Ethical and Professional Foundations of Safe Medication Administration by Nurses
Open Resources for Nursing (Open RN)
The American Nurses Association (ANA) is a professional organization that represents the interests of the nation’s four million registered nurses and is at the forefront of improving the quality of health care for all.[1] The ANA establishes ethical and professional standards for nurses that also guide safe administration of medications. These code of ethics and professional standards are described in ANA publications titled Code of Ethics for Nurses and Nursing: Scope and Standards of Practice.
Code of Ethics for Nurses
The ANA developed the Code of Ethics for Nurses as a guide for carrying out nursing responsibilities in a manner consistent with quality in nursing care and the ethical obligations of the profession.[2] Several provisions from the Code of Ethics impact how nurses should administer medication in an ethical manner. A summary of each provision from the Code of Ethics and how it pertains to medication administration is outlined below:
- Provision 1 focuses on respect for human dignity and the right for self-determination: “The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person.”
- Provision 2 states, “The nurse’s primary commitment is to the client…”[3] In health care settings, nurses often experience several competing loyalties, such as to their employer, to the doctor(s), to their supervisor, or to others on the health care team. However, the client should always receive the primary commitment of the nurse. Additionally, the client has the right to accept, refuse, or terminate any treatment, including medications.
- Provision 3 states, “The nurse promotes, advocates for, and protects the rights, health, and safety of the patient…”[4] This provision includes a nurse’s responsibility to promote a culture of safety for clients. If errors occur, they must be reported, and nurses should ensure responsible disclosure of errors to clients. This also includes proper disclosure of questionable practices, such as drug diversion or impaired practice by any professional.
- Provision 4 involves authority, accountability, and responsibility by a nurse to follow legal requirements, such as state practice acts and professional standards of care.
- Provision 5 includes the responsibility of the nurse to promote health and safety.
- Provision 6 focuses on virtues that make a nurse a morally good person. For example, nurses are held accountable to use their clinical judgment to avoid causing harm to clients (maleficence) and to do good (beneficence). When administering medications, nurses should validate the medication is doing more “good” than “harm” (adverse or side effects).
- Provision 7 focuses on a nurse practicing within the professional standards set forth by their state nurse practice act, as well as standards established by professional nursing organizations.
- Provision 8 explains that a nurse must address the social determinants of health, such as poverty, education, safe medication, and health care disparities.[5]
Whenever a nurse provides client care, the ANA’s Code of Ethics should be used as a guide for professional ethical behavior.
View the ANA’s Code of Ethics for Nurses.
Critical Thinking Activity 2.2a
A nurse is preparing to administer medications to a client. While reviewing the chart, the nurse notices two medications with similar mechanisms of action have been prescribed by two different providers.
What is the nurse’s best response?
Note: Answers to the Critical Thinking activities can be found in the “Answer Key” sections at the end of the book.
Standards and Scope of Practice
The ANA publishes Nursing: Scope and Standards of Practice. This resource establishes national standards for nurses and is updated regularly.[6]
The ANA defines the scope of nursing as “the protection, promotion, and optimization of health and abilities, prevention of illness and injury, facilitation of healing, alleviation of suffering through the diagnosis and treatment of human response, and advocacy in the care of individuals, families, groups, communities, and populations.” A registered nurse (RN) is defined as an individual who is educationally prepared and licensed by a state to practice as a registered nurse. Nursing practice is characterized by the following tenets[7]:
- Caring and health are central to the practice of the registered nurse.
- Nursing practice is individualized to the unique needs of the health care consumer.
- Registered nurses use the nursing process to plan and provide individualized care for health care consumers.
- Nurses coordinate care by establishing partnerships to reach a shared goal of delivering safe, quality health care.
The ANA establishes Standards of Practice and Standards of Professional Performance in the Nursing: Scope and Standards of Practice publication. State nurse practice acts further define the scope of practice of RNs and Licensed Practical Nurses/Vocational Nurses (LPNs/VNs) within each state. Nurse practice acts are further discussed in the “Legal Foundations and National Guidelines for Safe Medication Administration” section of this chapter.
The ANA’s Nursing: Scope and Standards of Practice publication can be purchased on the nursingworld.org website or borrowed from many libraries.
Standards of Practice
The ANA’s Standards of Practice are authoritative statements of duties that all registered nurses, regardless of role, population, or specialty, are expected to perform competently. Standards of Practice include assessment, diagnosis, outcome identification, planning, implementation, and evaluation (ADOPIE) components of providing client care, also known as the “nursing process.” When nurses safely administer medication, all components of ADOPIE are addressed.
Assessment
The “Assessment” Standard of Practice is defined as, “The registered nurse collects pertinent data and information relative to the health care consumer’s health or the situation.”[8] A registered nurse uses a systematic method to collect and analyze client data. Assessment includes physiological data, as well as psychological, sociocultural, spiritual, economic, and lifestyle data. For example, when a nurse assesses multiple pieces of data for a hospitalized client with pain, this is considered part of a comprehensive pain assessment.
