9.3 Measuring and Improving Quality
Open Resources for Nursing (Open RN)
Now that we have discussed the various ways that quality health care is defined, let’s discuss how quality care is measured, evaluated, and improved.
Utilization Review
Thinking back to value-based reimbursement models discussed in the “Health Care Economics” chapter, recall how health care agencies are reimbursed from Medicare, Medicaid, and private insurance based on their quality performance measures. A utilization review is an investigation of health care services performed by doctors, nurses, and other health care team members to ensure money is not wasted covering unnecessary or inefficient expenditures for proper treatment. Utilization review also allows organizations to objectively measure how their health care services and resources are being used to best meet their patients’ needs. Information from patients’ medical records is analyzed, along with patient demographics, to evaluate resource allocation, efficiency, and quality of health promotion initiatives.[1] See Figure 9.3[2] for an illustration of utilization review related to costs.

Using Informatics to Promote Quality
Utilization review relies on the collection of meaningful data from health records to determine if quality metrics are being met. Informatics refers to using information and technology to communicate, manage knowledge, mitigate error, and support decision-making.[3] Informatics allows members of the health care team to share, store, and analyze health-related information. Nurses have an important role in informatics. Nursing informatics is the science and practice of integrating nursing knowledge with information and communication technologies to promote the health of people, families, and communities worldwide.[4] It is a nursing specialty with certification available from the ANCC. See Figure 9.4[5] for an artistic rendition of informatics.

These are several benefits of using informatics in health care[6]:
- Improvement of Patient Safety: Informatics allows for up-to-date information sharing by both the patient and members of the health care team. Using informatics can help to reduce the occurrence of medication errors, as well as monitor patient side effects and overall health status. For example, barcode scanning has reduced medication errors by ensuring the correct dose is administered to the correct patient at the correct time.
- Reduction of Delays in Care: Some health care informatics systems allow for direct communication between health care team members and patients. The ability to ask and answer questions without needing to schedule an office appointment promotes the ability for care to be delivered efficiently in a cost-effective manner.
- Reduction of Waste: The use of informatics to share information between care team members reduces waste associated with duplication of tests or exams when more than one provider is on the care team. Additionally, patients can request their records be shared with health providers from other health organizations, which reduces duplication and unnecessary spending across the nation.
- Promotion of Patient-Centered Care: Many informatics systems have “patient portal” options where the patient and/or designated personnel are able to be active participants in the care planning and health promotion processes. Informatics offers an inclusive environment for patients to communicate and share directly with their care team regardless of physical location and timing.
- Support of Quality Improvement: The continuous process of quality improvement requires the ability to collect and analyze data in a systematic and reliable manner. Using informatics provides members of the health care team a secure place to store data, as well as the ability to review in a timely manner.
Quality Indicators
The National Database of Nursing Quality Indicators (NDNQI) was developed as a national nursing database used to evaluate quality in nursing care. This database was purchased by Press Ganey in 2014. In collaboration with the American Nursing Association (ANA), the original NDNQI database established nurse-sensitive quality indicators such as these[7]:
- Nursing Care Hours Per Patient Day
- Hospital-Acquired Pressure Injuries
- RN Job Satisfaction
Nurses use quality indicators to support practice changes with evidence directly related to improved patient outcomes.
Quality Improvement
Quality Improvement (QI) is a systematic process using measurable data to improve health care services and the overall health status of patients.[8] QI is one of the competencies of the Quality and Safety Education (QSEN) project and defined as, “using data to monitor the outcomes of care processes and using improvement methods to design and test changes to continuously improve the quality and safety of health care systems.”[9]
The overall goal of the QI process is to improve the quality and safety of health care. The process of quality improvement is very similar to the nursing process, but its purpose is to answer these three main questions:
- What are we trying to accomplish?
- How will we know if a change is an improvement?
- What changes can we make that will result in an improvement?
See Figure 9.5[10] for an illustration of the quality improvement process.
