Basic Concepts Related to Wounds
Open Resources for Nursing (Open RN)
Phases of Wound Healing
When skin is injured, there are four phases of wound healing that take place: hemostasis, inflammatory, proliferative, and maturation.[1] See Figure 20.1[2] for an illustration of the phases of wound healing.
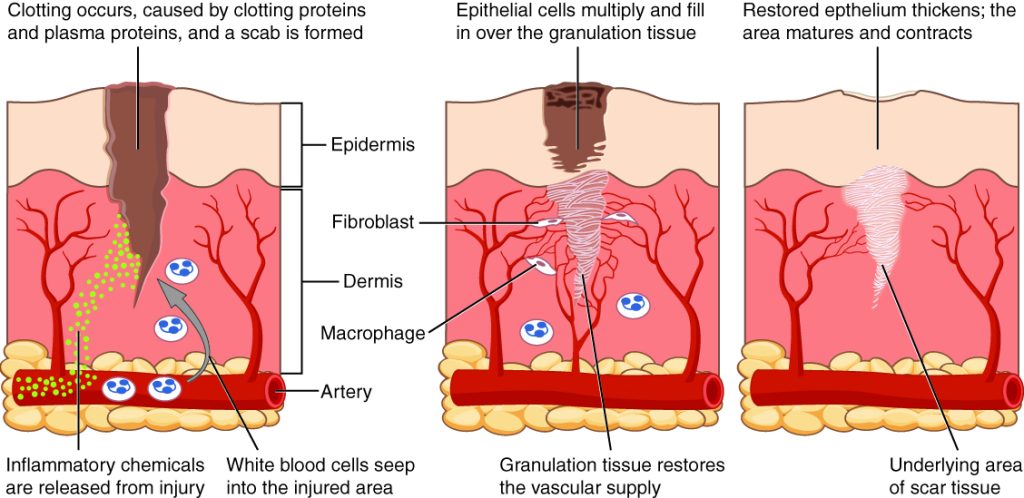
To illustrate the phases of wound healing, imagine that you accidentally cut your finger with a knife as you were slicing an apple. Immediately after the injury occurs, blood vessels constrict, and clotting factors are activated. This is referred to as the hemostasis phase. Clotting factors form clots that stop the bleeding and act as a barrier to prevent bacterial contamination. Platelets release growth factors that alert various cells to start the repair process at the wound location. The hemostasis phase lasts up to 60 minutes, depending on the severity of the injury.[3],[4]
After the hemostasis phase, the inflammatory phase begins. Vasodilation occurs so that white blood cells in the bloodstream can move into the wound to start cleaning the wound bed. The inflammatory process appears to the observer as edema (swelling), erythema (redness), and exudate. Exudate is fluid that oozes out of a wound, also commonly called pus.[5],[6]
The proliferative phase begins within a few days after the injury and includes four important processes: epithelialization, angiogenesis, collagen formation, and contraction. Epithelialization refers to the development of new epidermis and granulation tissue. Granulation tissue is new connective tissue with new, fragile, thin-walled capillaries. Collagen is formed to provide strength and integrity to the wound. At the end of the proliferation phase, the wound begins to contract in size.[7],[8]
Capillaries begin to develop within the wound 24 hours after injury during a process called angiogenesis. These capillaries bring more oxygen and nutrients to the wound for healing. When performing dressing changes, it is essential for the nurse to protect this granulation tissue and the associated new capillaries. Healthy granulation tissue appears pink due to the new capillary formation. It is also moist, painless to the touch, and may appear “bumpy.” Conversely, unhealthy granulation tissue is dark red and painful. It bleeds easily with minimal contact and may be covered by shiny white or yellow fibrous tissue referred to as biofilm that must be removed because it impedes healing. Unhealthy granulation tissue is often caused by an infection, so wound cultures should be obtained when infection is suspected. The provider can then prescribe appropriate antibiotic treatment based on the culture results.[9]
During the maturation phase, collagen continues to be created to strengthen the wound. Collagen contributes strength to the wound to prevent it from reopening. A wound typically heals within 4-5 weeks and often leaves behind a scar. The scar tissue is initially firm, red, and slightly raised from the excess collagen deposition. Over time, the scar begins to soften, flatten, and become pale in about nine months.[10]
Types of Wound Healing
There are three types of wound healing: primary intention, secondary intention, and tertiary intention. Healing by primary intention means that the wound is sutured, stapled, glued, or otherwise closed so the wound heals beneath the closure. This type of healing occurs with clean-edged lacerations or surgical incisions, and the closed edges are referred to as approximated. See Figure 20.2[11] for an image of a surgical wound healing by primary intention.

Secondary intention occurs when the edges of a wound cannot be approximated (brought together), so the wound fills in from the bottom up by the production of granulation tissue. Examples of wounds that heal by secondary intention are pressure injuries and chainsaw injuries. Wounds that heal by secondary intention are at higher risk for infection and must be protected from contamination. See Figure 20.3[12] for an image of a wound healing by secondary intention.

Tertiary intention refers to a wound that has had to remain open or has been reopened, often due to severe infection. The wound is typically closed at a later date when infection has resolved. Wounds that heal by secondary and tertiary intention have delayed healing times and increased scar tissue.
Wound Closures
Lacerations and surgical wounds are typically closed with sutures, staples, or dermabond to facilitate healing by primary intention. See Figure 20.4[13] for an image of sutures, Figure 20.5[14] for an image of staples, and Figure 20.6[15] for an image of a wound closed with dermabond, a type of sterile surgical glue. Based on agency policy, the nurse may remove sutures and staples based on a provider order. See Figure 20.7[16] for an image of a disposable staple remover. See the checklists in the subsections later in this chapter for procedures related to surgical and staple removal.




Common Types of Wounds
There are several different types of wounds. It is important to understand different types of wounds when providing wound care because each type of wound has different characteristics and treatments. Additionally, treatments that may be helpful for one type of wound can be harmful for another type. Common types of wounds include skin tears, venous ulcers, arterial ulcers, diabetic foot wounds, and pressure injuries.[17]
Skin Tears
Skin tears are wounds caused by mechanical forces such as shear, friction, or blunt force. They typically occur in the fragile, nonelastic skin of older adults or in patients undergoing long-term corticosteroid therapy. Skin tears can be caused by the simple mechanical force used to remove an adhesive bandage or from friction as the skin brushes against a surface. Skin tears occur in the epidermis and dermis but do not extend through the subcutaneous layer. The wound bases of skin tears are typically fragile and bleed easily.[18]
Venous Ulcers
Venous ulcers are caused by lack of blood return to the heart causing pooling of fluid in the veins of the lower legs. The resulting elevated hydrostatic pressure in the veins causes fluid to seep out, macerate the skin, and cause venous ulcerations. Maceration refers to the softening and wasting away of skin due to excess fluid. Venous ulcers typically occur on the medial lower leg and have irregular edges due to the maceration. There is often a dark-colored discoloration of the lower legs, due to blood pooling and leakage of iron into the skin called hemosiderin staining. For venous ulcers to heal, compression dressings must be used, along with multilayer bandage systems, to control edema and absorb large amounts of drainage.[19] See Figure 20.8[20] for an image of a venous ulcer.

Arterial Ulcers
Arterial ulcers are caused by lack of blood flow and oxygenation to tissues. They typically occur in the distal areas of the body such as the feet, heels, and toes. Arterial ulcers have well-defined borders with a “punched out” appearance where there is a localized lack of blood flow. They are typically painful due to the lack of oxygenation to the area. The wound base may become necrotic (black) due to tissue death from ischemia. Wound dressings must maintain a moist environment, and treatment must include the removal of necrotic tissue. In severe arterial ulcers, vascular surgery may be required to reestablish blood supply to the area.[21] See Figure 20.9[22] for an image of an arterial ulcer on a patient’s foot.

Diabetic Ulcers
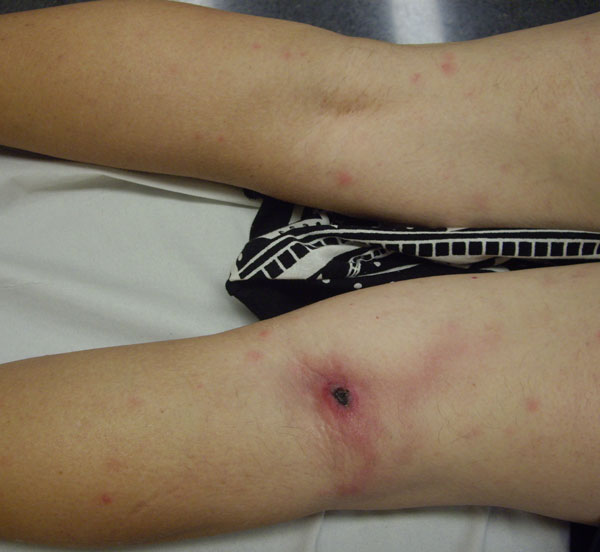
Diabetic ulcers are also called neuropathic ulcers because peripheral neuropathy is commonly present in patients with diabetes. Peripheral neuropathy is a medical condition that causes decreased sensation of pain and pressure, especially in the lower extremities. Diabetic ulcers typically develop on the plantar aspect of the feet and toes of a patient with diabetes due to lack of sensation of pressure or injury. See Figure 20.10[23] for an image of a diabetic ulcer. Wound healing is compromised in patients with diabetes due to the disease process. In addition, there is a higher risk of developing an infection that can reach the bone requiring amputation of the area. To prevent diabetic ulcers from occurring, it is vital for nurses to teach meticulous foot care to patients with diabetes and encourage the use of well-fitting shoes.[24]

Pressure Injuries
Pressure injuries are defined as “localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.”[25] Shear occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue. For example, when a patient slides down in bed, the outer skin remains immobile because it remains attached to the sheets due to friction, but deeper tissue attached to the bone moves as the patient slides down. This opposing movement of the outer layer of skin and the underlying tissues causes the capillaries to stretch and tear, which then impacts the blood flow and oxygenation of the surrounding tissues.
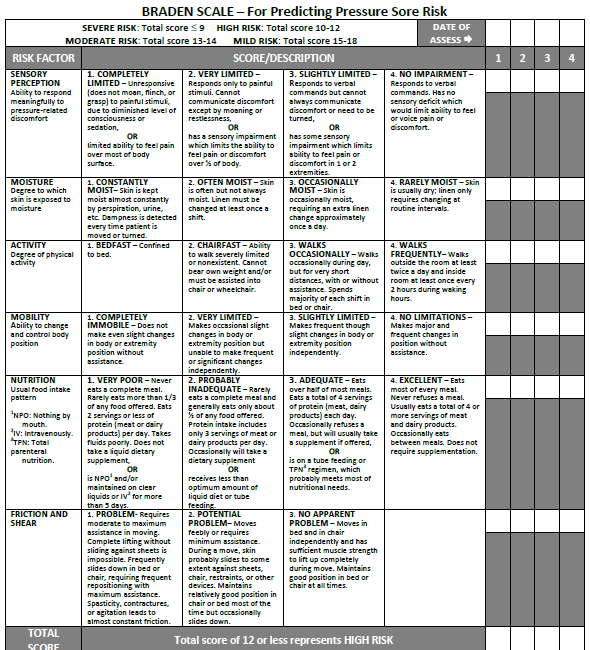
Braden Scale
Several factors place a patient at risk for developing pressure injuries, including nutrition, mobility, sensation, and moisture. The Braden Scale is a tool commonly used in health care to provide an objective assessment of a patient’s risk for developing pressure injuries. See Figure 20.11[26] for an image of a Braden Scale. The six risk factors included on the Braden Scale are sensory perception, moisture, activity, mobility, nutrition, and friction/shear, and these factors are rated on a scale from 1-4 with 1 being “completely limited” to 4 being “no impairment.” The scores from the six categories are added, and the total score indicates a patient’s risk for developing a pressure injury. A total score of 15-19 indicates mild risk, 13-14 indicates moderate risk, 10-12 indicates high risk, and less than or equal to 9 indicates severe risk. Nurses create care plans using these scores to plan interventions that prevent or treat pressure injuries.
For more information about using the Braden Scale, go to the “Integumentary” chapter of the Open RN Nursing Fundamentals textbook.
Staging
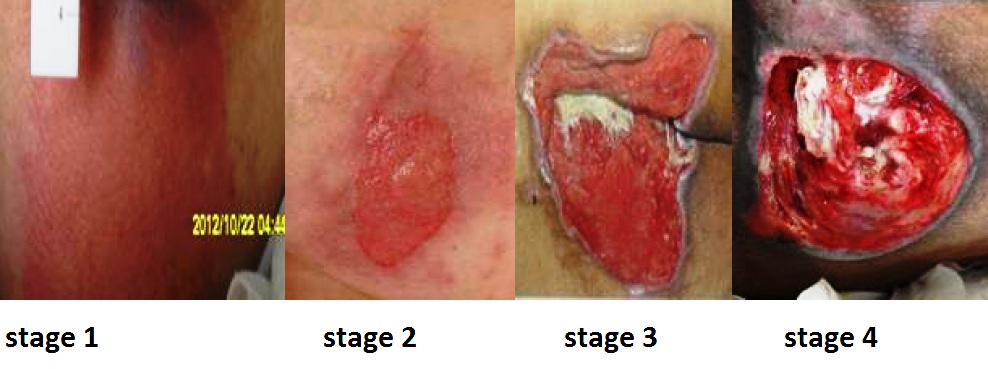
Pressure injuries commonly occur on the sacrum, heels, ischial tuberosity, and coccyx. The 2016 National Pressure Ulcer Advisory Panel (NPUAP) Pressure Injury Staging System now uses the term “pressure injury” instead of pressure ulcer because an injury can occur without an ulcer present. Pressure injuries are staged from 1 through 4 based on the extent of tissue damage. For example, Stage 1 pressure injuries have reddened but intact skin, and Stage 4 pressure injuries have deep, open ulcers affecting underlying tissue and structures such as muscles, ligaments, and tendons. See Figure 20.12[27] for an image of the four stages of pressure injuries.[28] The NPUAP’s definitions of the four stages of pressure injuries are described below:
- Stage 1 pressure injuries are intact skin with a localized area of nonblanchable erythema where prolonged pressure has occurred. Nonblanchable erythema is a medical term used to describe skin redness that does not turn white when pressed.
- Stage 2 pressure injuries are partial-thickness loss of skin with exposed dermis. The wound bed is viable and may appear like an intact or ruptured blister. Stage 2 pressure injuries heal by reepithelialization and not by granulation tissue formation.[29]
- Stage 3 pressure injuries are full-thickness tissue loss in which fat is visible, but cartilage, tendon, ligament, muscle, and bone are not exposed. The depth of tissue damage varies by anatomical location. Undermining and tunneling may occur in Stage 3 and 4 pressure injuries. Undermining occurs when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound’s edge. Tunneling refers to passageways underneath the surface of the skin that extend from a wound and can take twists and turns. Slough and eschar may also be present in Stage 3 and 4 pressure injuries. Slough is an inflammatory exudate that is usually light yellow, soft, and moist. Eschar is dark brown/black, dry, thick, and leathery dead tissue. See Figure 20.13 [30] for an image of eschar in the center of the wound. If slough or eschar obscures the wound so that tissue loss cannot be assessed, the pressure injury is referred to as unstageable.[31] In most wounds, slough and eschar must be removed by debridement for healing to occur.
- Stage 4 pressure injuries are full-thickness tissue loss like Stage 3 pressure injuries, but also have exposed cartilage, tendon, ligament, muscle, or bone. Osteomyelitis (bone infection) may be present.[32]
View a supplementary YouTube video on Pressure Injuries[33]
Factors Affecting Wound Healing
Multiple factors affect a wound’s ability to heal and are referred to as local and systemic factors. Local factors refer to factors that directly affect the wound, whereas systemic factors refer to the overall health of the patient and their ability to heal. Local factors include localized blood flow and oxygenation of the tissue, the presence of infection or a foreign body, and venous sufficiency. Venous insufficiency is a medical condition where the veins in the legs do not adequately send blood back to the heart, resulting in a pooling of fluids in the legs.[34]
Systemic factors that affect a patient’s ability to heal include nutrition, mobility, stress, diabetes, age, obesity, medications, alcohol use, and smoking.[35] When a nurse is caring for a patient with a wound that is not healing as anticipated, it is important to further assess for the potential impact of these factors:
- Nutrition. Nutritional deficiencies can have a profound impact on healing and must be addressed for chronic wounds to heal. Protein is one of the most important nutritional factors affecting wound healing. For example, in patients with pressure injuries, 30 to 35 kcal/kg of calorie intake with 1.25 to 1.5g/kg of protein and micronutrients supplementation is recommended daily.[36] In addition, vitamin C and zinc deficiency have many roles in wound healing. It is important to collaborate with a dietician to identify and manage nutritional deficiencies when a patient is experiencing poor wound healing.[37]
- Stress. Stress causes an impaired immune response that results in delayed wound healing. Although a patient cannot necessarily control the amount of stress in their life, it is possible to control one’s reaction to stress with healthy coping mechanisms. The nurse can help educate the patient about healthy coping strategies.
- Diabetes. Diabetes causes delayed wound healing due to many factors such as neuropathy, atherosclerosis (a buildup of plaque that obstructs blood flow in the arteries resulting in decreased oxygenation of tissues), a decreased host immune resistance, and increased risk for infection.[38] Read more about neuropathy and diabetic ulcers under the “Common Types of Wounds” subsection. Nurses provide vital patient education to patients with diabetes to effectively manage the disease process for improved wound healing.
- Age. Older adults have an altered inflammatory response that can impair wound healing. Nurses can educate patients about the importance of exercise for improved wound healing in older adults.[39]
- Obesity. Obese individuals frequently have wound complications, including infection, dehiscence, hematoma formation, pressure injuries, and venous injuries. Nurses can educate patients about healthy lifestyle choices to reduce obesity in patients with chronic wounds.[40]
- Medications. Medications such as corticosteroids impair wound healing due to reduced formation of granulation tissue.[41] When assessing a chronic wound that is not healing as expected, it is important to consider the side effects of the patient’s medications.
- Alcohol consumption. Research shows that exposure to alcohol impairs wound healing and increases the incidence of infection.[42] Patients with impaired healing of chronic wounds should be educated to avoid alcohol consumption.
- Smoking. Smoking impacts the inflammatory phase of the wound healing process, resulting in poor wound healing and an increased risk of infection.[43] Patients who smoke should be encouraged to stop smoking.
Lab Values Affecting Wound Healing
When a chronic wound is not healing as expected, laboratory test results may provide additional clues regarding the causes of the delayed healing. See Table 20.2 for lab results that offer clues to systemic issues causing delayed wound healing.[44]
Table 20.2 Lab Values Associated with Delayed Wound Healing[45]
| Abnormal Lab Value | Rationale |
|---|---|
| Low hemoglobin | Low hemoglobin indicates less oxygen is transported to the wound site. |
| Elevated white blood cells (WBC) | Increased WBC indicates infection is occurring. |
| Low platelets | Platelets are important during the proliferative phase in the creation of granulation tissue and angiogenesis.[46] |
| Low albumin | Low albumin indicates decreased protein levels. Protein is required for effective wound healing. |
| Elevated blood glucose or hemoglobin A1C | Elevated blood glucose and hemoglobin A1C levels indicate poor management of diabetes mellitus, a disease that impacts wound healing. |
| Elevated serum BUN and creatinine | BUN and creatinine levels are indicators of kidney function, with elevated levels indicating worsening kidney function. Elevated BUN (blood urea nitrogen) levels impact wound healing. |
| Positive wound culture | Positive wound cultures indicate an infection is present and provide additional information, including the type and number of bacteria present, as well as identifying antibiotics to which the bacteria is susceptible. The nurse reviews this information when administering antibiotics to ensure the prescribed therapy is effective for the type of bacteria present. |
Wound Complications
In addition to delayed wound healing, several other complications can occur. Three common complications are the development of a hematoma, infection, or dehiscence. These complications should be immediately reported to the health care provider.
Hematoma
A hematoma is an area of blood that collects outside of the larger blood vessels. A hematoma is more severe than ecchymosis (bruising) that occurs when small veins and capillaries under the skin break. The development of a hematoma at a surgical site can lead to infection and incisional dehiscence.[47] See Figure 20.14[48] for an image of a hematoma.

Infection
A break in the skin allows bacteria to enter and begin to multiply. Microbial contamination of wounds can progress from localized infection to systemic infection, sepsis, and subsequent life- and limb-threatening infection. Signs of a localized wound infection include redness, warmth, and tenderness around the wound. Purulent or malodorous drainage may also be present. Signs that a systemic infection is developing and requires urgent medical management include the following[49]:
- Fever over 101 F (38 C)
- Overall malaise (lack of energy and not feeling well)
- Change in level of consciousness/increased confusion
- Increasing or continual pain in the wound
- Expanding redness or swelling around the wound
- Loss of movement or function of the wounded area
Dehiscence
Dehiscence refers to the separation of the edges of a surgical wound. A dehisced wound can appear fully open where the tissue underneath is visible, or it can be partial where just a portion of the wound has torn open. Wound dehiscence is always a risk in a surgical wound, but the risk increases if the patient is obese, smokes, or has other health conditions, such as diabetes, that impact wound healing. Additionally, the location of the wound and the amount of physical activity in that area also increase the chances of wound dehiscence.[50] See Figure 20.15[51] for an image of dehiscence in an abdominal surgical wound in a 50-year-old obese female with a history of smoking and malnutrition.
Wound dehiscence can occur suddenly, especially in abdominal wounds when the patient is coughing or straining. Evisceration is a rare but severe surgical complication when dehiscence occurs, and the abdominal organs protrude out of the incision. Signs of impending dehiscence include redness around the wound margins and increasing drainage from the incision. The wound will also likely become increasingly painful. Suture breakage can be a sign that the wound has minor dehiscence or is about to dehisce.[52]
To prevent wound dehiscence, surgical patients must follow all post-op instructions carefully. The patient must move carefully and protect the skin from being pulled around the wound site. They should also avoid tensing the muscles surrounding the wound and avoid heavy lifting as advised.[53]

