7. Organizational Culture
Open Resources for Nursing (Open RN) and Amy Ertwine
Organizational Culture
The formal leaders of an organization provide a sense of direction and overall guidance for their employees by establishing organizational vision, mission, and values statements. An organization’s vision statement defines why the organization exists, describes how the organization is unique from similar organizations, and specifies what the organization is striving to be. The mission statement describes how the organization will fulfill its vision and establishes a common course of action for future endeavors. See Figure 4.1[1] for an illustration of a mission statement. A values statement establishes the values of an organization that assist with the achievement of its vision and mission. A values statement also provides strategic guidelines for decision-making, both internally and externally, by members of the organization. A values statement may also be reflected as the organization’s “core values,” which are the foundational ideals that guide the organization’s actions and decision-making processes. The vision, mission, and values statements are expressed in a concise and clear manner that is easily understood by members of the organization and the public.[2]

Organizational culture refers to the implicit values and beliefs that reflect the norms and traditions of an organization. An organization’s vision, mission, and values statements are the foundation of organizational culture. Because individual organizations have their own vision, mission, and values statements, each organization has a different culture.[3] Organizational culture helps reflect the expected norms and behaviors that are inherent to an organization. Expected conduct is comprised of the unwritten rules and standards that reflect how employees should behave in different situations. The culture also informs the common communication styles that are inherent to an organization, including both formal and informal channels. The culture may also be manifested outwardly through various symbols and artifacts that embedded within the organization. These may include specific logos, objects, or other physical manifestations of elements that represent the organization’s culture. Some organizations may also reflect their cultural values through activities or ceremonies held within the community.
As health care continues to evolve and new models of care are introduced, nursing managers must develop innovative approaches that address change while aligning with that organization’s vision, mission, and values. Leaders embrace the organization’s mission, identify how individuals’ work contributes to it, and ensure that outcomes advance the organization’s mission and purpose. Leaders use vision, mission, and values statements for guidance when determining appropriate responses to critical events and unforeseen challenges that are common in a complex health care system. Successful organizations require employees to be committed to following these strategic guidelines during the course of their work activities. Employees who understand the relationship between their own work and the mission and purpose of the organization will contribute to a stronger health care system that excels in providing first-class patient care. The vision, mission, and values provide a common organization-wide frame of reference for decision-making for both leaders and staff.[4] It is important for employees in health care organizations to have understanding of how their roles and responsibilities connect to the broader mission and vision of the organization. This alignment fosters a cohesive work environment where each staff member is motivated by a shared purpose, leading to more effective and high-quality patient care. It is important that both the leader and employee have clarity in the underlying vision, mission, and values of an organization. This involves responsibility for both the leader and employee. Leaders must articulate the organization’s vision, mission, and values clearly and consistently. This involves regular communication through meetings, written materials, etc. Employees share in the responsibility by being empowered to ask questions and seek clarification on how their daily tasks contribute to the organization’s overarching goals.
Learning Activity
Investigate the mission, vision, and values of a potential employer, as you would do prior to an interview for a job position.
Reflective Questions
- How well do the organization’s vision and values align with your personal values regarding health care?
- How well does the organization’s mission align with your professional objective in your resume?
Followership
Followership is described as the upward influence of individuals on their leaders and their teams. The actions of followers have an important influence on staff performance and patient outcomes. Being an effective follower requires individuals to contribute to the team not only by doing as they are told, but also by being aware and raising relevant concerns. Effective followers realize that they can initiate change and disagree or challenge their leaders if they feel their organization or unit is failing to promote wellness and deliver safe, value-driven, and compassionate care. Leaders who gain the trust and dedication of followers are more effective in their leadership role. Everybody has a voice and a responsibility to take ownership of the workplace culture, and good followership contributes to the establishment of high-functioning and safety-conscious teams.[5] Key elements of effective followership include proactive engagement, constructive communication, collaboration, advocacy, continuous improvement, and a supportive leadership environment.
In order to demonstrate proactive engagement, followers must also be initiators. Effective followers do not passively wait for instruction by rather take initiative to address issues, propose solutions, and contribute to ideas. They recognize the importance of their voice in engaging in problem-solving and understand that being an effective follower does not mean being passive in their role. Effective followers also employ a keen situational awareness where they maintain vigilant assessment of the environment and potential risks, ensuring that they act in the best interests of clients. They must be confident that they can raise concerns if they identify potential problems or unsafe practices. This reflects a culture where followers feels that their feedback is welcomed and valued. Effective followership also involves communication practices in which the message is clearly conveyed, measures to confirm the message are employed, and the confirmation is received. To be an effective follower, support of the team’s goals must be a central tenet of one’s work. Collaboration with others involves supporting colleagues and working together toward the common goal even when viewpoints may differ. Identifying strategies that create a respectful opportunity to debate and explore different opinions is important to effective followership. Additionally, followers must take accountability for their own actions while understanding how their role and performance impacts the function of the team, as well as client outcomes. Effective followers also practice ethical advocacy, ensuring that the needs of clients are prioritized and respected. This advocacy also involves the ability to courageously challenge any decisions or actions that may jeopardize care or organizational values. Finally, effective followers engage in continuous learning to enhance their skills and knowledge. They seek feedback and use the feedback to contribute to their own performance and also the growth of the team. Effective followership is further cultivated when leaders and followers come together with mutual respect, trust, and work with a purposeful drive toward shared goals that reflect the organization’s mission.
Team members impact patient safety by following teamwork guidelines for good followership. For example, strategies such as closed-loop communication are important tools to promote patient safety.
Read more about communication and teamwork strategies in the “Collaboration Within the Interprofessional Team” chapter.
Leadership and Management Characteristics
Leadership and management are terms often used interchangeably, but they are two different concepts with many overlapping characteristics. Leadership is the art of establishing direction and influencing and motivating others to achieve their maximum potential to accomplish tasks, objectives, or projects.[6],[7] See Figure 4.2[8] for an illustration of team leadership. There is no universally accepted definition or theory of nursing leadership, but there is increasing clarity about how it differs from management.[9] Management refers to roles that focus on tasks such as planning, organizing, prioritizing, budgeting, staffing, coordinating, and reporting.[10] The overriding function of management has been described as providing order and consistency to organizations, whereas the primary function of leadership is to produce change and movement.[11] View a comparison of the characteristics of management and leadership in Table 4.2a.

Table 4.2a. Management and Leadership Characteristics[12]
| MANAGEMENT | LEADERSHIP |
|---|---|
Planning, Organizing, and Prioritizing
|
Establishing Direction
|
Budgeting and Staffing
|
Influencing Others
|
Coordinating and Problem-Solving
|
Motivating
|
Leader Vs. Manager Case Activity
Utilizing the information from the table above, review the following cases and identify whether the individual is serving as a leader or manager based upon the actions taken within the case scenario. Include supportive rationale for your decision regarding the role.
Case 1: Sima, the head nurse, reviews the upcoming schedule and allocates resources to ensure each shift is adequately staffed. She also makes assignments for the nursing staff based on their skills and patient needs. Additionally, she is responsible for hiring new staff and, when necessary, terminating employees who do not meet performance standards.
Case 2: Juan, a senior nurse, is passionate about improving patient care. He identifies an issue with the current handoff process between shifts and proposes a new strategy that incorporates evidence-based practices to enhance communication and reduce errors. He reaches out to his team at their monthly department meetings in order to develop a shared vision for this change and encourages them to partner with him on the new process.
Case 3: Maria, a unit supervisor, holds a meeting to set specific goals and time frames for the department’s upcoming projects. She prioritizes tasks for the team and establishes policies and procedures to ensure these tasks are completed efficiently and within the given deadlines.
Case 4: Emily, the nurse director, is tasked with preparing the budget for the upcoming fiscal year. She allocates resources effectively to ensure all departments are adequately funded. Emily also manages the staffing needs, ensuring that the hiring and termination processes are handled efficiently.
Case 5: Rachel, an experienced nurse, takes the time to build effective teamwork within her unit. She advocates for her patients, their families, and the nursing profession as a whole. Rachel communicates openly and listens to her team’s concerns, ensuring everyone feels valued and heard.
Not all nurses are managers, but all nurses are leaders because they encourage individuals to achieve their goals. The American Nurses Association (ANA) established Leadership as a Standard of Professional Performance for all registered nurses. Standards of Professional Performance are “authoritative statements of action and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently.”[13] See the competencies of the ANA Leadership standard in the following box and additional content in other chapters of this book.
Competencies of ANA’s Leadership Standard of Professional Performance
- Promotes effective relationships to achieve quality outcomes and a culture of safety
- Leads decision-making groups
- Engages in creating an interprofessional environment that promotes respect, trust, and integrity
- Embraces practice innovations and role performance to achieve lifelong personal and professional goals
- Communicates to lead change, influence others, and resolve conflict
- Implements evidence-based practices for safe, quality health care and health care consumer satisfaction
- Demonstrates authority, ownership, accountability, and responsibility for appropriate delegation of nursing care
- Mentors colleagues and others to embrace their knowledge, skills, and abilities
- Participates in professional activities and organizations for professional growth and influence
- Advocates for all aspects of human and environmental health in practice and policy
Read additional content related to leadership and management activities in corresponding chapters of this book:
- Read about the culture of safety in the “Legal Implications” chapter.
- Read about effective interprofessional teamwork and resolving conflict in the “Collaboration Within the Interprofessional Team” chapter.
- Read about quality improvement and implementing evidence-based practices in the “Quality and Evidence-Based Practice” chapter.
- Read more about delegation, supervision, and accountability in the “Delegation and Supervision” chapter.
- Read about professional organizations and advocating for patients, communities, and their environments in the “Advocacy” chapter.
