6. Delegation
Open Resources for Nursing (Open RN) and Amy Ertwine
There has been significant national debate over the difference between assignment and delegation over the past few decades. In 2019 the National Council of State Boards of Nursing (NCSBN) and the American Nurses Association (ANA) published updated joint National Guidelines on Nursing Delegation (NGND).[1] These guidelines apply to all levels of nursing licensure (advanced practice registered nurses [APRN], registered nurses [RN], and licensed practical/vocational nurses [LPN/VN]) when delegating when there is no specific guidance provided by the state’s Nurse Practice Act (NPA).[2] It is important to note that states have different laws and rules/regulations regarding delegation, so it is the responsibility of all licensed nurses to know what is permitted in their jurisdiction.
The NGND defines a delegatee as an RN, LPN/VN, or AP who is delegated a nursing responsibility by either an APRN, RN, or LPN/VN, is competent to perform the task, and verbally accepts the responsibility.[3] Delegation is allowing a delegatee to perform a specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role and not routinely performed, but the individual has obtained additional training and validated their competence to perform the delegated responsibility.[4] However, the licensed nurse still maintains accountability for overall client care. Delegated responsibility is a nursing activity, skill, or procedure that is transferred from a licensed nurse to a delegatee.[5] Accountability is defined as being answerable to oneself and others for one’s own choices, decisions, and actions as measured against a standard. Therefore, if a nurse does not feel it is appropriate to delegate a certain responsibility to a delegatee, the delegating nurse should perform the activity themselves.[6]
Delegation is summarized in the NGND as the following[7]:
- A delegatee is allowed to perform a specific nursing activity, skill, or procedure that is outside the traditional role and basic responsibilities of the delegatee’s current job.
- The delegatee has obtained the additional education and training and validated competence to perform the care/delegated responsibility. The context and processes associated with competency validation will be different for each activity, skill, or procedure being delegated. Competency validation should be specific to the knowledge and skill needed to safely perform the delegated responsibility, as well as to the level of the practitioner (e.g., RN, LPN/VN, AP) to whom the activity, skill, or procedure has been delegated. The licensed nurse who delegates the “responsibility” maintains overall accountability for the client, but the delegatee bears the responsibility for completing the delegated activity, skill, or procedure.
- The licensed nurse cannot delegate nursing clinical judgment or any activity that will involve nursing clinical judgment or critical decision-making to AP.
- Nursing responsibilities are delegated by a licensed nurse who has the authority to delegate and the delegated responsibility is within the delegator’s scope of practice.
An example of delegation is medication administration that is delegated by a licensed nurse to AP with additional training in some agencies, according to agency policy. This task is outside the traditional role of AP, but the delegatee has received additional training for this delegated responsibility and has completed competency validation in completing this task accurately.
An example illustrating the difference between assignment and delegation is assisting patients with eating. Feeding patients is typically part of the routine role of AP. However, if a client has recently experienced a stroke (i.e., cerebrovascular accident) or is otherwise experiencing swallowing difficulties (e.g., dysphagia), this task cannot be assigned to AP because it is not considered routine care. Instead, the RN should perform this task themselves or delegate it to an AP who has received additional training on feeding assistance.