Diagnosis
The “Diagnosis” Standard of Practice is defined as, “The registered nurse analyzes the assessment data to determine actual or potential diagnoses, problems, and issues.”[9] A nursing diagnosis is the nurse’s clinical judgment about the client’s response to actual or potential health conditions or needs. Nursing diagnoses are used to create the nursing care plan and are different than medical diagnoses.[10]
Outcomes Identification
The “Outcomes Identification” Standard of Practice is defined as, “The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation.”[11] The nurse sets measurable and achievable short- and long-term goals and specific outcomes in collaboration with the client based on their assessment data and nursing diagnoses.
Planning
The “Planning” Standard of Practice is defined as, “The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes.”[12] Assessment data, diagnoses, and goals are used to select evidence-based nursing interventions customized to each client’s needs and concerns. Goals, expected outcomes, and nursing interventions are documented in the client’s nursing care plan so that nurses, as well as other health professionals, have access to it for continuity of care.[13]
Implementation
The “Implementation” Standard of Practice is defined as, “The nurse implements the identified plan.”[14] Nursing interventions are implemented or delegated to licensed practical nurses/vocational nurses (LPNs/VNs) or unlicensed assistive personnel (UAP) with supervision. Interventions are also documented in the client’s electronic medical record as they are completed.[15]
The “Implementation” Standard of Professional Practice also includes the subcategories “Coordination of Care” and “Health Teaching and Health Promotion” to promote health and a safe environment.[16]
Coordination of Care
The ANA standard for coordination of care states, “The registered nurse coordinates care delivery.”[17] When ensuring medications are administered safely, the nurse collaborates with the client and the interprofessional health care team to meet mutually agreed upon outcomes. The nurse also engages the client in self-care to achieve their preferred goals for quality of life. For example, one client with chronic pain may have a pain management goal of “5” with their quality of life preference of having the ability to participate in social activities with friends but not experiencing burdensome side effect of medication. Another client with chronic pain may have a pain management goal of “0” with a quality of life preference of having no pain no matter what the side effects. The nurse advocates for these clients’ goals and preferences with the interprofessional team.
Nurses also serve vital roles in ensuring safe transitions and continuity of care regarding clients’ use of medications. Additional information about safe medication use and transitions of care is discussed in the “Preventing Medication Errors” section of this chapter.
Health Teaching and Health Promotion
When administering medications, nurses teach clients about the medications and potential side effects to promote optimal health. The ANA standard for health teaching and health promotion states, “The registered nurse employs strategies to teach and promote health and wellness.”[18] Specific behaviors related to teaching about medication are as follows[19]:
- Use health teaching and health promotion methods in collaboration with the client’s values, beliefs, health practices, developmental level, learning needs, readiness and ability to learn, language preference, spirituality, culture, and socioeconomic status.
- Provide clients with information and education about intended effects and potential adverse effects of the plan of care.
- Provide anticipatory guidance to clients to promote health and prevent or reduce risk.
In the book Preventing Medication Errors by the Institute of Medicine (2007), the following are additional key national guidelines when teaching clients about safe use of their medications:
- Clients should maintain an active list of all prescription drugs, over-the-counter (OTC) drugs, and dietary supplements they are taking, the reasons for taking them, and any known drug allergies. Every provider involved in the medication-use process for a client should have access to this list.
- Clients should be provided information about side effects, contraindications, methods for handling adverse reactions, and sources for obtaining additional objective, high-quality information.[20]
Evaluation
The “Evaluation” Standard of Practice is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.”[21] During evaluation, nurses assess the client and compare the findings against the initial assessment to determine the effectiveness of the interventions and overall nursing care plan. Both the client’s status and the effectiveness of the nursing care must be continuously evaluated and modified as needed.[22]
Read additional information about the nursing process in the “Nursing Process” chapter of Open RN Nursing Fundamentals.
Standards of Professional Performance
ANA’s Standards of Professional Performance describe a competent level of behavior for nurses, including activities related to ethics, culturally congruent practice, communication, collaboration, leadership, education, evidence-based practice, and quality of practice.[23]
The ANA defines culturally congruent practice as the application of evidence-based nursing that is in agreement with the preferred cultural values, beliefs, worldview, and practices of the health care consumer and other stakeholders. Cultural competence represents the process by which nurses demonstrate culturally congruent practice. Nurses must assess the cultural beliefs and practices of their clients and implement culturally congruent interventions when administering medications and teaching about them. Additional information about cultural implications for medication administration is further discussed in the “Cultural and Social Determinants Related to Medication Administration” section later in this chapter.
Critical Thinking Activity 2.2b
A nurse is preparing to administer metoprolol, a cardiac medication, to a client and implements the nursing process:
ASSESSES the vital signs prior to administration and discovers the heart rate is 48.
DIAGNOSES that the heart rate is too low to safely administer the medication per the parameters provided. Establishes the OUTCOME to keep the client’s heart rate within normal range of 60-100.
PLANS to call the provider, as well as report this incident in the shift handoff report.
Implements INTERVENTIONS by withholding the metoprolol at this time, documenting the incident that the medication is withheld, and notifying the provider.
Continues to EVALUATE the client status throughout the shift after not receiving the metoprolol.
The nurse is providing health teaching to a client about the medication before discharge. The nurse provides a handout with instructions, as well as a list of the current medications.
What other information should be provided to the client?