Media Attributions
- 417_Tissue_Repair
- Ventriculoperitoneal_shunt_-_surgical_wound_healing_-_belly_-_day_12
- Atrophied_skin
- Wound_closed_with_surgical_sutures
- Surgical_staples1
- Incision_wound_on_child’s_arm,_closed_with_Dermabond
- 24503995344_82cc1c6bcd_o
- Úlceras_antes_da_cirurgia
- Arterial_ulcer_peripheral_vascular_disease
- Diabetic_Planta_ulcer
- braden_Scale
- Wound_stage
- Inoculation_eschar_Rickettsia_sibirica_mongolitimonae_infection
- 3109068066_debefe26fd_o
- Bogota_bag
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- “417 Tissue Repair.jpg” by OpenStax College is licensed under CC BY 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Grubbs and Mannah and is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Grubbs and Mannah and is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Grubbs and Mannah and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Alhajj, Bansal, and Goyal and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Grubbs and Mannah and is licensed under CC BY 4.0 ↵
- “Ventriculoperitoneal shunt - surgical wound healing - belly - day 12.jpg” by Hansmuller is licensed under CC BY-SA 4.0 ↵
- “Atrophied skin.png” by sansea2 is licensed under CC BY-SA 3.0 ↵
- “Wound closed with surgical sutures.jpg” by Wikip2011 is licensed under CC BY-SA 3.0 ↵
- “Surgical staples1.jpg” by Llywrch is licensed under CC BY-SA 2.5 ↵
- “Incision wound on child's arm, closed with Dermabond.jpg” by ragesoss is licensed under CC BY-SA 3.0 ↵
- “Not quite scissors - TROML - 1366” by Clint Budd is licensed under CC BY 2.0 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- “Úlceras_antes_da_cirurgia.JPG” by Nini00 is licensed under CC BY-SA 3.0 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- “Arterial ulcer peripheral vascular disease.jpg” by Jonathan Moore is licensed under CC BY 3.0 ↵
- “Diabetic Planta ulcer.jpg” by Dr. Lorimer is licensed under CC BY-SA 4.0 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://journals.lww.com/jwocnonline/Fulltext/2016/11000/Revised_National_Pressure_Ulcer_Advisory_Panel.3.aspx ↵
- The Braden Scale, from Prevention Plus, is included on the basis of Fair Use. ↵
- “Wound stage.jpg” by Babagolzadeh is licensed under CC BY-SA 3.0 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- "Inoculation_eschar_Rickettsia_sibirica_mongolitimonae_infection.jpg" by José M. Ramos, Isabel Jado, Sergio Padilla, Mar Masiá, Pedro Anda, and Félix Gutiérrez is licensed under CC0 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- RegisteredNurseRN. (2018, March 7). Pressure ulcers (injuries) stages, prevention, assessment | Stage 1, 2, 3, 4 unstageable NCLEX [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/MDtPik1UE6k ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Grey, J. E., Enoch, S., & Harding, K. G. (2006). Wound assessment. BMJ (Clinical research ed.), 332(7536), 285–288. https://doi.org/10.1136/bmj.332.7536.285 ↵
- Grey, J. E., Enoch, S., & Harding, K. G. (2006). Wound assessment. BMJ (Clinical research ed.), 332(7536), 285–288. https://doi.org/10.1136/bmj.332.7536.285 ↵
- This work is a derivative of StatPearls by Grubbs and Mannah is licensed under CC BY 4.0 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/won.0000000000000281 ↵
- “Ankle swell and internal bleeding” by Glen Bowman is licensed under CC BY-SA 2.0 ↵
- WoundSource. (2016, October 19). 8 signs of wound infection. https://www.woundsource.com/blog/8-signs-wound-infection ↵
- WoundSource. (2018, March 28). Complications in chronic wound healing and associated interventions. https://www.woundsource.com/blog/complications-in-chronic-wound-healing-and-associated-interventions ↵
- “Bogota bag.png” by Suarez-Grau, J. M., Guadalajara Jurado, J. F., Gómez Menchero, J., Bellido Luque, J. A. is licensed under CC BY 4.0 ↵
- WoundSource. (2018, March 28). Complications in chronic wound healing and associated interventions. https://www.woundsource.com/blog/complications-in-chronic-wound-healing-and-associated-interventions ↵
- WoundSource. (2018, March 28). Complications in chronic wound healing and associated interventions. https://www.woundsource.com/blog/complications-in-chronic-wound-healing-and-associated-interventions ↵
Before discussing specific procedures related to facilitating bowel and bladder function, let’s review basic concepts related to urinary and bowel elimination. When facilitating alternative methods of elimination, it is important to understand the anatomy and physiology of the gastrointestinal and urinary systems, as well as the adverse effects of various conditions and medications on elimination. Use the information below to review information about these topics.
For more information about the anatomy and physiology of the gastrointestinal system and medications used to treat diarrhea and constipation, visit the "Gastrointestinal" chapter of the Open RN Nursing Pharmacology textbook.
For more information about the anatomy and physiology of the kidneys and diuretic medications used to treat fluid overload, visit the "Cardiovascular and Renal System" chapter in Open RN Nursing Pharmacology textbook.
For more information about applying the nursing process to facilitate elimination, visit the "Elimination" chapter in Open RN Nursing Fundamentals.
Urinary Elimination Devices
This section will focus on the devices used to facilitate urinary elimination. Urinary catheterization is the insertion of a catheter tube into the urethral opening and placing it in the neck of the urinary bladder to drain urine. There are several types of urinary elimination devices, such as indwelling catheters, intermittent catheters, suprapubic catheters, and external devices. Each of these types of devices is described in the following subsections.
Indwelling Catheter
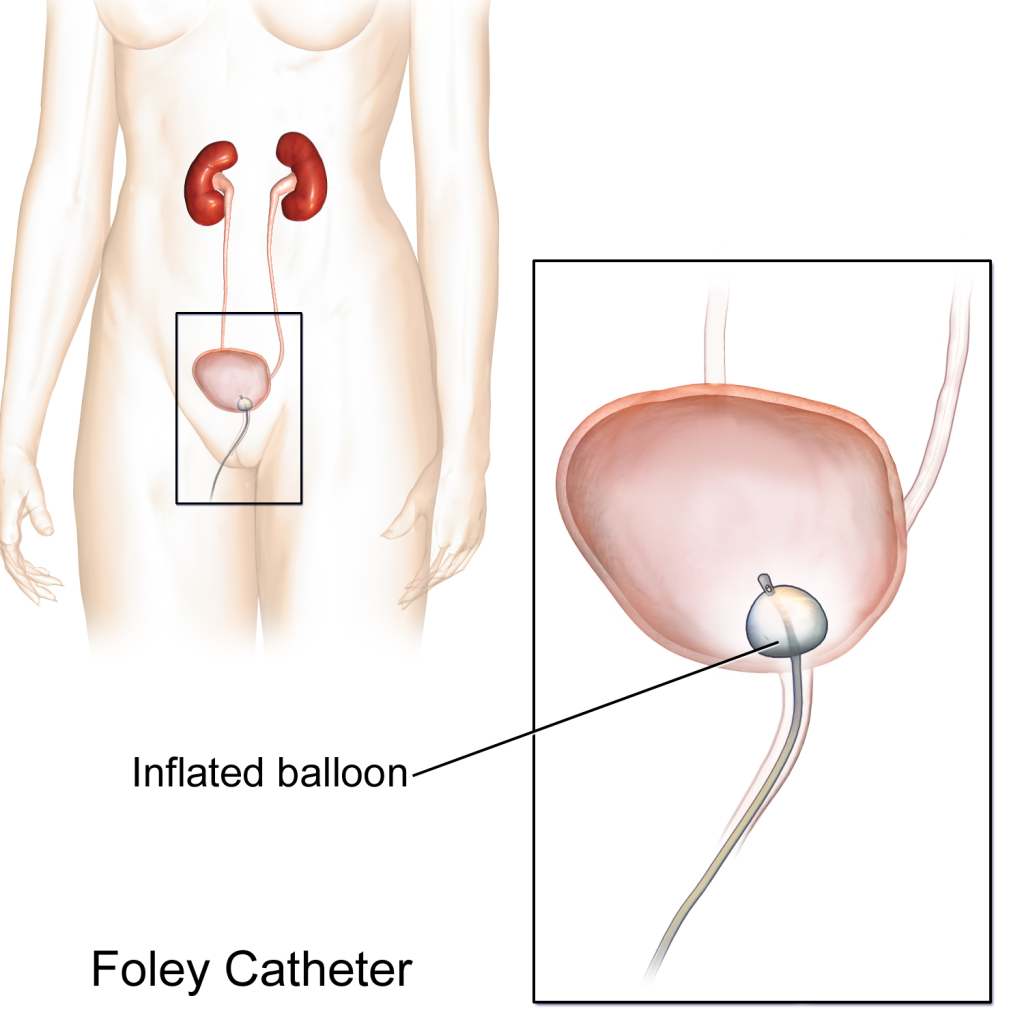
An indwelling catheter, often referred to as a “Foley catheter,” refers to a urinary catheter that remains in place after insertion into the bladder for the continual collection of urine. It has a balloon on the insertion tip to maintain placement in the neck of the bladder. The other end of the catheter is attached to a drainage bag for the collection of urine. See Figure 21.1[1] for an illustration of the anatomical placement of an indwelling catheter in the bladder neck.
The distal end of an indwelling catheter has a urine drainage port that is connected to a drainage bag. The size of the catheter is marked at this end using the French catheter scale. A balloon port is also located at this end, where a syringe is inserted to inflate the balloon after it is inserted into the bladder. The balloon port is marked with the amount of fluid required to fill the balloon. See Figure 21.2[2] for an image of the parts of an indwelling catheter.
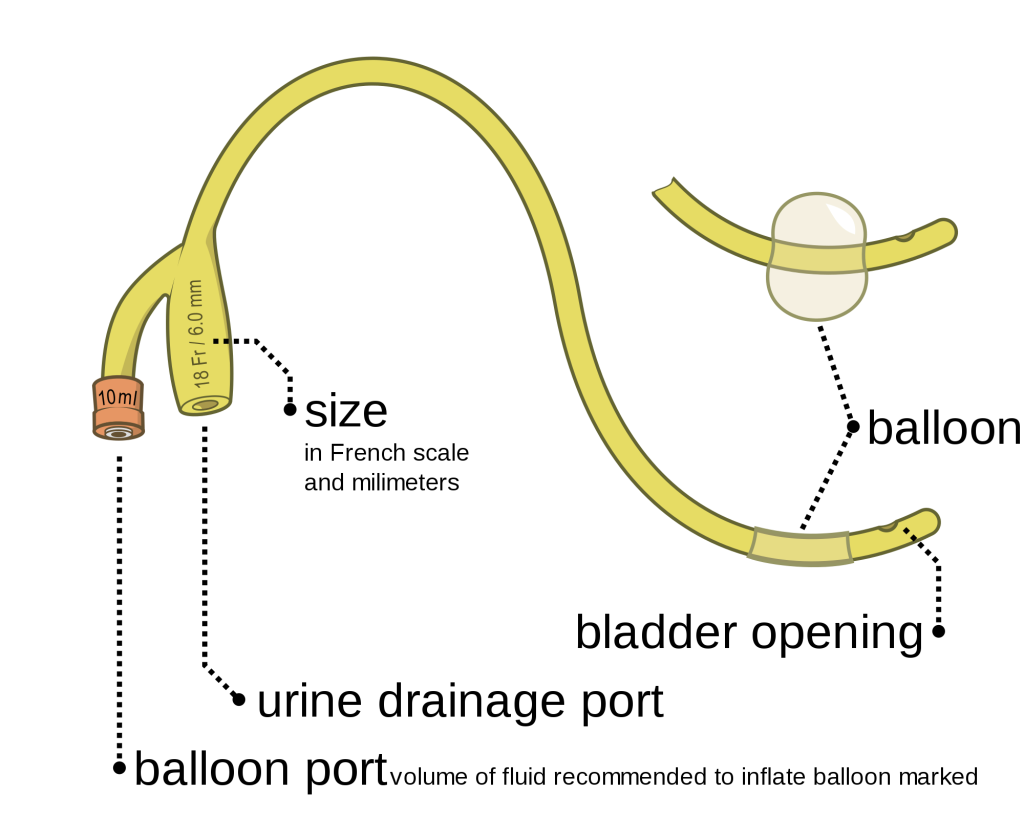
Catheters have different sizes, with the larger the number indicating a larger diameter of the catheter. See Figure 21.3[3] for an image of the French catheter scale.
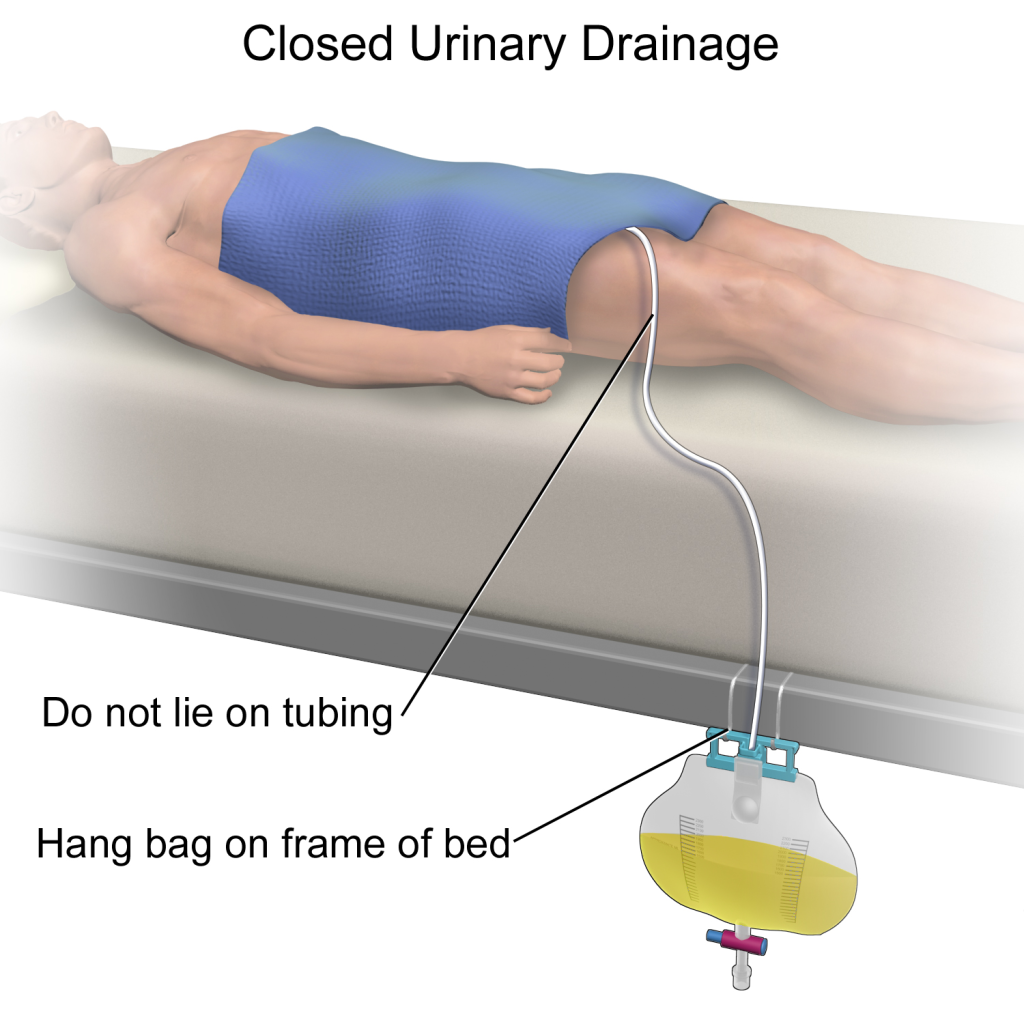
There are two common types of bags that may be attached to an indwelling catheter. During inpatient or long-term care, larger collection bags that can hold up to two liters of fluid are used. See Figure 21.4[4] for an image of a typical collection bag attached to an indwelling catheter. These bags should be emptied when they are half to two-thirds full to prevent traction on the urethra from the bag. Additionally, the collection bag should always be placed below the level of the patient’s bladder so that urine flows out of the bladder and urine does not inadvertently flow back into the bladder. Ensure the tubing is not coiled, kinked, or compressed so that urine can flow unobstructed into the bag. Slack should be maintained in the tubing to prevent injury to the patient's urethra. To prevent the development of a urinary tract infection, the bag should not be permitted to touch the floor.

See Figure 21.5[5] for an illustration of the placement of the urine collection bag when the patient is lying in bed.
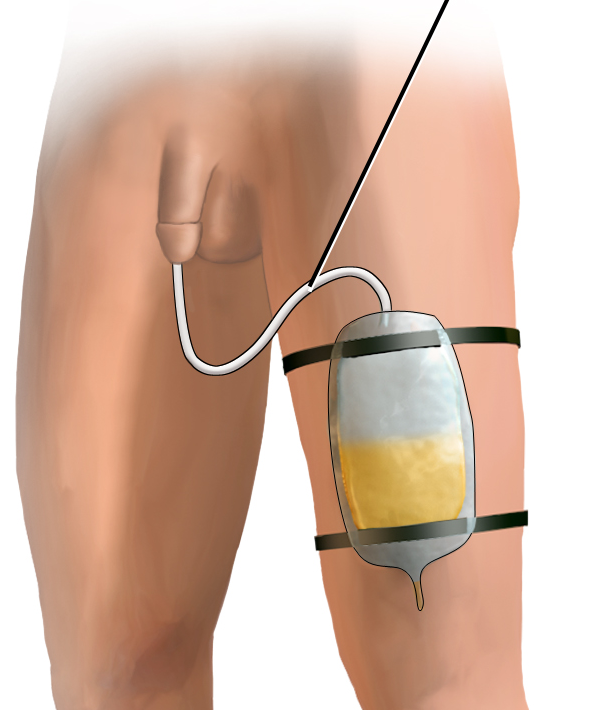
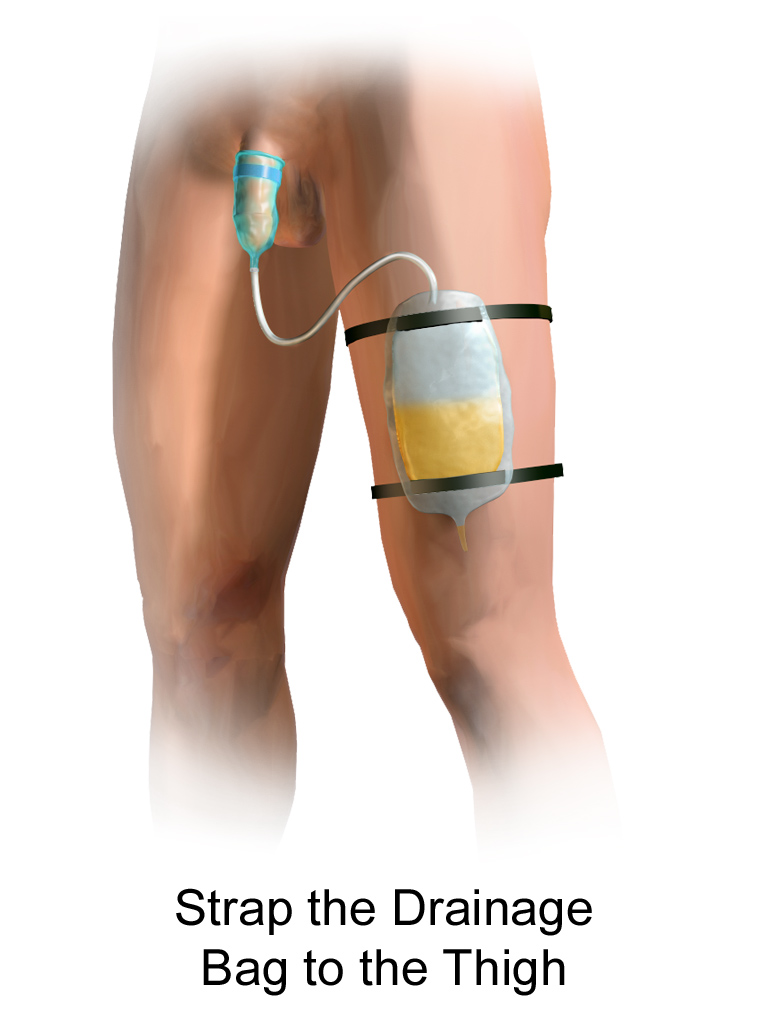
A second type of urine collection bag is a leg bag. Leg bags provide discretion when the patient is in public because they can be worn under clothing. However, leg bags are small and must be emptied more frequently than those used during inpatient care. Figure 21.6[6] for an image of leg bag and Figure 21.7[7] for an illustration of an indwelling catheter attached to a leg bag.

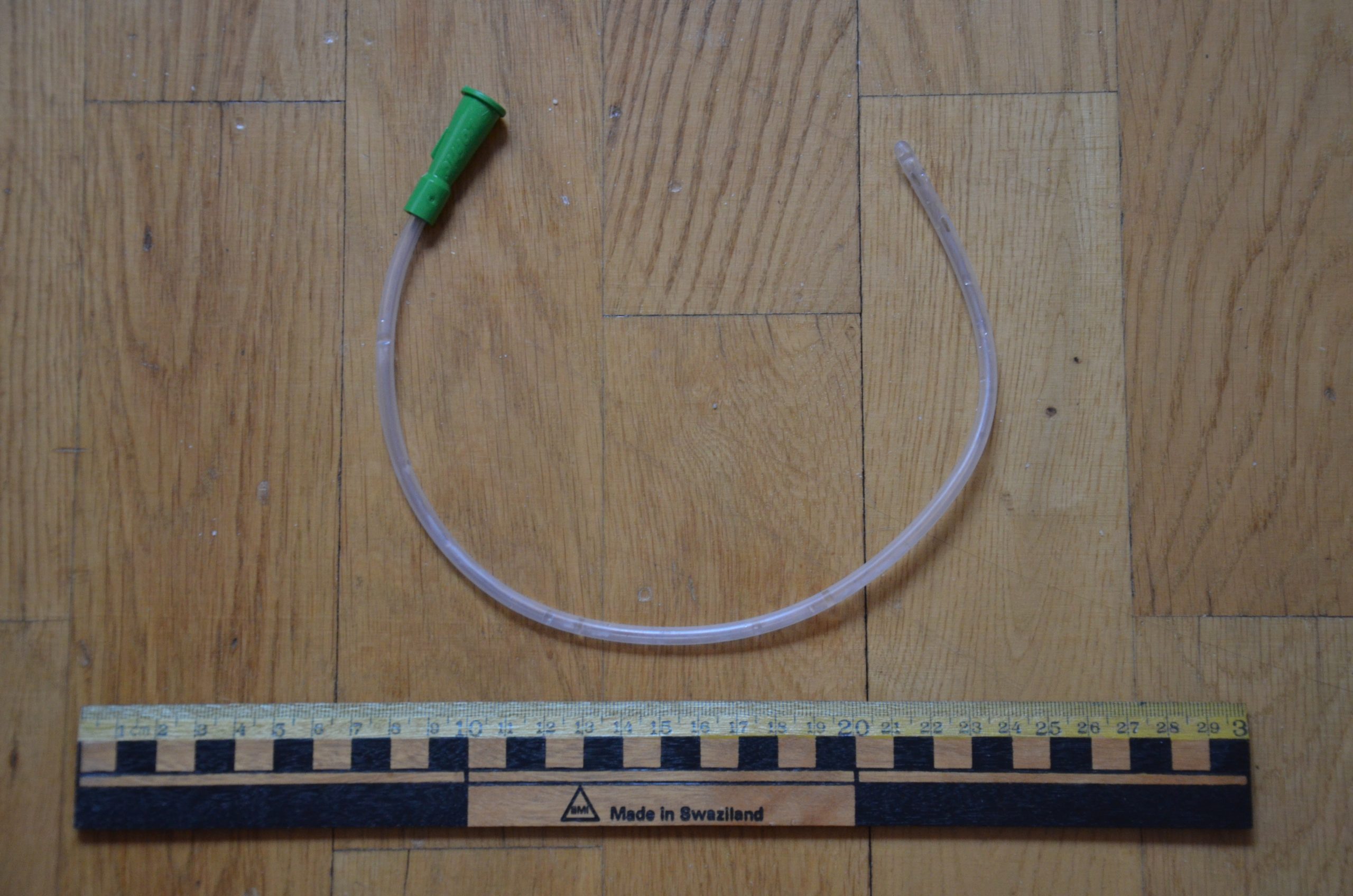
Straight Catheter
A straight catheter is used for intermittent urinary catheterization. The catheter is inserted to allow for the flow of urine and then immediately removed, so a balloon is not required at the insertion tip. See Figure 21.8[8] for an image of a straight catheter. Intermittent catheterization is used for the relief of urinary retention. It may be performed once, such as after surgery when a patient is experiencing urinary retention due to the effects of anesthesia, or performed several times a day to manage chronic urinary retention. Some patients may also independently perform self-catheterization at home to manage chronic urinary retention caused by various medical conditions. In some situations, a straight catheter is also used to obtain a sterile urine specimen for culture when a patient is unable to void into a sterile specimen cup. According to the Centers for Disease Control and Prevention (CDC), intermittent catheterization is preferred to indwelling urethral catheters whenever feasible because of decreased risk of developing a urinary tract infection.[9]
Other Types of Urinary Catheters
Coude Catheter Tip
Coude catheter tips are curved to follow the natural curve of the urethra during catheterization. They are often used when catheterizing male patients with enlarged prostate glands. See Figure 21.9[10] for an example of a urinary catheter with a coude tip. During insertion, the tip of the coude catheter must be pointed anteriorly or it can cause damage to the urethra. A thin line embedded in the catheter provides information regarding orientation during the procedure; maintain the line upwards to keep it pointed anteriorly.

Irrigation Catheter
Irrigation catheters are typically used after prostate surgery to flush the surgical area. These catheters are larger in size to allow for irrigation of the bladder to help prevent the formation of blood clots and to flush them out. See Figure 21.10[11] for an image comparing a larger 20 French catheter (typically used for irrigation) to a 14 French catheter (typically used for indwelling catheters).

Suprapubic Catheters
Suprapubic catheters are surgically inserted through the abdominal wall into the bladder. This type of catheter is typically inserted when there is a blockage within the urethra that does not allow the use of a straight or indwelling catheter. Suprapubic catheters may be used for a short period of time for acute medical conditions or may be used permanently for chronic conditions. See Figure 21.11[12] for an image of a suprapubic catheter. The insertion site of a suprapubic catheter must be cleaned regularly according to agency policy with appropriate steps to prevent skin breakdown.

Male Condom Catheter
A condom catheter is a noninvasive device used for males with incontinence. It is placed over the penis and connected to a drainage bag. This device protects and promotes healing of the skin around the perineal area and inner legs and is used as an alternative to an indwelling urinary catheter. See Figure 21.12[13] for an image of a condom catheter and Figure 21.13[14] for an illustration of a condom catheter attached to a leg bag.

