7.6 Teams and Teamwork
Open Resources for Nursing (Open RN)
Now that we have reviewed the first three IPEC competencies related to valuing team members, understanding team members’ roles and responsibilities, and using structured interprofessional communication strategies, let’s discuss strategies that promote effective teamwork. The fourth IPEC competency states, “Apply relationship-building values and the principles of team dynamics to perform effectively in different team roles to plan, deliver, and evaluate patient/population-centered care and population health programs and policies that are safe, timely, efficient, effective, and equitable.”[1] See the following box for the components of this IPEC competency.
Components of IPEC’s Teams and Teamwork Competency[2]
- Describe the process of team development and the roles and practices of effective teams.
- Develop consensus on the ethical principles to guide all aspects of teamwork.
- Engage health and other professionals in shared patient-centered and population-focused problem-solving.
- Integrate the knowledge and experience of health and other professions to inform health and care decisions, while respecting patient and community values and priorities/preferences for care.
- Apply leadership practices that support collaborative practice and team effectiveness.
- Engage self and others to constructively manage disagreements about values, roles, goals, and actions that arise among health and other professionals and with patients, families, and community members.
- Share accountability with other professions, patients, and communities for outcomes relevant to prevention and health care.
- Reflect on individual and team performance for individual, as well as team, performance improvement.
- Use process improvement to increase effectiveness of interprofessional teamwork and team-based services, programs, and policies.
- Use available evidence to inform effective teamwork and team-based practices.
- Perform effectively on teams and in different team roles in a variety of settings.
Developing effective teams is critical for providing health care that is patient-centered, safe, timely, effective, efficient, and equitable.[3] See Figure 7.5[4] for an image illustrating interprofessional teamwork.

Nurses collaborate with the interprofessional team by not only assigning and coordinating tasks, but also by promoting solid teamwork in a positive environment. A nursing leader, such as a charge nurse, identifies gaps in workflow, recognizes when task overload is occurring, and promotes the adaptability of the team to respond to evolving patient conditions. Qualities of a successful team are described in the following box.[5]
Qualities of A Successful Team[6]
- Promote a respectful atmosphere
- Define clear roles and responsibilities for team members
- Regularly and routinely share information
- Encourage open communication
- Implement a culture of safety
- Provide clear directions
- Share responsibility for team success
- Balance team member participation based on the current situation
- Acknowledge and manage conflict
- Enforce accountability among all team members
- Communicate the decision-making process
- Facilitate access to needed resources
- Evaluate team outcomes and adjust as needed
TeamSTEPPS®
TeamSTEPPS® is an evidence-based framework used to optimize team performance across the health care system. It is a mnemonic standing for Team Strategies and Tools to Enhance Performance and Patient Safety. The Agency for Healthcare Research and Quality (AHRQ) and the Department of Defense (DoD) developed the TeamSTEPPS® framework as a national initiative to improve patient safety by improving teamwork skills and communication.[7]
View this video about the TeamSTEPPS® framework[8]:
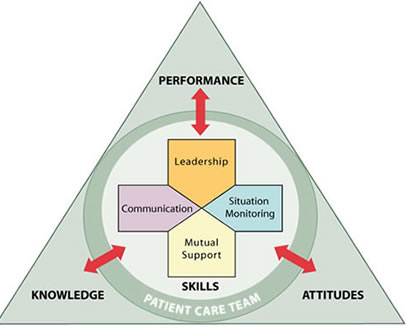
TeamSTEPPS® is based on establishing team structure and four teamwork skills: communication, leadership, situation monitoring, and mutual support.[9] See Figure 7.6[10] for an image of the TeamSTEPPS® framework followed by a description of each TeamSTEPPS® skill. The components of this model are described in the following subsections.
Team Structure
A nursing leader establishes team structure by assigning or identifying team members’ roles and responsibilities, holding team members accountable, and including clients and families as part of the team.
Communication
Communication is the first skill of the TeamSTEPPS® framework. As previously discussed, it is defined as a “structured process by which information is clearly and accurately exchanged among team members.” All team members should use these skills to ensure accurate interprofessional communication:
- Provide brief, clear, specific, and timely information to other team members.
- Seek information from all available sources.
- Use ISBARR and handoff techniques to communicate effectively with team members.
- Use closed-loop communication to verify information is communicated, understood, and completed.
- Document appropriately to facilitate continuity of care across interprofessional team members.
These communication strategies are further described in the “Interprofessional Communication” section of this chapter.
Leadership
Leadership is the second skill of the TeamSTEPPS® framework. As previously discussed, it is defined as the “ability to maximize the activities of team members by ensuring that team actions are understood, changes in information are shared, and team members have the necessary resources.” An example of a nursing team leader in an inpatient setting is the charge nurse.
Effective team leaders demonstrate the following responsibilities[11]:
- Organize the team.
- Identify and articulate clear goals (i.e., share the plan).
- Assign tasks and responsibilities.
- Monitor and modify the plan and communicate changes.
- Review the team’s performance and provide feedback when needed.
- Manage and allocate resources.
- Facilitate information sharing.
- Encourage team members to assist one another.
- Facilitate conflict resolution in a learning environment.
- Model effective teamwork.
Three major leadership tasks include sharing a plan, monitoring and modifying the plan according to situations that occur, and reviewing team performance. Tools to perform these tasks are discussed in the following subsections.
Sharing the Plan
Nursing team leaders identify and articulate clear goals to the team at the start of the shift during inpatient care using a “brief.” The brief is a short session to share a plan, discuss team formation, assign roles and responsibilities, establish expectations and climate, and anticipate outcomes and contingencies. See a Brief Checklist in the following box with questions based on TeamSTEPPS®.[12]
Brief Checklist
During the brief, the team should address the following questions[13]:
___ Who is on the team?
___ Do all members understand and agree upon goals?
___ Are roles and responsibilities understood?
___ What is our plan of care?
___ What are staff and provider’s availability throughout the shift?
___ How is workload shared among team members?
___ Who are the sickest clients on the unit?
___ Which clients have a high fall risk or require 1:1?
___ Do any clients have behavioral issues requiring consistent approaches by the team?
___ What resources are available?
Monitoring and Modifying the Plan
Throughout the shift, it is often necessary for the nurse leader to modify the initial plan as patient situations change on the unit. A huddle is a brief meeting before and/or during a shift to establish situational awareness, reinforce plans already in place, and adjust the teamwork plan as needed. Read more about situational awareness in the “Situation Monitoring” subsection below.
Reviewing the Team’s Performance
When a significant or emergent event occurs during a shift, such as a “code,” it is important to later review the team’s performance and reflect on lessons learned by holding a “debrief” session. A debrief is an informal information exchange session designed to improve team performance and effectiveness through reinforcement of positive behaviors and reflection on lessons learned.[14] See the following box for a Debrief Checklist.
Debrief Checklist[15]
The team should address the following questions during a debrief:
___ Was communication clear?
___ Were roles and responsibilities understood?
___ Was situation awareness maintained?
___ Was workload distribution equitable?
___ Was task assistance requested or offered?
___ Were errors made or avoided?
___ Were resources available?
___ What went well?
___ What should be improved?
Situation Monitoring
Situation monitoring is the third skill of the TeamSTEPPS® framework and defined as the “process of actively scanning and assessing situational elements to gain information or understanding, or to maintain awareness to support team functioning.” Situation monitoring refers to the process of continually scanning and assessing the situation to gain and maintain an understanding of what is going on around you. Situation awareness refers to a team member knowing what is going on around them. The team leader creates a shared mental model to ensure all team members have situation awareness and know what is going on as situations evolve. The STEP tool is used by team leaders to assist with situation monitoring.[16]
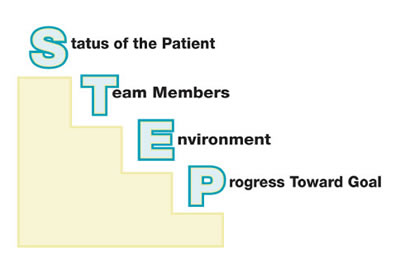
STEP
The STEP tool is a situation monitoring tool used to know what is going on with you, your patients, your team, and your environment. STEP stands for Status of the patients, Team members, Environment, and Progress toward goal. See an illustration of STEP in Figure 7.7.[17] The components of the STEP tool are described in the following box.[18]
STEP Tool[19]
Status of Patients: “What is going on with your patients?”
__ Patient History
__ Vital Signs
__ Medications
__ Physical Exam
__ Plan of Care
__ Psychosocial Issues
Team Members: “What is going on with you and your team?”(See the “I’M SAFE Checklist” below.)
__ Fatigue
__ Workload
__ Task Performance
__ Skill
__ Stress
Environment: Knowing Your Resources
__ Facility Information
__ Administrative Information
__ Human Resources
__ Triage Acuity
__ Equipment
Progression Towards Goal:
__ Status of the Team’s Patients
__ Established Goals of the Team
__ Tasks/Actions of the Team
__ Appropriateness of the Plan and are Modifications Needed?
Cross-Monitoring
As the STEP tool is implemented, the team leader continues to cross monitor to reduce the incidence of errors. Cross-monitoring includes the following[20]:
- Monitoring the actions of other team members.
- Providing a safety net within the team.
- Ensuring that mistakes or oversights are caught quickly and easily.
- Supporting each other as needed.
I’M SAFE Checklist
The I’M SAFE mnemonic is a tool used to assess one’s own safety status, as well as that of other team members in their ability to provide safe patient care. See the I’M SAFE Checklist in the following box.[21] If a team member feels their ability to provide safe care is diminished because of one of these factors, they should notify the charge nurse or other nursing supervisor. In a similar manner, if a nurse notices that another member of the team is impaired or providing care in an unsafe manner, it is an ethical imperative to protect clients and report their concerns according to agency policy.[22]
I’m SAFE Checklist[23]
__ I: Illness
__M: Medication
__S: Stress
__A: Alcohol and Drugs
__F: Fatigue
__E: Eating and Elimination
Read an example of a nursing team leader performing situation monitoring using the STEP tool in the following box.
