6.6 COPD
Open Resources for Nursing (Open RN)
Overview
Pathophysiology
Chronic obstructive pulmonary disease (COPD) is a chronic, progressive, and incurable respiratory condition that causes breathing difficulties and reduced lung function. COPD is characterized by the obstruction of airflow in and out of the lungs. The primary cause of COPD is cigarette smoking. A deficiency of Alpha 1 antitrypsin, an enzyme with lung protective properties, is also a potential cause of COPD. Other causes of COPD include prolonged exposure to irritants that damage the lungs, such as environmental exposures, including air pollution, dust, chemicals, or secondhand smoke.[1]
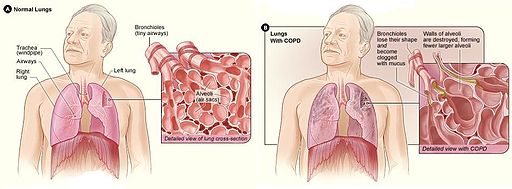
COPD includes two conditions called chronic bronchitis and emphysema. Chronic bronchitis is an inflammation of the bronchi and bronchioles characterized by increased mucus and chronic productive cough for at least three months of the year for at least two consecutive years. Emphysema is a destructive problem of lung elastic tissue that reduces its ability to recoil after stretching, leading to hyperinflation of the lung.
Most people who have COPD have a mixture of both emphysema and chronic bronchitis in different proportions, and the seriousness of each condition varies from person to person. In COPD, there is less air flow in and out of the airways because of one or more reasons[2]:
- The airways and alveoli lose their elastic quality.
- The walls between many of the air sacs are destroyed.
- The walls of the airways become thick and inflamed.
- The airways make more mucus than usual and can become clogged.
COPD is a progressive disease, meaning that symptoms worsen over time. In the early stages of COPD, individuals may not experience noticeable symptoms, but as the condition advances, breathing difficulties become more pronounced. Although there is no cure, treatments and lifestyle changes such as quitting smoking can help clients feel better, stay more active, and slow the progress of the disease. Oxygen therapy, pulmonary rehabilitation, and medications are prescribed to manage symptoms and enhance quality of life. Individuals with advanced COPD may require palliative and/or hospice care services.[3] See Figure 6.22[4] for an illustration of COPD.
Symptoms
Common symptoms of COPD include the following[5]:
- Dyspnea, especially with physical activity. Clients may report breathing takes more effort or they are gasping for air.
- Fatigue due to reduced oxygenation of the body’s tissues and muscles.
- An ongoing cough or a cough that produces a lot of mucus, sometimes called a smoker’s cough. This is often the first symptom of COPD. However, they are not always strong enough to cough up the mucus due to the associated fatigue.
- Audible wheezing (i.e., a whistling or squeaky sound when breathing).
- Chest tightness or heaviness. Clients may report it is hard to take a deep breath or it’s painful to breathe.
- Nail clubbing from chronic hypoxia.
- Barrel chest due to hyperinflated alveoli
Acid-Base Balance
Because of the changes that occur in the bronchioles/alveoli and the air trapping that occurs in clients with COPD, the ability to inhale oxygen and exhale carbon dioxide is affected. It is common for clients with moderate to severe COPD to have ABG results with lower levels of dissolved oxygen in the blood (PaO2) and higher levels of dissolved carbon dioxide in the blood (PaCO2). As carbon dioxide is retained in the body, clients with COPD often develop chronic compensated respiratory acidosis as the kidneys compensate and retain bicarbonate to neutralize the acidic pH.[6]
Clients with acute exacerbations of COPD may develop uncompensated respiratory acidosis as gas exchange worsens. For this reason, ABGs are a common diagnostic test for clients hospitalized with a COPD exacerbation. Acute exacerbations of COPD are further discussed in the following subsection.
Review information about ABG analysis and respiratory acidosis in the “Acid-Base Balance” section in the “Fluids and Electrolytes” chapter in Open RN Nursing Fundamentals, 2e.
Acute Exacerbations of COPD
In addition to chronic symptoms of COPD that worsen over time, clients can also experience acute exacerbations of COPD. Environmental triggers and respiratory infections can lead to a sudden worsening of symptoms called a COPD exacerbation. During a COPD exacerbation, clients have worsening dyspnea and oxygen saturation levels lower than their baseline. If associated with a respiratory infection, they may also have a fever, increased chest tightness, worsening cough, and purulent sputum. Acute exacerbations often require hospitalization, so rapid recognition of these symptoms and notification of the health care provider are vital.
Clients with acute exacerbations of COPD undergo additional diagnostic testing, such as a chest X-ray, complete blood count (with a focus on WBCs), and ABG. Read more about these diagnostic tests in the “General Respiratory System Assessment and Interventions” section. ABG results may indicate uncompensated respiratory acidosis as the PaCO2 levels increase and the kidneys are no longer able to compensate for the retained CO2. ABG results help guide medical treatment.
Inhaled or oral steroids and additional bronchodilators may be prescribed. Antibiotics may be prescribed when a respiratory bacterial infection is suspected or confirmed. Severe symptoms may require hospitalization. Intravenous corticosteroids may be prescribed, along with noninvasive positive pressure ventilation, commonly referred to as CPAP or BiPAP. In very severe cases, intubation and mechanical ventilation may be required.
Oxygen Therapy
Long-term oxygen therapy (LTOT) is prescribed for clients with chronic obstructive pulmonary disease (COPD) when oxygen saturation levels are 88% or less when at rest and in a stable clinical condition. Research indicates that LTOT improves survival benefits and quality of life for clients with COPD with chronic hypoxemia. Other positive outcomes include decreased depression, improved cognitive function, improved exercise capacity, and decreased hospital admission rates.[7] Respiratory therapists typically assist clients in setting up LTOT, establish the oxygenation device and oxygen flow rates, and provide health teaching about its safe use in the home. Nurses reinforce this information on discharge and during follow-up visits.
