Wound Therapy
Open Resources for Nursing (Open RN)
Wound therapy is often prescribed by a multidisciplinary team that can include the provider, a wound care nurse, a dietician, and the bedside nurse who performs dressing changes. Topical dressings should be selected that create an environment conducive to healing the specific type of wound and its causes. It is important to perform the following actions when providing wound care:
- Prevent and manage infection
- Cleanse the wound
- Debride the wound
- Maintain appropriate moisture in the wound
- Control odor
- Manage wound pain
- Consider the big picture[1]
Each of these objectives is further discussed in the following subsections.
Prevent and Manage Infection
One of the primary goals of wound dressings is to protect the wound base from bacteria and contaminants (i.e., urine and feces). If new signs of infection are present during a wound dressing change, wound swabs should be taken according to agency policy and the need for a wound culture and possible antibiotic therapy discussed with the primary provider.[2]
Silver sulfadiazine is an example of a common topical antibiotic prescribed for wounds. Topical antibiotics are covered with a secondary dressing.[3]
Cleanse the Wound
Routine cleansing should be performed at each dressing change with products that are physiologically compatible with wound tissue. Normal saline is the most gentle solution and is typically delivered using a syringe or commercial cleansers. See Figure 20.20[4] for an image of wound irrigation with a syringe. Commercial cleansers may be used, but hydrogen peroxide, betadine, and acetic acid should be avoided because these agents can be cytotoxic.[5]

Debride the Wound
Debridement is the removal of nonviable tissue in a wound. If necrotic (black) tissue is present in the wound bed, it must be removed in most circumstances for the wound to heal. However, one exception is stable, dry eschar on a patient’s heel that should be left in place until the patient’s vascular status is determined.[6]
Wound debridement can be accomplished using several methods, such as autolytic, enzymatic, or sharp wound debridement. Autolytic debridement occurs when moist topical dressings foster the breakdown of necrotic tissue. Enzymatic debridement occurs when prescribed topical agents are directly applied to the wound bed.[7] Collagenase ointment is an example of a topical enzymatic debridement ointment that is applied daily (or more frequently if the dressing becomes soiled) and covered with sterile gauze or a foam dressing.[8] Sharp wound debridement is performed by a trained health care provider and may be at the bedside or in the operating room. Sharp debridement is an invasive procedure using a scalpel or scissors to remove necrotic tissue so that only viable tissue remains. See Figure 20.21[9] for an image of a wound that has been surgically debrided of necrotic tissue.

Maintain Appropriate Moisture in the Wound
Wound dressings should maintain a moist wound environment to facilitate the development of granulation tissue. However, excessive exudate must be managed with dressings that absorb excess moisture to avoid maceration of the surrounding tissue.[10] For example, dressings such as alginate or hydrofiber are used in wounds with large amounts of exudate to maintain an appropriate moisture level but also prevent maceration of tissue. Frequent dressing changes may also be required in wounds with heavy drainage.
Eliminate Dead Space
Deep wounds and tunneling should be packed with dressings to keep the wound bed moist. Sterile gauze dressings moistened with normal saline or hydrogel-impregnated dressings are examples of packing agents used to keep the wound bed moist. Packing material should be easy to remove from the wound base during each dressing change to avoid injuring the fragile granulation tissue. Keep in mind that dressings made of alginate have a slight greenish tint when removed and should not be confused with purulent drainage.
Control Odor
If odor is present in a wound, the nurse should consult with the health care provider about the frequency of dressing changes, wound cleansing agents, and the possible need for topical antimicrobial therapy or debridement. Room deodorants can be obtained for use after dressing changes.[11]
Manage Wound Pain
Wounds that are becoming increasingly painful should be assessed for potential infection or dehiscence. The nurse should plan on administering medication to the patient before performing dressing changes on wounds that are painful. If pain medication is not ordered, then the nurse should contact the health care provider for a prescription before performing the dressing change.[12]
Protect Periwound Skin
Heavily draining wounds or the improper use of moist dressings can cause maceration of the periwound skin. The nurse should apply dressings carefully to maintain wound bed moisture yet also protect the periwound skin. Skin barrier creams, skin protective wipes, or skin barrier wafers can also be used to protect the periwound skin.[13]
Consider the Big Picture
Most wounds do not occur in isolation but also have other systemic or local factors that impact wound healing. Be sure to consider the following points when caring for patients with wounds with delayed wound healing:
- Minimize pressure and shear for patients with pressure injuries. For example, a patient with a pressure injury should be repositioned at least every two hours to minimize pressure.
- Educate patients with neuropathy and decreased sensation about preventing further injury. For example, a patient with diabetes should wear well-fitting shoes and never go barefoot to prevent injuries.
- Control edema in patients with venous ulcers through the use of compression dressings.
- Promote adequate perfusion to patients with arterial ulcers. For example, in most cases, the extremity of a patient with an arterial ulcer should not be elevated.
- Protect fragile skin in patients with skin tears to prevent further injury.
- Manage blood sugar levels in patients with diabetes mellitus for optimal healing.
- Promote good nutrition and hydration for all patients with wounds. Consult a registered dietician to assess the patient’s nutritional status and develop a nutrition plan if needed.[14]
- Document ongoing assessment findings and wound interventions for good communication and continuity of care across the multidisciplinary health care team.
- Concerns about the healing of a chronic wound or the dressings ordered should be communicated to the health care provider. Referral to a specialized wound care nurse is often helpful.
Media Attributions
- DSC_1732
- Open_wound_after_debridement_of_NF
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- “DSC_1732-150x150.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/4-5-complex-dressing-change/ ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- National Institutes of Health. (2019, May 17). DailyMed - Collagenase santyl ointment. U.S. National Library of Medicine. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=6b6fbfc6-98fa-46aa-88ef-ab00fbb08ffd ↵
- “Open wound after debridement of NF.jpg” by Morphx1982 is licensed under CC BY-SA 4.0 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
[latexpage]
In the previous section, we calculated medication doses that were provided in a liquid form in a given concentration. Medications are also commonly supplied in dry form, such as powders or crystals, that must be reconstituted with fluid before they are administered parenterally by injection. Reconstitution is the process of adding a liquid diluent to a dry ingredient to make a specific concentration of liquid. See Figure 5.9[1] for an example of a vial of medication that requires reconstitution. When reconstituting medications, it is important to follow the reconstitution instructions carefully so the medication is prepared in the correct concentration. When calculating the dosage of reconstituted medication to administer to the patient, the amount of fluid used to dilute the medication must also be considered. Let’s practice using dimensional analysis to determine how much of a reconstituted medication should be administered.