Example of Situation Monitoring
Two emergent situations occur simultaneously on a busy medical-surgical hospital unit as one patient codes and another develops a postoperative hemorrhage. The charge nurse is performing situation monitoring by continually scanning and assessing the status of all patients on the unit and directing additional assistance where it is needed. Each nursing team member maintains situation awareness by being aware of what is happening on the unit, in addition to caring for the patients they have been assigned. The charge nurse creates a shared mental model by ensuring all team members are aware of their evolving responsibilities as the situation changes. The charge nurse directs additional assistance to the emergent patients while also ensuring appropriate coverage for the other patients on the unit to ensure all patients receive safe and effective care.
For example, as the “code” is called, the charge nurse directs two additional nurses and two additional assistive personnel to assist with the emergent patients while the other nurses and assistive personnel are directed to “cover” the remaining patients, answer call lights, and assist patients to the bathroom to prevent falls. Additionally, the charge nurse is aware that after performing a few rounds of CPR for the coding patient, the assistive personnel must be switched with another team member to maintain effective chest compressions. As the situation progresses, the charge nurse evaluates the status of all patients and makes adjustments to the plan as needed.
Mutual Support
Mutual support is the fourth skill of the TeamSTEPPS® framework and defined as the “ability to anticipate and support team members’ needs through accurate knowledge about their responsibilities and workload.” Mutual support includes providing task assistance, giving feedback, and advocating for patient safety by using assertive statements to correct a safety concern. Managing conflict is also a component of supporting team members’ needs.
Task Assistance
Helping other team members with tasks builds a strong team. Task assistance includes the following components[24]:
- Team members protect each other from work-overload situations.
- Effective teams place all offers and requests for assistance in the context of patient safety.
- Team members foster a climate where it is expected that assistance will be actively sought and offered.
Example of Task Assistance
In a previous example, one patient on the unit was coding while another was experiencing a postoperative hemorrhage. After the emergent care was provided and the hemorrhaging patient was stabilized, Sue, the nurse caring for the hemorrhaging patient, finds many scheduled medications for her other patients are past due. Sue reaches out to Sam, another nurse on the team, and requests assistance. Sam agrees to administer a scheduled IV antibiotic to a stable third patient so Sue can administer oral medications to her remaining patients. Sam knows that on an upcoming shift, he may need to request assistance from Sue when unexpected situations occur. In this manner, team members foster a climate where assistance is actively sought and offered to maintain patient safety.
Feedback
Feedback is provided to a team member for the purpose of improving team performance. Effective feedback should follow these parameters[25]:
- Timely: Provided soon after the target behavior has occurred.
- Respectful: Focused on behaviors, not personal attributes.
- Specific: Related to a specific task or behavior that requires correction or improvement.
- Directed towards improvement: Suggestions are made for future improvement.
- Considerate: Team members’ feelings should be considered and privacy provided. Negative information should be delivered with fairness and respect.
Advocating for Safety with Assertive Statements
When a team member perceives a potential patient safety concern, they should assertively communicate with the decision-maker to protect patient safety. This strategy holds true for ALL team members, no matter their position within the hierarchy of the health care environment. The message should be communicated to the decision-maker in a firm and respectful manner using the following steps[26]:
- Make an opening.
- State the concern.
- State the problem (real or perceived).
- Offer a solution.
- Reach agreement on next steps.
Examples of Using Assertive Statements to Promote Patient Safety
A nurse notices that a team member did not properly wash their hands during patient care. Feedback is provided immediately in a private area after the team member left the patient room: “I noticed you didn’t wash your hands when you entered the patient’s room. Can you help me understand why that didn’t occur?” (Wait for an answer.) “Performing hand hygiene is essential for protecting our patients from infection. It is also hospital policy, and we are audited for compliance to this policy. Let me know if you have any questions and I will check back with you later in the shift.” (Monitor the team member for appropriate hand hygiene for the remainder of the shift.)
Two-Challenge Rule
When an assertive statement is ignored by the decision-maker, the team member should assertively voice their concern at least two times to ensure that it has been heard by the decision-maker. This strategy is referred to as the two-challenge rule. When this rule is adopted as a policy by a health care organization, it empowers all team members to pause care if they sense or discover an essential safety breach. The decision-maker being challenged is expected to acknowledge the concern has been heard.[27]
CUS Assertive Statements
During emergent situations, when stress levels are high or when situations are charged with emotion, the decision-maker may not “hear” the message being communicated, even when the two-challenge rule is implemented. It is helpful for agencies to establish assertive statements that are well-recognized by all staff as implementation of the two-challenge rule. These assertive statements are referred to as the CUS mnemonic: “I am Concerned – I am Uncomfortable – This is a Safety issue!”[28] See Figure 7.8[29] for an illustration of CUS assertive statements.

Using these scripted messages may effectively catch the attention of the decision-maker. However, if the safety issue still isn’t addressed after the second statement or the use of “CUS” assertive statements, the team member should take a stronger course of action and utilize the agency’s chain of command. For the two-challenge rule and CUS assertive statements to be effective within an agency, administrators must support a culture of safety and emphasize the importance of these initiatives to promote patient safety.
Read an example of a nurse using assertive statements in the following box.
Assertive Statement Example
A nurse observes a new physician resident preparing to insert a central line at a patient’s bedside. The nurse notes the resident has inadvertently contaminated the right sterile glove prior to insertion.
Nurse: “Dr. Smith, I noticed that you contaminated your sterile gloves when preparing the sterile field for central line insertion. I will get a new set of sterile gloves for you.”
Dr. Smith: (Ignores nurse and continues procedure.)
Nurse: “Dr. Smith, please pause the procedure. I noticed that you contaminated your right sterile glove by touching outside the sterile field. I will get a new set of sterile gloves for you.”
Dr. Smith: “My gloves are fine.” (Prepares to initiate insertion.)
Nurse: “Dr. Smith – I am concerned! I am uncomfortable! This is a safety issue!”
Dr. Smith: (Stops procedure, looks up, and listens to the nurse.) “I’ll wait for that second pair of gloves.”
Managing Conflict
Conflict is not uncommon on interprofessional teams, especially when there are diverse perspectives from multiple staff regarding patient care. Nurse leaders must be prepared to manage conflict to support the needs of their team members.
When conflict occurs, the DESC tool can be used to help resolve conflict by using “I statements.” DESC is a mnemonic that stands for the following[30]:
- D: Describe the specific situation or behavior; provide concrete data.
- E: Express how the situation makes you feel/what your concerns are using “I” statements.
- S: Suggest other alternatives and seek agreement.
- C: Consequences stated in terms of impact on established team goals while striving for consensus.
The DESC tool should be implemented in a private area with a focus on WHAT is right, not WHO is right. Read an example of a nurse using the DESC tool in the following box.
Example of Using the DESC Tool[31]
Situation: A physician became angry at a nurse who was inserting a patient’s Foley catheter and yelled at the nurse in front of the patient and other team members. The nurse later addressed the physician in a private area outside the patient’s room using the DESC tool and “I statements”:
D: “I noticed you got angry at me when I inserted the patient’s Foley catheter.”
E: “I’m concerned how you addressed that issue in front of the patient and three other staff members. It made me feel bad in front of the patient and my colleagues.”
S: “In the future, if you have an issue with how I do things, please pull me aside privately to discuss your concern.”
C: “Our organization has a policy for managing communication challenges among team members if we can’t agree on this alternative.”
Managing interpersonal conflict resolution is described further in the “Conflict Resolution” section.
View a detailed video webinar describing the TeamSTEPPS® principles.[32]
Team Qualitities Case Application
Mary is recovering from a stroke and requires comprehensive care involving multiple disciplines. Her care team has scheduled interdisciplinary team meetings twice a week to discussion Mary’s progress, adjust her care plan, and address any concerns. Dr. Patel is Mary’s primary physician and consults with Chris (physical therapist) and Emily (speech therapist) before making any changes to Mary’s medication that might affect her therapy sessions. Chris and Emily coordinate their therapy schedules to help maximize Mary’s participation and avoid conflicting sessions and fatigue. Laura is Mary’s social worker and has a large roster of patients. Laura struggles to include Mary’s family in the discharge planning discussions but feels that she has identified an appropriate facility that Mary and her family will be receptive to for discharge. She moves forward with the patient placement paperwork. Lisa is Mary’s dietician, and she has identified a dietary plan that will best contribute to Mary’s nutritional needs and healing. She acknowledges that Mary’s dietary preferences are much different than what she has selected in her dietary plan, but Lisa knows that she has identified the best dietary plan to meet Mary’s energy needs.
Identify which team members are demonstrating team success strategies and how they are demonstrated?
Which team members are not demonstrating team success strategies? How could these team members modify their approach?
