Basic Concepts of Oxygenation
Open Resources for Nursing (Open RN)
When assessing a patient’s oxygenation status, it is important for the nurse to have an understanding of the underlying structures of the respiratory system to best understand their assessment findings.
Visit the “Respiratory Assessment” chapter for more information about the structures of the respiratory system.
For more information about common respiratory conditions and medications used to treat them, visit the “Respiratory” chapter in Open RN Nursing Pharmacology.
View supplementary YouTube videos on oxygenation basics:
TED-Ed video on Oxygen’s Journey[1]
Breathing Mechanics[2]
Gas Exchange[3]
Carbon Dioxide Transport[4]
Assessing Oxygenation Status
A patient’s oxygenation status is routinely assessed using pulse oximetry, referred to as SpO2. SpO2 is an estimated oxygenation level based on the saturation of hemoglobin measured by a pulse oximeter. Because the majority of oxygen carried in the blood is attached to hemoglobin within the red blood cell, SpO2 estimates how much hemoglobin is “saturated” with oxygen. The target range of SpO2 for an adult is 95-100%.[5] For patients with chronic respiratory conditions, such as COPD, the target range for SpO2 is often lower at 88% to 92%.
Although SpO2 is an efficient, noninvasive method to assess a patient’s oxygenation status, it is an estimate and not always accurate. For example, decreased peripheral circulation can also cause a misleading low SpO2 level due to lack of blood flow to the area in which the pulse oximeter is attached. Another example of an inaccurate reading is if the patient is severely anemic with a decreased hemoglobin level. They may have a normal SpO2 reading because their existing hemoglobin is saturated with oxygen, even though the available oxygen is not enough to meet the metabolic demands of their body.
A more specific measurement of oxygen and carbon dioxide in the blood is obtained through an arterial blood gas (ABG). ABG results are often obtained for patients who have deteriorating or unstable respiratory status requiring urgent and emergency treatment. An ABG is a blood sample that is typically drawn from the radial artery by a respiratory therapist, emergency or critical care nurse, or health care provider. ABG results evaluate oxygen, carbon dioxide, pH, and bicarbonate levels. The partial pressure of oxygen in the blood is referred to as PaO2. The normal PaO2 level of a healthy adult is 80 to 100 mmHg. The PaO2 reading is more accurate than a SpO2 reading because it is not affected by hemoglobin levels. The PaCO2 level is the partial pressure of carbon dioxide in the blood. The normal PaCO2 level of a healthy adult is 35-45 mmHg. The normal range of pH level for arterial blood is 7.35-7.45, and the normal range for the bicarbonate (HCO3) level is 22-26. The SaO2 level is also obtained, which is the calculated arterial oxygen saturation level. See Table 11.2a for a summary of normal ranges of ABG values.[6]
Table 11.2a Normal Ranges of ABG Values
| Value | Description | Normal Range |
|---|---|---|
| pH | Acid-base balance of blood | 7.35-7.45 |
| PaO2 | Partial pressure of oxygen | 80-100 mmHg |
| PaCO2 | Partial pressure of carbon dioxide | 35-45 mmHg |
| HCO3 | Bicarbonate level | 22-26 mEq/L |
| SaO2 | Calculated oxygen saturation | 95-100% |
Read more information about interpreting ABG results in the “Acid Base” section of the “Fluids and Electrolytes” chapter in Open RN Nursing Fundamentals, 2e.
Hypoxia and Hypercapnia
Hypoxia is defined as a reduced level of tissue oxygenation. Hypoxia has many causes, ranging from respiratory and cardiac conditions to anemia. Hypoxemia is a specific type of hypoxia that is defined as decreased partial pressure of oxygen in the blood (PaO2), measured by an arterial blood gas (ABG).
Early signs of hypoxia are anxiety, confusion, and restlessness. As hypoxia worsens, the patient’s level of consciousness and vital signs will worsen, with increased respiratory rate and heart rate and decreased pulse oximetry readings. Late signs of hypoxia include bluish discoloration of the skin and mucous membranes called cyanosis. Cyanosis is most easily seen around the lips and in the oral mucosa. A sign of chronic hypoxia is clubbing, a gradual enlargement of the fingertips (see Figure 11.1[7]). See Table 11.2b for symptoms and signs of hypoxia.[8]

Hypercapnia is an elevated level of carbon dioxide in the blood. This level is measured by the PaCO2 level in an ABG test and is indicated when the PaCO2 level is higher than 45. Hypercapnia is typically caused by hypoventilation or areas of the alveoli that are ventilated but not perfused. In a state of hypercapnia or hypoventilation, there is an accumulation of carbon dioxide in the blood. The increased carbon dioxide causes the pH of the blood to drop, leading to a state of respiratory acidosis.
You can read more about respiratory acidosis in the “Fluids and Electrolytes” chapter of the Open RN Nursing Fundamentals book.