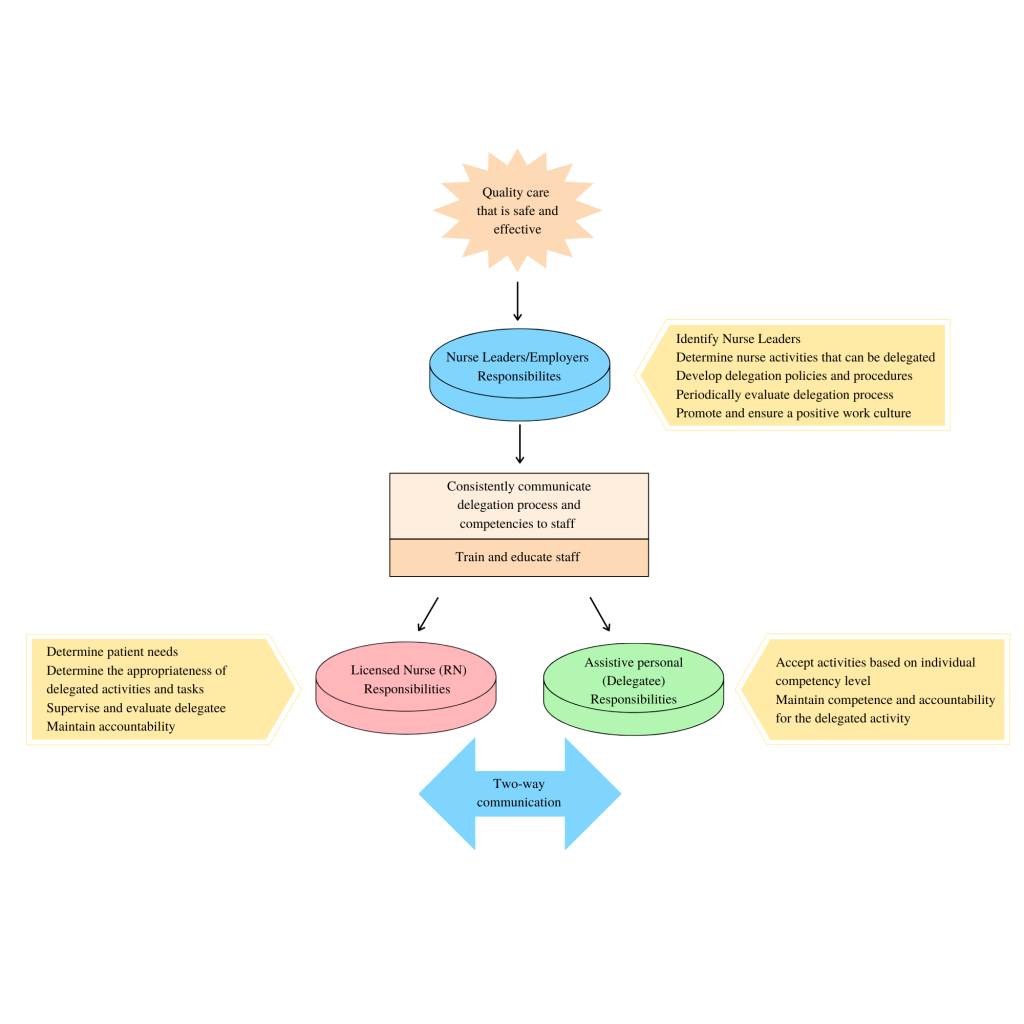
The delegation process is multifaceted. See Figure 3.2[8] for an illustration of the intersecting responsibilities of the employer/nurse leader, licensed nurse, and delegatee with two-way communication that protects the safety of the public. “Delegation begins at the administrative/nurse leader level of the organization and includes determining nursing responsibilities that can be delegated, to whom, and under what circumstances; developing delegation policies and procedures; periodically evaluating delegation processes; and promoting a positive culture/work environment. The licensed nurse is responsible for determining client needs and when to delegate, ensuring availability to the delegatee, evaluating outcomes, and maintaining accountability for delegated responsibility. Finally, the delegatee must accept activities based on their competency level, maintain competence for delegated responsibility, and maintain accountability for delegated activity.”[9]
Five Rights of Delegation
How does the RN determine what tasks can be delegated, when, and to whom? According to the National Council of State Boards of Nursing (NCSBN), RNs should use the five rights of delegation to ensure proper and appropriate delegation: right task, right circumstance, right person, right directions and communication, and right supervision and evaluation[10]:
- Right task: The activity falls within the delegatee’s job description or is included as part of the established policies and procedures of the nursing practice setting. The facility needs to ensure the policies and procedures describe the expectations and limits of the activity and provide any necessary competency training.
- Right circumstance: The health condition of the client must be stable. If the client’s condition changes, the delegatee must communicate this to the licensed nurse, and the licensed nurse must reassess the situation and the appropriateness of the delegation.[11]
- Right person: The licensed nurse, along with the employer and the delegatee, is responsible for ensuring that the delegatee possesses the appropriate skills and knowledge to perform the activity.[12]
- Right directions and communication: Each delegation situation should be specific to the client, the nurse, and the delegatee. The licensed nurse is expected to communicate specific instructions for the delegated activity to the delegatee; the delegatee, as part of two-way communication, should ask any clarifying questions. This communication includes any data that need to be collected, the method for collecting the data, the time frame for reporting the results to the licensed nurse, and additional information pertinent to the situation. The delegatee must understand the terms of the delegation and must agree to accept the delegated activity. The licensed nurse should ensure the delegatee understands they cannot make any decisions or modifications in carrying out the activity without first consulting the licensed nurse.[13]
- Right supervision and evaluation: The licensed nurse is responsible for monitoring the delegated activity, following up with the delegatee at the completion of the activity, and evaluating client outcomes. The delegatee is responsible for communicating client information to the licensed nurse during the delegation situation. The licensed nurse should be ready and available to intervene as necessary. The licensed nurse should ensure appropriate documentation of the activity is completed.[14]
Simply stated, the licensed nurse determines the right person is assigned the right tasks for the right clients under the right circumstances. When determining what aspects of care can be delegated, the licensed nurse uses clinical judgment while considering the client’s current clinical condition, as well as the abilities of the health care team member. The RN must also consider if the circumstances are appropriate for delegation. For example, although obtaining routine vital signs on stable clients may be appropriate to delegate to assistive personnel, obtaining vital signs on an unstable client is not appropriate to delegate.