Female External Urinary Catheter
Female external urinary catheters (FEUC) have been recently introduced into practice to reduce the incidence of catheter-associated urinary tract infection (CAUTI) in women.[15] The external female catheter device is made of a purewick material that is placed externally over the female’s urinary meatus. The wicking material is attached to a tube that is hooked to a low-suction device. When the wick becomes saturated with urine, it is suctioned into a drainage canister. Preliminary studies have found that utilizing the FEUC device reduced the risk for CAUTI.[16],[17]
View these supplementary YouTube videos on female external urinary catheters:
Students demonstrate use of PureWick female external catheter[18]
How to use the use the PureWick - a female external catheter[19]
Safely and accurately placing an indwelling urinary catheter poses several challenges that require the nurse to use clinical judgment. Challenges can include anatomical variations in a specific patient, medical conditions affecting patient positioning, and maintaining sterility of the procedure with confused or agitated patients. See the checklists on Foley Catheter Insertion (Male) and Foley Catheter Insertion (Female) for detailed instructions.
Nursing interventions to prevent the development of a catheter-associated urinary tract infection (CAUTI) on insertion include the following[20]:
- Determine if insertion of an indwelling catheter meets CDC guidelines.
- Select the smallest-sized catheter that is appropriate for the patient, typically a 14 French.
- Obtain assistance as needed to facilitate patient positioning, visualization, and insertion. Many agencies require two nurses for the insertion of indwelling catheters.
- Perform perineal care before inserting a urinary catheter and regularly thereafter.
- Perform hand hygiene before and after insertion, as well as during any manipulation of the device or site.
- Maintain strict aseptic technique during insertion and use sterile gloves and equipment.
- Inflate the balloon after insertion per manufacturer instructions. It is not recommended to preinflate the balloon prior to insertion.
- Properly secure the catheter after insertion to prevent tissue damage.
- Keep the drainage bag below the bladder but not resting on the floor.
- Check the system to ensure there are no kinks or obstructions to urine flow.
- Provide routine hygiene of the urinary meatus during daily bathing and cleanse the perineal area after every bowel movement. In uncircumcised males, gently retract the foreskin, cleanse the meatus, and then return the foreskin to the original position. Do not cleanse the periurethral area with antiseptics after the catheter is in place.[21] To avoid contaminating the urinary tract, always clean by wiping away from the urinary meatus.
- Empty the collection bag regularly using a separate, clean collecting container for each patient. Avoid splashing and prevent contact of the drainage spigot with the nonsterile collecting container or other surfaces. Never allow the bag to touch the floor.[22],[23]
Video Review of Thompson Rivers University's Urinary Catheterization:
Swelling in tissues caused by fluid retention.
With an understanding of the basic structures and primary functions of the respiratory system, the nurse collects subjective and objective data to perform a focused respiratory assessment.
Subjective Assessment
Collect data using interview questions, paying particular attention to what the patient is reporting. The interview should include questions regarding any current and past history of respiratory health conditions or illnesses, medications, and reported symptoms. Consider the patient’s age, gender, family history, race, culture, environmental factors, and current health practices when gathering subjective data. The information discovered during the interview process guides the physical exam and subsequent patient education. See Table 10.3a for sample interview questions to use during a focused respiratory assessment.[26]
Table 10.3a Interview Questions for Subjective Assessment of the Respiratory System
| Interview Questions | Follow-up |
|---|---|
| Have you ever been diagnosed with a respiratory condition, such as asthma, COPD, pneumonia, or allergies?
Do you use oxygen or peak flow meter? Do you use home respiratory equipment like CPAP, BiPAP, or nebulizer devices? |
Please describe the conditions and treatments. |
| Are you currently taking any medications, herbs, or supplements for respiratory concerns? | Please identify what you are taking and the purpose of each. |
| Have you had any feelings of breathlessness
(dyspnea)? |
Note: If the shortness of breath is severe or associated with chest pain, discontinue the interview and obtain emergency assistance.
Are you having any shortness of breath now? If yes, please rate the shortness of breath from 0-10 with "0" being none and "10" being severe? Does anything bring on the shortness of breath (such as activity, animals, food, or dust)? If activity causes the shortness of breath, how much exertion is required to bring on the shortness of breath? When did the shortness of breath start? Is the shortness of breath associated with chest pain or discomfort? How long does the shortness of breath last? What makes the shortness of breath go away? Is the shortness of breath related to a position, like lying down? Do you sleep in a recliner or upright in bed? Do you wake up at night feeling short of breath? How many pillows do you sleep on? How does the shortness of breath affect your daily activities? |
| Do you have a cough? | When you cough, do you bring up anything? What color is the phlegm?
Do you cough up any blood (hemoptysis)? Do you have any associated symptoms with the cough such as fever, chills, or night sweats? How long have you had the cough? Does anything bring on the cough (such as activity, dust, animals, or change in position)? What have you used to treat the cough? Has it been effective? |
| Do you smoke or vape? | What products do you smoke/vape? If cigarettes are smoked, how many packs a day do you smoke?
How long have you smoked/vaped? Have you ever tried to quit smoking/vaping? What strategies gave you the best success? Are you interested in quitting smoking/vaping? If the patient is ready to quit, the five successful interventions are the "5 A's": Ask, Advise, Assess, Assist, and Arrange. Ask - Identify and document smoking status for every patient at every visit. Advise - In a clear, strong, and personalized manner, urge every user to quit. Assess - Is the user willing to make a quitting attempt at this time? Assist - For the patient willing to make a quitting attempt, use counseling and pharmacotherapy to help them quit. Arrange - Schedule follow-up contact, in person or by telephone, preferably within the first week after the quit date.[27] |
Life Span Considerations
Depending on the age and capability of the child, subjective data may also need to be retrieved from a parent and/or legal guardian.
Pediatric
- Is your child up-to-date with recommended immunizations?
- Is your child experiencing any cold symptoms (such as runny nose, cough, or nasal congestion)?
- How is your child’s appetite? Is there any decrease or change recently in appetite or wet diapers?
- Does your child have any hospitalization history related to respiratory illness?
- Did your child have any history of frequent ear infections as an infant?
Older Adult
- Have you noticed a change in your breathing?
- Do you get short of breath with activities that you did not before?
- Can you describe your energy level? Is there any change from previous?
Objective Assessment
A focused respiratory objective assessment includes interpretation of vital signs; inspection of the patient’s breathing pattern, skin color, and respiratory status; palpation to identify abnormalities; and auscultation of lung sounds using a stethoscope. For more information regarding interpreting vital signs, see the “General Survey” chapter. The nurse must have an understanding of what is expected for the patient’s age, gender, development, race, culture, environmental factors, and current health condition to determine the meaning of the data that is being collected.
Evaluate Vital Signs
The vital signs may be taken by the nurse or delegated to unlicensed assistive personnel such as a nursing assistant or medical assistant. Evaluate the respiratory rate and pulse oximetry readings to verify the patient is stable before proceeding with the physical exam. The normal range of a respiratory rate for an adult is 12-20 breaths per minute at rest, and the normal range for oxygen saturation of the blood is 94–98% (SpO₂).[28] Bradypnea is less than 12 breaths per minute, and tachypnea is greater than 20 breaths per minute.
Inspection
Inspection during a focused respiratory assessment includes observation of level of consciousness, breathing rate, pattern and effort, skin color, chest configuration, and symmetry of expansion.
- Assess the level of consciousness. The patient should be alert and cooperative. Hypoxemia (low blood levels of oxygen) or hypercapnia (high blood levels of carbon dioxide) can cause a decreased level of consciousness, irritability, anxiousness, restlessness, or confusion.
- Obtain the respiratory rate over a full minute. The normal range for the respiratory rate of an adult is 12-20 breaths per minute.
- Observe the breathing pattern, including the rhythm, effort, and use of accessory muscles. Breathing effort should be nonlabored and in a regular rhythm. Observe the depth of respiration and note if the respiration is shallow or deep. Pursed-lip breathing, nasal flaring, audible breathing, intercostal retractions, anxiety, and use of accessory muscles are signs of respiratory difficulty. Inspiration should last half as long as expiration unless the patient is active, in which case the inspiration-expiration ratio increases to 1:1.
- Observe the pattern of expiration and patient position. Patients who experience difficulty expelling air, such as those with emphysema, may have prolonged expiration cycles. Some patients may experience difficulty with breathing specifically when lying down. This symptom is known as orthopnea. Additionally, patients who are experiencing significant breathing difficulty may experience most relief while in a “tripod” position. This can be achieved by having the patient sit at the side of the bed with legs dangling toward the floor. The patient can then rest their arms on an overbed table to allow for maximum lung expansion. This position mimics the same position you might take at the end of running a race when you lean over and place your hands on your knees to “catch your breath.”
- Observe the patient’s color in their lips, face, hands, and feet. Patients with light skin tones should be pink in color. For those with darker skin tones, assess for pallor on the palms, conjunctivae, or inner aspect of the lower lip. Cyanosis is a bluish discoloration of the skin, lips, and nail beds, which may indicate decreased perfusion and oxygenation. Pallor is the loss of color, or paleness of the skin or mucous membranes and usually the result of reduced blood flow, oxygenation, or decreased number of red blood cells.
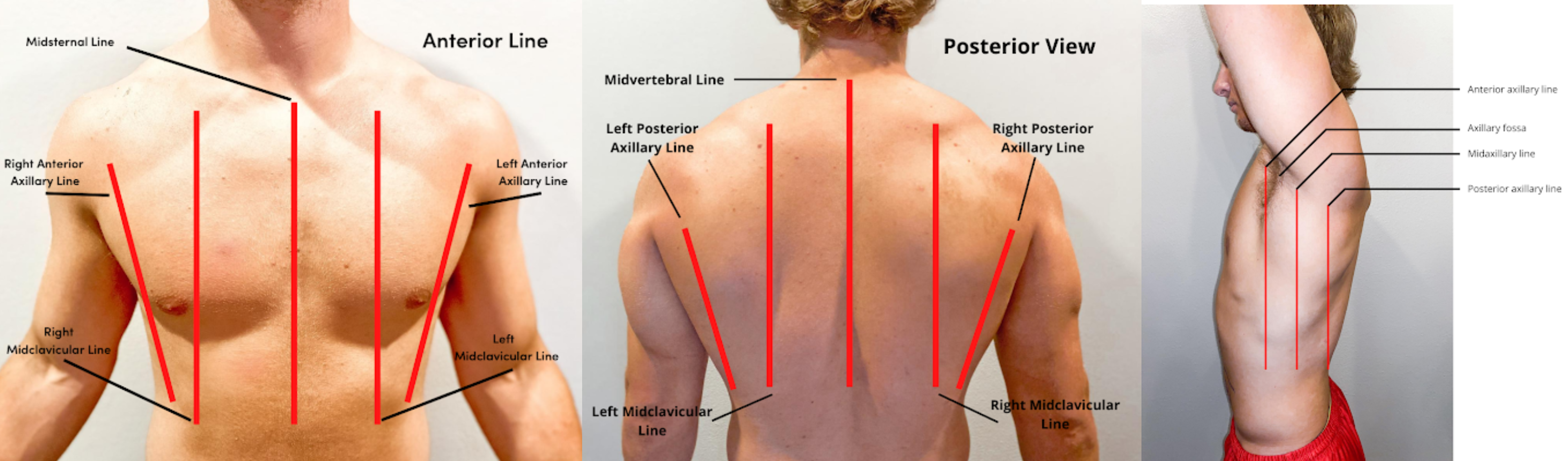
- Inspect the chest for symmetry and configuration. The trachea should be midline, and the clavicles should be symmetrical. See Figure 10.2[29] for visual landmarks when inspecting the thorax anteriorly, posteriorly, and laterally. Note the location of the ribs, sternum, clavicle, and scapula, as well as the underlying lobes of the lungs.
- Chest movement should be symmetrical on inspiration and expiration.
- Observe the anterior-posterior diameter of the patient’s chest and compare to the transverse diameter. The expected anteroposterior-transverse ratio should be 1:2. A patient with a 1:1 ratio is described as barrel-chested. This ratio is often seen in patients with chronic obstructive pulmonary disease due to hyperinflation of the lungs. See Figure 10.3[30] for an image of a patient with a barrel chest.
- Older patients may have changes in their anatomy, such as kyphosis, an outward curvature of the spine.
- Inspect the fingers for clubbing if the patient has a history of chronic respiratory disease. Clubbing is a bulbous enlargement of the tips of the fingers due to chronic hypoxia. See Figure 10.4[31] for an image of clubbing.


Palpation
- Palpation of the chest may be performed to investigate for areas of abnormality related to injury or procedural complications. For example, if a patient has a chest tube or has recently had one removed, the nurse may palpate near the tube insertion site to assess for areas of air leak or crepitus. Crepitus feels like a popping or crackling sensation when the skin is palpated and is a sign of air trapped under the subcutaneous tissues. If palpating the chest, use light pressure with the fingertips to examine the anterior and posterior chest wall. Chest palpation may be performed to assess specifically for growths, masses, crepitus, pain, or tenderness.
- Confirm symmetric chest expansion by placing your hands on the anterior or posterior chest at the same level, with thumbs over the sternum anteriorly or the spine posteriorly. As the patient inhales, your thumbs should move apart symmetrically. Unequal expansion can occur with pneumonia, thoracic trauma, such as fractured ribs, or pneumothorax.
Auscultation
Using the diaphragm of the stethoscope, listen to the movement of air through the airways during inspiration and expiration. Instruct the patient to take deep breaths through their mouth. Listen through the entire respiratory cycle because different sounds may be heard on inspiration and expiration. Allow the patient to rest between respiratory cycles, if needed, to avoid fatigue with deep breathing during auscultation. As you move across the different lung fields, the sounds produced by airflow vary depending on the area you are auscultating because the size of the airways change.
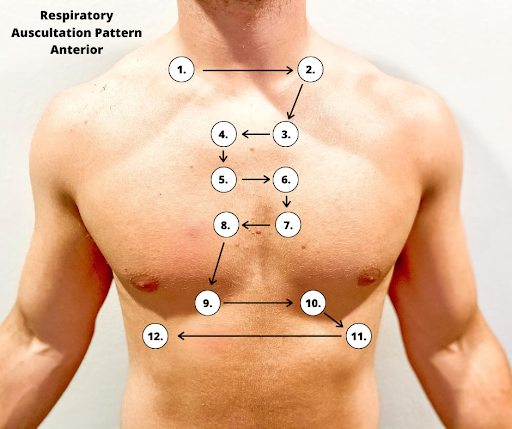
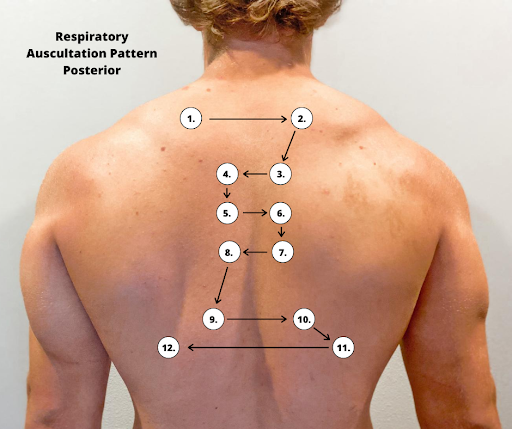
Correct placement of the stethoscope during auscultation of lung sounds is important to obtain a quality assessment. The stethoscope should not be placed over clothes or hair because these may create inaccurate sounds from friction. The best position to listen to lung sounds is with the patient sitting upright; however, if the patient is acutely ill or unable to sit upright, turn them side to side in a lying position. Avoid listening over bones, such as the scapulae or clavicles or over the female breasts to ensure you are hearing adequate sound transmission. Listen to sounds from side to side rather than down one side and then down the other side. This side-to-side pattern allows you to compare sounds in symmetrical lung fields. See Figures 10.5[32] and 10.6[33] for landmarks of stethoscope placement over the anterior and posterior chest wall.
Expected Breath Sounds
It is important upon auscultation to have awareness of expected breath sounds in various anatomical locations.
- Bronchial breath sounds are heard over the trachea and larynx and are high-pitched and loud.
- Bronchovesicular sounds are medium-pitched and heard over the major bronchi.
- Vesicular breath sounds are heard over the lung surfaces, are lower-pitched, and often described as soft, rustling sounds.
Adventitious Lung Sounds
Adventitious lung sounds are sounds heard in addition to normal breath sounds. They most often indicate an airway problem or disease, such as accumulation of mucus or fluids in the airways, obstruction, inflammation, or infection. These sounds include rales/crackles, rhonchi/wheezes, stridor, and pleural rub:
- Coarse crackles, also called rhonchi, are low-pitched, loud, continuous sounds frequently heard on expiration. They are a sign of turbulent airflow through secretions in the large airways.
Rhonchi Lung Sounds on YouTube [34]
- Fine crackles, also called rales, are popping or crackling sounds heard on inspiration. They occur in association with conditions that cause fluid to accumulate within the alveolar and interstitial spaces, such as heart failure or pneumonia. Fine crackles are soft, high-pitched, and very brief. For this reason, it is essential to listen to lung sounds with the stethoscope placed on the patient's skin and not over their clothing or hospital gown. The sound is similar to that produced by rubbing strands of hair together close to your ear.
- Wheezes are whistling-type noises produced during expiration (and sometimes inspiration) when air is forced through airways narrowed by bronchoconstriction or associated mucosal edema. For example, patients with asthma commonly have wheezing.
- Stridor is heard only on inspiration. It is associated with mechanical obstruction at the level of the trachea/upper airway.
- Pleural rub may be heard on either inspiration or expiration and sounds like the rubbing together of leather. A pleural rub is heard when there is inflammation of the lung pleura, resulting in friction as the surfaces rub against each other.[35]
Life Span Considerations
Children
There are various respiratory assessment considerations that should be noted with assessment of children.
- The respiratory rate in children less than 12 months of age can range from 30-60 breaths per minute, depending on whether the infant is asleep or active.
- Infants have irregular or periodic newborn breathing in the first few weeks of life; therefore, it is important to count the respirations for a full minute. During this time, you may notice periods of apnea lasting up to 10 seconds. This is not abnormal unless the infant is showing other signs of distress. Signs of respiratory distress in infants and children include nasal flaring and sternal or intercostal retractions.
- Up to three months of age, infants are considered “obligate” nose-breathers, meaning their breathing is primarily through the nose.
- The anteroposterior-transverse ratio is typically 1:1 until the thoracic muscles are fully developed around six years of age.
Older Adults
As the adult person ages, the cartilage and muscle support of the thorax becomes weakened and less flexible, resulting in a decrease in chest expansion. Older adults may also have weakened respiratory muscles, and breathing may become shallower. The anteroposterior-transverse ratio may be 1:1 if there is significant curvature of the spine (kyphosis).
Percussion
Percussion is an advanced respiratory assessment technique that is used by advanced practice nurses and other health care providers to gather additional data in the underlying lung tissue. By striking the fingers of one hand over the fingers of the other hand, a sound is produced over the lung fields that helps determine if fluid is present. Dull sounds are heard with high-density areas, such as pneumonia or atelectasis, whereas clear, low-pitched, hollow sounds are heard in normal lung tissue.
![]()
- Because infants breathe primarily through the nose, nasal congestion can limit the amount of air getting into the lungs.
- Attempt to assess an infant’s respiratory rate while the infant is at rest and content rather than when the infant is crying. Counting respirations by observing abdominal breathing movements may be easier for the novice nurse than counting breath sounds, as it can be difficult to differentiate lung and heart sounds when auscultating newborns.
- Auscultation of lungs during crying is not a problem. It will enhance breath sounds.
- The older patient may have a weakening of muscles that support respiration and breathing. Therefore, the patient may report tiring easily during the assessment when taking deep breaths. Break up the assessment by listening to the anterior lung sounds and then the heart sounds and allowing the patient to rest before listening to the posterior lung sounds.
- Patients with end-stage COPD may have diminished lung sounds due to decreased air movement. This abnormal assessment finding may be the patient’s baseline or normal and might also include wheezes and fine crackles as a result of chronic excess secretions and/or bronchoconstriction.[36],[37]
Expected Versus Unexpected Findings
See Table 10.3b for a comparison of expected versus unexpected findings when assessing the respiratory system.[38]
Table 10.3b Expected Versus Unexpected Respiratory Assessment Findings
| Assessment | Expected Findings | Unexpected Findings (Document and notify provider if a new finding*) |
|---|---|---|
| Inspection | Work of breathing effortless
Regular breathing pattern Respiratory rate within normal range for age Chest expansion symmetrical Absence of cyanosis or pallor Absence of accessory muscle use, retractions, and/or nasal flaring Anteroposterior: transverse diameter ratio 1:2 |
Labored breathing
Irregular rhythm Increased or decreased respiratory rate Accessory muscle use, pursed-lip breathing, nasal flaring (infants), and/or retractions Presence of cyanosis or pallor Asymmetrical chest expansion Clubbing of fingernails |
| Palpation | No pain or tenderness with palpation. Skin warm and dry; no crepitus or masses | Pain or tenderness with palpation, crepitus, palpable masses, or lumps |
| Percussion | Clear, low-pitched, hollow sound in normal lung tissue | Dull sounds heard with high-density areas, such as pneumonia or atelectasis |
| Auscultation | Bronchovesicular and vesicular sounds heard over appropriate areas
Absence of adventitious lung sounds |
Diminished lung sounds
Adventitious lung sounds, such as fine crackles/rales, wheezing, stridor, or pleural rub |
| *CRITICAL CONDITIONS to report immediately | Decreased oxygen saturation <92%[39]
Pain Worsening dyspnea Decreased level of consciousness, restlessness, anxiousness, and/or irritability |
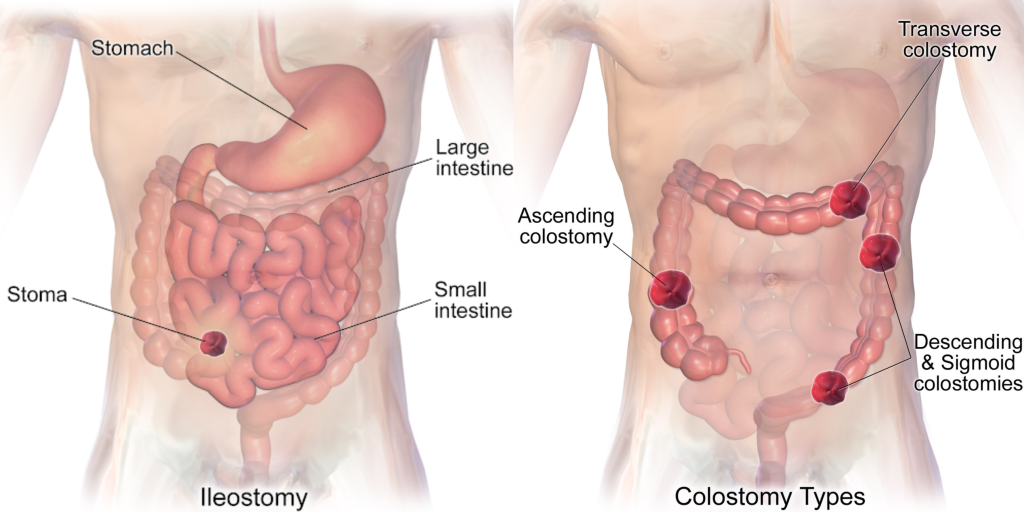
An ostomy is the surgical procedure that creates an opening (stoma) from an area inside the body to the outside of the body. In ostomies related to elimination, a stoma is an opening on the abdomen that is connected to the gastrointestinal or urinary system to allow waste (i.e., urine or feces) to be collected in a pouch. See Figure 21.14[40] for an image of a stoma. A stoma can be permanent, such as when an organ is removed, or temporary, such as when an organ requires time to heal. Ostomies are created for patients with conditions such as cancer of the bowel or bladder, inflammatory bowel diseases, or perforation of the colon.

There are several different kinds of ostomies related to elimination. Common types of ostomies include the following:
- Ileostomy: The lower end of the small intestine (ileum) is attached to a stoma to bypass the colon, rectum, and anus.
- Colostomy: The colon is attached to a stoma to bypass the rectum and the anus.
- Urostomy: The ureters (tubes that carry urine from the kidney to the bladder) are attached to a stoma to bypass the bladder.[41]
See Figure 21.15[42] comparing the anatomical locations of ileostomies and various sites of colostomies. It is important for the nurse to understand the site of a patient’s colostomy because the site impacts the characteristics of the waste. For example, due to the natural digestive process of the colon and absorption of water, waste from an ileostomy or a colostomy placed in the anterior ascending colon will be watery compared to waste from an ostomy placed in the descending colon.
The tissue of a stoma is very delicate. Immediately after surgery, a stoma is swollen, but it will shrink in size over several weeks. A healthy, healed stoma appears moist and dark red or pink in color. Stomas that are swollen; dry; have malodorous discharge; or are bluish, purple, black, or pale should be reported to the provider. The skin surrounding a stoma can easily become irritated from the pouch adhesive or leakage of fluid from the stoma, so the nurse must perform interventions to prevent skin breakdown. Any identified signs of skin breakdown should be reported to the provider.[43]
Stoma appliances are supplied as a one- or two-piece set. A two-piece set consists of an ostomy barrier (also called a wafer) and a pouch. The ostomy barrier is the part of the appliance that sticks to the skin with a hole that is fitted around the stoma. The pouch collects the waste and must be emptied regularly. It attaches to the ostomy barrier in a clicking motion to secure the two parts, similar to how a plastic storage container cover snaps to a container to create a seal. The pouching system must be completely sealed to prevent leaking of the waste and to protect the surrounding peristomal skin. The pouch has an end with an opening where the waste is drained and is closed using a plastic clip or VelcroTM strip.[44] In a one-piece stoma appliance set, the ostomy barrier and the pouch are one piece. See Figure 21.16[45] for an image of a stoma with an ostomy barrier in place. See Figure 21.17[46] for an image of a patient with an ileostomy appliance with a pouch attached.
Individuals with colostomies, ileostomies, and urostomies have no sensation and no control over the output of the stoma. Depending on the type of system, the ostomy appliance can last from four to seven days, but the pouch must be changed if there is leaking, odor, excessive skin exposure, or itching or burning under the skin barrier. Patients with pouches can swim and take showers with the pouching system on.[47]


When changing an ostomy appliance, the ostomy barrier is cut to fit closely around the stoma without impinging on it. See the "Checklist for Ostomy Appliance Change" for detailed instructions. The nurse measures the stoma with a template and then cuts and fits the ostomy barrier to a size that is 2 mm larger than the stoma.[48] See Figure 21.18[49] for an image of a nurse measuring and cutting the ostomy barrier to fit around a stoma.
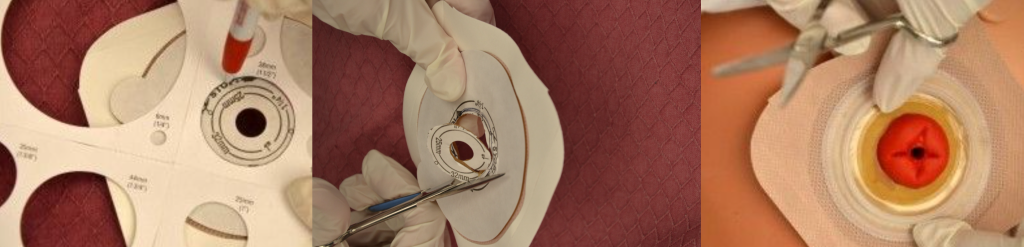
After the skin barrier is applied to the skin, the pouch is snapped to the barrier. See Figure 21.19[50] for an image of applying the pouch.