Practice Problem: Reconstituted Medication
Patient Information:
Name: Liam Vang, DOB: 04/04/20xx, Age 8, Allergies: NKDA, Weight: 60 kg
Provider Order: Cefazolin 500 mg IM every 8 hours
Medication Supplied: See Figure 5.10[2] for the drug label of the medication as it is supplied.
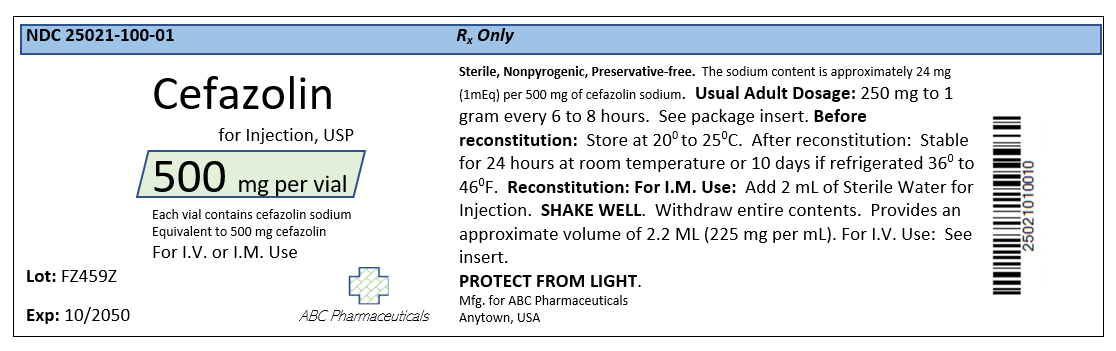
- Start by reading the order and the drug label. Liam has an order to receive 500 mg of Cefazolin. The vial of medication in powder form states there are 500 mg per vial. The powder must be reconstituted before it can be administered. The reconstitution instructions on the label state to add 2 mL of sterile water to the vial to reconstitute the powder into a liquid form for injection. The label states that after the powder is reconstituted with the 2 mL of diluent, the concentration of fluid will be 225 mg/mL. See a close-up image of reconstitution instructions in Figure 5.11.[3]
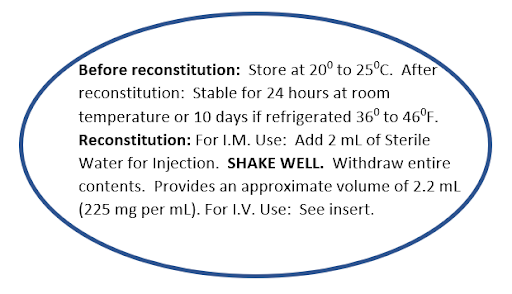
When setting up the problem, we need to identify the correct information to include in the equation. There are several numbers we may be tempted to try to incorporate into our equation, such as 500 mg per vial, 2 mL diluent, and approximate volume of 2.2 mL. These are numbers specific to the reconstitution process. However, keep in mind that our final goal is to calculate the number of mL of fluid to administer after the medication is reconstituted, so this will be the goal unit. The other piece of important information that the drug label states is that the reconstituted medication will provide a concentration of 225 mg/mL.
2. Start by identifying the goal unit for which you are solving, which is mL to administer as an injection:
\[
mL~=~?
\]
3. Set up the first fraction by matching the numerator to the goal unit of mL. In this problem, we know from the drug label that the known concentration of the reconstituted medication is 225 mg per mL, so add 1 mL to the numerator and 225 mg to the denominator:
\[
mL=\frac{1~mL}{225~mg}
\]
4. Set up the second fraction with mg in the numerator with the intent to cross off mg diagonally. Look at the given information to determine how it relates to mg. The order tells us to give Liam 500 mg of the medication. Place 500 in the numerator of the second fraction with one in the denominator so that mg will cross off diagonally:
\[
mL=\frac{1~mL}{225~mg}~~x~~\frac{500~mg}{1}
\]
5. Cross off units diagonally. Multiply across the numerators and the denominators, and then divide the final fraction for the answer in mL:
\[
mL=\frac{1~mL}{225~\cancel{mg}}~~x~~\frac{500~\cancel{mg}}{1}~~=~~\frac{500~mL}{225}~=~2.2222~mL
\]
6. Because the patient is a child, round to hundredth for the final answer: 2.22 mL
View supplementary YouTube videos for Using Dimensional Analysis to Calculate Reconstitution [4],[5]:

