5.7 Coronary Artery Disease
Open Resources for Nursing (Open RN)
Overview
Coronary artery disease (CAD) is caused by plaque buildup that causes the inside of the coronary arteries to narrow over time, which can partially or totally block the blood flow to the muscle tissue of the heart. As previously discussed in this chapter, the process of plaque buildup is referred to as atherosclerosis.
Risk Factors
There are a variety of risk factors for CAD, referred to as modifiable and nonmodifiable risk factors. Modifiable risk factors include high blood pressure; high cholesterol; smoking; obesity; physical inactivity; and diets high in saturated fats, trans fats, sodium, and refined sugars. Chronic stress and excessive alcohol consumption can also play a role in the development of coronary artery disease.[1],[2] Nurses play an important role in educating clients about modifiable risk factors for CAD and healthy lifestyle choices that can reduce these risks.
There are also numerous nonmodifiable risk factors for coronary artery disease. The risk of coronary artery disease increases with age; men over the age of 45 and women over the age of 55 are at higher risk. Family history and genetics are also nonmodifiable risk factors, especially if a client has a first-degree relative who has been diagnosed with coronary artery disease or had a myocardial infarction (i.e., heart attack), especially at a young age. Specific ethnic groups, such as African Americans are also at higher risk for the development of cardiovascular disease.[3],[4]
Angina
As blood flow becomes partially blocked in coronary arteries due to atherosclerosis, individuals often experience chest pain called angina. Angina is caused by lack of oxygenated blood flow to heart muscle tissue, referred to as ischemia. See Figure 5.28[5] for an image of a client experiencing angina.[6] Because angina is caused by blockage of oxygenated blood flow to the heart tissue, it is often brought on by physical activity and an increased demand for oxygenated blood. Physical activity stimulates the heart to beat faster with stronger contractions to distribute oxygenated blood flow to muscle tissue throughout the body. However, if coronary arteries are partially blocked, the heart tissue itself may not receive enough oxygenated blood flow as this workload increases, resulting in angina.

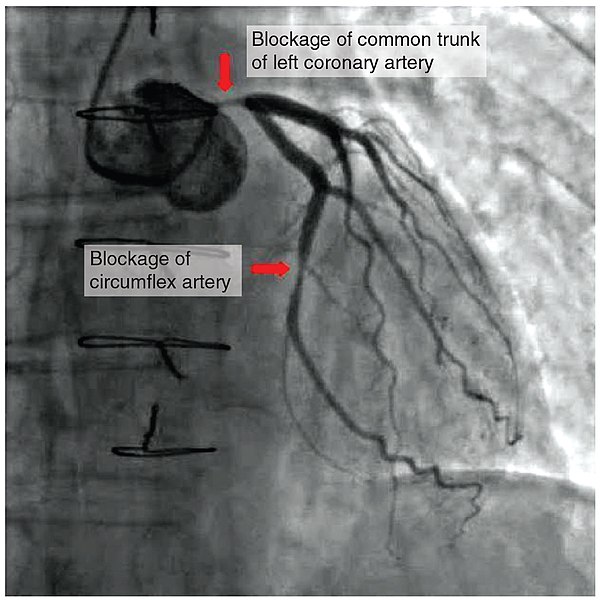
Angina is classified as stable or unstable. View Table 5.7 to compare the characteristics of stable versus unstable angina. Stable angina is caused by narrowing of the coronary arteries, resulting in partial blockage of blood flow. It is chronic, predictable, and relieved with rest or nitroglycerin. Clients may live with stable angina for several years and managed with medication. However, unstable angina is caused by worsening or a sudden blockage of blood flow to the heart that falls under the umbrella term of acute coronary syndrome (ACS). ACS refers to conditions that cause a sudden decrease in oxygenated blood flow to the cardiac muscle, ranging from unstable angina to myocardial infarction. As previously discussed, unstable angina is characterized by chest pain that does not resolve completely with rest or nitroglycerin. Myocardial infarction (MI), commonly referred to as a “heart attack,” occurs when there is a sudden blockage within the coronary arteries. Figure 5.29[7] shows a blockage in the coronary arteries of a client during a coronary angiogram that can result in a myocardial infarction without intervention.
Table 5.7. Characteristics of Stable and Acute Coronary Syndrome[8],[9]
| Characteristic | Stable Angina | ACS |
|---|---|---|
| Trigger | Typically triggered by exercise or emotional stress. | May occur at rest or with minimal exertion, sometimes with no apparent trigger. |
| Predictability | Generally predictable based on an individual’s specific activities. For example, an individual may be aware that climbing stairs will cause angina. | Unpredictable in terms of when it occurs and its severity. It may occur suddenly without warning. |
| Duration of Symptoms | Short duration that typically resolves within five minutes of rest or administration of nitroglycerin. | Longer duration than five minutes. Rest and/or nitroglycerin may improve but not completely resolve the pain. |
| Frequency | Predictable frequency. | Episodes of angina become more frequent over time. |
| Severity | Often described as pressure, heaviness, tightness, or squeezing over a broad area of the chest. | Often associated with shortness of breath and may also include symptoms of nausea, vomiting, diaphoresis, dizziness, and palpitations. Women may only experience fatigue and indigestion-type symptoms. |
| Progression | Rarely progresses to a myocardial infarction. | A serious warning sign of an impending myocardial infarction. |
| Management | Managed with lifestyle modifications and medications. | Requires immediate medical attention to prevent a myocardial infarction. |
When a myocardial infarction occurs, there are three types of potential damage to the cardiac muscle tissue: ischemia, injury, and infarction. When ischemia occurs, the viability of the tissue may be preserved if oxygen is promptly restored, and the heart muscle can recover without permanent damage. On an ECG, ischemia to cardiac muscle tissue is indicated by ST segment depression.
Next to the area of ischemia may be tissues that were injured. These tissues can be viable as long as oxygen is delivered to the tissue by pathways that circumvent the blockage. For example, providing supplemental oxygen during an MI may help save injured areas from necrosis (death). Areas of injury to cardiac muscle tissues may be indicated on an ECG by ST segment elevation. See Figure 5.30[10] for an illustration of ST elevations indicated by red arrows on an ECG strip.

The most significant area of damage during an MI is an area of infarct. Infarcted tissue has been deprived of oxygen for so long that the damage is irreversible, and the tissue has died. Troponin is a protein found in heart muscle cells that is released into the bloodstream when tissues have died and is used to help diagnose myocardial infarction. Cardiac muscle tissue that has died due to an infarct also causes a Q wave change on an ECG.[11] See Figure 5.31[12] for an illustration of a myocardial infarction.
Additional information regarding medical treatment for MI is provided in the following box.
Medical Treatment for MI
Nurses must recognize signs of unstable angina and implement appropriate action, such as notifying the provider and/or obtaining emergency assistance. Common interventions include the following[13],[14],[15]:
- Obtain stat ECG.
- Administer oxygen if SpO2 is less than 92% or per agency protocol, which helps ensure that the heart tissue receives adequate oxygen.
- Administer nitroglycerin to dilate the blood vessels and improve blood flow to the heart.
- Administer aspirin to reduce the opportunity for clot formation.
- Analgesics (such as morphine) may be prescribed to help reduce discomfort and cardiac workload, but morphine is no longer considered first-line treatment because of higher risk of death and adverse clinical outcomes.
- Mild anxiolytics may be prescribed for very anxious clients.
- Antiplatelet medications (such as clopidogrel) may be prescribed to reduce platelet aggregation and clot formation.
- Beta-blockers may be prescribed to reduce myocardial oxygen consumption by lowering heart rate, blood pressure, and myocardial contractility.
- Revascularization procedures, such as cardiac catheterization, stenting, or coronary artery bypass grafting surgery, may be required if vessel occlusion is significant.
Read additional information about MI treatment in the National Library of Medicine’s StatPearl Myocardial Infarction.
View a supplementary YouTube video[16] about acute coronary syndrome: How to Treat a Heart Attack
Assessment
Nurses assess subjective and objective data on physical examination and by reviewing laboratory and diagnostic test results.
Angina is the most common symptom of CAD. However, for many people, the first sign of CAD is a myocardial infarction (MI). Symptoms of an MI include the following[17]:
- Angina (Often described as heaviness, pressure, squeezing, or the feeling of something sitting on the chest)
- Shortness of breath
- Diaphoresis (Often described as “cold sweat”)
- Weakness
- Lightheadedness
- Nausea (Often described as “indigestion” or “feeling sick to your stomach”)
- Pain or discomfort in the jaw, arms, or shoulder
Over time, CAD can weaken the heart muscle. This may lead to heart failure, a serious condition where the heart can’t pump blood the way it should.[18]
Diagnostic Testing
Health care providers order various tests to assess the presence and severity of blockages within the coronary arteries. Depending on the severity of symptoms, providers may also order a coronary catheterization, considered the “gold standard” for the diagnosis of CAD. Common diagnostic tests related to CAD include the following.[19],[20],[21],[22]
- Troponin: A blood test used to help diagnose myocardial infarction that measures protein released into the bloodstream when heart tissue is damaged. Review normal reference ranges for common diagnostic tests in “Appendix A – Normal Reference Ranges.”