Physical and Emotional Assessment
Patients may have other medical conditions that affect their ability to manage their ostomy care. Conditions such as arthritis, vision changes, Parkinson’s disease, or post-stroke complications can hinder a patient’s coordination and ability to manage the ostomy. In addition, the emotional burden of coping with an ostomy may be devastating for some patients and may affect their self-esteem, body image, quality of life, and ability to be intimate. It is common for patients with ostomies to struggle with body image and their altered pattern of elimination. Nurses can promote healthy coping by ensuring the patient has appropriate referrals to a wound/ostomy nurse specialist, a social worker, and support groups. Nurses should also be aware of their nonverbal cues when assisting a patient with their appliance changes. It is vital not to show signs of disgust at the appearance of the ostomy or at the odor that may be present when changing an appliance or pouching system.[51]
View a supplementary YouTube video on Changing an Ostomy Pouch[52]
Urostomy Care
A urostomy is similar to a colostomy, but it is an artificial opening for passing urine. Urostomies are surgically created due to medical conditions such as bladder cancer, removal of the bladder, trauma, spinal cord injuries, or congenital abnormalities.
A urostomy patient has no voluntary control of urine, so the pouching system must be emptied regularly. Many patients empty their urostomy bag every two to four hours or when the pouch becomes one-third full. The pouch may also be attached to a drainage bag for overnight drainage. Patients with a urostomy are at risk for urinary tract infections (UTIs), so it is important to educate them regarding the signs and symptoms of an infection.
If a small amount of a fresh urine is needed for specimen collection for urinalysis or culture, aspirate the urine from the needleless sampling port with a sterile syringe after cleansing the port with a disinfectant.[53] See the "Checklist for Obtaining a Urine Specimen from a Foley Catheter" for more detailed instructions. Do not collect the urine that is already in the collection bag because it is contaminated and will lead to an erroneous test result.
It is the nurse’s responsibility to assess for a patient’s continued need for an indwelling catheter daily and to advocate for removal when appropriate.[54] Prolonged use of indwelling catheters increases the risk of developing CAUTIs. For patients who require an indwelling catheter for operative purposes, the catheter is typically removed within 24 hours or less. Some agencies have a protocol for the removal of indwelling catheters, whereas others require a prescription from a provider. For additional instructions about how to remove an indwelling catheter, see the "Checklist for Foley Removal."
When removing an indwelling urinary catheter, it is considered a standard of practice to document the time and track the time of the first void. This information is also communicated during handoff reports. If the patient is unable to void within 4-6 hours and/or complains of bladder fullness, the nurse determines if incomplete bladder emptying is occurring according to agency policy. The ANA has made the following recommendations to assess for incomplete bladder emptying:
- The patient should be prompted to urinate.
- If urination volume is less than 180 mL, the nurse should perform a bladder scan to determine the post-void residual. A bladder scan is a bedside test performed by nurses that uses ultrasonic waves to determine the amount of fluid in the bladder.
- If a bladder scanner is not available, a straight urinary catheterization is performed.[55]
When a urinary catheter is removed, instruct the patient on the following guidelines:
- Increase or maintain fluid intake (unless contraindicated).
- Void when able with the goal to urinate within six hours after removal of the catheter. Inform the nurse of the void so that the amount can be measured and documented.
- Be aware that there may be a mild burning sensation during the first void.
- Report any burning, discomfort, frequency, or small amounts of urine when voiding.
- Report an inability to void, bladder tenderness, or distension.
When preparing to insert an indwelling urinary catheter, it is important to use the nursing process to plan and provide care to the patient. Begin by assessing the appropriateness of inserting an indwelling catheter according to CDC criteria as discussed in the “Preventing CAUTI” section of this chapter. Determine if alternative measures can be used to facilitate elimination and address any concerns with the prescribing provider before proceeding with the provider order.
Subjective Assessment
In addition to verifying the appropriateness of the insertion of an indwelling catheter according to CDC recommendations, it is also important to assess for any conditions that may interfere with the insertion of a urinary catheter when feasible. See suggested interview questions prior to inserting an indwelling catheter and their rationale in Table 21.8a.
Table 21.8a Suggested Interview Questions Prior to Urinary Catheterization
| Interview Questions | Rationale |
|---|---|
| Do you have any history of urinary problems such as frequent urinary tract infections, urinary tract surgeries, or bladder cancer?
For males: Do you have any history of prostate enlargement or prostate problems? For females: Have you had any gynecological surgeries? |
Previous medical conditions and surgeries may interfere with urinary catheter placement. Information about a male patient’s prostate will assist in determining the size and type of catheter used. (Recall that using a catheter with a coude tip is helpful when a male patient has an enlarged prostate.) If a patient has a history of previous urinary tract infections, they may be at higher risk of developing CAUTI. |
| Have you ever had a urinary catheter placed in the past? If so, were there any problems with placement or did you experience any problems while the catheter was in place? | Questioning the patient about placement and prior catheterizations assists the nurse in identifying any problems with catheterization or if the patient has had the procedure before, they may know what to expect. |
| Do you have any questions about this procedure? How do you feel about undergoing catheterization? | The nurse should encourage patient involvement with their care and identify any fears or anxiety. Nurses can decrease or eliminate these fears and anxieties with additional information or reassurance. |
| Do you take any medications that increase urination such as diuretics or any medications that decrease urgency or frequency? If so, please describe. | Identifying medications that increase or decrease urine output is important to consider when monitoring urine output after the catheter is in place. |
| Have you had any orthopedic surgeries that may affect your ability to bend your knees or hips? Are you able to tolerate lying flat for a short period of time? | The patient may not be able to tolerate the positioning required for catheter insertion. If so, additional assistance from other staff may be required for patient comfort and safety. |
Cultural Considerations
When inserting urinary catheters, be aware of and respect cultural beliefs related to privacy, family involvement, and the request for a same-gender nurse. Inserting a urinary catheter requires visualization and manipulation of anatomical areas that are considered private by most patients. These procedures can cause emotional distress, especially if the patient has experienced any history of abuse or trauma.
Objective Assessment
In addition to performing a subjective assessment, there are several objective assessments to complete prior to insertion. See Table 21.8b for a list of objective assessments and their rationale.
Table 21.8b Objective Assessment
| Objective Data Collection | Rationale |
|---|---|
| Review the patient’s medical record for any documented medical conditions the patient may not have reported, such as urethral strictures, structural problems with the bladder or urethra, or frequent urinary tract infections. | Any type of obstruction or scar tissue within these areas may prevent the catheter from advancing into the bladder. |
| Analyze the patient's weight and most recent electrolyte values. | Weight is used to determine a patient's fluid status, especially if they have fluid overload. Electrolyte levels are also affected by fluid balance and the use of diuretic medications. Establish a baseline to use to evaluate outcomes after placing the urinary catheter. |
| Determine the patient's level of consciousness, ability to cooperate, developmental level, and age. | Evaluate the patient’s ability to follow directions and cooperate during the procedure and seek additional assistance during the procedure if needed. This data will impact how to explain the procedure to the patient. |
| Perform physical assessment of the bladder and perineum. Palpate the bladder for signs of fullness and discomfort. (Bladder emptying may also be assessed using a bladder scanner per agency policy). Inspect the perineum for erythema, discharge, drainage, skin ulcerations, or odor. Note the position of anatomical landmarks. For example, in females identify the urethra versus the vaginal opening. | A full bladder produces discomfort and urgency to void, especially on palpation. These symptoms should be relieved with the placement of a urinary catheter.
Identify any abnormal physical signs in the perineal area that may interfere with comfort during insertion. Determining the urethral opening improves accuracy and ease of insertion. |
| When examining the perineal area, note the approximate diameter of the urinary meatus. Choose the smallest, appropriately sized diameter catheter. | An appropriately sized catheter is important to avoid unnecessary discomfort or trauma to the urinary tissue. Catheters that are 14 French diameter are typically used in adults. |
Life Span Considerations
Children
It is often helpful to explain the catheterization procedure using a doll or toy. According to agency policy, a parent, caregiver, or other adult should be present in the room during the procedure. Asking a younger child to blow into a straw can help relax the pelvic muscles during catheterization.
Older Adults
The urethral meatus of older women may be difficult to identify due to atrophy of the urogenital tissue. The risk of developing a urinary tract infection may also be increased due to chronic disease and incontinence.
Expected Outcomes/Planning
Expected patient outcomes following urinary catheterization should be planned and then evaluated and documented after the procedure is completed. See Table 21.8c for sample expected outcomes related to urinary catheterization.
Table 21.8c Expected Outcomes of Urinary Catheterization
| Expected Outcomes | Rationale |
|---|---|
| The patient’s bladder is nondistended and not palpable. | Verifies appropriate bladder emptying. |
| The patient reports no abdominal or bladder discomfort or pressure. | Verifies correct catheter placement by allowing urine flow and relieving discomfort or pressure. |
| Urine output is at least 30 mL/hr. | Verifies correct catheter placement and appropriate kidney functioning. If urine output is less than 30 mL/hour, check tubing for kinking and obstruction, and notify the provider if there is no improvement after manipulating the tubing. |
| Patient verbalizes understanding of the purpose of the catheter and signs of a urinary tract infection to report. | Verifies the patient's understanding of the procedure and signs of complications. |
Implementation
When inserting an indwelling urinary catheter, the expected finding is that the catheter is inserted accurately and without discomfort, and immediate flow of clear, yellow urine into the collection bag occurs. However, unexpected events and findings can occur. See Table 21.8d for examples of unexpected findings and suggested follow-up actions.
Table 21.8d Unexpected Findings and Follow-Up Actions
| Unexpected Findings | Follow-Up Action |
|---|---|
| Urine flow does not occur when catheterizing a female patient. | The catheter may have entered the vagina and not the urethral meatus. Leave the catheter in the vagina as a landmark to avoid incorrect reinsertion. Obtain a new catheter kit and cleanse the urinary meatus again before reinsertion. If reinsertion is successful into the bladder, remove the catheter that is in vagina after the second attempt. |
| Sterile field is broken during the procedure. | If supplies or the catheter become contaminated, obtain a new catheter kit and restart the procedure. |
| Patient reports continued bladder pain or discomfort although urinary flow indicates correct catheter placement. | Ensure there is no tension pulling at the catheter. It may be helpful to deflate the balloon and advance the catheter another 2-3 inches to ensure it is in the bladder and not the urethra. If these actions do not resolve the discomfort, notify the provider because it is possible the patient is experiencing bladder spasms. Continue to monitor urine output for clarity, color, and amount and for signs of urinary tract infection. |
| The nurse is unable to advance the catheter on a male patient with an enlarged prostate. | Do not force advancement because this may cause further damage. Ask the patient to take deep breaths and try again. If a second attempt is unsuccessful, obtain a coude catheter and attempt to reinsert. If unsuccessful with a coude catheter, notify the provider. |
| Urine is cloudy, concentrated, malodorous, dark amber in color, or contains sediment, blood, or pus. | Notify the health care provider of signs and symptoms of a possible urinary tract infection. Obtain a urine specimen as prescribed. |
Evaluation
Evaluate the success of the expected outcomes established prior to the procedure.
Sample Documentation for Expected Findings
A size 14F Foley catheter inserted per provider prescription. Indication: Prolonged urinary retention. Procedure and purpose of Foley catheter explained to patient. Patient denies allergies to iodine, orthopedic limitations, or previous genitourinary surgeries. Balloon inflated with 10 mL of sterile water. Patient verbalized no discomfort or pain with balloon inflation or during the procedure. Peri-care provided before and after procedure. Catheter tubing secured to right upper thigh with stat lock. Drainage bag attached, tubing coiled loosely with no kinks, bag is below bladder level on bed frame. Urine drained with procedure 375 mL. Urine is clear, amber in color, no sediment. Patient resting comfortably; instructed the patient to notify the nurse if develops any bladder pain, discomfort, or spasms. Patient verbalized understanding.
Sample Documentation for Unexpected Findings
A size 14F Foley catheter inserted per provider prescription. Indication is for oliguria with accurate output measurements required. Procedure and purpose of Foley catheter explained to patient. Patient denies allergies to iodine, orthopedic limitations, or previous genitourinary surgeries. As the balloon was being inflated with sterile water, patient began to report discomfort. Water removed, catheter advanced one inch and balloon reinflated with 10 mL of sterile water. Patient denied discomfort after the catheter advancement. Catheter tubing secured to right upper thigh with stat lock. Drainage bag attached, tubing coiled loosely with no kinks, bag is below bladder level. Urine drained with procedure 100 mL. Urine is dark amber, noticeable sediment in tubing, with foul odor. Patient resting comfortably, denies any bladder pain or discomfort. Instructed the patient to notify the nurse if develops any bladder pain, discomfort, or urinary spasms. Patient verbalized understanding. Notify the health care provider of urine assessment. Continue monitoring patient for any new or worsening symptoms such as change in mental status, fever, chills, or hematuria.
Use the checklist below to review the steps for completion of “Foley Catheter Insertion (Male).”
See Figure 21.20[56] for an image of a Foley catheter kit.
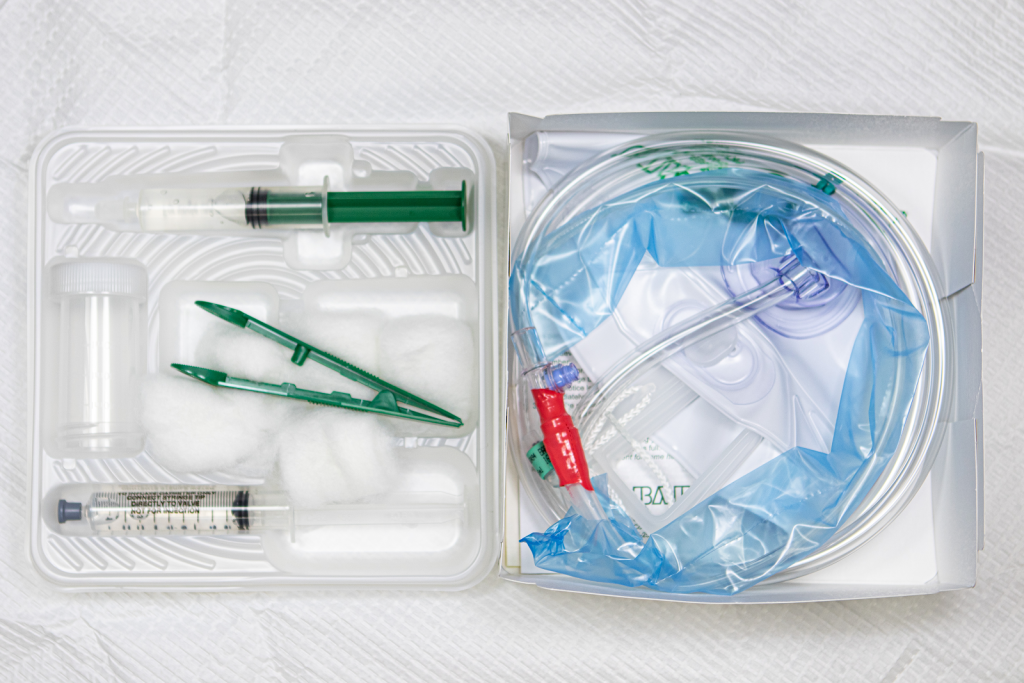
View an instructor demonstration of Male Foley Catheter Insertion[57]:
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Gather supplies: peri-care supplies, clean nonsterile gloves, Foley catheter kit, extra pair of sterile gloves, VelcroTM catheter securement device to secure Foley catheter to leg, wastebasket, and light source (i.e., goose neck lamp or flashlight).
- Perform safety steps:
- Perform hand hygiene.
- Check the room for transmission-based precautions.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain the process to the patient.
- Be organized and systematic.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure the patient’s privacy and dignity.
- Assess ABCs.
- Assess for latex/iodine allergies, enlarged prostate, joint limitations for positioning, and any history of previous issues with catheterization.
- Prepare the area for the procedure:
- Place hand sanitizer for use during/after procedure on the table near the bed.
- Place the catheter kit and peri-care supplies on the over-the-bed table.
- Secure the wastebasket near the bed for disposal.
- Ensure adequate lighting. Enlist assistance for positioning if needed.
- Raise the opposite side rail. Set the bed to a comfortable height.
- Position the male patient supine with legs extended. Uncover the patient, exposing the patient’s groin, legs, and feet for positioning and sterile field.
- Apply clean nonsterile gloves and perform peri-care.
- Remove gloves and perform hand hygiene.
- Open the outer package wrapping. Remove the sterile wrapped box with the paper label facing upward to avoid spilling contents and place it on the bedside table or, if possible, between the patient’s legs. Place the plastic package wrapping at the end of the bed or on the side of the bed near you, with the opening facing you or facing upwards for waste.
- Open the kit to create and position a sterile field (if on bedside table):
- Open first flap away from you.
- Open second flap toward you.
- Open side flaps.
- Only touch the outer 1” edge of the field to position the sterile field on the table.
- Carefully remove the sterile drape from the kit. Touching only the outermost edges of the drape, unfold and place the touched side of the drape closest to linen, under the patient. Vertically position the drape between the patient’s legs to allow space for the sterile box and sterile tray. Do not reach over the drape as it is placed.
- Wash your hands and apply sterile gloves.
- OPTIONAL: Place the fenestrated drape over the patient’s perineal area with gloves on inside of the drape, away from the patient's gown, with peri-area visible through the opening. Maintain sterility.
- Empty the syringe or package of lubricant into the plastic tray. Place the empty syringe/package on the sterile outer package.
- Simulate application (do not open) of the iodine cleanser to the cotton. Place package on sterile outer package.
- Remove the sterile urine specimen container and cap and set them aside.
- Remove the tray from the top of the box and place on sterile drape.
- Carefully remove the plastic catheter covering, while keeping the catheter in the container. Attach the syringe filled with sterile water to the balloon port of the catheter; keep the catheter sterile.
- Lubricate the tip of the catheter by dipping it in lubricant and replace it in the box. Maintain sterility.
- If preparing the kit on a bedside table, place the plastic tray on top of the sterile box and carry it as one unit to the sterile drape between the patient’s legs, taking care not to touch your gloves on the patient's legs or bed linens.
- Place the top plastic tray on the sterile drape nearest to the patient.
- Tell the patient that you are going to clean the catheterization area and they will feel a cold sensation.
- With your nondominant hand, grasp the penis and retract the foreskin if present; position at a 90-degree angle. Your nondominant hand will now be nonsterile. This hand must remain in place throughout the procedure.
- With your sterile dominant hand, use the forceps to pick up a cotton ball. Cleanse the glans penis with a saturated cotton ball in a circular motion from the center of the meatus outward. Discard the cotton ball after use into the plastic outer wrap, not crossing the sterile field. Repeat for a total of three times using a new cotton ball each time. Discard the forceps in the plastic bag without touching your sterile gloved hand to the bag.
- Pick up the catheter with your sterile dominant hand. Instruct the patient to take a deep breath and exhale or “bear down” as if to void, as you steadily insert the catheter, maintaining sterility of the catheter, until urine is noted in the tube.
- Once urine is noted, continue inserting to the catheter bifurcation.
- With your nondominant/nonsterile hand, continue to hold the penis, and use your thumb and index finger to stabilize the catheter. With the dominant hand, inflate the retention balloon with the water-filled syringe to the level indicated on the balloon port of the catheter. With the plunger still pressed, remove the syringe and set it aside. Pull back on the catheter slightly until resistance is met, confirming the balloon is in place. Replace the foreskin, if retracted, for the procedure.
 If the patient experiences pain during balloon inflation, deflate the balloon and insert the catheter farther into the bladder. If pain continues with the balloon inflation, remove the catheter and notify the patient’s provider.
If the patient experiences pain during balloon inflation, deflate the balloon and insert the catheter farther into the bladder. If pain continues with the balloon inflation, remove the catheter and notify the patient’s provider. - Remove the sterile draping and supplies from the bed area and place them on the bedside table. Remove the bath blanket and reposition the patient.
- Remove your gloves and perform hand hygiene.
- Apply new gloves. Secure the catheter with the securement device, allowing room to not pull on the catheter.
- Place the drainage bag below the level of the bladder and attach the bag to the bed frame.
- Perform peri-care as needed.
- Dispose of waste and used supplies.
- Remove your gloves and perform hand hygiene.
- Assist the patient to a comfortable position, ask if they have any questions, and thank them for their time.
- Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Perform hand hygiene.
- Document the procedure and related assessment findings. Report any concerns according to agency policy.
Use the checklist below to review the steps for completion of “Foley Catheter Insertion (Female).”
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Gather supplies: peri-care supplies, clean gloves, Foley catheter kit, extra pair of sterile gloves, VelcroTM catheter securement device to secure Foley catheter to leg, wastebasket, and light source (i.e., goose neck lamp or flashlight).
- Perform safety steps:
- Perform hand hygiene.
- Check the room for transmission-based precautions.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain the process to the patient.
- Be organized and systematic.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure the patient’s privacy and dignity.
- Assess ABCs.
- Assess for latex/iodine allergies, GYN surgeries, joint limitations for positioning, and any history of previous difficulties with catheterization.
- Prepare the area for the procedure:
- Place hand sanitizer for use during/after procedure on the table near the bed.
- Place the catheter kit and peri-care supplies on the over-the-bed table.
- Secure the wastebasket near the bed for disposal.
- Ensure adequate lighting. Enlist assistance for positioning if needed.
- Raise the opposite side rail. Set the bed to a comfortable height.
- Position the female patientin a dorsal recumbent position. Uncover the patient, exposing the patient’s groin, legs, and feet for positioning and sterile field (female = dorsal recumbent; may need assistance to position patient and help support legs). Drape the patient with a bath blanket, exposing only the necessary area for patient privacy.
- Apply nonsterile gloves and perform peri-care.
- Remove gloves and perform hand hygiene.
- Create a sterile field on the over-the-bed table.
- Open the outer package wrapping. Remove the sterile wrapped box with the paper label facing upward to avoid spilling contents and place it on the bedside table or, if possible, between the patient’s legs. Place the plastic package wrapping at the end of the bed or on the side of the bed near you, with the opening facing you or facing upwards for waste.
- Open the kit to create and position a sterile field:
- Open the first flap away from you.
- Open the second flap toward you.
- Open side flaps.
- Only touch within the outer 1” edge to position the sterile field on the table.
- Carefully remove the sterile drape from the kit. Touching only the outermost edges of the drape, unfold and place the touched side of drape closest to linen, under the patient. Vertically position the drape between the patient’s legs to allow space for the sterile box and sterile tray.
- Wash your hands and apply sterile gloves.
- OPTIONAL: Place the fenestrated drape over the patient’s perineal area with gloves on inside of the drape, away from the patient’s gown, with peri-area visible through the opening. Maintain sterility.
- Empty the lubricant syringe or package into the plastic tray. Place the empty syringe/package on the sterile outer package.
- Simulate application of iodine/antimicrobial cleanser to cotton balls.
- Remove the sterile urine specimen container and cap and set them aside.
- Remove the tray from the top of the box and place it on the sterile drape.
- Carefully remove the plastic catheter covering, while keeping the catheter in the sterile box. Attach the syringe filled with sterile water to the balloon port of the catheter; keep the catheter sterile.
- Lubricate the tip of the catheter by dipping it in lubricant and place it in the box while maintaining sterility.
- If preparing the kit on the bedside table, prepare to move the items to the patient. Place the plastic tray on top of the sterile box and carry as one unit to the sterile drape between the patient’s legs, taking care not to touch your gloves to the patient’s legs or bed linens.
- Place the plastic top tray on the sterile drape nearest to the patient.
- Tell the patient that you are going to clean the catheterization area and they will feel a cold sensation.
- With your nondominant hand, gently spread the labia minora and visualize the urinary meatus. Your nondominant hand will now be nonsterile. This hand must remain in place throughout the procedure.
- With your dominant hand, use an antiseptic swab or pick up a sterile antiseptic soaked cotton ball with plastic forceps to clean the labia minora farthest from you using a downward stroke, then discard the swab or cotton ball. Repeat for the labia minora closest to you. Use another antiseptic swab or antiseptic soaked cotton ball to clean the area between the labia minora. Discard the cotton ball after use into the plastic bag, not crossing the sterile field. Repeat for a total of three times using a new cotton ball each time. Discard the forceps in the plastic bag without touching the sterile gloved hand to the bag.[58]
- Pick up the catheter with your sterile dominant hand. Instruct the patient to take a deep breath and exhale or “bear down” as if to void, as you steadily insert the catheter maintaining sterility of the catheter until urine is noted.
- Once urine is noted, continue inserting the catheter 2-3" farther.” Do not force the catheter.
- With your dominant hand, inflate the retention balloon with the water-filled syringe to the level indicated on the balloon port of the catheter. With the plunger still pressed, remove the syringe and set it aside. Pull back on the catheter until resistance is met, confirming the balloon is in place.