Patients with hypercapnia can present with tachycardia, dyspnea, flushed skin, confusion, headaches, and dizziness. If the hypercapnia develops gradually over time, such as in a patient with chronic obstructive pulmonary disease (COPD), symptoms may be mild or may not be present at all. Hypercapnia is managed by addressing its underlying cause. A noninvasive positive pressure device such as a BiPAP may provide support to patients who are having trouble breathing normally, but if this is not sufficient, intubation may be required.[9]
Table 11.2b Symptoms and Signs of Hypoxia
| Signs & Symptoms | Description |
|---|---|
| Restlessness | Patient may become increasingly fidgety, move about the bed, demonstrate signs of anxiety and agitation. Restlessness is an early sign of hypoxia. |
| Tachycardia | An elevated heart rate (above 100 beats per minute in adults) can be an early sign of hypoxia. |
| Tachypnea | An increased respiration rate (above 20 breaths per minute in adults) is an indication of respiratory distress. |
| Shortness of breath (Dyspnea) | Shortness of breath is a subjective symptom of not getting enough air. Depending on severity, dyspnea causes increased levels of anxiety. |
| Oxygen saturation level (SpO2) | Oxygen saturation levels should be above 94% for an adult without an underlying respiratory condition. |
| Use of accessory muscles | Use of neck or intercostal muscles when breathing is an indication of respiratory distress. |
| Noisy breathing | Audible noises with breathing are an indication of respiratory conditions. Assess lung sounds with a stethoscope for adventitious sounds such as wheezing, rales, or crackles. Secretions can plug the airway, thereby decreasing the amount of oxygen available for gas exchange in the lungs. |
| Flaring of nostrils or pursed-lip breathing | Flaring is a sign of hypoxia, especially in infants. Pursed-lip breathing is a technique often used in patients with COPD. This breathing technique increases the amount of carbon dioxide exhaled so that more oxygen can be inhaled. |
| Position of patient | Patients in respiratory distress may sit up or lean over by resting arms on their legs to enhance lung expansion. Patients who are hypoxic may not be able to lie flat in bed. |
| Ability of patient to speak in full sentences | Patients in respiratory distress may be unable to speak in full sentences or may need to catch their breath between sentences. |
| Skin color (Cyanosis) | Changes in skin color to bluish or gray are a late sign of hypoxia. |
| Confusion or loss of consciousness (LOC) | This is a worsening sign of hypoxia. |
| Clubbing | Clubbing, a gradual enlargement of the fingertips, is a sign of chronic hypoxia. |
Treating Hypoxia
Acute hypoxia is a medical emergency and should be treated promptly with oxygen therapy. Failure to initiate oxygen therapy when needed can result in serious harm or death of the patient. Although oxygen is considered a medication that requires a prescription, oxygen therapy may be initiated without a physician’s order in emergency situations as part of the nurse’s response to the “ABCs,” a common abbreviation for airway, breathing, and circulation. Most agencies have a protocol in place that allows nurses to apply oxygen in emergency situations. After applying oxygen as needed, the nurse then contacts the provider, respiratory therapist, or rapid response team, depending on the severity of hypoxia. Devices such high-flow oxymasks, CPAP, BiPAP, or mechanical ventilation may be initiated by the respiratory therapist or provider to deliver higher amounts of inspired oxygen. Various types of oxygenation devices are further explained in the “Oxygenation Equipment” section.
Prescription orders for oxygen therapy will include two measurements of oxygen to be delivered – the oxygen flow rate and the fraction of inspired oxygen (FiO2). The oxygen flow rate is the number dialed up on the oxygen flow meter between 1 L/minute and 15 L/minute. Fio2 is the concentration of oxygen the patient inhales. Room air contains 21% oxygen concentration, so the FiO2 for supplementary oxygen therapy will range from 21% to 100% concentration.
In addition to administering oxygen therapy, there are several other interventions the nurse should consider implementing to a hypoxic patient. Additional interventions used to treat hypoxia in conjunction with oxygen therapy are outlined in Table 11.2c.[10]
Table 11.2c Interventions to Manage Hypoxia
| Interventions | Additional Information |
|---|---|
| Raise the Head of the Bed | Raising the head of the bed to high Fowler’s position promotes effective chest expansion and diaphragmatic descent, maximizes inhalation, and decreases the work of breathing. Patients with COPD who are short of breath may gain relief by sitting upright or leaning over a bedside table while in bed. |
| Encourage Enhanced Breathing and Coughing Techniques | Enhanced breathing and coughing techniques such as using pursed-lip breathing, coughing and deep breathing, huffing technique, incentive spirometry, and flutter valves may assist patients to clear their airway while maintaining their oxygen levels. See the following “Enhanced Breathing and Coughing Techniques” subsection for additional information regarding these techniques. |
| Manage Oxygen Therapy and Equipment | If the patient is already on supplemental oxygen, ensure the equipment is turned on, set at the required flow rate, correctly positioned on the patient, and properly connected to an oxygen supply source. If a portable tank is being used, check the oxygen level in the tank. Ensure the connecting oxygen tubing is not kinked, which could obstruct the flow of oxygen. Feel for the flow of oxygen from the exit ports on the oxygen equipment. In hospitals where medical air and oxygen are used, ensure the patient is connected to the oxygen flow port. Hospitals in America follow the national standard that oxygen flow ports are green and air outlets are yellow. |
| Assess the Need for Respiratory Medications | Pharmacological management is essential for patients with respiratory disease such as asthma, COPD, or severe allergic response. Bronchodilators effectively relax smooth muscles and open airways. Glucocorticoids relieve inflammation and also assist in opening air passages. Mucolytics decrease the thickness of pulmonary secretions so that they can be expectorated more easily. |
| Provide Oral Suctioning if Needed | Some patients may have a weakened cough that inhibits their ability to clear secretions from the mouth and throat. Patients with muscle disorders or those who have experienced a cerebral vascular accident (CVA) are at risk for aspiration pneumonia, which is caused by the accidental inhalation of material from the mouth or stomach. Provide oral suction if the patient is unable to clear secretions from the mouth and pharynx. See the chapter on “Tracheostomy Care and Suctioning” for additional details on suctioning. |
| Provide Pain Relief If Needed | Provide adequate pain relief if the patient is reporting pain. Pain increases anxiety and may inhibit the patient’s ability to take in full breaths. |
| Consider the Side Effects of Pain Medications | A common side effect of pain medication is sedation and respiratory depression.
