Basic Concepts
Open Resources for Nursing (Open RN)
Before learning how to use the nursing process, it is important to understand basic concepts concerning how critical thinking relates to nursing practice. Let’s take a deeper look at how nurses think.
Critical Thinking and Clinical Reasoning
Nurses make decisions while providing client care by using critical thinking and clinical reasoning. Critical thinking is a broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.”[1] Using critical thinking means that nurses take extra steps to maintain client safety and don’t just “follow orders.” It also means the accuracy of client information is validated and plans for caring for clients are based on their needs, current clinical practice, and research.
“Critical thinkers” possess certain attitudes that foster rational thinking. These attitudes are as follows:
- Independence of thought: Thinking on your own
- Fair-mindedness: Treating every viewpoint in an unbiased, unprejudiced way
- Insight into egocentricity and sociocentricity: Thinking of the greater good and not just thinking of yourself. Knowing when you are thinking of yourself (egocentricity) and when you are thinking or acting for the greater good (sociocentricity)
- Intellectual humility: Recognizing your intellectual limitations and abilities
- Nonjudgmental: Using professional ethical standards and not basing your judgments on your own personal or moral standards
- Integrity: Being honest and demonstrating strong moral principles
- Perseverance: Persisting in doing something despite it being difficult
- Confidence: Believing in yourself to complete a task or activity
- Interest in exploring thoughts and feelings: Wanting to explore different ways of knowing
- Curiosity: Asking “why” and wanting to know more
Clinical reasoning is defined as, “A complex cognitive process that uses formal and informal thinking strategies to gather and analyze client information, evaluate the significance of this information, and weigh alternative actions.”[2] To make sound judgments about client care, nurses must generate alternatives, weigh them against the evidence, and choose the best course of action. The ability to clinically reason develops over time and is based on knowledge and experience.[3]
Inductive and Deductive Reasoning and Clinical Judgment
Inductive and deductive reasoning are important critical thinking skills. They help the nurse use clinical judgment when implementing the nursing process.
Inductive reasoning involves noticing cues, making generalizations, and creating hypotheses based on specific information or incidents. Cues are data that fall outside of expected findings that give the nurse a hint or indication of a client’s potential problem or condition. The nurse organizes these cues into patterns and creates a generalization. A generalization is a judgment formed from a set of facts, cues, and observations and is similar to gathering pieces of a jigsaw puzzle into patterns until the whole picture becomes more clear. Based on generalizations created from patterns of data, the nurse creates a hypothesis regarding a client problem. A hypothesis is a proposed explanation for a situation. It attempts to explain the “why” behind the problem that is occurring. If a “why” is identified, then a solution can begin to be explored.
No one can draw conclusions without first noticing cues. Paying close attention to a client, the environment, and interactions with family members is critical for inductive reasoning. As you work to improve your inductive reasoning, begin by first noticing details about the things around you. A nurse is similar to the detective looking for cues in Figure 4.1.[4] Be mindful of your five primary senses: the things that you hear, feel, smell, taste, and see. Nurses need strong inductive reasoning patterns and be able to take action quickly, especially in emergency situations. They can see how certain objects or events form a pattern (i.e., generalization) that indicates a common problem (i.e., hypothesis).
Example: A nurse assesses a client and finds the surgical incision site is red, warm, and tender to the touch. The nurse recognizes these cues form a pattern of signs of infection and creates a hypothesis that the incision has become infected. The provider is notified of the client’s change in condition, and a new prescription is received for an antibiotic. This is an example of the use of inductive reasoning in nursing practice.

Deductive reasoning is another type of critical thinking that is referred to as “top-down thinking.” Deductive reasoning relies on using a general standard or rule to create a strategy. Deductive reasoning relies on a general statement or hypothesis – sometimes called a premise or standard – that is held to be true. The premise is used to reach a specific, logical conclusion. Nurses use standards set by their state’s Nurse Practice Act, federal regulations, the American Nursing Association, professional organizations, and their employer to make decisions about client care and solve problems.
Example: Based on research findings, hospital leaders determine clients recover more quickly if they receive adequate rest. The hospital creates a policy for quiet zones at night by initiating no overhead paging, promoting low-speaking voices by staff, and reducing lighting in the hallways. (See Figure 4.2).[5] The nurse further implements this policy by organizing care for clients that promotes periods of uninterrupted rest at night. This is an example of deductive thinking because the intervention is applied to all clients regardless if they have difficulty sleeping or not.
Clinical judgment is the result of critical thinking and clinical reasoning using inductive and deductive reasoning. Clinical judgment is defined by the National Council of State Boards of Nursing (NCSBN) as, “The observed outcome of critical thinking and decision-making. It uses nursing knowledge to observe and assess presenting situations, identify a prioritized client concern, and generate the best possible evidence-based solutions in order to deliver safe client care.”[6] The NCSBN administers the national licensure exam (NCLEX) that evaluates the decision-making ability of nursing graduates and sets a minimum standard for safe, competent nursing care by entry-level licensed nurses. The NCLEX uses the NCSBN Clinical Judgment Measurement Model (NCJMM) to measure clinical judgment.
Evidence-based practice (EBP) is defined by the American Nurses Association (ANA) as, “A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and client, family, group, community, and population preferences and values.”[7]
Nursing Process
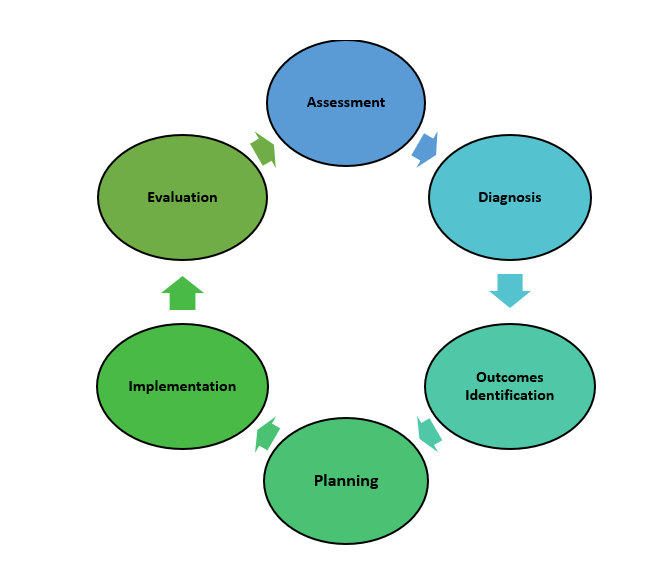
The nursing process is a critical thinking model based on a systematic approach to client-centered care. Nurses use the nursing process to perform clinical reasoning and make clinical judgments when providing client care. The nursing process is based on the Standards of Professional Nursing Practice established by the American Nurses Association (ANA). These standards are authoritative statements of the actions and behaviors that all registered nurses (RNs), regardless of role, population, specialty, and setting, are expected to perform competently.[8] The mnemonic ADOPIE is an easy way to remember the ANA Standards and the nursing process. Each letter refers to the six components of the nursing process: Assessment, Diagnosis, Outcomes Identification, Planning, Implementation, and Evaluation.
The nursing process is a continuous, cyclical process that is constantly adapting to the client’s current health status. See Figure 4.3[9] for an illustration of the nursing process.
The ANA’s Standards of Professional Nursing Practice associated with each component of the nursing process are described below.
Assessment
The “Assessment” Standard of Practice is defined as, “The registered nurse collects pertinent data and information relative to the health care consumer’s health or the situation.”[10] A registered nurse uses a systematic method to collect and analyze client data. Assessment includes physiological data, as well as psychological, sociocultural, spiritual, economic, and lifestyle data. For example, a nurse’s assessment of a hospitalized client in pain includes recognizing cues such as the client’s response to pain, such as the inability to get out of bed, refusal to eat, withdrawal from family members, or anger directed at hospital staff.[11]
Licensed practical/vocational nurses (LPN/VNs) assist with gathering data according to their state’s scope of practice, but do not analyze data because this is outside their scope of practice. The “Assessment” component of the nursing process is further described in the “Assessment” section of this chapter.
Diagnosis
The “Diagnosis” Standard of Practice is defined as, “The registered nurse analyzes the assessment data to determine actual or potential diagnoses, problems, and issues.”[12] A nursing diagnosis is the nurse’s clinical judgment about the response from the client to actual or potential health conditions or needs. Nursing diagnoses are the bases for the nurse’s care plan and are different than medical diagnoses.[13]
Analyzing assessment data and formulating a nursing diagnosis is outside the scope of practice for LPN/VNs, and as such, they do not assist with this phase of the nursing process. The “Diagnosis” component of the nursing process is further described in the “Diagnosis” section of this chapter.
Outcome Identification
The “Outcome Identification” Standard of Practice is defined as, “The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation.”[14] The nurse sets measurable and achievable short- and long-term goals and specific outcomes in collaboration with the client based on their assessment data and nursing diagnoses.
Outcome identification is outside the scope of practice of LPN/VNs, and as such, they do not assist with this phase of the nursing process. The “Outcome Identification” component of the nursing process is further described in the “Outcome Identification” section of this chapter.
Planning
The “Planning” Standard of Practice is defined as, “The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes.”[15] Assessment data, diagnoses, and goals are used to select evidence-based nursing interventions customized to each client’s needs in order to achieve their previously established goals and outcomes. Nursing interventions are planned and documented by RNs in the client’s nursing care plan so that nurses, as well as other health professionals, can refer to it for continuity of care.[16]
The “Planning” component of the nursing process is further described in the “Planning” section of this chapter.
Nursing Care Plans
Creating nursing care plans is a part of the “Planning” step of the nursing process. A nursing care plan is a type of documentation that demonstrates the individualized planning and delivery of nursing care for each specific client using the nursing process. RNs create nursing care plans so that the care provided to the client across shifts is consistent among health care personnel. Some interventions can be delegated to LPN/VNs or trained Unlicensed Assistive Personnel (UAPs) with RN supervision.
Creating the nursing care plan is outside the scope of practice, and as such, the LPN/VNs do not perform this task, although they may contribute to it. Developing nursing care plans and implementing appropriate delegation are further discussed under the “Planning” and “Implementation of Interventions” sections of this chapter.
Implementation
The “Implementation” Standard of Practice is defined as, “The nurse implements the identified plan.”[17] Nursing interventions are implemented or delegated with supervision according to the care plan to assure continuity of care across multiple nurses and health professionals caring for the client. Interventions are documented in the client’s electronic medical record as they are completed.[18] LPN/VNs implement interventions contained in the nursing care plan, provided they are within their scope of practice. The LPN/VN is responsible for documenting the interventions they perform in the client’s medical record.
The “Implementation” Standard of Professional Practice also includes the subcategories “Coordination of Care” and “Health Teaching and Health Promotion” to promote health and a safe environment.[19]
The “Implementation” component of the nursing process is further described in the “Implementation of Interventions” section of this chapter.
Evaluation
The “Evaluation” Standard of Practice is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.”[20] During evaluation, nurses reassess the client and compare the findings against established outcomes to determine the effectiveness of the interventions and overall nursing care plan. During this phase, RNs ask, “Were outcomes met? Are any modifications required for the nursing care plan?” Both the client’s status and the effectiveness of the nursing care plan are continuously evaluated and modified as needed.[21]
Evaluating and modifying the nursing care plan is outside the scope of practice of LPN/VNs, although they can assist in gathering assessment data to assist the RN in performing this step of the nursing process. The “Evaluation” component of the nursing process is further described in the “Evaluation” section of this chapter.
Benefits of Using the Nursing Process
Using the nursing process has many benefits for nurses, clients, and other members of the health care team. The benefits of using the nursing process include the following:
- Promotes quality client care
- Decreases omissions and duplications
- Provides a guide for all staff involved to provide consistent and responsive care
- Encourages collaborative management of a client’s health care problems
- Improves client safety
- Improves client satisfaction
- Identifies a client’s goals and strategies to attain them
- Increases the likelihood of achieving positive client outcomes
- Saves time, energy, and frustration by creating a care plan that is accessible to all staff caring for a client
By using these components of the nursing process as a critical thinking model, nurses plan outcomes and interventions that are customized to the client’s specific needs, ensure the interventions are evidence-based, and evaluate the effectiveness of interventions in meeting the client’s needs.
NCSBN Clinical Judgment Measurement Model
The NCSBN Clinical Judgment Measurement Model (NCJMM) complements the nursing process, but it is a model that assesses an NCLEX candidate’s clinical judgment. Terminology used by this model includes recognize cues, analyze cues, prioritize hypotheses, generate solutions, take action, and evaluate outcomes. See Figure 4.3b[22] and Table 4.2a for comparisons of NCJMM terms and the nursing process.[23],[24],[25]
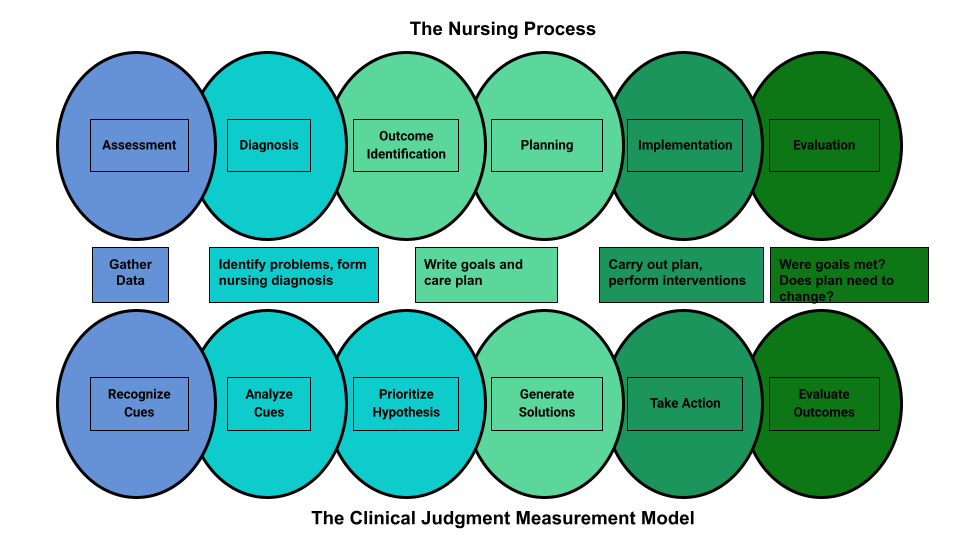
Figure 4.3b Comparison of the Steps of the NCJMM to the Nursing Process
Table 4.2a Comparison of the NCJMM to the Nursing Process
| NCSBN Clinical Judgment Skill | Description | Corresponding Step of the Nursing Process |
|---|---|---|
| Recognize Cues | What data is clinically significant?
Determining what client findings are significant, most important, and of immediate concern to the nurse (i.e., identifying “relevant cues”). |
Assessment |
| Analyze Cues | What does the data mean?
Analyzing data to determine if it is “expected” or “unexpected” or “normal” or “abnormal” for this client at this time according to their age, development, and clinical status. Making a clinical judgment concerning the client’s “human response to health conditions/life processes, or a vulnerability for that response”; also referred to as “forming a hypothesis.” |
Diagnosis
(Analysis of Data) |
| Prioritize Hypotheses | What hypotheses should receive priority attention?
Ranking client conditions and problems according to urgency, complexity, and time. |
Planning |
| Generate Solutions | What should be done?
Planning individualized interventions that meet the desired outcomes for the client; may include gathering additional assessment data. |
Planning |
| Take Action | What will I do now?
Implementing interventions that are safe and most appropriate for the client’s current priority conditions and problems. |
Implementation |
| Evaluate Outcomes | Did the interventions work?
Comparing actual client outcomes with desired client outcomes to determine effectiveness of care and making appropriate revisions to the nursing care plan. |
Evaluation |
Learning activities are incorporated throughout this book to help students practice answering NCLEX Next Generation-style test questions.
Review Scenario A in the following box for an example of a nurse using the nursing process and NCJMM skills while providing client care.
Client Scenario A: Using the Nursing Process[26]

A nurse is caring for a hospitalized client with a medical diagnosis of heart failure who has a prescription to receive furosemide 80mg IV every morning. The nurse uses critical thinking according to the nursing process and the NCJMM before administering the prescribed medication:
Assessment/Recognize Cues: During the morning assessment, the nurse notes that the client has a blood pressure of 98/60, heart rate of 100, respirations of 18, and a temperature of 98.7F.
Diagnosis/Analyze Cues: The nurse reviews the medical record for the client’s vital signs baseline and observes the blood pressure trend is around 110/70 and the heart rate in the 80s.
Planning/Prioritize Hypothesis: The nurse recognizes cues (assessment data) that form a pattern related to fluid imbalance and hypothesizes that the client may be dehydrated.
Planning/Generate Solutions: The nurse gathers additional information and notes the client’s weight has decreased four pounds since yesterday. The nurse talks with the client and validates the hypothesis when the client reports that their mouth feels like cotton, and they feel light-headed. By using critical thinking and clinical judgment, the nurse diagnoses the client with the nursing diagnosis Fluid Volume Deficit and plans interventions for reestablishing fluid balance.
