Blood Glucose Monitoring
Open Resources for Nursing (Open RN)
Blood glucose monitoring is performed on patients with diabetes mellitus and other conditions that cause elevated blood sugar levels. Diabetes mellitus is a common medical condition that affects the body’s ability to produce insulin in the pancreas and use insulin at the cellular level. There are two types of diabetes mellitus, type 1 and type 2. Type 1 diabetes mellitus is an autoimmune disease that damages the beta cells of the pancreas so they do not produce insulin; thus, synthetic insulin must be administered by injection or infusion. It typically begins in childhood or adolescence. Type 2 diabetes mellitus accounts for approximately 95 percent of all cases and is highly correlated with obesity and inactivity. During type 2 diabetes, the cells of the body become resistant to the effects of insulin, and the pancreas increases its production of insulin. However, over time, the pancreas may no longer be able to produce insulin. In many cases, type 2 diabetes can be managed by moderate weight loss, regular physical activity, and a healthy diet. However, if blood glucose levels cannot be controlled with healthy lifestyle choices, oral diabetic medication is prescribed and eventually, the administration of insulin may be required.[1] Prediabetes is a medical condition where blood sugar levels are higher than normal, but not high enough yet to be diagnosed as type 2 diabetes. Approximately one in three American adults have prediabetes. Gestational diabetes is a type of diabetes that occurs during pregnancy in women who did not have diabetes before they were pregnant.
Diabetic patients require frequent blood glucose monitoring to administer customized medication therapy to prevent long-term complications from occurring. Hospitalized patients who do not have diabetes may also require frequent blood glucose monitoring due to elevations that can occur as a result of the stress of hospitalization, surgical procedures, and side effects of medications. Additionally, patients receiving enteral feedings typically have their blood glucose monitored every six hours. Health care providers prescribe the frequency of blood glucose monitoring; testing is typically performed before meals and at bedtime. For some patients, a standardized sliding-scale insulin protocol may be prescribed with instructions on the medication administration record (MAR) for administration of insulin based on their blood glucose results.[2],[3] See Table 19.2 for an example of a sliding-scale insulin protocol.
Table 19.2 Sample Sliding-Scale Insulin Protocol
Instructions: Check patient’s blood sugar before meals, at bedtime, and as needed for symptoms of hypoglycemia or hyperglycemia. Use the following table to administer insulin lispro PRN.
| Blood Sugar Range | Lispro Insulin Instructions |
|---|---|
| Less than 70 | Hold all insulin and initiate hypoglycemia protocol. |
| 70-150 | 0 units |
| 151-174 | 2 units |
| 175-199 | 4 units |
| 200-224 | 6 units |
| 225-249 | 8 units |
| 250-274 | 10 units |
| 275-299 | 12 units |
| Greater than 300 | Administer 14 units and call the provider. |
Hypoglycemia
When caring for patients with diabetes mellitus and monitoring their blood glucose readings, it is important to continually monitor for signs of hypoglycemia. Hypoglycemia is defined as blood sugar readings less than 70 and signs and symptoms such as the following:
- Shakiness
- Feeling nervous or anxious
- Sweating, chills, and clamminess
- Irritability or impatience
- Confusion
- Fast heartbeat
- Feeling light-headed or dizzy
- Hunger
- Nausea
- Color draining from the skin (pallor)
- Feeling sleepy
- Feeling weak or having no energy
- Blurred/impaired vision
- Tingling or numbness in the lips, tongue, or cheeks
- Headaches
- Coordination problems or clumsiness
- Nightmares or crying out during sleep
- Seizures[4]
A low blood sugar level triggers the release of epinephrine (adrenaline), the “fight-or-flight” hormone. Epinephrine causes the symptoms of hypoglycemia such as a rapid heartbeat, sweating, and anxiety. If a patient’s blood sugar level continues to drop, the brain has impaired functioning. This may lead to seizures and a coma.[5]
If a nurse suspects hypoglycemia is occurring, a blood sugar reading should be obtained, and appropriate actions taken. Most agencies have a hypoglycemia protocol based on the “15-15 Rule.” The 15-15 Rule is to provide 15 grams of carbohydrate and recheck the blood glucose after 15 minutes. If the reading is still below 70 mg/dL, another serving of 15 grams of carbohydrate should be provided and the process continued until the blood sugar is above 70 mg/dL. Fifteen grams of carbohydrate includes options like 4 ounces of juice or regular soda, hard candy, or glucose tablets. If a patient is experiencing severe hypoglycemia and cannot swallow, a glucagon injection or intravenous administration of dextrose may be required.[6]
Hyperglycemia
Hyperglycemia is defined as elevated blood glucose and often causes signs and symptoms such as frequent urination and increased thirst. Hyperglycemia occurs when the patient’s body does not produce enough insulin or cannot use the insulin properly at the cellular level. There are many potential causes of hyperglycemia, such as not receiving enough medication to effectively control blood glucose, eating more than planned, exercising less than planned, or increased stress from an illness, surgery, hospitalization, or other life events.
