5. Tenets of Prioritization
Open Resources for Nursing (Open RN) and Amy Ertwine
Prioritization
As new nurses begin their career, they look forward to caring for others, promoting health, and saving lives. However, when entering the health care environment, they often discover there are numerous and competing demands for their time and attention. Patient care is often interrupted by call lights, rounding physicians, and phone calls from the laboratory department or other interprofessional team members. Even individuals who are strategic and energized in their planning can feel frustrated as their task lists and planned patient-care activities build into a long collection of “to dos.”
Without utilization of appropriate prioritization strategies, nurses can experience time scarcity, a feeling of racing against a clock that is continually working against them. Functioning under the burden of time scarcity can cause feelings of frustration, inadequacy, and eventually burnout. Time scarcity can also impact patient safety, resulting in adverse events and increased mortality.[1] Additionally, missed or rushed nursing activities can negatively impact patient satisfaction scores that ultimately affect an institution’s reimbursement levels.
It is vital for nurses to plan patient care and implement their task lists while ensuring that critical interventions are safely implemented first. Identifying priority patient problems and implementing priority interventions are skills that require ongoing cultivation as one gains experience in the practice environment.[2] To develop these skills, students must develop an understanding of organizing frameworks and prioritization processes for delineating care needs. These frameworks provide structure and guidance for meeting the multiple and ever-changing demands in the complex health care environment.
Let’s consider a clinical scenario in the following box to better understand the implications of prioritization and outcomes.
Scenario A
Imagine you are beginning your shift on a busy medical-surgical unit. You receive a handoff report on four medical-surgical patients from the night shift nurse:
- Patient A is a 34-year-old total knee replacement patient, post-op Day 1, who had an uneventful night. It is anticipated that she will be discharged today and needs patient education for self-care at home.
- Patient B is a 67-year-old male admitted with weakness, confusion, and a suspected urinary tract infection. He has been restless and attempting to get out of bed throughout the night. He has a bed alarm in place.
- Patient C is a 49-year-old male, post-op Day 1 for a total hip replacement. He has been frequently using his patient-controlled analgesia (PCA) pump and last rated his pain as a “6.”
- Patient D is a 73-year-old male admitted for pneumonia. He has been hospitalized for three days and receiving intravenous (IV) antibiotics. His next dose is due in an hour. His oxygen requirements have decreased from 4 L/minute of oxygen by nasal cannula to 2 L/minute by nasal cannula.
Based on the handoff report you received, you ask the nursing assistant to check on Patient B while you do an initial assessment on Patient D. As you are assessing Patient D’s oxygenation status, you receive a phone call from the laboratory department relating a critical lab value on Patient C, indicating his hemoglobin is low. The provider calls and orders a STAT blood transfusion for Patient C. Patient A rings the call light and states she and her husband have questions about her discharge and are ready to go home. The nursing assistant finds you and reports that Patient B got out of bed and experienced a fall during the handoff reports.
It is common for nurses to manage multiple and ever-changing tasks and activities like this scenario, illustrating the importance of self-organization and priority setting. This chapter will further discuss the tools nurses can use for prioritization.
- Cho, S., Lee, J., You, S. J., Song, K. J., & Hong, K. J. (2020). Nurse staffing, nurses prioritization, missed care, quality of nursing care, and nurse outcomes. International Journal of Nursing Practice, 26(1), e12803. https://doi.org/10.1111/ijn.12803 ↵
- Jessee, M. A. (2019). Teaching prioritization: “Who, what, & why?” Journal of Nursing Education, 58(5), 302-305. https://doi.org/10.3928/01484834-20190422-10 ↵
Professional communication with other members of the health care team is an important component of every nurse’s job. See Figure 2.8[1] for an image illustrating communication between health care team members. Common types of professional interactions include reports to health care team members, handoff reports, and transfer reports. Reports may be verbal (e.g., reports given in person, by telephone, or recorded) or written (e.g., reports provided electronically or by fax).

