20.3 Assessing Wounds
Open Resources for Nursing (Open RN)
Wounds should be assessed and documented at every dressing change. Wound assessment should include the following components:
- Anatomic location
- Type of wound (if known)
- Degree of tissue damage
- Wound bed
- Wound size
- Wound edges and periwound skin
- Signs of infection
- Pain[1]
These components are further discussed in the following sections.
Anatomic Location and Type of Wound
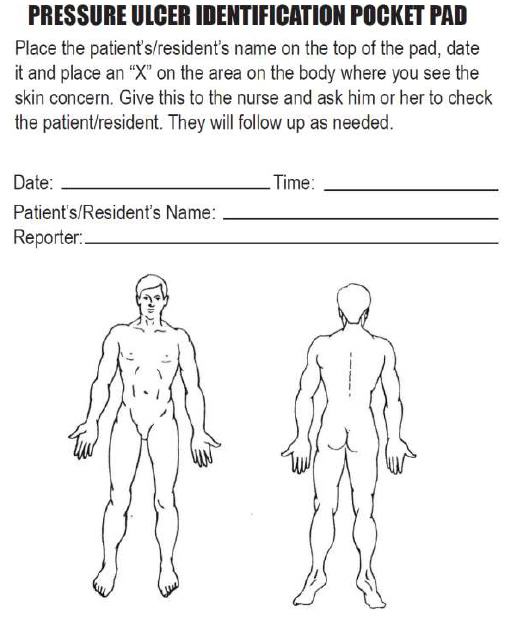
The location of the wound should be documented clearly using correct anatomical terms and numbering. This will ensure that if more than one wound is present, the correct one is being assessed and treated. Many agencies use images to facilitate communication regarding the location of wounds among the health care team. See Figure 20.16[2] for an example of facility documentation that includes images to indicate wound location.
The location of a wound also provides information about the cause and type of a wound. For example, a wound over the sacral area of an immobile patient is likely a pressure injury, and a wound near the ankle of a patient with venous insufficiency is likely a venous ulcer. For successful healing, different types of wounds require different treatments based on the cause of the wound.
Degree of Tissue Damage
It is important to continually assess the degree of tissue damage in pressure injuries because the level of damage can worsen if they are not treated appropriately. Refer to the “Staging” subsection of “Pressure Injuries” in the “Basic Concepts Related to Wounds” section for more information about tissue damage.
Wound Base
Assess the color of the wound base. Recall that healthy granulation tissue appears pink due to the new capillary formation. It is moist, painless to the touch, and may appear “bumpy.” Conversely, unhealthy granulation tissue is dark red and painful. It bleeds easily with minimal contact and may be covered with biofilm. The appearance of slough (yellow) or eschar (black) in the wound base should be documented and communicated to the health care provider because it likely will need to be removed for healing. Tunneling and undermining should also be assessed, documented, and communicated.
Type and Amount of Exudate
The color, consistency, and amount of exudate (drainage) should be assessed and documented at every dressing change. The amount of drainage from wounds is categorized as scant, small/minimal, moderate, or large/copious. Use the following descriptions to select the appropriate terms[3]:
- No exudate: The wound base is dry.
- Scant amount of exudate: The wound is moist, but no measurable amount of exudate appears on the dressing.
- Minimal amount of exudate: Exudate covers less than 25% of the size of the bandage.
- Moderate amount of drainage: Wound tissue is wet, and drainage covers 25% to 75% of the size of the bandage.
- Large or copious amount of drainage: Wound tissue is filled with fluid, and exudate covers more than 75% of the bandage.[4]
The type of wound drainage should be described using medical terms such as serosanguinous, sanguineous, serous, or purulent.
