7.5 Diabetes Mellitus
Open Resources for Nursing (Open RN)
Diabetes mellitus (DM) is a chronic medical condition marked by persistently elevated blood glucose levels, a condition called hyperglycemia. This occurs as a result of the body’s inability to properly regulate blood glucose due to issues with insulin secretion by the pancreas, cellular insulin resistance, or both.
Pathophysiology
The pathophysiology of diabetes mellitus is related to dysfunction of the islet cells of the pancreas. As previously discussed in the “Review of Anatomy and Physiology of the Endocrine System” section, the islet cells regulate the secretion of insulin and glucagon to balance blood glucose levels.
During type 1 diabetes, the immune system mistakenly attacks and destroys beta islet cells, leading to an absolute deficiency of insulin. During type 2 diabetes, the body’s cells become resistant to the effects of insulin and/or the pancreas does not produce sufficient insulin to meet the body’s needs. Gestational diabetes occurs during pregnancy and typically resolves after the baby is born. However, gestational diabetes increases the mother’s risk of developing type 2 diabetes later in life. Latent autoimmune diabetes in adults (LADA) is a type of diabetes that starts in adulthood and slowly gets worse over time. Like type 1 diabetes, LADA occurs when the pancreas stops making insulin because an autoimmune process is damaging islet cells in the pancreas. However, unlike type 1 diabetes, in LADA the process happens slowly so people often don’t need to take insulin right away.[1]
The development of type 1 DM is influenced by genetics, autoimmune factors, and/or viral infections. Autoimmune factors and viral infections can destroy the islet cells of the pancreas, rendering them incapable of producing insulin.
The development of DM type 2 is influenced by a combination of genetic, lifestyle, and environmental factors. Risk often increases as individuals age, with greater onset occurring after age 45. Family history, obesity, metabolic syndrome, and lifestyle factors such as lack of physical activity increase risk for the development of DM type 2. Metabolic syndrome is a group of conditions that increase the risk of coronary heart disease, diabetes, and stroke. The conditions include elevated blood pressure, blood glucose, and triglyceride levels, as well as increased waist circumference.[2] Women who experienced gestational diabetes during pregnancy are also at greater risk for developing DM type 2. Additionally, certain ethnic groups, including African Americans, Hispanics, Native Americans, and Pacific Islanders, also have increased genetic risk for developing DM type 2.[3]
See a free risk test for type 2 diabetes from the American Diabetes Association: 60-Second Type 2 Diabetes Risk Test.
Potential Long-Term Complications
In all types of diabetes, insulin does not effectively facilitate the uptake of glucose by the body’s cells. Elevated blood sugar levels damage blood vessels and nerves and can lead to long-term, serious complications. Examples of complications related to DM include the following[4]:
- Cardiovascular Disease: Damage to blood vessels due elevated blood sugar can result in arteriosclerosis, atherosclerosis, coronary artery disease, and heart attacks.
- Hypertension: DM damages the lumen of blood vessels and can lead to rigidity and development or exacerbation of high blood pressure, which further increases the risk of heart disease.
- Kidney Failure: DM is a leading cause of kidney disease, referred to as diabetic nephropathy. Over time, DM can cause kidney failure, which may necessitate renal dialysis or kidney transplantation.
- Blindness: Damage to the blood vessels in the eyes causes diabetic retinopathy and reduced vision. If left untreated, vision impairment and eventually blindness can occur.
- Stroke: DM increases the risk of stroke due to its impact on cerebral blood vessels, making them susceptible to clot formation or rupture, which can result in a stroke.
- Neuropathy: DM causes nerve damage, often affecting the legs and feet. Symptoms include pain, tingling, and numbness called paresthesia.
- Peripheral Vascular Disease: DM may cause circulatory problems in the lower extremities, which can result in foot ulcerations and nonhealing foot wounds that can result in amputation.
- Infection and Sepsis: DM increases the risk of severe infection that can cause early death.
Acute Complications: Hypoglycemia and Hyperglycemia
Clients with diabetes mellitus can develop acute complications called hypoglycemia (low blood glucose levels) and extreme hyperglycemia (high blood glucose levels).
Hypoglycemia
Hypoglycemia is defined as blood glucose levels below 70 mg/dL. Hypoglycemia is a common side effect of medications used to lower blood sugar, especially insulin or oral medications that affect the release of insulin (e.g., sulfonylureas and biguanides). Common causes of hypoglycemia in clients taking diabetic medications include the following[5]:
- Too much insulin administered or too high of dose of oral medication
- Excessive physical activity
- Mismatch of medication administration and meal administration or delayed or missed meals
- Excessive alcohol consumption
Initial signs and symptoms of hypoglycemia include confusion, hunger, shakiness or tremors, sweating, tachycardia, anxiety and irritability, weakness or fatigue, dizziness or lightheadedness, and blurred vision. A low blood glucose level triggers the release of epinephrine (the “fight or flight” hormone) that causes symptoms such as tachycardia, sweating, tingling, and anxiety. Left untreated, hypoglycemia can cause serious neurological effects, such as loss of consciousness, seizures, coma, and death due to lack of glucose delivery to brain cells.[6]
Hypoglycemia may be difficult to recognize in the elderly and in people who are taking beta-adrenergic blocking drugs.
Nurses must monitor clients diagnosed with diabetes mellitus very closely for signs and symptoms of hypoglycemia and provide rapid treatment. A general rule used by the American Diabetes Association is the 15-15 Rule, which suggests consuming or administering 15 grams of a carbohydrate, followed by a 15-minute wait and then remeasurement of blood glucose level to assess if blood glucose has returned to normal levels. These steps are repeated until blood glucose is at least 70 mg/dL.[7] Most agencies have a “Hypoglycemia Protocol” for immediate treatment without the need to first notify the provider. See the following box for an example of a hypoglycemia protocol, but always follow agency policy.
Sample Hypoglycemia Protocol[8],[9]
Mild Hypoglycemia (Blood glucose less than 70 mg/dL but greater than 40 mg/dL):
- Provide 10-15 grams of a simple, fasting-acting carbohydrate to immediately raise blood glucose levels, such as:
-
- ½ cup of fruit juice
- ½ cup of regular soft drink
- 8 oz. of skim milk
- 3 graham crackers
- If food is not available or appropriate to administer to the client, some agency protocols advise administering a glucose tablet or gel.
- After administering 10-15 grams of carbohydrate, recheck the bedside glucose level in 15 minutes to ensure it has risen.
- A meal tray or complex carbohydrates may be provided if appropriate and the client is able to swallow.
- If symptoms persist and the blood glucose level remains below 70 mg/dL, repeat administration of 10-15 grams of carbohydrate and recheck the bedside blood glucose level every 15 minutes until it is above 70 mg/dL.
- Notify the provider of the hypoglycemic event.
Moderate Hypoglycemia (Blood glucose less than 40 mg/dL but greater than 20 mg/dL):
- Moderate hypoglycemia may manifest with symptoms like cold, clammy skin, rapid pulse, and drowsiness.
- Administer 15-30 grams of carbohydrates, if the client is able to safely swallow.
- A meal tray or complex carbohydrates may be provided if appropriate and the client is able to swallow.
- Encourage ingestion of additional food items with protein, such as low-fat milk or cheese, 10-15 minutes after the carbohydrate ingestion.
- Recheck the bedside glucose level in 15 minutes after carbohydrate administration.
- If symptoms persist and the blood glucose level remains below 70 mg/dL, repeat administration of 10-15 grams of carbohydrate and recheck the bedside blood glucose every 15 minutes until it is above 70 mg/dL.
- Notify the provider of the hypoglycemic event.
Severe Hypoglycemia (Blood glucose less than 20 mg/dL):
- Severe hypoglycemia can be life-threatening and is characterized by the inability to swallow, unconsciousness, or convulsions. It is imperative to call for emergency assistance according to agency protocol.
- Administer glucagon nasal spray, glucagon injection, or D50 IV push per agency protocol.
- If the person remains unconscious after ten minutes, administer a second dose.
- Notify the individual’s health care provider and follow their instructions.
- If the person remains unconscious, transport them to the Emergency Department (ED) for further evaluation.
- After the person regains consciousness and is no longer nauseated, offer a small meal to stabilize blood sugar levels.
Hyperglycemia
Hyperglycemia occurs when a fasting blood glucose level is above 126 mg/dL, and severe hyperglycemia is generally defined as greater than 250 mg/dL. Hyperglycemia can cause acute complications called diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS):
- Diabetic Ketoacidosis (DKA) occurs during severe hyperglycemia episodes if the client’s pancreas is no longer producing insulin. It most commonly occurs in clients with type 1 DM, but it can also occur in clients with type 2 diabetes if their pancreas is no longer producing insulin. Because of the lack of insulin available to transport glucose into cells, the body breaks down fatty acids for energy, and ketones are created. Ketones cause metabolic acidosis, which can be a life-threatening condition. DKA is often triggered by a combination of factors, including uncontrolled high blood sugar and increased stress on the body, such as infection or trauma. In some cases, individuals are not aware they have type 1 DM until they are hospitalized with DKA and the diagnosis of diabetes mellitus is established. DKA is also associated with elevated potassium levels that can cause life-threatening cardiac arrhythmias. DKA is typically treated with insulin drips, IV fluids, and medications to restore normal electrolyte and pH balance.
- Hyperosmolar Hyperglycemic State (HHS) is an extremely severe hyperglycemia that occurs in individuals with type 2 DM. Because the pancreas of an individual with DM type 2 is still producing some insulin that moves glucose into cells, fatty acids are not broken down into ketones, so DKA does not occur. However, the blood glucose level becomes so abnormally elevated that severe cellular dehydration occurs, resulting in life-threatening hypotension and elevated serum sodium levels. HHS is typically triggered by prolonged periods of extremely high blood sugar, often due to illness, infection, or inadequate management of DM. HHS is treated with IV fluids, insulin drips, and medications to restore electrolyte balance.[10],[11] See Table 7.5a comparing the signs and symptoms of hypoglycemia and hyperglycemia.