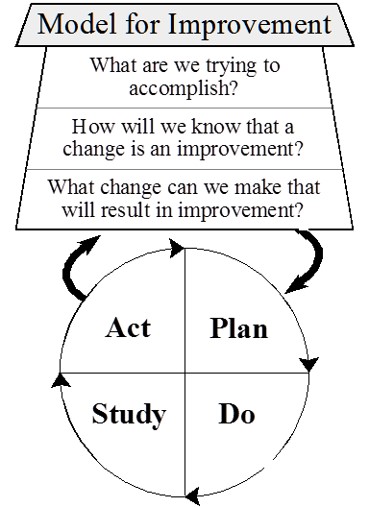
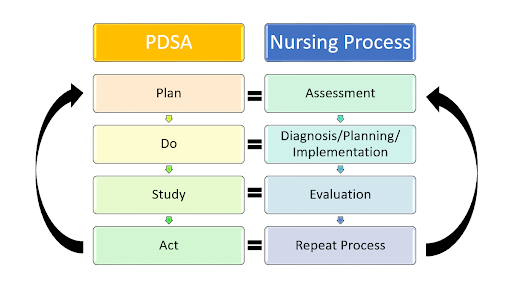
To answer these questions, QI is a continuous process in which a project is planned, interventions are implemented, data is collected, results are studied, and outcomes are evaluated. The process is repeated after additional planning. During the QI process, four key steps are used to evaluate current patient care and determine if changes are needed. These components are referred to as Plan, Do, Study, and Act:
- Plan: The first step in the QI process is to identify what you will be testing or focusing on and what will be measured. Similar to the nursing process where subjective and objective data are collected, the nurse determines what data will be needed during the QI process. The nurse also determines a timeline for the QI project, such as one year, including a specific framework for when data is collected and when it will be reviewed. For example, fall rates will decrease 10% in one year.
- Do: After the plan is determined, the nurse works with a health care team to implement the project and ensure data collection occurs.
- Study: During this phase, the nurse works with the health care team to review and analyze the data that was collected and determine if the outcomes were achieved or not.
- Act: In the fourth step of the QI process, the team discusses the outcomes. In this step the team identifies barriers, strengths, and weaknesses and then decides if additional changes are needed in nursing practice. The QI process is continuous, so the QI team uses outcome findings to continue the process of Plan, Do, Study, and Act to ensure safe, quality patient care.
PDSA Fall Rates Example
Reducing Patient Fall Rates
Objective: Decrease the patient fall rate in the hospital by 10% within one year.
Plan
- Identify the Focus: The QI project will focus on reducing patient falls in the hospital.
- Determine What to Measure: The primary metric will be the fall rate, calculated as the number of falls per 1,000 patient days.
- Collect Data: Baseline fall rates will be collected for the past year to understand current performance.
- Set Goals: Aim to reduce the fall rate by 10% within one year.
- Develop a Timeline:
- Initial Planning and Baseline Data Collection: Month 1
- Intervention Implementation: Months 2-4
- Data Collection and Monitoring: Months 2-12
- Initial Data Analysis: Month 6
- Final Data Analysis and Review: Month 12
Do
- Implement Interventions: Conduct fall prevention training sessions for all nursing staff. Ensure that patient rooms are free from clutter and that non-slip mats are in place. Install bed alarms and provide non-slip socks for patients. Implement a protocol for frequent rounding, especially for high-risk patients.
- Data Collection: Continuously collect data on fall incidents, including the circumstances of each fall.
Study
- Data Analysis: Review the fall rates monthly and compare them to the baseline data. Analyze trends and identify any patterns in the fall incidents. Determine if the interventions are associated with a reduction in fall rates.
2. Outcome Evaluation: Assess whether the goal of a 10% reduction in fall rates is being met. Identify any unexpected outcomes.
Act
- Discuss Outcomes: Hold meetings with the health care team to discuss the results. Identify barriers to successful implementation (e.g., lack of compliance with protocols, insufficient training). Recognize strengths (e.g., effective use of bed alarms, positive feedback from staff).
- Make Adjustments: If the fall rate has not decreased as expected, identify additional changes that might be needed (e.g., more frequent training, adjusting the rounding protocol). If successful, consider ways to further enhance the fall prevention program.
- Continuous Improvement: Use the findings to plan the next cycle of improvements. Set new goals based on the outcomes and continue the PDSA cycle to maintain and further improve patient safety
See Figure 9.6[11] for an illustration comparing the QI process to the nursing process.
