9.3 Cardiovascular Assessment
Open Resources for Nursing (Open RN)
A thorough assessment of the heart provides valuable information about the function of a patient’s cardiovascular system. Understanding how to properly assess the cardiovascular system and identifying both normal and abnormal assessment findings will allow the nurse to provide quality, safe care to the patient.
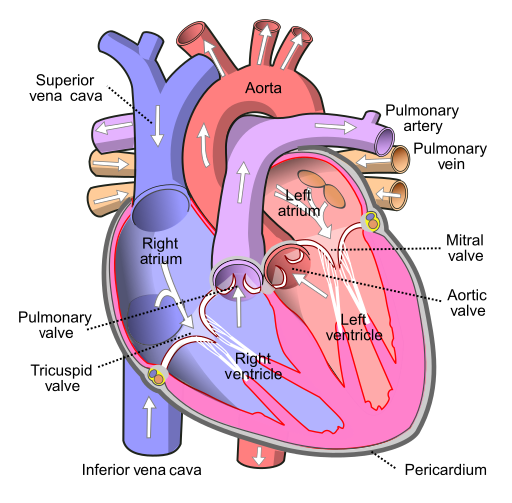
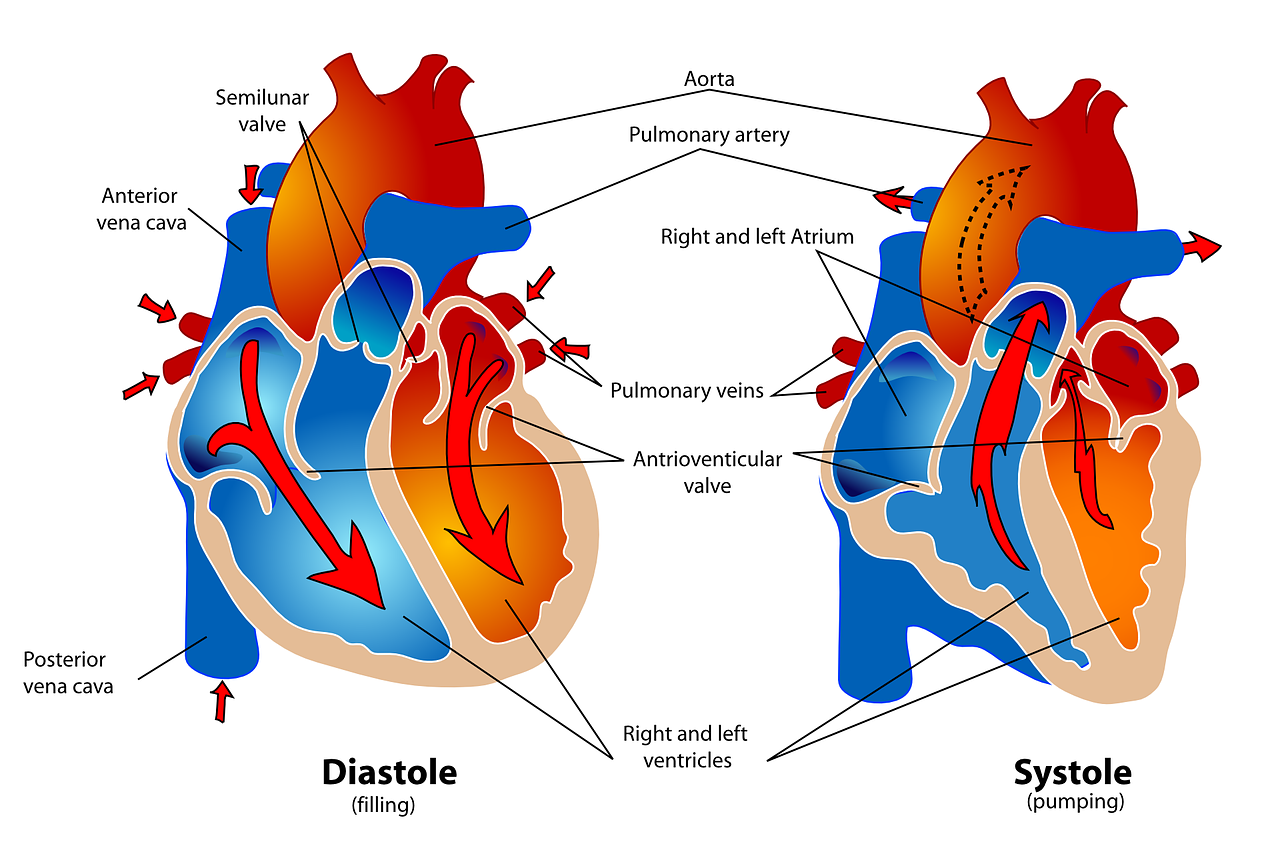
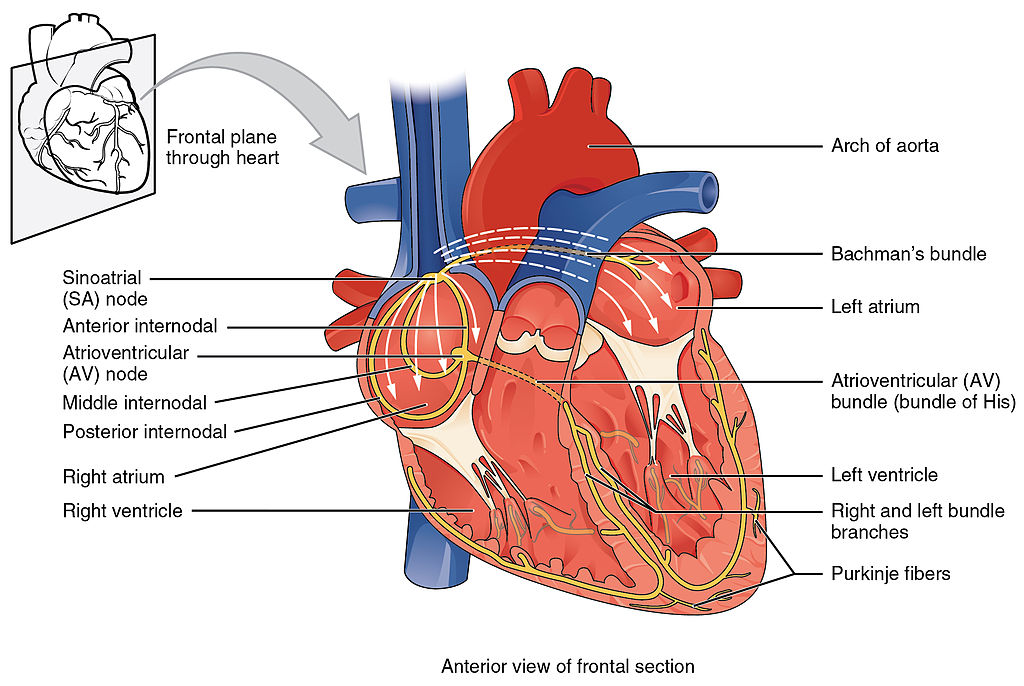
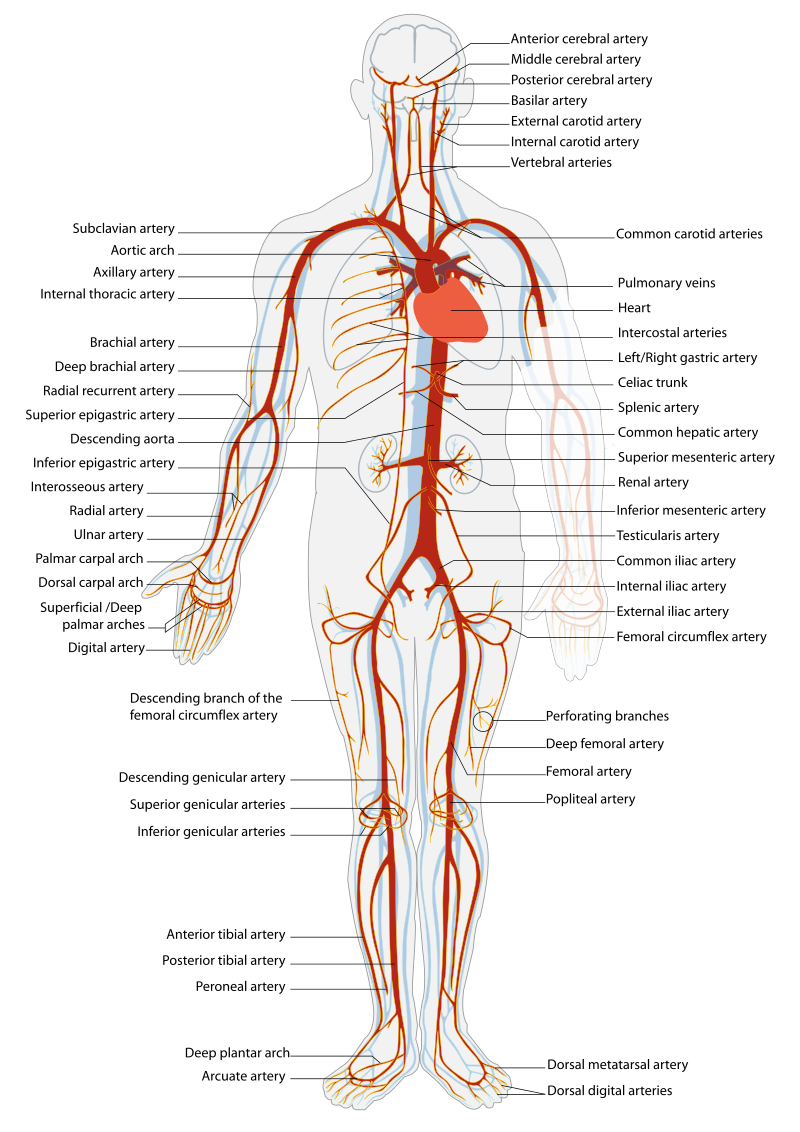
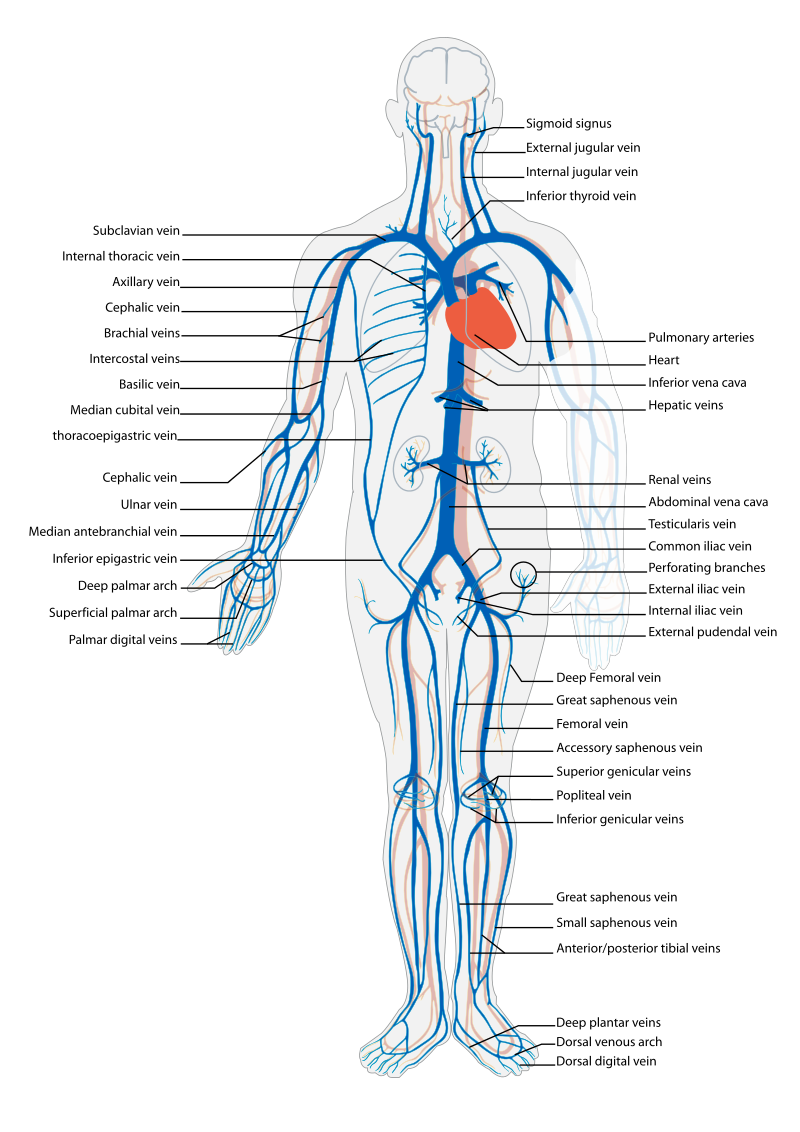
Before assessing a patient’s cardiovascular system, it is important to understand the various functions of the cardiovascular system. In addition to the information provided in the “Review of Cardiac Basics” section, the following images provide an overview of the cardiovascular system. Figure 9.1[1] provides an overview of the structure of the heart. Note the main cardiac structures are the atria, ventricles, and heart valves. Figure 9.2[2] demonstrates blood flow through the heart. Notice the flow of deoxygenated blood from the posterior and superior vena cava into the right atria and ventricle during diastole (indicated by blue coloring of these structures). The right ventricle then pumps deoxygenated blood to the lungs via the pulmonary artery during systole. At the same time, oxygenated blood from the lungs returns to the left atria and ventricle via the pulmonary veins during diastole (indicated by red coloring of these structures) and then is pumped out to the body via the aorta during systole. Figure 9.3[3] demonstrates the conduction system of the heart. This image depicts the conduction pathway through the heart as the tissue responds to electrical stimulation. Figure 9.4[4] illustrates the arteries of the circulatory system, and Figure 9.5[5] depicts the veins of the circulatory system. The purpose of these figures is to facilitate understanding of the electrical and mechanical function of the heart within the cardiovascular system.
Assessing the cardiovascular system includes performing several subjective and objective assessments. At times, assessment findings are modified according to life span considerations.
Subjective Assessment
The subjective assessment of the cardiovascular and peripheral vascular system is vital for uncovering signs of potential dysfunction. To complete the subjective cardiovascular assessment, the nurse begins with a focused interview. The focused interview explores past medical and family history, medications, cardiac risk factors, and reported symptoms. Symptoms related to the cardiovascular system include chest pain, peripheral edema, unexplained sudden weight gain, shortness of breath (dyspnea), irregular pulse rate or rhythm, dizziness, or poor peripheral circulation. Any new or worsening symptoms should be documented and reported to the health care provider.
Table 9.3a outlines questions used to assess symptoms related to the cardiovascular and peripheral vascular systems. Table 9.3b outlines questions used to assess medical history, medications, and risk factors related to the cardiovascular system. Information obtained from the interview process is used to tailor future patient education by the nurse.[6],[7],[8]
Table 9.3a Interview Questions for Cardiovascular and Peripheral Vascular Systems[9]
| Symptom | Question |
Follow-Up Safety Note: If findings indicate current severe symptoms suggestive of myocardial infarction or another critical condition, suspend the remaining cardiovascular assessment and obtain immediate assistance according to agency policy or call 911. |
|---|---|---|
| Chest Pain | Have you had any pain or pressure in your chest, neck, or arm? | Review how to assess a patient’s chief complaint using the PQRSTU method in the “Health History” chapter.
|
| Shortness of Breath
(Dyspnea) |
Do you ever feel short of breath with activity?
Do you ever feel short of breath at rest? Do you feel short of breath when lying flat? |
What level of activity elicits shortness of breath?
How long does it take you to recover? Have you ever woken up from sleeping feeling suddenly short of breath How many pillows do you need to sleep, or do you sleep in a chair (orthopnea)? Has this recently changed? |
| Edema | Have you noticed swelling of your feet or ankles?
Have you noticed your rings, shoes, or clothing feel tight at the end of the day? Have you noticed any unexplained, sudden weight gain? Have you noticed any new abdominal fullness? |
Has this feeling of swelling or restriction gotten worse?
Is there anything that makes the swelling better (e.g., sitting with your feet elevated)? How much weight have you gained? Over what time period have you gained this weight? |
| Palpitations | Have you ever noticed your heart feels as if it is racing or “fluttering” in your chest?
Have you ever felt as if your heart “skips” a beat? |
Are you currently experiencing palpitations?
When did palpitations start? Have you previously been treated for palpitations? If so, what treatment did you receive? |
| Dizziness (Syncope) |
Do you ever feel light-headed?
Do you ever feel dizzy? Have you ever fainted? |
Can you describe what happened?
Did you have any warning signs? Did this occur with position change? |
| Poor Peripheral Circulation | Do your hands or feet ever feel cold or look pale or bluish?
Do you have pain in your feet or lower legs when exercising? |
What, if anything, brings on these symptoms?
How much activity is needed to cause this pain? Is there anything, such as rest, that makes the pain better? |
| Calf Pain | Do you currently have any constant pain in your lower legs? | Can you point to the area of pain with one finger? |
Table 9.3b Interview Questions Exploring Cardiovascular Medical History, Medications, and Cardiac Risk Factors
| Topic | Questions |
|---|---|
| Medical History | Have you ever been diagnosed with any heart or circulation conditions, such as high blood pressure, coronary artery disease, peripheral vascular disease, high cholesterol, heart failure, or valve problems?
Have you had any procedures done to improve your heart function, such as ablation or stent placement? Have you ever had a heart attack or stroke? |
| Medications | Do you take any heart-related medications, herbs, or supplements to treat blood pressure, chest pain, high cholesterol, cardiac rhythm, fluid retention, or the prevention of clots? |
| Cardiac Risk Factors | Have your parents or siblings been diagnosed with any heart conditions?
Do you smoke or vape?
If you do not currently smoke, have you smoked in the past?
Are you physically active during the week?
What does a typical day look like in your diet?
Do you drink alcoholic drinks?
Would you say you experience stress in your life?
How many hours of sleep do you normally get each day?
|
Objective Assessment
The physical examination of the cardiovascular system involves the interpretation of vital signs, inspection, palpation, and auscultation of heart sounds as the nurse evaluates for sufficient perfusion and cardiac output.
For more information about assessing a patient’s oxygenation status as it relates to their cardiac output, visit the “Oxygenation” chapter in Open RN Nursing Fundamentals.
Equipment needed for a cardiovascular assessment includes a stethoscope, penlight, centimeter ruler or tape measure, and sphygmomanometer.[10]
Evaluate Vital Signs and Level of Consciousness
Interpret the blood pressure and pulse readings to verify the patient is stable before proceeding with the physical exam. Assess the level of consciousness; the patient should be alert and cooperative.
Inspection
- Skin color to assess perfusion. Inspect the face, lips, and fingertips for cyanosis or pallor. Cyanosis is a bluish discoloration of the skin, lips, and nail beds and indicates decreased perfusion and oxygenation. Pallor is the loss of color, or paleness of the skin or mucous membranes, as a result of reduced blood flow, oxygenation, or decreased number of red blood cells. Patients with light skin tones should be pink in color. For those with darker skin tones, assess for pallor on the palms, conjunctiva, or inner aspect of the lower lip.
- Jugular Vein Distension (JVD). Inspect the neck for JVD that occurs when the increased pressure of the superior vena cava causes the jugular vein to bulge, making it most visible on the right side of a person’s neck. JVD should not be present in the upright position or when the head of bed is at 30-45 degrees.
- Precordium for abnormalities. Inspect the chest area over the heart (also called precordium) for deformities, scars, or any abnormal pulsations the underlying cardiac chambers and great vessels may produce.
- Extremities:
- Upper Extremities: Inspect the fingers, arms, and hands bilaterally noting Color, Warmth, Movement, Sensation (CWMS). Alterations or bilateral inconsistency in CWMS may indicate underlying conditions or injury. Assess capillary refill by compressing the nail bed until it blanches and record the time taken for the color to return to the nail bed. Normal capillary refill is less than 3 seconds.[11]
- Lower Extremities: Inspect the toes, feet, and legs bilaterally, noting CWMS, capillary refill, and the presence of peripheral edema, superficial distended veins, and hair distribution. Document the location and size of any skin ulcers.
