Diagnosis
Open Resources for Nursing (Open RN)
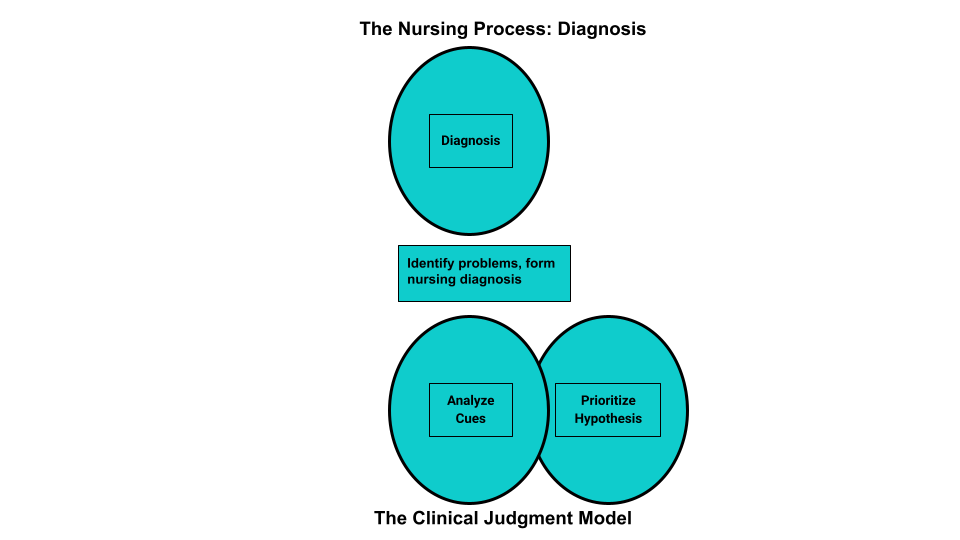
Diagnosis is the second step of the nursing process (and the second Standard of Practice by the American Nurses Association). This standard is defined as, “The registered nurse analyzes assessment data to determine actual or potential diagnoses, problems, and issues.” The RN “prioritizes diagnoses, problems, and issues based on mutually established goals to meet the needs of the health care consumer across the health–illness continuum and the care continuum.” Diagnoses, problems, strengths, and issues are documented in a manner that facilitates the development of expected outcomes and a collaborative plan.[1] See Figure 4.7a for an illustration of how the Diagnosis phase of the nursing process corresponds to the NCSBN Clinical Judgment Measurement Model (NCJMM).[2]
Analyzing Assessment Data
After collection of assessment data, the RN analyzes the data to form generalizations and create and prioritize hypotheses for nursing diagnoses. Steps for analyzing assessment data include performing data analysis, clustering information, identifying hypotheses for potential nursing diagnosis, performing additional in-depth assessment as needed, and establishing nursing diagnosis statements. The nursing diagnoses are then prioritized and the nursing care plan is developed based on them.[3] Analyzing assessment data is completed by an RN and falls outside of the scope of practice of the LPN/VN. However, LPN/VNs must understand data analysis so that new, concerning data is promptly reported to the RN for follow-up.
Performing Data Analysis
After nurses collect assessment data from a client, they use their nursing knowledge to analyze that data to determine if it is “expected” or “unexpected” or “normal” or “abnormal” for that client according to their age, development, and baseline status. From there, nurses determine what data is “clinically relevant” as they prioritize their nursing care.[4]
Example of Analyzing Cues
In Scenario C in the “Assessment” section of this chapter, the nurse analyzes the vital signs data and determines the blood pressure, heart rate, and respiratory rate are elevated, and the oxygen saturation is decreased for this client. These findings are considered “relevant cues” because they are abnormal compared to this client’s baseline and may indicate a new health problem or complication is occurring.
Clustering Information/Seeing Patterns/Making Hypotheses
After analyzing the data and determining relevant cues, the nurse begins clustering data into similar domains or patterns. Evidence-based assessment frameworks, such as Gordon’s Functional Health Patterns, assist nurses in clustering data based on patterns of human responses. See the box below for an outline of Gordon’s Functional Health Patterns.[5] Concepts related to many of these patterns will be discussed in chapters later in this book.
Gordon’s Functional Health Patterns[6]
Health Perception-Health Management: A client’s perception of their health and well-being and how it is managed
Nutritional-Metabolic: Food and fluid consumption relative to metabolic need
Elimination: Excretory function, including bowel, bladder, and skin
Activity-Exercise: Exercise and daily activities
Sleep-Rest: Sleep, rest, and daily activities
Cognitive-Perceptual: Perception and cognition
Self-perception and Self-concept: Self-concept and perception of self-worth, self-competency, body image, and mood state
Role-Relationship: Role engagements and relationships
Sexuality-Reproductive: Reproduction and satisfaction or dissatisfaction with sexuality
Coping-Stress Tolerance: Coping and effectiveness in terms of stress tolerance
Value-Belief: Values, beliefs (including spiritual beliefs), and goals that guide choices and decisions
Example of Using Gordon’s Health Patterns to Cluster Data
Refer to Scenario C in the “Assessment” section of this chapter. The nurse clusters the following relevant cues: elevated blood pressure, elevated respiratory rate, crackles in the lungs, weight gain, worsening edema, shortness of breath, medical history of heart failure, and currently prescribed a diuretic medication into a pattern of fluid balance, which can be classified under Gordon’s Nutritional-Metabolic Functional Health Pattern. Based on the related data in this cluster, the nurse makes a hypothesis that the client has excess fluid volume present.
Identifying Nursing Diagnoses
After the nurse has analyzed and clustered the data from the client assessment, the next step is to begin to answer the question, “What are my client’s human responses to their health condition(s) (i.e., their nursing diagnoses)?” A nursing diagnosis is defined as, “A clinical judgment concerning a human response to health conditions/life processes, or a vulnerability for that response, by an individual, family, group, or community.”[7] Nursing diagnoses are customized to each client and drive the development of the nursing care plan. The nurse should refer to a care planning resource and review the definitions and defining characteristics of the hypothesized nursing diagnoses to determine if additional in-depth assessment is needed before selecting the most accurate nursing diagnosis. Formulation of nursing diagnoses is completed by an RN and is outside the scope of practice of LPN/VNs.
Nursing diagnoses are developed by nurses, for use by nurses. For example, NANDA International (NANDA-I) is a global professional nursing organization that develops nursing terminology that names actual or potential human responses to health problems and life processes based on research findings.[8] Currently, there are over 220 NANDA-I nursing diagnoses developed by nurses around the world. This list is continuously updated, with new nursing diagnoses added and old nursing diagnoses retired that no longer have supporting evidence. A list of commonly used NANDA-I diagnoses is listed in Appendix A. For a full list of NANDA-I nursing diagnoses, refer to a current nursing care plan reference.
NANDA-I nursing diagnoses are grouped into 13 domains that assist the nurse in selecting diagnoses based on the patterns of clustered data. These domains are similar to Gordon’s Functional Health Patterns and include health promotion, nutrition, elimination and exchange, activity/rest, perception/cognition, self-perception, role relationship, sexuality, coping/stress tolerance, life principles, safety/protection, comfort, and growth/development.
NANDA Diagnoses and the NCLEX
Knowledge regarding specific NANDA-I nursing diagnoses is not assessed on the NCLEX. However, analyzing cues, clustering data, forming appropriate hypotheses, and prioritizing hypotheses are components of clinical judgment assessed on the NCLEX and used in nursing practice. Read more about the Next Generation NCLEX in the “Scope of Practice” chapter.
