9.3 Natural Defenses Against Infection
Open Resources for Nursing (Open RN)
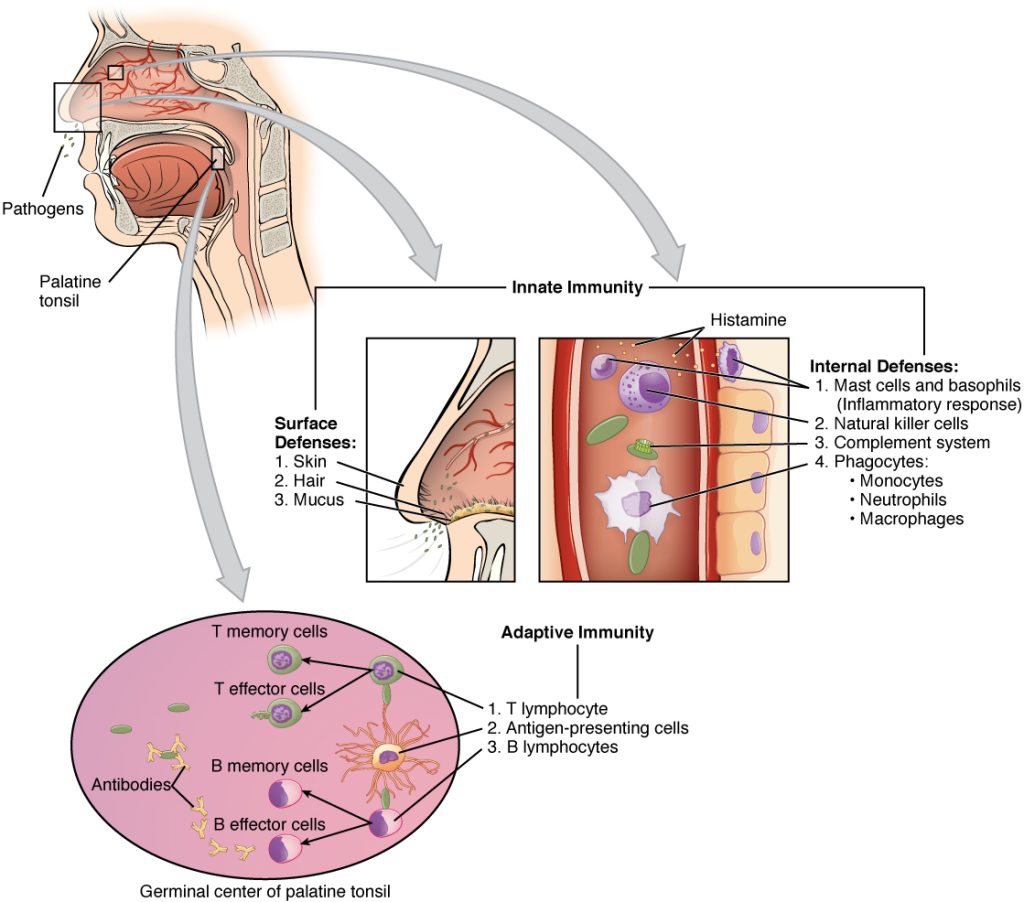
There are two basic ways the body defends against pathogens: nonspecific innate immunity and specific adaptive immunity.