- Edema: Note any presence of edema. Peripheral edema is swelling that can be caused by infection, thrombosis, or venous insufficiency due to an accumulation of fluid in the tissues. (See Figure 9.6[12] for an image of pedal edema.)[13]
- Deep Vein Thrombosis (DVT): A deep vein thrombosis (DVT) is a blood clot that forms in a vein deep in the body. DVT requires emergency notification of the health care provider and immediate follow-up because of the risk of developing a life-threatening pulmonary embolism.[14] Inspect the lower extremities bilaterally. Assess for size, color, temperature, and for presence of pain in the calves. Unilateral warmth, redness, tenderness, swelling in the calf, or sudden onset of intense, sharp muscle pain that increases with dorsiflexion of the foot is an indication of a deep vein thrombosis (DVT).[15] See Figure 9.7[16] for an image of a DVT in the patient’s right leg, indicated by unilateral redness and edema.


Auscultation
Heart Sounds
Auscultation is routinely performed over five specific areas of the heart to listen for corresponding valvular sounds. These auscultation sites are often referred to by the mnemonic “APE To Man,” referring to Aortic, Pulmonic, Erb’s point, Tricuspid, and Mitral areas (see Figure 9.8[17] for an illustration of cardiac auscultation areas). The aortic area is the second intercostal space to the right of the sternum. The pulmonic area is the second intercostal space to the left of the sternum. Erb’s point is directly below the pulmonic area and located at the third intercostal space to the left of the sternum. The tricuspid (or parasternal) area is at the fourth intercostal space to the left of the sternum. The mitral (also called apical or left ventricular area) is the fifth intercostal space at the midclavicular line.
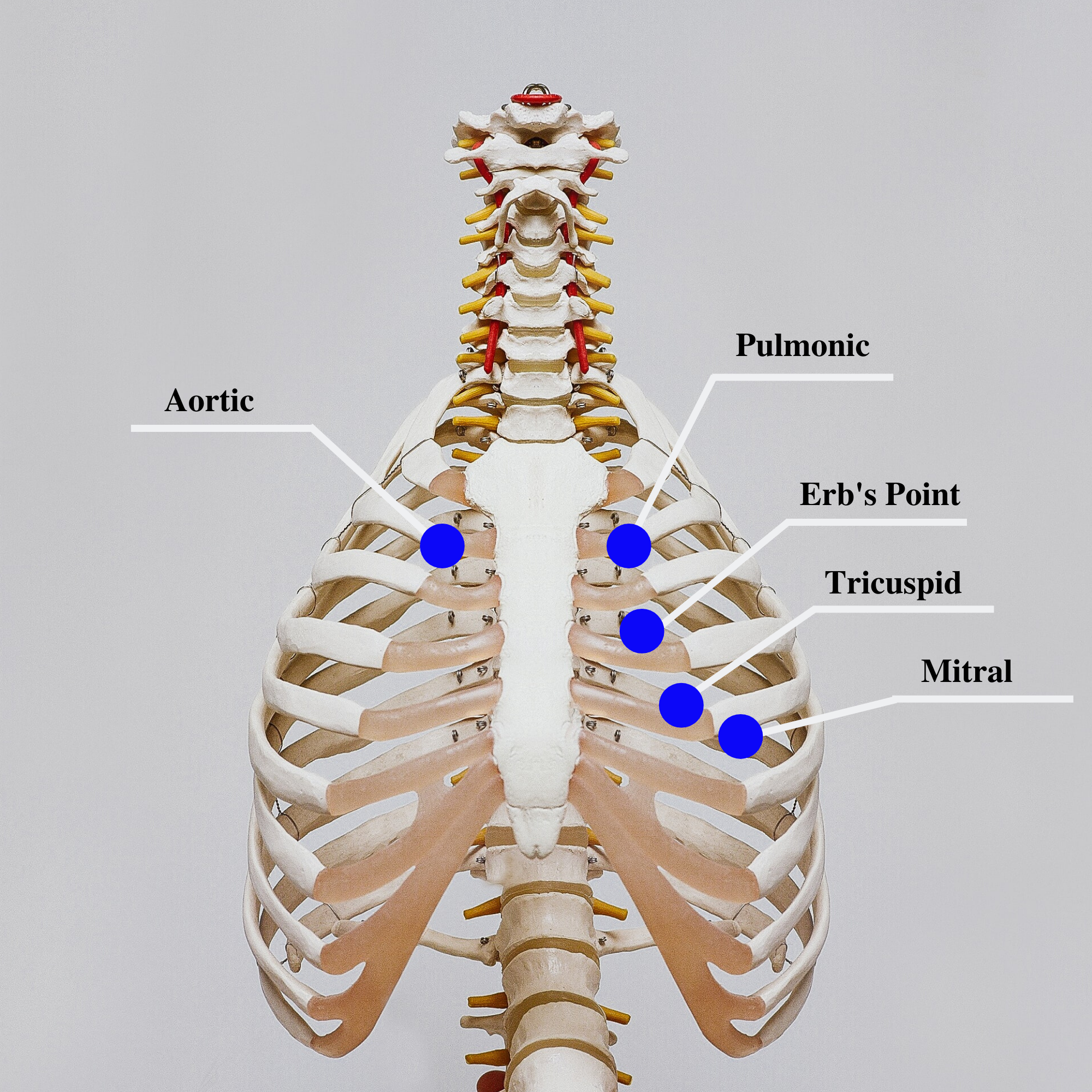
Auscultation usually begins at the aortic area (upper right sternal edge). Use the diaphragm of the stethoscope to carefully identify the S1 and S2 sounds. They will make a “lub-dub” sound. Note that when listening over the area of the aortic and pulmonic valves, the “dub” (S2) will sound louder than the “lub” (S1). Move the stethoscope sequentially to the pulmonic area (upper left sternal edge), Erb’s point (left third intercostal space at the sternal border), and tricuspid area (fourth intercostal space. When assessing the mitral area for female patients, it is often helpful to ask them to lift up their breast tissue so the stethoscope can be placed directly on the chest wall. Repeat this process with the bell of the stethoscope. The apical pulse should be counted over a 60-second period. For an adult, the heart rate should be between 60 and 100 with a regular rhythm to be considered within normal range. The apical pulse is an important assessment to obtain before the administration of many cardiac medications.
The first heart sound (S1) identifies the onset of systole, when the atrioventricular (AV) valves (mitral and tricuspid) close and the ventricles contract and eject the blood out of the heart. The second heart sound (S2) identifies the end of systole and the onset of diastole when the semilunar valves close, the AV valves open, and the ventricles fill with blood. S1 corresponds to the palpable pulse. When auscultating, it is important to identify the S1 (“lub”) and S2 (“dub”) sounds, evaluate the rate and rhythm of the heart, and listen for any extra heart sounds.
![]() Auscultating Heart Sounds
Auscultating Heart Sounds
- To effectively auscultate heart sounds, patient repositioning may be required. If it difficult to hear the heart sounds, ask the patient to lean forward if they are able, or lie on their left side. These positions move the heart closer to their chest wall and can increase the volume of the heart sounds heard on auscultation. This repositioning may be helpful in patients with increased adipose tissue in their chest wall or larger breasts.
- It is common to hear lung sounds when auscultating the heart sounds. It may be helpful to ask the patient to briefly hold their breath if lung sounds impede adequate heart auscultation. Limit the holding of breath to 10 seconds or as tolerated by the patient.
- Environmental noise can cause difficulty in auscultating heart sounds. Removing environmental noise by turning down the television volume or shutting the door may be required for an accurate assessment.
- Patients may try to talk to you as you are assessing their heart sounds. It is often helpful to explain the procedure such as, “I am going to take a few minutes to listen carefully to the sounds of blood flow going through your heart. Please try not to speak while I am listening, so I can hear the sounds better.”
Extra Heart Sounds
Extra heart sounds include clicks, murmurs, S3 and S4 sounds, and pleural friction rubs. These extra sounds can be difficult for a novice to distinguish, so if you notice any new or different sounds, consult an advanced practitioner or notify the provider. A midsystolic click, associated with mitral valve prolapse, may be heard with the diaphragm at the apex or left lower sternal border.
A click may be followed by a murmur. A murmur is a blowing or whooshing sound that signifies turbulent blood flow often caused by a valvular defect. New murmurs not previously recorded should be immediately communicated to the health care provider. In the aortic area, listen for possible murmurs of aortic stenosis and aortic regurgitation with the diaphragm of the stethoscope. In the pulmonic area, listen for potential murmurs of pulmonic stenosis and pulmonary and aortic regurgitation. In the tricuspid area, at the fourth and fifth intercostal spaces along the left sternal border, listen for the potential murmurs of tricuspid regurgitation, tricuspid stenosis, or ventricular septal defect.
S3 and S4 sounds, if present, are often heard best by asking the patient to lie on their left side and listening over the apex with the bell of the stethoscope. An S3 sound, also called a ventricular gallop, occurs after the S2 and sounds like “lub-dub-dah,” or a sound similar to a horse galloping. An S3 can occur when a patient is experiencing fluid overload, such as during an acute exacerbation of heart failure.[18] It can also be a normal finding in pregnancy due to increased blood flow through the ventricles.
The S4 sound, also called atrial gallop, occurs immediately before the S1 and sounds like “ta-lub-dub.” An S4 sound can occur with decreased ventricular compliance or coronary artery disease.[19]
A pericardial friction rub is caused by inflammation of the pericardium, with a creaky-scratchy noise generated as the parietal and visceral membranes rub together. It is best heard at the apex or left lower sternal border with the diaphragm as the patient sits up, leans forward, and holds their breath.
Carotid Sounds
The carotid artery may be auscultated for bruits. Bruits are a swishing sound due to turbulence in the blood vessel and may be heard due to atherosclerotic changes.
Palpation
Palpation is used to evaluate peripheral pulses, capillary refill, and for the presence of edema. When palpating these areas, also pay attention to the temperature and moisture of the skin.
Pulses
Compare the rate, rhythm, and quality of arterial pulses bilaterally, including the carotid, radial, brachial, posterior tibialis, and dorsalis pedis pulses. Review additional information about obtaining pulses in the “General Survey” chapter. Bilateral comparison for all pulses (except the carotid) is important for determining subtle variations in pulse strength. Carotid pulses should be palpated on one side at a time to avoid decreasing perfusion of the brain. The posterior tibial artery is located just behind the medial malleolus. It can be palpated by scooping the patient’s heel in your hand and wrapping your fingers around so that the tips come to rest on the appropriate area just below the medial malleolus. The dorsalis pedis artery is located just lateral to the extensor tendon of the big toe and can be identified by asking the patient to flex their toe while you provide resistance to this movement. Gently place the tips of your second, third, and fourth fingers adjacent to the tendon, and try to feel the pulse.
The quality of the pulse is graded on a scale of 0 to 3, with 0 being absent pulses, 1 being decreased pulses, 2 is within normal range, and 3 being increased (also referred to as “bounding”). If unable to palpate a pulse, additional assessment is needed. First, determine if this is a new or chronic finding. Second, if available, use a Doppler ultrasound to determine the presence or absence of the pulse. Many agencies use Doppler ultrasound to document if a nonpalpable pulse is present. If the pulse is not found, this could be a sign of an emergent condition requiring immediate follow-up and provider notification. See Figures 9.9[20] and 9.10[21] for images of assessing pedal pulses.


Capillary Refill
The capillary refill test is performed on the nail beds to monitor perfusion, the amount of blood flow to tissue. Pressure is applied to a fingernail or toenail until it pales, indicating that the blood has been forced from the tissue under the nail. This paleness is called blanching. Once the tissue has blanched, pressure is removed. Capillary refill time is defined as the time it takes for the color to return after pressure is removed. If there is sufficient blood flow to the area, a pink color should return within 2 seconds after the pressure is removed.[22]
Review of Capillary Refill Test on YouTube[23].
Edema
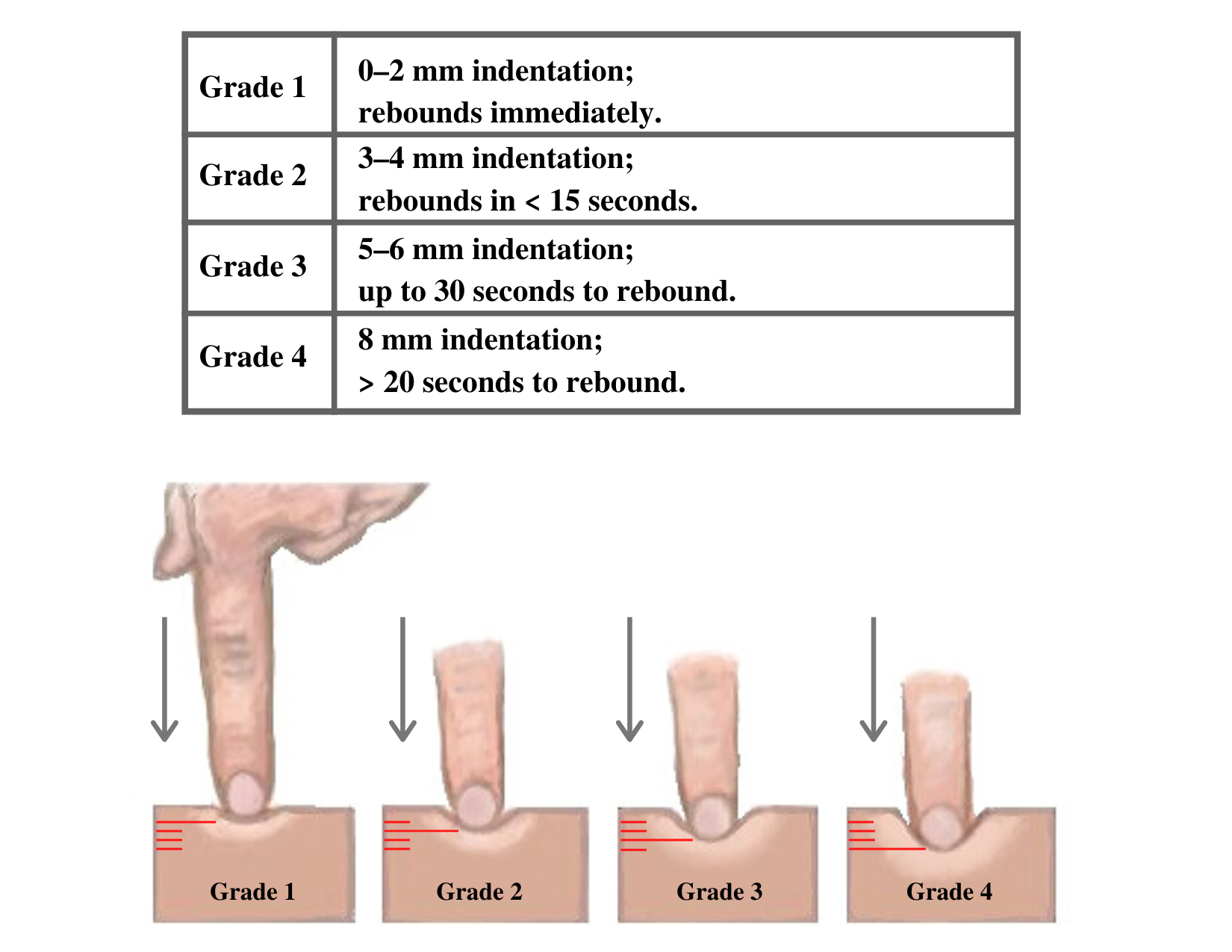
Edema occurs when one can visualize visible swelling caused by a buildup of fluid within the tissues. If edema is present on inspection, palpate the area to determine if the edema is pitting or nonpitting. Press on the skin to assess for indentation, ideally over a bony structure, such as the tibia. If no indentation occurs, it is referred to as nonpitting edema. If indentation occurs, it is referred to as pitting edema. See Figure 9.11[24] for images demonstrating pitting edema.

Note the depth of the indention and how long it takes for the skin to rebound back to its original position. The indentation and time required to rebound to the original position are graded on a scale from 1 to 4. Edema rated at 1+ indicates a barely detectable depression with immediate rebound, and 4+ indicates a deep depression with a time lapse of over 20 seconds required to rebound. See Figure 9.12[25] for an illustration of grading edema. Additionally, it is helpful to note edema may be difficult to observe in larger patients. It is also important to monitor for sudden changes in weight, which is considered a probable sign of fluid volume overload.
Heaves or Thrills
You may observe advanced practice nurses and other health care providers palpating the anterior chest wall to detect any abnormal pulsations the underlying cardiac chambers and great vessels may produce. Precordial movements should be evaluated at the apex (mitral area). It is best to examine the precordium with the patient supine because if the patient is turned on the left side, the apical region of the heart is displaced against the lateral chest wall, distorting the chest movements.[26] A heave or lift is a palpable lifting sensation under the sternum and anterior chest wall to the left of the sternum that suggests severe right ventricular hypertrophy. A thrill is a vibration felt on the skin of the precordium or over an area of turbulence, such as an arteriovenous fistula or graft.
Life Span Considerations
The cardiovascular assessment and expected findings should be modified according to common variations across the life span.
Infants and Children
A murmur may be heard in a newborn in the first few days of life until the ductus arteriosus closes.
When assessing the cardiovascular system in children, it is important to assess the apical pulse. Parameters for expected findings vary according to age group. After a child reaches adolescence, a radial pulse may be assessed. Table 9.3c outlines the expected apical pulse rate by age.
Table 9.3c Expected Apical Pulse by Age
| Age Group | Heart Rate |
|---|---|
| Preterm | 120-180 |
| Newborn (0 to 1 month) | 100-160 |
| Infant (1 to 12 months) | 80-140 |
| Toddler (1 to 3 years) | 80-130 |
| Preschool (3 to 5 years) | 80-110 |
| School Age (6 to 12 years) | 70-100 |
| Adolescents (13 to 18 years) | 60-90 |
Older Adults
In adults over age 65, irregular heart rhythms and extra sounds are more likely. An “irregularly irregular” rhythm suggests atrial fibrillation, and further investigation is required if this is a new finding. See the box below for more information about atrial fibrillation.
For more information on atrial fibrillation, visit the CDC Atrial Fibrillation webpage.
Expected Versus Unexpected Findings
After completing a cardiovascular assessment, it is important for the nurse to use critical thinking to determine if any findings require follow-up. Depending on the urgency of the findings, follow-up can range from calling the health care provider to calling the rapid response team. Table 9.3d compares examples of expected findings, meaning those considered within normal limits, to unexpected findings, which require follow-up. Critical conditions are those that should be reported immediately and may require notification of a rapid response team.
Table 9.3d Expected Versus Unexpected Findings on Cardiac Assessment
| Assessment | Expected Findings | Unexpected Findings (Document and notify the provider if this is a new finding*) |
|---|---|---|
| Inspection | Apical impulse may or may not be visible | Scars not previously documented that could indicate prior cardiac surgeries
Heave or lift observed in the precordium Chest anatomy malformations |
| Palpation | Apical pulse felt over midclavicular fifth intercostal space | Apical pulse felt to the left of the midclavicular fifth intercostal space
Additional movements over precordium such as a heave, lift, or thrill |
| Auscultation | S1 and S2 heart sounds in a regular rhythm | New irregular heart rhythm
Extra heart sounds such as a murmur, S3, or S4 |
| *CRITICAL CONDITIONS to report immediately | Symptomatic tachycardia at rest (HR>100 bpm)
Symptomatic bradycardia (HR<60 bpm) New systolic blood pressure (<100 mmHg) Orthostatic blood pressure changes (see “Blood Pressure” chapter for more information) New irregular heart rhythm New extra heart sounds such as a murmur, S3, or S4 New abnormal cardiac rhythm changes Reported chest pain, calf pain, or worsening shortness of breath |
See Table 9.3e for a comparison of expected versus unexpected findings when assessing the peripheral vascular system.