Nursing Diagnoses vs. Medical Diagnoses
You may be asking yourself, “How are nursing diagnoses different from medical diagnoses?” Medical diagnoses focus on diseases or other medical problems that have been identified by the physician, physician’s assistant, or advanced nurse practitioner. Nursing diagnoses focus on the human response to health conditions and life processes and are made independently by RNs. Clients with the same medical diagnosis will often respond differently to that diagnosis and thus have different nursing diagnoses. For example, two clients have the same medical diagnosis of heart failure. However, one client may be interested in learning more information about the condition and the medications used to treat it, whereas another client may be experiencing anxiety when thinking about the effects this medical diagnosis will have on their family. The nurse must consider these different responses when creating the nursing care plan. Nursing diagnoses consider the client’s and family’s needs, attitudes, strengths, challenges, and resources as a customized nursing care plan is created to provide holistic and individualized care for each client.
Example of a Medical Diagnosis
A medical diagnosis identified for Ms. J. in Scenario C in the “Assessment” section is heart failure. This cannot be used as a nursing diagnosis because it is outside the nurse’s scope of practice to make a medical diagnosis, but it is considered as an “associated condition” when creating hypotheses for nursing diagnoses. Associated conditions are medical diagnoses, injuries, procedures, medical devices, or pharmacological agents that are not independently modifiable by the nurse, but support accuracy in nursing diagnosis. The nursing diagnosis in Scenario C will relate to the client’s responses to her medical diagnosis of heart failure, such as “Excess Fluid Volume.”
Additional Definitions Used in NANDA-I Nursing Diagnoses
The following definitions are used in association with NANDA-I nursing diagnoses.
Patient
The NANDA-I definition of a “patient” includes the following:
- Individual: a single human being distinct from others (i.e., a person).
- Caregiver: a family member or helper who regularly looks after a child or a sick, elderly, or disabled person.
- Family: two or more people having continuous or sustained relationships, perceiving reciprocal obligations, sensing common meaning, and sharing certain obligations toward others; related by blood and/or choice.
- Group: a number of people with shared characteristics, such as an ethnic group.
- Community: a group of people living in the same locale under the same governance. Examples include neighborhoods and cities.[9]
Age
The age of the person who is the subject of the diagnosis is defined by the following terms[10]:
- Fetus: an unborn human more than eight weeks after conception, until birth.
- Neonate: a person less than 28 days of age.
- Infant: a person greater than 28 days and less than 1 year of age.
- Child: a person aged 1 to 9 years.
- Adolescent: a person aged 10 to 19 years.
- Adult: a person older than 19 years of age unless national law defines a person as being an adult at an earlier age.
- Older adult: a person greater than 65 years of age.
Time
The duration of the diagnosis is defined by the following terms[11]:
- Acute: lasting less than three months.
- Chronic: lasting greater than three months.
- Intermittent: stopping or starting again at intervals.
- Continuous: uninterrupted, going on without stop.
Two terms used to assist in creating nursing diagnoses are at-risk populations and associated conditions[12]:
- At-risk populations are groups of people who share a characteristic that causes each member to be susceptible to a particular human response, such as demographics, health/family history, stages of growth/development, or exposure to certain events/experiences.
- Associated conditions are medical diagnoses, injuries, procedures, medical devices, or pharmacological agents. These conditions are not independently modifiable by the nurse, but support accuracy in nursing diagnosis.[13]
Types of Nursing Diagnoses
There are four types of NANDA-I nursing diagnoses:[14]
- Problem-Focused
- Health Promotion – Wellness
- Risk
- Syndrome
A problem-focused nursing diagnosis is a “clinical judgment concerning an undesirable human response to health condition/life processes that exist in an individual, family, group, or community.”[15] To make an accurate problem-focused diagnosis, related factors and defining characteristics must be present. Related factors (also called etiology) are causes that contribute to the diagnosis. Defining characteristics are cues, signs, and symptoms that cluster into patterns.[16] Defining characteristics are the signs and symptoms that a nurse can observe, hear, feel, or smell and cluster into patterns underlying nursing diagnoses.
A health promotion-wellness nursing diagnosis is “a clinical judgment concerning motivation and desire to increase well-being and to actualize human health potential.” These responses are expressed by the client’s readiness to enhance specific health behaviors.[17] A health promotion-wellness diagnosis is used when the client is willing to improve a lack of knowledge, coping, or other identified need.
A risk nursing diagnosis is “a clinical judgment concerning the vulnerability of an individual, family, group, or community for developing an undesirable human response to health conditions/life processes.”[18] A risk nursing diagnosis must be supported by risk factors that contribute to the increased vulnerability. A risk nursing diagnosis is different from the problem-focused diagnosis in that the problem has not yet actually occurred. Problem diagnoses should not be automatically viewed as more important than risk diagnoses because sometimes a risk diagnosis can have the highest priority for a client.[19]
A syndrome nursing diagnosis is a “clinical judgment concerning a specific cluster of nursing diagnoses that occur together and are best addressed together and through similar interventions.”[20]
Establishing Nursing Diagnosis Statements
NANDA-I recommends creating statements for nursing diagnosis that include the nursing diagnosis and related factors as exhibited by defining characteristics. The accuracy of the nursing diagnosis is validated when a nurse is able to clearly link the defining characteristics, related factors, and/or risk factors found during the client’s assessment.[21]
To create a nursing diagnosis statement, the RN analyzes the client’s subjective and objective data and clusters the data into patterns. Based on these patterns, the RN generates hypotheses for nursing diagnoses based on how the patterns meet defining characteristics of a nursing diagnosis. Recall that “defining characteristics” are the signs and symptoms related to a nursing diagnosis.[22] Defining characteristics are included in care planning resources for each nursing diagnosis, along with a definition of that diagnosis, so the nurse can select the most accurate diagnosis.
Example
An RN clusters objective and subjective data such as weight, height, and dietary intake as a pattern related to nutritional status and then compares these signs and symptoms to the defining characteristics for the NANDA nursing diagnosis, “Imbalanced Nutrition: Less Than Body Requirement.”
When creating a nursing diagnosis statement, the nurse also identifies the cause, or etiology, of the problem for that specific client. Recall that the term “related factors” refers to the underlying causes (etiology) of a client’s problem or situation. Related factors should not refer to medical diagnoses, but instead should be causes that the nurse can treat. When possible, the nursing interventions planned for nursing diagnoses should attempt to modify or remove these underlying causes of the nursing diagnosis.[23]
Creating nursing diagnosis statements is also called “using PES format.” The PES mnemonic no longer applies to the current terminology used by NANDA-I, but the components of a nursing diagnosis statement remain the same. A nursing diagnosis statement should contain the problem, related factors, and defining characteristics. These terms fit under the former PES format in this manner:
Problem (P): The problem (i.e., the nursing diagnosis)
Etiology (E): The related factors (i.e., the etiology/cause) of the nursing diagnosis; phrased as “related to” or “R/T”
Signs and Symptoms (S): The defining characteristics manifested by the client (i.e., the signs and symptoms/subjective and objective data/clinical cues) that led to the identification of that nursing diagnosis/hypothesis for the client; phrased with “as manifested by” (AMB) or “as evidenced by” (AEB).
Examples of different types of nursing diagnoses are further explained in the following sections.
Problem-Focused Nursing Diagnosis
A problem-focused nursing diagnosis contains all three components of the PES format:
Problem (P): Client problem (nursing diagnosis)
Etiology (E): Related factors causing the nursing diagnosis
Signs and Symptoms (S): Defining characteristics/cues manifested by that client (i.e., the signs and symptoms demonstrating there is a problem)
Example of a Problem-Focused Nursing Diagnosis
Refer to Scenario C of the “Assessment” section of this chapter. The cluster of data for Ms. J. (elevated blood pressure, elevated respiratory rate, crackles in the lungs, weight gain, worsening edema, and shortness of breath) are defining characteristics for the NANDA-I Nursing Diagnosis Excess Fluid Volume. The NANDA-I definition of Excess Fluid Volume is “surplus intake and/or retention of fluid.” The related factor (etiology) of the problem is that the client has excessive fluid intake.[24]
The components of a problem-focused nursing diagnosis statement for Ms. J. would be:
Problem (P): Excess Fluid Volume
Etiology (E): Related to excessive fluid intake
Signs and Symptoms (S): As manifested by bilateral basilar crackles in the lungs, bilateral 2+ pitting edema of the ankles and feet, increased weight of 1ten pounds, and the client reports, “My ankles are so swollen.”
