21.2 Basic Concepts
Open Resources for Nursing (Open RN)
Before discussing specific procedures related to facilitating bowel and bladder function, let’s review basic concepts related to urinary and bowel elimination. When facilitating alternative methods of elimination, it is important to understand the anatomy and physiology of the gastrointestinal and urinary systems, as well as the adverse effects of various conditions and medications on elimination. Use the information below to review information about these topics.
For more information about the anatomy and physiology of the gastrointestinal system and medications used to treat diarrhea and constipation, visit the “Gastrointestinal” chapter of the Open RN Nursing Pharmacology textbook.
For more information about the anatomy and physiology of the kidneys and diuretic medications used to treat fluid overload, visit the “Cardiovascular and Renal System” chapter in Open RN Nursing Pharmacology textbook.
For more information about applying the nursing process to facilitate elimination, visit the “Elimination” chapter in Open RN Nursing Fundamentals.
Urinary Elimination Devices
This section will focus on the devices used to facilitate urinary elimination. Urinary catheterization is the insertion of a catheter tube into the urethral opening and placing it in the neck of the urinary bladder to drain urine. There are several types of urinary elimination devices, such as indwelling catheters, intermittent catheters, suprapubic catheters, and external devices. Each of these types of devices is described in the following subsections.
Indwelling Catheter
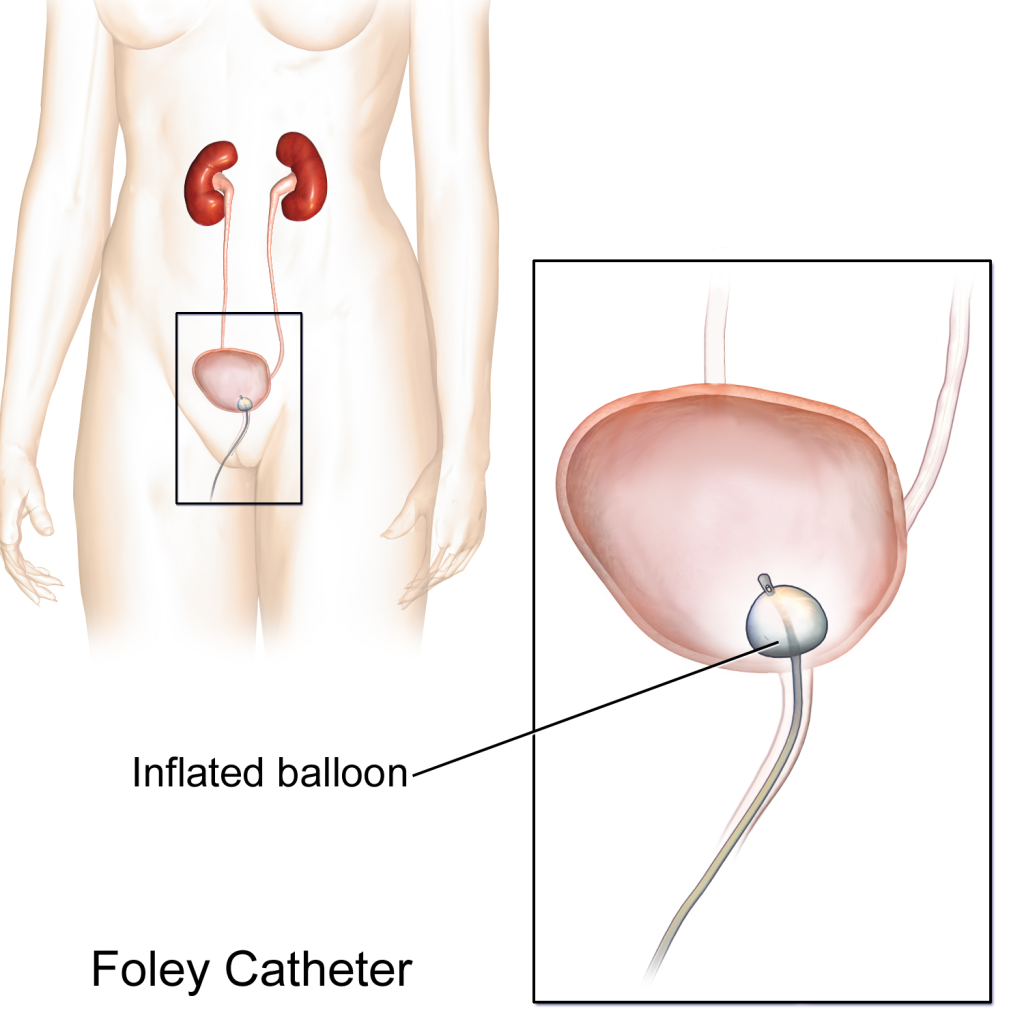
An indwelling catheter, often referred to as a “Foley catheter,” refers to a urinary catheter that remains in place after insertion into the bladder for the continual collection of urine. It has a balloon on the insertion tip to maintain placement in the neck of the bladder. The other end of the catheter is attached to a drainage bag for the collection of urine. See Figure 21.1[1] for an illustration of the anatomical placement of an indwelling catheter in the bladder neck.