If the patient experiences pain during balloon inflation, deflate the balloon and insert the catheter farther into the bladder. If pain continues with the balloon inflation, remove the catheter and notify the patient's provider. - Remove the sterile draping and supplies from the bed area and place them on the bedside table. Remove the bath blanket and reposition the patient.
- Remove your gloves and perform hand hygiene.
- Apply new gloves. Secure the catheter with securement device, allowing room as to not pull on the catheter.
- Place the drainage bag below the level of the bladder, attaching it to the bed frame.
- Perform peri-care as needed.
- Dispose of waste and used supplies.
- Remove gloves and perform hand hygiene.
- Assist the patient to a comfortable position, ask if they have any questions, and thank them for their time.
- Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Perform hand hygiene.
- Document the procedure and related assessment findings. Report any concerns according to agency policy.
Use the checklist below to review the steps for completion of “Foley Removal.”
View an instructor demonstration of Removing a Foley Catheter[59]:
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Verify order.
- Gather supplies: urinary graduated cylinder, gloves, 10-mL syringe, peri-care supplies, chux/waterproof pad, and wastebasket.
- Perform safety steps:
- Perform hand hygiene.
- Check the room for transmission-based precautions.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain the process to the patient.
- Be organized and systematic.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure the patient’s privacy and dignity.
- Assess ABCs.
- Place peri-care supplies, chux, and syringe on the overbed table. Place the wastebasket near the bed and place the urinary graduate on the floor (on a barrier such as a paper towel) near the Foley bag:
- Empty urine from the tubing into the catheter bag. Empty the catheter bag into the urinary graduate.
- Note amount of urine for I & O.
- Empty graduate in the bathroom.
- Remove gloves. Perform hand hygiene and then apply clean nonsterile gloves.
- Uncover the patient so that only the genital area and catheter are exposed.
- Place a protective pad under the patient.
- Remove any securement device holding the catheter to the upper thigh.
- Attach the 10-mL syringe into the balloon port and remove all the fluid from the balloon; while holding the plunger, detach the syringe.
- Ask the patient to take a deep breath and exhale, as you remove the catheter on expiration. Stop if resistance is met.
- Inspect the catheter to determine if it was removed intact; place it in the wastebasket or facility-approved receptacle.
- Cleanse the perineal area or allow the patient to cleanse the area.
- Remove the catheter materials and waste and place them in the wastebasket.
- Remove gloves and perform hand hygiene.
- Assist the patient to a comfortable position, ask if they have any questions, and thank them for their time.
- Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Perform hand hygiene.
- Document the procedure and related assessment findings. Report any concerns according to agency policy.
Please follow the checklist below to review the steps for completion of “Straight Catheterization for Female/Male."
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Gather supplies: peri-care supplies, nonsterile gloves, straight catheter kit, extra pair of sterile gloves, and preprinted patient label.
- Perform safety steps:
- Perform hand hygiene.
- Check the room for transmission-based precautions.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain the process to the patient.
- Be organized and systematic.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure the patient’s privacy and dignity.
- Assess ABCs.
- Assess for latex/iodine allergies, joint limitations for positioning, and history of previous difficulties with catheterization:
- Female: Ask about previous gynecological surgeries.
- Male: Ask about previous diagnosis of enlarged prostate.
- Place the hand sanitizer and other supplies for use during/after procedure on the table near the bed.
- Place the catheter kit and peri-care supplies on the over-the-bed table.
- Ensure adequate lighting. Enlist assistance for positioning if needed.
- Raise the opposite side rail. Set the bed to a comfortable height.
- Position the patient supine and uncover the patient, exposing the patient’s groin, legs, and feet for positioning and sterile field (male = supine, legs extended; female = dorsal recumbent; may need assistance to position patient and help support legs).
- Wash your hands, apply clean gloves, and clean the perineal area.
- Remove your gloves and perform hand hygiene.
- Open the package. Take out the sterile package and place it on the table. Place the plastic package wrapping at end of the bed or on the side of the bed near you.
- Open the kit extending the outer wrapping to create a sterile field; position the sterile field on the table to create space for opening gloves at the end of the table.
- Place the sterile pad/sheet under the patient without contaminating the center of the drape by only holding onto the edges of the drape.
- Perform hand hygiene and apply sterile gloves.
- (Optional use of fenestrated drape). Place the fenestrated drape over the patient’s perineal area, keeping your gloves sterile by folding the corners of the sterile drape over the sterile gloves before approaching the patient.
- If a urine specimen is ordered, remove the sterile specimen container and remove the lid, if attached. Set the container on the sterile drape and invert the lid to maintain sterility. Position the container on the sterile drape to be within reach during the procedure.
- Place the plastic tray with cotton balls and forceps on the sterile drape. Simulate opening the iodine solution and simulate pouring on the cotton balls; set the iodine package on the drape. Iodine cannot be used on mannequins.
- Locate the catheter in the bottom of the tray; leave it in the tray. Open the water-soluble sterile lubricant and empty it into the bottom of the tray.
- Put the plastic tray with saturated cotton balls horizontally on top of the tray to fit above the catheter and lubricant, which are located in the bottom of the tray.
- Make sure that the sterile specimen container is within reach of your dominant hand. Then, carefully move the tray as a unit with supplies inside to the sterile drape between the patient’s legs.
- Tell the patient that you are now going to start the cleaning process and that there will be a cold sensation:
- Once the nondominant/nonsterile hand touches the patient, the position is held throughout the procedure until the catheter is inserted.
- Inspect for the urinary meatus:
- Female: Gently spread the labia minora with your thumb and index finger of your nondominant hand and visualize the urinary meatus.
- Male: Gently grasp the penis with the nondominant hand and retract the foreskin if present.
- Cleanse the urinary meatus:
- Female: With your dominant hand, use an antiseptic swab or pick up a sterile antiseptic soaked cotton ball with plastic forceps to clean the labia minora farthest from you using a downward stroke, then discard the swab or cotton ball. Repeat for the labia minora closest to you. Use another antiseptic swab or antiseptic soaked cotton ball to clean the area between the labia minora. With the dominant sterile gloved hand, pick up the lubricated catheter about 4 inches from the end for stability. Place the distal end in the receptacle.
- Male: With your sterile dominant hand, use the forceps to pick up a cotton ball. Cleanse the glans penis with the antimicrobial cleanser using a circular motion from the center of the meatus outward to the base of the glans. Discard each cotton ball after use without crossing the sterile field. Continue to hold the penis perpendicular to the body with your nondominant hand. With the dominant sterile gloved hand, pick up the lubricated catheter about 4 inches from the end for stability. Place the distal end in the receptacle.
- Steadily insert the catheter, maintaining sterility into the meatus until a return of urine occurs.
- Continue inserting another 1-2 inches and hold the catheter in place.
- When urine begins to drain out of the catheter, pinch the catheter with your thumb and index finger of your nondominant/nonsterile hand while continuing to hold the labia apart or penis perpendicular to the body.
- With your dominant/sterile hand, obtain the sterile specimen container from the table and put it under the catheter.
- Release clamping/pinching of the catheter, allowing urine to drain into the sterile specimen container.
- When the container is almost full, use your dominant hand to remove the container from under the stream of urine and set it on the table, maintaining sterility.
- Allow urine to continue to flow into the receptacle provided until the flow of urine stops.
- Tell the patient that the catheter will be removed. Instruct the patient to take a deep breath and exhale, and then remove the catheter and place it on the sterile drape on the bed.
- Carefully remove the urine container full of urine from the bed and place it on the kit wrapper on the table. Do not put the urine container directly on the table.
- Put the cap on the sterile specimen container, maintaining sterility.
- Remove the catheter and other supplies from the patient’s bed; provide peri-care. For males, replace foreskin if it was retracted for the procedure.
- Remove your gloves; wash hands and apply new gloves.
- Write the date, time collected, and your initials on the two preprinted patient labels.
- With an antibacterial wipe, clean the outer surface of the specimen container.
- Apply one patient label to the specimen container and one patient label to the outside of the clear biohazard bag for transport to the lab.
- Place the specimen container in the biohazard bag.
- Measure and dispose of the urine in the bathroom.
- Remove your gloves and perform hand hygiene.
- Assist the patient to a comfortable position, ask if they have any questions, and thank them for their time.
- Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Send the specimen to the lab for processing.
- Document the procedure and related assessment findings. Report any concerns according to agency policy.
Use the checklist below to review the steps for completion of an “Ostomy Appliance Change."
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Gather supplies: washcloth and warm water, stoma products/appliances per order/patient preference (wafer, bag, clip), gauze, pads, sizing measures, scissors, pen, nonsterile gloves, skin prep or other skin products per patient preference, and wastebasket.
- Perform safety steps:
- Perform hand hygiene.
- Check the room for transmission-based precautions.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain the process to the patient.
- Be organized and systematic.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure the patient’s privacy and dignity.
- Assess ABCs.
- Set the bed to a comfortable height; raise the opposite side rail.
- Ask the patient about preferences, usual practices, care, and maintenance at home.
- Apply nonsterile gloves.
- Position the patient according to patient status:
- Assist the patient to the bathroom and have them sit on the toilet to be near the sink for ease of process.
- If in bed, uncover the patient, exposing only the abdomen. Apply drape/chux under the patient or ostomy pouch. Place the wastebasket near the bed.
- Empty the pouch depending on the type of the appliance and the location type of procedure:
- Remove the pouch and empty it into the toilet.
- Set pouch aside in the basin or receptacle if at bedside.
- Assess ostomy bag contents and remove current ostomy appliance (keep clamp if present).
- Remove adhesive residue from the skin with adhesive remover wipes.
- Cleanse the stoma and surrounding skin with gauze and room temperature tap water; pat dry the skin.
- Assess the condition of the stoma and peristomal skin.
- Place new gauze pad over the stoma while you are preparing the new wafer and pouch.
- Trace the pattern onto the paper backing of the wafer and cut the wafer. (If a pattern is available, cut the new wafer prior to removing the pouch). No more than 1/8th inch (2 mm) of skin around the stoma should be exposed for correct fit.
- Apply skin prep and wait until tacky (optional).
- Remove the gauze pad from the orifice of the stoma.
- Remove the paper backing from the wafer and place it on the skin with the stoma centered in the cutout opening of the wafer; press gently on the wafer to remove air/seal to the skin.
- Apply pouch to wafer with clamp on pouch and opening in downward position.
- Attach and close the pouch clamp.
- Dispose of used supplies and wrappings.
- Remove your gloves and perform hand hygiene.
- Assist the patient to a comfortable position, ask if they have any questions, and thank them for their time.
- Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Document the procedure and related assessment findings. Report any concerns according to agency policy.
Learning Activities
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
1. Your patient complains of pain while you are inflating the balloon during a urinary catheter insertion. Describe your next steps.
2. Your patient is admitted with a fractured head of the right femur and is scheduled for surgery in the next six hours. You have a prescription to insert a Foley catheter. After you assess the patient’s ability for the recommended position to insert the catheter, you note that the patient is unable to move the right leg and should not move the leg. Describe how you will proceed with the procedure.
3. A patient with a new colostomy refuses to look at the stoma or participate in changing the pouching system. What are some suggestions to help your patient adjust to the stoma?
4. The nurse is caring for a female patient who is experiencing inadequate bladder emptying. The nurse obtains an order to determine post-void residual. Which catheter type would the nurse use to evaluate post-void residual?
- Coude catheter
- Indwelling catheter
- Straight catheter
- Foley catheter
5. The nurse is caring for a patient who had a colostomy placed two days earlier. The nurse notes that the stoma is moist and beefy red. Which action should the nurse be expected to take based on these findings?
- Notify the physician of the findings immediately.
- Remove the bag and apply pressure to the stoma.
- Document the assessment findings of the stoma.
- Change the appliance pouch and clean the skin.
6. The nurse is providing patient education on the care of an ostomy. Which of the following statements by the patient would indicate that further education is necessary?
- “I should plan to replace the pouch system every 8-10 days.”
- “Wafer should be cut 1/16 to 1/8 an inch larger than the stoma.”
- “It is important to chew all foods completely and slowly.”
- “I will keep a diary of the foods I eat and my stool pattern.”
![]()
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 21, Assignment 1.
![]()
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 21, Assignment 2.
![]()
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 21, Assignment 3.
Learning Objectives
- Safely perform nasal, oral, pharyngeal, and tracheostomy suctioning
- Provide tracheostomy care
- Explain procedure to patient
- Adapt procedure to reflect variations across the life span
- Document actions and observations
- Recognize and report significant deviations from norms
This chapter will discuss tracheostomy care and various types of suctioning (e.g., oral, nasal, pharyngeal, and tracheostomy) performed by nurses. The purpose of respiratory suctioning is to maintain a patent airway and improve oxygenation by removing mucous secretions and foreign material (e.g., vomit or gastric secretions). During oral suctioning, a rigid plastic suction catheter is typically used in a patient’s mouth to remove oral secretions. Nasal and pharyngeal suctioning are performed with a sterile, soft, flexible catheter to remove accumulated saliva, pulmonary secretions, blood, vomitus, or other foreign material from nasopharyngeal areas that cannot be removed by the patient’s spontaneous cough or other less invasive procedures.[60] Tracheostomy suctioning uses a sterile catheter that is inserted through a tracheostomy tube into a patient’s trachea. A tracheostomy tube is a tube that is inserted through a surgical opening in the neck to the trachea to create an artificial airway. Tracheostomies require routine care to prevent infection and obstruction, as well as frequent suctioning to maintain a patent airway.[61] Tracheostomy care and suctioning are performed collaboratively by nurses and respiratory therapists.
Respiratory System Anatomy
It is important for the nurse to have an understanding of the underlying structures of the respiratory system before performing suctioning to ensure that care is given to protect sensitive tissues and that airways are appropriately assessed during the suctioning procedure. See Figure 22.1[62] for an illustration of the anatomy of the respiratory system.
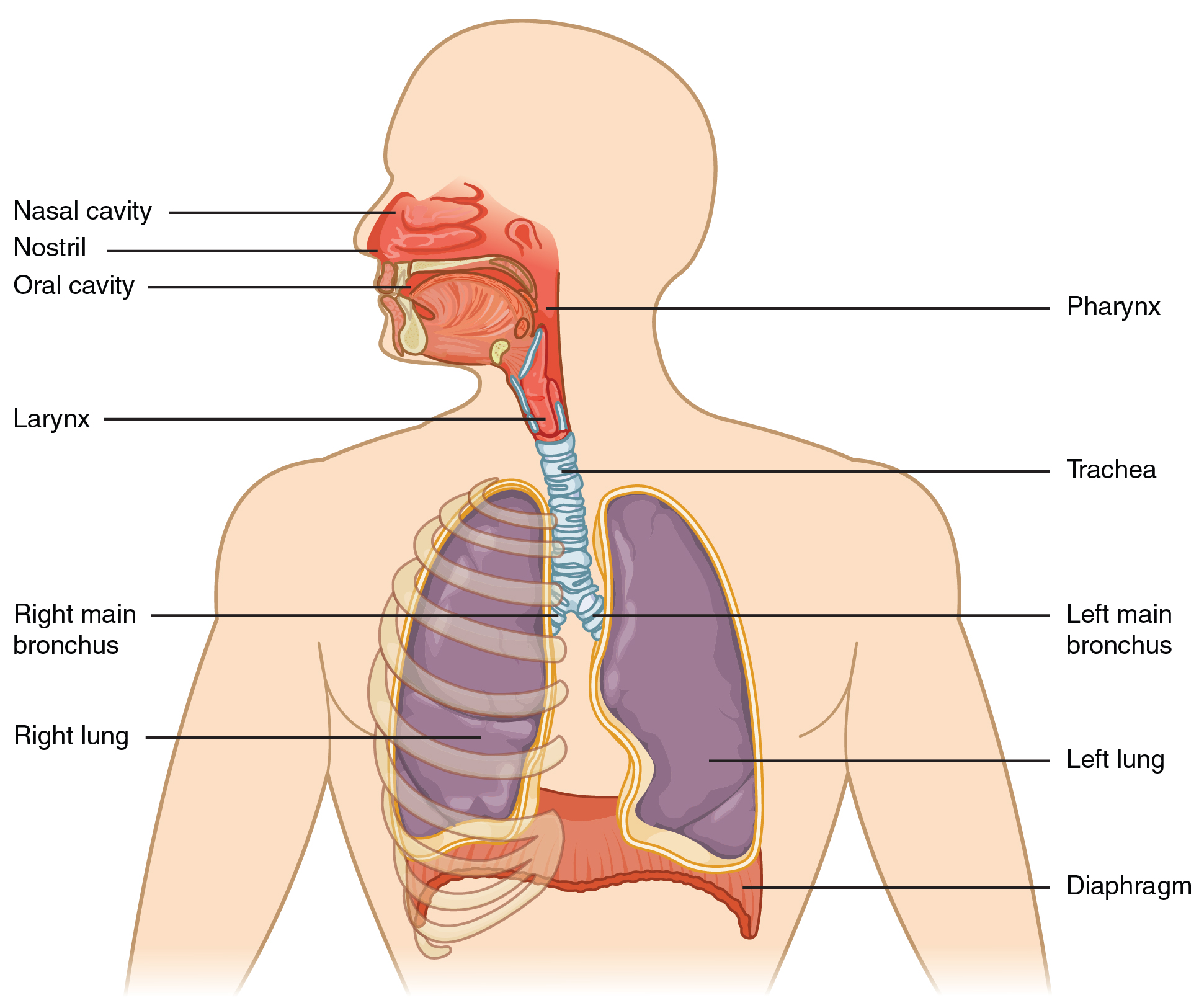
Maintaining a patent airway is a top priority and one of the “ABCs” of patient care (i.e., Airway, Breathing, and Circulation). Suctioning is often required in acute care settings for patients who cannot maintain their own airway due to a variety of medical conditions such as respiratory failure, stroke, unconsciousness, or postoperative care. The suctioning procedure is useful for removing mucus that may obstruct the airway and compromise the patient’s breathing ability.
To read more details about the respiratory system, see the “Respiratory Assessment” chapter.
Respiratory Failure and Respiratory Arrest
Respiratory failure and respiratory arrest often require emergency suctioning. Respiratory failure is a life-threatening condition that is caused when the respiratory system cannot get enough oxygen from the lungs into the blood to oxygenate the tissues, or there are high levels of carbon dioxide in the blood that the body cannot effectively eliminate via the lungs. Acute respiratory failure can happen quickly without much warning. It is often caused by a disease or injury that affects breathing, such as pneumonia, opioid overdose, stroke, or a lung or spinal cord injury. Acute respiratory failure requires emergency treatment. Untreated respiratory failure can lead to respiratory arrest.
Signs and symptoms of respiratory failure include shortness of breath (dyspnea), rapid breathing (tachypnea), rapid heart rate (tachycardia), unusual sweating (diaphoresis), decreasing pulse oximetry readings below 90%, and air hunger (a feeling as if you can't breathe in enough air). In severe cases, signs and symptoms may include cyanosis (a bluish color of the skin, lips, and fingernails), confusion, and sleepiness.
The main goal of treating respiratory failure is to ensure that sufficient oxygen reaches the lungs and is transported to the other organs while carbon dioxide is cleared from the body.[63] Treatment measures may include suctioning to clear the airway while also providing supplemental oxygen using various oxygenation devices. Severe respiratory distress may require intubation and mechanical ventilation, or the emergency placement of a tracheostomy may be performed if the airway is obstructed. For additional details about oxygenation and various oxygenation devices, go to the “Oxygen Therapy" chapter.
Tracheostomy
A tracheostomy is a surgically created opening called a stoma that goes from the front of the patient’s neck into the trachea. A tracheostomy tube is placed through the stoma and directly into the trachea to maintain an open (patent) airway. See Figure 22.2[64] for an illustration of a patient with a tracheostomy tube in place.
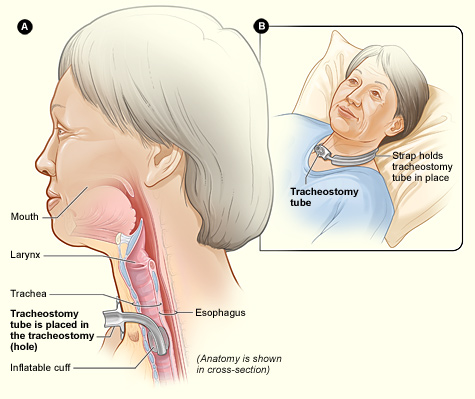
Placement of a tracheostomy tube may be performed emergently or as a planned procedure due to the following:
- A large object blocking the airway
- Respiratory failure or arrest
- Severe neck or mouth injuries
- A swollen or blocked airway due to inhalation of harmful material such as smoke, steam, or other toxic gases
- Cancer of the throat or neck, which can affect breathing by pressing on the airway
- Paralysis of the muscles that affect swallowing
- Surgery around the larynx that prevents normal breathing and swallowing
- Long-term oxygen therapy via a mechanical ventilator[65]
See Figure 22.3[66] for an image of the parts of a tracheostomy tube. The outside end of the outer cannula has a flange that is placed against the patient’s neck. The flange is secured around the patient’s neck with tie straps, and a split 4" x 4" tracheostomy dressing is placed under the flange to absorb secretions. A cuff is typically present on the distal end of the outer cannula to make a tight seal in the airway. (See the top image in Figure 22.3.) The cuff is inflated and deflated with a syringe attached to the pilot balloon. Most tracheostomy tubes have a hollow inner cannula inside the outer cannula that is either disposable or removed for cleaning as part of the tracheostomy care procedure. (See the middle image of Figure 22.3.) A solid obturator is used during the initial tracheostomy insertion procedure to help guide the outer cannula through the tracheostomy and into the airway. (See the bottom image of Figure 22.3.) It is removed after insertion and the inner cannula is slid into place.

When a tracheostomy is placed, the provider determines if a fenestrated or unfenestrated outer cannula is needed based on the patient's condition. A fenestrated tube is used for patients who can speak with their tracheostomy tube in place. Under the guidance of a speech pathologist and respiratory therapist, the inner cannula is eventually removed from a fenestrated tube and the cuff deflated so the patient is able to speak. Otherwise, a patient with a tracheostomy tube is unable to speak because there is no airflow over the vocal cords, and alternative communication measures, such as a whiteboard, pen and paper, or computer device with note-taking ability, must be put into place by the nurse. Suctioning should never be performed through a fenestrated tube without first inserting a nonfenestrated inner cannula, or severe tracheal damage can occur. See Figure 22.4[67] for images of a fenestrated and nonfenestrated outer cannula.

Caring for a patient with a tracheostomy tube includes providing routine tracheostomy care and suctioning. Tracheostomy care is a procedure performed routinely to keep the flange, tracheostomy dressing, ties or straps, and surrounding area clean to reduce the introduction of bacteria into the trachea and lungs. The inner cannula becomes occluded with secretions and must be cleaned or replaced frequently according to agency policy to maintain an open airway. Suctioning through the tracheostomy tube is also performed to remove mucus and to maintain a patent airway.
Subjective Assessment
If appropriate, perform a focused interview collecting a brief history of respiratory conditions and assess for feelings of shortness of breath (dyspnea), sputum production, and coughing.
Objective Assessment
Prior to suctioning, a baseline assessment for indications of respiratory distress and the need for suctioning should be obtained and documented, including, but not limited to, the following:
- Secretions from the mouth and/or tracheal stoma
- Auscultation of lung sounds
- Heart rate
- Respiratory rate
- Cardiac rhythm
- Oxygen saturation
- Skin color and perfusion
- Effectiveness of cough[68]
Prepare the patient by explaining the procedure and providing adequate sedation and pain relief as needed. Place the patient in semi-Fowler’s position if conscious or in a lateral position facing you if they are unconscious. While suctioning the patient, if signs of worsening respiratory distress occur, stop the procedure and request emergency assistance. The following should be monitored during and following the procedure:
- Lung sounds
- Skin color
- Breathing pattern and rate
- Oxygenation (pulse oximeter)
- Pulse rate
- Dysrhythmias if electrocardiogram is available
- Color, consistency, and volume of secretions
- Presence of bleeding or evidence of physical trauma
- Subjective response, including pain
- Cough
- Laryngospasm (spasm of the vocal cords that can result in airway obstruction)[69]
After completing suctioning, the outcomes from the procedure should be evaluated and documented, including the following:
- Improvement of lung sounds
- Removal of secretions
- Improvement of pulse oximetry
- Decreased work of breathing
- Stabilized respiratory rate
- Decreased dyspnea
Be aware that the patient's lung sounds may not clear completely after suctioning, but the removal of secretions should improve the patency of the patient's airway.
Potential complications resulting from this procedure include nasal irritation/bleeding, gagging/vomiting, discomfort and pain, and uncontrolled coughing. Potential adverse reactions include mucosal hemorrhage, laceration of nasal turbinate, perforation of the pharynx, hypoxia/hypoxemia, cardiac dysrhythmias/arrest, bradycardia, elevated blood pressure, hypotension, respiratory arrest, laryngospasm, bronchoconstriction, bronchospasm, hospital-acquired infection, atelectasis, increased intracranial pressure, and pneumothorax.
Suctioning via the oropharyngeal (mouth) and nasopharyngeal (nasal) routes is performed to remove accumulated saliva, pulmonary secretions, blood, vomitus, and other foreign material from these areas that cannot be removed by the patient’s spontaneous cough or other less invasive procedures. Nasal and pharyngeal suctioning are performed in a wide variety of settings, including critical care units, emergency departments, inpatient acute care, skilled nursing facility care, home care, and outpatient/ambulatory care. Suctioning is indicated when the patient is unable to clear secretions and/or when there is audible or visible evidence of secretions in the large/central airways that persist in spite of the patient's best cough effort. Need for suctioning is evidenced by one or more of the following:
- Visible secretions in the airway
- Chest auscultation of coarse, gurgling breath sounds, rhonchi, or diminished breath sounds
- Reported feeling of secretions in the chest
- Suspected aspiration of gastric or upper airway secretions
- Clinically apparent increased work of breathing
- Restlessness
- Unrelieved coughing[70]
In emergent situations, a provider order is not necessary for suctioning to maintain a patient’s airway. However, routine suctioning does require a provider order.
For oropharyngeal suctioning, a device called a Yankauer suction tip is typically used for suctioning mouth secretions. A Yankauer device is rigid and has several holes for suctioning secretions that are commonly thick and difficult for the patient to clear. See Figure 22.5[71] for an image of a Yankauer device. In many agencies, Yankauer suctioning can be delegated to trained assistive personnel if the patient is stable, but the nurse is responsible for assessing and documenting the patient’s respiratory status.