Note: Answers to the Critical Thinking activities can be found in the “Answer Key” sections at the end of the book.
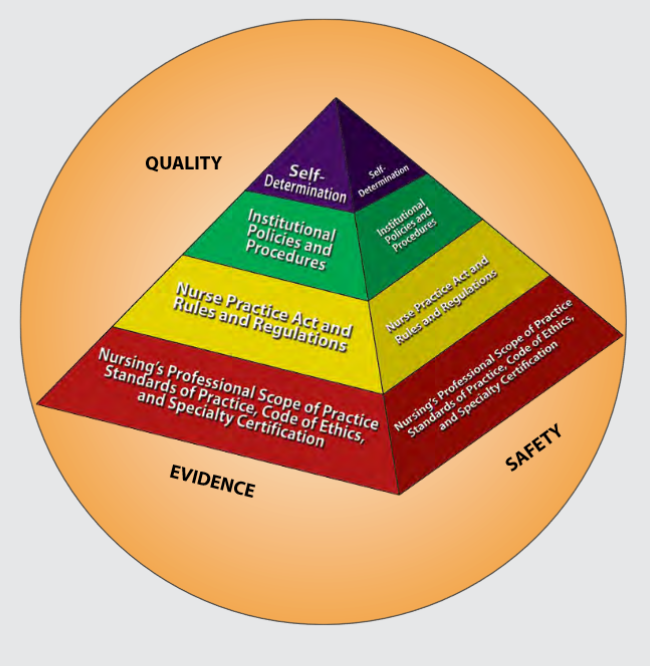
Figure 2.1 is an image from Nursing: Scope and Standards of Practice by the ANA that illustrates how the scope of practice, standards of practice, and code of ethics form the “base” of nursing practice.[24] Nursing practice is further guided by the Nurse Practice Act in the state in which a nurse works, federal and state rules and regulations, institutional policies and procedures, and self-determination by the individual nurse. All these components are required to provide quality, safe client care that is evidence-based. These components will be further discussed in the remaining sections of this chapter.
NCLEX and the Clinical Judgment Model
The National Council Licensure Examination (NCLEX) is the national exam that graduates must pass successfully to obtain their nursing license after graduating from a nursing program of study. The NCLEX-PN is taken to become a licensed practical/vocational nurse (LPN/VN), and the NCLEX-RN is taken to become a licensed registered nurse (RN). The purpose of the NCLEX is to evaluate if a nursing graduate demonstrates the ability to provide safe, competent, entry-level nursing care. The NCLEX is developed by the National Council of State Boards of Nursing (NCSBN), an independent, nonprofit organization composed of the 50 state boards of nursing and other regulatory agencies.[25]
A new edition of the NCLEX was launched in April 2023 that contains “Next Generation” questions. The Next Generation NCLEX (NGN) assesses how well the candidate can think critically and use clinical judgment. The NCSBN defines clinical judgment as “the observed outcome of critical thinking and decision-making. It is an iterative process with multiple steps that uses nursing knowledge to observe and assess presenting situations, identify a prioritized client concern and generate the best possible evidence-based solutions in order to deliver safe client care.”
The NCLEX uses the NCSBN’s Clinical Judgment Measurement Model (NCJMM) to assess the candidate’s ability to use safe clinical judgment when providing nursing care. Exam questions used to assess clinical judgment may be contained in a case study or as individual stand-alone items. A case study contains six questions that are associated with the same client scenario and addresses the following steps in clinical judgment[26]:
- Recognize cues: Identify relevant and important information from different sources (e.g., medical history, vital signs).
- Analyze cues: Organize and connect the recognized cues to the client’s clinical presentation.
- Prioritize hypotheses: Evaluate and prioritize hypotheses (based on urgency, likelihood, risk, difficulty, time constraints, etc.).
- Generate solutions: Identify expected outcomes and use hypotheses to define a set of interventions for the expected outcomes.
- Take action: Implement the solution(s) that address the highest priority.
- Evaluate outcomes: Compare observed outcomes to expected outcomes.
Throughout this book, learning activities are provided to assist students in learning how to apply the nursing process (i.e., ANA’s Standards of Care) to answer NGN-style questions that evaluate clinical judgment. Some of these activities are written, with answers in the Answer Key at the end of the book, and others are interactive and require use of the online book.
Media Attributions
- ORN-Icons_lightbulb-300×300-1
- American Nurses Association. (2019). About ANA. https://www.nursingworld.org/ana/about-ana/ ↵
- American Nurses Association. (2015). Code of ethics for nurses with interpretive statements. https://www.nursingworld.org/coe-view-only ↵
- American Nurses Association. (2015). Code of ethics for nurses with interpretive statements. https://www.nursingworld.org/coe-view-only ↵
- American Nurses Association. (2015). Code of ethics for nurses with interpretive statements. https://www.nursingworld.org/coe-view-only ↵
- American Nurses Association. (2015). Code of ethics for nurses with interpretive statements. https://www.nursingworld.org/coe-view-only ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (3rd ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.) The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- Institute of Medicine. (2007). Preventing medication errors. The National Academies Press. https://doi.org/10.17226/11623 ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2015). Nursing: Scope and standards of practice (3rd ed.). American Nurses Association. ↵
- NCSBN. https://www.ncsbn.org/nclex.htm ↵
- NCSBN. (n.d.). 2023 NCLEX-RN test plan. https://www.ncsbn.org/exams/testplans.page ↵
A True Story of a New Nurse’s Introduction to Ethical Dilemmas
A new nurse graduate meets Mary, a 70-year-old woman who was living alone at home with Amyotrophic Lateral Sclerosis (ALS or also referred to as “Lou Gehrig’s disease”). Mary’s husband died many years ago and they did not have children. She had a small support system, including relatives who lived out of state and friends with whom she had lost touch since her diagnosis. Mary was fiercely independent and maintained her nutrition and hydration through a gastrostomy tube to avoid aspiration.
