16.2 Basic Concepts
Open Resources for Nursing (Open RN)
Let’s begin by reviewing the basic anatomy and physiology of the urinary and gastrointestinal systems.
Urinary System
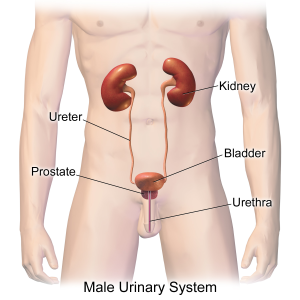
The urinary system, also referred to as the renal system or urinary tract, consists of the kidneys, ureters, bladder, and urethra. The purpose of the urinary system is to eliminate waste from the body, regulate blood volume and blood pressure, control levels of electrolytes and metabolites, and regulate blood pH. The kidneys filter blood in the nephrons and remove waste in the form of urine. Urine exits the kidney via the ureters and enters the urinary bladder, where it is stored until it is expelled by urination (also referred to as voiding).[1] See Figure 16.1[2] for an image of the male urinary system. The female urinary system is similar except for a smaller urethra.
A healthy adult with normal kidney function produces 800-2,000 mL of urine per day, depending on fluid intake, as well as the amount of fluid lost through sweating and breathing. The bladder typically holds about 360-480 mL of urine. As the bladder fills, it sends signals to the brain that it is time to urinate. The urinary tract includes two sets of muscles that work together as a sphincter, closing off the urethra to keep urine in the bladder until the brain sends signals to urinate. Urination occurs when the brain sends signals to the wall of the bladder to contract and squeeze urine out of the bladder and through the urethra. Frequency of urination depends on how quickly the kidneys produce urine and how much urine a person’s bladder can comfortably hold.[3]
Normal urine should be clear, pale to light yellow in color, and not foul-smelling. However, some foods or medications may change the smell or color of urine. For instance, phenazopyridine (Pyridium), a common medication prescribed to treat the pain, frequency, and burning associated with urinary tract infections, can cause urine to appear orange.[4]
Nurses frequently monitor and document a client’s urine output as part of the overall plan of care. It can be collected by placing a collection hat in the client’s toilet and then measured in a graduated cylinder. If the client has an indwelling catheter, the urine is emptied every shift from the catheter bag and measured in a graduated cylinder. For infants and toddlers, the number of daily wet diapers provides a general measure of urine output. For more specific measurement of urine output during hospitalization, wet diapers are weighed.
Terms commonly used to document conditions related to the urinary tract are as follows:
- Anuria: Absence of urine output, typically found during kidney failure, defined as less than 50 mL of urine over a 24-hour period.
- Dysuria: Painful or difficult urination.
- Frequency: The need to urinate several times during the day or at night (nocturia) in normal or less-than-normal volumes. It may be accompanied by a feeling of urgency.[5]
- Hematuria: Blood in the urine, either visualized or found during microscopic analysis.
- Oliguria: Decreased urine output, defined as less than 500 mL of urine in adults in a 24-hour period. In hospitalized clients, oliguria is further defined as less than 0.5 mL of urine per kilogram per hour for adults and children or less than 1 mL of urine per kilogram per hour for infants.[6] New oliguria should be reported to the health care provider because it can indicate dehydration, fluid retention, or decreasing kidney function.
- Nocturia: The need to get up at night on a regular basis to urinate. Nocturia often causes sleep deprivation that affects a person’s quality of life.[7]
- Polyuria: Greater than 2.5 liters of urine output over 24 hours, also referred to as diuresis. Urine is typically clear with no color.[8] New polyuria should be reported to the health care provider because it can be a sign of many medical conditions.
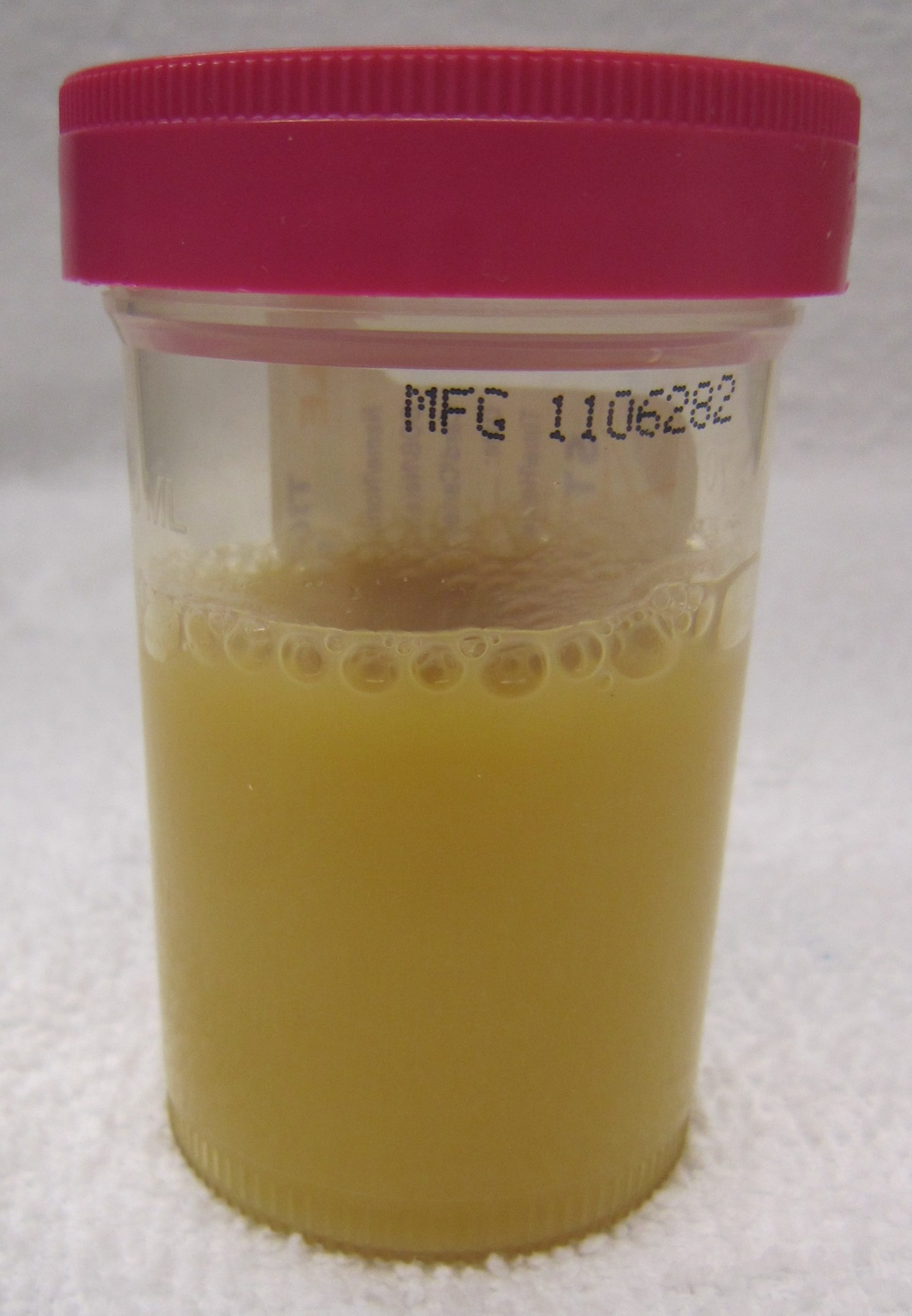
- Pyuria: At least ten white blood cells in each cubic millimeter of urine in a urine sample, typically indicating infection. In severe infections, pus may be visible in the urine.[9] See Figure 16.2[10] for an image of pyuria for a client with urosepsis.
- Urgency: A sensation of an urgent need to void.[11] Urgency can cause urge incontinence if the client is not able to reach the bathroom quickly.
View an activity reviewing the Vascular System of the Kidneys.
Gastrointestinal System
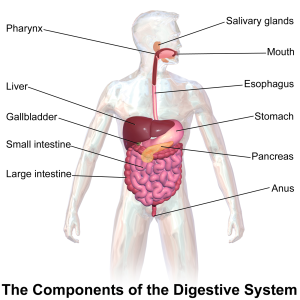
The gastrointestinal (GI) system includes the mouth, esophagus, stomach, small intestine, large intestine, and anus. See Figure 16.3[12] for an image of the gastrointestinal system. Ingested food and liquid are pushed through the GI tract by peristalsis, the involuntary contraction and relaxation of muscle creating wave-like movements of the intestines. The stomach mixes food and liquid with digestive enzymes and then empties into the small intestine. The muscles of the small intestine mix food with enzymes and bile from the pancreas, liver, and intestine and push the mixture forward for further digestion. Bacteria in the GI tract, called normal flora or microbiome, also assist with digestion. The walls of the small intestine absorb water and the digested nutrients into the bloodstream. As peristalsis continues, the waste products of the digestive process move into the large intestine. The large intestine absorbs water and changes the waste from liquid into stool. The rectum, at the lower end of the large intestine, stores stool until it is pushed out of the anus during a bowel movement.[13]
This section will focus on common alterations in bowel elimination, including constipation, diarrhea, and bowel incontinence. These alterations are common symptoms of several diseases and conditions of the gastrointestinal system. Nurses provide care to help manage these alterations.
Terms related to alterations in bowel elimination include the following:
- Black stools: Black-colored stools can be side effects of iron supplements or bismuth subsalicylate (Pepto-Bismol).
- Rectal bleeding: Rectal bleeding refers to bright red blood in the stools, also referred to as hematochezia. It is a sign of bleeding from the lower GI tract. Rectal bleeding can range in severity from minimal drops of blood on the toilet tissue caused by hemorrhoids to severe bleeding in large amounts that are life-threatening and require emergency care.[14] New bleeding should always be reported to the health care provider.
- Tarry stools: Stools that are black, sticky, and appear like tar are referred to as melena. Melena is typically caused by bleeding in the upper part of the gastrointestinal tract, such as the esophagus, stomach, or the first part of the small intestine, or due to the client swallowing blood. The blood appears darker and tarry-looking because it undergoes digestion on its way through the GI tract.[15] Bleeding from the upper part of the GI tract can also range from mild to life-threatening, depending upon the cause, and should always be reported to the health care provider.
Review information about digestion in the “Nutrition” chapter or read more information about the “Gastrointestinal” system in Open RN Nursing Pharmacology, 2e.
Newborns and Infants
Meconium refers to the first bowel movement of a newborn that appears sticky and black to dark green in color. See Figure 16.4[16] for an image of meconium. The stool of a breastfed baby usually appears like a curdled yellow, while that of a formula-fed baby is pastier. Breastfed babies often have bowel movements after every feeding. Formula-fed babies tend to have fewer bowel movements.

Toddlers
Toddlers usually begin the process of toilet training between two and three years old. Enuresis is the term used to describe incontinence when sleeping (i.e., bed-wetting). Enuresis in children is considered normal unless it continues past seven or eight years of age, when it should be addressed with a pediatrician. Toddlers often have undigested food in their bowel movements due to the intestinal system not fully digesting some foods, such as corn or grapes.
Children
School-aged children may be at risk for developing constipation due to delaying bowel movements during school times until they are in the privacy of their homes. The longer the stool sits in the colon, the more water is absorbed by the intestines, and the harder stool becomes to pass.
Adults
Adult females often develop urinary incontinence related to pregnancy and delivery, menopause, or vaginal hysterectomy. Adult males may have urgency and urinary retention with possible overflow urinary incontinence as their prostate enlarges. Adults over the age of 30 may develop nocturia.
Older Adults
Peristalsis typically slows as aging occurs. Older adults should be encouraged to increase fluids, fiber, and activity, as appropriate, to prevent constipation. If a client is not able to meet the goal of a bowel movement with soft, formed stools every three days, then a bowel management program should be initiated.
Now that we have reviewed the basic structure and function of the urinary and gastrointestinal systems, let’s review the common alterations of urinary tract infection, urinary incontinence, urinary retention, constipation, diarrhea, and bowel incontinence in the following sections.
