9.3 Cardiovascular Assessment
Open Resources for Nursing (Open RN)
A thorough assessment of the heart provides valuable information about the function of a patient’s cardiovascular system. Understanding how to properly assess the cardiovascular system and identifying both normal and abnormal assessment findings will allow the nurse to provide quality, safe care to the patient.
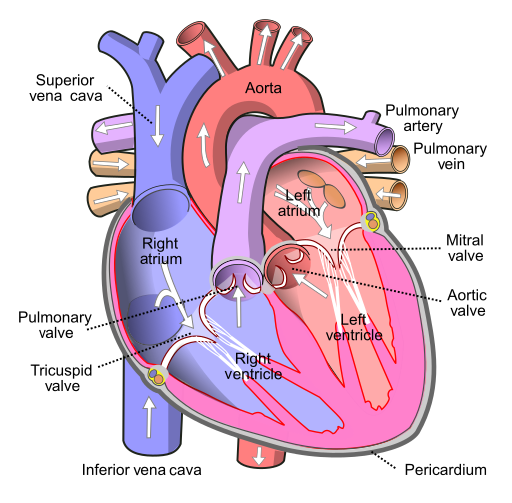
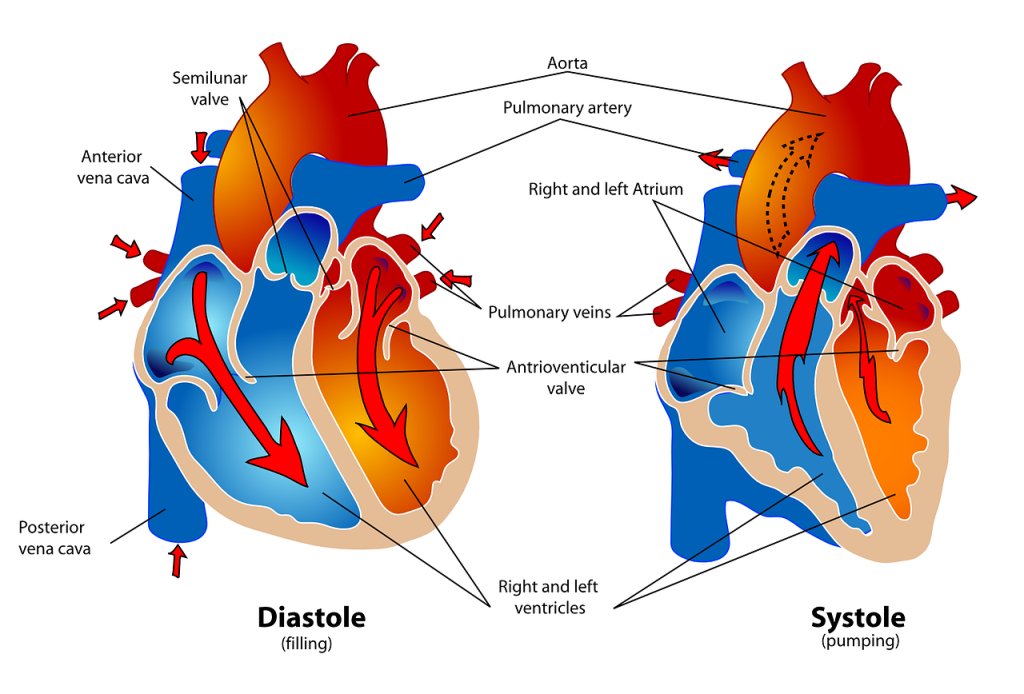
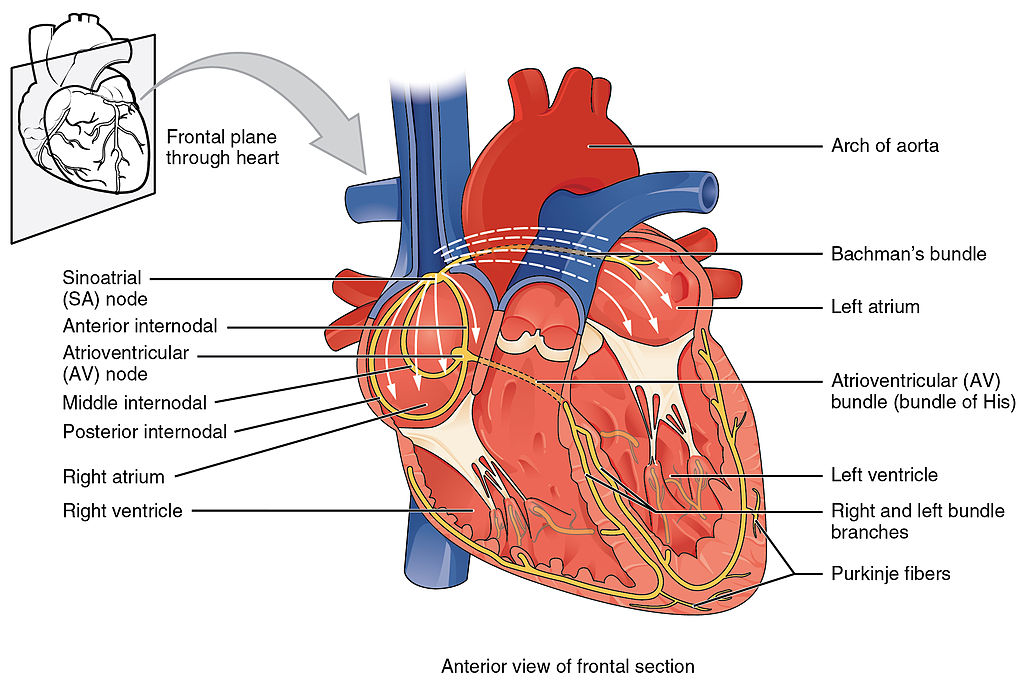
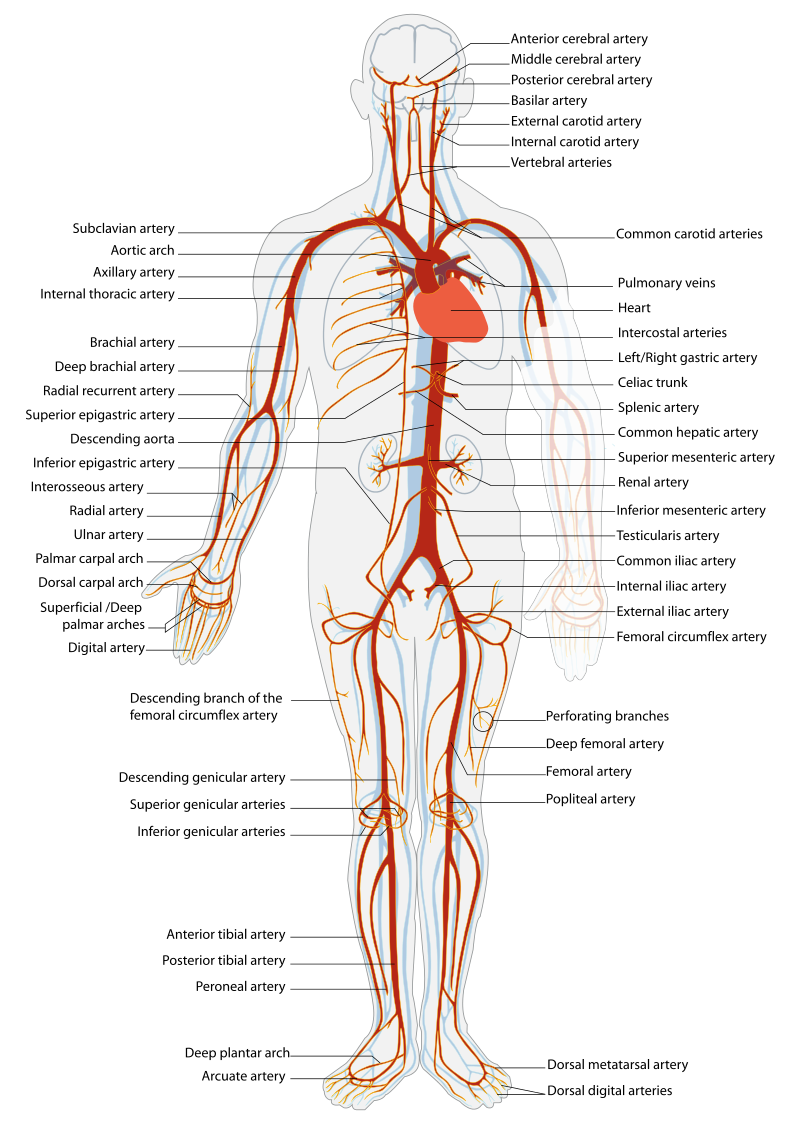
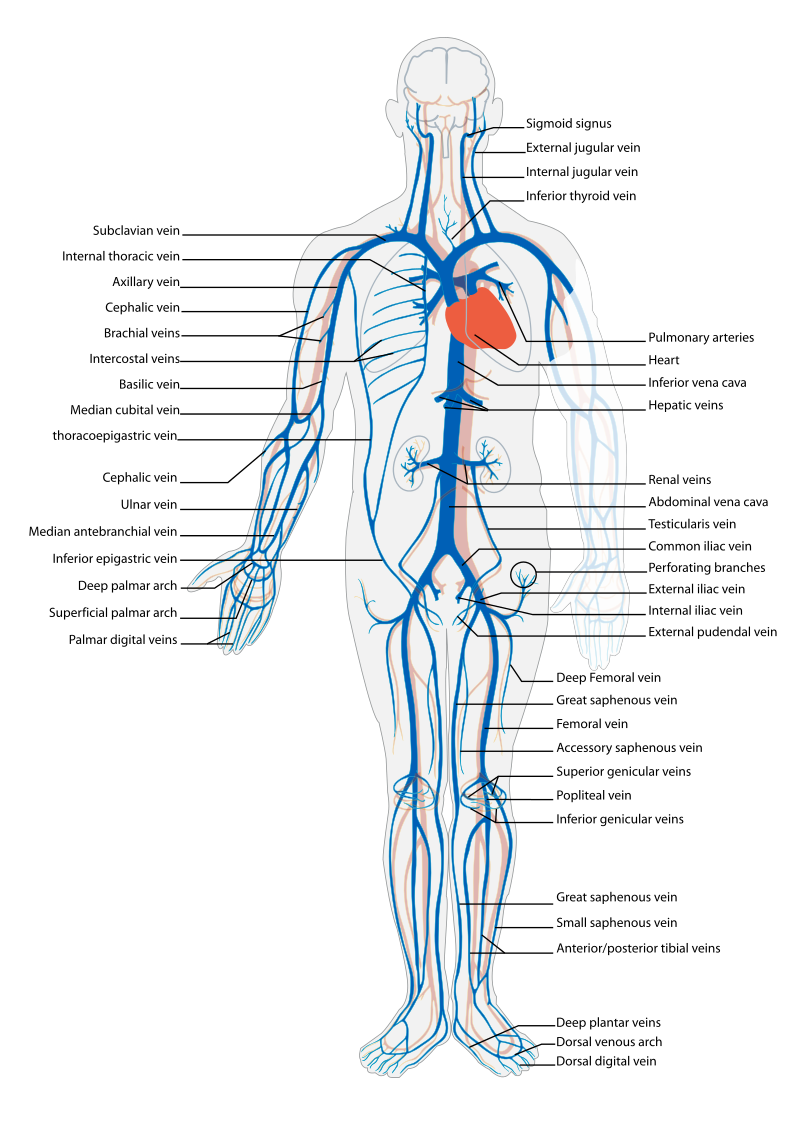
Before assessing a patient’s cardiovascular system, it is important to understand the various functions of the cardiovascular system. In addition to the information provided in the “Review of Cardiac Basics” section, the following images provide an overview of the cardiovascular system. Figure 9.1[1] provides an overview of the structure of the heart. Note the main cardiac structures are the atria, ventricles, and heart valves. Figure 9.2[2] demonstrates blood flow through the heart. Notice the flow of deoxygenated blood from the posterior and superior vena cava into the right atria and ventricle during diastole (indicated by blue coloring of these structures). The right ventricle then pumps deoxygenated blood to the lungs via the pulmonary artery during systole. At the same time, oxygenated blood from the lungs returns to the left atria and ventricle via the pulmonary veins during diastole (indicated by red coloring of these structures) and then is pumped out to the body via the aorta during systole. Figure 9.3[3] demonstrates the conduction system of the heart. This image depicts the conduction pathway through the heart as the tissue responds to electrical stimulation. Figure 9.4[4] illustrates the arteries of the circulatory system, and Figure 9.5[5] depicts the veins of the circulatory system. The purpose of these figures is to facilitate understanding of the electrical and mechanical function of the heart within the cardiovascular system.
Assessing the cardiovascular system includes performing several subjective and objective assessments. At times, assessment findings are modified according to life span considerations.
Subjective Assessment
