2. Communication
Open Resources for Nursing (Open RN) and Amy Ertwine
Effective communication is a vital component of proper assignment, delegation, and supervision. It is also one of the Standards of Professional Performance established by the American Nurses Association (ANA).[1] Research has identified that new graduate nurses are more susceptible to stress and isolation within their job roles due to poor communication and teamwork within the interdisciplinary team.[2] Strong communication skills foster a supportive work environment and colleagial relationships that benefit both patients and nursing staff.
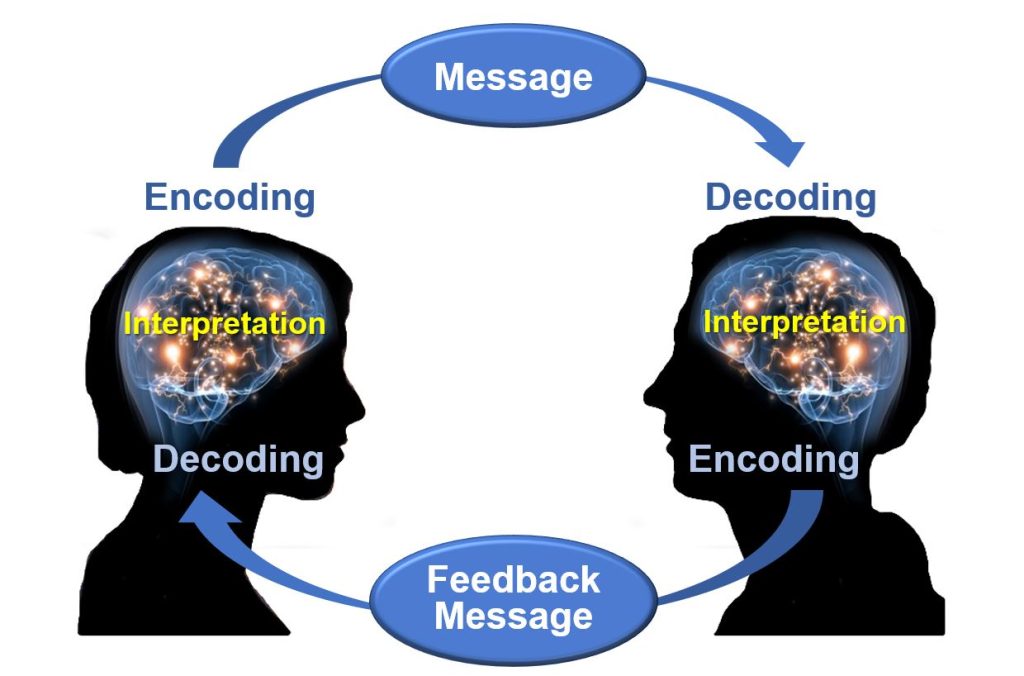
Consider the fundamentals of good communication practices. Effective communication requires each interaction to include a sender of the message, a clear and concise message, and a receiver who can decode and interpret that message. The receiver also provides a feedback message back to the sender in response to the received message. See Figure 3.1[3] for an image of effective communication between a sender and receiver. This feedback message is referred to as closed-loop communication in health care settings. Closed-loop communication enables the person giving the instructions to hear what they said reflected back and to confirm that their message was received correctly. It also allows the person receiving the instructions to verify and confirm the actions to be taken. If closed-loop communication is not used, the receiver may nod or say “OK,” and the sender may assume the message has been effectively transmitted, but this may not be the case and can lead to errors and client harm.
An example of closed-loop communication can be found in the following exchange:
- RN: “Jane, can you get a set of vitals on Mr. Smith and let me know if the results are outside of normal range?”
- Jane, CNA: “OK, I’ll get a set of vitals on Mr. Smith and let you know if they are out of range.”