Nonspecific Innate Immunity
Nonspecific innate immunity is a system of defenses in the body that targets invading pathogens in a nonspecific manner. It is called “innate” because it is present from the moment we are born. Nonspecific innate immunity includes physical defenses, chemical defenses, and cellular defenses.[1]
Physical Defenses
Physical defenses are the body’s most basic form of defense against infection. They include physical barriers to microbes, such as skin and mucous membranes, as well as mechanical defenses that physically remove microbes and debris from areas of the body where they might cause harm or infection. In addition, a person’s microbiome provides physical protection against disease as normal flora compete with pathogens for nutrients and cellular-binding sites.[2]
Skin
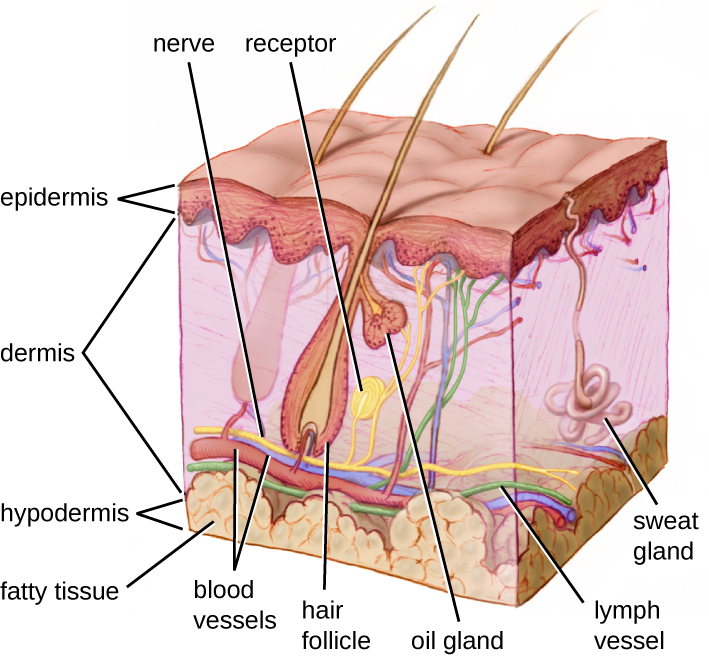
One of the body’s most important physical barriers is the skin barrier, which is composed of three layers of closely packed cells. See Figure 9.5[3] for an illustration of the layers of skin. The topmost layer of skin called the epidermis consists of cells that are packed with keratin. Keratin makes the skin’s surface mechanically tough and resistant to degradation by bacteria. Infections can occur when the skin barrier is broken, allowing the entry of opportunistic pathogens that infect the skin tissue surrounding the wound and possibly spread to deeper tissues.[4]
Mucus Membranes
The mucous membranes lining the nose, mouth, lungs, and urinary and digestive tracts provide another nonspecific barrier against potential pathogens. Mucous membranes consist of a layer of epithelial cells bound by tight junctions. The epithelial cells secrete a moist, sticky substance called mucous. Mucous covers and protects the fragile cell layers beneath it and also traps debris, including microbes. Mucus secretions also contain antimicrobial peptides.[5]
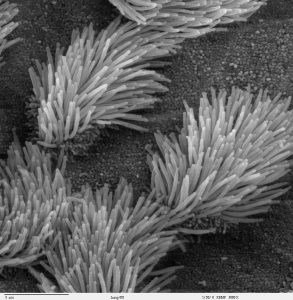
In many regions of the body, mechanical actions flush mucus (along with trapped or dead microbes) out of the body or away from potential sites of infection. For example, in the respiratory system, inhalation can bring microbes, dust, mold spores, and other small airborne debris into the body. This debris becomes trapped in the mucus lining the respiratory tract. The epithelial cells lining the upper parts of the respiratory tract have hair-like appendages known as cilia. Movement of the cilia propels debris-laden mucus out and away from the lungs. The expelled mucus is then swallowed and destroyed in the stomach, coughed up, or sneezed out. This system of removal is often called the mucociliary escalator. Disruption of the mucociliary escalator by the damaging effects of smoking can lead to increased colonization of bacteria in the lower respiratory tract and frequent infections, which highlights the importance of this physical barrier to host defenses.[6] See Figure 9.6[7] for an image of a magnified mucociliary escalator.
Like the respiratory tract, the digestive tract is a portal of entry through which microbes enter the body, and the mucous membranes lining the digestive tract provide a nonspecific physical barrier against ingested microbes. The intestinal tract is lined with epithelial cells, interspersed with mucus-secreting goblet cells. This mucus mixes with material received from the stomach, trapping foodborne microbes and debris, and is moved forward through the digestive tract via the mechanical action of peristalsis. Peristalsis refers to involuntary contraction and relaxation of the muscles of the intestine, creating wave-like movements that push digested content forward in the digestive tract.[8] For this reason, feces can contain microorganisms that can cause the spread of infection, making it essential to perform good hand hygiene to prevent transmission of disease through the fecal-oral route.
