Implementation of Interventions
Open Resources for Nursing (Open RN)
Implementation is the fifth step of the nursing process (and the fifth Standard of Practice by the American Nurses Association). This standard is defined as, “The registered nurse implements the identified plan.” The RN may delegate planned interventions after considering the circumstance, person, task, communication, supervision, and evaluation, as well as the state Nurse Practice Act, federal regulation, and agency policy.[1]
Implementation of interventions requires the RN to use critical thinking and clinical judgment. After the initial plan of care is developed, continual reassessment of the client is necessary to detect any changes in the client’s condition requiring modification of the plan. The need for continual client reassessment underscores the dynamic nature of the nursing process and is crucial to providing safe care.
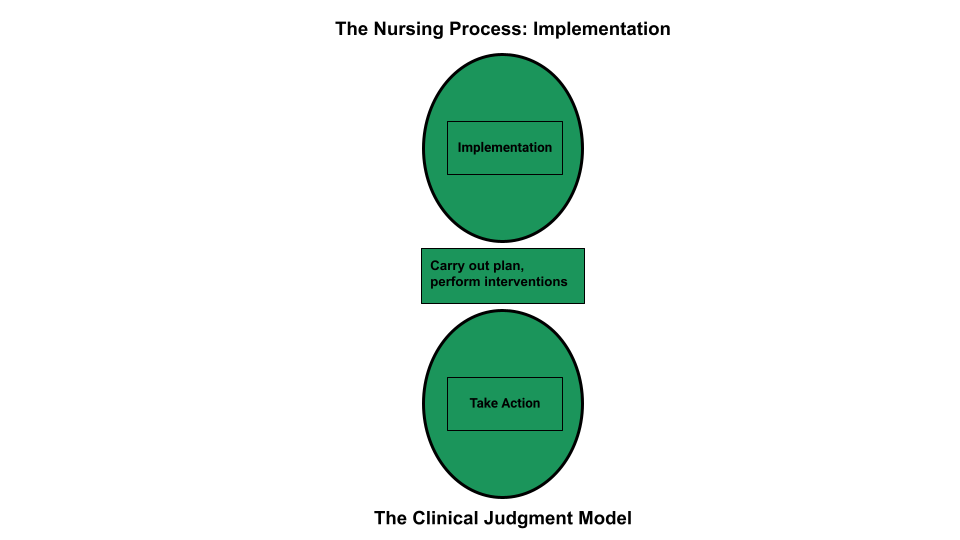
During the implementation phase of the nursing process, the nurse prioritizes planned interventions, assesses client safety while implementing interventions, delegates interventions as appropriate, and documents interventions performed. LPN/VNs have an active role in the Implementation phase, provided the interventions falls within the LPN/VN scope of practice. See Figure 4.14 for an illustration of how the Implementation phase of the nursing process correlates to NCSBN’s Clinical Judgment Measurement Model.[2]
Prioritizing Implementation of Interventions
Prioritizing implementation of interventions follows a similar method as to prioritizing nursing diagnoses. Maslow’s Hierarchy of Needs and the ABCs of airway, breathing, and circulation are used to establish top priority interventions. When possible, least invasive actions are usually preferred due to the risk of injury from invasive options. Read more about methods for prioritization under the “Diagnosis” section of this chapter.
The potential impact on future events, especially if a task is not completed at a certain time, is also included when prioritizing nursing interventions. For example, if a client is scheduled to undergo a surgical procedure later in the day, the nurse prioritizes initiating a NPO (nothing by mouth) prescription prior to completing pre-op client education about the procedure. The rationale for this decision is that if the client eats food or drinks water, the surgery time will be delayed. Knowing and understanding the client’s purpose for care, current situation, and expected outcomes are necessary to accurately prioritize interventions.
Client Safety
It is essential to consider client safety when implementing interventions. At times, clients may experience a change in condition that makes a planned nursing intervention or provider prescription no longer safe to implement. For example, an established nursing care plan for a client states, “The nurse will ambulate the client 100 feet three times daily.” However, during assessment this morning, the client reports feeling dizzy today, and their blood pressure is 90/60. Using critical thinking and clinical judgment, the nurse decides to not implement the planned intervention of ambulating the client. This decision and supporting assessment findings should be documented in the client’s chart and also communicated during the shift handoff report, along with appropriate notification of the provider of the client’s change in condition.