A correctly written problem-focused nursing diagnosis statement for Ms. J. would be written as follows:
Excess Fluid Volume related to excessive fluid intake as manifested by bilateral basilar crackles in the lungs, bilateral 2+ pitting edema of the ankles and feet, an increase weight of 1ten pounds, and the client reports, “My ankles are so swollen.”
Health-Promotion Nursing Diagnosis
A health-promotion nursing diagnosis statement contains the problem (P) and the defining characteristics (S). The defining characteristics component of a health-promotion nursing diagnosis statement should begin with the phrase “expresses desire to enhance,” followed by what the client states in relation to improving their health status:[25]
A health-promotion diagnosis statement consists of the following:
Problem (P): Client problem (nursing diagnosis)
Signs and Symptoms (S): The client’s expressed desire to enhance
Example of a Health-Promotion Nursing Diagnosis
Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. demonstrates a readiness to improve her health status when she told the nurse that she would like to “learn more about my health so I can take better care of myself.” This statement is a defining characteristic of the NANDA-I nursing diagnosis Readiness for Enhanced Health Management, which is defined as “a pattern of regulating and integrating into daily living a therapeutic regimen for the treatment of illness and its sequelae, which can be strengthened.”[26]
The components of a health-promotion nursing diagnosis for Ms. J. would be:
Problem (P): Readiness for Enhanced Health Management
Symptoms (S): Expressed desire to “learn more about my health so I can take better care of myself.”
A correctly written health-promotion nursing diagnosis statement for Ms. J. would be written as follows:
Enhanced Readiness for Health Promotion as manifested by expressed desire to “learn more about my health so I can take better care of myself.”
Risk Nursing Diagnosis
A risk nursing diagnosis should be supported by evidence of the client’s risk factors for developing that problem. Different experts recommend different phrasing. NANDA-I 2018-2020 recommends using the phrase “as evidenced by” to refer to the risk factors for developing that problem.[27]
A risk diagnosis consists of the following:
Problem (P): Client problem (nursing diagnosis)
As Evidenced By: Risk factors for developing the problem
Example of a Risk Nursing Diagnosis
Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. has an increased risk of falling due to vulnerability from the dizziness and weakness she is experiencing. The NANDA-I definition of Risk for Falls is “increased susceptibility to falling, which may cause physical harm and compromise health.”[28]
The components of a risk nursing diagnosis statement for Ms. J. would be:
Problem (P): Risk for Falls
As Evidenced By: Dizziness and decreased lower extremity strength
A correctly written risk nursing diagnosis statement for Ms. J. would be written as follows:
Risk for Falls as evidenced by dizziness and decreased lower extremity strength.
Syndrome Nursing Diagnosis
A syndrome nursing diagnosis statement is a cluster of nursing diagnoses that occur together and are best addressed together and through similar interventions. To create a syndrome diagnosis, two or more nursing diagnoses must be used as defining characteristics (S) that create a syndrome. Related factors may be used if they add clarity to the definition but are not required.[29]
A syndrome statement consists of these items:
Problem (P): The syndrome
Signs and Symptoms (S): The defining characteristics are two or more similar nursing diagnoses
Example of a Syndrome Nursing Diagnosis
Refer to Scenario C in the “Assessment” section of this chapter. Clustering the data for Ms. J. identifies several similar NANDA-I nursing diagnoses that can be categorized as a syndrome. For example, Activity Intolerance is defined as “insufficient physiological or psychological energy to endure or complete required or desired daily activities.” Social Isolation is defined as “aloneness experienced by the individual and perceived as imposed by others and as a negative or threatening state.” These diagnoses can be included under the NANDA-I syndrome named Risk for Frail Elderly Syndrome. This syndrome is defined as a “dynamic state of unstable equilibrium that affects the older individual experiencing deterioration in one or more domains of health (physical, functional, psychological, or social) and leads to increased susceptibility to adverse health effects, in particular disability.”[30]
Example
The components of a syndrome nursing diagnosis for Ms. J. would be:
Problem (P): Risk for Frail Elderly Syndrome
Signs and Symptoms (S): The nursing diagnoses of Activity Intolerance and Social Isolation
Additional related factor: Fear of falling
A correctly written syndrome diagnosis statement for Ms. J. would be written as follows:
Risk for Frail Elderly Syndrome related to activity intolerance, social isolation, and fear of falling
See Table 4.4a for a summary of the types of nursing diagnoses.
Table 4.4a. Types of Nursing Diagnoses
| Diagnosis | What Is It? | Example of Nursing Diagnosis Statement |
| Problem-Focused (Actual) | Problem is present at the time of assessment | (PES) Fluid Volume Excess R/T excessive fluid intake AEB bilateral basilar crackles in the lungs, bilateral 2+ pitting edema in the ankles and feet, an increased weight of 10 pounds over 1 week, and the client reports, “My ankles feel swollen.” |
| Health-Promotion | A motivation/desire to increase well-being or a client’s strength | Enhanced Readiness for Health Promotion AEB expressed desire to “learn more about health so I can take better care of myself.” |
| Risk | Problem is likely to develop | Risk for Falls AEB dizziness and decreased lower extremity strength |
| Syndrome | Cluster of nursing diagnoses that occur together and are best addressed together | Risk for Frail Elderly Syndrome R/T activity intolerance, social isolation, and fear of falling |
Clinical Tip: It can feel overwhelming for nursing students to determine which nursing diagnoses to use for their clients due to the complexity of nursing diagnoses. Rest assured, use of nursing diagnoses becomes easier with practice and exposure to client care plans. Refer to trustworthy sources, such as a nursing diagnosis handbook or reputable care-planning resources to become aware of current NANDA-I nursing diagnoses.
Nursing diagnoses can be viewed to establish familiarity with them on the nandadiagnoses.com website, but but be aware this is not an official NANDA nursing diagnosis site. Evidence-based care planning resources should be used when planning clientcare.
Prioritization
After identifying nursing diagnoses, the next step is prioritizing diagnoses and actions according to the specific needs of the client. Nurses prioritize their actions while providing client care multiple times every day. Prioritization is the skillful process of deciding which actions to complete first for client safety and optimal client outcomes. Through prioritization, the most significant nursing problems, as well as the most important interventions in the nursing care plan, are identified.
Client care situations fall somewhere between routine care and a medical crisis. It is essential that life-threatening concerns and crises are identified immediately and addressed quickly. Depending on the severity of a problem, the steps of the nursing process may be performed in a matter of seconds for life-threatening concerns, such as respiratory arrest or cardiac arrest. Critical situations can occur at any time when providing nursing care for clients, and the steps of the nursing process must be performed rapidly. Nursing students must have a full understanding of how to correctly analyze cues, cluster data, form appropriate hypotheses, and prioritize hypotheses to take appropriate action using clinical judgment. Nurses recognize cues signaling a change in client condition, apply evidence-based practices in a crisis, and communicate effectively with interprofessional team members.
There are several concepts used to prioritize, including Maslow’s Hierarchy of Needs, the “ABCs” (Airway, Breathing and Circulation), and acute, uncompensated conditions. See the infographic in Figure 4.7[31] on The How To of Prioritization.

