5.5 Hypertension
Open Resources for Nursing (Open RN)
Overview
Normal blood pressure is defined as less than 120/80 mm Hg in adults. Hypertension refers to chronically elevated blood pressure greater than 120/80 mm Hg. Hypertension is very common, affecting millions of individuals worldwide. See Figure 5.26[1] for an image of a health care professional obtaining a blood pressure reading.

There are several classifications of blood pressure based on the systolic and diastolic readings. See Table 5.5 for classifications of hypertension according to the American Heart Association.[2]
Table 5.5. Blood Pressure Classifications[3]
| Blood Pressure Classification | Systolic (mm Hg) | Diastolic (mm Hg) |
|---|---|---|
| Normal | Less than 120 | Less than 80 |
| Elevated (Prehypertension) | 120-129 | Less than 80 |
| Hypertension Stage 1 | 130-139 | 80-89 |
| Hypertension Stage 2 | 140 or higher | 90 or higher |
| Hypertensive Crisis | Higher than 180 | Higher than 120 |
Causes of Hypertension
Hypertension can be due to a primary cause or as a secondary cause. Primary hypertension is the most common type of hypertension and has no identifiable cause. It typically develops gradually over time and is influenced by various risk factors such as genetics, age, race, diet, lifestyle, and stress.
Secondary hypertension is the result of an underlying medical condition or medication. Conditions such as kidney disease, hormonal disorders, or the use of medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), pseudoephedrine or phenylephrine, and estrogen-containing birth control pills can contribute to secondary hypertension. Additionally, medical conditions like diabetes, kidney disease, and sleep apnea can increase one’s risk of developing hypertension.
Risk factors for developing hypertension include age, family history, and lifestyle factors. Individuals with obesity, diets high in sodium, excessive alcohol intake, chronic stress, and limited physical activity are at higher risk for developing hypertension.[4] For this reason, health teaching about lifestyle modifications is essential for nurses to provide to clients experiencing prehypertension or hypertension.
Assessment
Many individuals with hypertension have no symptoms and are unaware of the condition until they have an elevated blood pressure reading collected. If individuals have an elevated blood pressure reading, providers will typically repeat the reading at another appointment before making a diagnosis and beginning treatment. They may ask the individual to collect blood pressures at various dates/times at home or when out in the community and keep a tracking log. Many individuals with hypertension are asymptomatic although some develop symptoms as a result of hypertension, such as a headache, dizziness, or fainting.[5] Untreated hypertension can lead to significant health complications such as myocardial infarction (heart attack), heart failure, cerebrovascular accident (stroke), vision loss, kidney damage.
Diagnostic Testing
Diagnostic testing for hypertension involves recording blood pressures on at least two separate occasions. Blood pressure should be measured in both arms while a client is seated and relaxed. Many providers who suspect hypertension will also evaluate for signs of organ damage as a result of sustained elevated blood pressures. These evaluations may include an echocardiogram to examine for left ventricular hypertrophy (enlargement), fundoscopic examination of retinal blood vessels within the eyes, and kidney function tests to evaluate for elevated levels of serum creatinine or decreased glomerular filtration rate (GFR).[6],[7] Review normal reference ranges for common diagnostic tests in “Appendix A – Normal Reference Ranges.”
Read additional information about how to accurately obtain a blood pressure reading in the “Blood Pressure” chapter of Open RN Nursing Skills, 2e.
Nursing Diagnoses
Nursing priorities for clients diagnosed with hypertension include managing blood pressure levels, promoting healthy lifestyle modifications, and providing health teaching. Common nursing diagnoses for clients with hypertension are as follows[8]:
- Risk for Decreased Cardiac Output
- Risk for Unstable Blood Pressure
- Readiness for Enhanced Health Self-Management
Outcome Identification
Outcome identification involves setting short- and long-term goals and creating expected outcome statements tailored to the client’s specific needs. These outcomes should be measurable and responsive to nursing interventions.
These are some sample expected outcomes for common nursing diagnoses related to hypertension:
- The client will demonstrate improved knowledge of hypertension management by verbalizing three lifestyle modifications.
- The client will maintain blood pressure within the recommended target range of SBP between 100-119 mm Hg and DBP less than 80 mm Hg.
- The client will actively engage in self-monitoring blood pressure and maintain a record of readings to bring to the next appointment.
- The client will verbalize three symptoms of reduced tissue perfusion to promptly report to the health care provider.