- National Institute of Diabetes and Digestive and Kidney Diseases. (2020, June). The urinary tract & how it works. U.S. Department of Health and Human Services. https://www.niddk.nih.gov/health-information/urologic-diseases/urinary-tract-how-it-works ↵
- “Urinary_System_(Male).png” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2020, June). The urinary tract & how it works. U.S. Department of Health and Human Services. https://www.niddk.nih.gov/health-information/urologic-diseases/urinary-tract-how-it-works ↵
- National Institutes of Health. (2019, August 28). Pyridium. DailyMed. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=165d01d4-a9f7-2293-e054-00144ff8d46c ↵
- Maddukuri, G. (2021, January). Urinary frequency. Merck Manual Professional Version. https://www.merckmanuals.com/professional/genitourinary-disorders/symptoms-of-genitourinary-disorders/urinary-frequency ↵
- Berry, C. (2020, November). Oliguria. Merck Manual Professional Version. https://www.merckmanuals.com/professional/critical-care-medicine/approach-to-the-critically-ill-patient/oliguria ↵
- This work is a derivative of StatPearls by Leslie, Sajjad, & Singh and is licensed under CC BY 4.0 ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2021. Urination - excessive amount; [updated 2021, Feb 8; cited 2021, Feb 16]. https://medlineplus.gov/ency/article/003146.htm ↵
- Cherney, K. (2018, August 30). Everything you should know about pyuria. Healthline. https://www.healthline.com/health/pyuria ↵
- “Pyuria2011.JPG” by James Heilman, MD is licensed under CC BY-SA 3.0 ↵
- Maddukuri, G. (2021, January). Urinary frequency. Merck Manual Professional Version. https://www.merckmanuals.com/professional/genitourinary-disorders/symptoms-of-genitourinary-disorders/urinary-frequency ↵
- “Blausen_0316_DigestiveSystem.png” by Blausen.com staff is licensed under CC BY 3.0 ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2017, December). Your digestive system & how it works. U.S. Department of Health and Human Services. https://www.niddk.nih.gov/health-information/digestive-diseases/digestive-system-how-it-works ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2021. Rectal bleeding; [updated 2021, Feb 8; cited 2021, Feb 16]. https://medlineplus.gov/ency/article/007741.htm ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2021. Black or tarry stools; [updated 2021, Feb 8; cited 2021, Feb 16]. https://medlineplus.gov/ency/article/003130.htm#:~:text=Black%20or%20tarry%20stools%20with,used%20to%20describe%20this%20finding ↵
- Meconium_Diaper.jpg” by Azoreg is licensed under CC BY-SA 3.0 ↵
8.2 Case Study Maria's Journey Through the Health Care System
1. Maria's financial stress can lead to poor medication adherence, unhealthy dietary choices, and infrequent medical visits. This results in poorly controlled diabetes and increased risk of complications. Additionally, the constant stress of managing her finances can raise cortisol levels, negatively impacting her blood sugar control.
2. Programs such as sliding scale fees at clinics, subsidies for medications, food assistance programs like SNAP, and community-based health initiatives could help reduce the financial burden on individuals like Maria. Expanding Medicaid and implementing prescription drug assistance programs are also effective measures.
3. Improved health literacy can empower Maria to understand her condition better, follow her treatment plan accurately, make healthier lifestyle choices, and seek timely medical help. This knowledge can lead to better diabetes control, fewer complications, and overall improved health outcomes.
4. Community health workshops, educational programs at local community centers, partnerships with local schools to provide health education, and accessible online resources can enhance health education. These programs should focus on diabetes self-management, nutrition, and general health literacy.
5. The lack of accessible health care services can lead to delayed treatment, worsening of Maria's condition, increased complications, and ultimately higher health care costs due to emergency care and hospitalizations. Poor access to health care also reduces preventive care opportunities, contributing to the progression of chronic diseases like diabetes.
6. Solutions include expanding community health centers, providing mobile health clinics, increasing funding for public health initiatives, and implementing telehealth services to reach underserved populations. Additionally, policies that incentivize health care providers to work in underserved areas and improving public transportation to healthcare facilities can help.
7. Living in a food desert forces Maria to consume high-calorie, low-nutrient foods, which can lead to poor diabetes control and increased complications. Limited access to healthy foods makes it challenging to follow dietary recommendations for managing diabetes.
8. Initiatives could include improving public transportation routes, providing subsidized transportation vouchers, partnering with ride-sharing services, and developing community-based transport programs. Mobile clinics and telehealth services can also mitigate transportation barriers by bringing healthcare services directly to the community.
9. A lack of social support can lead to feelings of isolation, depression, and reduced motivation to adhere to treatment plans. Social support is crucial for emotional well-being and effective disease management. Without it, Maria may struggle more with managing her diabetes and overall health.
10. Community programs such as neighborhood watch groups, community centers offering social activities, mental health support groups, and safe spaces for exercise can enhance social support and safety. Initiatives to improve public safety, such as increased police presence and community policing, can also create a safer environment for residents to engage in outdoor activities and social interactions.
Answers to interactive elements are given within the interactive element.
Answers to interactive elements are given within the interactive element.
Answers to interactive elements are given within the interactive element.
Answers to interactive elements are given within the interactive element.
Answers to interactive elements are given within the interactive element.
Answers to interactive elements are given within the interactive element.
Answers to interactive elements are given within the interactive element.
Answers to interactive elements are given within the interactive element.
Answers to interactive elements are given within the interactive element.
Exercises
Please utilize the "Suite of Patients" and suggested prompt activities below to engage your students in knowledge application associated with the various learning units throughout the text.
Unit Patients
- 56-year-old female admitted yesterday afternoon with nausea/vomiting and right-sided upper abdominal pain that increases after eating. Has had two stools since admit and vomiting stopped after dose of Zofran in ER. Had ERCP yesterday afternoon for dilated biliary duct. She is scheduled for OR this morning for cholecystectomy. Only medical history is depression and surgical history of C-section x2. She does not take any medications routinely at home. She is accompanied by her 17-year-old daughter.
- 65-year-old male hospitalized three days prior with malaise, cough, cachexia, and 30 pounds of unintentional weight loss over past six weeks. He has a remote history of alcohol and drug abuse but has been sober for more than 10 years. He was diagnosed with acquired immunodeficiency syndrome (AIDS), pneumocystis pneumonia (PCP), and oral candidiasis. He is being treated with IV fluids, IV Bactrim, and IV fluconazole. He is divorced and has one daughter. His ex-wife came to the hospital yesterday to visit. He has no visitors currently. The patient is very quiet and withdrawn.
- 32-year-old nonbinary person, who was transferred from the ICU this morning after being extubated. Patient was admitted five days prior with COVID. Patient cannot have visitors due to COVID status. Continues four liters nasal cannula oxygen.
- 29-year-old female with cellulitis on right arm from infiltration from heroine injection. Her wife is present, along with their 4-year-old son. She had an I&D yesterday and may need to have repeat procedure tomorrow. Currently on IV antibiotics.
- 52-year-old male with gangrene of fourth toe from having a nail through sole of shoe. Patient has a history of uncontrolled diabetes, hypertension (HTN), peripheral vascular disease (PVD), chronic kidney disease (CKD) stage 2, and peripheral neuropathy. Receiving IV antibiotics and scheduled for toe amputation tomorrow. He has no visitors.
- 82-year-old female who had elective right hip replacement for uncontrolled hip pain and degenerative joint disease (DJD). She has a history of type 2 diabetes mellitus on metformin and dietary restrictions; previous hysterectomy, osteoporosis, carpal tunnel repair, and rheumatoid arthritis, which she takes oral methotrexate to control. She has a son who is visiting. Expected to be discharged today.
- 68-year-old male awaiting nursing home placement following admission for hepatic encephalopathy from alcoholism. He was medically cleared last week but is a registered sex offender and has yet to find placement. He has an activated power of attorney, who is a state-appointed guardian. He continues to get up without calling, makes inappropriate remarks to staff, and had a fall three days prior. Other history is bipolar disorder, alcohol abuse, type 2 diabetic, chronic kidney disease stage 3, and hypertension.
- 19-year-old female admitted for what is presumed Benadryl overdose last evening. On room air, needs to have 1:1 sitter present. Patient is not responding to questions; does not know if this is accidental overdose or intentional. History of previous intentional overdose, depression, and anxiety. Dad is present and demanding to know if a toxicology screen was completed and what it showed.
- 61-year-old male admitted six days prior with confusion. Was found by a neighbor wandering. Works at the local gas station. Initial work up shows what appears to be lung cancer with brain metastasis. Patient does not have a power of attorney. He is not married and is estranged from his son. Neighbor who found him is a friend and is willing to become guardian. History from neighbor and review of medical records shows a history of smoking. Neighbor says it does appear he has lost weight recently but hadn’t mentioned other concerns when he had talked to him about two weeks ago. In the process of paperwork to be completed for guardianship. Patient had been aspirating when eating; decision to start nasal gastric feed was made yesterday by ethics committee. Awaiting guardianship for further decision on biopsy for confirmed diagnoses and decision to proceed with treatment or switch to hospice care.
- 45-year-old female admitted last evening who is short of breath, dizzy, light-headed, and gastrointestinal bleed. Esophagogastroduodenoscopy (EGD) scheduled for this morning. If negative, will need prep for colonoscopy and then colonoscopy tomorrow. Patient has little medical history except had recently returned from an overseas trip and had chest and back pain about two days after returning. Had been found to have a saddle PE and was hospitalized for five days on heparin drip and discharged home with coumadin about a week prior. Patient continued to have back and intermittent chest pain and had been taking ibuprofen 1-2 times daily since discharge. Husband brought her in last night when she was found to have a Hgb of 6.2. Husband is furious that no one told them she should not be taking ibuprofen on previous discharge.
- 64-year-old male with BKA for nonhealing diabetic ulcer; scheduled to go to rehab today if bed becomes available. Lives alone in a second floor, low-income apartment without an elevator. Does not have any visitors.
- 32-year-old male admitted 15 days prior for newly diagnosed AML. Received induction therapy starting 13 days ago. Patient is at nadir, will need 1 unit of PRBCs for a Hgb of 6.2 today and a unit of platelets for a platelet count of 8. Patient has had fevers for the past two days and is currently receiving vancomycin and cefepime. Also, on prophylactic acyclovir and fluconazole. Patient has mucositis and is on PCA pump and receiving TPN and diet as tolerated (magic mouthwash before meals).
- Cachexic 25-year-old female with history of cystic fibrosis. Admitted for CF exacerbation overnight. Eats during the day and is tube fed overnight. Admitted for extensive pulmonary toileting, IV antibiotics (tobramycin and cefuroxime), continued home respiratory treatments. Patient also needs to have nutrition recommendations reviewed during this hospitalization. She is here with her boyfriend. The boyfriend also has two school-aged children who would like to visit.
- 78-year-old male with a history of HTN and hypothyroid. Admitted two days prior to abdominal pain and nausea/vomiting. Had a colectomy yesterday for perforated diverticulitis. Patient is NPO and has NG tube in place. Had nausea overnight. His wife is expected to visit later today; she went home after return from OR yesterday.
- 89-year-old female admitted from nursing home yesterday with increased confusion. Has a history of dementia, HTN, type 2 diabetes, and dysphagia. Was found to have a UTI. Started on IV Levaquin; awaiting urine cultures. Expected discharge tomorrow. She has been trying to get up frequently overnight. No family present. Needs 1:1 supervision for all feedings.
- 82-year-old man admitted with COPD exacerbation and is on 2 L of home oxygen baseline. Oxygen saturation was 78% on arrival and has not been able to do ADLs because of shortness of breath. Has CAD, HTN, and PAD. Lives in a duplex with his granddaughter who lives on the other side. His granddaughter called yesterday.
- 68-year-old male who is morbidly obese and admitted two days prior for shortness of breath with CHF. Patient is on IV bumex and is down 25 pounds since admit. He has a history of HTN, CAD, post CABG, and CKD stage 2. Expected discharge today.
- 36-year-old female admitted for excessive uterine bleeding four days prior. Newly diagnosed with uterine cancer. Patient had open hysterectomy, oophorectomy, salpingotomy, and lymph node biopsy. Had diagnostics, port placement, and staging over the past three days. Expected discharge today. Her husband is here with their 16-month-old daughter. The husband has been very inattentive during this hospitalization and has expected her to watch their daughter over the last couple days and even left to go for lunch yesterday while leaving the daughter in the room.
- 68-year-old male with history of stage 3 CKD and admitted with AKI on CKD yesterday. Patient has had nausea and vomiting for past 36 hours; baseline creatinine of 1.8 and was 4.6 on admit. Has been given fluid hydration and is down to 3.2 this morning.
- Bed open.
- It is “ortho day” in the OR. There are three patients scheduled. 1 is a 54-year-old male with bilateral knee replacement (0800 surgery time) and scheduled for observation admit. 68-year-old women with right knee (1100 surgery time) and expected to be discharged. 78-year-old male with hip replacement (1300 OR time) and scheduled for observation admit.
- 72-year-old female waiting for a bed in the emergency room. Arrived overnight with hypoxia, cough, SOB. Positive for influenza.
Classroom Activity Ideas:
Prioritization
Put students in groups and a patient assignment (4-5 patients). Have them identify who they would see first, second, etc. Why?
Students will review all of the patients on the unit. Have them identify those who are most critical and why.
Add in “changes of conditions” – Patient with AKI on CKD morning labs showed a K of 7.2 and Na of 118. AML spikes temp of 103.6 and develops hives and chest tightness when PRBCs are infusing. Newly diagnosed uterine cancer patient states she is concerned going home with her husband because she feels the abuse is going to get worse now that she is sick.
Classroom Activity Ideas:
Delegation/Supervision
Different staffing assignments: 5 RNs/2 CNAs; 4 RNS, 2 LPNs, 2 CNAs; charge nurse/no change nurse. Have students identify appropriate assignments, tasks for delegation, etc.
Consider different types of acute care units – would you organize assignments differently?
Classroom Activity Ideas:
Legal
Develop a scenario in which one patient is upset about not being taught about ibuprofen. Consider the legal implications associated with the lack of education.
How would a student address the father who wants to get information on daughter who overdosed?
Can a 17-year-old daughter be at the hospital without another guardian?
Classroom Activity Ideas:
Economics
Talk about isolation/PPE use and staffing ratios.
Have students utilize a couple different staffing tools to see acuity score.
Classroom Activity Ideas:
Quality/Evidence-Based Practice
Have students look up EBP guideline on one of their patients in their assignment (e.g., when to transfuse with blood and platelets for AML patient, ERCP prior to cholecystectomy, etc.).
Classroom Activity Ideas:
Ethical Practice
Patient who is waiting guardianship placement - diagnosed with new brain tumor.
Classroom Activity Ideas:
Managing the Nursing Team
Talk about the ways a charge nurse, nurse manager, and RN work with these patients.
Have each team assigned a new patient (post op, one in ED) with different methods of assigning – choosing who the new patient for the day would be, assigning at start of shift, and during the day.
Have one of the nurses refuse a new patient.
Classroom Activity Ideas:
Collaborating with Multidisciplinary Team
With your assigned patients, whom would you interact with during the day (e.g., PT, OT, ST, provider, lab, case management)?
Classroom Activity Ideas:
Advocacy
What community agencies might you recommend to the patients with whom you are working?
How would you work with a patient (e.g., the hip patient #6) who doesn’t feel comfortable being discharged today?
Exercises
Please utilize the "Suite of Patients" and suggested prompt activities below to engage your students in knowledge application associated with the various learning units throughout the text.
Unit Patients
- 56-year-old female admitted yesterday afternoon with nausea/vomiting and right-sided upper abdominal pain that increases after eating. Has had two stools since admit and vomiting stopped after dose of Zofran in ER. Had ERCP yesterday afternoon for dilated biliary duct. She is scheduled for OR this morning for cholecystectomy. Only medical history is depression and surgical history of C-section x2. She does not take any medications routinely at home. She is accompanied by her 17-year-old daughter.
- 65-year-old male hospitalized three days prior with malaise, cough, cachexia, and 30 pounds of unintentional weight loss over past six weeks. He has a remote history of alcohol and drug abuse but has been sober for more than 10 years. He was diagnosed with acquired immunodeficiency syndrome (AIDS), pneumocystis pneumonia (PCP), and oral candidiasis. He is being treated with IV fluids, IV Bactrim, and IV fluconazole. He is divorced and has one daughter. His ex-wife came to the hospital yesterday to visit. He has no visitors currently. The patient is very quiet and withdrawn.
- 32-year-old nonbinary person, who was transferred from the ICU this morning after being extubated. Patient was admitted five days prior with COVID. Patient cannot have visitors due to COVID status. Continues four liters nasal cannula oxygen.
- 29-year-old female with cellulitis on right arm from infiltration from heroine injection. Her wife is present, along with their 4-year-old son. She had an I&D yesterday and may need to have repeat procedure tomorrow. Currently on IV antibiotics.
- 52-year-old male with gangrene of fourth toe from having a nail through sole of shoe. Patient has a history of uncontrolled diabetes, hypertension (HTN), peripheral vascular disease (PVD), chronic kidney disease (CKD) stage 2, and peripheral neuropathy. Receiving IV antibiotics and scheduled for toe amputation tomorrow. He has no visitors.
- 82-year-old female who had elective right hip replacement for uncontrolled hip pain and degenerative joint disease (DJD). She has a history of type 2 diabetes mellitus on metformin and dietary restrictions; previous hysterectomy, osteoporosis, carpal tunnel repair, and rheumatoid arthritis, which she takes oral methotrexate to control. She has a son who is visiting. Expected to be discharged today.
- 68-year-old male awaiting nursing home placement following admission for hepatic encephalopathy from alcoholism. He was medically cleared last week but is a registered sex offender and has yet to find placement. He has an activated power of attorney, who is a state-appointed guardian. He continues to get up without calling, makes inappropriate remarks to staff, and had a fall three days prior. Other history is bipolar disorder, alcohol abuse, type 2 diabetic, chronic kidney disease stage 3, and hypertension.
- 19-year-old female admitted for what is presumed Benadryl overdose last evening. On room air, needs to have 1:1 sitter present. Patient is not responding to questions; does not know if this is accidental overdose or intentional. History of previous intentional overdose, depression, and anxiety. Dad is present and demanding to know if a toxicology screen was completed and what it showed.
- 61-year-old male admitted six days prior with confusion. Was found by a neighbor wandering. Works at the local gas station. Initial work up shows what appears to be lung cancer with brain metastasis. Patient does not have a power of attorney. He is not married and is estranged from his son. Neighbor who found him is a friend and is willing to become guardian. History from neighbor and review of medical records shows a history of smoking. Neighbor says it does appear he has lost weight recently but hadn’t mentioned other concerns when he had talked to him about two weeks ago. In the process of paperwork to be completed for guardianship. Patient had been aspirating when eating; decision to start nasal gastric feed was made yesterday by ethics committee. Awaiting guardianship for further decision on biopsy for confirmed diagnoses and decision to proceed with treatment or switch to hospice care.
- 45-year-old female admitted last evening who is short of breath, dizzy, light-headed, and gastrointestinal bleed. Esophagogastroduodenoscopy (EGD) scheduled for this morning. If negative, will need prep for colonoscopy and then colonoscopy tomorrow. Patient has little medical history except had recently returned from an overseas trip and had chest and back pain about two days after returning. Had been found to have a saddle PE and was hospitalized for five days on heparin drip and discharged home with coumadin about a week prior. Patient continued to have back and intermittent chest pain and had been taking ibuprofen 1-2 times daily since discharge. Husband brought her in last night when she was found to have a Hgb of 6.2. Husband is furious that no one told them she should not be taking ibuprofen on previous discharge.
- 64-year-old male with BKA for nonhealing diabetic ulcer; scheduled to go to rehab today if bed becomes available. Lives alone in a second floor, low-income apartment without an elevator. Does not have any visitors.
- 32-year-old male admitted 15 days prior for newly diagnosed AML. Received induction therapy starting 13 days ago. Patient is at nadir, will need 1 unit of PRBCs for a Hgb of 6.2 today and a unit of platelets for a platelet count of 8. Patient has had fevers for the past two days and is currently receiving vancomycin and cefepime. Also, on prophylactic acyclovir and fluconazole. Patient has mucositis and is on PCA pump and receiving TPN and diet as tolerated (magic mouthwash before meals).
- Cachexic 25-year-old female with history of cystic fibrosis. Admitted for CF exacerbation overnight. Eats during the day and is tube fed overnight. Admitted for extensive pulmonary toileting, IV antibiotics (tobramycin and cefuroxime), continued home respiratory treatments. Patient also needs to have nutrition recommendations reviewed during this hospitalization. She is here with her boyfriend. The boyfriend also has two school-aged children who would like to visit.
- 78-year-old male with a history of HTN and hypothyroid. Admitted two days prior to abdominal pain and nausea/vomiting. Had a colectomy yesterday for perforated diverticulitis. Patient is NPO and has NG tube in place. Had nausea overnight. His wife is expected to visit later today; she went home after return from OR yesterday.
- 89-year-old female admitted from nursing home yesterday with increased confusion. Has a history of dementia, HTN, type 2 diabetes, and dysphagia. Was found to have a UTI. Started on IV Levaquin; awaiting urine cultures. Expected discharge tomorrow. She has been trying to get up frequently overnight. No family present. Needs 1:1 supervision for all feedings.
- 82-year-old man admitted with COPD exacerbation and is on 2 L of home oxygen baseline. Oxygen saturation was 78% on arrival and has not been able to do ADLs because of shortness of breath. Has CAD, HTN, and PAD. Lives in a duplex with his granddaughter who lives on the other side. His granddaughter called yesterday.
- 68-year-old male who is morbidly obese and admitted two days prior for shortness of breath with CHF. Patient is on IV bumex and is down 25 pounds since admit. He has a history of HTN, CAD, post CABG, and CKD stage 2. Expected discharge today.
- 36-year-old female admitted for excessive uterine bleeding four days prior. Newly diagnosed with uterine cancer. Patient had open hysterectomy, oophorectomy, salpingotomy, and lymph node biopsy. Had diagnostics, port placement, and staging over the past three days. Expected discharge today. Her husband is here with their 16-month-old daughter. The husband has been very inattentive during this hospitalization and has expected her to watch their daughter over the last couple days and even left to go for lunch yesterday while leaving the daughter in the room.
- 68-year-old male with history of stage 3 CKD and admitted with AKI on CKD yesterday. Patient has had nausea and vomiting for past 36 hours; baseline creatinine of 1.8 and was 4.6 on admit. Has been given fluid hydration and is down to 3.2 this morning.
- Bed open.
- It is “ortho day” in the OR. There are three patients scheduled. 1 is a 54-year-old male with bilateral knee replacement (0800 surgery time) and scheduled for observation admit. 68-year-old women with right knee (1100 surgery time) and expected to be discharged. 78-year-old male with hip replacement (1300 OR time) and scheduled for observation admit.
- 72-year-old female waiting for a bed in the emergency room. Arrived overnight with hypoxia, cough, SOB. Positive for influenza.
Classroom Activity Ideas:
Prioritization
Put students in groups and a patient assignment (4-5 patients). Have them identify who they would see first, second, etc. Why?
Students will review all of the patients on the unit. Have them identify those who are most critical and why.
Add in “changes of conditions” – Patient with AKI on CKD morning labs showed a K of 7.2 and Na of 118. AML spikes temp of 103.6 and develops hives and chest tightness when PRBCs are infusing. Newly diagnosed uterine cancer patient states she is concerned going home with her husband because she feels the abuse is going to get worse now that she is sick.
Classroom Activity Ideas:
Delegation/Supervision
Different staffing assignments: 5 RNs/2 CNAs; 4 RNS, 2 LPNs, 2 CNAs; charge nurse/no change nurse. Have students identify appropriate assignments, tasks for delegation, etc.
Consider different types of acute care units – would you organize assignments differently?
Classroom Activity Ideas:
Legal
Develop a scenario in which one patient is upset about not being taught about ibuprofen. Consider the legal implications associated with the lack of education.
How would a student address the father who wants to get information on daughter who overdosed?
Can a 17-year-old daughter be at the hospital without another guardian?
Classroom Activity Ideas:
Economics
Talk about isolation/PPE use and staffing ratios.
Have students utilize a couple different staffing tools to see acuity score.
Classroom Activity Ideas:
Quality/Evidence-Based Practice
Have students look up EBP guideline on one of their patients in their assignment (e.g., when to transfuse with blood and platelets for AML patient, ERCP prior to cholecystectomy, etc.).
Classroom Activity Ideas:
Ethical Practice
Patient who is waiting guardianship placement - diagnosed with new brain tumor.
Classroom Activity Ideas:
Managing the Nursing Team
Talk about the ways a charge nurse, nurse manager, and RN work with these patients.
Have each team assigned a new patient (post op, one in ED) with different methods of assigning – choosing who the new patient for the day would be, assigning at start of shift, and during the day.
Have one of the nurses refuse a new patient.
Classroom Activity Ideas:
Collaborating with Multidisciplinary Team
With your assigned patients, whom would you interact with during the day (e.g., PT, OT, ST, provider, lab, case management)?
Classroom Activity Ideas:
Advocacy
What community agencies might you recommend to the patients with whom you are working?
How would you work with a patient (e.g., the hip patient #6) who doesn’t feel comfortable being discharged today?
A
ABCs: Airway, breathing, and circulation. (Chapter 2.3)
Accountability: Being answerable to oneself and others for one’s own choices, decisions, and actions as measured against a standard. (Chapter 3.4)
Accreditation: A review process to determine if an agency meets the defined standards of quality determined by the accrediting body. (Chapter 9.2)
Actual problems: Nursing problems currently occurring with the patient. (Chapter 2.3)
Acuity: The level of patient care that is required based on the severity of a patient’s illness or condition. (Chapter 2.3)
Acuity-based staffing: A patient assignment model that takes into account the level of patient care required based on the severity of a patient’s illness or condition. (Chapter 8.5)
Acuity-rating staffing models: A staffing model used to make patient assignments that reflects the individualized nursing care required for different types of patients. (Chapter 2.3)
Acute conditions: Conditions having a sudden onset. (Chapter 2.3)
Administrative law: Law made by government agencies that have been granted the authority to pass rules and regulations. For example, each state’s Board of Nursing is an example of administrative law. (Chapter 5.2)
Admission: Refers to an initial visit or contact with a client. (Chapter 7.8)
Advanced directives: Written instruction, such as a living will or durable power of attorney for health care, recognized under state law, relating to the provision of health care when the individual is incapacitated. (Chapter 5.6)
Advocacy: The act or process of pleading for, supporting, or recommending a cause or course of action. Advocacy may be for persons (whether an individual, group, population, or society) or for an issue, such as potable water or global health. (Chapter 6.2, Chapter 10.2)
Affordable Care Act (ACA): Legislation enacted in 2010 to increase consumers’ access to health care coverage and protect them from insurance practices that restrict care or significantly increase the cost of care. (Chapter 8.2)
ANA’s Standards of Professional Practice: Standards describing a competent level of nursing practice as demonstrated by the critical thinking model known as the nursing process. The nursing process includes the components of assessment, diagnosis, outcomes identification, planning, implementation, and evaluation. (Chapter 1.1)
ANA’s Standards of Professional Performance: Standards describing a competent level of behavior in the professional nursing role, including activities related to ethics, advocacy, respectful and equitable practice, communication, collaboration, leadership, education, scholarly inquiry, quality of practice, professional practice evaluation, resource stewardship, and environmental health. (Chapter 1.1, Chapter 9.2)
Assault: Intentionally putting another person in reasonable apprehension of an imminent harmful or offensive contact. (Chapter 5.2)
Assignment: Routine care, activities, and procedures that are within the authorized scope of practice of the RN, LPN/VN, or routine functions of the assistive personnel. (Chapter 3.3)
Assistive personnel (AP): Any assistive personnel (formerly referred to as ‘‘unlicensed” assistive personnel [UAP]) trained to function in a supportive role, regardless of title, to whom a nursing responsibility may be delegated. This includes, but is not limited to, certified nursing assistants or aides (CNAs), patient-care technicians (PCTs), certified medical assistants (CMAs), certified medication aides, and home health aides. (Chapter 3.1)
Autonomy: The capacity to determine one’s own actions through independent choice, including demonstration of competence. (Chapter 6.2)
B
Battery: Intentional causation of harmful or offensive contact with another’s person without that person’s consent. (Chapter 5.2)
Beneficence: The bioethical principle of benefiting others by preventing harm, removing harmful conditions, or affirmatively acting to benefit another or others, often going beyond what is required by law. (Chapter 6.2)
Benner’s Novice to Expert Theory: A theory by Dr. Patricia Benner that explains how new hires develop skills and a holistic understanding of patient care over time, resulting from a combination of a strong educational foundation and thorough clinical experiences. Benner’s theory identifies five levels of nursing experience: novice, advanced beginner, competent, proficient, and expert. (Chapter 11.5)
Board of Nursing: The state-specific licensing and regulatory body that sets standards for safe nursing care and issues nursing licenses to qualified candidates, based on the Nurse Practice Act. (Chapter 1.1)
Brief: A short session to share a plan, discuss team formation, assign roles and responsibilities, establish expectations and climate, and anticipate outcomes and contingencies. (Chapter 7.6)
Budget: An estimate of revenue and expenses over a specified period of time, usually over a year. (Chapter 8.5)
Burnout: A condition manifested physically and psychologically with a loss of motivation. (Chapter 12.6)
C
Capacity: A functional determination that an individual is or is not capable of making a medical decision within a given situation. (Chapter 5.6)
Capital budgets: Budgets used to plan investments and upgrades to tangible assets that lose or gain value over time. Capital is something that can be touched, such as buildings or computers. (Chapter 8.5)
Change: The process of altering or replacing existing knowledge, skills, attitudes, systems, policies, or procedures. (Chapter 4.3)
Change agent: Anyone who has the skill and power to stimulate, facilitate, and coordinate the change effort. (Chapter 4.3)
Change management: Process of making changes in a deliberate, planned, and systematic manner. (Chapter 4.3)
Chronic conditions: Conditions that have a slow onset and may gradually worsen over time. (Chapter 2.3)
Civil law: Law focusing on the rights, responsibilities, and legal relationships between private citizens. (Chapter 5.2)
Clinical reasoning: “A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions.” (Chapter 2.4)
Closed-loop communication: A communication strategy used to ensure that information conveyed by the sender is heard by the receiver and completed. (Chapter 3.2, Chapter 7.5)
Code of ethics: A set of ethical principles established by a profession that is designed to govern decision-making and assist individuals to distinguish right from wrong. (Chapter 6.2)
Collective bargaining: Negotiation of wages and other conditions of employment by an organized body of employees. (Chapter 10.4)
Commission: Doing something a reasonable nurse would not have done. (Chapter 5.2)
Communication conflict: Occurs when there is a failure in the exchange of information. (Chapter 7.7)
Compassion fatigue: A state of chronic and continuous self-sacrifice and/or prolonged exposure to difficult situations that affect a health care professional’s physical, emotional, and spiritual well-being. (Chapter 12.6)
Competence: In a legal sense, the ability of an individual to participate in legal proceedings. A judge decides if an individual is “competent” or “incompetent.” (Chapter 5.6)
Confidentiality: The right of an individual to have personal, identifiable medical information kept private. (Chapter 5.2)
Consequentialism: An ethical theory used to determine whether or not an action is right by the consequences of the action. For example, most people agree that lying is wrong, but if telling a lie would help save a person’s life, consequentialism says it’s the right thing to do. (Chapter 6.2)
Constitutional law: The rights, privileges, and responsibilities established by the U.S. Constitution. For example, the right to privacy is a right established by the constitution. (Chapter 5.2)
Constructive feedback: Supportive feedback that offers solutions to areas of weakness. (Chapter 3.5)
Continuity of care: The use of information on past events and personal circumstances to make current care appropriate for each individual. (Chapter 7.8)
Contracts: Binding written, verbal, or implied agreements. (Chapter 5.2)
Co-pay: A flat fee the consumer pays at the time of receiving a health care service as a part of their health care plan. (Chapter 8.3)
Core measures: National standards of care and treatment processes for common conditions. These processes are proven to reduce complications and lead to better patient outcomes. (Chapter 9.2)
Core values: The foundational ideals that guide the organization’s actions and decision-making processes. (Chapter 4.2)
Crime: A type of behavior defined by Congress or state legislature as deserving of punishment. (Chapter 5.2)
Criminal law: A system of laws concerned with punishment of individuals who commit crimes. (Chapter 5.2)
Critical thinking: A broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.” (Chapter 2.4)
Cultural diversity: A term used to describe cultural differences among clients, family members, and health care team members. (Chapter 7.3)
Cultural humility: A humble and respectful attitude toward individuals of other cultures that pushes one to challenge their own cultural biases, realize they cannot possibly know everything about other cultures, and approach learning about other cultures as a lifelong goal and process. (Chapter 6.2, Chapter 7.3)
Culture of safety: Organizational culture that embraces error reporting by employees with the goal of identifying systemic causes of problems that can be addressed to improve patient safety. Just Culture is a component of a culture of safety. (Chapter 4.2, Chapter 5.5))
CURE hierarchy: A strategy for prioritization based on identifying “critical” needs, “urgent” needs, “routine” needs, and “extras.” (Chapter 2.3)
CUS statements: Assertive statements that are well-recognized by all staff across a health care agency as implementation of the two-challenge rule. These assertive statements are “I am Concerned – I am Uncomfortable – This is a Safety issue!” (Chapter 7.6)
D
Data cues: Pieces of significant clinical information that direct the nurse toward a potential clinical concern or a change in condition. (Chapter 2.3)
Debrief: An informal information exchange session designed to improve team performance and effectiveness through reinforcement of positive behaviors and reflecting on lessons learned after a significant event occurs. (Chapter 7.6)
Deductible: The amount of money a consumer pays for health care before their insurance plan pays anything. These amounts generally apply per person per calendar year. (Chapter 8.3)
Defamation of character: An act of making negative, malicious, and false remarks about another person to damage their reputation. Slander is spoken defamation and libel is written defamation. (Chapter 5.2)
Defendants: The parties named in a lawsuit. (Chapter 5.2)
Delegated responsibility: A nursing activity, skill, or procedure that is transferred from a license nurse to a delegatee. (Chapter 3.4)
Delegatee: An RN, LPN/VN, or AP who is delegated a nursing responsibility by either an APRN, RN, or LPN/VN who is competent to perform the task and verbally accepts the responsibility. (Chapter 3.4)
Delegation: Allowing a delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role but in which they have received additional training. (Chapter 3.4)
Delegator: An APRN, RN, or LPN/VN who requests a specially trained delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role. (Chapter 3.4)
Deontology: An ethical theory based on rules that distinguish right from wrong. (Chapter 6.2)
DESC: A tool used to help resolve conflict. DESC is a mnemonic that stands for Describe the specific situation or behavior and provide concrete data, Express how the situation makes you feel/what your concerns are using “I” messages, Suggest other alternatives and seek agreement, and Consequences are stated in terms of impact on established team goals while striving for consensus. (Chapter 7.6)
Discharge: The completion of care and services in a health care facility and the client is sent home (or to another health care facility). (Chapter 7.8)
Durable power of attorney for healthcare (DPOAHC): Person chosen to speak on one’s behalf if one becomes incapacitated. (Chapter 5.6)
Duty of reasonable care: Legal obligations nurses have to their patients to adhere to current standards of practice. (Chapter 5.2)
E
Economics: The study of how society makes decisions about its limited resources. (Chapter 8.1)
Ethical conflict: Occurs when individuals or groups have fundamentally different beliefs and values. (Chapter 7.7)
Ethical dilemma: Conflict resulting from competing values that requires a decision to be made from equally desirable or undesirable options. (Chapter 6.3)
Ethical principles: Principles used to define nurses’ moral duties and aid in ethical analysis and decision-making. Foundational ethical principles include autonomy (self-determination), beneficence (do good), nonmaleficence (do no harm), justice (fairness), and veracity (tell the truth). (Chapter 6.2)
Ethics: A system of moral principles that a society uses to identify right from wrong. (Chapter 6.2)
Ethics committee: A formal committee established by a health care organization to problem-solve ethical dilemmas. (Chapter 6.4)
Evidence-Based Practice (EBP): A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and patient, family, group, community, and population preferences and values. (Chapter 8.4, Chapter 9.4, Chapter 10.7)
Expected conditions: Conditions that are likely to occur or anticipated in the course of an illness, disease, or injury. (Chapter 2.3)
Extrinsic factors: External elements that impact health care costs. (Chapter 8.2)
F
False imprisonment: An act of restraining another person causing that person to be confined in a bounded area. Restraints can be physical, verbal, or chemical. (Chapter 5.2)
Feedback: Information is provided to a team member for the purpose of improving team performance. Feedback should be timely, respectful, specific, directed towards improvement, and considerate. (Chapter 7.6)
Felonies: Serious crimes that cause the perpetrator to be imprisoned for greater than one year. (Chapter 5.2)
Fidelity: An ethical principle meaning keeping promises. (Chapter 6.2)
Five rights of delegation: Right task, right circumstance, right person, right directions and communication, and right supervision and evaluation. (Chapter 3.4)
Floating: An agency strategy that asks nurses to temporarily work on a different unit to help cover a short-staffed shift. (Chapter 8.5)
Followership: The upward influence of individuals on their leaders and their teams. (Chapter 4.2)
Fraud: An act of deceiving an individual for personal gain. (Chapter 5.2)
G
Goal conflict: Happens when the objectives of individuals or groups are incompatible. (Chapter 7.7)
Good Samaritan Law: State law providing protections against negligence claims to individuals who render aid to people experiencing medical emergencies outside of clinical environments. (Chapter 5.2)
Grievance process: A process for resolving disagreements between employees and management. (Chapter 10.4)
H
Handoff reports: A transfer and acceptance of patient care responsibility achieved through effective communication. It is a real-time process of passing patient specific information from one caregiver to another, or from one team of caregivers to another, for the purpose of ensuring the continuity and safety of the patient’s care. (Chapter 7.5)
Harmful stress: Stress (also referred to as “distress”) not adequately self-managed resulting in physical, mental, and behavioral consequences. (Chapter 12.3)
Health care disparity: Differences in access to health care and insurance coverage. (Chapter 8.4)
Health disparities: Differences in health outcomes that result from social determinants of health (SDOH). (Chapter 8.4)
Horizontal aggression: Hostile behavior among one’s peers. (Chapter 7.7)
Huddle: A brief meeting during a shift to reestablish situational awareness, reinforce plans already in place, and adjust the teamwork plan as needed. (Chapter 7.6)
I
I’M SAFE: A tool used to assess one’s own safety status, as well as that of other team members in their ability to provide safe patient care. It is a mnemonic standing for personal safety risks as a result of Illness, Medication, Stress, Alcohol and Drugs, Fatigue, and Eating and Elimination. (Chapter 7.6)
Informatics: Using information and technology to communicate, manage knowledge, mitigate error, and support decision-making. This allows members of the health care team to share, store, and analyze health-related information. (Chapter 9.3, Chapter 10.7)
Informed consent: The fundamental right of a client to accept or reject health care. (Chapter 5.6)
Infractions: Minor offenses, such as speeding tickets, that result in fines but not jail time. (Chapter 5.2)
Institutional liability: When the healthcare institution (e.g., hospital, clinic) is held responsible for the actions of its employees or for failing to implement adequate policies and procedures to prevent harm. (Chapter 5.3)
Institutional Review Board (IRB): A group that has been formally designated to review and monitor biomedical research involving human subjects. (Chapter 6.4)
Intentional tort: An act of commission with the intent of harming or causing damage to another person. Examples of intentional torts include assault, battery, false imprisonment, slander, libel, and breach of privacy or client confidentiality. (Chapter 5.2)
Interdisciplinary care conferences: Meetings where interprofessional team members professionally collaborate, share their expertise, and plan collaborative interventions to meet client needs. (Chapter 7.8)
Interprofessional collaborative practice: Multiple health workers from different professional backgrounds working together with patients, families, caregivers, and communities to deliver the highest quality of care. (Chapter 7.1)
Intrinsic factors: Factors that are inherent to the characteristics and needs of the population. (Chapter 8.2)
I-PASS: A mnemonic used as a structured communication tool among interprofessional team members. I-PASS stands for Illness severity, Patient summary, Action list, Situation awareness, and Synthesis by the receiver. (Chapter 7.5)
ISBARR: A mnemonic for the components to include when communicating with another health care team member: Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat back. (Chapter 7.5, Chapter 10.7)
J
Just Culture: A culture where people feel safe raising questions and concerns and report safety events in an environment that emphasizes a nonpunitive response to errors and near misses. Clear lines are drawn between human error, at-risk, and reckless employee behaviors. (Chapter 4.2)
Justice: A moral obligation to act on the basis of equality and equity and a standard linked to fairness for all in society. (Chapter 6.2)
L
Laws: Rules and regulations created by society and enforced by courts, statutes, and/or professional licensure boards. (Chapter 5.2)
Leadership: The art of establishing direction and influencing and motivating others to achieve their maximum potential to accomplish tasks, objectives, or projects. (Chapter 4.2)
Libel: Written defamation. (Chapter 5.2)
Licensure: The process by which a State Board of Nursing (SBON) grants permission to an individual to engage in nursing practice after verifying the applicant has attained the competency necessary to perform the scope of practice of a registered nurse (RN). The SBON verifies three components:
- Verification of graduation from an approved prelicensure RN nursing education program
- Verification of successful completion of NCLEX-RN examination
- A criminal background check (in some states) (Chapter 11.3)
Living will: A type of advance directive in which an individual identifies what treatments they would like to receive or refuse if they become incapacitated and unable to make decisions.