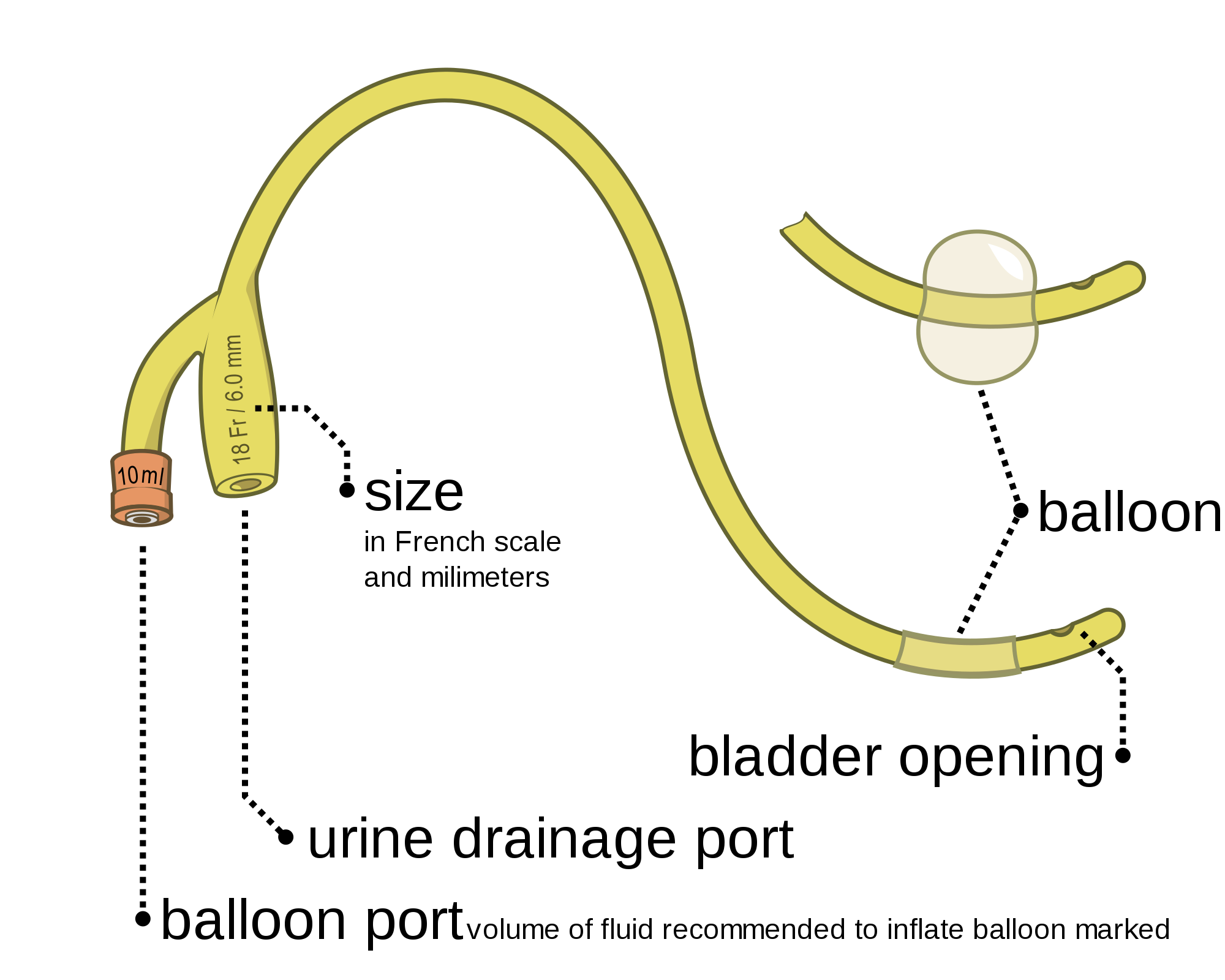
The distal end of an indwelling catheter has a urine drainage port that is connected to a drainage bag. The size of the catheter is marked at this end using the French catheter scale. A balloon port is also located at this end, where a syringe is inserted to inflate the balloon after it is inserted into the bladder. The balloon port is marked with the amount of fluid required to fill the balloon. See Figure 21.2[2] for an image of the parts of an indwelling catheter.
Catheters have different sizes, with the larger the number indicating a larger diameter of the catheter. See Figure 21.3[3] for an image of the French catheter scale.