Read additional information about oxygen equipment and safety measures in the “Oxygen Therapy” chapter of Open RN Nursing Skills, 2e.
Clients with COPD may be prescribed supplementary oxygen therapy during acute exacerbations of COPD or for long-term therapy. When administering oxygen to a client with COPD, it is important to understand how their respiratory drive differs from people who do not have COPD. As previously discussed in the “Review of Anatomy and Physiology of the Respiratory System” section of this chapter, an individual’s respiratory drive is primarily based on the level of carbon dioxide in their bloodstream. As carbon dioxide levels increase, the brain stimulates faster respiratory rates.
Clients with COPD chronically retain carbon dioxide, and their body’s response to high PaCO2 levels to stimulate breathing becomes blunted. Instead of relying on PaCO2 levels to initiate breathing, their brains primarily rely on dissolved oxygen levels in the bloodstream, referred to as hypoxic drive. For this reason, supplementary oxygen must be administered carefully to clients with COPD. Administering high-flow oxygen to a COPD client could potentially suppress their drive to breathe and cause a decreased respiratory rate, leading to additional carbon dioxide retention. To ensure the safe administration of supplemental oxygen to clients with COPD, it is crucial to follow these guidelines[8]:
- Aim for their prescribed target oxygen saturation level (usually between 88-92%).
- Provide oxygen at a low-flow rate, typically no more than 2-3 liters unless otherwise prescribed, to prevent the suppression of the client’s hypoxic drive.
- Continuously monitor the client’s pulse oximetry level, respiratory rate, and clinical condition. Titrate oxygen therapy to maintain the targeted oxygen saturation range while simultaneously avoiding suppression of their hypoxic drive to breathe.
COPD and Right-Sided Heart Failure
Clients with severe COPD may develop right-sided heart failure called cor pulmonale. As the right ventricle has to work harder to pump blood into the lungs that are hyperinflated, the cardiac muscle may enlarge and become less efficient.[9]
Review information about right-sided heart failure in the “Heart Failure” section of the “Cardiovascular Alterations” chapter.
Assessment
Clinical manifestations of COPD often develop as a result of reduced lung function. As with any chronic illness, it is vital for the nurse to be aware of a client’s baseline status to recognize signs of clinical deterioration requiring health care provider notification. See Table 6.6 for a summary of common manifestations of COPD across body systems.
Table 6.6. Clinical Manifestations of COPD[10],[11]
| Body System | Clinical Manifestations of COPD |
|---|---|
| Respiratory | Chronic cough, excessive sputum production, wheezing, dyspnea, reduced activity tolerance, barrel chest, adventitious lung sounds such as wheezing and rhonchi (coarse crackles), and frequent respiratory infections |
| Cardiovascular | Right-sided heart failure (Cor pulmonale) increases capillary refill time |
| Gastrointestinal | Decreased appetite and difficulty eating due to shortness of breath |
| Musculoskeletal | Reduced muscle strength or muscle wasting |
| Psychological & Emotional Well-Being | Anxiety and depression, reduced quality of life, and social isolation |
| Integumentary | Clubbing of the fingers and decreased skin turgor |
| Neurological | New onset confusion or change in level of consciousness if hypoxia or hypercapnia is present |
| General Symptoms | Fatigue or weakness |
Diagnostic Testing
The primary diagnostic test for COPD is spirometry. Spirometry can detect COPD even before symptoms are recognized. Spirometry test results determine the severity of COPD and are used to set treatment goals. Read more about spirometry testing under “Pulmonary Function Tests” in the General Respiratory System Assessment and Interventions” section of this chapter.
Clients with chronic COPD may also exhibit elevated levels of red blood cells, hemoglobin (Hgb), and hematocrit (HCT) as a compensatory response to chronic hypoxemia, which stimulates the production of red blood cells to carry more oxygen. This is referred to as secondary polycythemia.
Clients who are hospitalized for an acute COPD exacerbation have additional diagnostic testing performed, such as ABG, sputum samples, and chest X-rays.
- Arterial Blood Gas (ABG): As discussed earlier in this chapter, clients with stable, chronic COPD are often in a continual state of compensated respiratory acidosis due to carbon dioxide retention. However, clients experiencing an acute exacerbation of COPD often have ABG results indicating hypoxemia (low PaO2) and worsening hypercapnia (high PaCO2), resulting in uncompensated respiratory acidosis.
- Sputum Samples: Sputum samples may be obtained if an upper respiratory infection is suspected. These samples can help identify the presence of infection or other respiratory conditions.
- Chest X-ray: A chest X-ray may be obtained to assess for pneumonia. In clients with advanced COPD, the lungs may appear hyperinflated due to the destruction of alveolar walls and the trapping of air. The diaphragm may appear lower and flattened as a result of increased lung volume and hyperinflation. The weakened diaphragm has difficulty contracting effectively.
Review normal reference ranges for common diagnostic tests in “Appendix A – Normal Reference Ranges.”
Nursing Diagnoses
Nursing priorities for clients with COPD focus on improving respiratory function, enhancing quality of life, and promoting self-management.
Nursing diagnoses for clients with COPD are formulated based on the client’s assessment data, medical history, and specific needs. These nursing diagnoses guide the development of individualized care plans and interventions. Common nursing diagnoses are as follows[12]:
- Decreased Activity Tolerance
- Ineffective Airway Clearance
- Impaired gas exchange
- Anxiety
- Imbalanced Nutrition: Less Than Body Requirements
- Powerlessness
- Impaired Social Interaction
- Readiness for Enhanced Health Self-Management
Outcome Identification
Outcome identification includes setting short- and long-term goals and creating expected outcome statements customized for the client’s specific needs. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions.