If a patient’s blood glucose is greater than 240 mg/dL, their urine is typically checked for ketones. Ketones indicate a condition called ketoacidosis may be occurring. Ketoacidosis occurs in patients whose pancreas is no longer creating insulin, so fats are broken down for energy and waste products called ketones are produced. If the kidneys cannot effectively eliminate ketones in the urine, they build up in the blood and cause ketoacidosis. Ketoacidosis is a life-threatening condition that requires immediate notification of the provider for treatment. Symptoms of ketoacidosis include fruity-smelling breath, nausea, vomiting, very dry mouth, and shortness of breath. Treatment of ketoacidosis often requires the administration of intravenous insulin while the patient is closely monitored in a critical care inpatient unit.[7]
For more information about diabetes mellitus, measuring blood sugar levels, and diabetic medications, visit the “Endocrine” chapter in Open RN Nursing Pharmacology.
Glucometer Use
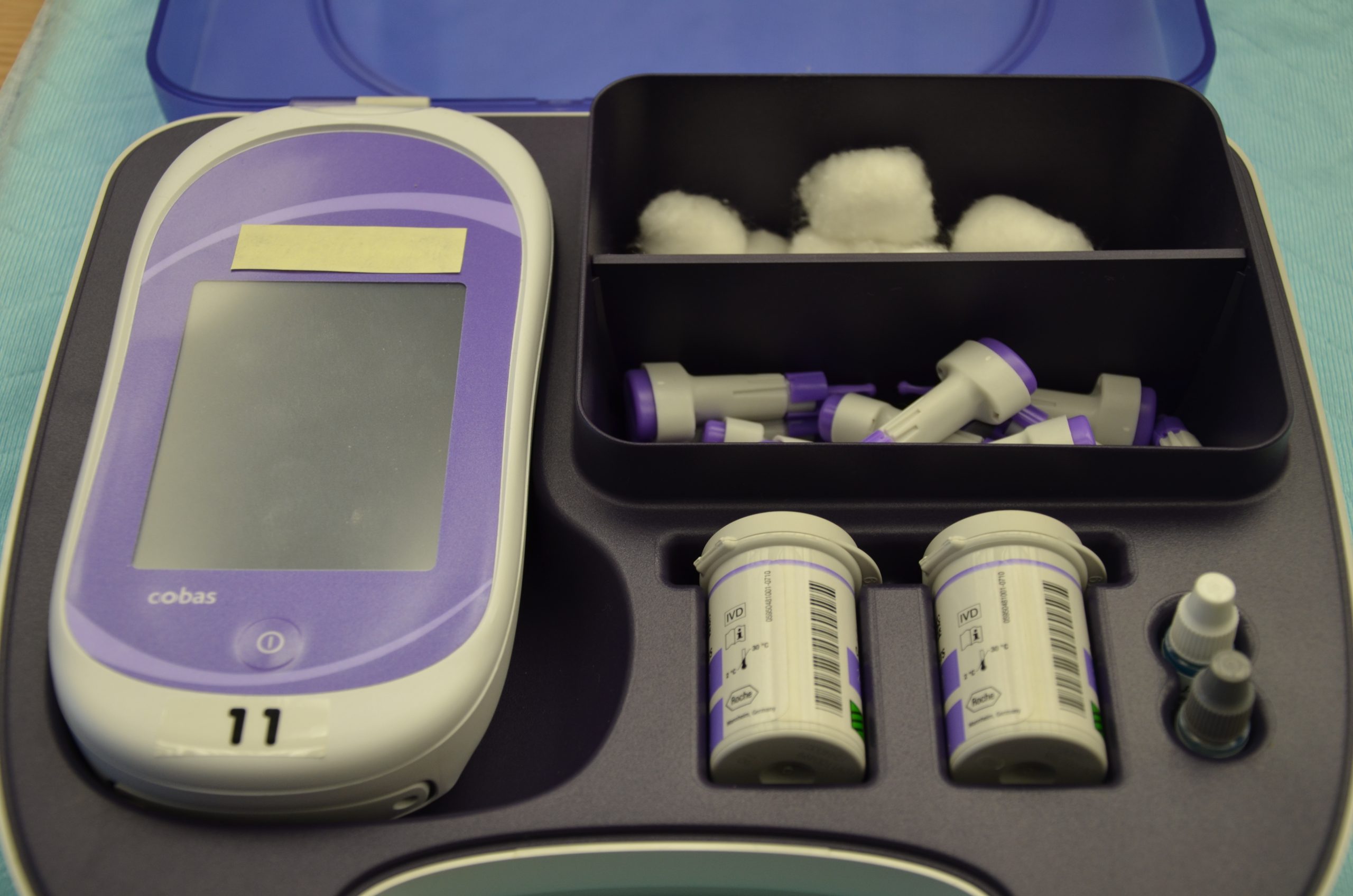
It is typically the responsibility of a nurse to perform bedside blood glucose readings, but in some agencies, this procedure may be delegated to trained nursing assistants or medical assistants. See Figure 19.1[8] for an image of a standard bedside glucometer kit that contains a glucometer, lancets, reagent strips, and calibration drops. Prior to performing a blood glucose test, read the manufacturer’s instructions and agency policy because they may vary across devices and sites. Ensure the glucometer has been calibrated per agency policy.[9]
