8.3 Applying the Nursing Process
Open Resources for Nursing (Open RN)
Now that we have discussed various concepts related to oxygenation and hypoxia, we will explain how a nurse uses the nursing process to care for clients with alterations in oxygenation.
Assessment
When assessing a client’s oxygenation status, there are several subjective and objective assessments to include.
Subjective Assessment
The primary symptom to assess when a client is experiencing decreased oxygenation is their level of dyspnea, the medical term for the subjective feeling of shortness of breath or difficulty breathing. Clients can be asked to rate their dyspnea on a scale of 0-10, similar to using a pain rating scale.[1] The feeling of dyspnea can be very disabling for clients. There are many interventions that a nurse can implement to help improve the feeling of dyspnea and, thus, improve a client’s overall quality of life.
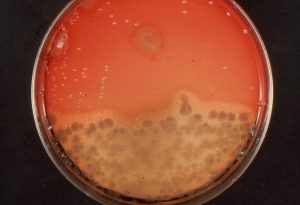
It is also important to ask clients if they are experiencing a cough. If a cough is present, determine if sputum is present, and if so, the color and amount of sputum. Sputum is mucus and other secretions that are coughed up and expelled from the mouth. The body always produces mucus to keep the delicate tissues of the respiratory tract moist so small particles of foreign matter can be trapped and forced out, but when there is an infection in the lungs, an excess of mucus is produced. The body attempts to get rid of this excess by coughing it up as sputum. The color of a client’s sputum can provide cues for underlying medical conditions. For example, sputum caused by a respiratory infection is often yellow, green, or brown and often referred to as purulent sputum.[2] See Figure 8.7[3] for an image of purulent sputum.

Clients should be asked if they are experiencing chest pain. Chest pain can occur with several types of respiratory and cardiac conditions, some of which are emergent. If the client reports chest pain, first determine if it is an emergency by asking questions such as:
- “Does it feel like something is sitting on your chest?”
- “Is the pain radiating into your jaw or arm?”
- “Do you feel short of breath, dizzy, or nauseated?”
If any of these symptoms are occurring, seek emergency medical assistance according to agency policy. If it is not a medical emergency, perform a focused assessment on the chest pain, including onset, location, duration, characteristics, alleviating or aggravating factors, radiation, and if any treatment has been used for the pain.[4] Noncardiac chest pain tends to worsen with coughing and deep breathing.
Objective Assessment
Focused objective assessments for a client suspected of experiencing decreased oxygenation include assessing the airway; evaluating respiratory rate, effort, and quality; analyzing pulse oximetry readings; auscultating lung sounds for adventitious sounds; and evaluating the heart rate for tachycardia.
Signs of cyanosis or clubbing should be noted. Clubbing is the enlargement of the fingertips that occurs with chronic hypoxia such as in chronic obstructive pulmonary disease (COPD) or congenital deficits in pediatric clients. See Figure 8.8[5] for an image of clubbing.

Another sign of chronic hypoxia that often occurs in clients with chronic respiratory diseases like COPD includes an increased anterior-posterior chest diameter, often referred to as a barrel chest. A barrel chest results from air trapping in the alveoli. See Figure 8.9[6] for an image of a barrel chest.

Diagnostic Tests and Lab Work
Diagnostic tests and lab work are based on the client’s medical condition that is causing the decreased oxygenation. For example, clients with a productive cough may have a chest X-ray or sputum culture ordered, and clients experiencing respiratory distress often have arterial blood gas (ABG) tests performed.
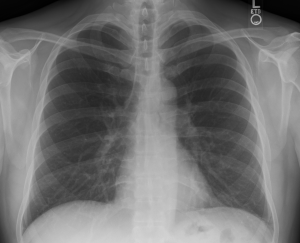
A chest X-ray is a fast and painless imaging test that uses certain electromagnetic waves to create pictures of the structures in and around the chest. This test can help diagnose and monitor conditions such as pneumonia, heart failure, lung cancer, and tuberculosis. Health care providers also use chest X-rays to see how well certain treatments are working and to check for complications after certain procedures or surgeries. Chest X-rays are contraindicated during pregnancy.[7],[8] See Figure 8.10[9] for an image of a chest X-ray.
A sputum culture is a diagnostic test that evaluates the type and number of bacteria present in sputum. The client is asked to cough deeply and spit any mucus that comes up into a sterile specimen container. The sample is sent to a lab where it is placed in a special dish and is watched for two to three days or longer to see if bacteria or other disease-causing germs grow. The data is used to determine appropriate antimicrobial therapy.[10] See Figure 8.11[11] for an image of a sputum culture.