Endothelia
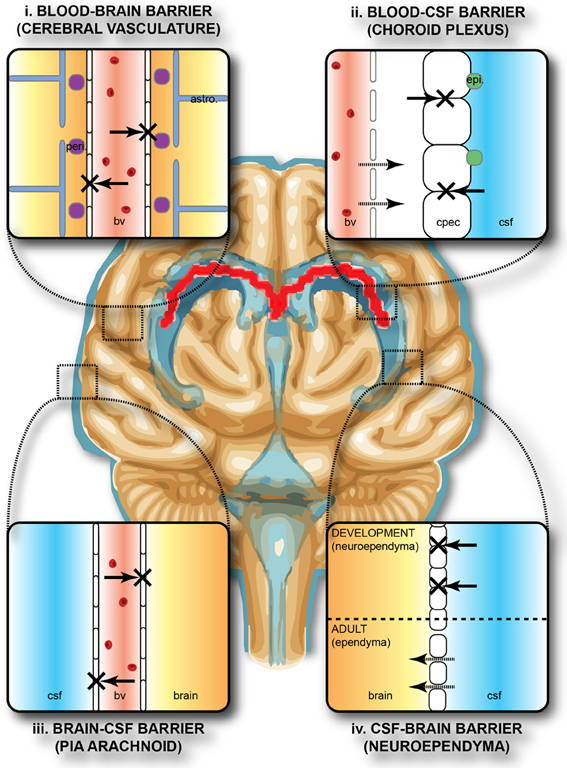
The epithelial cells lining the urogenital tract, blood vessels, lymphatic vessels, and other tissues are known as endothelia. These tightly packed cells provide an effective frontline barrier against invaders. The endothelia of the blood-brain barrier, for example, protects the central nervous system (CNS) from microorganisms. Infection of the CNS can quickly lead to serious and often fatal inflammation. The protection of the blood-brain barrier keeps the cerebrospinal fluid that surrounds the brain and spinal cord sterile.[9] See Figure 9.7[10] for an illustration of the blood-brain barrier.
Mechanical Defenses
In addition to physical barriers that keep microbes out, the body has several mechanical defenses that physically remove pathogens from the body and prevent them from taking up residence. For example, the flushing action of urine and tears serves to carry microbes away from the body. The flushing action of urine is responsible for the normally sterile environment of the urinary tract. The eyes have additional physical barriers and mechanical mechanisms for preventing infections. The eyelashes and eyelids prevent dust and airborne microorganisms from reaching the surface of the eye. Any microbes or debris that make it past these physical barriers is flushed out by the mechanical action of blinking, which bathes the eye in tears, washing debris away.[11] See Figure 9.8[12] for an image of an infant’s eyelashes that prevent dust from reaching the surface of the eye.

Microbiome
Normal flora that contributes to an individual’s microbiome serve as an important first-line defense against invading pathogens. Through their occupation of cellular binding sites and competition for available nutrients, normal flora prevents the early steps of pathogen attachment and proliferation required for the establishment of an infection. For example, in the vagina, normal flora competes with opportunistic pathogens like Candida albicans. This competition prevents yeast infection by limiting the availability of nutrients and inhibiting the growth of Candida, keeping its population in check. Similar competitions occur between normal flora and potential pathogens on the skin, in the upper respiratory tract, and in the gastrointestinal tract.[13]
The importance of the normal flora in host defenses is highlighted by a person’s increased susceptibility to infectious diseases when their microbiome is disrupted or eliminated. For example, treatment with antibiotics can significantly deplete the normal flora of the gastrointestinal tract, providing an advantage for pathogenic bacteria such as Clostridium difficile (C-diff) to colonize and cause diarrheal infection. Diarrhea caused by C-diff can be severe and potentially lethal. In fact, a recent strategy for treating recurrent C-diff infections is fecal transplantation that involves the transfer of fecal material from a donor into the intestines of the client as a method of restoring their normal flora.[14]
Chemical Defenses
In addition to physical defenses, our nonspecific innate immune system uses several chemical mediators that inhibit microbial invaders. The term chemical mediators encompass a wide array of substances found in various fluids and tissues throughout the body. For example, sebaceous glands in the dermis secrete an oil called sebum that is released onto the skin surface through hair follicles. Sebum provides an additional layer of defense by helping seal off the pore of the hair follicle and preventing bacteria on the skin’s surface from invading sweat glands and surrounding tissue. Environmental factors can affect these chemical defenses of the skin. For example, low humidity in the winter makes the skin drier and more susceptible to pathogens normally inhibited by the skin’s low pH. Application of skin moisturizer restores moisture and essential oils to the skin and helps prevent dry skin from becoming infected.[15]