Table 7.5a. Signs and Symptoms DKA and HHS[12],[13]
| Condition | Signs and Symptoms |
|---|---|
| Diabetic Ketoacidosis (DKA) | Elevated blood glucose levels greater than 250 with glucose and ketones in the urine, excessive thirst, frequent urination, abdominal pain, nausea and vomiting, deep and labored breathing (Kussmaul respirations), confusion and altered mental status, fruity breath odor, and hyperkalemia. |
| Hyperosmolar Hyperglycemic State (HHS) | Elevated blood sugar levels, extreme dehydration with elevated serum sodium levels, excessive thirst, altered mental status, confusion and weakness, and coma. |
Assessment
Clinical manifestations of diabetes mellitus are related to chronically elevated blood sugar levels, resulting in damage to blood vessels, nerves, and tissues. See Table 7.5b for a summary of potential assessment findings across body systems and organs for clients with diabetes mellitus.
Table 7.5b. Clinical Manifestations of Diabetes Mellitus and Potential Complications[14],[15]
| Body System or Organ | Clinical Manifestations |
|---|---|
| Cardiovascular | Hypertension (high blood pressure), elevated cholesterol and triglycerides levels, and increased risk of heart disease and stroke |
| Nervous | Neuropathy (nerve damage) and paresthesia |
| Eyes | Diabetic retinopathy, vision changes, and potential blindness |
| Kidneys | Diabetic nephropathy (kidney damage), proteinuria (excess protein in urine), and renal failure |
| Gastrointestinal/Genitourinary | Polydipsia (excessive thirst), polyphagia (excessive hunger), polyuria (excessive urination), gastroparesis (delayed stomach emptying), nausea, and vomiting |
| Skin | Acanthosis nigricans (hyperpigmentation of the skin often found in the axilla, groin, and folds of the neck), sudomotor neuropathy (absence of sweating in the extremities that causes dry skin and can lead to foot ulcerations), slow wound healing, and skin infections |
| Musculoskeletal | Diabetic myopathy (muscle weakness) and charcot joint (joint damage) |
| Reproductive | Polycystic ovary syndrome (PCOS) in women and erectile dysfunction in men |
| Respiratory | Increased risk of obstructive sleep apnea |
| Immune | Increased susceptibility to infections and slower healing |
Diagnostic Testing
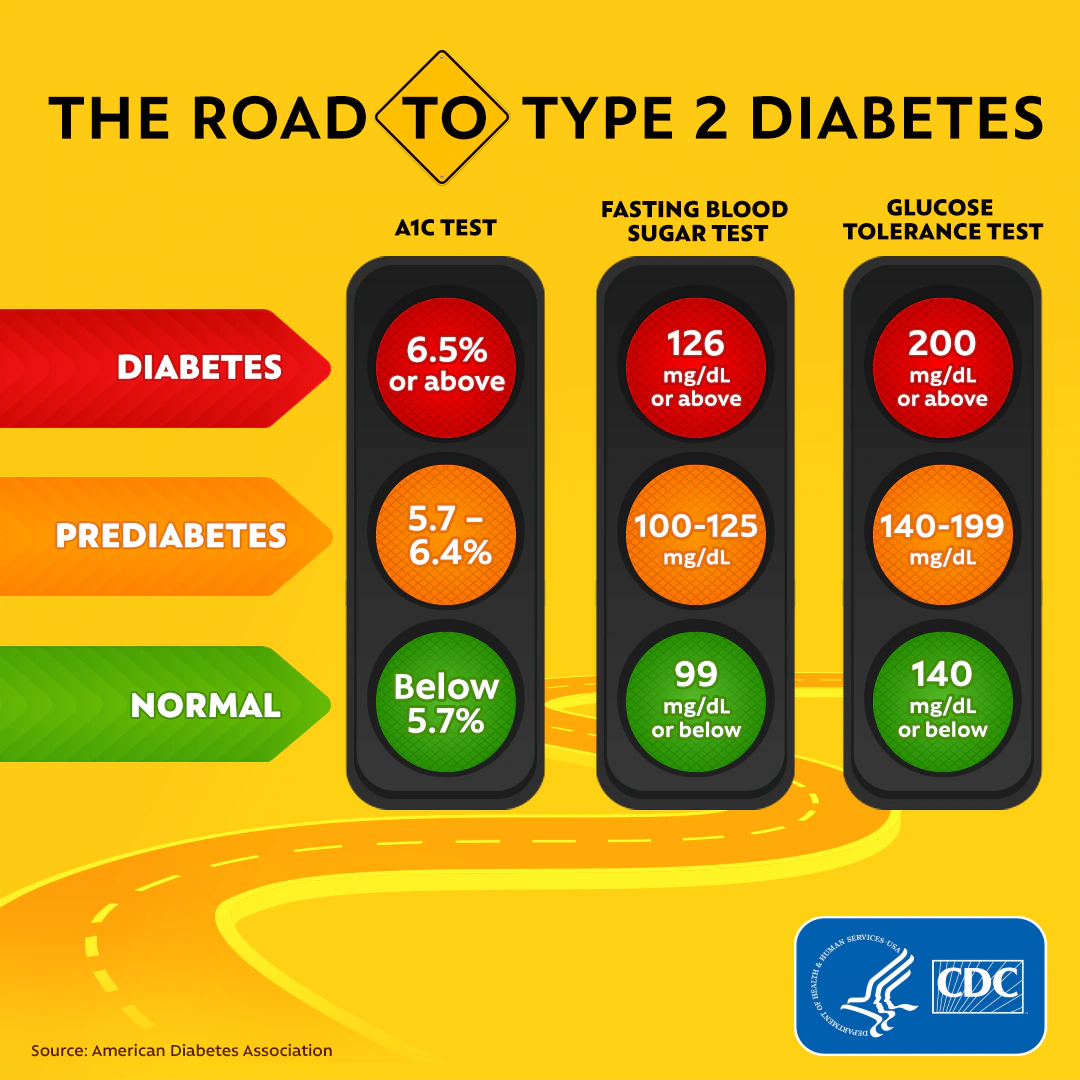
Diagnostic testing related to DM includes several tests to identify the presence of elevated blood glucose or glucose in the urine. The most common tests used to diagnose type 2 DM are fasting blood glucose, hemoglobin A1C, and glucose tolerance test. See Figure 7.8[16] for an infographic from the Centers for Disease Control and Prevention comparing lab results for normal, prediabetes, and type 2 diabetes.
Common diagnostic tests for DM include the following[17],[18]:
- Fasting blood glucose (FBG): FBG assesses an individual’s blood glucose level when they have had no caloric intake for at least eight hours (although water intake is permitted). The blood sample must be collected before food, insulin, or oral antidiabetic agents have been administered. Normal fasting blood glucose range is between 70-100 mg/dL. Diabetes mellitus is diagnosed when fasting blood glucose levels consistently measure 126 mg/dL or higher on two separate tests. Impaired fasting glucose is identified in levels that range between 100 to 125 milligrams per deciliter (mg/dL), which means blood glucose levels are elevated, but not high enough to be classified as diabetes.[19],[20]
- Random blood glucose: Random blood glucose measures the level of glucose in the blood at any given time, without the requirement for fasting. This test is often used for quick assessments of blood sugar levels, especially during emergency or urgent care settings. The normal range for random plasma glucose levels is typically less than 140 mg/dL.[21],[22] Random blood sugar greater than 200 mg/dL can be a sign of diabetes mellitus.
- Hemoglobin A1C (HbA1C): Hemoglobin A1C assesses an individual’s average blood glucose levels over the preceding two to three months. HbA1C is a form of hemoglobin, a protein found in red blood cells. When glucose is in the bloodstream, it attaches to hemoglobin, forming glycated hemoglobin. The percentage of hemoglobin that is glycated is directly proportional to the average blood glucose levels during the red blood cells’ life spans, which is approximately 120 days. The normal range for HbA1C is typically less than 5.7%. An HbA1C level between 5.7% and 6.4% (or 39-47 mmol/mol) is indicative of prediabetes, which means that blood glucose levels are higher than normal but not yet in the diabetic range. An HbA1C level of 6.5% (or 48 mmol/mol) or higher is diagnostic of diabetes mellitus.[23],[24]
- Oral glucose tolerance tests (GTT): GTT evaluates the body’s ability to regulate blood glucose levels, especially after consuming a high dose of glucose. The results are typically reported as blood glucose levels measured at different time points (such as fasting, 1 hour post-glucose consumption, and 2 hours post-glucose consumption). These are the normal results by time frame:
- Fasting blood glucose (FBG): Less than 100 mg/dL
- 1-hour post-glucose load: Less than 200 mg/dL
- 2-hour post-glucose load: Less than 140 mg/dL
Elevated blood glucose levels at any of these time points may indicate impaired glucose tolerance and diabetes mellitus.[25],[26]
Preparation: Before the test, the individual is required to fast overnight (usually for at least eight hours) to ensure a stable baseline blood glucose level. During this fasting period, the person should avoid eating or drinking anything except for water.
Initial Blood Sample: A baseline fasting blood sample is collected to measure the individual’s fasting blood glucose level.
Glucose Solution: After the fasting sample is taken, the person is given a glucose solution to drink. This solution contains a standardized amount of glucose (usually 75 grams), which is typically dissolved in water.
Blood Samples: Blood samples are collected at specified intervals after the glucose solution is consumed. The most common time points for these samples are at one hour and two hours after drinking the glucose solution. In some cases, a sample may also be taken at three hours.
- C-peptide: C-peptide is generally found in amounts in the blood equal to the amount of insulin because insulin and C-peptide are linked when they are first produced by the pancreas. Therefore, the level of C-peptide is an indirect measure of the amount of insulin being produced by the pancreas. A C-peptide test may be ordered when diabetes mellitus has been initially diagnosed to determine if type 1 or type 2 diabetes mellitus (DM) is present. Type 1 DM is diagnosed when the pancreas does not make any insulin, so the level of C-peptide is also low. In type 2 DM, the pancreas continues to produce insulin, so C-peptide levels are normal or high. Fasting C-peptide levels are typically around 0.5 to 2.0 ng/mL.[29],[30]
- Urine Tests for Ketones or Glucose
- Ketones: Ketones are metabolic byproducts of fatty acid metabolism, typically produced in the liver. In healthy individuals, ketones are efficiently metabolized, and only minimal amounts appear in the urine. However, under specific circumstances in clients with DM type 1, such as lack of food intake when ill or the development of DKA, elevated ketone levels in the urine indicate the body is using fat as the major source of energy. Ketones may be monitored using urine ketone strips for clients with blood glucose levels over 240 mg/dL to watch for DKA and determine the need for prompt follow-up.