For clients experiencing respiratory distress, arterial blood gas (ABG) tests are often ordered. Additional details about ABG tests are discussed in the “Oxygenation Basic Concepts” section of this chapter, as well as in the “Acid-Base Balance” section of the “Fluid and Electrolytes” chapter. See Table 8.3a for a summary of normal ranges of ABG values in adults.
Table 8.3a Normal Ranges of ABG Values in Adults
| Value | Description | Normal Range |
|---|---|---|
| pH | Acid-base balance of blood | 7.35-7.45 |
| PaO2 | Partial pressure of oxygen | 80-100 mmHg |
| PaCO2 | Partial pressure of carbon dioxide | 35-45 mmHg |
| HCO3 | Bicarbonate level | 22-26 mEq/L |
| SaO2 | Calculated oxygen saturation | 95-100% |
Diagnoses
Commonly used NANDA-I nursing diagnoses for clients experiencing decreased oxygenation and dyspnea include Impaired Gas Exchange, Ineffective Breathing Pattern, Ineffective Airway Clearance, Decreased Cardiac Output, and Activity Intolerance. See Table 8.3b for definitions and selected defining characteristics for these commonly used nursing diagnoses.[12] Use a current, evidence-based nursing care plan resource when creating a care plan for a client.
Table 8.3b NANDA-I Nursing Diagnoses Related to Decreased Oxygenation and Dyspnea
| NANDA-I Nursing Diagnoses | Definition | Selected Defining Characteristics |
|---|---|---|
| Impaired Gas Exchange | Excess or deficit in oxygenation and/or carbon dioxide elimination at the alveolar-capillary membrane. |
|
| Ineffective Breathing Pattern | Inspiration and/or expiration that does not provide adequate ventilation. | |
| Ineffective Airway Clearance | Inability to clear secretions or obstructions from the respiratory tract to maintain a clear airway. |
|
| Decreased Cardiac Output | Inadequate blood pumped by the heart to meet the metabolic demands of the body. |
|
| Activity Intolerance | Activity Intolerance: Insufficient physiological or psychological energy to endure or complete required or desired daily activities. |
|
For example, nurses commonly care for clients with chronic obstructive pulmonary disease (COPD). To select an accurate nursing diagnosis for a specific client with COPD, the nurse compares assessment findings with the defining characteristics of various nursing diagnoses. The nurse may select Ineffective Breathing Pattern after validating this client is demonstrating the associated signs and symptoms related to this nursing diagnosis:
- Dyspnea
- Increase in anterior-posterior chest diameter (e.g., barrel chest)
- Nasal flaring
- Orthopnea
- Prolonged expiration phase
- Pursed-lip breathing
- Tachypnea
- Use of accessory muscles to breathe
- Use of three-point position
Outcome Identification
A broad goal(s) for clients experiencing alterations in oxygenation is:
- The client will have adequate movement of air into and out of the lungs.[13]
A sample “SMART” outcome for a client experiencing dyspnea is:
- The client’s reported level of dyspnea will be within their stated desired range of 1-2 throughout their hospital stay.
Planning Interventions
According to NOC and NIC Linkages to NANDA-I and Clinical Conditions[14] and Nursing Interventions Classification (NIC),[15] Anxiety Reduction and Respiratory Monitoring are common categories of independent nursing interventions used to care for clients experiencing dyspnea and alterations in oxygenation. Anxiety Reduction is defined as, “Minimizing apprehension, dread, foreboding, or uneasiness related to an unidentified source of anticipated danger.”[16] Respiratory Monitoring is defined as, “Collection and analysis of client data to ensure airway patency and adequate gas exchange.”[17] Selected nursing interventions related to anxiety reduction and respiratory monitoring are listed in the following box.