For more information about interventions to manage respiratory depression, see the “Oxygenation” chapter in the Open RN Nursing Fundamentals textbook. |
| Consider Other Devices to Enhance Clearance of Secretions | Chest physiotherapy and specialized devices assist with secretion clearance, such as handheld flutter valves or vests that inflate and vibrate the chest wall. Consider requesting a consultation with a respiratory therapist based on the patient’s situation. |
| Plan Frequent Rest Periods Between Activities | Patients experiencing hypoxia often feel short of breath and fatigue easily. Allow the patient to rest frequently, and space out interventions to decrease oxygen demand in patients whose reserves are likely limited. |
| Consider Other Potential Causes of Dyspnea | If a patient’s level of dyspnea is worsening, assess for other underlying causes in addition to the primary diagnosis. Are there other respiratory, cardiovascular, or hematological conditions such as anemia occurring? Start by reviewing the patient’s most recent hemoglobin and hematocrit lab results. Completing a thorough assessment may reveal abnormalities in these systems to report to the health care provider. |
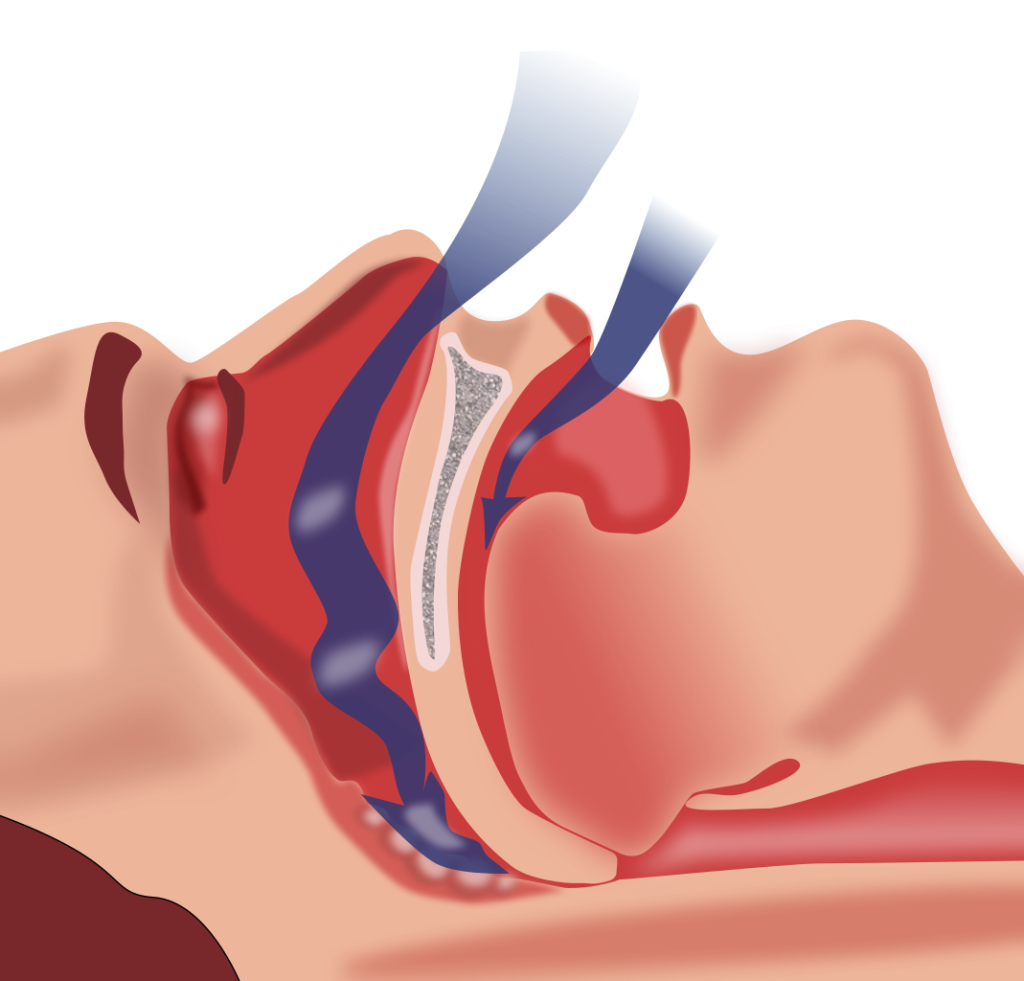
| Consider Obstructive Sleep Apnea | Patients with obstructive sleep apnea (OSA) are often not previously diagnosed prior to hospitalization. The nurse may notice the patient snores, has pauses in breathing while snoring, or awakens not feeling rested. These signs may indicate the patient is unable to maintain an open airway while sleeping, resulting in periods of apnea and hypoxia. If these apneic periods are noticed but have not been previously documented, the nurse should report these findings to the health care provider for further testing and follow-up. Testing consists of using continuous pulse oximetry while the patient is sleeping to determine if the patient is hypoxic during these episodes and if a CPAP device should be prescribed. See the box below for additional information regarding OSA. |
| Anxiety | Anxiety often accompanies the feeling of dyspnea and can worsen it. Anxiety in patients with COPD is chronically undertreated. It is important for the nurse to address the feelings of anxiety and dyspnea. Anxiety can be relieved by teaching enhanced breathing and coughing techniques, encouraging relaxation techniques, or administering antianxiety medications. |
Obstructive Sleep Apnea (OSA) is the most common type of sleep apnea. See Figure 11.2[11] for an illustration of OSA. As soft tissue falls to the back of the throat, it impedes the passage of air (blue arrows) through the trachea and is characterized by repeated episodes of complete or partial obstructions of the upper airway during sleep. The episodes of breathing cessations are called “apneas,” meaning “without breath.” Despite the effort to breathe, apneas are associated with a reduction in blood oxygen saturation due to the obstruction of the airway. Treatment for OSA often includes the use of a CPAP device.
Enhanced Breathing and Coughing Techniques
In addition to oxygen therapy and the interventions listed in Table 11.2c to implement for a patient experiencing dyspnea and hypoxia, there are several techniques a nurse can teach a patient to use to enhance their breathing and coughing. These techniques include pursed-lip breathing, incentive spirometry, coughing and deep breathing, and the huffing technique.