- Electrocardiogram (ECG or EKG): Measures the electrical activity, rate, and rhythm of the heart.
- Echocardiogram: Uses ultrasound (special sound wave) to create images of the heart.
- Exercise Stress Test: Evaluates the heart rate and rhythm while walking on a treadmill to determine how well the heart is working when it has to pump more blood.
- Cardiac Catheterization and Coronary Angiogram: Examines the inside of the coronary arteries for blockage by inserting a thin, flexible tube through an artery in the groin, arm, or neck to reach the heart. During the coronary angiogram, dye is administered to view the coronary arteries. Review additional information about cardiac catheterizations under the “Diagnostic Testing” subsection in the “General Cardiovascular System Assessment” section.
- Coronary Artery Calcium Scan: Examines coronary arteries for calcium buildup and plaque through computed tomography (CT).
- Cardiac Magnetic Resonance Imaging (MRI): Uses a magnetic field and radiofrequency waves to create detailed pictures of the heart and arteries.
- Coronary Computed Tomography (CCTA): Uses X-rays to take images of the heart and blood vessels. A computer combines the images to create a three-dimensional (3D) image of the heart.
Nursing Diagnoses
Nursing priorities for clients with CAD involve addressing inadequate oxygenation and managing pain, fatigue, activity intolerance, impaired cardiac output, and anxiety. Nursing diagnoses for clients with CAD are formulated based on the client’s assessment data, medical history, and specific needs. These nursing diagnoses guide the development of individualized care plans and interventions. Recall that symptoms of CAD are related to decreased oxygenated blood flow in the coronary arteries and can range from stable, chronic angina to acute coronary syndrome (ACS).[23]
Common nursing diagnoses for stable CAD include the following[24]:
- Acute Pain
- Risk for Decreased Cardiac Tissue Perfusion
- Risk for Decreased Cardiac Output
- Readiness for Enhanced Health Self-Management
Outcome Identification
Outcome identification includes setting short- and long-term goals and creating expected outcome statements customized for the client’s specific needs. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions.
Sample expected outcomes for common nursing diagnoses related to CAD are as follows:
- The client will maintain adequate cardiac tissue perfusion as evidenced by the following vital sign ranges: SBP between 90 mm Hg – 120 mm Hg, HR 60-99 bpm, and O2 saturation greater than 92%.
- The client will report relief of angina within 5-10 minutes of rest and/or administration of nitroglycerin.
- The client will verbalize a decreased level of anxiety and demonstrate the use of relaxation techniques (e.g., deep breathing exercises) to effectively manage anxiety.
- The client will be able to participate in activities of daily living (ADLs) and physical activity.
Interventions
Medical Interventions
Medical interventions for CAD are aimed at managing symptoms, slowing disease progression, and improving quality of life. These interventions are typically prescribed by health care providers based on the severity of CAD, the client’s risk factors, and individualized needs and goals. Common medical interventions used to address CAD include medication therapy and lifestyle modifications. For severe CAD, surgical treatment may be performed.[25],[26]
Medication Therapy
Several classes of medications are used to treat CAD:
- Antiplatelet Medications: Help reduce the buildup of thrombotic plaque in the coronary arteries. Common medications include aspirin and clopidogrel.
- Cholesterol-Lowering Medications: Reduce the risk of atherosclerosis and plaque buildup. Common medications include statins like atorvastatin and simvastatin to lower LDL blood levels.
- Antihypertensive Medications: Control blood pressure and reduce strain on the heart. Common medications include beta-blockers, ACE inhibitors, and calcium channel blockers.
- Nitroglycerin: Relaxes and dilates coronary blood vessels to increase blood flow to cardiac muscle tissue and resolve angina.
- Antianginal Medications: Reduce the frequency and severity of angina. Examples include isosorbide, beta-blockers, and calcium channel blockers.
- Antiarrhythmic Medications: Used to manage abnormal rhythms. Because abnormal heart rhythms are associated with CAD, medications like beta-blockers or calcium channel blockers may be prescribed.
- Thrombolytic Therapy: Used to dissolve blood clots that are blocking coronary arteries during an acute myocardial infarction.
Read more information about these medication classes in “Cardiovascular & Renal System Medications” in Open RN Nursing Pharmacology, 2e.
View supplementary YouTube videos[27],[28],[29],[30] on common cardiac medications:
- Calcium channel blockers: CCBs for Hypertension (high blood pressure) or Arrhythmias (irregular heartbeat)
- ACE inhibitors: How do ACE inhibitors work?
- Nitrates: A Patient Guide: Nitroglycerin Jennifer Riccobono 252 subscribers Subscribe
Lifestyle Modifications
Several evidence-based lifestyle modifications are recommended by health care providers, including the following[31]:
- Healthy Weight: Carrying extra weight can put extra stress on the heart and blood vessels. Clients are encouraged to follow a healthy diet and incorporate regular physical activity to maintain a healthy weight.
- Heart Healthy Diet: A heart-healthy diet low in saturated fats, trans fats, cholesterol, and sodium is encouraged. Emphasis is placed on consuming fruits, vegetables, whole grains, and lean proteins while also considering cultural and religious diet preferences.
- Moderate Alcohol Consumption: Alcohol consumption can elevate blood pressure and should be consumed in moderation. Men should have no more than two drinks per day, and women no more than one drink per day.
- Regular Physical Activity: Physical activity is recommended to maintain a healthy weight and lower blood pressure, blood cholesterol, and blood sugar levels. For adults, the Surgeon General recommends 2 hours and 30 minutes of moderate-intensity exercise, like brisk walking or bicycling, every week. Children and adolescents should get 1 hour of physical activity every day.[32]
- Smoking Cessation: Smoking is a significant risk factor for CAD. If clients smoke, they are encouraged to consider quitting at every health care visit through counseling and nicotine replacement therapy.
- Mental Health: Various studies have shown the impact of trauma, depression, anxiety, and stress on the body, including stress on the heart. Clients are encouraged to talk to their health care providers about their mental health.
Surgical Interventions
In severe cases of CAD, these surgical procedures may be performed by cardiologists:
- Cardiac Catheterization With Angioplasty: A catheter is inserted into a narrowed coronary artery during cardiac catheterization. During the procedure, a balloon at the end of the catheter is inflated to widen the artery and improve blood flow. A small mesh device, known as a stent, may also be inserted to help keep the coronary artery open after the procedure is completed. Review information about cardiac catheterization under the “Diagnostic Testing” subsection in the “General Cardiovascular System Assessment” section.
- Coronary Artery Bypass Grafting (CABG): Blocked coronary arteries are bypassed using grafts (i.e., veins or arteries obtained from elsewhere in the body) to create new pathways for blood to flow to the heart muscle.
Cardiac Rehabilitation
Cardiac rehabilitation is a supervised program that includes physical activity, education about healthy lifestyle choices, and counseling to find ways to relieve stress and improve mental health. It is typically prescribed for clients who have had cardiac surgery, a myocardial infarction, or have been diagnosed with heart failure. Cardiac rehabilitation can help prevent another, perhaps more serious, heart attack and helps clients build heart-healthy habits.[33]
Read more information about How Cardiac Rehabilitation Can Help Heal Your Heart by the CDC.
Nursing Interventions
Nursing interventions for CAD focus on medication management, health teaching, safety promotion, and psychosocial support to facilitate overall cardiovascular health.
Medication Management
Prescribed medications are safely administered, and monitoring is provided for therapeutic effect and potential side effects. Teaching is provided about the role of medications, potential side effects, and when to notify the provider.
Health Teaching
Health teaching is provided about CAD, its risk factors, and the role of prescribed treatments and medications.
Guidance is provided for tracking blood pressure and monitoring cholesterol levels with lab work. Lifestyle modifications, as outlined under the “Medical Interventions” subsection, are taught and reinforced. Client understanding is evaluated, and follow-up teaching and/or cardiac rehabilitation is recommended as indicated.
Safety Promotion
Clients experiencing angina are taught how to properly use and store nitroglycerin.
Nitroglycerin Safety
Client teaching for nitroglycerin is crucial as it helps individuals understand how to use this medication safely and effectively.