Media Attributions
- 400845937-huge
- tslogo1med
- stepfig1
- cusfig1
- Interprofessional Education Collaborative. IPEC core competencies. https://www.ipecollaborative.org/ipec-core-competencies ↵
- Interprofessional Education Collaborative. IPEC core competencies. https://www.ipecollaborative.org/ipec-core-competencies ↵
- Interprofessional Education Collaborative Expert Panel. (2011). Core competencies for interprofessional collaborative practice: Report on an expert panel. Interprofessional Education Collaborative. https://ipec.memberclicks.net/assets/2011-Original.pdf ↵
- “400845937-huge.jpg” by Flamingo Images is used under license from Shutterstock.com ↵
- O’Daniel, M., & Rosenstein, A. H. (2011). Professional communication and team collaboration. In: Hughes R.G. (Ed.). Patient safety and quality: An evidence-based handbook for nurses. Agency for Healthcare Research and Quality (US); Chapter 33. https://www.ncbi.nlm.nih.gov/books/NBK2637 ↵
- O’Daniel, M., & Rosenstein, A. H. (2011). Professional communication and team collaboration. In: Hughes R.G. (Ed.). Patient safety and quality: An evidence-based handbook for nurses. Agency for Healthcare Research and Quality (US); Chapter 33. https://www.ncbi.nlm.nih.gov/books/NBK2637 ↵
- AHRQ. (2019, June). TeamSTEPPS 2.0. https://www.ahrq.gov/teamstepps/instructor/index.html ↵
- AHRQ Patient Safety. (2015, April 29). TeamSTEPPS overview [Video]. YouTube. All rights reserved. https://youtu.be/p4n9xPRtSuU ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- “tslogo1med.jpg” by unknown author is licensed under Public Domain. Access for free at https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- “stepfig1.jpg” by unknown author is licensed under Public Domain. Access for free at https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- “cusfig1.jpg” by unknown author is licensed under Public Domain. Access for free at https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ. (2020, January). Pocket guide: TeamSTEPPS. https://www.ahrq.gov/teamstepps/instructor/essentials/pocketguide.html ↵
- AHRQ Patient Safety. (2017, July 26). Introduction to the fundamentals of TeamSTEPPS® concepts and tools [Video]. YouTube. Video in the Public Domain. https://youtu.be/fxlRtpzsUug ↵
Pharmacodynamics
So far in this chapter, we have learned the importance of pharmacokinetics in how the body absorbs, distributes, metabolizes, and excretes a medication. Now let's consider how drugs act on target sites of action in the body, referred to as pharmacodynamics.
Mechanism of action is a medical term that describes how a medication works in the body. For example, did you know that an osmotic laxative like magnesium citrate attracts and binds with water? The mechanism of action for this medication is it pulls water into the bowel, which softens stool and increases the likelihood of a bowel movement.
A drug’s mechanism of action may refer to how it affects a specific receptor. Many drugs bind to specific receptors on the surface of cells to cause an action. For example, morphine binds to a specific receptor that inhibits transmission of nerve impulses along the pain pathway and decreases a client's feelings of pain.
Other medications inhibit specific enzymes for a desired effect. For example, earlier in this chapter we discussed how monoamine oxidase inhibitors (MAOIs) are prescribed as antidepressants because they block monoamine oxidase, the enzyme that breaks down serotonin and dopamine. This blockage increases the concentration of serotonin and dopamine in the central nervous system and increases a client's feelings of pleasure.
Agonist and Antagonist Actions
Drugs have agonistic or antagonistic effects on receptor sites. An agonist binds tightly to a receptor to produce a desired effect. An antagonist competes with other molecules and blocks a specific action or response at a receptor site. See Figure 1.7[1] for an illustration of how a beta-blocker, an antagonist cardiac medication, blocks specific action on the beta receptors of a cardiac cell.
Agonistic and antagonistic effects on receptors for common classes of medications are further discussed in the “Autonomic Nervous System” chapter.
Critical Thinking Activity 1.7
Atenolol (Tenormin) is an antagonist medication. Does the nurse anticipate this will cause a specific action or block a specific action at a receptor site?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" section at the end of the book.
Assessments Prior to Injection Administration
When administering any parenteral injection, the nurse assesses the patient prior to administration for safe medication administration. See Table 18.7 to review assessments prior to medication administration.
Table 18.7 Assessments Prior to Injection Administration
| Assessment | Rationale/Considerations |
|---|---|
| Check the MAR with the written medication prescription for accuracy and completeness. | Prevent medication errors. |
| Perform the rights of medication administration, including patient’s name, medication name and dose, route, time of administration, and verify the expiration date. | Prevent medication errors. Discard medication if expired. |
| Label syringes with medication names as you prepare them. | Label syringes during the procedure to administer medications safely according to The Joint Commission.[2] |
| Assess and review a patient's current medical condition, past medical history, and medication history. | Identify the need for the medication, as well as any possible contraindications for the administration of prescribed medication to the specific patient. |
| Assess the patient's history of medication allergies or nondrug allergies that may interfere with the medication. If there is a history of allergic reactions, document the type of reaction if possible (e.g., hives, rash, swelling, difficulty breathing). If there is an allergy to prescriber medication, do not prepare it and notify the prescribing provider. | Safely administer medication. |
| Review a current, evidence-based drug reference to determine medication action, indication for medication, normal dosage range, and potential side effects. Identify peak and onset times, as well as any nursing considerations. | Safely administer medication and plan to monitor the patient’s response. For example, by knowing the peak onset of fast-acting insulin, the nurse anticipates when the patient may be most at risk for a hypoglycemic reaction. |
| Review and assess pertinent laboratory results (i.e., blood glucose, partial thromboplastin time). Be aware of abnormal kidney and liver function results because they may affect metabolism of medication. Notify the prescriber of any concerns. | Collect data to determine if the medication should be withheld to ensure proper dosage and to establish a baseline for measuring the patient’s response to the drug. |
| Observe the patient’s verbal and nonverbal reactions to the injection. | Be aware of the patient’s level of anxiety and use distractions and other therapeutic techniques to reduce pain and anxiety. |
| Perform patient assessments, such as vital signs, lung sounds, or pain level, as indicated, prior to medication administration. | Obtain baseline data to ensure medication administration is appropriate at this time and to establish a baseline for measuring the patient’s response to the medication. |
| Assess for contraindications to subcutaneous or intramuscular injections such as muscle atrophy or decreased blood flow to the tissue. | Assess for contraindications because reduced muscle and blood flow interfere with the drug absorption and distribution. |
| Assess the patient’s knowledge of the medication. | Perform patient education about the medication as needed. |
| Assess the skin and tissue quality around the area of the intended injection site. Note any bruising, nonintact skin, abrasions, masses, or scar tissue. Avoid these areas and choose another recommended location. | Assess skin and tissue quality to avoid unnecessary or further injury to the already compromised skin integrity. Areas that are scarred or atrophied can affect the absorption and distribution of the medication. |
Evaluation
Nurses evaluate for possible complications of parenteral medication administration that may occur as a result of a medication error or as an adverse reaction. Complications may occur if a medication is prepared incorrectly, if the medication is injected incorrectly, or if an adverse effect occurs after the medication is injected. Unexpected outcomes can occur such as nerve or tissue damage, ineffective absorption of the medication, pain, bleeding, or infection.
An adverse reaction may develop as a result of an injected medication. An adverse reaction may also occur despite appropriate administration of medication and can happen for various reasons. A reaction may be evident within minutes or days after the exposure to the injectable medication. An unexpected outcome may range from a minor reaction, like a skin rash, to serious and life-threatening events such as anaphylaxis, hemorrhaging, and even death.
If a suspected complication occurs during administration, immediately stop the injection. Assess and monitor vital signs, notify the health care provider, and document an incident report.
Assessments Prior to Injection Administration
When administering any parenteral injection, the nurse assesses the patient prior to administration for safe medication administration. See Table 18.7 to review assessments prior to medication administration.
Table 18.7 Assessments Prior to Injection Administration
| Assessment | Rationale/Considerations |
|---|---|
| Check the MAR with the written medication prescription for accuracy and completeness. | Prevent medication errors. |
| Perform the rights of medication administration, including patient’s name, medication name and dose, route, time of administration, and verify the expiration date. | Prevent medication errors. Discard medication if expired. |
| Label syringes with medication names as you prepare them. | Label syringes during the procedure to administer medications safely according to The Joint Commission.[3] |
| Assess and review a patient's current medical condition, past medical history, and medication history. | Identify the need for the medication, as well as any possible contraindications for the administration of prescribed medication to the specific patient. |
| Assess the patient's history of medication allergies or nondrug allergies that may interfere with the medication. If there is a history of allergic reactions, document the type of reaction if possible (e.g., hives, rash, swelling, difficulty breathing). If there is an allergy to prescriber medication, do not prepare it and notify the prescribing provider. | Safely administer medication. |
| Review a current, evidence-based drug reference to determine medication action, indication for medication, normal dosage range, and potential side effects. Identify peak and onset times, as well as any nursing considerations. | Safely administer medication and plan to monitor the patient’s response. For example, by knowing the peak onset of fast-acting insulin, the nurse anticipates when the patient may be most at risk for a hypoglycemic reaction. |
| Review and assess pertinent laboratory results (i.e., blood glucose, partial thromboplastin time). Be aware of abnormal kidney and liver function results because they may affect metabolism of medication. Notify the prescriber of any concerns. | Collect data to determine if the medication should be withheld to ensure proper dosage and to establish a baseline for measuring the patient’s response to the drug. |
| Observe the patient’s verbal and nonverbal reactions to the injection. | Be aware of the patient’s level of anxiety and use distractions and other therapeutic techniques to reduce pain and anxiety. |
| Perform patient assessments, such as vital signs, lung sounds, or pain level, as indicated, prior to medication administration. | Obtain baseline data to ensure medication administration is appropriate at this time and to establish a baseline for measuring the patient’s response to the medication. |
| Assess for contraindications to subcutaneous or intramuscular injections such as muscle atrophy or decreased blood flow to the tissue. | Assess for contraindications because reduced muscle and blood flow interfere with the drug absorption and distribution. |
| Assess the patient’s knowledge of the medication. | Perform patient education about the medication as needed. |
| Assess the skin and tissue quality around the area of the intended injection site. Note any bruising, nonintact skin, abrasions, masses, or scar tissue. Avoid these areas and choose another recommended location. | Assess skin and tissue quality to avoid unnecessary or further injury to the already compromised skin integrity. Areas that are scarred or atrophied can affect the absorption and distribution of the medication. |
Evaluation
Nurses evaluate for possible complications of parenteral medication administration that may occur as a result of a medication error or as an adverse reaction. Complications may occur if a medication is prepared incorrectly, if the medication is injected incorrectly, or if an adverse effect occurs after the medication is injected. Unexpected outcomes can occur such as nerve or tissue damage, ineffective absorption of the medication, pain, bleeding, or infection.