Interventions
Medical Interventions
Medical interventions play an important role in managing hypertension. These interventions are important for minimizing impact on other organs and potential complications like heart failure, kidney disease, and vision loss.
Lifestyle Modifications
Lifestyle changes are often the first step in hypertension management and can be effective in lowering blood pressure. Recommendations may include the following:
- Dietary Changes: Reducing sodium intake, following a heart-healthy diet (such as the DASH or Mediterranean diets), and limiting alcohol intake.
- Regular Physical Activity: Engaging in regular aerobic exercise, such as brisk walking or swimming, as recommended by a health care provider.
- Weight Management: Achieving and maintaining a healthy weight through diet and exercise.
- Smoking Cessation: Encouraging smoking cessation and providing resources when the client is ready to quit.
Medication Management
Antihypertensive medications are prescribed to control blood pressure, especially if lifestyle modifications alone are insufficient. Classes of medications used to treat hypertension include the following[9],[10]:
- Diuretics: Eliminate excess sodium and fluid, thus reducing blood volume and blood pressure.
- Beta-Blockers: Block beta-receptors, causing decreased heart rate and force of heart contractions, thus lowering blood pressure. Select beta-blockers may appear to also cause vasodilation through the alpha-1 receptor blockade.
- Angiotensin-converting enzyme (ACE) Inhibitors: Block the conversion of Angiotensin I to Angiotensin II in the renin-angiotensin-aldosterone system, leading to vasodilation and sodium and water excretion, thus lowering blood pressure.
- Angiotensin II Receptor Blockers (ARBs): Block the effects of Angiotensin II, a hormone that causes vasoconstriction, thus lowering blood pressure.
- Calcium Channel Blockers: Relax blood vessels by blocking calcium, thus causing vasodilation and decreased blood pressure.
- Alpha-Agonists: Stimulate alpha-receptors, promoting vasodilation and reducing blood pressure.
- Direct Vasodilators: Directly relax vascular smooth muscle, causing vasodilation and reducing blood pressure.
Read additional information about antihypertensive medications in the “Antihypertensives” section of the “Cardiovascular & Renal Systems” chapter in Open RN Nursing Pharmacology, 2e.
Nursing Interventions
Nursing interventions for hypertension management are essential in helping clients maintain healthy blood pressure levels and prevent complications due to damage to other organs such as the heart, kidneys, brain, and eyes.
Blood Pressure Monitoring
Nurses teach clients how to accurately measure their blood pressure at home and record blood pressure readings in a log. They encourage clients to share home blood pressure logs during follow-up appointments with their health care provider.
Medication Management
Nurses safely administer antihypertensive medications and provide health teaching about their role in blood pressure management, potential side effects, and when to notify the provider. They teach clients about the importance of adhering to their prescribed drug treatment regimen and to consult with their provider before making any changes.
Health Teaching
Health teaching focuses on empowering clients to make healthy lifestyle changes to maintain normal blood pressure.
Lifestyle Modification
Nurses teach clients about the importance of blood pressure control to prevent damage to other organs. They also teach about recommended dietary changes (such as a low-sodium diet), regular exercise, and smoking cessation to promote heart health.
Stress Management
Nurses teach relaxation techniques and stress management strategies, such as deep breathing exercises, progressive muscle relaxation, or guided imagery. They promote healthy coping mechanisms and encourage clients to seek counseling if needed.
Evaluation
During the evaluation stage, nurses determine the effectiveness of nursing interventions for a specific client. The previously identified expected outcomes are reviewed to determine if they were met, partially met, or not met by the time frames indicated. If outcomes are not met or only partially met by the time frame indicated, the nursing care plan is revised. Evaluation should occur every time the nurse implements interventions with a client, reviews updated laboratory or diagnostic test results, or discusses the care plan with other members of the interprofessional team.