- Instruct the client on the correct method of administration based on the prescribed form (sublingual tablets, transdermal patch, or spray).
- If using sublingual tablets, advise client to be in a seated position and then place the tablet under the tongue and allow it to dissolve.
- Clearly explain the prescribed dosage and the frequency with which nitroglycerin should be taken. Clients should be instructed to self-administer one tablet every five minutes for a total of three doses.
- Pain relief should start within one to two minutes of administration.
- Nitroglycerin tablets should be stored in their original container and protected from light.
- Inform clients about potential side effects of nitroglycerin, such as hypotension, headache, dizziness, or flushing. These effects are usually temporary but should be reported to the health care provider if persistent.
Clients and their family members are taught to recognize symptoms of an unstable angina and/or myocardial infarction and when to call 911.
Psychosocial Support
Nurses address the emotional and psychological impact of CAD by providing emotional support and making referrals to mental health professionals as indicated. Clients are also encouraged to participate in support groups and cardiac rehabilitation programs to maintain heart-healthy lifestyles.
Evaluation
During the evaluation stage, nurses determine the effectiveness of nursing interventions for a specific client. The previously identified expected outcomes are reviewed to determine if they were met, partially met, or not met by the time frames indicated. If outcomes are not met or only partially met by the time frame indicated, the nursing care plan is revised. Evaluation should occur every time the nurse implements interventions with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with other members of the interprofessional team.
![]() RN Recap: Coronary Artery Disease
RN Recap: Coronary Artery Disease
View a brief YouTube video overview of CAD[34]:
Media Attributions
- 2016_Occluded_Coronay_Arteries
- Heart_attack-NIH
- RN Recap Icon
- Simons, M., & Alpert, J. S. (2022). Acute coronary syndrome: Terminology and classification. Retrieved August 27, 2023, from https://www.uptodate.com/ ↵
- This work is a derivative of StatPearls by Mechanic, Gavin, Grossman, & Ziegler and is licensed under CC BY 4.0 ↵
- Simons, M., & Alpert, J. S. (2022). Acute coronary syndrome: Terminology and classification. Retrieved August 27, 2023, from https://www.uptodate.com/ ↵
- This work is a derivative of StatPearls by Mechanic, Gavin, Grossman, & Ziegler and is licensed under CC BY 4.0 ↵
- “51096039583” by Marco Verch Professional Photographer’s photostream is licensed under CC BY 2.0 ↵
- Simons, M., & Alpert, J. S. (2022). Acute coronary syndrome: Terminology and classification. Retrieved August 27, 2023, from https://www.uptodate.com/ ↵
- “2016 Occluded Coronay Arteries.jpg” by OpenStax College is licensed under CC BY 3.0 ↵
- This work is a derivative of StatPearls by Goyal & Zeltser and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Gillen & Goyal and is licensed under CC BY 4.0 ↵
- “ST Elevations” by Meredith Pomietlo is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Mechanic, Gavin, Grossman, & Ziegler and is licensed under CC BY 4.0 ↵
- “Heart_attack-NIH.gif” by NIH: National Heart, Lung and Blood Institute is in the Public Domain. ↵
- This work is a derivative of StatPearls by Goyal & Zeltser and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Gillen & Goyal and is licensed under CC BY 4.0 ↵
- Ojha, N., & Dhamoon, A.S. (2023, Aug 8). Myocardial Infarction. In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK537076/ ↵
- 7activestudio. (2017, January 15). How to treat a heart attack [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=QllguanpKic ↵
- Centers for Disease Control and Prevention. (2023, April 14). Heart disease. https://www.cdc.gov/heartdisease/index.htm ↵
- Centers for Disease Control and Prevention. (2023, April 14). Heart disease. https://www.cdc.gov/heartdisease/index.htm ↵
- Simons, M., & Alpert, J. S. (2022). Acute coronary syndrome: Terminology and classification. Retrieved August 27, 2023, from https://www.uptodate.com/ ↵
- Centers for Disease Control and Prevention. (2023, April 14). Heart disease. https://www.cdc.gov/heartdisease/index.htm ↵
- American Heart Association. (2023, April 12). Cardiac computed tomography angiography (CCTA). https://www.heart.org/en/health-topics/heart-attack/diagnosing-a-heart-attack/cardiac-computed-tomography ↵
- American Heart Association. (2023, April 13). Cardiac magnetic resonance imaging (MRI). https://www.heart.org/en/health-topics/heart-attack/diagnosing-a-heart-attack/magnetic-resonance-imaging-mri ↵
- This work is a derivative of StatPearls by Mechanic, Gavin, Grossman, & Ziegler and is licensed under CC BY 4.0 ↵
- Flynn Makic, M. B., & Martinez-Kratz, M. R. (2023). Ackley and Ladwig’s Nursing diagnosis handbook: An evidence-based guide to planning care (13th ed.). ↵
- Simons, M., & Alpert, J. S. (2022). Acute coronary syndrome: Terminology and classification. Retrieved August 27, 2023, from https://www.uptodate.com/ ↵
- This work is a derivative of StatPearls by Mechanic, Gavin, Grossman, & Ziegler and is licensed under CC BY 4.0 ↵
- 7activestudio. (2017, January 15). How to treat a heart Attack [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=QllguanpKic ↵
- Drugs in Motion. (2018, December 10). CCBs for hypertension (high blood pressure) or arrhythmias (irregular heartbeat) [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=QeVIGjJbE6g ↵
- British Heart Foundation. (2018, October 2). How do ACE inhibitors work? [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=xIlaQuRaZmk ↵
- Riccobono, J. (2012, September 11). A patient guide: Nitroglycerin [Video]. YouTube. All rights reserved. https://www.youtube.com/watch?v=pII49Kn14Q8 ↵
- Centers for Disease Control and Prevention. (2023, April 14). Heart disease. https://www.cdc.gov/heartdisease/index.htm ↵
- Centers for Disease Control and Prevention. (2023, April 14). Heart disease. https://www.cdc.gov/heartdisease/index.htm ↵
- Centers for Disease Control and Prevention. (2023, April 14). Heart disease. https://www.cdc.gov/heartdisease/index.htm ↵
- Open RN Project. (2024, April 4). Health Alterations - Chapter 5 Cardiovascular - Coronary artery disease [Video]. YouTube. CC BY-NC 4.0 https://www.youtube.com/watch?v=5KaFXLcRKNQ ↵
Applying the Nursing Process: Assessment
When performing a comprehensive assessment on an older adult, the findings are used to establish their baseline status of physical, cognitive, psychosocial, and spiritual well-being. It is appropriate to consider the potential impact of declining strength and physical functioning on their psychological status using Erikson’s developmental stage of “Integrity versus Despair.” It is also important to consider the impact of chronic disease on their ability to function and complete Activities of Daily Living (ADLs). Many older adults who are able to perform ADLs without assistance consider themselves healthy.
When performing an assessment on an older adult, modification of communication techniques may be required, as discussed in the “Sensory Impairments” and “Cognitive Impairments” chapters. It is important to allow adequate time for older individuals to reply to questions thoughtfully and to move through the requests contained in a physical assessment comfortably.
It is helpful to use an evidence-based tool to assess for frequent needs of older adults, such as the Fulmer SPICES tool. The SPICES tool focuses on areas of common problems for aging individuals and can lead to early intervention and treatment. The SPICES tool includes assessment of the following:
S: Sleep Disorders
P: Problems with Eating or Feeding
I: Incontinence
C: Confusion
E: Evidence of Falls
S: Skin Breakdown[1]
Several free assessment tools for common issues in older adults are located at The Hartford Institute of Geriatric Nursing website. Use the box below to explore available tools.