The subjective assessment of the cardiovascular and peripheral vascular system is vital for uncovering signs of potential dysfunction. To complete the subjective cardiovascular assessment, the nurse begins with a focused interview. The focused interview explores past medical and family history, medications, cardiac risk factors, and reported symptoms. Symptoms related to the cardiovascular system include chest pain, peripheral edema, unexplained sudden weight gain, shortness of breath (dyspnea), irregular pulse rate or rhythm, dizziness, or poor peripheral circulation. Any new or worsening symptoms should be documented and reported to the health care provider.
Table 9.3a outlines questions used to assess symptoms related to the cardiovascular and peripheral vascular systems. Table 9.3b outlines questions used to assess medical history, medications, and risk factors related to the cardiovascular system. Information obtained from the interview process is used to tailor future patient education by the nurse.[6],[7],[8]
Table 9.3a Interview Questions for Cardiovascular and Peripheral Vascular Systems[9]
| Symptom | Question |
Follow-Up Safety Note: If findings indicate current severe symptoms suggestive of myocardial infarction or another critical condition, suspend the remaining cardiovascular assessment and obtain immediate assistance according to agency policy or call 911. |
|---|---|---|
| Chest Pain | Have you had any pain or pressure in your chest, neck, or arm? | Review how to assess a patient’s chief complaint using the PQRSTU method in the “Health History” chapter.
|
| Shortness of Breath
(Dyspnea) |
Do you ever feel short of breath with activity?
Do you ever feel short of breath at rest? Do you feel short of breath when lying flat? |
What level of activity elicits shortness of breath?
How long does it take you to recover? Have you ever woken up from sleeping feeling suddenly short of breath How many pillows do you need to sleep, or do you sleep in a chair (orthopnea)? Has this recently changed? |
| Edema | Have you noticed swelling of your feet or ankles?
Have you noticed your rings, shoes, or clothing feel tight at the end of the day? Have you noticed any unexplained, sudden weight gain? Have you noticed any new abdominal fullness? |
Has this feeling of swelling or restriction gotten worse?
Is there anything that makes the swelling better (e.g., sitting with your feet elevated)? How much weight have you gained? Over what time period have you gained this weight? |
| Palpitations | Have you ever noticed your heart feels as if it is racing or “fluttering” in your chest?
Have you ever felt as if your heart “skips” a beat? |
Are you currently experiencing palpitations?