Nasopharyngeal suctioning removes secretions from the nasal cavity, pharynx, and throat by inserting a flexible, soft suction catheter through the nares. This type of suctioning is performed when oral suctioning with a Yankauer is ineffective. See Figure 22.6[72] for an image of a sterile suction catheter.
![“DSC_0210-150x150.jpg” by British Columbia Institute of Technology (BCIT) is licensed under CC BY 4.0. [/footnote] Access for free at https://opentextbc.ca/clinicalskills/chapter/5-7-oral-suctioning/ Photo of a sterile suction catheter being handled by a person wearing gloves](https://opencontent.ccbcmd.edu/app/uploads/sites/30/2024/08/DSC_0210-scaled-1.jpg)
Extension tubing is used to attach the Yankauer or suction catheter device to a suction canister that is attached to wall suction or a portable suction source. The amount of suction is set to an appropriate pressure according to the patient’s age. See Figure 22.7[73] for an image of extension tubing attached to a suction canister that is connected to a wall suctioning source.
![“DSC_0206-e1437445438554.jpg” by by British Columbia Institute of Technology (BCIT) is licensed under CC BY 4.0. [/footnote]. Access for free at https://opentextbc.ca/clinicalskills/chapter/5-7-oral-suctioning/ Photo showing tubing attaching suction canister to wall suction source](https://opencontent.ccbcmd.edu/app/uploads/sites/30/2024/08/DSC_0206-e1437445438554-scaled-1.jpg)
Follow agency policy regarding setting suction pressure. Pressure should not exceed 150 mm Hg because higher pressures have been shown to cause trauma, hypoxemia, and atelectasis. The following ranges are appropriate pressure according to the patient's age:
- Neonates: 60-80 mm Hg
- Infants: 80-100 mm Hg
- Children: 100-120 mm Hg
- Adults: 100-150 mm Hg
Checklist for Oropharyngeal or Nasopharyngeal Suctioning
Use the checklist below to review the steps for completion of “Oropharyngeal or Nasopharyngeal Suctioning.”
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Gather supplies: Yankauer or suction catheter, suction machine or wall suction device, suction canister, connecting tubing, pulse oximeter, stethoscope, PPE (e.g., mask, goggles or face shield, nonsterile gloves), sterile gloves for suctioning with sterile suction catheter, towel or disposable paper drape, nonsterile basin or disposable cup, water soluble lubricant, normal saline or tap water.
- Perform safety steps:
- Perform hand hygiene.
- Check the room for transmission-based precautions.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain the process to the patient.
- Be organized and systematic.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure the patient’s privacy and dignity.
- Assess ABCs.
- Adjust the bed to a comfortable working height and lower the side rail closest to you.
- Position the patient:
- If conscious, place the patient in a semi-Fowler’s position.
- If unconscious, place the patient in the lateral position, facing you.
- Move the bedside table close to your work area and raise it to waist height.
- Place a towel or waterproof pad across the patient’s chest.
- Adjust the suction to the appropriate pressure:
- Adults and adolescents: no more than 150 mm Hg
- Children: no more than 120 mmHg
- Infants: no more than 100 mm Hg
- Neonates: no more than 80 mm Hg
For a portable unit:
- Adults: 10 to 15 cm Hg
- Adolescents: 8 to 15 cm Hg
- Children: 8 to 10 cm Hg
- Infants: 8 to 10 cm Hg
- Neonates: 6 to 8 cm Hg
- Put on a clean glove and occlude the end of the connection tubing to check suction pressure.
- Place the connecting tubing in a convenient location (e.g., at the head of the bed).
- Open the sterile suction package using aseptic technique. (NOTE: The open wrapper or container becomes a sterile field to hold other supplies.) Carefully remove the sterile container, touching only the outside surface. Set it up on the work surface and fill with sterile saline using sterile technique.
- Place a small amount of water-soluble lubricant on the sterile field, taking care to avoid touching the sterile field with the lubricant package.
- Increase the patient’s supplemental oxygen level or apply supplemental oxygen per facility policy or primary care provider order.
- Don additional PPE. Put on a face shield or goggles and mask.
- Don sterile gloves. The dominant hand will manipulate the catheter and must remain sterile.
- The nondominant hand is considered clean rather than sterile and will control the suction valve on the catheter.
- In the home setting and other community-based settings, maintenance of sterility is not necessary.
- With the dominant gloved hand, pick up the sterile suction catheter. Pick up the connecting tubing with the nondominant hand and connect the tubing and suction catheter.
- Moisten the catheter by dipping it into the container of sterile saline. Occlude the suction valve on the catheter to check for suction.
- Encourage the patient to take several deep breaths.
- Apply lubricant to the first 2 to 3 inches of the catheter, using the lubricant that was placed on the sterile field.
- Remove the oxygen delivery device, if appropriate. Do not apply suction as the catheter is inserted. Hold the catheter between your thumb and forefinger.
- Insert the catheter. For nasopharyngeal suctioning, gently insert the catheter through the naris and along the floor of the nostril toward the trachea. Roll the catheter between your fingers to help advance it. Advance the catheter approximately 5 to 6 inches to reach the pharynx. For oropharyngeal suctioning, insert the catheter through the mouth, along the side of the mouth toward the trachea. Advance the catheter 3 to 4 inches to reach the pharynx.
- Apply suction by intermittently occluding the suction valve on the catheter with the thumb of your nondominant hand and continuously rotate the catheter as it is being withdrawn.[75]
- Suction only on withdrawal and do not suction for more than 10 to 15 seconds at a time to minimize tissue trauma.
- Replace the oxygen delivery device using your nondominant hand, if appropriate, and have the patient take several deep breaths.
- Flush the catheter with saline. Assess the effectiveness of suctioning by listening to lung sounds and repeat, as needed, and according to the patient’s tolerance. Wrap the suction catheter around your dominant hand between attempts:
- Repeat the procedure up to three times until gurgling or bubbling sounds stop, and respirations are quiet. Allow 30 seconds to 1 minute between passes to allow reoxygenation and reventilation.[76]
- When suctioning is completed, remove gloves from the dominant hand over the coiled catheter, pulling them off inside out.
- Remove the glove from the nondominant hand and dispose of gloves, catheter, and the container with solution in the appropriate receptacle.
- Turn off the suction. Remove the supplemental oxygen placed for suctioning, if appropriate.
- Remove face shield or goggles and mask; perform hand hygiene.
- Perform oral hygiene on the patient after suctioning.
- Reassess the patient’s respiratory status, including respiratory rate, effort, oxygen saturation, and lung sounds.
- Assist the patient to a comfortable position, ask if they have any questions, and thank them for their time.
- Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Perform hand hygiene.
- Document the procedure and related assessment findings. Report any concerns according to agency policy.
Sample Documentation
Sample Documentation of Expected Findings
Patient complaining of difficulty coughing up secretions. Order obtained for nasopharyngeal suctioning. Procedure explained to patient. Vitals signs prior to procedure: heart rate 88 regular, respiratory rate 28/minute, O2 saturation 88% on room air. Coarse rhonchi present over anterior upper airway. No cyanosis. Patient suctioned through left nare x 1 at 120 mm Hg with small amount clear, white, thick sputum obtained. Post-procedure vital signs: heart rate 78 regular, respiratory rate 18/minute, O2 saturation 94% room air. Lung sounds clear to auscultation and no cyanosis present.
Sample Documentation of Unexpected Findings
Patient complaining of difficulty expectorating secretions. Order obtained for nasopharyngeal suctioning and procedure explained to patient. Vital signs prior to procedure: heart rate 88 and regular, respiratory rate 28/minute, and O2 sat 88% room air. Coarse rhonchi present over anterior upper airway. No cyanosis. After first suctioning pass, patient coughing uncontrollably. Procedure stopped and emergency assistance requested from respiratory therapist. Post-procedure vital signs: heart rate 78 and regular, respiratory rate 18/minute, and O2 sat 94% room air. Course rhonchi remain over anterior upper airway but no cyanosis present. Dr. Smith notified and STAT order for chest X-ray received. Dr. Smith to be called with results.
Tracheostomy care is provided on a routine basis to keep the tracheostomy tube’s flange, inner cannula, and surrounding area clean and dry and to reduce the amount of bacteria entering the artificial airway, lungs, and maintain skin integrity. See Figure 22.9[77] for an image of a sterile tracheostomy care kit.
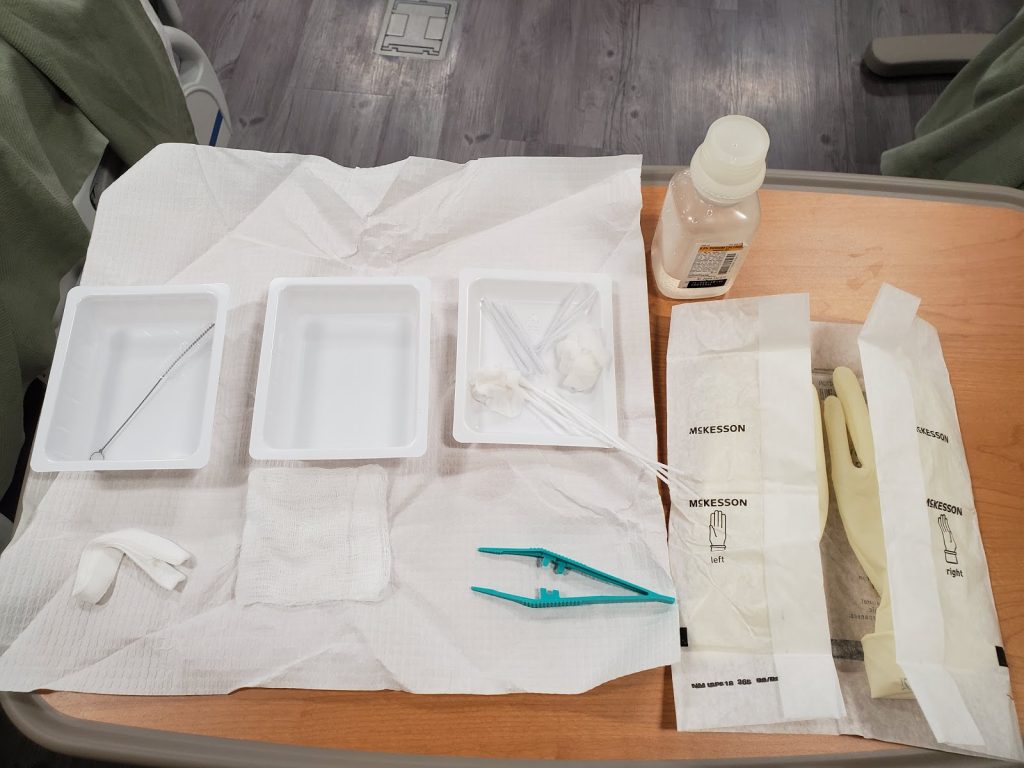
Replacing and Cleaning an Inner Cannula
The primary purpose of the inner cannula is to prevent tracheostomy tube obstruction. Many sources of obstruction can be prevented if the inner cannula is regularly cleaned and replaced. Some inner cannulas are designed to be disposable, while others are reusable for a number of days. Follow agency policy for inner cannula replacement or cleaning, but as a rule of thumb, inner cannula cleaning should be performed every 12-24 hours at a minimum. Cleaning may be needed more frequently depending on the type of equipment, the amount and thickness of secretions, and the patient’s ability to cough up the secretions.
Changing the inner cannula may encourage the patient to cough and bring mucus out of the tracheostomy. For this reason, the inner cannula should be replaced prior to changing the tracheostomy dressing to prevent secretions from soiling the new dressing. If the inner cannula is disposable, no cleaning is required.[78]
Checklist for Tracheostomy Care With a Reusable Inner Cannula
Use the checklist below to review the steps for completion of “Tracheostomy Care.”
Stoma site should be assessed and a clean dressing applied at least once per shift. Wet or soiled dressings should be changed immediately.[79] Follow agency policy regarding cleaning the inner cannula; it should be inspected at least twice daily and cleaned as needed.
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Gather supplies: bedside table, towel, sterile gloves, pulse oximeter, PPE (i.e., mask, goggles, gown, or face shield), tracheostomy suctioning equipment, bag valve mask (should be located in the room), and a sterile tracheostomy care kit (or sterile cotton-tipped applicators, sterile manufactured tracheostomy split sponge dressing, sterile basin, normal saline, and a disposable inner cannula or a small, sterile brush to clean the reusable inner cannula).
- Perform safety steps:
- Perform hand hygiene.
- Check the room for transmission-based precautions.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain the process to the patient and ask if they have any questions.
- Be organized and systematic.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure the patient’s privacy and dignity.
- Assess ABCs.
- Raise the bed to waist level and place the patient in a semi-Fowler’s position.
- Verify that there is a backup tracheostomy kit available.
- Don appropriate PPE.
- Perform tracheal suctioning if indicated.
- Remove and discard the tracheostomy dressing. Inspect drainage on the dressing for color and amount and note any odor.
- Inspect stoma site for redness, drainage, and signs and symptoms of infection.
- Remove the gloves and perform proper hand hygiene.
- Open the sterile package and loosen the bottle cap of sterile saline.
- Don one sterile glove on the dominant hand.
- Open the sterile drape and place it on the patient’s chest.
- Set up the equipment on the sterile field.
- Remove the cap and pour saline in both basins with the ungloved hand (4"-6” above basin).
- Don the second sterile glove.
- Prepare and arrange supplies. Place pipe cleaners, trach ties, trach dressing, and forceps on the field. Moisten cotton applicators and place them in the third (empty) basin. Moisten two 4" x 4" pads in saline, wring out, open, and separately place each one in the third basin. Leave one 4" x 4" dry.
- With nondominant “contaminated” hand, remove the trach collar (if applicable) and remove (unlock and twist) the inner cannula. If the patient requires continuous supplemental oxygen, place the oxygenation device near the outer cannula or ask a staff member to assist in maintaining the oxygen supply to the patient.
- Place the inner cannula in the saline basin.
- Pick up the inner cannula with your nondominant hand, holding it only by the end usually exposed to air.
- With your dominant hand, use a brush to clean the inner cannula. Place the brush back into the saline basin.
- After cleaning, place the inner cannula in the second saline basin with your nondominant hand and agitate for approximately 10 seconds to rinse off debris. Repeat cleansing with brush as needed.
- Dry the inner cannula with the pipe cleaners and place the inner cannula back into the outer cannula. Lock it into place and pull gently to ensure it is locked appropriately. Reattach the preexisting oxygenation device.
- Clean the stoma with cotton applicators using one on the superior aspect and one on the inferior aspect.
- With your dominant, noncontaminated hand, moisten sterile gauze with sterile saline and wring out excess. Assess the stoma for infection and skin breakdown caused by flange pressure. Clean the stoma with the moistened gauze starting at the 12 o’clock position of the stoma and wipe toward the 3 o’clock position. Begin again with a new gauze square at 12 o’clock and clean toward 9 o’clock. To clean the lower half of the site, start at the 3 o’clock position and clean toward 6 o’clock; then wipe from 9 o’clock to 6 o’clock, using a clean moistened gauze square for each wipe. Continue this pattern on the surrounding skin and tube flange. Avoid using a hydrogen peroxide mixture because it can impair healing.[80]
- Use sterile gauze to dry the area.
- Apply the sterile tracheostomy split sponge dressing by only touching the outer edges.
- Replace trach ties as needed. (The literature overwhelmingly recommends a two-person technique when changing the securing device to prevent tube dislodgement. In the two-person technique, one person holds the trach tube in place while the other changes the securing device). Thread the clean tie through the opening on one side of the trach tube. Bring the tie around the back of the neck, keeping one end longer than the other. Secure the tie on the opposite side of the trach. Make sure that only one finger can be inserted under the tie.
- Remove the old tracheostomy ties.
- Remove gloves and perform proper hand hygiene.
- Provide oral care. Oral care keeps the mouth and teeth not only clean, but also has been shown to prevent hospital-acquired pneumonia.
- Lower the bed to the lowest position. If the patient is on a mechanical ventilator, the head of the bed should be maintained at 30-45 degrees to prevent ventilator-associated pneumonia.
- Assist the patient to a comfortable position, ask if they have any questions, and thank them for their time.
- Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Perform hand hygiene.
- Document the procedure and related assessment findings. Report any concerns according to agency policy.
Sample Documentation
Sample Documentation of Expected Findings
Tracheostomy care provided with sterile technique. Stoma site free of redness or drainage. Inner cannula cleaned and stoma dressing changed. Patient tolerated the procedure without difficulties.
Sample Documentation of Unexpected Findings
Tracheostomy care provided with sterile technique. Stoma site is erythematous, warm, and tender to palpation. Inner cannula cleaned and stoma dressing changed. Patient tolerated the procedure without difficulties. Dr. Smith notified of change in condition of stoma at 1315 and stated would assess the patient this afternoon.
View the following YouTube videos from Santa Fe College for more information on tracheostomy care and suctioning:
Nurses access patients' veins to collect blood (i.e., perform phlebotomy) and to administer intravenous (IV) therapy. This section will describe several methods for collecting blood, as well as review the basic concepts of IV therapy.
Blood Collection
Nurses collect blood samples from patients using several methods, including venipuncture, capillary blood sampling, and blood draws from venous access devices. Blood may also be drawn from arteries by specially trained professionals for certain laboratory testing.
Venipuncture
Venipuncture involves the process of introducing a needle into a patient’s vein to collect a blood sample or insert an IV catheter. See Figure 23.1[83] for an image of venipuncture. Blood sampling with venipuncture may be initiated by nurses, phlebotomists, or other trained personnel. Venipuncture for collection of a blood sample is an important part of data collection to assess a patient’s health status. It is commonly performed to examine hematologic and immune issues such as the body’s oxygen-carrying capacity, infection, and clotting function. It is also useful for assessing metabolic and nutrition issues such as electrolyte status and kidney functioning.
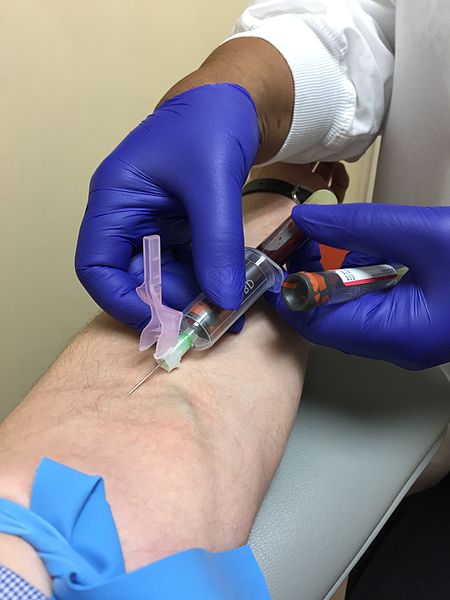
Blood collection is commonly performed via venipuncture from veins in the arms or hands. The most common sites for venipuncture are the large veins located on the antecubital fossa (i.e., the inner side of the elbow). These veins are often preferred for venipuncture because their larger size increases their ability to withstand repetitive blood sampling. However, these veins are not preferred for intravenous therapy due to the mechanical obstruction that can occur in the IV catheter when the elbow joint is contracted.
To perform the skill of venipuncture, the nurse performs many similar steps that occur with IV cannulation. The process of venipuncture for blood sample collection is outlined in the Open RN Nursing Advanced Skills "Perform Venipuncture Blood Draw" checklist.
Blood Samples From Central Venous Access Devices
Blood may also be collected by nurses from a patient's existing central venous access device (CVAD). A CVAD is a type of vascular access that involves the insertion of a catheter into a large vein in the arm, neck, chest, or groin.[84]
CVADs are discussed in more detail in the Open RN Nursing Advanced Skills "Manage Central Lines" chapter that also contains the "Obtain a Blood Sample From a CVAD" checklist.
Capillary Blood Sampling
Nurses also collect small amounts of blood for testing via capillary blood sampling. Capillary blood testing occurs when blood is collected from capillaries located near the surface of the skin. Capillaries in the fingers are used for testing in adults whereas capillaries in the heels are used for infants. An example of capillary blood testing is bedside glucose testing. See Figure 23.2[85] for an image of capillary blood glucose testing.
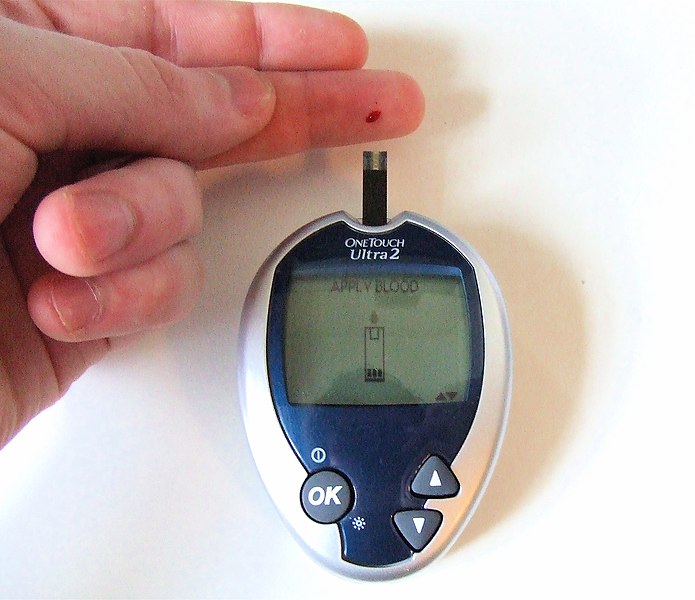
Capillary blood testing is typically used when repetitive sampling is needed. However, not all blood tests can be performed on capillary blood, and some clinical conditions make capillary blood testing inappropriate, such as when a patient is hypotensive with limited venous return.
Review how to perform capillary blood glucose testing in the "Blood Glucose Monitoring" section of the "Specimen Collection" chapter of Open RN Nursing Skills.
Arterial Blood Sampling
Arterial blood sampling occurs when blood is obtained via puncture into an artery by specially trained registered nurses and other health care personnel, such as respiratory therapists, physicians, nurse practitioners, and physician assistants. Arterial blood collection is most commonly performed to assess the body’s acid-base balance in a diagnostic test called an arterial blood gas. (For more information on arterial blood gas interpretation, please review Open RN Nursing Fundamentals Chapter 15). The most common access site for arterial blood sampling is the radial artery. See Figure 23.3[86] for an image of arterial blood sampling. Arterial blood tests are known to be more painful for the patient than venipuncture and have a higher risk of complications such as bleeding and arterial occlusion with subsequent ischemia to the area distal to the puncture.
Arterial Lines
For patients who require repetitive arterial blood sampling or are hemodynamically unstable, an arterial line may be inserted by specially trained personnel. Arterial lines are specialized tubes that are inserted and maintained in an artery to assist with continuous blood pressure monitoring. They also allow for repeated blood sampling without repetitive puncture, thus decreasing the amount of discomfort for the patient. The radial artery is the most common site used for arterial lines. Nurses must not confuse arterial lines with peripheral or central vein access devices. Arterial lines can be distinguished from venous lines by their specialized pressure tubing, which is firm and non-pliable and is connected to a pressure bag to maintain constant pressurized fluid in the tubing. Medications, fluid boluses, and maintenance IV fluids must never be infused through an arterial line. See Figure 23.3[87] for an image of arterial lines. The condition of the arterial access site, as well as perfusion of the patient's hand, is continually monitored when an arterial line is in place to prevent complications.