Selected Nursing Interventions to Reduce Anxiety and Perform Respiratory Monitoring
Anxiety Reduction
- Use a calm, reassuring approach
- Explain all procedures, including sensations likely to be experienced during the procedure
- Provide factual information concerning diagnosis, treatment, and prognosis
- Stay with the client to promote safety and reduce fear
- Encourage the family to stay with the client, as appropriate
- Listen attentively
- Create an atmosphere of trust
- Encourage verbalization of feelings, perceptions, and fears
- Identify when level of anxiety changes
- Provide diversional activities geared toward the reduction of tension
- Instruct the client on the use of relaxation techniques
- Administer medications to reduce anxiety, as appropriate
Respiratory Monitoring
- Monitor rate, rhythm, depth, and effort of respirations
- Note chest movement, watching for symmetry and use of accessory muscles
- Monitor for noisy respirations such as snoring
- Monitor breathing patterns
- Monitor oxygen saturation levels in sedated clients
- Provide for noninvasive continuous oxygen sensors with appropriate alarm systems in clients with risk factors per agency policy and as indicated
- Auscultate lung sounds, noting areas of decreased or absent ventilation and presence of adventitious sounds
- Monitor client’s ability to cough effectively
- Note onset, characteristics, and duration of cough
- Monitor the client’s respiratory secretions
- Provide frequent intermittent monitoring of respiratory status in at-risk clients
- Monitor for dyspnea and events that improve and worsen it
- Monitor chest X-ray reports as appropriate
- Note changes in ABG values if ordered and notify provider as appropriate
- Institute resuscitation efforts as needed
- Institute respiratory therapy treatments as needed
In addition to the independent nursing interventions listed in the preceding box, several nursing interventions can be implemented to manage hypoxia, such as teaching enhanced breathing and coughing techniques, repositioning, managing oxygen therapy, administering medications, and providing suctioning. Refer to Table 8.2b in the “Oxygenation Basic Concepts” section earlier in this chapter for information about these interventions.
For additional details regarding managing oxygen therapy, see the “Oxygen Therapy” chapter in Open RN Nursing Skills, 2e.
Read more information about respiratory medications in the “Respiratory” chapter in Open RN Nursing Pharmacology, 2e.
Clients should also receive individualized health promotion teaching to enhance their respiratory status. Health promotion teaching includes encouraging activities such as the following:
- Receiving an annual influenza vaccine
- Receiving a pneumococcal vaccine every five years as indicated
- Stopping smoking
- Drinking adequate fluids to thin respiratory secretions
- Participating in physical activity as tolerated
Implementing Interventions
When implementing interventions that have been planned to enhance oxygenation, it is always important to assess the client’s current level of dyspnea and modify interventions based on the client’s current status. For example, if dyspnea has worsened, some interventions may no longer be appropriate (such as ambulating), and additional interventions may be needed (such as consulting with a respiratory therapist or administering additional medication).
Evaluation
After implementing interventions, the effectiveness of interventions should be documented, and the overall nursing care plan evaluated. Focused reassessments for evaluating improvement of oxygenation status include analyzing the client’s heart rate, respiratory rate, pulse oximetry reading, and lung sounds, in addition to asking the client to rate their level of dyspnea.
Media Attributions
- Acopaquia
- barrel-chest-1024×706
- Chest_Xray_PA_3-8-2010
- 4888319912_b663098d46_h
- Registered Nurses' Association of Ontario. (2005). Nursing care of dyspnea: The 6th vital sign in individuals with chronic obstructive pulmonary disease. https://rnao.ca/bpg/guidelines/dyspnea ↵
- Barrel, A. (2017, August 13). What is a sputum culture test? MedicalNewsToday. https://www.medicalnewstoday.com/articles/318924#what-is-a-sputum-culture-test ↵
- “Sputnum.JPG” by Zhangmoon618 is licensed under CC0 ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Chest Pain; [updated 2020, August 4]. https://medlineplus.gov/ency/article/003079.htm ↵
- “Acopaquia.jpg” by Desherinka is licensed under CC BY-SA 4.0 ↵
- “Normal A-P Chest Image.jpg" and "Barrel Chest.jpg" by Meredith Pomietlo for Chippewa Valley Technical College are licensed under CC BY 4.0 ↵
- National Heart, Lung, and Blood Institute. (n.d.). Chest x-ray. https://www.nhlbi.nih.gov/health-topics/chest-x-ray ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Chest x-ray; [updated 2020, August 4]. https://medlineplus.gov/ency/article/003804.htm ↵