Implementation/Take Action: The nurse withholds the administration of IV furosemide and contacts the health care provider to discuss the client’s current fluid status. After contacting the provider, the nurse initiates additional nursing interventions to promote oral intake and closely monitors hydration status.
Evaluation/Evaluate Outcomes: By the end of the shift, the nurse evaluates the client status and determines that fluid balance has been restored.
In Scenario A, the nurse is using clinical judgment and not just “following orders” to administer the Lasix as scheduled. The nurse assesses the client, recognizes and analyzes cues, creates a hypothesis regarding the fluid status, plans and implements nursing interventions, and evaluates outcomes. While performing these steps, the nurse promotes client safety by contacting the provider before administering a medication that could cause harm to the client at this time.
Holistic Nursing Care
Using the nursing process and clinical judgment while implementing evidence-based practices is referred to as the “science of nursing.” Before getting deeper into the science of nursing in the remainder of this chapter, it is important to discuss the “art of nursing” that relies on holistic care provided in a compassionate and caring manner using the nursing process.
The American Nurses Association (ANA) defines nursing as, “Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in the recognition of the connection of all humanity.”[27]
The ANA further describes nursing as a learned profession built on a core body of knowledge that integrates both the art and science of nursing. The art of nursing is defined as, “Unconditionally accepting the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care.”[28]
Nurses care for individuals holistically, including their emotional, spiritual, psychosocial, cultural, and physical needs. They consider problems, issues, and needs that the person experiences as a part of a family and a community as they use the nursing process. Review a scenario illustrating holistic nursing care provided to a client and their family in the following box.
Holistic Nursing Care Scenario
A single mother brings her child to the emergency room for ear pain and a fever. The physician diagnoses the child with an ear infection and prescribes an antibiotic. The mother is advised to make a follow-up appointment with their primary provider in two weeks. While providing discharge teaching, the nurse discovers that the family is unable to afford the expensive antibiotic prescribed and cannot find a primary care provider in their community they can reach by a bus route. The nurse asks a social worker to speak with the mother about affordable health insurance options and available providers in her community and follows up with the prescribing physician to obtain a prescription for a less expensive generic antibiotic. In this manner, the nurse provides holistic care and advocates for improved health for the child and their family.
Caring and the Nursing Process
The American Nurses Association (ANA) states, “The act of caring is foundational to the practice of nursing.”[29] Successful use of the nursing process requires the development of a care relationship with the client. A care relationship is a mutual relationship that requires the development of trust between both parties. This trust is often referred to as the development of rapport and underlies the art of nursing. While establishing a caring relationship, the whole person is assessed, including the individual’s beliefs, values, and attitudes, while also acknowledging the vulnerability and dignity of the client and family. Assessing and caring for the whole person takes into account the physical, mental, emotional, and spiritual aspects of being a human being.[30] Caring interventions can be demonstrated in simple gestures such as active listening, making eye contact, using therapeutic touch, and providing emotional support while respecting their cultural beliefs associated with caring behaviors.[31] See Figure 4.4[32] for an image of a nurse using touch as a therapeutic communication technique to communicate caring.
Dr. Jean Watson is a nurse theorist who has published many works on the art and science of caring in the nursing profession. Her theory of human caring sought to balance the cure orientation of medicine, giving nursing its unique disciplinary, scientific, and professional standing with itself and the public. Dr. Watson’s caring philosophy encourages nurses to be authentically present with their clients while creating a healing environment.[33]

Now that we have discussed basic concepts related to the nursing process, as well as the science and art of nursing, let’s look more deeply at each component of the nursing process in the following sections.
Media Attributions
- 3550755709_d8be7ba08b_b
- 2786901401_78efa24a0a_k
- pasted image 0
- Nursing Process and NCJMM
- hospice-1793998_1280
- Klenke-Borgmann, L., Cantrell, M. A., & Mariani, B. (2020). Nurse educator’s guide to clinical judgment: A review of conceptualization, measurement, and development. Nursing Education Perspectives, 41(4), 215-221. ↵
- Klenke-Borgmann, L., Cantrell, M. A., & Mariani, B. (2020). Nurse educator’s guide to clinical judgment: A review of conceptualization, measurement, and development. Nursing Education Perspectives, 41(4), 215-221. ↵
- Powers, L., Pagel, J., & Herron, E. (2020). Nurse preceptors and new graduate success. American Nurse Journal, 15(7), 37-39. ↵
- “The Detective” by paurian is licensed under CC BY 2.0 ↵
- “In the Quiet Zone…” by C.O.D. Library is licensed under CC BY-NC-SA 2.0 ↵
- NCSBN. (n.d.). NCSBN clinical judgment model. https://www.ncsbn.org/14798.htm ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- “The Nursing Process” by Kim Ernstmeyer at Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (3rd ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.) The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- “Nursing Process and NCJMM” by Tami Davis is licensed under CC BY 4.0 ↵
- NCSBN (n.d.) NCSBN Clinical Judgment Measurement Model. https://www.ncsbn.org/14798.htm ↵
- Ignativicius, V., & Silvestri, L. (2022). Preparing for the Next-Generation NCLEX (NGN): A “how-to” step-by-step faculty resource manual. Elsevier. https://evolve.elsevier.com/education/wp-content/uploads/sites/2/NGN_FacultyGuide_Final.pdf ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- “Patient Image in LTC.JPG” by ARISE project is licensed under CC BY 4.0 ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- Walivaara, B., Savenstedt, S., & Axelsson, K. (2013). Caring relationships in home-based nursing care - registered nurses’ experiences. The Open Journal of Nursing, 7, 89-95. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3722540/pdf/TONURSJ-7-89.pdf ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- “hospice-1793998_1280.jpg” by truthseeker08 is licensed under CC0 ↵
- Watson Caring Science Institute. (n.d.). Watson Caring Science Institute. Jean Watson, PHD, RN, AHN-BC, FAAN, (LL-AAN). https://www.watsoncaringscience.org/jean-bio/ ↵
Organizational Culture
The formal leaders of an organization provide a sense of direction and overall guidance for their employees by establishing organizational vision, mission, and values statements. An organization’s vision statement defines why the organization exists, describes how the organization is unique from similar organizations, and specifies what the organization is striving to be. The mission statement describes how the organization will fulfill its vision and establishes a common course of action for future endeavors. See Figure 4.1[1] for an illustration of a mission statement. A values statement establishes the values of an organization that assist with the achievement of its vision and mission. A values statement also provides strategic guidelines for decision-making, both internally and externally, by members of the organization. A values statement may also be reflected as the organization's "core values," which are the foundational ideals that guide the organization's actions and decision-making processes. The vision, mission, and values statements are expressed in a concise and clear manner that is easily understood by members of the organization and the public.[2]

Organizational culture refers to the implicit values and beliefs that reflect the norms and traditions of an organization. An organization’s vision, mission, and values statements are the foundation of organizational culture. Because individual organizations have their own vision, mission, and values statements, each organization has a different culture.[3] Organizational culture helps reflect the expected norms and behaviors that are inherent to an organization. Expected conduct is comprised of the unwritten rules and standards that reflect how employees should behave in different situations. The culture also informs the common communication styles that are inherent to an organization, including both formal and informal channels. The culture may also be manifested outwardly through various symbols and artifacts that embedded within the organization. These may include specific logos, objects, or other physical manifestations of elements that represent the organization's culture. Some organizations may also reflect their cultural values through activities or ceremonies held within the community.
As health care continues to evolve and new models of care are introduced, nursing managers must develop innovative approaches that address change while aligning with that organization’s vision, mission, and values. Leaders embrace the organization’s mission, identify how individuals’ work contributes to it, and ensure that outcomes advance the organization’s mission and purpose. Leaders use vision, mission, and values statements for guidance when determining appropriate responses to critical events and unforeseen challenges that are common in a complex health care system. Successful organizations require employees to be committed to following these strategic guidelines during the course of their work activities. Employees who understand the relationship between their own work and the mission and purpose of the organization will contribute to a stronger health care system that excels in providing first-class patient care. The vision, mission, and values provide a common organization-wide frame of reference for decision-making for both leaders and staff.[4] It is important for employees in health care organizations to have understanding of how their roles and responsibilities connect to the broader mission and vision of the organization. This alignment fosters a cohesive work environment where each staff member is motivated by a shared purpose, leading to more effective and high-quality patient care. It is important that both the leader and employee have clarity in the underlying vision, mission, and values of an organization. This involves responsibility for both the leader and employee. Leaders must articulate the organization's vision, mission, and values clearly and consistently. This involves regular communication through meetings, written materials, etc. Employees share in the responsibility by being empowered to ask questions and seek clarification on how their daily tasks contribute to the organization's overarching goals.