It is important to note that quality improvement is different from nursing research. QI evaluates processes in place and determines if changes are needed, whereas the goal of research is to identify new innovations in nursing practice.[12]
Barriers to Quality Improvement
Barriers to quality improvement (QI) in health care organizations can be multifaceted, arising from a range of systemic, cultural, and practical challenges. One of the primary barriers is resistance to change among health care professionals. This resistance can stem from a lack of understanding of QI principles, fear of additional workload, or skepticism about the effectiveness of new practices. Overcoming this barrier requires robust education and training programs that highlight the benefits of QI initiatives and provide staff with the skills and knowledge needed to implement changes effectively. Also, having transparent conversations, discussing the process steps, and engaging staff questions are paramount.[13]
Another significant barrier is inadequate data management systems. Quality improvement relies heavily on accurate and timely data to identify areas for improvement, track progress, and measure outcomes. However, many health care organizations struggle with fragmented or outdated information systems that hinder data collection and analysis. Investing in modern, integrated health information technologies can facilitate better data management and support QI efforts. It also saves significant manpower and staff resources, allowing for more rapid identification of issues and trends.[14]
Resource constraints also pose a substantial challenge to quality improvement in health care. Financial limitations, staffing shortages, and limited time can impede the ability to implement and sustain QI initiatives. Organizations may find it difficult to allocate the necessary resources for training, process redesign, and continuous monitoring. Addressing this barrier often requires strategic planning, prioritization of QI projects, and seeking external funding or partnerships to support initiatives. Many organizations may have quality departments while others may utilize nursing staff to complete QI initiatives.[15]
Cultural factors in health care organizations can also impede quality improvement. Organizational culture that does not prioritize patient safety and continuous improvement can undermine QI efforts. This barrier can be addressed by fostering a culture of transparency, accountability, and collaboration. Leadership plays a crucial role in setting the tone and demonstrating a commitment to quality improvement. Engaging all levels of staff in QI processes and celebrating successes can help build a positive culture that supports ongoing improvement.[16]
Lastly, regulatory and policy constraints can limit the scope and flexibility of QI initiatives. Health care organizations operate within a complex regulatory environment that can sometimes create barriers to innovative practices. Navigating these regulations while attempting to implement QI can be challenging. Advocacy for policy changes that support QI, along with a thorough understanding of existing regulations, can help organizations find ways to work within or adapt to these constraints.[17]
Media Attributions
- informatics-1322241_1920
- Model_for_Improvement
- unnamed (1)
- Institute of Medicine (US) Committee on Utilization Management by Third Parties, Gray, B. H., & Field, M. J., (Eds.). (1989). Controlling costs and changing patient care? The role of utilization management. National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK235000 ↵
- “Analyzing_Financial_Data_(5099605109).jpg” by Dave Dugdale is licensed under CC BY-SA 2.0 ↵
- QSEN Institute. (n.d.). QSEN competencies: Quality improvement (QI). https://qsen.org/competencies/pre-licensure-ksas/#quality_improvement ↵
- AMIA. (n.d.). Informatics: Research and practice. https://amia.org/about-amia/why-informatics/informatics-research-and-practice ↵
- “informatics-1322241_1920.jpg” by mariojsantos at Pixabay.com is licensed under CC0 ↵
- Otokiti, A. (2019). Using informatics to improve healthcare quality. International Journal of Health Care Qual Assurance, 32(2), 425-430. https://doi.org/10.1108/ijhcqa-03-2018-0062 ↵
- Montalvo, I. (2007). The National Database of Nursing Quality Indicators (NDNQI). The Online Journal of Issues in Nursing, 12(3). https://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Volume122007/No3Sept07/NursingQualityIndicators.aspx ↵
- Study.com. (n.d.). What is economics? - Definition, history, timeline & importance [Video]. https://study.com/academy/lesson/what-is-economics-definition-history-timeline-importance.html ↵
- QSEN Institute. (n.d.). QSEN competencies: Quality improvement (QI). https://qsen.org/competencies/pre-licensure-ksas/#quality_improvement ↵
- “Model_for_Improvement.jpg” by Cliffnorman is licensed under CC BY-SA 4.0 ↵
- “Comparison_QI Process_Nursing Process.jpg” by Amy Tyznik, MPTC for Open RN is licensed under CC BY 4.0 ↵
