in the palm one at a time and open. Finally, open the flap (closest to you) toward you, while also protecting the other opened flaps from springing back onto the wrapped item.
- Peel pouches (i.e., gloves, gauze, syringes, etc.) can be opened by firmly grasping each side of the sealed edge with the thumb side of each hand parallel to the seal and pulling carefully apart.
- Drop items from six inches away from the sterile field.
- Sterile solutions should be poured into a sterile bowl or tray from the side of the sterile field and not directly over it. Use only sealed, sterile, unexpired solutions when pouring onto a sterile field. Solution should be held six inches away from the field as it is being poured. Avoid splashing solutions because this allows wicking and transfer of microbes. After pouring of solution stops, it should not be restarted because the edge is considered contaminated. See Figure 4.18[95] of an image of a nurse pouring sterile solution into a receptacle in a sterile field before the procedure begins.
- Don sterile gloves away from the sterile field to avoid contaminating the sterile field.

Use the checklist below to review the steps for completion of "Hand Hygiene With Soap and Water."
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Remove jewelry according to agency policy; push your sleeves above your wrists.
- Turn on the water and adjust the flow so that the water is warm. Wet your hands thoroughly, keeping your hands and forearms lower than your elbows. Avoid splashing water on your uniform.
- Apply a palm-sized amount of hand soap.
- Perform hand hygiene using plenty of lather and friction for at least 15 seconds:
- Rub hands palm to palm
- Back of right and left hand (fingers interlaced)
- Palm to palm with fingers interlaced
- Rotational rubbing of left and right thumbs
- Rub your fingertips against the palm of your opposite hand
- Rub wrists
- Repeat sequence at least 2 times
- Keep fingertips pointing downward throughout
- Clean under your fingernails with disposable nail cleaner (if applicable).
- Wash for a minimum of 20 seconds.
- Keep your hands and forearms lower than your elbows during the entire washing.
- Rinse your hands with water, keeping your fingertips pointing down so water runs off your fingertips. Do not shake water from your hands.
- Do not lean against the sink or touch the inside of the sink during the hand-washing process.
- Dry your hands thoroughly from your fingers to wrists with a paper towel or air dryer.
- Dispose of the paper towel(s).
- Use a new paper towel to turn off the water.
- Dispose of the paper towel.
Use the checklist below to review the steps for completion of "Hand Hygiene With Soap and Water."
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Remove jewelry according to agency policy; push your sleeves above your wrists.
- Turn on the water and adjust the flow so that the water is warm. Wet your hands thoroughly, keeping your hands and forearms lower than your elbows. Avoid splashing water on your uniform.
- Apply a palm-sized amount of hand soap.
- Perform hand hygiene using plenty of lather and friction for at least 15 seconds:
- Rub hands palm to palm
- Back of right and left hand (fingers interlaced)
- Palm to palm with fingers interlaced
- Rotational rubbing of left and right thumbs
- Rub your fingertips against the palm of your opposite hand
- Rub wrists
- Repeat sequence at least 2 times
- Keep fingertips pointing downward throughout
- Clean under your fingernails with disposable nail cleaner (if applicable).
- Wash for a minimum of 20 seconds.
- Keep your hands and forearms lower than your elbows during the entire washing.
- Rinse your hands with water, keeping your fingertips pointing down so water runs off your fingertips. Do not shake water from your hands.
- Do not lean against the sink or touch the inside of the sink during the hand-washing process.
- Dry your hands thoroughly from your fingers to wrists with a paper towel or air dryer.
- Dispose of the paper towel(s).
- Use a new paper towel to turn off the water.
- Dispose of the paper towel.
Use the checklist below to review the steps for completion of "Hand Hygiene With Alcohol-Based Hand Sanitizer."
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Gather supplies (antiseptic hand rub).
- Remove jewelry according to agency policy; push your sleeves above your wrists.
- Apply enough product into the palm of one hand and enough to cover your hands thoroughly, per product directions.
- Rub your hands together, covering all surfaces of your hands and fingers with antiseptic until the alcohol is dry (a minimum of 20-30 seconds):
- Rub hands palm to palm
- Back of right and left hand (fingers interlaced)
- Palm to palm with fingers interlaced
- Rotational rubbing of left and right thumbs
- Rub your fingertips against the palm of your opposite hand
- Rub your wrists
- Repeat hand sanitizing sequence a minimum of two times.
- Repeat hand sanitizing sequence until the product is dry.
Use the checklist below to review the steps for completion of "Hand Hygiene With Alcohol-Based Hand Sanitizer."
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Gather supplies (antiseptic hand rub).
- Remove jewelry according to agency policy; push your sleeves above your wrists.
- Apply enough product into the palm of one hand and enough to cover your hands thoroughly, per product directions.
- Rub your hands together, covering all surfaces of your hands and fingers with antiseptic until the alcohol is dry (a minimum of 20-30 seconds):
- Rub hands palm to palm
- Back of right and left hand (fingers interlaced)
- Palm to palm with fingers interlaced
- Rotational rubbing of left and right thumbs
- Rub your fingertips against the palm of your opposite hand
- Rub your wrists
- Repeat hand sanitizing sequence a minimum of two times.
- Repeat hand sanitizing sequence until the product is dry.
Use the checklist below to review the steps for completion of "Applying and Removing Personal Protective Equipment."[96]
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Check the provider's order for the type of precautions.
- Ensure that all supplies are available before check-off begins: isolation cart, gowns, gloves, mask, goggles/face shields, etc.
- Perform hand hygiene.
- Apply PPE in the correct order:
- 1st (GOWN): Gown should cover outer garments. Pull the sleeves down to the wrists, and tie at neck & waist.
- 2nd (MASK/RESPIRATOR): Apply surgical mask or N95 respirator if indicated by transmission-based precaution. Fit the mask around the nose and chin, securing bands around ears or tie straps at top of head and base of neck.
- 3rd (EYE PROTECTION): Apply goggles/face shield if indicated for patient condition or transmission-based precautions.
- 4th (CLEAN GLOVES): Pull on gloves to cover the wrist of the gown.
- Remove PPE in the correct order:
- 1st REMOVE GLOVES: REMEMBER: GLOVE TO GLOVE; SKIN TO SKIN. Do not touch contaminated gloves to your skin. Take off the contaminated glove with your gloved hand, wrapping the contaminated glove in the palm of your gloved hand. Take off the glove with your bare hand to the skin of your wrist, moving inside of the glove to remove the contaminated glove inside out over the other glove. Note: If the gown is tied in front, untie it prior to removing your glove.
- 2nd REMOVE GOWN: Untie all ties (or unsnap all buttons). Some gown ties can be broken rather than untied. Do so in a gentle manner, avoiding a forceful movement. Reach up to the shoulders and carefully pull the gown down and away from the body. Rolling the gown down is an acceptable approach. Dispose in trash receptacle.
- 3rd PERFORM HAND HYGIENE.
- 4th REMOVE FACE SHIELD or GOGGLES: Carefully remove face shield or goggles by grabbing the strap and pulling upwards and away from head. Do not touch the front of face shield or goggles.
- 5th REMOVE MASK or RESPIRATOR: Do not touch the front of the face shield or goggles.
- Respirator: Remove the bottom strap by touching only the strap and bringing it carefully over the head. Grasp the top strap and bring it carefully over the head, and then pull the respirator away from the face without touching the front of the respirator.
- Face mask: Carefully untie (or unhook from the ears) and pull it away from the face without touching the front.
- 6th PERFORM HAND HYGIENE after removing the mask.