Learning Activity
Investigate the mission, vision, and values of a potential employer, as you would do prior to an interview for a job position.
Reflective Questions
- How well do the organization’s vision and values align with your personal values regarding health care?
- How well does the organization’s mission align with your professional objective in your resume?
Followership
Followership is described as the upward influence of individuals on their leaders and their teams. The actions of followers have an important influence on staff performance and patient outcomes. Being an effective follower requires individuals to contribute to the team not only by doing as they are told, but also by being aware and raising relevant concerns. Effective followers realize that they can initiate change and disagree or challenge their leaders if they feel their organization or unit is failing to promote wellness and deliver safe, value-driven, and compassionate care. Leaders who gain the trust and dedication of followers are more effective in their leadership role. Everybody has a voice and a responsibility to take ownership of the workplace culture, and good followership contributes to the establishment of high-functioning and safety-conscious teams.[5] Key elements of effective followership include proactive engagement, constructive communication, collaboration, advocacy, continuous improvement, and a supportive leadership environment.
In order to demonstrate proactive engagement, followers must also be initiators. Effective followers do not passively wait for instruction by rather take initiative to address issues, propose solutions, and contribute to ideas. They recognize the importance of their voice in engaging in problem-solving and understand that being an effective follower does not mean being passive in their role. Effective followers also employ a keen situational awareness where they maintain vigilant assessment of the environment and potential risks, ensuring that they act in the best interests of clients. They must be confident that they can raise concerns if they identify potential problems or unsafe practices. This reflects a culture where followers feels that their feedback is welcomed and valued. Effective followership also involves communication practices in which the message is clearly conveyed, measures to confirm the message are employed, and the confirmation is received. To be an effective follower, support of the team's goals must be a central tenet of one's work. Collaboration with others involves supporting colleagues and working together toward the common goal even when viewpoints may differ. Identifying strategies that create a respectful opportunity to debate and explore different opinions is important to effective followership. Additionally, followers must take accountability for their own actions while understanding how their role and performance impacts the function of the team, as well as client outcomes. Effective followers also practice ethical advocacy, ensuring that the needs of clients are prioritized and respected. This advocacy also involves the ability to courageously challenge any decisions or actions that may jeopardize care or organizational values. Finally, effective followers engage in continuous learning to enhance their skills and knowledge. They seek feedback and use the feedback to contribute to their own performance and also the growth of the team. Effective followership is further cultivated when leaders and followers come together with mutual respect, trust, and work with a purposeful drive toward shared goals that reflect the organization's mission.
Team members impact patient safety by following teamwork guidelines for good followership. For example, strategies such as closed-loop communication are important tools to promote patient safety.
Read more about communication and teamwork strategies in the “Collaboration Within the Interprofessional Team” chapter.
Leadership and Management Characteristics
Leadership and management are terms often used interchangeably, but they are two different concepts with many overlapping characteristics. Leadership is the art of establishing direction and influencing and motivating others to achieve their maximum potential to accomplish tasks, objectives, or projects.[6],[7] See Figure 4.2[8] for an illustration of team leadership. There is no universally accepted definition or theory of nursing leadership, but there is increasing clarity about how it differs from management.[9] Management refers to roles that focus on tasks such as planning, organizing, prioritizing, budgeting, staffing, coordinating, and reporting.[10] The overriding function of management has been described as providing order and consistency to organizations, whereas the primary function of leadership is to produce change and movement.[11] View a comparison of the characteristics of management and leadership in Table 4.2a.

Table 4.2a. Management and Leadership Characteristics[12]
| MANAGEMENT | LEADERSHIP |
|---|---|
Planning, Organizing, and Prioritizing
|
Establishing Direction
|
Budgeting and Staffing
|
Influencing Others
|
Coordinating and Problem-Solving
|
Motivating
|
Leader Vs. Manager Case Activity
Utilizing the information from the table above, review the following cases and identify whether the individual is serving as a leader or manager based upon the actions taken within the case scenario. Include supportive rationale for your decision regarding the role.
Case 1: Sima, the head nurse, reviews the upcoming schedule and allocates resources to ensure each shift is adequately staffed. She also makes assignments for the nursing staff based on their skills and patient needs. Additionally, she is responsible for hiring new staff and, when necessary, terminating employees who do not meet performance standards.
Case 2: Juan, a senior nurse, is passionate about improving patient care. He identifies an issue with the current handoff process between shifts and proposes a new strategy that incorporates evidence-based practices to enhance communication and reduce errors. He reaches out to his team at their monthly department meetings in order to develop a shared vision for this change and encourages them to partner with him on the new process.
Case 3: Maria, a unit supervisor, holds a meeting to set specific goals and time frames for the department’s upcoming projects. She prioritizes tasks for the team and establishes policies and procedures to ensure these tasks are completed efficiently and within the given deadlines.
Case 4: Emily, the nurse director, is tasked with preparing the budget for the upcoming fiscal year. She allocates resources effectively to ensure all departments are adequately funded. Emily also manages the staffing needs, ensuring that the hiring and termination processes are handled efficiently.
Case 5: Rachel, an experienced nurse, takes the time to build effective teamwork within her unit. She advocates for her patients, their families, and the nursing profession as a whole. Rachel communicates openly and listens to her team’s concerns, ensuring everyone feels valued and heard.
Not all nurses are managers, but all nurses are leaders because they encourage individuals to achieve their goals. The American Nurses Association (ANA) established Leadership as a Standard of Professional Performance for all registered nurses. Standards of Professional Performance are “authoritative statements of action and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently.”[13] See the competencies of the ANA Leadership standard in the following box and additional content in other chapters of this book.
Competencies of ANA’s Leadership Standard of Professional Performance
- Promotes effective relationships to achieve quality outcomes and a culture of safety
- Leads decision-making groups
- Engages in creating an interprofessional environment that promotes respect, trust, and integrity
- Embraces practice innovations and role performance to achieve lifelong personal and professional goals
- Communicates to lead change, influence others, and resolve conflict
- Implements evidence-based practices for safe, quality health care and health care consumer satisfaction
- Demonstrates authority, ownership, accountability, and responsibility for appropriate delegation of nursing care
- Mentors colleagues and others to embrace their knowledge, skills, and abilities
- Participates in professional activities and organizations for professional growth and influence
- Advocates for all aspects of human and environmental health in practice and policy
Read additional content related to leadership and management activities in corresponding chapters of this book:
- Read about the culture of safety in the “Legal Implications” chapter.
- Read about effective interprofessional teamwork and resolving conflict in the “Collaboration Within the Interprofessional Team” chapter.
- Read about quality improvement and implementing evidence-based practices in the “Quality and Evidence-Based Practice” chapter.
- Read more about delegation, supervision, and accountability in the “Delegation and Supervision” chapter.
- Read about professional organizations and advocating for patients, communities, and their environments in the “Advocacy” chapter.
- Read about budgets and staffing in the “Health Care Economics” chapter.
- Read about prioritization in the “Prioritization” chapter.
Leadership Theories and Styles
In the 1930s Kurt Lewin, the father of social psychology, originally identified three leadership styles: authoritarian, democratic, and laissez-faire.[14],[15]
Authoritarian leadership means the leader has full power. Authoritarian leaders tell team members what to do and expect team members to execute their plans. When fast decisions must be made in emergency situations, such as when a patient “codes,” the authoritarian leader makes quick decisions and provides the group with direct instructions. However, there are disadvantages to authoritarian leadership. Authoritarian leaders are more likely to disregard creative ideas of other team members, causing resentment and stress.[16]
Democratic leadership balances decision-making responsibility between team members and the leader. Democratic leaders actively participate in discussions, but also make sure to listen to the views of others. For example, a nurse supervisor may hold a meeting regarding an increased incidence of patient falls on the unit and ask team members to share their observations regarding causes and potential solutions. The democratic leadership style often leads to positive, inclusive, and collaborative work environments that encourage team members’ creativity. Under this style, the leader still retains responsibility for the final decision.[17]
Laissez-faire is a French word that translates to English as, “leave alone.” Laissez-faire leadership gives team members total freedom to perform as they please. Laissez-faire leaders do not participate in decision-making processes and rarely offer opinions. The laissez-faire leadership style can work well if team members are highly skilled and highly motivated to perform quality work. However, without the leader’s input, conflict and a culture of blame may occur as team members disagree on roles, responsibilities, and policies. By not contributing to the decision-making process, the leader forfeits control of team performance.[18]
Over the decades, Lewin’s original leadership styles have evolved into many styles of leadership in health care, such as passive-avoidant, transactional, transformational, servant, resonant, and authentic.[19],[20] Many of these leadership styles have overlapping characteristics. See Figure 4.3[21] for a comparison of various leadership styles in terms of engagement.