Implementing interventions goes far beyond implementing provider prescriptions and completing tasks identified on the nursing care plan and must focus on client safety. As frontline providers, nurses are in the position to stop errors before they reach the client.
In 2000 the Institute of Medicine (IOM) issued the historic, groundbreaking report titled To Err Is Human: Building a Safer Health System. The report stated that as many as 98,000 people die in U.S. hospitals each year as a result of preventable medical errors. To Err Is Human broke the silence that previously surrounded the consequences of medical errors and set a national agenda for reducing medical errors and improving client safety through the design of a safer health system.[3] In 2007 the IOM published a follow-up report titled Preventing Medication Errors and reported that more than 1.5 million Americans are injured every year in American hospitals, and the average hospitalized client experiences at least one medication error each day. This report emphasized actions that health care systems could take to improve medication safety.[4]
The Quality and Safety Education for Nurses (QSEN) project began in 2005 to assist in preparing future nurses to continuously improve the quality and safety of the health care systems in which they work. The vision of the QSEN project is to “inspire health care professionals to put quality and safety as core values to guide their work.”[5] Nurses and nursing students are expected to participate in quality improvement (QI) initiatives by identifying gaps where change is needed and assisting in implementing initiatives to resolve these gaps. Quality improvement is defined as, “The combined and unceasing efforts of everyone – health care professionals, clients and their families, researchers, payers, planners and educators – to make the changes that will lead to better client outcomes (health), better system performance (care), and better professional development (learning).”[6]
Delegation of Interventions
While implementing interventions, RNs may elect to delegate nursing tasks. Delegation is defined by the American Nurses Association as, “The assignment of the performance of activities or tasks related to client care to unlicensed assistive personnel or licensed practical nurses (LPNs) while retaining accountability for the outcome.”[7] RNs are accountable for determining the appropriateness of the delegated task according to the condition of the client and the circumstance; the communication provided to an appropriately trained LPN or UAP; the level of supervision provided; and the evaluation and documentation of the task completed. The RN must also be aware of the state Nurse Practice Act, federal regulations, and agency policy before delegating. The RN cannot delegate responsibilities requiring clinical judgment.[8] See the following box for information regarding legal requirements associated with delegation according to the Nurse Practice Act.
Delegation According to the Wisconsin Nurse Practice Act[9]
“During the supervision and direction of delegated acts a Registered Nurse shall do all of the following:
(a) Delegate tasks commensurate with educational preparation and demonstrated abilities of the person supervised.
(b) Provide direction and assistance to those supervised.
(c) Observe and monitor the activities of those supervised.
(d) Evaluate the effectiveness of acts performed under supervision.
The standard of practice for Licensed Practical Nurses in Wisconsin states, “In the performance of acts in basic patient situations, the LPN shall, under the general supervision of an RN or the direction of a provider:
(a) Accept only patient care assignments which the LPN is competent to perform.
(b) Provide basic nursing care. Basic nursing care is defined as care that can be performed following a defined nursing procedure with minimal modification in which the responses of the patient to the nursing care are predictable.
(c) Record nursing care given and report to the appropriate person changes in the condition of a patient.
(d) Consult with a provider in cases where an LPN knows or should know a delegated act may harm a patient.
(e) Perform the following other acts when applicable:
- Assist with the collection of data.
- Assist with the development and revision of a nursing care plan.
- Reinforce the teaching provided by an RN provider and provide basic health care instruction.
- Participate with other health team members in meeting basic patient needs.”
Read additional details about the scope of practice of registered nurses (RNs) and licensed practical nurses (LPNs) in Wisconsin’s Nurse Practice Act in Chapter N 6 Standards of Practice.
Read more about the American Nurses Association’s Principles for Delegation.
Table 4.7 outlines general guidelines for delegating nursing tasks in the state of Wisconsin according to the role of the health care team member.
