23.8 Functional Health and Activities of Daily Living
Open Resources for Nursing (Open RN)
Functional health assessment collects data related to the patient’s functioning and their physical and mental capacity to participate in Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs). Activities of Daily Living (ADLs) are daily basic tasks that are fundamental to everyday functioning (e.g., hygiene, elimination, dressing, eating, ambulating/moving). See Figure 2.2[1] for an illustration of ADLs.

Instrumental Activities of Daily Living (IADL) are more complex daily tasks that allow patients to function independently such as managing finances, paying bills, purchasing and preparing meals, managing one’s household, taking medications, and facilitating transportation. See Figure 2.3[2] for an illustration of IADLs. Assessment of IADLs is particularly important to inquire about with young adults who have just moved into their first place, as well as with older patients with multiple medical conditions and/or disabilities.

Information obtained when assessing functional health provides the nurse a holistic view of a patient’s human response to illness and life conditions. It is helpful to use an assessment framework, such as Gordon’s Functional Health Patterns,[3] to organize interview questions according to evidence-based patterns of human responses. Using this framework provides the patient and their family members an opportunity to identify health-related concerns to the nurse that may require further in-depth assessment. It also verifies patient understanding of conditions so that misperceptions can be clarified. This framework includes the following categories:
- Nutritional-Metabolic: Food and fluid consumption relative to metabolic need
- Elimination: Excretion including bowel and bladder
- Activity-Exercise: Activity and exercise
- Sleep-Rest: Sleep and rest
- Cognitive-Perceptual: Cognition and perception
- Role-Relationship: Roles and relationships
- Sexuality-Reproductive: Sexuality and reproduction
- Coping-Stress Tolerance: Coping and effectiveness of managing stress
- Value-Belief: Values, beliefs, and goals that guide choices and decisions
- Self-Perception and Self-Concept: Self-concept and mood state[4]
- Health Perception-Health Management: A patient’s perception of their health and well-being and how it is managed. This is an umbrella category of all the categories above and underlies performing a health history.
The functional health section can be started by saying, “I would like to ask you some questions about factors that affect your ability to function in your day-to-day life. Feel free to share any health concerns that come to mind during this discussion.” Focused interview questions for each category are included in Table 2.8. Each category is further described below.
Nutrition
The nutritional category includes, but is not limited to, food and fluid intake, usual diet, financial ability to purchase food, time and knowledge to prepare meals, and appetite. This is also an opportune time to engage in health promotion discussions about healthy eating. Be aware of signs for malnutrition and obesity, especially if rapid and excessive weight loss or weight gain have occurred.
Life Span Considerations
When assessing nutritional status, the types of questions asked and the level of detail depend on the developmental age and health of the patient. Family members may also provide important information.
- Infants: Ask parents about using breast milk or formula, amount, frequency, supplements, problems, and introductions of new foods.
- Pregnant women: Include questions about the presence of nausea and vomiting and intake of folic acid, iron, omega-3 fatty acids, vitamin D, and calcium.
- Older adults or patients with disabling illnesses: Inquire about the ability to purchase and cook their food, decreased sense of taste, ability to chew or swallow foods, loss of appetite, and enough fiber and nutrients.[5]
Elimination
Elimination refers to the removal of waste products through the urine and stool. Health care professionals refer to urinating as voiding and stool elimination as having a bowel movement. Familiar terminology may need to be used with patients, such as “pee” and “poop.”
Constipation commonly occurs in hospitalized patients, so it is important to assess the date of their last bowel movement and monitor the frequency, color, and consistency of their stool.
Assess urine concentration, frequency, and odor, especially if concerned about urinary tract infection or incontinence. Findings that require further investigation include dysuria (pain or difficulty upon urination), blood in the stool, melena (black, tarry stool), constipation, diarrhea, or excessive laxative use.[6]
Life Span Considerations
When assessing elimination, the types of questions asked and the level of detail depends on the developmental age and health of the patient.
Toddlers: Ask parents or guardians about toilet training. Toilet training takes several months, occurs in several stages, and varies from child to child. It is influenced by culture and depends on physical and emotional readiness, but most children are toilet trained between 18 months and three years.
Older Adults: Constipation and incontinence are common symptoms associated with aging. Additional focused questions may be required to further assess these issues.[7]
Mobility, Activity, and Exercise
Mobility refers to a patient’s ability to move around (e.g., sit up, sit down, stand up, walk). Activity and exercise refer to informal and/or formal activity (e.g., walking, swimming, yoga, strength training). In addition to assessing the amount of exercise, it is also important to assess activity because some people may not engage in exercise but have an active lifestyle (e.g., walk to school or work in a physically demanding job).
Findings that require further investigation include insufficient aerobic exercise and identified risks for falls.[8]
Life Span Considerations
Mobility and activity depend on developmental age and a patient’s health and illness status. With infants, it is important to assess their ability to meet specific developmental milestones at each well-baby visit. Mobility can become problematic for patients who are ill or are aging and can result in self-care deficits. Thus, it is important to assess how a patient’s mobility is affecting their ability to perform ADLs and IADLs.[9]
Sleep and Rest
The sleep and rest category refers to a patient’s pattern of rest and sleep and any associated routines or sleeping medications used. Although it varies for different people and their life circumstances, obtaining eight hours of sleep every night is a general guideline. Findings that require further investigation include disruptive sleep patterns and reliance on sleeping pills or other sedative medications.[10]
Life Span Considerations
Older Adults: Disruption in sleep patterns can be especially troublesome for older adults. Assessing sleep patterns and routines will contribute to collaborative interventions for improved rest.[11]
Cognitive and Perceptual
The cognitive and perceptual category focuses on a person’s ability to collect information from the environment and use it in reasoning and other thought processes. This category includes the following:
- Adequacy of vision, hearing, taste, touch, feeling, and smell
- Any assistive devices used
- Pain level and pain management
- Cognitive functional abilities, such as orientation, memory, reasoning, judgment, and decision-making[12]
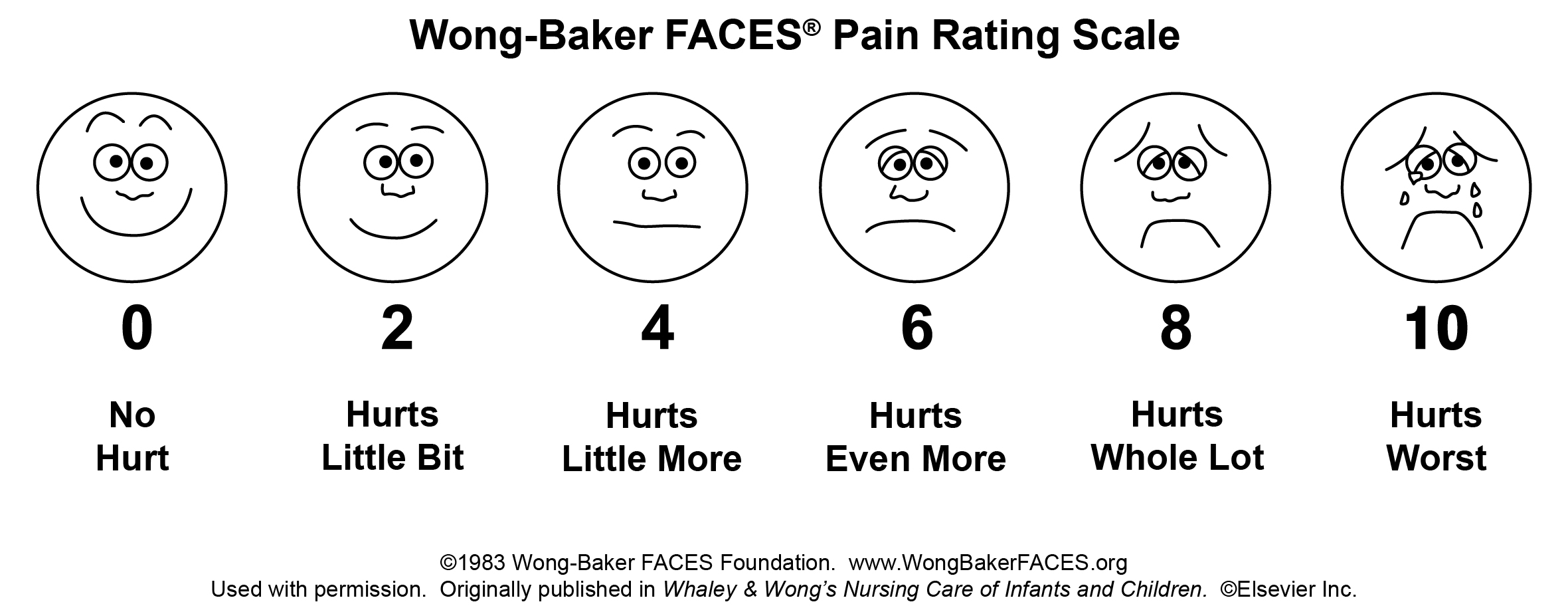
If a patient is experiencing pain, it is important to perform an in-depth assessment using the PQRSTU method described in the “Reason for Seeking Health Care” section of this chapter. It is also helpful to use evidence-based assessment tools when assessing pain, especially for patients who are unable to verbally describe the severity of their pain. See Figure 2.4[13] for an image of the Wong-Baker FACES tool that is commonly used in health care.
Life Span Considerations
Older Adults: Older adults are especially at risk for problems in the cognitive and perceptual category. Be alert for cues that suggest deficits are occurring that have not been previously diagnosed.
Roles – Relationships
Quality of life is greatly influenced by the roles and relationships established with family, friends, and the broader community. Roles often define our identity. For example, a patient may describe themselves as a “mother of an 8-year-old.” This category focuses on roles and relationships that may be influenced by health-related factors or may offer support during illness.[14] Findings that require further investigation include indications that a patient does not have any meaningful relationships or has “negative” or abusive relationships in their lives.
Life Span Considerations
Be sensitive to cues when assessing individuals with any of the following characteristics: isolation from family and friends during crisis, language barriers, loss of a significant person or pet, loss of job, significant home care needs, prolonged caregiving, history of abuse, history of substance abuse, or homelessness.[15]
Sexuality – Reproduction
Sexuality and sexual relations are an aspect of health that can be affected by illness, aging, and medication. This category includes a person’s gender identity and sexual orientation, as well as reproductive issues. It involves a combination of emotional connection, physical companionship (holding hands, hugging, kissing) and sexual activity that impact one’s feeling of health.[16]
The Joint Commission has defined terms to use when caring for diverse patients. Gender identity is a person’s basic sense of being male, female, or other gender.[17] Gender expression are characteristics in appearance, personality, and behavior that are culturally defined as masculine or feminine.[18] Sexual orientation is the preferred term used when referring to an individual’s physical and/or emotional attraction to the same and/or opposite gender.[19] LGBTQ is an acronym standing for the lesbian, gay, bisexual, transgender, and queer population. It is an umbrella term that generally refers to a group of people who are diverse in gender identity and sexual orientation. It is important to provide a safe environment to discuss health issues because the LGBTQ population experiences higher rates of smoking, alcohol use, substance abuse, HIV and other STD infections, anxiety, depression, suicidal ideation and attempts, and eating disorders as a result of stigma and marginalization.[20]
Life Span Considerations
Although sexuality is frequently portrayed in the media, individuals often consider these topics as private subjects. Use sensitivity when discussing these topics with different age groups across cultural beliefs while maintaining professional boundaries.
Advancing Effective Communication, Cultural Competence, and Patient- and Family-Centered Care for the Lesbian, Gay, Bisexual, and Transgender (LGBT) Community.
Coping-Stress Tolerance
Individuals experience stress that can lead to dysfunction if not managed in a healthy manner. Throughout life, healthy and unhealthy coping strategies are learned. Coping strategies are behaviors used to manage anxiety. Effective strategies control anxiety and lead to problem-solving but ineffective strategies can lead to abuse of food, tobacco, alcohol, or drugs.[21] Nurses teach and reinforce effective coping strategies.
Substance Use and Abuse
Alcohol, tobacco products, marijuana, and drugs are often used as ineffective coping strategies. It is important to use a nonjudgmental approach when assessing a patient’s use of substances, so they do not feel stigmatized. Substance abuse can affect people of all ages. Make a distinction between use and abuse as you assess frequency of use and patterns of behavior. Substance abuse often causes disruption in everyday function (e.g., loss of employment, deterioration of relationships, or precarious living circumstances) because of dependence on a substance. Action is needed if patients indicate that they have a problem with substance use or show signs of dependence, addiction, or binge drinking.[22]
Life Span Considerations
Some individuals are at increased risk for problems with coping strategies and stress management. Be sensitive to cues when assessing individuals with characteristics such as uncertainty in medical diagnosis or prognosis, financial problems, marital problems, poor job fit, or few close friends and family members.[23]
Value-Belief
This category includes values and beliefs that guide decisions about health care and can also provide strength and comfort to individuals. It is common for a person’s spirituality and values to be influenced by religious faith. A value is an accepted principle or standard of an individual or group. A belief is something accepted as true with a sense of certainty. Spirituality is a way of living that comes from a set of values and beliefs that are important to a person. The Joint Commission asks health care professionals to respect patients’ cultural and personal values, beliefs, and preferences and accommodate patients’ rights to religious and other spiritual services.[24] When performing an assessment, use open-ended questions to allow the patient to share values and beliefs they believe are important. For example, ask, “I am interested in your spiritual and religious beliefs and how they relate to your health. Can you share with me any spiritual beliefs or religious practices that are important to you during your stay?”
Self-Perception and Self-Concept
The focus of this category is on the subjective thoughts, feelings, and attitudes of a patient about themself. Self-concept refers to all the knowledge a person has about themself that makes up who they are (i.e., their identity). Self-esteem refers to a person’s self-evaluation of these items as being worthy or unworthy. Body image is a mental picture of one’s body related to appearance and function. It is best to assess these items toward the end of the interview because you will have already collected data that contributes to an understanding of the patient’s self-concept. Factors that influence a patient’s self-concept vary from person to person and include elements of life they value, such as talents, education, accomplishments, family, friends, career, financial status, spirituality, and religion.[25] The self-perception and self-concept category also focuses on feelings and mood states such as happiness, anxiety, hope, power, anger, fear, depression, and control.[26]
Life Span Considerations
Some individuals are at risk for problems with self-perception and self-concept. Be sensitive to cues when assessing individuals with characteristics such as uncertainty regarding a medical diagnosis or surgery, significant personal loss, history of abuse or neglect, loss of body part or function, or history of substance abuse.[27]
Violence and Trauma
There are many types of violence that a person may experience, including neglect or physical, emotional, mental, sexual, or financial abuse. You are legally mandated to report suspected cases of child abuse or neglect, as well as suspected cases of elder abuse. At any time, if you or the patient is in immediate danger, follow agency policy and procedure.
Trauma results from violence or other distressing events in a life. Collaborative intervention with the patient is required when violence and trauma are identified. People respond in different ways to trauma. It is important to use a trauma-informed approach when caring for patients who have experienced trauma. For example, a patient may respond to the traumatic situation in a way that seems unfitting (such as with laughter, ambivalence, or denial). This does not mean the patient is lying but can be a symptom of trauma. To reduce the effects of trauma, it is important to implement collaborative interventions to support patients who have experienced trauma.[28]
Loss of Body Part
A person can have negative feelings or perceptions about the characteristics, function, or limits of a body part as a result of a medical condition, surgery, trauma, or mental condition. Pay attention to cues, such as neglect of a body part or negative comments about a body part and use open-ended questions to obtain additional information.
Mental Health
Mental health is frequently underscreened and unaddressed in health care. The mental health of all patients should be assessed, even if they appear well or state they have no mental health concerns so that any changes in condition are quickly noticed and treatment implemented. Mental health includes emotional and psychological symptoms that can affect a patient’s day-to-day ability to function. The World Health Organization (2014) defines mental health as “a state of well-being in which every individual realizes their own potential, can cope with normal stresses of life, can work productively and fruitfully, and is able to make a contribution to their community.”[29] Mental illness includes conditions diagnosed by a health care provider, such as depression, anxiety, addiction, schizophrenia, post-traumatic stress disorder, and others. Mental illness can disrupt everyday functioning and affect a person’s employment, education, and relationships.
It is helpful to begin this component of a mental health assessment with a statement such as, “Mental health is an important part of our lives, so I ask all patients about their mental health and any concerns or questions they may have.”[30] Be attentive of critical findings that require intervention. For example, if a patient talks about feeling hopeless or depressed, it is important to screen for suicidal thinking. Begin with an open-ended question, such as, “Have you ever felt like hurting yourself?” If the patient responds with a “Yes,” then progress with specific questions that assess the immediacy and the intensity of the feelings. For example, you may say, “Tell me more about that feeling. Have you been thinking about hurting yourself today? Have you put together a plan to hurt yourself?” When assessing for suicidal thinking, be aware that a patient most at risk is someone who has a specific plan about self-harm and can specify how and when they will do it. They are particularly at risk if planning self-harm within the next 48 hours. The age of the patient is not a factor in this determination of risk. If you believe the patient is at high risk, do not leave the patient alone. Collaborate with them regarding an immediate plan for emergency care.[31]
Health Perception-Health Management
Health perception-health management is an umbrella term encompassing all of the categories described above, as well as environmental health.
Environmental Health
Environmental health refers to the safety of a patient’s physical environment, also called a social determinant of health. Examples of environmental health include, but are not limited to, exposure to violence in the home or community; air pollution; and availability of grocery stores, health care providers, and public transportation. Findings that require further investigation include a patient living in unsafe environments.[32]
See Table 2.8 for sample focused questions for all categories related to functional health.[33]
Table 2.8 Focused Interview Questions for Functional Health Categories[34]
Begin this section by saying, “I would like to ask you some questions about factors that affect your ability to function in your day-to-day life. Feel free to share any health concerns that come to mind during this discussion.”
| Category | Focused Questions |
|---|---|
| Nutrition | Tell me about your diet.
What foods do you usually eat? What fluids do you usually drink every day? What have you eaten in the last 24 hours? Is this typical of your usual eating pattern? Tell me about your appetite. Have you had any changes in your appetite? Do you have any goals related to your nutrition? Do you have any financial concerns about purchasing food? Are you able to prepare the meals you want to eat? |
| Elimination | When was your last bowel movement?
Do you have any problems with constipation, diarrhea, or incontinence? Do you take laxatives or stool softeners? Do you have any problems urinating, such as frequent urination or burning on urination? Do you ever experience leaking or dribbling of urine? |
| Mobility, Activity, and Exercise | Tell me about your ability to move around.
Do you have any problems sitting up, standing up, or walking? Do you use any mobility aids (e.g., cane, walker, wheelchair)? Tell me about the activity and/or exercise in which you engage. What type? How frequent? For how long? |
| Sleep and Rest | Tell me about your sleep routine. How many hours of sleep do you usually get?
Do you feel rested when you awaken? Do you do anything to wind down before you go to bed (e.g., watch TV, read)? Do you take any sleeping medication? Do you take any naps during the day? |
| Cognitive and Perceptual | Are you having any pain?
Note: If present, use the PQRSTU method to further assess pain. Are you having any issues with seeing, hearing, smelling, tasting, or feeling things? Have you noticed any changes in memory or problems concentrating? Have you noticed any changes in the ability to make decisions? What is the easiest way for you to learn (e.g., written materials, explanations, or learning-by-doing)? |
| Roles and Relationships | Tell me about the most influential relationships in your life with family and friends.
How do these relationships influence your day-to-day life, health, and illness? Who are the people with whom you talk to when you require support or are struggling in your life? Do you have family or others dependent on you? Have you had any recent losses of someone important to you, a pet, or a job? Do you feel safe in your current relationship? |
| Sexuality-Reproduction | The expression of love and caring in a sexual relationship and creation of family are often important aspects in a person’s life. Do you have any concerns about your sexual health?
Tell me about the ways that you ensure your safety when engaging in intimate and sexual practices. |
| Coping-Stress | Tell me about the stress in your life.
Have you experienced a recent loss in your life that has impacted you? How do you cope with stress? |
| Values-Belief | I am interested in your spiritual and religious beliefs and how they relate to your health. Can you share with me any spiritual beliefs or religious practices that are important to you? |
| Self-Perception and Self-Concept |
Tell me what makes you who you are. How would you describe yourself? Have you noticed any changes in how you view your body or the things you can do? Are these a problem for you? Have you found yourself feeling sad, angry, fearful, or anxious? What helps you to feel better when this happens? Have you ever used any tobacco products (e.g., cigarettes, pipes, vaporizers, hookah)? If so, how much? How much alcohol do you drink every week? Have you used cannabis products? If so, how often do you use them? Have you ever used drugs or prescription drugs that were not prescribed for you? If so, what type? Have you ever felt you had a problem with any of these substances because they affected your daily life? If so, tell me more. Do you want to quit any of these substances? Many patients have experienced violence or trauma in their lives. Have you experienced any violence or trauma in your life? How has it affected you? Would you like to talk with someone about it?
|
| Health Perception – Health Management |
Tell me about how you take care of yourself and manage your home. Have you had any falls in the past six months? Do you have enough finances to pay your bills and purchase food, medications, and other needed items? Do you have any current or future concerns about being able to function independently? Tell me about where you live. Do you have any concerns about safety in your home or neighborhood? Tell me about any factors in your environment that may affect your health. Do you have any concerns about how your environment is affecting your health? |
- “ADL-1024x534.jpg” by unknown is licensed under CC BY-SA 4.0. Access for free at https://ecampusontario.pressbooks.pub/healthassessment/chapter/functional-health/ ↵
- “iADL-1024x494.jpg” by unknown is licensed under CC BY-SA 4.0. Access for free at https://ecampusontario.pressbooks.pub/healthassessment/chapter/functional-health/ ↵
- Gordon, M. (2008). Assess notes nursing: Nursing assessment and diagnostic reasoning for clinical practice. F. A. Davis Company. ↵
- Gordon, M. (2008). Assess notes nursing: Nursing assessment and diagnostic reasoning for clinical practice. F.A. Davis Company. ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- Gordon, M. (2008). Assess notes nursing: Nursing assessment and diagnostic reasoning for clinical practice. F.A. Davis Company. ↵
- Wong-Baker FACES Foundation. (2020). Wong-Baker FACES® Pain Rating Scale. ↵
- Gordon, M. (2008). Assess notes nursing: Nursing assessment and diagnostic reasoning for clinical practice. F. A. Davis Company. ↵
- Gordon, M. (2008). Assess notes nursing: Nursing assessment and diagnostic reasoning for clinical practice. F. A. Davis Company. ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- The Joint Commission. (2011). Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/health-equity/lgbtfieldguide_web_linked_verpdf.pdf downloaded from https://www.jointcommission.org/resources/patient-safety-topics/health-equity/#t=_Tab_StandardsFAQs&sort=relevancy ↵
- The Joint Commission. (2011). Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/health-equity/lgbtfieldguide_web_linked_verpdf.pdf downloaded from https://www.jointcommission.org/resources/patient-safety-topics/health-equity/#t=_Tab_StandardsFAQs&sort=relevancy ↵
- The Joint Commission. (2011). Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/health-equity/lgbtfieldguide_web_linked_verpdf.pdf downloaded from https://www.jointcommission.org/resources/patient-safety-topics/health-equity/#t=_Tab_StandardsFAQs&sort=relevancy ↵