Unexpected Findings
While cognitive impairment and memory deficits are not considered normal aspects of aging, there are common expected physiological changes that occur with aging. Nurses should be familiar with these expected findings so that deviations from the expected can be adequately addressed. See Table 19.3 for a comparison of expected versus unexpected findings in an older adult that require notification of the health care provider.[3]
Table 19.3 Expected Versus Unexpected Findings[4]
| Assessment | Expected Findings | New Unexpected Findings to Report to the Health Care Provider |
|---|---|---|
| Cardiovascular system |
|
*CRITICAL CONDITIONS requiring immediate notification or contact of emergency services: Chest pain; symptomatic hypotension or hypertension; new onset or changes in oxygenation |
| Respiratory system |
|
*CRITICAL CONDITIONS requiring immediate notification or contact of emergency services: Hemoptysis; decreased oxygen saturation levels not responding to treatments; labored breathing |
| Musculoskeletal system |
|
*CRITICAL CONDITIONS requiring immediate notification or contact of emergency services: Sudden onset of unilateral weakness, facial drooping, or slurred speech; falls with suspected injury |
| Genitourinary system |
|
*CRITICAL CONDITIONS requiring immediate notification or contact of emergency services: Urine output less than 30 mL/hour |
| Gastrointestinal system |
|
*CRITICAL CONDITIONS requiring immediate notification or contact of emergency services: Absent bowel sounds or rigid, distended abdomen |
| Integumentary system |
|
|
| Endocrine system |
|
*CRITICAL CONDITIONS requiring immediate notification or contact of emergency services: Symptomatic blood glucose less than 50 or greater than 400[5] |
| Immune system |
|
*CRITICAL CONDITIONS requiring immediate notification or contact of emergency services: Suspected or actual infection with two or more of the following signs indicating possible sepsis: Temperature > 38 C or <36 C, Heart rate > 90 bpm, Respiratory rate > 20 or PaCO2 < 32, WBC > 12,000 or < 4,000 or over 10% immature forms or bands[6] |
| Reproductive system |
|
|
Health Promotion
One of the goals of Healthy People 2030 is to improve the health and well-being for older adults. It is estimated that by 2060 almost a quarter of the U.S. population will be age 65 or older. Older adults are at higher risk for chronic health problems like diabetes, osteoporosis, and Alzheimer’s disease. In addition, 1 in 3 older adults fall each year, with falls being a leading cause of injury for this age group. Older adults are also more likely to go to the hospital for infectious diseases such as pneumonia, which is a leading cause of death for this age group. Nurses can ensure older adults get preventive care, including vaccines to protect against the flu and pneumonia, to help them stay healthy. Other goals for older adults established by Healthy People 2030 include early detection of dementia with appropriate intervention; decreased hospitalization for urinary infections, falls, and pneumonia; decreased incidence of medication-related safety issues; improved physical activity; improved oral health; decreased complications of osteoporosis; and reduced vision loss from macular degeneration.[7]
Nurses can advocate for improved health care for older adults while actively involving them in decisions about their care and promoting their quality of life. Common areas of health promotion for older adults include nutrition, physical activity, safe medication use, and psychosocial well-being.
Nutrition
Heart disease, cancer, chronic lung disease, and stroke are the leading causes of death in older adults. Nurses can provide health teaching that focuses on good nutrition, physical activity, smoking cessation, and moderate alcohol use to promote improved health outcomes.[8] However, nutrition can pose special challenges for the older adult. Chewing can be a problem if there are difficulties with dentition. Lack of oral care, missing teeth, or poorly fitting dentures can cause individuals to avoid intake of healthy foods. Regular dental care should be encouraged when working with older adults. Finances often impact nutritional intake when older adults have difficulty meeting their basic needs of housing, food, and health care. Additionally, the inability to plan, shop, and prepare meals because of activity intolerance, cognitive impairments, or physical limitations can impact nutrition. Nurses can initiate referrals to social workers or case managers for assistance with financial or health care concerns, as well as promote community resources such as Meals on Wheels or senior citizen meal site centers. Assisting individuals to meet their nutritional needs is an important aspect of health promotion.
Physical Activity
Physical activity is important throughout the life span. Older individuals may be limited in their ability to engage in physical activity due to various factors such as physical limitations, pain, and fear of falling. Musculoskeletal problems, such as impaired balance and arthritis, can impair an individual’s ability to walk or participate in regular exercise. Helping older adults find appropriate ways to maintain activity is an important nursing intervention. Nurses can advocate for the older adult by encouraging them to regularly attend health care checks with their provider and discuss concerns that limit their activity. Older adults should be reassured that pain is not considered a normal part of aging and can be effectively treated so they can maintain physical activity comfortably.
Safe Medication Use
Because of the increased incidence of chronic disease, many older adults take multiple medications to manage their symptoms and conditions. Polypharmacy, the use of many medications, increases a person’s risk of adverse medication effects. Older adults may be prescribed medications by multiple providers, and they can become confused when attempting to safely manage their daily medication use. There are also changes in absorption, distribution, metabolism, and excretion of drugs as an individual ages that impact the safe use of any medications.
The American Geriatrics Society maintains a list of medications to potentially avoid or use with caution in older adults because of the risk for harm. This list is called "AGS Beers Criteria." Updated reports are published in the Journal of the American Geriatric Society.[9] Use the following box to view the most current report.
In addition to cautiously using medications listed on the ABG Beers Criteria list with older adults, nurses can promote other safety strategies with medications. For example, older adults should have all of their medications prescribed from multiple providers filled at the same pharmacy to check for interactions and replications. It is also helpful to use a daily pill dispenser to ensure medications are taken as prescribed.
Nurses should also perform medication reconciliation during all clinic visits and on admission to health care agencies to review the client's current use of all medications.
Psychosocial Well-Being
As individuals age, they often experience loss of significant others, family members, and friends. These losses create increased risk for social isolation and depression. Poor mobility and transportation issues can also add to social isolation. As male older adults experience multiple losses, their risk for suicide increases.[10] Nurses can provide information about community resources and outreach programs to promote social interaction for individuals experiencing isolation.
Older adults are also at risk for other safety issues, such as elder abuse and financial exploitation. Read more about safety considerations for older adults in the "Safety" chapter.
Aging individuals continue to have sexual needs, and this aspect of their overall health should not be ignored. Assessment of these needs allows the nurse to integrate these aspects into the client’s plan of care and make appropriate referrals when necessary.
Adapting Health Teaching
As discussed throughout this chapter, there are many considerations when working with the older adult population and promoting optimal health and quality of life. It is also important to modify teaching methods depending on the individual’s knowledge, skills, and abilities. For example, some older adults readily engage in using electronic technology, but others have low digital literacy or experience difficulty when accessing electronic health resources. Nurses should adapt health teaching to the needs of the individual and provide verbal, written, or electronic resources as needed, while considering any sensory, cognitive, or functional impairments. The ultimate goal of health promotion and health teaching is to improve their understanding, motivation, and engagement in self-management and promote their quality of life.
Standard Versus Transmission-Based Precautions
Standard Precautions
Standard precautions are used when caring for all patients to prevent health care associated infections. According to the Centers for Disease Control and Prevention (CDC), standard precautions are “the minimum infection prevention practices that apply to all patient care, regardless of suspected or confirmed infection status of the patient, in any setting where health care is delivered.”[11] They are based on the principle that all blood, body fluids (except sweat), nonintact skin, and mucous membranes may contain transmissible infectious agents. These standards reduce the risk of exposure for the health care worker and protect the patient from potential transmission of infectious organisms.
Current standard precautions according to the CDC (2019) include the following:
- Appropriate hand hygiene
- Use of personal protective equipment (e.g., gloves, gowns, masks, eyewear) whenever infectious material exposure may occur
- Appropriate patient placement and care using transmission-based precautions when indicated
- Respiratory hygiene/cough etiquette
- Proper handling and cleaning of environment, equipment, and devices
- Safe handling of laundry
- Sharps safety (i.e., engineering and work practice controls)
- Aseptic technique for invasive nursing procedures such as parenteral medication administration[12]
Each of these standard precautions is described in more detail in the following subsections.
Transmission-Based Precautions
In addition to standard precautions, transmission-based precautions are used for patients with documented or suspected infection, or colonization, of highly transmissible or epidemiologically important pathogens. Epidemiologically important pathogens include, but are not limited to, Coronavirus disease (COVID-19), Clostridium difficile (C-diff), Methicillin-resistant staphylococcus aureus (MRSA), Vancomycin-resistant enterococci (VRE), Respiratory syncytial sirus (RSV), measles, and tuberculosis (TB). For patients with these types of pathogens, standard precautions are used along with specific transmission-based precautions.
There are four categories of transmission-based precautions: contact precautions, enhanced barrier precautions, droplet precautions, and airborne precautions. Transmission-based precautions are used when the route(s) of transmission is (are) not completely interrupted using standard precautions alone. Some diseases, such as tuberculosis, have multiple routes of transmission so more than one transmission-based precautions category must be implemented. See Table 4.2 outlining the categories of transmission precautions with associated PPE and other precautions. When possible, patients with transmission-based precautions should be placed in a single occupancy room with dedicated patient care equipment (e.g., blood pressure cuffs, stethoscope, thermometer). Transport of the patient and unnecessary movement outside the patient room should be limited. However, when transmission-based precautions are implemented, it is also important for the nurse to make efforts to counteract possible adverse effects of these precautions on patients, such as anxiety, depression, perceptions of stigma, and reduced contact with clinical staff.