Examples of other chemical defenses are enzymes, pH level, and chemical mediators. Enzymes in saliva and the digestive tract eliminate most pathogens that manage to survive the acidic environment of the stomach. In the urinary tract, the slight acidity of urine inhibits the growth of potential pathogens in the urinary tract. The respiratory tract also uses various chemical mediators in the nasal passages, trachea, and lungs that have antibacterial properties.[16]
Plasma Protein Mediators
In addition to physical, mechanical, and chemical defenses, there are also nonspecific innate immune factors in plasma, the fluid portion of blood, such as acute-phase proteins, complement proteins, and cytokines. These plasma protein mediators contribute to the inflammatory response.[17]
An example of an acute-phase protein is C-reactive protein. High levels of C-reactive protein indicate inflammation caused by a serious infection or other medical condition.[18]
Complement proteins are always present in the blood and tissue fluids, allowing them to be activated quickly. They aid in the destruction of pathogens by piercing their outer membranes (cell lysis) or by making them more attractive to phagocytic cells such as macrophages.[19]
Cytokines are proteins that affect interaction and communication between cells. When a pathogen enters the body, the first immune cell to notice the pathogen is like the conductor of an orchestra. That cell directs all the other immune cells by creating and sending out messages (cytokines) to the rest of the organs or cells in the body to respond to and initiate inflammation. Too many cytokines can have a negative effect and result in what’s known as a cytokine storm.[20],[21] A cytokine storm is a severe immune reaction in which the body releases too many cytokines into the blood too quickly. A cytokine storm can occur as a result of an infection, autoimmune condition, or other disease. Signs and symptoms include high fever, inflammation, severe fatigue, and nausea. A cytokine storm can be severe or life-threatening and lead to multiple organ failure. For example, many COVID-19 complications and deaths were caused by a cytokine storm.[22],[23]
Inflammation
Inflammation is a response triggered by a cascade of chemical mediators and occurs when pathogens successfully breach the nonspecific innate immune system or when an injury occurs. Although inflammation is often perceived as a negative consequence of injury or disease, it is a necessary process that recruits cellular defenses needed to eliminate pathogens, remove damaged and dead cells, and initiate repair mechanisms. Excessive inflammation, however, can result in local tissue damage, and in severe cases, such as sepsis, it can become deadly.[24]
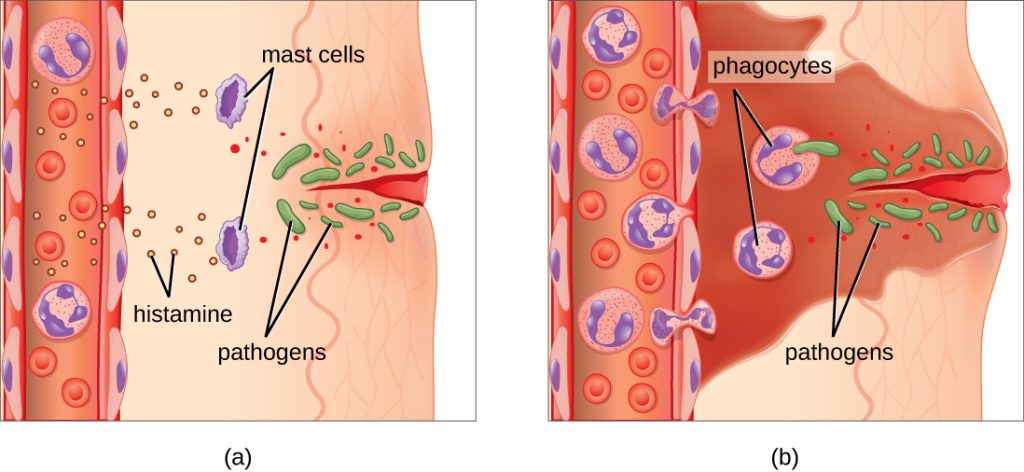
An immediate response to tissue injury is acute inflammation. Vasoconstriction occurs to minimize blood loss if injury has occurred. Vasoconstriction is followed by vasodilation with increased permeability of the blood vessels due to the release of histamine by mast cells. Histamine contributes to the five observable signs of the inflammatory response: erythema (redness), edema (swelling), heat, pain, and altered function. It is also associated with an influx of phagocytes at the site of injury and/or infection. See Figure 9.9[25] for an illustration of the inflammatory response, with (a) demonstrating when mast cells detect injury to nearby cells and release histamine, initiating an inflammatory response and (b) illustrating where histamine increases blood flow to the wound site and the associated increased vascular permeability allows fluid, proteins, phagocytes, and other immune cells to enter infected tissue. These events result in the swelling and reddening of the injured site. The increased blood flow to the injured site causes it to feel warm. Inflammation is also associated with pain due to these events stimulating nerve pain receptors in the tissue. Increasing numbers of neutrophils are then recruited to the area to fight pathogens. As the fight rages on, white blood cells are recruited to the area, and pus forms from the accumulation of neutrophils, dead cells, tissue fluids, and lymph. Typically, after a few days, macrophages clear out this pus.[26] During injury, if this nonspecific inflammatory process does not successfully kill the pathogens, infection occurs.