- Sanguineous: Sanguineous exudate is fresh bleeding.[5]
- Serous: Serous drainage is clear, thin, watery plasma. It’s normal during the inflammatory stage of wound healing, and small amounts are considered normal wound drainage.[6]
- Serosanguinous: Serosanguineous exudate contains serous drainage with small amounts of blood present.[7]
- Purulent: Purulent exudate is thick and opaque. It can be tan, yellow, green, or brown. It is never considered normal in a wound bed, and new purulent drainage should always be reported to the health care provider.[8] See Figure 20.17[9] for an image of purulent drainage.

Wound Size
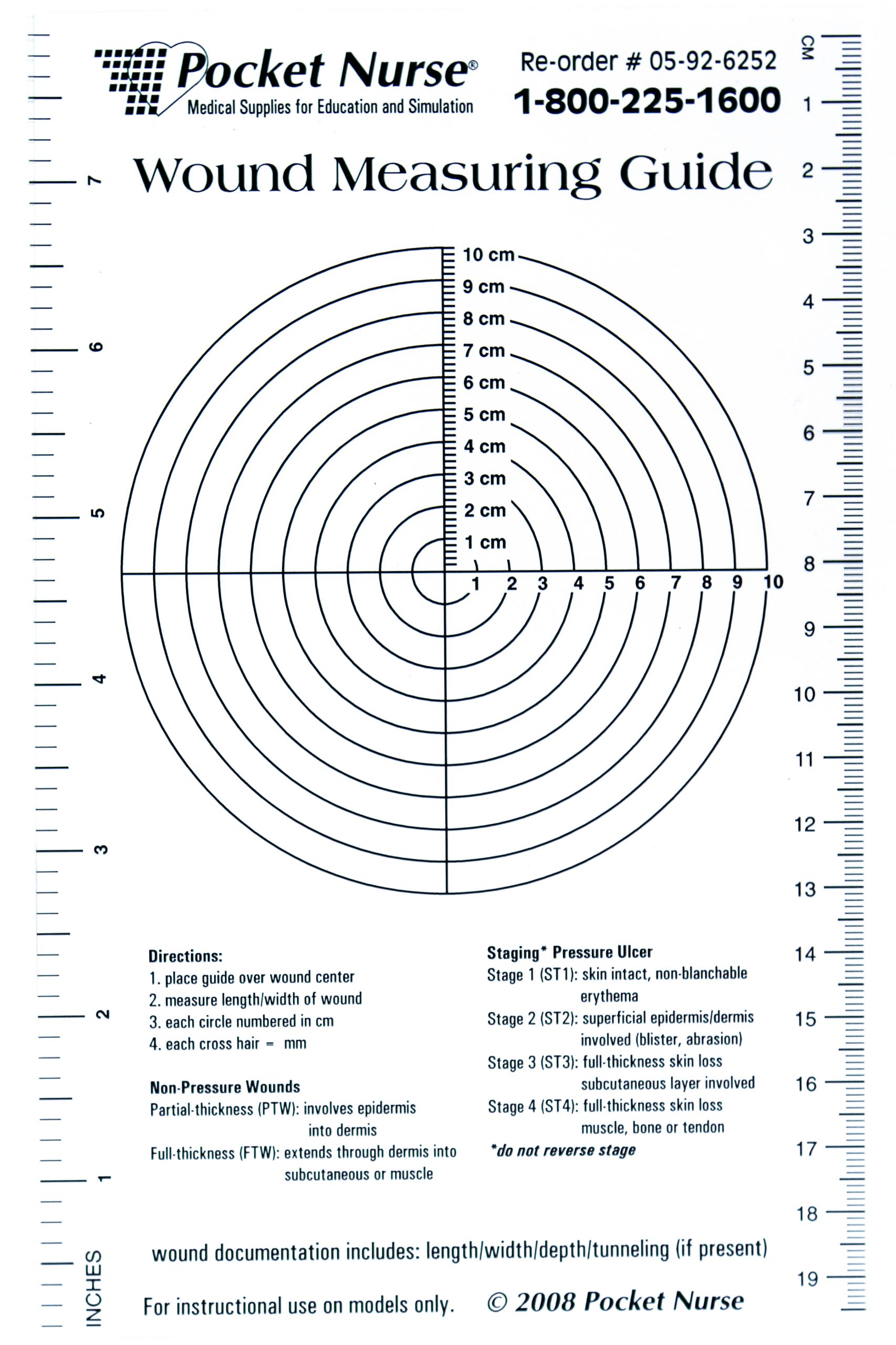
Wounds should be measured on admission and during every dressing change to evaluate for signs of healing. Accurate wound measurements are vital for monitoring wound healing. Measurements should be taken in the same manner by all clinicians to maintain consistent and accurate documentation of wound progress. This can be difficult to accomplish with oddly shaped wounds because there can be confusion about how consistently to measure them. Wounds should be described by length by width, with the length of the wound based on the head-to-toe axis. The width of a wound should be measured from side to side laterally. If a wound is deep, the deepest point of the wound should be measured to the wound surface using a sterile, cotton-tipped applicator. Many facilities use disposable, clear plastic measurement tools to measure the area of a wound healing by secondary intention. Measurements are typically documented in centimeters. See Figure 20.18[10] for an image of a wound measurement tool.