Closed-loop communication is vital for communication among health care team members to avoid misunderstandings that can cause unsafe client care. According to the HIPAA Journal, poor communication leads to a “reduction in the quality of care, poor client outcomes, wastage of resources, and high health care costs.”[4] Parameters for reporting results and the results that should be expected are often left unsaid rather than spelled out in sufficient detail. It is imperative for the RN to provide clear, complete, concise instructions when delegating. A lack of clarity can lead to misunderstanding, unfinished tasks, incomplete care, and/or medical errors.[5]
Effective communication is at the core of proper assignment, delegation, and supervision. With effective communication at the beginning of every shift, each nursing team member should have a clear plan for their shift, what to do and why, and what and when to report to the RN or team leader. Communication should continue throughout the shift as tasks are accomplished and patients’ needs change. Effective communication improves client outcomes and satisfaction scores, as well as improving team morale by enhancing the collaborative relationships of the health care team.
The RN is accountable for clear, concise, correct, and complete communication when making assignments and delegating, both initially and throughout the shift. These communication characteristics can be remembered by using the mnemonic the “4 Cs”:
- Clear: Information is understood by the listener. Asking the listener to restate the instructions and the plan can be helpful to determine whether the communication is clear.
- Concise: Sufficient information should be provided to accurately perform the task, but excessive or irrelevant information should be avoided because it can confuse the listener and waste precious time.
- Correct: Correct communication is not vague or confusing. Accurate information is also aligned with agency policy and the team member’s scope of practice as defined by their state’s Nurse Practice Act and other state regulations.
- Complete: Complete instructions leave no room for doubt. Always ask if further information or clarification is needed, especially regarding tasks that are infrequently performed or include unique instructions.[6]
The use of closed-loop communication is the best method to achieve clear, concise, correct, and complete information exchanged among team members. Closed-loop communication allows team members the opportunity to verify and validate the exchange of information. By repeating back information, members confirm the exchange has occurred, understanding is clear, and expectations are heard.
Closed-loop communication should also be used when the RN is receiving a verbal order from a provider. For example, when the resuscitation team leader gives a verbal order of “Epinephrine 1 mg/mL IV push now,” the RN confirms correct understanding of the order by repeating back, “I will prepare Epinephrine 1 mg/mL to be given IV push now.” After the provider confirms the verbal order and the task is completed, the nurse confirms completion of the task by stating, “Epinephrine 1 mg/mL IV push was administered.”
In addition to using closed-loop communication, a common format used by health care team members to exchange client information is ISBARR, a mnemonic for the components of Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat Back. ISBARR and other communication strategies are discussed in more detail in the “Interprofessional Communication” section of the “Collaboration Within the Interprofessional Team” chapter.
Media Attributions
- Osgood-Schramm-model-of-communication
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- Leonard, J.C., Whiteman, K., Stephens, K., Henry, C., Swanson-Bieaman, B. (2022). Imporving communication and collaboration skills in graduate nurses: An evidence-based approach. The Online Journal of Issues in Nursing, 27(2), 3. https://www.doi.org/10.3912/OJIN.Vol27No02Man03 ↵
- “Osgood-Schramm-model-of-communication.jpg” by Jordan Smith at eCampus Ontario is licensed under CC BY 4.0. Access for free at https://ecampusontario.pressbooks.pub/communicationatwork/chapter/1-3-the-communication-process/ ↵
- HIPAA Journal. (n.d.). Effects of poor communication in healthcare. https://www.hipaajournal.com/effects-of-poor-communication-in-healthcare/ ↵
- HIPAA Journal. (n.d.). Effects of poor communication in healthcare. https://www.hipaajournal.com/effects-of-poor-communication-in-healthcare/ ↵
- LaCharity, L. A., Kumagai, C. K., & Bartz, B. (2019). Prioritization, delegation and assignment (4th ed.). Mosby, p. 6. ↵
As discussed previously, the American Nurses Association (ANA) defines advocacy at the individual level as educating health care consumers so they can consider actions, interventions, or choices related to their own personal beliefs, attitudes, and knowledge to achieve the desired outcome. In this way, the health care consumer learns self-management and decision-making.[1] Advocacy at the interpersonal level is defined as empowering health care consumers by providing emotional support, assistance in obtaining resources, and necessary help through interactions with families and significant others in their social support network.[2]
What does advocacy look like in a nurse’s daily practice? The following are some examples provided by an oncology nurse[3]:
- Ensure Safety. Ensure the client is safe when being treated in a health care facility and when they are discharged by communicating with case managers or social workers about the client’s need for home health or assistance after discharge so it is arranged before they go home.