Reports to Health Care Team Members
Nurses routinely report information to other nurses and health care team members, as well as urgently contact health care providers to report changes in client status.
Standardized methods of communication have been developed to allow information to be exchanged between health care team members in a structured, concise, and accurate manner to ensure safe client care. One common format used by health care team members to exchange client information is ISBARR, a mnemonic for the components of Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat back or a simpler version called SBAR:
-
- Introduction: Introduce your name, role, and the agency from which you are calling.
- Situation: Provide the client’s name and location, why you are calling, recent vital signs, and the status of the client.
- Background: Provide pertinent background information about the client such as admitting medical diagnoses, code status, recent relevant lab or diagnostic results, and allergies.
- Assessment: Share abnormal assessment findings and your evaluation of the current client situation.
- Request/Recommendations: State what you would like the provider to do, such as reassess the client, order a lab/diagnostic test, prescribe/change medication, etc.
- Repeat back: If you are receiving new orders from a provider, repeat them to confirm accuracy. Be sure to document communication with the provider in the client’s chart.
Read an example of an ISBARR report in the following box. Information is provided to a printable ISBARR reference card.
Sample ISBARR Report From a Nurse to a Health Care Provider
I: “Hello Dr. Smith, this is Jane White, RN from the Med Surg unit.”
S: “I am calling to tell you about Ms. White in Room 210, who is experiencing an increase in pain, as well as redness at her incision site. The client has no known allergies and is a full code. Her recent vital signs were BP 160/95, heart rate 90, respiratory rate 22, O2 sat 96%, and temperature 38 degrees Celsius. She is stable but her pain is worsening.”
B: “Ms. White is a 65-year-old female, admitted yesterday post hip surgical replacement. She has been rating her pain at 3 or 4 out of 10 since surgery with her scheduled medication, but now she is rating the pain as a 7, with no relief from her scheduled medication of Vicodin 5/325 mg administered an hour ago. She is scheduled for physical therapy later this morning and is stating she won’t be able to participate because of the pain this morning.”
A: “I just assessed the surgical site, and her dressing was clean, dry, and intact, but there is 4 cm redness surrounding the incision, and it is warm and tender to the touch. There is moderate serosanguinous drainage. Otherwise, her lungs are clear, and her heart rate is regular. I am concerned her incision site may be becoming infected and that she will have difficulty with therapy if her pain remains uncontrolled.”
R: “I am calling to request an order for a CBC and increased dose of pain medication.”
R: “I am repeating back the order to confirm that you are ordering a STAT CBC and an increase of her Vicodin to 10/325 mg.”
View or print an ISBARR reference card
Handoff Reports
Handoff reports are defined by The Joint Commission as “a transfer and acceptance of client care responsibility achieved through effective communication. It is a real-time process of passing client specific information from one caregiver to another, or from one team of caregivers to another, for the purpose of ensuring the continuity and safety of the client’s care.”[2] In 2017, The Joint Commission issued a critical alert about inadequate handoff communication that has resulted in client harm such as wrong-site surgeries, delays in treatment, falls, and medication errors. Strategies for improving handoff communication have been implemented at agencies across the country.
Although many types of nursing shift-to-shift handoff reports have been used over the years, evidence strongly supports that bedside handoff reports increase client safety, as well as client and nurse satisfaction, by effectively communicating current, accurate client information in real time.[3] See Figure 2.9[4] for an image illustrating two nurses participating in a handoff report. Bedside reports typically occur in hospitals and include the client, along with the off-going and the oncoming nurses in a face-to-face handoff report conducted at the client's bedside. HIPAA rules must be kept in mind if visitors are present, or the room is not a private room. Family members may be included with the client’s permission. See a sample checklist for a bedside handoff report from the Agency for Healthcare Research and Quality in Figure 2.10.[5] Although a bedside handoff report is similar to an ISBARR report, it contains additional information to ensure continuity of care across nursing shifts. For example, the “assessment” portion of the bedside handoff report includes detailed pertinent data the oncoming nurse needs to know, such as current head-to-toe assessment findings to establish a baseline; information about equipment such as IVs, catheters, and drainage tubes; and recent changes in medications, lab results, diagnostic tests, and treatments.
![]"618721604-huge" by Rido is used under license from Shutterstock.com. Image showing two nurses discussing a chart both are holding](https://opencontent.ccbcmd.edu/app/uploads/sites/30/2024/07/618721604-huge-scaled-1.jpg)
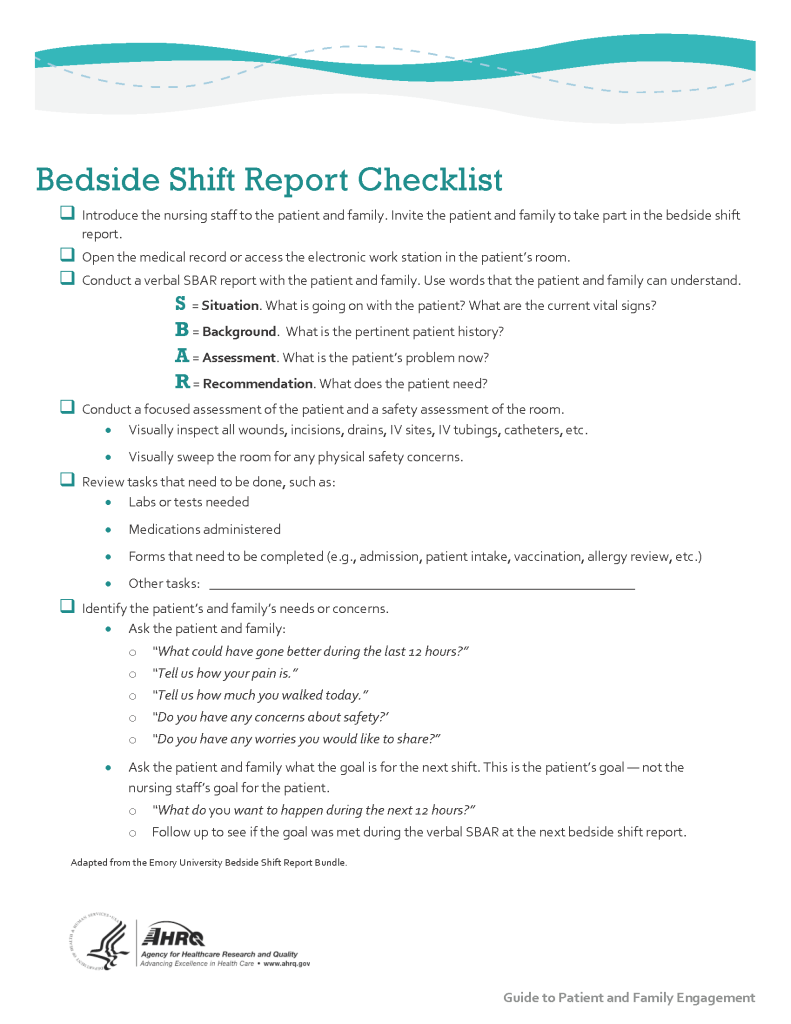
Print a copy of the AHRQ Bedside Shift Report Checklist.
View a video on creating shift reports.[6]
Transfer Reports
Transfer reports are provided by nurses when transferring a client to another unit or to another agency. Transfer reports contain similar information as bedside handoff reports but are even more detailed when the client is being transferred to another agency. Checklists are often provided by agencies to ensure accurate, complete information is shared.
Conflict in the Workplace
Nurses encounter conflict in their daily work environment, such as misunderstandings or disagreements among staff, clients, providers, family members, or other individuals. Nurses must learn communication methods that lessen conflict and enhance interactions that lead to a better work environment.
Read additional information about "Conflict Resolution" in Open RN Nursing Health Alterations.