Before beginning the procedure, determine if there are any conditions present that could affect the reading. For example, is the patient fasting? Has the patient already begun eating? Is the patient demonstrating any symptoms of hypoglycemia or hyperglycemia? Keep your patient safe by applying your knowledge of diabetes, the medication being administered, and the uniqueness of the patient to make appropriate clinical judgments regarding the procedure and associated medication administration.[10]
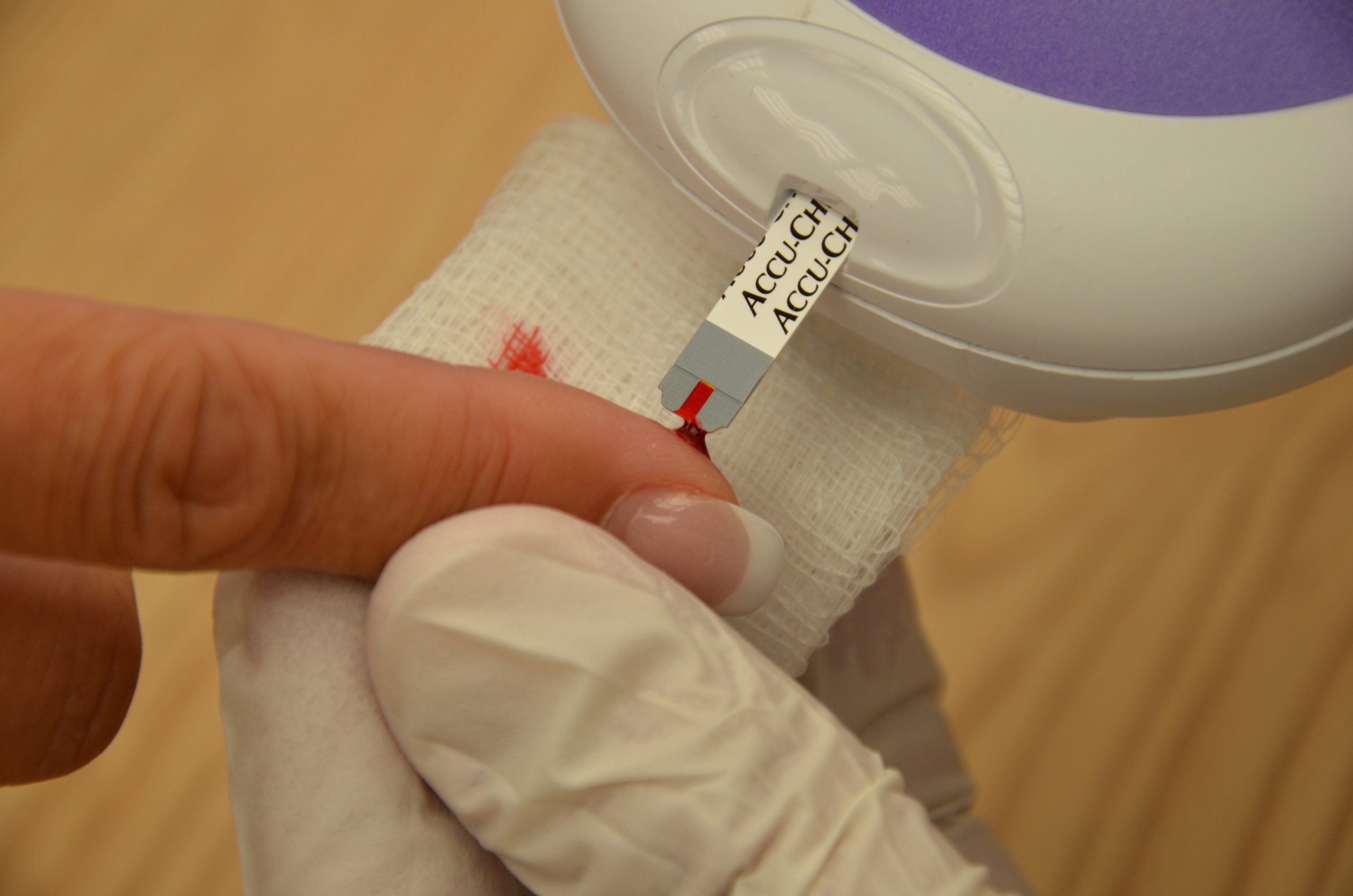
See the “Checklist for Blood Glucose Monitoring” for details regarding the procedure. It is often important to keep the patient’s hand warm and in a dependent position to promote vasodilation and obtain a good blood sample. If necessary, warm compresses can be applied for 10 minutes prior to the procedure to promote vasodilation. Follow the manufacturer’s instructions to prepare the glucometer for measurement. After applying clean gloves, clean the patient’s skin with an alcohol wipe for 30 seconds, allow the site to dry, and then puncture the skin using the lancet. See Figure 19.2[11] for an image of performing a skin puncture using a lancet.