Sample expected outcomes for common nursing diagnoses related to COPD include the following:
- The client will maintain a patent airway as evidenced by clear breath sounds and absence of wheezing or crackles.
- The client will maintain oxygen saturation within the specified target range (i.e., 88-92%).
- The client will report increased ability to perform daily activities without excessive fatigue or dyspnea.
- The client will achieve and maintain an appropriate body weight and body mass index (BMI) for their age and height.
- The client will participate in support groups with other individuals with COPD.
Interventions
Medical Interventions
The primary intervention for clients with COPD who smoke is smoking cessation. Other medical interventions for COPD aim to achieve effective symptom control, improve lung function, prevent exacerbations, and enhance the client’s quality of life. These interventions are prescribed by health care providers based on the client’s COPD severity and their individualized needs.
Smoking Cessation
The chemicals in cigarettes, e-cigarettes, and cigars can damage the lungs and cause worsening symptoms, increase the risk of exacerbations, and decrease lung function. Continued smoking can also make lungs unresponsive to COPD medications.
Read more information about smoking cessation on the American Lung Association’s Quit Smoking web page.
Medication Therapy
Common medications prescribed for COPD are as follows[13],[14],[15]:
- Bronchodilators: Short-acting beta-agonists (SABAs) and long-acting beta-agonists (LABAs) help relax airway muscles, improving airflow. Anticholinergic bronchodilators reduce bronchoconstriction and mucus production.
- Short-acting Beta-Agonists (SABAs): SABAs relieve symptomatic bronchoconstriction and improve airflow. They provide quick relief of symptoms. Albuterol is a Beta-2 agonist that relaxes the smooth muscle of bronchioles, producing bronchodilation. Ipratropium is an anticholinergic that blocks the action of acetylcholine in the smooth muscle of the bronchioles, causing bronchodilation.
- Long-acting Beta-Agonists (LABAs): LABAs, like salmeterol, work as long-acting bronchodilators to maintain airway patency over an extended period. They are used as maintenance therapy for clients with moderate to severe COPD to reduce symptoms and exacerbations by promoting bronchodilation throughout the day.
- Inhaled Corticosteroids (ICS): ICS, like fluticasone, reduce and control inflammation in the airways and lung tissues.
- Corticosteroids: Some clients with severe COPD, or those experiencing an acute exacerbation of COPD, require oral corticosteroids, like prednisone, to systemically reduce airway inflammation and suppress the immune response. Clients who are hospitalized for an acute exacerbation of COPD may be prescribed intravenous corticosteroids, like methylprednisolone IV, to rapidly reduce the immune response.
- Mucolytics: Mucolytic agents, like oral guaifenesin, may be used to thin mucus, making it easier to clear sputum from the airways. Some clients with severe COPD may be prescribed acetylcysteine or dornase alfa that are administered via a nebulizer.
- Oxygen Therapy: Clients with severe COPD may be prescribed long-term oxygen therapy. Review the “Oxygen Therapy” discussion in the “Overview” subsection.
Read more information about medication classes used to treat COPD in the “Respiratory System” chapter of Open RN Nursing Pharmacology, 2e.
Immunizations
Clients diagnosed with COPD are encouraged to remain up-to-date on recommended vaccinations, including influenza, pneumococcal (pneumonia), respiratory syncytial virus (RSV), pertussis (Tdap), and COVID vaccines.
Review current information about “Recommended Vaccines By Age” from the Centers for Disease Control and Prevention (CDC).
Pulmonary Rehabilitation
Clients with COPD are often referred for pulmonary rehabilitation. Pulmonary rehabilitation is a supervised program that includes exercise training, health education, and breathing techniques for people who have chronic lung conditions like COPD.[16]
Read additional information about pulmonary rehabilitation on the National Heart, Lung, and Blood Institute’s “Pulmonary Rehabilitation” web page.
Surgery
Surgery is usually a last resort for people with COPD who have severe symptoms that have not improved from medication therapy. Potential surgeries for severe COPD include the following[17],[18]:
- Bullectomy: In a bullectomy, one or more very large bullae are removed from the lungs. Bullae are larger air spaces that form when the walls of the air sacs are destroyed. These air spaces can become so large that they interfere with breathing.
- Implantation of One-way Endobronchial Valves: Valves may be implanted in one of the bronchial tubes that allow air to exit the damaged parts of the lung, but not reenter.
- Lung Volume Reduction Surgery (LVRS): LVRS helps people with severe emphysema that affects the upper lung lobes. LVRS is not a cure for COPD but may improve exercise capacity and quality of life. The goal of the surgery is to remove about 30 percent of the most diseased lung tissue. While this reduces the size of the lungs, it also allows the remaining healthier part of the lungs to work better. LVRS also can help the diaphragm to return to its normal shape, allowing the person to breathe more efficiently and improve lung capacity.
- Lung Transplant: Lung transplant may be considered for individuals with advanced COPD who have not responded to other treatments. It may be considered if the client’s lung damage cannot be repaired; if the client has had three or more severe, acute exacerbations of COPD within the last year; or they are not a candidate for LVRS. The transplant team will evaluate the client to see if they are physically and emotionally healthy enough for a lung transplant. Important factors include being a nonsmoker and at a healthy weight. Clients who are deemed qualified to receive a lung transplant are placed on a waiting list to receive a single- or double-lung transplant. After surgery, the client will remain on immunosuppressive medications for the rest of their life.
Nursing Interventions
Nursing interventions for COPD are centered around improving respiratory function, managing symptoms, and enhancing the client’s quality of life. These interventions are designed to provide holistic care and support to individuals with COPD.