Pursed-Lip Breathing
Pursed-lip breathing is a technique that allows people to control their oxygenation and ventilation. The technique requires a person to inspire through the nose and exhale through the mouth at a slow controlled flow. See Figure 11.3[12] for an illustration of pursed-lip breathing. This type of exhalation gives the person a puckered or pursed appearance. By prolonging the expiratory phase of respiration, a small amount of positive end-expiratory pressure (PEEP) is created in the airways that helps to keep them open so that more air can be exhaled, thus reducing air trapping that occurs in some conditions such as COPD. Pursed-lip breathing often relieves the feeling of shortness of breath, decreases the work of breathing, and improves gas exchange. People also regain a sense of control over their breathing while simultaneously increasing their relaxation.[13]

View a supplementary YouTube video on pursed-lip breathing from the COPD Foundation called Breathing Techniques.[14]
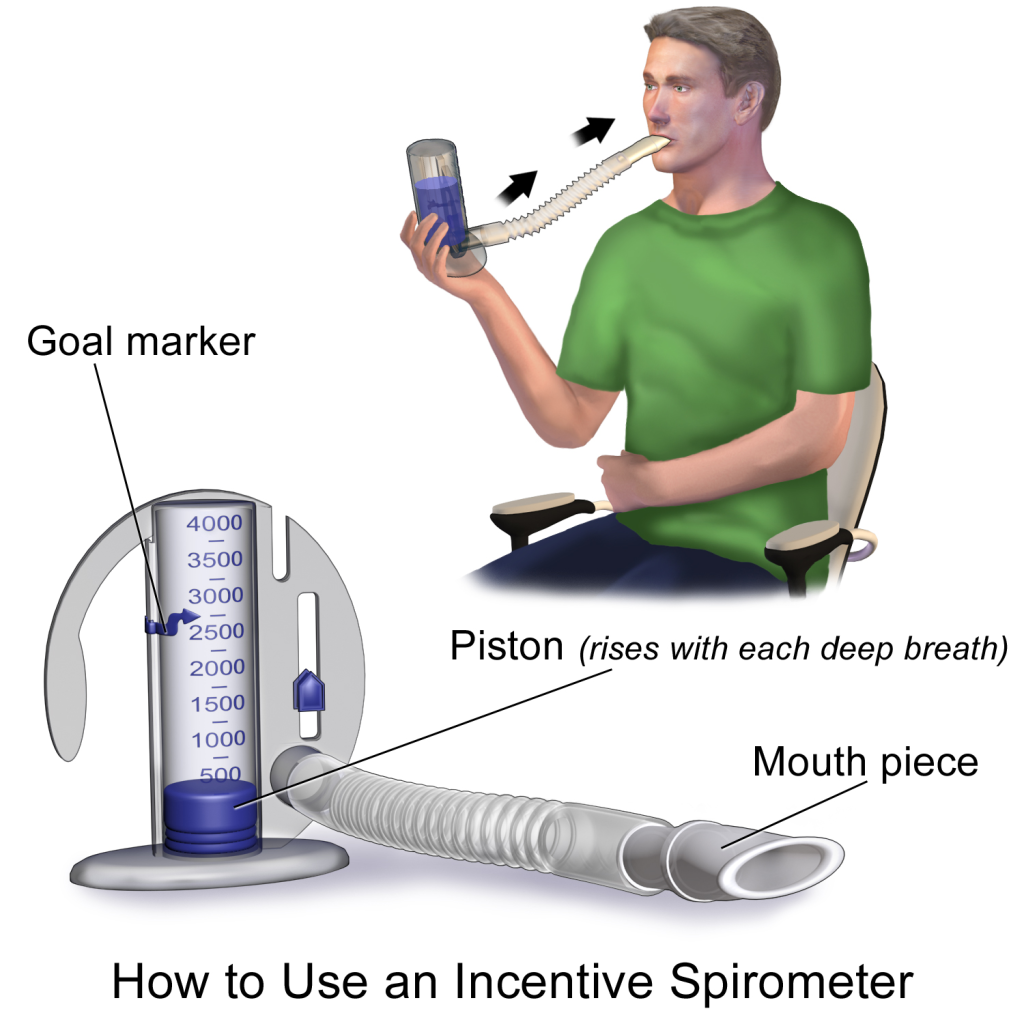
Incentive Spirometry
An incentive spirometer is a medical device often prescribed after surgery to prevent and treat atelectasis. Atelectasis occurs when alveoli become deflated or filled with fluid and can lead to pneumonia. See Figure 11.4[15] for an image of a patient using an incentive spirometer. While sitting upright, the patient should breathe in slowly and deeply through the tubing with the goal of raising the piston to a specified level. The patient should attempt to hold their breath for 5 seconds, or as long as tolerated, and then rest for a few seconds. This technique should be repeated by the patient 10 times every hour while awake.[16] The nurse may delegate this intervention to unlicensed assistive personnel, but the frequency in which it is completed and the volume achieved should be documented and monitored by the nurse.
Coughing and Deep Breathing
Teaching the coughing and deep breathing technique is similar to incentive spirometry but no device is required. The patient is encouraged to take deep, slow breaths and then exhale slowly. After each set of breaths, the patient should cough. This technique is repeated 3 to 5 times every hour.
Huffing Technique
The huffing technique is helpful for patients who have difficulty coughing. Teach the patient to inhale with a medium-sized breath and then make a sound like “Ha” to push the air out quickly with the mouth slightly open.
Vibratory PEP Therapy
Vibratory positive expiratory pressure (PEP) therapy uses handheld devices such as “flutter valves” or “Acapella” devices for patients who need assistance in clearing mucus from their airways. These devices (see Figure 11.5[17]) require a prescription and are used in collaboration with a respiratory therapist or advanced health care provider. To use vibratory PEP therapy, the patient should sit up, take a deep breath, and blow into the device. A flutter valve within the device creates vibrations that help break up the mucus so the patient can cough it up and spit it out. Additionally, a small amount of positive end-expiratory pressure (PEEP) is created in the airways that helps to keep them open so that more air can be exhaled.

View a supplementary YouTube video on using a flutter valve device from NHS University Hospitals Plymouth Physiotherapy called Acapella[18]
Media Attributions
- Acopaquia
- 1069px-Obstruction_ventilation_apnée_sommeil.svg
- aid611002-v4-728px-Live-With-Chronic-Obstructive-Pulmonary-Disease-Step-8
- Incentive_Spirometer (1)
- Flutter Valve Breathing Device 3I3A0982
- TED-Ed. (2017, April 13). Oxygen’s surprisingly complex journey through your body - Edna Butler [Video]. YouTube. All rights reserved. https://youtu.be/GVU_zANtroE ↵
- Forciea, B. (2015, May 12). Anatomy and physiology: Respiratory system: Breathing mechanics (v2.0) [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/X-J5Xgg3l6s ↵
- Forciea, B. (2015, May 12). Respiratory system: Gas exchange (v2.0) [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/uVWko7_v7MM ↵
- Forciea, B. (2015, May 12). Respiratory system: C02 transport (v2.0) [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/BmrvqZoxHYI ↵
- Hill, B., & Annesley, S. H. (2020). Monitoring respiratory rate in adults. British Journal of Nursing, 29(1), 12–16. https://doi.org/10.12968/bjon.2020.29.1.12 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- “Acopaquia.jpg” by Desherinka is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Patel, Miao, Yetiskul, and Majmundar and is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- “Obstruction ventilation apnée sommeil.svg” by Habib M’henni is in the Public Domain. ↵
- This work is derivative of "aid611002-v4-728px-Live-With-Chronic-Obstructive-Pulmonary-Disease-Step-8.jpg" by unknown and is licensed under CC BY-NC-SA 3.0. Access for free at https://www.wikihow.com/Live-With-Chronic-Obstructive-Pulmonary-Disease ↵
- This work is a derivative of StatPearls by Nguyen and Duong and is licensed under CC BY 4.0 ↵
- COPD Foundation. (2020, April 17). Breathing techniques [Video]. YouTube. All rights reserved. https://youtu.be/ZJPJjZRHmy8 ↵
- “Incentive Spirometer.pngsommeil.svg” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- Cleveland Clinic. (2018, May 2). Incentive spirometer. https://my.clevelandclinic.org/health/articles/4302-incentive-spirometer ↵
- “Flutter Valve Breathing Device 3I3A0982.jpg” by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- NHS University Hospitals Plymouth Physiotherapy. (2015, May 12). Acapella [Video]. YouTube. All rights reserved. https://youtu.be/XOvonQVCE6Y ↵
An estimated oxygenation level based on the saturation level of hemoglobin measured by a pulse oximeter.
A sample of arterial blood that measures the oxygen, carbon dioxide, and bicarbonate levels.
The partial pressure of dissolved oxygen in the blood measured by arterial blood gas samples.
Preventing medication errors has been a key target for improving safety since the 1990s. Despite error reduction strategies, implementing new technologies, and streamlining processes, medication errors remain a significant concern with error rates of 8%-25% during medication administration.[1] Furthermore, a substantial proportion of errors occur in hospitalized children due to the complexity of weight-based pediatric dosing.[2]
Several prevention initiatives have been developed to ensure safe medication administration such as the following strategies[3]:
- Routinely checking the rights of medication administration
- Standardizing communication such as "tall man lettering," alerts to "look alike-sound alike" drug names, avoidance of abbreviations, and standards for expressing numerical dosages
- Focusing on high-alert medications that have a higher likelihood of resulting in patient harm if involved in an administration error, such as anticoagulants, insulins, opioids, and chemotherapy agents
- Standardizing labelling of medication using visual cues as safeguards
- Optimizing nursing workflow to minimize errors, such as minimizing interruptions and double checking high alert medications
- Implementing technology like barcode medication administration and smart infusion pumps
Read the article "Medication Administration Errors" on the Agency of Healthcare Research and Quality (AHRQ) website.[4]
The Joint Commission's National Patient Safety Goals related to mediation administration were previously discussed in the "Legal Foundations and National Guidelines for Safe Medication Administration" section of this chapter. This section will further discuss additional safety initiatives established by the Institute of Medicine (IOM), World Health Organization (WHO), Institute for Safe Medication Practices (ISMP), and Quality and Safe Education for Nurses (QSEN) to prevent medication errors.
Institute of Medicine
To Err is Human: Building a Safer Health System Report
The national focus on reducing medical errors has been in place since the 1990s. The Institute of Medicine (IOM) released a historic report in 1999 titled To Err is Human: Building a Safer Health System. The report stated that errors caused between 44,000 and 98,000 deaths every year in American hospitals and over one million injuries. The IOM report called for a 50% reduction in medical errors over five years. Its goal was to break the cycle of inaction regarding medical errors by advocating for a comprehensive approach to improving patient safety. The IOM 1999 report changed the focus of patient safety from dispensing blame to improving systems.[5]
Preventing Medication Errors Report
In 2007 the IOM published a follow-up report titled Preventing Medication Errors, reporting that more than 1.5 million Americans are injured every year in American hospitals, and the average hospitalized client experiences at least one medication error each day. This report emphasized actions that health care systems, providers, funders, and regulators could take to improve medication safety. These recommendations included actions such as having all U.S. prescriptions written and dispensed electronically, promoting widespread use of medication reconciliation, and performing additional research on drug errors and their prevention. The report also emphasized actions that client can take to prevent medication errors, such as maintaining active medication lists and bringing their medications to appointments for review.[6]
The Preventing Medication Errors report included specific actions for nurses to improve medication safety. The box below summarizes key actions.[7]
Improving Medication Safety: Actions for Nurses
- Establish safe work environments for medication preparation, administration, and documentation; for instance, reduce distractions and provide appropriate lighting.
- Maintain a culture of rigorous commitment to principles of safety in medication administration (for example, consistently checking the rights of medication administration and also performing double checks with colleagues as recommended).
- Remove barriers and facilitate the involvement of client surrogates in checking the administration and monitoring the medication effects.
- Foster a commitment to clients’ rights as co-consumers of their care.
- Develop aids for clients or their surrogates to support self-management of medications.
- Enhance communication skills and team training to be prepared and confident in questioning medication orders and evaluating client responses to drugs.
- Actively advocate for the development, testing, and safe implementation of electronic health records.
- Work to improve systems that address "near misses" in the work environment.
- Realize they are part of a system and do their part to evaluate the efficacy of new safety systems and technology.
- Contribute to the development and implementation of error reporting systems and support a culture that values accurate reporting of medication errors.
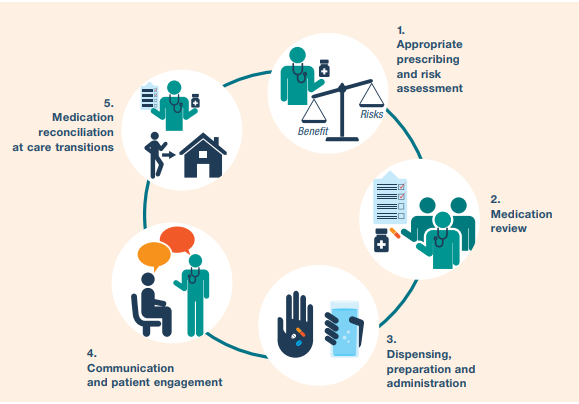
World Health Organization: Medication Without Harm
In 2019, the World Health Organization (WHO) identified “Medication Without Harm” as the theme for the third Global Patient Safety Challenge with the goal of reducing severe, avoidable medication-related harm by 50% over the next five years. As part of the Global Patient Safety Challenge: Medication Without Harm, the WHO has prioritized three areas to protect clients from harm while maximizing the benefit from medication[8]:
- Medication safety in high-risk situations
- Medication safety in polypharmacy
- Medication safety in transitions of care
Read more information about the WHO initiative called Medication Without Harm.
View the follow YouTube video explaining how to avoid harm from medications.
Medication Without Harm[9]
A summary of strategies to reduce harm and ensure medication safety is provided in Figure 2.3.[10]
Medication Safety in High-Risk Situations
The first priority of the WHO Medications Without Harm initiative, medication safety in high-risk situations, includes the components of high-risk medications, provider-client relations, and systems factors.
High-Risk (High-Alert) Medications
High-risk medications are drugs that bear a heightened risk of causing significant client harm when they are used in error.[11]
High-risk medication can be remembered using the mnemonic “A PINCH.” The information in the box below describes these medications included with the “A PINCH” mnemonic.
High-Risk Medication Group Examples of Medication
A: Anti-infective Amphotericin, aminoglycosides
P: Potassium & other electrolytes Injections of potassium & other electrolytes
I: Insulin All types of insulin
N: Narcotics & other sedatives Opioids, such as morphine; Benzodiazepines
C: Chemotherapeutic agents Methotrexate and vincristine
H: Heparin & anticoagulants Warfarin and enoxaparin
Note: Based on research, the Institute of Safe Medication Practices (ISMP) has expanded this list of high-risk medications. The updated list can be viewed in the box below.
Strategies for safe administration of high-alert medication include the following:
- Standardizing the ordering, storage, preparation, and administration of these products
- Improving access to information about these drugs
- Employing clinical decision support and automated alerts
- Using redundancies such as automated or independent double-checks when necessary
Provider-Patient Relations
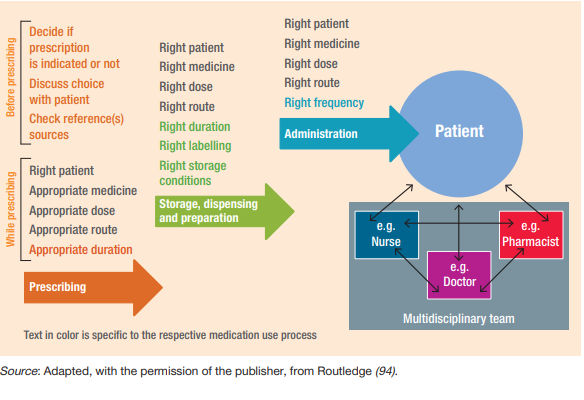
In addition to high-risk medications, a second component of medication safety in high-risk situations includes provider and client factors. This component relates to either the health care professional providing care or the client being treated. Even the most dedicated health care professional is fallible and can make errors. The act of prescribing, dispensing, and administering a medicine is complex and involves several health care professionals. The client should be the center of what should be a "prescribing partnership."[12] See Figure 2.4 for an illustration of the prescribing partnership.[13]
Life Span Considerations
Other risk factors can exist in specific clients across the life span. For example, adverse drug events occur most often at the extremes of life (in the very young and very old). In the older adult population, frail clients are likely to receive several medications concurrently, which adds to the risk of adverse drug events. In addition, the harm of some of these medication combinations may be synergistic, meaning the risk is greater when medications are taken together than the sum of the risks of individual agents. In neonates (particularly premature neonates), elimination routes through the kidney or liver may not be fully developed. The very young and very old are also less likely to tolerate adverse drug reactions, either because their homeostatic mechanisms are not yet fully developed, or they may have deteriorated. Medication errors in children, where doses may have to be calculated in relation to body weight or age, are also a source of major concern. Additionally, certain medical conditions predispose clients to an increased risk of adverse drug reactions, particularly renal or hepatic dysfunction and cardiac failure. Interprofessional strategies to address these potential harms are based on a systems approach with a "prescribing partnership" between the client, the prescriber, the pharmacist, and the nurse that includes verifying orders when concerns exist.
Systems Factors
In addition to high-risk medications and provider-patient relations, systems factors also contribute to medication safety in high-risk situations. Systems factors can contribute to error-provoking conditions for several reasons. The unit may be busy or understaffed, which can contribute to inadequate supervision or failure to remember to check important information. Interruptions during critical processes (e.g., administration of medicines) can also occur, which can have significant implications for patient safety. Tiredness and the need to multitask when busy or flustered can also contribute to error and can be compounded by poor electronic medical record design. Preparing and administering intravenous medications are also particularly error prone. Strategies for reducing errors include checking at each step of the medication administration process; preventing interruptions; using electronic provider order entry; and utilizing prescribing assessment tools, such as the Beers Criteria, to evaluate for potentially inappropriate medication use in older adults.[14] The Beers Criteria is a list of potentially harmful medications or medications with side effects that outweigh the benefit of taking the medication.
Read additional information about the updated Beers Criteria by the American Geriatrics Society.
Medication Safety in Polypharmacy
The second priority of the WHO Medications Without Harm initiative relates to medication safety in polypharmacy. Polypharmacy is the concurrent use of multiple medications. Although there is no standard definition, polypharmacy is often defined as the routine use of five or more medications including over-the-counter, prescription, and complementary medicines.
As people age, they are more likely to suffer from multiple chronic illnesses and take multiple medications. It is essential to use a person-centered approach to ensure their medications are appropriate to gain the most benefits without harm and to ensure the client is part of the decision-making process. Appropriate polypharmacy is present when all medicines are prescribed for the purpose of achieving specific therapeutic objectives that have been agreed with the client; therapeutic objectives are actually being achieved or there is a reasonable chance they will be achieved in the future; medication therapy has been optimized to minimize the risk of adverse drug reactions; and the client is motivated and able to take all medicines as intended.
Inappropriate polypharmacy is present when one or more medications are prescribed that are no longer needed. One or more medications may no longer be needed because there is no evidence-based indication, the indication has expired or the dose is unnecessarily high, they fail to achieve the therapeutic objectives they were intended to achieve, one or the combination of several medications put the client at a high risk of adverse drug reactions, or the client is not willing or able to take the medications as intended.[15]
When clients transition across health care settings, medication review by nurses is essential to prevent harm caused by inappropriate polypharmacy. [16]
Review questions to address during a medication review in Chapter 2 of WHO's Medication Safety in Polypharmacy Technical Report.[17]
Medication Safety in Transitions of Care
The third priority of the WHO Medications Without Harm initiative relates to medication safety during transitions of care. View the interactive activity below to see how medications are reconciled during transitions of care from admission to discharge in a hospital setting.
Interactive Activity
"Medication Reconciliation Process" by E. Christman for Open RN is licensed under CC BY 4.0
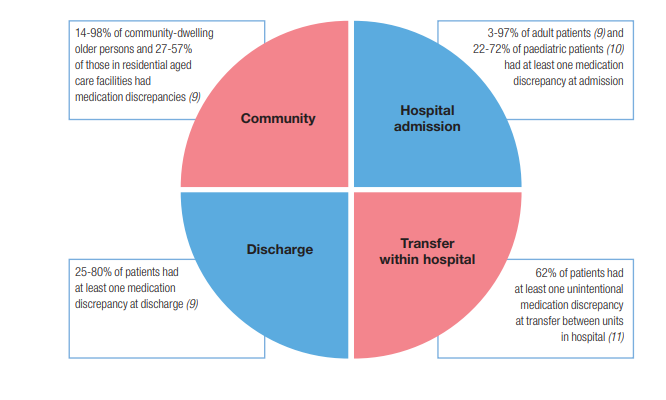
Medication errors can occur during transitions across settings. Figure 2.5[18] is an image from the World Health Organization showing ranges of percentage of errors that occur during common transitions of care.
Key strategies for improving medication safety during transitions of care include the following:
- Implementing formal structured processes for medication reconciliation at all transition points of care. Steps of effective medication reconciliation are to build the best possible medication history by interviewing the client and verifying with at least one reliable information source, reconciling and updating the medication list, and communicating with the client and future health care providers about changes in their medications.
- Partnering with clients, families, caregivers, and health care professionals to agree on treatment plans, ensuring clients are equipped to manage their medications safely, and ensuring clients have an up-to-date medication list.
- Where necessary, prioritizing clients at high risk of medication-related harm for enhanced support such as post-discharge contact by a nurse.[19]
Critical Thinking Activity 2.5a
A nurse is performing medication reconciliation for an elderly client admitted from home. The client does not have a medication list and cannot report the names, dosages, and frequencies of the medication taken at home.
What other sources can the nurse use to obtain medication information?
Note: Answers to the Critical Thinking activities can be found in the “Answer Key” section at the end of the book.
Institute for Safe Medication Practices
The Institute for Safe Medication Practices (ISMP) is respected as the gold standard for medication safety information. It is a nonprofit organization devoted entirely to preventing medication errors. ISMP collects and analyzes thousands of medication error and adverse event reports each year through its voluntary reporting program and then issues alerts regarding errors happening across the nation. The ISMP has established several prevention strategies for safe medication administration, including lists of high-alert medications, error-prone abbreviations to avoid, do not crush medications, look-alike and sound-alike drugs, and error-prone conditions that lead to error by nurses and student nurses. Each of these initiatives is further described below.[20]
Error-Prone Abbreviations
ISMP's List of Error-Prone Abbreviations, Symbols, and Dose Designations contains abbreviations, symbols, and dose designations that have been reported through the ISMP National Medication Errors Reporting Program as being frequently misinterpreted and involved in harmful medication errors. These abbreviations, symbols, and dose designations should never be used when communicating medical information. Note that this list has additional abbreviations than those contained in The Joint Commission's Do Not Use List of Abbreviations. Review the information below for the ISMP list of error-prone abbreviations to avoid. Some examples of abbreviations that were commonly used that should now be avoided are qd, qod, qhs, BID, QID, D/C, subq, and APAP.[21]
Strategies to avoid mistakes related to error-prone abbreviations include not using these abbreviations in medical documentation. Furthermore, if a nurse receives a prescription containing an error-prone abbreviation, it should be clarified with the provider and the order rewritten without the abbreviation.
Download the ISMP List of Error-Prone Abbreviations to Avoid PDF.
Do Not Crush List
The IMSP maintains a list of oral dosage medication that should not be crushed, commonly referred to as the “Do Not Crush” list. These medications are typically extended-release formulations.[22] Strategies for preventing harm related to oral medication that should not be crushed include requesting an order for a liquid form or a different route if the client cannot safely swallow the pill form.
Look-Alike and Sound-Alike (LASA) Drugs
ISMP maintains a list of drug names containing look-alike and sound-alike name pairs such as Adderall and Inderal. These medications require special safeguards to reduce the risk of errors and minimize harm.
Safeguards may include the following:
- Using both the brand and generic names on prescriptions and labels
- Including the purpose of the medication on prescriptions
- Changing the appearance of look-alike product names to draw attention to their dissimilarities
- Configuring computer selection screens to prevent look-alike names from appearing consecutively[23]
Download the ISMP's List of Confused Drug Names PDF.