If needed, gently squeeze above the site to obtain a large drop of blood. Do not milk or massage the finger because it may introduce excess tissue fluid and hemolyze the specimen. Wipe away the first drop of blood and use the second drop for the blood sample. Follow agency policy and manufacturer instructions regarding placement of the drop of blood for absorption on the reagent strip. See Figure 19.3[12] for an image of a nurse absorbing the patient’s drop of blood on the reagent strip. Timeliness is essential in gathering an appropriate specimen before clotting occurs or the glucometer times out.
Cleanse the glucometer and document the blood glucose results according to agency policy. Report any concerns about patient symptoms or blood sugar results according to agency policy.
Life Span Considerations
Blood glucose samples should be taken from the heel of newborns and infants up to the age of six months. When obtaining a sample from the heel, the sample is taken from the medial or lateral plantar surface.
View a supplementary YouTube video on Obtaining a Bedside Blood Glucose[13]
Media Attributions
- DSC_0718 (1)
- This work is a derivative of Nursing Pharmacology by Open RN licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- Donihi, A. C., DiNardo, M. M., DeVita, M. A., & Korytkowski, M. T. (2006). Use of a standardized protocol to decrease medication errors and adverse events related to sliding scale insulin. Quality & Safety in Health Care, 15(2), 89–91. https://doi.org/10.1136/qshc.2005.014381 ↵
- American Diabetes Association. (n.d.). Hypoglycemia (Low blood sugar). https://www.diabetes.org/diabetes/medication-management/blood-glucose-testing-and-control/hypoglycemia ↵
- American Diabetes Association. (n.d.). Hypoglycemia (Low blood sugar). https://www.diabetes.org/diabetes/medication-management/blood-glucose-testing-and-control/hypoglycemia ↵
- American Diabetes Association. (n.d.). Hypoglycemia (Low blood sugar). https://www.diabetes.org/diabetes/medication-management/blood-glucose-testing-and-control/hypoglycemia ↵
- American Diabetes Association. (n.d.). Hyperglycemia (High blood glucose). https://www.diabetes.org/diabetes/medication-management/blood-glucose-testing-and-control/hyperglycemia ↵
- “DSC_0718.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/8-2-glucometer-use/ ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- “DSC_1130.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/8-2-glucometer-use/ ↵
- “DSC_1141.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/8-2-glucometer-use/ ↵
- RegisteredNurseRN. (2015, August 12). How to prick fingertips with a lancet device for checking a blood sugar | Nursing skills [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/JPJ4l7QZ9eM ↵
Learning Activities
Chest Pain Case Study (Case Study answers are located in the Answer Key at the end of the book.)[1]
Mrs. Fatima Khan is a 58-year-old female who presents to the emergency department complaining of severe chest pain that started approximately 30 minutes ago. She describes the pain as a crushing sensation located in the center of her chest, radiating to her left arm. She rates the pain as 9/10 on the pain scale and reports associated symptoms of diaphoresis, nausea, and shortness of breath. She has a medical history of hypertension, hyperlipidemia, and type 2 diabetes mellitus and no known allergies. Current medications include lisinopril 10 mg daily, metformin 1000 mg twice daily, and atorvastatin 40 mg daily.
Vital Signs: BP 180/100mmHg, HR 110 bpm, RR 24 bpm, O2 sat 92% on room air, Temperature 37.0 C (98.6 F).
Physical Examination: Client is diaphoretic with a S3 gallop, shallow respirations, and audible crackles bilaterally. Skin is cool, clammy, and pale.
Laboratory and Diagnostic Results:
-
- Troponin: Elevated (> 0.04 ng/mL)
- CK-MB: Elevated
- Blood Glucose: 220 mg/dL
- Total Cholesterol: 240 mg/dL
- ECG: ST-segment elevation in leads II, III, aVF, and V1-V6
- Echocardiogram: Left ventricular dysfunction with decreased ejection fraction (EF 30%)
Questions:
- What is the significance of elevated troponin levels in a client with suspected MI?
- How do elevated CK-MB levels contribute to the diagnosis of MI, and how do they differ from troponin levels in timing and specificity?
- Why is it important to monitor blood glucose levels in a client with acute MI, and what impact can elevated levels have on the client's prognosis?
- Describe the role of total cholesterol levels in the assessment of cardiovascular risk and their relevance in the management of MI.