- The Joint Commission. (2011). Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/health-equity/lgbtfieldguide_web_linked_verpdf.pdf downloaded from https://www.jointcommission.org/resources/patient-safety-topics/health-equity/#t=_Tab_StandardsFAQs&sort=relevancy ↵
- Gordon, M. (2008). Assess notes nursing: Nursing assessment and diagnostic reasoning for clinical practice. F. A. Davis Company. ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- Gordon, M. (2008). Assess notes nursing: Nursing assessment and diagnostic reasoning for clinical practice. F. A. Davis Company. ↵
- The Joint Commission. (2018). The source, 16(1). https://store.jcrinc.com/assets/1/14/ts_16_2018_01.pdf ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- Gordon, M. (2008). Assess notes nursing: Nursing assessment and diagnostic reasoning for clinical practice. F. A. Davis Company. ↵
- Gordon, M. (2008). Assess notes nursing: Nursing assessment and diagnostic reasoning for clinical practice. F. A. Davis Company. ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, and Mistry licensed under CC BY-SA 4.0 ↵
The period of a disease after the initial entry of the pathogen into the host but before symptoms develop.
The disease stage after the incubation period when the pathogen continues to multiply and the host begins to experience general signs and symptoms of illness that result from activation of the immune system, such as fever, pain, soreness, swelling, or inflammation.
Infections that develop rapidly and generally last only 10-14 days.
Learning Objectives
- Distinguish among the different levels of nursing education
- Specify the ethical and legal boundaries of the student nurse as presented in the Code of Ethics and the Nurse Practice Act
- Detail responsibility for maintaining client confidentiality
- Describe the contribution of all members of the health care team
- Identify the role of evidence-based practice in nursing
- Identify the concept of quality in client care
- Discuss nursing scope of practice and standards of care
- Compare various settings in which nurses work
- Outline professional nursing organizations
Scope of practice refers to services a trained health professional is deemed competent to perform and permitted to undertake according to the terms of their professional nursing license.[1] Nursing scope of practice provides a legal framework and structured guidance for activities that practical nurses and registered nurses can perform based on their nursing license. As a nursing student, and in the future as a nurse, it is always important to consider if you can perform a task you are requested to do based on your legal scope of practice - or are you putting your nursing education or nursing license at risk?
Nurses must also follow standards when providing nursing care. Standards are set by several organizations, including your state’s Nurse Practice Act, the American Nurses Association (ANA), agency policies and procedures, and federal regulators. These standards help guide nursing actions with the intent that safe, competent care is provided to the public.
This chapter will provide an overview of basic concepts related to nursing scope of practice and standards of care.
Health Care Settings
There are several levels of health care including primary, secondary, and tertiary care. Each of these levels focuses on different aspects of health care and is typically provided in different settings.
Primary Care
Primary care promotes wellness and prevents disease. This care includes health promotion, education, protection (such as immunizations), early disease screening, and environmental considerations. Settings providing this type of health care include physician offices, public health clinics, school nursing, and community health nursing.
Secondary care
Secondary care occurs when a person has contracted an illness or injury and requires medical care. Secondary care is often referred to as acute care. Secondary care can range from uncomplicated care to repair a small laceration or treat a strep throat infection to more complicated emergent care such as treating a head injury sustained in an automobile accident. Whatever the problem, the client needs medical and nursing attention to return to a state of health and wellness. Secondary care is provided in settings such as physician offices, clinics, urgent care facilities, or hospitals. Specialized units include areas such as critical care, burn units, neurosurgery, cardiac surgery, and transplant services.
Tertiary Care
Tertiary care addresses the long-term effects from chronic illnesses or conditions with the purpose to restore a client's maximum physical and mental function. The goal of tertiary care is to achieve the highest level of functioning possible while managing the chronic illness. For example, a client who falls and fractures their hip will need secondary care to set the broken bones, but may need tertiary care to regain their strength and ability to walk even after the bones have healed. Clients with incurable diseases, such as dementia, may need specialized tertiary care to provide support they need for daily functioning. Tertiary care settings include rehabilitation units, assisted living facilities, adult day care, skilled nursing units, home care, and hospice centers.
Health Care Team
No matter the setting, quality health care requires a team of health care professionals collaboratively working together to deliver holistic, individualized care. Nursing students must be aware of the roles and contributions of various health care team members. The health care team consists of health care providers, nurses (licensed practical nurses, registered nurses, and advanced practice registered nurses), unlicensed assistive personnel, and a variety of interprofessional team members.
Health Care Providers
The Wisconsin Nurse Practice Act defines a health care provider as, "A physician, podiatrist, dentist, optometrist, or advanced practice nurse.”[2] Providers are responsible for ordering diagnostic tests such as blood work and X-rays, diagnosing a client’s medical condition, developing a medical treatment plan, and prescribing medications. In a hospital setting, the medical treatment plan developed by a provider is communicated in the “History and Physical” component of the client's medical record with associated prescriptions (otherwise known as "orders"). Prescriptions or “orders” include diagnostic and laboratory tests, medications, and general parameters regarding the care that each client is to receive. Nurses should respectfully clarify prescriptions they have questions or concerns about to ensure safe client care. Providers typically visit hospitalized clients daily in what is referred to as "rounds." It is helpful for nurses and nursing students to attend provider rounds for their assigned clients to be aware of and provide input regarding the current medical treatment plan, seek clarification, or ask questions. This helps to ensure that the provider, nurse, and client have a clear understanding of the goals of care and minimizes the need for follow-up phone calls.
Nurses
There are three levels of nurses as defined by each state's Nurse Practice Act: Licensed Practical Nurse/Vocational Nurse (LPN/LVN), Registered Nurse (RN), and Advanced Practice Registered Nurse (APRN).
Licensed Practical/Vocational Nurses
The National Council of State Boards of Nursing (NCSBN) defines a licensed practical nurse (LPN) as, “An individual who has completed a state-approved practical or vocational nursing program, passed the NCLEX-PN examination, and is licensed by a state board of nursing to provide client care.”[3] In some states, the term licensed vocational nurse (LVN) is used. LPNs/LVNs typically work under the supervision of a registered nurse, advanced practice registered nurse, or physician.[4] LPNs provide "basic nursing care" and work with stable and/or chronically ill populations. Basic nursing care is defined by the Wisconsin Nurse Practice Act as “care that can be performed following a defined nursing procedure with minimal modification in which the responses of the client to the nursing care are predictable.”[5] LPNs/LVNs typically collect client assessment information, administer medications, and perform nursing procedures according to their scope of practice in that state. The Open RN Nursing Skills, 2e textbook discusses the skills and procedures that LPNs frequently perform in Wisconsin. See the following box for additional details about the scope of practice of the Licensed Practical Nurse in Wisconsin.
Scope of Practice for Licensed Practical Nurses in Wisconsin[6]
"The Wisconsin Nurse Practice Act defines the scope of practice for Licensed Practical Nurses as the following: “In the performance of acts in basic patient situations, the LPN shall, under the general supervision of an RN or the direction of a provider:
(a) Accept only patient care assignments which the LPN is competent to perform.
(b) Provide basic nursing care.
(c) Record nursing care given and report to the appropriate person changes in the condition of a patient.
(d) Consult with a provider in cases where an LPN knows or should know a delegated act may harm a patient.
(e) Perform the following other acts when applicable:
- Assist with the collection of data.
- Assist with the development and revision of a nursing care plan.
- Reinforce the teaching provided by an RN provider and provide basic health care instruction.
- Participate with other health team members in meeting basic patient needs.”
Registered Nurses
The NCSBN defines a Registered Nurse (RN) as “An individual who has graduated from a state-approved school of nursing, passed the NCLEX-RN examination and is licensed by a state board of nursing to provide client care.”[7] Registered Nurses (RNs) use the nursing process as a critical thinking model as they make decisions and use clinical judgment regarding client care. The nursing process is discussed in more detail in the “Nursing Process” chapter of this book. RNs may be delegated tasks from providers or may delegate tasks to LPNs and UAPs with supervision. See the following box for additional details about the scope of practice for Registered Nurses in the state of Wisconsin.
Scope of Practice for Registered Nurses in Wisconsin[8]
(1) "GENERAL NURSING PROCEDURES. An RN shall utilize the nursing process in the execution of general nursing procedures in the maintenance of health, prevention of illness or care of the ill. The nursing process consists of the steps of assessment, planning, intervention, and evaluation. This standard is met through performance of each of the following steps of the nursing process:
(a) Assessment. Assessment is the systematic and continual collection and analysis of data about the health status of a patient culminating in the formulation of a nursing diagnosis.
(b) Planning. Planning is developing a nursing plan of care for a patient, which includes goals and priorities derived from the nursing diagnosis.
(c) Intervention. Intervention is the nursing action to implement the plan of care by directly administering care or by directing and supervising nursing acts delegated to LPNs or less skilled assistants.
(d) Evaluation. Evaluation is the determination of a patient’s progress or lack of progress toward goal achievement, which may lead to modification of the nursing diagnosis.
(2) PERFORMANCE OF DELEGATED ACTS. In the performance of delegated acts, an RN shall do all of the following:
(a) Accept only those delegated acts for which there are protocols or written or verbal orders.
(b) Accept only those delegated acts for which the RN is competent to perform based on his or her nursing education, training or experience.
(c) Consult with a provider in cases where the RN knows or should know a delegated act may harm a patient.
(d) Perform delegated acts under the general supervision or direction of provider.
(3) SUPERVISION AND DIRECTION OF DELEGATED ACTS. In the supervision and direction of delegated acts, an RN shall do all of the following:
(a) Delegate tasks commensurate with educational preparation and demonstrated abilities of the person supervised.
(b) Provide direction and assistance to those supervised.
(c) Observe and monitor the activities of those supervised.
(d) Evaluate the effectiveness of acts performed under supervision."
Advanced Practice Registered Nurses
Advanced Practice Registered Nurses (APRN) are defined by the NCSBN as an RN who has a graduate degree and advanced knowledge. There are four categories of Advanced Practice Registered Nurses: Certified Nurse-Midwife (CNM), Clinical Nurse Specialist (CNS), Certified Nurse Practitioner (CNP), and Certified Registered Nurse Anesthetist (CRNA). APRNs can diagnose illnesses and prescribe treatments and medications. Additional information about advanced nursing degrees and roles is provided in the box below.
Advanced Practice Nursing Roles[9]
Nurse Practitioners: Nurse practitioners (NPs) work in a variety of settings and complete physical examinations, diagnose and treat common acute illness and manage chronic illness, order laboratory and diagnostic tests, prescribe medications and other therapies, provide health teaching and supportive counseling with an emphasis on prevention of illness and health maintenance, and refer clients to other health professionals and specialists as needed. In many states, NPs can function independently and manage their own clinics, whereas in other states physician supervision is required. NP certifications include, but are not limited to, Family Practice, Adult-Gerontology Primary Care and Acute Care, and Psychiatric/Mental Health.
To read more about NP certification, visit Nursing World's Our Certifications web page.
Clinical Nurse Specialists: Clinical Nurse Specialists (CNS) practice in a variety of health care environments and participate in mentoring other nurses, case management, research, designing and conducting quality improvement programs, and serving as educators and consultants. Specialty areas include, but are not limited to, Adult/Gerontology, Pediatrics, and Neonatal.
To read more about CNS certification, visit National Association of Clinical Nurse Specialist's What is a CNS? web page.
Certified Registered Nurse Anesthetists: Certified Registered Nurse Anesthetists (CRNAs) administer anesthesia and related care before, during, and after surgical, therapeutic, diagnostic, and obstetrical procedures, as well as provide airway management during medical emergencies. CRNAs deliver more than 65 percent of all anesthetics to clients in the United States. Practice settings include operating rooms, dental offices, and outpatient surgical centers.
To read more about CRNA certification, visit National Board of Certification & Recertification for Nurse Anesthetist's website.
Certified Nurse Midwives: Certified Nurse Midwives provide gynecological exams, family planning advice, prenatal care, management of low-risk labor and delivery, and neonatal care. Practice settings include hospitals, birthing centers, community clinics, and client homes.
To read more about CNM certification, visit the American Midwifery Certification Board website.
Unlicensed Assistive Personnel
Unlicensed Assistive Personnel (UAP) are defined by the NCSBN as, “Any unlicensed person, regardless of title, who performs tasks delegated by a nurse. This includes certified nursing aides/assistants (CNAs), patient care assistants (PCAs), patient care technicians (PCTs), state tested nursing assistants (STNAs), nursing assistants-registered (NA/Rs), or certified medication aides/assistants (MA-Cs). Certification of UAPs varies between jurisdictions.”[10]
CNAs, PCAs, and PCTs in Wisconsin generally work in hospitals and long-term care facilities and assist clients with daily tasks such as bathing, dressing, feeding, and toileting. They may also collect client information such as vital signs, weight, and input/output as delegated by the nurse. The RN remains accountable that delegated tasks have been completed and documented by the UAP.
Interprofessional Team Members
Nurses, as the coordinator of a client’s care, continuously review the plan of care to ensure all contributions of the multidisciplinary team are moving the client toward expected outcomes and goals. The roles and contributions of interprofessional health care team members are further described in the following box.
Interprofessional Team Member Roles[11]
Dieticians: Dieticians assess, plan, implement, and evaluate interventions, including those relating to dietary needs of those clients who need regular or therapeutic diets. They also provide dietary education and work with other members of the health care team when a client has dietary needs secondary to physical disorders such as difficulty swallowing.
Occupational Therapists (OT): Occupational therapists assess, plan, implement, and evaluate interventions, including those that facilitate the client's ability to achieve their highest possible level of independence in their activities of daily living such as bathing, grooming, eating, and dressing. They also provide clients with adaptive devices such as long shoehorns so the client can put their shoes on, sock pulls so they can independently pull on socks, adaptive silverware to facilitate independent eating, grabbers so the client can pick items up from the floor, and special devices to manipulate buttoning so the person can dress and button their clothing independently. OTs assess the home for safety and the need for assistive devices when the client is discharged home. They may recommend modifications to the home environment such as ramps, grab rails, and handrails to ensure safety and independence. OTs practice in all health care environments, including the home, hospital, and rehabilitation centers.
Pharmacists: Pharmacists ensure the safe prescribing and dispensing of medication and are a vital resource for nurses with questions or concerns about medications they are administering to clients. Pharmacists ensure that clients not only get the correct medication and dosing, but also have the guidance they need to use the medication safely and effectively.
Physical Therapists (PT): Physical therapists are licensed health care professionals who assess, plan, implement, and evaluate interventions, including those related to the client's functional abilities in terms of their strength, mobility, balance, gait, coordination, and joint range of motion. They supervise prescribed exercise activities according to a client’s condition and also provide and teach clients how to use assistive aids like walkers and canes and how to perform exercise regimens. Physical therapists practice in all health care environments, including the home, hospital, and rehabilitation centers.
Podiatrists: Podiatrists provide care and services to clients who have foot problems. They often work with clients who have diabetes to clip toenails and provide foot care to prevent complications.
Prosthetists: Prosthetists design, fit, and supply the client with an artificial body part such as a leg or arm prosthesis. They adjust prosthesis to ensure proper fit, comfort, and functioning.
Psychologists and Psychiatrists: Psychologists and psychiatrists provide mental health and psychiatric services to clients with mental health disorders and provide psychological support to family members and significant others as indicated.
Respiratory Therapists: Respiratory therapists treat respiratory-related conditions in clients. Their specialized respiratory care includes managing oxygen therapy; drawing arterial blood gases; managing clients on specialized oxygenation devices such as mechanical ventilators, CPAP, and Bi-PAP machines; administering respiratory medications like inhalers and nebulizers; intubating clients; assisting with bronchoscopy and other respiratory-related diagnostic tests; performing pulmonary hygiene measures like chest physiotherapy; and serving an integral role in providing respiratory support.
Social Workers: Social workers counsel clients and provide psychological support, help set up community resources according to clients' financial needs, and serve as part of the team that ensures continuity of care after the person is discharged.
Speech Therapists: Speech therapists assess, diagnose, and treat communication and swallowing disorders. For example, speech therapists help clients with a disorder called expressive aphasia. They also assist clients with using word boards and other electronic devices to facilitate communication. They assess clients with swallowing disorders called dysphagia and treat them in collaboration with other members of the health care team including nurses, dieticians, and health care providers.
Ancillary Department Members: Nurses also work with ancillary departments such as laboratory and radiology departments.
- Clinical laboratory departments provide a wide range of laboratory procedures that aid health care providers to diagnose, treat, and manage clients. These laboratories are staffed by medical technologists who test biological specimens collected from clients. Examples of laboratory tests performed include blood tests, blood banking, cultures, urine tests, and histopathology (changes in tissues caused by disease).[12]
- Radiology departments use imaging to assist providers in diagnosing and treating diseases seen within the body. They perform diagnostic tests such as X-rays, CTs, MRIs, nuclear medicine, PET scans, and ultrasound scans.
Chain of Command
Nurses rarely make client decisions in isolation, but instead consult with other nurses and interprofessional team members. Concerns and questions about client care are typically communicated according to that agency's chain of command. In the military, chain of command refers to a hierarchy of reporting relationships – from the bottom to the top of an organization – regarding who must answer to whom. The chain of command not only establishes accountability, but also lays out lines of authority and decision-making power. The chain of command also applies to health care. For example, a registered nurse in a hospital may consult a “charge nurse,” who may consult the “nurse supervisor,” who may consult the “director of nursing,” who may consult the "vice president of nursing." In a long-term care facility, a licensed practical/vocational nurse typically consults the registered nurse/charge nurse, who may consult with the director of nursing. Nursing students should always consult with their nursing instructor regarding questions or concerns about client care before “going up the chain of command.”
Nurse Specialties
Registered nurses can obtain several types of certifications as a nurse specialist. Certification is the formal recognition of specialized knowledge, skills, and experience demonstrated by the achievement of standards identified by a nursing specialty. See the following box for descriptions of common nurse specialties.
Common Nurse Specialties
Critical Care Nurses provide care to clients with serious, complex, and acute illnesses or injuries that require very close monitoring and extensive medication protocols and therapies. Critical care nurses most often work in intensive care units of hospitals.
Public Health Nurses work to promote and protect the health of populations based on knowledge from nursing, social, and public health sciences. Public health nurses most often work in municipal and state health departments.
Home Health/Hospice Nurses provide a variety of nursing services for chronically ill clients and their caregivers in the home, including end-of-life care.
Occupational/Employee Health Nurses provide health screening, wellness programs and other health teaching, minor treatments, and disease/medication management services to people in the workplace. The focus is on promotion and restoration of health, prevention of illness and injury, and protection from work-related and environmental hazards.
Oncology Nurses care for clients with various types of cancer, administering chemotherapy and providing follow-up care, teaching, and monitoring. Oncology nurses work in hospitals, outpatient clinics, and clients’ homes.
Perioperative/Operating Room Nurses provide preoperative and postoperative care to clients undergoing anesthesia or assist with surgical procedures by selecting and handling instruments, controlling bleeding, and suturing incisions. These nurses work in hospitals and outpatient surgical centers.
Rehabilitation Nurses care for clients with temporary and permanent disabilities within inpatient and outpatient settings such as clinics and home health care.
Psychiatric/Mental Health Nurses specialize in mental and behavioral health problems and provide nursing care to individuals with psychiatric disorders. Psychiatric nurses work in hospitals, outpatient clinics, and private offices.
School Nurses provide health assessment, intervention, and follow-up to maintain school compliance with health care policies and ensure the health and safety of staff and students. They administer medications and refer students for additional services when hearing, vision, and other issues become inhibitors to successful learning.
Telenursing refers to providing nursing care remotely using information and communication technology. Nursing care may include client education, support, health assessment and evaluation, and triage. While telenursing is not a specialty, it is provided in several specialty areas such as Critical Care and Emergency Departments. It is also provided in outpatient environments and encourages increased client interactions, especially in underserved rural areas.[13]
Other common specialty areas include a life span approach across health care settings and include maternal-child, neonatal, pediatric, and gerontological nursing.[14]
Damage that occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue.
The healing of a wound that has had to remain open or has been reopened, often due to severe infection.
Legal Considerations
As discussed earlier in this chapter, nurses can be reprimanded or have their licenses revoked for not appropriately following the Nurse Practice Act in the state they are practicing. Nurses can also be held legally liable for negligence, malpractice, or breach of client confidentiality when providing client care.