Medication Management
Nurses in all settings evaluate the effectiveness of the prescribed medication therapy for COPD and monitor for potential side effects. Clients are taught the purpose of prescribed medications, how to use the inhalers, their potential side effects, and when to notify the health care provider.
Dyspnea Management
The nurse continually monitors the client’s level of dyspnea and implements and teaches about strategies to manage dyspnea. For example, coughing and breathing techniques, positioning, and pursed-lip breathing are helpful techniques. The nurse also assists with other prescribed respiratory interventions, such as postural drainage, incentive spirometry, and vibratory pressure therapy. Postural drainage is a form of physical therapy where body fluids are drained from the lungs by working with gravity and changing position, along with chest percussion. Review information in the “General Respiratory System Assessment and Interventions” section earlier in this chapter.
Energy Management
Nurses teaching energy conservation techniques to clients with COPD to help them manage fatigue and activity intolerance.
Review energy management techniques in the “Anemia” section of the “Hematological Alterations” chapter.
Health Teaching
Nurses provide health teaching about several topics. If the client smokes, they are encouraged to stop smoking. Clients are taught about the COPD disease process and how to recognize symptoms of acute exacerbations that require prompt notification of the health care provider. Breathing techniques, such as diaphragmatic breathing and pursed-lip breathing, are demonstrated, and the client is asked to perform a return demonstration to demonstrate understanding. Clients are also taught the importance of maintaining current vaccinations to prevent illness, such as influenza, COVID-19, and pneumococcal.
Healthy lifestyle choices such as balanced nutrition and regular physical activity are encouraged to maintain a healthy weight. Clients are also encouraged to maintain proper hydration to keep secretions thin and easily removed by coughing.
Psychosocial Support
COPD is a chronic, progressive, incurable illness. Clients may experience feelings of powerlessness and hopelessness as the disease progresses and their ability to participate in activities they normally enjoy becomes limited. Nurses advocate for medical treatments, home oxygen therapy, and pulmonary rehabilitation to help clients to optimally manage dyspnea and improve activity intolerance. Clients are encouraged to verbalize their feelings, and nurses therapeutically promote positive coping strategies to empower clients to effectively self-manage their chronic disease at home.
Evaluation
During the evaluation stage, nurses determine the effectiveness of nursing interventions for a specific client. The previously identified expected outcomes are reviewed to determine if they were met, partially met, or not met by the time frames indicated. If outcomes are not met or only partially met by the time frame indicated, the nursing care plan is revised. Evaluation should occur every time the nurse implements interventions with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with other members of the interprofessional team.
![]() RN Recap: COPD
RN Recap: COPD
View a brief YouTube video[19] overview of COPD:
- National Heart, Lung, and Blood Institute. (2023, October 25). What is COPD? National Institutes of Health. https://www.nhlbi.nih.gov/health/copd ↵
- National Heart, Lung, and Blood Institute. (2023, October 25). What is COPD? National Institutes of Health. https://www.nhlbi.nih.gov/health/copd ↵
- National Heart, Lung, and Blood Institute. (2023, October 25). What is COPD? National Institutes of Health. https://www.nhlbi.nih.gov/health/copd ↵
- “Copd 2010Side.JPG” by National Heart, Lung, and Blood Institute is licensed in the Public Domain. ↵
- National Heart, Lung, and Blood Institute. (2023, October 25). What is COPD? National Institutes of Health. https://www.nhlbi.nih.gov/health/copd ↵
- This work is a derivative of StatPearls by Pahal, Hashmi, & Sharma and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Shebl, Modi, & Cates and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Pahal, Hashmi, & Sharma and is licensed under CC BY 4.0 ↵
- Mooney, L., et al. (2021). Impact of chronic obstructive pulmonary disease in patients with heart failure with preserved ejection fraction: Insights from PARAGON‐HF. Journal of the American Heart Association, 10(23), e021494. https://www.ahajournals.org/doi/10.1161/JAHA.121.021494#d1e3937 ↵
- King Han, M., Dransfield, M. T., & Martinez, F. J. (2023). Chronic obstructive pulmonary disease: Diagnosis and staging. UpToDate. Retrieved September 29, 2023, from https://www.uptodate.com/ ↵
- Stoller, J. K. (2023). COPD exacerbations: Management. UpToDate. Retrieved September 27, 2023, from https://www.uptodate.com/ ↵
- Flynn Makic, M. B., & Martinez-Kratz, M. R. (2023). Ackley and Ladwig’s Nursing diagnosis handbook: An evidence-based guide to planning care (13th ed.). Elsevier. ↵
- American Lung Association. (2023, April 28). COPD causes and risk factors. https://www.lung.org/lung-health-diseases/lung-disease-lookup/copd/what-causes-copd ↵
- King Han, M., Dransfield, M. T., & Martinez, F. J. (2023). Chronic obstructive pulmonary disease: Diagnosis and staging. UpToDate. Retrieved September 29, 2023, from https://www.uptodate.com/ ↵
- Stoller, J. K. (2023). COPD exacerbations: Management. UpToDate. Retrieved September 27, 2023, from https://www.uptodate.com/ ↵
- National Heart, Lung, and Blood Institute. (2023, October 25). What is COPD? National Institutes of Health. https://www.nhlbi.nih.gov/health/copd ↵
- National Heart, Lung, and Blood Institute. (2023, October 25). What is COPD? National Institutes of Health. https://www.nhlbi.nih.gov/health/copd ↵
- American Lung Association. (n.d.). Chronic obstructive pulmonary disease. COPD. https://www.lung.org/lung-health-diseases/lung-disease-lookup/copd ↵
- Open RN Project. (2024, April 4).Health Alterations - Chapter 6 Respiratory - COPD [Video]. YouTube. CC BY-NC 4.0. https://youtu.be/VMT3dT82Xfg ↵
Learning Objectives
- Collaborate with interprofessional team members when providing client care
- Manage conflict among clients and health care staff
- Perform procedures necessary to safely admit, transfer, and/or discharge a client
- Assess the need for referrals and obtain necessary orders
- Describe how the health care team meets the needs of diverse patients in a variety of settings
- Identify strategies to ensure productive, effective team functioning
All health care students must prepare to deliberately work together in clinical practice with a common goal of building a safer, more effective, patient-centered health care system. The World Health Organization (WHO) defines interprofessional collaborative practice as multiple health workers from different professional backgrounds working together with patients, families, caregivers, and communities to deliver the highest quality of care.[1]
Effective teamwork and communication have been proven to reduce medical errors, promote a safety culture, and improve patient outcomes.[2] The importance of effective interprofessional collaboration has become even more important as nurses advocate to reduce health disparities related to social determinants of health (SDOH). In these efforts, nurses work with people from a variety of professions, such as physicians, social workers, educators, policy makers, attorneys, faith leaders, government employees, community advocates, and community members. Nursing students must be prepared to effectively collaborate interprofessionally after graduation.[3]
The Interprofessional Education Collaborative (IPEC) has identified four core competencies for effective interprofessional collaborative practice. This chapter will review content related to these four core competencies and provide examples of how they relate to nursing.