When did palpitations start? Have you previously been treated for palpitations? If so, what treatment did you receive? |
| Dizziness (Syncope) |
Do you ever feel light-headed?
Do you ever feel dizzy? Have you ever fainted? |
Can you describe what happened?
Did you have any warning signs? Did this occur with position change? |
| Poor Peripheral Circulation | Do your hands or feet ever feel cold or look pale or bluish?
Do you have pain in your feet or lower legs when exercising? |
What, if anything, brings on these symptoms?
How much activity is needed to cause this pain? Is there anything, such as rest, that makes the pain better? |
| Calf Pain | Do you currently have any constant pain in your lower legs? | Can you point to the area of pain with one finger? |
Table 9.3b Interview Questions Exploring Cardiovascular Medical History, Medications, and Cardiac Risk Factors
| Topic | Questions |
|---|---|
| Medical History | Have you ever been diagnosed with any heart or circulation conditions, such as high blood pressure, coronary artery disease, peripheral vascular disease, high cholesterol, heart failure, or valve problems?
Have you had any procedures done to improve your heart function, such as ablation or stent placement? Have you ever had a heart attack or stroke? |
| Medications | Do you take any heart-related medications, herbs, or supplements to treat blood pressure, chest pain, high cholesterol, cardiac rhythm, fluid retention, or the prevention of clots? |
| Cardiac Risk Factors | Have your parents or siblings been diagnosed with any heart conditions?
Do you smoke or vape?
If you do not currently smoke, have you smoked in the past?
Are you physically active during the week?
What does a typical day look like in your diet?
Do you drink alcoholic drinks?
Would you say you experience stress in your life?
How many hours of sleep do you normally get each day?
|
Objective Assessment
The physical examination of the cardiovascular system involves the interpretation of vital signs, inspection, palpation, and auscultation of heart sounds as the nurse evaluates for sufficient perfusion and cardiac output.
For more information about assessing a patient’s oxygenation status as it relates to their cardiac output, visit the “Oxygenation” chapter in Open RN Nursing Fundamentals.
Equipment needed for a cardiovascular assessment includes a stethoscope, penlight, centimeter ruler or tape measure, and sphygmomanometer.[10]
Evaluate Vital Signs and Level of Consciousness
Interpret the blood pressure and pulse readings to verify the patient is stable before proceeding with the physical exam. Assess the level of consciousness; the patient should be alert and cooperative.
Inspection
- Skin color to assess perfusion. Inspect the face, lips, and fingertips for cyanosis or pallor. Cyanosis is a bluish discoloration of the skin, lips, and nail beds and indicates decreased perfusion and oxygenation. Pallor is the loss of color, or paleness of the skin or mucous membranes, as a result of reduced blood flow, oxygenation, or decreased number of red blood cells. Patients with light skin tones should be pink in color. For those with darker skin tones, assess for pallor on the palms, conjunctiva, or inner aspect of the lower lip.
- Jugular Vein Distension (JVD). Inspect the neck for JVD that occurs when the increased pressure of the superior vena cava causes the jugular vein to bulge, making it most visible on the right side of a person’s neck. JVD should not be present in the upright position or when the head of bed is at 30-45 degrees.
- Precordium for abnormalities. Inspect the chest area over the heart (also called precordium) for deformities, scars, or any abnormal pulsations the underlying cardiac chambers and great vessels may produce.
- Extremities:
- Upper Extremities: Inspect the fingers, arms, and hands bilaterally noting Color, Warmth, Movement, Sensation (CWMS). Alterations or bilateral inconsistency in CWMS may indicate underlying conditions or injury. Assess capillary refill by compressing the nail bed until it blanches and record the time taken for the color to return to the nail bed. Normal capillary refill is less than 3 seconds.[11]
- Lower Extremities: Inspect the toes, feet, and legs bilaterally, noting CWMS, capillary refill, and the presence of peripheral edema, superficial distended veins, and hair distribution. Document the location and size of any skin ulcers.
- Edema: Note any presence of edema. Peripheral edema is swelling that can be caused by infection, thrombosis, or venous insufficiency due to an accumulation of fluid in the tissues. (See Figure 9.6[12] for an image of pedal edema.)[13]
- Deep Vein Thrombosis (DVT): A deep vein thrombosis (DVT) is a blood clot that forms in a vein deep in the body. DVT requires emergency notification of the health care provider and immediate follow-up because of the risk of developing a life-threatening pulmonary embolism.[14] Inspect the lower extremities bilaterally. Assess for size, color, temperature, and for presence of pain in the calves. Unilateral warmth, redness, tenderness, swelling in the calf, or sudden onset of intense, sharp muscle pain that increases with dorsiflexion of the foot is an indication of a deep vein thrombosis (DVT).[15] See Figure 9.7[16] for an image of a DVT in the patient’s right leg, indicated by unilateral redness and edema.


Auscultation
Heart Sounds
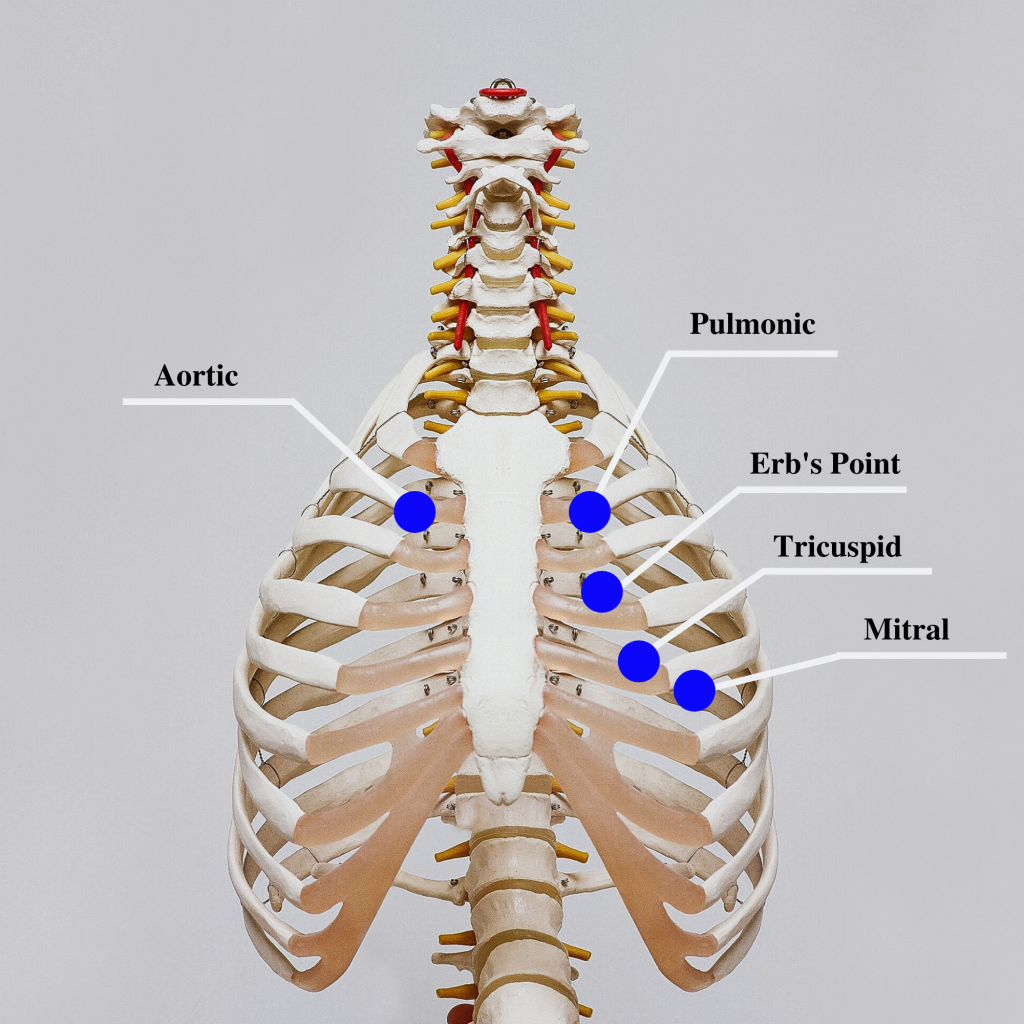
Auscultation is routinely performed over five specific areas of the heart to listen for corresponding valvular sounds. These auscultation sites are often referred to by the mnemonic “APE To Man,” referring to Aortic, Pulmonic, Erb’s point, Tricuspid, and Mitral areas (see Figure 9.8[17] for an illustration of cardiac auscultation areas). The aortic area is the second intercostal space to the right of the sternum. The pulmonic area is the second intercostal space to the left of the sternum. Erb’s point is directly below the pulmonic area and located at the third intercostal space to the left of the sternum. The tricuspid (or parasternal) area is at the fourth intercostal space to the left of the sternum. The mitral (also called apical or left ventricular area) is the fifth intercostal space at the midclavicular line.