Table 4.2 Transmission-Based Precautions[13]
| Precaution | Implementation | PPE and Other Precautions |
|---|---|---|
| Contact | Known or suspected infections with increased risk for contact transmission (e.g., draining wounds, fecal incontinence) or with epidemiologically important organisms, such as C-diff, MRSA, VRE, or RSV |
Note: Use only soap and water for hand hygiene in patients with C. difficile infection. |
| Enhanced barrier | Used during high-contact resident care activities for individuals colonized or infected with a multidrug-resistant organism (MDRO), as well as those at increased risk of MDRO acquisition |
|
| Droplet | Known or suspected infection with pathogens transmitted by large respiratory droplets generated by coughing, sneezing, or talking, such as influenza, coronavirus, or pertussis |
|
| Airborne | Known or suspected infection with pathogens transmitted by small respiratory droplets, such as measles, tuberculosis, and disseminated herpes zoster | Fit-tested N-95 respirator or PAPR
|
View a list of transmission-based precautions used for specific medical conditions at the CDC Guideline for Isolation Precautions.
Patient Transport
Several principles are used to guide transport of patients requiring transmission-based precautions. In the inpatient and residential settings, these principles include the following:
- Limiting transport for essential purposes only, such as diagnostic and therapeutic procedures that cannot be performed in the patient’s room
- Using appropriate barriers on the patient consistent with the route and risk of transmission (e.g., mask, gown, covering the affected areas when infectious skin lesions or drainage is present)
- Notify other health care personnel involved in the care of the patient of the transmission-based precautions. For example, when transporting the patient to radiology, inform the radiology technician of the precautions.[14]
Appropriate Hand Hygiene
Hand hygiene is the single most important practice to reduce the transmission of infectious agents in health care settings and is an essential element of standard precautions.[15] Routine handwashing during appropriate moments is a simple and effective way to prevent infection. However, it is estimated that health care professionals, on average, properly clean their hands less than 50% of the time it is indicated.[16] The Joint Commission, the organization that sets evidence-based standards of care for hospitals, recently updated its hand hygiene standards in 2018 to promote enforcement. If a Joint Commission surveyor witnesses an individual failing to properly clean their hands when it is indicated, a deficiency will be cited requiring improvement by the agency. This deficiency could potentially jeopardize a hospital’s accreditation status and their ability to receive payment for patient services. Therefore, it is essential for all health care workers to ensure they are using proper hand hygiene at the appropriate times.[17]
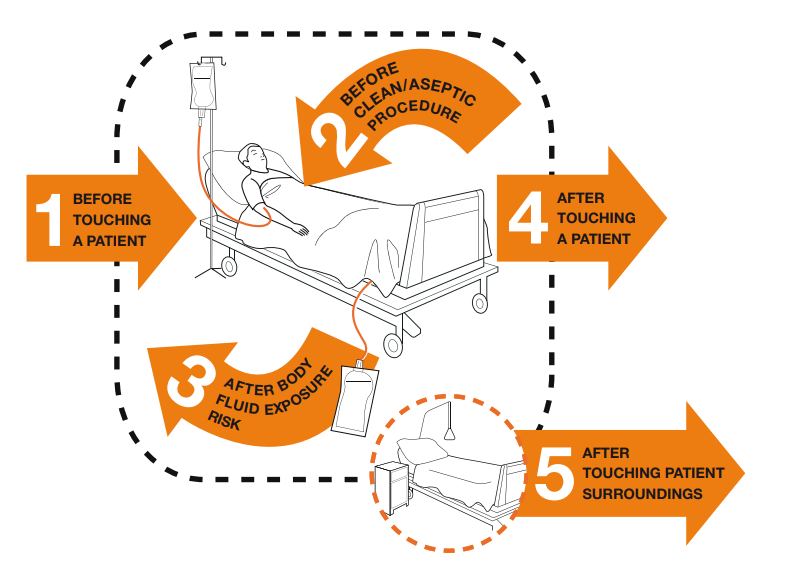
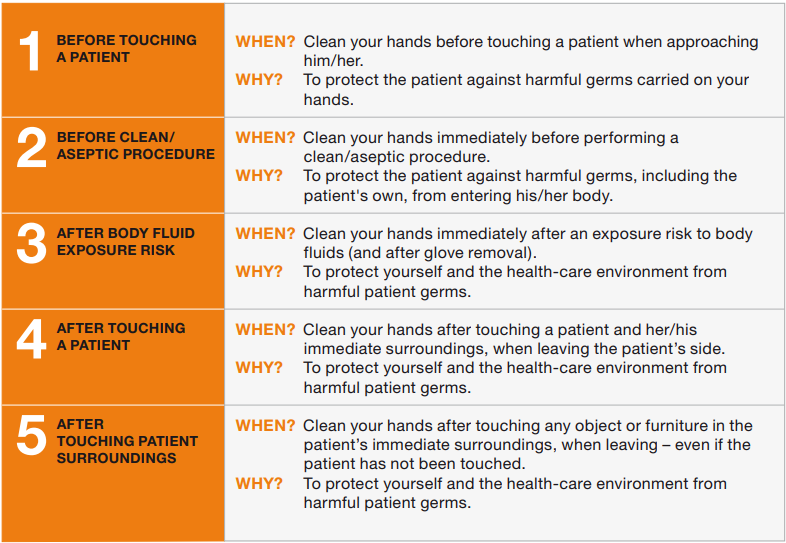
There are several evidence-based guidelines for performing appropriate hand hygiene. These guidelines include frequency of performing hand hygiene according to the care circumstances, solutions used, and technique performed. The Healthcare Infection Control Practices Advisory Committee (HICPAC) recommends health care personnel perform hand hygiene at specific times when providing care to patients. These moments are often referred to as the “Moments for Hand Hygiene.”[18] See Figures 4.1[19] and 4.2[20] for an illustration and application of the five moments of hand hygiene. The five moments of hand hygiene are as follows:
- Immediately before touching a patient
- Before performing an aseptic task or handling invasive devices
- Before moving from a soiled body site to a clean body site on a patient
- After touching a patient or their immediate environment
- After contact with blood, body fluids, or contaminated surfaces (with or without glove use)
When performing hand hygiene, washing with soap and water, or an approved alcohol-based hand rub solution that contains at least 60% alcohol, may be used. Unless hands are visibly soiled, an alcohol-based hand rub is preferred over soap and water in most clinical situations due to evidence of improved compliance. Handrubs are also preferred because they are generally less irritating to health care worker’s hands. However, it is important to recognize that alcohol-based rubs do not eliminate some types of germs, such as Clostridium difficile (C-diff).
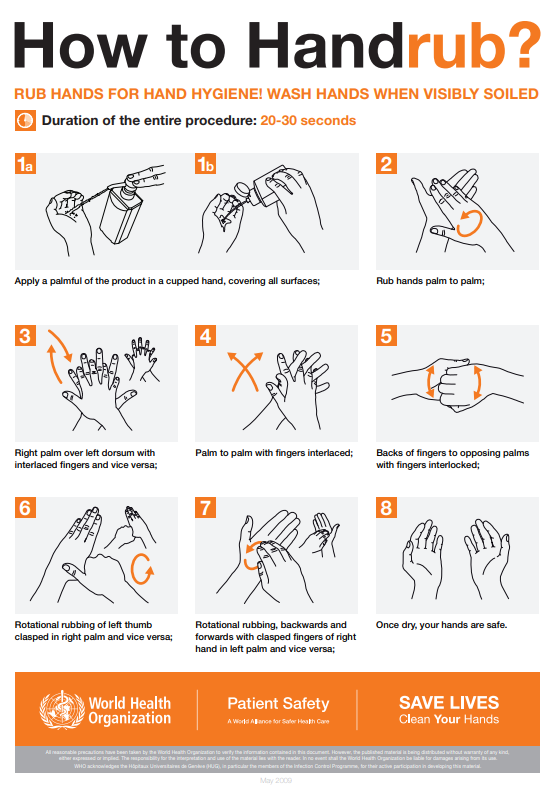
When using the alcohol-based handrub method, the CDC recommends the following steps. See Figure 4.3[21] for a handrub poster created by the World Health Organization.
- Apply product to the palm of one hand in an amount that will cover all surfaces.
- Rub hands together, covering all the surfaces of the hands, fingers, and wrists until the hands are dry. Surfaces include the palms and fingers, between the fingers, the backs of the hands and fingers, the fingertips, and the thumbs.