- Give Clients a Voice. Give clients a voice when they are vulnerable by staying in the room with them while the doctor explains their diagnosis and treatment options to help them ask questions, get answers, and translate information from medical jargon.
- Educate. Educate clients on how to manage their current or chronic conditions to improve the quality of their everyday life. For example, clients undergoing chemotherapy can benefit from the nurse teaching them how to take their anti-nausea medication in a way that will be most effective for them and will allow them to feel better between treatments.
- Protect Patient Rights. Know clients’ wishes for their care. Advocacy may include therapeutically communicating a client’s wishes to an upset family member who disagrees with their choices. In this manner, the client’s rights are protected and a healing environment is established.
- Double-Check for Errors. Know that everyone makes mistakes. Nurses often identify, stop, and fix errors made by interprofessional team members. They flag conflicting orders from multiple providers and notice oversights. Nurses should read provider orders and carefully compare new orders to previous documentation. If an order is unclear or raises concerns, a nurse should discuss their concerns with another nurse, a charge nurse, a pharmacist, or the provider before implementing it to ensure patient safety.
- Connect Clients to Resources. Help clients find resources inside and outside the hospital to support their well-being. Know resources in your agency, such as case managers or social workers who can assist with financial concerns, advance directives, health insurance, or transportation concerns. Request assistance from agency chaplains to support spiritual concerns. Promote community resources, such as patient or caregiver support networks, Meals on Wheels, or other resources to meet their needs.
Nurses must recognize their unique position in client advocacy to empower individuals to provide them with the support and resources to make their best judgment. The intimate and continuous nature of the nurse-patient relationship places nurses in a prime position to identify and address the needs and concerns of their patients. This relationship is built on trust, empathy, and consistent interaction, which allows nurses to gain a deep understanding of their patients' values, preferences, and personal circumstances. By leveraging this close proximity and strong rapport, nurses can effectively advocate for their patients, ensuring that their voices are heard, and their wishes are respected in all aspects of care.[4]
The power of the nurse-patient relationship extends beyond the immediate clinical environment. Nurses often act as liaisons between patients and the broader health care team, facilitating communication and ensuring that patient preferences are integrated into care plans. This advocacy role is crucial in navigating complex health care systems where patients may feel overwhelmed or marginalized. Nurses can help demystify medical jargon, explain treatment options, and support patients in making informed decisions that align with their values and goals. Through education and emotional support, nurses empower patients to take an active role in their own care, enhancing patient autonomy and satisfaction.[5]
In addition to direct patient care, nurses play a pivotal role in identifying systemic issues that affect patient outcomes. Their frontline perspective provides valuable insights into the barriers patients face in accessing quality care, such as socioeconomic challenges, cultural barriers, and institutional policies. By advocating for policy changes and improvements in health care delivery, nurses contribute to creating a more equitable and patient-centered health care system. Their advocacy efforts can lead to the implementation of practices and policies that better address the needs of diverse patient populations, ultimately improving health outcomes on a broader scale.[6]
Nurses' advocacy is also essential in situations where patients are unable to speak for themselves, such as in cases of severe illness, disability, or end-of-life care. In these instances, nurses must be vigilant in recognizing and addressing the needs of vulnerable patients, ensuring that their rights and dignity are upheld. This may involve working closely with families and caregivers, coordinating with interdisciplinary teams, and navigating ethical dilemmas to provide the best possible care for the patient.