An adverse reaction may develop as a result of an injected medication. An adverse reaction may also occur despite appropriate administration of medication and can happen for various reasons. A reaction may be evident within minutes or days after the exposure to the injectable medication. An unexpected outcome may range from a minor reaction, like a skin rash, to serious and life-threatening events such as anaphylaxis, hemorrhaging, and even death.
If a suspected complication occurs during administration, immediately stop the injection. Assess and monitor vital signs, notify the health care provider, and document an incident report.
Checklist for Parenteral Site Identification
Use the checklist below to review the steps for completion of "Parenteral Site Identification."
Directions: Identify parenteral injection sites, needle size/gauge, injection angle, and the appropriate amount that can be administered in each of the parenteral routes: intradermal, subcutaneous, and intramuscular.
- Describe the appropriate needle gauge, length, number of cc's, and angle for an intradermal injection:
- 25-27G
- 3/8” to 5/8”
- 0.1 mL (for TB testing)
- 5- to 15-degree angle
- Demonstrate locating the intradermal injection sites on a peer:
- Inner surface of the forearm
- Outer aspects upper arms
- Upper back below scapula
- Describe the appropriate needle gauge, length, number of mL, and angle for a subcutaneous injection:
- 25-31G
- ½” to 5/8”
- Up to 1 mL
- 45- to 90-degree angle
- Demonstrate locating the subcutaneous injection sites on a peer:
- Anterior thighs
- Abdomen
- Describe the appropriate needle gauge, length, number of mL, and angle for an adult intramuscular:
- 18-25G
- ½” - 1 ½” (based on age/size of patient and site used)
- <0.5 - 1 mL (infants and children), 2-3 mL (adults)
- 90-degree angle
- Demonstrate locating the intramuscular injection sites on a peer:
- Ventrogluteal
- Vastus lateralis
- Deltoid
- Explain how you would modify assessment techniques to reflect variations across the life span and body size variations.
Checklist for Parenteral Medication Injections
Use the checklist below to review the steps for completion of "Parenteral Medication Injections."
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
Special Considerations:
- Plan medication administration to avoid disruption.
- Dispense medication in a quiet area.
- Avoid conversation with others.
- Follow agency's no-interruption zone policy.
- Prepare medications for ONE patient at a time.
- Plan for disposal of sharps in an appropriate sharps disposal container.
- Check the orders and MAR for accuracy and completeness; clarify any unclear orders.
- Review pertinent information related to the medications: labs, last time medication was given, and medication information: generic name, brand name, dose, route, time, class, action, purpose, side effects, contraindications, and nursing considerations.
- Gather available supplies: correctly sized syringes and needles appropriate for medication, patient's size, and site of injection; diluent (if required); tape or patient label for each syringe; nonsterile gloves; sharps container; and alcohol wipes.
- Perform hand hygiene.
- While withdrawing medication from the medication dispensing system, perform the first check of the six rights of medication administration. Check expiration date and perform any necessary calculations.
Preparing the Medication for Administration
- Scrub the top of the vial of the correct medication. State the correct dose to be drawn.
- Remove the cap from the needle. Pull back on the plunger to draw air into the syringe equal to the dose.
- With the vial on a flat surface, insert the needle. Invert the vial and withdraw the correct amount of the medication. Expel any air bubbles. Remove the needle from the vial.
- Using the scoop method, recap the needle.
- Perform the second check of the six rights of medication administration, looking at the vial, syringe, and MAR.
- Label the syringe with the name of the drug and dose.
Additional Preparation Steps When Mixing Two Types of Insulin in One Syringe: Intermediate-Acting (NPH) and Short-Acting (Regular) Insulins
- Place the vials side by side on a flat surface: NPH on left and regular insulin on the right.
- Roll the NPH insulin between your hands to mix the solution. With an alcohol pad, scrub off the vial top of the NPH insulin. Using a new alcohol pad, scrub the vial top of the regular insulin. Discard any prep pads.
- Select the correct insulin syringe that will exactly measure the TOTAL dose of the amount of NPH and regular doses (30- and 50-unit syringes measure single units; 100-unit syringes only measure even numbered doses).
- Pull back on the plunger to draw air into the syringe equal to the dose of NPH insulin.
- With the NPH vial on a flat surface, remove the cap from the syringe, insert the needle into the NPH vial, and inject air. Do not let the tip of the needle touch the insulin solution. Withdraw the needle.
- Pull back on the plunger to draw air into the syringe equal to the dose of the regular insulin.
- With the regular vial on a flat surface, insert the needle into the regular vial, and inject air.
- With the needle still in the vial, invert the regular insulin vial and withdraw the correct dose. Remove the needle from the vial. Cap the needle using the scoop method.
- Roll the NPH insulin vial between your hands to mix the solution. Uncap the needle and insert the needle into the NPH insulin vial. Withdraw the correct amount of NPH insulin. Withdraw the needle and recap using the scoop method.
- Perform the second medication check of the combined dose looking at the vial, syringe, and MAR, verifying all the rights.
- Label the syringe with the name of the combined medications and doses.
Alternative Preparation Using an Insulin Pen
- Select the correct insulin pen to be used for the injection. Identify the dose to be given.
- Remove the cap from the insulin pen and clean the top (hub) with an alcohol prep pad. Attach the insulin pen needle without contaminating the needle or pen hub.
- Turn the dial to two units and with the pen pointing upward, push the injection button to prime the pen.
- Turn the dial to the correct dose.
- Perform the second medication check looking at the insulin pen and MAR, verifying all the rights.
Administration of Parenteral Medication
- Knock, enter the room, greet the patient, and provide for privacy.
- Perform safety steps:
- Perform hand hygiene.
- Check the room for transmission-based precautions.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain the process to the patient and ask if they have any questions.
- Be organized and systematic.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure the patient's privacy and dignity.
- Assess ABCs.
- Perform the third check of the six rights of medication administration at the patient's bedside after performing patient identification.
- Perform the following steps according to the type of parenteral medication.
INTRADERMAL - Administration of a TB Test
- Correctly identify the sites and verbalize the landmarks used for intradermal injections.
- Select the correct site for the TB test, verbalizing the anatomical landmarks and skin considerations.
- Put on nonsterile gloves if contact with blood or body fluids is likely or if your skin or the patient's skin isn't intact.
- Use an alcohol swab in a circular motion to clean the skin at the site; place the pad above the site to mark the site, if desired.
- Gently pull the skin away from the site.
- Insert the needle with the bevel facing upward, slowly at a 5- to 15-degree angle, and then advance no more than an eighth of an inch to cover the bevel.
- Use the thumb of the nondominant hand to push on the plunger to slowly inject the medication. Inspect the site, noting if a small bleb forms under the skin surface.
- Carefully withdraw the needle straight back out of the insertion site so not to disturb the bleb (do not massage or cover the site).
- Activate the safety feature of the needle and place the syringe in the sharps container.
- Teach the patient to return for a TB skin test reading in 48-72 hours and not to press on the site or apply a Band-Aid.
SUBCUTANEOUS - Administration of Insulin in a Syringe
- Correctly identify the sites and verbalize the landmarks used for subcutaneous injections. Ask the patient regarding a preferred site of medication administration.
- Put on nonsterile gloves if contact with blood or body fluids is likely or if your skin or the patient's skin isn't intact.
- Select an appropriate site and clean with an alcohol prep in a circular motion. Place the pad above the site to mark the location, if desired. Remove the cap from the needle without contaminating the needle.
- Pinch approximately an inch of subcutaneous tissue, creating a skinfold.
- Insert the needle at a 90-degree angle, release the patient's skin, and inject the medication. Withdraw the needle.
- Activate the safety feature of the needle and place the syringe in a sharps container.
SUBCUTANEOUS - Administration with an Insulin Pen
- Select the site and clean with an alcohol prep in a circular motion. Place the pad above the site to mark the location, if desired.
- Put on nonsterile gloves if contact with blood or body fluids is likely or if your skin or the patient's skin isn't intact.
- Remove the cap from the needle without contaminating the needle.
- Pinch approximately an inch of subcutaneous tissue, creating a skinfold.
- Insert the needle quickly at a 45- to 90-degree angle (depending upon the size of the patient), continue to hold the skinfold, and inject the medication. After the medication is injected, count to 10, remove the needle, and release the skinfold.
- Dispose of the needle in a sharps container. Replace the top cap to the insulin pen.
INTRAMUSCULAR - Deltoid
- Correctly identify the site and verbalize the landmarks used for a deltoid injection.
- Put on nonsterile gloves if contact with blood or body fluids is likely or if your skin or the patient's skin isn't intact.
- Use an alcohol swab in a circular motion to clean the skin at the site. Place a pad above the site to mark the location. Remove the cap from the needle without contaminating the needle.
- Depending on the muscle mass of the deltoid, either grasp the body of the muscle between the thumb and forefingers of the nondominant hand or spread the skin taut.
- Insert the needle at a 90-degree angle.
- Follow agency policy and manufacturer recommendations regarding aspiration.
- Continue to hold the muscle fold and inject the medication. After the medication is injected, count to 10, remove the needle, and release the muscle fold.
- Activate the safety on the syringe. Place the syringe in a sharps container.