- Read about budgets and staffing in the “Health Care Economics” chapter.
- Read about prioritization in the “Prioritization” chapter.
Leadership Theories and Styles
In the 1930s Kurt Lewin, the father of social psychology, originally identified three leadership styles: authoritarian, democratic, and laissez-faire.[14],[15]
Authoritarian leadership means the leader has full power. Authoritarian leaders tell team members what to do and expect team members to execute their plans. When fast decisions must be made in emergency situations, such as when a patient “codes,” the authoritarian leader makes quick decisions and provides the group with direct instructions. However, there are disadvantages to authoritarian leadership. Authoritarian leaders are more likely to disregard creative ideas of other team members, causing resentment and stress.[16]
Democratic leadership balances decision-making responsibility between team members and the leader. Democratic leaders actively participate in discussions, but also make sure to listen to the views of others. For example, a nurse supervisor may hold a meeting regarding an increased incidence of patient falls on the unit and ask team members to share their observations regarding causes and potential solutions. The democratic leadership style often leads to positive, inclusive, and collaborative work environments that encourage team members’ creativity. Under this style, the leader still retains responsibility for the final decision.[17]
Laissez-faire is a French word that translates to English as, “leave alone.” Laissez-faire leadership gives team members total freedom to perform as they please. Laissez-faire leaders do not participate in decision-making processes and rarely offer opinions. The laissez-faire leadership style can work well if team members are highly skilled and highly motivated to perform quality work. However, without the leader’s input, conflict and a culture of blame may occur as team members disagree on roles, responsibilities, and policies. By not contributing to the decision-making process, the leader forfeits control of team performance.[18]
Over the decades, Lewin’s original leadership styles have evolved into many styles of leadership in health care, such as passive-avoidant, transactional, transformational, servant, resonant, and authentic.[19],[20] Many of these leadership styles have overlapping characteristics. See Figure 4.3[21] for a comparison of various leadership styles in terms of engagement.

Passive-avoidant leadership is similar to laissez-faire leadership and is characterized by a leader who avoids taking responsibility and confronting others. Employees perceive the lack of control over the environment resulting from the absence of clear directives. Organizations with this type of leader have high staff turnover and low retention of employees. These types of leaders tend to react and take corrective action only after problems have become serious and often avoid making any decisions at all.[22]
Transactional leadership involves both the leader and the follower receiving something for their efforts; the leader gets the job done and the follower receives pay, recognition, rewards, or punishment based on how well they perform the tasks assigned to them.[23] Staff generally work independently with no focus on cooperation among employees or commitment to the organization.[24]
Transformational leadership involves leaders motivating followers to perform beyond expectations by creating a sense of ownership in reaching a shared vision.[25] It is characterized by a leader’s charismatic influence over team members and includes effective communication, valued relationships, and consideration of team member input. Transformational leaders know how to convey a sense of loyalty through shared goals, resulting in increased productivity, improved morale, and increased employees’ job satisfaction.[26] They often motivate others to do more than originally intended by inspiring them to look past individual self-interest and perform to promote team and organizational interests.[27]
Servant leadership focuses on the professional growth of employees while simultaneously promoting improved quality care through a combination of interprofessional teamwork and shared decision-making. Servant leaders assist team members to achieve their personal goals by listening with empathy and committing to individual growth and community-building. They share power, put the needs of others first, and help individuals optimize performance while forsaking their own personal advancement and rewards.[28]
Visit the Greenleaf Center site to learn more about What is Servant Leadership?
Resonant leaders are in tune with the emotions of those around them, use empathy, and manage their own emotions effectively. Resonant leaders build strong, trusting relationships and create a climate of optimism that inspires commitment even in the face of adversity. They create an environment where employees are highly engaged, making them willing and able to contribute with their full potential.[29]
Authentic leaders have an honest and direct approach with employees, demonstrating self-awareness, internalized moral perspective, and relationship transparency. They strive for trusting, symmetrical, and close leader–follower relationships; promote the open sharing of information; and consider others’ viewpoints.[30]
Table 4.2b. Characteristics of Leadership Styles
| Authoritarian | Democratic | Laissez-Faire or Passive-Avoidant |
|---|---|---|
|
|
|
| Transactional | Transformational | Servant |
|---|---|---|
|
|
|
| Resonant Leaders | Authentic Leaders |
|---|---|
|
|
Outcomes of Various Leadership Styles
Leadership styles affect team members, patient outcomes, and the organization. A systematic review of the literature published in 2021 showed significant correlations between leadership styles and nurses’ job satisfaction. Transformational leadership style had the greatest positive correlation with nurses’ job satisfaction, followed by authentic, resonant, and servant leadership styles. Passive-avoidant and laissez-faire leadership styles showed a negative correlation with nurses’ job satisfaction.[31] In this challenging health care environment, managers and nurse leaders must promote technical and professional competencies of their staff, but they must also act to improve staff satisfaction and morale by using appropriate leadership styles with their team.[32]
Systems Theory
Systems theory is based on the concept that systems do not function in isolation but rather there is an interdependence that exists between their parts. Systems theory assumes that most individuals strive to do good work but are affected by diverse influences within the system. Efficient and functional systems account for these diverse influences and improve outcomes by studying patterns and behaviors across the system.[33]
Many health care agencies have adopted a culture of safety based on systems theory. A culture of safety is an organizational culture that embraces error reporting by employees with the goal of identifying systemic causes of problems that can be addressed to improve patient safety. According to The Joint Commission, a culture of safety includes the following components[34]:
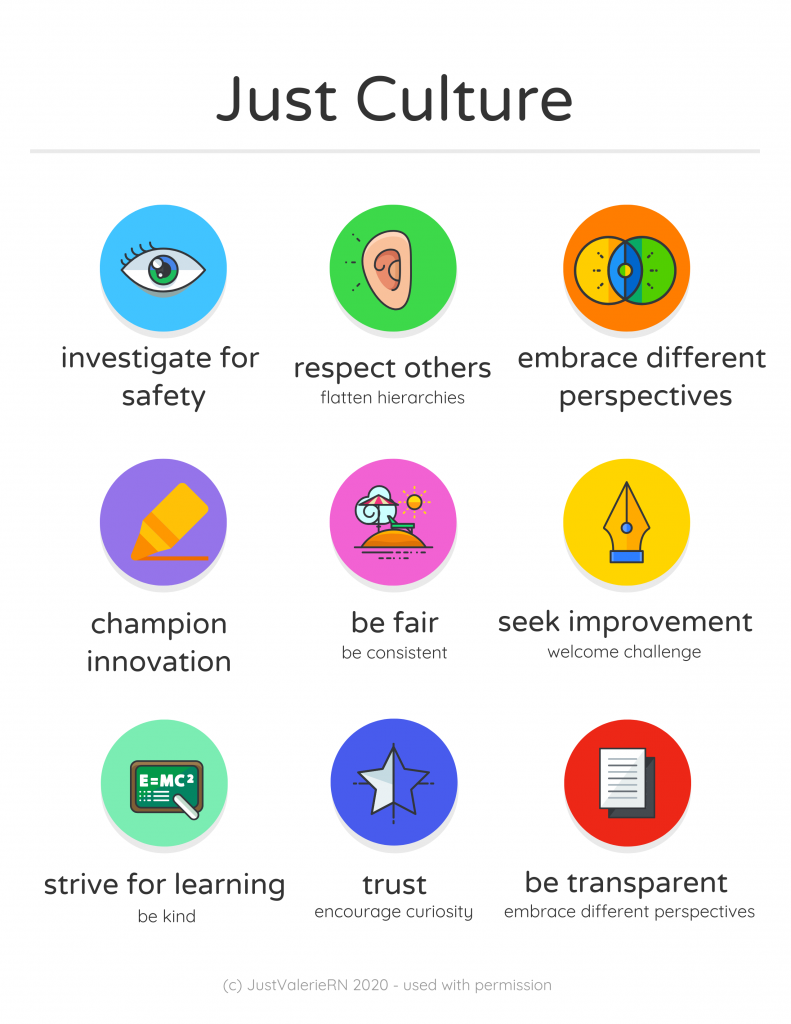
- Just Culture: A culture where people feel safe raising questions and concerns and report safety events in an environment that emphasizes a nonpunitive response to errors and near misses. Clear lines are drawn by managers between human error, at-risk, and reckless employee behaviors. See Figure 4.4[35] for an illustration of Just Culture.
- Reporting Culture: People realize errors are inevitable and are encouraged to speak up for patient safety by reporting errors and near misses. For example, nurses complete an “incident report” according to agency policy when a medication error occurs, or a client falls. Error reporting helps the agency manage risk and reduce potential liability.
- Learning Culture: People regularly collect information and learn from errors and successes while openly sharing data and information and applying best evidence to improve work processes and patient outcomes.
Just Culture
The American Nurses Association (ANA) officially endorses the Just Culture model. In 2019 the ANA published a position statement on Just Culture, stating, “Traditionally, healthcare’s culture has held individuals accountable for all errors or mishaps that befall patients under their care. By contrast, a Just Culture recognizes that individual practitioners should not be held accountable for system failings over which they have no control. A Just Culture also recognizes many individual or ‘active’ errors represent predictable interactions between human operators and the systems in which they work. However, in contrast to a culture that touts ‘no blame’ as its governing principle, a Just Culture does not tolerate conscious disregard of clear risks to patients or gross misconduct (e.g., falsifying a record or performing professional duties while intoxicated).”
The Just Culture model categorizes human behavior into three causes of errors. Consequences of errors are based on whether the error is a simple human error or caused by at-risk or reckless behavior.