As Mary’s disease progressed, the new nurse discussed several safety issues related to Mary living alone. As the new nurse shared several alternative options related to skilled nursing care with Mary, Mary shared her own plan. Mary said her plan included a combination of opioids, benzodiazepines, and a plastic bag to suffocate herself and be found by a nurse during a scheduled visit. In addition to safety issues and possible suicide ideation, the new nurse recognized she was in the midst of an ethical dilemma in terms of the treatment plan, her values and what she felt was best for Mary, and Mary’s preferences.
Applying the MORAL Ethical Decision-Making Model to Mary’s Case
| Massage the Dilemma | Data: Mary lives alone and does not want to go to a nursing home. She lacks social support. She has a progressive and incurable disease that affects her ability to swallow, talk, walk, and eventually breathe. She has made statements to staff indicating she prefers to die rather than leave her home to receive total care in a long-term care setting.
Ethical Conflicts: According to the deontological theory, suicide is always wrong. According to the consequentialism ethical theory, an action's morality depends on the consequences of that action. Mary has a progressive, incurable illness that requires total care that will force her to leave the home. She wishes to stay in her home until she dies. Ethical Goals: To honor Mary’s dignity and respect her autonomy in making treatment decisions. For Mary to experience a “good” death as she defines it, and neither hasten nor prolong her dying process through illegal or amoral interventions. |
|---|---|
| Outline the Options |
|
| Review Criteria and Resolve | Mary was assessed to be rational and capable of decision-making by a psychiatrist. Mary defined a “good” death as one occurring in her home and not in a hospital or long-term care setting. Mary did not want her life to be prolonged through the use of technology such as a ventilator.
Resolution: Mary elected to discontinue tube feeding and limit hydration to only that necessary for medication to provide comfort care and symptom management. |
| Affirm Position and Act | Although some health care members did not personally believe in discontinuing food and fluids through the g-tube based on their interpretation of the deontological ethical theory, Mary’s decision was acceptable both legally and ethically, based on the consequentialism ethical theory that the decision best supported Mary’s goals and respected her autonomy.
Daily visits were scheduled with hospice staff, including the nurse, nursing assistant, social worker, chaplain, and volunteers. Hired caregivers supplemented visits and in the last couple of days were scheduled around the clock. Mary died comfortably in her bed seven days after implementation of the agreed-upon plan. |
| Look Back | The health care team evaluated what happened during Mary’s situation and what could be learned from this ethical dilemma and applied to future patient-care scenarios. |
A True Story of a New Nurse’s Introduction to Ethical Dilemmas
A new nurse graduate meets Mary, a 70-year-old woman who was living alone at home with Amyotrophic Lateral Sclerosis (ALS or also referred to as “Lou Gehrig’s disease”). Mary’s husband died many years ago and they did not have children. She had a small support system, including relatives who lived out of state and friends with whom she had lost touch since her diagnosis. Mary was fiercely independent and maintained her nutrition and hydration through a gastrostomy tube to avoid aspiration.
As Mary’s disease progressed, the new nurse discussed several safety issues related to Mary living alone. As the new nurse shared several alternative options related to skilled nursing care with Mary, Mary shared her own plan. Mary said her plan included a combination of opioids, benzodiazepines, and a plastic bag to suffocate herself and be found by a nurse during a scheduled visit. In addition to safety issues and possible suicide ideation, the new nurse recognized she was in the midst of an ethical dilemma in terms of the treatment plan, her values and what she felt was best for Mary, and Mary’s preferences.
Applying the MORAL Ethical Decision-Making Model to Mary’s Case
| Massage the Dilemma | Data: Mary lives alone and does not want to go to a nursing home. She lacks social support. She has a progressive and incurable disease that affects her ability to swallow, talk, walk, and eventually breathe. She has made statements to staff indicating she prefers to die rather than leave her home to receive total care in a long-term care setting.
Ethical Conflicts: According to the deontological theory, suicide is always wrong. According to the consequentialism ethical theory, an action's morality depends on the consequences of that action. Mary has a progressive, incurable illness that requires total care that will force her to leave the home. She wishes to stay in her home until she dies. Ethical Goals: To honor Mary’s dignity and respect her autonomy in making treatment decisions. For Mary to experience a “good” death as she defines it, and neither hasten nor prolong her dying process through illegal or amoral interventions. |
|---|---|
| Outline the Options |
|
| Review Criteria and Resolve | Mary was assessed to be rational and capable of decision-making by a psychiatrist. Mary defined a “good” death as one occurring in her home and not in a hospital or long-term care setting. Mary did not want her life to be prolonged through the use of technology such as a ventilator.