M
Magnet® Recognition Program: An organizational credential that recognizes quality patient outcomes, nursing excellence, and innovations in professional nursing practice. (Chapter 10.4)
Malpractice: A specific term used for negligence committed by a professional with a license. (Chapter 5.2)
Management: Roles that focus on tasks such as planning, organizing, prioritizing, budgeting, staffing, coordinating, and reporting. (Chapter 4.2)
Mandatory overtime: A requirement by agencies for nurses to stay and care for patients beyond their scheduled shift when short staffing occurs. (Chapter 8.5)
Maslow’s Hierarchy of Needs: Prioritization strategies often reflect the foundational elements of physiological needs and safety and progress toward higher levels. (Chapter 2.3)
Medicaid: A joint federal and state program covering groups of eligible individuals, such as low-income families, qualified pregnant women and children, and individuals receiving Supplemental Security Income (SSI). States may choose to cover additional groups, such as individuals receiving home and community-based services and children in foster care who are not otherwise eligible. (Chapter 8.3)
Medicare: A federal health insurance program used by people aged 65 and older, younger individuals with permanent disabilities, and people with end-stage renal disease requiring dialysis or a kidney transplant. (Chapter 8.3)
Meta-analysis: A type of nursing research (also referred to as a “systematic review”) that compares the results of independent research studies asking similar research questions. This research often collects both quantitative and qualitative data to provide a well-rounded evaluation by providing both objective and subjective outcomes. (Chapter 9.4)
Mindfulness: Awareness that arises through paying attention, being on purpose and in the present moment, and being nonjudgmental. (Chapter 12.6)
Misdemeanors: Less serious crimes resulting in fines and/or imprisonment for less than one year. (Chapter 5.2)
Mission statement: An organization’s statement that describes how the organization will fulfill its vision and establishes a common course of action for future endeavors. (Chapter 4.2)
Moral conflict: Feelings occurring when an individual is uncertain about what values or principles should be applied to an ethical issue. (Chapter 6.3)
Moral courage: The willingness of an individual to speak out and do what is right in the face of forces that would lead us to act in some other way. (Chapter 6.3)
Moral distress: Feelings occurring when correct ethical action is identified but the individual feels constrained by competing values of an organization or other individuals. (Chapter 6.3)
Moral injury: The distressing psychological, behavioral, social, and sometimes spiritual aftermath of exposure to events that contradict deeply held moral beliefs and expectations. (Chapter 6.3)
Morality: Personal values, character, or conduct of individuals or groups within communities and societies. (Chapter 6.2)
Moral outrage: Feelings occurring when an individual witnesses immoral acts or practices they feel powerless to change. (Chapter 6.3)
Morals: The prevailing standards of behavior of a society that enable people to live cooperatively in groups. (Chapter 6.2)
Mutual support: The ability to anticipate and support team members’ needs through accurate knowledge about their responsibilities and workload. (Chapter 7.6)
N
NCLEX-RN: The exam that nursing graduates must pass successfully to obtain their nursing license and become a registered nurse. (Chapter 11.2)
NCLEX-RN Test Plan: A concise summary of the content and scope of the NCLEX that serves as an excellent guide for preparing for the exam. These plans are updated every three years based on surveys of newly licensed registered nurses to ensure the NCLEX questions reflect fair, comprehensive, current, and entry-level nursing competency. (Chapter 11.2)
Negligence: The failure to exercise the ordinary care a reasonable person would use in similar circumstances. Wisconsin civil jury instruction states, “A person is not using ordinary care and is negligent, if the person, without intending to do harm, does something (or fails to do something) that a reasonable person would recognize as creating an unreasonable risk of injury or damage to a person or property.” (Chapter 5.2)
Nonmaleficence: The bioethical principle that specifies a duty to do no harm and balances avoidable harm with benefits of good achieved. (Chapter 6.2)
Normal stress: Stress (also referred to as “eustress”) that does not have lasting consequences and is successfully managed by the individual who is experiencing it. (Chapter 12.3)
Nurse Licensure Compact (NLC): State legislation that allows nurses to practice in other NLC states with their original state’s nursing license without having to obtain additional licenses, contingent upon remaining a resident of that state. (Chapter 11.3)
Nurse Practice Act: Law enacted by a state’s legislature that defines the scope of nursing practice and establishes regulations for nursing practice within that state. (Chapter 1.1)
Nurse residency programs: A transition process that provides additional professional development for newly licensed nurses. These programs vary from institution to institution, but many start around the time the new graduate ends their orientation with a preceptor and continue to provide routine support throughout the year. (Chapter 11.5)
Nursing: Integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in recognition of the connection of all humanity.” (Chapter 1.1)
Nursing informatics: The science and practice integrating nursing, its information and knowledge, with information and communication technologies to promote the health of people, families, and communities worldwide. (Chapter 9.3)
Nursing process: Includes the components of assessment, diagnosis, outcomes identification, planning, implementation, and evaluation. (Chapter 1.1)
Nursing research: The systematic inquiry designed to develop knowledge about issues of importance to the nursing profession. The purpose of nursing research is to advance nursing practice through the discovery of new information. It is also used to provide scholarly evidence regarding improved patient outcomes resulting from nursing interventions. (Chapter 9.4)
Nursing team members: Advanced practice registered nurses (APRN), registered nurses (RN), licensed practical/vocational nurses (LPN/VN), and assistive personnel (AP). (Chapter 3.1)
O
Off with benefits: An agency staffing strategy when a nurse is not needed for their scheduled shift. The nurse does not typically receive an hourly wage and is not expected to report to work, but they still accrue benefits such as insurance and paid time off. (Chapter 8.5)
Omission: Not doing something a reasonable nurse would have done. (Chapter 5.2)
On call: An agency staffing strategy when a nurse is not immediately needed for their scheduled shift. They may have options to stay at work and complete work-related education or stay home. (Chapter 8.5)
Operating budgets: Budgets including personnel costs and annual facility operating costs. (Chapter 8.5)
Organizational culture: The implicit values and beliefs that reflect the norms and traditions of an organization. An organization’s vision, mission, and values statements are the foundation of organizational culture. (Chapter 4.2)
Orientation: A structured transition process when hired into a new position that may last from one to four months but can be longer depending on the specialty (e.g., Intensive Care or Labor and Delivery). Orientation is based on the new nurse’s demonstration and completion of competencies. During this time the novice RN will work with a preceptor to experience all the aspects of the role. (Chapter 11.5)
P
Paternalism: The interference by the state or an individual with another person, defended by the claim that the person interfered with will be better off or protected from harm. (Chapter 6.2)
Patient-centered care: The patient is the source of control and full partner in providing compassionate and coordinated care based on respect for patient’s preferences, values, and needs. (Chapter 10.7)
Patient safety goals: Guidelines specific to organizations accredited by The Joint Commission that focus on problems in health care safety and ways to solve them. (Chapter 9.2)
Pay for Performance: A reimbursement model, also known as value-based payment, that attaches financial incentives based on the performance of health care agencies and providers. (Chapter 8.4)
Peer-reviewed: Scholarly journal articles that have been reviewed independently by at least two other academic experts in the same field as the author(s) to ensure accuracy and quality. (Chapter 9.4)
Personality conflict: Arises from differences in individual temperaments, attitudes, and behaviors. (Chapter 7.7)
Plaintiff: The person bringing the lawsuit. (Chapter 5.2)
Policy: An expected course of action set by an agency. (Chapter 1.1)
Portfolio: A compilation of materials showcasing examples of previous work demonstrating one’s skills, qualifications, education, training, and experience. (Chapter 11.4)
Preceptors: Experienced and competent RNs who serve as a role model and a resource to a newly hired nurse. These nurses have the knowledge, skills, and the ability to coach the new RN into the nursing role and answer questions while also evaluating a new hire’s performance and providing feedback for improvement. (Chapter 11.5)
Primary source: An original study or report of an experiment or clinical problem. The evidence is typically written and published by the individual(s) conducting the research and includes a literature review, description of the research design, statistical analysis of the data, and discussion regarding the implications of the results. (Chapter 9.4)
Private law: Laws that govern the relationships between private entities. (Chapter 5.2)
Procedure: An official way of completing a task. (Chapter 1.1)
Protected Health Information (PHI): Individually identifiable health information and includes demographic data related to the individual’s past, present, or future physical or mental health or condition; the provision of health care to the individual; and the past, present, or future payment for the provision of health care to the individual. (Chapter 5.2)
Protocol: A detailed, written plan for performing a regimen of therapy. (Chapter 1.1)
Public law: Law regulating relations of individuals with the government or institutions. (Chapter 5.2)
Q
Qualitative studies: A type of study that provides subjective data, often focusing on the perception or experience of the participants. Data is collected through observations and open-ended questions and often referred to as experimental data. Data is interpreted by developing themes in participants’ views and observations. (Chapter 9.4)
Quality: The degree to which nursing services for health care consumers, families, groups, communities, and populations increase the likelihood of desirable outcomes and are consistent with evolving nursing knowledge. (Chapter 9.2)
Quality Improvement (QI): A systematic process using measurable data to improve health care services and the overall health status of patients. The QI process includes the steps of Plan, Do, Study, and Act. (Chapter 9.3, Chapter 10.7)
Quantitative studies: A type of study that provides objective data by using number values to explain outcomes. Researchers can use statistical analysis to determine strength of the findings, as well as identify correlations. (Chapter 9.4)
R
Ratio-based staffing models: A staffing model used to make patient assignments in terms of one nurse caring for a set number of patients. (Chapter 2.3)
Resiliency training: Educational sessions that foster feelings of mindfulness and sensitivity to self and cultivate professional development techniques that contribute to long-term engagement in the profession. (Chapter 12.7)
Resource stewardship: Using appropriate resources to plan, provide, and sustain evidence-based nursing services that are safe, effective, financially responsible, and used judiciously. (Chapter 8.6)
Resume: A document that highlights one’s background, education, skills, and accomplishments to potential employers. (Chapter 11.4)
Risk problem: A nursing problem that reflects that a patient may experience a problem but does not currently have signs reflecting the problem is actively occurring. (Chapter 2.3)
Role conflict: Arises when individuals have multiple, often conflicting, expectations associated with their roles. (Chapter 7.7)
S
Scope of practice: Procedures, actions, and processes that a health care practitioner is permitted to undertake in keeping with the terms of their professional license. (Chapter 3.3)
Secondary source: Evidence is written by an author who gathers existing data provided from research completed by another individual. This type of source analyzes and reports on findings from other research projects and may interpret findings or draw conclusions. In nursing research these sources are typically published as a systematic review and meta-analysis. (Chapter 9.4)