Negligence and Malpractice
Negligence is a general term that denotes conduct lacking in due care, carelessness, and a deviation from the standard of care that a reasonable person would use in a particular set of circumstances.[15] Malpractice is a more specific term that looks at a standard of care, as well as the professional status of the caregiver. [16]
To prove negligence or malpractice, the following elements must be established in a court of law[17]:
- Duty owed the client
- Breach of duty owed the client
- Foreseeability
- Causation
- Injury
- Damages
To avoid being sued for negligence or malpractice, it is essential for nurses and nursing students to follow the scope and standards of practice care set forth by their state’s Nurse Practice Act; the American Nurses Association; and employer policies, procedures, and protocols to avoid the risk of losing their nursing license. Examples of a nurse's breach of duty that can be viewed as negligence includes the following:[18]
- Failure to Assess: Nurses should assess for all potential nursing problems/diagnoses, not just those directly affected by the medical disease. For example, all clients should be assessed for fall risk and appropriate fall precautions implemented.
- Insufficient monitoring: Some conditions require frequent monitoring by the nurse, such as risk for falls, suicide risk, confusion, and self-injury.
- Failure to Communicate:
- Lack of documentation: A basic rule of thumb in a court of law is that if an assessment or action was not documented, it is considered not done. Nurses must document all assessments and interventions, in addition to the specific type of client documentation called a nursing care plan.
- Lack of provider notification: Changes in client condition should be urgently communicated to the health care provider based on client status. Documentation of provider notification should include the date, time, and person notified and follow-up actions taken by the nurse.
- Failure to Follow Protocols: Agencies and states have rules for reporting certain behaviors or concerns. For example, a nurse is considered a mandatory reporter by law and required to report suspicion of abuse or neglect of a child based on data gathered during an assessment.
Patient Self Determination Act
The Patient Self Determination Act (PSDA) of 1990 is an amendment made to the Social Security Act that requires health care facilities to inform clients of their right to be involved in their medical care decisions. This law specifically applies to facilities accepting Medicare or Medicaid funding but is considered a right of all clients regardless of their method of reimbursement.
Under the PSDA, clients must also be asked about their advance directives and care wishes. Clients must be provided with teaching about advance directives, appointment of an agent or surrogate in the event they become incapacitated, and their right to self-determination. Conversations about these topics and clients wishes must be documented in the medical record. It is considered an ethical duty of nurses and other health care professionals to ensure clients are aware and understand these healthcare-associated rights.[19]
Informed Consent
Informed consent is written consent voluntarily signed by a client who is competent and understands the terms of the consent without any form of coercion. In the event the client is a minor or deemed incompetent to make their own decisions, a parent or legal guardian signs the informed consent.[20]
Informed consent is crucial for upholding the client's right for self-determination. Informed consent provides documentation signed by the client of their understanding of health care being provided; its benefits, risks, potential complications; reasonable alternatives to treatment; and the right to withdraw consent. It is the health care provider's responsibility to fully discuss the treatment, procedure, or other health care action being proposed that requires consent. The nurse often signs as a witness to the client's signature on the form, affirming that person signed the form. However, it is not the nurse's responsibility or role to provide information. If the client (or their parent/legal guardian) expresses questions, concerns, or lack of understanding, the nurse has an ethical responsibility to notify the provider and advocate for further discussion before signing the form.[21]
In emergency situations where the delay to obtain consent would cause undue harm to the client, verbal or telephone consent may be temporarily obtained that is valid for no more than ten days. Verbal consent and the reason for verbal consent must be documented in the medical record by the provider.[22]
See the following box for examples of situations requiring informed consent in the state of Wisconsin according to the Wisconsin Department of Health Services.
Examples of Situations Requiring Informed Consent[23]
- Receipt of medications and/or treatment, including psychotropic medications (unless court-ordered)
- Undergoing customary treatment techniques and procedures
- Participation in experimental research
- Undergoing psychosurgery or other psychological treatment procedures
- Release of treatment records
- Videorecording
- Performance of labor beneficial to the facility
Confidentiality
In addition to negligence and malpractice, confidentiality is a major legal consideration for nurses and nursing students. Patient confidentiality is the right of an individual to have personal, identifiable medical information, referred to as their protected health information (PHI), protected and known only by those health care team members directly providing care to them. This right is protected by federal regulations called the Health Insurance Portability and Accountability Act (HIPAA). HIPAA was enacted in 1996 and was prompted by the need to ensure privacy and protection of personal health records and data in an environment of electronic medical records and third-party insurance payers. There are two main sections of HIPAA law, the Privacy Rule and the Security Rule. The Privacy Rule addresses the use and disclosure of individuals' health information. The Security Rule sets national standards for protecting the confidentiality, integrity, and availability of electronically protected health information. HIPAA regulations extend beyond medical records and apply to client information shared with others. Therefore, all types of client information should only be shared with health care team members who are actively providing care to them.
How do HIPAA regulations affect you as a student nurse? You are required to adhere to HIPAA guidelines from the moment you begin to provide client care. Nursing students may be disciplined or expelled by their nursing program for violating HIPAA. Nurses who violate HIPAA rules may be fired from their jobs or face lawsuits. See the following box for common types of HIPAA violations and ways to avoid them.
Common HIPAA Violations and Ways to Avoid Them[24]
- Gossiping in the hallways or otherwise talking about clients where other people can hear you. It is understandable that you will be excited about what is happening when you begin working with clients and your desire to discuss interesting things that occur. As a student, you will be able to discuss client care in a confidential manner behind closed doors with your instructor. However, as a health care professional, do not talk about clients in the hallways, elevator, breakroom, or with others who are not directly involved with that client’s care because it is too easy for others to overhear what you are saying.
- Mishandling medical records or leaving medical records unsecured. You can breach HIPAA rules by leaving your computer unlocked for anyone to access or by leaving written client charts in unsecured locations. You should never share your password with anyone else. Make sure that computers are always locked with a password when you step away from them and paper charts are closed and secured in an area where unauthorized people don’t have easy access to them. NEVER take records from a facility or include a client's name on paperwork that leaves the facility.
- Illegally or unauthorized accessing of client files. If someone you know, like a neighbor, coworker, or family member is admitted to the unit you are working on, do not access their medical record unless you are directly caring for them. Facilities have the capability of tracing everything you access within the electronic medical record and holding you accountable. This rule holds true for employees who previously cared for a client as a student; once your shift is over as a student, you should no longer access that client’s medical records.
- Sharing information with unauthorized people. Anytime you share medical information with anyone but the client themselves, you must have written permission to do so. For instance, if a husband comes to you and wants to know his spouse’s lab results, you must have permission from his spouse before you can share that information with him. Just confirming or denying that a client has been admitted to a unit or agency can be considered a breach of confidentiality. Furthermore, voicemails should not be left regarding protected client information.
- Information can generally be shared with the parents of children until they turn 18, although there are exceptions to this rule if the minor child seeks birth control, an abortion, or becomes pregnant. After a child turns 18, information can no longer be shared with the parent unless written permission is provided, even if the minor is living at home and/or the parents are paying for their insurance or health care. As a general rule, any time you are asked for client information, check first to see if the client has granted permission.
- Texting or e-mailing regarding client information on an unencrypted device. Only use properly encrypted devices that have been approved by your health care facility for e-mailing or faxing protected client information. Also, ensure that the information is being sent to the correct person, address, or phone number.
- Sharing information on social media. Never post anything on social media that has anything to do with your clients, the facility where you are working or have clinical, or even how your day went at the agency. Nurses and other professionals have been fired for violating HIPAA rules on social media.[25],[26],[27]
Social Media Guidelines
Nursing students, nurses, and other health care team members must use extreme caution when posting to Facebook, Instagram, Twitter, Snapchat, and other social media sites. Information related to clients, client care, and/or health care agencies should never be posted on social media; health care team members who violate this guideline can lose their jobs and may face legal action and students can be disciplined or expelled from their nursing program. Be aware that even if you think you are posting in a private group, the information can become public.
The American Nurses Association (ANA) has established the following principles for nurses using social media:[28]
- Nurses must not transmit or place online individually identifiable client information.
- Nurses must observe ethically prescribed professional client-nurse boundaries.
- Nurses should understand that clients, colleagues, organizations, and employers may view postings.
- Nurses should take advantage of privacy settings and seek to separate personal and professional information online.
- Nurses should bring content that could harm a client’s privacy, rights, or welfare to the attention of appropriate authorities.
- Nurses should participate in developing organizational policies governing online conduct.
In addition to these principles, the ANA has also provided these tips for nurses and nursing students using social media:[29]
- Remember that standards of professionalism are the same online as in any other circumstance.
- Do not share or post information or photos gained through the nurse-client relationship.
- Maintain professional boundaries in the use of electronic media. Online contact with clients blurs this boundary.
- Do not make disparaging remarks about clients, employers, or coworkers, even if they are not identified.
- Do not take photos or videos of clients on personal devices, including cell phones.
- Promptly report a breach of confidentiality or privacy.
Read more about the ANA's Social Media Principles.
Code of Ethics
In addition to legal considerations, there are also several ethical guidelines for nursing care.
There is a difference between morality, ethical principles, and a code of ethics. Morality refers to “personal values, character, or conduct of individuals within communities and societies.”[30] An ethical principle is a general guide, basic truth, or assumption that can be used with clinical judgment to determine a course of action. Four common ethical principles are beneficence (do good), nonmaleficence (do no harm), autonomy (control by the individual), and justice (fairness). A code of ethics is set for a profession and makes their primary obligations, values, and ideals explicit.
The American Nursing Association (ANA) guides nursing practice with the Code of Ethics for Nurses.[31] This code provides a framework for ethical nursing care and a guide for decision-making. The Code of Ethics for Nurses serves the following purposes:
- It is a succinct statement of the ethical values, obligations, duties, and professional ideals of nurses individually and collectively.
- It is the profession’s nonnegotiable ethical standard.
- It is an expression of nursing’s own understanding of its commitment to society.[32]
The ANA Code of Ethics contains nine provisions. See a brief description of each provision in the following box.
Provisions of the ANA Code of Ethics[33]
The nine provisions of the ANA Code of Ethics are briefly described below. The full code is available to read for free at Nursingworld.org.
Provision 1: The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person.
Provision 2: The nurse’s primary commitment is to the patient, whether an individual, family, group, community, or population.
Provision 3: The nurse promotes, advocates for, and protects the rights, health, and safety of the patient.
Provision 4: The nurse has authority, accountability, and responsibility for nursing practice; makes decisions; and takes action consistent with the obligation to promote health and to provide optimal care.
Provision 5: The nurse owes the same duties to self as to others, including the responsibility to promote health and safety, preserve wholeness of character and integrity, maintain competence, and continue personal and professional growth.
Provision 6: The nurse, through individual and collective effort, establishes, maintains, and improves the ethical environment of the work setting and conditions of employment that are conducive to safe, quality health care.
Provision 7: The nurse, in all roles and settings, advances the profession through research and scholarly inquiry, professional standards development, and the generation of both nursing and health policy.
Provision 8: The nurse collaborates with other health professionals and the public to protect human rights, promote health diplomacy, and reduce health disparities.
Provision 9: The profession of nursing, collectively through its professional organizations, must articulate nursing values, maintain the integrity of the profession, and integrate principles of social justice into nursing and health policy.
The ANA Center for Ethics and Human Rights
In addition to publishing the Code of Ethics, the ANA Center for Ethics and Human Rights was established to help nurses navigate ethical and value conflicts and life-and-death decisions, many of which are common to everyday practice.
Check your knowledge with the following questions:
Safety: A Basic Need
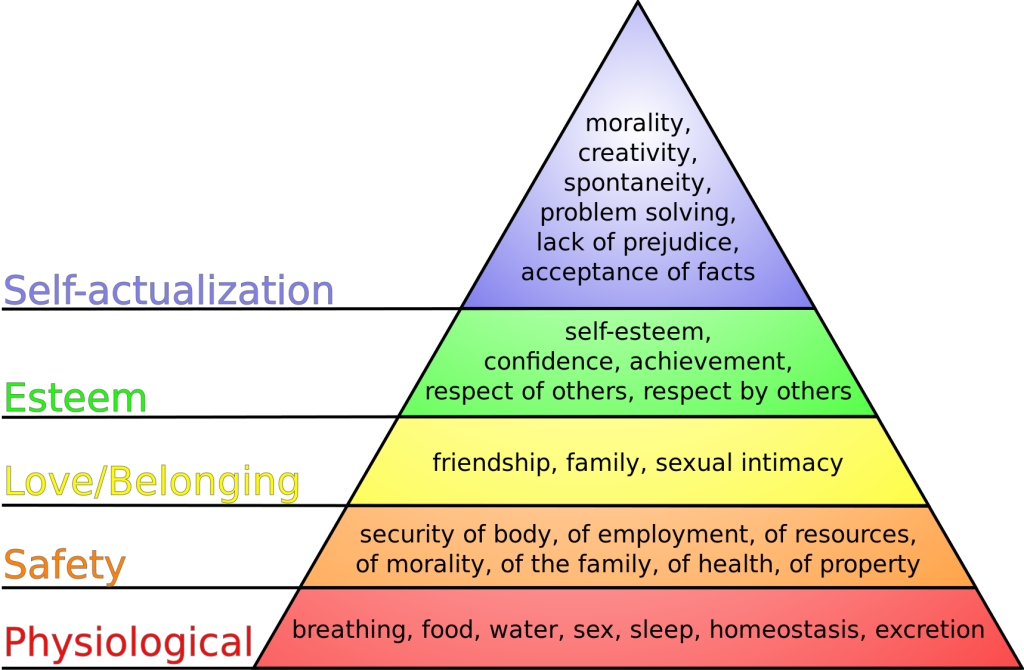
Safety is a basic foundational human need and always receives priority in client care. Nurses typically use Maslow’s Hierarchy of Needs to prioritize urgent client needs, with the bottom two rows of the pyramid receiving top priority. See Figure 5.1[34] for an image of Maslow’s Hierarchy of Needs. Safety is intertwined with basic physiological needs.
Consider the following scenario: You are driving back from a relaxing weekend at the lake and come upon a fiery car crash. You run over to the car to help anyone inside. When you get to the scene, you notice that the lone person in the car is not breathing. Your first priority is not to initiate rescue breathing inside the burning car, but to move the person to a safe place where you can safely provide CPR.
In nursing, the concept of client safety is central to everything we do in all health care settings. As a nurse, you play a critical role in promoting client safety while providing care. You also teach clients and their caregivers how to prevent injuries and remain safe in their homes and in the community. Safe client care also includes measures to keep you safe in the health care environment; if you become ill or injured, you will not be able to effectively care for others.
Safe client care is a commitment to providing the best possible care to every client and their caregivers in every moment of every day. Clients come to health care facilities expecting to be kept safe while they are treated for illnesses and injuries. Unfortunately, you may have heard stories about situations when that did not happen. Medical errors can be devastating to clients and their families. Consider the true story in the following box that illustrates factors affecting client safety.
The Josie King Story
In 2001, 18-month-old Josie King died as a result of medical errors in a well-known hospital from a hospital-acquired infection and an incorrectly administered pain medication. How did this preventable death happen? Watch this video of her mother, Sorrel King, telling Josie’s story and explaining how Josie’s death spurred her work on improving client safety in hospitals everywhere.[35]
Reflective Questions:
- What factors contributed to Josie’s death?
- How could these factors be resolved?
Never Events
The event described in the Josie King story is considered a “never event.” Never events are adverse events that are clearly identifiable, measurable, serious (resulting in death or significant disability), and preventable. In 2007 the Centers for Medicare and Medicaid Services (CMS) discontinued payment for costs associated with never events, and this policy has been adopted by most private insurance companies. Never events are publicly reported, with the goal of increasing accountability by health care agencies and improving the quality of client care. The current list of never events includes seven categories of events:
- Surgical or procedural event, such as surgery performed on the wrong body part
- Product or device, such as injury or death from a contaminated drug or device
- Client protection, such as client suicide in a health care setting
- Care management, such as death or injury from a medication error
- Environmental, such as death or injury as the result of using restraints
- Radiologic, such as a metallic object in an MRI area
- Criminal, such as death or injury of a client or staff member resulting from physical assault on the grounds of a health care setting
Sentinel Events
Sentinel events are very similar to never events although they may not be entirely preventable. They are defined by The Joint Commission as an “A client safety event that reaches a client and results in death, permanent harm, or severe temporary harm requiring interventions to sustain life." Such events are called "sentinel" because they signal the need for immediate investigation and response. Each accredited organization is strongly encouraged, but not required, to report sentinel events to The Joint Commission.[36] It is helpful to facilities to self-report sentinel events so that other facilities can learn from these events and future sentinel events can be prevented through knowledge sharing and risk reduction. Investigations into sentinel events are typically achieved through a process called root cause analysis.
Root cause analysis is a structured method used to analyze serious adverse events to identify underlying problems that increase the likelihood of errors, while avoiding the trap of focusing on mistakes by individuals. A multidisciplinary team analyzes the sequence of events leading up to the error with the goal of identifying how and why the event occurred. The ultimate goal of root cause analysis is to prevent future harm by eliminating hidden problems within a health care system that contribute to adverse events. For example, when a medication error occurs, a root cause analysis goes beyond focusing on the mistake by the nurse and looks at other system factors that contributed to the error, such as similar-looking drug labels, placement of similar-looking medications next to each other in a medication dispensing machine, or vague instructions in a provider order.
Root cause analysis uses human factors science as part of the investigation. Human factors focus on the interrelationships among humans, the tools and equipment they use in the workplace, and the environment in which they work. Safety in health care is ultimately dependent on humans - the doctors, nurses, and health care professionals - providing the care.
Near Misses
In addition to investigating sentinel events and never events, agencies use root cause analysis to investigate near misses. Near misses are defined by the World Health Organization (WHO) as, “An error that has the potential to cause an adverse event (client harm) but fails to do so because of chance or because it is intercepted.” Errors and near misses are rarely the result of poor motivation or incompetence of the health care professional but are often caused by key contributing factors such as poor communication, less-than-optimal teamwork, memory overload, reliance on memory for complex procedures, and lack of standardization of policies and procedures. In an effort to prevent near misses, medical errors, sentinel events, and never events, several safety strategies have been developed and implemented in health care organizations across the country. These strategies will be discussed throughout the remainder of the chapter.
Incident Reports and Client Safety
Recall from the previous discussion in Chapter 2.5 that an incident report is a specific type of documentation performed when there is an error, near miss, or other unexpected occurrence that occurs during client care. Incident reports are used to identify process problems or other areas that could benefit from safety and quality improvement and are not included in the client's medical record. They are a component of an agency's culture of safety and are used during investigations like root cause analysis to help improve the safety and quality of client care.
Effective communication is one of the Standards of Professional Performance established by the American Nurses Association. The standard states, “The registered nurse communicates effectively in all areas of practice.”[37] There are several concepts related to effective communication such as demonstrating appropriate verbal and nonverbal communication, using assertive communication, being aware of personal space, and overcoming common barriers to effective communication.
Types of Communication
Verbal Communication
Effective communication requires each interaction to include a sender of the message, a clear and concise message, and a receiver who can decode and interpret that message. The receiver also provides a feedback message back to the sender in response to the received message. See Figure 2.1[38] for an image of effective communication between a sender and receiver.
Nurses assist clients and their family members to understand health care needs and treatments by using verbal, nonverbal, and written communication. Verbal communication is more than just talking. Effective verbal communication is defined as an exchange of information using words understood by the receiver in a way that conveys professional caring and respect.[39] Nurses who speak using extensive medical jargon or slang may create an unintended barrier to their own verbal communication processes. When communicating with others, it is important for the nurse to assess the receiver’s preferred method of communication and individual receiver characteristics that might influence communication, and subsequently adapt communication to meet the receiver’s needs. For example, the nurse may adapt postsurgical verbal instruction for a pediatric versus an adult client. Although the information requirements regarding signs of infection, pain management, etc., might be similar, the way in which information is provided may be quite different based on developmental level. Regardless of the individual adaptations that are made, the nurse must be sure to always verify client understanding.
Nonverbal Communication
In addition to communicating verbally, the nurse must also be aware of messages sent by nonverbal communication. Nonverbal communication includes facial expressions, tone of voice, pace of the conversation, and body language. Nonverbal communication is more powerful than the verbal message and can have a tremendous impact on the communication experience, with up to 80% of communication being nonverbal communication (see Figure 2.2[40]). The importance of nonverbal communication during communication has also been described in percentages of 55, 38, and 7, meaning 55% of communication is body language, 38% is tone of voice, and 7% is the actual words spoken.[41]
Nonverbal communication includes body language and facial expressions, tone of voice, and pace of the conversation. For example, compare the nonverbal communication messages in Figures 2.3[42] and 2.4.[43] What nonverbal cues do you notice about both toddlers?