Tunneling can occur in a full-thickness wound that can lead to abscess formation. The depth of a tunneling can be measured by gently probing the tunneled area with a sterile, cotton-tipped applicator from the wound base to the end of the tract. When probing a tunnel, it is imperative to not force the swab but only insert until resistance is felt to prevent further damage to the area. The location of the tunnel in the wound should be documented using the analogy of a clock face, with 12:00 pointing toward the patient’s head.[11]
Undermining occurs when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound’s edge. Undermining is measured by inserting a probe under the wound edge directed almost parallel to the wound surface until resistance is felt. The amount of undermining is the distance from the probe tip to the point at which the probe is level with the wound edge. Clock terms are also used to identify the area of undermining.[12]
Wound Edges and Periwound Skin
If the wound is healing by primary intention, it should be documented if the wound edges are well-approximated (closed together) or if there are any signs of dehiscence. The skin outside the outer edges of the wound, called the periwound skin, provides information related to wound development or healing. For example, a venous ulcer often has excess wound drainage that macerates the periwound skin, giving it a wet, waterlogged appearance that is soft and grayish white in color.[13] See Figure 20.19[14] for an image of erythematous periwound with partial dehiscence.

Signs of Infection
Wounds should be continually monitored for signs of infection. Signs of localized wound infection include erythema (redness), induration (area of hardened tissue), pain, edema, purulent exudate (yellow or green drainage), and wound odor.[15] New signs of infection should be reported to the health care provider with an anticipated order for a wound culture.
Pain
The intensity of pain that a patient is experiencing with a wound should be assessed and documented. If a patient experiences pain during dressing changes, it should be managed with administration of pain medication before scheduled dressing changes. Be aware that the degree of pain may not correlate to the extent of tissue damage. For example, skin tears are often painful because the nerve endings are exposed in the dermal layer, whereas patients with severe diabetic ulcers on their feet may experience little or no pain because of existing neuropathic damage.[16]
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- “putool7bfig.jpg” by unknown is in the Public Domain. Access for free at https://www.ahrq.gov/patient-safety/settings/hospital/resource/pressureulcer/tool/pu7b.html ↵
- Wound Care Advisor. (n.d.). Exudate amounts. https://woundcareadvisor.com/exudate-amounts/#:~:text=Small%20or%20minimal%20amount%20of,than%2075%25%20of%20the%20bandage ↵
- Wound Care Advisor. (n.d.). Exudate amounts. https://woundcareadvisor.com/exudate-amounts/#:~:text=Small%20or%20minimal%20amount%20of,than%2075%25%20of%20the%20bandage ↵
- Wound Care Advisor. (n.d.). Exudate amounts. https://woundcareadvisor.com/exudate-amounts/#:~:text=Small%20or%20minimal%20amount%20of,than%2075%25%20of%20the%20bandage ↵
- Wound Care Advisor. (n.d.). Exudate amounts. https://woundcareadvisor.com/exudate-amounts/#:~:text=Small%20or%20minimal%20amount%20of,than%2075%25%20of%20the%20bandage ↵
- Wound Care Advisor. (n.d.). Exudate amounts. https://woundcareadvisor.com/exudate-amounts/#:~:text=Small%20or%20minimal%20amount%20of,than%2075%25%20of%20the%20bandage ↵
- Wound Care Advisor. (n.d.). Exudate amounts. https://woundcareadvisor.com/exudate-amounts/#:~:text=Small%20or%20minimal%20amount%20of,than%2075%25%20of%20the%20bandage ↵
- “Purulant knee aspirate.JPG” by James Heilman, MD is licensed under CC BY 3.0 ↵