Passive-avoidant leadership is similar to laissez-faire leadership and is characterized by a leader who avoids taking responsibility and confronting others. Employees perceive the lack of control over the environment resulting from the absence of clear directives. Organizations with this type of leader have high staff turnover and low retention of employees. These types of leaders tend to react and take corrective action only after problems have become serious and often avoid making any decisions at all.[22]
Transactional leadership involves both the leader and the follower receiving something for their efforts; the leader gets the job done and the follower receives pay, recognition, rewards, or punishment based on how well they perform the tasks assigned to them.[23] Staff generally work independently with no focus on cooperation among employees or commitment to the organization.[24]
Transformational leadership involves leaders motivating followers to perform beyond expectations by creating a sense of ownership in reaching a shared vision.[25] It is characterized by a leader’s charismatic influence over team members and includes effective communication, valued relationships, and consideration of team member input. Transformational leaders know how to convey a sense of loyalty through shared goals, resulting in increased productivity, improved morale, and increased employees’ job satisfaction.[26] They often motivate others to do more than originally intended by inspiring them to look past individual self-interest and perform to promote team and organizational interests.[27]
Servant leadership focuses on the professional growth of employees while simultaneously promoting improved quality care through a combination of interprofessional teamwork and shared decision-making. Servant leaders assist team members to achieve their personal goals by listening with empathy and committing to individual growth and community-building. They share power, put the needs of others first, and help individuals optimize performance while forsaking their own personal advancement and rewards.[28]
Visit the Greenleaf Center site to learn more about What is Servant Leadership?
Resonant leaders are in tune with the emotions of those around them, use empathy, and manage their own emotions effectively. Resonant leaders build strong, trusting relationships and create a climate of optimism that inspires commitment even in the face of adversity. They create an environment where employees are highly engaged, making them willing and able to contribute with their full potential.[29]
Authentic leaders have an honest and direct approach with employees, demonstrating self-awareness, internalized moral perspective, and relationship transparency. They strive for trusting, symmetrical, and close leader–follower relationships; promote the open sharing of information; and consider others’ viewpoints.[30]
Table 4.2b. Characteristics of Leadership Styles
| Authoritarian | Democratic | Laissez-Faire or Passive-Avoidant |
|---|---|---|
|
|
|
| Transactional | Transformational | Servant |
|---|---|---|
|
|
|
| Resonant Leaders | Authentic Leaders |
|---|---|
|
|
Outcomes of Various Leadership Styles
Leadership styles affect team members, patient outcomes, and the organization. A systematic review of the literature published in 2021 showed significant correlations between leadership styles and nurses’ job satisfaction. Transformational leadership style had the greatest positive correlation with nurses’ job satisfaction, followed by authentic, resonant, and servant leadership styles. Passive-avoidant and laissez-faire leadership styles showed a negative correlation with nurses’ job satisfaction.[31] In this challenging health care environment, managers and nurse leaders must promote technical and professional competencies of their staff, but they must also act to improve staff satisfaction and morale by using appropriate leadership styles with their team.[32]
Systems Theory
Systems theory is based on the concept that systems do not function in isolation but rather there is an interdependence that exists between their parts. Systems theory assumes that most individuals strive to do good work but are affected by diverse influences within the system. Efficient and functional systems account for these diverse influences and improve outcomes by studying patterns and behaviors across the system.[33]
Many health care agencies have adopted a culture of safety based on systems theory. A culture of safety is an organizational culture that embraces error reporting by employees with the goal of identifying systemic causes of problems that can be addressed to improve patient safety. According to The Joint Commission, a culture of safety includes the following components[34]:
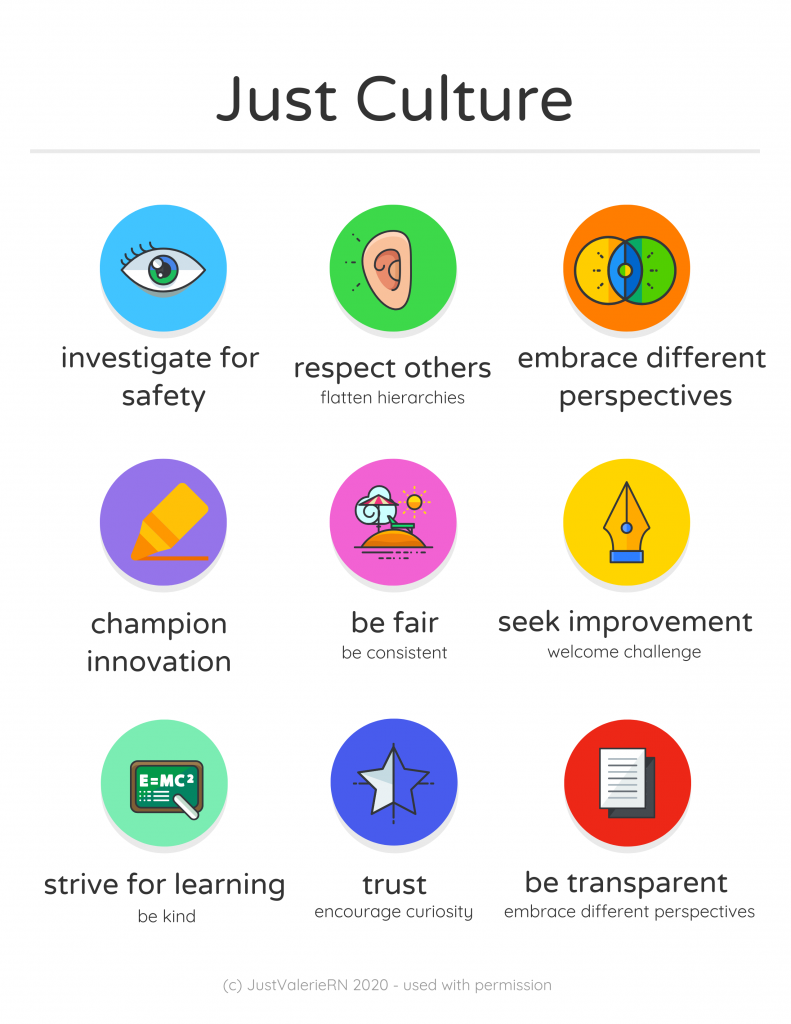
- Just Culture: A culture where people feel safe raising questions and concerns and report safety events in an environment that emphasizes a nonpunitive response to errors and near misses. Clear lines are drawn by managers between human error, at-risk, and reckless employee behaviors. See Figure 4.4[35] for an illustration of Just Culture.
- Reporting Culture: People realize errors are inevitable and are encouraged to speak up for patient safety by reporting errors and near misses. For example, nurses complete an “incident report” according to agency policy when a medication error occurs, or a client falls. Error reporting helps the agency manage risk and reduce potential liability.
- Learning Culture: People regularly collect information and learn from errors and successes while openly sharing data and information and applying best evidence to improve work processes and patient outcomes.
Just Culture
The American Nurses Association (ANA) officially endorses the Just Culture model. In 2019 the ANA published a position statement on Just Culture, stating, “Traditionally, healthcare’s culture has held individuals accountable for all errors or mishaps that befall patients under their care. By contrast, a Just Culture recognizes that individual practitioners should not be held accountable for system failings over which they have no control. A Just Culture also recognizes many individual or ‘active’ errors represent predictable interactions between human operators and the systems in which they work. However, in contrast to a culture that touts ‘no blame’ as its governing principle, a Just Culture does not tolerate conscious disregard of clear risks to patients or gross misconduct (e.g., falsifying a record or performing professional duties while intoxicated).”
The Just Culture model categorizes human behavior into three causes of errors. Consequences of errors are based on whether the error is a simple human error or caused by at-risk or reckless behavior.
- Simple human error: A simple human error occurs when an individual inadvertently does something other than what should have been done. Most medical errors are the result of human error due to poor processes, programs, education, environmental issues, or situations. These errors are managed by correcting the cause, looking at the process, and fixing the deviation. For example, a nurse appropriately checks the rights of medication administration three times, but due to the similar appearance and names of two different medications stored next to each other in the medication dispensing system, administers the incorrect medication to a patient. In this example, a root cause analysis reveals a system issue that must be modified to prevent future patient errors (e.g., change the labelling and storage of look alike-sound alike medication).