Error-Prone Conditions That Lead to Student Nurse Related Error
When analyzing errors involving student nurses reported to the USP-ISMP Medication Errors Reporting Program and the PA Patient Safety Reporting System, it appears that many errors arise from a distinct set of error-prone conditions or medications. Some student-related errors are similar in origin to those that seasoned licensed health care professionals make, such as misinterpreting an abbreviation, misidentifying drugs due to look-alike labels and packages, misprogramming a pump due to a pump design flaw, or simply making a mental slip when distracted. Other errors stem from system problems and practice issues that are rather unique to environments where students and hospital staff are caring together for clients. View the list of error-prone conditions that should be avoided using the following box.
Critical Thinking Activity 2.5b
A nurse is preparing to administer insulin to a client. The nurse is aware that insulin is a medication on the ISMP list of high-alert medications.
What strategies should the nurse implement to ensure safe administration of this medication to the client?
Note: Answers to the Critical Thinking activities can be found in the “Answer Key” section at the end of the book.
Quality and Safety Education for Nurses
The Quality and Safety Education for Nurses (QSEN) project's vision is to “inspire health care professionals to put quality and safety as core values to guide their work.” QSEN began in 2005 and is funded by the Robert Wood Johnson Foundation. Based on the Institute of Medicine (2003) competencies for nursing, QSEN further defined these quality and safety competencies for educating nursing students:
- Patient-Centered Care
- Teamwork & Collaboration
- Evidence-Based Practice
- Quality Improvement
- Safety
- Informatics[24]
View the QSEN website.
Below are supplementary QSEN learning resources related to patient safety and preventing errors during medication administration.
The Josie King Story and Medical Errors[25]
Summary of Nursing Considerations for Safe and Effective Medication Administration
Medication administration by nurses is not just a task on a daily task list; it is a system-wide process in collaboration with other health care team members to ensure safe and effective treatment. As part of the medication administration process, the nurse must consider ethics, laws, national guidelines, and cultural/social determinants before administering medication to a client. The nurse is the vital “last stop” for preventing errors and potential harm from medications before they reach the client. A list of nursing considerations whenever administering medications is outlined below.
Nursing Considerations for Safe and Effective Medication Administration
BEFORE Administering Medication
Ethics
- Will this medication do more good than harm for this client at this point in time?
- Has the client (or the client's decision maker) had a voice in the decision-making process regarding use of this medication? Have they been informed about this medication and the potential risks/benefits to consider?
- If there are any ethical concerns, advocate for client rights and autonomy and contact the provider and/or pursue the proper chain of command.
Laws and National Guidelines
- Be sure the prescription/order contains the proper information according to CMS guidelines.
- Are there any FDA Boxed Warnings for this drug? If so, is the client aware of the risks and what to do if they occur? This discussion should be documented.
- Is this a controlled substance? If so, follow guidelines and agency policy for controlled substances in terms of counting, wasting, and disposal. For prescriptions for outpatient use, advocate that Prescription Drug Monitoring Program guidelines are followed.
- Be aware of signs of drug diversion in other health care team members and follow up appropriately in the chain of command. You can also directly submit an online tip to the DEA at Rx Abuse Online Reporting.
- Follow the Joint Commission “SPEAK UP” guidelines if you have any concerns about the safe use of this medication, including, but not limited to:
- Unclear or “do not use” abbreviations
- Strategies for look alike-sound alike medications
- Any other concerns for error
- Follow your state's practice act regarding Scope of Practice and Rules of Conduct. Is administering this medication appropriate for your scope of practice and for this client? If not, protect your client from harm and your nursing license by notifying the appropriate contacts within your agency.
- Is this medication administration occurring during a transition of care from unit to unit, home to agency, or in preparation for discharge? If so, be sure proper medication reconciliation has been completed.
DURING Administration
- Use the nursing process as you ASSESS if this drug is appropriate to administer at this time and PLAN continued monitoring. Consider life span and disease process implications. If you NOTICE any findings that this medication may not be appropriate at this time for this client, withhold the medication and contact the provider.
- Assess if there are any cultural or social determinants that will impact the client's ability to use these medications safely and effectively. IMPLEMENT appropriate accommodations as needed and notify the provider.
- Follow The Joint Commission's National Patient Safety Goals as you correctly identify the client and follow guidelines to use medicines safely.
- If this is a high-alert medication, follow recommendations for safe administration (such as adding a second RN check, etc.).
- Reduce distractions in your environment as you prepare and administer medications.
- Do not crush medications unless safe to do so.
- Follow standards set by The Joint Commission and CMS:
- Checking rights of medication administration before administering any medication to a client
- Educate the client about their medication
- Dispose of unused controlled substances appropriately
- Document appropriately
AFTER Administration
- Continue to EVALUATE the client for potential side effects/adverse effects, as well as therapeutic effects of the medications.
- Document and verbally share your findings during handoff reports for safe continuity of care.
- If an error occurs, file an incident report and participate in root cause analysis to determine how to prevent it from happening again.
Bicarbonate level reflected in arterial blood gas results. Normal range is 22-26 meq/L.
Calculated arterial oxygen saturation level.
A reduced level of tissue oxygenation.
Decreased levels of oxygen in the blood.
A bluish discoloration of the skin, lips, and nail beds. It is an indication of decreased perfusion and oxygenation.
Increased carbon dioxide levels in the blood.
A feeling of shortness of breath.
A change in the configuration where the tips of the nails curve around the fingertips, usually caused by chronic low levels of oxygen in the blood.
Fraction of inspired oxygen (i.e. the concentration of oxygen inhaled). Room air contains 21% oxygen levels, and oxygenation devices can increase the inhaled concentration of oxygen up to 100%. However, FiO2 levels should be decreased as soon as feasible to do so to prevent lung injury.
OSA is characterized by repeated occurrences of complete or partial obstructions of the upper airway during sleep, resulting in apneic episodes.