- Glucose: Normally, there is very little or no glucose in urine. When blood glucose levels are very high in the blood, such as in uncontrolled diabetes, the glucose spills over into the urine. Glucose can also be found in urine when the kidneys are damaged or diseased. In the first part of the renal tubule, called the proximal tubule, glucose is reabsorbed from the filtrate into the bloodstream. The proximal tubule can only reabsorb a limited amount of glucose. Therefore, if the blood glucose level exceeds about 160 – 180 mg/dL, the proximal tubule becomes overwhelmed and begins to excrete glucose in the urine.[31],[32]
Review normal reference ranges for common diagnostic tests in “Appendix A – Normal Reference Ranges.”
Nursing Diagnoses
Nursing priorities for clients with diabetes mellitus revolve around managing blood glucose levels, preventing complications, providing health teaching, and promoting self-management of this chronic disease at home.
Nursing diagnoses for clients with diabetes are crafted based on a thorough assessment of the client’s condition, medical history, and their unique requirements. Common nursing diagnoses related to DM are the following[33]:
- Readiness for Enhanced Knowledge
- Imbalanced Nutrition
- Impaired Skin Integrity
- Ineffective Coping
- Ineffective Health Maintenance
- Risk for Infection
Outcome Identification
Outcome identification includes setting short- and long-term goals and creating expected outcome statements customized for the client’s specific needs. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions. Examples of expected outcomes for clients with DM include the following:
- The client will achieve and maintain stable blood glucose levels within the target range.
- The client will demonstrate understanding of diabetes self-management strategies following the health teaching sessions, including accurate monitoring of blood glucose levels and administration of medications.
- The client will achieve and maintain healthy weight.
- The client will demonstrate healthy skin integrity with no skin ulcers.
Interventions
Medical Interventions
Medical interventions for DM are designed to help individuals manage their blood glucose levels within a target range, prevent the development of complications, and improve their overall health and well-being. Specific interventions can vary based on the type of diabetes, the individual’s needs, and the health care provider’s recommendations. Medical interventions typically include medication therapy, blood glucose monitoring, dietary counseling, and weight management.
Medication Therapy
Medication therapy may include oral antidiabetic medications, insulin, or other injectable medication.
Non-Insulin Antidiabetic Medications
Non-insulin antidiabetic medications are prescribed for clients with type 2 DM. They may be used alone or in combination with insulin. See Table 7.5c for an overview of common non-insulin antidiabetic medications, their mechanisms of action, and nursing considerations.
Table 7.5c. Non-Insulin Antidiabetic Medications
| Medication | Examples | Mechanism of Action | Nursing Considerations |
|---|---|---|---|
| Biguanides | Metformin | Decrease the amount of glucose produced by the liver and increase the sensitivity of muscle cells to insulin. It also slows the absorption of glucose from the digestive tract. | Administer with meals to decrease potential side effects of nausea, vomiting, and diarrhea. Monitor RBC, hemoglobin, and renal function tests at least every year. Contraindicated in clients with kidney disease and should be temporarily discontinued in clients undergoing radiologic studies involving administration of iodinated contrast materials because of risk of acute renal function. It is also contraindicated in clients with metabolic acidosis. Increases risk for lactic acidosis and chills. Low blood pressure, muscle pain, or dyspnea should be immediately reported to the health care provider.[34],[35] |
| Sulfonylureas | Glipizide, glyburide, and glimepiride | Stimulate the pancreas to release more insulin when there is still some insulin production by the pancreas. | Should be administered 30 minutes before a meal to avoid hypoglycemia. Monitor for signs of hypoglycemia, abnormal liver function tests, and weight gain. Concurrent use of sulfonylureas and alcohol may cause a disulfiram-like reaction.[36],[37] |
| Dipeptidyl peptidase-4 (DPP-4) inhibitors | Sitagliptin and saxagliptin | Block the DPP-4 enzyme that inactivates incretin hormones, thus increasing the level of incretin. Incretins stimulate the release of insulin and reduce the production of glucagon.[38] | Monitor for hypoglycemia. Dose adjustment should occur for clients with kidney disease depending on their glomerular filtration rate. Report hypersensitivity reactions, blisters/erosions, headache, symptoms of pancreatitis, heart failure, severe arthralgia, and upper respiratory infection. |
| GLP-1 receptor agonists | Dulaglutide, exenatide, and liraglutide | Mimic the action of GLP-1, a naturally occurring hormone in the body that regulates blood sugar levels. GLP-1 is released from the intestines in response to food intake and stimulates the release of insulin from the pancreas, suppresses the release of glucagon, and promotes feelings of fullness, which can lead to reduced food intake.[39] | Injected subcutaneously. Instruct clients to stop eating when they feel full. Reducing food intake may lessen common side effects of nausea and vomiting. Long-acting GLP-1 receptor agonists should be taken on or around the same day each week.
Contraindicated for clients with severe kidney disease.[40] |
| Alpha-glucosidase inhibitors | Acarbose | Block gastrointestinal alpha-glucosidase enzymes in the gastrointestinal system that digest the starch, thus inhibiting the metabolism of sucrose to glucose.[41],[42] | Monitor serum creatinine and serum transaminase levels annually.[43],[44] |
| Thiazolidinediones | Pioglitazone | Increase cellular insulin sensitivity and cellular uptake of glucose.[45],[46] | Monitor for signs of heart failure, bladder cancer (hematuria, dysuria, and urinary urgency), and weight gain. Encourage periodic ophthalmologic exams.[47],[48] |
| Sodium-glucose co-transporter 2 SLT-2 inhibitors | Anaglifozin | Act on the kidneys to reduce the reabsorption of glucose and promote urinary glucose excretion.[49] | Monitor renal function and LDL.[50],[51] |
Insulin Therapy
Insulin therapy is used for individuals with type 1 DM and in some cases of type 2 DM when insufficient insulin is being produced by the pancreas or tight glycemic control is warranted in the hospital. The primary purpose of insulin therapy is to regulate and normalize blood glucose levels by supplementing or replacing the body’s natural insulin production.[52],[53] Client goals are to maintain their serum blood glucose in normal range and achieve their individualized target level of A1C (often 7%). See Figure 7.9[54] for an image of an insulin vial and the orange-capped syringe specifically used to administer insulin.

There are many different types of insulin with different times of onset, peak, and duration. Table 7.5d summarizes insulin classes.[55],[56]
Table 7.5d. Insulin Classes
| Class | Generic/Brand Name | Onset/Peak/Duration | Nursing Considerations |
|---|---|---|---|
| Rapid-Acting Insulin | Insulin lispro (Humalog)
Insulin aspart (Novolog) |
Onset: 15-30 minutes
Peak effect: 1-3 hours Duration: 3-5 hours |
Commonly prescribed to cover mealtime spikes in blood sugar levels. Administer within 15 minutes before a meal or immediately after a meal.
Afrezza, an inhaled insulin, is contraindicated in clients with asthma or COPD. |
| Short-Acting Insulin | Regular insulin (Humulin R or Novolin R) | Onset: 30 minutes
Peak effect: 3 hours Duration: 8 hours |
Commonly prescribed to control blood sugar between meals and at night. Administer 30 minutes before a meal. |
| Intermediate-Acting Insulin | Isophane insulin or NPH (Humulin N or Novolin N) | Onset: 1-2 hours
Peak effect: 6 hours (range 2.8-13 hours) Duration: Up to 24 hours |
Commonly prescribed in combination with other insulins to provide basal insulin coverage. Administer once or twice daily.
Gently roll or invert vial/pen several times to resuspend the insulin before administration. |
| Combination: Intermediate-Acting/Rapid-Acting | Humalog Mix 50/50
Humalog Mix 75/25 Novolog Mix 70/30 *First number is % of intermediate-acting insulin; second number is % of rapid-acting insulin |
Onset: 15-30 minutes
Peak effect of Humalog 50/50: 1-5 hours Duration: 11-22 hours |
*The first number is the % of intermediate-acting insulin; the second number is the % of rapid-acting insulin.
Administer twice daily, 15 minutes before a meal or immediately after a meal. Only administer subcutaneously. Gently roll or invert vial/pen several times to resuspend the insulin before administration. |
| Combination: Intermediate-Acting/Short-Acting | Humulin Mix 70/30
Novolin Mix 70/30 *First number is % of intermediate-acting insulin; second number is % of short-acting insulin |
Onset: 30-90 minutes
Peak effect: 1.5-6.5 hours Duration: 18-24 hours |
*The first number is the % of intermediate-acting insulin; the second number is the % of rapid-acting insulin.
Administer twice daily, 30-45 minutes before a meal. Only administer subcutaneously. Gently roll or invert vial/pen several times to resuspend the insulin before administration. Do not mix with other insulin. |
| Long-Acting Insulin | Glargine (Lantus)
Detemir (Levemir) |
Onset: 3-4 hours
Peak effect: None Duration: >24 hours |
Prescribed to provide consistent blood glucose levels with less variability throughout the day.
Administer once daily (sometimes dose is split and administered twice daily). Only administer subcutaneously. Do not mix with other insulin. |
Many types of insulins are available in prefilled pens with a dial to select the number of units to be administered. These pens are helpful for clients in self-administration of insulin. See Figure 7.10[57] for an image of a prefilled syringe.