- At-risk behavior: An error due to at-risk behavior occurs when a behavioral choice is made that increases risk where the risk is not recognized or is mistakenly believed to be justified. For example, a nurse scans a patient’s medication with a barcode scanner prior to administration, but an error message appears on the scanner. The nurse mistakenly interprets the error to be a technology problem and proceeds to administer the medication instead of stopping the process and further investigating the error message, resulting in the wrong dosage of a medication being administered to the patient. In this case, ignoring the error message on the scanner can be considered “at-risk behavior” because the behavioral choice was considered justified by the nurse at the time.
- Reckless behavior: Reckless behavior is an error that occurs when an action is taken with conscious disregard for a substantial and unjustifiable risk.[36] For example, a nurse arrives at work intoxicated and administers the wrong medication to the wrong patient. This error is considered due to reckless behavior because the decision to arrive intoxicated was made with conscious disregard for substantial risk.
These examples show three different causes of medication errors that would result in different consequences to the employee based on the Just Culture model. Under the Just Culture model, after root cause analysis is completed, system-wide changes are made to decrease factors that contributed to the error. Managers appropriately hold individuals accountable for errors if they were due to simple human error, at-risk behavior, or reckless behaviors.
If an individual commits a simple human error, managers console the individual and consider changes in training, procedures, and processes. In the “simple human error” above, system-wide changes would be made to change the label and location of the medication to prevent future errors from occurring with the same medication.
Individuals committing at-risk behavior are held accountable for their behavioral choice and often require coaching with incentives for less risky behaviors and situational awareness. In the “at-risk behavior” example above where the nurse ignored an error message on the barcode scanner, mandatory training on using a barcode scanner and responding to errors would be implemented, and the manager would track the employee’s correct usage of the barcode scanner for several months following training.
If an individual demonstrates reckless behavior, remedial action and/or punitive action is taken.[37] In the “reckless behavior” example above, the manager would report the nurse’s behavior to the state's Board of Nursing with mandatory substance abuse counseling to maintain their nursing license. Employment may be terminated with consideration of patterns of behavior.
A Just Culture in which employees aren't afraid to report errors is a highly successful way to enhance patient safety, increase staff and patient satisfaction, and improve outcomes. Success is achieved through good communication, effective management of resources, and an openness to changing processes to ensure the safety of patients and employees. The infographic in Figure 4.4[38] illustrates the components of a culture of safety and Just Culture.
The principles of culture of safety, including Just Culture, Reporting Culture, and Learning Culture are also being adopted in nursing education. It’s understood that mistakes are part of learning and that a shared accountability model promotes individual- and system-level learning for improved patient safety. Under a shared accountability model, students are responsible for the following[39]:
- Being fully prepared for clinical experiences, including laboratory and simulation assignments
- Being rested and mentally ready for a challenging learning environment
- Accepting accountability for their part in contributing to a safe learning environment
- Behaving professionally
- Reporting their own errors and near mistakes
- Keeping up-to-date with current evidence-based practice
- Adhering to ethical and legal standards
Students know they will be held accountable for their actions but will not be blamed for system faults that lie beyond their control. They can trust that a fair process will be used to determine what went wrong if a patient care error or near miss occurs. Student errors and near misses are addressed based on an investigation determining if it was simple human error, an at-risk behavior, or reckless behavior. For example, a simple human error by a student can be addressed with coaching and additional learning opportunities to remedy the knowledge deficit. However, if a student acts with recklessness (for example, repeatedly arrives to clinical unprepared despite previous faculty feedback or falsely documents an assessment or procedure), they are appropriately and fairly disciplined, which may include dismissal from the program.[40]
See Table 4.2c describing classifications of errors using the Just Culture model.
Table 4.2c. Classification of Errors Using the Just Culture Model
| Human Error | At-Risk Behavior | Reckless Behavior |
|---|---|---|
| The caregiver made an error while working appropriately and focusing on the patient’s best interests. | The caregiver made a potentially unsafe choice resulting from faulty or self-serving decision-making. | The caregiver knowingly violated a rule and/or made a dangerous or unsafe choice. |
| Investigation reveals system factors contributing to similar errors by others with similar knowledge and skills. | Investigation reveals the system supports risky action and the caregiver requires coaching. | Investigation reveals the caregiver is accountable and needs retraining. |
| Manage by fixing system errors in processes, procedures, training, design, or environment. | Manage by coaching the caregiver and fixing any system issues:
|
Manage by disciplining the caregiver. If the system supports reckless behavior, it requires fixing. |
| CONSOLE | COACH | PUNISH |
Systems leadership refers to a set of skills used to catalyze, enable, and support the process of systems-level change that is encouraged by the Just Culture Model. Systems leadership is comprised of three interconnected elements:[41]
- The Individual: The skills of collaborative leadership to enable learning, trust-building, and empowered action among stakeholders who share a common goal
- The Community: The tactics of coalition building and advocacy to develop alignment and mobilize action among stakeholders in the system, both within and between organizations
- The System: An understanding of the complex systems shaping the challenge to be addressed
Just Culture Case Review
Review the following case descriptions. Identify the classification of error that has occurred and the recommended actions that should occur.
A chief nursing officer receives a daily report of organization incident reports and reviews the following incident:
Incident Description
Patient Mr. Joe Doden, Room 13067, Medical-Surgical floor
On the afternoon of May 15, 2024, Nurse Sarah was responsible for administering Mr. Joe Doden's insulin dose. The insulin vials used by the hospital had recently been redesigned by the manufacturer, which led to changes in the labeling. The patient was scheduled to receive ten units of regular insulin at 14:30. However, at 1450 the patient turns on his call light, reports feeling unwell. He is shaky, confused, and sweating profusely. The patient's glucose is checked, and he is found to be hypoglycemic. He is treated based upon the hypoglycemia protocol and recovers without further complication.
Case Investigation A
Action: Sarah RN who administered the insulin was following the protocol but mistakenly read the dosage due to a poorly designed label on the insulin vial. The nurse was focused on the patient’s best interests and followed all required steps.
Findings: The investigation revealed that the labeling on the insulin vials was confusing and had led to similar errors by other nurses in the past. The system's design flaw contributed significantly to the error.
How would you classify this error? What actions should be taken?
Case Investigation B
Action: Sarah RN, due to time pressure and a high patient load, decided to skip the double-check protocol for administering the same insulin dose, believing it would save time without causing harm.
Findings: The investigation revealed that the hospital’s workload and time pressures often led to shortcuts in following safety protocols.
How would you classify this error? What actions should be taken?
Case Investigation C
Action: Sarah RN, is familiar with the protocol and knowingly bypassed the double check system, dismissing its importance and administering a medication dose on her own.
Findings: The investigation found that the nurse had a history of disregarding safety protocols, showing a pattern of reckless behavior. This behavior was not supported by the hospital’s policies or environment.
How would you classify this error? What actions should be taken?
Change is constant in the health care environment. Change is defined as the process of altering or replacing existing knowledge, skills, attitudes, systems, policies, or procedures.[42] The outcomes of change must be consistent with an organization’s mission, vision, and values. Although change is a dynamic process that requires alterations in behavior and can cause conflict and resistance, change can also stimulate positive behaviors and attitudes and improve organizational outcomes and employee performance. Change can result from identified problems or from the incorporation of new knowledge, technology, management, or leadership. Problems may be identified from many sources, such as quality improvement initiatives, employee performance evaluations, or accreditation survey results.[43]
Nurse managers must deal with the fears and concerns triggered by change. They should recognize that change may not be easy and may be met with enthusiasm by some and resistance by others. Leaders should identify individuals who will be enthusiastic about the change (referred to as “early adopters”), as well as those who will be resisters (referred to as "laggers"). Early adopters should be involved to build momentum, and the concerns of resisters should be considered to identify barriers. Data should be collected, analyzed, and communicated so the need for change (and its projected consequences) can be clearly articulated. Managers should articulate the reasons for change, the way(s) the change will affect employees, the way(s) the change will benefit the organization, and the desired outcomes of the change process.[44] See Figure 4.5[45] for an illustration of communicating upcoming change.