Fever
A fever is part of the inflammatory response that extends beyond the site of infection and affects the entire body, resulting in an overall increase in body temperature. Like other forms of inflammation, a fever enhances the nonspecific innate immune defenses by stimulating white blood cells to kill pathogens. The rise in body temperature also inhibits the growth of many pathogens. During fever, the client’s skin may appear pale due to vasoconstriction of the blood vessels in the skin to divert blood flow away from extremities, minimize the loss of heat, and raise the body’s core temperature. The hypothalamus also stimulates the shivering of muscles to generate heat and raise the core temperature.[27]
A low-level fever is thought to help an individual overcome an illness. However, in some instances, this immune response can be too strong, causing tissue and organ damage and, in severe cases, even death. For example, Staphylococcus aureus and Streptococcus pyogenes are capable of producing superantigens that cause toxic shock syndrome and scarlet fever, respectively. Both of these conditions are associated with extremely high fevers in excess of 42 °C (108 °F) that must be managed to prevent tissue injury and death.[28]
When a fever breaks, the hypothalamus stimulates vasodilation, resulting in a return of blood flow to the skin and a subsequent release of heat from the body. The hypothalamus also stimulates sweating, which cools the skin as the sweat evaporates.[29]
Specific Adaptive Immunity
Now that we have discussed several nonspecific innate defenses against a pathogen, let’s discuss specific adaptive immunity. Specific adaptive immunity is the immune response that is activated when the nonspecific innate immune response is insufficient to control an infection. There are two types of adaptive responses: the cell-mediated immune response, which is carried out by T cells, and the humoral immune response, which is controlled by activated B cells and antibodies.[30]
B cells mature in the bone marrow. B cells make Y-shaped proteins called antibodies that are specific to each pathogen and lock onto its surface and mark it for destruction by other immune cells. The five classes of antibodies are IgG, IgM, IgA, IgD, and IgE. They also turn into memory B cells. Memory B cells are stored and released in the event a specific antigen reappears in the future. This allows the immune system to mount a quick defense because of the previously created memory B cells.[31]
T cells mature in the thymus. T cells are categorized into three classes: helper T cells, regulatory T cells, and cytotoxic T cells. Helper T cells stimulate B cells to make antibodies and help killer cells develop. Killer T cells directly kill cells that have already been infected by a pathogen. T cells also use cytokines as messenger molecules to send chemical instructions to the rest of the immune system to ramp up its response.[32]
Specific adaptive immunity also creates memory cells for each specific pathogen that provides the host with long-term protection from reinfection with that pathogen. On reexposure, these memory cells facilitate an efficient and quick immune response. For example, when an individual recovers from chicken pox, the body develops a memory of the varicella-zoster virus that will specifically protect it from reinfection if it is exposed to the virus again. Vaccines are administered with the purpose of enhancing a person’s specific adaptive immunity.[33]
See Figure 9.10[34] for an illustration of innate immunity and specific adaptive immunity that occur in response to a pathogen entering the body through the nose.