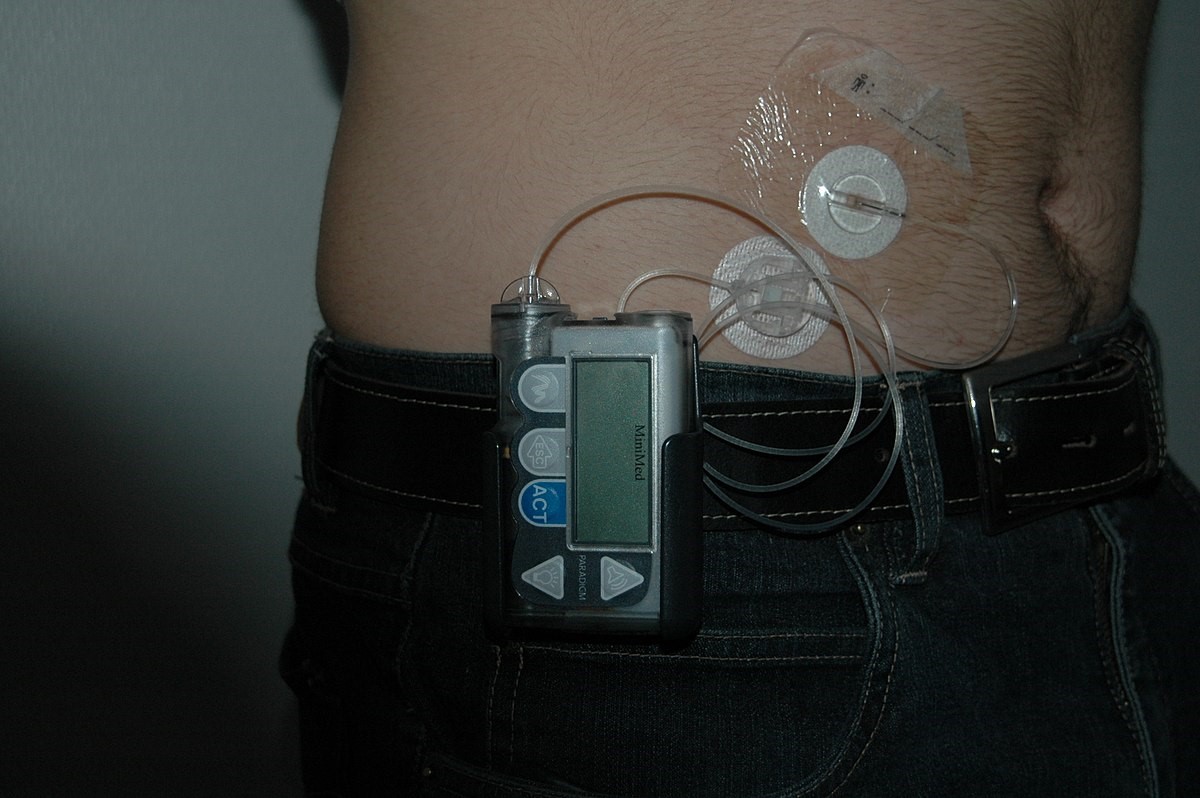
Insulin pumps are small, programmable devices that deliver a continuous supply of insulin into the body, mimicking the function of a healthy pancreas. Bolus doses of insulin can also be self-administered to cover meals or correct high blood sugar levels.
The pump’s settings are programmable, allowing users to customize basal rates, insulin-to-carbohydrate ratios, and correction factors to match variations in daily activities, diet, and metabolism for clients. The pump contains a reservoir filled with rapid-acting insulin, which is connected to the body via small, flexible tubing. There are also patch pumps without tubing. The insulin is delivered subcutaneously, typically in the fatty tissue beneath the skin. Insulin pumps and patch pumps are often integrated with continuous glucose monitoring sensors that allow real-time monitoring of blood glucose levels with automated adjustments to insulin delivery, enhancing overall blood sugar control. Insulin pumps can contribute to better blood sugar management by reducing the risk of hypoglycemia (low blood sugar) and offering more precise control over insulin dosage. The pump offers greater flexibility in terms of lifestyle and meal timing, as users can adjust insulin delivery based on their daily routines. This can lead to a more convenient and adaptable approach. See Figure 7.11[58] for an image of an individual with an insulin pump and continuous glucose monitoring system.
Review additional information about medication classes used to treat diabetes mellitus in the “Antidiabetics” section of the “Endocrine” chapter in Open RN Nursing Pharmacology, 2e.
Blood Glucose Monitoring
Routine monitoring of blood glucose levels is a common component of diabetes management for clients with type 1 DM and for some clients with type 2 DM depending upon their prescribed medication therapy. Individuals typically check their blood glucose levels before meals and at bedtime and may administer additional insulin based on their glucose level before eating. See Figure 7.12[59] for an image of a blood glucose monitoring device.

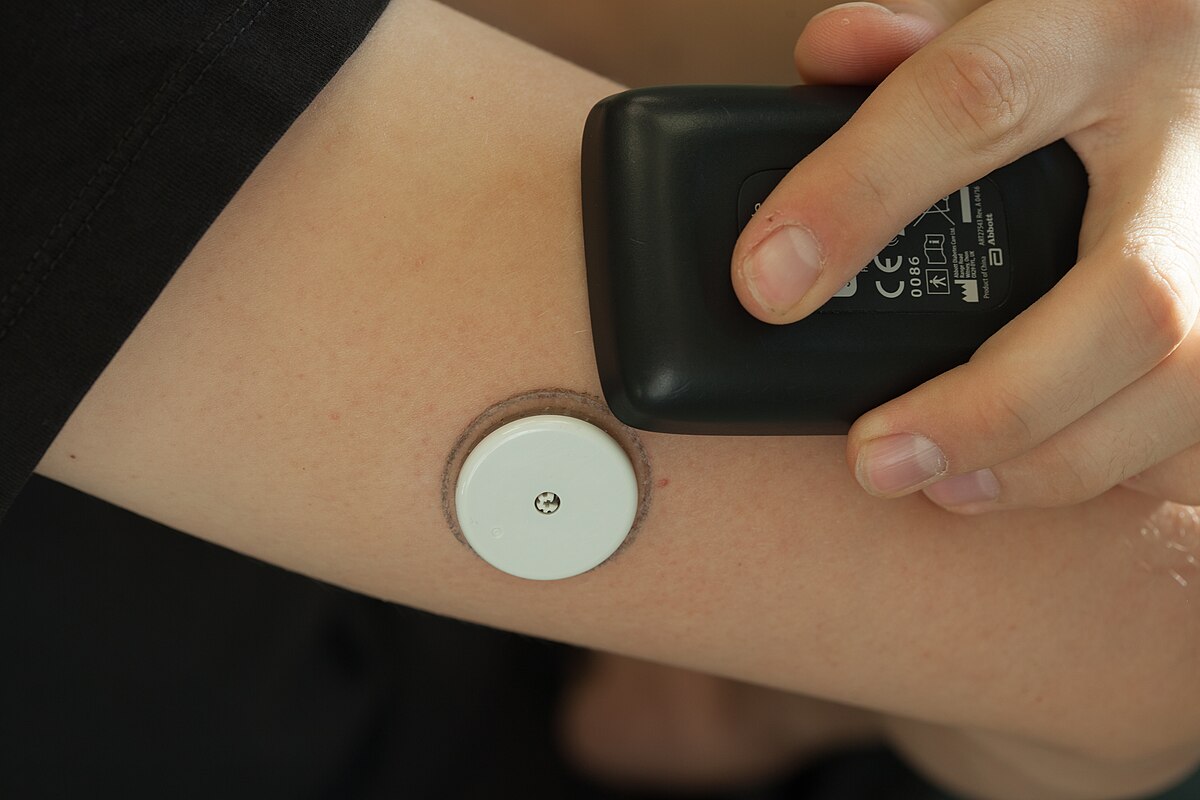
A continuous glucose sensor (CGS) is a medical device designed to monitor and track blood glucose levels in the interstitial fluid. The sensor transmits real-time data to a display device, often a dedicated receiver or a smartphone app. This allows individuals with diabetes, as well as their health care providers, to observe trends and patterns in glucose levels. The sensor has customizable alarms and alerts to notify users of high or low glucose levels. This feature helps individuals take prompt action to address potential issues and maintain better control over their blood sugar. Some advanced CGS integrate with insulin pumps, creating a closed-loop system. This allows for automated adjustments to insulin delivery based on real-time glucose data, contributing to more precise and responsive diabetes management. See Figure 7.13[60] for an image of a continuous glucose sensor.
Dietary Counseling
Referrals are made to registered dieticians to assist with blood glucose management through dietary modifications and carbohydrate counting. Controlling carbohydrate intake, portion sizes, and choosing foods with a low glycemic index can help stabilize blood sugar levels. Diabetic education is multifaceted and successful when individualizing for each client. Dietary counseling principles are described in the following box.
Dietary Counseling Principles[61]
Nutrition plays a crucial role in managing diabetes; therefore, meal planning is an essential part. To create an effective and sustainable meal plan, it is important to consider various factors, such as culture, socioeconomic status, and lifestyle, while also adhering to these specific dietary guidelines:
- Realistic and Flexible Meal Planning: Meal planning for diabetes should be realistic and flexible to fit the individual’s preferences, daily schedule, and dietary restrictions. It’s important to create a plan that can be maintained over the long-term.
- Consider Cultural Preferences: Cultural background can greatly influence food choices and eating habits. When creating a meal plan, it’s important to consider cultural preferences and adapt recipes to make them more diabetes-friendly while still honoring traditional dishes.
- Socioeconomic Status: Economic factors can impact access to certain foods. It’s essential to choose cost-effective, nutritious options and provide guidance on making healthy choices within a limited budget.
- Carbohydrates: Carbohydrates are a crucial component of meal planning for individuals with diabetes. Carbohydrates are “counted” for each meal to help quantify insulin for meal-time dosing. Individuals with diabetes maintain best glycemic control by distributing carbohydrates evenly throughout the day and adhering to controlled portion sizes. The glycemic index of simple and complex carbohydrates must also be considered when making food choices. The glycemic index indicates how quickly a carbohydrate-containing food raises blood sugar. Choosing low-glycemic index foods can help prevent rapid spikes in blood glucose levels.
- Protein: Protein should constitute 15%-20% of total daily calories. Lean sources of protein, such as poultry, fish, tofu, legumes, and low-fat dairy, are excellent choices. They can help stabilize blood sugar levels and promote a feeling of fullness.
- Fat and Cholesterol: Saturated fat intake should be less than 7% of total daily calories. Saturated fats can raise cholesterol levels and increase the risk of heart disease. Choose healthier fats like those found in nuts, seeds, avocados, and olive oil.
Minimize intake of trans fats, which are often found in processed and fried foods. Trans fats can have a negative impact on heart health.