Resolution: Mary elected to discontinue tube feeding and limit hydration to only that necessary for medication to provide comfort care and symptom management. |
| Affirm Position and Act | Although some health care members did not personally believe in discontinuing food and fluids through the g-tube based on their interpretation of the deontological ethical theory, Mary’s decision was acceptable both legally and ethically, based on the consequentialism ethical theory that the decision best supported Mary’s goals and respected her autonomy.
Daily visits were scheduled with hospice staff, including the nurse, nursing assistant, social worker, chaplain, and volunteers. Hired caregivers supplemented visits and in the last couple of days were scheduled around the clock. Mary died comfortably in her bed seven days after implementation of the agreed-upon plan. |
| Look Back | The health care team evaluated what happened during Mary’s situation and what could be learned from this ethical dilemma and applied to future patient-care scenarios. |
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activities are provided as immediate feedback.)
Ethical Application & Reflection Activity
Case A
Filmmaker Lulu Wang first shared a story about her grandmother on This American Life podcast and later turned it into the 2019 movie The Farewell starring Awkwafina. Both share the challenges of a Chinese-born but U.S.-raised woman returning to China and a family who has chosen to not disclose that the grandmother has been given a Stage IV lung cancer diagnosis and three months to live. Listen to the podcast and then answer the following questions:
585: In Defense of Ignorance Act One: What You Don't Know
1. Reflect on the similarities and differences of your family culture with that of the Billi family. Consider things such as what family gatherings, formal and informal, look like and spoken and unspoken rules related to communication and behavior.
2. The idea of “good” lies and “bad” lies is introduced in the podcast. Nai Nai’s family supports the decision to not tell her about her Stage IV lung cancer, stage a wedding as the excuse to visit and say their goodbyes, and even alter a medical report as good lies necessary to support her mental health, well-being, and happiness. Is the family applying deontological or utilitarian ethics to the situation? Defend your response.
3. Define the following ethical principles and identify examples from this story:
- Autonomy
- Beneficence
- Nonmaleficence
- Paternalism
4. Imagine this story is happening in the United States rather than China and you are the nurse admitting Nai Nai to an inpatient oncology unit. Using the ethical problem-solving model of your choice, identify and support your solution to the ethical dilemma posed when her family requests that Nai Nai not be told that she has cancer.
Ethical Application & Reflection Activity
Case B
You are caring for a 32-year-old client who has been in a persistent vegetative state for many years. There is an outdated advanced directive that is confusing on the issue of food and fluids, though clear about not wanting to be on a ventilator if she were in a coma. Her husband wants the feeding tube removed but is unable to say that it would have been the client’s wish. He says that it is his decision for her. Her two adult siblings and parents reject this as a possibility because they say that “human life is sacred” and that the daughter believed this. They say their daughter is alive and should receive nursing care, including feeding. The health care team does not know what to do ethically and fear being sued by either the husband, siblings, or the parents. What do you need to know about this clinical situation? What are the values and obligations at stake in this case? What values or obligations should be affirmed and why? How might that be done?
1. Define the problem.
2. List what facts/information you have.
3. What are the stakeholders' positions?
- Patient:
- Spouse:
- Family:
- Health Care Team:
- Facility:
- Community:
4. How might the stakeholders' values differ?
5. What are your values in this situation?
6. Do your values conflict with those of the patient? Describe.

Test your knowledge using this NCLEX Next Generation-style Case Study. You may reset and resubmit your answers to this question an unlimited number of times.[1]
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activities are provided as immediate feedback.)
Ethical Application & Reflection Activity
Case A
Filmmaker Lulu Wang first shared a story about her grandmother on This American Life podcast and later turned it into the 2019 movie The Farewell starring Awkwafina. Both share the challenges of a Chinese-born but U.S.-raised woman returning to China and a family who has chosen to not disclose that the grandmother has been given a Stage IV lung cancer diagnosis and three months to live. Listen to the podcast and then answer the following questions:
585: In Defense of Ignorance Act One: What You Don't Know
1. Reflect on the similarities and differences of your family culture with that of the Billi family. Consider things such as what family gatherings, formal and informal, look like and spoken and unspoken rules related to communication and behavior.
2. The idea of “good” lies and “bad” lies is introduced in the podcast. Nai Nai’s family supports the decision to not tell her about her Stage IV lung cancer, stage a wedding as the excuse to visit and say their goodbyes, and even alter a medical report as good lies necessary to support her mental health, well-being, and happiness. Is the family applying deontological or utilitarian ethics to the situation? Defend your response.
3. Define the following ethical principles and identify examples from this story:
- Autonomy
- Beneficence
- Nonmaleficence
- Paternalism
4. Imagine this story is happening in the United States rather than China and you are the nurse admitting Nai Nai to an inpatient oncology unit. Using the ethical problem-solving model of your choice, identify and support your solution to the ethical dilemma posed when her family requests that Nai Nai not be told that she has cancer.