“Cardiology Glossary Cards” by Open RN is licensed under CC BY-NC 4.0
“Cardiology Question Set 1” by Open RN is licensed under CC BY-NC 4.0
“Cardiology Question Set 2” by Open RN is licensed under CC BY-NC 4.0
![]()
Test your knowledge on pediatric cardiovascular conditions using this NCLEX Next Generation-style bowtie question. You may reset and resubmit your answers to this question an unlimited number of times.[3]
![]()
Test your knowledge on heart failure using this NCLEX Next Generation-style multiple response question. You may reset and resubmit your answers to this question an unlimited number of times.[4]
![]()
Test your knowledge on heart failure using this NCLEX Next Generation-style case study. You may reset and resubmit your answers to this question an unlimited number of times.[5]
![]()
Test your knowledge using this NCLEX Next Generation-style question. You may reset and resubmit your answers to this question an unlimited number of times.[6]
![]()
Test your knowledge on peripheral arterial disease using this NCLEX Next Generation-style case study. You may reset and resubmit your answers to this question an unlimited number of times.[7]
![]()
Test your knowledge on venous insufficiency using this NCLEX Next Generation-style case study. You may reset and resubmit your answers to this question an unlimited number of times.[8]
![]()
Test your knowledge on myocardial infarction using this NCLEX Next Generation-style case study. You may reset and resubmit your answers to this question an unlimited number of times.[9]
Telehealth Scenarios
Telehealth is an innovative technology that can bridge the gap between health care professionals and clients, especially for clients who live in remote areas. Telehealth makes health care not only more accessible but can also provide continuity of care and prevent unnecessary hospitalizations. Nurses who provide telehealth services become digital communicators and educators, clinical expertise with empathy and effective online communication.
Practice using effective telehealth communication in the following three scenarios with an 80-year-old Hispanic male who has chronic heart failure and is self-managing his condition at home[10]
Alejandro Hernandez, Telehealth Visit 1: Post-hospitalization Follow-Up
Alejandro Hernandez, Telehealth Visit 2: Identifying Learning Needs
Alejandro Hernandez, Telehealth Visit 3: Evaluating Effectiveness of Health Teaching
Learning Activities
Chest Pain Case Study (Case Study answers are located in the Answer Key at the end of the book.)[11]
Mrs. Fatima Khan is a 58-year-old female who presents to the emergency department complaining of severe chest pain that started approximately 30 minutes ago. She describes the pain as a crushing sensation located in the center of her chest, radiating to her left arm. She rates the pain as 9/10 on the pain scale and reports associated symptoms of diaphoresis, nausea, and shortness of breath. She has a medical history of hypertension, hyperlipidemia, and type 2 diabetes mellitus and no known allergies. Current medications include lisinopril 10 mg daily, metformin 1000 mg twice daily, and atorvastatin 40 mg daily.
Vital Signs: BP 180/100mmHg, HR 110 bpm, RR 24 bpm, O2 sat 92% on room air, Temperature 37.0 C (98.6 F).
Physical Examination: Client is diaphoretic with a S3 gallop, shallow respirations, and audible crackles bilaterally. Skin is cool, clammy, and pale.
Laboratory and Diagnostic Results:
-
- Troponin: Elevated (> 0.04 ng/mL)
- CK-MB: Elevated
- Blood Glucose: 220 mg/dL
- Total Cholesterol: 240 mg/dL
- ECG: ST-segment elevation in leads II, III, aVF, and V1-V6
- Echocardiogram: Left ventricular dysfunction with decreased ejection fraction (EF 30%)
Questions:
- What is the significance of elevated troponin levels in a client with suspected MI?
- How do elevated CK-MB levels contribute to the diagnosis of MI, and how do they differ from troponin levels in timing and specificity?
- Why is it important to monitor blood glucose levels in a client with acute MI, and what impact can elevated levels have on the client's prognosis?
- Describe the role of total cholesterol levels in the assessment of cardiovascular risk and their relevance in the management of MI.
“Cardiology Glossary Cards” by Open RN is licensed under CC BY-NC 4.0
“Cardiology Question Set 1” by Open RN is licensed under CC BY-NC 4.0
“Cardiology Question Set 2” by Open RN is licensed under CC BY-NC 4.0
![]()
Test your knowledge on pediatric cardiovascular conditions using this NCLEX Next Generation-style bowtie question. You may reset and resubmit your answers to this question an unlimited number of times.[13]
![]()
Test your knowledge on heart failure using this NCLEX Next Generation-style multiple response question. You may reset and resubmit your answers to this question an unlimited number of times.[14]
![]()
Test your knowledge on heart failure using this NCLEX Next Generation-style case study. You may reset and resubmit your answers to this question an unlimited number of times.[15]
![]()
Test your knowledge using this NCLEX Next Generation-style question. You may reset and resubmit your answers to this question an unlimited number of times.[16]
![]()
Test your knowledge on peripheral arterial disease using this NCLEX Next Generation-style case study. You may reset and resubmit your answers to this question an unlimited number of times.[17]
![]()
Test your knowledge on venous insufficiency using this NCLEX Next Generation-style case study. You may reset and resubmit your answers to this question an unlimited number of times.[18]
![]()
Test your knowledge on myocardial infarction using this NCLEX Next Generation-style case study. You may reset and resubmit your answers to this question an unlimited number of times.[19]
Telehealth Scenarios
Telehealth is an innovative technology that can bridge the gap between health care professionals and clients, especially for clients who live in remote areas. Telehealth makes health care not only more accessible but can also provide continuity of care and prevent unnecessary hospitalizations. Nurses who provide telehealth services become digital communicators and educators, clinical expertise with empathy and effective online communication.