Nurses should be attentive to their nonverbal communication cues and the messages they provide to clients and their families. Nurses should be purposeful in their use of nonverbal communication that conveys a feeling of caring.[44] What nonverbal cues do you notice about the nurse in Figure 2.5[45] that provide a perception of professional caring?

Nurses use nonverbal communication such as directly facing clients at eye level, leaning slightly forward, and making eye contact to communicate they care about what the person is telling them and they have their full attention.[46]
![]()
It is common for health care team members in an acute care setting to enter a client’s room and begin interacting with a client who is seated or lying in bed. However, it is important to remember that initial or sensitive communication exchanges are best received by the client if the nurse and client are at eye level. Bringing a chair to the client’s bedside can help to facilitate engagement in the communication exchange. SOLER is common mnemonic used to facilitate nonverbal communication (sit with open posture and lean in with good eye contact in a relaxed manner).
Communication Styles
In addition to verbal and nonverbal communication, people communicate with others using one of three styles: passive, aggressive, or assertive. A passive communicator puts the rights of others before their own. Passive communicators tend to be apologetic or sound tentative when they speak and often do not speak up if they feel they are being wronged. Aggressive communicators, on the other hand, come across as advocating for their own rights despite possibly violating the rights of others. They tend to communicate in a way that tells others their feelings don’t matter. Assertive communicators, in contrast, respect the rights of others while also standing up for their own ideas and rights when communicating. An assertive person is direct, but not insulting or offensive.[47] Assertive communication refers to a way of conveying information that describes the facts and the sender’s feelings without disrespecting the receiver’s feelings. Using “I” messages such as, “I feel…,” “I understand…,” or “Help me to understand…” are strategies for assertive communication. This method of communicating is different from aggressive communication that uses “you” messages and can feel as if the sender is verbally attacking the receiver rather than dealing with the issue at hand. For example, instead of saying to a coworker, “Why is it always so messy in your clients’ rooms? I dread following you on the next shift!,” an assertive communicator would use “I” messages to say, “I feel frustrated spending the first part of my shift decluttering our clients’ rooms. Help me understand why it is a challenge to keep things organized during your shift?”
Using assertive communication is an effective way to solve problems with clients, coworkers, and health care team members.
View this supplementary YouTube video on How to Communicate Assertively.
Personal Space
While being aware of verbal and nonverbal messages and communicating assertively, it is also important to be aware of others’ personal space. Proxemics is the study of personal space and provides guidelines for professional communication. The public zone is over 10 feet of distance between people and generally avoids physical contact. The social zone is four to 10 feet of distance between people. It is used during social interactions and business settings. The personal zone is 18 inches to four feet of space and is generally reserved for friends and family. Less than 18 inches is reserved for close relationships but may be invaded when in crowds or playing sports.[48] Nurses usually communicate within the social zone to maintain professional boundaries. However, when assessing clients and performing procedures, nurses often move into a client's personal zone. Nurses must be aware of clients’ feelings of psychological discomfort that can occur when invading this zone. Additionally, cultural considerations may impact the appropriateness of personal space when providing client care. See Figure 2.6 for example of personal space zones.[49]
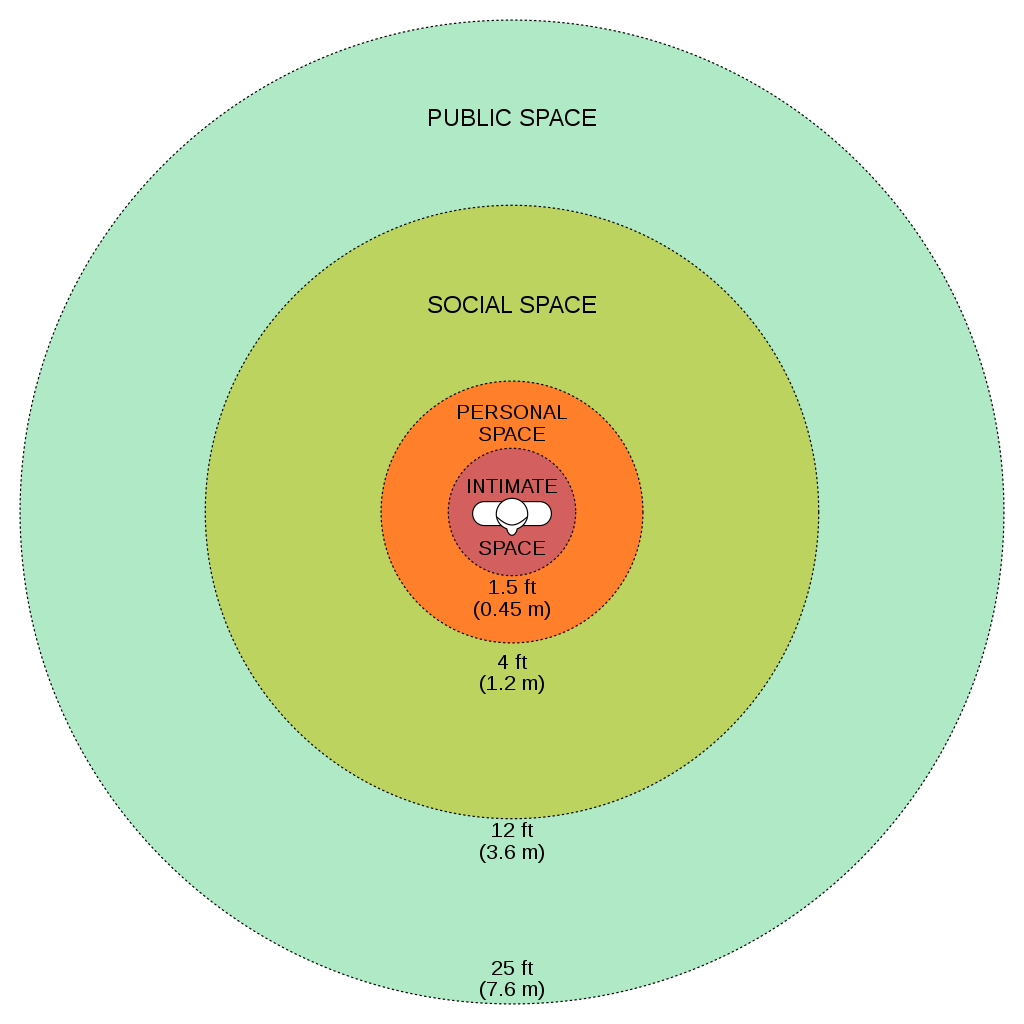
Overcoming Common Barriers to Communication
Nurses must reflect on personal factors that influence their ability to communicate effectively. There are many factors that can cause the message you are trying to communicate to become distorted and not perceived by the receiver in the way you intended. For this reason, is important to seek feedback that your message is clearly understood. Nurses must be aware of these potential barriers and try to reduce their impact by continually seeking feedback and checking understanding.[50]
Common barriers to communication in health care and strategies to overcome them are described in the following box.[51]
Common Barriers to Communication in Health Care
- Jargon: Avoid using medical terminology, complicated, or unfamiliar words. When communicating with clients, explain information in plain language that is easy to understand by those without a medical or nursing background.
- Lack of attention: Nurses are typically very busy with several tasks to complete for multiple clients. It is easy to become focused on the tasks instead of the client. When entering a client’s room, it is helpful to pause, take a deep breath, and mindfully focus on the client in front of you to give them your full attention. Clients should feel as if they are the center of your attention when you are with them, no matter how many other things you have going on.
- Noise and other distractions: Health care environments can be very noisy with people talking in the room or hallway, the TV playing, alarms beeping, and pages occurring overhead. Create a calm, quiet environment when communicating with clients by closing doors to the hallway, reducing the volume of the TV, or moving to a quieter area, if possible.
- Light: A room that is too dark or too light can create communication barriers. Ensure the lighting is appropriate according to the client's preference.
- Hearing and speech problems: If your client has hearing or speech problems, implement strategies to enhance communication. See the “Adapting Your Communication” subsection below for strategies to address hearing and speech problems.
- Language differences: If English is not your client’s primary language, it is important to seek a medical interpreter and to also provide written handouts in the client’s preferred language when possible. Most agencies have access to an interpreter service available by phone if they are not available on-site.
- Differences in cultural beliefs: The norms of social interaction vary greatly in different cultures, as well as the ways that emotions are expressed. For example, the concept of personal space varies among cultures, and some clients are stoic about pain whereas others are more verbally expressive. Read more about caring for diverse clients in the “Diverse Patients” chapter.
- Psychological barriers: Psychological states of the sender and the receiver affect how the message is sent, received, and perceived. For example, if nurses are feeling stressed and overwhelmed with required tasks, the nonverbal communication associated with their messages such as lack of eye contact, a hurried pace, or a short tone can affect how the client perceives the message. If a client is feeling stressed, they may not be able to “hear” the message or they may perceive it differently than it was intended. It is important to be aware of signs of the stress response in ourselves and our clients and implement appropriate strategies to manage the stress response. See the box below for more information about strategies to manage the stress response.
- Physiological barriers: It is important to be aware of clients’ potential physiological barriers when communicating. For example, if a client is in pain, they are less likely to hear and remember what was said, so pain relief should be provided as needed before providing client education. However, it is also important to remember that sedatives and certain types of pain medications often impair the client’s ability to receive and perceive messages so health care documents cannot be signed by a client after receiving these types of medications.
- Physical barriers for nonverbal communication: Providing information via e-mail or text is often less effective than face-to-face communication. The inability to view the nonverbal communication associated with a message such as tone of voice, facial expressions, and general body language often causes misinterpretation of the message by the receiver. When possible, it is best to deliver important information to others using face-to-face communication so that nonverbal communication is included with the message.
- Differences in perception and viewpoints: Everyone has their own beliefs and perspectives and wants to feel “heard.” When clients feel their beliefs or perspectives are not valued, they often become disengaged from the conversation or the plan of care. Nurses should provide health care information in a nonjudgmental manner, even if the client’s perspectives, viewpoints, and beliefs are different from their own.
Managing the Stress Response[52]
The stress response is a common psychological barrier to effective communication. It can affect the message sent by the sender or how it is received by the receiver. The stress response is a common reaction to life events, such as a nurse feeling stressed by being overwhelmed with tasks to complete for multiple clients, or a client feeling stressed when admitted to a hospital or receiving a new diagnosis. Symptoms of the stress response include irritability, sweaty palms, a racing heart, difficulty concentrating, and impaired sleep. It is important to recognize symptoms of the stress response in ourselves and our clients and use strategies to manage the stress response when communicating. Strategies to manage the stress response include the following:
- Use relaxation breathing. Become aware of your breathing. Take a deep breath in your nose and blow it out through your mouth. Repeat this process at least three times in succession and then as often as needed throughout the day.
- Make healthy diet choices. Avoid caffeine, nicotine, and junk food because these items can increase feelings of anxiety or being on edge.
- Make time for exercise. Exercise stimulates the release of natural endorphins that reduce the body’s stress response and also helps to improve sleep.
- Get enough sleep. Set aside at least 30 minutes before going to bed to wind down from the busyness of the day. Avoid using electronic devices like cell phones before bedtime because the backlight can affect negatively impact sleep.
- Use progressive relaxation. There are several types of relaxation techniques that focus on reducing muscle tension and using mental imagery to induce calmness. Progressive relaxation generally includes the following steps:
- Start by lying down somewhere comfortable and firm, such as a rug or mat on the floor. Get yourself comfortable.
- Relax and try to let your mind go blank. Breathe slowly, deeply, and comfortably, while gradually and consciously relaxing all your muscles, one by one.
- Work around the body one main muscle area at a time, breathing deeply, calmly, and evenly. For each muscle group, clench the muscles tightly and hold for a few seconds, and then relax them completely. Repeat the process, noticing how it feels. Do this for each of your feet, calves, thighs, buttocks, stomach, arms, hands, shoulders, and face.
Professional communication with other members of the health care team is an important component of every nurse’s job. See Figure 2.8[53] for an image illustrating communication between health care team members. Common types of professional interactions include reports to health care team members, handoff reports, and transfer reports. Reports may be verbal (e.g., reports given in person, by telephone, or recorded) or written (e.g., reports provided electronically or by fax).

Reports to Health Care Team Members
Nurses routinely report information to other nurses and health care team members, as well as urgently contact health care providers to report changes in client status.
Standardized methods of communication have been developed to allow information to be exchanged between health care team members in a structured, concise, and accurate manner to ensure safe client care. One common format used by health care team members to exchange client information is ISBARR, a mnemonic for the components of Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat back or a simpler version called SBAR:
-
- Introduction: Introduce your name, role, and the agency from which you are calling.
- Situation: Provide the client’s name and location, why you are calling, recent vital signs, and the status of the client.
- Background: Provide pertinent background information about the client such as admitting medical diagnoses, code status, recent relevant lab or diagnostic results, and allergies.
- Assessment: Share abnormal assessment findings and your evaluation of the current client situation.
- Request/Recommendations: State what you would like the provider to do, such as reassess the client, order a lab/diagnostic test, prescribe/change medication, etc.
- Repeat back: If you are receiving new orders from a provider, repeat them to confirm accuracy. Be sure to document communication with the provider in the client’s chart.
Read an example of an ISBARR report in the following box. Information is provided to a printable ISBARR reference card.
Sample ISBARR Report From a Nurse to a Health Care Provider
I: “Hello Dr. Smith, this is Jane White, RN from the Med Surg unit.”
S: “I am calling to tell you about Ms. White in Room 210, who is experiencing an increase in pain, as well as redness at her incision site. The client has no known allergies and is a full code. Her recent vital signs were BP 160/95, heart rate 90, respiratory rate 22, O2 sat 96%, and temperature 38 degrees Celsius. She is stable but her pain is worsening.”
B: “Ms. White is a 65-year-old female, admitted yesterday post hip surgical replacement. She has been rating her pain at 3 or 4 out of 10 since surgery with her scheduled medication, but now she is rating the pain as a 7, with no relief from her scheduled medication of Vicodin 5/325 mg administered an hour ago. She is scheduled for physical therapy later this morning and is stating she won’t be able to participate because of the pain this morning.”
A: “I just assessed the surgical site, and her dressing was clean, dry, and intact, but there is 4 cm redness surrounding the incision, and it is warm and tender to the touch. There is moderate serosanguinous drainage. Otherwise, her lungs are clear, and her heart rate is regular. I am concerned her incision site may be becoming infected and that she will have difficulty with therapy if her pain remains uncontrolled.”
R: “I am calling to request an order for a CBC and increased dose of pain medication.”
R: “I am repeating back the order to confirm that you are ordering a STAT CBC and an increase of her Vicodin to 10/325 mg.”
View or print an ISBARR reference card
Handoff Reports
Handoff reports are defined by The Joint Commission as “a transfer and acceptance of client care responsibility achieved through effective communication. It is a real-time process of passing client specific information from one caregiver to another, or from one team of caregivers to another, for the purpose of ensuring the continuity and safety of the client’s care.”[54] In 2017, The Joint Commission issued a critical alert about inadequate handoff communication that has resulted in client harm such as wrong-site surgeries, delays in treatment, falls, and medication errors. Strategies for improving handoff communication have been implemented at agencies across the country.
Although many types of nursing shift-to-shift handoff reports have been used over the years, evidence strongly supports that bedside handoff reports increase client safety, as well as client and nurse satisfaction, by effectively communicating current, accurate client information in real time.[55] See Figure 2.9[56] for an image illustrating two nurses participating in a handoff report. Bedside reports typically occur in hospitals and include the client, along with the off-going and the oncoming nurses in a face-to-face handoff report conducted at the client's bedside. HIPAA rules must be kept in mind if visitors are present, or the room is not a private room. Family members may be included with the client’s permission. See a sample checklist for a bedside handoff report from the Agency for Healthcare Research and Quality in Figure 2.10.[57] Although a bedside handoff report is similar to an ISBARR report, it contains additional information to ensure continuity of care across nursing shifts. For example, the “assessment” portion of the bedside handoff report includes detailed pertinent data the oncoming nurse needs to know, such as current head-to-toe assessment findings to establish a baseline; information about equipment such as IVs, catheters, and drainage tubes; and recent changes in medications, lab results, diagnostic tests, and treatments.
![]"618721604-huge" by Rido is used under license from Shutterstock.com. Image showing two nurses discussing a chart both are holding](https://opencontent.ccbcmd.edu/app/uploads/sites/32/2024/08/618721604-huge-scaled-1.jpg)
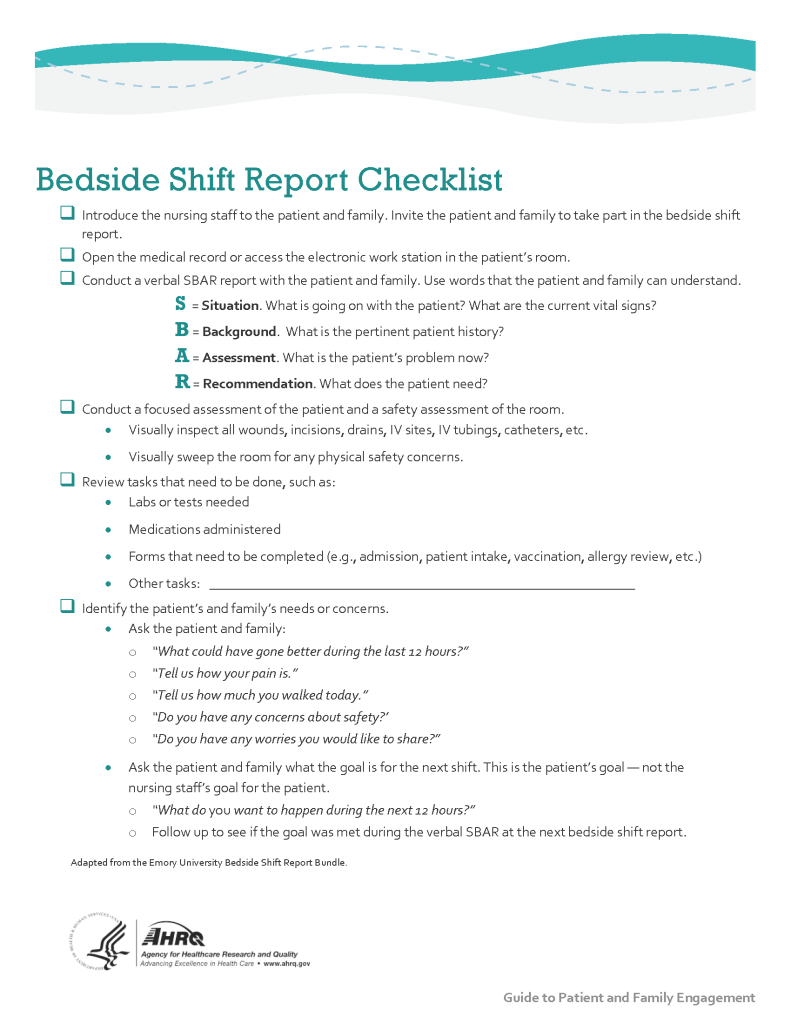
Print a copy of the AHRQ Bedside Shift Report Checklist.
View a video on creating shift reports.[58]
Transfer Reports
Transfer reports are provided by nurses when transferring a client to another unit or to another agency. Transfer reports contain similar information as bedside handoff reports but are even more detailed when the client is being transferred to another agency. Checklists are often provided by agencies to ensure accurate, complete information is shared.
Conflict in the Workplace
Nurses encounter conflict in their daily work environment, such as misunderstandings or disagreements among staff, clients, providers, family members, or other individuals. Nurses must learn communication methods that lessen conflict and enhance interactions that lead to a better work environment.
Read additional information about "Conflict Resolution" in Open RN Nursing Health Alterations.
Before learning how to use the nursing process, it is important to understand basic concepts concerning how critical thinking relates to nursing practice. Let's take a deeper look at how nurses think.
Critical Thinking and Clinical Reasoning
Nurses make decisions while providing client care by using critical thinking and clinical reasoning. Critical thinking is a broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.”[59] Using critical thinking means that nurses take extra steps to maintain client safety and don’t just “follow orders.” It also means the accuracy of client information is validated and plans for caring for clients are based on their needs, current clinical practice, and research.
“Critical thinkers” possess certain attitudes that foster rational thinking. These attitudes are as follows:
- Independence of thought: Thinking on your own
- Fair-mindedness: Treating every viewpoint in an unbiased, unprejudiced way
- Insight into egocentricity and sociocentricity: Thinking of the greater good and not just thinking of yourself. Knowing when you are thinking of yourself (egocentricity) and when you are thinking or acting for the greater good (sociocentricity)
- Intellectual humility: Recognizing your intellectual limitations and abilities
- Nonjudgmental: Using professional ethical standards and not basing your judgments on your own personal or moral standards
- Integrity: Being honest and demonstrating strong moral principles
- Perseverance: Persisting in doing something despite it being difficult
- Confidence: Believing in yourself to complete a task or activity
- Interest in exploring thoughts and feelings: Wanting to explore different ways of knowing
- Curiosity: Asking “why” and wanting to know more
Clinical reasoning is defined as, “A complex cognitive process that uses formal and informal thinking strategies to gather and analyze client information, evaluate the significance of this information, and weigh alternative actions.”[60] To make sound judgments about client care, nurses must generate alternatives, weigh them against the evidence, and choose the best course of action. The ability to clinically reason develops over time and is based on knowledge and experience.[61]
Inductive and Deductive Reasoning and Clinical Judgment
Inductive and deductive reasoning are important critical thinking skills. They help the nurse use clinical judgment when implementing the nursing process.
Inductive reasoning involves noticing cues, making generalizations, and creating hypotheses based on specific information or incidents. Cues are data that fall outside of expected findings that give the nurse a hint or indication of a client’s potential problem or condition. The nurse organizes these cues into patterns and creates a generalization. A generalization is a judgment formed from a set of facts, cues, and observations and is similar to gathering pieces of a jigsaw puzzle into patterns until the whole picture becomes more clear. Based on generalizations created from patterns of data, the nurse creates a hypothesis regarding a client problem. A hypothesis is a proposed explanation for a situation. It attempts to explain the “why” behind the problem that is occurring. If a “why” is identified, then a solution can begin to be explored.
No one can draw conclusions without first noticing cues. Paying close attention to a client, the environment, and interactions with family members is critical for inductive reasoning. As you work to improve your inductive reasoning, begin by first noticing details about the things around you. A nurse is similar to the detective looking for cues in Figure 4.1.[62] Be mindful of your five primary senses: the things that you hear, feel, smell, taste, and see. Nurses need strong inductive reasoning patterns and be able to take action quickly, especially in emergency situations. They can see how certain objects or events form a pattern (i.e., generalization) that indicates a common problem (i.e., hypothesis).
Example: A nurse assesses a client and finds the surgical incision site is red, warm, and tender to the touch. The nurse recognizes these cues form a pattern of signs of infection and creates a hypothesis that the incision has become infected. The provider is notified of the client’s change in condition, and a new prescription is received for an antibiotic. This is an example of the use of inductive reasoning in nursing practice.