Self-care: Actions that individuals take to maintain health of oneself. (Chapter 12.6)
Shared governance: A shared leadership model between management and employees working together to achieve common goals. (Chapter 10.4)
Shared mental model: The actions of a team leader that ensure all team members have situation awareness and are “on the same page” as situations evolve on the unit. (Chapter 7.6)
Situation awareness: The awareness of a team member knowing what is going on around them. (Chapter 7.6)
Situation monitoring: The process of continually scanning and assessing the situation to gain and maintain an understanding of what is going on around you. (Chapter 7.6)
Slander: Spoken defamation. (Chapter 5.2)
Social Determinants of Health (SDOH): Conditions in the places where people live, learn, work, and play, such as unstable housing, low-income areas, unsafe neighborhoods, or substandard education that affect a wide range of health risks and outcomes. (Chapter 8.2, Chapter 8.4, Chapter 10.4)
Standards of Professional Nursing Practice: Authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently. (Chapter 1.1)
Statutory law: Written laws enacted by the federal or state legislature. For example, the Nurse Practice Act in each state is an example of statutory law that is enacted by the state government. (Chapter 5.2)
STEP tool: A situation monitoring tool used to know what is going on with you, your patients, your team, and your environment. STEP stands for Status of the patients, Team members, Environment, and Progress Toward Goal. (Chapter 7.6)
Student liability: When the student nurse is held responsible for their own actions that cause harm to patients or violate protocols. (Chapter 5.3)
Supervision: Appropriate monitoring of the delegated activity, evaluation of patient outcomes, and follow-up with the delegatee at the completion of the activity. (Chapter 3.4)
Supervisory liability: When a clinical supervisor or preceptor is held responsible for the actions of the student nurse or for failing to properly supervise them. (Chapter 5.3)
Systems leadership: A set of skills used to catalyze, enable, and support the process of systems-level change that focuses on the individual, the community, and the system. (Chapter 4.2)
Systems theory: The concept that systems do not function in isolation but rather there is an interdependence that exists between their parts. Systems theory assumes that most individuals strive to do good work but are affected by diverse influences within the system. (Chapter 4.2)
T
Team nursing: A common staffing pattern that uses a combination of Registered Nurses (RNs), Licensed Practical/Vocational Nurses (LPN/VNs), and Assistive Personnel (AP) to care for a group of patients. (Chapter 8.5)
*eamSTEPPS® (Team Strategies and Tools to Enhance Performance and Patient Safety): An evidence-based framework to improve client safety through effective communication in health care environments consisting of four core competencies: communication, leadership, situation monitoring, and mutual support. (Chapter 7.6, Chapter 10.7)
Teamwork and collaboration: Functioning effectively within nursing and interprofessional teams, fostering open communication, mutual respect, and shared decision-making to achieve quality patient care. (Chapter 10.7)
Temporary permit: A permit issued by the State Board of Nursing (SBON) that allows the applicant to practice practical nursing under the direct supervision of a registered nurse until their RN license is granted. (Chapter 11.3)
Time estimation: A prioritization strategy including the review of planned tasks and allocation of time believed to be required to complete each task. (Chapter 2.5)
Time scarcity: A feeling of racing against a clock that is continually working against you. (Chapter 2.2)
Titrate: Making adjustments to medication dosage per an established protocol to obtain a desired therapeutic outcome. (Chapter 3.3)
Tort: An act of commission or omission that causes injury or harm to another person for which the courts impose liability. In the context of torts, “injury” describes the invasion of any legal right, whereas “harm” describes a loss or detriment the individual suffers. Torts are classified as intentional or unintentional. (Chapter 5.2)
Two-challenge rule: A strategy for advocating for patient safety that includes a team member assertively voicing their concern at least two times to ensure that it has been heard by the decision-maker. (Chapter 7.6)
U
Unexpected conditions: Conditions that are not likely to occur in the normal progression of an illness, disease, or injury. (Chapter 2.3)
Unintentional tort: Acts of omission (not doing something a person has a responsibility to do) or inadvertently doing something causing unintended accidents leading to injury, property damage, or financial loss. Examples of unintentional torts impacting nurses include negligence and malpractice. (Chapter 5.2)
Utilitarianism: A type of consequentialism that determines whether or not actions are right based on their consequences, with the standard being achieving the greatest good for the greatest number of people. (Chapter 6.2)
Utilization review: An investigation by insurance agencies and other health care funders on services performed by doctors, nurses, and other health care team members to ensure money is not wasted covering things that are unnecessary for proper treatment or are inefficient. This review also allows organizations to objectively measure how effectively health care services and resources are being used to best meet their patients’ needs. (Chapter 9.3)
V
Values: Individual beliefs that motivate people to act one way or another and serve as a guide for behavior. (Chapter 6.2)
Values statement: The organization’s established values that support its vision and mission and provide strategic guidelines for decision-making, both internally and externally, by members of the organization. (Chapter 4.2)
Veracity: An ethical principle meaning telling the truth. (Chapter 6.2)
Vision statement: An organization’s statement that defines why the organization exists, describes how the organization is unique and different from similar organizations, and specifies what the organization is striving to be. (Chapter 4.2)
W
Whistleblower: A person who exposes any kind of information or activity that is deemed illegal, unethical, or not correct within an organization. (Chapter 10.5)
A
ABCs: Airway, breathing, and circulation. (Chapter 2.3)
Accountability: Being answerable to oneself and others for one’s own choices, decisions, and actions as measured against a standard. (Chapter 3.4)
Accreditation: A review process to determine if an agency meets the defined standards of quality determined by the accrediting body. (Chapter 9.2)
Actual problems: Nursing problems currently occurring with the patient. (Chapter 2.3)
Acuity: The level of patient care that is required based on the severity of a patient’s illness or condition. (Chapter 2.3)
Acuity-based staffing: A patient assignment model that takes into account the level of patient care required based on the severity of a patient’s illness or condition. (Chapter 8.5)
Acuity-rating staffing models: A staffing model used to make patient assignments that reflects the individualized nursing care required for different types of patients. (Chapter 2.3)
Acute conditions: Conditions having a sudden onset. (Chapter 2.3)
Administrative law: Law made by government agencies that have been granted the authority to pass rules and regulations. For example, each state’s Board of Nursing is an example of administrative law. (Chapter 5.2)
Admission: Refers to an initial visit or contact with a client. (Chapter 7.8)
Advanced directives: Written instruction, such as a living will or durable power of attorney for health care, recognized under state law, relating to the provision of health care when the individual is incapacitated. (Chapter 5.6)
Advocacy: The act or process of pleading for, supporting, or recommending a cause or course of action. Advocacy may be for persons (whether an individual, group, population, or society) or for an issue, such as potable water or global health. (Chapter 6.2, Chapter 10.2)
Affordable Care Act (ACA): Legislation enacted in 2010 to increase consumers’ access to health care coverage and protect them from insurance practices that restrict care or significantly increase the cost of care. (Chapter 8.2)
ANA’s Standards of Professional Practice: Standards describing a competent level of nursing practice as demonstrated by the critical thinking model known as the nursing process. The nursing process includes the components of assessment, diagnosis, outcomes identification, planning, implementation, and evaluation. (Chapter 1.1)
ANA’s Standards of Professional Performance: Standards describing a competent level of behavior in the professional nursing role, including activities related to ethics, advocacy, respectful and equitable practice, communication, collaboration, leadership, education, scholarly inquiry, quality of practice, professional practice evaluation, resource stewardship, and environmental health. (Chapter 1.1, Chapter 9.2)
Assault: Intentionally putting another person in reasonable apprehension of an imminent harmful or offensive contact. (Chapter 5.2)
Assignment: Routine care, activities, and procedures that are within the authorized scope of practice of the RN, LPN/VN, or routine functions of the assistive personnel. (Chapter 3.3)
Assistive personnel (AP): Any assistive personnel (formerly referred to as ‘‘unlicensed” assistive personnel [UAP]) trained to function in a supportive role, regardless of title, to whom a nursing responsibility may be delegated. This includes, but is not limited to, certified nursing assistants or aides (CNAs), patient-care technicians (PCTs), certified medical assistants (CMAs), certified medication aides, and home health aides. (Chapter 3.1)
Autonomy: The capacity to determine one’s own actions through independent choice, including demonstration of competence. (Chapter 6.2)
B
Battery: Intentional causation of harmful or offensive contact with another’s person without that person’s consent. (Chapter 5.2)
Beneficence: The bioethical principle of benefiting others by preventing harm, removing harmful conditions, or affirmatively acting to benefit another or others, often going beyond what is required by law. (Chapter 6.2)
Benner’s Novice to Expert Theory: A theory by Dr. Patricia Benner that explains how new hires develop skills and a holistic understanding of patient care over time, resulting from a combination of a strong educational foundation and thorough clinical experiences. Benner’s theory identifies five levels of nursing experience: novice, advanced beginner, competent, proficient, and expert. (Chapter 11.5)
Board of Nursing: The state-specific licensing and regulatory body that sets standards for safe nursing care and issues nursing licenses to qualified candidates, based on the Nurse Practice Act. (Chapter 1.1)
Brief: A short session to share a plan, discuss team formation, assign roles and responsibilities, establish expectations and climate, and anticipate outcomes and contingencies. (Chapter 7.6)
Budget: An estimate of revenue and expenses over a specified period of time, usually over a year. (Chapter 8.5)
Burnout: A condition manifested physically and psychologically with a loss of motivation. (Chapter 12.6)
C
Capacity: A functional determination that an individual is or is not capable of making a medical decision within a given situation. (Chapter 5.6)
Capital budgets: Budgets used to plan investments and upgrades to tangible assets that lose or gain value over time. Capital is something that can be touched, such as buildings or computers. (Chapter 8.5)
Change: The process of altering or replacing existing knowledge, skills, attitudes, systems, policies, or procedures. (Chapter 4.3)
Change agent: Anyone who has the skill and power to stimulate, facilitate, and coordinate the change effort. (Chapter 4.3)
Change management: Process of making changes in a deliberate, planned, and systematic manner. (Chapter 4.3)
Chronic conditions: Conditions that have a slow onset and may gradually worsen over time. (Chapter 2.3)
Civil law: Law focusing on the rights, responsibilities, and legal relationships between private citizens. (Chapter 5.2)
Clinical reasoning: “A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions.” (Chapter 2.4)
Closed-loop communication: A communication strategy used to ensure that information conveyed by the sender is heard by the receiver and completed. (Chapter 3.2, Chapter 7.5)
Code of ethics: A set of ethical principles established by a profession that is designed to govern decision-making and assist individuals to distinguish right from wrong. (Chapter 6.2)
Collective bargaining: Negotiation of wages and other conditions of employment by an organized body of employees. (Chapter 10.4)
Commission: Doing something a reasonable nurse would not have done. (Chapter 5.2)
Communication conflict: Occurs when there is a failure in the exchange of information. (Chapter 7.7)