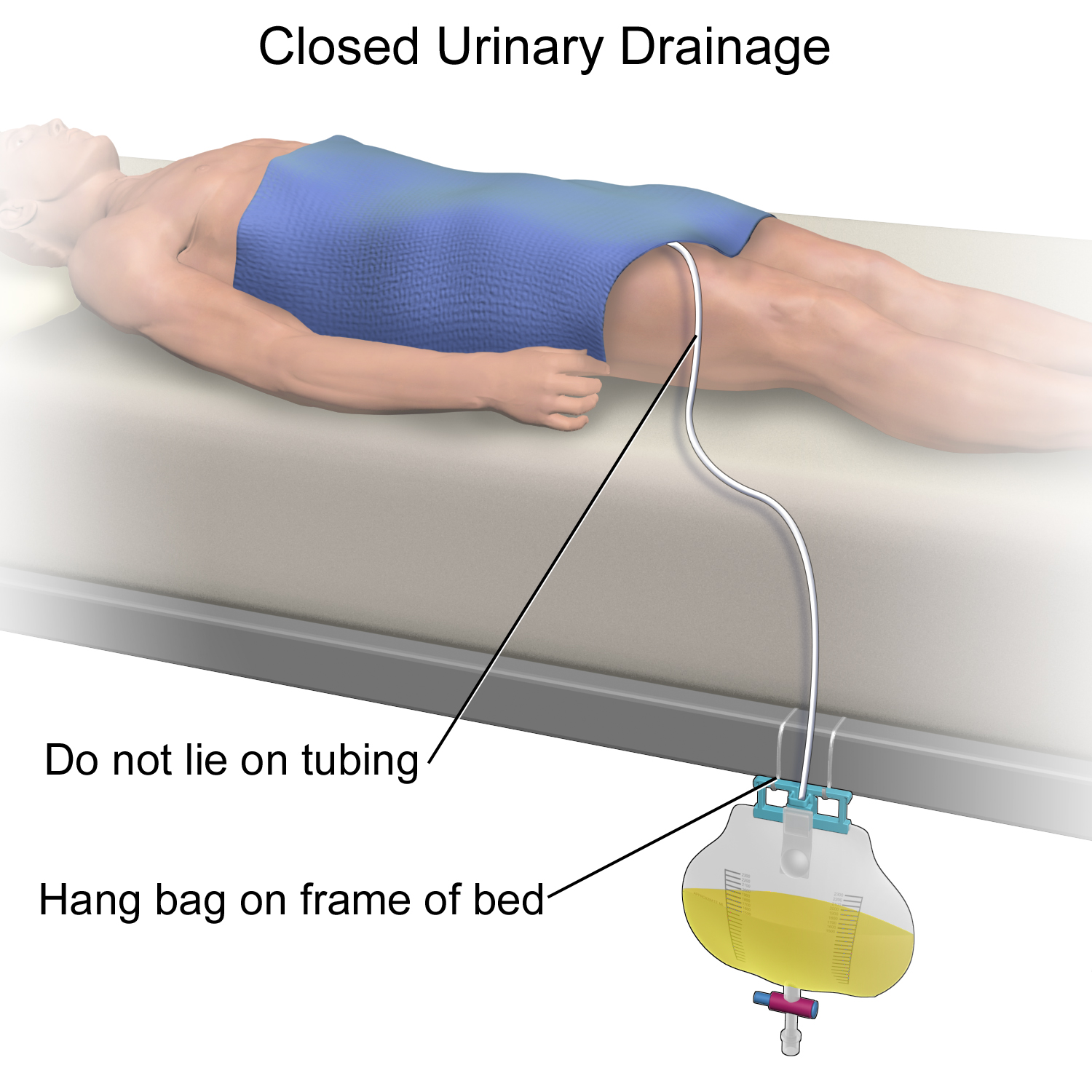
There are two common types of bags that may be attached to an indwelling catheter. During inpatient or long-term care, larger collection bags that can hold up to two liters of fluid are used. See Figure 21.4[4] for an image of a typical collection bag attached to an indwelling catheter. These bags should be emptied when they are half to two-thirds full to prevent traction on the urethra from the bag. Additionally, the collection bag should always be placed below the level of the patient’s bladder so that urine flows out of the bladder and urine does not inadvertently flow back into the bladder. Ensure the tubing is not coiled, kinked, or compressed so that urine can flow unobstructed into the bag. Slack should be maintained in the tubing to prevent injury to the patient’s urethra. To prevent the development of a urinary tract infection, the bag should not be permitted to touch the floor.

See Figure 21.5[5] for an illustration of the placement of the urine collection bag when the patient is lying in bed.
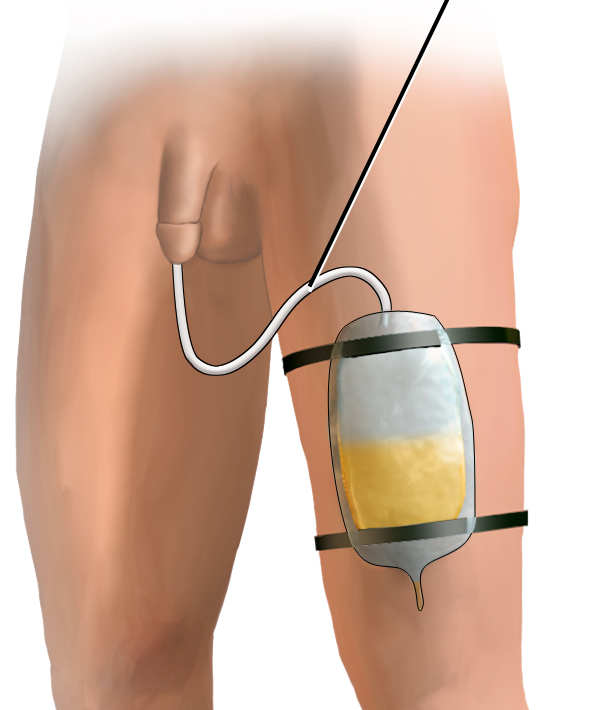
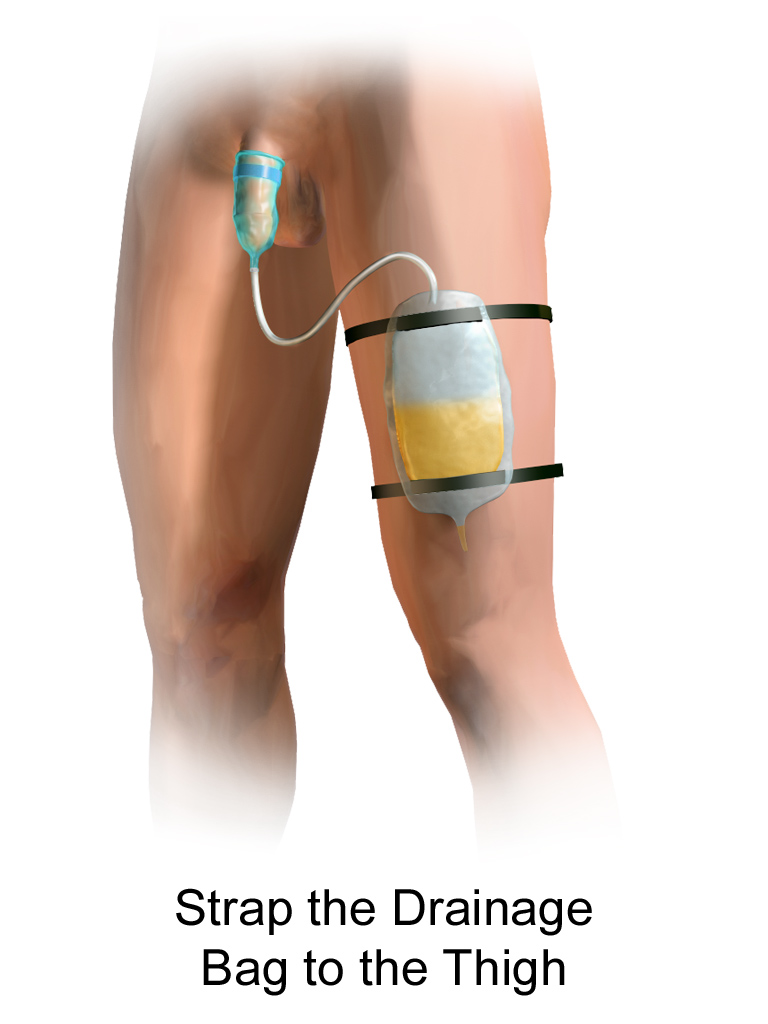
A second type of urine collection bag is a leg bag. Leg bags provide discretion when the patient is in public because they can be worn under clothing. However, leg bags are small and must be emptied more frequently than those used during inpatient care. Figure 21.6[6] for an image of leg bag and Figure 21.7[7] for an illustration of an indwelling catheter attached to a leg bag.

Straight Catheter
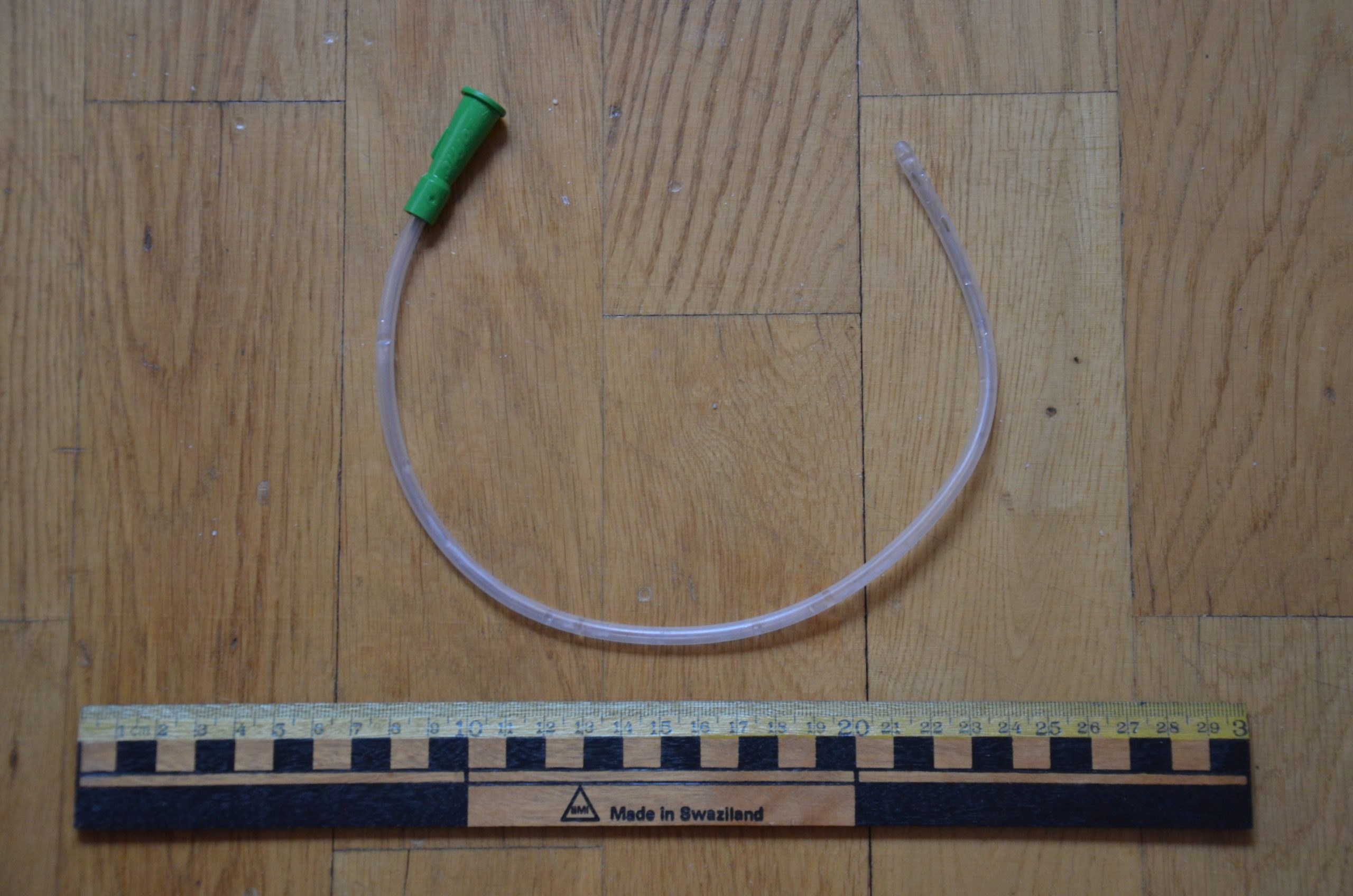