INTRAMUSCULAR - Vastus Lateralis
- Correctly identify the site and verbalize the landmarks to locate the vastus lateralis site.
- Put on nonsterile gloves if contact with blood or body fluids is likely or if your skin or the patient's skin isn't intact.
- Use an alcohol swab in a circular motion to clean the skin at the site. Place the pad above the site to mark the location. Remove the cap from the needle without contaminating the needle.
- Depending on the muscle mass of the vastus lateralis, either grasp the body of the muscle between the thumb and forefingers of the nondominant hand or spread the skin taut.
- Insert the needle at a 90-degree angle.
- Follow agency policy and manufacturer recommendations regarding aspiration.
- Continue to hold the muscle fold and inject the medication. After the medication is injected, count to 10, remove the needle, and release the muscle fold.
- Activate the safety on the syringe. Put the needle in a sharps container.
INTRAMUSCULAR - Ventrogluteal (Using the Z-track Technique)
- Correctly identify and verbalize the landmarks used to locate the ventrogluteal site.
- Put on nonsterile gloves if contact with blood or body fluids is likely or if your skin or the patient's skin isn't intact.
- Use an alcohol swab in a circular motion to clean the skin at the site and place a pad above the site to mark the location. Remove the cap from the needle without contaminating the needle.
- Place the ulnar surface of the hand approximately 1 – 3 inches from the selected site; press down and pull the skin and subcutaneous tissue to the side or downward.
- Maintaining tissue traction, hold the syringe like a dart and insert the needle into the skin at 90 degrees.
- Maintaining tissue traction, use the available thumb and index finger to help stabilize the syringe.
- Follow agency policy and manufacturer recommendations regarding aspiration. If aspiration is required, pull back the plunger and observe for blood return. If there is no blood return, inject the medication. If blood return is observed, remove the needle, and prepare a new medication.
- Maintaining tissue traction, wait 10 seconds with the needle still in the skin to allow the muscle to absorb the medication. Withdraw the needle from the site and then release traction. Do not rub/massage the site.
- Activate the safety feature of the needle; place in a sharps container.
Following Conclusion of All Injections
- Assess site; apply Band-Aid if necessary and appropriate.
- Remove gloves. Perform hand hygiene.
- Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Document medication administered, including the site used for the injection.
View an instructor demonstration of an Intradermal Injection[4]:
View an instructor demonstration of a Subcutaneous Injection (Insulin)[5]:
View an instructor demonstration of an Intramuscular Injection[6]:
View an instructor demonstration of Using an Insulin Pen[7]:
The intramuscular (IM) injection route is used to place medication in muscle tissue. Muscle has an abundant blood supply that allows medications to be absorbed faster than the subcutaneous route.
Factors that influence the choice of muscle to use for an intramuscular injection include the patient’s size, as well as the amount, viscosity, and type of medication. The length of the needle must be long enough to pass through the subcutaneous tissue to reach the muscle, so needles up to 1.5 inches long may be selected. However, if a patient is thin, a shorter needle length is used because there is less fat tissue to advance through to reach the muscle. Additionally, the muscle mass of infants and young children cannot tolerate large amounts of medication volume. Medication fluid amounts up to 0.5-1 mL can be injected in one site in infants and children, whereas adults can tolerate 2-3 mL. Intramuscular injections are administered at a 90-degree angle. Research has found administering medications at 10 seconds per mL is an effective rate for IM injections, but always review the drug administration rate per pharmacy or manufacturer’s recommendations.[8]
Anatomic Sites
Anatomic sites must be selected carefully for intramuscular injections and include the ventrogluteal, vastus lateralis, and the deltoid. The vastus lateralis site is preferred for infants because that muscle is most developed. The ventrogluteal site is generally recommended for IM medication administration in adults, but IM vaccines may be administered in the deltoid site. Additional information regarding injections in each of these sites is provided in the following subsections.
Ventrogluteal
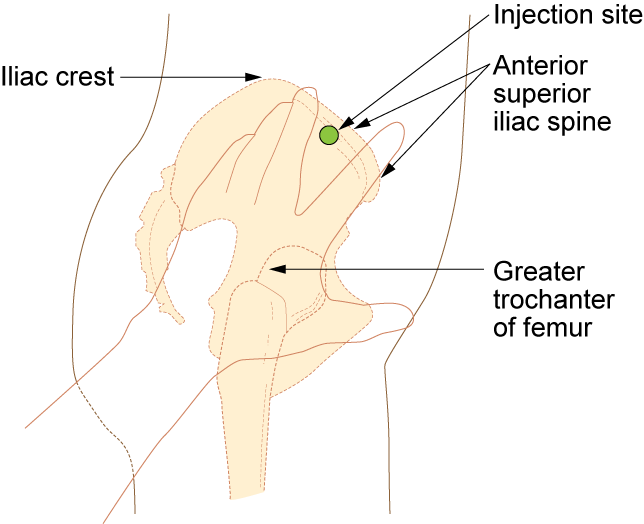
This site involves the gluteus medius and minimus muscle and is the safest injection site for adults and children because it provides the greatest thickness of gluteal muscles, is free from penetrating nerves and blood vessels, and has a thin layer of fat. To locate the ventrogluteal site, place the patient in a supine or lateral position. Use your right hand for the left hip or your left hand for the right hip. Place the heel or palm of your hand on the greater trochanter, with the thumb pointed toward the belly button. Extend your index finger to the anterior superior iliac spine and spread your middle finger pointing towards the iliac crest. Insert the needle into the "V" formed between your index and middle fingers. This is the preferred site for all oily and irritating solutions for patients of any age.[9] See Figure 18.31[10] for an image demonstrating how to accurately locate the ventrogluteal site using your hand.
The needle gauge used at the ventrogluteal site is determined by the solution of the medication ordered. An aqueous solution can be given with a 20- to 25-gauge needle, whereas viscous or oil-based solutions are given with 18- to 21-gauge needles. The needle length is based on patient weight and body mass index. A thin adult may require a 5/8-inch to 1-inch (16 mm to 25 mm) needle, while an average adult may require a 1-inch (25 mm) needle, and a larger adult (over 70 kg) may require a 1-inch to 1½-inch (25 mm to 38 mm) needle. Children and infants require shorter needles. Refer to agency policies regarding needle length for infants, children, and adolescents. Up to 3 mL of medication may be administered in the ventrogluteal muscle of an average adult and up to 1 mL in children. See Figure 18.32[11] for an image of locating the ventrogluteal site on a patient.

Vastus Lateralis
The vastus lateralis site is commonly used for immunizations in infants and toddlers because the muscle is thick and well-developed. This muscle is located on the anterior lateral aspect of the thigh and extends from one hand’s breadth above the knee to one hand’s breadth below the greater trochanter. The outer middle third of the muscle is used for injections. To help relax the patient, ask the patient to lie flat with knees slightly bent or have the patient in a sitting position. See Figure 18.33[12] for an image of the vastus lateralis injection site.
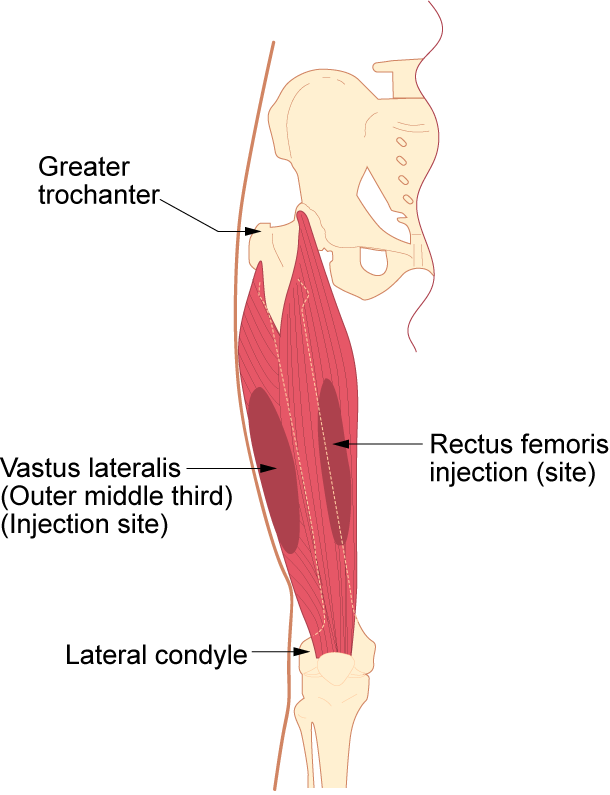
The length of the needle used at the vastus lateralis site is based on the patient’s age, weight, and body mass index. In general, the recommended needle length for an adult is 1 inch to 1 ½ inches (25 mm to 38 mm), but the needle length is shorter for children. Refer to agency policy for pediatric needle lengths. The gauge of the needle is determined by the type of medication administered. Aqueous solutions can be given with a 20- to 25-gauge needle; oily or viscous medications should be administered with 18- to 21-gauge needles. A smaller gauge needle (22 to 25 gauge) should be used with children. The maximum amount of medication for a single injection in an adult is 3 mL. See Figure 18.34[13] for an image of an intramuscular injection being administered at the vastus lateralis site.

Deltoid
The deltoid muscle has a triangular shape and is easy to locate and access. To locate the injection site, begin by having the patient relax their arm. The patient can be standing, sitting, or lying down. To locate the landmark for the deltoid muscle, expose the upper arm and find the acromion process by palpating the bony prominence. The injection site is in the middle of the deltoid muscle, about 1 inch to 2 inches (2.5 cm to 5 cm) below the acromion process. To locate this area, lay three fingers across the deltoid muscle and below the acromion process. The injection site is generally three finger widths below in the middle of the muscle. See Figure 18.35[14] for an illustration for locating the deltoid injection site.