Practice using effective telehealth communication in the following three scenarios with an 80-year-old Hispanic male who has chronic heart failure and is self-managing his condition at home[20]
Alejandro Hernandez, Telehealth Visit 1: Post-hospitalization Follow-Up
Alejandro Hernandez, Telehealth Visit 2: Identifying Learning Needs
Alejandro Hernandez, Telehealth Visit 3: Evaluating Effectiveness of Health Teaching
Acute coronary syndrome: A group of conditions that involves a sudden compromise in blood flow to the myocardium. (Chapter 5.7)
Afterload: The force the ventricles must generate to pump blood against the resistance in the vessels. (Chapter 5.2)
Aneurysm: Dilation or bulging of a blood vessel caused by weakened vessel walls. (Chapter 5.12)
Angina: Chest pain or discomfort that is unpredictable and occurs at rest or with minimal exertion. (Chapter 5.7)
Angioplasty: Use of a balloon to stretch open a blocked artery. (Chapter 5.3)
Ankle-brachial index (ABI): An assessment comparing the blood pressure in the arms (brachial artery) to that in the ankles (dorsalis pedis or posterior tibial arteries). (Chapter 5.9)
Arteriosclerosis: The thickening and stiffening of arterial walls. (Chapter 5.6)
Artery: A blood vessel that carries blood away from the heart. (Chapter 5.2)
Ascites: Abnormal fluid accumulation in the abdomen. (Chapter 5.3, Chapter 5.8)
Atherosclerosis: Buildup of cholesterol, fatty deposits, and wastes within the lining of the arteries. (Chapter 5.6)
Blood pressure: The force exerted by blood on the walls of the blood vessels. (Chapter 5.2)
Bradycardia: The condition in which resting rate drops below 60 bpm. (Chapter 5.2, Chapter 5.3)
Capillary: A microscopic channel that supplies blood to the tissue cells where nutrients and wastes are exchanged at the cellular level. (Chapter 5.2)
Capillary refill test: Test performed on the nail beds to monitor perfusion. (Chapter 5.3)
Cardiac catheterization: A diagnostic procedure used to visualize the coronary arteries, heart chambers, and great vessels; also known as coronary angiography or angiogram. (Chapter 5.3)
Cardiac output (CO): Measurement of the amount of blood pumped by each ventricle in one minute. (Chapter 5.2)
Cardiac stress test: A diagnostic procedure used to evaluate the performance and function of the heart during physical activity; also known as an exercise stress test or treadmill test. (Chapter 5.3)
Cardiovascular disease (CVD): Disease that affects the heart and blood vessels. (Chapter 5.1)
Clipping: A surgical procedure involving the placement of a small metal clip at the base of the aneurysm to block blood flow into it and prevent rupture. (Chapter 5.12)
Coiling: A minimally invasive procedure involving the insertion of tiny coils into the aneurysm through a catheter to promote clotting within the aneurysm and prevent blood flow into it. (Chapter 5.12)
Compliance: The ability of any compartment to expand to accommodate increased content. (Chapter 5.2)
Contractility: The force or strength of the contraction itself. (Chapter 5.2)
Coronary angiogram: A procedure that uses a special dye (contrast material) and X-rays to see how blood flows through the arteries in the heart. (Chapter 5.3)
Coronary artery disease (CAD): Plaque buildup that causes the inside of the coronary arteries to narrow over time, which can partially or totally block the blood flow to the muscle tissue of the heart. (Chapter 5.7)
D-dimer: A blood test that is a marker for the presence of blood clots, specifically the breakdown products of fibrin that result from the dissolution of a blood clot. (Chapter 5.11)
Deep vein thrombosis: A blood clot in a peripheral deep vein. (Chapter 5.11)
Diastole: Period of relaxation that occurs as the chambers fill with blood. (Chapter 5.2)
Duplex ultrasonography: An imaging test that uses sound waves to look at the flow of blood in the veins. (Chapter 5.11)
Dyspnea: Shortness of breath. (Chapter 5.3, Chapter 5.8)
Dysrhythmia: An altered conduction of the electrical signal through the heart, resulting in an abnormal rate or rhythm.