Auscultation usually begins at the aortic area (upper right sternal edge). Use the diaphragm of the stethoscope to carefully identify the S1 and S2 sounds. They will make a “lub-dub” sound. Note that when listening over the area of the aortic and pulmonic valves, the “dub” (S2) will sound louder than the “lub” (S1). Move the stethoscope sequentially to the pulmonic area (upper left sternal edge), Erb’s point (left third intercostal space at the sternal border), and tricuspid area (fourth intercostal space. When assessing the mitral area for female patients, it is often helpful to ask them to lift up their breast tissue so the stethoscope can be placed directly on the chest wall. Repeat this process with the bell of the stethoscope. The apical pulse should be counted over a 60-second period. For an adult, the heart rate should be between 60 and 100 with a regular rhythm to be considered within normal range. The apical pulse is an important assessment to obtain before the administration of many cardiac medications.
The first heart sound (S1) identifies the onset of systole, when the atrioventricular (AV) valves (mitral and tricuspid) close and the ventricles contract and eject the blood out of the heart. The second heart sound (S2) identifies the end of systole and the onset of diastole when the semilunar valves close, the AV valves open, and the ventricles fill with blood. S1 corresponds to the palpable pulse. When auscultating, it is important to identify the S1 (“lub”) and S2 (“dub”) sounds, evaluate the rate and rhythm of the heart, and listen for any extra heart sounds.
![]() Auscultating Heart Sounds
Auscultating Heart Sounds
- To effectively auscultate heart sounds, patient repositioning may be required. If it difficult to hear the heart sounds, ask the patient to lean forward if they are able, or lie on their left side. These positions move the heart closer to their chest wall and can increase the volume of the heart sounds heard on auscultation. This repositioning may be helpful in patients with increased adipose tissue in their chest wall or larger breasts.
- It is common to hear lung sounds when auscultating the heart sounds. It may be helpful to ask the patient to briefly hold their breath if lung sounds impede adequate heart auscultation. Limit the holding of breath to 10 seconds or as tolerated by the patient.
- Environmental noise can cause difficulty in auscultating heart sounds. Removing environmental noise by turning down the television volume or shutting the door may be required for an accurate assessment.
- Patients may try to talk to you as you are assessing their heart sounds. It is often helpful to explain the procedure such as, “I am going to take a few minutes to listen carefully to the sounds of blood flow going through your heart. Please try not to speak while I am listening, so I can hear the sounds better.”
Extra Heart Sounds
Extra heart sounds include clicks, murmurs, S3 and S4 sounds, and pleural friction rubs. These extra sounds can be difficult for a novice to distinguish, so if you notice any new or different sounds, consult an advanced practitioner or notify the provider. A midsystolic click, associated with mitral valve prolapse, may be heard with the diaphragm at the apex or left lower sternal border.
A click may be followed by a murmur. A murmur is a blowing or whooshing sound that signifies turbulent blood flow often caused by a valvular defect. New murmurs not previously recorded should be immediately communicated to the health care provider. In the aortic area, listen for possible murmurs of aortic stenosis and aortic regurgitation with the diaphragm of the stethoscope. In the pulmonic area, listen for potential murmurs of pulmonic stenosis and pulmonary and aortic regurgitation. In the tricuspid area, at the fourth and fifth intercostal spaces along the left sternal border, listen for the potential murmurs of tricuspid regurgitation, tricuspid stenosis, or ventricular septal defect.
S3 and S4 sounds, if present, are often heard best by asking the patient to lie on their left side and listening over the apex with the bell of the stethoscope. An S3 sound, also called a ventricular gallop, occurs after the S2 and sounds like “lub-dub-dah,” or a sound similar to a horse galloping. An S3 can occur when a patient is experiencing fluid overload, such as during an acute exacerbation of heart failure.[18] It can also be a normal finding in pregnancy due to increased blood flow through the ventricles.
The S4 sound, also called atrial gallop, occurs immediately before the S1 and sounds like “ta-lub-dub.” An S4 sound can occur with decreased ventricular compliance or coronary artery disease.[19]
A pericardial friction rub is caused by inflammation of the pericardium, with a creaky-scratchy noise generated as the parietal and visceral membranes rub together. It is best heard at the apex or left lower sternal border with the diaphragm as the patient sits up, leans forward, and holds their breath.
Carotid Sounds
The carotid artery may be auscultated for bruits. Bruits are a swishing sound due to turbulence in the blood vessel and may be heard due to atherosclerotic changes.
Palpation
Palpation is used to evaluate peripheral pulses, capillary refill, and for the presence of edema. When palpating these areas, also pay attention to the temperature and moisture of the skin.
Pulses
Compare the rate, rhythm, and quality of arterial pulses bilaterally, including the carotid, radial, brachial, posterior tibialis, and dorsalis pedis pulses. Review additional information about obtaining pulses in the “General Survey” chapter. Bilateral comparison for all pulses (except the carotid) is important for determining subtle variations in pulse strength. Carotid pulses should be palpated on one side at a time to avoid decreasing perfusion of the brain. The posterior tibial artery is located just behind the medial malleolus. It can be palpated by scooping the patient’s heel in your hand and wrapping your fingers around so that the tips come to rest on the appropriate area just below the medial malleolus. The dorsalis pedis artery is located just lateral to the extensor tendon of the big toe and can be identified by asking the patient to flex their toe while you provide resistance to this movement. Gently place the tips of your second, third, and fourth fingers adjacent to the tendon, and try to feel the pulse.
The quality of the pulse is graded on a scale of 0 to 3, with 0 being absent pulses, 1 being decreased pulses, 2 is within normal range, and 3 being increased (also referred to as “bounding”). If unable to palpate a pulse, additional assessment is needed. First, determine if this is a new or chronic finding. Second, if available, use a Doppler ultrasound to determine the presence or absence of the pulse. Many agencies use Doppler ultrasound to document if a nonpalpable pulse is present. If the pulse is not found, this could be a sign of an emergent condition requiring immediate follow-up and provider notification. See Figures 9.9[20] and 9.10[21] for images of assessing pedal pulses.


Capillary Refill
The capillary refill test is performed on the nail beds to monitor perfusion, the amount of blood flow to tissue. Pressure is applied to a fingernail or toenail until it pales, indicating that the blood has been forced from the tissue under the nail. This paleness is called blanching. Once the tissue has blanched, pressure is removed. Capillary refill time is defined as the time it takes for the color to return after pressure is removed. If there is sufficient blood flow to the area, a pink color should return within 2 seconds after the pressure is removed.[22]
Review of Capillary Refill Test on YouTube[23].