Maslow’s Hierarchy of Needs is used to categorize the most urgent client needs. The bottom levels of the pyramid represent the top priority needs of physiological needs intertwined with safety. See Figure 4.8[32] for an image of Maslow’s Hierarchy of Needs. You may be asking yourself, “What about the ABCs – isn’t airway the most important?” The answer to that question is “it depends on the situation and the associated safety considerations.” Consider this scenario – you are driving home after a lovely picnic in the country and come across a fiery car crash. As you approach the car, you see that the passenger is not breathing. Using Maslow’s Hierarchy of Needs to prioritize your actions, you remove the passenger from the car first due to safety even though he is not breathing. After ensuring safety and calling for help, you follow the steps to perform cardiopulmonary resuscitation (CPR) to establish circulation, airway, and breathing until help arrives.
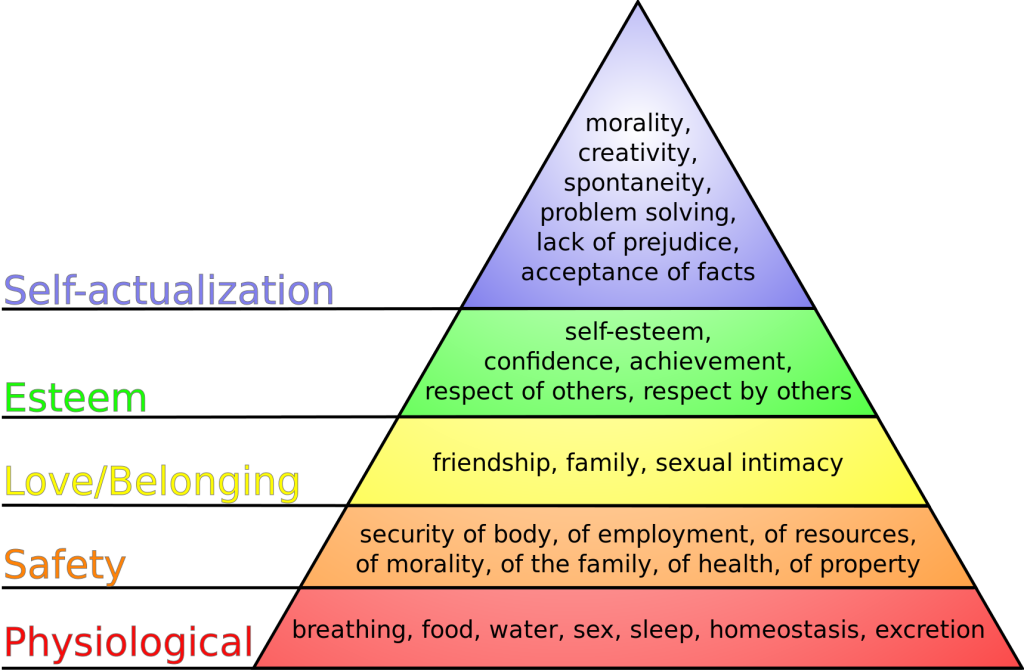
In addition to using Maslow’s Hierarchy of Needs and the ABCs of airway, breathing, and circulation, the nurse also considers if the client’s condition is an acute or chronic problem. Acute, uncompensated conditions require priority interventions over chronic conditions. Additionally, actual problems generally receive priority over potential problems, but risk problems sometimes receive priority depending on the client vulnerability and risk factors.
Example of Prioritization
Refer to Scenario C in the “Assessment” section of this chapter. Four types of nursing diagnoses were identified for Ms. J.: Excess Fluid Volume, Enhanced Readiness for Health Promotion, Risk for Falls, and Risk for Frail Elderly Syndrome. The top priority diagnosis is Excess Fluid Volume because this condition affects the physiological needs of breathing, homeostasis, and excretion. However, the Risk for Falls diagnosis comes in a close second because of safety implications and potential injury that could occur if the client fell.
Media Attributions
- Diagnosis in the Nursing Process Compared to the NCJMM
- Prioritization infograph picture
- Maslow’s_hierarchy_of_needs.svg
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- “Diagnosis in the Nursing Process Compared to the NCJMM” by Tami Davis is licensed under CC BY 4.0 ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- Gordon, M. (2008). Assess notes: Nursing assessment and diagnostic reasoning. F.A. Davis Company. ↵
- Gordon, M. (2008). Assess notes: Nursing assessment and diagnostic reasoning. F.A. Davis Company. ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- NANDA International. (n.d.). Glossary of terms. https://nanda.org/nanda-i-resources/glossary-of-terms/ ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- “The How To of Prioritization” by Valerie Palarski for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Maslow's hierarchy of needs.svg” by J. Finkelstein is licensed under CC BY-SA 3.0 ↵
With the increased emphasis on the impact of stress for health care professionals, many organizations and nursing programs have identified resources for formal stress reduction and mitigation. See Figure 12.7[1] for an illustration of stress management. Many of these models and resources have emerged as a professional necessity to help facilitate coping for individuals encountering innumerable job-related stressors. The U.S. Department of Veterans Affairs developed a Stress First Aid (SFA) framework to improve stress management in oneself and in others.[2] Many organizations are moving to frameworks such as the Stress First Aid framework and other stress management programs to help provide health care professionals with the knowledge, skills, and resources to aid in stress management reduction.
The Stress First Aid (SFA) framework offers the health care professional an opportunity to examine stress along a continuum, from normal stress that allows for adaptive functioning to signs of harmful stress requiring intensive intervention. It provides health care professionals with core functions for progressing through stress identification and resolution. The seven core functions are: Check, Coordinate, Cover, Calm, Connect, Competence, and Confidence.[3] The SFA model encourages health care professionals to self-reflect on a stress experience and take action to facilitate self-resolution and resource identification.

Many health care organizations embrace wellness as a foundational tenet of workplace culture. They have dedicated wellness committees or wellness champions who promote initiatives aimed at improving stress management among staff.[4] These formalized committees or positions reflect organizational commitment to the importance of self-care and personal wellness. When nursing graduates are interviewing for their first nursing positions, wellness initiatives may be a consideration when exploring professional employment benefits and organizational support structures.
The impact of wellness and stress-reduction strategies is often included in new hire orientation and nurse residency programs. Many nurse residency programs formally acknowledge in their curriculum that novice nurses must be educated about the signs of stress.[5] Novice nurses are particularly vulnerable to harmful stressors during their role transition. Many organizations provide training about strategies and resources to assist with coping and stress reduction, which is referred to as resiliency training programs.[6] Resiliency training fosters feelings of mindfulness, sensitivity to self, and professional development techniques that contribute to long-term engagement in the profession.
Read about ways to manage stress from the U.S. Department of Health and Human Services Office on Women's Health.
Burnout: A condition manifested physically and psychologically with a loss of motivation.
Compassion fatigue: A state of chronic and continuous self-sacrifice and/or prolonged exposure to difficult situations that affect a health care professional’s physical, emotional, and spiritual well-being.
Harmful stress: Stress (also referred to as "distress") not adequately self-managed resulting in physical, mental, and behavioral consequences.[7]
Mindfulness: Awareness that arises through paying attention, being on purpose and in the present moment, and being nonjudgmental.
Normal stress: Stress (also referred to as "eustress") that does not have lasting consequences and is successfully managed by the individual who is experiencing it.[8]
Resiliency training: Educational sessions that foster feelings of mindfulness and sensitivity to self and cultivate professional development techniques that contribute to long-term engagement in the profession.
Self-care: Actions that individuals take to maintain health of oneself.
Learning Objectives
- Develop a current professional resume or portfolio
- Identify steps for preparing for the NCLEX-RN examination
- Identify actions for obtaining nursing credentials
- Identify strategies for successful nursing interviews
- Identify goals for lifelong learning and professional development
Preparing to enter the workforce as a registered nurse (RN) can be a challenging but exciting time. Being aware of available resources to help navigate this process will decrease stress and make the process more manageable. This chapter will discuss how to prepare for the NCLEX-RN examination, obtain a nursing license, create a resume and portfolio, effectively participate in an interview, transition into the RN role, and become a lifelong learner.
As previously discussed, the action of providing nursing care can result in significant stress. The stress response is exacerbated when experiencing extreme or repeated stressors, such as client deaths. In some health care settings, nurses do not have time to resolve grief from one loss before another death occurs. This lack of time to resolve grief has been exacerbated during the COVID-19 pandemic where many units continually filled with clients requiring high levels of skilled nursing care. Additionally, some patients with COVID died without the face-to-face support of friends and family due to visitor restrictions. This resulted in the end-of-life transition supported solely by the health care staff. Many nurses felt additional stress due to supporting both the client and the client’s family during this challenging time.
Compassion fatigue and burnout occur frequently with nurses and other health care professionals who experience cumulative deaths that are not addressed therapeutically. Compassion fatigue is a state of chronic and continuous self-sacrifice and/or prolonged exposure to difficult situations that affect a health care professional’s physical, emotional, and spiritual well-being. This can lead to a person being unable to care for or empathize with someone’s suffering. Additionally, many individuals who experience compassion fatigue may become detached from the emotions associated with the care experience or client needs. These individuals can often appear numb to the severity of the circumstance of the events that are occurring. Burnout can be manifested physically and psychologically with a loss of motivation. It can be triggered by workplace demands, lack of resources to perform work professionally and safely, interpersonal relationship stressors, or work policies that can lead to diminished caring and cynicism.[9] See Figure 12.4[10] for an image depicting a nurse at home experiencing burnout due to exposure to multiple competing demands of work, school, and family responsibilities.

With the significant dangers of burnout and compassion fatigue within the nursing profession, it is important to acknowledge actions and strategies to facilitate self-care. Self-care can occur in many actions that individuals take to maintain self-health and is critically important for preventing compassion fatigue and burnout.
To facilitate self-care, nurses must recognize the need to take time off, seek out individual healthy coping mechanisms, and voice concerns within their workplace. Prayer, meditation, exercise, art, and music are examples of healthy coping mechanisms that nurses can use for self-care. Nurses should reflect on what actions bring them personal satisfaction and rejuvenation. These strategies should then be purposefully included to help reduce the influence of work-related stressors. For example, perhaps you are a nurse working in a busy Level 1 trauma center and emergency department. You are nearing the end of your third 12-hour shift and have the following day off. The unit manager approaches you and states that there has been an ill call for tomorrow’s evening shift. You are offered premium pay to come in and work. Although there is a part of you that is interested in receiving the premium pay, you also take a moment to think about your current situation. You are tired from working three 12-hour shifts the last three days and had plans to go to your child’s baseball game tomorrow evening. Taking stock of these reflective thoughts, you politely decline the additional shift. Acknowledging your fatigue and the satisfaction that you will feel in attending your child’s game are important parts of facilitating self-care. Although you could have chosen to work the shift, taking time to look inwardly on what will bring about the greatest rejuvenation and avoid burnout will help cultivate professional engagement.
Additionally, nurses must recognize when outside resources are needed to mitigate stress and facilitate self-care. Many organizations sponsor employee assistance programs that provide counseling services. These programs can be of great value and benefit in allowing individuals to share both individual and employment stressors. For example, employee assistance programs can address employment-related stressors, such as cumulative client deaths, as well as personal challenges impacting one’s work role, such as a family illness. The support of an impartial, trained professional can be very helpful as individuals navigate through stressful stimuli.
There are specific stress stimuli that may require specialized intervention. For example, after a client death resulting from trauma, many organizations hold debriefing sessions to allow individuals who participated in care to come together to verbalize their feelings. These sessions are often held with the support of chaplains to facilitate individual coping and verbalization of feelings. Debriefing sessions can be very helpful as individuals experience collegial support in working through traumatic stress stimuli.
Read more about the role of chaplains in facilitating coping in the “Spirituality” chapter in Open RN Nursing Fundamentals, 2e.
Reflective Questions
Throughout your nursing career, there will be times to stop and pay attention to warning signs of compassion fatigue and burnout. Here are some questions to consider:
- Has my behavior changed?
- Do I communicate differently with others?
- What destructive habits tempt me?
- Do I project my inner pain onto others?[11]
Strategies for Self-Care
By becoming self-aware regarding signs of stress, you can implement self-care strategies to prevent compassion fatigue and burnout. Use the following “A’s” to assist in building resilience, connection, and compassion:
- Attention: Become aware of your physical, psychological, social, and spiritual health. For what are you grateful? What are your areas of improvement? This protects you from drifting through life on autopilot.
- Acknowledgement: Honestly look at all you have witnessed as a health care professional. What insight have you experienced? Acknowledging the pain of loss you have witnessed protects you from invalidating the experiences.
- Affection: Choose to look at yourself with kindness and warmth. Affection prevents you from becoming bitter and “being too hard” on yourself.
- Acceptance: Choose to be at peace and welcome all aspects of yourself. By accepting both your talents and imperfections, you can protect yourself from impatience, victim mentality, and blame.[12]
Cultivating Care of Self
Taking care of oneself can feel as if it goes against the nature of the nursing role, but it is a vital component for professional success. Provision 5 of the American Nurses Association Code of Ethics states, “The nurse owes the same duties to self as to others, including the responsibility to promote health and safety, preserve wholeness of character and integrity, maintain competence, and continue personal and professional growth.”[13] In a profession where one spends most of their time thinking about the needs of others, it can be difficult to recognize when special care and attention is needed for one’s own health. However, there are many strategies that nurses can use to help them navigate stress and prioritize their own health and wellness. Although not every strategy may be “right” for every nurse, it is critical for nurses to find actionable interventions to help them address their own stress.
Here are some examples of stress management strategies:
- Meditation. Meditation can induce feelings of calm and clear-headedness, improving concentration and attention. Research has shown that meditation increases the brain’s gray matter density, which can reduce sensitivity to pain, enhance the immune system, help regulate difficult emotions, and relieve stress. Mindfulness meditation in particular has been proven helpful for people with depression and anxiety, cancer, fibromyalgia, chronic pain, rheumatoid arthritis, type 2 diabetes, chronic fatigue syndrome, and cardiovascular disease.[14] See Figure 12.5[15] for an image of an individual participating in meditation.

- Yoga. Yoga is a centuries-old spiritual practice that creates a sense of union within the practitioner through physical postures, ethical behaviors, and breath expansion. The systematic practice of yoga has been found to reduce inflammation and stress, decrease depression and anxiety, lower blood pressure, and increase feelings of well-being.[16] See Figure 12.6[17] for an image of an individual participating in yoga.