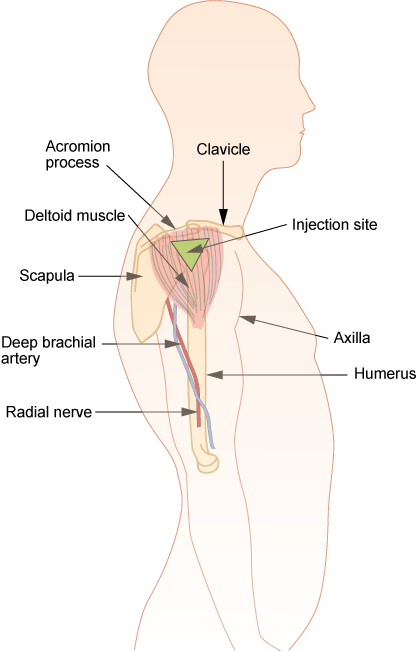
Select the needle length based on the patient’s age, weight, and body mass. In general, for an adult male weighing 60 kg to 118 kg (130 to 260 lbs), a 1-inch (25 mm) needle is sufficient. For women under 60 kg (130 lbs), a ⅝-inch (16 mm) needle is sufficient, while for women between 60 kg and 90 kg (130 to 200 lbs) a 1-inch (25 mm) needle is required. A 1 ½-inch (38 mm) length needle may be required for women over 90 kg (200 lbs) for a deltoid IM injection. For immunizations, a 22- to 25-gauge needle should be used. Refer to agency policy regarding specifications for infants, children, adolescents, and immunizations. The maximum amount of medication for a single injection is generally 1 mL. See Figure 18.36[15] for an image of locating the deltoid injection site on a patient.

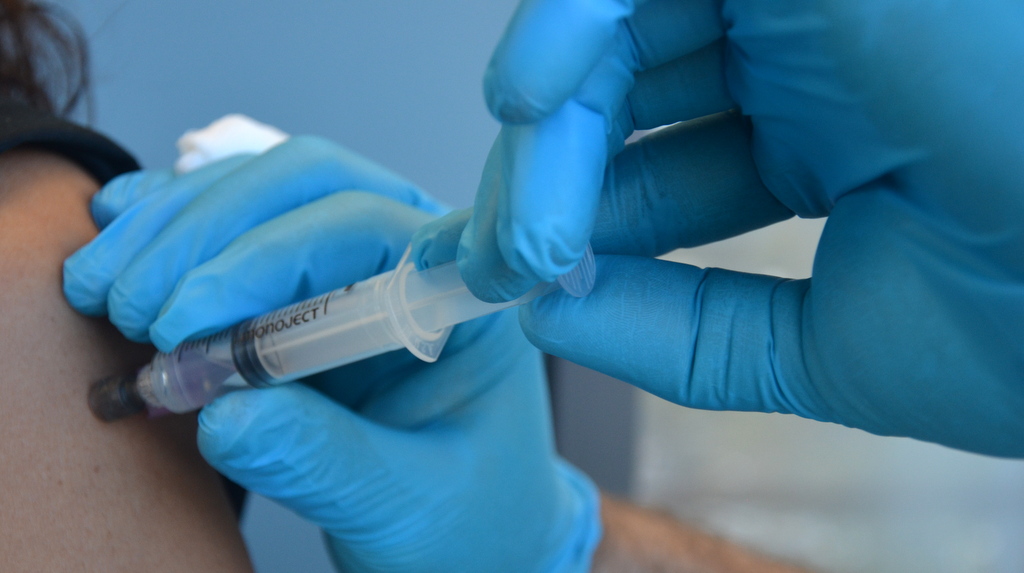
Description of Procedure
When administering an intramuscular injection, the procedure is similar to a subcutaneous injection, but instead of pinching the skin, stabilize the skin around the injection site with your nondominant hand. With your dominant hand, hold the syringe like a dart and insert the needle quickly into the muscle at a 90-degree angle using a steady and smooth motion. After the needle pierces the skin, use the thumb and forefinger of the nondominant hand to hold the syringe. If aspiration is indicated according to agency policy and manufacturer recommendations, pull the plunger back to aspirate for blood. If no blood appears, inject the medication slowly and steadily. If blood appears, discard the syringe and needle and prepare the medication again. See Figure 18.37[16] for an image of aspirating for blood. After the medication is completely injected, leave the needle in place for ten seconds, and then remove the needle using a smooth, steady motion. Remove the needle at the same angle at which it was inserted. Cover the injection site with sterile gauze using gentle pressure and apply a Band-Aid if needed.[17]
Z-track Method for IM injections
Evidence-based practice supports using the Z-track method for administration of intramuscular injections. This method prevents the medication from leaking into the subcutaneous tissue, allows the medication to stay in the muscles, and can minimize irritation.[19]
The Z-track method creates a zigzag path to prevent medication from leaking into the subcutaneous tissue. This method may be used for all injections or may be specified by the medication.
Displace the patient’s skin in a Z-track manner by pulling the skin down or to one side about 1 inch (2 cm) with your nondominant hand before administering the injection. With the skin held to one side, quickly insert the needle at a 90-degree angle. After the needle pierces the skin, continue pulling on the skin with the nondominant hand, and at the same time, grasp the lower end of the syringe barrel with the fingers of the nondominant hand to stabilize it. Move your dominant hand and pull the end of the plunger to aspirate for blood, if indicated. If no blood appears, inject the medication slowly. Once the medication is given, leave the needle in place for ten seconds. After the medication is completely injected, remove the needle using a smooth, steady motion, and then release the skin. See Figure 18.38[20] for an illustration of the Z-track method.
![“Z-track-process-1.png“ and "Z-track-process-3.png" by British Columbia Institute of Technology (BCIT) is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/6-8-iv-push-medications-and-saline-lock-flush/[/footnote] Illustration showing two parts of the Z track method](https://opencontent.ccbcmd.edu/app/uploads/sites/30/2024/08/ztrack-1-1024x409.png)
Special Considerations for IM Injections
- Avoid using sites with atrophied muscle because they will poorly absorb medications.
- If repeated IM injections are given, sites should be rotated to decrease the risk of hypertrophy.
- Older adults and thin patients may only tolerate up to 2 milliliters in a single injection.
- Choose a site that is free from pain, infection, abrasions, or necrosis.
- The dorsogluteal site should be avoided for intramuscular injections because of the risk for injury. If the needle inadvertently hits the sciatic nerve, the patient may experience partial or permanent paralysis of the leg.
The intramuscular (IM) injection route is used to place medication in muscle tissue. Muscle has an abundant blood supply that allows medications to be absorbed faster than the subcutaneous route.
Factors that influence the choice of muscle to use for an intramuscular injection include the patient’s size, as well as the amount, viscosity, and type of medication. The length of the needle must be long enough to pass through the subcutaneous tissue to reach the muscle, so needles up to 1.5 inches long may be selected. However, if a patient is thin, a shorter needle length is used because there is less fat tissue to advance through to reach the muscle. Additionally, the muscle mass of infants and young children cannot tolerate large amounts of medication volume. Medication fluid amounts up to 0.5-1 mL can be injected in one site in infants and children, whereas adults can tolerate 2-3 mL. Intramuscular injections are administered at a 90-degree angle. Research has found administering medications at 10 seconds per mL is an effective rate for IM injections, but always review the drug administration rate per pharmacy or manufacturer’s recommendations.[23]
Anatomic Sites
Anatomic sites must be selected carefully for intramuscular injections and include the ventrogluteal, vastus lateralis, and the deltoid. The vastus lateralis site is preferred for infants because that muscle is most developed. The ventrogluteal site is generally recommended for IM medication administration in adults, but IM vaccines may be administered in the deltoid site. Additional information regarding injections in each of these sites is provided in the following subsections.
Ventrogluteal
This site involves the gluteus medius and minimus muscle and is the safest injection site for adults and children because it provides the greatest thickness of gluteal muscles, is free from penetrating nerves and blood vessels, and has a thin layer of fat. To locate the ventrogluteal site, place the patient in a supine or lateral position. Use your right hand for the left hip or your left hand for the right hip. Place the heel or palm of your hand on the greater trochanter, with the thumb pointed toward the belly button. Extend your index finger to the anterior superior iliac spine and spread your middle finger pointing towards the iliac crest. Insert the needle into the "V" formed between your index and middle fingers. This is the preferred site for all oily and irritating solutions for patients of any age.[24] See Figure 18.31[25] for an image demonstrating how to accurately locate the ventrogluteal site using your hand.
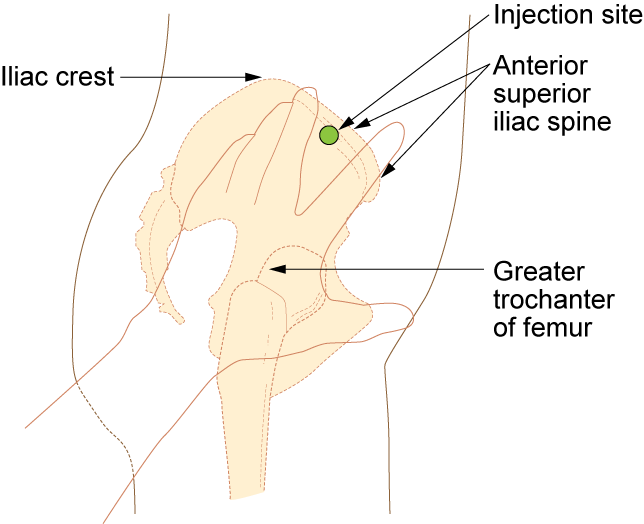
The needle gauge used at the ventrogluteal site is determined by the solution of the medication ordered. An aqueous solution can be given with a 20- to 25-gauge needle, whereas viscous or oil-based solutions are given with 18- to 21-gauge needles. The needle length is based on patient weight and body mass index. A thin adult may require a 5/8-inch to 1-inch (16 mm to 25 mm) needle, while an average adult may require a 1-inch (25 mm) needle, and a larger adult (over 70 kg) may require a 1-inch to 1½-inch (25 mm to 38 mm) needle. Children and infants require shorter needles. Refer to agency policies regarding needle length for infants, children, and adolescents. Up to 3 mL of medication may be administered in the ventrogluteal muscle of an average adult and up to 1 mL in children. See Figure 18.32[26] for an image of locating the ventrogluteal site on a patient.