Intravenous Therapy
In addition to collecting blood samples, nurses also access patients' veins to administer intravenous therapy.Intravenous therapy (IV therapy) involves the administration of substances such as fluids, electrolytes, blood products, nutrition, or medications directly into a patient's vein. The intravenous route is preferred to administer fluids and medications when rapid onset of the medication or fluid is needed. The direct administration of medication into the bloodstream allows for a more rapid onset of medication actions, restoration of hydration, and correction of nutritional deficits. IV therapy is often used to restore fluids and/or resolve electrolyte imbalances more efficiently than what would be achieved via the oral route.
Fluid Balance
Fluid balance is an important part of optimal cellular functioning, and administration of fluids via the venous system provides an efficient way to quickly correct fluid imbalances. Additionally, many individuals who are physically unwell may not be able to tolerate fluids administered through their gastrointestinal tract, so IV administration is necessary. When administering IV therapy, the nurse needs to understand the nature of the solution being administered and how it will affect the patient's condition.
When patients experience deficient fluid volume, intravenous (IV) fluids are often used to restore fluid to the intravascular compartment or to facilitate the movement of fluid between compartments through the process of osmosis. There are three types of IV fluids: isotonic, hypotonic, and hypertonic.[88]
Review movement of fluid between compartments of the body in the "Basic Fluid and Electrolyte Concepts" section of the "Fluids and Electrolytes" chapter in Open RN Nursing Fundamentals.
Isotonic Solutions
Isotonic solutions are IV fluids that have a similar concentration of dissolved particles as found in the blood. Examples of isotonic IV solutions are 0.9% normal saline (0.9% NaCl) or lactated ringers (LR). Because the concentration of isotonic IV fluid is similar to the concentration of blood, the fluid stays in the intravascular space, and osmosis does not cause fluid movement between cells. See Figure 23.4[89] for an illustration of isotonic IV solution administration that does not cause osmotic movement of fluid.
Isotonic solutions are used to treat fluid volume deficit (also called hypovolemia) to replace extracellular fluid that has been lost due to bleeding, dehydration, shock, burns, trauma, and gastrointestinal tract fluid loss (such as diarrhea). IV therapy with isotonic fluids will increase a patient's blood pressure. However, infusion of too much isotonic fluid can cause excessive fluid volume (also referred to as hypervolemia) and must be used with caution in patients with hypertension, heart failure, and renal disease due to the potential for fluid overload.[90]
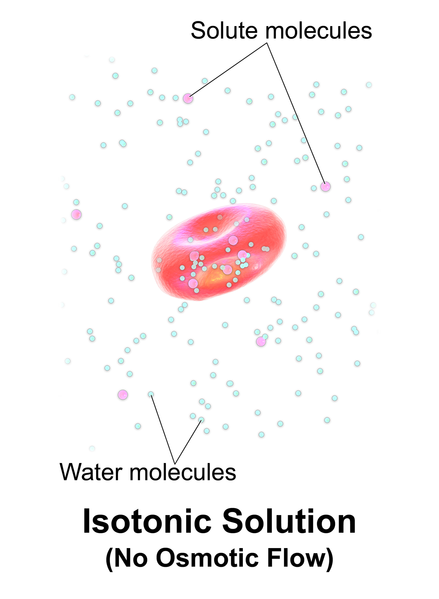
Hypotonic Solutions
Hypotonic solutions have a lower concentration of dissolved solutes than blood. An example of a hypotonic IV solution is 0.45% normal saline (0.45% NaCl). Another example of hypotonic fluid is dextrose 5% in water (D5W). D5W is isotonic in the bag but becomes hypotonic after the dextrose is rapidly metabolized by the body.
When hypotonic IV solutions are infused, it results in a decreased concentration of dissolved solutes in the blood as compared to the intracellular space. This imbalance causes osmotic movement of water from the intravascular compartment into the intracellular space. For this reason, hypotonic fluids are used to treat cellular dehydration. See Figure 23.5[91] for an illustration of the osmotic movement of fluid into a cell when a hypotonic IV solution is administered, causing lower concentration of solutes (pink molecules) in the bloodstream compared to within the cell.[92]
Hypotonic solutions are used for patients whose cells have become dehydrated, such as during diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemia, and fluids must be pushed back into the cells. However, if too much fluid moves out of the intravascular compartment into the cells, cerebral edema, worsening hypovolemia, and hypotension can occur. Therefore, patient status should be monitored carefully when hypotonic solutions are infused.[93]
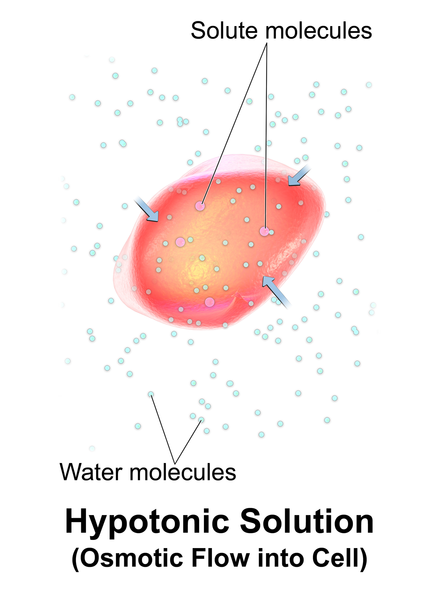
Hypertonic Solutions
Hypertonic solutions have a higher concentration of dissolved particles than blood. An example of hypertonic IV solution is 3% normal saline (3% NaCl). When infused, hypertonic fluids cause an increased concentration of dissolved solutes in the intravascular space compared to the cells. This causes the osmotic movement of water out of the cells and into the intravascular space to dilute the solutes in the blood. See Figure 23.6[94] for an illustration of osmotic movement of fluid out of a cell when hypertonic IV fluid is administered due to a higher concentration of solutes (pink molecules) in the bloodstream compared to the cell.
Hypertonic solutions move water out of the cells of the body and into the bloodstream. They are commonly used for patients with cerebral edema, severe hyponatremia, or some types of post-op patients. Hypertonic solutions must be used very cautiously due to potentially rapid side effects of fluid overload resulting in pulmonary edema, so they are typically administered in intensive care units (ICU). Hypertonic fluids should not be administered to patients with DKA because it will worsen their cellular dehydration.
When administering hypertonic fluids, it is essential to monitor for signs of fluid overload, such as significantly elevated blood pressure and difficulties breathing. Additionally, if hypertonic solutions with sodium are given, the patient's serum sodium level should be closely monitored.[95]
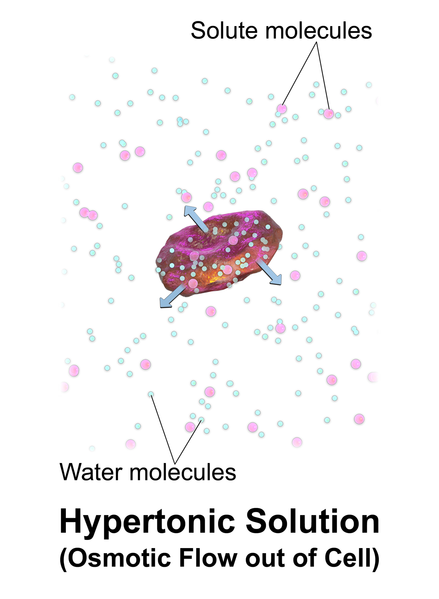
See Figure 23.7[96] for an illustration comparing how different types of IV solutions affect red blood cell size.
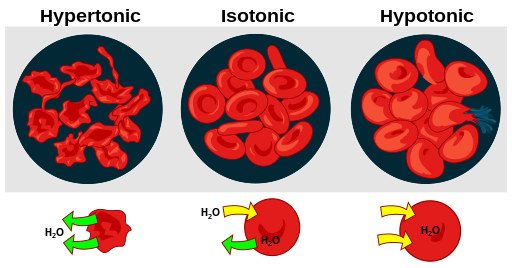
IV fluids are considered medications. As with all medications, nurses must check the rights of medication administration according to agency policy before administering IV fluids. What began as five rights of medication administration has been extended to eight rights according to the American Nurses Association. These eight rights include the following[97]:
- Right Patient
- Right Medication
- Right Dose
- Right Time
- Right Route
- Right Documentation
- Right Reason
- Right Response
Nurses also check for patient allergies, expiration date of the fluid, and compatibility of the fluid with any other fluids, medications, or blood products being administered intravenously. With any IV infusion, it is important for the nurse to pay close attention to the provider's order and make sure that it contains the specific type of fluid, any additives or medications, amount to be infused, rate of infusion, and the length of time that the therapy should continue. The nurse should also carefully assess a patient's hydration status and oral intake to ensure that IV fluids are stopped appropriately as a patent's condition changes. For example, weight should be assessed daily for patients receiving IV fluids to monitor for fluid overload.
Review how to check the rights of medication administration in the “Administration of Enteral Medications” chapter of Open RN Nursing Skills.
Electrolyte Imbalance
In addition to rapidly improving hydration status, IV fluids may also be administered to rapidly correct electrolyte imbalances. Infusing fluids with electrolytes such as potassium, calcium, and magnesium can correct electrolyte imbalances more rapidly and effectively than by oral supplementation. However, nurses must collaborate with the interprofessional team to identify medications that should and should not be given through peripheral veins. Current standards of care consider continuous peripheral infusion therapy of electrolytes to be inappropriate because of potential vascular endothelial damage. Ideally, peripheral IV therapy should be isotonic and consistent with physiological pH; otherwise, central venous access should be used.[98]
Electrolytes administered via the IV route must always be administered cautiously at the correct infusion rate because over supplementation can be deadly. For example, potassium infusions administered too rapidly into a patient's system can cause sudden cardiac arrest.
Blood Administration
Blood and blood components are administered by registered nurses via IV infusion, typically through larger sized IV catheters. Blood and blood components are transfused through a special transfusion administration set that has a filter designed to retain potentially harmful particles. Specific procedures for verifying the correct patient and correct blood product are performed prior to transfusion to prevent transfusion reactions that can be life-threatening. Administration of blood and blood components, including the use of infusion devices and ancillary equipment, and the identification, evaluation, and reporting of adverse events related to transfusion are established in agency policies, procedures, and/or practice guidelines. Read more information about blood administration in the "Administer Blood Products" chapter in Open RN Nursing Advanced Skills.
Nutrition
Nutritional therapy can be administered through an intravenous route for patients who do not have an adequately functioning gastrointestinal tract and/or are unable to take in food or fluids appropriately. Peripheral nutrition may be ordered through a peripheral IV site for nutritional needs such as albumin replacement.
Total parenteral nutrition (TPN) may be ordered for a patient based on their specific electrolyte and/or nutritional needs. TPN is a very concentrated solution that must be administered via a central line. Central lines are placed in a larger vessel rather than a smaller, peripheral vessel. Accessing a central vessel requires additional training and expertise to prevent complications with insertion and is further discussed in the Open RN Nursing Advanced Skills "Manage Central Lines” chapter. If a nurse receives an order for TPN therapy for a patient who does not have central line access, the order should be clarified with the prescribing provider.
Medications
The IV route is preferred for the administration of many medications when immediate onset is required. For example, many types of pain medications can be given directly into the bloodstream with a much more rapid onset of action than if they were to be administered orally. Rapid relief of pain can be achieved in minutes rather than hours required for oral medications to reach their peak. Rapid onset can also be achieved with other medications such as those used to treat cardiac emergencies or severe allergic reactions to quickly restore patients to optimal body functioning. Additional information about IV administration of medications is discussed in the Open RN Nursing Advanced Skills "Administer IV Push Medications” chapter.
IV Administration Equipment
Intravenous (IV) substances are administered through flexible plastic tubing called an IV administration set. The IV administration set connects the bag of solution to the patient’s IV access site. There are two major types of IV administration sets: primary administration sets and secondary administration sets. Administration sets require routine replacement to prevent infection. Follow agency policy regarding tubing changes before initiating a new bag of fluid or medications. See a summary of general guidelines for IV therapy and administration equipment in the box at the end of this section.
Primary Administration Sets
Primary administration sets can be used to infuse continuous or intermittent fluids, electrolytes, or medications. These substances may be administered by infusion pump or by gravity, and each method requires its own type of administration set.
Primary fluids are typically administered using an IV pump. An IV pump is the safest method of administration to ensure specific amounts of fluid are administered. The rate of infusion through an IV pump is typically calculated in mL/hour.
For infusion by gravity, a primary IV administration set can be a macro-drip or a micro-drip solution set. Macro-drip sets are used for routine primary infusions for adults. Micro-drip IV tubing is used in pediatric or neonatal care where small amounts of fluids are administered over a long period of time. A macro-drip infusion set delivers fluid at 10, 15, or 20 drops per milliliter, whereas a micro-drip infusion set delivers 60 drops per milliliter. The drop factor is located on the packaging of the IV tubing and is important to verify when calculating medication administration rates.
Primary IV administration sets consist of the following parts:
- Sterile spike: Used to spike the IV fluid bag and must be kept sterile.
- Roller clamp: Used to regulate the speed or stop an infusion by gravity.
- Drip chamber: Allows air to rise out from a fluid so that it is not passed onto the patient. The drip chamber should be kept ¼ to ½ full of solution. When setting a rate by gravity to "drops per minute," the dripping from this chamber is counted.
- Backcheck valve: Prevents fluid or medication from travelling up into the primary IV bag.
- Access ports: Used to infuse secondary medications and to administer IV push medications. These may also be referred to as “Y ports.”
Secondary Administration Sets
Secondary IV administration sets are used to intermittently administer a secondary medication, such as an antibiotic, while the primary IV is also running. Secondary IV tubing is shorter in length than primary tubing and is connected to a primary line via an access port above the infusion pump. The infusion pump is then set at the prescribed secondary infusion rate while the secondary medication is administered. By hanging the secondary medication bag higher than the primary bag, gravity pulls fluid from the secondary bag until it is empty rather than the primary bag.
Secondary medications may be “piggybacked” into primary infusion lines so the solution from the primary fluid line can be used to prime the secondary tubing. To prime the secondary tubing, after the secondary tubing is connected to the primary tubing, the bag connected to the secondary tubing is held lower than the primary bag, causing fluid from the primary tubing to backflow up the secondary tubing. This eliminates air from the secondary tubing.
See Figure 23.8[99] for an illustration of the setup of primary and secondary administration sets for primary administration of fluids and secondary administration of medication by gravity. See Figure 23.9[100] for an image of an IV infusion pump.
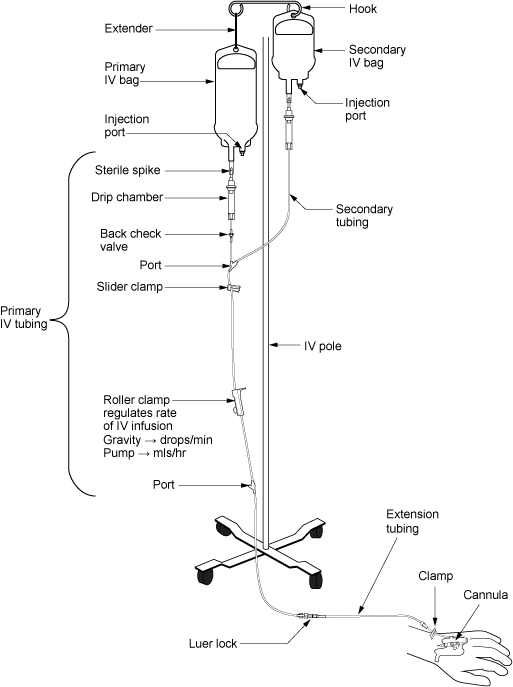

Priming IV Tubing
Primary administration sets, secondary administration sets, and extension tubing must be primed with IV solution to prevent air from entering the patient's circulatory system and causing an air embolism. Priming refers to the process of filling the IV tubing with IV solution prior to attaching it to the patient. Review steps for setting up and priming primary and secondary administration sets using the information in the following box.
Review checklists of steps for "Primary IV Solution Administration" and "Secondary IV Solution Administration" in the "IV Therapy Management" chapter of Open RN Nursing Skills.
Infection Control
Aseptic technique must be maintained throughout all IV therapy procedures, including initiation of IV access, preparing and maintaining IV equipment, administering IV fluids and medications, and discontinuing an IV system. Hand hygiene and strict aseptic technique must be performed when handling all IV equipment. These standards can be reviewed in the “Aseptic Technique” chapter. Additionally, if an IV catheter or IV administration set should become contaminated by contact with a nonsterile surface, it should be replaced with a new one to prevent introducing bacteria or other contaminants into the system.
Types of Venous Access
There are several types of venous access devices used to administer IV therapy that are categorized as peripheral devices or central devices. Venous access device selection is tailored to each patient's needs and to the type, duration, and frequency of infusion.
Peripheral Devices
Peripheral venous access devices are commonly used for short-term IV therapy in the hospital setting. A peripheral IV is an intravenous catheter inserted by percutaneous venipuncture into a peripheral vein and held in place with a sterile transparent dressing. The transparent dressing helps to keep the site sterile, prevents accidental dislodgement, and allows the nurse to visualize the insertion site through the dressing. A securement device may be added to prevent accidental dislodgement.
The patient’s upper extremities (hands and arms) are the preferred sites for insertion. However, a potential limitation of using the hand veins is they are smaller than the cephalic, basilic, or brachial veins in the arm. If the patient requires rapid infusions where a larger gauge IV is warranted, the larger veins in the upper arm should be considered.
Peripheral IVs are used for short-term infusions of fluids, medications, or blood. Peripheral IVs are easy to monitor and can be inserted at the bedside by nurses and other trained professionals. After IV access has been obtained, the hub of an intravenous catheter is attached to a short extension set or a primary IV administration set. Luer lock connectors on the extension tubing and/or administration sets permit syringes to be attached to administer medications or fluid flushes.
Saline lock refers to the use of a short extension set that allows IV access without requiring ongoing IV infusions. When not in use, the lock is flushed with saline according to agency policy and clamped to ensure the site remains sterile and blood does not flow out of the extension tubing. See Figure 23.10[101] for an image of a saline lock.

If the patient requires continuous infusion of IV fluids, the extension tubing from the IV catheter is connected to a primary IV administration set. The IV tubing can be run through an infusion pump to administer fluids or medications at a programmed rate of infusion (typically calculated in mL/hour) or via gravity by setting a drip rate with the roller clamp (typically calculated at drops/minute). Manufacturers list the drop rate on the IV packaging. Because of the risk of error that can occur with infusion by gravity, many agencies require the use of an infusion pump to ensure correct flow rate.
Contraindications to Peripheral IV Access Sites
Before inserting a peripheral IV, the patient should be assessed for contraindications related to insertion sites in the upper extremities. For example, patients who have a history of lumpectomy or mastectomy, an arteriovenous fistula, or current lymphedema often have restrictions that prohibit venipuncture into the affected extremity.[102] Additionally, deep vein thrombosis (DVT), fractures, contractures, or extensive scarring may also prohibit the placement of a peripheral IV. Hospitalized patients may have signage or a bracelet stating "limb alert" to alert heath care professionals to these conditions.
Midline Peripheral Catheters
Midline peripheral catheters have a larger catheter (i.e., 16-18 gauge) that allows for rapid infusions. Insertion is ultrasound-guided and can be inserted by RNs with additional training or other trained professionals. Midline catheters are typically inserted into the basilic, cephalic, or brachial veins of the upper arm with the tip placed near the level of the axilla. They are much longer and inserted deeper than a peripheral IV, but do not extend into a central vessel, so they are not considered a central line. Therefore, they have a lower risk of infection than central venous access. Any medication that can be administered through a peripheral line can be administered via a midline peripheral catheter. They can also be used for longer duration than traditional peripheral venous access, which is ideal for patients needing extended hospital stays or IV access. Based on agency policy, midline catheters may also be used for blood sample collection, thus limiting the number of venipunctures a patient receives. Site care for a midline peripheral catheter is similar to a peripheral IV dressing change.[103],[104]
Central Venous Access Devices
A central venous access device (CVAD) is a type of vascular access established by specially trained registered nurses and other health care personnel. It involves the insertion of a tube into a vein in the neck, chest, or groin and threaded into a central vein (most commonly the internal jugular, subclavian, or femoral) and advanced until the tip of the catheter resides within the inferior vena cava, superior vena cava, or right atrium.[105] Only specially trained health professionals may insert central venous access devices, but nurses provide routine care of CVADs, including dressing changes. See Figure 23.11[106] for an image of a central line requiring a dressing change.