- “Chest Xray PA 3-8-2010.png” by Stillwaterising is licensed under CC0 ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Routine sputum culture; [updated 2020, Aug 4]. https://medlineplus.gov/ency/article/003723.htm ↵
- “m241-8 Blood agar culture of sputum from patient with pneumonia. Comprimised host. Colonies of Candida albicans and pseudomonas aeruginosa (LeBeau)” by Microbe World is licensed under CC BY-NC-SA 2.0 ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York, p. 230. ↵
- Johnson, M., Moorhead, S., Bulechek, G., Butcher, H., Maas, M., & Swanson, E. (2012). NOC and NIC linkages to NANDA-I and clinical conditions: Supporting critical reasoning and quality care. Elsevier, pp. 54-55. ↵
- Johnson, M., Moorhead, S., Bulechek, G., Butcher, H., Maas, M., & Swanson, E. (2012). NOC and NIC linkages to NANDA-I and clinical conditions: Supporting critical reasoning and quality care. Elsevier, pp. 54-55. ↵
- Butcher, H., Bulechek, G., Dochterman, J., & Wagner, C. (2018). Nursing interventions classification (NIC). Elsevier, pp. 71 and 321. ↵
- Johnson, M., Moorhead, S., Bulechek, G., Butcher, H., Maas, M., & Swanson, E. (2012). NOC and NIC linkages to NANDA-I and clinical conditions: Supporting critical reasoning and quality care. Elsevier, pp. 54-55. ↵
- Butcher, H., Bulechek, G., Dochterman, J., & Wagner, C. (2018). Nursing interventions classification (NIC). Elsevier, pp. 71 and 321. ↵
Implementation is the fifth step of the nursing process (and the fifth Standard of Practice by the American Nurses Association). This standard is defined as, "The registered nurse implements the identified plan." The RN may delegate planned interventions after considering the circumstance, person, task, communication, supervision, and evaluation, as well as the state Nurse Practice Act, federal regulation, and agency policy.[1]
Implementation of interventions requires the RN to use critical thinking and clinical judgment. After the initial plan of care is developed, continual reassessment of the client is necessary to detect any changes in the client’s condition requiring modification of the plan. The need for continual client reassessment underscores the dynamic nature of the nursing process and is crucial to providing safe care.
During the implementation phase of the nursing process, the nurse prioritizes planned interventions, assesses client safety while implementing interventions, delegates interventions as appropriate, and documents interventions performed. LPN/VNs have an active role in the Implementation phase, provided the interventions falls within the LPN/VN scope of practice. See Figure 4.14 for an illustration of how the Implementation phase of the nursing process correlates to NCSBN's Clinical Judgment Measurement Model.[2]
Prioritizing Implementation of Interventions
Prioritizing implementation of interventions follows a similar method as to prioritizing nursing diagnoses. Maslow’s Hierarchy of Needs and the ABCs of airway, breathing, and circulation are used to establish top priority interventions. When possible, least invasive actions are usually preferred due to the risk of injury from invasive options. Read more about methods for prioritization under the “Diagnosis” section of this chapter.
The potential impact on future events, especially if a task is not completed at a certain time, is also included when prioritizing nursing interventions. For example, if a client is scheduled to undergo a surgical procedure later in the day, the nurse prioritizes initiating a NPO (nothing by mouth) prescription prior to completing pre-op client education about the procedure. The rationale for this decision is that if the client eats food or drinks water, the surgery time will be delayed. Knowing and understanding the client's purpose for care, current situation, and expected outcomes are necessary to accurately prioritize interventions.
Client Safety
It is essential to consider client safety when implementing interventions. At times, clients may experience a change in condition that makes a planned nursing intervention or provider prescription no longer safe to implement. For example, an established nursing care plan for a client states, “The nurse will ambulate the client 100 feet three times daily.” However, during assessment this morning, the client reports feeling dizzy today, and their blood pressure is 90/60. Using critical thinking and clinical judgment, the nurse decides to not implement the planned intervention of ambulating the client. This decision and supporting assessment findings should be documented in the client’s chart and also communicated during the shift handoff report, along with appropriate notification of the provider of the client’s change in condition.
Implementing interventions goes far beyond implementing provider prescriptions and completing tasks identified on the nursing care plan and must focus on client safety. As frontline providers, nurses are in the position to stop errors before they reach the client.