The Interprofessional Education Collaborative (IPEC) established standard core competencies for effective interprofessional collaborative practice. The competencies guide the education of future health professionals with the necessary knowledge, skills, values, and attitudes to collaboratively work together in providing client care. See Table 7.2 for a description of the four IPEC core competencies.[4] Each of these competencies will be further discussed in the following sections of this chapter.
Table 7.2. IPEC Core Competencies[5]
| Competency 1: Values/Ethics for Interprofessional Practice
Work with individuals of other professions to maintain a climate of mutual respect and shared values. |
|---|
| Competency 2: Roles/Responsibilities
Use the knowledge of one’s own role and those of other professions to appropriately assess and address the health care needs of patients and to promote and advance the health of populations. |
| Competency 3: Interprofessional Communication
Communicate with patients, families, communities, and professionals in health and other fields in a responsive and responsible manner that supports a team approach to the promotion and maintenance of health and the prevention and treatment of disease. |
| Competency 4: Teams and Teamwork
Apply relationship-building values and the principles of team dynamics to perform effectively in different team roles to plan, deliver, and evaluate patient/population-centered care and population health programs and policies that are safe, timely, efficient, effective, and equitable. |
The Interprofessional Education Collaborative (IPEC) established standard core competencies for effective interprofessional collaborative practice. The competencies guide the education of future health professionals with the necessary knowledge, skills, values, and attitudes to collaboratively work together in providing client care. See Table 7.2 for a description of the four IPEC core competencies.[6] Each of these competencies will be further discussed in the following sections of this chapter.
Table 7.2. IPEC Core Competencies[7]
| Competency 1: Values/Ethics for Interprofessional Practice
Work with individuals of other professions to maintain a climate of mutual respect and shared values. |
|---|
| Competency 2: Roles/Responsibilities
Use the knowledge of one’s own role and those of other professions to appropriately assess and address the health care needs of patients and to promote and advance the health of populations. |
| Competency 3: Interprofessional Communication
Communicate with patients, families, communities, and professionals in health and other fields in a responsive and responsible manner that supports a team approach to the promotion and maintenance of health and the prevention and treatment of disease. |
| Competency 4: Teams and Teamwork
Apply relationship-building values and the principles of team dynamics to perform effectively in different team roles to plan, deliver, and evaluate patient/population-centered care and population health programs and policies that are safe, timely, efficient, effective, and equitable. |
The first IPEC competency is related to values and ethics and states, “Work with individuals of other professions to maintain a climate of mutual respect and shared values.”[8] See the box below for the components related to this competency. Notice how these interprofessional competencies are very similar to the Standards of Professional Performance established by the American Nurses Association related to Ethics, Advocacy, Respectful and Equitable Practice, Communication, and Collaboration.[9]
Components of IPEC’s Values/Ethics for Interprofessional Practice Competency[10]
- Place interests of clients and populations at the center of interprofessional health care delivery and population health programs and policies, with the goal of promoting health and health equity across the life span.
- Respect the dignity and privacy of patients while maintaining confidentiality in the delivery of team-based care.
- Embrace the cultural diversity and individual differences that characterize patients, populations, and the health team.
- Respect the unique cultures, values, roles/responsibilities, and expertise of other health professions and the impact these factors can have on health outcomes.
- Work in cooperation with those who receive care, those who provide care, and others who contribute to or support the delivery of prevention and health services and programs.
- Develop a trusting relationship with patients, families, and other team members.
- Demonstrate high standards of ethical conduct and quality of care in contributions to team-based care.
- Manage ethical dilemmas specific to interprofessional patient/population-centered care situations.
- Act with honesty and integrity in relationships with patients, families, communities, and other team members.
- Maintain competence in one’s own profession appropriate to scope of practice.