- The process should take about 20 seconds, and the solution should be dry.[22]
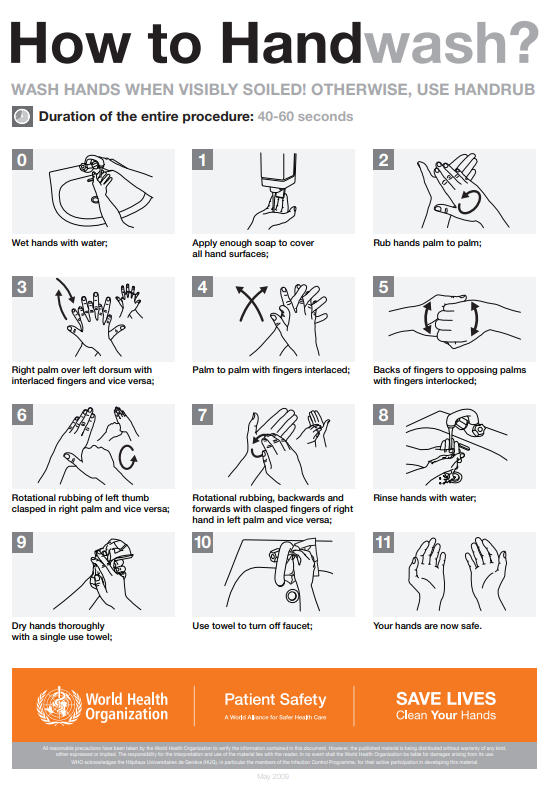
When washing with soap and water, the CDC recommends using the following steps. See Figure 4.4[23] for an image of a handwashing poster created by the World Health Organization.
- Wet hands with warm or cold running water and apply facility-approved soap.
- Lather hands by rubbing them together with the soap. Use the same technique as the handrub process to clean the palms and fingers, between the fingers, the backs of the hands and fingers, the fingertips, and the thumbs.
- Scrub thoroughly for at least 20 seconds.
- Rinse hands well under clean, running water.
- Dry the hands using a clean towel or disposable toweling.
- Use a clean paper towel to shut off the faucet.[24]
By performing hand hygiene at the proper moments and using appropriate techniques, you will ensure your hands are safe and you are not transmitting infectious organisms to yourself or others.
Hand Hygiene for Healthcare Workers on YouTube[25]
Personal Protective Equipment (PPE)
Personal protective equipment (PPE) includes gloves, gowns, face shields, goggles, and masks used to prevent the spread of infection to and from patients and health care providers. Depending on the anticipated exposure, PPE may include the use of gloves, a fluid-resistant gown, goggles or a face shield, and a mask or respirator. When used for a patient with transmission-based precautions, PPE supplies are typically stored in an isolation cart next to the patient’s room, and a card is posted on the door alerting staff and visitors to precautions needed before entering the room.
Gloves
Gloves protect both patients and health care personnel from exposure to infectious material that may be carried on the hands. Gloves are used to prevent contamination of health care personnel hands during activities such as the following:
- Anticipating direct contact with blood or body fluids, mucous membranes, nonintact skin, and other potentially infectious material
- Having direct contact with patients who are colonized or infected with pathogens transmitted by the contact route, such as Vancomycin-resistant enterococci (VRE), Methicillin-resistant staphylococcus aureus (MRSA), and Respiratory syncytial virus (RSV)
- Handling or touching visibly or potentially contaminated patient care equipment and environmental surfaces[26]
Nonsterile disposable medical gloves for routine patient care are made of a variety of materials, such as latex, vinyl, and nitrile. Many people are allergic to latex, so be sure to check for latex allergies for the patient and other health care professionals. See Figure 4.5[27] for an image of nonsterile medical gloves in various sizes in a health care setting. At times, gloves may need to be changed when providing care to a single patient to prevent cross-contamination of body sites. It is also necessary to change gloves if the patient interaction requires touching portable computer keyboards or other mobile equipment that is transported from room to room. Discarding gloves between patients is necessary to prevent transmission of infectious material. Gloves must not be washed for subsequent reuse because microorganisms cannot be reliably removed from glove surfaces, and continued glove integrity cannot be ensured.[28]

When gloves are worn in combination with other PPE, they are put on last. Gloves that fit snugly around the wrist should be used in combination with isolation gowns because they will cover the gown cuff and provide a more reliable continuous barrier for the arms, wrists, and hands.
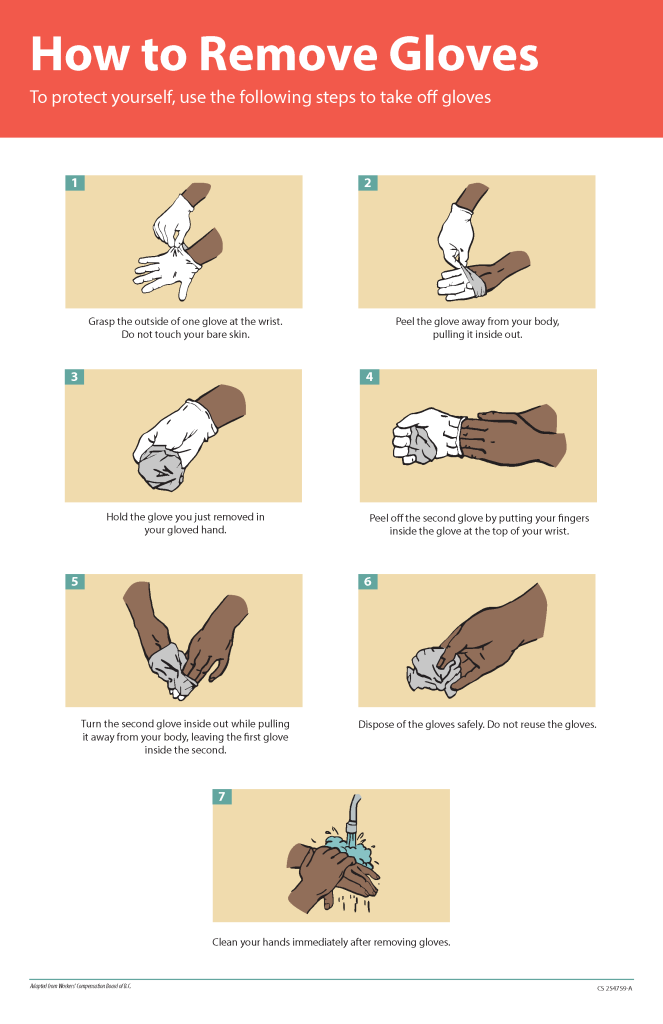
Gloves should be removed properly to prevent contamination. See Figure 4.6[29] for an illustration of properly removing gloves. Hand hygiene should be performed following glove removal to ensure the hands will not carry potentially infectious material that might have penetrated through unrecognized tears or contaminated the hands during glove removal. One method for properly removing gloves includes the following steps:
- Grasp the outside of one glove near the wrist. Do not touch your skin.
- Peel the glove away from your body, pulling it inside out.
- Hold the removed glove in your gloved hand.
- Put your fingers inside the glove at the top of your wrist and peel off the second glove.
- Turn the second glove inside out while pulling it away from your body, leaving the first glove inside the second.
- Dispose of the gloves safely. Do not reuse.
- Perform hand hygiene immediately after removing the gloves.[30]
Gowns
Isolation gowns are used to protect the health care worker’s arms and exposed body areas and to prevent contamination of their clothing with blood, body fluids, and other potentially infectious material. Isolation gowns may be disposable or washable/reusable. See Figure 4.7[31] for an image of a nurse wearing an isolation gown along with goggles and a respirator. When using standard precautions, an isolation gown is worn only if contact with blood or body fluid is anticipated. However, when contact transmission-based precautions are in place, donning of both gown and gloves upon room entry is indicated to prevent unintentional contact of clothing with contaminated environmental surfaces.