A central venous access device can be left in for longer periods of time and is useful for administering concentrated medications and fluids, such as TPN or hyperosmotic fluids, that would be otherwise irritating to smaller peripheral veins. However, central venous access devices have an increased risk for the development of bloodstream infections, so strict sterile technique is required during insertion, and aseptic technique is used for maintenance. Central venous access devices are further discussed in the "Manage Central Lines" chapter of Open RN Nursing Advanced Skills.
Peripheral Inserted Central Catheters
A peripheral inserted central catheter (PICC) is a thin, flexible tube inserted into a vein in the upper arm and guided into the superior vena cava. It is used to give intravenous fluids, blood transfusions, chemotherapy, and other medications requiring a central line. It can also be used for blood sampling. A PICC may stay in place for weeks or months and helps avoid the need for repeated needlesticks. PICC lines are further discussed in the "Manage Central Lines" chapter of Open RN Nursing Advanced Skills.
General Guidelines for IV Therapy
The following are general guidelines for peripheral IV therapy[107]:
- IV fluid therapy is ordered by a provider. The order must include the type of solution or medication, total amount of fluid, rate of infusion, duration, date, and time.
- IV therapy is an invasive procedure. Significant complications can occur if the wrong amount of IV fluids or incorrect medication is given or if aseptic technique is not strictly followed.
- Nurses must understand the indications and duration for IV therapy for each patient. Practice guidelines recommend that patients receiving IV therapy for more than six days should be assessed for an intermediate or long-term device such as a central venous access device (CVAD).
- Hospitalized patients may have an order for a small hourly infusion rate, such as 10-20 mL/hour, historically referred to in practice as a "to keep open" (TKO) or "keep vein open" (KVO) rate.
- IV administration sets require routine replacement to promote patient safety and reduce the risk of infection. Primary and secondary continuous administration sets used to administer solutions other than lipids, blood, or blood products are typically changed every 96 hours, or up to every 7 days, as directed by agency policy and/or the manufacturer’s instructions. Administration sets should also be changed if contamination or compromise in the integrity of the product or system is suspected. Secondary administration sets that are detached from a primary administration set are typically changed every 24 hours or as directed by agency policy. Administration sets should be labelled according to agency policy with the date of initiation or the date of change indicated.[108]
To prepare for intravenous therapy administration, the nurse should collect important subjective and objective assessment information from the patient.
Subjective Assessment
When performing the subjective assessment, the nurse should begin by focusing on data collection that may signify a potential complication if a patient receives IV infusion therapy. The nurse should begin by identifying if the patient has medication allergies or a latex allergy. The patient’s history should also be considered with special attention given to those with known congestive heart failure (CHF) or chronic kidney disease (CKD) because they are more susceptible to developing fluid overload. Additionally, the patient should be asked if they have any pain or discomfort in their IV access site now or during the infusion of medications or fluids.
Life Span Considerations
The needs and characteristics of special patient populations, including physiologic, developmental, communication/cognitive ability, and/or safety requirements, are identified and addressed in the planning, insertion, removal, care, management, and monitoring of vascular access devices (VADs) and with administration of infusion therapy.[109]
Children
Safety measures for a child with an IV infusion include assessing the IV site every hour for patency. Infused volumes and signs of fluid overload should be carefully assessed and documented frequently per agency policy.
Joint stabilization may be applied to deter the child from tampering with the IV site or tubing. However, it should be applied in a manner that permits visual inspection and assessment of the vascular access site and the vascular pathway, and it does not exert pressure that will cause circulatory constriction, pressure injury, or nerve damage in the area of flexion or under the device. Additionally, it should be removed periodically for assessment of circulatory status, range of motion and function, and skin integrity. Wooden tongue depressors should not be used as joint stabilization devices in preterm infants or immunocompromised individuals due to the risk of a fungal infection.[110]
Additionally, the tubing should be well-secured, and the dressing should remain free from moisture so the IV site is not compromised. Be aware that mobile children will require guidance to ensure that the tubing is not obstructed if they sit or lie on the tubing accidentally.
Older Adults
Nurses must recognize physiologic changes associated with the aging process and its effect on immunity, drug dosage and volume limitations, pharmacologic actions, interactions, side effects, monitoring parameters, and response to infusion therapy. Anatomical changes, including loss of thickness of the dermal skin layer, thickening of the tunica intima/media, and loss of connective tissue, contribute to vein fragility and present challenges in vascular access. Nurses must assess for any changes in cognitive abilities, dexterity, and the ability to communicate or learn (e.g., changes in vision, hearing, speech) that impact IV therapy.[111]
Older adults with an IV infusion should be frequently monitored for the development of fluid volume overload. Signs of fluid volume overload include elevated blood pressure and respiratory rate, decreased oxygen saturation, peripheral edema, fine crackles in the posterior lower lobes of the lungs, or signs of worsening heart failure. Additionally, older adults have delicate venous walls that may not withstand rapid infusion rates. It is important to monitor the IV site patency carefully when infusing large amounts of fluids at faster rates and appropriately modify the infusion rate.
Objective Assessment
Follow agency policy and procedures regarding IV therapy assessment and documentation. Current infusion standards indicate the venous access device site, the entire infusion system, and the patient should be assessed for signs of complications at a frequency dependent on a variety of factors, including the patient's age, condition, and cognition; the type and frequency of the intravenous fluid/medication; and the health care setting. In inpatient and nursing facilities, peripherally inserted IVs should be assessed at least every 4 hours with increased frequency of assessment every 1 to 2 hours for patients who are critically ill, sedated, or have cognitive deficits, and hourly for neonatal/pediatric patients and patients receiving infusions of vesicant medications.[112]
The entire IV infusion system, from the patient's IV insertion site and dressing to the IV solution container, is routinely assessed by the nurse for system integrity, infusion accuracy, identification of complications, and expiration dates throughout the course of treatment. The IV site should be free of redness, pallor, swelling, coolness, or warmth to the touch and the IV infusion should flow freely.[113]
The nurse should also be aware of different types of intravenous access that may be used for an infusion. For example, a peripherally inserted central catheter (PICC) looks similar to intravenous access but requires different assessment and monitoring as a central line. Please review Table 23.3 to consider the expected and unexpected assessment findings that may occur with peripheral IV therapy.
Table 23.3 Expected Versus Unexpected Findings With IV Therapy
| Assessment | Expected Findings | Unexpected Findings (document and notify provider if a new finding*) |
|---|---|---|
| Inspection | IV site free of redness, swelling, tenderness, coolness, or warmth to touch | IV site with redness, swelling, tenderness, coolness, or warmth to the touch |
| Patency | IV fluid flows freely | IV fluid does not flow; patient reports pain during flush |
| *CRITICAL CONDITIONS to report immediately | Notify the HCP if there is redness, warmth, or blisters at the site |
Sample Documentation of Expected Findings
Initiated IV infusion of normal saline at 125 mL/hr using existing 22-gauge IV catheter located in the right hand. The IV site is free from pain, coolness, redness, or swelling.
Sample Documentation of Unexpected Findings
Attempted to initiate IV infusion in right hand with existing 22-gauge IV catheter. IV site free from pain, redness, or signs of infiltration. IV site flushed readily with normal saline. Normal saline IV fluids connected at 200 mL/hour with immediate leaking around infusion site. Swelling noted superior to infusion site. Fluids stopped immediately.
Use the checklist below to review the steps for completion of “Primary IV Solution Administration.” Review the steps to safely administer all types of medication in the "Checklist for Oral Medication Administration" in the "Administration of Enteral Medications" chapter.
View an instructor demonstration of Primary IV Solution Administration[114]:
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Gather supplies: IV fluid, primary tubing, tubing change label, and alcohol pads/scrub hubs.
- Verify the provider order with the medication administration record (eMAR/MAR).
- Perform the first check of the six rights of medication administration while withdrawing the IV fluids from the medication dispensing unit. Check expiration date and verify patient allergies.
- Remove the IV solution from the packaging and gently apply pressure to the bag while inspecting for tears or leaks.
- Check the color and clarity of the solution.
- Perform the second check of the six rights of medication administration.
- Perform safety steps:
- Perform hand hygiene.
- Check the room for transmission-based precautions.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain the process to the patient and ask if they have any questions.
- Be organized and systematic.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure the patient’s privacy and dignity.
- Assess ABCs (airway, breathing, and circulation).
- Perform the third check of the rights of medication administration at the patient's bedside.
- Remove the primary IV tubing from the packaging. If administering IV fluid by gravity, note the drip factor on the package and calculate drops/min. Perform the necessary calculations for the infusion rate.
- Move the roller clamp so that it is halfway up the tubing and clamp it.
- Remove the cover from the tubing port on the bag of IV fluid.
- Remove the cap from the insertion spike on the tubing. While maintaining sterility, insert the spike into the tubing port of the bag of IV fluid.
- Squeeze the drip chamber two or three times to fill the chamber halfway.
- Loosen the cap from the end of the IV tubing and open the clamp to prime the tubing over the sink:
- If using multiple port tubing, invert the ports to prime them and to prevent air accumulation in line.
- If the solution is an antibiotic, take care to not waste solution while priming the tubing to ensure the patient receives the correct dosage.
- Once primed, clamp the IV tubing and check the entire length of the tubing for air bubbles. Tap the tubing gently to remove any air.
- Replace or tighten the cap on the end of the tubing.
- Label the primary IV fluid bag with the date and time. Place the tubing label on the tubing near the drip chamber.
- Assess the patient’s venipuncture site for signs and symptoms of vein irritation or infiltration. Do not proceed with administering fluids at this site if there are any concerns.
- Based on agency policy, vigorously cleanse the catheter cap on the patient's IV port with an alcohol pad/scrub hub (or the agency required cleansing agent) for at least fifteen seconds and allow it to dry.[115]
- Assess IV site patency according to agency policy. Purge a prefilled normal saline syringe of air. Attach the syringe onto the saline lock cap. Undo the clamp on the extension tubing. Inject 3 to 5 mL of normal saline using a turbulent stop-start technique. If resistance is felt, do not force the flush and do not proceed with IV solution administration; follow up according to agency policy.
- Remove the syringe from the IV cap and then clamp the extension tubing.
- Vigorously cleanse the catheter cap on the patient's IV port with an alcohol pad/scrub hub (or the agency required cleansing agent) for at least five seconds and allow it to dry.
- Remove the protective cap from the end of the primary tubing and attach it to the IV port while maintaining sterility.
- Move the slide clamp on the saline lock to open the tubing.
- Set the infusion rate based on the provider order:
- For infusion pump: Set volume to be infused and rate (mL/hr) to be administered.
- For gravity: Calculate drop per minute.
- Assess the patient’s IV site for signs and symptoms of vein irritation or infiltration after infusion begins.
- Secure the tubing to the patient’s arm.
- Assist the patient to a comfortable position, ask if they have any questions, and thank them for their time.
- Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Perform hand hygiene.
- Document the procedure and related assessment findings. Report any concerns according to agency policy. Include IV fluids on patient's input/output documentation.
Use the checklist below to review the steps for completion of “Secondary IV Solution Administration.” This checklist is used when fluids are already being administered via the primary IV tubing and a second IV solution is administered.
View an instructor demonstration of Secondary IV Solution Administration[116]:
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Gather supplies: secondary IV fluid/medication, secondary IV tubing, alcohol wipe/scrub hubs, and tubing labels.
- Verify the provider order with the medication administration record (eMAR/MAR).
- Perform the first check of the rights of medication administration while withdrawing the IV solution and tubing from the medication dispensing unit. Check expiration dates on the fluid and the tubing and verify allergies.
- Verify compatibility of the secondary IV solution with the other IV fluids the patient is currently receiving.
- Remove the IV solution from the packaging and gently apply pressure to the bag while inspecting for tears or leaks. Check the color and clarity of the solution.
- Perform the second check of the rights of medication administration.
- Perform safety steps:
- Perform hand hygiene.
- Check the room for transmission-based precautions.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain the process to the patient and ask if they have any questions.
- Be organized and systematic.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure the patient’s privacy and dignity.
- Assess ABCs (airway, breathing, circulation).
- Perform the third check of the rights of medication administration at the patient's bedside.
- If the patient is receiving the medication for the first time, teach the patient and family (if appropriate) about the potential adverse reactions and other concerns related to the medication.
- Remove the secondary IV tubing from the packaging.
- Place the roller clamp to the “off” position.
- Remove the protective sheath from the IV spike and the cover from the tubing port of the IV solution.
- Insert the spike into the IV bag while maintaining sterility.
- Prime the secondary IV tubing. Back priming is considered best practice and is performed using an infusion pump or gravity with primary fluids attached:
- Vigorously cleanse the Y port closest to the drip chamber with an alcohol pad/scrub hub (or the agency required cleansing agent) for at least five seconds and allow it to dry.
- Connect the secondary tubing to the port closest to the drip chamber. Lower the secondary bag below the primary bag and allow the fluid from the primary bag to fill the secondary tubing. Fill the secondary tubing until it reaches the drip chamber, and then raise the secondary bag above the primary line.
- Hang the secondary IV solution on the IV pole with the primary bag lower than the secondary bag.
- Label the secondary tubing near the drip chamber.
- Set the infusion rate:
- For infusion pump: Set the volume to be infused and the rate (mL/hr) to be administered based on the provider order.
- For gravity: The roller clamp on the secondary tubing will be opened completely, and the roller clamp on the primary tubing will be adjusted to deliver the prescribed rate.
 Take time to watch the IV fluid or medication to drip into the drip chamber to ensure the medication or fluid is flowing to the patient.
Take time to watch the IV fluid or medication to drip into the drip chamber to ensure the medication or fluid is flowing to the patient. - Assess the patient’s IV site for signs and symptoms of vein irritation or infiltration after infusion begins. Do not proceed with administering secondary fluids if there are any concerns about the site.
- Assist the patient to a comfortable position, ask if they have any questions, and thank them for their time.
- Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Perform hand hygiene.
- Document the procedure and assessment findings. Report any concerns according to agency policy.
Sample Documentation of Expected Findings
IV catheter on right hand discontinued with catheter tip intact. Site free from redness, warmth, tenderness, or swelling. Gauze applied with pressure for one minute with no bleeding noted. Dressing applied to site.
Sample Documentation of Unexpected Findings
IV catheter on right hand discontinued with IV catheter tip intact. Site free from redness, warmth, tenderness, or swelling. Gauze applied with pressure for one minute. Bleeding noted to continue around gauze dressing. Pressure held for five minutes, and hemostasis achieved. Dressing applied to site.
Use the checklist below to review the steps for completion of “Discontinuing an IV.”
View an instructor demonstration of IV Removal[117]:
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Gather supplies: gauze, tape, or a Band-Aid.
- Perform safety steps:
- Perform hand hygiene.
- Check the room for transmission-based precautions.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain the process to the patient.
- Be organized and systematic.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure the patient’s privacy and dignity.
- Assess ABCs (airway, breathing, circulation).
- Prepare the gauze and tape.
- Place the IV clamp to the “off” position (clamped).
- Perform hand hygiene and apply gloves.
- Loosen the edges of the transparent dressing and tape in the direction of the IV site.
- Place a gauze pad over the IV site and gently pull the IV out parallel to the skin in a slow and steady motion.
- Hold pressure on the IV site for 2-3 minutes. If the patient is on anticoagulant medication, you may need to hold for 5-10 minutes.
- Inspect the catheter to ensure it is intact and dispose of it in an appropriate container.
- Remove the gauze pad once bleeding has stopped and assess for any signs of infection at the site, such as redness, swelling, warmth, tenderness, or purulent drainage.
- Tape the gauze or apply a Band-Aid over the IV site.
- Remove gloves and perform hand hygiene.
- Assist the patient to a comfortable position, ask if they have any questions, and thank them for their time.
- Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Perform hand hygiene.
- Document the procedure and related assessment findings. Report any concerns according to agency policy.
View a supplementary YouTube video on Spiking and Priming an IV Bag[118]:
Learning Activities
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
The patient's IV site is cool to the touch and swollen. The patient states, “It hurts a little.” List in order the steps the nurse should take.
- Discontinue the IV
- Stop the IV infusion
- Elevate the affected site
- Document the findings
![]()
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 23, Assignment 1.
![]()
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 23, Assignment 2.
![]()
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 23, Assignment 3.
Answer Key to Chapter 1 Learning Activities
1. D - Patient is experiencing increased difficulty breathing. (Rationale: The severity of an airway concern and the life-threatening nature of the condition necessitates immediate notification of the provider).
Answers to interactive elements are given within the interactive element.
Collection of blood.
With an understanding of the basic structures and primary functions of the respiratory system, the nurse collects subjective and objective data to perform a focused respiratory assessment.
Subjective Assessment
Collect data using interview questions, paying particular attention to what the patient is reporting. The interview should include questions regarding any current and past history of respiratory health conditions or illnesses, medications, and reported symptoms. Consider the patient’s age, gender, family history, race, culture, environmental factors, and current health practices when gathering subjective data. The information discovered during the interview process guides the physical exam and subsequent patient education. See Table 10.3a for sample interview questions to use during a focused respiratory assessment.[119]
Table 10.3a Interview Questions for Subjective Assessment of the Respiratory System
| Interview Questions | Follow-up |
|---|---|
| Have you ever been diagnosed with a respiratory condition, such as asthma, COPD, pneumonia, or allergies?
Do you use oxygen or peak flow meter? Do you use home respiratory equipment like CPAP, BiPAP, or nebulizer devices? |
Please describe the conditions and treatments. |
| Are you currently taking any medications, herbs, or supplements for respiratory concerns? | Please identify what you are taking and the purpose of each. |
| Have you had any feelings of breathlessness
(dyspnea)? |
Note: If the shortness of breath is severe or associated with chest pain, discontinue the interview and obtain emergency assistance.
Are you having any shortness of breath now? If yes, please rate the shortness of breath from 0-10 with "0" being none and "10" being severe? Does anything bring on the shortness of breath (such as activity, animals, food, or dust)? If activity causes the shortness of breath, how much exertion is required to bring on the shortness of breath? When did the shortness of breath start? Is the shortness of breath associated with chest pain or discomfort? How long does the shortness of breath last? What makes the shortness of breath go away? Is the shortness of breath related to a position, like lying down? Do you sleep in a recliner or upright in bed? Do you wake up at night feeling short of breath? How many pillows do you sleep on? How does the shortness of breath affect your daily activities? |
| Do you have a cough? | When you cough, do you bring up anything? What color is the phlegm?
Do you cough up any blood (hemoptysis)? Do you have any associated symptoms with the cough such as fever, chills, or night sweats? How long have you had the cough? Does anything bring on the cough (such as activity, dust, animals, or change in position)? What have you used to treat the cough? Has it been effective? |
| Do you smoke or vape? | What products do you smoke/vape? If cigarettes are smoked, how many packs a day do you smoke?
How long have you smoked/vaped? Have you ever tried to quit smoking/vaping? What strategies gave you the best success? Are you interested in quitting smoking/vaping? If the patient is ready to quit, the five successful interventions are the "5 A's": Ask, Advise, Assess, Assist, and Arrange. Ask - Identify and document smoking status for every patient at every visit. Advise - In a clear, strong, and personalized manner, urge every user to quit. Assess - Is the user willing to make a quitting attempt at this time? Assist - For the patient willing to make a quitting attempt, use counseling and pharmacotherapy to help them quit. Arrange - Schedule follow-up contact, in person or by telephone, preferably within the first week after the quit date.[120] |
Life Span Considerations
Depending on the age and capability of the child, subjective data may also need to be retrieved from a parent and/or legal guardian.
Pediatric
- Is your child up-to-date with recommended immunizations?
- Is your child experiencing any cold symptoms (such as runny nose, cough, or nasal congestion)?
- How is your child’s appetite? Is there any decrease or change recently in appetite or wet diapers?
- Does your child have any hospitalization history related to respiratory illness?
- Did your child have any history of frequent ear infections as an infant?
Older Adult
- Have you noticed a change in your breathing?
- Do you get short of breath with activities that you did not before?
- Can you describe your energy level? Is there any change from previous?
Objective Assessment
A focused respiratory objective assessment includes interpretation of vital signs; inspection of the patient’s breathing pattern, skin color, and respiratory status; palpation to identify abnormalities; and auscultation of lung sounds using a stethoscope. For more information regarding interpreting vital signs, see the “General Survey” chapter. The nurse must have an understanding of what is expected for the patient’s age, gender, development, race, culture, environmental factors, and current health condition to determine the meaning of the data that is being collected.
Evaluate Vital Signs
The vital signs may be taken by the nurse or delegated to unlicensed assistive personnel such as a nursing assistant or medical assistant. Evaluate the respiratory rate and pulse oximetry readings to verify the patient is stable before proceeding with the physical exam. The normal range of a respiratory rate for an adult is 12-20 breaths per minute at rest, and the normal range for oxygen saturation of the blood is 94–98% (SpO₂).[121] Bradypnea is less than 12 breaths per minute, and tachypnea is greater than 20 breaths per minute.
Inspection
Inspection during a focused respiratory assessment includes observation of level of consciousness, breathing rate, pattern and effort, skin color, chest configuration, and symmetry of expansion.
- Assess the level of consciousness. The patient should be alert and cooperative. Hypoxemia (low blood levels of oxygen) or hypercapnia (high blood levels of carbon dioxide) can cause a decreased level of consciousness, irritability, anxiousness, restlessness, or confusion.
- Obtain the respiratory rate over a full minute. The normal range for the respiratory rate of an adult is 12-20 breaths per minute.
- Observe the breathing pattern, including the rhythm, effort, and use of accessory muscles. Breathing effort should be nonlabored and in a regular rhythm. Observe the depth of respiration and note if the respiration is shallow or deep. Pursed-lip breathing, nasal flaring, audible breathing, intercostal retractions, anxiety, and use of accessory muscles are signs of respiratory difficulty. Inspiration should last half as long as expiration unless the patient is active, in which case the inspiration-expiration ratio increases to 1:1.
- Observe the pattern of expiration and patient position. Patients who experience difficulty expelling air, such as those with emphysema, may have prolonged expiration cycles. Some patients may experience difficulty with breathing specifically when lying down. This symptom is known as orthopnea. Additionally, patients who are experiencing significant breathing difficulty may experience most relief while in a “tripod” position. This can be achieved by having the patient sit at the side of the bed with legs dangling toward the floor. The patient can then rest their arms on an overbed table to allow for maximum lung expansion. This position mimics the same position you might take at the end of running a race when you lean over and place your hands on your knees to “catch your breath.”
- Observe the patient’s color in their lips, face, hands, and feet. Patients with light skin tones should be pink in color. For those with darker skin tones, assess for pallor on the palms, conjunctivae, or inner aspect of the lower lip. Cyanosis is a bluish discoloration of the skin, lips, and nail beds, which may indicate decreased perfusion and oxygenation. Pallor is the loss of color, or paleness of the skin or mucous membranes and usually the result of reduced blood flow, oxygenation, or decreased number of red blood cells.
- Inspect the chest for symmetry and configuration. The trachea should be midline, and the clavicles should be symmetrical. See Figure 10.2[122] for visual landmarks when inspecting the thorax anteriorly, posteriorly, and laterally. Note the location of the ribs, sternum, clavicle, and scapula, as well as the underlying lobes of the lungs.
- Chest movement should be symmetrical on inspiration and expiration.
- Observe the anterior-posterior diameter of the patient’s chest and compare to the transverse diameter. The expected anteroposterior-transverse ratio should be 1:2. A patient with a 1:1 ratio is described as barrel-chested. This ratio is often seen in patients with chronic obstructive pulmonary disease due to hyperinflation of the lungs. See Figure 10.3[123] for an image of a patient with a barrel chest.
- Older patients may have changes in their anatomy, such as kyphosis, an outward curvature of the spine.
- Inspect the fingers for clubbing if the patient has a history of chronic respiratory disease. Clubbing is a bulbous enlargement of the tips of the fingers due to chronic hypoxia. See Figure 10.4[124] for an image of clubbing.
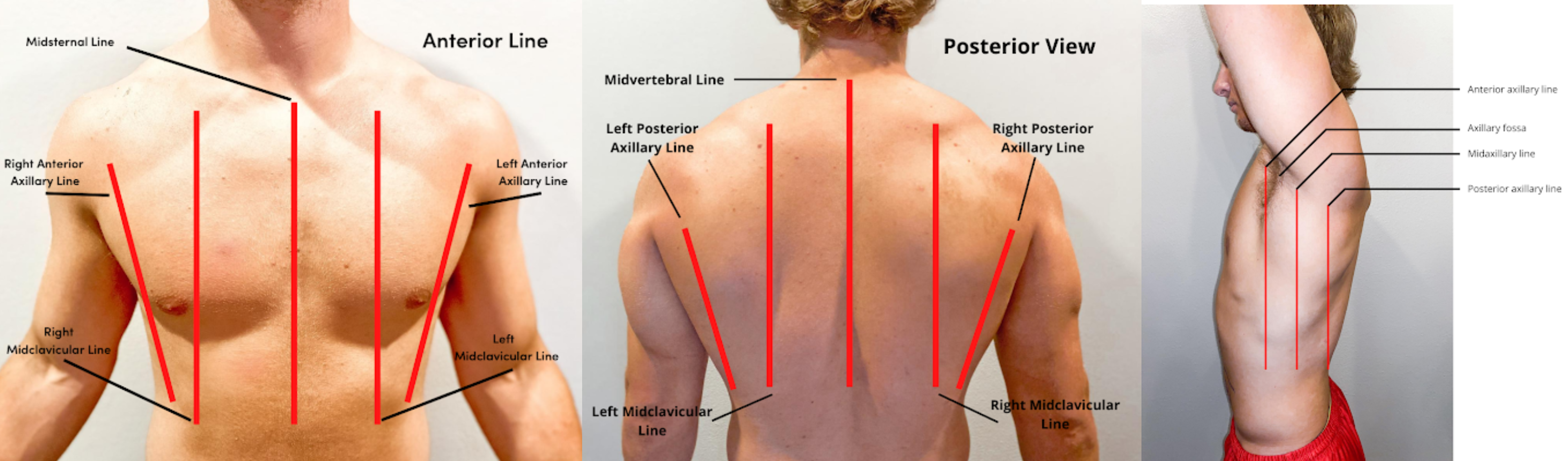


Palpation
- Palpation of the chest may be performed to investigate for areas of abnormality related to injury or procedural complications. For example, if a patient has a chest tube or has recently had one removed, the nurse may palpate near the tube insertion site to assess for areas of air leak or crepitus. Crepitus feels like a popping or crackling sensation when the skin is palpated and is a sign of air trapped under the subcutaneous tissues. If palpating the chest, use light pressure with the fingertips to examine the anterior and posterior chest wall. Chest palpation may be performed to assess specifically for growths, masses, crepitus, pain, or tenderness.
- Confirm symmetric chest expansion by placing your hands on the anterior or posterior chest at the same level, with thumbs over the sternum anteriorly or the spine posteriorly. As the patient inhales, your thumbs should move apart symmetrically. Unequal expansion can occur with pneumonia, thoracic trauma, such as fractured ribs, or pneumothorax.
Auscultation
Using the diaphragm of the stethoscope, listen to the movement of air through the airways during inspiration and expiration. Instruct the patient to take deep breaths through their mouth. Listen through the entire respiratory cycle because different sounds may be heard on inspiration and expiration. Allow the patient to rest between respiratory cycles, if needed, to avoid fatigue with deep breathing during auscultation. As you move across the different lung fields, the sounds produced by airflow vary depending on the area you are auscultating because the size of the airways change.
Correct placement of the stethoscope during auscultation of lung sounds is important to obtain a quality assessment. The stethoscope should not be placed over clothes or hair because these may create inaccurate sounds from friction. The best position to listen to lung sounds is with the patient sitting upright; however, if the patient is acutely ill or unable to sit upright, turn them side to side in a lying position. Avoid listening over bones, such as the scapulae or clavicles or over the female breasts to ensure you are hearing adequate sound transmission. Listen to sounds from side to side rather than down one side and then down the other side. This side-to-side pattern allows you to compare sounds in symmetrical lung fields. See Figures 10.5[125] and 10.6[126] for landmarks of stethoscope placement over the anterior and posterior chest wall.
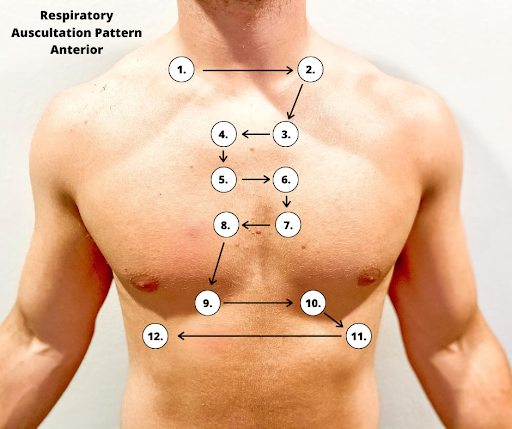
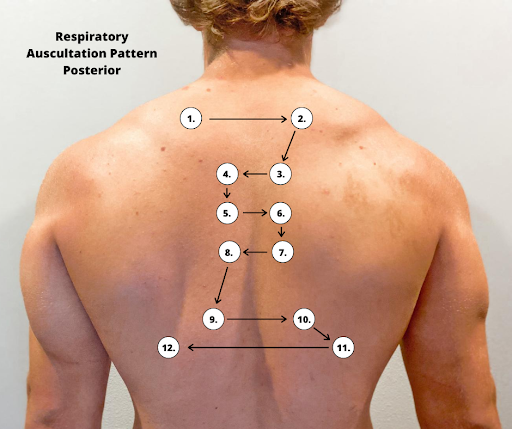
Expected Breath Sounds
It is important upon auscultation to have awareness of expected breath sounds in various anatomical locations.
- Bronchial breath sounds are heard over the trachea and larynx and are high-pitched and loud.
- Bronchovesicular sounds are medium-pitched and heard over the major bronchi.
- Vesicular breath sounds are heard over the lung surfaces, are lower-pitched, and often described as soft, rustling sounds.
Adventitious Lung Sounds
Adventitious lung sounds are sounds heard in addition to normal breath sounds. They most often indicate an airway problem or disease, such as accumulation of mucus or fluids in the airways, obstruction, inflammation, or infection. These sounds include rales/crackles, rhonchi/wheezes, stridor, and pleural rub:
- Coarse crackles, also called rhonchi, are low-pitched, loud, continuous sounds frequently heard on expiration. They are a sign of turbulent airflow through secretions in the large airways.
Rhonchi Lung Sounds on YouTube [127]
- Fine crackles, also called rales, are popping or crackling sounds heard on inspiration. They occur in association with conditions that cause fluid to accumulate within the alveolar and interstitial spaces, such as heart failure or pneumonia. Fine crackles are soft, high-pitched, and very brief. For this reason, it is essential to listen to lung sounds with the stethoscope placed on the patient's skin and not over their clothing or hospital gown. The sound is similar to that produced by rubbing strands of hair together close to your ear.
- Wheezes are whistling-type noises produced during expiration (and sometimes inspiration) when air is forced through airways narrowed by bronchoconstriction or associated mucosal edema. For example, patients with asthma commonly have wheezing.
- Stridor is heard only on inspiration. It is associated with mechanical obstruction at the level of the trachea/upper airway.
- Pleural rub may be heard on either inspiration or expiration and sounds like the rubbing together of leather. A pleural rub is heard when there is inflammation of the lung pleura, resulting in friction as the surfaces rub against each other.[128]
Life Span Considerations
Children
There are various respiratory assessment considerations that should be noted with assessment of children.
- The respiratory rate in children less than 12 months of age can range from 30-60 breaths per minute, depending on whether the infant is asleep or active.
- Infants have irregular or periodic newborn breathing in the first few weeks of life; therefore, it is important to count the respirations for a full minute. During this time, you may notice periods of apnea lasting up to 10 seconds. This is not abnormal unless the infant is showing other signs of distress. Signs of respiratory distress in infants and children include nasal flaring and sternal or intercostal retractions.
- Up to three months of age, infants are considered “obligate” nose-breathers, meaning their breathing is primarily through the nose.
- The anteroposterior-transverse ratio is typically 1:1 until the thoracic muscles are fully developed around six years of age.
Older Adults
As the adult person ages, the cartilage and muscle support of the thorax becomes weakened and less flexible, resulting in a decrease in chest expansion. Older adults may also have weakened respiratory muscles, and breathing may become shallower. The anteroposterior-transverse ratio may be 1:1 if there is significant curvature of the spine (kyphosis).
Percussion
Percussion is an advanced respiratory assessment technique that is used by advanced practice nurses and other health care providers to gather additional data in the underlying lung tissue. By striking the fingers of one hand over the fingers of the other hand, a sound is produced over the lung fields that helps determine if fluid is present. Dull sounds are heard with high-density areas, such as pneumonia or atelectasis, whereas clear, low-pitched, hollow sounds are heard in normal lung tissue.
![]()
- Because infants breathe primarily through the nose, nasal congestion can limit the amount of air getting into the lungs.
- Attempt to assess an infant’s respiratory rate while the infant is at rest and content rather than when the infant is crying. Counting respirations by observing abdominal breathing movements may be easier for the novice nurse than counting breath sounds, as it can be difficult to differentiate lung and heart sounds when auscultating newborns.
- Auscultation of lungs during crying is not a problem. It will enhance breath sounds.
- The older patient may have a weakening of muscles that support respiration and breathing. Therefore, the patient may report tiring easily during the assessment when taking deep breaths. Break up the assessment by listening to the anterior lung sounds and then the heart sounds and allowing the patient to rest before listening to the posterior lung sounds.
- Patients with end-stage COPD may have diminished lung sounds due to decreased air movement. This abnormal assessment finding may be the patient’s baseline or normal and might also include wheezes and fine crackles as a result of chronic excess secretions and/or bronchoconstriction.[129],[130]
Expected Versus Unexpected Findings
See Table 10.3b for a comparison of expected versus unexpected findings when assessing the respiratory system.[131]
Table 10.3b Expected Versus Unexpected Respiratory Assessment Findings
| Assessment | Expected Findings | Unexpected Findings (Document and notify provider if a new finding*) |
|---|---|---|
| Inspection | Work of breathing effortless
Regular breathing pattern Respiratory rate within normal range for age Chest expansion symmetrical Absence of cyanosis or pallor Absence of accessory muscle use, retractions, and/or nasal flaring Anteroposterior: transverse diameter ratio 1:2 |
Labored breathing
Irregular rhythm Increased or decreased respiratory rate Accessory muscle use, pursed-lip breathing, nasal flaring (infants), and/or retractions Presence of cyanosis or pallor Asymmetrical chest expansion Clubbing of fingernails |
| Palpation | No pain or tenderness with palpation. Skin warm and dry; no crepitus or masses | Pain or tenderness with palpation, crepitus, palpable masses, or lumps |
| Percussion | Clear, low-pitched, hollow sound in normal lung tissue | Dull sounds heard with high-density areas, such as pneumonia or atelectasis |
| Auscultation | Bronchovesicular and vesicular sounds heard over appropriate areas
Absence of adventitious lung sounds |
Diminished lung sounds
Adventitious lung sounds, such as fine crackles/rales, wheezing, stridor, or pleural rub |
| *CRITICAL CONDITIONS to report immediately | Decreased oxygen saturation <92%[132]
Pain Worsening dyspnea Decreased level of consciousness, restlessness, anxiousness, and/or irritability |
Answer Key to Chapter 3 Learning Activities
1. To safely obtain an individual's blood pressure, it is important to note the size of the patient to select the appropriate blood pressure cuff size. Additionally, it is important to note if the patient has any limb restrictions, such as an injury, mastectomy, lymph node removal, fistula placement, etc. Blood pressures should not be taken on any limb with a potential restriction.
Answers to interactive elements are given within the interactive element.