Ethical Application & Reflection Activity
Case B
You are caring for a 32-year-old client who has been in a persistent vegetative state for many years. There is an outdated advanced directive that is confusing on the issue of food and fluids, though clear about not wanting to be on a ventilator if she were in a coma. Her husband wants the feeding tube removed but is unable to say that it would have been the client’s wish. He says that it is his decision for her. Her two adult siblings and parents reject this as a possibility because they say that “human life is sacred” and that the daughter believed this. They say their daughter is alive and should receive nursing care, including feeding. The health care team does not know what to do ethically and fear being sued by either the husband, siblings, or the parents. What do you need to know about this clinical situation? What are the values and obligations at stake in this case? What values or obligations should be affirmed and why? How might that be done?
1. Define the problem.
2. List what facts/information you have.
3. What are the stakeholders' positions?
- Patient:
- Spouse:
- Family:
- Health Care Team:
- Facility:
- Community:
4. How might the stakeholders' values differ?
5. What are your values in this situation?
6. Do your values conflict with those of the patient? Describe.

Test your knowledge using this NCLEX Next Generation-style Case Study. You may reset and resubmit your answers to this question an unlimited number of times.[2]
Advocacy: The act or process of pleading for, supporting, or recommending a cause or course of action. Advocacy may be for persons (whether an individual, group, population, or society) or for an issue, such as potable water or global health.[3]
Autonomy: The capacity to determine one’s own actions through independent choice, including demonstration of competence.[4]
Beneficence: The bioethical principle of benefiting others by preventing harm, removing harmful conditions, or affirmatively acting to benefit another or others, often going beyond what is required by law.[5]
Code of ethics: A set of ethical principles established by a profession that is designed to govern decision-making and assist individuals to distinguish right from wrong.
Consequentialism: An ethical theory used to determine whether or not an action is right by the consequences of the action. For example, most people agree that lying is wrong, but if telling a lie would help save a person’s life, consequentialism says it’s the right thing to do.
Cultural humility: A humble and respectful attitude towards individuals of other cultures and an approach to learning about other cultures as a lifelong goal and process.
Deontology: An ethical theory based on rules that distinguish right from wrong.
Ethical dilemma: Conflict resulting from competing values that requires a decision to be made from equally desirable or undesirable options.
Ethical principles: Principles used to define nurses’ moral duties and aid in ethical analysis and decision-making.[6] Foundational ethical principles include autonomy (self-determination), beneficence (do good), nonmaleficence (do no harm), justice (fairness), and veracity (tell the truth).
Ethics: The formal study of morality from a wide range of perspectives.[7]
Ethics committee: A formal committee established by a health care organization to problem-solve ethical dilemmas.
Fidelity: An ethical principle meaning keeping promises.
Institutional Review Board (IRB): A group that has been formally designated to review and monitor biomedical research involving human subjects.
Justice: A moral obligation to act on the basis of equality and equity and a standard linked to fairness for all in society.[8]
Moral conflict: Feelings occurring when an individual is uncertain about what values or principles should be applied to an ethical issue.[9]
Moral courage: The willingness of an individual to speak out and do what is right in the face of forces that would lead us to act in some other way.[10]
Moral distress: Feelings occurring when correct ethical action is identified but the individual feels constrained by competing values of an organization or other individuals.[11]
Moral injury: The distressing psychological, behavioral, social, and sometimes spiritual aftermath of exposure to events that contradict deeply held moral beliefs and expectations.
Morality: Personal values, character, or conduct of individuals or groups within communities and societies.[12]
Moral outrage: Feelings occurring when an individual witnesses immoral acts or practices they feel powerless to change.[13]
Morals: The prevailing standards of behavior of a society that enable people to live cooperatively in groups.[14]
Nonmaleficence: The bioethical principle that specifies a duty to do no harm and balances avoidable harm with benefits of good achieved.[15]
Paternalism: The interference by the state or an individual with another person, defended by the claim that the person interfered with will be better off or protected from harm.[16]
Utilitarianism: A type of consequentialism that determines whether or not actions are right based on their consequences, with the standard being achieving the greatest good for the greatest number of people.
Values: Individual beliefs that motivate people to act one way or another and serve as a guide for behavior.[17]
Veracity: An ethical principle meaning telling the truth.
Advocacy: The act or process of pleading for, supporting, or recommending a cause or course of action. Advocacy may be for persons (whether an individual, group, population, or society) or for an issue, such as potable water or global health.[18]
Autonomy: The capacity to determine one’s own actions through independent choice, including demonstration of competence.[19]
Beneficence: The bioethical principle of benefiting others by preventing harm, removing harmful conditions, or affirmatively acting to benefit another or others, often going beyond what is required by law.[20]
Code of ethics: A set of ethical principles established by a profession that is designed to govern decision-making and assist individuals to distinguish right from wrong.
Consequentialism: An ethical theory used to determine whether or not an action is right by the consequences of the action. For example, most people agree that lying is wrong, but if telling a lie would help save a person’s life, consequentialism says it’s the right thing to do.
Cultural humility: A humble and respectful attitude towards individuals of other cultures and an approach to learning about other cultures as a lifelong goal and process.
Deontology: An ethical theory based on rules that distinguish right from wrong.