- Fiber: Fiber is beneficial for improving carbohydrate metabolism and lowering cholesterol levels. The American Heart Association (AHA) recommends a daily fiber intake of at least 25 grams. Incorporate fiber-rich foods like whole grains, fruits, vegetables, and legumes into the diet.
- Sweeteners: Artificial sweeteners can be included in a meal plan as long as they are used mindfully and not in excess.
- Alcohol: Alcohol consumption can affect blood glucose levels. While moderate alcohol use may not significantly impact blood sugar, it’s important to be cautious, as excessive alcohol intake can lead to hypoglycemia (low blood sugar). If alcohol is consumed, it should be done in moderation, and individuals with diabetes should monitor their blood sugar levels carefully.
Meal planning is a critical aspect of diabetes management, and there are various strategies to help individuals with diabetes maintain stable blood glucose levels. Two popular meal planning approaches are the exchange system and carbohydrate counting. These methods provide structure and flexibility to create balanced meals while helping individuals manage their blood sugar effectively.
Exchange System
The exchange system is a meal planning method that categorizes foods into three main groups: carbohydrates (CHO), meat and meat substitutes, and fats. This approach simplifies meal planning by assigning specific portion sizes to each food group, allowing for the substitution of foods within the same group without significantly affecting blood glucose levels.[62]
- Carbohydrates (CHO): This group includes foods like bread, rice, pasta, cereal, fruits, and starchy vegetables. In the exchange system, CHO foods are categorized into serving sizes with approximately equal carbohydrate content, making it easier to control blood sugar.
- Meat and Meat Substitutes: This group comprises sources of protein, such as lean meats, poultry, fish, tofu, legumes, and dairy products. These are essential for building and repairing body tissues.
- Fats: The fats group includes sources of dietary fat like oils, nuts, seeds, and butter. While fats don’t directly impact blood glucose, managing their intake is important for overall health and weight control.
Using the exchange system, individuals can create balanced meals by selecting a certain number of servings from each food group, providing predictability in blood glucose responses. This system is particularly helpful for those who prefer structured meal planning.
Carbohydrate Counting
Carbohydrate counting is a flexible and individualized approach to meal planning for people with diabetes. It focuses primarily on carbohydrates because they have the most significant impact on blood glucose levels. With carbohydrate counting, individuals keep track of the total grams of carbohydrates they consume in a meal, regardless of the food source. One carbohydrate choice is equal to 15 grams of carbohydrate. This method allows for more variety in food choices, as long as the total carbohydrate intake is consistent.[63],[64]
Carbohydrate counting involves these steps:
- Identifying carbohydrate-containing foods in a meal.
- Estimating the total grams of carbohydrates in each food item.
- Keeping track of the cumulative carbohydrate intake for the entire meal.
By understanding how different foods affect blood sugar and monitoring carbohydrate intake, individuals can better control their post-meal blood glucose levels. Carbohydrate counting is particularly useful for those who want more flexibility in their food choices and are willing to track carbohydrate intake accurately.[65]
Insulin may be administered after meals based on carbohydrate intake. See an example of this process in the following box.
Example of Carbohydrate Counting
Provider Order: Administer 2 units Humalog insulin for each carbohydrate choice eaten at breakfast, lunch, and dinner
Meal Ticket: Lunch
- 1 Turkey sandwich (30 grams)
- 0.5 cup quinoa (15 grams)
- 1 cup yogurt (15 grams)
How many units of insulin should be administered following the lunch meal?
(Remember 15 grams carbohydrate = 1 carb choice)
Total grams of carbohydrate eaten: 60 grams
60 grams/15 grams = 4 carbohydrate choices
4 carb choices X 2 units of Humalog insulin per carb choice = 8 units Humalog insulin administered
Weight Management & Exercise
Maintaining a healthy weight can improve blood glucose control, particularly in type 2 diabetes. Regular exercise can promote weight loss. Exercise increases cellular sensitivity to insulin and promotes the uptake of glucose from the bloodstream, thus helping to regulate blood glucose levels.
Exercise can also prevent common complications of diabetes, such as heart disease, peripheral arterial disease, kidney disease, and stroke. It also has a positive impact on mental health, reducing stress and anxiety, which can contribute to improved self-management of diabetes. See the following box for exercise guidelines for individuals with diabetes.[66]
Exercise Guidelines[67]
When implementing an exercise program for diabetes management, it is important to consider the following guidelines:
- Avoid exercising in extreme temperatures to avoid dehydration.
- Aim to exercise five to six days a week. Do not go more than 48 hours between exercise sessions. Logging workouts can help keep track of weekly exercise.
- Exercise about an hour after a meal to ensure adequate blood glucose levels.
- Regularly monitor blood glucose levels before, during, and after exercise. This helps individuals understand how physical activity affects their blood sugar.
- Educate individuals about the risk of hypoglycemia (low blood sugar) during and after exercise. They should know the symptoms and the strategies to prevent and manage hypoglycemia by having a source of fast-acting carbohydrates on hand.
- The type and duration of exercise can vary depending on individual preferences and physical capabilities. It can include aerobic exercises, strength training, and flexibility exercises. Aim for at least 150 minutes of moderate-intensity aerobic activity per week, as recommended by health guidelines.
- Exercise plans should be individualized to meet the specific needs and goals of each person with diabetes.
Nursing Interventions
Nursing interventions for diabetes management are essential in providing holistic care and support to individuals with diabetes. These interventions aim to help clients effectively manage their condition, prevent complications, and improve their overall quality of life. Nursing interventions include blood glucose level monitoring, medication management, health teaching, foot care, and health screening.
Blood Glucose Level Monitoring
During inpatient care, provider orders often indicate bedside blood glucose monitoring before every meal and bedtime. If insulin is prescribed, there is often a “sliding scale” component, where rapid-acting insulin is administered based on the blood glucose level. This sliding scale corrects for the blood sugar level before the meal. Added to this amount are units of insulin for the amount of carbohydrates consumed. Addressing both the blood sugar and quantity of carbohydrates consumed helps maintain tight glycemic control. See a common sliding scale insulin order in the following box.
Example of Sliding Scale Insulin Order
Obtain bedside blood glucose level before meals and bedtime. Use the following scale to administer Humalog insulin based on the blood glucose level:
- 150-199: 2 units
- 200-249: 4 units
- 250-299: 6 units
- 300-349: 8 units
- 350 – 399: 10 units
- 400 or over: Call the provider
Medication Management
Nurses administer prescribed antidiabetic medications during inpatient care and provide health teaching regarding the purpose of the medications, dosages, timing, and potential side effects. It is vital for clients to understand the onset, peak, and duration of insulin, as well as the importance of timing insulin administration with meal intake and carbohydrates consumed to prevent hypoglycemia. Nurses also teach clients how to self-administer insulin with return demonstration to ensure understanding.
Nurses also collaborate with health care providers to adjust medication prescriptions based on clients’ changing needs, responses to treatment, and potential barriers for medication therapy at home.
Foot Care
Clients with diabetes are at high risk for foot ulcers and injuries due to decreased blood flow and sensation of the lower extremities. Good foot care is vital for clients to keep their feet healthy. Nurses teach clients about proper foot care such as inspecting the feet daily (including between the toes), wearing appropriate footwear at all times, and avoiding walking barefoot. If individuals trim their toenails at home, they should do so carefully and immediately report any nonhealing breaks in the skin to their health care provider. During inpatient or long-term care, only podiatrists or specially trained nurses should trim toenails of diabetic clients to prevent unintended injury and potential infection. Annual podiatrist visits are recommended with immediate care for injuries or ulcers to prevent infection and potential amputation. See Figure 7.14[68] for an infographic from the Centers for Disease Control and Prevention on tips for healthy feet.

Health Teaching
Nurses provide comprehensive health teaching to individuals with diabetes and their family members. In many institutions, diabetic nurse educators provide extensive teaching on topics such as the nature of diabetes, blood glucose monitoring, medication management, and lifestyle modifications. However, all nurses continue to reinforce this information during every encounter to help promote effective self-management of this chronic condition. Return demonstration of skills related to blood glucose monitoring and administration of injections are vital to ensure client understanding.
Common health topics include the following:
- Monitoring their blood glucose levels using glucometers or continuous glucose monitoring systems.
- Interpreting blood glucose readings and making necessary adjustments to their treatment plan.
- Recognizing and managing episodes of low blood sugar (hypoglycemia) and high blood sugar (hyperglycemia) and when to notify the provider.
- Performing good foot care.
- Participating in routine care to prevent diabetic complications, such as annual eye and podiatrist exams.
- Understanding the importance of regular exercise and nutritional eating to reduce the risk of atherosclerosis and arteriosclerosis.
- Empowering clients to take an active role in their care by understanding the disease, treatment plan, and appropriate self-management.
- Preparing for sick days to keep blood glucose in target range. See the following box on general teaching to provider about planning for sick days.
Planning for Sick Days
Although a client’s food intake may decrease when ill, their blood glucose can become elevated due to the effects of cortisol that is released as part of the immune response. Clients with diabetes are also at risk for becoming seriously ill from colds or other respiratory viruses. Nurses should teach clients the following sick day guidelines[69]:
- Check your blood glucose at least every four hours and modify your insulin administration according to the results and the instructions provided by your health care provider. Notify your health care provider if your blood glucose is greater than 240 mg/dL.
- Drink plenty of fluids to prevent dehydration. If having difficulty keeping fluids down, try to sip fluids every 15 minutes.
- Eat simple carbohydrates like regular soda, Jell-O, or popsicles to keep your blood glucose up if you are having difficulty eating and are at risk for hypoglycemia.
- If your body does not have enough insulin, it creates ketones, placing you at risk for diabetic ketoacidosis (DKA). If you are at risk, test your urine for ketones every four to six hours or as directed by your health care provider.
- If you are vomiting or have diarrhea more than three times over 24 hours or have a fever over 101° F for 24 hours, call your health care provider.
- Be cautious with using over-the-counter cold medications because they can affect your blood glucose or your prescribed medication.
- Create an action plan with your health care team to use on sick days.