Table 9.3e Expected Versus Unexpected Peripheral Vascular Assessment Findings
| Assessment | Expected Findings | Unexpected Findings (Document or notify provider if new finding*) |
|---|---|---|
| Inspection | Skin color uniform and appropriate for race bilaterally
Equal hair distribution on upper and lower extremities Absence of jugular vein distention (JVD) Absence of edema Sensation and movement of fingers and toes intact |
Cyanosis or pallor, indicating decreased perfusion
Decreased or unequal hair distribution Presence of jugular vein distention (JVD) in an upright position or when head of bed is 30-45 degrees New or worsening edema Rapid and unexplained weight gain Impaired movement or sensation of fingers and toes |
| Palpation | Skin warm and dry
Pulses present and equal bilaterally Absence of edema Capillary refill less than 2 seconds |
Skin cool, excessively warm, or diaphoretic
Absent, weak/thready, or bounding pulses New irregular pulse New or worsening edema Capillary refill greater than 2 seconds Unilateral warmth, redness, tenderness, or edema, indicating possible deep vein thrombosis (DVT) |
| Auscultation | Carotid pulse | Carotid bruit |
| *CRITICAL CONDITIONS to report immediately | Cyanosis
Absent pulse (and not heard using Doppler device) Capillary refill time greater than 3 seconds Unilateral redness, warmth, and edema, indicating a possible deep vein thrombosis (DVT) |
“Sternum_composition.png” by Anatomography is licensed under CC BY-SA 2.1 Japan
“Sternum_composition.png” by Anatomography is licensed under CC BY-SA 2.1 Japan
- "Diagram of the human heart” by Wapcaplet is licensed under CC BY-SA 3.0 ↵
- "Diagram of the human heart” by Wapcaplet is licensed under CC BY-SA 3.0 ↵
- “2018 Conduction System of Heart.jpg” by OpenStax is licensed under CC-BY-3.0 ↵
- “Arterial System en.svg” by LadyofHats, Mariana Ruiz Villarreal is in the Public Domain. ↵
- “Venous system en.svg” by Lady of Hats Mariana Ruiz Vilarreal is in the Public Domain. ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology licensed under CC BY 4.0 ↵
- Felner, J. M. (1990). An overview of the cardiovascular system. In Walker, H. K., Hall, W. D., & Hurst, J. W. (Eds.), Clinical methods: The history, physical, and laboratory examinations (3rd ed., Chapter 7). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK393/ ↵
- Scott, C., & MacInnes, J. D. (2013, September 27). Cardiac patient assessment: putting the patient first. British Journal of Nursing, 15(9). https://doi.org/10.12968/bjon.2006.15.9.21091 ↵
- Scott, C., & MacInnes, J. D. (2013, September 27). Cardiac patient assessment: putting the patient first. British Journal of Nursing, 15(9). https://doi.org/10.12968/bjon.2006.15.9.21091 ↵
- Felner, J. M. (1990). An overview of the cardiovascular system. In Walker, H. K., Hall, W. D., & Hurst, J. W. (Eds.), Clinical methods: The history, physical, and laboratory examinations (3rd ed., Chapter 7). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK393/ ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology licensed under CC BY 4.0 ↵
- “Swollen feet at Harefield Hospital edema.jpg” by Ryaninuk is licensed under CC BY-SA 4.0 ↵
- Simon, E. C. (2014). Leg edema assessment and management. MEDSURG Nursing, 23(1), 44-53. ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology licensed under CC BY 4.0 ↵
- “Deep vein thrombosis of the right leg.jpg” by James Heilman, MD is licensed under CC BY-SA 3.0 ↵
- “Cardiac Auscultation Areas” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- Shono, A., Mori, S., Yatomi, A., Kamio, T., Sakai, J., Soga, F., Tanaka, H., & Hirata, K. I. (2019). Ultimate third heart sound. Internal Medicine, 58(17), 2535–2538. https://doi.org/10.2169/internalmedicine.2731-19 ↵
- Felner, J. M. (1990). An overview of the cardiovascular system. In Walker, H. K., Hall, W. D., & Hurst, J. W. (Eds.), Clinical methods: The history, physical, and laboratory examinations (3rd ed., Chapter 7). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK393/ ↵
- “DSC_2277.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/2-5-focussed-respiratory-assessment/ ↵
- “DSC_2314.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/2-5-focussed-respiratory-assessment/ ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Capillary nail refill test; [updated 2020, Aug 9] https://medlineplus.gov/ency/article/003394.htm ↵
- RegisteredNurseRN. (2022, March 21). Capillary Refill Time Test: Normal vs. Abnormal - Nursing Clincial Skills. [Video]. YouTube. Used with permission. All rights reserved. https://youtu.be/EwaDSZRH1LE ↵
- “Combinpedal.jpg” by James Heilman, MD is licensed under CC BY-SA 3.0 ↵
- “Grading of Edema” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- Felner, J. M. (1990). An overview of the cardiovascular system. In Walker, H. K., Hall, W. D., & Hurst, J. W. (Eds.), Clinical methods: The history, physical, and laboratory examinations (3rd ed., Chapter 7). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK393/ ↵
“Prevent residents from falling” is one of the National Patient Safety Goals for nursing care centers. Client falls, whether in the nursing care center, home, or hospital, are very common and can cause serious injury and death. Older adults have the highest risk of falling. Each year, 3 million older people are treated in emergency departments for fall injuries, and over 800,000 clients a year are hospitalized because of a head injury or hip fracture resulting from a fall. Many older adults who fall, even if they’re not injured, become afraid of falling. This fear may cause them to limit their everyday activities. However, when a person is less active, they become weaker, which further increases their chances of falling.[1]
Many conditions contribute to client falls, including the following:[2]
- Lower body weakness
- Vitamin D deficiency
- Difficulties with walking and balance
- Medications, such as tranquilizers, sedatives, antihypertensives, or antidepressants
- Vision problems
- Foot pain or poor footwear
- Environmental hazards, such as throw rugs or clutter that can cause tripping
Most falls are caused by a combination of risk factors. The more risk factors a person has, the greater their chances of falling. Many risk factors can be changed or modified to help prevent falls.
The Centers for Disease Control has developed a program called “STEADI - Stopping Elderly Accidents, Deaths & Injuries” to help reduce the risk of older adults from falling at home. Three screening questions to determine risk for falls are as follows:
- Do you feel unsteady when standing or walking?
- Do you have worries about falling?
- Have you fallen in the past year? If yes, how many times? Were you injured?
If the individual answers “Yes” to any of these questions, further assessment of risk factors is performed.[3]
Read more information about preventing falls in older adults at CDC's Older Adult Fall Prevention.
Fall Assessment Tools
By virtue of being ill, all hospitalized clients are at risk for falls, but some clients are at higher risk than others. Assessment is an ongoing process with the goal of identifying a client’s specific risk factors and implementing interventions in their care plan to decrease their risk of falling. Commonly used fall assessment tools used to identify clients at high risk for falls are the Morse Fall Scale, the Hendrich II Fall Risk Model, and the Hester Davis Scale for fall risk assessment. Read more about these fall risk assessment tools using the hyperlinks provided below. Key risk factors for falls in hospitalized clients are as follows:[4]
- History of falls: All clients with a recent history of falls, such as a fall in the past three months, should be considered at higher risk for future falls.
- Mobility problems and use of assistive devices: Clients who have problems with their gait or require an assistive device (such as a cane or a walker) for mobility are more likely to fall.
- Medications: Clients taking several prescription medications or those taking medications that could cause sedation, confusion, impaired balance, or orthostatic blood pressure changes are at higher risk for falls.
- Mental status: Clients with delirium, dementia, or psychosis may be agitated and confused, putting them at risk for falls.
- Incontinence: Clients who have urinary frequency or who have frequent toileting needs are at higher fall risk.
- Equipment: Clients who are tethered to equipment such as an IV pole or a Foley catheter are at higher risk of tripping.
- Impaired vision: Clients with impaired vision or those who require glasses but who are not wearing them are at a higher fall risk because of their decreased recognition of an environmental hazard.
- Orthostatic hypotension: Clients whose blood pressure drops upon standing often experience light-headedness or dizziness that can cause falls.[5]
View these common fall risk assessment tools:
Interventions to Prevent Falls
Universal fall precautions are established for all clients to reduce their risk for falling. In addition to universal fall precautions, a care plan is created based on the client's fall risk assessment findings to address their specific risks and needs.
Universal Fall Precautions
Falls are the most commonly reported client safety incidents in the acute care setting. Hospitals pose an inherent fall risk due to the unfamiliarity of the environment and various hazards in the hospital room that pose a risk. During inpatient care, nurses assess their clients’ risk for falling during every shift and implement interventions to reduce the risk of falling. Universal fall precautions have been developed that apply to all clients all the time. Universal fall precautions are called "universal" because they apply to all clients, regardless of fall risk, and revolve around keeping the client's environment safe and comfortable.[8]
Universal fall precautions include the following:
- Familiarize the client with the environment.
- Have the client demonstrate call light use.
- Maintain the call light within reach. See Figure 5.5[9] for an image of a call light.
- Keep the client's personal possessions within safe reach.
- Have sturdy handrails in client bathrooms, rooms, and hallways.
- Place the hospital bed in the low position when a client is resting. Raise the bed to a comfortable height when the client is transferring out of bed.
- Keep the hospital bed brakes locked.
- Keep wheelchair wheels in a "locked" position when stationary.
- Keep no-slip, comfortable, and well-fitting footwear on the client.
- Use night lights or supplemental lighting.
- Keep floor surfaces clean and dry. Clean up all spills promptly.
- Keep client care areas uncluttered.
- Follow safe client handling practices.[10]

Interventions Based on Risk Factors
Clients at elevated risk for falling require multiple, individualized interventions, in addition to universal fall precautions. There are many interventions available to prevent falls and fall-related injuries based on the client's specific risk factors. See Table 5.6a for interventions categorized by risk factor.[11]
Table 5.6a Interventions Based on Fall Risk Factors
| Risk Factor | Interventions |
|---|---|
| Altered Mental Status | Clients with new altered mental status should be assessed for delirium and treated by a trained nurse or physician. See a tool for assessing delirium below. For cognitively impaired clients who are agitated or trying to wander, more intense supervision (e.g., sitter or checks every 15 minutes) may be needed. Some hospitals implement designated safety zones that include low beds, mats for each side of the bed, nightlight, gait belt, and a "STOP" sign to remind clients not to get up. |
| Impaired Gait or Mobility | Clients with impaired gait or mobility will need assistance with mobility during their hospital stay. All clients should have any needed assistive devices, such as canes or walkers, in good repair at the bedside and within safe reach. If clients bring their assistive devices from home, staff should make sure these devices are safe for use in the hospital environment. Even with assistive devices, clients often need staff assistance when transferring out of bed or walking. Use a gait belt when assisting clients to transfer or ambulate per agency policy. |
| Frequent Toileting Needs | Clients with frequent toileting needs should be taken to the toilet on a regular basis via a scheduled rounding protocol. Read more about scheduled rounding in the following subsection. |
| Visual Impairment | Clients with visual impairment should have clean corrective lenses easily within reach and applied when walking. |
| High-Risk Medications (medicines that could cause sedation, confusion, impaired balance, orthostatic blood pressure changes, or cause frequent urination) | Clients on high-risk medications should have their medications reviewed by a pharmacist with fall risk in mind and recommendations made to the prescribing provider for discontinuation, substitution, or dose adjustment when possible. If a pharmacist is not immediately available, the prescribing provider should carry out a medication review. See Table 5.6b for a tool to review medications for fall risk. Clients on medications that cause orthostatic hypotension should have their orthostatic blood pressure routinely checked and reported. The client and their caregivers should be educated about fall risk and steps to prevent falls when the client is taking these medications. |
| Frequent Falls | Clients with a history of frequent falls should have their risk for injury assessed, including checking for a history of osteoporosis and use of aspirin and anticoagulants. |
Scheduled Hourly Rounding
Scheduled hourly rounds are scheduled hourly visits to each client’s room to integrate fall prevention activities with client care. Scheduled hourly rounds have been found to greatly decrease the incidence of falls because the client's needs are proactively met, reducing the motivation for the client to get out of bed unassisted. See the box below for a list of activities to complete during hourly rounds. These activities can be completed by unlicensed assistive personnel, nurses, or nurse managers.[12]
Hourly Rounding Protocol[13]
- Assess client pain levels using a pain-assessment scale. (If staff other than a nurse is doing the rounding and the client is in pain, contact the nurse immediately so the client does not have to use the call light for pain medication.)
- Put pain medication that is ordered “as needed” on an RN’s task list and offer the dose when it is due.
- Offer toileting assistance.
- Ensure the client is using correct footwear (e.g., specific shoes/slippers, no-skid socks).
- Check that the bed is in the locked position.
- Place the hospital bed in a low position when the client is resting; ask if the client needs to be repositioned and is comfortable.
- Make sure the call light/call bell button is within the client’s reach and the client can demonstrate accurate use.
- Put the telephone within the client’s reach.
- Put the TV remote control and bed light switch within the client’s reach.
- Put the bedside table next to the bed or across the bed.
- Put the tissue box and water within the client’s reach.
- Put the garbage can next to the bed.
- Prior to leaving the room, ask, “Is there anything I can do for you before I leave?"
- Tell the client that a member of the nursing staff (use names on whiteboard) will be back in the room in an hour to round again.
Medications Causing Elevated Risk for Falls
Evaluate medication-related fall risk for clients on admission and at regular intervals thereafter. Add up the point value (risk level) in Table 5.6b for every medication the client is taking. If the client is taking more than one medication in a particular risk category, the score should be calculated by (risk level score) x (number of medications in that risk level category). For a client at risk, a pharmacist should review the client’s list of medications and determine if medications may be tapered, discontinued, or changed to a safer alternative.[14]
Table 5.6b Medications Causing High Risk for Falls[15]
| Point Value (Risk Level) | Medication Class | Fall Risks |
|---|---|---|
| 3 (High) | Antipsychotics, anticonvulsants, and benzodiazepines | Sedation, dizziness, postural disturbances, altered gait and balance, and impaired cognition |
| 2 (Medium) | Antihypertensives, cardiac drugs, antiarrhythmics, and antidepressants | Induced orthostasis, impaired cerebral perfusion, and poor health status |
| 1 (Low) | Diuretics | Increased ambulation and induced orthostasis |
| Score ≥ 6 | Elevated risk for falls; ask pharmacist or prescribing provider to evaluate medications for possible modification to reduce risk |
View tools used to assess delirium and confusion in the Delirium Evaluation Bundle shared by the Agency for Healthcare Research and Quality.
Planning is the fourth step of the nursing process (and the fourth Standard of Practice by the American Nurses Association). This standard is defined as, "The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes." The RN develops an individualized, holistic, evidence-based plan in partnership with the health care consumer, family, significant others, and interprofessional team. Elements of the plan are prioritized for client safety and optimal client outcomes. The plan is modified according to the ongoing assessment of the health care consumer's response and other indicators. The plan is documented using standardized language or terminology.[16]
After expected outcomes are identified, the nurse begins planning nursing interventions to implement. Nursing interventions are evidence-based actions that the nurse performs to achieve client outcomes. Just as a provider makes medical diagnoses and writes prescriptions to improve the client's medical condition, a nurse formulates nursing diagnoses and plans nursing interventions to resolve client problems. Nursing interventions should focus on eliminating or reducing the related factors (etiology) of the nursing diagnoses when possible.[17] Nursing interventions, goals, and expected outcomes are written in the nursing care plan for continuity of care across shifts, nurses, and health professionals. Planning is outside the scope of practice for LPN/VNs, although they may assist in performing planned interventions during the Implementation phase according to their scope of practice. Refer to Figure 4.9a in the "Outcome Identification" section for a illustration of how the Planning phase of the nursing process correlates to NCSBN's Clinical Judgment Measurement Model.
Planning Nursing Interventions
You might be asking yourself, “How do I know what evidence-based nursing interventions to include in the nursing care plan?” There are several sources that nurses and nursing students can use to select nursing interventions. Many agencies have care planning tools and references included in the electronic health record that are easily documented in the client chart. Nurses can also refer to other care planning books or sources such as the Nursing Interventions Classification (NIC) system. Based on research and input from the nursing profession, NIC categorizes and describes nursing interventions that are regularly evaluated and updated. Interventions included in NIC are considered evidence-based nursing practices. The RN is responsible for using clinical judgment to make decisions about which interventions are best suited to meet an individualized client’s needs.[18]
Direct and Indirect Care
Nursing interventions are considered direct care or indirect care. Direct care refers to interventions that are carried out by having personal contact with clients. Examples of direct care interventions are wound care, repositioning, and ambulation. Indirect care interventions are performed when the nurse provides assistance in a setting other than with the client. Examples of indirect care interventions are attending care conferences, documenting, and communicating about client care with other providers.
Classification of Nursing Interventions
There are three types of nursing interventions: independent, dependent, and collaborative. (See Figure 4.12[19] for an image of a nurse collaborating with the health care team when planning interventions.)

Independent Nursing Interventions
Any intervention that the nurse can independently provide without obtaining a prescription or consulting another member of the health care team is considered an independent nursing intervention. An example of an independent nursing intervention is when the nurse monitors the client’s 24-hour intake/output record for trends because of a risk for imbalanced fluid volume. Another example of independent nursing interventions is the therapeutic communication that a nurse uses to assist clients to cope with a new medical diagnosis.
Example of an Independent Nursing Intervention
Refer to Scenario C in the "Assessment" section of this chapter. Ms. J. was diagnosed with Excess Fluid Volume. An example of an evidence-based independent nursing intervention is, “The nurse will reposition the client with dependent edema frequently, as appropriate.”[20] The nurse would individualize this evidence-based intervention to the client and include agency policy by stating, “The nurse will reposition the client every two hours.”
Dependent Nursing Interventions
Dependent nursing interventions require a prescription or order before they can be performed. Prescriptions are interventions specifically related to medication as directed by an authorized primary health care provider. An order is an intervention, remedy, or treatment as directed by an authorized primary health care provider.[21] A primary health care provider is a member of the health care team (usually a physician, advanced practice nurse, or physician’s assistant) who is licensed and authorized to formulate prescriptions on behalf of the client. For example, administering medication is a dependent nursing intervention. The nurse incorporates dependent interventions into the client's overall care plan by associating each intervention with the appropriate nursing diagnosis.
Example of a Dependent Nursing Intervention
Refer to Scenario C in the "Assessment" section of this chapter. Ms. J. was diagnosed with Excess Fluid Volume. An example of a dependent nursing intervention is, “The nurse will administer scheduled diuretics as prescribed.”
Collaborative Nursing Interventions
Collaborative nursing interventions are actions that the nurse carries out in collaboration with other health team members, such as physicians, social workers, respiratory therapists, physical therapists, and occupational therapists. These actions are developed in consultation with other health care professionals and incorporate their professional viewpoint.[22]
Example of a Collaborative Nursing Intervention
Refer to Scenario C in the "Assessment" section of this chapter. Ms. J. was diagnosed with Excess Fluid Volume. An example of a collaborative nursing intervention is the nurse consulting with a respiratory therapist when the client has deteriorating oxygen saturation levels. The respiratory therapist plans oxygen therapy and obtains a prescription from the provider. The nurse would document “The nurse will manage oxygen therapy in collaboration with the respiratory therapist" in the care plan.
Individualization of Interventions
It is vital for the planned interventions to be individualized to the client to be successful. For example, adding prune juice to the breakfast meal of a client with constipation will only work if the client likes to drink the prune juice. If the client does not like prune juice, then this intervention should not be included in the care plan. Collaboration with the client, family members, significant others, and the interprofessional team is essential for selecting effective interventions. There is not a set number of interventions required to be included in a nursing care plan, but instead, the number of quality individualized interventions is based on what is required to meet the specific, identified outcomes established for that client.
Creating Nursing Care Plans
Nursing care plans are created by registered nurses (RNs). Documentation of individualized nursing care plans are legally required in long-term care facilities by the Centers for Medicare and Medicaid Services (CMS) and in hospitals by The Joint Commission. CMS guidelines state, “Residents and their representative(s) must be afforded the opportunity to participate in their care planning process and to be included in decisions and changes in care, treatment, and/or interventions. This applies both to initial decisions about care and treatment, as well as the refusal of care or treatment. Facility staff must support and encourage participation in the care planning process. This may include ensuring that residents, families, or representatives understand the comprehensive care planning process, holding care planning meetings at the time of day when a resident is functioning at their best and client representatives can be present, providing sufficient notice in advance of the meeting, scheduling these meetings to accommodate a resident’s representative (such as conducting the meeting in-person, via a conference call, or video conferencing), and planning enough time for information exchange and decision-making. A resident has the right to select or refuse specific treatment options before the care plan is instituted.”[23] The Joint Commission conceptualizes the care planning process as the structuring framework for coordinating communication that will result in safe and effective care.[24]
Many facilities have established standardized nursing care plans with lists of possible interventions that can be customized for each specific client. Other facilities require the nurse to develop each care plan independently. Whatever the format, nursing care plans should be individualized to meet the specific and unique needs of each client. See Figure 4.13[25] for an image of a standardized care plan.

Nursing care plans created in nursing school can also be in various formats such as concept maps or tables. Some are fun and creative, while others are more formal. Appendix B contains a template that can be used for creating nursing care plans.
Implementation is the fifth step of the nursing process (and the fifth Standard of Practice by the American Nurses Association). This standard is defined as, "The registered nurse implements the identified plan." The RN may delegate planned interventions after considering the circumstance, person, task, communication, supervision, and evaluation, as well as the state Nurse Practice Act, federal regulation, and agency policy.[26]
Implementation of interventions requires the RN to use critical thinking and clinical judgment. After the initial plan of care is developed, continual reassessment of the client is necessary to detect any changes in the client’s condition requiring modification of the plan. The need for continual client reassessment underscores the dynamic nature of the nursing process and is crucial to providing safe care.
During the implementation phase of the nursing process, the nurse prioritizes planned interventions, assesses client safety while implementing interventions, delegates interventions as appropriate, and documents interventions performed. LPN/VNs have an active role in the Implementation phase, provided the interventions falls within the LPN/VN scope of practice. See Figure 4.14 for an illustration of how the Implementation phase of the nursing process correlates to NCSBN's Clinical Judgment Measurement Model.[27]
Prioritizing Implementation of Interventions
Prioritizing implementation of interventions follows a similar method as to prioritizing nursing diagnoses. Maslow’s Hierarchy of Needs and the ABCs of airway, breathing, and circulation are used to establish top priority interventions. When possible, least invasive actions are usually preferred due to the risk of injury from invasive options. Read more about methods for prioritization under the “Diagnosis” section of this chapter.
The potential impact on future events, especially if a task is not completed at a certain time, is also included when prioritizing nursing interventions. For example, if a client is scheduled to undergo a surgical procedure later in the day, the nurse prioritizes initiating a NPO (nothing by mouth) prescription prior to completing pre-op client education about the procedure. The rationale for this decision is that if the client eats food or drinks water, the surgery time will be delayed. Knowing and understanding the client's purpose for care, current situation, and expected outcomes are necessary to accurately prioritize interventions.
Client Safety
It is essential to consider client safety when implementing interventions. At times, clients may experience a change in condition that makes a planned nursing intervention or provider prescription no longer safe to implement. For example, an established nursing care plan for a client states, “The nurse will ambulate the client 100 feet three times daily.” However, during assessment this morning, the client reports feeling dizzy today, and their blood pressure is 90/60. Using critical thinking and clinical judgment, the nurse decides to not implement the planned intervention of ambulating the client. This decision and supporting assessment findings should be documented in the client’s chart and also communicated during the shift handoff report, along with appropriate notification of the provider of the client’s change in condition.
Implementing interventions goes far beyond implementing provider prescriptions and completing tasks identified on the nursing care plan and must focus on client safety. As frontline providers, nurses are in the position to stop errors before they reach the client.
In 2000 the Institute of Medicine (IOM) issued the historic, groundbreaking report titled To Err Is Human: Building a Safer Health System. The report stated that as many as 98,000 people die in U.S. hospitals each year as a result of preventable medical errors. To Err Is Human broke the silence that previously surrounded the consequences of medical errors and set a national agenda for reducing medical errors and improving client safety through the design of a safer health system.[28] In 2007 the IOM published a follow-up report titled Preventing Medication Errors and reported that more than 1.5 million Americans are injured every year in American hospitals, and the average hospitalized client experiences at least one medication error each day. This report emphasized actions that health care systems could take to improve medication safety.[29]
The Quality and Safety Education for Nurses (QSEN) project began in 2005 to assist in preparing future nurses to continuously improve the quality and safety of the health care systems in which they work. The vision of the QSEN project is to “inspire health care professionals to put quality and safety as core values to guide their work.”[30] Nurses and nursing students are expected to participate in quality improvement (QI) initiatives by identifying gaps where change is needed and assisting in implementing initiatives to resolve these gaps. Quality improvement is defined as, “The combined and unceasing efforts of everyone – health care professionals, clients and their families, researchers, payers, planners and educators – to make the changes that will lead to better client outcomes (health), better system performance (care), and better professional development (learning).”[31]
Delegation of Interventions
While implementing interventions, RNs may elect to delegate nursing tasks. Delegation is defined by the American Nurses Association as, “The assignment of the performance of activities or tasks related to client care to unlicensed assistive personnel or licensed practical nurses (LPNs) while retaining accountability for the outcome.”[32] RNs are accountable for determining the appropriateness of the delegated task according to the condition of the client and the circumstance; the communication provided to an appropriately trained LPN or UAP; the level of supervision provided; and the evaluation and documentation of the task completed. The RN must also be aware of the state Nurse Practice Act, federal regulations, and agency policy before delegating. The RN cannot delegate responsibilities requiring clinical judgment.[33] See the following box for information regarding legal requirements associated with delegation according to the Nurse Practice Act.
Delegation According to the Wisconsin Nurse Practice Act[34]
"During the supervision and direction of delegated acts a Registered Nurse shall do all of the following:
(a) Delegate tasks commensurate with educational preparation and demonstrated abilities of the person supervised.
(b) Provide direction and assistance to those supervised.
(c) Observe and monitor the activities of those supervised.
(d) Evaluate the effectiveness of acts performed under supervision.
The standard of practice for Licensed Practical Nurses in Wisconsin states, “In the performance of acts in basic patient situations, the LPN shall, under the general supervision of an RN or the direction of a provider:
(a) Accept only patient care assignments which the LPN is competent to perform.
(b) Provide basic nursing care. Basic nursing care is defined as care that can be performed following a defined nursing procedure with minimal modification in which the responses of the patient to the nursing care are predictable.
(c) Record nursing care given and report to the appropriate person changes in the condition of a patient.
(d) Consult with a provider in cases where an LPN knows or should know a delegated act may harm a patient.
(e) Perform the following other acts when applicable:
- Assist with the collection of data.
- Assist with the development and revision of a nursing care plan.
- Reinforce the teaching provided by an RN provider and provide basic health care instruction.
- Participate with other health team members in meeting basic patient needs.”
Read additional details about the scope of practice of registered nurses (RNs) and licensed practical nurses (LPNs) in Wisconsin's Nurse Practice Act in Chapter N 6 Standards of Practice.
Read more about the American Nurses Association's Principles for Delegation.
Table 4.7 outlines general guidelines for delegating nursing tasks in the state of Wisconsin according to the role of the health care team member.
Table 4.7 General Guidelines for Delegating Nursing Tasks
| RN | LPN | CNA | |
|---|---|---|---|
| Assessment | Complete client assessment | Assist with the collection of data for stable clients | Collect measurements such as weight, input/output, and vital signs in stable clients |
| Diagnosis | Analyze assessment data and create nursing diagnoses | Not applicable | Not applicable |
| Outcome Identification | Identify SMART client outcomes | Not applicable | Not applicable |
| Planning | Plan nursing interventions | Assist with the development of a nursing care plan | Not applicable |
| Implementation of Interventions | Implement independent, dependent, and collaborative nursing interventions; delegate interventions as appropriate, with supervision; document interventions performed | Participate with other health team members in meeting basic client needs and document interventions provided
Reinforce the teaching provided by an RN provider and provide basic health care instruction |
Implement and document delegated interventions associated with basic nursing care such as providing assistance in ambulating or tasks within their scope of practice |
| Evaluation | Evaluate the attainment of outcomes and revise the nursing care plan as needed | Contribute data regarding the achievement of client outcomes; assist in the revision of a nursing care plan | Not applicable |
Documentation of Interventions
As interventions are performed, they must be documented in the client’s record in a timely manner. As previously discussed in the “Ethical and Legal Issues” subsection of the “Basic Concepts” section, lack of documentation is considered a failure to communicate and a basis for legal action. A basic rule of thumb is if an intervention is not documented, it is considered not done in a court of law. It is also important to document administration of medication and other interventions in a timely manner to prevent errors that can occur due to delayed documentation time.
Coordination of Care and Health Teaching/Health Promotion
ANA's Standard of Professional Practice for Implementation also includes the standards 5A Coordination of Care and 5B Health Teaching and Health Promotion.[35] Coordination of Care includes competencies such as organizing the components of the plan, engaging the client in self-care to achieve goals, and advocating for the delivery of dignified and holistic care by the interprofessional team. Health Teaching and Health Promotion is defined as, “Employing strategies to teach and promote health and wellness.”[36] Client education is an important component of nursing care and should be included during every client encounter. For example, client education may include teaching about side effects while administering medications or teaching clients how to self-manage their conditions at home.
Putting It Together
See an example of implementation in the following box.
Example of Implementation
Refer to Scenario C in the "Assessment" section of this chapter. The nurse implemented the nursing care plan documented in Appendix C. Interventions related to breathing were prioritized. Administration of the diuretic medication was completed first, and lung sounds were monitored frequently for the remainder of the shift. Weighing the client before breakfast was delegated to the CNA. The client was educated about her medications and methods to use to reduce peripheral edema at home. All interventions were documented in the electronic medical record (EMR).
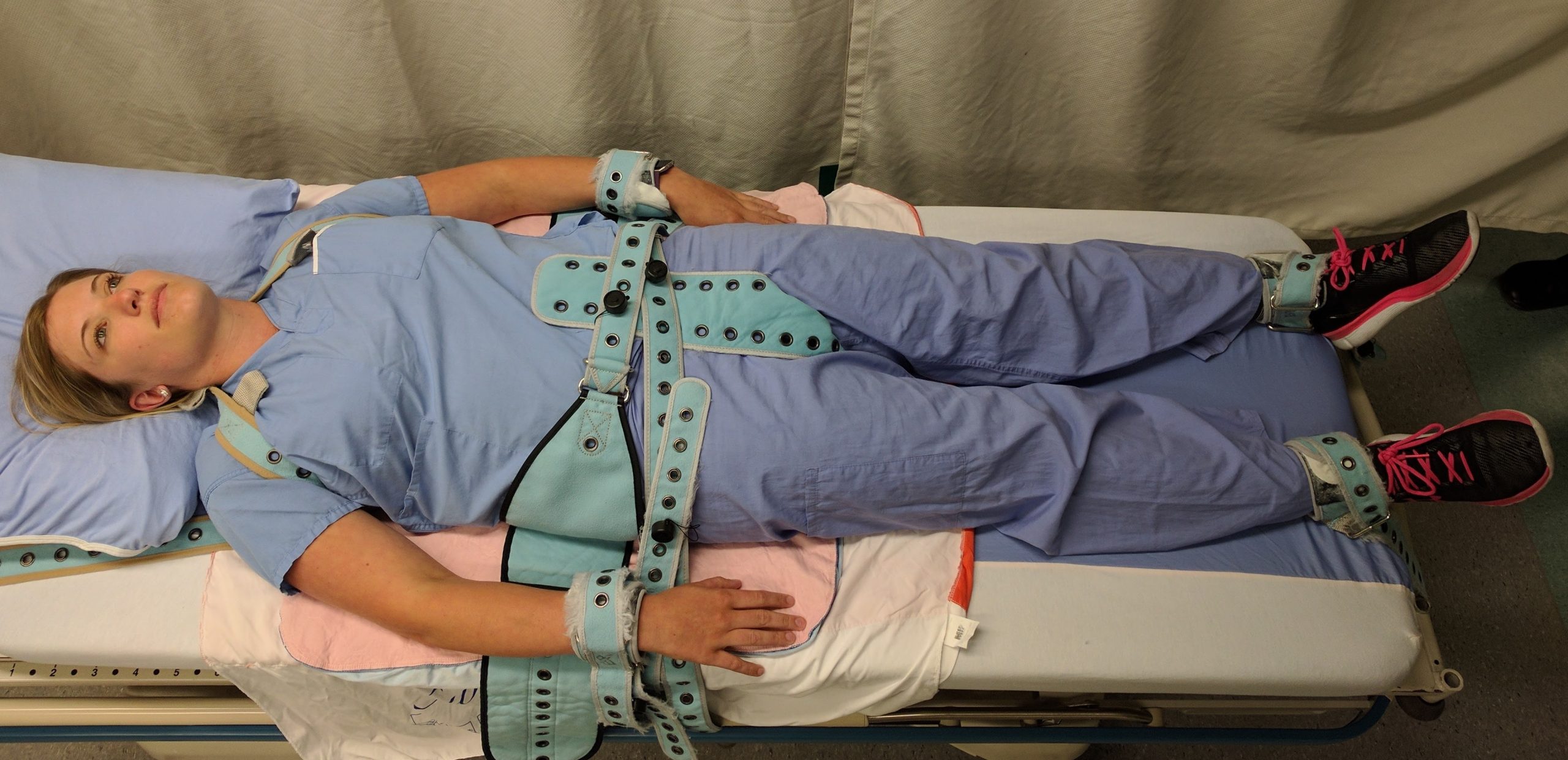
Definition of Restraints
Restraints are devices used in health care settings to prevent clients from causing harm to themselves or others when alternative interventions are not effective. A restraint is a device, method, or process that is used for the specific purpose of restricting a client’s freedom of movement without the permission of the person. See Figure 5.6[37] for an image of a simulated client with restraints applied.
Restraints include mechanical devices such as a tie wrist device, chemical restraints, or seclusion. The Joint Commission defines chemical restraint as a drug used to manage a client’s behavior, restrict the client’s freedom of movement, or impair the client’s ability to appropriately interact with their surroundings that is not standard treatment or dosage for the client’s condition. It is important to note that the definition states the medication “is not standard treatment or dosage for the client’s condition.”[38] Seclusion is defined as the confinement of a client in a locked room from which they cannot exit on their own. It is generally used as a method of discipline for behavior that can cause harm to themselves or others, or as a method of decreasing environmental stimulation. Seclusion limits freedom of movement because, although the client is not mechanically restrained, they cannot leave the area.
Although restraints are used with the intention to keep a client safe, they impact a client’s psychological safety and dignity and can cause additional safety issues and death. A restrained person has a natural tendency to struggle and try to remove the restraint and can fall or become fatally entangled in the restraint. Furthermore, immobility that results from the use of restraints can cause pressure injuries, contractures, and muscle loss. Restraints take a large emotional toll on the client’s self-esteem and may cause humiliation, fear, and anger.
Restraint Guidelines
The American Nurses Association (ANA) has established evidence-based guidelines that state a restraint-free environment is the standard of care. The ANA encourages the participation of nurses to reduce client restraints and seclusion in all health care settings. Restraining or secluding clients is viewed as contrary to the goals and ethical traditions of nursing because it violates the fundamental client rights of autonomy and dignity. However, the ANA also recognizes there are times when there is no viable option other than restraints to keep a client safe, such as during an acute psychotic episode when client and staff safety are in jeopardy due to aggression or assault. The ANA also states that restraints may be justified in some clients with severe dementia or delirium when they are at risk for serious injuries such as a hip fracture due to falling.
The ANA provides the following guidelines: “When restraint is necessary, documentation should be done by more than one witness. Once restrained, the client should be treated with humane care that preserves human dignity. In those instances where restraint, seclusion, or therapeutic holding is determined to be clinically appropriate and adequately justified, registered nurses who possess the necessary knowledge and skills to effectively manage the situation must be actively involved in the assessment, implementation, and evaluation of the selected emergency measure, adhering to federal regulations and the standards of The Joint Commission (2009) regarding appropriate use of restraints and seclusion.”[39] Nursing documentation typically includes information such as client behavior necessitating the restraint, alternatives to restraints that were attempted, the type of restraint used, the time it was applied, the location of the restraint, and client education regarding the restraint.
Medical Restraints
Restraints used to manage nonviolent, non-self-destructive behaviors are referred to as medical restraints. Medical restraints may be appropriate to manage behavior such as the client attempting to remove life-sustaining tubes, drains, IV catheters, urinary catheters, or endotracheal tubes. These types of restraints often include hand mitts or soft wrist restraints. Medical restraints may also be used for clients attempting to get out of bed and as such are a high risk for falls. These types of restraints include siderails, vest restraints, and roll belts. Each facility is required to have a policy in place for the use of medical restraints. Policies typically include requirements for documentation of the reason for the restraint, alternative measures tried, type of restraint applied, behavioral criteria for removal of restraint, range of motion and cares while in restraints, and the date and time the restraint is applied or removed. A medical restraint requires a registered nurse to apply or supervise application of the restraint, a new order every 24 hours, and may never be issued as an as needed order. If the primary care provider did not order the restraint, they should be notified as soon as possible. Medical restraints are more commonly encountered in the general hospital setting rather than behavioral restraints.[40],[41]
Behavioral Restraints
Restraints used to manage violent, self-destructive behaviors are referred to as behavioral restraints. Behavioral restraints are used when clients exhibit behaviors such as hitting or kicking staff or other clients, physically harming themselves or others, or threatening to do so. Behavioral restraints are used in emergency situations where safety concerns need to be immediately addressed to prevent harm. [42]
RNs need special training to apply behavioral restraints, including safe application of the restraint, maintaining personal safety, and techniques to de-escalate the violent or aggressive behavior. Behavioral restraints are typically used in mental health units, emergency departments, or critical care units. Similar to medical restraints, each agency must have a policy in place for the use of behavioral restraints. Health care facilities that accept Medicare and Medicaid reimbursement must also follow federal guidelines for the use of behavioral restraints that include the following:
Guidelines for the use of behavioral restraints include the following:
- When a restraint is the only viable option, it must be discontinued at the earliest possible time.
- Orders for the use of seclusion or restraint can never be written as a standing order or PRN (as needed).
- The treating physician must be consulted as soon as possible if the restraint or seclusion is not ordered by the client’s treating physician.
- A physician or licensed independent practitioner must see and evaluate the need for the restraint or seclusion within one hour after the initiation.
- After restraints have been applied, the nurse should follow agency policy for frequent monitoring and regularly changing the client's position to prevent complications. Nurses must also ensure the client's basic needs (i.e., hydration, nutrition, and toileting) are met. Some agencies require a 1:1 client sitter when restraints are applied.[43]
- Each written order for a physical restraint or seclusion is limited to 4 hours for adults, 2 hours for children and adolescents ages 9 to 17, or 1 hour for clients under 9. The original order may only be renewed in accordance with these limits for up to a total of 24 hours. After the original order expires, a physician or licensed independent practitioner (if allowed under state law) must see and assess the client before issuing a new order.[44]
Side Rails and Enclosed Beds
Side rails and enclosed beds may also be considered a restraint, depending on the purpose of the device. Recall the definition of a restraint as “a device, method, or process that is used for the specific purpose of restricting a clients freedom of movement or access to movement without the permission of the person.” If the purpose of raising the side rails is to prevent a client from voluntarily getting out of bed or attempting to exit the bed, then use of the side rails would be considered a restraint. On the other hand, if the purpose of raising the side rails is to prevent the client from inadvertently falling out of bed, or to help the client with repositioning, then it is not considered a restraint. If a client does not have the physical capacity to get out of bed, regardless if side rails are raised or not, then the use of side rails is not considered a restraint.[45]
Hand Mitts, Soft Limb Restraints, and Vest Restraints
A hand mitt is a large, soft glove that covers a confused client’s hand to prevent them from inadvertently dislodging medical equipment. Hand mitts are considered a restraint by The Joint Commission if used under these circumstances[46]:
- Are pinned or otherwise attached to the bed or bedding
- Are applied so tightly that the client's hands or finger are immobilized
- Are so bulky that the client's ability to use their hands is significantly reduced
- Cannot be easily removed intentionally by the client in the same manner it was applied by staff, considering the client's physical condition and ability to accomplish the objective
Soft limb restraints are a type of medical restraint that is designed to immobilize either one or both arms or legs through application around the wrist(s) or ankle(s). The restraint is made of a soft material designed to minimize the risk of pressure injuries or other injuries. Soft limb restraints are implemented to prevent inadvertent removal of tubes, drains, catheters, or other medical equipment by the client.[47]
Vest restraints are a type of mesh or cloth vest applied over the client's chest and tied to an immovable part of each side of the bed. The purpose of vest restraints is to prevent a client from getting out of bed and injuring themselves. As with any restraint, vest restraints should only be used for impulsive or confused clients when other alternatives are not effective, and not as a means of convenience.[48]
It is important for the nurse to be aware of current best practices and guidelines for restraint use because they are continuously changing. For example, meal trays on chairs were previously used in long-term care facilities to prevent residents from getting out of the chair and falling. However, by the definition of a restraint, this action is now considered a restraint and is no longer used. Instead, several alternative interventions to restraints are now being used.