Edema
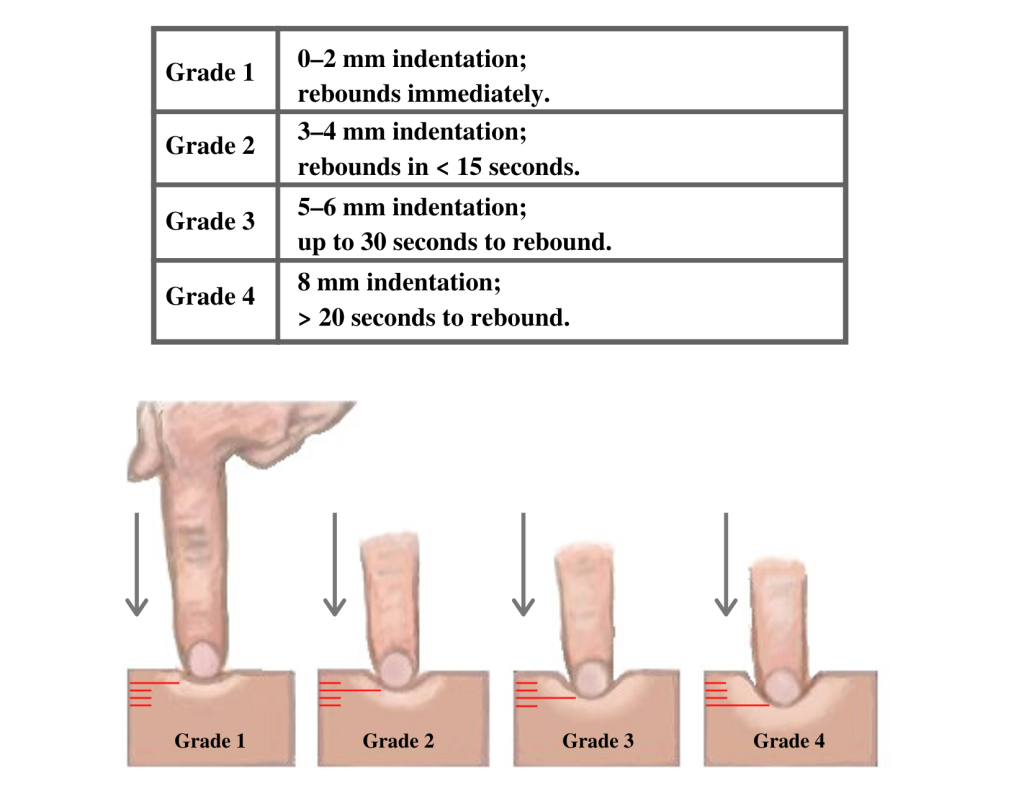
Edema occurs when one can visualize visible swelling caused by a buildup of fluid within the tissues. If edema is present on inspection, palpate the area to determine if the edema is pitting or nonpitting. Press on the skin to assess for indentation, ideally over a bony structure, such as the tibia. If no indentation occurs, it is referred to as nonpitting edema. If indentation occurs, it is referred to as pitting edema. See Figure 9.11[24] for images demonstrating pitting edema.

Note the depth of the indention and how long it takes for the skin to rebound back to its original position. The indentation and time required to rebound to the original position are graded on a scale from 1 to 4. Edema rated at 1+ indicates a barely detectable depression with immediate rebound, and 4+ indicates a deep depression with a time lapse of over 20 seconds required to rebound. See Figure 9.12[25] for an illustration of grading edema. Additionally, it is helpful to note edema may be difficult to observe in larger patients. It is also important to monitor for sudden changes in weight, which is considered a probable sign of fluid volume overload.
Heaves or Thrills
You may observe advanced practice nurses and other health care providers palpating the anterior chest wall to detect any abnormal pulsations the underlying cardiac chambers and great vessels may produce. Precordial movements should be evaluated at the apex (mitral area). It is best to examine the precordium with the patient supine because if the patient is turned on the left side, the apical region of the heart is displaced against the lateral chest wall, distorting the chest movements.[26] A heave or lift is a palpable lifting sensation under the sternum and anterior chest wall to the left of the sternum that suggests severe right ventricular hypertrophy. A thrill is a vibration felt on the skin of the precordium or over an area of turbulence, such as an arteriovenous fistula or graft.
Life Span Considerations
The cardiovascular assessment and expected findings should be modified according to common variations across the life span.
Infants and Children
A murmur may be heard in a newborn in the first few days of life until the ductus arteriosus closes.
When assessing the cardiovascular system in children, it is important to assess the apical pulse. Parameters for expected findings vary according to age group. After a child reaches adolescence, a radial pulse may be assessed. Table 9.3c outlines the expected apical pulse rate by age.
Table 9.3c Expected Apical Pulse by Age
| Age Group | Heart Rate |
|---|---|
| Preterm | 120-180 |
| Newborn (0 to 1 month) | 100-160 |
| Infant (1 to 12 months) | 80-140 |
| Toddler (1 to 3 years) | 80-130 |
| Preschool (3 to 5 years) | 80-110 |
| School Age (6 to 12 years) | 70-100 |
| Adolescents (13 to 18 years) | 60-90 |
Older Adults
In adults over age 65, irregular heart rhythms and extra sounds are more likely. An “irregularly irregular” rhythm suggests atrial fibrillation, and further investigation is required if this is a new finding. See the box below for more information about atrial fibrillation.
For more information on atrial fibrillation, visit the CDC Atrial Fibrillation webpage.
Expected Versus Unexpected Findings
After completing a cardiovascular assessment, it is important for the nurse to use critical thinking to determine if any findings require follow-up. Depending on the urgency of the findings, follow-up can range from calling the health care provider to calling the rapid response team. Table 9.3d compares examples of expected findings, meaning those considered within normal limits, to unexpected findings, which require follow-up. Critical conditions are those that should be reported immediately and may require notification of a rapid response team.
Table 9.3d Expected Versus Unexpected Findings on Cardiac Assessment
| Assessment | Expected Findings | Unexpected Findings (Document and notify the provider if this is a new finding*) |
|---|---|---|
| Inspection | Apical impulse may or may not be visible | Scars not previously documented that could indicate prior cardiac surgeries
Heave or lift observed in the precordium Chest anatomy malformations |
| Palpation | Apical pulse felt over midclavicular fifth intercostal space | Apical pulse felt to the left of the midclavicular fifth intercostal space
Additional movements over precordium such as a heave, lift, or thrill |
| Auscultation | S1 and S2 heart sounds in a regular rhythm | New irregular heart rhythm
Extra heart sounds such as a murmur, S3, or S4 |
| *CRITICAL CONDITIONS to report immediately | Symptomatic tachycardia at rest (HR>100 bpm)
Symptomatic bradycardia (HR<60 bpm) New systolic blood pressure (<100 mmHg) Orthostatic blood pressure changes (see “Blood Pressure” chapter for more information) New irregular heart rhythm New extra heart sounds such as a murmur, S3, or S4 New abnormal cardiac rhythm changes Reported chest pain, calf pain, or worsening shortness of breath |
See Table 9.3e for a comparison of expected versus unexpected findings when assessing the peripheral vascular system.
Table 9.3e Expected Versus Unexpected Peripheral Vascular Assessment Findings
| Assessment | Expected Findings | Unexpected Findings (Document or notify provider if new finding*) |
|---|---|---|
| Inspection | Skin color uniform and appropriate for race bilaterally
Equal hair distribution on upper and lower extremities Absence of jugular vein distention (JVD) Absence of edema Sensation and movement of fingers and toes intact |
Cyanosis or pallor, indicating decreased perfusion
Decreased or unequal hair distribution Presence of jugular vein distention (JVD) in an upright position or when head of bed is 30-45 degrees New or worsening edema Rapid and unexplained weight gain Impaired movement or sensation of fingers and toes |
| Palpation | Skin warm and dry
Pulses present and equal bilaterally Absence of edema Capillary refill less than 2 seconds |
Skin cool, excessively warm, or diaphoretic
Absent, weak/thready, or bounding pulses New irregular pulse New or worsening edema Capillary refill greater than 2 seconds Unilateral warmth, redness, tenderness, or edema, indicating possible deep vein thrombosis (DVT) |
| Auscultation | Carotid pulse | Carotid bruit |
| *CRITICAL CONDITIONS to report immediately | Cyanosis
Absent pulse (and not heard using Doppler device) Capillary refill time greater than 3 seconds Unilateral redness, warmth, and edema, indicating a possible deep vein thrombosis (DVT) |
“Sternum_composition.png” by Anatomography is licensed under CC BY-SA 2.1 Japan
“Sternum_composition.png” by Anatomography is licensed under CC BY-SA 2.1 Japan
Media Attributions
- 512px-Diagram_of_the_human_heart_(cropped)
- human-41546_1280
- 2018_Conduction_System_of_Heart
- image4
- image5
- image7
- image8
- image9
- image10
- 2201px-Combinpedal
- image12
- "Diagram of the human heart” by Wapcaplet is licensed under CC BY-SA 3.0 ↵
- "Diagram of the human heart” by Wapcaplet is licensed under CC BY-SA 3.0 ↵
- “2018 Conduction System of Heart.jpg” by OpenStax is licensed under CC-BY-3.0 ↵
- “Arterial System en.svg” by LadyofHats, Mariana Ruiz Villarreal is in the Public Domain. ↵
- “Venous system en.svg” by Lady of Hats Mariana Ruiz Vilarreal is in the Public Domain. ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology licensed under CC BY 4.0 ↵
- Felner, J. M. (1990). An overview of the cardiovascular system. In Walker, H. K., Hall, W. D., & Hurst, J. W. (Eds.), Clinical methods: The history, physical, and laboratory examinations (3rd ed., Chapter 7). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK393/ ↵
- Scott, C., & MacInnes, J. D. (2013, September 27). Cardiac patient assessment: putting the patient first. British Journal of Nursing, 15(9). https://doi.org/10.12968/bjon.2006.15.9.21091 ↵
- Scott, C., & MacInnes, J. D. (2013, September 27). Cardiac patient assessment: putting the patient first. British Journal of Nursing, 15(9). https://doi.org/10.12968/bjon.2006.15.9.21091 ↵
- Felner, J. M. (1990). An overview of the cardiovascular system. In Walker, H. K., Hall, W. D., & Hurst, J. W. (Eds.), Clinical methods: The history, physical, and laboratory examinations (3rd ed., Chapter 7). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK393/ ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology licensed under CC BY 4.0 ↵
- “Swollen feet at Harefield Hospital edema.jpg” by Ryaninuk is licensed under CC BY-SA 4.0 ↵
- Simon, E. C. (2014). Leg edema assessment and management. MEDSURG Nursing, 23(1), 44-53. ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology licensed under CC BY 4.0 ↵
- “Deep vein thrombosis of the right leg.jpg” by James Heilman, MD is licensed under CC BY-SA 3.0 ↵
- “Cardiac Auscultation Areas” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- Shono, A., Mori, S., Yatomi, A., Kamio, T., Sakai, J., Soga, F., Tanaka, H., & Hirata, K. I. (2019). Ultimate third heart sound. Internal Medicine, 58(17), 2535–2538. https://doi.org/10.2169/internalmedicine.2731-19 ↵
- Felner, J. M. (1990). An overview of the cardiovascular system. In Walker, H. K., Hall, W. D., & Hurst, J. W. (Eds.), Clinical methods: The history, physical, and laboratory examinations (3rd ed., Chapter 7). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK393/ ↵
- “DSC_2277.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/2-5-focussed-respiratory-assessment/ ↵
- “DSC_2314.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/2-5-focussed-respiratory-assessment/ ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Capillary nail refill test; [updated 2020, Aug 9] https://medlineplus.gov/ency/article/003394.htm ↵
- RegisteredNurseRN. (2022, March 21). Capillary Refill Time Test: Normal vs. Abnormal - Nursing Clincial Skills. [Video]. YouTube. Used with permission. All rights reserved. https://youtu.be/EwaDSZRH1LE ↵
- “Combinpedal.jpg” by James Heilman, MD is licensed under CC BY-SA 3.0 ↵
- “Grading of Edema” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- Felner, J. M. (1990). An overview of the cardiovascular system. In Walker, H. K., Hall, W. D., & Hurst, J. W. (Eds.), Clinical methods: The history, physical, and laboratory examinations (3rd ed., Chapter 7). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK393/ ↵
The National Council Licensure Examination for Registered Nurses (NCLEX-RN) is the exam that nursing graduates must pass successfully to obtain their nursing license and become a registered nurse. The purpose of the NCLEX is to evaluate if a nursing graduate (i.e., candidate) is competent to provide safe, competent, entry-level nursing care. The NCLEX-RN is developed by the National Council of State Board of Nursing (NCSBN), an independent, nonprofit organization composed of the 50 state boards of nursing and other regulatory agencies.[1]
The NCLEX-RN is a pass/fail examination administered on a computer using computer adaptive testing (CAT). CAT means that every time a candidate answers a test item, the computer reestimates their ability based on all their previous answers and the difficulty of those items. The computer then selects the next item based on an estimated 50% chance of the candidate answering it correctly. In this manner, the next item is not too easy nor too difficult, and a candidate’s true ability level is determined. Each item is perceived by the candidate as challenging because it is targeted to their ability. With each item answered, the computer's estimate of the candidate’s ability becomes more precise.
The computer stops providing items when it is 95% certain that the candidate’s ability is clearly above or clearly below the passing standard, the candidate has received the maximum number of questions, or the candidate has run out of time without demonstrating a competence level to pass. Testing accommodations may be provided for eligible candidates with the authorization of the candidate’s State Board of Nursing (SBON).[2],[3]
See an image of a simulated graduate taking the NCLEX in Figure 11.1.[4]

Read more about the NCLEX at https://www.ncsbn.org/nclex.htm.
Watch a video about how the NCLEX uses computer assistive technology (CAT) at https://www.ncsbn.org/356.htm.
Registering to Take the NCLEX
Before you can register to take the NCLEX, you will need an Authorization to Test (ATT). To receive an ATT, complete the following steps[5]:
- Apply for a nurse license from your State Board of Nursing (SBON) or other nursing regulatory body
- Register with Pearson VUE and pay the exam fee
- Wait to receive your ATT from Pearson Vue
- Schedule your exam with Pearson VUE
Be sure to start this process well in advance of your target date for taking the NCLEX.
Read specific instructions regarding registering and taking the NCLEX-RN by downloading the most current NCLEX-Candidate Bulletin from the NCSBN. The content includes the following:
- Registering for the exam
- Scheduling the exam
- Understanding test site rules and regulations
- Preparing for the day of the exam
Download the most current NCLEX-Candidate Bulletin from https://www.ncsbn.org/nclex.htm.
Next Generation NCLEX
A new edition of NCLEX was released in 2023 with “Next Generation” questions.