Vastus Lateralis
The vastus lateralis site is commonly used for immunizations in infants and toddlers because the muscle is thick and well-developed. This muscle is located on the anterior lateral aspect of the thigh and extends from one hand’s breadth above the knee to one hand’s breadth below the greater trochanter. The outer middle third of the muscle is used for injections. To help relax the patient, ask the patient to lie flat with knees slightly bent or have the patient in a sitting position. See Figure 18.33[27] for an image of the vastus lateralis injection site.
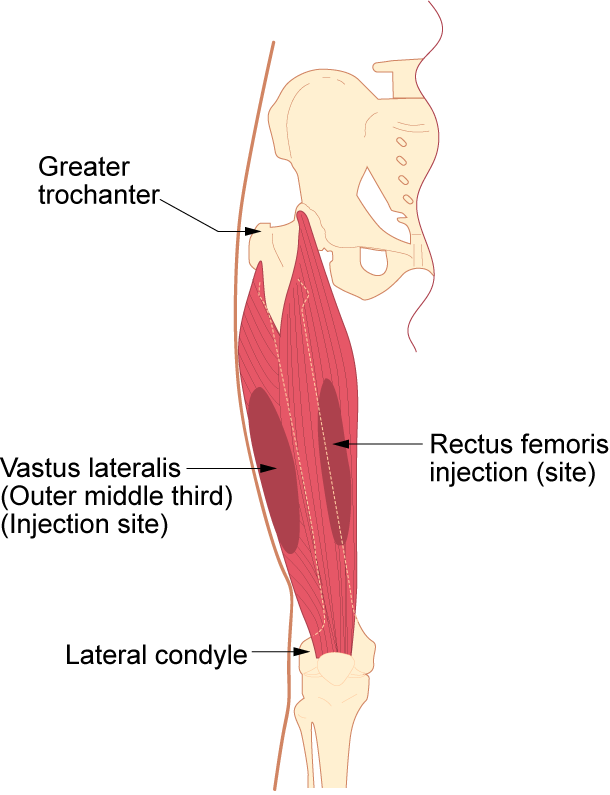
The length of the needle used at the vastus lateralis site is based on the patient’s age, weight, and body mass index. In general, the recommended needle length for an adult is 1 inch to 1 ½ inches (25 mm to 38 mm), but the needle length is shorter for children. Refer to agency policy for pediatric needle lengths. The gauge of the needle is determined by the type of medication administered. Aqueous solutions can be given with a 20- to 25-gauge needle; oily or viscous medications should be administered with 18- to 21-gauge needles. A smaller gauge needle (22 to 25 gauge) should be used with children. The maximum amount of medication for a single injection in an adult is 3 mL. See Figure 18.34[28] for an image of an intramuscular injection being administered at the vastus lateralis site.

Deltoid
The deltoid muscle has a triangular shape and is easy to locate and access. To locate the injection site, begin by having the patient relax their arm. The patient can be standing, sitting, or lying down. To locate the landmark for the deltoid muscle, expose the upper arm and find the acromion process by palpating the bony prominence. The injection site is in the middle of the deltoid muscle, about 1 inch to 2 inches (2.5 cm to 5 cm) below the acromion process. To locate this area, lay three fingers across the deltoid muscle and below the acromion process. The injection site is generally three finger widths below in the middle of the muscle. See Figure 18.35[29] for an illustration for locating the deltoid injection site.
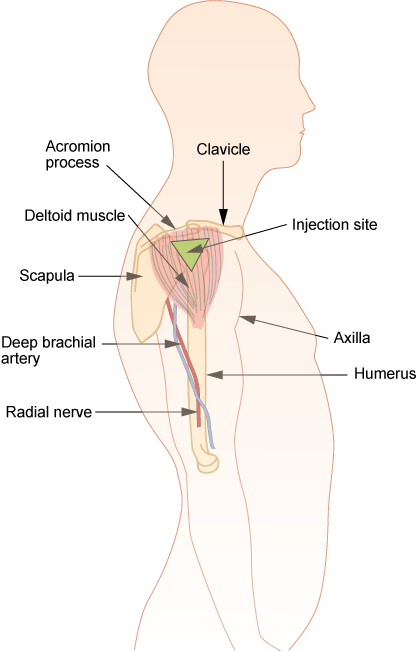
Select the needle length based on the patient’s age, weight, and body mass. In general, for an adult male weighing 60 kg to 118 kg (130 to 260 lbs), a 1-inch (25 mm) needle is sufficient. For women under 60 kg (130 lbs), a ⅝-inch (16 mm) needle is sufficient, while for women between 60 kg and 90 kg (130 to 200 lbs) a 1-inch (25 mm) needle is required. A 1 ½-inch (38 mm) length needle may be required for women over 90 kg (200 lbs) for a deltoid IM injection. For immunizations, a 22- to 25-gauge needle should be used. Refer to agency policy regarding specifications for infants, children, adolescents, and immunizations. The maximum amount of medication for a single injection is generally 1 mL. See Figure 18.36[30] for an image of locating the deltoid injection site on a patient.

Description of Procedure
When administering an intramuscular injection, the procedure is similar to a subcutaneous injection, but instead of pinching the skin, stabilize the skin around the injection site with your nondominant hand. With your dominant hand, hold the syringe like a dart and insert the needle quickly into the muscle at a 90-degree angle using a steady and smooth motion. After the needle pierces the skin, use the thumb and forefinger of the nondominant hand to hold the syringe. If aspiration is indicated according to agency policy and manufacturer recommendations, pull the plunger back to aspirate for blood. If no blood appears, inject the medication slowly and steadily. If blood appears, discard the syringe and needle and prepare the medication again. See Figure 18.37[31] for an image of aspirating for blood. After the medication is completely injected, leave the needle in place for ten seconds, and then remove the needle using a smooth, steady motion. Remove the needle at the same angle at which it was inserted. Cover the injection site with sterile gauze using gentle pressure and apply a Band-Aid if needed.[32]
Z-track Method for IM injections
Evidence-based practice supports using the Z-track method for administration of intramuscular injections. This method prevents the medication from leaking into the subcutaneous tissue, allows the medication to stay in the muscles, and can minimize irritation.[34]
The Z-track method creates a zigzag path to prevent medication from leaking into the subcutaneous tissue. This method may be used for all injections or may be specified by the medication.
Displace the patient’s skin in a Z-track manner by pulling the skin down or to one side about 1 inch (2 cm) with your nondominant hand before administering the injection. With the skin held to one side, quickly insert the needle at a 90-degree angle. After the needle pierces the skin, continue pulling on the skin with the nondominant hand, and at the same time, grasp the lower end of the syringe barrel with the fingers of the nondominant hand to stabilize it. Move your dominant hand and pull the end of the plunger to aspirate for blood, if indicated. If no blood appears, inject the medication slowly. Once the medication is given, leave the needle in place for ten seconds. After the medication is completely injected, remove the needle using a smooth, steady motion, and then release the skin. See Figure 18.38[35] for an illustration of the Z-track method.
![“Z-track-process-1.png“ and "Z-track-process-3.png" by British Columbia Institute of Technology (BCIT) is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/6-8-iv-push-medications-and-saline-lock-flush/[/footnote] Illustration showing two parts of the Z track method](https://opencontent.ccbcmd.edu/app/uploads/sites/30/2024/08/ztrack-1-1024x409.png)
Special Considerations for IM Injections
- Avoid using sites with atrophied muscle because they will poorly absorb medications.
- If repeated IM injections are given, sites should be rotated to decrease the risk of hypertrophy.
- Older adults and thin patients may only tolerate up to 2 milliliters in a single injection.
- Choose a site that is free from pain, infection, abrasions, or necrosis.
- The dorsogluteal site should be avoided for intramuscular injections because of the risk for injury. If the needle inadvertently hits the sciatic nerve, the patient may experience partial or permanent paralysis of the leg.
Checklist for Parenteral Site Identification
Use the checklist below to review the steps for completion of "Parenteral Site Identification."
Directions: Identify parenteral injection sites, needle size/gauge, injection angle, and the appropriate amount that can be administered in each of the parenteral routes: intradermal, subcutaneous, and intramuscular.
- Describe the appropriate needle gauge, length, number of cc's, and angle for an intradermal injection:
- 25-27G
- 3/8” to 5/8”
- 0.1 mL (for TB testing)
- 5- to 15-degree angle
- Demonstrate locating the intradermal injection sites on a peer:
- Inner surface of the forearm
- Outer aspects upper arms
- Upper back below scapula
- Describe the appropriate needle gauge, length, number of mL, and angle for a subcutaneous injection:
- 25-31G
- ½” to 5/8”
- Up to 1 mL
- 45- to 90-degree angle
- Demonstrate locating the subcutaneous injection sites on a peer:
- Anterior thighs
- Abdomen
- Describe the appropriate needle gauge, length, number of mL, and angle for an adult intramuscular:
- 18-25G
- ½” - 1 ½” (based on age/size of patient and site used)
- <0.5 - 1 mL (infants and children), 2-3 mL (adults)
- 90-degree angle
- Demonstrate locating the intramuscular injection sites on a peer:
- Ventrogluteal
- Vastus lateralis
- Deltoid
- Explain how you would modify assessment techniques to reflect variations across the life span and body size variations.