Alternatives to Restraints
Many alternatives to using restraints in long-term care centers have been developed. Most interventions focus on the individualization of client care and elimination of medications with side effects that cause aggression and the need for restraints. Common interventions used as alternatives to restraints include routine daily schedules, regular feeding times, intentional rounding, frequent toileting, and effective pain management.[49]
Diversionary techniques such as television, music, games, or looking out a window can also be used to help to calm a restless client. Encouraging restless clients to spend time in a supervised area, such as a dining room, lounge, or near the nurses’ station, helps to prevent their desire to get up and move around. If these techniques are not successful, bed and chair alarms or the use of a sitter at the bedside are also considered alternatives to restraints.
You have now learned how to perform each step of the nursing process according to the ANA Standards of Professional Nursing Practice. Critical thinking, clinical reasoning, and clinical judgment are used when assessing the client, creating a nursing care plan, and implementing interventions. Frequent reassessment, with revisions to the care plan as needed, is important to help the client achieve expected outcomes. Throughout the entire nursing process, the client always remains the cornerstone of nursing care. Providing individualized, client-centered care and evaluating whether that care has been successful in achieving client outcomes are essential for providing safe, professional nursing practice.
Video Review of Creating a Sample Care Plan[50]
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Instructions: Apply what you’ve learned in this chapter by creating a nursing care plan using the following scenario. Use the template in Appendix B as a guide.
The client, Mark S., is a 57-year-old male who was admitted to the hospital with “severe” abdominal pain that was unable to be managed in the Emergency Department. The physician has informed Mark that he will need to undergo some diagnostic tests. The tests are scheduled for the morning.
After receiving the news about his condition and the need for diagnostic tests, Mark begins to pace the floor. He continues to pace constantly. He keeps asking the nurse the same question (“How long will the tests take?”) about his tests over and over again. The client also remarked, “I’m so uptight I will never be able to sleep tonight.” The nurse observes that the client avoids eye contact during their interactions and that he continually fidgets with the call light. His eyes keep darting around the room. He appears tense and has a strained expression on his face. He states, “My mouth is so dry.” The nurse observes his vital signs to be: T 98, P 104, R 30, BP 180/96. The nurse notes that his skin feels sweaty (diaphoretic) and cool to the touch.
Critical Thinking Activity:
-
- Group (cluster) the cues (subjective and objective data).
- Create a problem-focused nursing diagnosis (hypothesis).
- Develop a broad goal and then identify an expected outcome in “SMART” format.
- Outline three interventions for the nursing diagnosis to meet the goal and their rationale. Cite an evidence-based source for the interventions and rationale
- Imagine that you implemented the interventions that you identified. Evaluate the degree to which the expected outcome was achieved: Met - Partially Met - Not Met.

Test your knowledge using this NCLEX Next Generation-style question. You may reset and resubmit your answers to this question an unlimited number of times.[51]
ADOPIE: An easy way to remember the ANA Standards and the nursing process. Each letter refers to the six components of the nursing process: Assessment, Diagnosis, Outcomes Identification, Planning, Implementation, and Evaluation. (Chapter 4.2)
Art of nursing: Unconditionally acceptance of the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care.[52] (Chapter 4.2)
At-risk populations: Groups of people who share a characteristic that causes each member to be susceptible to a particular human response, such as demographics, health/family history, stages of growth/development, or exposure to certain events/experiences.[53] (Chapter 4.4)
Associated conditions: Medical diagnoses, injuries, procedures, medical devices, or pharmacological agents. These conditions are not independently modifiable by the nurse, but support accuracy in nursing diagnosis.[54] (Chapter 4.4)
Care relationship: A relationship described as one in which the whole person is assessed while balancing the vulnerability and dignity of the client and family.[55] (Chapter 4.2)
Client: Individual, family, or group, which includes significant others and populations.[56] (Chapter 4.2)
Clinical judgment: The observed outcome of critical thinking and decision-making. It is an iterative process that uses nursing knowledge to observe and access presenting situations, identify a prioritized client concern, and generate the best possible evidence-based solutions in order to deliver safe client care.[57] (Chapter 4.2)
Clinical reasoning: A complex cognitive process that uses formal and informal thinking strategies to gather and analyze client information, evaluate the significance of this information, and weigh alternative actions. [58] (Chapter 4.2)
Clustering data: Grouping data into similar domains or patterns. (Chapter 4.4)
Collaborative nursing interventions: Nursing interventions that require cooperation among health care professionals and unlicensed assistive personnel (UAP). (Chapter 4.6)
Coordination of care: While implementing interventions during the nursing process, includes competencies such as organizing the components of the plan with input from the health care consumer, engaging the client in self-care to achieve goals, and advocating for the delivery of dignified and person-centered care by the interprofessional team.[59] (Chapter 4.7)
Critical thinking: Reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.[60] (Chapter 4.2)
Cues: Subjective or objective data that gives the nurse a hint or indication of a potential problem, process, or disorder. (Chapter 4.2)
Deductive reasoning: “Top-down thinking” or moving from the general to the specific. Deductive reasoning relies on a general statement or hypothesis—sometimes called a premise or standard—that is held to be true. The premise is used to reach a specific, logical conclusion. (Chapter 4.2)
Defining characteristics: Observable cues/inferences that cluster as manifestations of a problem-focused, health-promotion diagnosis, or syndrome. This does not only imply those things that the nurse can see, but also things that are seen, heard (e.g., the client/family tells us), touched, or smelled.[61] (Chapter 4.4)
Delegation: The assignment of the performance of activities or tasks related to client care to unlicensed assistive personnel while retaining accountability for the outcome.[62] (Chapter 4.7)
Dependent nursing interventions: Interventions that require a prescription from a physician, advanced practice nurse, or physician’s assistant. (Chapter 4.6)
Direct care: Interventions that are carried out by having personal contact with a client. (Chapter 4.6)
Electronic Medical Record (EMR): An electronic version of the client’s medical record. (Chapter 4.3)
Evidence-Based Practice (EBP): A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and client, family, group, community, and population preferences and values.[63] (Chapter 4.2)
Expected outcomes: Statements of measurable action for the client within a specific time frame and in response to nursing interventions. “SMART” outcome statements are specific, measurable, action-oriented, realistic, and include a time frame. (Chapter 4.5)
Functional Health Patterns: An evidence-based assessment framework for identifying client problems and risks during the assessment phase of the nursing process. (Chapter 4.4)
Generalization: A judgment formed from a set of facts, cues, and observations. (Chapter 4.2)
Goals: Broad statements of purpose that describe the aim of nursing care. (Chapter 4.5)
Health promotion-wellness nursing diagnosis: A clinical judgment concerning motivation and desire to increase well-being and to actualize human health potential. (Chapter 4.4)
Health teaching and health promotion: Employing strategies to teach and promote health and wellness.[64] (Chapter 4.7)
Hypothesis: A proposed explanation for a situation. It attempts to explain the “why” behind the problem that is occurring. (Chapter 4.2)
Independent nursing interventions: Any intervention that the nurse can provide without obtaining a prescription or consulting anyone else. (Chapter 4.6)
Indirect care: Interventions performed by the nurse in a setting other than directly with the client. An example of indirect care is creating a nursing care plan. (Chapter 4.6)
Inductive reasoning: A type of reasoning that involves forming generalizations based on specific incidents. (Chapter 4.2)
Inference: Interpretations or conclusions based on cues, personal experiences, preferences, or generalizations. (Chapter 4.3)
Licensed Practical Nurses or Licensed Vocational Nurses (LPNs/LVNs): Nurses who have had specific training and passed a licensing exam. The training is generally less than that of a Registered Nurse. The scope of practice of an LPN/LVN is determined by the facility and the state’s Nurse Practice Act. (Chapter 4.3)
Maslow’s Hierarchy of Needs: A theory used to prioritize the most urgent client needs to address first. The bottom levels of the pyramid represent the most important physiological needs intertwined with safety. (Chapter 4.4)
Medical diagnosis: A disease or illness diagnosed by a physician or advanced health care provider such as a nurse practitioner or physician’s assistant. Medical diagnoses are a result of clustering signs and symptoms to determine what is medically affecting an individual. (Chapter 4.3)
Nursing: Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in the recognition of the connection of all humanity.[65] (Chapter 4.2)
Nursing care plan: Specific documentation of the planning and delivery of nursing care that is required by The Joint Commission. (Chapter 4.2)
Nursing diagnosis: A clinical judgment concerning a human response to health conditions/life processes, or a vulnerability for that response, by an individual, family, group, or community. (Chapter 4.4)
Nursing interventions: Evidence-based actions that the nurse performs to achieve client outcomes. (Chapter 4.6)
Nursing process: A systematic approach to client-centered care with steps including assessment, diagnosis, outcome identification, planning, implementation, and evaluation; otherwise known by the mnemonic “ADOPIE.” (Chapter 4.1)
Objective data: Data that the nurse can see, touch, smell, or hear or is reproducible such as vital signs. Laboratory and diagnostic results are also considered objective data. (Chapter 4.3)
Order: An intervention, remedy or treatment as directed by an authorized primary health care provider.[66] (Chapter 4.6)
Outcome: A measurable behavior demonstrated by the client's response to nursing interventions.[67] (Chapter 4.5)
PES format: The format of a nursing diagnosis statement that includes:
- Problem (P) - statement of the client problem (i.e., the nursing diagnosis)
- Etiology (E) - related factors (etiology) contributing to the cause of the nursing diagnosis
- Signs and Symptoms (S) - defining characteristics manifested by the client of that nursing diagnosis (Chapter 4.4)
Physical examination: A systematic data collection method of the body that uses the techniques of inspection, auscultation, palpation, and percussion. (Chapter 4.3)
Prescription: Intervention as it relates to medication specifically as directed by an authorized primary health care provider.[68] (Chapter 4.6)
Primary data: Information collected from the client. (Chapter 4.3)
Primary health care provider: Member of the health care team (usually a medical physician, nurse practitioner, etc.) licensed and authorized to formulate prescriptions on behalf of the client.[69] (Chapter 4.6)
Prioritization: The skillful process of deciding which actions to complete first for client safety and optimal client outcomes. (Chapter 4.4)
Problem-focused nursing diagnosis: A clinical judgment concerning an undesirable human response to health condition/life processes that exist in an individual, family, group, or community. (Chapter 4.4)
Quality improvement: The “combined and unceasing efforts of everyone -- health care professionals, clients and their families, researchers, payers, planners, and educators -- to make the changes that will lead to better client outcomes (health), better system performance (care), and better professional development (learning).”[70] (Chapter 4.7)
Rapport: Developing a relationship of mutual trust and understanding. (Chapter 4.2)
Registered Nurse (RN): A nurse who has had a designated amount of education and training in nursing and is licensed by a state Board of Nursing. (Chapter 4.3)
Related factors: The underlying cause (etiology) of a nursing diagnosis. (Chapter 4.4)
Risk nursing diagnosis: A clinical judgment concerning the vulnerability of an individual, family, group, or community for developing an undesirable human response to health conditions/life processes. (Chapter 4.4)
Secondary data: Information collected from sources other than the client. (Chapter 4.3)
Subjective data: Data that the client or family reports or data that the nurse makes as an inference, conclusion, or assumption, such as “The client appears anxious.” (Chapter 4.3)
Syndrome nursing diagnosis: A clinical judgment concerning a specific cluster of nursing diagnoses that occur together and are best addressed together and through similar interventions. (Chapter 4.4)
Unlicensed Assistive Personnel (UAP): Any unlicensed personnel trained to function in a supportive role, regardless of title, to whom a nursing responsibility may be delegated.[71] (Chapter 4.3)
Definition of Restraints
Restraints are devices used in health care settings to prevent clients from causing harm to themselves or others when alternative interventions are not effective. A restraint is a device, method, or process that is used for the specific purpose of restricting a client’s freedom of movement without the permission of the person. See Figure 5.6[72] for an image of a simulated client with restraints applied.
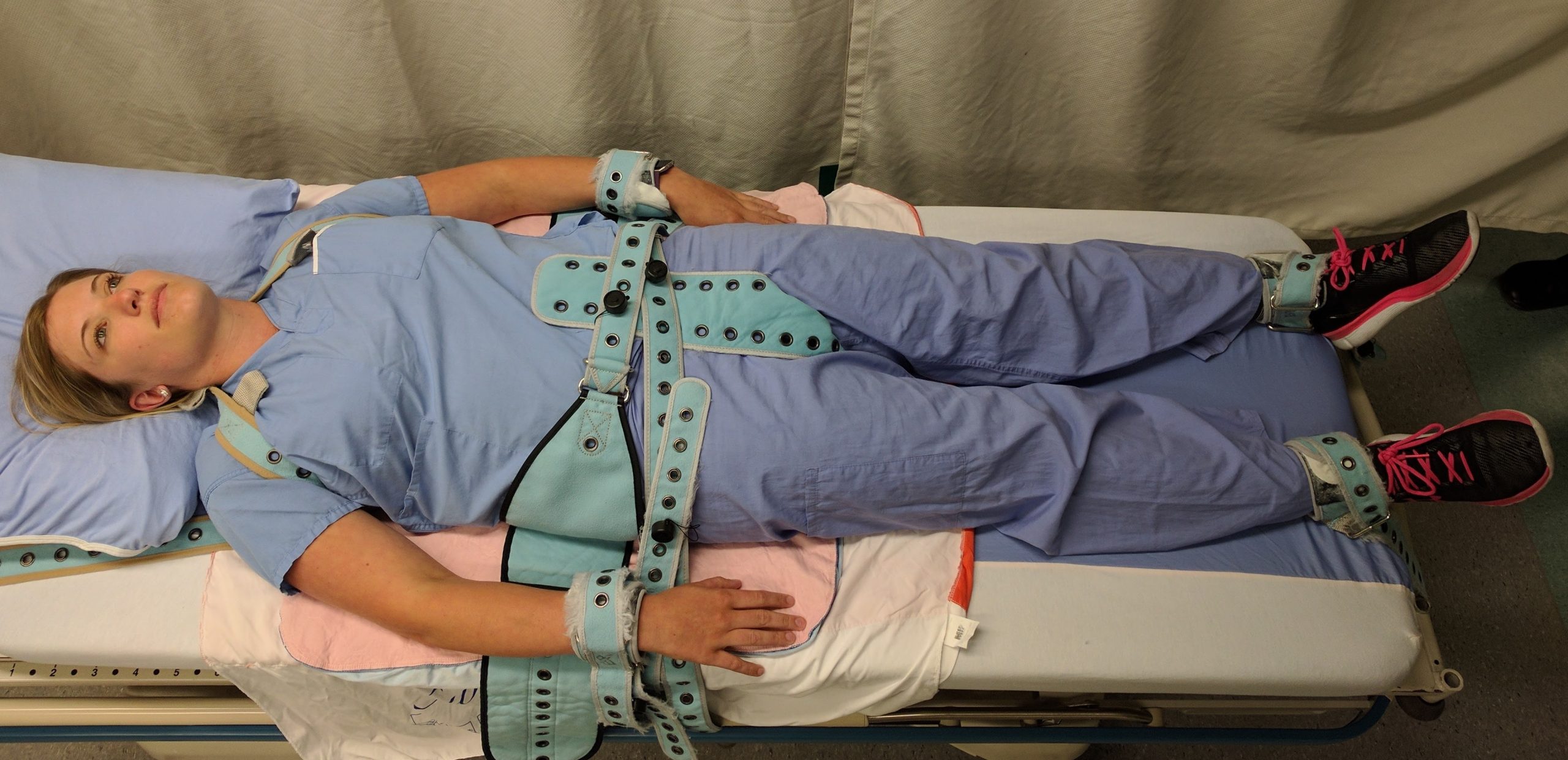
Restraints include mechanical devices such as a tie wrist device, chemical restraints, or seclusion. The Joint Commission defines chemical restraint as a drug used to manage a client’s behavior, restrict the client’s freedom of movement, or impair the client’s ability to appropriately interact with their surroundings that is not standard treatment or dosage for the client’s condition. It is important to note that the definition states the medication “is not standard treatment or dosage for the client’s condition.”[73] Seclusion is defined as the confinement of a client in a locked room from which they cannot exit on their own. It is generally used as a method of discipline for behavior that can cause harm to themselves or others, or as a method of decreasing environmental stimulation. Seclusion limits freedom of movement because, although the client is not mechanically restrained, they cannot leave the area.
Although restraints are used with the intention to keep a client safe, they impact a client’s psychological safety and dignity and can cause additional safety issues and death. A restrained person has a natural tendency to struggle and try to remove the restraint and can fall or become fatally entangled in the restraint. Furthermore, immobility that results from the use of restraints can cause pressure injuries, contractures, and muscle loss. Restraints take a large emotional toll on the client’s self-esteem and may cause humiliation, fear, and anger.
Restraint Guidelines
The American Nurses Association (ANA) has established evidence-based guidelines that state a restraint-free environment is the standard of care. The ANA encourages the participation of nurses to reduce client restraints and seclusion in all health care settings. Restraining or secluding clients is viewed as contrary to the goals and ethical traditions of nursing because it violates the fundamental client rights of autonomy and dignity. However, the ANA also recognizes there are times when there is no viable option other than restraints to keep a client safe, such as during an acute psychotic episode when client and staff safety are in jeopardy due to aggression or assault. The ANA also states that restraints may be justified in some clients with severe dementia or delirium when they are at risk for serious injuries such as a hip fracture due to falling.
The ANA provides the following guidelines: “When restraint is necessary, documentation should be done by more than one witness. Once restrained, the client should be treated with humane care that preserves human dignity. In those instances where restraint, seclusion, or therapeutic holding is determined to be clinically appropriate and adequately justified, registered nurses who possess the necessary knowledge and skills to effectively manage the situation must be actively involved in the assessment, implementation, and evaluation of the selected emergency measure, adhering to federal regulations and the standards of The Joint Commission (2009) regarding appropriate use of restraints and seclusion.”[74] Nursing documentation typically includes information such as client behavior necessitating the restraint, alternatives to restraints that were attempted, the type of restraint used, the time it was applied, the location of the restraint, and client education regarding the restraint.