- Agency for Healthcare Research and Quality. (2013, May). Module 4. Approaches to quality improvement. Practice facilitation handbook. https://www.ahrq.gov/ncepcr/tools/pf-handbook/mod4.html ↵
- Giannitrapani, K., Satija. A., Ganesh, A., Gamboa, R., Fereydooni, S., Hennings, T., Chandrashekaran, S., Mickelsen, J., DeNatale, M., Spruijt, O., Bhatnagar, S., & Lorenz, K. A. (2021). Barriers and facilitators of using quality improvement to foster locally initiated innovation in palliative care services in India. Journal of General Internal Medicine, 36(2), 366-373. https://doi.org/10.1007/s11606-020-06152-y. ↵
- Giannitrapani, K., Satija. A., Ganesh, A., Gamboa, R., Fereydooni, S., Hennings, T., Chandrashekaran, S., Mickelsen, J., DeNatale, M., Spruijt, O., Bhatnagar, S., Lorenz, K. A. (2021). Barriers and facilitators of using quality improvement to foster locally initiated innovation in palliative care services in India. Journal of General Internal Medicine, 36(2), 366-373. https://doi.org/ 10.1007/s11606-020-06152-y. ↵
- Alexander, C., Tschannen, D., Argetsinger, D., Hakim, H., & Milner, K. A. (2022). A qualitative study on barriers and facilitators of quality improvement engagement by frontline nurses and leaders. Journal of Nursing Management, 30(3), 694-701. https://doi.org/10.1111/jonm.13537. ↵
- Alexander, C., Tschannen, D., Argetsinger, D., Hakim, H., & Milner, K. A. (2022). A qualitative study on barriers and facilitators of quality improvement engagement by frontline nurses and leaders. Journal of Nursing Management, 30(3), 694-701. https://doi.org/10.1111/jonm.13537. ↵
- Alexander, C., Tschannen, D., Argetsinger, D., Hakim, H., & Milner, K. A. (2022). A qualitative study on barriers and facilitators of quality improvement engagement by frontline nurses and leaders. Journal of Nursing Management, 30(3), 694-701. htttps://doi.org/10.1111/jonm.13537. ↵
The cost of health care in the United States is higher than any other country in the world and has a significant financial impact on our economy.[1] U.S. health care spending grew 4.1 percent in 2022, reaching $ 4.5 trillion or $13,493 per person. Health care spending accounts for 17.3 percent of our Gross Domestic Product (GDP), the total value of goods produced and services provided annually.[2] See Figure 8.1[3] for a graph of health care cost as a percentage of GDP in the United States compared to other countries around the world.

Despite spending more money on health care than other high-income countries, the United States has some of the poorest health outcomes, such as the lowest life expectancy, the highest infant mortality rate, and a higher prevalence of chronic diseases.[4] The increasing costs of health care also have several negative impacts on society, employers, and individuals, including the following effects[5]:
- When the government spends more on health care, the national debt increases and funds available for other programs decrease.
- When people spend more on health care, they have less money to spend on other items.
- When health insurance is paid by employers, employees are paid less.
- When employers spend more on health care, the costs of their products and services increase. Jobs may be moved to countries with lower health care costs.
- An increasing number of people cannot afford health care insurance. When people without health care insurance receive health care, they often cannot pay for it. As a result of unpaid bills, this care is indirectly paid for by other people paying increased insurance premiums and taxes.
- People without health care insurance may not seek preventative care and develop a more costly, serious medical disorder that could have been prevented.
- Medical bills that are not covered by health insurance can cause bankruptcy.
There are several national trends affecting the cost of health care and related impacts, including the aging population, increased costs of medical technology, increased prescription medication cost, the Affordable Care Act, social determinants of health, etc. These trends can be further classified as intrinsic or extrinsic factors. Intrinsic factors related to increased health care costs are inherent to the characteristics and needs of the population. One significant intrinsic factor is the demographics of the population, such as age, gender, and overall health status. An aging population, for example, typically requires more medical care due to the prevalence of chronic conditions and the natural decline in health associated with aging. Another intrinsic factor is the demand for health care services. As people become more health-conscious, the demand for preventive care, regular check-ups, and advanced treatments rises, leading to increased overall health care spending. Additionally, the extent and nature of health insurance coverage play a crucial role. Comprehensive insurance plans often lead to higher utilization of health care services, as insured individuals are more likely to seek medical care, knowing that a significant portion of the costs will be covered by their insurance.