Read more information about planning for sick days from the American Diabetes Association at https://diabetes.org/getting-sick-with-diabetes/sick-days
Health Screenings
Nurses promote routine health screenings for clients with diabetes, including annual eye exams and routine kidney function tests, lipid profiles, and blood pressure monitoring. Kidney function tests often include microalbumin, an early detection of kidney dysfunction. Nurses also coordinate referrals to specialists, such as ophthalmologists, podiatrists, or endocrinologists.
Evaluation
Evaluation focuses on the effectiveness of the nursing interventions by reviewing the client’s expected outcomes to determine if they were met by the time frames indicated. During the evaluation phase, nurses use critical thinking to analyze reassessment data and determine if a client’s expected outcomes have been met, partially met, or not met by the time frames established. If outcomes are not met or only partially met by the time frame indicated, the care plan should be revised. Reassessment should occur every time the nurse interacts with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with others on the interprofessional team.
Nurses refer to the previously identified outcome statements and perform reassessments to determine if they have been met by the current nursing care plan or if additional interventions are required. For example, the nurse would perform assessments related to the previously established outcome criteria and determine if they were “met” or if additional interventions are required.
![]() RN Recap: Diabetes Type 2
RN Recap: Diabetes Type 2
View a brief YouTube video of diabetes mellitus type 2[70]:
Media Attributions
- CDC_Diabetes_Social_Ad_Concept_A2_Facebook
- 4973474372_691d2b2391_h
- Human_insulin_100_IU-1ml_pen_yellow_background_(02)
- 1200px-Wearing_pump
- 5585751341_d0b0df9d56_o
- FreeStyle_libre_am_Oberarm_und_Auslesegerät-5
- 337438-A_FootCare_Infographic_3.10_final
- Mayo Clinic. (2023, June 14). Latent autoimmune diabetes in adults - What is it? https://www.mayoclinic.org/diseases-conditions/type-1-diabetes/expert-answers/lada-diabetes/faq-20057880 ↵
- National Heart, Lung, and Blood Institute. (2022, May 18). What Is metabolic syndrome? National Institutes of Health. https://www.nhlbi.nih.gov/health/metabolic-syndrome ↵
- Robertson, R. P. (2023). Type 2 diabetes mellitus: Prevalence and risk factors. UpToDate. Retrieved October 20, 2023, from https://www.wolterskluwer.com/en/solutions/uptodate ↵
- Inzucchi, S. E., & Lupsa, B. (2022). Glycemic control and vascular complications in type 2 diabetes mellitus. UpToDate. Retrieved October 19, 2023, from https://www.wolterskluwer.com/en/solutions/uptodate ↵
- American Diabetes Association. (n.d.). Hypoglycemia (low blood glucose). https://diabetes.org/living-with-diabetes/treatment-care/hypoglycemia ↵
- American Diabetes Association. (n.d.). Hypoglycemia (low blood glucose). https://diabetes.org/living-with-diabetes/treatment-care/hypoglycemia ↵
- American Diabetes Association. (n.d.). Hypoglycemia (low blood glucose). https://diabetes.org/living-with-diabetes/treatment-care/hypoglycemia ↵
- This work is a derivative of StatPearls by Matthew & Thoppil and is licensed under CC BY 4.0 ↵
- American Diabetes Association. (n.d.). Hypoglycemia. https://diabetes.org/living-with-diabetes/treatment-care/hypoglycemia#:~:text=Treatment%E2%80%94The%20%2215%2D15,at%20least%2070%20mg%2FdL ↵
- This work is a derivative of StatPearls by Brady & Rawla and is licensed under CC BY 4.0 ↵
- Robertson, R. P. (2023). Type 2 diabetes mellitus: Prevalence and risk factors. UpToDate. Retrieved October 20, 2023, from https://www.wolterskluwer.com/en/solutions/uptodate ↵
- This work is a derivative of Endotext by Gosmanov, Gosmanova, & Kitabchi and is licensed under CC BY 4.0 ↵
- Centers for Disease Control and Prevention. (2022, December 30). Low blood sugar. https://www.cdc.gov/diabetes/basics/low-blood-sugar.html ↵
- This work is a derivative of StatPearls by Brady & Rawla and is licensed under CC BY 4.0 ↵
- Robertson, R. P. (2023). Type 2 diabetes mellitus: Prevalence and risk factors. UpToDate. Retrieved October 20, 2023, from www.uptodate.com ↵
- “CDC_Diabetes_Social_Ad_Concept_A2_Facebook” by unknown author for Centers for Disease Control and Prevention is licensed in the Public Domain. Access for free at https://www.cdc.gov/diabetes/basics/getting-tested.html. ↵
- Centers for Disease Control & Prevention. (2023, February 28). Diabetes tests. https://www.cdc.gov/diabetes/basics/getting-tested.html ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2022, July). Diabetes tests and diagnosis. National Institutes of Health. https://www.niddk.nih.gov/health-information/diabetes/overview/tests-diagnosis ↵
- Centers for Disease Control & Prevention. (2023, February 28). Diabetes tests. https://www.cdc.gov/diabetes/basics/getting-tested.html ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2022, July). Diabetes tests and diagnosis. National Institutes of Health. https://www.niddk.nih.gov/health-information/diabetes/overview/tests-diagnosis ↵
- Centers for Disease Control & Prevention. (2023, February 28). Diabetes tests. https://www.cdc.gov/diabetes/basics/getting-tested.html ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2022, July). Diabetes tests and diagnosis. National Institutes of Health. https://www.niddk.nih.gov/health-information/diabetes/overview/tests-diagnosis ↵
- Centers for Disease Control & Prevention. (2023, February 28). Diabetes tests. https://www.cdc.gov/diabetes/basics/getting-tested.html ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2022, July). Diabetes tests and diagnosis. National Institutes of Health. https://www.niddk.nih.gov/health-information/diabetes/overview/tests-diagnosis ↵
- Centers for Disease Control & Prevention. (2023, February 28). Diabetes tests. https://www.cdc.gov/diabetes/basics/getting-tested.html ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2022, July). Diabetes tests and diagnosis. National Institutes of Health. https://www.niddk.nih.gov/health-information/diabetes/overview/tests-diagnosis ↵
- Centers for Disease Control & Prevention. (2023, February 28). Diabetes tests. https://www.cdc.gov/diabetes/basics/getting-tested.html ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2022, July). Diabetes tests and diagnosis. National Institutes of Health. https://www.niddk.nih.gov/health-information/diabetes/overview/tests-diagnosis ↵
- Centers for Disease Control & Prevention. (2023, February 28). Diabetes tests. https://www.cdc.gov/diabetes/basics/getting-tested.html ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2022, July). Diabetes tests and diagnosis. National Institutes of Health. https://www.niddk.nih.gov/health-information/diabetes/overview/tests-diagnosis ↵
- Centers for Disease Control & Prevention. (2023, February 28). Diabetes tests. https://www.cdc.gov/diabetes/basics/getting-tested.html ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2022, July). Diabetes tests and diagnosis. National Institutes of Health. https://www.niddk.nih.gov/health-information/diabetes/overview/tests-diagnosis ↵
- This work is a derivative of StatPearls by Goyal, Singhal, Jialal, & Castano and is licensed under CC BY 4.0 ↵
- This work is a derivative of Nursing Pharmacology 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Ganesan, Rana & Sultan and is licensed under CC BY 4.0 ↵
- This work is a derivative of Nursing Pharmacology 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Ganesan, Rana & Sultan and is licensed under CC BY 4.0 ↵
- American Diabetes Association. (n.d.). What are my options for type 2 diabetes medications? https://diabetes.org/health-wellness/medication/oral-other-injectable-diabetes-medications ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2022, March). Insulin, medicines, & other diabetes treatment. National Institutes of Health. https://www.niddk.nih.gov/health-information/diabetes/overview/insulin-medicines-treatments ↵
- This work is a derivative of StatPearls by Collins & Costello and is licensed under CC BY 4.0 ↵
- This work is a derivative of Nursing Pharmacology 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Ganesan, Rana & Sultan and is licensed under CC BY 4.0 ↵
- This work is a derivative of Nursing Pharmacology 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Ganesan, Rana & Sultan and is licensed under CC BY 4.0 ↵
- This work is a derivative of Nursing Pharmacology 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Ganesan, Rana & Sultan and is licensed under CC BY 4.0 ↵
- This work is a derivative of Nursing Pharmacology 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Ganesan, Rana & Sultan and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Padda, Mahtani & Parmar and is licensed under CC BY 4.0 ↵
- This work is a derivative of Nursing Pharmacology 2e by Open RN and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Ganesan, Rana & Sultan and is licensed under CC BY 4.0 ↵
- American Diabetes Association. (n.d.). What are my options for type 2 diabetes medications? https://diabetes.org/health-wellness/medication/oral-other-injectable-diabetes-medications ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2022, March). Insulin, medicines, & other diabetes treatment. National Institutes of Health. https://www.niddk.nih.gov/health-information/diabetes/overview/insulin-medicines-treatments ↵
- “4973474372_691d2b2391_h.jpg” by Brian J. Matis is licensed under CC BY-NC-SA 2.0 ↵
- This work is a derivative of Nursing Pharmacology 2e by Open RN and is licensed under CC BY 4.0 ↵
- National Institute of Diabetes and Digestive and Kidney Diseases. (2022, March). Insulin, medicines, & other diabetes treatment. National Institutes of Health. https://www.niddk.nih.gov/health-information/diabetes/overview/insulin-medicines-treatments ↵
- “Human_insulin_100_IU-1ml_pen_yellow_background_%2802%29.jpg” by Wesalius is licensed under CC BY 4.0 ↵
- “Wearing_pump.JPG” by Bjorn Heller is licensed under CC BY-SA 2.0 DE LIZENZVERTRAG ↵
- “5585751341_affc34fe84_e.jpg” by Bradley Johnson is licensed under CC BY-NC-ND 2.0 ↵
- “FreeStyle_libre_am_Oberarm_und_Auslesegerät-5.JPG” by Thirunavukkarasye-Raveendran is licensed under CC BY 4.0 ↵
- Lin, C.-L., Huang, L.-C., Chang, Y. T., Chen, R.-Y., & Yang, S.-H. (2021). Effectiveness of health coaching in diabetes control and lifestyle improvement: A randomized-controlled trial. Nutrients, 13(11), 3878. https://doi.org/10.3390/nu13113878 ↵
- Delahanty, L. (2023). Nutritional considerations in type 2 diabetes mellitus. UpToDate. Retrieved October 22, 2023, from www.uptodate.com ↵
- American Diabetes Association. (n.d.). Carb counting and diabetes. https://diabetes.org/food-nutrition/understanding-carbs/carb-counting-and-diabetes ↵
- Delahanty, L. (2023). Nutritional considerations in type 2 diabetes mellitus. UpToDate. Retrieved October 22, 2023, from www.uptodate.com ↵
- American Diabetes Association. (n.d.). Carb counting and diabetes. https://diabetes.org/food-nutrition/understanding-carbs/carb-counting-and-diabetes ↵
- Centers for Disease Control & Prevention. (2022, November 3). Get active! https://www.cdc.gov/diabetes/managing/active.html#:~:text=The%20goal%20is%20to%20get,%2C%20shoulders%2C%20and%20arms) ↵
- Centers for Disease Control & Prevention. (2022, November 3). Get active! https://www.cdc.gov/diabetes/managing/active.html#:~:text=The%20goal%20is%20to%20get,%2C%20shoulders%2C%20and%20arms) ↵
- "337438-A_FootCare_Infographic_3.10_final" by unknown author for Centers for Disease Control and Prevention is licensed in the Public Domain. Access for free at https://www.cdc.gov/diabetes/library/socialmedia/infographics/feet-healthy.html. ↵
- American Diabetes Association. (n.d.). Diabetes and planning for sick days. https://diabetes.org/getting-sick-with-diabetes/sick-days ↵
- Open RN Project. (2024, April 19). Health Alterations - Chapter 7 Endocrine - Diabetes mellitus type 2 [Video]. YouTube. CC BY-NC 4.0 https://youtu.be/d8rPuWVscTk ↵
Answer Key to Chapter 1 Learning Activities
1. D - Patient is experiencing increased difficulty breathing. (Rationale: The severity of an airway concern and the life-threatening nature of the condition necessitates immediate notification of the provider).