- Journaling. Journaling can help a person become more aware of their inner life and feel more connected to experiences. Studies show that writing during difficult times may help a person find meaning in life’s challenges and become more resilient in the face of obstacles. When journaling, it can be helpful to focus on three basic questions: What experiences give me energy? What experiences drain my energy? Were there any experiences today where I felt alive and experienced “flow”? Allow yourself to write freely, without stopping to edit or worry about spelling and grammar.[18]
- Prayer. Prayer can elicit the relaxation response, along with feelings of hope, gratitude, and compassion, all of which have a positive effect on overall well-being. There are several types of prayer rooted in the belief that there is a higher power that has some level of influence over one’s life. This belief can provide a sense of comfort and support in difficult times. A recent study found that clinically depressed adults who believed their prayers were heard by a concerned presence responded much better to treatment than those who did not believe.[19]
- Spiritual community. Join a spiritual group, such as a church, synagogue, temple, mosque, meditation center, yoga class, or other local group that meets to discuss spiritual issues. The benefits of social support are well-documented, and having a spiritual community to turn to for fellowship can provide a sense of belonging and support.[20]
- Nurturing relationships. Relationships with family, significant others, and friends aren’t static – they are living, dynamic aspects of our lives that require attention and care. To benefit from strong connections with others, you should take charge of your relationships and put in the time and energy you would any other aspect of your well-being. It can be helpful to create rituals together. With busy schedules and the presence of online social media that offer the façade of real contact, it’s very easy to drift from friends. Research has found that people who deliberately make time for gatherings or trips enjoy stronger relationships and more positive energy. An easy way to do this is to create a standing ritual that you can share and that doesn’t create more stress, such as talking on the telephone on Fridays or sharing a walk during lunch breaks.[21]
- Mindfulness. Mindfulness has been defined as, “Awareness that arises through paying attention, on purpose, in the present moment, and nonjudgmentally.” Mindfulness has also been described as, “Non-elaborative, nonjudgmental, present-centered awareness in which each thought, feeling, and sensation that arises is acknowledged and accepted as it is.” Mindfulness helps us be present in our lives and gives us some control over our reactions and repetitive thought patterns. It helps us pause, get a clearer picture of a situation, and respond more skillfully. Compare your default state to mindfulness when studying for an exam in a difficult course or preparing for a clinical experience. What do you do? Do you tell yourself, “I am not good at this” or “I am going to look stupid”? Does this distract you from paying attention to studying or preparing? How might it be different if you had an open attitude with no concern or judgment about your performance? What if you directly experienced the process as it unfolded, including the challenges, anxieties, insights, and accomplishments, while acknowledging each thought or feeling and accepting it without needing to figure it out or explore it further? If practiced regularly, mindfulness helps a person start to see the habitual patterns that lead to automatic negative reactions that create stress. By observing these thoughts and emotions instead of reacting to them, a person can develop a broader perspective and can choose a more effective response.[22]
- Nature. Spending time in nature is cited by many individuals as a spiritual practice that contributes to their mental health.[23]
- Physical activity. Regular physical activity, such as brisk walking, can relieve stress and tension. [24]
Explore additional free resources regarding well-being and resilience:
The National Council Licensure Examination for Registered Nurses (NCLEX-RN) is the exam that nursing graduates must pass successfully to obtain their nursing license and become a registered nurse. The purpose of the NCLEX is to evaluate if a nursing graduate (i.e., candidate) is competent to provide safe, competent, entry-level nursing care. The NCLEX-RN is developed by the National Council of State Board of Nursing (NCSBN), an independent, nonprofit organization composed of the 50 state boards of nursing and other regulatory agencies.[25]
The NCLEX-RN is a pass/fail examination administered on a computer using computer adaptive testing (CAT). CAT means that every time a candidate answers a test item, the computer reestimates their ability based on all their previous answers and the difficulty of those items. The computer then selects the next item based on an estimated 50% chance of the candidate answering it correctly. In this manner, the next item is not too easy nor too difficult, and a candidate’s true ability level is determined. Each item is perceived by the candidate as challenging because it is targeted to their ability. With each item answered, the computer's estimate of the candidate’s ability becomes more precise.
The computer stops providing items when it is 95% certain that the candidate’s ability is clearly above or clearly below the passing standard, the candidate has received the maximum number of questions, or the candidate has run out of time without demonstrating a competence level to pass. Testing accommodations may be provided for eligible candidates with the authorization of the candidate’s State Board of Nursing (SBON).[26],[27]
See an image of a simulated graduate taking the NCLEX in Figure 11.1.[28]

Read more about the NCLEX at https://www.ncsbn.org/nclex.htm.
Watch a video about how the NCLEX uses computer assistive technology (CAT) at https://www.ncsbn.org/356.htm.
Registering to Take the NCLEX
Before you can register to take the NCLEX, you will need an Authorization to Test (ATT). To receive an ATT, complete the following steps[29]:
- Apply for a nurse license from your State Board of Nursing (SBON) or other nursing regulatory body
- Register with Pearson VUE and pay the exam fee
- Wait to receive your ATT from Pearson Vue
- Schedule your exam with Pearson VUE
Be sure to start this process well in advance of your target date for taking the NCLEX.
Read specific instructions regarding registering and taking the NCLEX-RN by downloading the most current NCLEX-Candidate Bulletin from the NCSBN. The content includes the following:
- Registering for the exam
- Scheduling the exam
- Understanding test site rules and regulations
- Preparing for the day of the exam
Download the most current NCLEX-Candidate Bulletin from https://www.ncsbn.org/nclex.htm.
Next Generation NCLEX
A new edition of NCLEX was released in 2023 with “Next Generation” questions.
The Next Generation NCLEX (Next Gen) uses evolving case studies and new types of test questions based on a new NCSBN Clinical Judgment Measurement Model (NCJMM) that assesses how well the candidate can think critically and use clinical judgment when providing nursing care. The NCJMM assess the candidate's ability to recognize cues, analyze cues, prioritize hypotheses, generate solutions, take actions, and evaluate outcomes.[30]
Five new Next Generation test item types are called extended multiple response, extended drag and drop, cloze (drop-down), extended hot spot (highlighting), and matrix-grid:
- Extended Multiple Response: Extended Multiple Response items allow candidates to select one or more answer options at a time. This item type is similar to the current NCLEX multiple response item but has more options and uses partial credit scoring.[31]
- Extended Drag and Drop: Extended Drag and Drop items allow candidates to move or place response options into answer spaces. This item type is like the current NCLEX ordered response items but not all of the response options may be required to answer the item. In some items, there may be more response options than answer spaces.[32]
- Cloze (Drop – Down): Cloze (Drop - Down) items allow candidates to select one option from a drop-down list. There can be more than one drop-down list in a cloze item. These drop-down lists can be used as words or phrases within a sentence or within tables and charts.[33]
- Enhanced Hot Spot (Highlighting): Enhanced Hot Spot items allow candidates to select their answer by highlighting predefined words or phrases. Candidates can select and deselect the highlighted parts by clicking on the words or phrases. These types of items allow an individual to read a portion of a client medical record (e.g., a nursing note, medical history, lab values, medication record, etc.), and then select the words or phrases that answer the item.[34]
- Matrix/Grid: Matrix/Grid items allow the candidate to select one or more answer options for each row and/or column. This item type can be useful in measuring multiple aspects of the clinical scenario with a single item. In the example below, each of the eight rows will need to have one of the three answer choices selected.[35]
View a NCSBN video on Next Generation test items.
Participate in an NCLEX tutorial at https://www.ncsbn.org/nclex-tutorial.htm.
Preparing for the Examination
Since the first day of nursing school, you have been working towards successfully passing the NCLEX-RN. After you graduate, it is important to implement strategies for success for taking the NCLEX, such as reviewing the NCLEX-RN Test Plan, setting up a dedicated review schedule based on your test date, and reviewing material you learned throughout nursing school.[36]
NCLEX Test Plan
The NCLEX-RN Test Plan provides a concise summary of the content and scope of the exam and serves as an excellent guide for preparation. NCLEX-RN test plans are updated every three years based on surveys of newly licensed registered nurses to ensure the NCLEX questions reflect fair, comprehensive, current, and entry-level nursing competency.[37]
The NCLEX Test Plan categorizes test questions based on categories and subcategories referred to as “Client Needs”[38]:
- Safe and Effective Care Environment
- Management of Care
- Safety and Infection Control
- Health Promotion and Maintenance
- Psychosocial Integrity
- Physiological Integrity
- Basic Care and Comfort
- Pharmacological and Parenteral Therapies
- Reduction of Risk Potential
- Physiological Adaptation
In addition, the following concepts are applied throughout the client needs categories[39]:
- Nursing Process
- Caring
- Communication and Documentation
- Teaching and Learning
- Culture and Spirituality
Download the current NCLEX-RN Test Plan from https://www.ncsbn.org/testplans.htm.