Table 4.7 General Guidelines for Delegating Nursing Tasks
| RN | LPN | CNA | |
|---|---|---|---|
| Assessment | Complete client assessment | Assist with the collection of data for stable clients | Collect measurements such as weight, input/output, and vital signs in stable clients |
| Diagnosis | Analyze assessment data and create nursing diagnoses | Not applicable | Not applicable |
| Outcome Identification | Identify SMART client outcomes | Not applicable | Not applicable |
| Planning | Plan nursing interventions | Assist with the development of a nursing care plan | Not applicable |
| Implementation of Interventions | Implement independent, dependent, and collaborative nursing interventions; delegate interventions as appropriate, with supervision; document interventions performed | Participate with other health team members in meeting basic client needs and document interventions provided
Reinforce the teaching provided by an RN provider and provide basic health care instruction |
Implement and document delegated interventions associated with basic nursing care such as providing assistance in ambulating or tasks within their scope of practice |
| Evaluation | Evaluate the attainment of outcomes and revise the nursing care plan as needed | Contribute data regarding the achievement of client outcomes; assist in the revision of a nursing care plan | Not applicable |
Documentation of Interventions
As interventions are performed, they must be documented in the client’s record in a timely manner. As previously discussed in the “Ethical and Legal Issues” subsection of the “Basic Concepts” section, lack of documentation is considered a failure to communicate and a basis for legal action. A basic rule of thumb is if an intervention is not documented, it is considered not done in a court of law. It is also important to document administration of medication and other interventions in a timely manner to prevent errors that can occur due to delayed documentation time.
Coordination of Care and Health Teaching/Health Promotion
ANA’s Standard of Professional Practice for Implementation also includes the standards 5A Coordination of Care and 5B Health Teaching and Health Promotion.[10] Coordination of Care includes competencies such as organizing the components of the plan, engaging the client in self-care to achieve goals, and advocating for the delivery of dignified and holistic care by the interprofessional team. Health Teaching and Health Promotion is defined as, “Employing strategies to teach and promote health and wellness.”[11] Client education is an important component of nursing care and should be included during every client encounter. For example, client education may include teaching about side effects while administering medications or teaching clients how to self-manage their conditions at home.
Putting It Together
See an example of implementation in the following box.
Example of Implementation
Refer to Scenario C in the “Assessment” section of this chapter. The nurse implemented the nursing care plan documented in Appendix C. Interventions related to breathing were prioritized. Administration of the diuretic medication was completed first, and lung sounds were monitored frequently for the remainder of the shift. Weighing the client before breakfast was delegated to the CNA. The client was educated about her medications and methods to use to reduce peripheral edema at home. All interventions were documented in the electronic medical record (EMR).
Media Attributions
- Implementation in the Nursing Process Compared to the NCJMM
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- “Implementation Phase of the Nursing Process Compared to the NCSBN Clinical Judgment Model” by Tami Davis is licensed by CC BY 4.0. ↵
- Institute of Medicine (US) Committee on Quality of Health Care in America, Kohn, L. T., Corrigan, J. M., & Donaldson, M. S. (Eds.). (2000). To err is human: Building a safer health system. National Academies Press. https://pubmed.ncbi.nlm.nih.gov/25077248/ ↵
- Institute of Medicine. (2007). Preventing medication errors. National Academies Press. https://doi.org/10.17226/11623. ↵
- QSEN Institute. (n.d.). Project overview: The evolution of the quality and safety education for nurses (QSEN) initiative. http://qsen.org/about-qsen/project-overview/ ↵
- Batalden, P. B., & Davidoff, F. (2007). What is "quality improvement" and how can it transform healthcare?. BMJ Quality & Safety, 16(1), 2–3. https://doi.org/10.1136/qshc.2006.022046 ↵
- American Nurses Association. (2013). ANA’s principles for delegation by registered nurses to unlicensed assistive personnel (UAP). American Nurses Association. https://www.nursingworld.org/~4af4f2/globalassets/docs/ana/ethics/principlesofdelegation.pdf ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- Wisconsin Administrative Code. (2018). Chapter N 6 standards of practice for registered nurses and licensed practical nurses. https://docs.legis.wisconsin.gov/code/admin_code/n/6.pdf ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
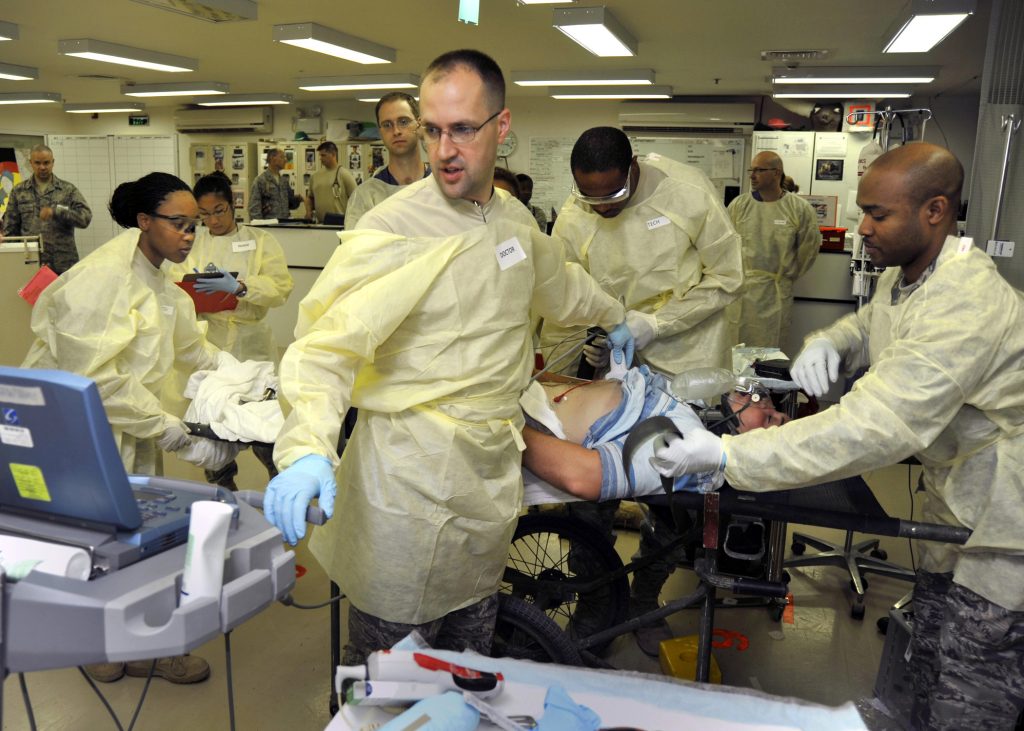
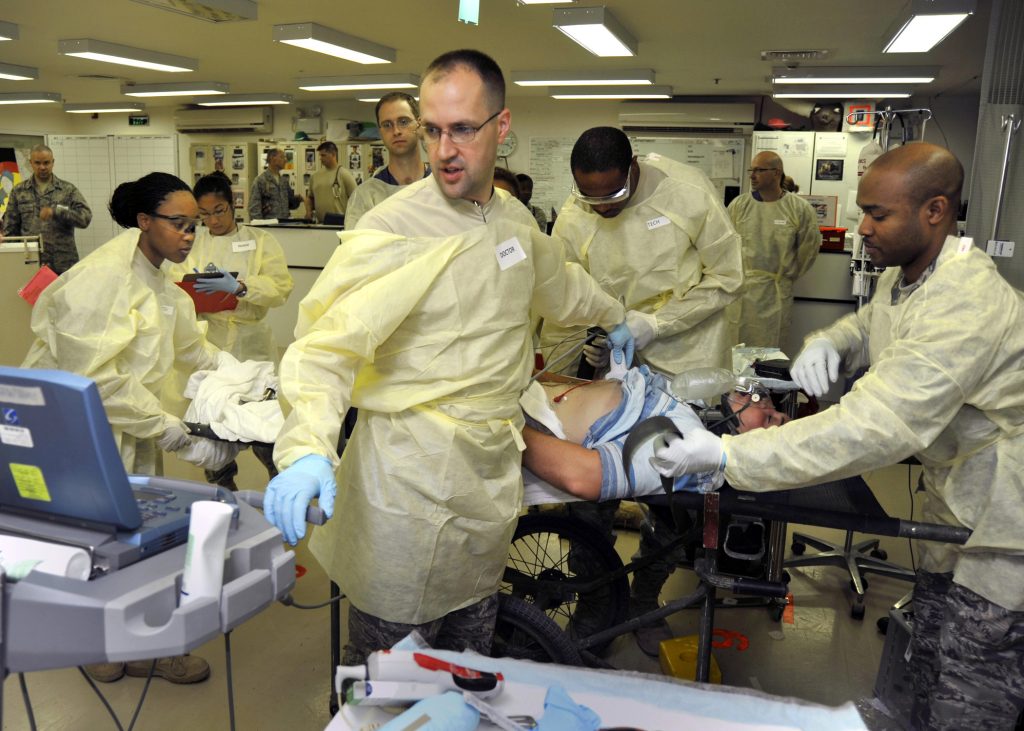
Stress within any health care profession occurs as a result of the challenging and dynamic conditions experienced in day-to-day work. See Figure 12.1[1] for an illustration of stress in a health care environment. Nurses and health care professionals are taxed with supporting clients and families in times of extensive life stress and change. Individuals who seek out care often experience rapid life changes as the result of a new diagnosis, altered body function, death of a family member, or significant mental distress. Nurses are frontline staff members who help clients and their families navigate these health stressors. It can be difficult to provide frontline support without taking on some of the stress encountered. As clients and families navigate their feelings of fear, frustration, anxiety, and anger, nurses are often the support members who first hear and react to these feelings. It is important to recognize the constant barrage of these emotions can take a toll, and it is challenging to not assume this emotional burden.
In addition to the emotional burden of providing support for multiple clients and their family members, nurses experience a variety of other stressors inherent to the health care environment itself. These stressors include issues such as environmental stress, increased workload, changing practice conditions, lack of resources, communication barriers, unfavorable working conditions, frequency of engagement with a variety of personnel, challenges in care coordination, workplace violence, alarm fatigue, and staff turnover. Research has identified that the variety of stressors experienced by nursing staff result in inherently greater levels of stress than that experienced in the wider working population.[2] Therefore, nurses must acknowledge the variety of stressors they encounter within the profession and identify strategies to mitigate these forces.