The Next Generation NCLEX (Next Gen) uses evolving case studies and new types of test questions based on a new NCSBN Clinical Judgment Measurement Model (NCJMM) that assesses how well the candidate can think critically and use clinical judgment when providing nursing care. The NCJMM assess the candidate's ability to recognize cues, analyze cues, prioritize hypotheses, generate solutions, take actions, and evaluate outcomes.[6]
Five new Next Generation test item types are called extended multiple response, extended drag and drop, cloze (drop-down), extended hot spot (highlighting), and matrix-grid:
- Extended Multiple Response: Extended Multiple Response items allow candidates to select one or more answer options at a time. This item type is similar to the current NCLEX multiple response item but has more options and uses partial credit scoring.[7]
- Extended Drag and Drop: Extended Drag and Drop items allow candidates to move or place response options into answer spaces. This item type is like the current NCLEX ordered response items but not all of the response options may be required to answer the item. In some items, there may be more response options than answer spaces.[8]
- Cloze (Drop – Down): Cloze (Drop - Down) items allow candidates to select one option from a drop-down list. There can be more than one drop-down list in a cloze item. These drop-down lists can be used as words or phrases within a sentence or within tables and charts.[9]
- Enhanced Hot Spot (Highlighting): Enhanced Hot Spot items allow candidates to select their answer by highlighting predefined words or phrases. Candidates can select and deselect the highlighted parts by clicking on the words or phrases. These types of items allow an individual to read a portion of a client medical record (e.g., a nursing note, medical history, lab values, medication record, etc.), and then select the words or phrases that answer the item.[10]
- Matrix/Grid: Matrix/Grid items allow the candidate to select one or more answer options for each row and/or column. This item type can be useful in measuring multiple aspects of the clinical scenario with a single item. In the example below, each of the eight rows will need to have one of the three answer choices selected.[11]
View a NCSBN video on Next Generation test items.
Participate in an NCLEX tutorial at https://www.ncsbn.org/nclex-tutorial.htm.
Preparing for the Examination
Since the first day of nursing school, you have been working towards successfully passing the NCLEX-RN. After you graduate, it is important to implement strategies for success for taking the NCLEX, such as reviewing the NCLEX-RN Test Plan, setting up a dedicated review schedule based on your test date, and reviewing material you learned throughout nursing school.[12]
NCLEX Test Plan
The NCLEX-RN Test Plan provides a concise summary of the content and scope of the exam and serves as an excellent guide for preparation. NCLEX-RN test plans are updated every three years based on surveys of newly licensed registered nurses to ensure the NCLEX questions reflect fair, comprehensive, current, and entry-level nursing competency.[13]
The NCLEX Test Plan categorizes test questions based on categories and subcategories referred to as “Client Needs”[14]:
- Safe and Effective Care Environment
- Management of Care
- Safety and Infection Control
- Health Promotion and Maintenance
- Psychosocial Integrity
- Physiological Integrity
- Basic Care and Comfort
- Pharmacological and Parenteral Therapies
- Reduction of Risk Potential
- Physiological Adaptation
In addition, the following concepts are applied throughout the client needs categories[15]:
- Nursing Process
- Caring
- Communication and Documentation
- Teaching and Learning
- Culture and Spirituality
Download the current NCLEX-RN Test Plan from https://www.ncsbn.org/testplans.htm.
Review Schedule
Many students find it helpful to create and follow a study calendar with topics to review based on the NCLEX Test Plan.
Reviewing Material
Some graduates prefer to attend an NCLEX review course to prepare for the examination whereas others prefer to review their notes from nursing school on their own. Be sure to review the NCLEX Candidate Rules before the day of the examination.[16],[17]
Day of the Examination
On the day of the examination, it is normal to experience some anxiety. However, it is important to use techniques to manage anxiety, so it does not impact your ability to think through and answer the test questions. Use positive self-talk and remind yourself that you have been preparing for this examination since the first day of nursing school. Read additional tips for the day of the NCLEX and tips for testing in the following boxes.
| Tips for the Day of the NCLEX[18] |
|---|
|
| Tips for Testing[19] |
|---|
|
After the Examination
If your State Board of Nursing (SBON) or nursing regulatory body (NRB) participates in the “Quick Results Service,” you can receive your “unofficial” results two business days after the exam if you pay for this service. Official results are sent to you approximately six weeks after the exam.[20]
If you didn't pass the exam, you'll receive an NCLEX Candidate Performance Report (CPR). The CPR is an individualized document that shows how a candidate performed in each of the test plan content areas. Graduates who fail the exam can use the CPR as a guide to prepare them to retake the exam.[21]
If you need to retake the exam, you will need to wait a minimum of 45 days before you can retake the NCLEX per NCSBN policy. This length of time is determined by your SBON (or NRB) and will be reflected in your new ATT’s validity dates. Read the steps for retaking the NCLEX in the following box.
| Steps for Retaking the NCLEX |
|---|
|
Advocacy
The American Nurses Association (ANA) emphasizes that advocacy is fundamental to nursing practice in every setting. See Figure 10.1[22] for an illustration of advocacy. Advocacy is defined as the act or process of pleading for, supporting, or recommending a cause or course of action. Advocacy may be for individuals, groups, organizations, communities, society, or policy issues[23]:
- Individual: The nurse educates health care consumers so they can consider actions, interventions, or choices related to their own personal beliefs, attitudes, and knowledge to achieve the desired outcome. In this way, the health care consumer learns self-management and decision-making.[24]
- Interpersonal: The nurse empowers health care consumers by providing emotional support, assistance in obtaining resources, and necessary help through interactions with families and significant others in their social support network.[25]
- Organization and Community: The nurse supports cultural and social transformation of organizations, communities, or populations. Registered nurses understand their obligation to help improve environmental and societal conditions related to health, wellness, and care of the health care consumer.[26]
- Policy: The nurse promotes inclusion of the health care consumers’ voices into policy, legislation, and regulation about issues such as health care access, reduction of health care costs and financial burden, protection of the health care consumer, and environmental health, such as safe housing and clear water.[27]
Advocacy at each of these levels will be further discussed in later sections of this chapter.
Advocacy is one of the ANA’s Standards of Professional Performance. The Standards of Professional Performance are “authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently."[28] See the following box to read the competencies associated with the ANA’s Advocacy Standard of Professional Performance.[29]
Competencies of ANA’s Advocacy Standard of Professional Performance[30]
- Champions the voice of the health care consumer.
- Recommends appropriate levels of care, timely and appropriate transitions, and allocation of resources to optimize outcomes.
- Promotes safe care of health care consumers, safe work environments, and sufficient resources.
- Participates in health care initiatives on behalf of the health care consumer and the system(s) where nursing happens.
- Demonstrates a willingness to address persistent, pervasive systemic issues.
- Informs the political arena about the role of nurses and the vital components necessary for nurses and nursing to provide optimal care delivery.
- Empowers all members of the health care team to include the health care consumer in care decisions, including limitation of treatment and end-of-life care.
- Embraces diversity, equity, inclusivity, health promotion, and health care for individuals of diverse geographic, cultural, ethnic, racial, gender, and spiritual backgrounds across the life span.
- Develops policies that improve care delivery and access for underserved and vulnerable populations.
- Promotes policies, regulations, and legislation at the local, state, and national levels to improve health care access and delivery of health care.
- Considers societal, political, economic, and cultural factors to address social determinants of health.
- Role models advocacy behavior.
- Addresses the urgent need for a diverse and inclusive workforce as a strategy to improve outcomes related to the social determinants of health and inequities in the health care system.
- Advances policies, programs, and practices within the health care environment that maintain, sustain, and restore the environment and natural world.
- Contributes to professional organizations.
Reflective Questions
- What Advocacy competencies have you already demonstrated during your nursing education?
- What Advocacy competencies are you most interested in performing next?
- What questions do you have about ANA’s Advocacy competencies?