In 2000 the Institute of Medicine (IOM) issued the historic, groundbreaking report titled To Err Is Human: Building a Safer Health System. The report stated that as many as 98,000 people die in U.S. hospitals each year as a result of preventable medical errors. To Err Is Human broke the silence that previously surrounded the consequences of medical errors and set a national agenda for reducing medical errors and improving client safety through the design of a safer health system.[3] In 2007 the IOM published a follow-up report titled Preventing Medication Errors and reported that more than 1.5 million Americans are injured every year in American hospitals, and the average hospitalized client experiences at least one medication error each day. This report emphasized actions that health care systems could take to improve medication safety.[4]
The Quality and Safety Education for Nurses (QSEN) project began in 2005 to assist in preparing future nurses to continuously improve the quality and safety of the health care systems in which they work. The vision of the QSEN project is to “inspire health care professionals to put quality and safety as core values to guide their work.”[5] Nurses and nursing students are expected to participate in quality improvement (QI) initiatives by identifying gaps where change is needed and assisting in implementing initiatives to resolve these gaps. Quality improvement is defined as, “The combined and unceasing efforts of everyone – health care professionals, clients and their families, researchers, payers, planners and educators – to make the changes that will lead to better client outcomes (health), better system performance (care), and better professional development (learning).”[6]
Delegation of Interventions
While implementing interventions, RNs may elect to delegate nursing tasks. Delegation is defined by the American Nurses Association as, “The assignment of the performance of activities or tasks related to client care to unlicensed assistive personnel or licensed practical nurses (LPNs) while retaining accountability for the outcome.”[7] RNs are accountable for determining the appropriateness of the delegated task according to the condition of the client and the circumstance; the communication provided to an appropriately trained LPN or UAP; the level of supervision provided; and the evaluation and documentation of the task completed. The RN must also be aware of the state Nurse Practice Act, federal regulations, and agency policy before delegating. The RN cannot delegate responsibilities requiring clinical judgment.[8] See the following box for information regarding legal requirements associated with delegation according to the Nurse Practice Act.
Delegation According to the Wisconsin Nurse Practice Act[9]
"During the supervision and direction of delegated acts a Registered Nurse shall do all of the following:
(a) Delegate tasks commensurate with educational preparation and demonstrated abilities of the person supervised.
(b) Provide direction and assistance to those supervised.
(c) Observe and monitor the activities of those supervised.
(d) Evaluate the effectiveness of acts performed under supervision.
The standard of practice for Licensed Practical Nurses in Wisconsin states, “In the performance of acts in basic patient situations, the LPN shall, under the general supervision of an RN or the direction of a provider:
(a) Accept only patient care assignments which the LPN is competent to perform.
(b) Provide basic nursing care. Basic nursing care is defined as care that can be performed following a defined nursing procedure with minimal modification in which the responses of the patient to the nursing care are predictable.
(c) Record nursing care given and report to the appropriate person changes in the condition of a patient.
(d) Consult with a provider in cases where an LPN knows or should know a delegated act may harm a patient.
(e) Perform the following other acts when applicable:
- Assist with the collection of data.
- Assist with the development and revision of a nursing care plan.
- Reinforce the teaching provided by an RN provider and provide basic health care instruction.
- Participate with other health team members in meeting basic patient needs.”
Read additional details about the scope of practice of registered nurses (RNs) and licensed practical nurses (LPNs) in Wisconsin's Nurse Practice Act in Chapter N 6 Standards of Practice.
Read more about the American Nurses Association's Principles for Delegation.
Table 4.7 outlines general guidelines for delegating nursing tasks in the state of Wisconsin according to the role of the health care team member.
Table 4.7 General Guidelines for Delegating Nursing Tasks
| RN | LPN | CNA | |
|---|---|---|---|
| Assessment | Complete client assessment | Assist with the collection of data for stable clients | Collect measurements such as weight, input/output, and vital signs in stable clients |
| Diagnosis | Analyze assessment data and create nursing diagnoses | Not applicable | Not applicable |
| Outcome Identification | Identify SMART client outcomes | Not applicable | Not applicable |
| Planning | Plan nursing interventions | Assist with the development of a nursing care plan | Not applicable |
| Implementation of Interventions | Implement independent, dependent, and collaborative nursing interventions; delegate interventions as appropriate, with supervision; document interventions performed | Participate with other health team members in meeting basic client needs and document interventions provided
Reinforce the teaching provided by an RN provider and provide basic health care instruction |
Implement and document delegated interventions associated with basic nursing care such as providing assistance in ambulating or tasks within their scope of practice |
| Evaluation | Evaluate the attainment of outcomes and revise the nursing care plan as needed | Contribute data regarding the achievement of client outcomes; assist in the revision of a nursing care plan | Not applicable |
Documentation of Interventions
As interventions are performed, they must be documented in the client’s record in a timely manner. As previously discussed in the “Ethical and Legal Issues” subsection of the “Basic Concepts” section, lack of documentation is considered a failure to communicate and a basis for legal action. A basic rule of thumb is if an intervention is not documented, it is considered not done in a court of law. It is also important to document administration of medication and other interventions in a timely manner to prevent errors that can occur due to delayed documentation time.