- “Sample Wound Measuring Guide.jpg” by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- WoundEducators.com. (2016, July 1). Wound undermining. https://woundeducators.com/measure-wound-undermining/#:~:text=Wound%20undermining%20occurs%20when%20the,surface%20until%20resistance%20is%20felt ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- “Post operative wound.JPG” by Intermedichbo is licensed under CC BY-SA 3.0 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
Demographic and biographic data includes basic characteristics about the patient, such as their name, contact information, birthdate, age, gender and preferred pronouns, allergies, languages spoken and preferred language, relationship status, occupation, and resuscitation status.[1] See Table 2.4a for sample focused questions used to gather demographic and biological data.
Table 2.4a Demographic and Biological Data
| Data | Focused Interview Questions |
|---|---|
| Name
Contact Information Emergency Contact Information |
What is your full name?
What do you prefer to be called? What is your address? What is your phone number? Whom can we contact in an emergency? What is their relationship to you? At what number can we contact them? |
| Birthdate
Age |
What is your birthdate?
What is your current age? |
| Gender | What is your biological gender?
With what gender do you identify? What are your preferred pronouns (he/him/his, she/her/hers, them/they/theirs, etc.)? |
| Allergies | Do you have any allergies?
How do you react to each allergen? |
| Preferred Language | What is your primary language that you prefer to speak?
Note: If English is not their primary language, offer to obtain a medical interpreter as needed. |
| Relationship Status | Tell me about your relationship status.
*Avoid questions that imply expected behaviors, such as:
|
| Occupation and Education | What is your occupation?
Where do you work or go to school? What is the highest level of education you have completed? |
| Resuscitation Status | Have you considered preferences for resuscitation if your heart stops or you stop breathing, also called CPR?
Do you have any advance directives on file with a hospital or provider, such as a “Living Will” or “Power of Attorney for Health Care”? Would you like more information about advance directives? |
See Table 2.4b for a sample demographic form used during a complete health history.
Table 2.4b Sample Demographic Form[2]
|
Demographic Information Form Interview Date: Patient Name: Address: Emergency Contact Name: Relationship:
Date of Birth: Age: Sex: Male / Female / Another Option Gender You Self-Identify With: Preferred Pronouns:
Allergies:
Primary Language: Interpreter needed: Yes / No
Relationship Status:
Occupation/Education:
Resuscitation Status:
Information from: Patient / Other Patient Accompanied: Yes / No Details: |
|---|
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activities are provided as immediate feedback.)
Ethical Application & Reflection Activity
Case A
Filmmaker Lulu Wang first shared a story about her grandmother on This American Life podcast and later turned it into the 2019 movie The Farewell starring Awkwafina. Both share the challenges of a Chinese-born but U.S.-raised woman returning to China and a family who has chosen to not disclose that the grandmother has been given a Stage IV lung cancer diagnosis and three months to live. Listen to the podcast and then answer the following questions:
585: In Defense of Ignorance Act One: What You Don't Know
1. Reflect on the similarities and differences of your family culture with that of the Billi family. Consider things such as what family gatherings, formal and informal, look like and spoken and unspoken rules related to communication and behavior.