A straight catheter is used for intermittent urinary catheterization. The catheter is inserted to allow for the flow of urine and then immediately removed, so a balloon is not required at the insertion tip. See Figure 21.8[8] for an image of a straight catheter. Intermittent catheterization is used for the relief of urinary retention. It may be performed once, such as after surgery when a patient is experiencing urinary retention due to the effects of anesthesia, or performed several times a day to manage chronic urinary retention. Some patients may also independently perform self-catheterization at home to manage chronic urinary retention caused by various medical conditions. In some situations, a straight catheter is also used to obtain a sterile urine specimen for culture when a patient is unable to void into a sterile specimen cup. According to the Centers for Disease Control and Prevention (CDC), intermittent catheterization is preferred to indwelling urethral catheters whenever feasible because of decreased risk of developing a urinary tract infection.[9]
Other Types of Urinary Catheters
Coude Catheter Tip
Coude catheter tips are curved to follow the natural curve of the urethra during catheterization. They are often used when catheterizing male patients with enlarged prostate glands. See Figure 21.9[10] for an example of a urinary catheter with a coude tip. During insertion, the tip of the coude catheter must be pointed anteriorly or it can cause damage to the urethra. A thin line embedded in the catheter provides information regarding orientation during the procedure; maintain the line upwards to keep it pointed anteriorly.