- Simple human error: A simple human error occurs when an individual inadvertently does something other than what should have been done. Most medical errors are the result of human error due to poor processes, programs, education, environmental issues, or situations. These errors are managed by correcting the cause, looking at the process, and fixing the deviation. For example, a nurse appropriately checks the rights of medication administration three times, but due to the similar appearance and names of two different medications stored next to each other in the medication dispensing system, administers the incorrect medication to a patient. In this example, a root cause analysis reveals a system issue that must be modified to prevent future patient errors (e.g., change the labelling and storage of look alike-sound alike medication).
- At-risk behavior: An error due to at-risk behavior occurs when a behavioral choice is made that increases risk where the risk is not recognized or is mistakenly believed to be justified. For example, a nurse scans a patient’s medication with a barcode scanner prior to administration, but an error message appears on the scanner. The nurse mistakenly interprets the error to be a technology problem and proceeds to administer the medication instead of stopping the process and further investigating the error message, resulting in the wrong dosage of a medication being administered to the patient. In this case, ignoring the error message on the scanner can be considered “at-risk behavior” because the behavioral choice was considered justified by the nurse at the time.
- Reckless behavior: Reckless behavior is an error that occurs when an action is taken with conscious disregard for a substantial and unjustifiable risk.[36] For example, a nurse arrives at work intoxicated and administers the wrong medication to the wrong patient. This error is considered due to reckless behavior because the decision to arrive intoxicated was made with conscious disregard for substantial risk.
These examples show three different causes of medication errors that would result in different consequences to the employee based on the Just Culture model. Under the Just Culture model, after root cause analysis is completed, system-wide changes are made to decrease factors that contributed to the error. Managers appropriately hold individuals accountable for errors if they were due to simple human error, at-risk behavior, or reckless behaviors.
If an individual commits a simple human error, managers console the individual and consider changes in training, procedures, and processes. In the “simple human error” above, system-wide changes would be made to change the label and location of the medication to prevent future errors from occurring with the same medication.
Individuals committing at-risk behavior are held accountable for their behavioral choice and often require coaching with incentives for less risky behaviors and situational awareness. In the “at-risk behavior” example above where the nurse ignored an error message on the barcode scanner, mandatory training on using a barcode scanner and responding to errors would be implemented, and the manager would track the employee’s correct usage of the barcode scanner for several months following training.
If an individual demonstrates reckless behavior, remedial action and/or punitive action is taken.[37] In the “reckless behavior” example above, the manager would report the nurse’s behavior to the state’s Board of Nursing with mandatory substance abuse counseling to maintain their nursing license. Employment may be terminated with consideration of patterns of behavior.
A Just Culture in which employees aren’t afraid to report errors is a highly successful way to enhance patient safety, increase staff and patient satisfaction, and improve outcomes. Success is achieved through good communication, effective management of resources, and an openness to changing processes to ensure the safety of patients and employees. The infographic in Figure 4.4[38] illustrates the components of a culture of safety and Just Culture.
The principles of culture of safety, including Just Culture, Reporting Culture, and Learning Culture are also being adopted in nursing education. It’s understood that mistakes are part of learning and that a shared accountability model promotes individual- and system-level learning for improved patient safety. Under a shared accountability model, students are responsible for the following[39]:
- Being fully prepared for clinical experiences, including laboratory and simulation assignments
- Being rested and mentally ready for a challenging learning environment
- Accepting accountability for their part in contributing to a safe learning environment
- Behaving professionally
- Reporting their own errors and near mistakes
- Keeping up-to-date with current evidence-based practice
- Adhering to ethical and legal standards
Students know they will be held accountable for their actions but will not be blamed for system faults that lie beyond their control. They can trust that a fair process will be used to determine what went wrong if a patient care error or near miss occurs. Student errors and near misses are addressed based on an investigation determining if it was simple human error, an at-risk behavior, or reckless behavior. For example, a simple human error by a student can be addressed with coaching and additional learning opportunities to remedy the knowledge deficit. However, if a student acts with recklessness (for example, repeatedly arrives to clinical unprepared despite previous faculty feedback or falsely documents an assessment or procedure), they are appropriately and fairly disciplined, which may include dismissal from the program.[40]
See Table 4.2c describing classifications of errors using the Just Culture model.
Table 4.2c. Classification of Errors Using the Just Culture Model
| Human Error | At-Risk Behavior | Reckless Behavior |
|---|---|---|
| The caregiver made an error while working appropriately and focusing on the patient’s best interests. | The caregiver made a potentially unsafe choice resulting from faulty or self-serving decision-making. | The caregiver knowingly violated a rule and/or made a dangerous or unsafe choice. |
| Investigation reveals system factors contributing to similar errors by others with similar knowledge and skills. | Investigation reveals the system supports risky action and the caregiver requires coaching. | Investigation reveals the caregiver is accountable and needs retraining. |
| Manage by fixing system errors in processes, procedures, training, design, or environment. | Manage by coaching the caregiver and fixing any system issues:
|
Manage by disciplining the caregiver. If the system supports reckless behavior, it requires fixing. |
| CONSOLE | COACH | PUNISH |
Systems leadership refers to a set of skills used to catalyze, enable, and support the process of systems-level change that is encouraged by the Just Culture Model. Systems leadership is comprised of three interconnected elements:[41]
- The Individual: The skills of collaborative leadership to enable learning, trust-building, and empowered action among stakeholders who share a common goal
- The Community: The tactics of coalition building and advocacy to develop alignment and mobilize action among stakeholders in the system, both within and between organizations
- The System: An understanding of the complex systems shaping the challenge to be addressed
Just Culture Case Review
Review the following case descriptions. Identify the classification of error that has occurred and the recommended actions that should occur.
A chief nursing officer receives a daily report of organization incident reports and reviews the following incident:
Incident Description
Patient Mr. Joe Doden, Room 13067, Medical-Surgical floor
On the afternoon of May 15, 2024, Nurse Sarah was responsible for administering Mr. Joe Doden’s insulin dose. The insulin vials used by the hospital had recently been redesigned by the manufacturer, which led to changes in the labeling. The patient was scheduled to receive ten units of regular insulin at 14:30. However, at 1450 the patient turns on his call light, reports feeling unwell. He is shaky, confused, and sweating profusely. The patient’s glucose is checked, and he is found to be hypoglycemic. He is treated based upon the hypoglycemia protocol and recovers without further complication.
Case Investigation A
Action: Sarah RN who administered the insulin was following the protocol but mistakenly read the dosage due to a poorly designed label on the insulin vial. The nurse was focused on the patient’s best interests and followed all required steps.
Findings: The investigation revealed that the labeling on the insulin vials was confusing and had led to similar errors by other nurses in the past. The system’s design flaw contributed significantly to the error.
How would you classify this error? What actions should be taken?
Case Investigation B
Action: Sarah RN, due to time pressure and a high patient load, decided to skip the double-check protocol for administering the same insulin dose, believing it would save time without causing harm.
Findings: The investigation revealed that the hospital’s workload and time pressures often led to shortcuts in following safety protocols.
How would you classify this error? What actions should be taken?
Case Investigation C
Action: Sarah RN, is familiar with the protocol and knowingly bypassed the double check system, dismissing its importance and administering a medication dose on her own.
Findings: The investigation found that the nurse had a history of disregarding safety protocols, showing a pattern of reckless behavior. This behavior was not supported by the hospital’s policies or environment.
How would you classify this error? What actions should be taken?