Gowns are usually the first piece of PPE to be donned. Isolation gowns should be removed before leaving the patient room to prevent possible contamination of the environment outside the patient’s room. Isolation gowns should be removed in a manner that prevents contamination of clothing or skin. The outer, “contaminated,” side of the gown is turned inward and rolled into a bundle, and then it is discarded into a designated container to contain contamination. See more information about putting on and removing PPE in the subsection below.[32]

Masks
The mucous membranes of the mouth, nose, and eyes are susceptible portals of entry for infectious agents. Masks are used to protect these sites from entry of large infectious droplets. See Figure 4.8[33] for an image of nurse wearing a surgical mask. Masks have three primary purposes in health care settings:
- Used by health care personnel to protect them from contact with infectious material from patients (e.g., respiratory secretions and sprays of blood or body fluids), consistent with standard precautions and droplet transmission precautions
- Used by health care personnel when engaged in procedures requiring sterile technique to protect patients from exposure to infectious agents potentially carried in a health care worker’s mouth or nose
- Placed on coughing patients to limit potential dissemination of infectious respiratory secretions from the patient to others in public areas (i.e., respiratory hygiene)[34]
Masks may be used in combination with goggles or a face shield to provide more complete protection for the face. Masks should not be confused with respirators used during airborne transmission-based precautions to prevent inhalation of small, aerosolized infectious droplets.[35]

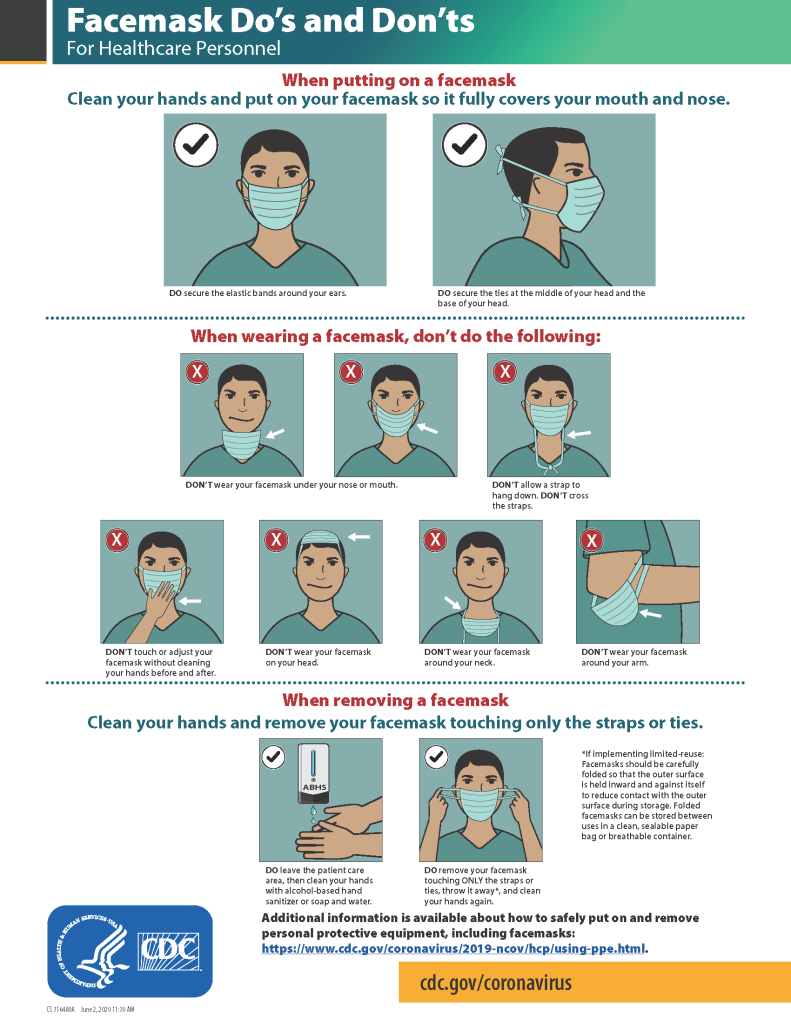
It is important to properly wear and remove masks to avoid contamination. See Figure 4.9[36] for CDC face mask recommendations for health care personnel.
Goggles/Face Shields
Eye protection chosen for specific work situations (e.g., goggles or face shields) depends upon the circumstances of exposure, other PPE used, and personal vision needs. Personal eyeglasses are not considered adequate eye protection. See Figure 4.10[37] for an image of a health care professional wearing a face shield along with a N95 respirator.

Respirators and PAPRs
Respiratory protection used during airborne transmission precautions requires the use of special equipment. Traditionally, a fitted respirator mask with N95 or higher filtration has been worn by health care professionals to prevent inhalation of small airborne infectious particles. A user-seal check (formerly called a “fit check”) should be performed by the wearer of a respirator each time a respirator is donned to minimize air leakage around the facepiece.
A newer piece of equipment used for respiratory protection is the powered air-purifying respirator (PAPR). A PAPR is an air-purifying respirator that uses a blower to force air through filter cartridges or canisters into the breathing zone of the wearer. This process creates an air flow inside either a tight-fitting facepiece or loose-fitting hood or helmet, providing a higher level of protection against aerosolized pathogens, such as COVID-19, than a N95 respirator. See Figure 4.11[38] for an example of PAPR in use.

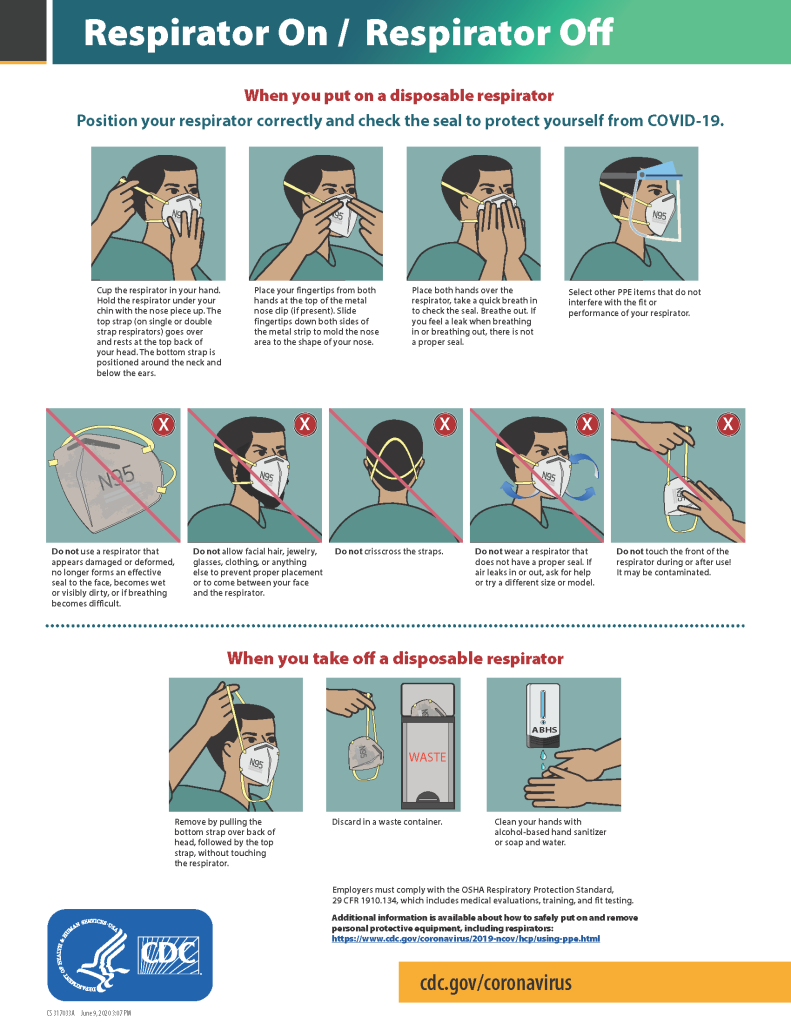
The CDC currently recommends N95 or higher level respirators for personnel exposed to patients with suspected or confirmed tuberculosis and other airborne diseases, especially during aerosol-generating procedures such as respiratory-tract suctioning.[39] It is important to apply, wear, and remove respirators appropriately to avoid contamination. See Figure 4.12[40] for CDC recommendations when wearing disposable respirators.
How to Put On (Don) PPE Gear
Follow agency policy for donning PPE according to transmission-based precautions. More than one donning method for putting on PPE may be acceptable. The CDC recommends the following steps for donning PPE[41]:
- Identify and gather the proper PPE to don. Ensure the gown size is correct.
- Perform hand hygiene using hand sanitizer or wash hands with soap and water.
- Put on the isolation gown. Tie all of the ties on the gown. Assistance may be needed by other health care personnel to tie back ties.
- Based on specific transmission-based precautions and agency policy, put on a mask or N95 respirator. The top strap should be placed on the crown (top) of the head, and the bottom strap should be at the base of the neck. If the mask has loops, hook them appropriately around your ears. Masks and respirators should extend under the chin, and both your mouth and nose should be protected. Perform a user-seal check each time you put on a respirator. If the respirator has a nosepiece, it should be fitted to the nose with both hands, but it should not be bent or tented. Masks typically require the nosepiece to be pinched to fit around the nose, but do not pinch the nosepiece of a respirator with one hand. Do not wear a respirator or mask under your chin or store it in the pocket of your scrubs between patients.
- Put on a face shield or goggles when indicated. When wearing an N95 respirator with eye protection, select eye protection that does not affect the fit or seal of the respirator and one that does not affect the position of the respirator. Goggles provide excellent protection for the eyes, but fogging is common. Face shields provide full-face coverage.