After the decision has been made to delegate, the nurse assigning the tasks must communicate appropriately with the delegatee and provide the right directions and supervision. Communication is key to successful delegation. Clear, concise, and closed-loop communication is essential to ensure successful completion of the delegated task in a safe manner. During the final step of delegation, also referred to as supervision, the nurse verifies and evaluates that the task was performed correctly, appropriately, safely, and competently. Read more about supervision in the following section on “Supervision.” See Table 3.4 for additional questions to consider for each “right” of delegation.
Table 3.4. Rights of Delegation[15]
| Rights of Delegation | Description | Questions to Consider When Delegating |
|---|---|---|
| Right Task | A task that can be transferred to a member of the nursing team for a specific client. |
|
| Right Circumstances | The client is stable. |
|
| Right Person | The person delegating the task has the appropriate scope of practice to do so. The task is also appropriate for this delegatee’s skills and knowledge. |
|
| Right Directions and Communication | The task or activity is clearly defined and described. |
|
| Right Supervision and Evaluation | The RN appropriately monitors the delegated activity, evaluates client outcomes, and follows up with the delegatee at the completion of the activity. |
|
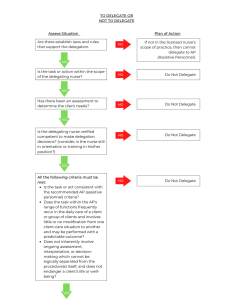
Keep in mind that any nursing intervention that requires specific nursing knowledge, clinical judgment, or use of the nursing process can only be delegated to another RN. Examples of these types of tasks include initial preoperative or admission assessments, client teaching, and creation and evaluation of a nursing care plan. See Figure 3.3[16] for an algorithm based on the 2019 National Guidelines for Nursing Delegation that can be used when deciding if a nursing task can be delegated.[17]
Responsibilities of the Licensed Nurse
The licensed nurse has several responsibilities as part of the delegation process. According to the NGND, any decision to delegate a nursing responsibility must be based on the needs of the client or population, the stability and predictability of the client’s condition, the documented training and competence of the delegatee, and the ability of the licensed nurse to supervise the delegated responsibility and its outcome with consideration to the available staff mix and client acuity. Additionally, the licensed nurse must consider the state Nurse Practice Act regarding delegation and the employer’s policies and procedures prior to making a final decision to delegate. Licensed nurses must be aware that delegation is at the nurse’s discretion, with consideration of the particular situation. The licensed nurse maintains accountability for the client, while the delegatee is responsible for the delegated activity, skill, or procedure. If, under the circumstances, a nurse does not feel it is appropriate to delegate a certain responsibility to a delegatee, the delegating nurse should perform the activity.[18]
1. The licensed nurse must determine when and what to delegate based on the practice setting, the client’s needs and condition, the state’s/jurisdiction’s provisions for delegation, and the employer’s policies and procedures regarding delegating a specific responsibility. The licensed nurse must determine the needs of the client and whether those needs are matched by the knowledge, skills, and abilities of the delegatee and can be performed safely by the delegatee. The licensed nurse cannot delegate any activity that requires clinical reasoning, nursing judgment, or critical decision-making. The licensed nurse must ultimately make the final decision whether an activity is appropriate to delegate to the delegatee based on the “Five Rights of Delegation.”
- Rationale: The licensed nurse, who is present at the point of care, is in the best position to assess the needs of the client and what can or cannot be delegated in specific situations.[19]
2. The licensed nurse must communicate with the delegatee who will be assisting in providing client care. This should include reviewing the delegatee’s assignment and discussing delegated responsibilities, including information on the client’s condition/stability, any specific information pertaining to a certain client (e.g., no blood draws in the right arm), and any specific information about the client’s condition that should be communicated back to the licensed nurse by the delegatee.
- Rationale: Communication must be a two-way process involving both the licensed nurse delegating the activity and the delegatee being delegated the responsibility. Evidence shows that the better the communication between the nurse and the delegatee, the more optimal the outcome. The licensed nurse must provide information about the client and care requirements. This includes any specific issues related to any delegated responsibilities. These instructions should include any unique client requirements. The licensed nurse must instruct the delegatee to regularly communicate the status of the client.[20]
3. The licensed nurse must be available to the delegatee for guidance and questions, including assisting with the delegated responsibility, if necessary, or performing it themselves if the client’s condition or other circumstances warrant doing so.
- Rationale: Delegation calls for nursing judgment throughout the process. The final decision to delegate rests in the hands of the licensed nurse as they have overall accountability for the client.[21]
4. The licensed nurse must follow up with the delegatee and the client after the delegated responsibility has been completed.
- Rationale: The licensed nurse who delegates the “responsibility” maintains overall accountability for the client, while the delegatee is responsible for the delegated activity, skill, or procedure.[22]
5. The licensed nurse must provide feedback information about the delegation process and any issues regarding delegatee competence level to the nurse leader. Licensed nurses in the facility need to communicate to the nurse leader responsible for delegation any issues arising related to delegation and any individual whom they identify as not being competent in a specific responsibility or unable to use good judgment and decision-making.
- Rationale: This will allow the nurse leader responsible for delegation to develop a plan to address the situation.[23]
The decision of whether or not to delegate or assign is based on the RN’s judgment concerning the condition of the client, the competence of the nursing team member, and the degree of supervision that will be required of the RN if a task is delegated.[24]
Responsibilities of the Delegatee
Everyone is responsible for the well-being of clients. While the nurse is ultimately accountable for the overall care provided to a client, the delegatee shares the responsibility for the client and is fully responsible for the delegated activity, skill, or procedure.[25] The delegatee has the following responsibilities:
1. The delegatee must accept only the delegated responsibilities that they are appropriately trained and educated to perform and feel comfortable doing given the specific circumstances in the health care setting and client’s condition. The delegatee should confirm acceptance of the responsibility to carry out the delegated activity. If the delegatee does not believe they have the appropriate competency to complete the delegated responsibility, then the delegatee should not accept the delegated responsibility. This includes informing the nursing leadership if they do not feel they have received adequate training to perform the delegated responsibility, do not perform the procedure frequently enough to do it safely, or their knowledge and skills need updating.
- Rationale: The delegatee shares the responsibility to keep clients safe, and this includes only performing activities, skills, or procedures in which they are competent and comfortable doing.[26]
2. The delegatee must maintain competency for the delegated responsibility.
- Rationale: Competency is an ongoing process. Even if properly taught, the delegatee may become less competent if they do not frequently perform the procedure. Given that the delegatee shares the responsibility for the client, the delegatee also has a responsibility to maintain competency.[27]
3. The delegatee must communicate with the licensed nurse in charge of the client. This includes any questions related to the delegated responsibility and follow-up on any unusual incidents that may have occurred while the delegatee was performing the delegated responsibility, any concerns about a client’s condition, and any other information important to the client’s care.
- Rationale: The delegatee is a partner in providing client care. They are interacting with the client/family and caring for the client. This information and two-way communication are important for successful delegation and optimal outcomes for the client.[28]
4. Once the delegatee verifies acceptance of the delegated responsibility, the delegatee is accountable for carrying out the delegated responsibility correctly and completing timely and accurate documentation per facility policy.
- Rationale: The delegatee cannot delegate to another individual. If the delegatee is unable to complete the responsibility or feels as though they need assistance, the delegatee should inform the licensed nurse immediately so the licensed nurse can assess the situation and provide support. Only the licensed nurse can determine if it is appropriate to delegate the activity to another individual. If at any time the licensed nurse determines they need to perform the delegated responsibility, the delegatee must relinquish responsibility upon request of the licensed nurse.[29]
Responsibilities of the Employer/Nurse Leader
The employer and nurse leaders also have responsibilities related to safe delegation of client care:
1. The employer must identify a nurse leader responsible for oversight of delegated responsibilities for the facility. If there is only one licensed nurse within the practice setting, that licensed nurse must be responsible for oversight of delegated responsibilities for the facility.