Nursing, medical, and other health professional programs typically educate students in “silos” with few opportunities to collaboratively work together in the classroom or in clinical settings. However, after being hired for their first job, these graduates are thrown into complex clinical situations and expected to function as part of the team. One of the first steps in learning how to function as part of an effective interprofessional team is to value each health care professional’s contribution to quality, patient-centered care. Mutual respect and trust are foundational to effective interprofessional working relationships for collaborative care delivery across the health professions. Collaborative care also honors the diversity reflected in the individual expertise each profession brings to care delivery.[11]
Cultural diversity is a term used to describe cultural differences among clients, family members, and health care team members. While it is useful to be aware of specific traits of a culture, it is just as important to understand that each individual is unique, and there are always variations in beliefs among individuals within a culture. Nurses should, therefore, refrain from making assumptions about the values and beliefs of members of specific cultural groups.[12] Instead, a better approach is recognizing that culture is not a static, uniform characteristic but instead realizing there is diversity within every culture and in every person. The American Nurses Association (ANA) defines cultural humility as, “A humble and respectful attitude toward individuals of other cultures that pushes one to challenge their own cultural biases, realize they cannot possibly know everything about other cultures, and approach learning about other cultures as a lifelong goal and process.”[13] It is imperative for nurses to integrate culturally responsive care into their nursing practice and interprofessional collaborative practice.
Read more about cultural diversity, cultural humility, and integrating culturally responsive care in the “Diverse Patients” chapter of Open RN Nursing Fundamentals, 2e.
Nurses value the expertise of interprofessional team members and integrate this expertise when providing patient-centered care. Some examples of valuing and integrating the expertise of interprofessional team members include the following:
- A nurse is caring for a patient admitted with chronic heart failure to a medical-surgical unit. During the shift the patient’s breathing becomes more labored and the patient states, “My breathing feels worse today.” The nurse ensures the patient’s head of bed is elevated, oxygen is applied according to the provider orders, and the appropriate scheduled and PRN medications are administered, but the patient continues to complain of dyspnea. The nurse calls the respiratory therapist and requests a STAT consult. The respiratory therapist assesses the patient and recommends implementation of BiPAP therapy. The provider is notified and an order for BiPAP is received. The patient reports later in the shift the dyspnea is resolved with the BiPAP therapy.
- A nurse is working in the Emergency Department when an adolescent patient arrives via ambulance experiencing a severe asthma attack. The paramedic provides a handoff report with the patient's current vital signs, medications administered, and intravenous (IV) access established. The paramedic also provides information about the home environment, including information about vaping products and a cat in the adolescent’s bedroom. The nurse thanks the paramedic for sharing these observations and plans to use information about the home environment to provide patient education about asthma triggers and tobacco cessation after the patient has been stabilized.
- A nurse is working in a long-term care environment with several assistive personnel (AP) who work closely with the residents providing personal cares and have excellent knowledge regarding their baseline status. Today, after helping Mrs. Smith with her morning bath, one of the APs tells the nurse, “Mrs. Smith doesn’t seem like herself today. She was very tired and kept falling asleep while I was talking to her, which is not her normal behavior.” The nurse immediately assesses Mrs. Smith and confirms her somnolescence and confirms her vital signs are within her normal range. The nurse reviews Mrs. Smith’s chart and notices that a new prescription for furosemide was started last month but no potassium supplements were ordered. The nurse notifies the provider of the patient’s change in status and receives an order for lab work including an electrolyte panel. The results indicate that Mrs. Smith’s potassium level has dropped to an abnormal level, which is the likely cause of her fatigue and somnolescence. The provider is notified, and an order is received for a potassium supplement. The nurse thanks the AP for recognizing and reporting Mrs. Smith’s change in status and successfully preventing a poor patient outcome such as a life-threatening cardiac dysrhythmia.
Effective patient-centered, interprofessional collaborative practice improves patient outcomes. View supplementary material and reflective questions in the following box.[14]
View the “How does interprofessional collaboration impact care: The patient’s perspective?” video on YouTube regarding patients' perspectives about the importance of interprofessional collaboration.
Read Ten Lessons in Collaboration. Although this is an older publication, it provides ten lessons to consider in collaborative relationships and practice. The discussion reflects many components of collaboration that have been integral to nursing practice in interprofessional teamwork and leadership.
Reflective Questions
- What is the difference between patient-centered care and disease-centered care?
- Why is it important for health professionals to collaborate?
The first IPEC competency is related to values and ethics and states, “Work with individuals of other professions to maintain a climate of mutual respect and shared values.”[15] See the box below for the components related to this competency. Notice how these interprofessional competencies are very similar to the Standards of Professional Performance established by the American Nurses Association related to Ethics, Advocacy, Respectful and Equitable Practice, Communication, and Collaboration.[16]
Components of IPEC’s Values/Ethics for Interprofessional Practice Competency[17]
- Place interests of clients and populations at the center of interprofessional health care delivery and population health programs and policies, with the goal of promoting health and health equity across the life span.
- Respect the dignity and privacy of patients while maintaining confidentiality in the delivery of team-based care.
- Embrace the cultural diversity and individual differences that characterize patients, populations, and the health team.
- Respect the unique cultures, values, roles/responsibilities, and expertise of other health professions and the impact these factors can have on health outcomes.
- Work in cooperation with those who receive care, those who provide care, and others who contribute to or support the delivery of prevention and health services and programs.
- Develop a trusting relationship with patients, families, and other team members.
- Demonstrate high standards of ethical conduct and quality of care in contributions to team-based care.
- Manage ethical dilemmas specific to interprofessional patient/population-centered care situations.
- Act with honesty and integrity in relationships with patients, families, communities, and other team members.
- Maintain competence in one’s own profession appropriate to scope of practice.