Ethical dilemma: Conflict resulting from competing values that requires a decision to be made from equally desirable or undesirable options.
Ethical principles: Principles used to define nurses’ moral duties and aid in ethical analysis and decision-making.[21] Foundational ethical principles include autonomy (self-determination), beneficence (do good), nonmaleficence (do no harm), justice (fairness), and veracity (tell the truth).
Ethics: The formal study of morality from a wide range of perspectives.[22]
Ethics committee: A formal committee established by a health care organization to problem-solve ethical dilemmas.
Fidelity: An ethical principle meaning keeping promises.
Institutional Review Board (IRB): A group that has been formally designated to review and monitor biomedical research involving human subjects.
Justice: A moral obligation to act on the basis of equality and equity and a standard linked to fairness for all in society.[23]
Moral conflict: Feelings occurring when an individual is uncertain about what values or principles should be applied to an ethical issue.[24]
Moral courage: The willingness of an individual to speak out and do what is right in the face of forces that would lead us to act in some other way.[25]
Moral distress: Feelings occurring when correct ethical action is identified but the individual feels constrained by competing values of an organization or other individuals.[26]
Moral injury: The distressing psychological, behavioral, social, and sometimes spiritual aftermath of exposure to events that contradict deeply held moral beliefs and expectations.
Morality: Personal values, character, or conduct of individuals or groups within communities and societies.[27]
Moral outrage: Feelings occurring when an individual witnesses immoral acts or practices they feel powerless to change.[28]
Morals: The prevailing standards of behavior of a society that enable people to live cooperatively in groups.[29]
Nonmaleficence: The bioethical principle that specifies a duty to do no harm and balances avoidable harm with benefits of good achieved.[30]
Paternalism: The interference by the state or an individual with another person, defended by the claim that the person interfered with will be better off or protected from harm.[31]
Utilitarianism: A type of consequentialism that determines whether or not actions are right based on their consequences, with the standard being achieving the greatest good for the greatest number of people.
Values: Individual beliefs that motivate people to act one way or another and serve as a guide for behavior.[32]
Veracity: An ethical principle meaning telling the truth.
Learning Objectives
- Collaborate with interprofessional team members when providing client care
- Manage conflict among clients and health care staff
- Perform procedures necessary to safely admit, transfer, and/or discharge a client
- Assess the need for referrals and obtain necessary orders
- Describe how the health care team meets the needs of diverse patients in a variety of settings
- Identify strategies to ensure productive, effective team functioning
All health care students must prepare to deliberately work together in clinical practice with a common goal of building a safer, more effective, patient-centered health care system. The World Health Organization (WHO) defines interprofessional collaborative practice as multiple health workers from different professional backgrounds working together with patients, families, caregivers, and communities to deliver the highest quality of care.[33]
Effective teamwork and communication have been proven to reduce medical errors, promote a safety culture, and improve patient outcomes.[34] The importance of effective interprofessional collaboration has become even more important as nurses advocate to reduce health disparities related to social determinants of health (SDOH). In these efforts, nurses work with people from a variety of professions, such as physicians, social workers, educators, policy makers, attorneys, faith leaders, government employees, community advocates, and community members. Nursing students must be prepared to effectively collaborate interprofessionally after graduation.[35]
The Interprofessional Education Collaborative (IPEC) has identified four core competencies for effective interprofessional collaborative practice. This chapter will review content related to these four core competencies and provide examples of how they relate to nursing.
The Interprofessional Education Collaborative (IPEC) established standard core competencies for effective interprofessional collaborative practice. The competencies guide the education of future health professionals with the necessary knowledge, skills, values, and attitudes to collaboratively work together in providing client care. See Table 7.2 for a description of the four IPEC core competencies.[36] Each of these competencies will be further discussed in the following sections of this chapter.
Table 7.2. IPEC Core Competencies[37]
| Competency 1: Values/Ethics for Interprofessional Practice
Work with individuals of other professions to maintain a climate of mutual respect and shared values. |
|---|
| Competency 2: Roles/Responsibilities
Use the knowledge of one’s own role and those of other professions to appropriately assess and address the health care needs of patients and to promote and advance the health of populations. |
| Competency 3: Interprofessional Communication
Communicate with patients, families, communities, and professionals in health and other fields in a responsive and responsible manner that supports a team approach to the promotion and maintenance of health and the prevention and treatment of disease. |
| Competency 4: Teams and Teamwork
Apply relationship-building values and the principles of team dynamics to perform effectively in different team roles to plan, deliver, and evaluate patient/population-centered care and population health programs and policies that are safe, timely, efficient, effective, and equitable. |
The first IPEC competency is related to values and ethics and states, “Work with individuals of other professions to maintain a climate of mutual respect and shared values.”[38] See the box below for the components related to this competency. Notice how these interprofessional competencies are very similar to the Standards of Professional Performance established by the American Nurses Association related to Ethics, Advocacy, Respectful and Equitable Practice, Communication, and Collaboration.[39]
Components of IPEC’s Values/Ethics for Interprofessional Practice Competency[40]
- Place interests of clients and populations at the center of interprofessional health care delivery and population health programs and policies, with the goal of promoting health and health equity across the life span.