Coordination of Care and Health Teaching/Health Promotion
ANA's Standard of Professional Practice for Implementation also includes the standards 5A Coordination of Care and 5B Health Teaching and Health Promotion.[10] Coordination of Care includes competencies such as organizing the components of the plan, engaging the client in self-care to achieve goals, and advocating for the delivery of dignified and holistic care by the interprofessional team. Health Teaching and Health Promotion is defined as, “Employing strategies to teach and promote health and wellness.”[11] Client education is an important component of nursing care and should be included during every client encounter. For example, client education may include teaching about side effects while administering medications or teaching clients how to self-manage their conditions at home.
Putting It Together
See an example of implementation in the following box.
Example of Implementation
Refer to Scenario C in the "Assessment" section of this chapter. The nurse implemented the nursing care plan documented in Appendix C. Interventions related to breathing were prioritized. Administration of the diuretic medication was completed first, and lung sounds were monitored frequently for the remainder of the shift. Weighing the client before breakfast was delegated to the CNA. The client was educated about her medications and methods to use to reduce peripheral edema at home. All interventions were documented in the electronic medical record (EMR).
Implementation is the fifth step of the nursing process (and the fifth Standard of Practice by the American Nurses Association). This standard is defined as, "The registered nurse implements the identified plan." The RN may delegate planned interventions after considering the circumstance, person, task, communication, supervision, and evaluation, as well as the state Nurse Practice Act, federal regulation, and agency policy.[12]
Implementation of interventions requires the RN to use critical thinking and clinical judgment. After the initial plan of care is developed, continual reassessment of the client is necessary to detect any changes in the client’s condition requiring modification of the plan. The need for continual client reassessment underscores the dynamic nature of the nursing process and is crucial to providing safe care.
During the implementation phase of the nursing process, the nurse prioritizes planned interventions, assesses client safety while implementing interventions, delegates interventions as appropriate, and documents interventions performed. LPN/VNs have an active role in the Implementation phase, provided the interventions falls within the LPN/VN scope of practice. See Figure 4.14 for an illustration of how the Implementation phase of the nursing process correlates to NCSBN's Clinical Judgment Measurement Model.[13]
Prioritizing Implementation of Interventions
Prioritizing implementation of interventions follows a similar method as to prioritizing nursing diagnoses. Maslow’s Hierarchy of Needs and the ABCs of airway, breathing, and circulation are used to establish top priority interventions. When possible, least invasive actions are usually preferred due to the risk of injury from invasive options. Read more about methods for prioritization under the “Diagnosis” section of this chapter.
The potential impact on future events, especially if a task is not completed at a certain time, is also included when prioritizing nursing interventions. For example, if a client is scheduled to undergo a surgical procedure later in the day, the nurse prioritizes initiating a NPO (nothing by mouth) prescription prior to completing pre-op client education about the procedure. The rationale for this decision is that if the client eats food or drinks water, the surgery time will be delayed. Knowing and understanding the client's purpose for care, current situation, and expected outcomes are necessary to accurately prioritize interventions.
Client Safety
It is essential to consider client safety when implementing interventions. At times, clients may experience a change in condition that makes a planned nursing intervention or provider prescription no longer safe to implement. For example, an established nursing care plan for a client states, “The nurse will ambulate the client 100 feet three times daily.” However, during assessment this morning, the client reports feeling dizzy today, and their blood pressure is 90/60. Using critical thinking and clinical judgment, the nurse decides to not implement the planned intervention of ambulating the client. This decision and supporting assessment findings should be documented in the client’s chart and also communicated during the shift handoff report, along with appropriate notification of the provider of the client’s change in condition.
Implementing interventions goes far beyond implementing provider prescriptions and completing tasks identified on the nursing care plan and must focus on client safety. As frontline providers, nurses are in the position to stop errors before they reach the client.