Nursing, medical, and other health professional programs typically educate students in “silos” with few opportunities to collaboratively work together in the classroom or in clinical settings. However, after being hired for their first job, these graduates are thrown into complex clinical situations and expected to function as part of the team. One of the first steps in learning how to function as part of an effective interprofessional team is to value each health care professional’s contribution to quality, patient-centered care. Mutual respect and trust are foundational to effective interprofessional working relationships for collaborative care delivery across the health professions. Collaborative care also honors the diversity reflected in the individual expertise each profession brings to care delivery.[18]
Cultural diversity is a term used to describe cultural differences among clients, family members, and health care team members. While it is useful to be aware of specific traits of a culture, it is just as important to understand that each individual is unique, and there are always variations in beliefs among individuals within a culture. Nurses should, therefore, refrain from making assumptions about the values and beliefs of members of specific cultural groups.[19] Instead, a better approach is recognizing that culture is not a static, uniform characteristic but instead realizing there is diversity within every culture and in every person. The American Nurses Association (ANA) defines cultural humility as, “A humble and respectful attitude toward individuals of other cultures that pushes one to challenge their own cultural biases, realize they cannot possibly know everything about other cultures, and approach learning about other cultures as a lifelong goal and process.”[20] It is imperative for nurses to integrate culturally responsive care into their nursing practice and interprofessional collaborative practice.
Read more about cultural diversity, cultural humility, and integrating culturally responsive care in the “Diverse Patients” chapter of Open RN Nursing Fundamentals, 2e.
Nurses value the expertise of interprofessional team members and integrate this expertise when providing patient-centered care. Some examples of valuing and integrating the expertise of interprofessional team members include the following:
- A nurse is caring for a patient admitted with chronic heart failure to a medical-surgical unit. During the shift the patient’s breathing becomes more labored and the patient states, “My breathing feels worse today.” The nurse ensures the patient’s head of bed is elevated, oxygen is applied according to the provider orders, and the appropriate scheduled and PRN medications are administered, but the patient continues to complain of dyspnea. The nurse calls the respiratory therapist and requests a STAT consult. The respiratory therapist assesses the patient and recommends implementation of BiPAP therapy. The provider is notified and an order for BiPAP is received. The patient reports later in the shift the dyspnea is resolved with the BiPAP therapy.
- A nurse is working in the Emergency Department when an adolescent patient arrives via ambulance experiencing a severe asthma attack. The paramedic provides a handoff report with the patient's current vital signs, medications administered, and intravenous (IV) access established. The paramedic also provides information about the home environment, including information about vaping products and a cat in the adolescent’s bedroom. The nurse thanks the paramedic for sharing these observations and plans to use information about the home environment to provide patient education about asthma triggers and tobacco cessation after the patient has been stabilized.
- A nurse is working in a long-term care environment with several assistive personnel (AP) who work closely with the residents providing personal cares and have excellent knowledge regarding their baseline status. Today, after helping Mrs. Smith with her morning bath, one of the APs tells the nurse, “Mrs. Smith doesn’t seem like herself today. She was very tired and kept falling asleep while I was talking to her, which is not her normal behavior.” The nurse immediately assesses Mrs. Smith and confirms her somnolescence and confirms her vital signs are within her normal range. The nurse reviews Mrs. Smith’s chart and notices that a new prescription for furosemide was started last month but no potassium supplements were ordered. The nurse notifies the provider of the patient’s change in status and receives an order for lab work including an electrolyte panel. The results indicate that Mrs. Smith’s potassium level has dropped to an abnormal level, which is the likely cause of her fatigue and somnolescence. The provider is notified, and an order is received for a potassium supplement. The nurse thanks the AP for recognizing and reporting Mrs. Smith’s change in status and successfully preventing a poor patient outcome such as a life-threatening cardiac dysrhythmia.
Effective patient-centered, interprofessional collaborative practice improves patient outcomes. View supplementary material and reflective questions in the following box.[21]
View the “How does interprofessional collaboration impact care: The patient’s perspective?” video on YouTube regarding patients' perspectives about the importance of interprofessional collaboration.
Read Ten Lessons in Collaboration. Although this is an older publication, it provides ten lessons to consider in collaborative relationships and practice. The discussion reflects many components of collaboration that have been integral to nursing practice in interprofessional teamwork and leadership.
Reflective Questions
- What is the difference between patient-centered care and disease-centered care?
- Why is it important for health professionals to collaborate?
The second IPEC competency relates to the roles and responsibilities of health care professionals and states, “Use the knowledge of one’s own role and those of other professions to appropriately assess and address the health care needs of patients and to promote and advance the health of populations.”[22]
See the following box for the components of this competency. It is important to understand the roles and responsibilities of the other health care team members; recognize one’s limitations in skills, knowledge, and abilities; and ask for assistance when needed to provide quality, patient-centered care.
Components of IPEC’s Roles/Responsibilities Competency[23]
- Communicate one’s roles and responsibilities clearly to patients, families, community members, and other professionals.
- Recognize one’s limitations in skills, knowledge, and abilities.
- Engage with diverse professionals who complement one’s own professional expertise, as well as associated resources, to develop strategies to meet specific health and health care needs of patients and populations.
- Explain the roles and responsibilities of other providers and the manner in which the team works together to provide care, promote health, and prevent disease.
- Use the full scope of knowledge, skills, and abilities of professionals from health and other fields to provide care that is safe, timely, efficient, effective, and equitable.
- Communicate with team members to clarify each member’s responsibility in executing components of a treatment plan or public health intervention.
- Forge interdependent relationships with other professions within and outside of the health system to improve care and advance learning.
- Engage in continuous professional and interprofessional development to enhance team performance and collaboration.
- Use unique and complementary abilities of all members of the team to optimize health and patient care.
- Describe how professionals in health and other fields can collaborate and integrate clinical care and public health interventions to optimize population health.