Compassion fatigue: A state of chronic and continuous self-sacrifice and/or prolonged exposure to difficult situations that affect a health care professional’s physical, emotional, and spiritual well-being. (Chapter 12.6)
Competence: In a legal sense, the ability of an individual to participate in legal proceedings. A judge decides if an individual is “competent” or “incompetent.” (Chapter 5.6)
Confidentiality: The right of an individual to have personal, identifiable medical information kept private. (Chapter 5.2)
Consequentialism: An ethical theory used to determine whether or not an action is right by the consequences of the action. For example, most people agree that lying is wrong, but if telling a lie would help save a person’s life, consequentialism says it’s the right thing to do. (Chapter 6.2)
Constitutional law: The rights, privileges, and responsibilities established by the U.S. Constitution. For example, the right to privacy is a right established by the constitution. (Chapter 5.2)
Constructive feedback: Supportive feedback that offers solutions to areas of weakness. (Chapter 3.5)
Continuity of care: The use of information on past events and personal circumstances to make current care appropriate for each individual. (Chapter 7.8)
Contracts: Binding written, verbal, or implied agreements. (Chapter 5.2)
Co-pay: A flat fee the consumer pays at the time of receiving a health care service as a part of their health care plan. (Chapter 8.3)
Core measures: National standards of care and treatment processes for common conditions. These processes are proven to reduce complications and lead to better patient outcomes. (Chapter 9.2)
Core values: The foundational ideals that guide the organization’s actions and decision-making processes. (Chapter 4.2)
Crime: A type of behavior defined by Congress or state legislature as deserving of punishment. (Chapter 5.2)
Criminal law: A system of laws concerned with punishment of individuals who commit crimes. (Chapter 5.2)
Critical thinking: A broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.” (Chapter 2.4)
Cultural diversity: A term used to describe cultural differences among clients, family members, and health care team members. (Chapter 7.3)
Cultural humility: A humble and respectful attitude toward individuals of other cultures that pushes one to challenge their own cultural biases, realize they cannot possibly know everything about other cultures, and approach learning about other cultures as a lifelong goal and process. (Chapter 6.2, Chapter 7.3)
Culture of safety: Organizational culture that embraces error reporting by employees with the goal of identifying systemic causes of problems that can be addressed to improve patient safety. Just Culture is a component of a culture of safety. (Chapter 4.2, Chapter 5.5))
CURE hierarchy: A strategy for prioritization based on identifying “critical” needs, “urgent” needs, “routine” needs, and “extras.” (Chapter 2.3)
CUS statements: Assertive statements that are well-recognized by all staff across a health care agency as implementation of the two-challenge rule. These assertive statements are “I am Concerned – I am Uncomfortable – This is a Safety issue!” (Chapter 7.6)
D
Data cues: Pieces of significant clinical information that direct the nurse toward a potential clinical concern or a change in condition. (Chapter 2.3)
Debrief: An informal information exchange session designed to improve team performance and effectiveness through reinforcement of positive behaviors and reflecting on lessons learned after a significant event occurs. (Chapter 7.6)
Deductible: The amount of money a consumer pays for health care before their insurance plan pays anything. These amounts generally apply per person per calendar year. (Chapter 8.3)
Defamation of character: An act of making negative, malicious, and false remarks about another person to damage their reputation. Slander is spoken defamation and libel is written defamation. (Chapter 5.2)
Defendants: The parties named in a lawsuit. (Chapter 5.2)
Delegated responsibility: A nursing activity, skill, or procedure that is transferred from a license nurse to a delegatee. (Chapter 3.4)
Delegatee: An RN, LPN/VN, or AP who is delegated a nursing responsibility by either an APRN, RN, or LPN/VN who is competent to perform the task and verbally accepts the responsibility. (Chapter 3.4)
Delegation: Allowing a delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role but in which they have received additional training. (Chapter 3.4)
Delegator: An APRN, RN, or LPN/VN who requests a specially trained delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role. (Chapter 3.4)
Deontology: An ethical theory based on rules that distinguish right from wrong. (Chapter 6.2)
DESC: A tool used to help resolve conflict. DESC is a mnemonic that stands for Describe the specific situation or behavior and provide concrete data, Express how the situation makes you feel/what your concerns are using “I” messages, Suggest other alternatives and seek agreement, and Consequences are stated in terms of impact on established team goals while striving for consensus. (Chapter 7.6)
Discharge: The completion of care and services in a health care facility and the client is sent home (or to another health care facility). (Chapter 7.8)
Durable power of attorney for healthcare (DPOAHC): Person chosen to speak on one’s behalf if one becomes incapacitated. (Chapter 5.6)
Duty of reasonable care: Legal obligations nurses have to their patients to adhere to current standards of practice. (Chapter 5.2)
E
Economics: The study of how society makes decisions about its limited resources. (Chapter 8.1)
Ethical conflict: Occurs when individuals or groups have fundamentally different beliefs and values. (Chapter 7.7)
Ethical dilemma: Conflict resulting from competing values that requires a decision to be made from equally desirable or undesirable options. (Chapter 6.3)
Ethical principles: Principles used to define nurses’ moral duties and aid in ethical analysis and decision-making. Foundational ethical principles include autonomy (self-determination), beneficence (do good), nonmaleficence (do no harm), justice (fairness), and veracity (tell the truth). (Chapter 6.2)
Ethics: A system of moral principles that a society uses to identify right from wrong. (Chapter 6.2)
Ethics committee: A formal committee established by a health care organization to problem-solve ethical dilemmas. (Chapter 6.4)
Evidence-Based Practice (EBP): A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and patient, family, group, community, and population preferences and values. (Chapter 8.4, Chapter 9.4, Chapter 10.7)
Expected conditions: Conditions that are likely to occur or anticipated in the course of an illness, disease, or injury. (Chapter 2.3)
Extrinsic factors: External elements that impact health care costs. (Chapter 8.2)
F
False imprisonment: An act of restraining another person causing that person to be confined in a bounded area. Restraints can be physical, verbal, or chemical. (Chapter 5.2)
Feedback: Information is provided to a team member for the purpose of improving team performance. Feedback should be timely, respectful, specific, directed towards improvement, and considerate. (Chapter 7.6)
Felonies: Serious crimes that cause the perpetrator to be imprisoned for greater than one year. (Chapter 5.2)
Fidelity: An ethical principle meaning keeping promises. (Chapter 6.2)
Five rights of delegation: Right task, right circumstance, right person, right directions and communication, and right supervision and evaluation. (Chapter 3.4)
Floating: An agency strategy that asks nurses to temporarily work on a different unit to help cover a short-staffed shift. (Chapter 8.5)
Followership: The upward influence of individuals on their leaders and their teams. (Chapter 4.2)
Fraud: An act of deceiving an individual for personal gain. (Chapter 5.2)
G
Goal conflict: Happens when the objectives of individuals or groups are incompatible. (Chapter 7.7)
Good Samaritan Law: State law providing protections against negligence claims to individuals who render aid to people experiencing medical emergencies outside of clinical environments. (Chapter 5.2)
Grievance process: A process for resolving disagreements between employees and management. (Chapter 10.4)
H
Handoff reports: A transfer and acceptance of patient care responsibility achieved through effective communication. It is a real-time process of passing patient specific information from one caregiver to another, or from one team of caregivers to another, for the purpose of ensuring the continuity and safety of the patient’s care. (Chapter 7.5)
Harmful stress: Stress (also referred to as “distress”) not adequately self-managed resulting in physical, mental, and behavioral consequences. (Chapter 12.3)
Health care disparity: Differences in access to health care and insurance coverage. (Chapter 8.4)
Health disparities: Differences in health outcomes that result from social determinants of health (SDOH). (Chapter 8.4)
Horizontal aggression: Hostile behavior among one’s peers. (Chapter 7.7)
Huddle: A brief meeting during a shift to reestablish situational awareness, reinforce plans already in place, and adjust the teamwork plan as needed. (Chapter 7.6)
I
I’M SAFE: A tool used to assess one’s own safety status, as well as that of other team members in their ability to provide safe patient care. It is a mnemonic standing for personal safety risks as a result of Illness, Medication, Stress, Alcohol and Drugs, Fatigue, and Eating and Elimination. (Chapter 7.6)
Informatics: Using information and technology to communicate, manage knowledge, mitigate error, and support decision-making. This allows members of the health care team to share, store, and analyze health-related information. (Chapter 9.3, Chapter 10.7)
Informed consent: The fundamental right of a client to accept or reject health care. (Chapter 5.6)
Infractions: Minor offenses, such as speeding tickets, that result in fines but not jail time. (Chapter 5.2)
Institutional liability: When the healthcare institution (e.g., hospital, clinic) is held responsible for the actions of its employees or for failing to implement adequate policies and procedures to prevent harm. (Chapter 5.3)
Institutional Review Board (IRB): A group that has been formally designated to review and monitor biomedical research involving human subjects. (Chapter 6.4)
Intentional tort: An act of commission with the intent of harming or causing damage to another person. Examples of intentional torts include assault, battery, false imprisonment, slander, libel, and breach of privacy or client confidentiality. (Chapter 5.2)
Interdisciplinary care conferences: Meetings where interprofessional team members professionally collaborate, share their expertise, and plan collaborative interventions to meet client needs. (Chapter 7.8)
Interprofessional collaborative practice: Multiple health workers from different professional backgrounds working together with patients, families, caregivers, and communities to deliver the highest quality of care. (Chapter 7.1)
Intrinsic factors: Factors that are inherent to the characteristics and needs of the population. (Chapter 8.2)
I-PASS: A mnemonic used as a structured communication tool among interprofessional team members. I-PASS stands for Illness severity, Patient summary, Action list, Situation awareness, and Synthesis by the receiver. (Chapter 7.5)
ISBARR: A mnemonic for the components to include when communicating with another health care team member: Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat back. (Chapter 7.5, Chapter 10.7)
J
Just Culture: A culture where people feel safe raising questions and concerns and report safety events in an environment that emphasizes a nonpunitive response to errors and near misses. Clear lines are drawn between human error, at-risk, and reckless employee behaviors. (Chapter 4.2)
Justice: A moral obligation to act on the basis of equality and equity and a standard linked to fairness for all in society. (Chapter 6.2)
L
Laws: Rules and regulations created by society and enforced by courts, statutes, and/or professional licensure boards. (Chapter 5.2)
Leadership: The art of establishing direction and influencing and motivating others to achieve their maximum potential to accomplish tasks, objectives, or projects. (Chapter 4.2)
Libel: Written defamation. (Chapter 5.2)
Licensure: The process by which a State Board of Nursing (SBON) grants permission to an individual to engage in nursing practice after verifying the applicant has attained the competency necessary to perform the scope of practice of a registered nurse (RN). The SBON verifies three components:
- Verification of graduation from an approved prelicensure RN nursing education program
- Verification of successful completion of NCLEX-RN examination
- A criminal background check (in some states) (Chapter 11.3)
Living will: A type of advance directive in which an individual identifies what treatments they would like to receive or refuse if they become incapacitated and unable to make decisions.