- Rationale: The nurse leader has the ability to assess the needs of the facility, understand the type of knowledge and skill needed to perform a specific nursing responsibility, and be accountable for maintaining a safe environment for clients. They are also aware of the knowledge, skill level, and limitations of the licensed nurses and AP. Additionally, the nurse leader is positioned to develop appropriate staffing models that take into consideration the need for delegation. Therefore, the decision to delegate begins with a thorough assessment by a nurse leader designated by the institution to oversee the process.[30]
2. The designated nurse leader responsible for delegation, ideally with a committee (consisting of other nurse leaders) formed for the purposes of addressing delegation, must determine which nursing responsibilities may be delegated, to whom, and under what circumstances. The nurse leader must be aware of the state Nurse Practice Act and the laws/rules and regulations that affect the delegation process and ensure all institutional policies are in accordance with the law.
- Rationale: A systematic approach to the delegation process fosters communication and consistency of the process throughout the facility.[31]
3. Policies and procedures for delegation must be developed. The employer/nurse leader must outline specific responsibilities that can be delegated and to whom these responsibilities can be delegated. The policies and procedures should also indicate what may not be delegated. The employer must periodically review the policies and procedures for delegation to ensure they remain consistent with current nursing practice trends and that they are consistent with the state Nurse Practice Act. (Institution/employer policies can be more restrictive, but not less restrictive.)
- Rationale: Policies and procedures standardize the appropriate method of care and ensure safe practices. Having a policy and procedure specific to delegation and delegated responsibilities eliminates questions from licensed nurses and AP about what can be delegated and how they should be performed.[32]
4. The employer/nurse leader must communicate information about delegation to the licensed nurses and AP and educate them about what responsibilities can be delegated. This information should include the competencies of delegatees who can safely perform a specific nursing responsibility.
- Rationale: Licensed nurses must be aware of the competence level of staff and expectations for delegation (as described within the policies and procedures) to make informed decisions on whether or not delegation is appropriate for the given situahttps://www.nursingworld.org/content-hub/resources/nursing-leadership/delegation-in-nursing/tion. Licensed nurses maintain accountability for the client. However, the delegatee has responsibility for the delegated activity, skill, or procedure.
In summary, delegation is the transfer of the nurse’s responsibility for a task while retaining professional accountability for the client’s overall outcome. The decision to delegate is based on the nurse’s judgment, the act of delegation must be clearly defined by the nurse, and the outcomes of delegation are an extension of the nurse’s guidance and supervision. Delegation, when rooted in mutual respect and trust, is a key component to an effective health care team.
Delegation is an integral skill in the nursing profession to help manage the complexities of the dynamic and ever-changing health care environment. Delegation in nursing has been found to increase employee empowerment, decrease burnout, increase role commitment, and improve job satisfaction.[33] Cultivating delegation skills helps nurses better manage the complexities of their client care role, ensuring that their clients are safely cared for and outcomes are optimized. Delegation skills, like other nursing skills, require purposeful development and do not necessarily come easily when first transitioning into the nursing role. It is important that the new graduate nurse does not mistake delegation for pompous or arrogant behavior. Delegation requires mutual respect between the delegator and delegatee. Delegation is not seen as a sign or weakness and does not reflect one’s desire to shirk their work responsibilities. Instead, delegation reflects strong leadership and organizational skills in which the nurse leader demonstrates that they understand how to leverage their team’s strengths in order to achieve optimal care outcomes.
To help avoid any perception of arrogance in the delegation of an activity, it is important that the new graduate nurse approaches the task of delegation with humility. Clarity in the communication of the delegated responsibility is critical, and the rationale behind the delegation should be communicated to the delegatee. Within the task of delegation, the delegator should express appreciation for the delegatee and their contributions in the collaborative health care environment. Additionally, it is important to understand that no specific nurse delegated task is outside of the “nurse” role. For example, ambulating a client does not to an unlicensed assistive personnel simply because that individual is able to perform that task. Rather, nurses must be willing to perform delegated tasks themselves when necessary. This reflects a team-oriented mindset and helps to reinforce among the care team that all roles are critical to optimizing client care. For new graduate nurses who first transition into a specific health care setting, having the opportunity to shadow individuals in various work roles helps to foster a team mindset. Asking questions of various team members regarding their work role can help a new graduate nurse demonstrate respect and value for other roles.
Examples of helpful questions may include the following:
- “What is the biggest challenge in your typical workday?”
- “What do you most enjoy about your job?”
- “How is it best to communicate with you when the unit is busy?”
- “What do you think people misunderstand most about your role?”