2. The idea of “good” lies and “bad” lies is introduced in the podcast. Nai Nai’s family supports the decision to not tell her about her Stage IV lung cancer, stage a wedding as the excuse to visit and say their goodbyes, and even alter a medical report as good lies necessary to support her mental health, well-being, and happiness. Is the family applying deontological or utilitarian ethics to the situation? Defend your response.
3. Define the following ethical principles and identify examples from this story:
- Autonomy
- Beneficence
- Nonmaleficence
- Paternalism
4. Imagine this story is happening in the United States rather than China and you are the nurse admitting Nai Nai to an inpatient oncology unit. Using the ethical problem-solving model of your choice, identify and support your solution to the ethical dilemma posed when her family requests that Nai Nai not be told that she has cancer.
Ethical Application & Reflection Activity
Case B
You are caring for a 32-year-old client who has been in a persistent vegetative state for many years. There is an outdated advanced directive that is confusing on the issue of food and fluids, though clear about not wanting to be on a ventilator if she were in a coma. Her husband wants the feeding tube removed but is unable to say that it would have been the client’s wish. He says that it is his decision for her. Her two adult siblings and parents reject this as a possibility because they say that “human life is sacred” and that the daughter believed this. They say their daughter is alive and should receive nursing care, including feeding. The health care team does not know what to do ethically and fear being sued by either the husband, siblings, or the parents. What do you need to know about this clinical situation? What are the values and obligations at stake in this case? What values or obligations should be affirmed and why? How might that be done?
1. Define the problem.
2. List what facts/information you have.
3. What are the stakeholders' positions?
- Patient:
- Spouse:
- Family:
- Health Care Team:
- Facility:
- Community:
4. How might the stakeholders' values differ?
5. What are your values in this situation?
6. Do your values conflict with those of the patient? Describe.

Test your knowledge using this NCLEX Next Generation-style Case Study. You may reset and resubmit your answers to this question an unlimited number of times.[3]
Demographic and biographic data includes basic characteristics about the patient, such as their name, contact information, birthdate, age, gender and preferred pronouns, allergies, languages spoken and preferred language, relationship status, occupation, and resuscitation status.[4] See Table 2.4a for sample focused questions used to gather demographic and biological data.
Table 2.4a Demographic and Biological Data
| Data | Focused Interview Questions |
|---|---|
| Name
Contact Information Emergency Contact Information |
What is your full name?
What do you prefer to be called? What is your address? What is your phone number? Whom can we contact in an emergency? What is their relationship to you? At what number can we contact them? |
| Birthdate
Age |
What is your birthdate?
What is your current age? |
| Gender | What is your biological gender?
With what gender do you identify? What are your preferred pronouns (he/him/his, she/her/hers, them/they/theirs, etc.)? |
| Allergies | Do you have any allergies?
How do you react to each allergen? |
| Preferred Language | What is your primary language that you prefer to speak?
Note: If English is not their primary language, offer to obtain a medical interpreter as needed. |
| Relationship Status | Tell me about your relationship status.
*Avoid questions that imply expected behaviors, such as:
|
| Occupation and Education | What is your occupation?
Where do you work or go to school? What is the highest level of education you have completed? |
| Resuscitation Status | Have you considered preferences for resuscitation if your heart stops or you stop breathing, also called CPR?
Do you have any advance directives on file with a hospital or provider, such as a “Living Will” or “Power of Attorney for Health Care”? Would you like more information about advance directives? |
See Table 2.4b for a sample demographic form used during a complete health history.
Table 2.4b Sample Demographic Form[5]
|
Demographic Information Form Interview Date: Patient Name: Address: Emergency Contact Name: Relationship:
Date of Birth: Age: Sex: Male / Female / Another Option Gender You Self-Identify With: Preferred Pronouns:
Allergies:
Primary Language: Interpreter needed: Yes / No
Relationship Status:
Occupation/Education:
Resuscitation Status:
Information from: Patient / Other Patient Accompanied: Yes / No Details: |
|---|