Checklist for Parenteral Medication Injections
Use the checklist below to review the steps for completion of "Parenteral Medication Injections."
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
Special Considerations:
- Plan medication administration to avoid disruption.
- Dispense medication in a quiet area.
- Avoid conversation with others.
- Follow agency's no-interruption zone policy.
- Prepare medications for ONE patient at a time.
- Plan for disposal of sharps in an appropriate sharps disposal container.
- Check the orders and MAR for accuracy and completeness; clarify any unclear orders.
- Review pertinent information related to the medications: labs, last time medication was given, and medication information: generic name, brand name, dose, route, time, class, action, purpose, side effects, contraindications, and nursing considerations.
- Gather available supplies: correctly sized syringes and needles appropriate for medication, patient's size, and site of injection; diluent (if required); tape or patient label for each syringe; nonsterile gloves; sharps container; and alcohol wipes.
- Perform hand hygiene.
- While withdrawing medication from the medication dispensing system, perform the first check of the six rights of medication administration. Check expiration date and perform any necessary calculations.
Preparing the Medication for Administration
- Scrub the top of the vial of the correct medication. State the correct dose to be drawn.
- Remove the cap from the needle. Pull back on the plunger to draw air into the syringe equal to the dose.
- With the vial on a flat surface, insert the needle. Invert the vial and withdraw the correct amount of the medication. Expel any air bubbles. Remove the needle from the vial.
- Using the scoop method, recap the needle.
- Perform the second check of the six rights of medication administration, looking at the vial, syringe, and MAR.
- Label the syringe with the name of the drug and dose.
Additional Preparation Steps When Mixing Two Types of Insulin in One Syringe: Intermediate-Acting (NPH) and Short-Acting (Regular) Insulins
- Place the vials side by side on a flat surface: NPH on left and regular insulin on the right.
- Roll the NPH insulin between your hands to mix the solution. With an alcohol pad, scrub off the vial top of the NPH insulin. Using a new alcohol pad, scrub the vial top of the regular insulin. Discard any prep pads.
- Select the correct insulin syringe that will exactly measure the TOTAL dose of the amount of NPH and regular doses (30- and 50-unit syringes measure single units; 100-unit syringes only measure even numbered doses).
- Pull back on the plunger to draw air into the syringe equal to the dose of NPH insulin.
- With the NPH vial on a flat surface, remove the cap from the syringe, insert the needle into the NPH vial, and inject air. Do not let the tip of the needle touch the insulin solution. Withdraw the needle.
- Pull back on the plunger to draw air into the syringe equal to the dose of the regular insulin.
- With the regular vial on a flat surface, insert the needle into the regular vial, and inject air.
- With the needle still in the vial, invert the regular insulin vial and withdraw the correct dose. Remove the needle from the vial. Cap the needle using the scoop method.
- Roll the NPH insulin vial between your hands to mix the solution. Uncap the needle and insert the needle into the NPH insulin vial. Withdraw the correct amount of NPH insulin. Withdraw the needle and recap using the scoop method.
- Perform the second medication check of the combined dose looking at the vial, syringe, and MAR, verifying all the rights.
- Label the syringe with the name of the combined medications and doses.
Alternative Preparation Using an Insulin Pen
- Select the correct insulin pen to be used for the injection. Identify the dose to be given.
- Remove the cap from the insulin pen and clean the top (hub) with an alcohol prep pad. Attach the insulin pen needle without contaminating the needle or pen hub.
- Turn the dial to two units and with the pen pointing upward, push the injection button to prime the pen.
- Turn the dial to the correct dose.
- Perform the second medication check looking at the insulin pen and MAR, verifying all the rights.
Administration of Parenteral Medication
- Knock, enter the room, greet the patient, and provide for privacy.
- Perform safety steps:
- Perform hand hygiene.
- Check the room for transmission-based precautions.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain the process to the patient and ask if they have any questions.
- Be organized and systematic.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure the patient's privacy and dignity.
- Assess ABCs.
- Perform the third check of the six rights of medication administration at the patient's bedside after performing patient identification.
- Perform the following steps according to the type of parenteral medication.
INTRADERMAL - Administration of a TB Test
- Correctly identify the sites and verbalize the landmarks used for intradermal injections.
- Select the correct site for the TB test, verbalizing the anatomical landmarks and skin considerations.
- Put on nonsterile gloves if contact with blood or body fluids is likely or if your skin or the patient's skin isn't intact.
- Use an alcohol swab in a circular motion to clean the skin at the site; place the pad above the site to mark the site, if desired.
- Gently pull the skin away from the site.
- Insert the needle with the bevel facing upward, slowly at a 5- to 15-degree angle, and then advance no more than an eighth of an inch to cover the bevel.
- Use the thumb of the nondominant hand to push on the plunger to slowly inject the medication. Inspect the site, noting if a small bleb forms under the skin surface.
- Carefully withdraw the needle straight back out of the insertion site so not to disturb the bleb (do not massage or cover the site).
- Activate the safety feature of the needle and place the syringe in the sharps container.
- Teach the patient to return for a TB skin test reading in 48-72 hours and not to press on the site or apply a Band-Aid.
SUBCUTANEOUS - Administration of Insulin in a Syringe
- Correctly identify the sites and verbalize the landmarks used for subcutaneous injections. Ask the patient regarding a preferred site of medication administration.
- Put on nonsterile gloves if contact with blood or body fluids is likely or if your skin or the patient's skin isn't intact.
- Select an appropriate site and clean with an alcohol prep in a circular motion. Place the pad above the site to mark the location, if desired. Remove the cap from the needle without contaminating the needle.
- Pinch approximately an inch of subcutaneous tissue, creating a skinfold.
- Insert the needle at a 90-degree angle, release the patient's skin, and inject the medication. Withdraw the needle.
- Activate the safety feature of the needle and place the syringe in a sharps container.
SUBCUTANEOUS - Administration with an Insulin Pen
- Select the site and clean with an alcohol prep in a circular motion. Place the pad above the site to mark the location, if desired.
- Put on nonsterile gloves if contact with blood or body fluids is likely or if your skin or the patient's skin isn't intact.
- Remove the cap from the needle without contaminating the needle.
- Pinch approximately an inch of subcutaneous tissue, creating a skinfold.
- Insert the needle quickly at a 45- to 90-degree angle (depending upon the size of the patient), continue to hold the skinfold, and inject the medication. After the medication is injected, count to 10, remove the needle, and release the skinfold.
- Dispose of the needle in a sharps container. Replace the top cap to the insulin pen.
INTRAMUSCULAR - Deltoid
- Correctly identify the site and verbalize the landmarks used for a deltoid injection.
- Put on nonsterile gloves if contact with blood or body fluids is likely or if your skin or the patient's skin isn't intact.
- Use an alcohol swab in a circular motion to clean the skin at the site. Place a pad above the site to mark the location. Remove the cap from the needle without contaminating the needle.
- Depending on the muscle mass of the deltoid, either grasp the body of the muscle between the thumb and forefingers of the nondominant hand or spread the skin taut.
- Insert the needle at a 90-degree angle.
- Follow agency policy and manufacturer recommendations regarding aspiration.
- Continue to hold the muscle fold and inject the medication. After the medication is injected, count to 10, remove the needle, and release the muscle fold.
- Activate the safety on the syringe. Place the syringe in a sharps container.
INTRAMUSCULAR - Vastus Lateralis
- Correctly identify the site and verbalize the landmarks to locate the vastus lateralis site.
- Put on nonsterile gloves if contact with blood or body fluids is likely or if your skin or the patient's skin isn't intact.
- Use an alcohol swab in a circular motion to clean the skin at the site. Place the pad above the site to mark the location. Remove the cap from the needle without contaminating the needle.
- Depending on the muscle mass of the vastus lateralis, either grasp the body of the muscle between the thumb and forefingers of the nondominant hand or spread the skin taut.
- Insert the needle at a 90-degree angle.
- Follow agency policy and manufacturer recommendations regarding aspiration.
- Continue to hold the muscle fold and inject the medication. After the medication is injected, count to 10, remove the needle, and release the muscle fold.
- Activate the safety on the syringe. Put the needle in a sharps container.
INTRAMUSCULAR - Ventrogluteal (Using the Z-track Technique)
- Correctly identify and verbalize the landmarks used to locate the ventrogluteal site.
- Put on nonsterile gloves if contact with blood or body fluids is likely or if your skin or the patient's skin isn't intact.
- Use an alcohol swab in a circular motion to clean the skin at the site and place a pad above the site to mark the location. Remove the cap from the needle without contaminating the needle.
- Place the ulnar surface of the hand approximately 1 – 3 inches from the selected site; press down and pull the skin and subcutaneous tissue to the side or downward.
- Maintaining tissue traction, hold the syringe like a dart and insert the needle into the skin at 90 degrees.
- Maintaining tissue traction, use the available thumb and index finger to help stabilize the syringe.
- Follow agency policy and manufacturer recommendations regarding aspiration. If aspiration is required, pull back the plunger and observe for blood return. If there is no blood return, inject the medication. If blood return is observed, remove the needle, and prepare a new medication.
- Maintaining tissue traction, wait 10 seconds with the needle still in the skin to allow the muscle to absorb the medication. Withdraw the needle from the site and then release traction. Do not rub/massage the site.
- Activate the safety feature of the needle; place in a sharps container.
Following Conclusion of All Injections
- Assess site; apply Band-Aid if necessary and appropriate.
- Remove gloves. Perform hand hygiene.
- Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Document medication administered, including the site used for the injection.