Extrinsic factors are external elements that impact health care costs. One of the most prominent extrinsic factors is the availability and adoption of medical technology. Advanced diagnostic tools, treatment methods, and surgical techniques can drive up costs due to their high development, implementation, and maintenance expenses. While these technologies can significantly improve patient outcomes, they also contribute to rising health care expenditures. Another critical extrinsic factor is the cost of prescription drugs. Pharmaceutical pricing strategies, including research and development costs, marketing, and profit margins, often lead to high prices for medications, especially for new and specialized drugs. Workforce costs are also a significant extrinsic factor. The salaries and benefits of health care professionals, including doctors, nurses, and administrative staff, constitute a substantial portion of health care expenses. These costs are influenced by factors such as education and training requirements, labor market conditions, and regulatory policies. Addressing these extrinsic factors requires strategic planning and policy interventions to balance cost containment with the quality and accessibility of health care services.
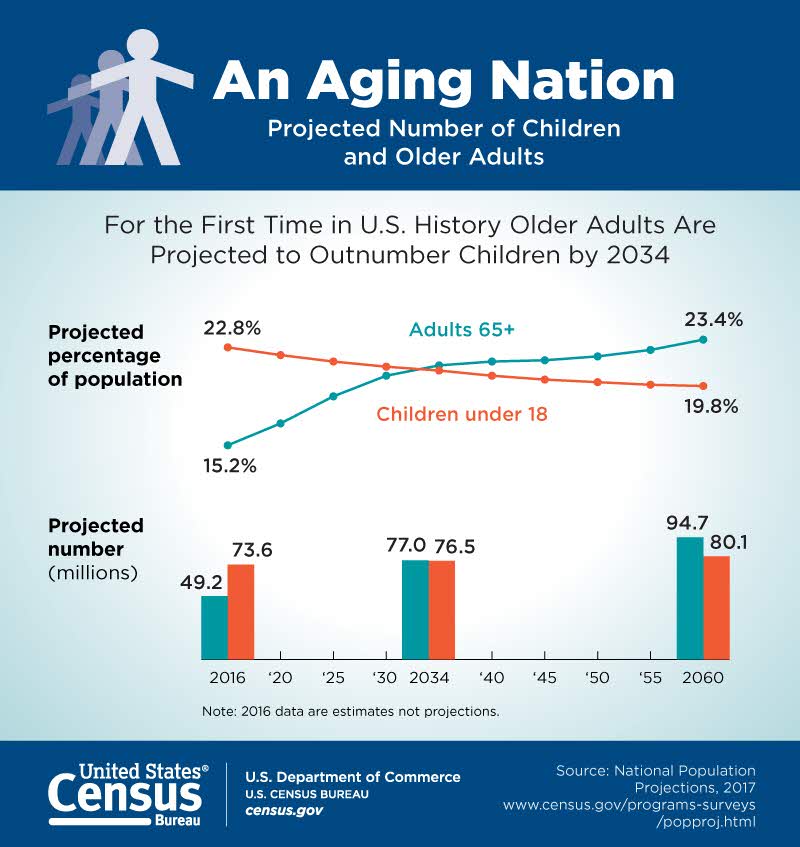
Aging Population
According to the Agency for Healthcare Research and Quality (AHRQ), the United States has a growing number of older adults (age 65 years or older) who are living longer than previous generations. It is anticipated that older adults will make up more than 20 percent of the U.S. population by 2030.[6] See Figure 8.2[7] for an illustration of the aging population from the U.S. Census Bureau. This change in demographics will result in increased national health care costs because older adults typically experience more chronic conditions than younger populations, requiring expensive specialty and long-term care.[8]
Increased Costs of Medical Technology
Highly visible medical technologies, such as organ transplantation, diagnostic imaging systems, and biotechnology products, attract both praise and blame. Evolving medical technologies may save lives and improve a client’s health status, but they are also viewed as a dominant cause of continued escalation of medical costs. Research suggests that medical technology accounts for about 10 to 40 percent of the increase in health care expenditures over time.[9] These costs also lead to further ethical dilemmas as decisions regarding what scarce resources are provided to which patients are made. See Figure 8.3[10] for an image of common technology used in health care.

Medical technologies, especially new ones, must justify their costs in a climate of competing claims on limited resources. Resource allocation follows American society's objective of cost effectiveness: if a new technology improves health outcomes at a lower cost than existing technologies, it should be adopted; otherwise, it should not.[11]
Increased Prescription Medication Costs
Retail prices for commonly-used prescription medications continue to increase twice as much as inflation, contributing to increased health care costs and making these life-sustaining medicines potentially unaffordable to many Americans. According to a recent AARP Rx Price Watch report, in 2020 prices for 260 commonly used medications increased 2.9 percent while the general rate of inflation was 1.3 percent.[12] For example, the cost of Symbicort, a medication used to treat asthma and COPD, increased 46 percent, from $2,940 to $4,282.[13] See Figure 8.4[14] for an illustration related to prescription medication costs.