Medical Restraints
Restraints used to manage nonviolent, non-self-destructive behaviors are referred to as medical restraints. Medical restraints may be appropriate to manage behavior such as the client attempting to remove life-sustaining tubes, drains, IV catheters, urinary catheters, or endotracheal tubes. These types of restraints often include hand mitts or soft wrist restraints. Medical restraints may also be used for clients attempting to get out of bed and as such are a high risk for falls. These types of restraints include siderails, vest restraints, and roll belts. Each facility is required to have a policy in place for the use of medical restraints. Policies typically include requirements for documentation of the reason for the restraint, alternative measures tried, type of restraint applied, behavioral criteria for removal of restraint, range of motion and cares while in restraints, and the date and time the restraint is applied or removed. A medical restraint requires a registered nurse to apply or supervise application of the restraint, a new order every 24 hours, and may never be issued as an as needed order. If the primary care provider did not order the restraint, they should be notified as soon as possible. Medical restraints are more commonly encountered in the general hospital setting rather than behavioral restraints.[75],[76]
Behavioral Restraints
Restraints used to manage violent, self-destructive behaviors are referred to as behavioral restraints. Behavioral restraints are used when clients exhibit behaviors such as hitting or kicking staff or other clients, physically harming themselves or others, or threatening to do so. Behavioral restraints are used in emergency situations where safety concerns need to be immediately addressed to prevent harm. [77]
RNs need special training to apply behavioral restraints, including safe application of the restraint, maintaining personal safety, and techniques to de-escalate the violent or aggressive behavior. Behavioral restraints are typically used in mental health units, emergency departments, or critical care units. Similar to medical restraints, each agency must have a policy in place for the use of behavioral restraints. Health care facilities that accept Medicare and Medicaid reimbursement must also follow federal guidelines for the use of behavioral restraints that include the following:
Guidelines for the use of behavioral restraints include the following:
- When a restraint is the only viable option, it must be discontinued at the earliest possible time.
- Orders for the use of seclusion or restraint can never be written as a standing order or PRN (as needed).
- The treating physician must be consulted as soon as possible if the restraint or seclusion is not ordered by the client’s treating physician.
- A physician or licensed independent practitioner must see and evaluate the need for the restraint or seclusion within one hour after the initiation.
- After restraints have been applied, the nurse should follow agency policy for frequent monitoring and regularly changing the client's position to prevent complications. Nurses must also ensure the client's basic needs (i.e., hydration, nutrition, and toileting) are met. Some agencies require a 1:1 client sitter when restraints are applied.[78]
- Each written order for a physical restraint or seclusion is limited to 4 hours for adults, 2 hours for children and adolescents ages 9 to 17, or 1 hour for clients under 9. The original order may only be renewed in accordance with these limits for up to a total of 24 hours. After the original order expires, a physician or licensed independent practitioner (if allowed under state law) must see and assess the client before issuing a new order.[79]
Side Rails and Enclosed Beds
Side rails and enclosed beds may also be considered a restraint, depending on the purpose of the device. Recall the definition of a restraint as “a device, method, or process that is used for the specific purpose of restricting a clients freedom of movement or access to movement without the permission of the person.” If the purpose of raising the side rails is to prevent a client from voluntarily getting out of bed or attempting to exit the bed, then use of the side rails would be considered a restraint. On the other hand, if the purpose of raising the side rails is to prevent the client from inadvertently falling out of bed, or to help the client with repositioning, then it is not considered a restraint. If a client does not have the physical capacity to get out of bed, regardless if side rails are raised or not, then the use of side rails is not considered a restraint.[80]
Hand Mitts, Soft Limb Restraints, and Vest Restraints
A hand mitt is a large, soft glove that covers a confused client’s hand to prevent them from inadvertently dislodging medical equipment. Hand mitts are considered a restraint by The Joint Commission if used under these circumstances[81]:
- Are pinned or otherwise attached to the bed or bedding
- Are applied so tightly that the client's hands or finger are immobilized
- Are so bulky that the client's ability to use their hands is significantly reduced
- Cannot be easily removed intentionally by the client in the same manner it was applied by staff, considering the client's physical condition and ability to accomplish the objective
Soft limb restraints are a type of medical restraint that is designed to immobilize either one or both arms or legs through application around the wrist(s) or ankle(s). The restraint is made of a soft material designed to minimize the risk of pressure injuries or other injuries. Soft limb restraints are implemented to prevent inadvertent removal of tubes, drains, catheters, or other medical equipment by the client.[82]
Vest restraints are a type of mesh or cloth vest applied over the client's chest and tied to an immovable part of each side of the bed. The purpose of vest restraints is to prevent a client from getting out of bed and injuring themselves. As with any restraint, vest restraints should only be used for impulsive or confused clients when other alternatives are not effective, and not as a means of convenience.[83]
It is important for the nurse to be aware of current best practices and guidelines for restraint use because they are continuously changing. For example, meal trays on chairs were previously used in long-term care facilities to prevent residents from getting out of the chair and falling. However, by the definition of a restraint, this action is now considered a restraint and is no longer used. Instead, several alternative interventions to restraints are now being used.
Alternatives to Restraints
Many alternatives to using restraints in long-term care centers have been developed. Most interventions focus on the individualization of client care and elimination of medications with side effects that cause aggression and the need for restraints. Common interventions used as alternatives to restraints include routine daily schedules, regular feeding times, intentional rounding, frequent toileting, and effective pain management.[84]
Diversionary techniques such as television, music, games, or looking out a window can also be used to help to calm a restless client. Encouraging restless clients to spend time in a supervised area, such as a dining room, lounge, or near the nurses’ station, helps to prevent their desire to get up and move around. If these techniques are not successful, bed and chair alarms or the use of a sitter at the bedside are also considered alternatives to restraints.
Learning Objectives
- Identify safety considerations for adults of all ages
- Indicate correct identification of client prior to performing any client care measures
- Describe industry standards and regulations regarding microbiological, physical, and environmental safety
- Differentiate safety considerations among diverse clients
- Apply decision-making related to measures to minimize use of restraints
A national focus on reducing medical errors has been in place since 1999 when the Institute of Medicine (IOM) released a report titled To Err is Human: Building a Safer Health System. This historic report broke the silence surrounding health care errors and encouraged safety to be built into the processes of providing client care. It was soon followed by the establishment of several safety initiatives by The Joint Commission, including the release of annual National Patient Safety Goals. Additionally, the Quality and Safety Education for Nurses (QSEN) Institute was developed to promote emphasis on high-quality, safe client care in nursing. This chapter will discuss several safety initiatives that promote a safe health care environment.
Learning Objectives
- Identify safety considerations for adults of all ages
- Indicate correct identification of client prior to performing any client care measures
- Describe industry standards and regulations regarding microbiological, physical, and environmental safety
- Differentiate safety considerations among diverse clients
- Apply decision-making related to measures to minimize use of restraints
A national focus on reducing medical errors has been in place since 1999 when the Institute of Medicine (IOM) released a report titled To Err is Human: Building a Safer Health System. This historic report broke the silence surrounding health care errors and encouraged safety to be built into the processes of providing client care. It was soon followed by the establishment of several safety initiatives by The Joint Commission, including the release of annual National Patient Safety Goals. Additionally, the Quality and Safety Education for Nurses (QSEN) Institute was developed to promote emphasis on high-quality, safe client care in nursing. This chapter will discuss several safety initiatives that promote a safe health care environment.
Safety: A Basic Need
Safety is a basic foundational human need and always receives priority in client care. Nurses typically use Maslow’s Hierarchy of Needs to prioritize urgent client needs, with the bottom two rows of the pyramid receiving top priority. See Figure 5.1[85] for an image of Maslow’s Hierarchy of Needs. Safety is intertwined with basic physiological needs.
Consider the following scenario: You are driving back from a relaxing weekend at the lake and come upon a fiery car crash. You run over to the car to help anyone inside. When you get to the scene, you notice that the lone person in the car is not breathing. Your first priority is not to initiate rescue breathing inside the burning car, but to move the person to a safe place where you can safely provide CPR.
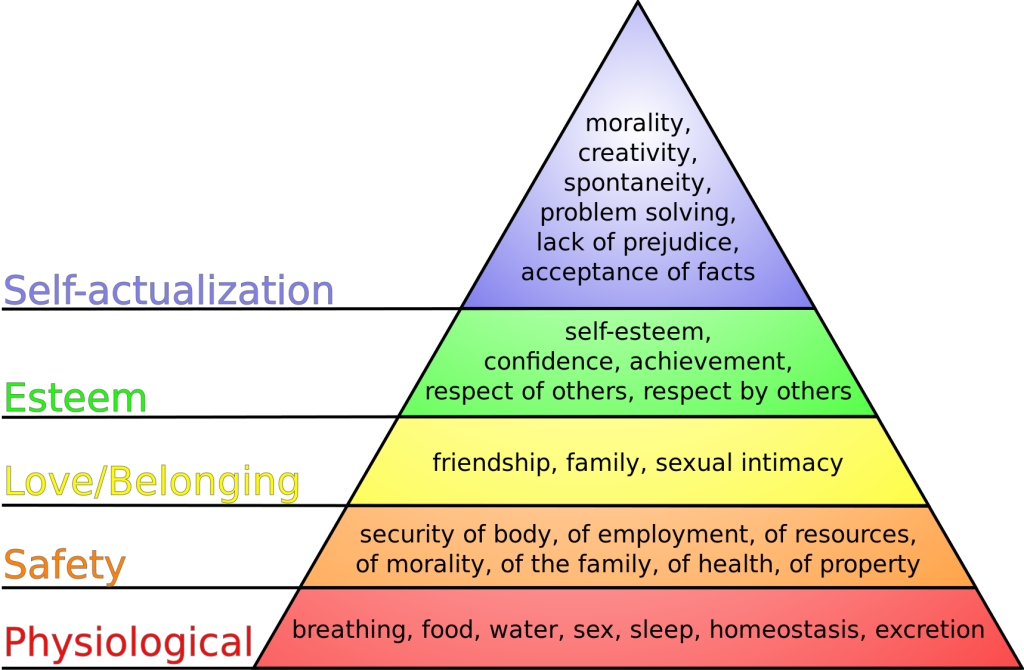
In nursing, the concept of client safety is central to everything we do in all health care settings. As a nurse, you play a critical role in promoting client safety while providing care. You also teach clients and their caregivers how to prevent injuries and remain safe in their homes and in the community. Safe client care also includes measures to keep you safe in the health care environment; if you become ill or injured, you will not be able to effectively care for others.
Safe client care is a commitment to providing the best possible care to every client and their caregivers in every moment of every day. Clients come to health care facilities expecting to be kept safe while they are treated for illnesses and injuries. Unfortunately, you may have heard stories about situations when that did not happen. Medical errors can be devastating to clients and their families. Consider the true story in the following box that illustrates factors affecting client safety.
The Josie King Story
In 2001, 18-month-old Josie King died as a result of medical errors in a well-known hospital from a hospital-acquired infection and an incorrectly administered pain medication. How did this preventable death happen? Watch this video of her mother, Sorrel King, telling Josie’s story and explaining how Josie’s death spurred her work on improving client safety in hospitals everywhere.[86]
Reflective Questions:
- What factors contributed to Josie’s death?
- How could these factors be resolved?
Never Events
The event described in the Josie King story is considered a “never event.” Never events are adverse events that are clearly identifiable, measurable, serious (resulting in death or significant disability), and preventable. In 2007 the Centers for Medicare and Medicaid Services (CMS) discontinued payment for costs associated with never events, and this policy has been adopted by most private insurance companies. Never events are publicly reported, with the goal of increasing accountability by health care agencies and improving the quality of client care. The current list of never events includes seven categories of events:
- Surgical or procedural event, such as surgery performed on the wrong body part
- Product or device, such as injury or death from a contaminated drug or device
- Client protection, such as client suicide in a health care setting
- Care management, such as death or injury from a medication error
- Environmental, such as death or injury as the result of using restraints
- Radiologic, such as a metallic object in an MRI area
- Criminal, such as death or injury of a client or staff member resulting from physical assault on the grounds of a health care setting
Sentinel Events
Sentinel events are very similar to never events although they may not be entirely preventable. They are defined by The Joint Commission as an “A client safety event that reaches a client and results in death, permanent harm, or severe temporary harm requiring interventions to sustain life." Such events are called "sentinel" because they signal the need for immediate investigation and response. Each accredited organization is strongly encouraged, but not required, to report sentinel events to The Joint Commission.[87] It is helpful to facilities to self-report sentinel events so that other facilities can learn from these events and future sentinel events can be prevented through knowledge sharing and risk reduction. Investigations into sentinel events are typically achieved through a process called root cause analysis.
Root cause analysis is a structured method used to analyze serious adverse events to identify underlying problems that increase the likelihood of errors, while avoiding the trap of focusing on mistakes by individuals. A multidisciplinary team analyzes the sequence of events leading up to the error with the goal of identifying how and why the event occurred. The ultimate goal of root cause analysis is to prevent future harm by eliminating hidden problems within a health care system that contribute to adverse events. For example, when a medication error occurs, a root cause analysis goes beyond focusing on the mistake by the nurse and looks at other system factors that contributed to the error, such as similar-looking drug labels, placement of similar-looking medications next to each other in a medication dispensing machine, or vague instructions in a provider order.
Root cause analysis uses human factors science as part of the investigation. Human factors focus on the interrelationships among humans, the tools and equipment they use in the workplace, and the environment in which they work. Safety in health care is ultimately dependent on humans - the doctors, nurses, and health care professionals - providing the care.
Near Misses
In addition to investigating sentinel events and never events, agencies use root cause analysis to investigate near misses. Near misses are defined by the World Health Organization (WHO) as, “An error that has the potential to cause an adverse event (client harm) but fails to do so because of chance or because it is intercepted.” Errors and near misses are rarely the result of poor motivation or incompetence of the health care professional but are often caused by key contributing factors such as poor communication, less-than-optimal teamwork, memory overload, reliance on memory for complex procedures, and lack of standardization of policies and procedures. In an effort to prevent near misses, medical errors, sentinel events, and never events, several safety strategies have been developed and implemented in health care organizations across the country. These strategies will be discussed throughout the remainder of the chapter.
Incident Reports and Client Safety
Recall from the previous discussion in Chapter 2.5 that an incident report is a specific type of documentation performed when there is an error, near miss, or other unexpected occurrence that occurs during client care. Incident reports are used to identify process problems or other areas that could benefit from safety and quality improvement and are not included in the client's medical record. They are a component of an agency's culture of safety and are used during investigations like root cause analysis to help improve the safety and quality of client care.
Safety: A Basic Need
Safety is a basic foundational human need and always receives priority in client care. Nurses typically use Maslow’s Hierarchy of Needs to prioritize urgent client needs, with the bottom two rows of the pyramid receiving top priority. See Figure 5.1[88] for an image of Maslow’s Hierarchy of Needs. Safety is intertwined with basic physiological needs.
Consider the following scenario: You are driving back from a relaxing weekend at the lake and come upon a fiery car crash. You run over to the car to help anyone inside. When you get to the scene, you notice that the lone person in the car is not breathing. Your first priority is not to initiate rescue breathing inside the burning car, but to move the person to a safe place where you can safely provide CPR.
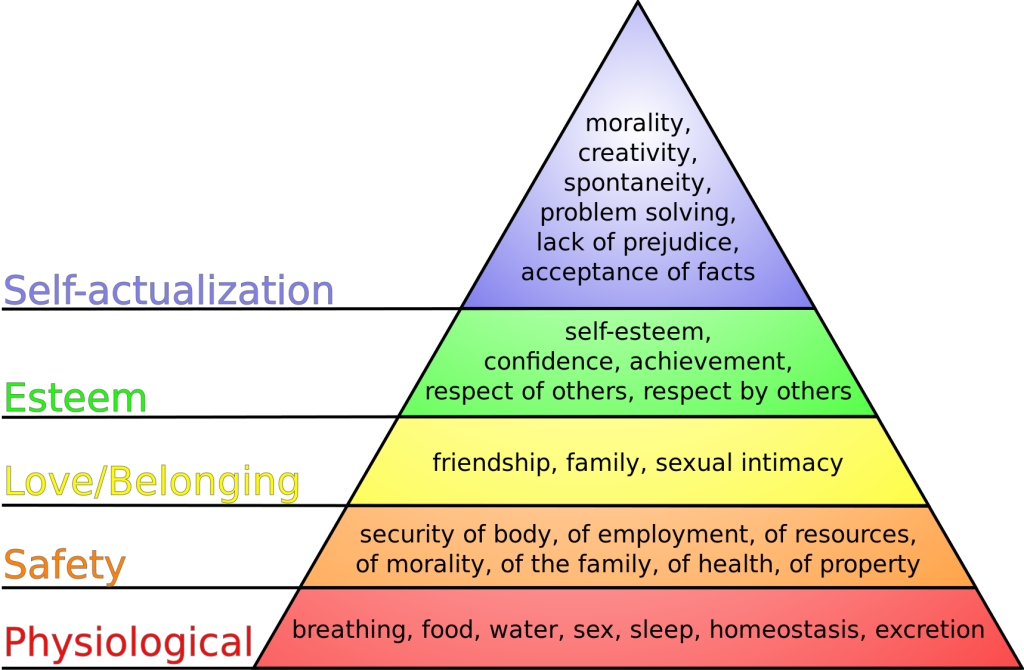
In nursing, the concept of client safety is central to everything we do in all health care settings. As a nurse, you play a critical role in promoting client safety while providing care. You also teach clients and their caregivers how to prevent injuries and remain safe in their homes and in the community. Safe client care also includes measures to keep you safe in the health care environment; if you become ill or injured, you will not be able to effectively care for others.
Safe client care is a commitment to providing the best possible care to every client and their caregivers in every moment of every day. Clients come to health care facilities expecting to be kept safe while they are treated for illnesses and injuries. Unfortunately, you may have heard stories about situations when that did not happen. Medical errors can be devastating to clients and their families. Consider the true story in the following box that illustrates factors affecting client safety.
The Josie King Story
In 2001, 18-month-old Josie King died as a result of medical errors in a well-known hospital from a hospital-acquired infection and an incorrectly administered pain medication. How did this preventable death happen? Watch this video of her mother, Sorrel King, telling Josie’s story and explaining how Josie’s death spurred her work on improving client safety in hospitals everywhere.[89]
Reflective Questions:
- What factors contributed to Josie’s death?
- How could these factors be resolved?
Never Events
The event described in the Josie King story is considered a “never event.” Never events are adverse events that are clearly identifiable, measurable, serious (resulting in death or significant disability), and preventable. In 2007 the Centers for Medicare and Medicaid Services (CMS) discontinued payment for costs associated with never events, and this policy has been adopted by most private insurance companies. Never events are publicly reported, with the goal of increasing accountability by health care agencies and improving the quality of client care. The current list of never events includes seven categories of events:
- Surgical or procedural event, such as surgery performed on the wrong body part
- Product or device, such as injury or death from a contaminated drug or device
- Client protection, such as client suicide in a health care setting
- Care management, such as death or injury from a medication error
- Environmental, such as death or injury as the result of using restraints
- Radiologic, such as a metallic object in an MRI area
- Criminal, such as death or injury of a client or staff member resulting from physical assault on the grounds of a health care setting
Sentinel Events
Sentinel events are very similar to never events although they may not be entirely preventable. They are defined by The Joint Commission as an “A client safety event that reaches a client and results in death, permanent harm, or severe temporary harm requiring interventions to sustain life." Such events are called "sentinel" because they signal the need for immediate investigation and response. Each accredited organization is strongly encouraged, but not required, to report sentinel events to The Joint Commission.[90] It is helpful to facilities to self-report sentinel events so that other facilities can learn from these events and future sentinel events can be prevented through knowledge sharing and risk reduction. Investigations into sentinel events are typically achieved through a process called root cause analysis.
Root cause analysis is a structured method used to analyze serious adverse events to identify underlying problems that increase the likelihood of errors, while avoiding the trap of focusing on mistakes by individuals. A multidisciplinary team analyzes the sequence of events leading up to the error with the goal of identifying how and why the event occurred. The ultimate goal of root cause analysis is to prevent future harm by eliminating hidden problems within a health care system that contribute to adverse events. For example, when a medication error occurs, a root cause analysis goes beyond focusing on the mistake by the nurse and looks at other system factors that contributed to the error, such as similar-looking drug labels, placement of similar-looking medications next to each other in a medication dispensing machine, or vague instructions in a provider order.
Root cause analysis uses human factors science as part of the investigation. Human factors focus on the interrelationships among humans, the tools and equipment they use in the workplace, and the environment in which they work. Safety in health care is ultimately dependent on humans - the doctors, nurses, and health care professionals - providing the care.
