7.8 Parathyroid Disorders
Open Resources for Nursing (Open RN)
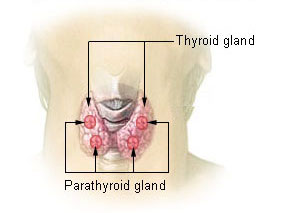
The parathyroid glands are found around the thyroid. They regulate calcium excretion by secreting parathyroid hormone (PTH). See Figure 7.22[1] for an illustration of the parathyroid glands.
PTH secretion occurs as part of a negative feedback loop in response to low calcium levels in the blood. Calcium is reabsorbed in both the kidneys and intestine and released from the bones to increase serum calcium levels. Due to the inverse relationship of calcium and phosphorus, low calcium levels result in elevated phosphate levels in the blood.
Hypoparathyroidism
The primary cause of hypoparathyroidism is a complication of a thyroidectomy or head and neck surgery when the parathyroid glands are inadvertently removed, resulting in hypocalcemia. Signs and symptoms of hypocalcemia often impact the musculoskeletal, nervous, and cardiac systems. Hypocalcemia may result in numbness, paresthesia, muscle cramps, and cardiac dysrhythmias. If severe, hypocalcemia can cause laryngospasm, tetany (involuntary muscle contraction), and seizures. Chvostek’s sign is a classic sign of acute hypocalcemia and is an involuntary twitching of facial muscles when the facial nerve is tapped. A second classic sign of acute hypocalcemia is Trousseau’s sign, a hand spasm caused by inflating a blood pressure cuff to a level above systolic pressure for three minutes.[2]
Hypoparathyroidism is treated with calcium supplements and calcitriol (vitamin D). Dietary recommendations for clients with hypoparathyroidism include food sources that are high in calcium, vitamin D, and low in phosphorus. Phosphate binders may also be prescribed if phosphorus levels are elevated. Clients treated for hypoparathyroidism with calcium and calcitriol must have periodic blood tests performed for calcium, phosphorus, and renal function. The absence of PTH reduces the reabsorption of calcium in the kidneys, so they are also at risk for developing kidney stones as a result of calcium deposits building up in the kidney tissue.[3] This is especially common in conditions of chronic hypoparathyroidism. This risk can be minimized by titrating therapy to keep the serum calcium level in the low-normal range. In most cases, this will be sufficient to prevent muscle cramps and paresthesia yet limit the risk of kidney stones.[4]
Hyperparathyroidism
Hyperparathyroidism is overactivation of parathyroid glands causing excessive release of parathyroid hormone, resulting in hypercalcemia. Hypercalcemia results from PTH encouraging bone breakdown and increased absorption of calcium from intestines and kidneys. Signs and symptoms of hypercalcemia include nausea, vomiting, constipation, increased thirst and/or urination, dysrhythmias, bone pain, kidney stones, lethargy/fatigue, and skeletal muscle weakness. Other associated symptoms include nonspecific client complaints such as depression, memory loss, fatigue, sleep problems, bone or muscle pains, gastroesophageal reflux disease, and decreased concentration.[5]
Hyperparathyroidism is often diagnosed when elevated calcium levels are discovered on lab work that was prescribed for other medical reasons. The most common cause of hyperparathyroidism is a parathyroid tumor that is treated and cured with surgery. Additional interventions include administration of IV fluids, calcium chelators, and furosemide. Postoperatively, there is typically significant improvement in the previously reported nonspecific symptoms, resulting in improved quality of life. Potential postoperative complications include hematoma formation leading to airway obstruction, hypoparathyroidism/hypocalcemia, and laryngeal nerve injury. Postoperative hypocalcemia is treated with calcium and vitamin D supplementation.[6]
![]() RN Recap: Hyperparathyroidism and Hypoparathyroidism
RN Recap: Hyperparathyroidism and Hypoparathyroidism
View a brief YouTube video overview of hyperparathyroidism and hypoparathyroidism[7]:
Media Attributions
- Illu_thyroid_parathyroid
- “Illu_thyroid_parathyroid.jpg” by unknown author for National Cancer Institute is licensed in the Public Domain. ↵
- This work is a derivative of StatPearls by Hans & Levine and is licensed under CC BY 4.0 ↵
- Abdullah, A. (2021). Chronic hypoparathyroidism linked to higher risk of kidney stones. https://hypoparathyroidismnews.com/news/chronic-hypoparathyroidism-linked-significantly-higher-risk-kidney-stones-calcification-large-study/ ↵
- This work is a derivative of StatPearls by Hans & Levine and is licensed under CC BY 4.0 ↵
- Madkhali, T., Alhefdhi, A., Chen, H., & Elfenbein, D. (2016). Primary hyperparathyroidism. Ulusal Cerrahi Dergisi, 32(1), 58-66. https://doi.org/10.5152/ucd.2015.3032 ↵
- Madkhali, T., Alhefdhi, A., Chen, H., & Elfenbein, D. (2016). Primary hyperparathyroidism. Ulusal Cerrahi Dergisi, 32(1), 58-66. https://doi.org/10.5152/ucd.2015.3032 ↵
- Open RN Project. (2024, June 23). Health Alterations - Chapter 7 - Hyperparathyroidism & hypoparathyroidism [Video]. You Tube. CC BY-NC 4.0 https://youtu.be/jPW7O4QB0_4?si=Rly_Fs0CIfqRkgwN ↵
Difficulty swallowing.
A swishing sound heard upon auscultation.
A swishing sound heard upon auscultation.
A decreased level of consciousness with a score of less than 8 on the Glasgow Coma Scale.