![]() RN Recap: Hypertension
RN Recap: Hypertension
View a brief YouTube video overview of hypertension[11]:
Media Attributions
- 361018310_5e1e670da6_o
- RN Recap Icon
- “Monthly check up” by Bryan Mason is licensed under CC BY 2.0 ↵
- Basile, J., & Bloch, M. J. (2023). Overview of hypertension in adults. UpToDate. Retrieved August 29, 2023, from https://www.uptodate.com/ ↵
- Basile, J., & Bloch, M. J. (2023). Overview of hypertension in adults. UpToDate. Retrieved August 29, 2023, from https://www.uptodate.com/ ↵
- Mann, J., & Flack, J. M. (2023). Choice of drug therapy in primary hypertension. UpToDate. Retrieved August 29, 2023, from https://www.uptodate.com/ ↵
- Basile, J., & Bloch, M. J. (2023). Overview of hypertension in adults. UpToDate. Retrieved August 29, 2023, from https://www.uptodate.com/ ↵
- Basile, J., & Bloch, M. J. (2023). Overview of hypertension in adults. UpToDate. Retrieved August 29, 2023, from https://www.uptodate.com/ ↵
- Mann, J., & Flack, J. M. (2023). Choice of drug therapy in primary hypertension. UpToDate. Retrieved August 29, 2023, from https://www.uptodate.com/ ↵
- Flynn Makic, M. B., & Martinez-Kratz, M. R. (2023). Ackley and Ladwig’s Nursing diagnosis handbook: An evidence-based guide to planning care. (13th ed.). ↵
- Basile, J., & Bloch, M. J. (2023). Overview of hypertension in adults. UpToDate. Retrieved August 29, 2023, from https://www.uptodate.com/ ↵
- Mann, J., & Flack, J. M. (2023). Choice of drug therapy in primary hypertension. UpToDate. Retrieved August 29, 2023, from https://www.uptodate.com/ ↵
- Open RN Project. (2024, June 23). Health Alterations - Chapter 5 -Hypertension [Video]. You Tube. CC BY-NC 4.0 https://youtu.be/NSiJp4OjLiA?si=3rwB6IBKQKwvQcy1 ↵
What is Blood Pressure?
A blood pressure reading is the measurement of the force of blood against the walls of the arteries as the heart pumps blood through the body. It is reported in millimeters of mercury (mmHg). This pressure changes in the arteries when the heart is contracting compared to when it is resting and filling with blood. Blood pressure is typically expressed as the reflection of two numbers, systolic pressure and diastolic pressure. The systolic blood pressure is the maximum pressure on the arteries during systole, the phase of the heartbeat when the ventricles contract. This is the top number of a blood pressure reading. Systole causes the ejection of blood out of the ventricles and into the aorta and pulmonary arteries. The diastolic blood pressure is the resting pressure on the arteries during diastole, the phase between each contraction of the heart when the ventricles are filling with blood. This is the bottom number of the blood pressure reading.[1] Therefore, 120/80 indicates the systolic blood pressure is 120 mm Hg and the diastolic blood pressure is 80 mm Hg.
Blood pressure measurements are obtained using a stethoscope and a sphygmomanometer, also called a blood pressure cuff. To obtain a manual blood pressure reading, the blood pressure cuff is placed around a patient's extremity, and a stethoscope is placed over an artery. For most blood pressure readings, the cuff is usually placed around the upper arm, and the stethoscope is placed over the brachial artery. The cuff is inflated to constrict the artery until the pulse is no longer palpable, and then it is deflated slowly. The American Heart Association (AHA) recommends that the blood pressure cuff be inflated at least 30 mmHg above the point at which the radial pulse is no longer palpable. The first appearance of sounds, called Korotkoff sounds, are noted as the systolic blood pressure reading. Korotkoff sounds are named after Dr. Korotkoff, who first discovered the audible sounds of blood pressure when the arm is constricted.[2] The blood pressure cuff continues to be deflated until Korotkoff sounds disappear. The last Korotkoff sounds reflect the diastolic blood pressure reading.[3] It is important to deflate the cuff slowly at no more than 2-3 mmHg per second to ensure that the absence of pulse is noted promptly and that the reading is accurate. Blood pressure readings are documented as systolic blood pressure/diastolic pressure, for example, 120/80 mmHg.
Abnormal blood pressure readings can signify an area of concern and a need for intervention. Normal adult blood pressure is less than 120/80 mmHg. Hypertension is the medical term for elevated blood pressure readings of 130/80 mmHg or higher. See Table 3.2 for blood pressure categories according to the 2017 American College of Cardiology and American Heart Association Blood Pressure Guidelines.[4] Prior to diagnosing a person with hypertension, the health care provider will calculate an average blood pressure based on two or more blood pressure readings obtained on two or more occasions.
For more information about hypertension and blood pressure medications, visit the "Cardiovascular and Renal System" chapter in Open RN Nursing Pharmacology.