Near Misses
In addition to investigating sentinel events and never events, agencies use root cause analysis to investigate near misses. Near misses are defined by the World Health Organization (WHO) as, “An error that has the potential to cause an adverse event (client harm) but fails to do so because of chance or because it is intercepted.” Errors and near misses are rarely the result of poor motivation or incompetence of the health care professional but are often caused by key contributing factors such as poor communication, less-than-optimal teamwork, memory overload, reliance on memory for complex procedures, and lack of standardization of policies and procedures. In an effort to prevent near misses, medical errors, sentinel events, and never events, several safety strategies have been developed and implemented in health care organizations across the country. These strategies will be discussed throughout the remainder of the chapter.
Incident Reports and Client Safety
Recall from the previous discussion in Chapter 2.5 that an incident report is a specific type of documentation performed when there is an error, near miss, or other unexpected occurrence that occurs during client care. Incident reports are used to identify process problems or other areas that could benefit from safety and quality improvement and are not included in the client's medical record. They are a component of an agency's culture of safety and are used during investigations like root cause analysis to help improve the safety and quality of client care.
Every year, national safety goals are published by The Joint Commission to improve clientsafety. National Patient Safety Goals are goals and recommendations tailored to seven different types of health care agencies based on client safety data from experts and stakeholders. The seven health care areas include ambulatory health care settings, behavioral health care settings, critical access hospitals, home care, hospital settings, laboratories, nursing care centers, and office-based surgery settings. These goals are updated annually based on safety data and include evidence-based interventions. It is important for nurses and nursing students to be aware of the current National Patient Safety Goals for the settings in which they provide client care and use the associated recommendations.
The National Patient Safety Goals for nursing care settings (otherwise known as long-term care centers) are described in Table 5.5. (Note that the term “bedsore” is used in the last goal. This is a historic term for the current term “pressure injuries.”)
Table 5.5 National Patient Safety Goals for Nursing Care Centers[91]
| Goal | Recommendations and Rationale |
|---|---|
| Identify residents correctly | Use at least two ways to identify clients. For example, use the client’s or resident’s name and date of birth. This is done to make sure that each client gets the correct medication and treatment. |
| Use medicines safely | Take extra care with clients who take medications to thin their blood.
Record and pass along correct information about a client’s medications. Find out what medications the client is taking. Compare those medications to new medications prescribed for the client. Give the client written information about the medications they need to take. Tell the client it is important to bring their up-to-date list of medications every time they visit a doctor. |
| Prevent infection | Use the hand hygiene guidelines from the Centers for Disease Control and Prevention or the World Health Organization. Set goals for improving hand cleaning. |
| Prevent residents from falling | Find out which clients are most likely to fall. For example, is the client taking any medications that might make them weak, dizzy, or sleepy? Implement fall precautions for these clients. |
| Prevent bed sores | Find out which clients are most likely to have bed sores (i.e., pressure injuries). Take action to prevent pressure injuries in these clients at risk. Per agency protocol, frequently assess clients for pressure injuries. |
Read more about National Patient Safety Goals established by The Joint Commission.
Read more details about how to identify clients correctly, administer medications safely, and prevent infection by visiting the following sections in Open RN Nursing Skills, 2e:
- Initiating Patient Interaction
- Aseptic Technique Basic Concepts
- Basic Concepts of Administering Medications
Read more about "Pressure Injuries" (the current term used for "bed sores") in the "Integumentary" chapter of this book.
Safety strategies have been developed based on research to reduce the likelihood of errors and to create safe standards of care. Examples of safety initiatives include strategies to prevent medication errors, standardized checklists, and structured team communication tools.
Medication Errors
Several initiatives have been developed nationally to prevent medication errors, such as the establishment of a “Do Not Use List of Abbreviations," a “List of Error-Prone Abbreviations,” “Frequently Confused Medication List,” “High-Alert Medications List,” and the “Do Not Crush List.” Additionally, it is considered a standard of care for nurses to perform three checks of the rights of medication administration whenever administering medication. View more information about these safety initiatives to prevent medication errors in the box below. Specific strategies to prevent medication errors are discussed in the “Preventing Medication Errors” of the “Legal/Ethical” chapter of the Open RN Nursing Pharmacology, 2e textbook. The rights of medication administration are discussed in the “Basic Concepts of Administering Medications” section of the “Administration of Enteral Medications” chapter of the Open RN Nursing Skills, 2e textbook.
Read more about safety initiatives implemented to prevent medication errors:
Checklists
Performance of complex medical procedures is often based on memory, even though humans are prone to short-term memory loss, especially when we are multitasking or under stress. The point-of-care checklist is an example of a client care safety initiative that reduces this reliance on fallible memory. For example, a surgical checklist developed by the World Health Organization (WHO) has been adopted by most surgical providers around the world as a standard of care. It has significantly decreased injuries and deaths caused by surgeries by focusing on teamwork and communication. The Association of PeriOperative Registered Nurses (AORN) combined recommendations from The Joint Commission and the WHO to create a specific surgical checklist for nurses. See Figure 5.2[92] for an image of the WHO surgical checklist.
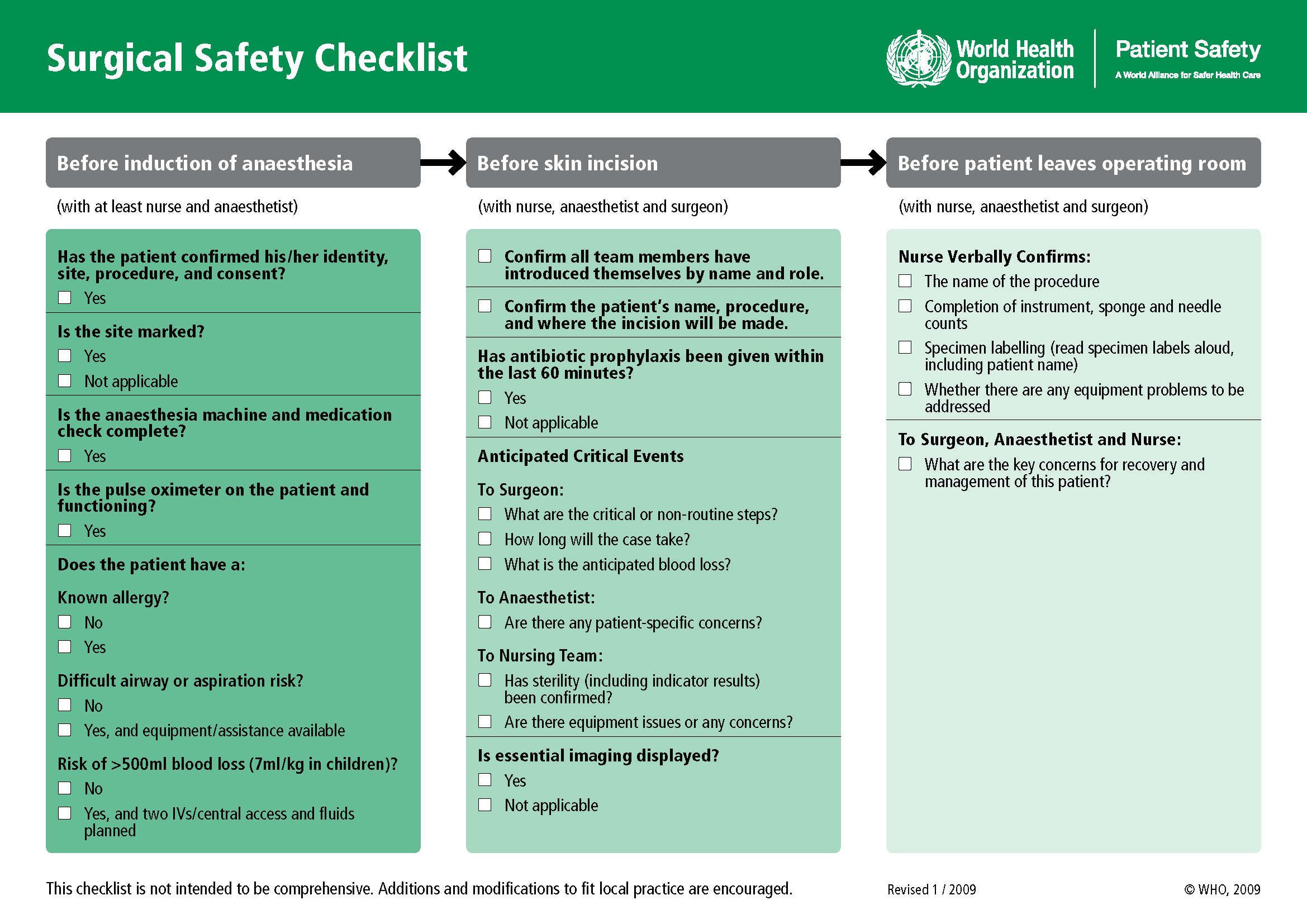
View an example of a Preop Checklist in the "Preoperative Care" section of the "Perioperative" chapter of Open RN Nursing Health Alterations.
Team Communication
Nurses routinely communicate with multidisciplinary health care team members and contact health care providers to report changes in client status. Serious client harm can occur when client information is absent, incomplete, erroneous, or delayed during team communication. Standardized methods of communication are used to ensure that accurate information is exchanged among team members in a structured and concise manner, such as ISBARR reports and handoff reports.
ISBARR is a mnemonic for the components of Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat back. See Figure 5.3[93] for an image of an ISBARR reference card.
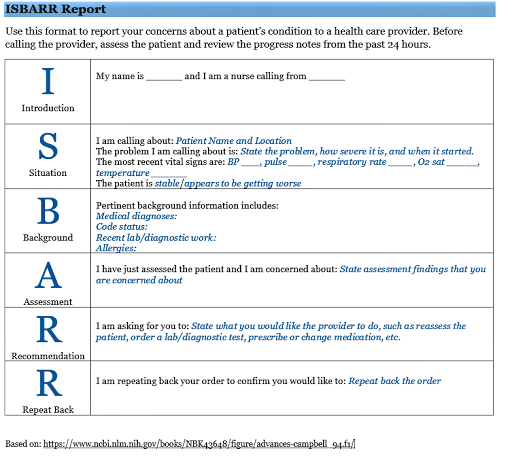
Handoff reports are a specific type of team communication as client care is transferred. Handoff reports are defined by The Joint Commission as, “A transfer and acceptance of client care responsibility achieved through effective communication. It is a real-time process of passing client specific information from one caregiver to another, or from one team of caregivers to another, for the purpose of ensuring the continuity and safety of the client’s care.”[94]
Review information about ISBARR and handoff reports in Chapter 2.4.
Safety strategies have been developed based on research to reduce the likelihood of errors and to create safe standards of care. Examples of safety initiatives include strategies to prevent medication errors, standardized checklists, and structured team communication tools.
Medication Errors
Several initiatives have been developed nationally to prevent medication errors, such as the establishment of a “Do Not Use List of Abbreviations," a “List of Error-Prone Abbreviations,” “Frequently Confused Medication List,” “High-Alert Medications List,” and the “Do Not Crush List.” Additionally, it is considered a standard of care for nurses to perform three checks of the rights of medication administration whenever administering medication. View more information about these safety initiatives to prevent medication errors in the box below. Specific strategies to prevent medication errors are discussed in the “Preventing Medication Errors” of the “Legal/Ethical” chapter of the Open RN Nursing Pharmacology, 2e textbook. The rights of medication administration are discussed in the “Basic Concepts of Administering Medications” section of the “Administration of Enteral Medications” chapter of the Open RN Nursing Skills, 2e textbook.
Read more about safety initiatives implemented to prevent medication errors:
Checklists
Performance of complex medical procedures is often based on memory, even though humans are prone to short-term memory loss, especially when we are multitasking or under stress. The point-of-care checklist is an example of a client care safety initiative that reduces this reliance on fallible memory. For example, a surgical checklist developed by the World Health Organization (WHO) has been adopted by most surgical providers around the world as a standard of care. It has significantly decreased injuries and deaths caused by surgeries by focusing on teamwork and communication. The Association of PeriOperative Registered Nurses (AORN) combined recommendations from The Joint Commission and the WHO to create a specific surgical checklist for nurses. See Figure 5.2[95] for an image of the WHO surgical checklist.
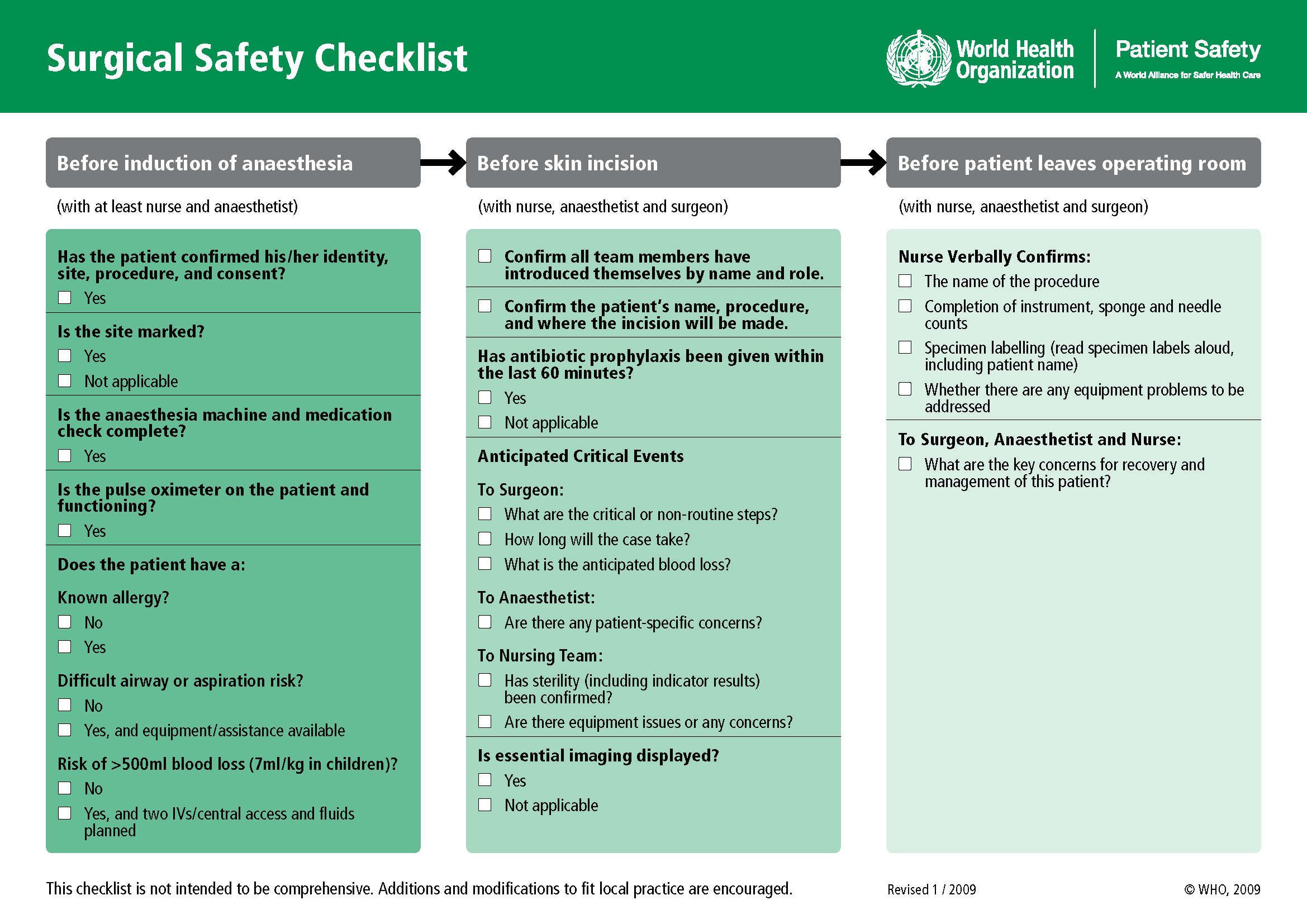
View an example of a Preop Checklist in the "Preoperative Care" section of the "Perioperative" chapter of Open RN Nursing Health Alterations.
Team Communication
Nurses routinely communicate with multidisciplinary health care team members and contact health care providers to report changes in client status. Serious client harm can occur when client information is absent, incomplete, erroneous, or delayed during team communication. Standardized methods of communication are used to ensure that accurate information is exchanged among team members in a structured and concise manner, such as ISBARR reports and handoff reports.
ISBARR is a mnemonic for the components of Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat back. See Figure 5.3[96] for an image of an ISBARR reference card.
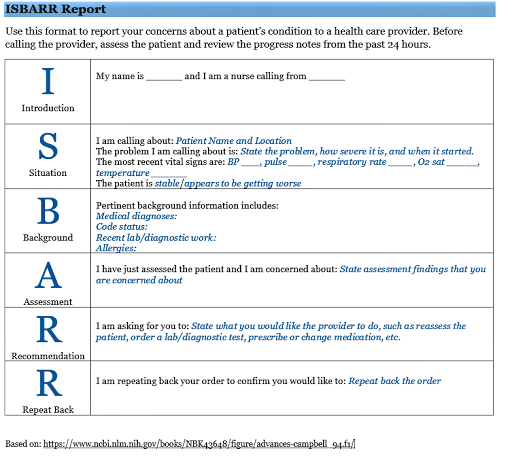
Handoff reports are a specific type of team communication as client care is transferred. Handoff reports are defined by The Joint Commission as, “A transfer and acceptance of client care responsibility achieved through effective communication. It is a real-time process of passing client specific information from one caregiver to another, or from one team of caregivers to another, for the purpose of ensuring the continuity and safety of the client’s care.”[97]
Review information about ISBARR and handoff reports in Chapter 2.4.
In addition to implementing safety strategies to improve safe client care, leaders of a health care agency must also establish a culture of safety. A culture of safety reflects the behaviors, beliefs, and values within and across all levels of an organization as they relate to safety and clinical excellence, with a focus on people. In 2021 The Joint Commission released a sentinel event regarding the essential role of leadership in establishing a culture of safety. According to The Joint Commission, leadership has an obligation to be accountable for protecting the safety of all health care consumers, including clients, employees, and visitors. Without adequate leadership and an effective culture of safety, there is higher risk for adverse events. Inadequate leadership can contribute to adverse effects in a variety of ways, including, but not limited to, the following[98]:
- Insufficient support of client safety event reporting
- Lack of feedback or response to staff and others who report safety vulnerabilities
- Allowing intimidation of staff who report events
- Refusing to consistently prioritize and implement safety recommendations
- Not addressing staff burnout
Three components of a culture of safety are the following[99]:
- Just Culture: People are encouraged, even rewarded, for providing essential safety-related information, but clear lines are drawn between human error and at-risk or reckless behaviors.
- Reporting Culture: People report errors and near-misses.
- Learning Culture: The willingness and the competence to draw the right conclusions from safety information systems, and the will to implement major reforms when their need is indicated.
The American Nurses Association further describes a culture of safety as one that includes openness and mutual respect when discussing safety concerns and solutions without shifting to individual blame, a learning environment with transparency and accountability, and reliable teams. In contrast, complexity, lack of clear measures, hierarchical authority, the “blame game,” and lack of leadership are examples of barriers that do not promote a culture of safety. If staff fear reprisal for mistakes and errors, they will be less likely to report errors, processes will not be improved, and client safety will continue to be impaired. See the following box for an example of safety themes established during a health care institution’s implementation of a culture of safety.
Safety Themes in a Culture of Safety[100]
Kaiser Permantente implemented a culture of safety in 2001 that focused on instituting the following six strategic themes:
- Safe culture: Creating and maintaining a strong safety culture, with client safety and error reduction embraced as shared organizational values.
- Safe care: Ensuring that the actual and potential hazards associated with high-risk procedures, processes, and client care populations are identified, assessed, and managed in a way that demonstrates continuous improvement and ultimately ensures that clients are free from accidental injury or illness.
- Safe staff: Ensuring that staff possess the knowledge and competence to perform required duties safely and contribute to improving system safety performance.
- Safe support systems: Identifying, implementing, and maintaining support systems—including knowledge-sharing networks and systems for responsible reporting—that provide the right information to the right people at the right time.