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 1 Learning Activities
1. D - Patient is experiencing increased difficulty breathing. (Rationale: The severity of an airway concern and the life-threatening nature of the condition necessitates immediate notification of the provider).
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 2 Learning Activities
1. To demonstrate respect for individual culture beliefs, the nurse should use open-ended questions to explore the patient's culture. Demonstrating engagement and interest in learning more about the patient's culture facilitates therapeutic communication and information sharing. Requesting that the patient share cultural background/information that the patient believes is important to their health care demonstrates respect and inclusion for different cultural beliefs and practices.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 3 Learning Activities
1. To safely obtain an individual's blood pressure, it is important to note the size of the patient to select the appropriate blood pressure cuff size. Additionally, it is important to note if the patient has any limb restrictions, such as an injury, mastectomy, lymph node removal, fistula placement, etc. Blood pressures should not be taken on any limb with a potential restriction.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 4 Learning Activities
1. The five moments of hand hygiene occur: 1) before touching a patient, 2) before a procedure, 3) after a procedure/body fluid exposure risk, 4) after touching a patient, 5) after touching a patient's surroundings.
When entering a patient's room to perform the skill of intermittent catheterization, hand hygiene should be performed:
- Upon entry into the room
- After touching the patient's surroundings and preparing for the procedure
- Before touching the patient
- After the procedure/ body fluid exposure risk
- After touching the patient's surroundings
- Upon exiting the room
2. B - Patient on Clostridium Difficile (C-Diff) contact precautions, D - Hands are visibly soiled
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 5 Learning Activities
Section 5.3 Military Time
- 7:30 PM
- 12:30 AM
- 0900
- 2200
Section 5.4 Household and Metric Equivalents
- 5 mL
- 30 mL
- 500 mg
- 3636 grams
- 0.7 cm
Section 5.5 Rounding
- 6.5
- 6.5
- 5.5
- 5.5
- 0.19
- 0.19
- 0.2
- 0.2
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 5 Learning Activities
Section 5.3 Military Time
- 7:30 PM
- 12:30 AM
- 0900
- 2200
Section 5.4 Household and Metric Equivalents
- 5 mL
- 30 mL
- 500 mg
- 3636 grams
- 0.7 cm
Section 5.5 Rounding
- 6.5
- 6.5
- 5.5
- 5.5
- 0.19
- 0.19
- 0.2
- 0.2
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 6 Learning Activities
- D - remove obstacles when ambulating (Rationale: Cranial nerve II is the optic nerve, which governs vision. The nurse can provide safety for the visually impaired patient by clearing the path of obstacles when ambulating.)
- A - cerebral function (Rationale: The mental status examination assesses functions governed by the cerebrum. Some of these are orientation, attention span, judgment, and abstract reasoning.)
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 6 Learning Activities
- D - remove obstacles when ambulating (Rationale: Cranial nerve II is the optic nerve, which governs vision. The nurse can provide safety for the visually impaired patient by clearing the path of obstacles when ambulating.)
- A - cerebral function (Rationale: The mental status examination assesses functions governed by the cerebrum. Some of these are orientation, attention span, judgment, and abstract reasoning.)
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 7 Learning Activities
1. To alleviate pain and discomfort associated with strep throat, the patient may receive instruction to:
- Drink soothing liquids such as lemon tea with honey or ice water
- Gargle several times a day with warm salt water made of 1/2 tsp. of salt in 1 cup of water
- Suck on hard candies or throat lozenges
- Use a cool-mist vaporizer or humidifier to moisten the air
- Try over-the-counter pain medicines, such as acetaminophen
2. B - white patches noted on both tonsils, D - speech is slurred, E - thyroid enlarged
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 8 Learning Activities
1. Signs of auditory challenges may be reflected with a patient asking the nurse to repeat instruction, tilting the head to one side or angling an ear forward, inappropriate responses, garbled speech, attempts at lipreading, etc.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 8 Learning Activities
1. Signs of auditory challenges may be reflected with a patient asking the nurse to repeat instruction, tilting the head to one side or angling an ear forward, inappropriate responses, garbled speech, attempts at lipreading, etc.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 9 Learning Activities
- C - Heart Failure (Rationale: The patient's symptoms indicate fluid volume overload and reflect a clinical diagnosis of heart failure.)
- B - Stay with the patient and notify the HCP of the ECG results (Rationale: The patient's cardiac rhythm change is reflective of an abnormality. This change should be communicated to the health care provider.)
Answers to H5P interactive elements are given within the interactive element.
Answer Key to Chapter 9 Learning Activities
- C - Heart Failure (Rationale: The patient's symptoms indicate fluid volume overload and reflect a clinical diagnosis of heart failure.)
- B - Stay with the patient and notify the HCP of the ECG results (Rationale: The patient's cardiac rhythm change is reflective of an abnormality. This change should be communicated to the health care provider.)
Answers to H5P interactive elements are given within the interactive element.
Answer Key to Chapter 10 Learning Activities
- B - Sitting upright (Rationale: The patient who is short of breath will experience greatest comfort sitting in an upright position. This position will also allow for comprehensive auscultation of all lung fields.)
- fluid or mucus
- A - Assess pulse oximeter probe site to ensure accurate reading (Rationale: If the patient's clinical presentation does not align with collected metrics, it is important confirm the metric prior to implementing additional action.)
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 10 Learning Activities
- B - Sitting upright (Rationale: The patient who is short of breath will experience greatest comfort sitting in an upright position. This position will also allow for comprehensive auscultation of all lung fields.)
- fluid or mucus
- A - Assess pulse oximeter probe site to ensure accurate reading (Rationale: If the patient's clinical presentation does not align with collected metrics, it is important confirm the metric prior to implementing additional action.)
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 11 Learning Activities
-
Priority Actions First Assess pulse oximetry Second Assess lung sounds Third Apply oxygen as ordered Four Reassess pulse oximetry Fifth Institute actions to improve oxygenation Sixth Teach oxygen safety (Rationale: Priority of actions includes the gathering of assessment information to reflect the patient’s respiratory condition. Once you have collected information, intervention can be initiated with application of oxygen if needed and subsequent reassessment of the pulse oximetry reading. Additional actions to improve patient oxygenation and lung capacity can then be implemented with coughing, deep breathing, and use of incentive spirometry. Finally, once the patient experiences improvement in oxygenation and breathing status, reinforcement of oxygen education and safety measures would be appropriate.)
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 11 Learning Activities
-
Priority Actions First Assess pulse oximetry Second Assess lung sounds Third Apply oxygen as ordered Four Reassess pulse oximetry Fifth Institute actions to improve oxygenation Sixth Teach oxygen safety (Rationale: Priority of actions includes the gathering of assessment information to reflect the patient’s respiratory condition. Once you have collected information, intervention can be initiated with application of oxygen if needed and subsequent reassessment of the pulse oximetry reading. Additional actions to improve patient oxygenation and lung capacity can then be implemented with coughing, deep breathing, and use of incentive spirometry. Finally, once the patient experiences improvement in oxygenation and breathing status, reinforcement of oxygen education and safety measures would be appropriate.)
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 12 Learning Activities
- A - Nausea, B - Vomiting, D - Bloating
- A - Bowel Sounds
- B - There are hypoactive bowel sounds in all quadrants, C - Firmness is palpated in left lower quadrant
- SAMPLE NOTE:
D (SO): Patient reports ongoing constipation without bowel movement for greater than 24 hours. The patient reports intermittent nausea that is increasing in frequency and has had one episode of vomiting. The patient’s abdomen appears bloated, and bowel sounds are hypoactive in all quadrants. There is notable firmness present in the left lower quadrant with palpation. The patient denies tenderness.
A: Provider updated regarding patient’s bowel status and assessment. Order received to administer Milk of Magnesia 30 mL PO times one dose. Medication was administered at 0800.
R (P). Patient reported having a large formed brown stool at 1100. Stool is noted to be soft and brown. Patient reports relief from nausea. Bowel sounds are noted in all quadrants. Will continue to monitor bowel status.