Change Theories
There are several change theories that nurse leaders may adopt when implementing change. Two traditional change theories are known as Lewin’s Unfreeze-Change-Refreeze Model and Lippitt’s Seven-Step Change Theory.[46]
Lewin’s Change Model
Kurt Lewin, the father of social psychology, introduced the classic three-step model of change known as Unfreeze-Change-Refreeze Model that requires prior learning to be rejected and replaced. Lewin’s model has three major concepts: driving forces, restraining forces, and equilibrium. Driving forces are those that push in a direction and cause change to occur. They facilitate change because they push the person in a desired direction. They cause a shift in the equilibrium towards change. Restraining forces are those forces that counter the driving forces. They hinder change because they push the person in the opposite direction. They cause a shift in the equilibrium that opposes change. Equilibrium is a state of being where driving forces equal restraining forces, and no change occurs. It can be raised or lowered by changes that occur between the driving and restraining forces.[47],[48]
- Step 1: Unfreeze the status quo. Unfreezing is the process of altering behavior to agitate the equilibrium of the current state. This step is necessary if resistance is to be overcome and conformity achieved. Unfreezing can be achieved by increasing the driving forces that direct behavior away from the existing situation or status quo while decreasing the restraining forces that negatively affect the movement from the existing equilibrium. Nurse leaders can initiate activities that can assist in the unfreezing step, such as motivating participants by preparing them for change, building trust and recognition for the need to change, and encouraging active participation in recognizing problems and brainstorming solutions within a group.[49]
- Step 2: Change. Change is the process of moving to a new equilibrium. Nurse leaders can implement actions that assist in movement to a new equilibrium by persuading employees to agree that the status quo is not beneficial to them; encouraging them to view the problem from a fresh perspective; working together to search for new, relevant information; and connecting the views of the group to well-respected, powerful leaders who also support the change.[50]
- Step 3: Refreeze. Refreezing refers to attaining equilibrium with the newly desired behaviors. This step must take place after the change has been implemented for it to be sustained over time. If this step does not occur, it is very likely the change will be short-lived and employees will revert to the old equilibrium. Refreezing integrates new values into community values and traditions. Nursing leaders can reinforce new patterns of behavior and institutionalize them by adopting new policies and procedures.[51]
Example Using Lewin’s Change Theory
A new nurse working in a rural medical-surgical unit identifies that bedside handoff reports are not currently being used during shift reports.
Step 1: Unfreeze: The new nurse recognizes a change is needed for improved patient safety and discusses the concern with the nurse manager. Current evidence-based practice is shared regarding bedside handoff reports between shifts for patient safety.[52] The nurse manager initiates activities such as scheduling unit meetings to discuss evidence-based practice and the need to incorporate bedside handoff reports.
Step 2: Change: The nurse manager gains support from the director of nursing to implement organizational change and plans staff education about bedside report checklists and the manner in which they are performed.
Step 3: Refreeze: The nurse manager adopts bedside handoff reports in a new unit policy and monitors staff for effectiveness.
Lippitt’s Seven-Step Change Theory
Lippitt’s Seven-Step Change Theory expands on Lewin’s change theory by focusing on the role of the change agent. A change agent is anyone who has the skill and power to stimulate, facilitate, and coordinate the change effort. Change agents can be internal, such as nurse managers or employees appointed to oversee the change process, or external, such as an outside consulting firm. External change agents are not bound by organizational culture, politics, or traditions, so they bring a different perspective to the situation and challenge the status quo. However, this can also be a disadvantage because external change agents lack an understanding of the agency's history, operating procedures, and personnel.[53] The seven-step model includes the following steps[54]:
- Step 1: Diagnose the problem. Examine possible consequences, determine who will be affected by the change, identify essential management personnel who will be responsible for fixing the problem, collect data from those who will be affected by the change, and ensure those affected by the change will be committed to its success.
- Step 2: Evaluate motivation and capability for change. Identify financial and human resources capacity and organizational structure.
- Step 3: Assess the change agent’s motivation and resources, experience, stamina, and dedication.
- Step 4: Select progressive change objectives. Define the change process and develop action plans and accompanying strategies.
- Step 5: Explain the role of the change agent to all employees and ensure the expectations are clear.
- Step 6: Maintain change. Facilitate feedback, enhance communication, and coordinate the effects of change.
- Step 7: Gradually terminate the helping relationship of the change agent.
Example Using Lippitt’s Seven-Step Change Theory
Refer to the previous example of using Lewin’s change theory on a medical-surgical unit to implement bedside handoff reporting. The nurse manager expands on the Unfreeze-Change-Refreeze Model by implementing additional steps based on Lippitt’s Seven-Step Change Theory:
- The nurse manager collects data from team members affected by the changes and ensures their commitment to success.
- Early adopters are identified as change agents on the unit who are committed to improving patient safety by implementing evidence-based practices such as bedside handoff reporting.
- Action plans (including staff education and mentoring), timelines, and expectations are clearly communicated to team members as progressive change objectives. Early adopters are trained as “super-users” to provide staff education and mentor other nurses in using bedside handoff checklists across all shifts.
- The nurse manager facilitates feedback and encourages two-way communication about challenges as change is implemented on the unit. Positive reinforcement is provided as team members effectively incorporate change.
- Bedside handoff reporting is implemented as a unit policy, and all team members are held accountable for performing accurate bedside handoff reporting.
Read more about additional change theories in the Current Theories of Change Management pdf.
Change Management
Change management is the process of making changes in a deliberate, planned, and systematic manner.[55] It is important for nurse leaders and nurse managers to remember a few key points about change management[56]:
- Employees will react differently to change, no matter how important or advantageous the change is purported to be. Recognizing this variability is crucial for effectively managing the transition process.
- Basic needs will influence reaction to change, such as the need to be part of the change process, the need to be able to express oneself openly and honestly, and the need to feel that one has some control over the impact of change. Ensuring these needs are met can significantly reduce resistance.
- Change often results in a feeling of loss due to changes in established routines. Employees may react with shock, anger, and resistance, but ideally will eventually accept and adopt change. Acknowledging these feelings and providing support can facilitate smoother transitions.
- Change must be managed realistically, without false hopes and expectations, yet with enthusiasm for the future. Employees should be provided information honestly and allowed to ask questions and express concerns. This transparency builds trust and helps in aligning everyone towards common goals.
Strategies for Effective Change Management
- Engage Stakeholders Early: Involve key stakeholders in the planning stages of the change process. Their input can provide valuable insights and help in identifying potential challenges early on.
- Communicate Clearly and Frequently: Clear and frequent communication is essential. Use multiple channels to disseminate information and ensure that the message is consistent and comprehensible to all staff members.
- Provide Training and Resources: Equip employees with the necessary skills and resources to adapt to the change. This might include training sessions, informational materials, or access to support personnel.
- Build a Supportive Culture: Create an environment where change is viewed positively. Encourage collaboration and create opportunities for employees to share their experiences and strategies for adapting to change.
- Monitor and Adjust: Continuously monitor the progress of the change initiative and be prepared to make adjustments as needed. Solicit feedback from employees and be responsive to their concerns.
There are multiple strategies that can employed to overcome resistance to change. First, it is important to understand the underlying reasons for resistance. Resistance is commonly aligned to feelings of fear, lack of trust in leadership, or logistical concerns regarding workload, seniority, etc. To implement change effectively, a leader should empower staff by making sure they feel that their voice is respected and valued. When individuals feel valued and hear, they are more likely to support change, even if they do not personally agree with all elements associated with the change. Leaders also must understand that change is stressful for individuals. Depending on the significance of change, a leader may take actions to ensure that employee assistance programs, support groups, or additional counseling services or resources are available. These additional resources can be beneficial for individuals as they work through the emotions associated with the proposed change. Additionally, the benefits for any change should be clearly described. It is important to highlight how the proposed change will help improve work processes and patient care quality. It is also helpful to acknowledge and demonstrate appreciation for early adopters of the change. This can provide motivation and encouragement for others to follow suit and fosters a positive attitude toward future changes.
Jamie has recently completed his orientation to the emergency department at a busy Level 1 trauma center. The environment is fast-paced, and there are typically a multitude of patients who require care. Jamie appreciates his colleagues and the collaboration that is reflected among members of the health care team, especially in times of stress. Jamie is providing care for an 8-year-old patient who has broken her arm when there is a call that there are three Level 1 trauma patients approximately five minutes from the ER. The trauma surgeon reports to the ER, and multiple members of the trauma team report to the ER intake bays. If you were Jamie, what leadership style would you hope the trauma surgeon uses with the team?
In a stressful clinical care situation, where rapid action and direction are needed, an autocratic leadership style is most effective. There is no time for debating different approaches to care in a situation where immediate intervention may be required. Concise commands, direction, and responsive action from the team are needed to ensure that patient care interventions are delivered quickly to enhance chance of survival and recovery.
Jamie has recently completed his orientation to the emergency department at a busy Level 1 trauma center. The environment is fast-paced, and there are typically a multitude of patients who require care. Jamie appreciates his colleagues and the collaboration that is reflected among members of the health care team, especially in times of stress. Jamie is providing care for an 8-year-old patient who has broken her arm when there is a call that there are three Level 1 trauma patients approximately five minutes from the ER. The trauma surgeon reports to the ER, and multiple members of the trauma team report to the ER intake bays. If you were Jamie, what leadership style would you hope the trauma surgeon uses with the team?