Nurses communicate with several individuals during a typical shift. For example, during inpatient care, nurses may communicate with patients and their family members; pharmacists and pharmacy technicians; providers from different specialties; physical, speech, and occupational therapists; dietary aides; respiratory therapists; chaplains; social workers; case managers; nursing supervisors, charge nurses, and other staff nurses; assistive personnel; nursing students; nursing instructors; security guards; laboratory personnel; radiology and ultrasound technicians; and surgical team members. Providing holistic, quality, safe, and effective care means every team member taking care of patients must work collaboratively and understand the knowledge, skills, and scope of practice of the other team members. Table 7.4 provides examples of the roles and responsibilities of common health care team members that nurses frequently work with when providing patient care. To fully understand the roles and responsibilities of the multiple members of the complex health care delivery system, it is beneficial to spend time shadowing those within these roles.
Table 7.4. Roles and Responsibilities of Members of the Health Care Team
| Member | Role/Responsibilities |
|---|---|
| Assistive Personnel (e.g., certified nursing assistants [CNA], patient-care technicians [PCT], certified medical assistants [CMA], certified medication aides, and home health aides) | Work under the direct supervision of the RN. (Read more about Assistive Personnel (AP) in the “Delegation and Supervision” chapter.) |
| Licensed Practical/Vocational Nurses (LPN/VN) | Assist the RN by performing routine, basic nursing care with predictable outcomes. (Read more details in the “Delegation and Supervision” chapter.) |
| Registered Nurses (RN) | Use the nursing process to assess, diagnose, identify expected outcomes, plan and implement interventions, and evaluate care according to the Nurse Practice Act of the state they are employed. |
| Charge Nurses or Nursing Supervisors | Supervise members of the nursing team and overall patient care on the unit (or organization) to ensure quality, safe care is delivered. |
| Directors of Nursing (DON), Chief Nursing Officer (CNO), or Vice President of Patient Services | Ensure federal and state regulations and standards are being followed and are accountable for all aspects of patient care. |
| Clinical Nurse Specialist (CNS) | Practice in a variety of health care environments and participate in mentoring other nurses, case management, research, designing and conducting quality improvement programs, and serving as educators and consultants. |
| Nurse Practitioners (NP) or Advanced Practice Registered Nurses (APRN) | Work in a variety of settings and complete physical examinations, diagnose and treat common acute illness, manage chronic illness, order laboratory and diagnostic tests, prescribe medications and other therapies, provide health teaching and supportive counseling with an emphasis on prevention of illness and health maintenance, and refer clients to other health professionals and specialists as needed. NPs have advanced knowledge with a graduate degree and national certification. |
| Certified Registered Nurse Anesthetists (CRNA) | Administer anesthesia and related care before, during, and after surgical, therapeutic, diagnostic, and obstetrical procedures, as well as provide airway management during medical emergencies. |
| Certified Nurse Midwives (CNM) | Provide gynecological exams, family planning guidance, prenatal care, management of low-risk labor and delivery, and neonatal care. |
| Medical Doctors (MD) | Licensed providers who diagnose, treat, and direct medical care. There are many types of physician specialists such as surgeons, pulmonologists, neurologists, cardiologists, nephrologists, pediatricians, and ophthalmologists. |
| Physician Assistants (PA) | Work under the direct supervision of a medical doctor as licensed and certified professionals following protocols based on the state in which they practice. |
| Doctors of Osteopathy (DO) | Licensed providers similar to medical physicians but with different educational preparation and licensing exams. They provide care, prescribe, and can perform surgeries. |
| Dieticians | Assess, plan, implement, and evaluate interventions related to specific dietary needs of clients, including regular or therapeutic diets. Formulate diets for clients with dysphagia or other physical disorders and provide dietary education such as diabetes education. |
| Physical Therapists (PT) | Develop and implement a plan of care as a licensed professional for clients with dysfunctional physical abilities, including joints, strength, mobility, gait, balance, and coordination. |
| Occupational Therapists (OT) | Plan, provide, and evaluate care for clients with dysfunction affecting their independence and ability to complete activities of daily living (ADLs). Assist clients in using adaptive devices to reach optimal levels of functioning and provide home safety assessments. |
| Speech Therapists (ST) | Develop and initiate a plan of care for clients diagnosed with communication and swallowing disorders. |
| Respiratory Therapists (RT) | Specialize in treating clients with respiratory disorders or conditions in collaboration with providers. Provide treatments such as CPAP, BiPAP, respiratory treatments and medications like aerosol nebulizers, chest physiotherapy, and postural drainage. They also intubate clients, assist with bronchoscopies, manage mechanical ventilation, and perform pulmonary function tests. |
| Social Workers (SW) | Provide a liaison between the community and the health care setting to ensure continuity of care after discharge. Assist clients with establishing community resources, health insurance, and advance directives. |
| Psychologists and Psychiatrists | Provide mental health services to clients in both acute and long-term settings. As physician specialists, psychiatrists prescribe medications and perform other medical treatments for mental health disorders. Psychologists focus on counseling. |
| Nurse Case Managers or Discharge Planners | Ensure clients are provided with effective and efficient medical care and services, during inpatient care and post-discharge, while also managing the cost of these services. |
The coordination and delivery of safe, quality patient care demands reliable teamwork and collaboration across the organizational and community boundaries. Clients often have multiple visits across multiple providers working in different organizations. Communication failures between health care settings, departments, and team members is the leading cause of patient harm.[24] The health care system is becoming increasingly complex requiring collaboration among diverse health care team members.
The goal of good interprofessional collaboration is improved patient outcomes, as well as increased job satisfaction of health care team professionals. Patients receiving care with poor teamwork are almost five times as likely to experience complications or death. Hospitals in which staff report higher levels of teamwork have lower rates of workplace injuries and illness, fewer incidents of workplace harassment and violence, and lower turnover.[25]
Valuing and understanding the roles of team members are important steps toward establishing good interprofessional teamwork. Another step is learning how to effectively communicate with interprofessional team members.