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- “OSC_Microbio_17_02_Skin.jpg” by OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology@9.8/pages/17-1-physical-defenses. ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- The Integrative HMP (iHMP) Research Network Consortium. (2019). Proctor, L. M., Creasy, H. H., et. al. The integrative human microbiome project. Nature, 569, 641–648. https://doi.org/10.1038/s41586-019-1238-8 ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- “Bronchiolar_epithelium_3_-_SEM.jpg” by Charles Daghlian is licensed by CC0 ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- “Protective_barriers_of_the_brain.jpg” by Stolp H. B., Liddelow S. A., Sá-Pereira I., Dziegielewska K. M., & Saunders N. R. is licensed under CC BY-SA 3.0 ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- “Eyelashes_of_a_2-month-old_baby_boy.png” by Karthik.yerramilly is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Concepts of Biology - 1st Canadian Edition by Molnar & Gair and is licensed under CC BY 4.0. ↵
- Sproston, N. R., & Ashworth, J. J. (2018). Role of c-reactive protein at sites of inflammation and infection. Frontiers in Immunology, 9, 754. https://doi.org/10.3389/fimmu.2018.00754 ↵
- Complement. (2018). In Britannica. https://www.britannica.com/science/complement-immune-system-component ↵
- Arango Duque, G., & Descoteaux, A. (2014). Macrophage cytokines: Involvement in immunity and infectious diseases. Frontiers in Immunology, 5, 491. https://doi.org/10.3389/fimmu.2014.00491 ↵
- National Cancer Institute (n.d.) NCI dictionary of cancer terms. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/cytokine-storm ↵
- Hojyo, S., Uchida, M., Tanaka, K., et al. (2020). How COVID-19 induces cytokine storm with high mortality. Inflammation and Regeneration, 40(37). https://doi.org/10.1186/s41232-020-00146-3 ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- “OSC_Microbio_17_06_Erythema.jpg” by OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/17-5-inflammation-and-fever. ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- “2211_Cooperation_Between_Innate_and_Immune_Responses.jpg” by OpenStax is licensed under CC BY 3.0. ↵
A system of defenses in the body that targets invading pathogens in a nonspecific manner that is present from the moment we are born.
Exercises
Please utilize the "Suite of Patients" and suggested prompt activities below to engage your students in knowledge application associated with the various learning units throughout the text.
Unit Patients
- 56-year-old female admitted yesterday afternoon with nausea/vomiting and right-sided upper abdominal pain that increases after eating. Has had two stools since admit and vomiting stopped after dose of Zofran in ER. Had ERCP yesterday afternoon for dilated biliary duct. She is scheduled for OR this morning for cholecystectomy. Only medical history is depression and surgical history of C-section x2. She does not take any medications routinely at home. She is accompanied by her 17-year-old daughter.
- 65-year-old male hospitalized three days prior with malaise, cough, cachexia, and 30 pounds of unintentional weight loss over past six weeks. He has a remote history of alcohol and drug abuse but has been sober for more than 10 years. He was diagnosed with acquired immunodeficiency syndrome (AIDS), pneumocystis pneumonia (PCP), and oral candidiasis. He is being treated with IV fluids, IV Bactrim, and IV fluconazole. He is divorced and has one daughter. His ex-wife came to the hospital yesterday to visit. He has no visitors currently. The patient is very quiet and withdrawn.
- 32-year-old nonbinary person, who was transferred from the ICU this morning after being extubated. Patient was admitted five days prior with COVID. Patient cannot have visitors due to COVID status. Continues four liters nasal cannula oxygen.
- 29-year-old female with cellulitis on right arm from infiltration from heroine injection. Her wife is present, along with their 4-year-old son. She had an I&D yesterday and may need to have repeat procedure tomorrow. Currently on IV antibiotics.
- 52-year-old male with gangrene of fourth toe from having a nail through sole of shoe. Patient has a history of uncontrolled diabetes, hypertension (HTN), peripheral vascular disease (PVD), chronic kidney disease (CKD) stage 2, and peripheral neuropathy. Receiving IV antibiotics and scheduled for toe amputation tomorrow. He has no visitors.
- 82-year-old female who had elective right hip replacement for uncontrolled hip pain and degenerative joint disease (DJD). She has a history of type 2 diabetes mellitus on metformin and dietary restrictions; previous hysterectomy, osteoporosis, carpal tunnel repair, and rheumatoid arthritis, which she takes oral methotrexate to control. She has a son who is visiting. Expected to be discharged today.