Irrigation Catheter
Irrigation catheters are typically used after prostate surgery to flush the surgical area. These catheters are larger in size to allow for irrigation of the bladder to help prevent the formation of blood clots and to flush them out. See Figure 21.10[11] for an image comparing a larger 20 French catheter (typically used for irrigation) to a 14 French catheter (typically used for indwelling catheters).

Suprapubic Catheters
Suprapubic catheters are surgically inserted through the abdominal wall into the bladder. This type of catheter is typically inserted when there is a blockage within the urethra that does not allow the use of a straight or indwelling catheter. Suprapubic catheters may be used for a short period of time for acute medical conditions or may be used permanently for chronic conditions. See Figure 21.11[12] for an image of a suprapubic catheter. The insertion site of a suprapubic catheter must be cleaned regularly according to agency policy with appropriate steps to prevent skin breakdown.

Male Condom Catheter
A condom catheter is a noninvasive device used for males with incontinence. It is placed over the penis and connected to a drainage bag. This device protects and promotes healing of the skin around the perineal area and inner legs and is used as an alternative to an indwelling urinary catheter. See Figure 21.12[13] for an image of a condom catheter and Figure 21.13[14] for an illustration of a condom catheter attached to a leg bag.

Female External Urinary Catheter
Female external urinary catheters (FEUC) have been recently introduced into practice to reduce the incidence of catheter-associated urinary tract infection (CAUTI) in women.[15] The external female catheter device is made of a purewick material that is placed externally over the female’s urinary meatus. The wicking material is attached to a tube that is hooked to a low-suction device. When the wick becomes saturated with urine, it is suctioned into a drainage canister. Preliminary studies have found that utilizing the FEUC device reduced the risk for CAUTI.[16],[17]
View these supplementary YouTube videos on female external urinary catheters:
Students demonstrate use of PureWick female external catheter[18]
How to use the use the PureWick – a female external catheter[19]
- “Foley Catheter.png” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- “Foley catheter inflated and deflated EN.svg” by Olek Remesz (wiki-pl: Orem, commons: Orem) is licensed under CC BY-SA 3.0 ↵
- “French catheter scale.gif” by Glitzy queen00 is licensed under CC BY-SA 3.0 ↵
- “DSC_2104.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://ecampusontario.pressbooks.pub/clinicalskills/chapter/2-2-head-to-toe-assessment-checklist/ ↵
- “Closed Urinary Drainage.png” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- “Leg Bag_3I3A0667.jpg” by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Foley Catheter Drainage (cropped).png” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- “Urinary catheter.JPG” by Bengt Oberger is licensed under CC BY-SA 3.0 ↵
- Centers for Disease Control and Prevention. (2015, November 15). Catheter-associated urinary tract infections (CAUTI). https://www.cdc.gov/infectioncontrol/guidelines/cauti/ ↵
- “Self Cath_3I3A0676.jpg” by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Irrigation Catheter and a 14 Fr. Catheter - 3I3A0753.jpg” by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “NewlyPlaceSubprapubic.jpg” by James Heilman, MD is licensed under CC BY-SA 4.0 ↵
- “Male External Cath 1 .jpg” by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Condom Cather Drainage.png” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- Eckert, L., Mattia, L., Patel, S., Okumura, R., Reynolds, P., & Stuiver, I. Reducing the risk of indwelling catheter-associated urinary tract infection in female patients by implementing an alternative female external urinary collection device: A quality improvement project. Journal of Wound Ostomy Continence Nursing, 47(1), 50-53. https://doi.org/10.1097/won.0000000000000601 ↵
- Eckert, L., Mattia, L., Patel, S., Okumura, R., Reynolds, P., & Stuiver, I. Reducing the risk of indwelling catheter-associated urinary tract infection in female patients by implementing an alternative female external urinary collection device: A quality improvement project. Journal of Wound Ostomy Continence Nursing, 47(1), 50-53. https://doi.org/10.1097/won.0000000000000601 ↵
- Glover, E., Bleeker, E., Bauermeister, A., Koehlmoos, A., & Van Whye, M. (2018). External catheters and reducing adverse effects in the female inpatient. Northwestern College Department of Nursing. https://nwcommons.nwciowa.edu/cgi/viewcontent.cgi?article=1026&context=celebrationofresearch ↵
- Madrid, S. (2019, June 19). Purewick [Video]. YouTube. All rights reserved. https://youtu.be/1rnQaHvIMBc ↵
- Newton, C. (2016, August 4). PureWick user instructions [Video]. YouTube. All rights reserved.https://youtu.be/xSOuvcShikw ↵
Answer Key to Chapter 21 Learning Activities
-
- Deflate the balloon, ensure flow of urine, advance the catheter, and attempt reinflation.