In 2000 the Institute of Medicine (IOM) issued the historic, groundbreaking report titled To Err Is Human: Building a Safer Health System. The report stated that as many as 98,000 people die in U.S. hospitals each year as a result of preventable medical errors. To Err Is Human broke the silence that previously surrounded the consequences of medical errors and set a national agenda for reducing medical errors and improving client safety through the design of a safer health system.[14] In 2007 the IOM published a follow-up report titled Preventing Medication Errors and reported that more than 1.5 million Americans are injured every year in American hospitals, and the average hospitalized client experiences at least one medication error each day. This report emphasized actions that health care systems could take to improve medication safety.[15]
The Quality and Safety Education for Nurses (QSEN) project began in 2005 to assist in preparing future nurses to continuously improve the quality and safety of the health care systems in which they work. The vision of the QSEN project is to “inspire health care professionals to put quality and safety as core values to guide their work.”[16] Nurses and nursing students are expected to participate in quality improvement (QI) initiatives by identifying gaps where change is needed and assisting in implementing initiatives to resolve these gaps. Quality improvement is defined as, “The combined and unceasing efforts of everyone – health care professionals, clients and their families, researchers, payers, planners and educators – to make the changes that will lead to better client outcomes (health), better system performance (care), and better professional development (learning).”[17]
Delegation of Interventions
While implementing interventions, RNs may elect to delegate nursing tasks. Delegation is defined by the American Nurses Association as, “The assignment of the performance of activities or tasks related to client care to unlicensed assistive personnel or licensed practical nurses (LPNs) while retaining accountability for the outcome.”[18] RNs are accountable for determining the appropriateness of the delegated task according to the condition of the client and the circumstance; the communication provided to an appropriately trained LPN or UAP; the level of supervision provided; and the evaluation and documentation of the task completed. The RN must also be aware of the state Nurse Practice Act, federal regulations, and agency policy before delegating. The RN cannot delegate responsibilities requiring clinical judgment.[19] See the following box for information regarding legal requirements associated with delegation according to the Nurse Practice Act.
Delegation According to the Wisconsin Nurse Practice Act[20]
"During the supervision and direction of delegated acts a Registered Nurse shall do all of the following:
(a) Delegate tasks commensurate with educational preparation and demonstrated abilities of the person supervised.
(b) Provide direction and assistance to those supervised.
(c) Observe and monitor the activities of those supervised.
(d) Evaluate the effectiveness of acts performed under supervision.
The standard of practice for Licensed Practical Nurses in Wisconsin states, “In the performance of acts in basic patient situations, the LPN shall, under the general supervision of an RN or the direction of a provider:
(a) Accept only patient care assignments which the LPN is competent to perform.
(b) Provide basic nursing care. Basic nursing care is defined as care that can be performed following a defined nursing procedure with minimal modification in which the responses of the patient to the nursing care are predictable.
(c) Record nursing care given and report to the appropriate person changes in the condition of a patient.
(d) Consult with a provider in cases where an LPN knows or should know a delegated act may harm a patient.
(e) Perform the following other acts when applicable:
- Assist with the collection of data.
- Assist with the development and revision of a nursing care plan.
- Reinforce the teaching provided by an RN provider and provide basic health care instruction.
- Participate with other health team members in meeting basic patient needs.”
Read additional details about the scope of practice of registered nurses (RNs) and licensed practical nurses (LPNs) in Wisconsin's Nurse Practice Act in Chapter N 6 Standards of Practice.
Read more about the American Nurses Association's Principles for Delegation.
Table 4.7 outlines general guidelines for delegating nursing tasks in the state of Wisconsin according to the role of the health care team member.
Table 4.7 General Guidelines for Delegating Nursing Tasks
| RN | LPN | CNA | |
|---|---|---|---|
| Assessment | Complete client assessment | Assist with the collection of data for stable clients | Collect measurements such as weight, input/output, and vital signs in stable clients |
| Diagnosis | Analyze assessment data and create nursing diagnoses | Not applicable | Not applicable |
| Outcome Identification | Identify SMART client outcomes | Not applicable | Not applicable |
| Planning | Plan nursing interventions | Assist with the development of a nursing care plan | Not applicable |
| Implementation of Interventions | Implement independent, dependent, and collaborative nursing interventions; delegate interventions as appropriate, with supervision; document interventions performed | Participate with other health team members in meeting basic client needs and document interventions provided
Reinforce the teaching provided by an RN provider and provide basic health care instruction |
Implement and document delegated interventions associated with basic nursing care such as providing assistance in ambulating or tasks within their scope of practice |
| Evaluation | Evaluate the attainment of outcomes and revise the nursing care plan as needed | Contribute data regarding the achievement of client outcomes; assist in the revision of a nursing care plan | Not applicable |
Documentation of Interventions
As interventions are performed, they must be documented in the client’s record in a timely manner. As previously discussed in the “Ethical and Legal Issues” subsection of the “Basic Concepts” section, lack of documentation is considered a failure to communicate and a basis for legal action. A basic rule of thumb is if an intervention is not documented, it is considered not done in a court of law. It is also important to document administration of medication and other interventions in a timely manner to prevent errors that can occur due to delayed documentation time.