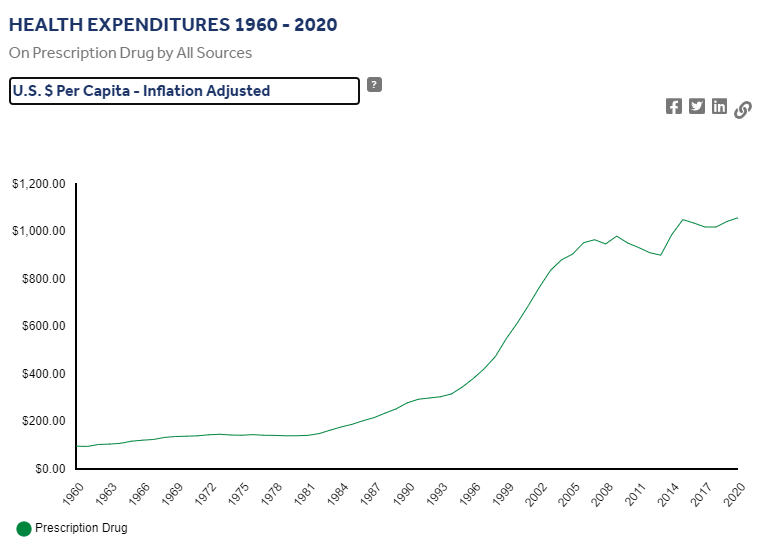
Although the majority of Americans have either public or private insurance that helps them pay for medications, increased medication prices result in higher health insurance premiums and higher taxpayer costs for the Medicare and Medicaid programs. Some insurance companies only cover approved formulary medications. As a result, national organizations like the American Association of Retired Persons (AARP) advocate for national policy changes, such as allowing Medicare to negotiate the prices of prescription medications with drug companies and allowing private insurance plans to have access to those lower prices.[15]
Many consumers find themselves tasked with the difficult decision of purchasing expensive medication or going without prescribed medication and paying for their families' housing and food. Nurses often become involved in case management activities when assisting clients to obtain medications they cannot afford. Nursing case management activities are discussed later in this chapter.
Affordable Care Act
The Patient Protection and Affordable Care Act (PPACA), also known as the Affordable Care Act (ACA) or Obamacare, was signed into law in 2010. The purpose of this legislation was to increase consumers' access to health care coverage and protect them from insurance practices that restricted care or significantly increased the cost of care. The ACA mandated health insurance coverage for employers and individuals. Employers were mandated to provide health care coverage based on the number of their employees, and individuals who were not covered through employer insurance plans were mandated to seek coverage through a newly created Marketplace. The Marketplace provides a central, website that offers three standard health insurance coverage levels to facilitate comparison by consumers. As a result of the ACA and associated Medicaid expansion, 32 million people had health care coverage in 2021.[16]
Key Provisions of the ACA
The ACA includes the following key provisions[17]:
- Insurers can no longer deny coverage or care for preexisting conditions like diabetes, asthma, and cancer.
- Young adults may remain on their parents’ insurance plans until they are 26 (even if they are married, financially independent, or not living with their parents).
- Health insurance plans cannot place annual or lifetime limits on coverage, except for nonessential exceptions, such as cosmetic procedures.
- Many preventive services must be provided, such as:
- Well-child visits, flu shots, and other common vaccines
- Screening tests for blood pressure and diabetes
- Diagnostic screening tests, such mammograms and colonoscopies
- Counseling services related to mental health and substance use
The ACA also provides an avenue for consumers to appeal insurance companies’ denials for care or payment of services and restricts situations in which an insurance carrier may cancel a policy.