- Utilize assistant to help with positioning and holding. Manipulation of the left leg should only occur, and additional personnel may be needed to assist in holding, providing light source, and retracting skin as needed.
- The patient should be encouraged to verbalize feelings related to the colostomy. Body image issues can be a significant concern with new stoma creation. The nurse should ensure that the patient is allowed to voice their feelings, while also reinforcing the measures required to provide care. Education regarding colostomy management can aid in empowerment and facilitate the beginning of normalization. Additionally, it can be helpful to provide guidance on measures for dress to accommodate the colostomy.
- C - Straight catheter
- C - Document the assessment findings of the stoma.
- A - "I should plan to replace the pouch system every 8-10 days."
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 21 Learning Activities
-
- Deflate the balloon, ensure flow of urine, advance the catheter, and attempt reinflation.
- Utilize assistant to help with positioning and holding. Manipulation of the left leg should only occur, and additional personnel may be needed to assist in holding, providing light source, and retracting skin as needed.
- The patient should be encouraged to verbalize feelings related to the colostomy. Body image issues can be a significant concern with new stoma creation. The nurse should ensure that the patient is allowed to voice their feelings, while also reinforcing the measures required to provide care. Education regarding colostomy management can aid in empowerment and facilitate the beginning of normalization. Additionally, it can be helpful to provide guidance on measures for dress to accommodate the colostomy.
- C - Straight catheter
- C - Document the assessment findings of the stoma.
- A - "I should plan to replace the pouch system every 8-10 days."
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 22 Learning Activities
- The items that you should have available include the replacement trach, Ambu bag, and suctioning kit.
- D - Check pulse oximetry, B - Suction patient, C - Provide oxygen via the tracheostomy collar if warranted, A - Assess lung sounds
Answers to interactive elements are given within the interactive element.
| Name | Classification | Description | Indication for Use | Instruction for Use | Other |
|---|---|---|---|---|---|
| Duoderm | Hydrocolloid | Contains gel-forming agents, impermeable to outside contaminants, promotes autolysis, reduces pain, and promotes moist wound healing. | Partial or full-thickness wounds; may be used to hold other dressing in place; avoid use with infections or diabetes. | Cleanse wound. Select dressing 1-2 inches larger than wound, apply light pressure to allow body heat to promote adhesion, change 3-5 days and PRN. | Watch for moisture buildup and odor. |
| Tegaderm | Transparent film | Permeable to oxygen and water vapor, protects from environmental contaminants, nonabsorbent, “second skin.” | PICC/IV site covers, dry wounds, contains moisture in wound when desired. | Cleanse wound. Use skin sealant around edges to hold firm. Change 4-7 days. | Use adhesive remover to remove and protect from skin tears in the elderly. |
| Steri-Strip | Adhesive | Surgical tape. | May be used for linear wound closure or placement after removal of staples or sutures on surgical wounds. | Apply adhesive sealant prior to application.
Apply perpendicular to wound edges to promote closure. |
|
| Tubigrip | Compression wrap/skin cover | Woven elastic fabric. | May be used as compression wrap or protection of skin. | Sizes vary from infant to body wrap. | When used as compression, double layer provides low end compression 15-20mm Hg. |
| Vaseline Gauze | Occlusive gauze | Woven gauze impregnated with petroleum. | May be used as a nonadherent dressing or to keep wounds moist. | Frequent changes.
Cleanse wound prior to each application. |
Watch for bacteria buildup and odor. |
| Xeroform Gauze | Occlusive gauze | Petrolatum impregnated gauze dressing with 3% bismuth tribromophenate. | The bismuth tribromophenate works to reduce wound odor easily.
It also has a nonsticking surface and protects the wound from contamination. Used for surgical incisions, donor sites, skin grafts, and first- and second- degree burns. |
Cleanse wound prior to placement.
Place dressing directly over wound. Cover with appropriate cover/ secondary dressing. |
Helps minimize bacterial buildup. |
| Coban | Elastic wrap | Sticks to itself without need for adhesive, pins, or clips. Wrap stays in place and is lightweight, porous, and comfortable for patients. Reduces pain. | Can be used as compression wrap. Holds primary dressing in place. Can be used to protect skin or medical device. | If using wrap as compression, verify pulse first.
Do not apply compression to infected area or exposed bone/organ. |
Do not tape to skin.
If used as compression, check pulse regularly. May be left in place up to 7 days. |
| Iodosorb Gel | Fiber gel | Absorbing fluids; removing exudate slough, and debris; and forming a gel over the wound surface. As the gel absorbs exudate, iodine is released, killing bacteria and changing color as the iodine is used up. | For use in cleaning wet ulcers and wounds such as venous stasis ulcers, pressure injuries, diabetic foot ulcers, and infected traumatic and surgical wounds. | Cleanse wound. Squeeze gel in shape of wound onto sterile gauze, apply to wound, and hold with secondary dressing. | May be used to eliminate pseudomonas bacteria.