- Safe place: Designing, constructing, operating, and maintaining the environment of health care to enhance its efficiency and effectiveness.
- Safe clients: Engaging clients and their families in reducing medical errors, improving overall system safety performance, and maintaining trust and respect.
A strong safety culture encourages all members of the health care team to identify and reduce risks to client safety by reporting errors and near misses so that root cause analysis can be performed and identified risks are removed from the system. However, in a poorly defined and implemented culture of safety, staff often conceal errors due to fear or shame. Nurses have been traditionally trained to believe that clinical perfection is attainable, and that “good” nurses do not make errors. Errors are perceived as being caused by carelessness, inattention, indifference, or uninformed decisions. Although expecting high standards of performance is appropriate and desirable, it can become counterproductive if it creates an expectation of perfection that impacts the reporting of errors and near misses. If employees feel shame when they make an error, they may feel pressure to hide or cover up errors. Evidence indicates that approximately three of every four errors are detected by those committing them, as opposed to being detected by an environmental cue or another person. Therefore, employees need to be able to trust that they can fully report errors without fear of being wrongfully blamed. This provides the agency with the opportunity to learn how to further improve processes and prevent future errors from occurring. For many organizations, the largest barrier in establishing a culture of safety is the establishment of trust. A model called “Just Culture” has successfully been implemented in many agencies to decrease the “blame game,” promote trust, and improve the reporting of errors.
Just Culture
The American Nurses Association (ANA) officially endorses the Just Culture model. In 2019 the ANA published a position statement on Just Culture, stating, “Traditionally, healthcare’s culture has held individuals accountable for all errors or mishaps that befall clients under their care. By contrast, a Just Culture recognizes that individual practitioners should not be held accountable for system failings over which they have no control. A Just Culture also recognizes many individual or ‘active’ errors represent predictable interactions between human operators and the systems in which they work. However, in contrast to a culture that touts ‘no blame’ as its governing principle, a Just Culture does not tolerate conscious disregard of clear risks to clients or gross misconduct (e.g., falsifying a record or performing professional duties while intoxicated).”
The Just Culture model categorizes human behavior into three causes of errors. Consequences of errors are based on whether the error is a simple human error or caused by at-risk or reckless behavior.
- Simple human error: A simple human error occurs when an individual inadvertently does something other than what should have been done. Most medical errors are the result of human error due to poor processes, programs, education, environmental issues, or situations. These errors are managed by correcting the cause, looking at the process, and fixing the deviation. For example, a nurse appropriately checks the rights of medication administration three times, but due to the similar appearance and names of two different medications stored next to each other in the medication dispensing system, administers the incorrect medication to a client. In this example, a root cause analysis reveals a system issue that must be modified to prevent future errors (e.g., change the labelling and storage of look alike-sound alike medication).
- At-risk behavior: An error due to at-risk behavior occurs when a behavioral choice is made that increases risk where the risk is not recognized or is mistakenly believed to be justified. For example, a nurse scans a client’s medication with a barcode scanner prior to administration, but an error message appears on the scanner. The nurse mistakenly interprets the error to be a technology problem and proceeds to administer the medication instead of stopping the process and further investigating the error message, resulting in the wrong dosage of a medication being administered to the client. In this case, ignoring the error message on the scanner can be considered “at-risk behavior” because the behavioral choice was considered justified by the nurse at the time.
- Reckless behavior: Reckless behavior is an error that occurs when an action is taken with conscious disregard for a substantial and unjustifiable risk.[101] For example, a nurse arrives at work intoxicated and administers the wrong medication to the wrong client. This error is considered due to reckless behavior because the decision to arrive intoxicated was made with conscious disregard for substantial risk.
These examples show three different causes of medication errors that would result in different consequences to the employee based on the Just Culture model. Under the Just Culture model, after root cause analysis is completed, system-wide changes are made to decrease factors that contributed to the error. Managers appropriately hold individuals accountable for errors if they were due to simple human error, at-risk behavior, or reckless behaviors.
If an individual commits a simple human error, managers console the individual and consider changes in training, procedures, and processes. In the “simple human error” above, system-wide changes would be made to change the label and location of the medication to prevent future errors from occurring with the same medication.
Individuals committing at-risk behavior are held accountable for their behavioral choice and often require coaching with incentives for less risky behaviors and situational awareness. In the “at-risk behavior” example above where the nurse ignored an error message on the barcode scanner, mandatory training on using a barcode scanner and responding to errors would be implemented, and the manager would track the employee’s correct usage of the barcode scanner for several months following training.
If an individual demonstrates reckless behavior, remedial action and/or punitive action is taken.[102] In the “reckless behavior” example above, the manager would report the nurse’s behavior to the state's Board of Nursing with mandatory substance abuse counseling to maintain their nursing license. Employment may be terminated with consideration of patterns of behavior.
A Just Culture in which employees aren't afraid to report errors is a highly successful way to enhance client safety, increase staff and client satisfaction, and improve outcomes. Success is achieved through good communication, effective management of resources, and an openness to changing processes to ensure the safety of clients and employees. The infographic in Figure 5.4[103] illustrates the components of a culture of safety and Just Culture.
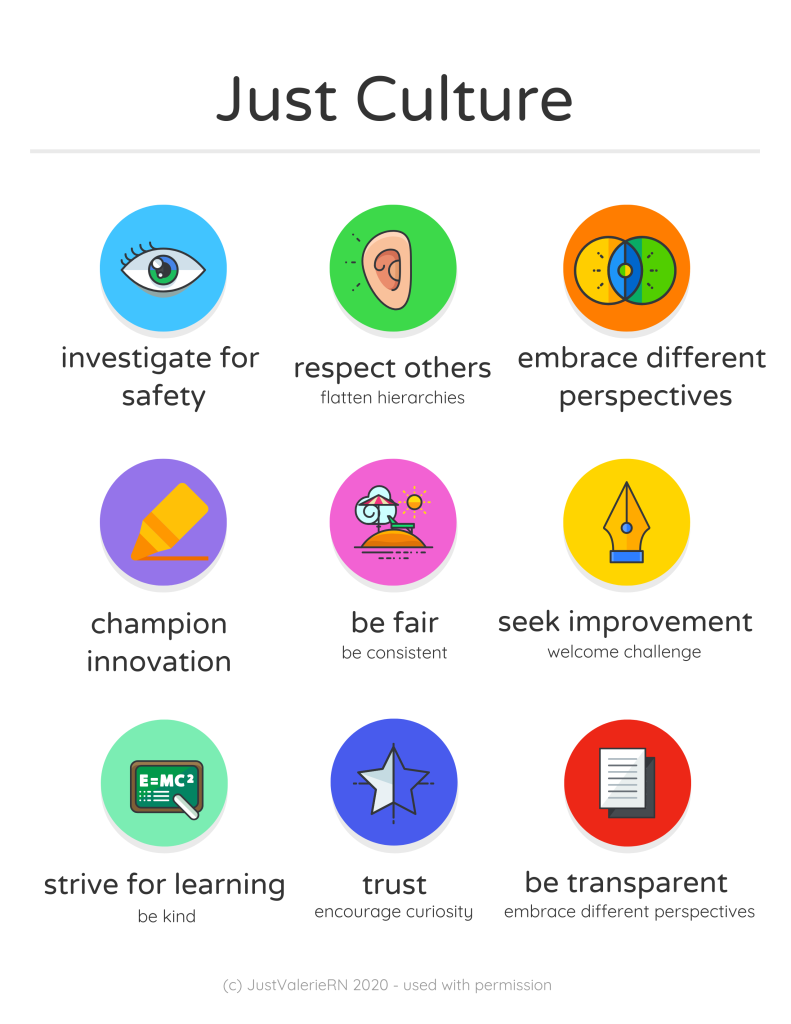
The principles of culture of safety, including Just Culture, Reporting Culture, and Learning Culture are also being adopted in nursing education. It’s understood that mistakes are part of learning and that a shared accountability model promotes individual- and system-level learning for improved client safety. Under a shared accountability model, students are responsible for the following[104]:
- Being fully prepared for clinical experiences, including laboratory and simulation assignments
- Being rested and mentally ready for a challenging learning environment
- Accepting accountability for their part in contributing to a safe learning environment
- Behaving professionally
- Reporting their own errors and near mistakes
- Keeping up-to-date with current evidence-based practice
- Adhering to ethical and legal standards
Students know they will be held accountable for their actions, but will not be blamed for system faults that lie beyond their control. They can trust that a fair process will be used to determine what went wrong if a client care error or near miss occurs. Student errors and near misses are addressed based on an investigation determining if it was simple human error, an at-risk behavior, or reckless behavior. For example, a simple human error by a student can be addressed with coaching and additional learning opportunities to remedy the knowledge deficit. However, if a student acts with recklessness (for example, repeatedly arrives to clinical unprepared despite previous faculty feedback or falsely documents an assessment or procedure), they are appropriately and fairly disciplined, which may include dismissal from the program.[105]
In addition to implementing safety strategies to improve safe client care, leaders of a health care agency must also establish a culture of safety. A culture of safety reflects the behaviors, beliefs, and values within and across all levels of an organization as they relate to safety and clinical excellence, with a focus on people. In 2021 The Joint Commission released a sentinel event regarding the essential role of leadership in establishing a culture of safety. According to The Joint Commission, leadership has an obligation to be accountable for protecting the safety of all health care consumers, including clients, employees, and visitors. Without adequate leadership and an effective culture of safety, there is higher risk for adverse events. Inadequate leadership can contribute to adverse effects in a variety of ways, including, but not limited to, the following[106]:
- Insufficient support of client safety event reporting
- Lack of feedback or response to staff and others who report safety vulnerabilities
- Allowing intimidation of staff who report events
- Refusing to consistently prioritize and implement safety recommendations
- Not addressing staff burnout
Three components of a culture of safety are the following[107]:
- Just Culture: People are encouraged, even rewarded, for providing essential safety-related information, but clear lines are drawn between human error and at-risk or reckless behaviors.
- Reporting Culture: People report errors and near-misses.
- Learning Culture: The willingness and the competence to draw the right conclusions from safety information systems, and the will to implement major reforms when their need is indicated.
The American Nurses Association further describes a culture of safety as one that includes openness and mutual respect when discussing safety concerns and solutions without shifting to individual blame, a learning environment with transparency and accountability, and reliable teams. In contrast, complexity, lack of clear measures, hierarchical authority, the “blame game,” and lack of leadership are examples of barriers that do not promote a culture of safety. If staff fear reprisal for mistakes and errors, they will be less likely to report errors, processes will not be improved, and client safety will continue to be impaired. See the following box for an example of safety themes established during a health care institution’s implementation of a culture of safety.
Safety Themes in a Culture of Safety[108]
Kaiser Permantente implemented a culture of safety in 2001 that focused on instituting the following six strategic themes:
- Safe culture: Creating and maintaining a strong safety culture, with client safety and error reduction embraced as shared organizational values.
- Safe care: Ensuring that the actual and potential hazards associated with high-risk procedures, processes, and client care populations are identified, assessed, and managed in a way that demonstrates continuous improvement and ultimately ensures that clients are free from accidental injury or illness.
- Safe staff: Ensuring that staff possess the knowledge and competence to perform required duties safely and contribute to improving system safety performance.
- Safe support systems: Identifying, implementing, and maintaining support systems—including knowledge-sharing networks and systems for responsible reporting—that provide the right information to the right people at the right time.
- Safe place: Designing, constructing, operating, and maintaining the environment of health care to enhance its efficiency and effectiveness.
- Safe clients: Engaging clients and their families in reducing medical errors, improving overall system safety performance, and maintaining trust and respect.
A strong safety culture encourages all members of the health care team to identify and reduce risks to client safety by reporting errors and near misses so that root cause analysis can be performed and identified risks are removed from the system. However, in a poorly defined and implemented culture of safety, staff often conceal errors due to fear or shame. Nurses have been traditionally trained to believe that clinical perfection is attainable, and that “good” nurses do not make errors. Errors are perceived as being caused by carelessness, inattention, indifference, or uninformed decisions. Although expecting high standards of performance is appropriate and desirable, it can become counterproductive if it creates an expectation of perfection that impacts the reporting of errors and near misses. If employees feel shame when they make an error, they may feel pressure to hide or cover up errors. Evidence indicates that approximately three of every four errors are detected by those committing them, as opposed to being detected by an environmental cue or another person. Therefore, employees need to be able to trust that they can fully report errors without fear of being wrongfully blamed. This provides the agency with the opportunity to learn how to further improve processes and prevent future errors from occurring. For many organizations, the largest barrier in establishing a culture of safety is the establishment of trust. A model called “Just Culture” has successfully been implemented in many agencies to decrease the “blame game,” promote trust, and improve the reporting of errors.
Just Culture
The American Nurses Association (ANA) officially endorses the Just Culture model. In 2019 the ANA published a position statement on Just Culture, stating, “Traditionally, healthcare’s culture has held individuals accountable for all errors or mishaps that befall clients under their care. By contrast, a Just Culture recognizes that individual practitioners should not be held accountable for system failings over which they have no control. A Just Culture also recognizes many individual or ‘active’ errors represent predictable interactions between human operators and the systems in which they work. However, in contrast to a culture that touts ‘no blame’ as its governing principle, a Just Culture does not tolerate conscious disregard of clear risks to clients or gross misconduct (e.g., falsifying a record or performing professional duties while intoxicated).”
The Just Culture model categorizes human behavior into three causes of errors. Consequences of errors are based on whether the error is a simple human error or caused by at-risk or reckless behavior.
- Simple human error: A simple human error occurs when an individual inadvertently does something other than what should have been done. Most medical errors are the result of human error due to poor processes, programs, education, environmental issues, or situations. These errors are managed by correcting the cause, looking at the process, and fixing the deviation. For example, a nurse appropriately checks the rights of medication administration three times, but due to the similar appearance and names of two different medications stored next to each other in the medication dispensing system, administers the incorrect medication to a client. In this example, a root cause analysis reveals a system issue that must be modified to prevent future errors (e.g., change the labelling and storage of look alike-sound alike medication).
- At-risk behavior: An error due to at-risk behavior occurs when a behavioral choice is made that increases risk where the risk is not recognized or is mistakenly believed to be justified. For example, a nurse scans a client’s medication with a barcode scanner prior to administration, but an error message appears on the scanner. The nurse mistakenly interprets the error to be a technology problem and proceeds to administer the medication instead of stopping the process and further investigating the error message, resulting in the wrong dosage of a medication being administered to the client. In this case, ignoring the error message on the scanner can be considered “at-risk behavior” because the behavioral choice was considered justified by the nurse at the time.
- Reckless behavior: Reckless behavior is an error that occurs when an action is taken with conscious disregard for a substantial and unjustifiable risk.[109] For example, a nurse arrives at work intoxicated and administers the wrong medication to the wrong client. This error is considered due to reckless behavior because the decision to arrive intoxicated was made with conscious disregard for substantial risk.
These examples show three different causes of medication errors that would result in different consequences to the employee based on the Just Culture model. Under the Just Culture model, after root cause analysis is completed, system-wide changes are made to decrease factors that contributed to the error. Managers appropriately hold individuals accountable for errors if they were due to simple human error, at-risk behavior, or reckless behaviors.
If an individual commits a simple human error, managers console the individual and consider changes in training, procedures, and processes. In the “simple human error” above, system-wide changes would be made to change the label and location of the medication to prevent future errors from occurring with the same medication.
Individuals committing at-risk behavior are held accountable for their behavioral choice and often require coaching with incentives for less risky behaviors and situational awareness. In the “at-risk behavior” example above where the nurse ignored an error message on the barcode scanner, mandatory training on using a barcode scanner and responding to errors would be implemented, and the manager would track the employee’s correct usage of the barcode scanner for several months following training.
If an individual demonstrates reckless behavior, remedial action and/or punitive action is taken.[110] In the “reckless behavior” example above, the manager would report the nurse’s behavior to the state's Board of Nursing with mandatory substance abuse counseling to maintain their nursing license. Employment may be terminated with consideration of patterns of behavior.
A Just Culture in which employees aren't afraid to report errors is a highly successful way to enhance client safety, increase staff and client satisfaction, and improve outcomes. Success is achieved through good communication, effective management of resources, and an openness to changing processes to ensure the safety of clients and employees. The infographic in Figure 5.4[111] illustrates the components of a culture of safety and Just Culture.
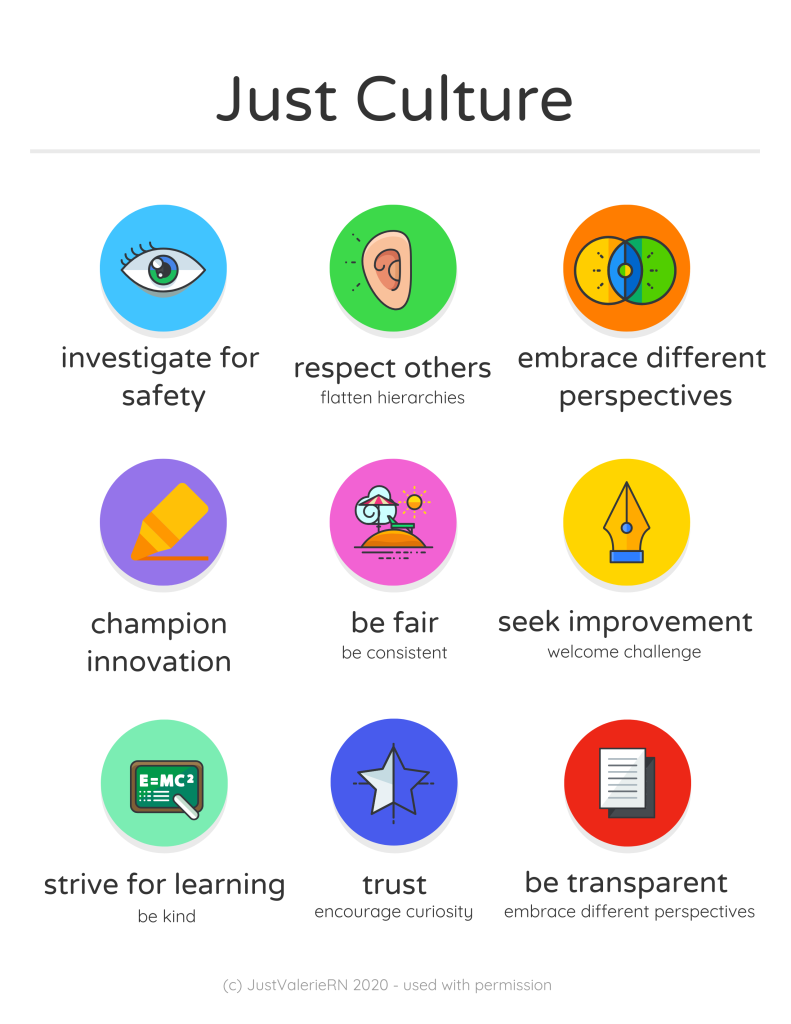
The principles of culture of safety, including Just Culture, Reporting Culture, and Learning Culture are also being adopted in nursing education. It’s understood that mistakes are part of learning and that a shared accountability model promotes individual- and system-level learning for improved client safety. Under a shared accountability model, students are responsible for the following[112]:
- Being fully prepared for clinical experiences, including laboratory and simulation assignments
- Being rested and mentally ready for a challenging learning environment
- Accepting accountability for their part in contributing to a safe learning environment
- Behaving professionally
- Reporting their own errors and near mistakes
- Keeping up-to-date with current evidence-based practice
- Adhering to ethical and legal standards
Students know they will be held accountable for their actions, but will not be blamed for system faults that lie beyond their control. They can trust that a fair process will be used to determine what went wrong if a client care error or near miss occurs. Student errors and near misses are addressed based on an investigation determining if it was simple human error, an at-risk behavior, or reckless behavior. For example, a simple human error by a student can be addressed with coaching and additional learning opportunities to remedy the knowledge deficit. However, if a student acts with recklessness (for example, repeatedly arrives to clinical unprepared despite previous faculty feedback or falsely documents an assessment or procedure), they are appropriately and fairly disciplined, which may include dismissal from the program.[113]