It is important to ensure that the team understands that care is optimized when they function as one collective unit and not in siloed roles. Each team member must feel valued and competent in their role. By understanding and practicing strategic delegation, new graduate nurses can overcome any misconceptions of arrogance and contribute positively to the healthcare team.
Please review the example below to consider variation in approach to task delegation.
Scenario A: Nurse June, a newly graduated nurse, is working in a busy hospital unit. She needs an unlicensed assistive personnel (UAP), Alex, to take vital signs of a patient. Nurse June approaches Alex in the hallway and says in an abrupt tone, “Alex, I need you to take Mr. Smith’s vital signs right now. I’m too busy to do it myself, and besides, that’s what you’re here for. Just get it done quickly.”
Analysis: June’s tone and words suggest she sees Alex’s role as less important and purely as a means to offload her tasks. June does not explain the urgency or importance of the task. June doesn’t acknowledge Alex’s effort or capability, making the request seem like a command rather than a collaborative effort.
Scenario B: Nurse June, a newly graduated nurse, is working in a busy hospital unit. She needs an unlicensed assistive personnel (UAP), Alex, to take vital signs of a patient. Nurse June approaches Alex and says, “Hi Alex, could you please help me by taking Mr. Smith’s vital signs? I’m handling a few urgent matters right now, and it would really help to have your support. I know you’re great at this, and your thoroughness really makes a difference in our patient care. Thank you so much!”
Analysis: June speaks to Alex with courtesy and acknowledges the value of his role. June clearly explains why she needs Alex’s help and the importance of the task. June acknowledges Alex’s competence and expresses gratitude, fostering feelings of value and respect.
Media Attributions
- Delegation
- Delegation-Decision-Tree-2a
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- “Delegation.png” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- NCSBN. (n.d.). Delegation. https://www.ncsbn.org/1625.htm ↵
- “Delegation Decision Tree.png” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation. https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- ANA. (2023, September 7). Delegation in nursing: How to build a stronger team. Retrieved from https://www.nursingworld.org/content-hub/resources/nursing-leadership/delegation-in-nursing/ ↵
Advocacy: The act or process of pleading for, supporting, or recommending a cause of course of action for individuals, groups, organizations, communities, society, or policy issues.
Collective bargaining: Negotiation of wages and other conditions of employment by an organized body of employees.
Evidence-based practice: Integrating scientific evidence with clinical expertise and patient/family preferences and values for delivery of optimal health care.[1]
Grievance process: A process for resolving disagreements between employees and management.
Informatics: Using information and technology to communicate, manage knowledge, mitigate error, and support decision-making.[2]
ISBARR: A mnemonic for the components to include when communicating with another health care team member: Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat back.
Magnet® Recognition Program: An organizational credential that recognizes quality patient outcomes, nursing excellence, and innovations in professional nursing practice.
Patient-centered care: The patient is the source of control and full partner in providing compassionate and coordinated care based on respect for patient’s preferences, values, and needs.[3]
Quality improvement: Using data to monitor the outcomes of care processes and using improvement methods to design and test changes to continuously improve the quality and safety of health care systems.[4]
Shared governance: A shared leadership model between management and employees working together to achieve common goals.
Social Determinants of Health (SDOH): The conditions in the environments where people live, learn, work, and play that affect a wide range of health, functioning, and quality of life outcomes and risks.
TeamSTEPPS® (Team Strategies and Tools to Enhance Performance and Patient Safety): An evidence-based framework to improve client safety through effective communication in health care environments consisting of four core competencies: communication, leadership, situation monitoring, and mutual support.
Teamwork and collaboration: Functioning effectively within nursing and interprofessional teams, fostering open communication, mutual respect, and shared decision-making to achieve quality patient care.[5]
Whistleblower: A person who exposes any kind of information or activity that is deemed illegal, unethical, or not correct within an organization.
Learning Objectives
- Develop a current professional resume or portfolio
- Identify steps for preparing for the NCLEX-RN examination
- Identify actions for obtaining nursing credentials
- Identify strategies for successful nursing interviews
- Identify goals for lifelong learning and professional development
Preparing to enter the workforce as a registered nurse (RN) can be a challenging but exciting time. Being aware of available resources to help navigate this process will decrease stress and make the process more manageable. This chapter will discuss how to prepare for the NCLEX-RN examination, obtain a nursing license, create a resume and portfolio, effectively participate in an interview, transition into the RN role, and become a lifelong learner.