Nursing is charged with emotional situations and topics even on days when no other situational stressors have significant impact. One cannot participate in the significant conversations that accompany health care decision-making, provide patient education, and promote individual coping without acknowledging these conversations are more impactful than deciding, “What should we make for dinner?” By acknowledging this inherent job stress, nurses recognize that eliminating stress within the profession is not possible. There will always be a level of stress that accompanies the health care environment, and this underscores the importance of stress identification, mitigation, and incorporation of stress-reduction strategies.[3]
Stress within any health care profession occurs as a result of the challenging and dynamic conditions experienced in day-to-day work. See Figure 12.1[4] for an illustration of stress in a health care environment. Nurses and health care professionals are taxed with supporting clients and families in times of extensive life stress and change. Individuals who seek out care often experience rapid life changes as the result of a new diagnosis, altered body function, death of a family member, or significant mental distress. Nurses are frontline staff members who help clients and their families navigate these health stressors. It can be difficult to provide frontline support without taking on some of the stress encountered. As clients and families navigate their feelings of fear, frustration, anxiety, and anger, nurses are often the support members who first hear and react to these feelings. It is important to recognize the constant barrage of these emotions can take a toll, and it is challenging to not assume this emotional burden.
In addition to the emotional burden of providing support for multiple clients and their family members, nurses experience a variety of other stressors inherent to the health care environment itself. These stressors include issues such as environmental stress, increased workload, changing practice conditions, lack of resources, communication barriers, unfavorable working conditions, frequency of engagement with a variety of personnel, challenges in care coordination, workplace violence, alarm fatigue, and staff turnover. Research has identified that the variety of stressors experienced by nursing staff result in inherently greater levels of stress than that experienced in the wider working population.[5] Therefore, nurses must acknowledge the variety of stressors they encounter within the profession and identify strategies to mitigate these forces.
Nursing is charged with emotional situations and topics even on days when no other situational stressors have significant impact. One cannot participate in the significant conversations that accompany health care decision-making, provide patient education, and promote individual coping without acknowledging these conversations are more impactful than deciding, “What should we make for dinner?” By acknowledging this inherent job stress, nurses recognize that eliminating stress within the profession is not possible. There will always be a level of stress that accompanies the health care environment, and this underscores the importance of stress identification, mitigation, and incorporation of stress-reduction strategies.[6]