Echocardiography: A noninvasive diagnostic test that uses sound waves (ultrasound) to create real-time images of the heart's structure and function. (Chapter 5.3)
Edema: Excess fluid around the cells. (Chapter 5.2)
Electrocardiogram (EKG or ECG): A recording of the electrical activity of the heart that allows health care professionals to assess the heart’s rhythm and identify various cardiac conditions. (Chapter 5.3)
Embolus: A portion of a thrombus that breaks free from the vessel wall and enters the circulation. (Chapter 5.6)
Endarterectomy: Surgical removal of plaque from the arteries. (Chapter 5.6)
Endovascular aneurysm repair (EVAR): A minimally invasive procedure where a stent graft is inserted into the aneurysm through small incisions in the groin or other access points. (Chapter 5.12)
Epicardial pacemakers: Pacemakers inserted through an incision in the chest, and the leads are attached to the heart. (Chapter 5.3)
Heart failure (HF): Occurs when the heart loses its effectiveness in pumping blood and is referred to as decreased cardiac output. (Chapter 5.8)
Heart rate (HR): The number of times the heart beats per minute. (Chapter 5.2)
Hematemesis: Vomiting of blood. (Chapter 5.12)
Hemoptysis: Coughing up blood. (Chapter 5.11)
Holter monitor: A portable device designed to continuously record a client's heart rhythm and electrical activity over an extended period, typically 24 to 48 hours. (Chapter 5.3)
Hypertension: Chronically elevated blood pressure greater than 120/80 mm Hg. (Chapter 5.5)
Hypervolemia: Excessive fluid volume. (Chapter 5.2)
Hypovolemia: Low blood volume. (Chapter 5.2)
Infarct: The most significant area of damage during an MI. (Chapter 5.7)
Infective endocarditis: A potentially life-threatening infection of the inner lining of the heart chambers and valves. (Chapter 5.13)
Injured: Tissues located next to ischemic area that can remain viable as long as oxygen is delivered to the tissue by pathways that circumvent the blockage. (Chapter 5.7)
Intermittent claudication: Muscle pain, cramping, or fatigue during physical activity (e.g., walking) that resolves with rest and recurs with activity. (Chapter 5.9)
Ischemia: Condition in which oxygenated blood flow to tissue is reduced. (Chapter 5.7)
Janeway lesions: Nontender, red, or hemorrhagic macules often found on the palms of the hands or soles of the feet. (Chapter 5.13)
Jugular venous distention (JVD): Distended jugular vein when client is positioned at 45 degrees. (Chapter 5.3)
Melena: Dark, tarry stools. (Chapter 5.12)
Metabolic syndrome: A group of conditions that increase the risk of coronary heart disease, diabetes, and stroke. The conditions include elevated blood pressure, blood glucose, and triglyceride levels, as well as increased waist circumference. (Chapter 5.3)
Modifiable risk factors: Risk factors that an individual can control through their actions, behavior, or lifestyle choices. (Chapter 5.3)
Murmurs: Abnormal heart sounds that may indicate valvular or structural heart abnormalities. (Chapter 5.3)
Myocardial infarction (MI): Commonly referred to as a “heart attack"; occurs when there is a sudden blockage within the coronary arteries that occludes oxygenated blood flow to the heart tissue. (Chapter 5.7)
Myocardial ischemia: Also known as "heart attack." Myocardial ischemia occurs when there is decreased blood flow through the coronary arteries. (Chapter 5.3)
Negative inotropic factors: Factors that increase contractility. (Chapter 5.2)
Nonmodifiable risk factors: Risk factors are those that cannot be changed. (Chapter 5.3)
Open surgical repair: An operation where the aneurysm is directly accessed, and a graft is sewn into place to replace the weakened section of the artery. (Chapter 5.12)
Orthopnea: Shortness of breath when lying flat. (Chapter 5.3, Chapter 5.8)
Osler's nodes: Tender subcutaneous nodules often found on the fingertips. (Chapter 5.13)
Paroxysmal nocturnal dyspnea: Sudden nighttime breathlessness. (Chapter 5.3)
Pectus carinatum: Protrusion of the chest. (Chapter 5.3)
Pectus excavatum: Depression of the chest. (Chapter 5.3)
Percutaneous transluminal angioplasty (PTA): A minimally invasive procedure in which a catheter is inserted into a narrowed artery and a balloon is inflated to compress the plaque and widen the artery. (Chapter 5.9)
Perfusion: The passage of blood through the blood vessels. (Chapter 5.2)
Pericardial friction rub: A high-pitched, scratchy sound that occurs when the inflamed pericardial layers rub against each other. (Chapter 5.3)
Peripheral artery disease (PAD): A type of atherosclerosis in which narrowed or blocked arteries reduce blood flow to the limbs, usually the legs; also known as peripheral vascular disease (PVD). (Chapter 5.9)
Poikilothermia: Coolness in an affected limb. (Chapter 5.9)
Point of maximum impulse (PMI): The location where the apex of the heart touches the chest wall. (Chapter 5.3)
Positive inotropic factors: Factors that increase contractility. (Chapter 5.2)
Precordium: Area over the heart. (Chapter 5.3)
Preload: End diastolic volume. (Chapter 5.2)
Primary hypertension: The most common type of hypertension that typically has no identifiable cause. It tends to develop gradually over time and is influenced by various risk factors such as genetics, age, race, diet, lifestyle, and stress. (Chapter 5.5)
Pulse: Expansion and recoiling of the arterial wall. (Chapter 5.2)
Roth spots: Retinal hemorrhages that are visible on fundoscopy. (Chapter 5.13)