Media Attributions
- Mission_statement
- 3D_Team_Leadership_Arrow_Concept
- Full_Range_Leadership_model-updated spelling
- “Mission_statement.jpg” by RadioFan (talk) is licensed under CC BY-SA 3.0 ↵
- This work is a derivative of Leadership and Influencing Change in Nursing by Joan Wagner and is licensed under CC BY 4.0 ↵
- This work is a derivative of Leadership and Influencing Change in Nursing by Joan Wagner and is licensed under CC BY 4.0 ↵
- This work is a derivative of Leadership and Influencing Change in Nursing by Joan Wagner and is licensed under CC BY 4.0 ↵
- This work is a derivative of Leadership and Influencing Change in Nursing by Joan Wagner and is licensed under CC BY 4.0 ↵
- Northhouse, P. (2004). Leadership: Theory and practice (9th ed.). Sage Publications. ↵
- Specchia, M. L., Cozzolino, M. R., Carini, E., Di Pilla, A., Galletti, C., Ricciardi, W., & Damiani, G. (2021). Leadership styles and nurses' job satisfaction. Results of a systematic review. International Journal of Environmental Research and Public Health, 18(4), 1552. https://doi.org/10.3390/ijerph18041552 ↵
- “3D_Team_Leadership_Arrow_Concept.jpg” by lumaxart is licensed under CC BY-SA 2.0 ↵
- Scully, N. J. (2015). Leadership in nursing: The importance of recognising inherent values and attributes to secure a positive future for the profession. Collegian, 22(4), 439-444. https://doi.org/10.1016/j.colegn.2014.09.004 ↵
- Hannaway, J. (1989). Managers managing: The workings of an administrative system. Oxford University Press, p. 39. ↵
- Northhouse, P. (2004). Leadership: Theory and practice (9th ed.). Sage Publications. ↵
- Northhouse, P. (2004). Leadership: Theory and practice (9th ed.). Sage Publications. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- Carlin, D. (2019, October 18). Democratic, authoritarian, laissez-faire: What type of leader are you? Forbes. https://www.forbes.com/sites/davidcarlin/2019/10/18/democratic-authoritarian-laissez-faire-what-type-of-leader-are-you/?sh=618359422a6b ↵
- Lewin, K., Lippitt, R., & White, R. K. (1939). Patterns of aggressive behavior in experimentally created “social climates.” Journal of Social Psychology, 10(2), 271-301. https://doi.org/10.1080/00224545.1939.9713366 ↵
- Carlin, D. (2019, October 18). Democratic, authoritarian, laissez-faire: What type of leader are you? Forbes. https://www.forbes.com/sites/davidcarlin/2019/10/18/democratic-authoritarian-laissez-faire-what-type-of-leader-are-you/?sh=618359422a6b ↵
- Carlin, D. (2019, October 18). Democratic, authoritarian, laissez-faire: What type of leader are you? Forbes. https://www.forbes.com/sites/davidcarlin/2019/10/18/democratic-authoritarian-laissez-faire-what-type-of-leader-are-you/?sh=618359422a6b ↵
- Carlin, D. (2019, October 18). Democratic, authoritarian, laissez-faire: What type of leader are you? Forbes. https://www.forbes.com/sites/davidcarlin/2019/10/18/democratic-authoritarian-laissez-faire-what-type-of-leader-are-you/?sh=618359422a6b ↵
- Northhouse, P. (2004). Leadership: Theory and practice (9th ed.). Sage Publications. ↵
- Specchia, M. L., Cozzolino, M. R., Carini, E., Di Pilla, A., Galletti, C., Ricciardi, W., & Damiani, G. (2021). Leadership styles and nurses' job satisfaction. Results of a systematic review. International Journal of Environmental Research and Public Health, 18(4), 1552. https://doi.org/10.3390/ijerph18041552 ↵
- “Full_Range_Leadership_model.jpg” by John Pons is licensed under Public Domain, CC0 ↵
- Specchia, M. L., Cozzolino, M. R., Carini, E., Di Pilla, A., Galletti, C., Ricciardi, W., & Damiani, G. (2021). Leadership styles and nurses' job satisfaction. Results of a systematic review. International Journal of Environmental Research and Public Health, 18(4), 1552. https://doi.org/10.3390/ijerph18041552 ↵
- Northhouse, P. (2004). Leadership: Theory and practice (9th ed.). Sage Publications. ↵
- Specchia, M. L., Cozzolino, M. R., Carini, E., Di Pilla, A., Galletti, C., Ricciardi, W., & Damiani, G. (2021). Leadership styles and nurses' job satisfaction. Results of a systematic review. International Journal of Environmental Research and Public Health, 18(4), 1552. https://doi.org/10.3390/ijerph18041552 ↵
- Northhouse, P. (2004). Leadership: Theory and practice (9th ed.). Sage Publications. ↵
- Specchia, M. L., Cozzolino, M. R., Carini, E., Di Pilla, A., Galletti, C., Ricciardi, W., & Damiani, G. (2021). Leadership styles and nurses' job satisfaction. Results of a systematic review. International Journal of Environmental Research and Public Health, 18(4), 1552. https://doi.org/10.3390/ijerph18041552 ↵
- Specchia, M. L., Cozzolino, M. R., Carini, E., Di Pilla, A., Galletti, C., Ricciardi, W., & Damiani, G. (2021). Leadership styles and nurses' job satisfaction. Results of a systematic review. International Journal of Environmental Research and Public Health, 18(4), 1552. https://doi.org/10.3390/ijerph18041552 ↵
- Specchia, M. L., Cozzolino, M. R., Carini, E., Di Pilla, A., Galletti, C., Ricciardi, W., & Damiani, G. (2021). Leadership styles and nurses' job satisfaction. Results of a systematic review. International Journal of Environmental Research and Public Health, 18(4), 1552. https://doi.org/10.3390/ijerph18041552 ↵
- Specchia, M. L., Cozzolino, M. R., Carini, E., Di Pilla, A., Galletti, C., Ricciardi, W., & Damiani, G. (2021). Leadership styles and nurses' job satisfaction. Results of a systematic review. International Journal of Environmental Research and Public Health, 18(4), 1552. https://doi.org/10.3390/ijerph18041552 ↵
- Specchia, M. L., Cozzolino, M. R., Carini, E., Di Pilla, A., Galletti, C., Ricciardi, W., & Damiani, G. (2021). Leadership styles and nurses' job satisfaction. Results of a systematic review. International Journal of Environmental Research and Public Health, 18(4), 1552. https://doi.org/10.3390/ijerph18041552 ↵
- Specchia, M. L., Cozzolino, M. R., Carini, E., Di Pilla, A., Galletti, C., Ricciardi, W., & Damiani, G. (2021). Leadership styles and nurses' job satisfaction. Results of a systematic review. International Journal of Environmental Research and Public Health, 18(4), 1552. https://doi.org/10.3390/ijerph18041552 ↵
- Specchia, M. L., Cozzolino, M. R., Carini, E., Di Pilla, A., Galletti, C., Ricciardi, W., & Damiani, G. (2021). Leadership styles and nurses' job satisfaction. Results of a systematic review. International Journal of Environmental Research and Public Health, 18(4), 1552. https://doi.org/10.3390/ijerph18041552 ↵
- Anderson, B. R. (2016). Improving health care by embracing systems theory. The Journal of Thoracic and Cardiovascular Surgery, 152(2), 593-594. https://www.jtcvs.org/article/S0022-5223(16)30001-0/pdf ↵
- The Joint Commission. (2017, March 1). The essential role of leadership in developing a safety culture. Sentinel Event Alert, Issue 57. https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/sea_57_safety_culture_leadership_0317pdf.pdf ↵
- “Just Culture Infographic.png” by Valeria Palarski 2020. Used with permission. ↵
- American Nursing Association. (2010). Position statement: Just culture. https://www.nursingworld.org/~4afe07/globalassets/practiceandpolicy/health-and-safety/just_culture.pdf ↵
- American Nursing Association. (2010). Position statement: Just culture. https://www.nursingworld.org/~4afe07/globalassets/practiceandpolicy/health-and-safety/just_culture.pdf ↵
- “Just Culture Infographic.png” by Valeria Palarski 2020. Used with permission. ↵
- Barnsteiner, J., & Disch, J. (2017). Creating a fair and just culture in schools of nursing. American Journal of Nursing, 117(11), 42-48. https;//doi.org/10.1097/01.NAJ.0000526747.84173.97. ↵
- Barnsteiner, J., & Disch, J. (2017). Creating a fair and just culture in schools of nursing. American Journal of Nursing, 117(11), 42-48. https://doi.org/ 10.1097/01.NAJ.0000526747.84173.97. ↵
- Dreier, L., Nabarro, D., & Nelson, J. (2019). Systems leadership for sustainable development: Strategies for achieving system change. CR Initiative at Harvard Kennedy School. https://www.hks.harvard.edu/sites/default/files/centers/mrcbg/files/Systems%20Leadership.pdf ↵
Sample Documentation of Expected Cardiac & Peripheral Vascular Findings
Patient denies chest pain or shortness of breath. Vital signs are within normal limits. Point of maximum impulse palpable at the fifth intercostal space of the midclavicular line. No lifts, heaves, or thrills identified on inspection or palpation. JVD absent. S1 and S2 heart sounds in regular rhythm with no murmurs or extra sounds. Skin is warm, pink, and dry. Capillary refill is less than two seconds. Color, movement, and sensation are intact in upper and lower extremities. Peripheral pulses are present (+2) and equal bilaterally. No peripheral edema is noted. Hair is distributed evenly on lower extremities.
Sample Documentation of Unexpected Cardiac & Peripheral Vascular Findings
Patient reports increase in breathing difficulty and increased swelling of bilateral lower extremities over the last three days. Diminished pulses (+1) bilaterally and pitting edema (+2) in the bilateral lower extremities. Upon auscultation, an S3 heart sound is noted, and the patient has bilateral crackles in the posterior bases of the lungs. Skin is pink, warm, and dry with capillary refill of < 2 seconds. All other pulses are present (+2), and no other areas of edema are noted. JVD is absent.
A thorough assessment of the heart provides valuable information about the function of a patient’s cardiovascular system. Understanding how to properly assess the cardiovascular system and identifying both normal and abnormal assessment findings will allow the nurse to provide quality, safe care to the patient.