Challenges to the ACA
Although the ACA has significantly increased the number of Americans with health insurance coverage, it continues to be debated. Debates focus on increased taxes, increased insurance premiums, and some people’s belief that mandated coverage is governmental intrusion on an individual’s rights. The Affordable Care Act has been challenged three times without success. In 2012 the U. S. Supreme Court upheld mandated coverage as a constitutional exercise of Congress’ taxing powers because it could be interpreted as an individual’s choice to maintain health insurance or pay a tax. However, in 2017 Congress set the penalty for failing to comply with the mandate at zero dollars after multiple attempts to repeal and replace the ACA. In June 2021 the U.S. Supreme Court rejected a third major challenge regarding the constitutionality of the ACA. In a 7-to-2 decision, the U.S. Supreme Court upheld the ACA based on the judgment that the states who brought forth the case did not prove damage to citizens because the fines for not having health coverage had been eliminated since the original legislation was passed.[18]
What to Expect Next
Given the Supreme Court’s recent decision regarding the ACA, it is expected the current administration will continue to advocate for the ACA and work towards making ACA tax credits permanent. Congress is also actively debating other legislative proposals to reduce health care costs, such as medication pricing reform and expanding Medicare eligibility age and benefits.[19]
Social Determinants of Health
Social Determinants of Health (SDOH) are the conditions in the environments where people live, learn, work, and play that affect a wide range of outcomes. SDOH include health care access and quality, neighborhood and environment, social and community context, economic stability, and education access and quality. These conditions have a major impact on people’s health and well-being, ultimately affecting national health care costs.[20]
SDOH directly impact individuals' health behaviors, their access to routine health care, and development of chronic disease. Yet, the United States spends a significantly lower percentage of its gross domestic product (GDP) on social services as compared to similar countries with better health outcomes.[21]
Healthy People 2030, established by the U.S. Department of Health and Human Services, identifies public health priorities to help individuals, organizations, and communities across the United States improve health and well-being over the next decade by addressing SDOH. One of Healthy People 2030’s goals states, “Create social, physical, and economic environments that promote attaining the full potential for health and well-being for all.”[22] Nurses act in many ways to address these priorities as they advocate for individuals, families, and communities.
Maria's Journey Through the Health Care System
Maria, a 45-year-old woman, lives in a low-income neighborhood in a large urban area. She works two part-time jobs to support her family of four and has limited access to health care due to financial constraints and transportation issues. Maria has been diagnosed with type 2 diabetes, and her health care outcomes are significantly influenced by various Social Determinants of Health (SDOH).
Maria's low income and unstable employment contribute to her inability to afford healthy food, medications, and regular medical check-ups. This economic instability exacerbates her diabetes, as she often skips doses of her medication to save money and cannot afford nutritious meals that would help manage her condition. The constant stress of making ends meet and providing for her family leads to increased cortisol levels, which can negatively impact her blood sugar control.
- How can Maria's financial stress impact her ability to manage her diabetes effectively?
2. What programs or policies could be implemented to assist individuals like Maria in managing their health care costs?
Maria has limited knowledge about diabetes management due to a lack of education and access to health information. This impacts her ability to understand and implement lifestyle changes or adhere to treatment plans. With limited education, Maria struggles to find better-paying jobs that could provide health insurance and more financial stability.
3. In what ways can improved health literacy impact Maria's diabetes management?
4. What community resources could be made available to enhance health education for individuals in Maria's situation?
The availability of health care services in Maria’s neighborhood is limited, with long wait times and fewer specialists. This results in delayed diagnoses and treatments for her diabetes-related complications. Maria lacks comprehensive health insurance, making it difficult for her to access primary and specialist care. High out-of-pocket costs deter her from seeking regular medical attention.
5. How does the lack of accessible health care services affect Maria's long-term health outcomes?
6. What are some potential solutions to improve health care access in underserved areas?
Maria lives in a food desert with limited access to fresh fruits and vegetables. She often relies on inexpensive, processed foods that worsen her diabetes. Public transportation in Maria’s area is unreliable, making it challenging for her to attend medical appointments. This lack of transportation contributes to missed check-ups and unmanaged diabetes.
7. How does living in a food desert affect Maria's ability to manage her diabetes?
8. What transportation initiatives could help individuals like Maria access healthcare services more easily?
Maria has a limited social network and lacks support from friends and family, which is crucial for managing a chronic condition like diabetes. This isolation can lead to depression and further neglect of her health. Living in a high-crime area, Maria feels unsafe walking outside for exercise, which is essential for diabetes management. This sedentary lifestyle negatively affects her health outcomes.
9. How does a lack of social support contribute to Maria's health challenges?
10. What community programs or interventions could be implemented to enhance social support and safety in high-crime areas?