- 68-year-old male awaiting nursing home placement following admission for hepatic encephalopathy from alcoholism. He was medically cleared last week but is a registered sex offender and has yet to find placement. He has an activated power of attorney, who is a state-appointed guardian. He continues to get up without calling, makes inappropriate remarks to staff, and had a fall three days prior. Other history is bipolar disorder, alcohol abuse, type 2 diabetic, chronic kidney disease stage 3, and hypertension.
- 19-year-old female admitted for what is presumed Benadryl overdose last evening. On room air, needs to have 1:1 sitter present. Patient is not responding to questions; does not know if this is accidental overdose or intentional. History of previous intentional overdose, depression, and anxiety. Dad is present and demanding to know if a toxicology screen was completed and what it showed.
- 61-year-old male admitted six days prior with confusion. Was found by a neighbor wandering. Works at the local gas station. Initial work up shows what appears to be lung cancer with brain metastasis. Patient does not have a power of attorney. He is not married and is estranged from his son. Neighbor who found him is a friend and is willing to become guardian. History from neighbor and review of medical records shows a history of smoking. Neighbor says it does appear he has lost weight recently but hadn’t mentioned other concerns when he had talked to him about two weeks ago. In the process of paperwork to be completed for guardianship. Patient had been aspirating when eating; decision to start nasal gastric feed was made yesterday by ethics committee. Awaiting guardianship for further decision on biopsy for confirmed diagnoses and decision to proceed with treatment or switch to hospice care.
- 45-year-old female admitted last evening who is short of breath, dizzy, light-headed, and gastrointestinal bleed. Esophagogastroduodenoscopy (EGD) scheduled for this morning. If negative, will need prep for colonoscopy and then colonoscopy tomorrow. Patient has little medical history except had recently returned from an overseas trip and had chest and back pain about two days after returning. Had been found to have a saddle PE and was hospitalized for five days on heparin drip and discharged home with coumadin about a week prior. Patient continued to have back and intermittent chest pain and had been taking ibuprofen 1-2 times daily since discharge. Husband brought her in last night when she was found to have a Hgb of 6.2. Husband is furious that no one told them she should not be taking ibuprofen on previous discharge.
- 64-year-old male with BKA for nonhealing diabetic ulcer; scheduled to go to rehab today if bed becomes available. Lives alone in a second floor, low-income apartment without an elevator. Does not have any visitors.
- 32-year-old male admitted 15 days prior for newly diagnosed AML. Received induction therapy starting 13 days ago. Patient is at nadir, will need 1 unit of PRBCs for a Hgb of 6.2 today and a unit of platelets for a platelet count of 8. Patient has had fevers for the past two days and is currently receiving vancomycin and cefepime. Also, on prophylactic acyclovir and fluconazole. Patient has mucositis and is on PCA pump and receiving TPN and diet as tolerated (magic mouthwash before meals).
- Cachexic 25-year-old female with history of cystic fibrosis. Admitted for CF exacerbation overnight. Eats during the day and is tube fed overnight. Admitted for extensive pulmonary toileting, IV antibiotics (tobramycin and cefuroxime), continued home respiratory treatments. Patient also needs to have nutrition recommendations reviewed during this hospitalization. She is here with her boyfriend. The boyfriend also has two school-aged children who would like to visit.
- 78-year-old male with a history of HTN and hypothyroid. Admitted two days prior to abdominal pain and nausea/vomiting. Had a colectomy yesterday for perforated diverticulitis. Patient is NPO and has NG tube in place. Had nausea overnight. His wife is expected to visit later today; she went home after return from OR yesterday.
- 89-year-old female admitted from nursing home yesterday with increased confusion. Has a history of dementia, HTN, type 2 diabetes, and dysphagia. Was found to have a UTI. Started on IV Levaquin; awaiting urine cultures. Expected discharge tomorrow. She has been trying to get up frequently overnight. No family present. Needs 1:1 supervision for all feedings.
- 82-year-old man admitted with COPD exacerbation and is on 2 L of home oxygen baseline. Oxygen saturation was 78% on arrival and has not been able to do ADLs because of shortness of breath. Has CAD, HTN, and PAD. Lives in a duplex with his granddaughter who lives on the other side. His granddaughter called yesterday.