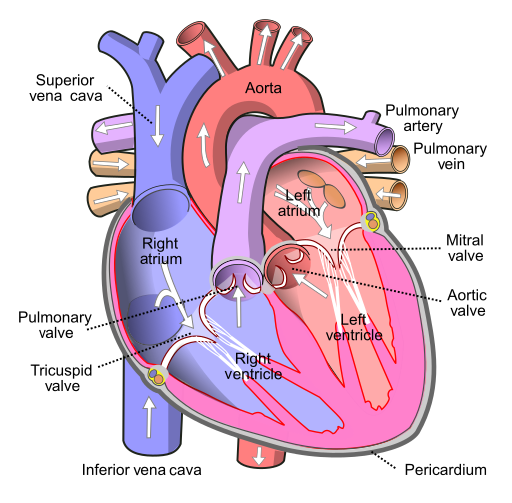
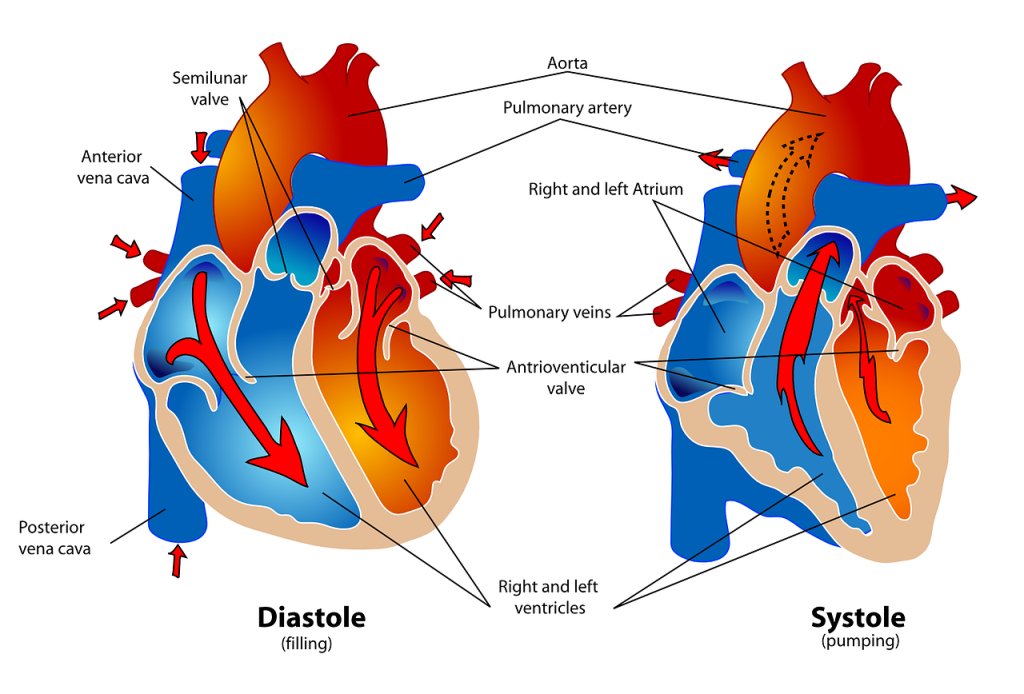
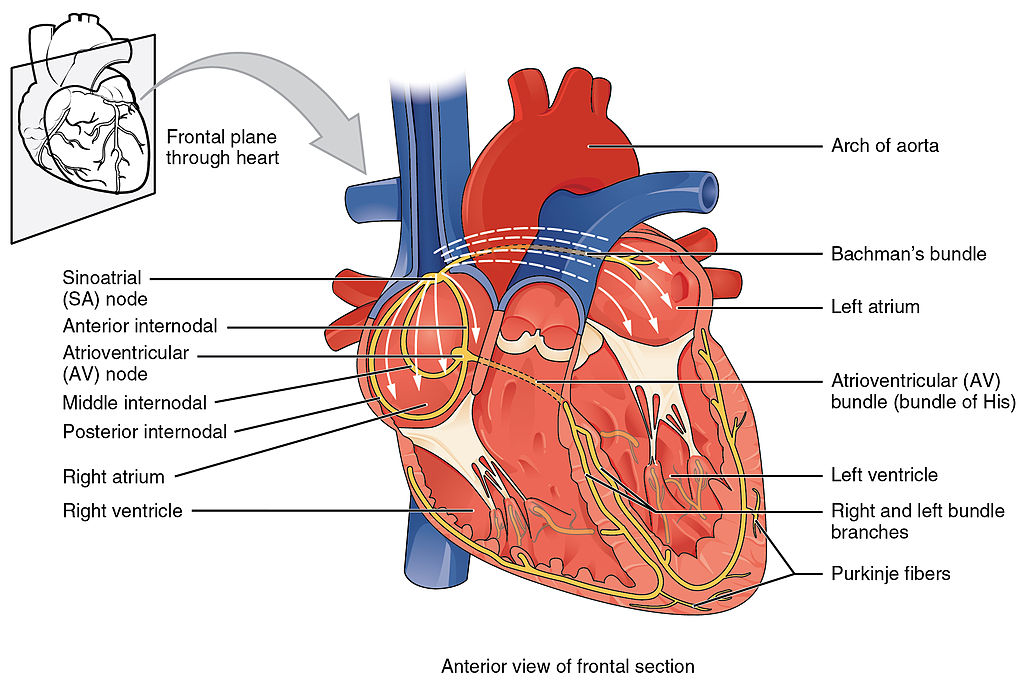
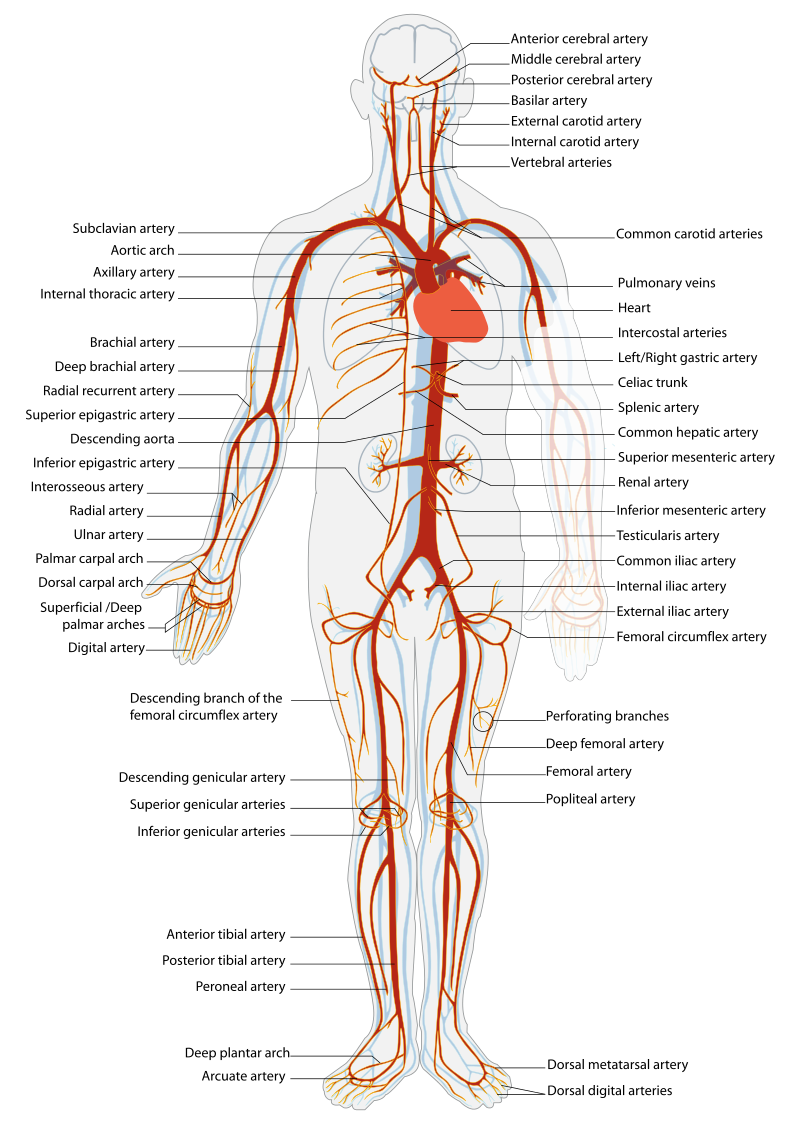
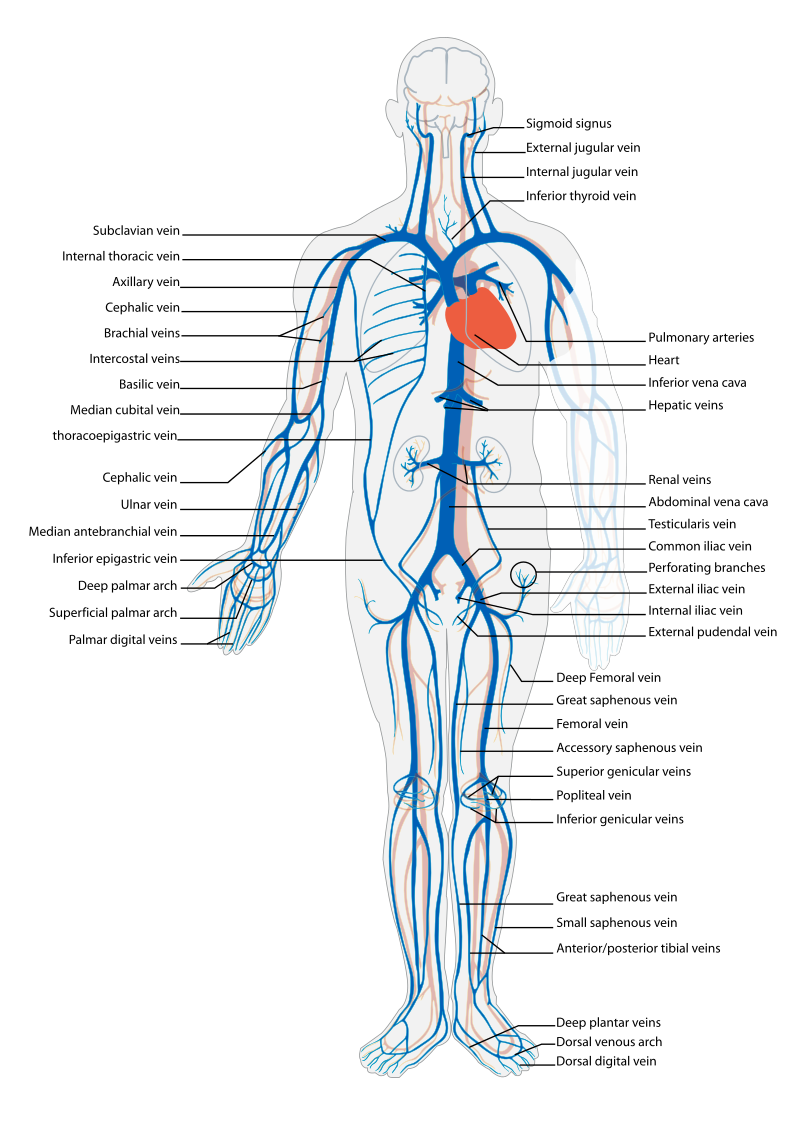
Before assessing a patient’s cardiovascular system, it is important to understand the various functions of the cardiovascular system. In addition to the information provided in the “Review of Cardiac Basics” section, the following images provide an overview of the cardiovascular system. Figure 9.1[1] provides an overview of the structure of the heart. Note the main cardiac structures are the atria, ventricles, and heart valves. Figure 9.2[2] demonstrates blood flow through the heart. Notice the flow of deoxygenated blood from the posterior and superior vena cava into the right atria and ventricle during diastole (indicated by blue coloring of these structures). The right ventricle then pumps deoxygenated blood to the lungs via the pulmonary artery during systole. At the same time, oxygenated blood from the lungs returns to the left atria and ventricle via the pulmonary veins during diastole (indicated by red coloring of these structures) and then is pumped out to the body via the aorta during systole. Figure 9.3[3] demonstrates the conduction system of the heart. This image depicts the conduction pathway through the heart as the tissue responds to electrical stimulation. Figure 9.4[4] illustrates the arteries of the circulatory system, and Figure 9.5[5] depicts the veins of the circulatory system. The purpose of these figures is to facilitate understanding of the electrical and mechanical function of the heart within the cardiovascular system.