Hypotension is the medical term for low blood pressure readings less than 90/60 mmHg.[5] Hypotension can be caused by dehydration, bleeding, cardiac conditions, and the side effects of many medications. Hypotension can be of significant concern because of the potential lack of perfusion to critical organs when blood pressures are low. Orthostatic hypotension is a drop in blood pressure that occurs when moving from a lying down (supine) or seated position to a standing (upright) position. When measuring blood pressure, orthostatic hypotension is defined as a decrease in blood pressure by at least 20 mmHg systolic or 10 mmHg diastolic within three minutes of standing. When a person stands, gravity moves blood from the upper body to the lower limbs. As a result, there is a temporary reduction in the amount of blood in the upper body for the heart to pump, which decreases blood pressure. Normally, the body quickly counteracts the force of gravity and maintains stable blood pressure and blood flow. In most people, this transient drop in blood pressure goes unnoticed. However, some patients with orthostatic hypotension can experience light-headedness, dizziness, or fainting. This is a significant safety concern because of the increased risk of falls and injury, particularly in older adults.[6] Orthostatic hypotension is also commonly referred to a postural hypotension. When obtaining orthostatic vital signs, the pulse rate may also be collected. If the pulse increases by 30 beats/minute or more while the patient stands (or sits if unable to stand), this indicates a significant change.
Perform the following actions when obtaining orthostatic vital signs:
- Have the patient stand upright for 1 minute if able.
- Obtain the blood pressure measurement while the patient stands using the same arm and the same equipment as the previous measurement that was taken with patient lying or sitting.
- Obtain the radial pulse again.
- Repeat the blood pressure and radial pulse measurements again at 3 minutes. Waiting several minutes before repeating the measurements allows time for the autonomic nervous system to compensate for blood volume shifts after position change in the patient without orthostatic hypotension.
- If the patient has symptoms that suggest orthostatic hypotension but doesn't have documented orthostatic hypotension, repeat blood pressure measurement.
Tip: Some patients may not demonstrate significant decreases in blood pressure until they stand for more than 3 minutes.
Table 3.2 Blood Pressure Categories[7]
| Blood Pressure Category | Systolic mm Hg | Diastolic mm Hg |
|---|---|---|
| Normal | Less than 120 | Less than80 |
| Elevated | 120-129 | Less than 80 |
| Stage 1 | 130-139 | 80-89 |
| Stage 2 | 140 or higher | Greater or equal to 90 |
| Hypertensive Crisis | Greater than 180 | Greater than 120 |
View Ahmend Alzawi's Korotkoff sounds video on YouTube.[8]
Equipment to Measure Blood Pressure
Manual Blood Pressure
A sphygmomanometer, commonly called a blood pressure cuff, is used to measure blood pressure while Korotkoff sounds are auscultated using a stethoscope. See Figure 3.1[9] for an image of a sphygmomanometer.