Verify allergies prior to use. |
| 2"x2" Gauze | Gauze | Wound cover. | Cleaning and coverage. | Apply to wound and tape. | Avoid applying tape to skin. |
| 3"x3” 4-ply Nonwoven | Gauze | Wound cover. | Cleaning and coverage. | Apply to wound and tape. | Avoid applying tape to skin. |
| 4"x4” 8-ply Gauze Sponge | Gauze | Wound cover. | Cleaning, coverage, and wet-to-dry. | Apply to wound and tape. | Avoid applying tape to skin. |
| 4"x4” 6-ply Drain Sponge | Gauze | Wound cover, trachea, PEG tube, drain cover/protection. | Use to surround trachea, drain, and PEG tube for protection and drainage absorption. | Cleanse area surrounding tube; apply surrounding the drain site top and bottom. | If applying tape to hold, use minimal tape to protect skin upon removal. |
| 6"x6” Super Sponge (“fluff”) | Gauze | Woven-layered, super absorbent for moderate to large drainage. | Wound cover drainage collection and wet-to-dry. | Cleanse wound. Apply and change as prescribed and wound drainage dictates. | Do not allow drainage-filled gauze to remain on wound surface for extended periods. Promotes bacteria and infection. |
| Abdominal Pad | Gauze | Absorbent of a soft nonwoven outer layer that quickly wicks fluid to a cellulose center. Cellulose quickly absorbs and disperses fluids laterally to prevent pooling. | Wound cover and heavy drainage collection. Keeps moisture off skin. Similar to incontinent pad. | Cleanse wound. Apply as prescribed and wound drainage dictates. | Do not allow drainage-filled pad to remain on wound surface for extended periods. Promotes bacteria and infection. |
| Optilock | Polymer | Super-absorbent polymer core locks in drainage under compression.
Adjusts absorption to the amount of drainage. Protects skin from maceration. Nonadherent wound contact layer. |
Pressure injuries, partial and full-thickness wounds, leg ulcers, lacerations and abrasions, and wounds under compression. | Cleanse wound. Apply to wound bed, and hold in place with tape, wrap, etc.
May be left in place up to 7 days if drainage is minimal. |
Do not allow drainage-filled pad to remain on wound surface for extended periods. Promotes bacteria and infection. |
| Kerlix 4” 6-ply Gauze Roll | Gauze | Prewashed, fluff-dried 100% woven gauze with crinkle-weave pattern for loft and bulk. Provides fast-wicking action, aeration, and absorbency. Comes in large variety of sizes. | Wound cover, wound packing, skin wrap protection, and wet-to-dry. | Cleanse wound and apply. | Change as prescribed. Do not allow drainage-filled gauze to remain on wound surface for extended periods. Promotes bacteria and infection. |
| 4” Stretch Bandage (“Kling”) | Gauze | Nonsterile absorbent gauze roll and stretches and conforms to the body shape and clings to itself as it is wrapped. Conforms to the wound area and offers flexibility to allow for body movement. | May be used to hold dressings in place or wrap for skin protection. | Apply as needed. | Avoid applying tape to skin. Apply tape to Kling to hold.
Comes in large variety of sizes. |
| Adaptic | Contact layer | Nonadhering dressing, primary wound contact dressing designed to minimize wound adherence and prevent maceration. Mesh impregnated with a specially formulated petroleum emulsion, and easy to remove and minimizes pain. | Dry to heavily exuding wounds for which adherence of dressing and exudate is to be prevented. | Cleanse wound. Apply to wound, apply primary dressing, and hold with appropriate dressing or tape. | May be used as a contact layer with wound VAC foam or cover skin tears. |
| Telfa | Composite | Made of cotton fabric with a perforated seal of polyester resin. This perforated seal acts as a nonadherent, preventing the dressing from sticking to the wound and/or acting as a barrier between the wound and excretions. | Covers cuts and abrasions. It is also used to prevent infection to sutured wounds and as an absorbent dressing for wound secretions. | Cleanse wound and apply as primary or secondary (contact) layer.
May be used with topical medications. |
Change daily or when saturated. |
| ¼” Plain Packing Strip | Gauze | 100% cotton, fine mesh gauze ideal for wet-to-dry packing.
Available in plain and iodoform (antiseptic). |
Used for packing or as drainage conduits in nasal, sinus, or tunnel packing. | Cleanse wound. Apply as packing or filler in wound tunnel, nasal passage, or sinus cavity. | Change daily or as prescribed.
Do not cut in small pieces to avoid not being able to locate them for removal. |
| Aquacel Ag (also comes as plain hydrofiber with no additives) | Hydrofiber | Primary wound dressing made from sodium carboxymethylcellulose. Textile fiber and presented in the form of fleece held together by a needle bonding process and is available both as a "ribbon” for packing cavities and as a flat nonwoven pad for application to larger open wounds. Fiber turns to gel when moistened by drainage. | Primary wound dressing to absorb large amounts of drainage. Silver component is antimicrobial. The dressing is easy to remove without causing pain or trauma and leaves minimal residue on the surface of the wound. | Cleanse wound. Apply to surface or lightly pack into wound.
Cover with secondary dressing. |
Some patients may be sensitive to silver.
Silver must remain in place for at least 24 hours to be effective. Change frequency as prescribed by physician. |
| Hydrofera Blue | Antimicrobial foam | Pulls bacteria-laden exudate up and away from the wound, which may facilitate healing. Provides a protective antibacterial cover that inhibits the growth of microorganisms. Foam impregnated with methylene blue. | Pressure injuries, diabetic ulcers, venous stasis ulcers, arterial ulcers, superficial burns, donor sites, post-surgical incisions, trauma wounds, abrasions, and lacerations. | Cleanse wound.