Assessing the cardiovascular system includes performing several subjective and objective assessments. At times, assessment findings are modified according to life span considerations.
Subjective Assessment
The subjective assessment of the cardiovascular and peripheral vascular system is vital for uncovering signs of potential dysfunction. To complete the subjective cardiovascular assessment, the nurse begins with a focused interview. The focused interview explores past medical and family history, medications, cardiac risk factors, and reported symptoms. Symptoms related to the cardiovascular system include chest pain, peripheral edema, unexplained sudden weight gain, shortness of breath (dyspnea), irregular pulse rate or rhythm, dizziness, or poor peripheral circulation. Any new or worsening symptoms should be documented and reported to the health care provider.
Table 9.3a outlines questions used to assess symptoms related to the cardiovascular and peripheral vascular systems. Table 9.3b outlines questions used to assess medical history, medications, and risk factors related to the cardiovascular system. Information obtained from the interview process is used to tailor future patient education by the nurse.[6],[7],[8]
Table 9.3a Interview Questions for Cardiovascular and Peripheral Vascular Systems[9]
| Symptom | Question |
Follow-Up Safety Note: If findings indicate current severe symptoms suggestive of myocardial infarction or another critical condition, suspend the remaining cardiovascular assessment and obtain immediate assistance according to agency policy or call 911. |
|---|---|---|
| Chest Pain | Have you had any pain or pressure in your chest, neck, or arm? | Review how to assess a patient's chief complaint using the PQRSTU method in the "Health History" chapter.
|
| Shortness of Breath
(Dyspnea) |
Do you ever feel short of breath with activity?
Do you ever feel short of breath at rest? Do you feel short of breath when lying flat? |
What level of activity elicits shortness of breath?
How long does it take you to recover? Have you ever woken up from sleeping feeling suddenly short of breath How many pillows do you need to sleep, or do you sleep in a chair (orthopnea)? Has this recently changed? |
| Edema | Have you noticed swelling of your feet or ankles?
Have you noticed your rings, shoes, or clothing feel tight at the end of the day? Have you noticed any unexplained, sudden weight gain? Have you noticed any new abdominal fullness? |
Has this feeling of swelling or restriction gotten worse?
Is there anything that makes the swelling better (e.g., sitting with your feet elevated)? How much weight have you gained? Over what time period have you gained this weight? |
| Palpitations | Have you ever noticed your heart feels as if it is racing or “fluttering” in your chest?
Have you ever felt as if your heart “skips” a beat? |
Are you currently experiencing palpitations?
When did palpitations start? Have you previously been treated for palpitations? If so, what treatment did you receive? |
| Dizziness (Syncope) |
Do you ever feel light-headed?
Do you ever feel dizzy? Have you ever fainted? |
Can you describe what happened?
Did you have any warning signs? Did this occur with position change? |
| Poor Peripheral Circulation | Do your hands or feet ever feel cold or look pale or bluish?
Do you have pain in your feet or lower legs when exercising? |
What, if anything, brings on these symptoms?
How much activity is needed to cause this pain? Is there anything, such as rest, that makes the pain better? |
| Calf Pain | Do you currently have any constant pain in your lower legs? | Can you point to the area of pain with one finger? |
Table 9.3b Interview Questions Exploring Cardiovascular Medical History, Medications, and Cardiac Risk Factors
| Topic | Questions |
|---|---|
| Medical History | Have you ever been diagnosed with any heart or circulation conditions, such as high blood pressure, coronary artery disease, peripheral vascular disease, high cholesterol, heart failure, or valve problems?
Have you had any procedures done to improve your heart function, such as ablation or stent placement? Have you ever had a heart attack or stroke? |
| Medications | Do you take any heart-related medications, herbs, or supplements to treat blood pressure, chest pain, high cholesterol, cardiac rhythm, fluid retention, or the prevention of clots? |
| Cardiac Risk Factors | Have your parents or siblings been diagnosed with any heart conditions?
Do you smoke or vape?
If you do not currently smoke, have you smoked in the past?
Are you physically active during the week?
What does a typical day look like in your diet?
Do you drink alcoholic drinks?
Would you say you experience stress in your life?
How many hours of sleep do you normally get each day?
|
Objective Assessment
The physical examination of the cardiovascular system involves the interpretation of vital signs, inspection, palpation, and auscultation of heart sounds as the nurse evaluates for sufficient perfusion and cardiac output.
For more information about assessing a patient's oxygenation status as it relates to their cardiac output, visit the "Oxygenation" chapter in Open RN Nursing Fundamentals.
Equipment needed for a cardiovascular assessment includes a stethoscope, penlight, centimeter ruler or tape measure, and sphygmomanometer.[10]
Evaluate Vital Signs and Level of Consciousness
Interpret the blood pressure and pulse readings to verify the patient is stable before proceeding with the physical exam. Assess the level of consciousness; the patient should be alert and cooperative.
Inspection
- Skin color to assess perfusion. Inspect the face, lips, and fingertips for cyanosis or pallor. Cyanosis is a bluish discoloration of the skin, lips, and nail beds and indicates decreased perfusion and oxygenation. Pallor is the loss of color, or paleness of the skin or mucous membranes, as a result of reduced blood flow, oxygenation, or decreased number of red blood cells. Patients with light skin tones should be pink in color. For those with darker skin tones, assess for pallor on the palms, conjunctiva, or inner aspect of the lower lip.
- Jugular Vein Distension (JVD). Inspect the neck for JVD that occurs when the increased pressure of the superior vena cava causes the jugular vein to bulge, making it most visible on the right side of a person's neck. JVD should not be present in the upright position or when the head of bed is at 30-45 degrees.
- Precordium for abnormalities. Inspect the chest area over the heart (also called precordium) for deformities, scars, or any abnormal pulsations the underlying cardiac chambers and great vessels may produce.
- Extremities:
- Upper Extremities: Inspect the fingers, arms, and hands bilaterally noting Color, Warmth, Movement, Sensation (CWMS). Alterations or bilateral inconsistency in CWMS may indicate underlying conditions or injury. Assess capillary refill by compressing the nail bed until it blanches and record the time taken for the color to return to the nail bed. Normal capillary refill is less than 3 seconds.[11]
- Lower Extremities: Inspect the toes, feet, and legs bilaterally, noting CWMS, capillary refill, and the presence of peripheral edema, superficial distended veins, and hair distribution. Document the location and size of any skin ulcers.
- Edema: Note any presence of edema. Peripheral edema is swelling that can be caused by infection, thrombosis, or venous insufficiency due to an accumulation of fluid in the tissues. (See Figure 9.6[12] for an image of pedal edema.)[13]
- Deep Vein Thrombosis (DVT): A deep vein thrombosis (DVT) is a blood clot that forms in a vein deep in the body. DVT requires emergency notification of the health care provider and immediate follow-up because of the risk of developing a life-threatening pulmonary embolism.[14] Inspect the lower extremities bilaterally. Assess for size, color, temperature, and for presence of pain in the calves. Unilateral warmth, redness, tenderness, swelling in the calf, or sudden onset of intense, sharp muscle pain that increases with dorsiflexion of the foot is an indication of a deep vein thrombosis (DVT).[15] See Figure 9.7[16] for an image of a DVT in the patient's right leg, indicated by unilateral redness and edema.


Auscultation
Heart Sounds
Auscultation is routinely performed over five specific areas of the heart to listen for corresponding valvular sounds. These auscultation sites are often referred to by the mnemonic “APE To Man,” referring to Aortic, Pulmonic, Erb’s point, Tricuspid, and Mitral areas (see Figure 9.8[17] for an illustration of cardiac auscultation areas). The aortic area is the second intercostal space to the right of the sternum. The pulmonic area is the second intercostal space to the left of the sternum. Erb's point is directly below the pulmonic area and located at the third intercostal space to the left of the sternum. The tricuspid (or parasternal) area is at the fourth intercostal space to the left of the sternum. The mitral (also called apical or left ventricular area) is the fifth intercostal space at the midclavicular line.
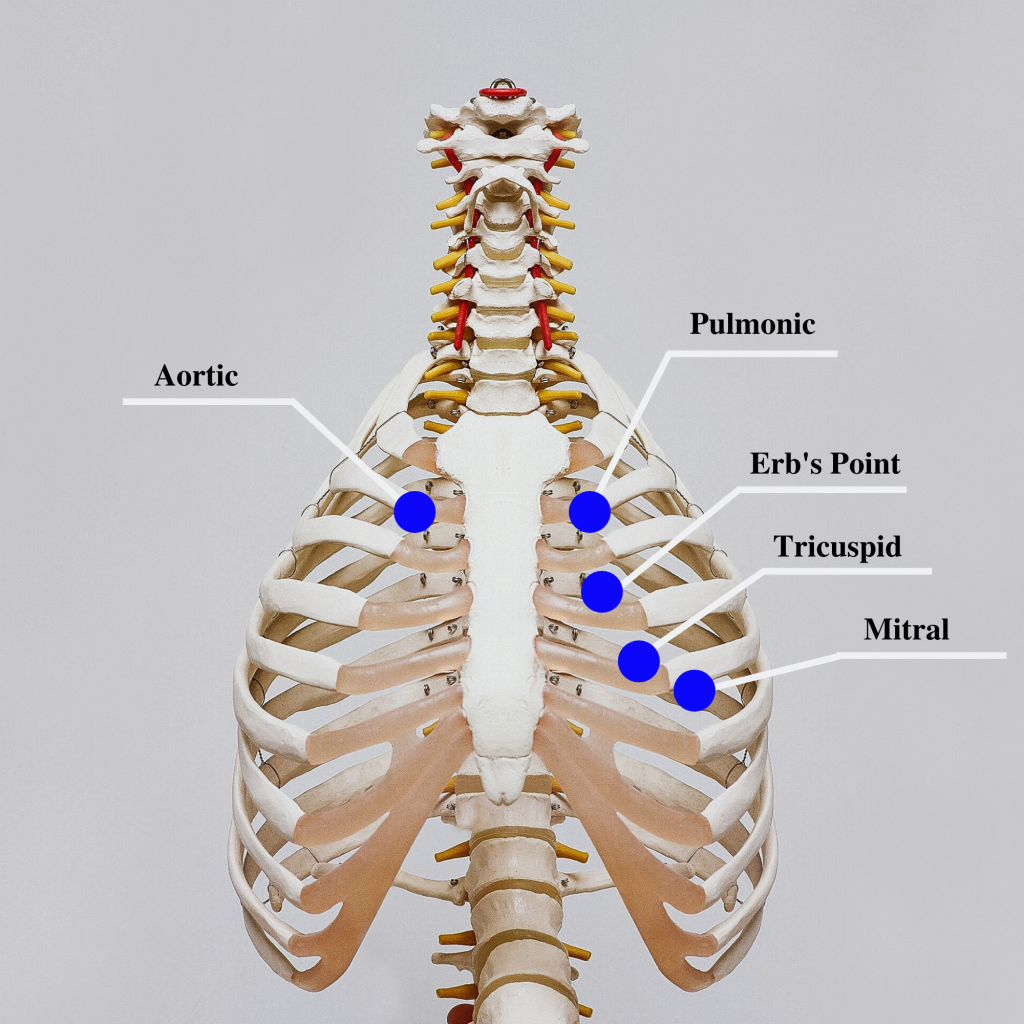
Auscultation usually begins at the aortic area (upper right sternal edge). Use the diaphragm of the stethoscope to carefully identify the S1 and S2 sounds. They will make a “lub-dub” sound. Note that when listening over the area of the aortic and pulmonic valves, the "dub" (S2) will sound louder than the "lub" (S1). Move the stethoscope sequentially to the pulmonic area (upper left sternal edge), Erb’s point (left third intercostal space at the sternal border), and tricuspid area (fourth intercostal space. When assessing the mitral area for female patients, it is often helpful to ask them to lift up their breast tissue so the stethoscope can be placed directly on the chest wall. Repeat this process with the bell of the stethoscope. The apical pulse should be counted over a 60-second period. For an adult, the heart rate should be between 60 and 100 with a regular rhythm to be considered within normal range. The apical pulse is an important assessment to obtain before the administration of many cardiac medications.
The first heart sound (S1) identifies the onset of systole, when the atrioventricular (AV) valves (mitral and tricuspid) close and the ventricles contract and eject the blood out of the heart. The second heart sound (S2) identifies the end of systole and the onset of diastole when the semilunar valves close, the AV valves open, and the ventricles fill with blood. S1 corresponds to the palpable pulse. When auscultating, it is important to identify the S1 ("lub") and S2 ("dub") sounds, evaluate the rate and rhythm of the heart, and listen for any extra heart sounds.
![]() Auscultating Heart Sounds
Auscultating Heart Sounds
- To effectively auscultate heart sounds, patient repositioning may be required. If it difficult to hear the heart sounds, ask the patient to lean forward if they are able, or lie on their left side. These positions move the heart closer to their chest wall and can increase the volume of the heart sounds heard on auscultation. This repositioning may be helpful in patients with increased adipose tissue in their chest wall or larger breasts.
- It is common to hear lung sounds when auscultating the heart sounds. It may be helpful to ask the patient to briefly hold their breath if lung sounds impede adequate heart auscultation. Limit the holding of breath to 10 seconds or as tolerated by the patient.
- Environmental noise can cause difficulty in auscultating heart sounds. Removing environmental noise by turning down the television volume or shutting the door may be required for an accurate assessment.
- Patients may try to talk to you as you are assessing their heart sounds. It is often helpful to explain the procedure such as, “I am going to take a few minutes to listen carefully to the sounds of blood flow going through your heart. Please try not to speak while I am listening, so I can hear the sounds better.”
Extra Heart Sounds
Extra heart sounds include clicks, murmurs, S3 and S4 sounds, and pleural friction rubs. These extra sounds can be difficult for a novice to distinguish, so if you notice any new or different sounds, consult an advanced practitioner or notify the provider. A midsystolic click, associated with mitral valve prolapse, may be heard with the diaphragm at the apex or left lower sternal border.
A click may be followed by a murmur. A murmur is a blowing or whooshing sound that signifies turbulent blood flow often caused by a valvular defect. New murmurs not previously recorded should be immediately communicated to the health care provider. In the aortic area, listen for possible murmurs of aortic stenosis and aortic regurgitation with the diaphragm of the stethoscope. In the pulmonic area, listen for potential murmurs of pulmonic stenosis and pulmonary and aortic regurgitation. In the tricuspid area, at the fourth and fifth intercostal spaces along the left sternal border, listen for the potential murmurs of tricuspid regurgitation, tricuspid stenosis, or ventricular septal defect.
S3 and S4 sounds, if present, are often heard best by asking the patient to lie on their left side and listening over the apex with the bell of the stethoscope. An S3 sound, also called a ventricular gallop, occurs after the S2 and sounds like “lub-dub-dah,” or a sound similar to a horse galloping. An S3 can occur when a patient is experiencing fluid overload, such as during an acute exacerbation of heart failure.[18] It can also be a normal finding in pregnancy due to increased blood flow through the ventricles.
The S4 sound, also called atrial gallop, occurs immediately before the S1 and sounds like “ta-lub-dub.” An S4 sound can occur with decreased ventricular compliance or coronary artery disease.[19]
A pericardial friction rub is caused by inflammation of the pericardium, with a creaky-scratchy noise generated as the parietal and visceral membranes rub together. It is best heard at the apex or left lower sternal border with the diaphragm as the patient sits up, leans forward, and holds their breath.
Carotid Sounds
The carotid artery may be auscultated for bruits. Bruits are a swishing sound due to turbulence in the blood vessel and may be heard due to atherosclerotic changes.
Palpation
Palpation is used to evaluate peripheral pulses, capillary refill, and for the presence of edema. When palpating these areas, also pay attention to the temperature and moisture of the skin.
Pulses
Compare the rate, rhythm, and quality of arterial pulses bilaterally, including the carotid, radial, brachial, posterior tibialis, and dorsalis pedis pulses. Review additional information about obtaining pulses in the "General Survey" chapter. Bilateral comparison for all pulses (except the carotid) is important for determining subtle variations in pulse strength. Carotid pulses should be palpated on one side at a time to avoid decreasing perfusion of the brain. The posterior tibial artery is located just behind the medial malleolus. It can be palpated by scooping the patient's heel in your hand and wrapping your fingers around so that the tips come to rest on the appropriate area just below the medial malleolus. The dorsalis pedis artery is located just lateral to the extensor tendon of the big toe and can be identified by asking the patient to flex their toe while you provide resistance to this movement. Gently place the tips of your second, third, and fourth fingers adjacent to the tendon, and try to feel the pulse.
The quality of the pulse is graded on a scale of 0 to 3, with 0 being absent pulses, 1 being decreased pulses, 2 is within normal range, and 3 being increased (also referred to as "bounding”). If unable to palpate a pulse, additional assessment is needed. First, determine if this is a new or chronic finding. Second, if available, use a Doppler ultrasound to determine the presence or absence of the pulse. Many agencies use Doppler ultrasound to document if a nonpalpable pulse is present. If the pulse is not found, this could be a sign of an emergent condition requiring immediate follow-up and provider notification. See Figures 9.9[20] and 9.10[21] for images of assessing pedal pulses.


Capillary Refill
The capillary refill test is performed on the nail beds to monitor perfusion, the amount of blood flow to tissue. Pressure is applied to a fingernail or toenail until it pales, indicating that the blood has been forced from the tissue under the nail. This paleness is called blanching. Once the tissue has blanched, pressure is removed. Capillary refill time is defined as the time it takes for the color to return after pressure is removed. If there is sufficient blood flow to the area, a pink color should return within 2 seconds after the pressure is removed.[22]
Review of Capillary Refill Test on YouTube[23].
Edema
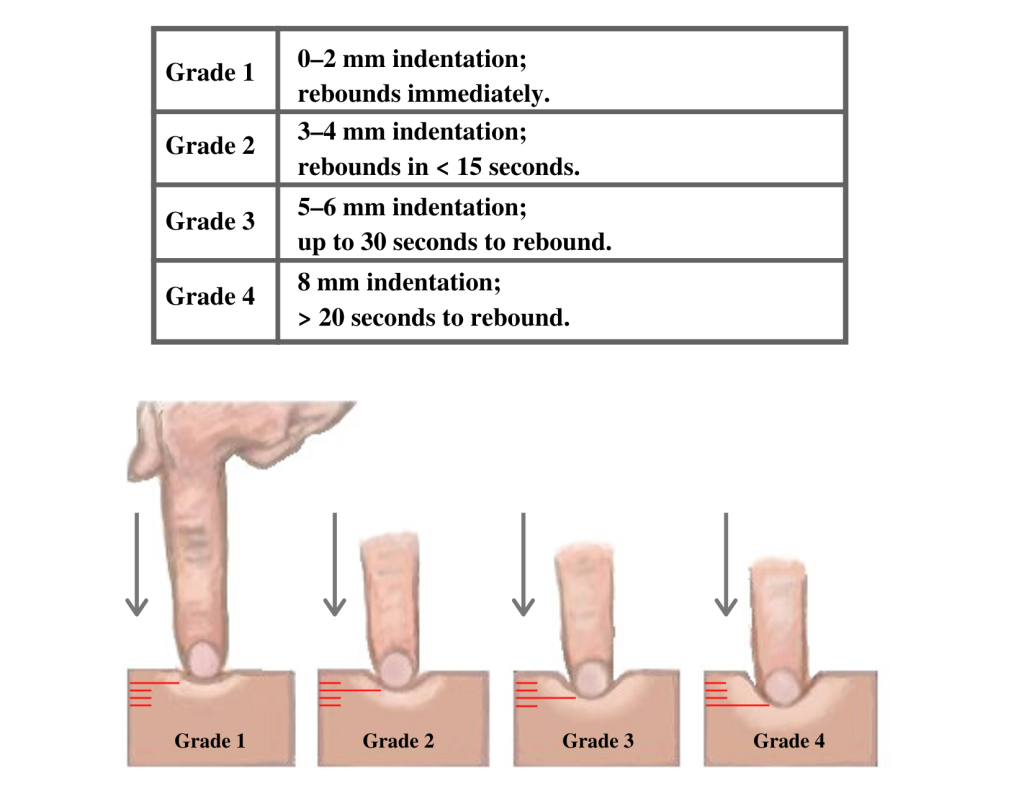
Edema occurs when one can visualize visible swelling caused by a buildup of fluid within the tissues. If edema is present on inspection, palpate the area to determine if the edema is pitting or nonpitting. Press on the skin to assess for indentation, ideally over a bony structure, such as the tibia. If no indentation occurs, it is referred to as nonpitting edema. If indentation occurs, it is referred to as pitting edema. See Figure 9.11[24] for images demonstrating pitting edema.

Note the depth of the indention and how long it takes for the skin to rebound back to its original position. The indentation and time required to rebound to the original position are graded on a scale from 1 to 4. Edema rated at 1+ indicates a barely detectable depression with immediate rebound, and 4+ indicates a deep depression with a time lapse of over 20 seconds required to rebound. See Figure 9.12[25] for an illustration of grading edema. Additionally, it is helpful to note edema may be difficult to observe in larger patients. It is also important to monitor for sudden changes in weight, which is considered a probable sign of fluid volume overload.
Heaves or Thrills
You may observe advanced practice nurses and other health care providers palpating the anterior chest wall to detect any abnormal pulsations the underlying cardiac chambers and great vessels may produce. Precordial movements should be evaluated at the apex (mitral area). It is best to examine the precordium with the patient supine because if the patient is turned on the left side, the apical region of the heart is displaced against the lateral chest wall, distorting the chest movements.[26] A heave or lift is a palpable lifting sensation under the sternum and anterior chest wall to the left of the sternum that suggests severe right ventricular hypertrophy. A thrill is a vibration felt on the skin of the precordium or over an area of turbulence, such as an arteriovenous fistula or graft.
Life Span Considerations
The cardiovascular assessment and expected findings should be modified according to common variations across the life span.
Infants and Children
A murmur may be heard in a newborn in the first few days of life until the ductus arteriosus closes.
When assessing the cardiovascular system in children, it is important to assess the apical pulse. Parameters for expected findings vary according to age group. After a child reaches adolescence, a radial pulse may be assessed. Table 9.3c outlines the expected apical pulse rate by age.
Table 9.3c Expected Apical Pulse by Age
| Age Group | Heart Rate |
|---|---|
| Preterm | 120-180 |
| Newborn (0 to 1 month) | 100-160 |
| Infant (1 to 12 months) | 80-140 |
| Toddler (1 to 3 years) | 80-130 |
| Preschool (3 to 5 years) | 80-110 |
| School Age (6 to 12 years) | 70-100 |
| Adolescents (13 to 18 years) | 60-90 |
Older Adults
In adults over age 65, irregular heart rhythms and extra sounds are more likely. An "irregularly irregular" rhythm suggests atrial fibrillation, and further investigation is required if this is a new finding. See the box below for more information about atrial fibrillation.
For more information on atrial fibrillation, visit the CDC Atrial Fibrillation webpage.
Expected Versus Unexpected Findings
After completing a cardiovascular assessment, it is important for the nurse to use critical thinking to determine if any findings require follow-up. Depending on the urgency of the findings, follow-up can range from calling the health care provider to calling the rapid response team. Table 9.3d compares examples of expected findings, meaning those considered within normal limits, to unexpected findings, which require follow-up. Critical conditions are those that should be reported immediately and may require notification of a rapid response team.
Table 9.3d Expected Versus Unexpected Findings on Cardiac Assessment
| Assessment | Expected Findings | Unexpected Findings (Document and notify the provider if this is a new finding*) |
|---|---|---|
| Inspection | Apical impulse may or may not be visible | Scars not previously documented that could indicate prior cardiac surgeries
Heave or lift observed in the precordium Chest anatomy malformations |
| Palpation | Apical pulse felt over midclavicular fifth intercostal space | Apical pulse felt to the left of the midclavicular fifth intercostal space
Additional movements over precordium such as a heave, lift, or thrill |
| Auscultation | S1 and S2 heart sounds in a regular rhythm | New irregular heart rhythm
Extra heart sounds such as a murmur, S3, or S4 |
| *CRITICAL CONDITIONS to report immediately | Symptomatic tachycardia at rest (HR>100 bpm)
Symptomatic bradycardia (HR<60 bpm) New systolic blood pressure (<100 mmHg) Orthostatic blood pressure changes (see “Blood Pressure” chapter for more information) New irregular heart rhythm New extra heart sounds such as a murmur, S3, or S4 New abnormal cardiac rhythm changes Reported chest pain, calf pain, or worsening shortness of breath |
See Table 9.3e for a comparison of expected versus unexpected findings when assessing the peripheral vascular system.
Table 9.3e Expected Versus Unexpected Peripheral Vascular Assessment Findings
| Assessment | Expected Findings | Unexpected Findings (Document or notify provider if new finding*) |
|---|---|---|
| Inspection | Skin color uniform and appropriate for race bilaterally
Equal hair distribution on upper and lower extremities Absence of jugular vein distention (JVD) Absence of edema Sensation and movement of fingers and toes intact |
Cyanosis or pallor, indicating decreased perfusion
Decreased or unequal hair distribution Presence of jugular vein distention (JVD) in an upright position or when head of bed is 30-45 degrees New or worsening edema Rapid and unexplained weight gain Impaired movement or sensation of fingers and toes |
| Palpation | Skin warm and dry
Pulses present and equal bilaterally Absence of edema Capillary refill less than 2 seconds |
Skin cool, excessively warm, or diaphoretic
Absent, weak/thready, or bounding pulses New irregular pulse New or worsening edema Capillary refill greater than 2 seconds Unilateral warmth, redness, tenderness, or edema, indicating possible deep vein thrombosis (DVT) |
| Auscultation | Carotid pulse | Carotid bruit |
| *CRITICAL CONDITIONS to report immediately | Cyanosis
Absent pulse (and not heard using Doppler device) Capillary refill time greater than 3 seconds Unilateral redness, warmth, and edema, indicating a possible deep vein thrombosis (DVT) |
“Sternum_composition.png” by Anatomography is licensed under CC BY-SA 2.1 Japan
“Sternum_composition.png” by Anatomography is licensed under CC BY-SA 2.1 Japan
Sample Documentation of Expected Cardiac & Peripheral Vascular Findings
Patient denies chest pain or shortness of breath. Vital signs are within normal limits. Point of maximum impulse palpable at the fifth intercostal space of the midclavicular line. No lifts, heaves, or thrills identified on inspection or palpation. JVD absent. S1 and S2 heart sounds in regular rhythm with no murmurs or extra sounds. Skin is warm, pink, and dry. Capillary refill is less than two seconds. Color, movement, and sensation are intact in upper and lower extremities. Peripheral pulses are present (+2) and equal bilaterally. No peripheral edema is noted. Hair is distributed evenly on lower extremities.
Sample Documentation of Unexpected Cardiac & Peripheral Vascular Findings
Patient reports increase in breathing difficulty and increased swelling of bilateral lower extremities over the last three days. Diminished pulses (+1) bilaterally and pitting edema (+2) in the bilateral lower extremities. Upon auscultation, an S3 heart sound is noted, and the patient has bilateral crackles in the posterior bases of the lungs. Skin is pink, warm, and dry with capillary refill of < 2 seconds. All other pulses are present (+2), and no other areas of edema are noted. JVD is absent.