In a stressful clinical care situation, where rapid action and direction are needed, an autocratic leadership style is most effective. There is no time for debating different approaches to care in a situation where immediate intervention may be required. Concise commands, direction, and responsive action from the team are needed to ensure that patient care interventions are delivered quickly to enhance chance of survival and recovery.
Learning Activities
Sample Scenario
An 89-year-old female resident with Alzheimer’s disease has been living at the nursing home for many years. The family decides they no longer want aggressive measures taken and request to the RN on duty that the resident’s code status be changed to Do Not Resuscitate (DNR). The evening shift RN documents a progress note that the family (and designated health care agent) requested that the resident’s status be made DNR. Due to numerous other responsibilities and needs during the evening shift, the RN does not notify the attending physician or relay the information during shift change or on the 24-hour report. The day shift RN does not read the night shift’s notes because of several immediate urgent situations. The family, who had been keeping vigil at the resident’s bedside throughout the night, leaves to go home to shower and eat. Upon return the next morning, they find the room full of staff and discover the staff performed CPR after their loved one coded. The resident was successfully resuscitated but now lies in a vegetative state. The family is unhappy and is considering legal action. They approach you, the current nurse assigned to the resident’s care, and state, “We followed your procedures to make sure this would not happen! Why was this not managed as we discussed?”[57]
Reflective Questions
- As the current nurse providing patient care, explain how you would therapeutically address this family’s concerns and use one or more leadership styles.
- As the charge nurse, explain how you would address the staff involved using one or more leadership styles.
- Explain how change theory can be implemented to ensure this type of situation does not recur.

Test your knowledge using this NCLEX Next Generation-style Case Study. You may reset and resubmit your answers to this question an unlimited number of times.[58]
Learning Activities
Sample Scenario
An 89-year-old female resident with Alzheimer’s disease has been living at the nursing home for many years. The family decides they no longer want aggressive measures taken and request to the RN on duty that the resident’s code status be changed to Do Not Resuscitate (DNR). The evening shift RN documents a progress note that the family (and designated health care agent) requested that the resident’s status be made DNR. Due to numerous other responsibilities and needs during the evening shift, the RN does not notify the attending physician or relay the information during shift change or on the 24-hour report. The day shift RN does not read the night shift’s notes because of several immediate urgent situations. The family, who had been keeping vigil at the resident’s bedside throughout the night, leaves to go home to shower and eat. Upon return the next morning, they find the room full of staff and discover the staff performed CPR after their loved one coded. The resident was successfully resuscitated but now lies in a vegetative state. The family is unhappy and is considering legal action. They approach you, the current nurse assigned to the resident’s care, and state, “We followed your procedures to make sure this would not happen! Why was this not managed as we discussed?”[59]
Reflective Questions
- As the current nurse providing patient care, explain how you would therapeutically address this family’s concerns and use one or more leadership styles.
- As the charge nurse, explain how you would address the staff involved using one or more leadership styles.
- Explain how change theory can be implemented to ensure this type of situation does not recur.

Test your knowledge using this NCLEX Next Generation-style Case Study. You may reset and resubmit your answers to this question an unlimited number of times.[60]
Change: The process of altering or replacing existing knowledge, skills, attitudes, systems, policies, or procedures.[61]
Change agent: Anyone who has the skill and power to stimulate, facilitate, and coordinate the change effort.
Change management: Process of making changes in a deliberate, planned, and systematic manner.
Core values: The foundational ideals that guide the organization's actions and decision-making processes.
Culture of safety: Organizational culture that embraces error reporting by employees with the goal of identifying systemic causes of problems that can be addressed to improve patient safety. Just Culture is a component of a culture of safety.
Followership: The upward influence of individuals on their leaders and their teams.
Just Culture: A culture where people feel safe raising questions and concerns and report safety events in an environment that emphasizes a nonpunitive response to errors and near misses. Clear lines are drawn between human error, at-risk, and reckless employee behaviors.
Leadership: The art of establishing direction and influencing and motivating others to achieve their maximum potential to accomplish tasks, objectives, or projects.[62],[63]
Management: Roles that focus on tasks such as planning, organizing, prioritizing, budgeting, staffing, coordinating, and reporting.[64]
Mission statement: An organization’s statement that describes how the organization will fulfill its vision and establishes a common course of action for future endeavors.
Organizational culture: The implicit values and beliefs that reflect the norms and traditions of an organization. An organization’s vision, mission, and values statements are the foundation of organizational culture.
Systems leadership: A set of skills used to catalyze, enable, and support the process of systems-level change that focuses on the individual, the community, and the system.
Systems theory: The concept that systems do not function in isolation but rather there is an interdependence that exists between their parts. Systems theory assumes that most individuals strive to do good work, but are affected by diverse influences within the system.
Values statement: The organization’s established values that support its vision and mission and provide strategic guidelines for decision-making, both internally and externally, by members of the organization.
Vision statement: An organization’s statement that defines why the organization exists, describes how the organization is unique and different from similar organizations, and specifies what the organization is striving to be.
Change: The process of altering or replacing existing knowledge, skills, attitudes, systems, policies, or procedures.[65]
Change agent: Anyone who has the skill and power to stimulate, facilitate, and coordinate the change effort.
Change management: Process of making changes in a deliberate, planned, and systematic manner.
Core values: The foundational ideals that guide the organization's actions and decision-making processes.
Culture of safety: Organizational culture that embraces error reporting by employees with the goal of identifying systemic causes of problems that can be addressed to improve patient safety. Just Culture is a component of a culture of safety.
Followership: The upward influence of individuals on their leaders and their teams.
Just Culture: A culture where people feel safe raising questions and concerns and report safety events in an environment that emphasizes a nonpunitive response to errors and near misses. Clear lines are drawn between human error, at-risk, and reckless employee behaviors.
Leadership: The art of establishing direction and influencing and motivating others to achieve their maximum potential to accomplish tasks, objectives, or projects.[66],[67]
Management: Roles that focus on tasks such as planning, organizing, prioritizing, budgeting, staffing, coordinating, and reporting.[68]
Mission statement: An organization’s statement that describes how the organization will fulfill its vision and establishes a common course of action for future endeavors.
Organizational culture: The implicit values and beliefs that reflect the norms and traditions of an organization. An organization’s vision, mission, and values statements are the foundation of organizational culture.
Systems leadership: A set of skills used to catalyze, enable, and support the process of systems-level change that focuses on the individual, the community, and the system.
Systems theory: The concept that systems do not function in isolation but rather there is an interdependence that exists between their parts. Systems theory assumes that most individuals strive to do good work, but are affected by diverse influences within the system.
Values statement: The organization’s established values that support its vision and mission and provide strategic guidelines for decision-making, both internally and externally, by members of the organization.
Vision statement: An organization’s statement that defines why the organization exists, describes how the organization is unique and different from similar organizations, and specifies what the organization is striving to be.
Nurses advocate for issues in their communities and their organizations.
Addressing Social Determinants of Health
Advocacy is commonly perceived as acting on behalf of a client, but it can be a much broader action than affecting a single client and their family members. Nurses advocate for building healthier communities by addressing social determinants of health (SDOH). SDOH are the conditions in the environments where people live, learn, work, and play that affect a wide range of outcomes. SDOH include health care access and quality, neighborhood and environment, social and community context, economic stability, and education access and quality. Social determinants of health (SDOH) have a major impact on people’s health, well-being, and quality of life. See Figure 10.2[69] for an illustration of SDOH.[70]

Specific examples of addressing SDOH include the following goals:
- Improving safe housing and public transportation
- Decreasing discrimination and violence
- Expanding quality education and job opportunities
- Increasing access to nutritious foods and physical activity opportunities
- Promoting clean air and clean water
- Enhancing language and literacy skills[71]
SDOH contribute to health disparities and inequities among different socioeconomic groups. For example, individuals who don't have access to grocery stores with healthy foods are less likely to have good nutrition, increasing their risk for health conditions like heart disease, diabetes, and obesity, and potentially lowering their life expectancy relative to people who do have access to healthy foods.[72]
One of Healthy People 2030’s goals specifically relates to advocacy regarding SDOH. The goal states, “Create social, physical, and economic environments that promote attaining the full potential for health and well-being for all.” Across the United States, people and organizations at the local, state, territorial, tribal, and national levels are working hard to improve health and reduce health disparities by addressing SDOH.[73] Read more information about these advocacy efforts in the following box.
Read more about efforts addressing SDOH at Healthy People 2030.