Review Schedule
Many students find it helpful to create and follow a study calendar with topics to review based on the NCLEX Test Plan.
Reviewing Material
Some graduates prefer to attend an NCLEX review course to prepare for the examination whereas others prefer to review their notes from nursing school on their own. Be sure to review the NCLEX Candidate Rules before the day of the examination.[40],[41]
Day of the Examination
On the day of the examination, it is normal to experience some anxiety. However, it is important to use techniques to manage anxiety, so it does not impact your ability to think through and answer the test questions. Use positive self-talk and remind yourself that you have been preparing for this examination since the first day of nursing school. Read additional tips for the day of the NCLEX and tips for testing in the following boxes.
| Tips for the Day of the NCLEX[42] |
|---|
|
| Tips for Testing[43] |
|---|
|
After the Examination
If your State Board of Nursing (SBON) or nursing regulatory body (NRB) participates in the “Quick Results Service,” you can receive your “unofficial” results two business days after the exam if you pay for this service. Official results are sent to you approximately six weeks after the exam.[44]
If you didn't pass the exam, you'll receive an NCLEX Candidate Performance Report (CPR). The CPR is an individualized document that shows how a candidate performed in each of the test plan content areas. Graduates who fail the exam can use the CPR as a guide to prepare them to retake the exam.[45]
If you need to retake the exam, you will need to wait a minimum of 45 days before you can retake the NCLEX per NCSBN policy. This length of time is determined by your SBON (or NRB) and will be reflected in your new ATT’s validity dates. Read the steps for retaking the NCLEX in the following box.
| Steps for Retaking the NCLEX |
|---|
|
The National Council Licensure Examination for Registered Nurses (NCLEX-RN) is the exam that nursing graduates must pass successfully to obtain their nursing license and become a registered nurse. The purpose of the NCLEX is to evaluate if a nursing graduate (i.e., candidate) is competent to provide safe, competent, entry-level nursing care. The NCLEX-RN is developed by the National Council of State Board of Nursing (NCSBN), an independent, nonprofit organization composed of the 50 state boards of nursing and other regulatory agencies.[46]
The NCLEX-RN is a pass/fail examination administered on a computer using computer adaptive testing (CAT). CAT means that every time a candidate answers a test item, the computer reestimates their ability based on all their previous answers and the difficulty of those items. The computer then selects the next item based on an estimated 50% chance of the candidate answering it correctly. In this manner, the next item is not too easy nor too difficult, and a candidate’s true ability level is determined. Each item is perceived by the candidate as challenging because it is targeted to their ability. With each item answered, the computer's estimate of the candidate’s ability becomes more precise.
The computer stops providing items when it is 95% certain that the candidate’s ability is clearly above or clearly below the passing standard, the candidate has received the maximum number of questions, or the candidate has run out of time without demonstrating a competence level to pass. Testing accommodations may be provided for eligible candidates with the authorization of the candidate’s State Board of Nursing (SBON).[47],[48]
See an image of a simulated graduate taking the NCLEX in Figure 11.1.[49]

Read more about the NCLEX at https://www.ncsbn.org/nclex.htm.
Watch a video about how the NCLEX uses computer assistive technology (CAT) at https://www.ncsbn.org/356.htm.
Registering to Take the NCLEX
Before you can register to take the NCLEX, you will need an Authorization to Test (ATT). To receive an ATT, complete the following steps[50]:
- Apply for a nurse license from your State Board of Nursing (SBON) or other nursing regulatory body
- Register with Pearson VUE and pay the exam fee
- Wait to receive your ATT from Pearson Vue
- Schedule your exam with Pearson VUE
Be sure to start this process well in advance of your target date for taking the NCLEX.
Read specific instructions regarding registering and taking the NCLEX-RN by downloading the most current NCLEX-Candidate Bulletin from the NCSBN. The content includes the following:
- Registering for the exam
- Scheduling the exam
- Understanding test site rules and regulations
- Preparing for the day of the exam
Download the most current NCLEX-Candidate Bulletin from https://www.ncsbn.org/nclex.htm.
Next Generation NCLEX
A new edition of NCLEX was released in 2023 with “Next Generation” questions.
The Next Generation NCLEX (Next Gen) uses evolving case studies and new types of test questions based on a new NCSBN Clinical Judgment Measurement Model (NCJMM) that assesses how well the candidate can think critically and use clinical judgment when providing nursing care. The NCJMM assess the candidate's ability to recognize cues, analyze cues, prioritize hypotheses, generate solutions, take actions, and evaluate outcomes.[51]
Five new Next Generation test item types are called extended multiple response, extended drag and drop, cloze (drop-down), extended hot spot (highlighting), and matrix-grid:
- Extended Multiple Response: Extended Multiple Response items allow candidates to select one or more answer options at a time. This item type is similar to the current NCLEX multiple response item but has more options and uses partial credit scoring.[52]
- Extended Drag and Drop: Extended Drag and Drop items allow candidates to move or place response options into answer spaces. This item type is like the current NCLEX ordered response items but not all of the response options may be required to answer the item. In some items, there may be more response options than answer spaces.[53]
- Cloze (Drop – Down): Cloze (Drop - Down) items allow candidates to select one option from a drop-down list. There can be more than one drop-down list in a cloze item. These drop-down lists can be used as words or phrases within a sentence or within tables and charts.[54]
- Enhanced Hot Spot (Highlighting): Enhanced Hot Spot items allow candidates to select their answer by highlighting predefined words or phrases. Candidates can select and deselect the highlighted parts by clicking on the words or phrases. These types of items allow an individual to read a portion of a client medical record (e.g., a nursing note, medical history, lab values, medication record, etc.), and then select the words or phrases that answer the item.[55]
- Matrix/Grid: Matrix/Grid items allow the candidate to select one or more answer options for each row and/or column. This item type can be useful in measuring multiple aspects of the clinical scenario with a single item. In the example below, each of the eight rows will need to have one of the three answer choices selected.[56]
View a NCSBN video on Next Generation test items.
Participate in an NCLEX tutorial at https://www.ncsbn.org/nclex-tutorial.htm.
Preparing for the Examination
Since the first day of nursing school, you have been working towards successfully passing the NCLEX-RN. After you graduate, it is important to implement strategies for success for taking the NCLEX, such as reviewing the NCLEX-RN Test Plan, setting up a dedicated review schedule based on your test date, and reviewing material you learned throughout nursing school.[57]
NCLEX Test Plan
The NCLEX-RN Test Plan provides a concise summary of the content and scope of the exam and serves as an excellent guide for preparation. NCLEX-RN test plans are updated every three years based on surveys of newly licensed registered nurses to ensure the NCLEX questions reflect fair, comprehensive, current, and entry-level nursing competency.[58]
The NCLEX Test Plan categorizes test questions based on categories and subcategories referred to as “Client Needs”[59]:
- Safe and Effective Care Environment
- Management of Care
- Safety and Infection Control
- Health Promotion and Maintenance
- Psychosocial Integrity
- Physiological Integrity
- Basic Care and Comfort
- Pharmacological and Parenteral Therapies
- Reduction of Risk Potential
- Physiological Adaptation
In addition, the following concepts are applied throughout the client needs categories[60]:
- Nursing Process
- Caring
- Communication and Documentation
- Teaching and Learning
- Culture and Spirituality
Download the current NCLEX-RN Test Plan from https://www.ncsbn.org/testplans.htm.