- 68-year-old male who is morbidly obese and admitted two days prior for shortness of breath with CHF. Patient is on IV bumex and is down 25 pounds since admit. He has a history of HTN, CAD, post CABG, and CKD stage 2. Expected discharge today.
- 36-year-old female admitted for excessive uterine bleeding four days prior. Newly diagnosed with uterine cancer. Patient had open hysterectomy, oophorectomy, salpingotomy, and lymph node biopsy. Had diagnostics, port placement, and staging over the past three days. Expected discharge today. Her husband is here with their 16-month-old daughter. The husband has been very inattentive during this hospitalization and has expected her to watch their daughter over the last couple days and even left to go for lunch yesterday while leaving the daughter in the room.
- 68-year-old male with history of stage 3 CKD and admitted with AKI on CKD yesterday. Patient has had nausea and vomiting for past 36 hours; baseline creatinine of 1.8 and was 4.6 on admit. Has been given fluid hydration and is down to 3.2 this morning.
- Bed open.
- It is “ortho day” in the OR. There are three patients scheduled. 1 is a 54-year-old male with bilateral knee replacement (0800 surgery time) and scheduled for observation admit. 68-year-old women with right knee (1100 surgery time) and expected to be discharged. 78-year-old male with hip replacement (1300 OR time) and scheduled for observation admit.
- 72-year-old female waiting for a bed in the emergency room. Arrived overnight with hypoxia, cough, SOB. Positive for influenza.
Classroom Activity Ideas:
Prioritization
Put students in groups and a patient assignment (4-5 patients). Have them identify who they would see first, second, etc. Why?
Students will review all of the patients on the unit. Have them identify those who are most critical and why.
Add in “changes of conditions” – Patient with AKI on CKD morning labs showed a K of 7.2 and Na of 118. AML spikes temp of 103.6 and develops hives and chest tightness when PRBCs are infusing. Newly diagnosed uterine cancer patient states she is concerned going home with her husband because she feels the abuse is going to get worse now that she is sick.
Classroom Activity Ideas:
Delegation/Supervision
Different staffing assignments: 5 RNs/2 CNAs; 4 RNS, 2 LPNs, 2 CNAs; charge nurse/no change nurse. Have students identify appropriate assignments, tasks for delegation, etc.
Consider different types of acute care units – would you organize assignments differently?
Classroom Activity Ideas:
Legal
Develop a scenario in which one patient is upset about not being taught about ibuprofen. Consider the legal implications associated with the lack of education.
How would a student address the father who wants to get information on daughter who overdosed?
Can a 17-year-old daughter be at the hospital without another guardian?
Classroom Activity Ideas:
Economics
Talk about isolation/PPE use and staffing ratios.
Have students utilize a couple different staffing tools to see acuity score.
Classroom Activity Ideas:
Quality/Evidence-Based Practice
Have students look up EBP guideline on one of their patients in their assignment (e.g., when to transfuse with blood and platelets for AML patient, ERCP prior to cholecystectomy, etc.).
Classroom Activity Ideas:
Ethical Practice
Patient who is waiting guardianship placement - diagnosed with new brain tumor.
Classroom Activity Ideas:
Managing the Nursing Team
Talk about the ways a charge nurse, nurse manager, and RN work with these patients.
Have each team assigned a new patient (post op, one in ED) with different methods of assigning – choosing who the new patient for the day would be, assigning at start of shift, and during the day.
Have one of the nurses refuse a new patient.
Classroom Activity Ideas:
Collaborating with Multidisciplinary Team
With your assigned patients, whom would you interact with during the day (e.g., PT, OT, ST, provider, lab, case management)?
Classroom Activity Ideas:
Advocacy
What community agencies might you recommend to the patients with whom you are working?
How would you work with a patient (e.g., the hip patient #6) who doesn’t feel comfortable being discharged today?
A response triggered by a cascade of chemical mediators that occur when pathogens successfully breach the nonspecific physical defenses of the immune system or when an injury occurs.
The immune response that is activated when the nonspecific innate immune response is insufficient to control an infection.
Immune cells that mature in the bone marrow and produce antibodies.
Y proteins created by B cells that are specific to each pathogen and lock onto its surface and mark it for destruction by other immune cells.
Immune cells that mature in the thymus.