- Respect the dignity and privacy of patients while maintaining confidentiality in the delivery of team-based care.
- Embrace the cultural diversity and individual differences that characterize patients, populations, and the health team.
- Respect the unique cultures, values, roles/responsibilities, and expertise of other health professions and the impact these factors can have on health outcomes.
- Work in cooperation with those who receive care, those who provide care, and others who contribute to or support the delivery of prevention and health services and programs.
- Develop a trusting relationship with patients, families, and other team members.
- Demonstrate high standards of ethical conduct and quality of care in contributions to team-based care.
- Manage ethical dilemmas specific to interprofessional patient/population-centered care situations.
- Act with honesty and integrity in relationships with patients, families, communities, and other team members.
- Maintain competence in one’s own profession appropriate to scope of practice.
Nursing, medical, and other health professional programs typically educate students in “silos” with few opportunities to collaboratively work together in the classroom or in clinical settings. However, after being hired for their first job, these graduates are thrown into complex clinical situations and expected to function as part of the team. One of the first steps in learning how to function as part of an effective interprofessional team is to value each health care professional’s contribution to quality, patient-centered care. Mutual respect and trust are foundational to effective interprofessional working relationships for collaborative care delivery across the health professions. Collaborative care also honors the diversity reflected in the individual expertise each profession brings to care delivery.[41]
Cultural diversity is a term used to describe cultural differences among clients, family members, and health care team members. While it is useful to be aware of specific traits of a culture, it is just as important to understand that each individual is unique, and there are always variations in beliefs among individuals within a culture. Nurses should, therefore, refrain from making assumptions about the values and beliefs of members of specific cultural groups.[42] Instead, a better approach is recognizing that culture is not a static, uniform characteristic but instead realizing there is diversity within every culture and in every person. The American Nurses Association (ANA) defines cultural humility as, “A humble and respectful attitude toward individuals of other cultures that pushes one to challenge their own cultural biases, realize they cannot possibly know everything about other cultures, and approach learning about other cultures as a lifelong goal and process.”[43] It is imperative for nurses to integrate culturally responsive care into their nursing practice and interprofessional collaborative practice.
Read more about cultural diversity, cultural humility, and integrating culturally responsive care in the “Diverse Patients” chapter of Open RN Nursing Fundamentals, 2e.
Nurses value the expertise of interprofessional team members and integrate this expertise when providing patient-centered care. Some examples of valuing and integrating the expertise of interprofessional team members include the following:
- A nurse is caring for a patient admitted with chronic heart failure to a medical-surgical unit. During the shift the patient’s breathing becomes more labored and the patient states, “My breathing feels worse today.” The nurse ensures the patient’s head of bed is elevated, oxygen is applied according to the provider orders, and the appropriate scheduled and PRN medications are administered, but the patient continues to complain of dyspnea. The nurse calls the respiratory therapist and requests a STAT consult. The respiratory therapist assesses the patient and recommends implementation of BiPAP therapy. The provider is notified and an order for BiPAP is received. The patient reports later in the shift the dyspnea is resolved with the BiPAP therapy.
- A nurse is working in the Emergency Department when an adolescent patient arrives via ambulance experiencing a severe asthma attack. The paramedic provides a handoff report with the patient's current vital signs, medications administered, and intravenous (IV) access established. The paramedic also provides information about the home environment, including information about vaping products and a cat in the adolescent’s bedroom. The nurse thanks the paramedic for sharing these observations and plans to use information about the home environment to provide patient education about asthma triggers and tobacco cessation after the patient has been stabilized.
- A nurse is working in a long-term care environment with several assistive personnel (AP) who work closely with the residents providing personal cares and have excellent knowledge regarding their baseline status. Today, after helping Mrs. Smith with her morning bath, one of the APs tells the nurse, “Mrs. Smith doesn’t seem like herself today. She was very tired and kept falling asleep while I was talking to her, which is not her normal behavior.” The nurse immediately assesses Mrs. Smith and confirms her somnolescence and confirms her vital signs are within her normal range. The nurse reviews Mrs. Smith’s chart and notices that a new prescription for furosemide was started last month but no potassium supplements were ordered. The nurse notifies the provider of the patient’s change in status and receives an order for lab work including an electrolyte panel. The results indicate that Mrs. Smith’s potassium level has dropped to an abnormal level, which is the likely cause of her fatigue and somnolescence. The provider is notified, and an order is received for a potassium supplement. The nurse thanks the AP for recognizing and reporting Mrs. Smith’s change in status and successfully preventing a poor patient outcome such as a life-threatening cardiac dysrhythmia.
Effective patient-centered, interprofessional collaborative practice improves patient outcomes. View supplementary material and reflective questions in the following box.[44]
View the “How does interprofessional collaboration impact care: The patient’s perspective?” video on YouTube regarding patients' perspectives about the importance of interprofessional collaboration.
Read Ten Lessons in Collaboration. Although this is an older publication, it provides ten lessons to consider in collaborative relationships and practice. The discussion reflects many components of collaboration that have been integral to nursing practice in interprofessional teamwork and leadership.
Reflective Questions
- What is the difference between patient-centered care and disease-centered care?
- Why is it important for health professionals to collaborate?