Review Schedule
Many students find it helpful to create and follow a study calendar with topics to review based on the NCLEX Test Plan.
Reviewing Material
Some graduates prefer to attend an NCLEX review course to prepare for the examination whereas others prefer to review their notes from nursing school on their own. Be sure to review the NCLEX Candidate Rules before the day of the examination.[61],[62]
Day of the Examination
On the day of the examination, it is normal to experience some anxiety. However, it is important to use techniques to manage anxiety, so it does not impact your ability to think through and answer the test questions. Use positive self-talk and remind yourself that you have been preparing for this examination since the first day of nursing school. Read additional tips for the day of the NCLEX and tips for testing in the following boxes.
| Tips for the Day of the NCLEX[63] |
|---|
|
| Tips for Testing[64] |
|---|
|
After the Examination
If your State Board of Nursing (SBON) or nursing regulatory body (NRB) participates in the “Quick Results Service,” you can receive your “unofficial” results two business days after the exam if you pay for this service. Official results are sent to you approximately six weeks after the exam.[65]
If you didn't pass the exam, you'll receive an NCLEX Candidate Performance Report (CPR). The CPR is an individualized document that shows how a candidate performed in each of the test plan content areas. Graduates who fail the exam can use the CPR as a guide to prepare them to retake the exam.[66]
If you need to retake the exam, you will need to wait a minimum of 45 days before you can retake the NCLEX per NCSBN policy. This length of time is determined by your SBON (or NRB) and will be reflected in your new ATT’s validity dates. Read the steps for retaking the NCLEX in the following box.
| Steps for Retaking the NCLEX |
|---|
|
Licensure is the process by which a State Board of Nursing (SBON) grants permission to an individual to engage in nursing practice after verifying the applicant has attained the competency necessary to perform the scope of practice of a registered nurse (RN).[67] The SBON verifies these three components:
- Verification of graduation from an approved prelicensure RN nursing education program
- Verification of successful completion of NCLEX-RN examination
- A criminal background check (in some states)[68]
In the United States there are three common types of prelicensure educational programs that prepare a student to become an RN, including a two-year associate degree of nursing (ADN), a hospital-based diploma program, or a four-year baccalaureate degree (BSN). Some universities offer an "Entry Level Master of Science in Nursing Track" for non-nurses holding a baccalaureate or master's degree in another field who wish to become a nurse. All graduates must pass the same NCLEX-RN to obtain their RN license from their SBON (or other nursing regulatory body).
Requirements for licensure renewal vary from state to state. Some states require continued education credits (CEUs), along with the payment of fees. In Wisconsin the nursing license is renewed every two years.
- Use this map for contact information for the State Boards of Nursing.
- Read more details on obtaining a Wisconsin RN license at https://dsps.wi.gov/Pages/Professions/RN/Default.aspx.
Nurse Licensure Compact
When applying for your nursing license from your State Board of Nursing (SBON), you may also be eligible to apply for a multistate license. The Nurse Licensure Compact (NLC) allows nurses to practice in other NLC states with their original state’s nursing license without having to obtain additional licenses, contingent upon remaining a resident of that state. Currently, 38 states have enacted the NLC. Read more information about the NLC using the information in the following box.
View the current Nurse Licensure Compact Map.
Read this algorithm on how to Navigate the Nurse Licensure Compact.
Read more information about the Nurse Licensure Compact Rules.
Watch a video for nursing students on the Nurse Licensure Compact.
Temporary Permit
In some states before taking the NCLEX, an applicant may apply to receive a temporary permit from their State Board of Nursing (SBON). A temporary permit allows the applicant to practice practical nursing under the direct supervision of a registered nurse until the RN license is granted. A temporary permit is typically valid for a period of three months or until the holder receives failing NCLEX results, whichever is shorter.
Read about the temporary permit available in Wisconsin.
Many students begin applying for their first nursing position before they graduate or take the NCLEX-RN. Read tips for employment in the following box.
| Tips for Employment |
|---|
|
During your job-search process, it is helpful to begin by reviewing Medicare’s quality ratings of health care agencies and providers. The “overall star rating” is based on how well the agency performs on various quality indicators and patient satisfaction surveys.
Review Medicare ratings of hospitals, nursing homes, home health agencies, and providers at www.medicare.gov/care-compare.
When applying for a job position, a resume and/or portfolio is typically included as part of the application process.
Resume
A resume is a document that highlights one’s background, education, skills, and accomplishments to potential employers. There are many types of resume formats, and some individuals elect to use online services to create a professional resume.
A resume typically includes the following components:
- Personal contact information
- Professional objective statement/Goals
- Education
- Work experience
- Awards and achievements
- Community service
- Languages, hobbies, volunteer experiences (optional)
When creating a resume, it is helpful to highlight skills and experience that separate you from the other candidates applying for the position. It is also helpful to tailor your resume to the skills and experience expressed in the job description.
- Read more details about what to put in a resume and nursing resumes and cover letters.
- View a sample resume.
- View a sample Online Resume Service.
Portfolio
A portfolio is a compilation of materials showcasing examples of previous work demonstrating one’s skills, qualifications, education, training, and experience. They can be submitted in electronic or paper form. See Figure 11.3[69] for an image of a sample electronic portfolio.
Some schools of nursing require portfolios to be completed throughout the program. These portfolios are a representation of work demonstrating the student's accomplishments.
Portfolios typically include the following:
- Personal contact information
- Resume
- Professional goals
- Skilled work with examples (e.g., a nursing care plan, process recording, teaching plan, etc.)
- Accomplishments (e.g., dean’s list)
- Degrees
- Certifications (e.g., CPR)
- Professional memberships (e.g., Student Nurse Association)
- Community service activities
- References (if requested)
- Read more about what to include in a portfolio.
- Visit an online portfolio service.
Interviewing
After applying for a position and submitting your resume and/or portfolio, you may be contacted to set up an interview. When you're interviewing for an RN position, you will be asked about your skills, experience, and your education. Some questions may be basic, such as, “Why did you become a nurse?” Other questions may be more difficult to answer, such as “Explain your strengths and weaknesses as an RN.” See Figure 11.4[70] for a simulated interview.

Interviewing for a new position can cause anxiety because you are required to answer questions and provide examples. A strategy to make the interview process easier and reduce anxiety is to prepare answers for commonly asked questions prior to the interview. Completing this task will help you prepare and increase your confidence. See common interview questions in the following box. It is helpful to tailor your answers to the skills and experience provided in the position description of the job you are seeking.
| Common Questions During an Interview |
|---|
|
Prior to your interview, research the organization's website. Be aware of their mission and vision statements and any “current events” in the news. Interviewers are impressed when an applicant has taken the time to learn about the organization and demonstrates interest.
Interviews may take place face-to-face, virtually on a computer, or over the phone. If you are interviewing face-to-face or virtually, dress for success in professional attire. If interviewing virtually, be sure to decrease distractions at home by turning off your phone and conducting the interview in a quiet space. Establish good eye contact with the interviewer and speak in a confident manner. Remember, this is the time to “sell your nursing self,” so highlight your achievements and what you are proud of accomplishing. See additional tips for interviews in the following box.
| Tips for Interviews |
|---|
|
The interview process is also an opportunity for you to determine if this position and agency is a good fit for you. Remember that it is important to select an agency that has good ratings for providing safe patient care and patient satisfaction. It is not worth taking a position that may place your nursing license at risk. Ask questions of the interviewer to clarify your understanding of the job position and expectations, agency policies, and workplace culture. Suggested interview questions are listed in the following box.
| Questions for Interviewer |
|---|
|