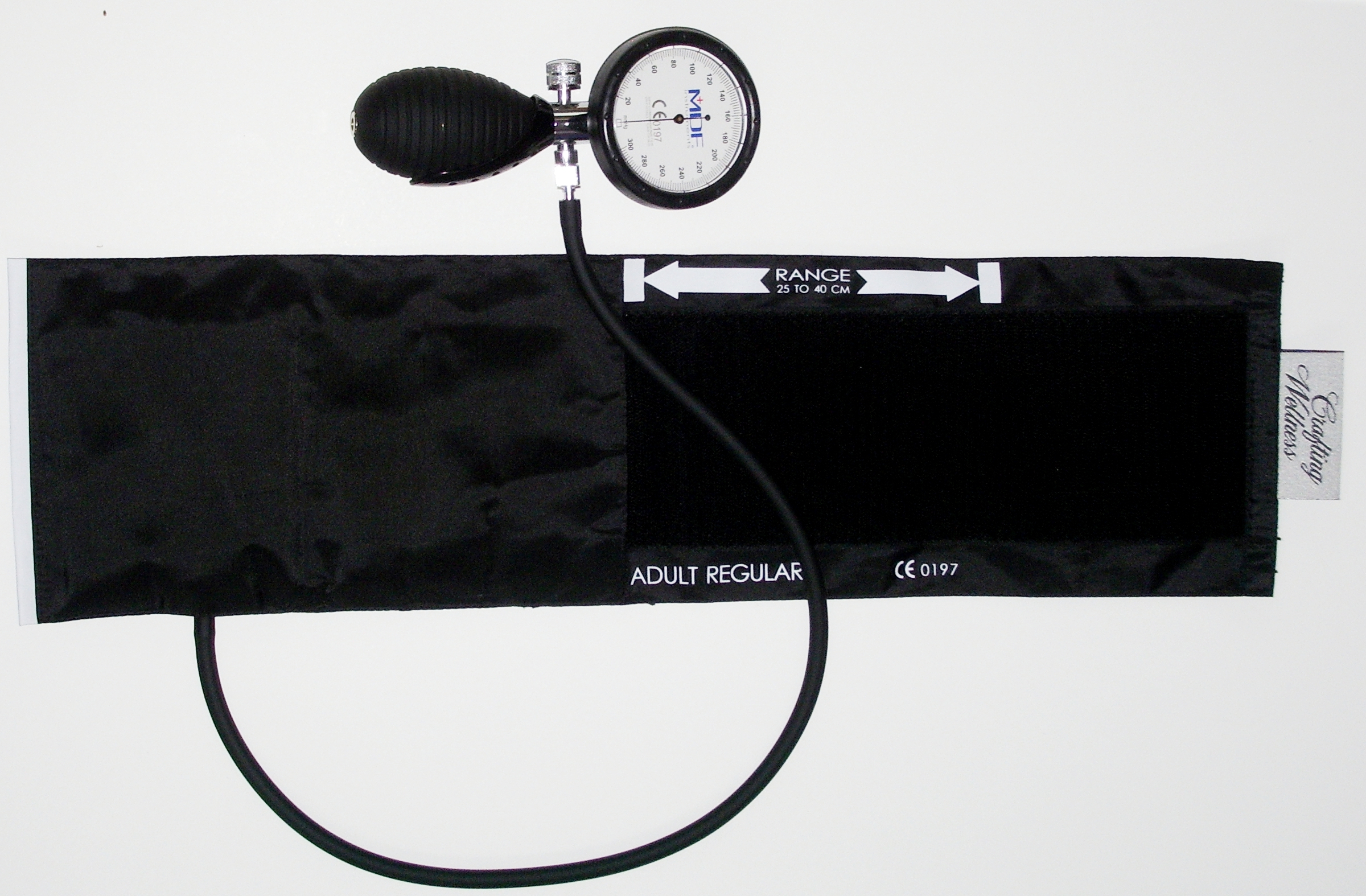
There are various sizes of blood pressure cuffs. It is crucial to select the appropriate size for the patient to obtain an accurate reading. An undersized cuff will cause an artificially high blood pressure reading, and an oversized cuff will produce an artificially low reading. See Figure 3.2[10] for an image of various sizes of blood pressure cuffs ranging in size for a large adult to an infant.

The width of the cuff should be 40% of the person’s arm circumference, and the length of the cuff’s bladder should be 80–100% of the person’s arm circumference. Keep in mind that only about half of the blood pressure cuff is the bladder and the other half is cloth with a hook and loop fastener to secure it around the arm.
View Ryerson University's accurate blood pressure cuff sizing video on YouTube.[11]
Automatic Blood Pressure Equipment
Automatic blood pressure monitors are often used in health care settings to efficiently measure blood pressure for multiple patients or to repeatedly measure a single patient’s blood pressure at a specific frequency such as every 15 minutes. See Figure 3.3[12] for an image of an automatic blood pressure monitor. To use an automatic blood pressure monitor, appropriately position the patient and place the correctly sized blood pressure cuff on their bare arm or other extremity. Press the start button on the monitor. The cuff will automatically inflate and then deflate at a rate of 2 mmHg per second. The monitor digitally displays the blood pressure reading when done. If the blood pressure reading is unexpected, it is important to follow up by obtaining a reading using a manual blood pressure cuff. Additionally, automatic blood pressure monitors should not be used if the patient has a rapid or irregular heart rhythm, such as atrial fibrillation, or has tremors as it may lead to an inaccurate reading.

Sample Documentation of Expected Findings
Blood pressure 120/80 on the left arm with the patient in a seated position using a manual cuff.
Sample Documentation of Unexpected Findings
Blood pressure reading on right arm 160/95. Blood pressure reading left arm 154/93 after patient rested 5 minutes. Reports no history of hypertension and currently not taking any blood pressure medications. Denies dizziness, headache, visual changes, or light-headedness. Dr. Smith notified of all of above and order for furosemide 20 mg PO now received.
Sample Documentation of Expected Findings
Blood pressure 120/80 on the left arm with the patient in a seated position using a manual cuff.
Sample Documentation of Unexpected Findings
Blood pressure reading on right arm 160/95. Blood pressure reading left arm 154/93 after patient rested 5 minutes. Reports no history of hypertension and currently not taking any blood pressure medications. Denies dizziness, headache, visual changes, or light-headedness. Dr. Smith notified of all of above and order for furosemide 20 mg PO now received.