Nurse Signature, Credentials, Date/Time
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 12 Learning Activities
- A - Nausea, B - Vomiting, D - Bloating
- A - Bowel Sounds
- B - There are hypoactive bowel sounds in all quadrants, C - Firmness is palpated in left lower quadrant
- SAMPLE NOTE:
D (SO): Patient reports ongoing constipation without bowel movement for greater than 24 hours. The patient reports intermittent nausea that is increasing in frequency and has had one episode of vomiting. The patient’s abdomen appears bloated, and bowel sounds are hypoactive in all quadrants. There is notable firmness present in the left lower quadrant with palpation. The patient denies tenderness.
A: Provider updated regarding patient’s bowel status and assessment. Order received to administer Milk of Magnesia 30 mL PO times one dose. Medication was administered at 0800.
R (P). Patient reported having a large formed brown stool at 1100. Stool is noted to be soft and brown. Patient reports relief from nausea. Bowel sounds are noted in all quadrants. Will continue to monitor bowel status.
Nurse Signature, Credentials, Date/Time
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 13 Learning Activities
- A - It measures muscle strength symmetry.
- C - 5 out of 5
- B - Inspection
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 14 Learning Activities
- A patient admitted with diarrhea is at risk for skin breakdown and dehydration. Assessment of the patient’s skin condition and hydration status would be important for assessing the severity of the patient’s illness. Hydration status can be assessed through evaluation of skin turgor with this patient due to normal skin elasticity in this age group.
Answers to interactive elements are given within the interactive element.
[latexpage]
Answer Key to Chapter 15 Learning Activities
- Dimensional Analysis:\[\frac{750~mg}{x~mL}~x~\frac{1~g}{1000~mg}~x~\frac{8~mL}{2~g}~=~\frac{6000}{2000}~=~{3~mL}\]
Ratio Proportion:
\[
\frac{750~mg}{X~mL}~=~\frac{2000~mg}{ 8~mL}
\]
\[
{750~mg}~x~{8~mL}~=~{2000~mg}~x~{X~mL}
\]
\[
\frac{6000~mg}{mL}~=~{2000~mg}~x~{X~mL}
\]
\[
\frac{6000~\cancel{mg}~mL}{2000~\cancel{mg}}~=~{X~mL}
\]
\[
3~mL~=~X~mL
\]
- If an incorrect medication is given, the nurse should promptly take the following actions:
- Assess the patient given the wrong medication. Assess for adverse effects related to the error.
- Notify the nurse manager/primary care provider regarding the medication error.
- Discuss the course of action to be taken.
- Implement action and continue to monitor the patient for signs of complication or change in condition.
- Report the incident via institution policy.
Answers to interactive elements are given within the interactive element.
[latexpage]
Answer Key to Chapter 15 Learning Activities
- Dimensional Analysis:\[\frac{750~mg}{x~mL}~x~\frac{1~g}{1000~mg}~x~\frac{8~mL}{2~g}~=~\frac{6000}{2000}~=~{3~mL}
\]
Ratio Proportion:
\[
\frac{750~mg}{X~mL}~=~\frac{2000~mg}{ 8~mL}
\]
\[
{750~mg}~x~{8~mL}~=~{2000~mg}~x~{X~mL}
\]
\[
\frac{6000~mg}{mL}~=~{2000~mg}~x~{X~mL}
\]
\[
\frac{6000~\cancel{mg}~mL}{2000~\cancel{mg}}~=~{X~mL}
\]
\[
3~mL~=~X~mL
\]
- If an incorrect medication is given, the nurse should promptly take the following actions:
- Assess the patient given the wrong medication. Assess for adverse effects related to the error.
- Notify the nurse manager/primary care provider regarding the medication error.
- Discuss the course of action to be taken.
- Implement action and continue to monitor the patient for signs of complication or change in condition.
- Report the incident via institution policy.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 16 Learning Activities
- Patients suffering from nausea or experiencing difficulty swallowing may not tolerate medications administered via the enteral route. For a patient experiencing pain, appropriate alternate methods of medication administration may be transdermal medication administration. Transdermal medications are beneficial in that they provide a consistent level of drug into the bloodstream during distribution.
- B - when placing a patch, the nurse should press firmly to the skin to ensure adequate adherence, C - gloves are required for patch application and removal, E - date and location of patch application should be promptly documented in the medication administration record (MAR).
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 16 Learning Activities
- Patients suffering from nausea or experiencing difficulty swallowing may not tolerate medications administered via the enteral route. For a patient experiencing pain, appropriate alternate methods of medication administration may be transdermal medication administration. Transdermal medications are beneficial in that they provide a consistent level of drug into the bloodstream during distribution.
- B - when placing a patch, the nurse should press firmly to the skin to ensure adequate adherence, C - gloves are required for patch application and removal, E - date and location of patch application should be promptly documented in the medication administration record (MAR).
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 17 Learning Activities
- D - slow or stop the infusion based on the patient's response.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 17 Learning Activities
- D - slow or stop the infusion based on the patient's response.
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 18 Learning Activities
- The optimal size needle would be 23G ⅝ inch with injection into the deltoid muscle. With the limited amount of fat tissue, a ⅝-inch needle will be sufficient for entering the muscular tissue. Additionally, a 23G diameter needle is adequate for aqueous and water-based medications.
- The optimal size needle would be 21G 1 1/2inch with injection into the ventrogluteal area. With the excess amount of adipose tissue, the nurse should ensure that the length of the needle would be appropriate to reach the intramuscular route.
- A - Injects 5 units of air into the regular insulin vial first and withdraws 5 units of regular insulin
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 18 Learning Activities
- The optimal size needle would be 23G ⅝ inch with injection into the deltoid muscle. With the limited amount of fat tissue, a ⅝-inch needle will be sufficient for entering the muscular tissue. Additionally, a 23G diameter needle is adequate for aqueous and water-based medications.
- The optimal size needle would be 21G 1 1/2inch with injection into the ventrogluteal area. With the excess amount of adipose tissue, the nurse should ensure that the length of the needle would be appropriate to reach the intramuscular route.
- A - Injects 5 units of air into the regular insulin vial first and withdraws 5 units of regular insulin
Answers to interactive elements are given within the interactive element.
Answer Key to Chapter 21 Learning Activities
-
- Deflate the balloon, ensure flow of urine, advance the catheter, and attempt reinflation.
- Utilize assistant to help with positioning and holding. Manipulation of the left leg should only occur, and additional personnel may be needed to assist in holding, providing light source, and retracting skin as needed.
- The patient should be encouraged to verbalize feelings related to the colostomy. Body image issues can be a significant concern with new stoma creation. The nurse should ensure that the patient is allowed to voice their feelings, while also reinforcing the measures required to provide care. Education regarding colostomy management can aid in empowerment and facilitate the beginning of normalization. Additionally, it can be helpful to provide guidance on measures for dress to accommodate the colostomy.
- C - Straight catheter
- C - Document the assessment findings of the stoma.
- A - "I should plan to replace the pouch system every 8-10 days."
Answers to interactive elements are given within the interactive element.
Checklists
Checklist for Handwashing
- Use the checklist below to review the steps for completion of "Hand Hygiene With Soap and Water."
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Remove jewelry according to agency policy; push your sleeves above your wrists.
- Turn on the water and adjust the flow so that the water is warm. Wet your hands thoroughly, keeping your hands and forearms lower than your elbows. Avoid splashing water on your uniform.
- Apply a palm-sized amount of hand soap.
- Perform hand hygiene using plenty of lather and friction for at least 15 seconds:
- Rub hands palm to palm
- Back of right and left hand (fingers interlaced)
- Palm to palm with fingers interlaced
- Rotational rubbing of left and right thumbs
- Rub your fingertips against the palm of your opposite hand
- Rub wrists
- Repeat sequence at least 2 times
- Keep fingertips pointing downward throughout
- Clean under your fingernails with disposable nail cleaner (if applicable).
- Wash for a minimum of 20 seconds.
- Keep your hands and forearms lower than your elbows during the entire washing.
- Rinse your hands with water, keeping your fingertips pointing down so water runs off your fingertips. Do not shake water from your hands.
- Do not lean against the sink or touch the inside of the sink during the hand-washing process.
- Dry your hands thoroughly from your fingers to wrists with a paper towel or air dryer.
- Dispose of the paper towel(s).
- Use a new paper towel to turn off the water.
- Dispose of the paper towel.
Checklist for using Hand Sanitizer
- Use the checklist below to review the steps for completion of "Hand Hygiene With Alcohol-Based Hand Sanitizer."
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
-
- Gather supplies (antiseptic hand rub).
- Remove jewelry according to agency policy; push your sleeves above your wrists.
- Apply enough product into the palm of one hand and enough to cover your hands thoroughly, per product directions.
- Rub your hands together, covering all surfaces of your hands and fingers with antiseptic until the alcohol is dry (a minimum of 20-30 seconds):
- Rub hands palm to palm
- Back of right and left hand (fingers interlaced)
- Palm to palm with fingers interlaced
- Rotational rubbing of left and right thumbs
- Rub your fingertips against the palm of your opposite hand
- Rub your wrists
- Repeat hand sanitizing sequence a minimum of two times.
- Repeat hand sanitizing sequence until the product is dry.
Checklist for Vital Signs
(See “Blood Pressure” chapter for Manual Blood Pressure Checklist)
- Knock, enter the room, greet the patient, and provide for privacy.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Perform hand hygiene and clean the stethoscope before approaching the patient.
- Ask the patient their name and date of birth for the first identifier and verify wristband while the patient is stating information. Then use one of the following for the second identifier:
- Scan wristband
- Compare name/DOB to MAR
- Ask staff to verify patient (LTC setting)
- Compare picture on MAR to patient
- Explain the procedure to the patient; ask if they have any questions.
- Obtain temperature using correct technique in Celsius. Inform instructor if temperature is out of range. Normal range: 98.6 F or 37 C.
- Obtain accurate pulse using radial artery. Inform instructor if pulse is out of range. Normal range for a pulse in an adult: 60-100 with regular rhythm.
- Obtain accurate respiratory rate over 60 seconds. Inform instructor if respiratory rate is out of range. Normal range for respiratory rate in an adult: 12-20.
- Obtain oxygen saturation reading (SpO2) using a pulse oximeter. Inform instructor if SpO2 is out of range. Normal range for SpO2: 94-100%.
- Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Perform hand hygiene and clean the stethoscope.
- Follow the agency policy for following up on vital signs outside of normal range.
- Document vital signs.