M
Magnet® Recognition Program: An organizational credential that recognizes quality patient outcomes, nursing excellence, and innovations in professional nursing practice. (Chapter 10.4)
Malpractice: A specific term used for negligence committed by a professional with a license. (Chapter 5.2)
Management: Roles that focus on tasks such as planning, organizing, prioritizing, budgeting, staffing, coordinating, and reporting. (Chapter 4.2)
Mandatory overtime: A requirement by agencies for nurses to stay and care for patients beyond their scheduled shift when short staffing occurs. (Chapter 8.5)
Maslow’s Hierarchy of Needs: Prioritization strategies often reflect the foundational elements of physiological needs and safety and progress toward higher levels. (Chapter 2.3)
Medicaid: A joint federal and state program covering groups of eligible individuals, such as low-income families, qualified pregnant women and children, and individuals receiving Supplemental Security Income (SSI). States may choose to cover additional groups, such as individuals receiving home and community-based services and children in foster care who are not otherwise eligible. (Chapter 8.3)
Medicare: A federal health insurance program used by people aged 65 and older, younger individuals with permanent disabilities, and people with end-stage renal disease requiring dialysis or a kidney transplant. (Chapter 8.3)
Meta-analysis: A type of nursing research (also referred to as a “systematic review”) that compares the results of independent research studies asking similar research questions. This research often collects both quantitative and qualitative data to provide a well-rounded evaluation by providing both objective and subjective outcomes. (Chapter 9.4)
Mindfulness: Awareness that arises through paying attention, being on purpose and in the present moment, and being nonjudgmental. (Chapter 12.6)
Misdemeanors: Less serious crimes resulting in fines and/or imprisonment for less than one year. (Chapter 5.2)
Mission statement: An organization’s statement that describes how the organization will fulfill its vision and establishes a common course of action for future endeavors. (Chapter 4.2)
Moral conflict: Feelings occurring when an individual is uncertain about what values or principles should be applied to an ethical issue. (Chapter 6.3)
Moral courage: The willingness of an individual to speak out and do what is right in the face of forces that would lead us to act in some other way. (Chapter 6.3)
Moral distress: Feelings occurring when correct ethical action is identified but the individual feels constrained by competing values of an organization or other individuals. (Chapter 6.3)
Moral injury: The distressing psychological, behavioral, social, and sometimes spiritual aftermath of exposure to events that contradict deeply held moral beliefs and expectations. (Chapter 6.3)
Morality: Personal values, character, or conduct of individuals or groups within communities and societies. (Chapter 6.2)
Moral outrage: Feelings occurring when an individual witnesses immoral acts or practices they feel powerless to change. (Chapter 6.3)
Morals: The prevailing standards of behavior of a society that enable people to live cooperatively in groups. (Chapter 6.2)
Mutual support: The ability to anticipate and support team members’ needs through accurate knowledge about their responsibilities and workload. (Chapter 7.6)
N
NCLEX-RN: The exam that nursing graduates must pass successfully to obtain their nursing license and become a registered nurse. (Chapter 11.2)
NCLEX-RN Test Plan: A concise summary of the content and scope of the NCLEX that serves as an excellent guide for preparing for the exam. These plans are updated every three years based on surveys of newly licensed registered nurses to ensure the NCLEX questions reflect fair, comprehensive, current, and entry-level nursing competency. (Chapter 11.2)
Negligence: The failure to exercise the ordinary care a reasonable person would use in similar circumstances. Wisconsin civil jury instruction states, “A person is not using ordinary care and is negligent, if the person, without intending to do harm, does something (or fails to do something) that a reasonable person would recognize as creating an unreasonable risk of injury or damage to a person or property.” (Chapter 5.2)
Nonmaleficence: The bioethical principle that specifies a duty to do no harm and balances avoidable harm with benefits of good achieved. (Chapter 6.2)
Normal stress: Stress (also referred to as “eustress”) that does not have lasting consequences and is successfully managed by the individual who is experiencing it. (Chapter 12.3)
Nurse Licensure Compact (NLC): State legislation that allows nurses to practice in other NLC states with their original state’s nursing license without having to obtain additional licenses, contingent upon remaining a resident of that state. (Chapter 11.3)
Nurse Practice Act: Law enacted by a state’s legislature that defines the scope of nursing practice and establishes regulations for nursing practice within that state. (Chapter 1.1)
Nurse residency programs: A transition process that provides additional professional development for newly licensed nurses. These programs vary from institution to institution, but many start around the time the new graduate ends their orientation with a preceptor and continue to provide routine support throughout the year. (Chapter 11.5)
Nursing: Integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in recognition of the connection of all humanity.” (Chapter 1.1)
Nursing informatics: The science and practice integrating nursing, its information and knowledge, with information and communication technologies to promote the health of people, families, and communities worldwide. (Chapter 9.3)
Nursing process: Includes the components of assessment, diagnosis, outcomes identification, planning, implementation, and evaluation. (Chapter 1.1)
Nursing research: The systematic inquiry designed to develop knowledge about issues of importance to the nursing profession. The purpose of nursing research is to advance nursing practice through the discovery of new information. It is also used to provide scholarly evidence regarding improved patient outcomes resulting from nursing interventions. (Chapter 9.4)
Nursing team members: Advanced practice registered nurses (APRN), registered nurses (RN), licensed practical/vocational nurses (LPN/VN), and assistive personnel (AP). (Chapter 3.1)
O
Off with benefits: An agency staffing strategy when a nurse is not needed for their scheduled shift. The nurse does not typically receive an hourly wage and is not expected to report to work, but they still accrue benefits such as insurance and paid time off. (Chapter 8.5)
Omission: Not doing something a reasonable nurse would have done. (Chapter 5.2)
On call: An agency staffing strategy when a nurse is not immediately needed for their scheduled shift. They may have options to stay at work and complete work-related education or stay home. (Chapter 8.5)
Operating budgets: Budgets including personnel costs and annual facility operating costs. (Chapter 8.5)
Organizational culture: The implicit values and beliefs that reflect the norms and traditions of an organization. An organization’s vision, mission, and values statements are the foundation of organizational culture. (Chapter 4.2)
Orientation: A structured transition process when hired into a new position that may last from one to four months but can be longer depending on the specialty (e.g., Intensive Care or Labor and Delivery). Orientation is based on the new nurse’s demonstration and completion of competencies. During this time the novice RN will work with a preceptor to experience all the aspects of the role. (Chapter 11.5)
P
Paternalism: The interference by the state or an individual with another person, defended by the claim that the person interfered with will be better off or protected from harm. (Chapter 6.2)
Patient-centered care: The patient is the source of control and full partner in providing compassionate and coordinated care based on respect for patient’s preferences, values, and needs. (Chapter 10.7)
Patient safety goals: Guidelines specific to organizations accredited by The Joint Commission that focus on problems in health care safety and ways to solve them. (Chapter 9.2)
Pay for Performance: A reimbursement model, also known as value-based payment, that attaches financial incentives based on the performance of health care agencies and providers. (Chapter 8.4)
Peer-reviewed: Scholarly journal articles that have been reviewed independently by at least two other academic experts in the same field as the author(s) to ensure accuracy and quality. (Chapter 9.4)
Personality conflict: Arises from differences in individual temperaments, attitudes, and behaviors. (Chapter 7.7)
Plaintiff: The person bringing the lawsuit. (Chapter 5.2)
Policy: An expected course of action set by an agency. (Chapter 1.1)
Portfolio: A compilation of materials showcasing examples of previous work demonstrating one’s skills, qualifications, education, training, and experience. (Chapter 11.4)
Preceptors: Experienced and competent RNs who serve as a role model and a resource to a newly hired nurse. These nurses have the knowledge, skills, and the ability to coach the new RN into the nursing role and answer questions while also evaluating a new hire’s performance and providing feedback for improvement. (Chapter 11.5)
Primary source: An original study or report of an experiment or clinical problem. The evidence is typically written and published by the individual(s) conducting the research and includes a literature review, description of the research design, statistical analysis of the data, and discussion regarding the implications of the results. (Chapter 9.4)
Private law: Laws that govern the relationships between private entities. (Chapter 5.2)
Procedure: An official way of completing a task. (Chapter 1.1)
Protected Health Information (PHI): Individually identifiable health information and includes demographic data related to the individual’s past, present, or future physical or mental health or condition; the provision of health care to the individual; and the past, present, or future payment for the provision of health care to the individual. (Chapter 5.2)
Protocol: A detailed, written plan for performing a regimen of therapy. (Chapter 1.1)
Public law: Law regulating relations of individuals with the government or institutions. (Chapter 5.2)
Q
Qualitative studies: A type of study that provides subjective data, often focusing on the perception or experience of the participants. Data is collected through observations and open-ended questions and often referred to as experimental data. Data is interpreted by developing themes in participants’ views and observations. (Chapter 9.4)
Quality: The degree to which nursing services for health care consumers, families, groups, communities, and populations increase the likelihood of desirable outcomes and are consistent with evolving nursing knowledge. (Chapter 9.2)
Quality Improvement (QI): A systematic process using measurable data to improve health care services and the overall health status of patients. The QI process includes the steps of Plan, Do, Study, and Act. (Chapter 9.3, Chapter 10.7)
Quantitative studies: A type of study that provides objective data by using number values to explain outcomes. Researchers can use statistical analysis to determine strength of the findings, as well as identify correlations. (Chapter 9.4)
R
Ratio-based staffing models: A staffing model used to make patient assignments in terms of one nurse caring for a set number of patients. (Chapter 2.3)
Resiliency training: Educational sessions that foster feelings of mindfulness and sensitivity to self and cultivate professional development techniques that contribute to long-term engagement in the profession. (Chapter 12.7)
Resource stewardship: Using appropriate resources to plan, provide, and sustain evidence-based nursing services that are safe, effective, financially responsible, and used judiciously. (Chapter 8.6)
Resume: A document that highlights one’s background, education, skills, and accomplishments to potential employers. (Chapter 11.4)
Risk problem: A nursing problem that reflects that a patient may experience a problem but does not currently have signs reflecting the problem is actively occurring. (Chapter 2.3)
Role conflict: Arises when individuals have multiple, often conflicting, expectations associated with their roles. (Chapter 7.7)
S
Scope of practice: Procedures, actions, and processes that a health care practitioner is permitted to undertake in keeping with the terms of their professional license. (Chapter 3.3)
Secondary source: Evidence is written by an author who gathers existing data provided from research completed by another individual. This type of source analyzes and reports on findings from other research projects and may interpret findings or draw conclusions. In nursing research these sources are typically published as a systematic review and meta-analysis. (Chapter 9.4)
Self-care: Actions that individuals take to maintain health of oneself. (Chapter 12.6)
Shared governance: A shared leadership model between management and employees working together to achieve common goals. (Chapter 10.4)
Shared mental model: The actions of a team leader that ensure all team members have situation awareness and are “on the same page” as situations evolve on the unit. (Chapter 7.6)
Situation awareness: The awareness of a team member knowing what is going on around them. (Chapter 7.6)
Situation monitoring: The process of continually scanning and assessing the situation to gain and maintain an understanding of what is going on around you. (Chapter 7.6)
Slander: Spoken defamation. (Chapter 5.2)
Social Determinants of Health (SDOH): Conditions in the places where people live, learn, work, and play, such as unstable housing, low-income areas, unsafe neighborhoods, or substandard education that affect a wide range of health risks and outcomes. (Chapter 8.2, Chapter 8.4, Chapter 10.4)
Standards of Professional Nursing Practice: Authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently. (Chapter 1.1)
Statutory law: Written laws enacted by the federal or state legislature. For example, the Nurse Practice Act in each state is an example of statutory law that is enacted by the state government. (Chapter 5.2)
STEP tool: A situation monitoring tool used to know what is going on with you, your patients, your team, and your environment. STEP stands for Status of the patients, Team members, Environment, and Progress Toward Goal. (Chapter 7.6)
Student liability: When the student nurse is held responsible for their own actions that cause harm to patients or violate protocols. (Chapter 5.3)
Supervision: Appropriate monitoring of the delegated activity, evaluation of patient outcomes, and follow-up with the delegatee at the completion of the activity. (Chapter 3.4)
Supervisory liability: When a clinical supervisor or preceptor is held responsible for the actions of the student nurse or for failing to properly supervise them. (Chapter 5.3)
Systems leadership: A set of skills used to catalyze, enable, and support the process of systems-level change that focuses on the individual, the community, and the system. (Chapter 4.2)
Systems theory: The concept that systems do not function in isolation but rather there is an interdependence that exists between their parts. Systems theory assumes that most individuals strive to do good work but are affected by diverse influences within the system. (Chapter 4.2)
T
Team nursing: A common staffing pattern that uses a combination of Registered Nurses (RNs), Licensed Practical/Vocational Nurses (LPN/VNs), and Assistive Personnel (AP) to care for a group of patients. (Chapter 8.5)
*eamSTEPPS® (Team Strategies and Tools to Enhance Performance and Patient Safety): An evidence-based framework to improve client safety through effective communication in health care environments consisting of four core competencies: communication, leadership, situation monitoring, and mutual support. (Chapter 7.6, Chapter 10.7)
Teamwork and collaboration: Functioning effectively within nursing and interprofessional teams, fostering open communication, mutual respect, and shared decision-making to achieve quality patient care. (Chapter 10.7)
Temporary permit: A permit issued by the State Board of Nursing (SBON) that allows the applicant to practice practical nursing under the direct supervision of a registered nurse until their RN license is granted. (Chapter 11.3)
Time estimation: A prioritization strategy including the review of planned tasks and allocation of time believed to be required to complete each task. (Chapter 2.5)
Time scarcity: A feeling of racing against a clock that is continually working against you. (Chapter 2.2)
Titrate: Making adjustments to medication dosage per an established protocol to obtain a desired therapeutic outcome. (Chapter 3.3)
Tort: An act of commission or omission that causes injury or harm to another person for which the courts impose liability. In the context of torts, “injury” describes the invasion of any legal right, whereas “harm” describes a loss or detriment the individual suffers. Torts are classified as intentional or unintentional. (Chapter 5.2)
Two-challenge rule: A strategy for advocating for patient safety that includes a team member assertively voicing their concern at least two times to ensure that it has been heard by the decision-maker. (Chapter 7.6)
U
Unexpected conditions: Conditions that are not likely to occur in the normal progression of an illness, disease, or injury. (Chapter 2.3)
Unintentional tort: Acts of omission (not doing something a person has a responsibility to do) or inadvertently doing something causing unintended accidents leading to injury, property damage, or financial loss. Examples of unintentional torts impacting nurses include negligence and malpractice. (Chapter 5.2)
Utilitarianism: A type of consequentialism that determines whether or not actions are right based on their consequences, with the standard being achieving the greatest good for the greatest number of people. (Chapter 6.2)
Utilization review: An investigation by insurance agencies and other health care funders on services performed by doctors, nurses, and other health care team members to ensure money is not wasted covering things that are unnecessary for proper treatment or are inefficient. This review also allows organizations to objectively measure how effectively health care services and resources are being used to best meet their patients’ needs. (Chapter 9.3)
V
Values: Individual beliefs that motivate people to act one way or another and serve as a guide for behavior. (Chapter 6.2)
Values statement: The organization’s established values that support its vision and mission and provide strategic guidelines for decision-making, both internally and externally, by members of the organization. (Chapter 4.2)
Veracity: An ethical principle meaning telling the truth. (Chapter 6.2)
Vision statement: An organization’s statement that defines why the organization exists, describes how the organization is unique and different from similar organizations, and specifies what the organization is striving to be. (Chapter 4.2)
W
Whistleblower: A person who exposes any kind of information or activity that is deemed illegal, unethical, or not correct within an organization. (Chapter 10.5)
A feeling of racing against a clock that is continually working against you.
A feeling of racing against a clock that is continually working against you.