Coordination of Care and Health Teaching/Health Promotion
ANA's Standard of Professional Practice for Implementation also includes the standards 5A Coordination of Care and 5B Health Teaching and Health Promotion.[21] Coordination of Care includes competencies such as organizing the components of the plan, engaging the client in self-care to achieve goals, and advocating for the delivery of dignified and holistic care by the interprofessional team. Health Teaching and Health Promotion is defined as, “Employing strategies to teach and promote health and wellness.”[22] Client education is an important component of nursing care and should be included during every client encounter. For example, client education may include teaching about side effects while administering medications or teaching clients how to self-manage their conditions at home.
Putting It Together
See an example of implementation in the following box.
Example of Implementation
Refer to Scenario C in the "Assessment" section of this chapter. The nurse implemented the nursing care plan documented in Appendix C. Interventions related to breathing were prioritized. Administration of the diuretic medication was completed first, and lung sounds were monitored frequently for the remainder of the shift. Weighing the client before breakfast was delegated to the CNA. The client was educated about her medications and methods to use to reduce peripheral edema at home. All interventions were documented in the electronic medical record (EMR).
Learning Objectives
- Accurately perform calculations using decimals, fractions, percentages, ratios, and/or proportions
- Convert between the metric and household systems
- Use military time
- Use dimensional analysis
- Accurately solve calculations related to conversions, dosages, liquid concentrations, reconstituted medications, weight-based medications, and intravenous infusions and evaluate final answer to ensure safe medication administration
The Institute of Medicine (IOM) has estimated that the average hospitalized patient experiences at least one medication error each day. Nurses are the last step in the medication administration process before the medication reaches the patient, so they bear the final responsibility to ensure the medication is safe. To safely prepare and administer medications, the nurse performs a variety of mathematical calculations, such as determining the number of tablets, calculating the amount of solution, and setting the rate of an intravenous infusion.[23]
Dosage calculation in clinical practice is more than just solving a math problem. Nurses must perform several tasks during drug calculations, such as reading drug labels for pertinent information, determining what information is needed to set up the math calculation, performing the math calculations, and then critically evaluating the answer to determine if it is within a safe dosage range for that specific patient. Finally, the nurse selects an appropriate measurement device to accurately measure the calculated dose or set the rate of administration.[24] This chapter will explain how to perform these tasks related to dosage calculations using authentic problems that a nurse commonly encounters in practice.
You have now learned how to perform each step of the nursing process according to the ANA Standards of Professional Nursing Practice. Critical thinking, clinical reasoning, and clinical judgment are used when assessing the client, creating a nursing care plan, and implementing interventions. Frequent reassessment, with revisions to the care plan as needed, is important to help the client achieve expected outcomes. Throughout the entire nursing process, the client always remains the cornerstone of nursing care. Providing individualized, client-centered care and evaluating whether that care has been successful in achieving client outcomes are essential for providing safe, professional nursing practice.
Video Review of Creating a Sample Care Plan[25]
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Instructions: Apply what you’ve learned in this chapter by creating a nursing care plan using the following scenario. Use the template in Appendix B as a guide.
The client, Mark S., is a 57-year-old male who was admitted to the hospital with “severe” abdominal pain that was unable to be managed in the Emergency Department. The physician has informed Mark that he will need to undergo some diagnostic tests. The tests are scheduled for the morning.
After receiving the news about his condition and the need for diagnostic tests, Mark begins to pace the floor. He continues to pace constantly. He keeps asking the nurse the same question (“How long will the tests take?”) about his tests over and over again. The client also remarked, “I’m so uptight I will never be able to sleep tonight.” The nurse observes that the client avoids eye contact during their interactions and that he continually fidgets with the call light. His eyes keep darting around the room. He appears tense and has a strained expression on his face. He states, “My mouth is so dry.” The nurse observes his vital signs to be: T 98, P 104, R 30, BP 180/96. The nurse notes that his skin feels sweaty (diaphoretic) and cool to the touch.
Critical Thinking Activity:
-
- Group (cluster) the cues (subjective and objective data).
- Create a problem-focused nursing diagnosis (hypothesis).
- Develop a broad goal and then identify an expected outcome in “SMART” format.
- Outline three interventions for the nursing diagnosis to meet the goal and their rationale. Cite an evidence-based source for the interventions and rationale
- Imagine that you implemented the interventions that you identified. Evaluate the degree to which the expected outcome was achieved: Met - Partially Met - Not Met.

Test your knowledge using this NCLEX Next Generation-style question. You may reset and resubmit your answers to this question an unlimited number of times.[26]