- Put on gloves. Gloves should cover the cuff (wrist) of the gown.
- You may now enter the patient’s room.
How to Take Off (Doff) PPE Gear
More than one doffing method for removing PPE may be acceptable. Train using your agency’s procedure, and practice until you have successfully mastered the steps to avoid contamination of yourself and others. There are established cases of nurses dying from disease transmitted during incorrect removal of PPE. Below are sample steps of doffing established by the CDC[44]:
- Remove the gloves. Ensure glove removal does not cause additional contamination of the hands. Gloves can be removed using more than one technique (e.g., glove-in-glove or bird beak).
- Remove the gown. Untie all ties (or unsnap all buttons). Some gown ties can be broken rather than untied; do so in a gentle manner and avoid a forceful movement. Reach up to the front of your shoulders and carefully pull the gown down and away from your body. Rolling the gown down is also an acceptable approach. Dispose of the gown in a trash receptacle. If it is a washable gown, place it in the specified laundry bin for PPE in the room.
- Health care personnel may now exit the patient room.
- Perform hand hygiene.
- Remove the face shield or goggles. Carefully remove the face shield or goggles by grabbing the strap and pulling upwards and away from head. Do not touch the front of the face shield or goggles.
- Remove and discard the respirator or face mask. Do not touch the front of the respirator or face mask. Remove the bottom strap by touching only the strap and bringing it carefully over the head. Grasp the top strap and bring it carefully over the head, and then pull the respirator away from the face without touching the front of the respirator. For masks, carefully untie (or unhook ties from the ears) and pull the mask away from your face without touching the front.
- Perform hand hygiene after removing the respirator/mask. If your workplace is practicing reuse, perform hand hygiene before putting it on again.
View a YouTube Video from the CDC on Putting on PPE[45]
View a YouTube Video from the CDC on Removing PPE[46]
Respiratory Hygiene
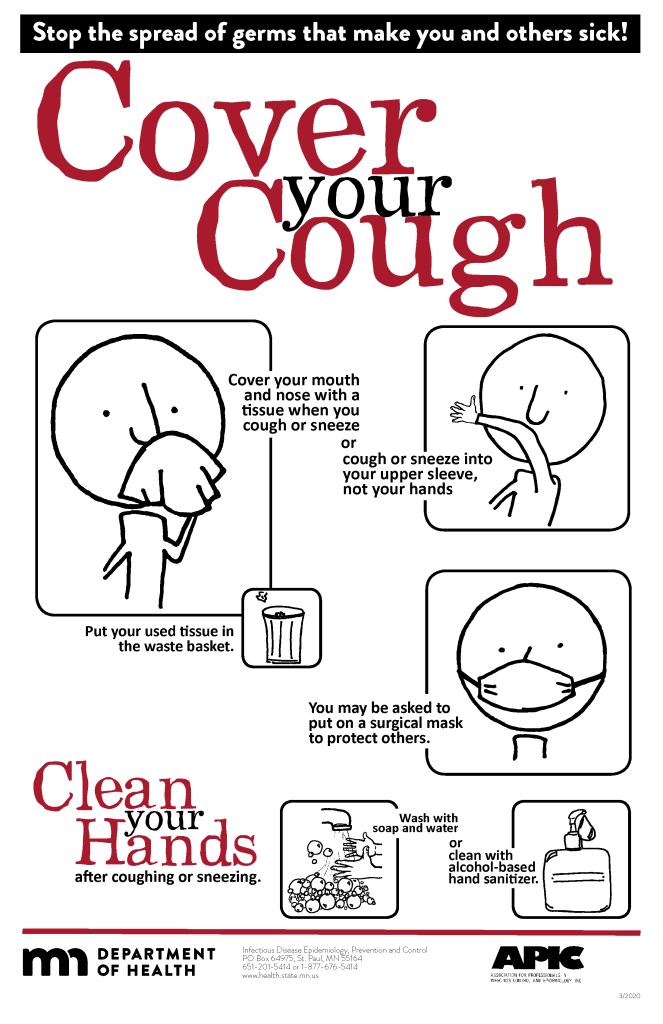
Respiratory hygiene is targeted at patients, accompanying family members and friends, and health care workers with undiagnosed transmissible respiratory infections. It applies to any person with signs of illness, including cough, congestion, rhinorrhea, or increased production of respiratory secretions when entering a health care facility. See Figure 4.13[47] for an example of a “Cover Your Cough” poster used in public areas to promote respiratory hygiene. The elements of respiratory hygiene include the following:
- Education of health care facility staff, patients, and visitors
- Posted signs, in language(s) appropriate to the population served, with instructions to patients and accompanying family members or friends
- Source control measures for a coughing person (e.g., covering the mouth/nose with a tissue when coughing and prompt disposal of used tissues, or applying surgical masks on the coughing person to contain secretions)
- Hand hygiene after contact with one’s respiratory secretions
- Spatial separation, ideally greater than 3 feet, of persons with respiratory infections in common waiting areas when possible.[48]
Health care personnel are advised to wear a mask and use frequent hand hygiene when examining and caring for patients with signs and symptoms of a respiratory infection. Health care personnel who have a respiratory infection are advised to avoid direct patient contact, especially with high-risk patients. If this is not possible, then a mask should be worn while providing patient care.[49]
Environmental Measures
Routine cleaning and disinfecting surfaces in patient-care areas are part of standard precautions. The cleaning and disinfecting of all patient-care areas are important for frequently touched surfaces, especially those closest to the patient that are most likely to be contaminated (e.g., bedrails, bedside tables, commodes, doorknobs, sinks, surfaces, and equipment in close proximity to the patient).
Medical equipment and instruments/devices must also be cleaned to prevent patient-to-patient transmission of infectious agents. For example, stethoscopes should be cleaned before and after use for all patients. Patients who have transmission-based precautions should have dedicated medical equipment that remains in their room (e.g., stethoscope, blood pressure cuff, thermometer). When dedicated equipment is not possible, such as a unit-wide bedside blood glucose monitor, disinfection after each patient’s use should be performed according to agency policy.[50]
Disposal of Contaminated Waste
Medical waste requires careful disposal according to agency policy. The Occupational Safety and Health Administration (OSHA) has established measures for discarding regulated medical waste items to protect the workers who generate medical waste, as well as those who manage the waste from point of generation to disposal. Contaminated waste is placed in a leak-resistant biohazard bag, securely closed, and placed in a labeled, leakproof, puncture-resistant container in a storage area. Sharps containers are used to dispose of sharp items such as discarded tubes with small amounts of blood, scalpel blades, needles, and syringes.[51]
Sharps Safety
Injuries due to needles and other sharps have been associated with transmission of blood-borne pathogens (BBP), including hepatitis B, hepatitis C, and HIV to health care personnel. The prevention of sharps injuries is an essential element of standard precautions and includes measures to handle needles and other sharp devices in a manner that will prevent injury to the user and to others who may encounter the device during or after a procedure. The Bloodborne Pathogens Standard is a regulation that prescribes safeguards to protect workers against health hazards related to blood-borne pathogens. It includes work practice controls, hepatitis B vaccinations, hazard communication and training, plans for when an employee is exposed to a BBP, and recordkeeping.
When performing procedures that include needles or other sharps, dispose of these items immediately in FDA-cleared sharps disposal containers. Additionally, to prevent needlestick injuries, needles and other contaminated sharps should not be recapped. See Figure 4.14[52] for an image of a sharps disposal container. FDA-cleared sharps disposal containers are made from rigid plastic and come marked with a line that indicates when the container should be considered full, which means it’s time to dispose of the container. When a sharps disposal container is about three-quarters full, follow agency policy for proper disposal of the container.
If you are stuck by a needle or other sharps or are exposed to blood or other potentially infectious materials in your eyes, nose, mouth, or on broken skin, immediately flood the exposed area with water and clean any wound with soap and water. Report the incident immediately to your instructor or employer and seek immediate medical attention according to agency and school policy.

Textiles and Laundry
Soiled textiles, including bedding, towels, and patient or resident clothing may be contaminated with pathogenic microorganisms. However, the risk of disease transmission is negligible if they are handled, transported, and laundered in a safe manner. Follow agency policy for handling soiled laundry using standard precautions. Key principles for handling soiled laundry are as follows:
- Do not shake items or handle them in any way that may aerosolize infectious agents.
- Avoid contact of one’s body and personal clothing with the soiled items being handled.
- Place soiled items in a laundry bag or designated bin in the patient’s room before transporting to a laundry area. When laundry chutes are used, they must be maintained to minimize dispersion of aerosols from contaminated items.[53]