S1: The first heart sound, often described as "lub," that corresponds to the closure of the atrioventricular valves (i.e., the mitral and tricuspid valves). (Chapter 5.3)
S2: The second heart sound, described as "dub," that corresponds to the closure of the semilunar valves (aortic and pulmonic valves). (Chapter 5.3)
S3: A low frequency heart sound, known as a ventricular gallop, that is heard shortly after the S2 and precedes S1. (Chapter 5.3)
S4: A sound heard late in the cardiac cycle, just before S1; known as an atrial gallop. (Chapter 5.3)
Secondary hypertension: Hypertension that occurs as the result of an underlying medical condition or medication. (Chapter 5.5)
Segmental pressure measurements: Blood pressure readings at multiple levels along the limbs (e.g., thigh, calf, ankle) to help identify specific locations of arterial narrowing or blockage. (Chapter 5.9)
Sinoatrial (SA) node: Establishes normal cardiac rhythm within the heart. (Chapter 5.2)
Sinus rhythm: Normal electrical pattern of the heart. (Chapter 5.2)
Splinter hemorrhages: Linear hemorrhages under the nails. (Chapter 5.13)
Stent: Insertion of a small mesh tube to help expand an artery. (Chapter 5.3)
Stroke volume (SV): The quantity of blood pumped out of the left ventricle with contraction of the heart muscle. (Chapter 5.2)
Systole: Period of contraction that the heart undergoes while it pumps blood into circulation. (Chapter 5.2)
Tachycardia: Heart rate over 100 beats per minute. (Chapter 5.2, Chapter 5.3)
Thrills: Vibratory sensations over the precordium, particularly in areas where murmurs are suspected. (Chapter 5.3)
Transesophageal echocardiogram: A invasive procedure that involves the insertion of an ultrasound probe via the esophagus to produce a more detailed ultrasound image of heart. (Chapter 5.3)
Transthoracic echocardiogram: A noninvasive diagnostic test that uses sound waves (ultrasound) to create real-time images of the heart's structure and function. (Chapter 5.3)
Transvenous pacemakers: Pacemakers inserted through a vein and threaded into the heart. (Chapter 5.3)
Troponin: A blood test used to help diagnose myocardial infarction that measures protein released into the bloodstream when heart tissue is damaged. (Chapter 5.7)
Veins: Blood vessels that return blood to the heart. (Chapter 5.2)
Venous insufficiency: A condition that occurs when the veins in the legs have difficulty returning blood back to the heart. (Chapter 5.10)
Venous reserve: Volume of venous blood located in venous networks within the liver, bone marrow, and integument. (Chapter 5.2)
Venous stasis: Slow blood flow in the veins, usually in the legs. (Chapter 5.8, Chapter 5.11)
Venules: Small veins. (Chapter 5.2)
Chest Pain Case Study Answers
1. What is the significance of elevated troponin levels in a client with suspected MI?
Elevated troponin levels in a client with suspected MI indicate myocardial damage or injury. Troponin is a highly sensitive and specific marker of cardiac muscle injury, and its elevation suggests necrosis of cardiomyocytes, which is characteristic of myocardial infarction. Troponin levels typically rise within four to six hours of the onset of chest pain, peak within 12-24 hours, and may remain elevated for several days, making it a valuable tool for diagnosing MI and assessing its severity.
2. How do elevated CK-MB levels contribute to the diagnosis of MI, and how do they differ from troponin levels in timing and specificity?
Elevated creatine kinase-MB (CK-MB) levels contribute to the diagnosis of MI by indicating myocardial damage, similar to troponin. However, CK-MB is less specific to cardiac tissue and can also be elevated in skeletal muscle injury. CK-MB levels typically rise within three to six hours of myocardial injury, peak within 12-24 hours, and return to baseline within 48-72 hours. Unlike troponin, CK-MB levels may be affected by skeletal muscle trauma or surgery, limiting its specificity compared to troponin.
3. Why is it important to monitor blood glucose levels in a client with acute MI, and what impact can elevated levels have on the client's prognosis?
Monitoring blood glucose levels in a client with acute MI is important because hyperglycemia is associated with worse outcomes and increased mortality in these clients. Elevated blood glucose levels during acute MI may exacerbate myocardial ischemia, promote inflammation and oxidative stress, and impair myocardial function. Tight glycemic control is, therefore, recommended to improve outcomes and reduce complications in clients with MI, including reducing the risk of arrhythmias, heart failure, and recurrent events.
4. Describe the role of total cholesterol levels in the assessment of cardiovascular risk and their relevance in the management of MI.
Total cholesterol levels play a role in assessing cardiovascular risk and guiding treatment strategies in clients with MI. Elevated total cholesterol, particularly low-density lipoprotein cholesterol (LDL-C), is a major modifiable risk factor for atherosclerotic cardiovascular disease, including MI. High cholesterol levels contribute to the development and progression of atherosclerosis, leading to coronary artery disease and myocardial infarction. Lowering cholesterol levels through lifestyle modifications and pharmacotherapy, such as statins, is essential for reducing the risk of recurrent cardiovascular events and improving long-term outcomes in clients with MI.
All of the answers to the interactive element are found within the element.