Deductive reasoning is another type of critical thinking that is referred to as “top-down thinking.” Deductive reasoning relies on using a general standard or rule to create a strategy. Deductive reasoning relies on a general statement or hypothesis - sometimes called a premise or standard - that is held to be true. The premise is used to reach a specific, logical conclusion. Nurses use standards set by their state's Nurse Practice Act, federal regulations, the American Nursing Association, professional organizations, and their employer to make decisions about client care and solve problems.
Example: Based on research findings, hospital leaders determine clients recover more quickly if they receive adequate rest. The hospital creates a policy for quiet zones at night by initiating no overhead paging, promoting low-speaking voices by staff, and reducing lighting in the hallways. (See Figure 4.2).[63] The nurse further implements this policy by organizing care for clients that promotes periods of uninterrupted rest at night. This is an example of deductive thinking because the intervention is applied to all clients regardless if they have difficulty sleeping or not.
Clinical judgment is the result of critical thinking and clinical reasoning using inductive and deductive reasoning. Clinical judgment is defined by the National Council of State Boards of Nursing (NCSBN) as, “The observed outcome of critical thinking and decision-making. It uses nursing knowledge to observe and assess presenting situations, identify a prioritized client concern, and generate the best possible evidence-based solutions in order to deliver safe client care.”[64] The NCSBN administers the national licensure exam (NCLEX) that evaluates the decision-making ability of nursing graduates and sets a minimum standard for safe, competent nursing care by entry-level licensed nurses. The NCLEX uses the NCSBN Clinical Judgment Measurement Model (NCJMM) to measure clinical judgment.
Evidence-based practice (EBP) is defined by the American Nurses Association (ANA) as, “A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and client, family, group, community, and population preferences and values.”[65]
Nursing Process
The nursing process is a critical thinking model based on a systematic approach to client-centered care. Nurses use the nursing process to perform clinical reasoning and make clinical judgments when providing client care. The nursing process is based on the Standards of Professional Nursing Practice established by the American Nurses Association (ANA). These standards are authoritative statements of the actions and behaviors that all registered nurses (RNs), regardless of role, population, specialty, and setting, are expected to perform competently.[66] The mnemonic ADOPIE is an easy way to remember the ANA Standards and the nursing process. Each letter refers to the six components of the nursing process: Assessment, Diagnosis, Outcomes Identification, Planning, Implementation, and Evaluation.
The nursing process is a continuous, cyclical process that is constantly adapting to the client’s current health status. See Figure 4.3[67] for an illustration of the nursing process.
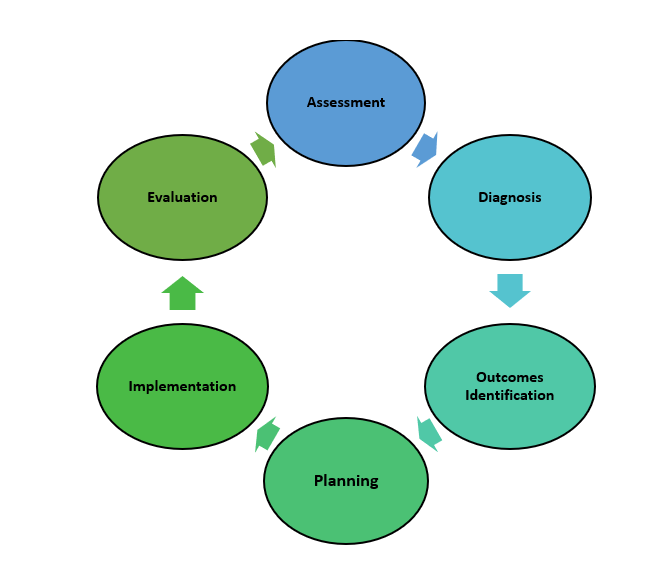
The ANA's Standards of Professional Nursing Practice associated with each component of the nursing process are described below.
Assessment
The "Assessment" Standard of Practice is defined as, “The registered nurse collects pertinent data and information relative to the health care consumer’s health or the situation.”[68] A registered nurse uses a systematic method to collect and analyze client data. Assessment includes physiological data, as well as psychological, sociocultural, spiritual, economic, and lifestyle data. For example, a nurse’s assessment of a hospitalized client in pain includes recognizing cues such as the client’s response to pain, such as the inability to get out of bed, refusal to eat, withdrawal from family members, or anger directed at hospital staff.[69]
Licensed practical/vocational nurses (LPN/VNs) assist with gathering data according to their state's scope of practice, but do not analyze data because this is outside their scope of practice. The "Assessment" component of the nursing process is further described in the "Assessment" section of this chapter.
Diagnosis
The "Diagnosis" Standard of Practice is defined as, “The registered nurse analyzes the assessment data to determine actual or potential diagnoses, problems, and issues.”[70] A nursing diagnosis is the nurse’s clinical judgment about the response from the client to actual or potential health conditions or needs. Nursing diagnoses are the bases for the nurse’s care plan and are different than medical diagnoses.[71]
Analyzing assessment data and formulating a nursing diagnosis is outside the scope of practice for LPN/VNs, and as such, they do not assist with this phase of the nursing process. The "Diagnosis" component of the nursing process is further described in the "Diagnosis" section of this chapter.
Outcome Identification
The "Outcome Identification" Standard of Practice is defined as, “The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation.”[72] The nurse sets measurable and achievable short- and long-term goals and specific outcomes in collaboration with the client based on their assessment data and nursing diagnoses.
Outcome identification is outside the scope of practice of LPN/VNs, and as such, they do not assist with this phase of the nursing process. The "Outcome Identification" component of the nursing process is further described in the "Outcome Identification" section of this chapter.
Planning
The "Planning" Standard of Practice is defined as, “The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes.”[73] Assessment data, diagnoses, and goals are used to select evidence-based nursing interventions customized to each client’s needs in order to achieve their previously established goals and outcomes. Nursing interventions are planned and documented by RNs in the client's nursing care plan so that nurses, as well as other health professionals, can refer to it for continuity of care.[74]
The "Planning" component of the nursing process is further described in the "Planning" section of this chapter.
Nursing Care Plans
Creating nursing care plans is a part of the "Planning" step of the nursing process. A nursing care plan is a type of documentation that demonstrates the individualized planning and delivery of nursing care for each specific client using the nursing process. RNs create nursing care plans so that the care provided to the client across shifts is consistent among health care personnel. Some interventions can be delegated to LPN/VNs or trained Unlicensed Assistive Personnel (UAPs) with RN supervision.
Creating the nursing care plan is outside the scope of practice, and as such, the LPN/VNs do not perform this task, although they may contribute to it. Developing nursing care plans and implementing appropriate delegation are further discussed under the “Planning” and “Implementation of Interventions” sections of this chapter.
Implementation
The "Implementation" Standard of Practice is defined as, "The nurse implements the identified plan.”[75] Nursing interventions are implemented or delegated with supervision according to the care plan to assure continuity of care across multiple nurses and health professionals caring for the client. Interventions are documented in the client’s electronic medical record as they are completed.[76] LPN/VNs implement interventions contained in the nursing care plan, provided they are within their scope of practice. The LPN/VN is responsible for documenting the interventions they perform in the client's medical record.
The "Implementation" Standard of Professional Practice also includes the subcategories "Coordination of Care" and "Health Teaching and Health Promotion" to promote health and a safe environment.[77]
The "Implementation" component of the nursing process is further described in the "Implementation of Interventions" section of this chapter.
Evaluation
The "Evaluation" Standard of Practice is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.”[78] During evaluation, nurses reassess the client and compare the findings against established outcomes to determine the effectiveness of the interventions and overall nursing care plan. During this phase, RNs ask, "Were outcomes met? Are any modifications required for the nursing care plan?" Both the client’s status and the effectiveness of the nursing care plan are continuously evaluated and modified as needed.[79]
Evaluating and modifying the nursing care plan is outside the scope of practice of LPN/VNs, although they can assist in gathering assessment data to assist the RN in performing this step of the nursing process. The "Evaluation" component of the nursing process is further described in the "Evaluation" section of this chapter.
Benefits of Using the Nursing Process
Using the nursing process has many benefits for nurses, clients, and other members of the health care team. The benefits of using the nursing process include the following:
- Promotes quality client care
- Decreases omissions and duplications
- Provides a guide for all staff involved to provide consistent and responsive care
- Encourages collaborative management of a client’s health care problems
- Improves client safety
- Improves client satisfaction
- Identifies a client’s goals and strategies to attain them
- Increases the likelihood of achieving positive client outcomes
- Saves time, energy, and frustration by creating a care plan that is accessible to all staff caring for a client
By using these components of the nursing process as a critical thinking model, nurses plan outcomes and interventions that are customized to the client’s specific needs, ensure the interventions are evidence-based, and evaluate the effectiveness of interventions in meeting the client’s needs.
NCSBN Clinical Judgment Measurement Model
The NCSBN Clinical Judgment Measurement Model (NCJMM) complements the nursing process, but it is a model that assesses an NCLEX candidate’s clinical judgment. Terminology used by this model includes recognize cues, analyze cues, prioritize hypotheses, generate solutions, take action, and evaluate outcomes. See Figure 4.3b[80] and Table 4.2a for comparisons of NCJMM terms and the nursing process.[81],[82],[83]
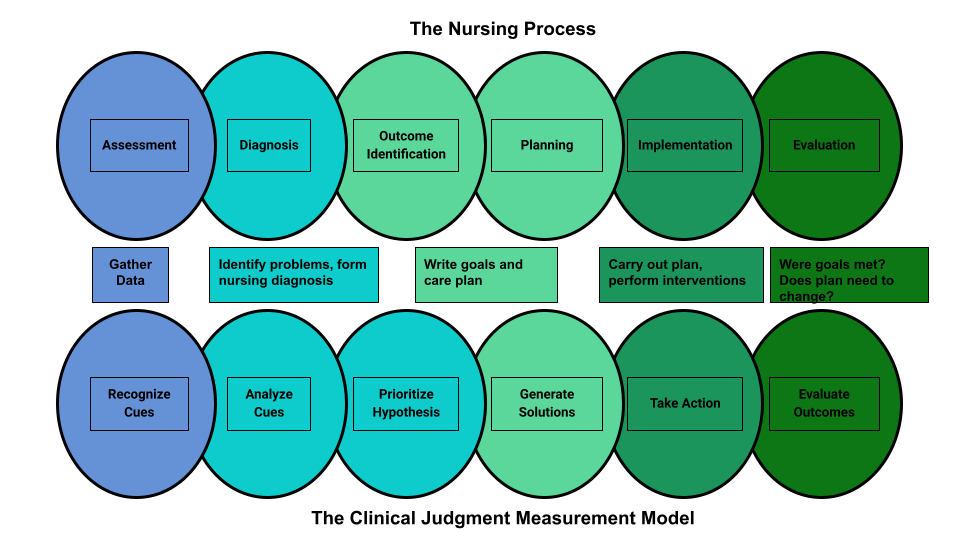
Figure 4.3b Comparison of the Steps of the NCJMM to the Nursing Process
Table 4.2a Comparison of the NCJMM to the Nursing Process
| NCSBN Clinical Judgment Skill | Description | Corresponding Step of the Nursing Process |
|---|---|---|
| Recognize Cues | What data is clinically significant?
Determining what client findings are significant, most important, and of immediate concern to the nurse (i.e., identifying “relevant cues”). |
Assessment |
| Analyze Cues | What does the data mean?
Analyzing data to determine if it is “expected” or “unexpected” or “normal” or “abnormal” for this client at this time according to their age, development, and clinical status. Making a clinical judgment concerning the client's “human response to health conditions/life processes, or a vulnerability for that response”; also referred to as “forming a hypothesis.” |
Diagnosis
(Analysis of Data) |
| Prioritize Hypotheses | What hypotheses should receive priority attention?
Ranking client conditions and problems according to urgency, complexity, and time. |
Planning |
| Generate Solutions | What should be done?
Planning individualized interventions that meet the desired outcomes for the client; may include gathering additional assessment data. |
Planning |
| Take Action | What will I do now?
Implementing interventions that are safe and most appropriate for the client’s current priority conditions and problems. |
Implementation |
| Evaluate Outcomes | Did the interventions work?
Comparing actual client outcomes with desired client outcomes to determine effectiveness of care and making appropriate revisions to the nursing care plan. |
Evaluation |
Learning activities are incorporated throughout this book to help students practice answering NCLEX Next Generation-style test questions.
Review Scenario A in the following box for an example of a nurse using the nursing process and NCJMM skills while providing client care.
Client Scenario A: Using the Nursing Process[84]

A nurse is caring for a hospitalized client with a medical diagnosis of heart failure who has a prescription to receive furosemide 80mg IV every morning. The nurse uses critical thinking according to the nursing process and the NCJMM before administering the prescribed medication:
Assessment/Recognize Cues: During the morning assessment, the nurse notes that the client has a blood pressure of 98/60, heart rate of 100, respirations of 18, and a temperature of 98.7F.
Diagnosis/Analyze Cues: The nurse reviews the medical record for the client’s vital signs baseline and observes the blood pressure trend is around 110/70 and the heart rate in the 80s.
Planning/Prioritize Hypothesis: The nurse recognizes cues (assessment data) that form a pattern related to fluid imbalance and hypothesizes that the client may be dehydrated.
Planning/Generate Solutions: The nurse gathers additional information and notes the client’s weight has decreased four pounds since yesterday. The nurse talks with the client and validates the hypothesis when the client reports that their mouth feels like cotton, and they feel light-headed. By using critical thinking and clinical judgment, the nurse diagnoses the client with the nursing diagnosis Fluid Volume Deficit and plans interventions for reestablishing fluid balance.
Implementation/Take Action: The nurse withholds the administration of IV furosemide and contacts the health care provider to discuss the client’s current fluid status. After contacting the provider, the nurse initiates additional nursing interventions to promote oral intake and closely monitors hydration status.
Evaluation/Evaluate Outcomes: By the end of the shift, the nurse evaluates the client status and determines that fluid balance has been restored.
In Scenario A, the nurse is using clinical judgment and not just “following orders” to administer the Lasix as scheduled. The nurse assesses the client, recognizes and analyzes cues, creates a hypothesis regarding the fluid status, plans and implements nursing interventions, and evaluates outcomes. While performing these steps, the nurse promotes client safety by contacting the provider before administering a medication that could cause harm to the client at this time.
Holistic Nursing Care
Using the nursing process and clinical judgment while implementing evidence-based practices is referred to as the "science of nursing." Before getting deeper into the science of nursing in the remainder of this chapter, it is important to discuss the "art of nursing" that relies on holistic care provided in a compassionate and caring manner using the nursing process.
The American Nurses Association (ANA) defines nursing as, “Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in the recognition of the connection of all humanity.”[85]
The ANA further describes nursing as a learned profession built on a core body of knowledge that integrates both the art and science of nursing. The art of nursing is defined as, "Unconditionally accepting the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care."[86]
Nurses care for individuals holistically, including their emotional, spiritual, psychosocial, cultural, and physical needs. They consider problems, issues, and needs that the person experiences as a part of a family and a community as they use the nursing process. Review a scenario illustrating holistic nursing care provided to a client and their family in the following box.
Holistic Nursing Care Scenario
A single mother brings her child to the emergency room for ear pain and a fever. The physician diagnoses the child with an ear infection and prescribes an antibiotic. The mother is advised to make a follow-up appointment with their primary provider in two weeks. While providing discharge teaching, the nurse discovers that the family is unable to afford the expensive antibiotic prescribed and cannot find a primary care provider in their community they can reach by a bus route. The nurse asks a social worker to speak with the mother about affordable health insurance options and available providers in her community and follows up with the prescribing physician to obtain a prescription for a less expensive generic antibiotic. In this manner, the nurse provides holistic care and advocates for improved health for the child and their family.
Caring and the Nursing Process
The American Nurses Association (ANA) states, "The act of caring is foundational to the practice of nursing."[87] Successful use of the nursing process requires the development of a care relationship with the client. A care relationship is a mutual relationship that requires the development of trust between both parties. This trust is often referred to as the development of rapport and underlies the art of nursing. While establishing a caring relationship, the whole person is assessed, including the individual’s beliefs, values, and attitudes, while also acknowledging the vulnerability and dignity of the client and family. Assessing and caring for the whole person takes into account the physical, mental, emotional, and spiritual aspects of being a human being.[88] Caring interventions can be demonstrated in simple gestures such as active listening, making eye contact, using therapeutic touch, and providing emotional support while respecting their cultural beliefs associated with caring behaviors.[89] See Figure 4.4[90] for an image of a nurse using touch as a therapeutic communication technique to communicate caring.
Dr. Jean Watson is a nurse theorist who has published many works on the art and science of caring in the nursing profession. Her theory of human caring sought to balance the cure orientation of medicine, giving nursing its unique disciplinary, scientific, and professional standing with itself and the public. Dr. Watson’s caring philosophy encourages nurses to be authentically present with their clients while creating a healing environment.[91]

Now that we have discussed basic concepts related to the nursing process, as well as the science and art of nursing, let’s look more deeply at each component of the nursing process in the following sections.
Learning Objectives
- Reflect upon personal and cultural values, beliefs, biases, and heritage[92]
- Embrace diversity, equity, inclusivity, health promotion, and health care for individuals of diverse geographic, cultural, ethnic, racial, gender, and spiritual backgrounds across the life span[93]
- Demonstrate respect, equity, and empathy in actions and interactions with all health care consumers[94]
- Participate in life-long learning to understand cultural preferences, worldviews, choices, and decision-making processes of diverse clients[95]
- Adapt care considering all aspects of diversity
- Identify principles of protecting client dignity
- Identify principles of holistic, client-centered care
- Identify strategies to advocate for clients
- Identify principles of religion and spirituality
No matter who we are or where we come from, every person was raised with cultural values and beliefs. The impact of culture on a person’s health is profound because it affects many health beliefs, such as perceived causes of illness, ways to prevent illness, and acceptance of medical treatments. Culturally responsive care integrates these cultural beliefs into an individual's health care. Culturally responsive care is intentional and promotes trust and rapport with clients. At its heart, culturally responsive care is client-centered care. The American Nurses Association (ANA) states, "The art of nursing is demonstrated by unconditionally accepting the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care."[96]
Nurses provide holistic care when incorporating their clients’ physical, mental, spiritual, cultural, and social needs into their health care (referred to as holism). As a nursing student, you are undertaking a journey of developing cultural competency with an attitude of cultural humility as you learn how to provide holistic care to your clients. Cultural competence is a lifelong process of applying evidence-based nursing in agreement with the cultural values, beliefs, worldview, and practices of clients to produce improved client outcomes.[97],[98],[99]
Cultural humility is defined by the American Nurses Association as, "A humble and respectful attitude toward individuals of other cultures that pushes one to challenge their own cultural biases, realize they cannot know everything about other cultures, and approach learning about other cultures as a life-long goal and process."[100] Nurses improve the quality of health care by understanding, respecting, and incorporating their clients' cultural values, beliefs, and preferences, which can ultimately help reduce health disparities.[101]
This chapter will introduce concepts related to adapting nursing care that considers all aspects of diversity.
After establishing a culturally sensitive environment and performing a cultural assessment, nurses and nursing students can continue to promote culturally responsive care. Culturally responsive care includes creating a culturally safe environment, using cultural negotiation, and considering the impact of culture on clients’ time orientation, space orientation, eye contact, and food choices.
Culturally Safe Environment
A primary responsibility of the nurse is to ensure the environment is culturally safe for the client. A culturally safe environment is a safe space for clients to interact with the nurse, without judgment or discrimination, where the client is free to express their cultural beliefs, values, and identity. This responsibility belongs to both the individual nurse and also to the larger health care organization.
Cultural Negotiation
Many aspects of nursing care are influenced by the client’s cultural beliefs, as well as the beliefs of the health care culture. For example, the health care culture in the United States places great importance on punctuality for medical appointments, yet a client may belong to a culture that views “being on time” as relative. In some cultures, time is determined simply by whether it is day or night or time to wake up, eat, or sleep. Making allowances or accommodations for these aspects of a client’s culture is instrumental in fostering the nurse-client relationship. This accommodation is referred to as cultural negotiation. See Figure 3.6[102] for an image illustrating cultural negotiation. During cultural negotiation, both the client and nurse seek a mutually acceptable way to deal with competing interests of nursing care, prescribed medical care, and the client’s cultural needs. Cultural negotiation is reciprocal and collaborative. When a client’s cultural needs do not significantly or adversely affect their treatment plan, their cultural needs should be accommodated when feasible.
As an example, think about the client previously discussed for whom a fixed schedule is at odds with their cultural views. Instead of teaching the client to take a daily medication at a scheduled time, the nurse could explain that the client should take the medication every day when he awakens rather than every morning at 0800. Another example of cultural negotiation is illustrated by a scenario in which the nurse is preparing a client for a surgical procedure. As the nurse goes over the preoperative checklist, the nurse asks the client to remove her head covering (hijab). The nurse is aware that personal items should be removed before surgery; however, the client wishes to keep on the hijab. As an act of cultural negotiation and respect for the client’s cultural beliefs, the nurse makes arrangements with the surgical team to keep the client’s hijab in place for the surgical procedure and covering the client’s hijab with a surgical cap.

Decision-Making
Health care culture in the United States mirrors cultural norms of the country, with an emphasis on individuality, personal freedom, and self-determination. Self-determination refers to a person's right to determine what will be done with and to their own body. This perspective may conflict with a client whose cultural background values group decision-making and decisions made to benefit the group, not necessarily the individual. As an example, in the 2019 film The Farewell, a Chinese-American family decides to not tell the family matriarch she is dying of cancer and only has a few months left to live. The family keeps this secret from the woman in the belief that the family should bear the emotional burden of this knowledge, which is a collectivistic viewpoint in contrast to American individualistic viewpoint.
Space Orientation
The amount of space that a person surrounds themselves with to feel comfortable is influenced by culture. See Figure 3.7[103] for an image illustrating space orientation. For example, for some people, it would feel awkward to stand four inches away from another person while holding a social conversation, but for others a small personal space is expected when conversing with another.[104] There are times when a nurse must enter a client’s intimate or personal space, which can cause emotional distress for some clients. The nurse should always ask for permission before entering a client’s personal space and explain why close contact is necessary and what is about to happen.
Clients may also be concerned about their modesty or being exposed. A client may deal with the violation of their space by removing themselves from the situation, pulling away, or closing their eyes. The nurse should recognize these cues for what they are, an expression of cultural preference, and allow the client to assume a position or distance that is comfortable for them.
Similar to cultural influences on personal space, touch is also culturally determined. This has implications for nurses because depending on the culture, it may be inappropriate for a male nurse to provide care for a female client and vice versa. In some cultures, it is also considered rude to touch a person’s head without permission.
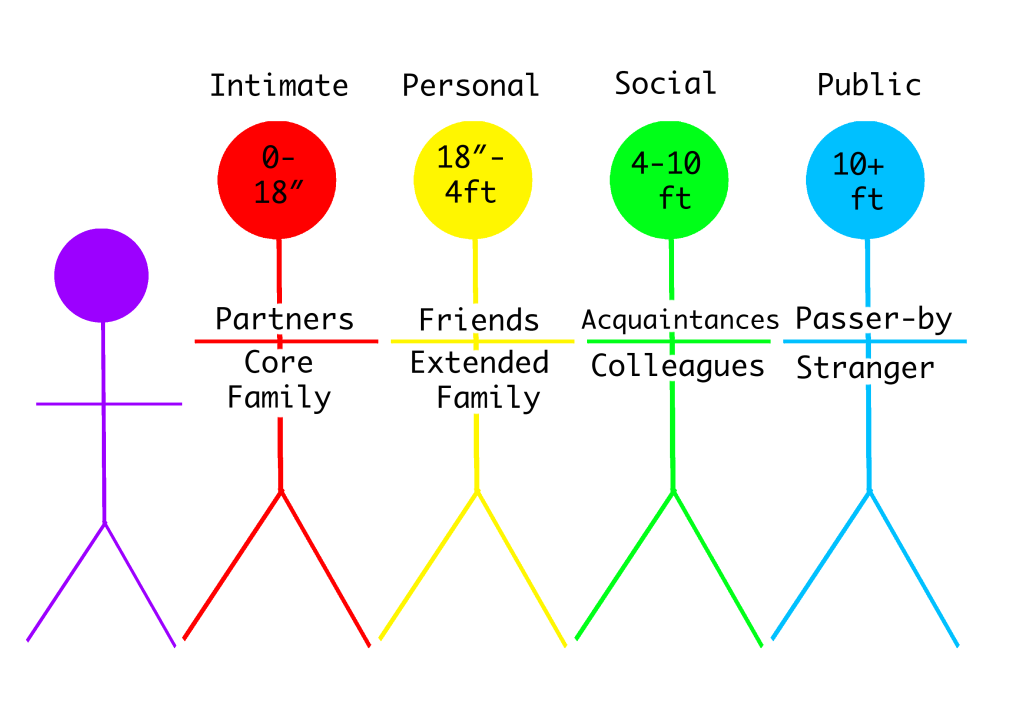
Review more information about space orientation in the "Communication" chapter.
Eye Contact
Eye contact is also a culturally mediated behavior. See Figure 3.8[105] for an image of eye contact. In the United States, direct eye contact is valued when communicating with others, but in some cultures, direct eye contact is interpreted as being rude or bold. Rather than making direct eye contact, a client may avert their eyes or look down at the floor to show deference and respect to the person who is speaking. The nurse should notice these cultural cues from the client and mirror the client’s behaviors when possible.
Food Choices
Culture plays a meaningful role in the dietary practices and food choices of many people. Food is used to celebrate life events and holidays. Most cultures have staple foods, such as bread, pasta, or rice and particular ways of preparing foods. See Figure 3.9[106] for an image of various food choices. Special foods are prepared to heal and to cure or to demonstrate kinship, caring, and love. For example, in the United States, chicken noodle soup is often prepared and provided to family members who are ill. In certain Asian cultures, individuals prefer "heating" or "cooling" foods depending on the illness, with the belief that each specific food will help bring balance back to their system.[107] Additionally, certain foods and beverages (such as meat and alcohol) are forbidden in some cultures. Nurses should accommodate or negotiate dietary requests of their clients, knowing that food holds such an important meaning to many people.

Read more information about cultural dietary preferences and restrictions in the "Common Religions and Spiritual Practices" section of the "Spirituality" chapter.
Summary
In summary, there are several steps in the journey of becoming a culturally competent nurse with cultural humility who provides culturally responsive care to clients. As you continue in your journey of developing cultural competency, keep the summarized points in the following box in mind.
Summary of Developing Cultural Competency
- Cultural competence is an ongoing process for nurses and takes dedication, time, and practice to develop.
- Pursuing the goal of cultural competence in nursing and other health care disciplines is a key strategy in reducing health care disparities.
- Culturally competent nurses recognize that culture functions as a source of values and comfort for clients, their families, and communities.
- Culturally competent nurses intentionally provide client-centered care with sensitivity and respect for culturally diverse populations.
- Misunderstandings, prejudices, and biases on the part of the health care provider interfere with the client’s health outcomes.
- Culturally competent nurses negotiate care with clients so the care is congruent with their cultural beliefs and values.
- Nurses should examine their own biases, ethnocentric views, and prejudices so as not to interfere with the client’s care.
- Nurses who respect and understand the cultural values and beliefs of their clients are more likely to develop positive, trusting relationships with their clients.
The freedom to express one’s cultural beliefs is a fundamental right of all people. Nurses realize that people speak, behave, and act in many different ways due to the influential role that culture plays in their lives and their view of the world. Cultural competence is a lifelong process of applying evidence-based nursing in agreement with the cultural values, beliefs, worldview, and practices of clients to produce improved client outcomes.[108],[109],[110]
Culturally competent care requires nurses to combine their knowledge and skills with awareness, curiosity, and sensitivity about their clients’ cultural beliefs. It takes motivation, time, and practice to develop cultural competence, and it will evolve throughout your nursing career. Culturally competent nurses have the power to improve the quality of care leading to better health outcomes for culturally diverse vs. Nurses who accept and uphold the cultural values and beliefs of their clients are more likely to develop supportive and trusting relationships with their clients. In turn, this opens the way for optimal disease and injury prevention and leads towards positive health outcomes for all clients.
The roots of providing culturally competent care are based on the original transcultural nursing theory developed by Dr. Madeleine Leininger. Transcultural nursing incorporates cultural beliefs and practices of individuals to help them maintain and regain health or to face death in a meaningful way.[111] See Figure 3.4[112] for an image of Dr. Madeleine Leininger. Read more about transcultural nursing theory in the following box.

Madeleine Leininger and the Transcultural Nursing Theory[113]
Dr. Madeleine Leininger (1925-2012) founded the transcultural nursing theory. She was the first professional nurse to obtain a PhD in anthropology. She combined the "culture" concept from anthropology with the "care" concept from nursing and reformulated these concepts into "culture care."
In the mid-1950s, no cultural knowledge base existed to guide nursing decisions or understand cultural behaviors as a way of providing therapeutic care. Leininger wrote the first books in the field and coined the term "culturally congruent practice." Culturally congruent practice describes nursing care that is in agreement with the preferred values, beliefs, worldview, and practices of the health care consumer.[114] She developed and taught the first transcultural nursing course in 1966, and master's and doctoral programs in transcultural nursing were launched shortly after. Dr. Leininger was honored as a Living Legend of the American Academy of Nursing in 1998.
Nurses have an ethical and moral obligation to provide culturally competent care to the clients they serve.[115] The "Respectful and Equitable Practice" Standard of Professional Performance set by the American Nurses Association (ANA) states that nurses must practice with cultural humility and inclusiveness. The ANA Code of Ethics also states that the nurse should collaborate with other health professionals, as well as the public, to protect human rights, fight discriminatory practices, and reduce disparities.[116] Additionally, the ANA Code of Ethics also states that nurses “are expected to be aware of their own cultural identifications in order to control their personal biases that may interfere with the therapeutic relationship. Self-awareness involves not only examining one’s culture but also examining perceptions and assumptions about the client’s culture...nurses should possess knowledge and understanding how oppression, racism, discrimination, and stereotyping affect them personally and in their work."[117]
Developing cultural competence begins in nursing school.[118],[119] Culture is an integral part of life, but its impact is often implicit. It is easy to assume that others share the same cultural values that you do, but each individual has their own beliefs, values, and preferences. Begin the examination of your own cultural beliefs and feelings by answering the questions below.[120]
Reflect on the following questions carefully and contemplate your responses as you begin your journey of providing culturally responsive care as a nurse. (Questions are adapted from the Anti-Defamation League's “Imagine a World Without Hate” Personal Self-Assessment Anti-Bias Behavior).[121]
- Who are you? With what cultural group or subgroups do you identify?
- When you meet someone from another culture/country/place, do you try to learn more about them?
- Do you notice instances of bias, prejudice, discrimination, and stereotyping against people of other groups or cultures in your environment (home, school, work, TV programs or movies, restaurants, places where you shop)?
- Have you reflected on your own upbringing and childhood to better understand your own implicit biases and the ways you have internalized messages you received?
- Do you ever consider your use of language to avoid terms or phrases that may be degrading or hurtful to other groups?
- When other people use biased language and behavior, do you feel comfortable speaking up and asking them to refrain?
- How ready are you to give equal attention, care, and support to people regardless of their culture, socioeconomic class, religion, gender expression, sexual orientation, or other “difference”?
The Process of Developing Cultural Competence
Dr. Josephine Campinha-Bacote is an influential nursing theorist and researcher who developed a model of cultural competence. The model asserts there are specific characteristics that a nurse becoming culturally competent possesses, including cultural awareness, cultural knowledge, cultural skill, and cultural encounters.[122]
Cultural awareness is a deliberate, cognitive process in which health care providers become appreciative and sensitive to the values, beliefs, attitudes, practices, and problem-solving strategies of a client’s culture. To become culturally aware, the nurse must undergo reflective exploration of personal cultural values while also becoming conscious of the cultural practices of others. In addition to reflecting on one’s own cultural values, the culturally competent nurse seeks to reverse harmful prejudices, ethnocentric views, and attitudes they have. Cultural awareness goes beyond a simple awareness of the existence of other cultures and involves an interest, curiosity, and appreciation of other cultures. Although cultural diversity training is typically a requirement for health care professionals, cultural desire refers to the intrinsic motivation and commitment on the part of a nurse to develop cultural awareness and cultural competency.
Acquiring cultural knowledge is another important step towards becoming a culturally competent nurse. Cultural knowledge refers to seeking information about cultural health beliefs and values to understand clients’ world views. To acquire cultural knowledge, the nurse actively seeks information about other cultures, including common practices, beliefs, values, and customs, particularly for those cultures that are prevalent within the communities they serve.[123] Cultural knowledge also includes understanding the historical backgrounds of culturally diverse groups in society, as well as physiological variations and the incidence of certain health conditions in culturally diverse groups. Cultural knowledge is best obtained through cultural encounters with clients from diverse backgrounds to learn about individual variations that occur within cultural groups and to prevent stereotyping.
While obtaining cultural knowledge, it is important to demonstrate cultural sensitivity. Cultural sensitivity means being tolerant and accepting of cultural practices and beliefs of people. Cultural sensitivity is demonstrated when the nurse conveys nonjudgmental interest and respect through words and action and an understanding that some health care treatments may conflict with a person’s cultural beliefs.[124] Cultural sensitivity also implies a consciousness of the damaging effects of stereotyping, prejudice, or biases on clients and their well-being. Nurses who fail to act with cultural sensitivity may be viewed as uncaring or inconsiderate, causing a breakdown in trust for the client and their family members. When a client experiences nursing care that contradicts with their cultural beliefs, they may experience moral or ethical conflict, nonadherence, or emotional distress.
Cultural desire, awareness, sensitivity, and knowledge are the building blocks for developing cultural skill. Cultural skill is reflected by the nurse’s ability to gather and synthesize relevant cultural information about their clients while planning care and using culturally sensitive communication skills. Nurses with cultural skill provide care consistent with their clients’ cultural needs and deliberately take steps to secure a safe health care environment that is free of discrimination or intolerance. For example, a culturally skilled nurse will make space and seating available within a client’s hospital room for accompanying family members when this support is valued by the client.[125]
A cultural encounter is a process where the nurse directly engages in face-to-face cultural interactions and other types of encounters with clients from culturally diverse backgrounds in order to modify existing beliefs about a cultural group and to prevent possible stereotyping.
By developing the characteristics of cultural awareness, cultural knowledge, cultural skill, and cultural encounters, a nurse develops cultural competence.
Diagnosis is the second step of the nursing process (and the second Standard of Practice by the American Nurses Association). This standard is defined as, "The registered nurse analyzes assessment data to determine actual or potential diagnoses, problems, and issues." The RN “prioritizes diagnoses, problems, and issues based on mutually established goals to meet the needs of the health care consumer across the health–illness continuum and the care continuum.” Diagnoses, problems, strengths, and issues are documented in a manner that facilitates the development of expected outcomes and a collaborative plan.[126] See Figure 4.7a for an illustration of how the Diagnosis phase of the nursing process corresponds to the NCSBN Clinical Judgment Measurement Model (NCJMM).[127]
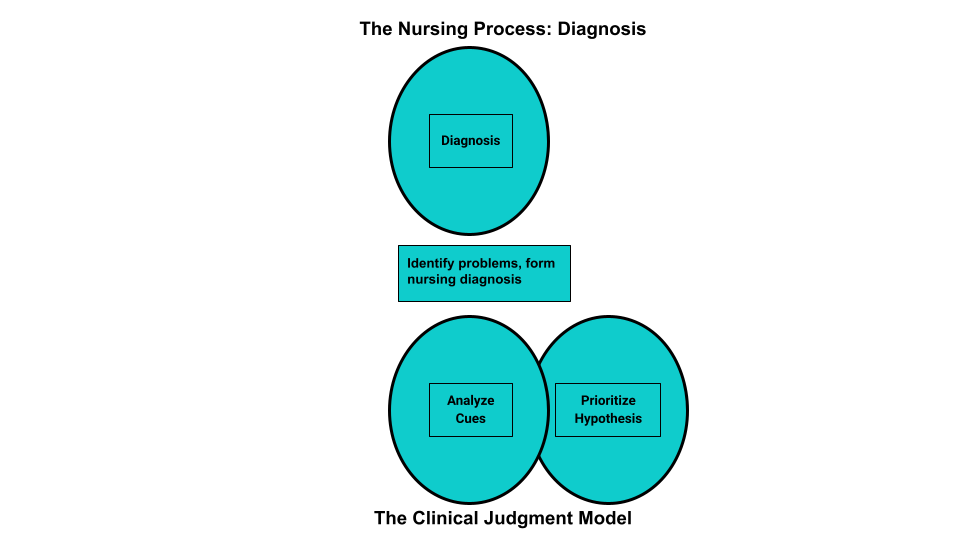
Analyzing Assessment Data
After collection of assessment data, the RN analyzes the data to form generalizations and create and prioritize hypotheses for nursing diagnoses. Steps for analyzing assessment data include performing data analysis, clustering information, identifying hypotheses for potential nursing diagnosis, performing additional in-depth assessment as needed, and establishing nursing diagnosis statements. The nursing diagnoses are then prioritized and the nursing care plan is developed based on them.[128] Analyzing assessment data is completed by an RN and falls outside of the scope of practice of the LPN/VN. However, LPN/VNs must understand data analysis so that new, concerning data is promptly reported to the RN for follow-up.
Performing Data Analysis
After nurses collect assessment data from a client, they use their nursing knowledge to analyze that data to determine if it is “expected” or “unexpected” or “normal” or “abnormal” for that client according to their age, development, and baseline status. From there, nurses determine what data is “clinically relevant” as they prioritize their nursing care.[129]
Example of Analyzing Cues
In Scenario C in the "Assessment" section of this chapter, the nurse analyzes the vital signs data and determines the blood pressure, heart rate, and respiratory rate are elevated, and the oxygen saturation is decreased for this client. These findings are considered “relevant cues" because they are abnormal compared to this client's baseline and may indicate a new health problem or complication is occurring.
Clustering Information/Seeing Patterns/Making Hypotheses
After analyzing the data and determining relevant cues, the nurse begins clustering data into similar domains or patterns. Evidence-based assessment frameworks, such as Gordon’s Functional Health Patterns, assist nurses in clustering data based on patterns of human responses. See the box below for an outline of Gordon’s Functional Health Patterns.[130] Concepts related to many of these patterns will be discussed in chapters later in this book.
Gordon’s Functional Health Patterns[131]
Health Perception-Health Management: A client’s perception of their health and well-being and how it is managed
Nutritional-Metabolic: Food and fluid consumption relative to metabolic need
Elimination: Excretory function, including bowel, bladder, and skin
Activity-Exercise: Exercise and daily activities
Sleep-Rest: Sleep, rest, and daily activities
Cognitive-Perceptual: Perception and cognition
Self-perception and Self-concept: Self-concept and perception of self-worth, self-competency, body image, and mood state
Role-Relationship: Role engagements and relationships
Sexuality-Reproductive: Reproduction and satisfaction or dissatisfaction with sexuality
Coping-Stress Tolerance: Coping and effectiveness in terms of stress tolerance
Value-Belief: Values, beliefs (including spiritual beliefs), and goals that guide choices and decisions
Example of Using Gordon's Health Patterns to Cluster Data
Refer to Scenario C in the "Assessment" section of this chapter. The nurse clusters the following relevant cues: elevated blood pressure, elevated respiratory rate, crackles in the lungs, weight gain, worsening edema, shortness of breath, medical history of heart failure, and currently prescribed a diuretic medication into a pattern of fluid balance, which can be classified under Gordon’s Nutritional-Metabolic Functional Health Pattern. Based on the related data in this cluster, the nurse makes a hypothesis that the client has excess fluid volume present.
Identifying Nursing Diagnoses
After the nurse has analyzed and clustered the data from the client assessment, the next step is to begin to answer the question, “What are my client’s human responses to their health condition(s) (i.e., their nursing diagnoses)?” A nursing diagnosis is defined as, "A clinical judgment concerning a human response to health conditions/life processes, or a vulnerability for that response, by an individual, family, group, or community."[132] Nursing diagnoses are customized to each client and drive the development of the nursing care plan. The nurse should refer to a care planning resource and review the definitions and defining characteristics of the hypothesized nursing diagnoses to determine if additional in-depth assessment is needed before selecting the most accurate nursing diagnosis. Formulation of nursing diagnoses is completed by an RN and is outside the scope of practice of LPN/VNs.
Nursing diagnoses are developed by nurses, for use by nurses. For example, NANDA International (NANDA-I) is a global professional nursing organization that develops nursing terminology that names actual or potential human responses to health problems and life processes based on research findings.[133] Currently, there are over 220 NANDA-I nursing diagnoses developed by nurses around the world. This list is continuously updated, with new nursing diagnoses added and old nursing diagnoses retired that no longer have supporting evidence. A list of commonly used NANDA-I diagnoses is listed in Appendix A. For a full list of NANDA-I nursing diagnoses, refer to a current nursing care plan reference.
NANDA-I nursing diagnoses are grouped into 13 domains that assist the nurse in selecting diagnoses based on the patterns of clustered data. These domains are similar to Gordon’s Functional Health Patterns and include health promotion, nutrition, elimination and exchange, activity/rest, perception/cognition, self-perception, role relationship, sexuality, coping/stress tolerance, life principles, safety/protection, comfort, and growth/development.
NANDA Diagnoses and the NCLEX
Knowledge regarding specific NANDA-I nursing diagnoses is not assessed on the NCLEX. However, analyzing cues, clustering data, forming appropriate hypotheses, and prioritizing hypotheses are components of clinical judgment assessed on the NCLEX and used in nursing practice. Read more about the Next Generation NCLEX in the "Scope of Practice" chapter.
Nursing Diagnoses vs. Medical Diagnoses
You may be asking yourself, “How are nursing diagnoses different from medical diagnoses?” Medical diagnoses focus on diseases or other medical problems that have been identified by the physician, physician’s assistant, or advanced nurse practitioner. Nursing diagnoses focus on the human response to health conditions and life processes and are made independently by RNs. Clients with the same medical diagnosis will often respond differently to that diagnosis and thus have different nursing diagnoses. For example, two clients have the same medical diagnosis of heart failure. However, one client may be interested in learning more information about the condition and the medications used to treat it, whereas another client may be experiencing anxiety when thinking about the effects this medical diagnosis will have on their family. The nurse must consider these different responses when creating the nursing care plan. Nursing diagnoses consider the client’s and family’s needs, attitudes, strengths, challenges, and resources as a customized nursing care plan is created to provide holistic and individualized care for each client.
Example of a Medical Diagnosis
A medical diagnosis identified for Ms. J. in Scenario C in the "Assessment" section is heart failure. This cannot be used as a nursing diagnosis because it is outside the nurse's scope of practice to make a medical diagnosis, but it is considered as an “associated condition” when creating hypotheses for nursing diagnoses. Associated conditions are medical diagnoses, injuries, procedures, medical devices, or pharmacological agents that are not independently modifiable by the nurse, but support accuracy in nursing diagnosis. The nursing diagnosis in Scenario C will relate to the client’s responses to her medical diagnosis of heart failure, such as "Excess Fluid Volume."
Additional Definitions Used in NANDA-I Nursing Diagnoses
The following definitions are used in association with NANDA-I nursing diagnoses.
Patient
The NANDA-I definition of a “patient” includes the following:
- Individual: a single human being distinct from others (i.e., a person).
- Caregiver: a family member or helper who regularly looks after a child or a sick, elderly, or disabled person.
- Family: two or more people having continuous or sustained relationships, perceiving reciprocal obligations, sensing common meaning, and sharing certain obligations toward others; related by blood and/or choice.
- Group: a number of people with shared characteristics, such as an ethnic group.
- Community: a group of people living in the same locale under the same governance. Examples include neighborhoods and cities.[134]
Age
The age of the person who is the subject of the diagnosis is defined by the following terms[135]:
- Fetus: an unborn human more than eight weeks after conception, until birth.
- Neonate: a person less than 28 days of age.
- Infant: a person greater than 28 days and less than 1 year of age.
- Child: a person aged 1 to 9 years.
- Adolescent: a person aged 10 to 19 years.
- Adult: a person older than 19 years of age unless national law defines a person as being an adult at an earlier age.
- Older adult: a person greater than 65 years of age.
Time
The duration of the diagnosis is defined by the following terms[136]:
- Acute: lasting less than three months.
- Chronic: lasting greater than three months.
- Intermittent: stopping or starting again at intervals.
- Continuous: uninterrupted, going on without stop.
Two terms used to assist in creating nursing diagnoses are at-risk populations and associated conditions[137]:
- At-risk populations are groups of people who share a characteristic that causes each member to be susceptible to a particular human response, such as demographics, health/family history, stages of growth/development, or exposure to certain events/experiences.
- Associated conditions are medical diagnoses, injuries, procedures, medical devices, or pharmacological agents. These conditions are not independently modifiable by the nurse, but support accuracy in nursing diagnosis.[138]
Types of Nursing Diagnoses
There are four types of NANDA-I nursing diagnoses:[139]
- Problem-Focused
- Health Promotion - Wellness
- Risk
- Syndrome
A problem-focused nursing diagnosis is a “clinical judgment concerning an undesirable human response to health condition/life processes that exist in an individual, family, group, or community.”[140] To make an accurate problem-focused diagnosis, related factors and defining characteristics must be present. Related factors (also called etiology) are causes that contribute to the diagnosis. Defining characteristics are cues, signs, and symptoms that cluster into patterns.[141] Defining characteristics are the signs and symptoms that a nurse can observe, hear, feel, or smell and cluster into patterns underlying nursing diagnoses.
A health promotion-wellness nursing diagnosis is “a clinical judgment concerning motivation and desire to increase well-being and to actualize human health potential.” These responses are expressed by the client’s readiness to enhance specific health behaviors.[142] A health promotion-wellness diagnosis is used when the client is willing to improve a lack of knowledge, coping, or other identified need.
A risk nursing diagnosis is “a clinical judgment concerning the vulnerability of an individual, family, group, or community for developing an undesirable human response to health conditions/life processes.”[143] A risk nursing diagnosis must be supported by risk factors that contribute to the increased vulnerability. A risk nursing diagnosis is different from the problem-focused diagnosis in that the problem has not yet actually occurred. Problem diagnoses should not be automatically viewed as more important than risk diagnoses because sometimes a risk diagnosis can have the highest priority for a client.[144]
A syndrome nursing diagnosis is a “clinical judgment concerning a specific cluster of nursing diagnoses that occur together and are best addressed together and through similar interventions.”[145]
Establishing Nursing Diagnosis Statements
NANDA-I recommends creating statements for nursing diagnosis that include the nursing diagnosis and related factors as exhibited by defining characteristics. The accuracy of the nursing diagnosis is validated when a nurse is able to clearly link the defining characteristics, related factors, and/or risk factors found during the client’s assessment.[146]
To create a nursing diagnosis statement, the RN analyzes the client’s subjective and objective data and clusters the data into patterns. Based on these patterns, the RN generates hypotheses for nursing diagnoses based on how the patterns meet defining characteristics of a nursing diagnosis. Recall that "defining characteristics" are the signs and symptoms related to a nursing diagnosis.[147] Defining characteristics are included in care planning resources for each nursing diagnosis, along with a definition of that diagnosis, so the nurse can select the most accurate diagnosis.
Example
An RN clusters objective and subjective data such as weight, height, and dietary intake as a pattern related to nutritional status and then compares these signs and symptoms to the defining characteristics for the NANDA nursing diagnosis, "Imbalanced Nutrition: Less Than Body Requirement."
When creating a nursing diagnosis statement, the nurse also identifies the cause, or etiology, of the problem for that specific client. Recall that the term "related factors" refers to the underlying causes (etiology) of a client’s problem or situation. Related factors should not refer to medical diagnoses, but instead should be causes that the nurse can treat. When possible, the nursing interventions planned for nursing diagnoses should attempt to modify or remove these underlying causes of the nursing diagnosis.[148]
Creating nursing diagnosis statements is also called “using PES format.” The PES mnemonic no longer applies to the current terminology used by NANDA-I, but the components of a nursing diagnosis statement remain the same. A nursing diagnosis statement should contain the problem, related factors, and defining characteristics. These terms fit under the former PES format in this manner:
Problem (P): The problem (i.e., the nursing diagnosis)
Etiology (E): The related factors (i.e., the etiology/cause) of the nursing diagnosis; phrased as “related to” or “R/T”
Signs and Symptoms (S): The defining characteristics manifested by the client (i.e., the signs and symptoms/subjective and objective data/clinical cues) that led to the identification of that nursing diagnosis/hypothesis for the client; phrased with “as manifested by" (AMB) or "as evidenced by" (AEB).
Examples of different types of nursing diagnoses are further explained in the following sections.
Problem-Focused Nursing Diagnosis
A problem-focused nursing diagnosis contains all three components of the PES format:
Problem (P): Client problem (nursing diagnosis)
Etiology (E): Related factors causing the nursing diagnosis
Signs and Symptoms (S): Defining characteristics/cues manifested by that client (i.e., the signs and symptoms demonstrating there is a problem)
Example of a Problem-Focused Nursing Diagnosis
Refer to Scenario C of the "Assessment" section of this chapter. The cluster of data for Ms. J. (elevated blood pressure, elevated respiratory rate, crackles in the lungs, weight gain, worsening edema, and shortness of breath) are defining characteristics for the NANDA-I Nursing Diagnosis Excess Fluid Volume. The NANDA-I definition of Excess Fluid Volume is “surplus intake and/or retention of fluid.” The related factor (etiology) of the problem is that the client has excessive fluid intake.[149]
The components of a problem-focused nursing diagnosis statement for Ms. J. would be:
Problem (P): Excess Fluid Volume
Etiology (E): Related to excessive fluid intake
Signs and Symptoms (S): As manifested by bilateral basilar crackles in the lungs, bilateral 2+ pitting edema of the ankles and feet, increased weight of 1ten pounds, and the client reports, “My ankles are so swollen.”
A correctly written problem-focused nursing diagnosis statement for Ms. J. would be written as follows:
Excess Fluid Volume related to excessive fluid intake as manifested by bilateral basilar crackles in the lungs, bilateral 2+ pitting edema of the ankles and feet, an increase weight of 1ten pounds, and the client reports, “My ankles are so swollen.”
Health-Promotion Nursing Diagnosis
A health-promotion nursing diagnosis statement contains the problem (P) and the defining characteristics (S). The defining characteristics component of a health-promotion nursing diagnosis statement should begin with the phrase “expresses desire to enhance,” followed by what the client states in relation to improving their health status:[150]
A health-promotion diagnosis statement consists of the following:
Problem (P): Client problem (nursing diagnosis)
Signs and Symptoms (S): The client’s expressed desire to enhance
Example of a Health-Promotion Nursing Diagnosis
Refer to Scenario C in the "Assessment" section of this chapter. Ms. J. demonstrates a readiness to improve her health status when she told the nurse that she would like to “learn more about my health so I can take better care of myself.” This statement is a defining characteristic of the NANDA-I nursing diagnosis Readiness for Enhanced Health Management, which is defined as “a pattern of regulating and integrating into daily living a therapeutic regimen for the treatment of illness and its sequelae, which can be strengthened.”[151]
The components of a health-promotion nursing diagnosis for Ms. J. would be:
Problem (P): Readiness for Enhanced Health Management
Symptoms (S): Expressed desire to “learn more about my health so I can take better care of myself.”
A correctly written health-promotion nursing diagnosis statement for Ms. J. would be written as follows:
Enhanced Readiness for Health Promotion as manifested by expressed desire to “learn more about my health so I can take better care of myself.”
Risk Nursing Diagnosis
A risk nursing diagnosis should be supported by evidence of the client’s risk factors for developing that problem. Different experts recommend different phrasing. NANDA-I 2018-2020 recommends using the phrase “as evidenced by” to refer to the risk factors for developing that problem.[152]
A risk diagnosis consists of the following:
Problem (P): Client problem (nursing diagnosis)
As Evidenced By: Risk factors for developing the problem
Example of a Risk Nursing Diagnosis
Refer to Scenario C in the "Assessment" section of this chapter. Ms. J. has an increased risk of falling due to vulnerability from the dizziness and weakness she is experiencing. The NANDA-I definition of Risk for Falls is “increased susceptibility to falling, which may cause physical harm and compromise health.”[153]
The components of a risk nursing diagnosis statement for Ms. J. would be:
Problem (P): Risk for Falls
As Evidenced By: Dizziness and decreased lower extremity strength
A correctly written risk nursing diagnosis statement for Ms. J. would be written as follows:
Risk for Falls as evidenced by dizziness and decreased lower extremity strength.
Syndrome Nursing Diagnosis
A syndrome nursing diagnosis statement is a cluster of nursing diagnoses that occur together and are best addressed together and through similar interventions. To create a syndrome diagnosis, two or more nursing diagnoses must be used as defining characteristics (S) that create a syndrome. Related factors may be used if they add clarity to the definition but are not required.[154]
A syndrome statement consists of these items:
Problem (P): The syndrome
Signs and Symptoms (S): The defining characteristics are two or more similar nursing diagnoses
Example of a Syndrome Nursing Diagnosis
Refer to Scenario C in the "Assessment" section of this chapter. Clustering the data for Ms. J. identifies several similar NANDA-I nursing diagnoses that can be categorized as a syndrome. For example, Activity Intolerance is defined as “insufficient physiological or psychological energy to endure or complete required or desired daily activities.” Social Isolation is defined as “aloneness experienced by the individual and perceived as imposed by others and as a negative or threatening state.” These diagnoses can be included under the NANDA-I syndrome named Risk for Frail Elderly Syndrome. This syndrome is defined as a “dynamic state of unstable equilibrium that affects the older individual experiencing deterioration in one or more domains of health (physical, functional, psychological, or social) and leads to increased susceptibility to adverse health effects, in particular disability.”[155]
Example
The components of a syndrome nursing diagnosis for Ms. J. would be:
Problem (P): Risk for Frail Elderly Syndrome
Signs and Symptoms (S): The nursing diagnoses of Activity Intolerance and Social Isolation
Additional related factor: Fear of falling
A correctly written syndrome diagnosis statement for Ms. J. would be written as follows:
Risk for Frail Elderly Syndrome related to activity intolerance, social isolation, and fear of falling
See Table 4.4a for a summary of the types of nursing diagnoses.
Table 4.4a. Types of Nursing Diagnoses
| Diagnosis | What Is It? | Example of Nursing Diagnosis Statement |
| Problem-Focused (Actual) | Problem is present at the time of assessment | (PES) Fluid Volume Excess R/T excessive fluid intake AEB bilateral basilar crackles in the lungs, bilateral 2+ pitting edema in the ankles and feet, an increased weight of 10 pounds over 1 week, and the client reports, "My ankles feel swollen." |
| Health-Promotion | A motivation/desire to increase well-being or a client's strength | Enhanced Readiness for Health Promotion AEB expressed desire to "learn more about health so I can take better care of myself." |
| Risk | Problem is likely to develop | Risk for Falls AEB dizziness and decreased lower extremity strength |
| Syndrome | Cluster of nursing diagnoses that occur together and are best addressed together | Risk for Frail Elderly Syndrome R/T activity intolerance, social isolation, and fear of falling |
Clinical Tip: It can feel overwhelming for nursing students to determine which nursing diagnoses to use for their clients due to the complexity of nursing diagnoses. Rest assured, use of nursing diagnoses becomes easier with practice and exposure to client care plans. Refer to trustworthy sources, such as a nursing diagnosis handbook or reputable care-planning resources to become aware of current NANDA-I nursing diagnoses.
Nursing diagnoses can be viewed to establish familiarity with them on the nandadiagnoses.com website, but but be aware this is not an official NANDA nursing diagnosis site. Evidence-based care planning resources should be used when planning clientcare.
Prioritization
After identifying nursing diagnoses, the next step is prioritizing diagnoses and actions according to the specific needs of the client. Nurses prioritize their actions while providing client care multiple times every day. Prioritization is the skillful process of deciding which actions to complete first for client safety and optimal client outcomes. Through prioritization, the most significant nursing problems, as well as the most important interventions in the nursing care plan, are identified.
Client care situations fall somewhere between routine care and a medical crisis. It is essential that life-threatening concerns and crises are identified immediately and addressed quickly. Depending on the severity of a problem, the steps of the nursing process may be performed in a matter of seconds for life-threatening concerns, such as respiratory arrest or cardiac arrest. Critical situations can occur at any time when providing nursing care for clients, and the steps of the nursing process must be performed rapidly. Nursing students must have a full understanding of how to correctly analyze cues, cluster data, form appropriate hypotheses, and prioritize hypotheses to take appropriate action using clinical judgment. Nurses recognize cues signaling a change in client condition, apply evidence-based practices in a crisis, and communicate effectively with interprofessional team members.
There are several concepts used to prioritize, including Maslow’s Hierarchy of Needs, the “ABCs” (Airway, Breathing and Circulation), and acute, uncompensated conditions. See the infographic in Figure 4.7[156] on The How To of Prioritization.

Maslow’s Hierarchy of Needs is used to categorize the most urgent client needs. The bottom levels of the pyramid represent the top priority needs of physiological needs intertwined with safety. See Figure 4.8[157] for an image of Maslow’s Hierarchy of Needs. You may be asking yourself, “What about the ABCs - isn't airway the most important?” The answer to that question is "it depends on the situation and the associated safety considerations." Consider this scenario - you are driving home after a lovely picnic in the country and come across a fiery car crash. As you approach the car, you see that the passenger is not breathing. Using Maslow’s Hierarchy of Needs to prioritize your actions, you remove the passenger from the car first due to safety even though he is not breathing. After ensuring safety and calling for help, you follow the steps to perform cardiopulmonary resuscitation (CPR) to establish circulation, airway, and breathing until help arrives.
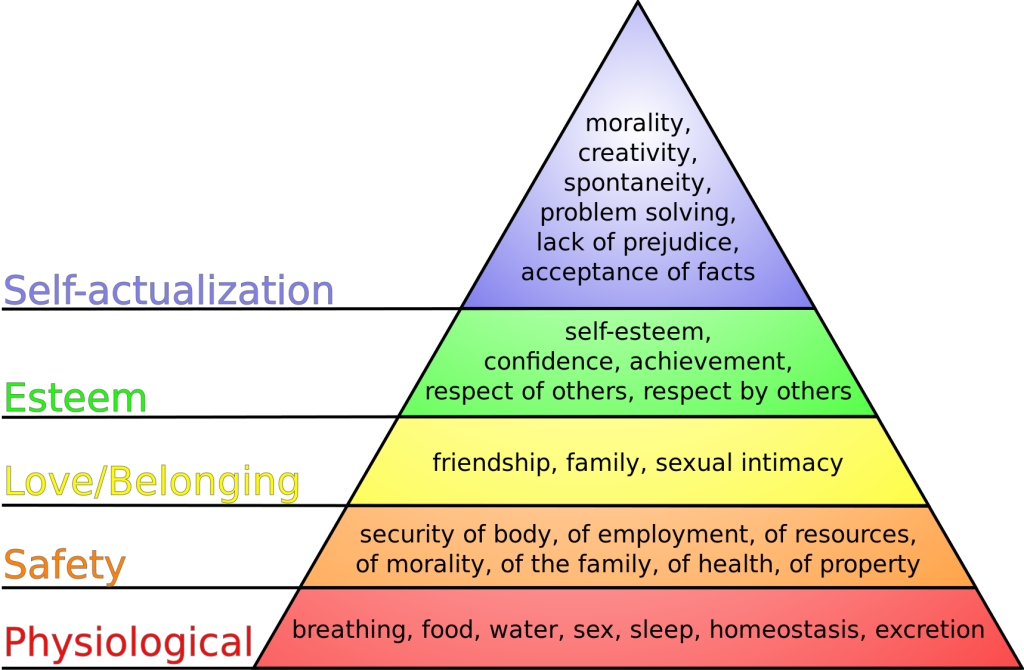
In addition to using Maslow’s Hierarchy of Needs and the ABCs of airway, breathing, and circulation, the nurse also considers if the client’s condition is an acute or chronic problem. Acute, uncompensated conditions require priority interventions over chronic conditions. Additionally, actual problems generally receive priority over potential problems, but risk problems sometimes receive priority depending on the client vulnerability and risk factors.
Example of Prioritization
Refer to Scenario C in the "Assessment" section of this chapter. Four types of nursing diagnoses were identified for Ms. J.: Excess Fluid Volume, Enhanced Readiness for Health Promotion, Risk for Falls, and Risk for Frail Elderly Syndrome. The top priority diagnosis is Excess Fluid Volume because this condition affects the physiological needs of breathing, homeostasis, and excretion. However, the Risk for Falls diagnosis comes in a close second because of safety implications and potential injury that could occur if the client fell.
Planning is the fourth step of the nursing process (and the fourth Standard of Practice by the American Nurses Association). This standard is defined as, "The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes." The RN develops an individualized, holistic, evidence-based plan in partnership with the health care consumer, family, significant others, and interprofessional team. Elements of the plan are prioritized for client safety and optimal client outcomes. The plan is modified according to the ongoing assessment of the health care consumer's response and other indicators. The plan is documented using standardized language or terminology.[158]
After expected outcomes are identified, the nurse begins planning nursing interventions to implement. Nursing interventions are evidence-based actions that the nurse performs to achieve client outcomes. Just as a provider makes medical diagnoses and writes prescriptions to improve the client's medical condition, a nurse formulates nursing diagnoses and plans nursing interventions to resolve client problems. Nursing interventions should focus on eliminating or reducing the related factors (etiology) of the nursing diagnoses when possible.[159] Nursing interventions, goals, and expected outcomes are written in the nursing care plan for continuity of care across shifts, nurses, and health professionals. Planning is outside the scope of practice for LPN/VNs, although they may assist in performing planned interventions during the Implementation phase according to their scope of practice. Refer to Figure 4.9a in the "Outcome Identification" section for a illustration of how the Planning phase of the nursing process correlates to NCSBN's Clinical Judgment Measurement Model.
Planning Nursing Interventions
You might be asking yourself, “How do I know what evidence-based nursing interventions to include in the nursing care plan?” There are several sources that nurses and nursing students can use to select nursing interventions. Many agencies have care planning tools and references included in the electronic health record that are easily documented in the client chart. Nurses can also refer to other care planning books or sources such as the Nursing Interventions Classification (NIC) system. Based on research and input from the nursing profession, NIC categorizes and describes nursing interventions that are regularly evaluated and updated. Interventions included in NIC are considered evidence-based nursing practices. The RN is responsible for using clinical judgment to make decisions about which interventions are best suited to meet an individualized client’s needs.[160]
Direct and Indirect Care
Nursing interventions are considered direct care or indirect care. Direct care refers to interventions that are carried out by having personal contact with clients. Examples of direct care interventions are wound care, repositioning, and ambulation. Indirect care interventions are performed when the nurse provides assistance in a setting other than with the client. Examples of indirect care interventions are attending care conferences, documenting, and communicating about client care with other providers.
Classification of Nursing Interventions
There are three types of nursing interventions: independent, dependent, and collaborative. (See Figure 4.12[161] for an image of a nurse collaborating with the health care team when planning interventions.)

Independent Nursing Interventions
Any intervention that the nurse can independently provide without obtaining a prescription or consulting another member of the health care team is considered an independent nursing intervention. An example of an independent nursing intervention is when the nurse monitors the client’s 24-hour intake/output record for trends because of a risk for imbalanced fluid volume. Another example of independent nursing interventions is the therapeutic communication that a nurse uses to assist clients to cope with a new medical diagnosis.
Example of an Independent Nursing Intervention
Refer to Scenario C in the "Assessment" section of this chapter. Ms. J. was diagnosed with Excess Fluid Volume. An example of an evidence-based independent nursing intervention is, “The nurse will reposition the client with dependent edema frequently, as appropriate.”[162] The nurse would individualize this evidence-based intervention to the client and include agency policy by stating, “The nurse will reposition the client every two hours.”
Dependent Nursing Interventions
Dependent nursing interventions require a prescription or order before they can be performed. Prescriptions are interventions specifically related to medication as directed by an authorized primary health care provider. An order is an intervention, remedy, or treatment as directed by an authorized primary health care provider.[163] A primary health care provider is a member of the health care team (usually a physician, advanced practice nurse, or physician’s assistant) who is licensed and authorized to formulate prescriptions on behalf of the client. For example, administering medication is a dependent nursing intervention. The nurse incorporates dependent interventions into the client's overall care plan by associating each intervention with the appropriate nursing diagnosis.
Example of a Dependent Nursing Intervention
Refer to Scenario C in the "Assessment" section of this chapter. Ms. J. was diagnosed with Excess Fluid Volume. An example of a dependent nursing intervention is, “The nurse will administer scheduled diuretics as prescribed.”
Collaborative Nursing Interventions
Collaborative nursing interventions are actions that the nurse carries out in collaboration with other health team members, such as physicians, social workers, respiratory therapists, physical therapists, and occupational therapists. These actions are developed in consultation with other health care professionals and incorporate their professional viewpoint.[164]
Example of a Collaborative Nursing Intervention
Refer to Scenario C in the "Assessment" section of this chapter. Ms. J. was diagnosed with Excess Fluid Volume. An example of a collaborative nursing intervention is the nurse consulting with a respiratory therapist when the client has deteriorating oxygen saturation levels. The respiratory therapist plans oxygen therapy and obtains a prescription from the provider. The nurse would document “The nurse will manage oxygen therapy in collaboration with the respiratory therapist" in the care plan.
Individualization of Interventions
It is vital for the planned interventions to be individualized to the client to be successful. For example, adding prune juice to the breakfast meal of a client with constipation will only work if the client likes to drink the prune juice. If the client does not like prune juice, then this intervention should not be included in the care plan. Collaboration with the client, family members, significant others, and the interprofessional team is essential for selecting effective interventions. There is not a set number of interventions required to be included in a nursing care plan, but instead, the number of quality individualized interventions is based on what is required to meet the specific, identified outcomes established for that client.
Creating Nursing Care Plans
Nursing care plans are created by registered nurses (RNs). Documentation of individualized nursing care plans are legally required in long-term care facilities by the Centers for Medicare and Medicaid Services (CMS) and in hospitals by The Joint Commission. CMS guidelines state, “Residents and their representative(s) must be afforded the opportunity to participate in their care planning process and to be included in decisions and changes in care, treatment, and/or interventions. This applies both to initial decisions about care and treatment, as well as the refusal of care or treatment. Facility staff must support and encourage participation in the care planning process. This may include ensuring that residents, families, or representatives understand the comprehensive care planning process, holding care planning meetings at the time of day when a resident is functioning at their best and client representatives can be present, providing sufficient notice in advance of the meeting, scheduling these meetings to accommodate a resident’s representative (such as conducting the meeting in-person, via a conference call, or video conferencing), and planning enough time for information exchange and decision-making. A resident has the right to select or refuse specific treatment options before the care plan is instituted.”[165] The Joint Commission conceptualizes the care planning process as the structuring framework for coordinating communication that will result in safe and effective care.[166]
Many facilities have established standardized nursing care plans with lists of possible interventions that can be customized for each specific client. Other facilities require the nurse to develop each care plan independently. Whatever the format, nursing care plans should be individualized to meet the specific and unique needs of each client. See Figure 4.13[167] for an image of a standardized care plan.