Licensure is the process by which a State Board of Nursing (SBON) grants permission to an individual to engage in nursing practice after verifying the applicant has attained the competency necessary to perform the scope of practice of a registered nurse (RN).[31] The SBON verifies these three components:
- Verification of graduation from an approved prelicensure RN nursing education program
- Verification of successful completion of NCLEX-RN examination
- A criminal background check (in some states)[32]
In the United States there are three common types of prelicensure educational programs that prepare a student to become an RN, including a two-year associate degree of nursing (ADN), a hospital-based diploma program, or a four-year baccalaureate degree (BSN). Some universities offer an "Entry Level Master of Science in Nursing Track" for non-nurses holding a baccalaureate or master's degree in another field who wish to become a nurse. All graduates must pass the same NCLEX-RN to obtain their RN license from their SBON (or other nursing regulatory body).
Requirements for licensure renewal vary from state to state. Some states require continued education credits (CEUs), along with the payment of fees. In Wisconsin the nursing license is renewed every two years. See Figure 11.2[33] for an image of a simulated nursing license.
- Use this map for contact information for the State Boards of Nursing.
- Read more details on obtaining a Wisconsin RN license at https://dsps.wi.gov/Pages/Professions/RN/Default.aspx.
Nurse Licensure Compact
When applying for your nursing license from your State Board of Nursing (SBON), you may also be eligible to apply for a multistate license. The Nurse Licensure Compact (NLC) allows nurses to practice in other NLC states with their original state’s nursing license without having to obtain additional licenses, contingent upon remaining a resident of that state. Currently, 38 states have enacted the NLC. Read more information about the NLC using the information in the following box.
View the current Nurse Licensure Compact Map.
Read this algorithm on how to Navigate the Nurse Licensure Compact.
Read more information about the Nurse Licensure Compact Rules.
Watch a video for nursing students on the Nurse Licensure Compact.
Temporary Permit
In some states before taking the NCLEX, an applicant may apply to receive a temporary permit from their State Board of Nursing (SBON). A temporary permit allows the applicant to practice practical nursing under the direct supervision of a registered nurse until the RN license is granted. A temporary permit is typically valid for a period of three months or until the holder receives failing NCLEX results, whichever is shorter.
Read about the temporary permit available in Wisconsin.
As discussed previously, the American Nurses Association (ANA) defines advocacy at the individual level as educating health care consumers so they can consider actions, interventions, or choices related to their own personal beliefs, attitudes, and knowledge to achieve the desired outcome. In this way, the health care consumer learns self-management and decision-making.[34] Advocacy at the interpersonal level is defined as empowering health care consumers by providing emotional support, assistance in obtaining resources, and necessary help through interactions with families and significant others in their social support network.[35]
What does advocacy look like in a nurse’s daily practice? The following are some examples provided by an oncology nurse[36]:
- Ensure Safety. Ensure the client is safe when being treated in a health care facility and when they are discharged by communicating with case managers or social workers about the client’s need for home health or assistance after discharge so it is arranged before they go home.
- Give Clients a Voice. Give clients a voice when they are vulnerable by staying in the room with them while the doctor explains their diagnosis and treatment options to help them ask questions, get answers, and translate information from medical jargon.
- Educate. Educate clients on how to manage their current or chronic conditions to improve the quality of their everyday life. For example, clients undergoing chemotherapy can benefit from the nurse teaching them how to take their anti-nausea medication in a way that will be most effective for them and will allow them to feel better between treatments.
- Protect Patient Rights. Know clients’ wishes for their care. Advocacy may include therapeutically communicating a client’s wishes to an upset family member who disagrees with their choices. In this manner, the client’s rights are protected and a healing environment is established.
- Double-Check for Errors. Know that everyone makes mistakes. Nurses often identify, stop, and fix errors made by interprofessional team members. They flag conflicting orders from multiple providers and notice oversights. Nurses should read provider orders and carefully compare new orders to previous documentation. If an order is unclear or raises concerns, a nurse should discuss their concerns with another nurse, a charge nurse, a pharmacist, or the provider before implementing it to ensure patient safety.
- Connect Clients to Resources. Help clients find resources inside and outside the hospital to support their well-being. Know resources in your agency, such as case managers or social workers who can assist with financial concerns, advance directives, health insurance, or transportation concerns. Request assistance from agency chaplains to support spiritual concerns. Promote community resources, such as patient or caregiver support networks, Meals on Wheels, or other resources to meet their needs.
Nurses must recognize their unique position in client advocacy to empower individuals to provide them with the support and resources to make their best judgment. The intimate and continuous nature of the nurse-patient relationship places nurses in a prime position to identify and address the needs and concerns of their patients. This relationship is built on trust, empathy, and consistent interaction, which allows nurses to gain a deep understanding of their patients' values, preferences, and personal circumstances. By leveraging this close proximity and strong rapport, nurses can effectively advocate for their patients, ensuring that their voices are heard, and their wishes are respected in all aspects of care.[37]
The power of the nurse-patient relationship extends beyond the immediate clinical environment. Nurses often act as liaisons between patients and the broader health care team, facilitating communication and ensuring that patient preferences are integrated into care plans. This advocacy role is crucial in navigating complex health care systems where patients may feel overwhelmed or marginalized. Nurses can help demystify medical jargon, explain treatment options, and support patients in making informed decisions that align with their values and goals. Through education and emotional support, nurses empower patients to take an active role in their own care, enhancing patient autonomy and satisfaction.[38]
In addition to direct patient care, nurses play a pivotal role in identifying systemic issues that affect patient outcomes. Their frontline perspective provides valuable insights into the barriers patients face in accessing quality care, such as socioeconomic challenges, cultural barriers, and institutional policies. By advocating for policy changes and improvements in health care delivery, nurses contribute to creating a more equitable and patient-centered health care system. Their advocacy efforts can lead to the implementation of practices and policies that better address the needs of diverse patient populations, ultimately improving health outcomes on a broader scale.[39]
Nurses' advocacy is also essential in situations where patients are unable to speak for themselves, such as in cases of severe illness, disability, or end-of-life care. In these instances, nurses must be vigilant in recognizing and addressing the needs of vulnerable patients, ensuring that their rights and dignity are upheld. This may involve working closely with families and caregivers, coordinating with interdisciplinary teams, and navigating ethical dilemmas to provide the best possible care for the patient.
Nurses advocate for issues in their communities and their organizations.
Addressing Social Determinants of Health
Advocacy is commonly perceived as acting on behalf of a client, but it can be a much broader action than affecting a single client and their family members. Nurses advocate for building healthier communities by addressing social determinants of health (SDOH). SDOH are the conditions in the environments where people live, learn, work, and play that affect a wide range of outcomes. SDOH include health care access and quality, neighborhood and environment, social and community context, economic stability, and education access and quality. Social determinants of health (SDOH) have a major impact on people’s health, well-being, and quality of life. See Figure 10.2[40] for an illustration of SDOH.[41]

Specific examples of addressing SDOH include the following goals:
- Improving safe housing and public transportation
- Decreasing discrimination and violence
- Expanding quality education and job opportunities
- Increasing access to nutritious foods and physical activity opportunities
- Promoting clean air and clean water
- Enhancing language and literacy skills[42]
SDOH contribute to health disparities and inequities among different socioeconomic groups. For example, individuals who don't have access to grocery stores with healthy foods are less likely to have good nutrition, increasing their risk for health conditions like heart disease, diabetes, and obesity, and potentially lowering their life expectancy relative to people who do have access to healthy foods.[43]
One of Healthy People 2030’s goals specifically relates to advocacy regarding SDOH. The goal states, “Create social, physical, and economic environments that promote attaining the full potential for health and well-being for all.” Across the United States, people and organizations at the local, state, territorial, tribal, and national levels are working hard to improve health and reduce health disparities by addressing SDOH.[44] Read more information about these advocacy efforts in the following box.
Read more about efforts addressing SDOH at Healthy People 2030.