Moisten foam with saline or sterile water. Ring out excess moisture. Apply to wound and hold with occlusive cover (Tegaderm, Duoder). |
Hydrofera Blue foam is effective against microorganisms commonly found in wounds, including MRSA, VRE, and Candida. |
| Polymem (Pink)
Polymem (Silver) |
Foam | Polymem contains a mild, nonionic, nontoxic, tissue-friendly cleansing agent, activated by moisture that is gradually released into the wound bed.
Built-in cleansing capabilities reduce the need to cleanse wounds during dressing changes, which can disrupt the growth of healthy tissue as the wounds heals. Wicks away up to ten times its weight in exudate. The absorption capability activates only if the material detects exudate. Nonstick surface to reduce pain and tissue loss during removal. |
Wounds with small to moderate drainage.
Pressure injuries, diabetic ulcers, venous stasis ulcers, arterial ulcers, superficial burns, donor sites, post-surgical incisions, trauma wounds, abrasions, and lacerations. |
Cleanse wound. Place uncut foam directly on wound. Hold with nonocclusive dressing to allow for moisture evaporation.
May use Kerlix, Kling, or Tubigrip to hold in place. |
May be changed daily or weekly depending on drainage amount.
Silver is most effective when left in place > 24 hours. Some patients complain of pain with use of silver. |
| Aquacel Ag Foam | Foam | Absorbs wound fluid and creates a soft gel, maintaining a moist wound environment. Locks in exudates through vertically wicking, reducing the risk of maceration. Helps minimize pain while in place and during dressing changes. | Wounds with small to moderate drainage. Pressure injuries, diabetic ulcers, venous stasis ulcers, arterial ulcers, superficial burns, donor sites, post-surgical incisions, trauma wounds abrasions, and lacerations. | Cleanse wound. Place uncut foam directly on wound. Hold with nonocclusive dressing to allow for moisture evaporation.
May use Kerlix, Kling, or Tubigrip to hold in place. |
May be changed daily or weekly depending on drainage amount.
Sliver is most effective when left in place > 21 hours. Some patients complain of pain with use of silver. |
| Lyofoam | Foam | Management of moderately to highly exuding wounds. Its high absorbency and fluid-handling capacity, combined with the reduced risk of maceration and leakage, provide a longer wear time. Waterproof backing film acts as a barrier to bacterial and viral penetration. Works under compression. | Moderate to heavy draining wounds. Pressure injuries, diabetic ulcers, venous stasis ulcers, arterial ulcers, superficial burns, donor sites, post-surgical incisions, trauma wounds, abrasions, and lacerations. | Cleanse wound. Place uncut foam directly on wound. Hold with nonocclusive dressing to allow for moisture evaporation.
May use Kerlix, Kling, or Tubigrip to hold in place. |
Monitor dressing frequently and change when saturated with drainage. |
| Mepilex Border | Foam | Absorbs and retains exudate and maintains a moist wound environment. The Safetac® layer seals the wound edges, preventing the exudate from leaking onto the surrounding skin, which minimizes the risk for maceration. The Safetac® layer ensures that the dressing can be changed without damaging the wound or surrounding skin or exposing the patient to additional pain. | For moderate to high exuding wounds, such as pressure injuries, leg and foot ulcers, traumatic wounds, and other secondary healing wounds.
May also be used for skin and pressure injury protection/prevention. |
Clean the wound prior to applying a dressing.
The dressing should overlap the wound bed by at least 2 cm onto the surrounding skin. |
Adhesive border is designed to be peeled back to view wound and reseal multiple times. Monitor wound frequently.
Comes in a variety of sizes. |
| Mepilex Border Ag | Foam | Silver has been added. Silver kills bacteria and might be used both for preventing infection and also on wounds with signs of local infection. The Safetac® layer ensures that the dressing can be changed without damaging the wound or surrounding skin or exposing the patient to additional pain. | For moderate to high exuding wounds, such as pressure injuries, leg and foot ulcers, traumatic wounds, and other secondary healing wounds. | Clean the wound prior to applying a dressing.
The dressing should overlap the wound bed by at least 2 cm onto the surrounding skin. |
Adhesive border is designed to be peeled back to view wound and reseal multiple times. Monitor wound frequently.
Comes in a variety of sizes. Mepilex surgical dressing has a super adhesive border and remains in place for 7-10 days. Some patients complain of pain with use of silver. |
| KCI Granufoam Black | Negative Pressure Wound Therapy (NPWT) | Promotes wound healing through Negative Pressure Wound Therapy (NPWT). This helps draw wound edges together, remove infectious materials, and actively promote granulation. By MD order. | Do not place foam dressings directly in contact with exposed blood vessels, anastomotic sites, organs, or nerves. | Detailed instruction for use available online at the myKCI website. | Consider pain control prior to application and removal. |
Learning Activities
(Answers to "Learning Activities" can be found in the '"Answer Key'" at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
1. Your patient turns on their call light. Upon entering your patient’s room, they say they are short of breath. Prioritize your actions from first to sixth.
Institute actions to improve oxygenation
Apply oxygen as ordered
Reassess pulse oximetry
Teach oxygen safety
Assess lung sounds
Assess pulse oximetry
| Priority | Actions |
|---|---|
| First | |
| Second | |
| Third | |
| Four | |
| Fifth | |
| Sixth |
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 11, Assignment 1.
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 11, Assignment 2.
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 11, Assignment 3.