Nursing care plans created in nursing school can also be in various formats such as concept maps or tables. Some are fun and creative, while others are more formal. Appendix B contains a template that can be used for creating nursing care plans.
In addition to implementing safety strategies to improve safe client care, leaders of a health care agency must also establish a culture of safety. A culture of safety reflects the behaviors, beliefs, and values within and across all levels of an organization as they relate to safety and clinical excellence, with a focus on people. In 2021 The Joint Commission released a sentinel event regarding the essential role of leadership in establishing a culture of safety. According to The Joint Commission, leadership has an obligation to be accountable for protecting the safety of all health care consumers, including clients, employees, and visitors. Without adequate leadership and an effective culture of safety, there is higher risk for adverse events. Inadequate leadership can contribute to adverse effects in a variety of ways, including, but not limited to, the following[168]:
- Insufficient support of client safety event reporting
- Lack of feedback or response to staff and others who report safety vulnerabilities
- Allowing intimidation of staff who report events
- Refusing to consistently prioritize and implement safety recommendations
- Not addressing staff burnout
Three components of a culture of safety are the following[169]:
- Just Culture: People are encouraged, even rewarded, for providing essential safety-related information, but clear lines are drawn between human error and at-risk or reckless behaviors.
- Reporting Culture: People report errors and near-misses.
- Learning Culture: The willingness and the competence to draw the right conclusions from safety information systems, and the will to implement major reforms when their need is indicated.
The American Nurses Association further describes a culture of safety as one that includes openness and mutual respect when discussing safety concerns and solutions without shifting to individual blame, a learning environment with transparency and accountability, and reliable teams. In contrast, complexity, lack of clear measures, hierarchical authority, the “blame game,” and lack of leadership are examples of barriers that do not promote a culture of safety. If staff fear reprisal for mistakes and errors, they will be less likely to report errors, processes will not be improved, and client safety will continue to be impaired. See the following box for an example of safety themes established during a health care institution’s implementation of a culture of safety.
Safety Themes in a Culture of Safety[170]
Kaiser Permantente implemented a culture of safety in 2001 that focused on instituting the following six strategic themes:
- Safe culture: Creating and maintaining a strong safety culture, with client safety and error reduction embraced as shared organizational values.
- Safe care: Ensuring that the actual and potential hazards associated with high-risk procedures, processes, and client care populations are identified, assessed, and managed in a way that demonstrates continuous improvement and ultimately ensures that clients are free from accidental injury or illness.
- Safe staff: Ensuring that staff possess the knowledge and competence to perform required duties safely and contribute to improving system safety performance.
- Safe support systems: Identifying, implementing, and maintaining support systems—including knowledge-sharing networks and systems for responsible reporting—that provide the right information to the right people at the right time.
- Safe place: Designing, constructing, operating, and maintaining the environment of health care to enhance its efficiency and effectiveness.
- Safe clients: Engaging clients and their families in reducing medical errors, improving overall system safety performance, and maintaining trust and respect.
A strong safety culture encourages all members of the health care team to identify and reduce risks to client safety by reporting errors and near misses so that root cause analysis can be performed and identified risks are removed from the system. However, in a poorly defined and implemented culture of safety, staff often conceal errors due to fear or shame. Nurses have been traditionally trained to believe that clinical perfection is attainable, and that “good” nurses do not make errors. Errors are perceived as being caused by carelessness, inattention, indifference, or uninformed decisions. Although expecting high standards of performance is appropriate and desirable, it can become counterproductive if it creates an expectation of perfection that impacts the reporting of errors and near misses. If employees feel shame when they make an error, they may feel pressure to hide or cover up errors. Evidence indicates that approximately three of every four errors are detected by those committing them, as opposed to being detected by an environmental cue or another person. Therefore, employees need to be able to trust that they can fully report errors without fear of being wrongfully blamed. This provides the agency with the opportunity to learn how to further improve processes and prevent future errors from occurring. For many organizations, the largest barrier in establishing a culture of safety is the establishment of trust. A model called “Just Culture” has successfully been implemented in many agencies to decrease the “blame game,” promote trust, and improve the reporting of errors.
Just Culture
The American Nurses Association (ANA) officially endorses the Just Culture model. In 2019 the ANA published a position statement on Just Culture, stating, “Traditionally, healthcare’s culture has held individuals accountable for all errors or mishaps that befall clients under their care. By contrast, a Just Culture recognizes that individual practitioners should not be held accountable for system failings over which they have no control. A Just Culture also recognizes many individual or ‘active’ errors represent predictable interactions between human operators and the systems in which they work. However, in contrast to a culture that touts ‘no blame’ as its governing principle, a Just Culture does not tolerate conscious disregard of clear risks to clients or gross misconduct (e.g., falsifying a record or performing professional duties while intoxicated).”
The Just Culture model categorizes human behavior into three causes of errors. Consequences of errors are based on whether the error is a simple human error or caused by at-risk or reckless behavior.
- Simple human error: A simple human error occurs when an individual inadvertently does something other than what should have been done. Most medical errors are the result of human error due to poor processes, programs, education, environmental issues, or situations. These errors are managed by correcting the cause, looking at the process, and fixing the deviation. For example, a nurse appropriately checks the rights of medication administration three times, but due to the similar appearance and names of two different medications stored next to each other in the medication dispensing system, administers the incorrect medication to a client. In this example, a root cause analysis reveals a system issue that must be modified to prevent future errors (e.g., change the labelling and storage of look alike-sound alike medication).
- At-risk behavior: An error due to at-risk behavior occurs when a behavioral choice is made that increases risk where the risk is not recognized or is mistakenly believed to be justified. For example, a nurse scans a client’s medication with a barcode scanner prior to administration, but an error message appears on the scanner. The nurse mistakenly interprets the error to be a technology problem and proceeds to administer the medication instead of stopping the process and further investigating the error message, resulting in the wrong dosage of a medication being administered to the client. In this case, ignoring the error message on the scanner can be considered “at-risk behavior” because the behavioral choice was considered justified by the nurse at the time.
- Reckless behavior: Reckless behavior is an error that occurs when an action is taken with conscious disregard for a substantial and unjustifiable risk.[171] For example, a nurse arrives at work intoxicated and administers the wrong medication to the wrong client. This error is considered due to reckless behavior because the decision to arrive intoxicated was made with conscious disregard for substantial risk.
These examples show three different causes of medication errors that would result in different consequences to the employee based on the Just Culture model. Under the Just Culture model, after root cause analysis is completed, system-wide changes are made to decrease factors that contributed to the error. Managers appropriately hold individuals accountable for errors if they were due to simple human error, at-risk behavior, or reckless behaviors.
If an individual commits a simple human error, managers console the individual and consider changes in training, procedures, and processes. In the “simple human error” above, system-wide changes would be made to change the label and location of the medication to prevent future errors from occurring with the same medication.
Individuals committing at-risk behavior are held accountable for their behavioral choice and often require coaching with incentives for less risky behaviors and situational awareness. In the “at-risk behavior” example above where the nurse ignored an error message on the barcode scanner, mandatory training on using a barcode scanner and responding to errors would be implemented, and the manager would track the employee’s correct usage of the barcode scanner for several months following training.
If an individual demonstrates reckless behavior, remedial action and/or punitive action is taken.[172] In the “reckless behavior” example above, the manager would report the nurse’s behavior to the state's Board of Nursing with mandatory substance abuse counseling to maintain their nursing license. Employment may be terminated with consideration of patterns of behavior.
A Just Culture in which employees aren't afraid to report errors is a highly successful way to enhance client safety, increase staff and client satisfaction, and improve outcomes. Success is achieved through good communication, effective management of resources, and an openness to changing processes to ensure the safety of clients and employees. The infographic in Figure 5.4[173] illustrates the components of a culture of safety and Just Culture.
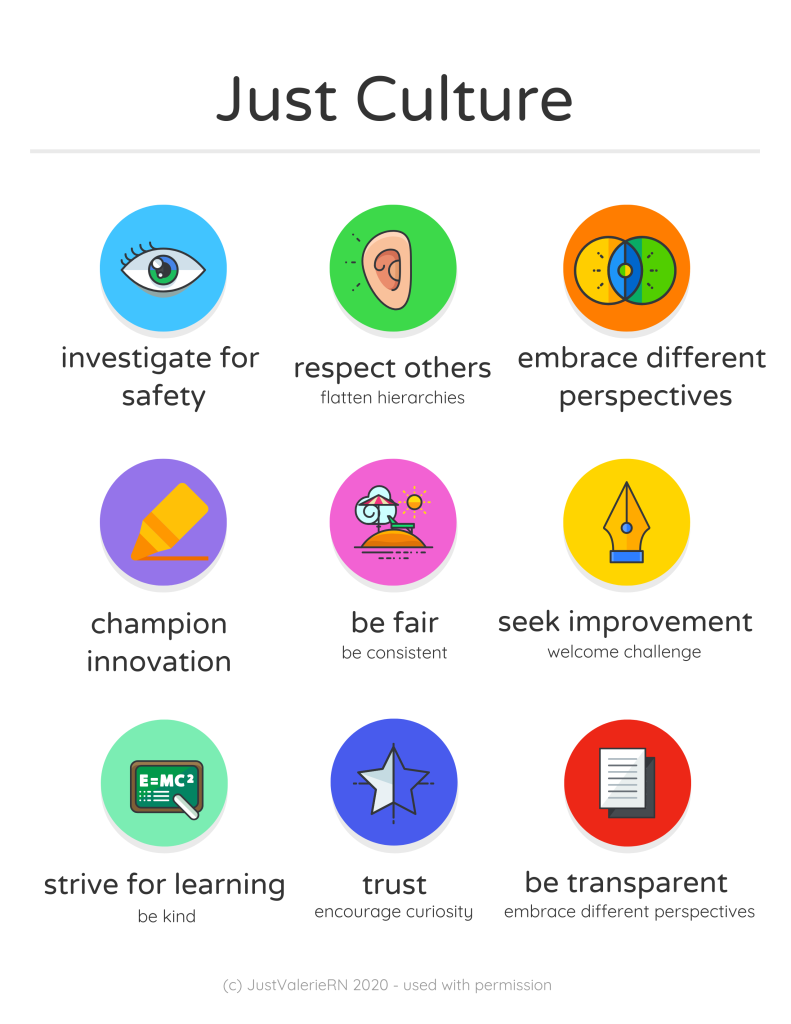
The principles of culture of safety, including Just Culture, Reporting Culture, and Learning Culture are also being adopted in nursing education. It’s understood that mistakes are part of learning and that a shared accountability model promotes individual- and system-level learning for improved client safety. Under a shared accountability model, students are responsible for the following[174]:
- Being fully prepared for clinical experiences, including laboratory and simulation assignments
- Being rested and mentally ready for a challenging learning environment
- Accepting accountability for their part in contributing to a safe learning environment
- Behaving professionally
- Reporting their own errors and near mistakes
- Keeping up-to-date with current evidence-based practice
- Adhering to ethical and legal standards
Students know they will be held accountable for their actions, but will not be blamed for system faults that lie beyond their control. They can trust that a fair process will be used to determine what went wrong if a client care error or near miss occurs. Student errors and near misses are addressed based on an investigation determining if it was simple human error, an at-risk behavior, or reckless behavior. For example, a simple human error by a student can be addressed with coaching and additional learning opportunities to remedy the knowledge deficit. However, if a student acts with recklessness (for example, repeatedly arrives to clinical unprepared despite previous faculty feedback or falsely documents an assessment or procedure), they are appropriately and fairly disciplined, which may include dismissal from the program.[175]
“Prevent residents from falling” is one of the National Patient Safety Goals for nursing care centers. Client falls, whether in the nursing care center, home, or hospital, are very common and can cause serious injury and death. Older adults have the highest risk of falling. Each year, 3 million older people are treated in emergency departments for fall injuries, and over 800,000 clients a year are hospitalized because of a head injury or hip fracture resulting from a fall. Many older adults who fall, even if they’re not injured, become afraid of falling. This fear may cause them to limit their everyday activities. However, when a person is less active, they become weaker, which further increases their chances of falling.[176]
Many conditions contribute to client falls, including the following:[177]
- Lower body weakness
- Vitamin D deficiency
- Difficulties with walking and balance
- Medications, such as tranquilizers, sedatives, antihypertensives, or antidepressants
- Vision problems
- Foot pain or poor footwear
- Environmental hazards, such as throw rugs or clutter that can cause tripping
Most falls are caused by a combination of risk factors. The more risk factors a person has, the greater their chances of falling. Many risk factors can be changed or modified to help prevent falls.
The Centers for Disease Control has developed a program called “STEADI - Stopping Elderly Accidents, Deaths & Injuries” to help reduce the risk of older adults from falling at home. Three screening questions to determine risk for falls are as follows:
- Do you feel unsteady when standing or walking?
- Do you have worries about falling?
- Have you fallen in the past year? If yes, how many times? Were you injured?
If the individual answers “Yes” to any of these questions, further assessment of risk factors is performed.[178]
Read more information about preventing falls in older adults at CDC's Older Adult Fall Prevention.
Fall Assessment Tools
By virtue of being ill, all hospitalized clients are at risk for falls, but some clients are at higher risk than others. Assessment is an ongoing process with the goal of identifying a client’s specific risk factors and implementing interventions in their care plan to decrease their risk of falling. Commonly used fall assessment tools used to identify clients at high risk for falls are the Morse Fall Scale, the Hendrich II Fall Risk Model, and the Hester Davis Scale for fall risk assessment. Read more about these fall risk assessment tools using the hyperlinks provided below. Key risk factors for falls in hospitalized clients are as follows:[179]
- History of falls: All clients with a recent history of falls, such as a fall in the past three months, should be considered at higher risk for future falls.
- Mobility problems and use of assistive devices: Clients who have problems with their gait or require an assistive device (such as a cane or a walker) for mobility are more likely to fall.
- Medications: Clients taking several prescription medications or those taking medications that could cause sedation, confusion, impaired balance, or orthostatic blood pressure changes are at higher risk for falls.
- Mental status: Clients with delirium, dementia, or psychosis may be agitated and confused, putting them at risk for falls.
- Incontinence: Clients who have urinary frequency or who have frequent toileting needs are at higher fall risk.
- Equipment: Clients who are tethered to equipment such as an IV pole or a Foley catheter are at higher risk of tripping.
- Impaired vision: Clients with impaired vision or those who require glasses but who are not wearing them are at a higher fall risk because of their decreased recognition of an environmental hazard.
- Orthostatic hypotension: Clients whose blood pressure drops upon standing often experience light-headedness or dizziness that can cause falls.[180]
View these common fall risk assessment tools:
Interventions to Prevent Falls
Universal fall precautions are established for all clients to reduce their risk for falling. In addition to universal fall precautions, a care plan is created based on the client's fall risk assessment findings to address their specific risks and needs.
Universal Fall Precautions
Falls are the most commonly reported client safety incidents in the acute care setting. Hospitals pose an inherent fall risk due to the unfamiliarity of the environment and various hazards in the hospital room that pose a risk. During inpatient care, nurses assess their clients’ risk for falling during every shift and implement interventions to reduce the risk of falling. Universal fall precautions have been developed that apply to all clients all the time. Universal fall precautions are called "universal" because they apply to all clients, regardless of fall risk, and revolve around keeping the client's environment safe and comfortable.[183]
Universal fall precautions include the following:
- Familiarize the client with the environment.
- Have the client demonstrate call light use.
- Maintain the call light within reach. See Figure 5.5[184] for an image of a call light.
- Keep the client's personal possessions within safe reach.
- Have sturdy handrails in client bathrooms, rooms, and hallways.
- Place the hospital bed in the low position when a client is resting. Raise the bed to a comfortable height when the client is transferring out of bed.
- Keep the hospital bed brakes locked.
- Keep wheelchair wheels in a "locked" position when stationary.
- Keep no-slip, comfortable, and well-fitting footwear on the client.
- Use night lights or supplemental lighting.
- Keep floor surfaces clean and dry. Clean up all spills promptly.
- Keep client care areas uncluttered.
- Follow safe client handling practices.[185]

Interventions Based on Risk Factors
Clients at elevated risk for falling require multiple, individualized interventions, in addition to universal fall precautions. There are many interventions available to prevent falls and fall-related injuries based on the client's specific risk factors. See Table 5.6a for interventions categorized by risk factor.[186]
Table 5.6a Interventions Based on Fall Risk Factors
| Risk Factor | Interventions |
|---|---|
| Altered Mental Status | Clients with new altered mental status should be assessed for delirium and treated by a trained nurse or physician. See a tool for assessing delirium below. For cognitively impaired clients who are agitated or trying to wander, more intense supervision (e.g., sitter or checks every 15 minutes) may be needed. Some hospitals implement designated safety zones that include low beds, mats for each side of the bed, nightlight, gait belt, and a "STOP" sign to remind clients not to get up. |
| Impaired Gait or Mobility | Clients with impaired gait or mobility will need assistance with mobility during their hospital stay. All clients should have any needed assistive devices, such as canes or walkers, in good repair at the bedside and within safe reach. If clients bring their assistive devices from home, staff should make sure these devices are safe for use in the hospital environment. Even with assistive devices, clients often need staff assistance when transferring out of bed or walking. Use a gait belt when assisting clients to transfer or ambulate per agency policy. |
| Frequent Toileting Needs | Clients with frequent toileting needs should be taken to the toilet on a regular basis via a scheduled rounding protocol. Read more about scheduled rounding in the following subsection. |
| Visual Impairment | Clients with visual impairment should have clean corrective lenses easily within reach and applied when walking. |
| High-Risk Medications (medicines that could cause sedation, confusion, impaired balance, orthostatic blood pressure changes, or cause frequent urination) | Clients on high-risk medications should have their medications reviewed by a pharmacist with fall risk in mind and recommendations made to the prescribing provider for discontinuation, substitution, or dose adjustment when possible. If a pharmacist is not immediately available, the prescribing provider should carry out a medication review. See Table 5.6b for a tool to review medications for fall risk. Clients on medications that cause orthostatic hypotension should have their orthostatic blood pressure routinely checked and reported. The client and their caregivers should be educated about fall risk and steps to prevent falls when the client is taking these medications. |
| Frequent Falls | Clients with a history of frequent falls should have their risk for injury assessed, including checking for a history of osteoporosis and use of aspirin and anticoagulants. |
Scheduled Hourly Rounding
Scheduled hourly rounds are scheduled hourly visits to each client’s room to integrate fall prevention activities with client care. Scheduled hourly rounds have been found to greatly decrease the incidence of falls because the client's needs are proactively met, reducing the motivation for the client to get out of bed unassisted. See the box below for a list of activities to complete during hourly rounds. These activities can be completed by unlicensed assistive personnel, nurses, or nurse managers.[187]
Hourly Rounding Protocol[188]
- Assess client pain levels using a pain-assessment scale. (If staff other than a nurse is doing the rounding and the client is in pain, contact the nurse immediately so the client does not have to use the call light for pain medication.)
- Put pain medication that is ordered “as needed” on an RN’s task list and offer the dose when it is due.
- Offer toileting assistance.
- Ensure the client is using correct footwear (e.g., specific shoes/slippers, no-skid socks).
- Check that the bed is in the locked position.
- Place the hospital bed in a low position when the client is resting; ask if the client needs to be repositioned and is comfortable.
- Make sure the call light/call bell button is within the client’s reach and the client can demonstrate accurate use.
- Put the telephone within the client’s reach.
- Put the TV remote control and bed light switch within the client’s reach.
- Put the bedside table next to the bed or across the bed.
- Put the tissue box and water within the client’s reach.
- Put the garbage can next to the bed.
- Prior to leaving the room, ask, “Is there anything I can do for you before I leave?"
- Tell the client that a member of the nursing staff (use names on whiteboard) will be back in the room in an hour to round again.
Medications Causing Elevated Risk for Falls
Evaluate medication-related fall risk for clients on admission and at regular intervals thereafter. Add up the point value (risk level) in Table 5.6b for every medication the client is taking. If the client is taking more than one medication in a particular risk category, the score should be calculated by (risk level score) x (number of medications in that risk level category). For a client at risk, a pharmacist should review the client’s list of medications and determine if medications may be tapered, discontinued, or changed to a safer alternative.[189]
Table 5.6b Medications Causing High Risk for Falls[190]
| Point Value (Risk Level) | Medication Class | Fall Risks |
|---|---|---|
| 3 (High) | Antipsychotics, anticonvulsants, and benzodiazepines | Sedation, dizziness, postural disturbances, altered gait and balance, and impaired cognition |
| 2 (Medium) | Antihypertensives, cardiac drugs, antiarrhythmics, and antidepressants | Induced orthostasis, impaired cerebral perfusion, and poor health status |
| 1 (Low) | Diuretics | Increased ambulation and induced orthostasis |
| Score ≥ 6 | Elevated risk for falls; ask pharmacist or prescribing provider to evaluate medications for possible modification to reduce risk |
View tools used to assess delirium and confusion in the Delirium Evaluation Bundle shared by the Agency for Healthcare Research and Quality.

