9. QSEN: Advocating for Patient Safety and Quality Care in Nursing Education
Open Resources for Nursing (Open RN)
The Quality and Safety Education for Nurses (QSEN) project began advocating for safe, quality patient care in 2005 by defining six competencies for nursing graduates. This initiative was created after a decade of review and investigation into the high number and high cost of medical errors in the United States. The goal of the QSEN initiative was to prepare future nurses with the knowledge, skills, and attitudes needed to improve the quality and safety of the health care system. Historically, nursing education focused on knowledge and skill acquisition, but did not address the attitudes and values of the nurse. The QSEN competencies are designed to train nursing students in prelicensure nursing programs. The six QSEN competencies, as shown in Figure 10.6,[1] are Patient-Centered Care, Teamwork and Collaboration, Evidence-Based Practice, Quality Improvement, Safety, and Informatics.[2]
Read the QSEN Prelicensure Table of Competencies.
Patient-Centered Care
The Patient-Centered Care QSEN competency advocates for the client as “the source of control and full partner in providing compassionate and coordinated care based on respect for patient’s preferences, values, and needs.”[3] This competency encourages nurses to consider clients’ cultural traditions and personal beliefs while providing compassionate care. Patient-centered care also includes the family in the care team. The goal of patient-centered care is to improve the individual’s health outcomes. Integration of this competency has led to improved patient satisfaction scores, reduced expenses, and a positive care environment.[4]
Teamwork and Collaboration
The Teamwork and Collaboration QSEN competency focuses on functioning effectively within nursing and interprofessional teams and fostering open communication, mutual respect, and shared decision-making to achieve quality patient care.[5] Effective communication has been proven to reduce errors and improve client safety.[6] The Joint Commission also includes improved communication as one of the National Patient Safety Goals, aligning with this QSEN competency. Collaboration requires information sharing across disciplines with respect for the knowledge, skills, and experience of each team member. Two examples of tools used to promote effective teamwork and collaboration are ISBARR and TeamSTEPPS®. Additionally, “principles of collaboration” have been established by the ANA.
ISBARR
Several communication tools have been developed to improve communication in various health care settings. ISBARR is an example of a well-established communication tool. As previously discussed in the “Collaboration Within the Interprofessional Team” chapter, ISBARR is a mnemonic for the components to include when communicating with other health care team members: Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat back.[7]
TeamSTEPPS®
As previously discussed in the “Collaboration Within the Interprofessional Team” chapter, TeamSTEPPS® (Team Strategies and Tools to Enhance Performance and Patient Safety) is a well-established framework to improve client safety through effective communication in health care environments. It consists of four core competencies: communication, leadership, situation monitoring, and mutual support.
Principles of Collaboration
The American Nurses Association (ANA) and the American Organization of Nurse Executives (AONE) jointly created the “Principles of Collaboration” to guide nurses in creating, enhancing, and sustaining collaborative relationships. These principles include effective communication, authentic relationships, and a learning environment and culture. The principle of authentic relationships includes the following guidelines[8]:
- Be true to yourself – be sure your actions match your words and those around you are confident that what they see is what they get.
- Empower others to have ideas, to share those ideas, and to participate in projects that leverage or enact those ideas.
- Recognize and leverage each other’s strengths.
- Be honest 100% of the time – with yourself and with others.
- Respect others’ personalities, needs, and wants.
- Ask for what you want but stay open to negotiating the difference.
- Assume good intent from others’ words and actions, and assume they are doing their best.
Read more about the “Principles of Collaboration” by the ANA and AONE.
Evidence-Based Practice
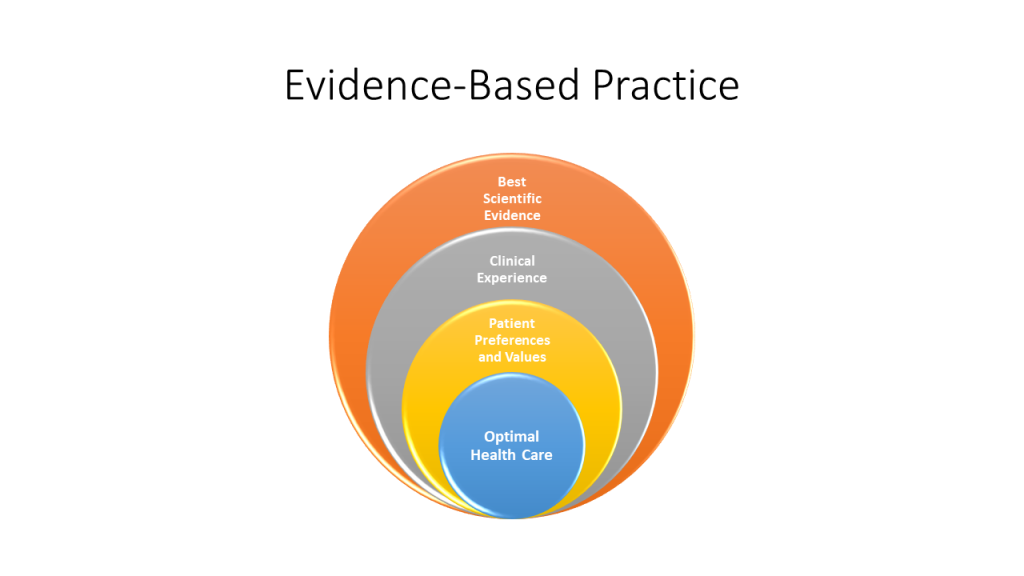
The Evidence-Based Practice QSEN competency focuses on integrating scientific evidence with clinical expertise and client/family preferences and values for delivery of optimal health care.[9] See Figure 10.7[10] for an illustration of Evidence-Based Practices (EBP). Read more about EPB in the “Quality and Evidence-Based Practice” chapter. Read examples of evidence-based improvements in the following box.
Read these examples of evidence-based practice improvements:
Quality Improvement
The Quality Improvement QSEN competency focuses on using data to monitor the outcomes of care processes and using improvement methods to design and test changes to continuously improve the quality and safety of health care systems.[11] The goal of this competency is to improve processes, policies, and clinical decisions to improve client outcomes and system performance. As the pool of nursing literature grows and nursing practices have been updated to reflect current evidence, health care organizations have seen improvements in quality, safety, and experienced cost savings.[12]
Read more about the quality improvement processes in the “Quality and Evidence-Based Practice” chapter.
Safety
The Safety QSEN competency focuses on minimizing “risk of harm to patients and providers through both system effectiveness and individual performance.”[13] Although safety is embedded in all of the QSEN competencies, this competency specifically advocates for preventing client harm. Despite the health care industry’s continued focus on process improvement and improving client outcomes, errors continue to occur, and nurses are often involved in these events as frontline caregivers. Safe nursing practice starts with an awareness of the potential risks for client harm in every situation.
Several initiatives have been adopted to reduce risk for client harm, such as double-checking high-risk medications and verifying a patient’s name and date of birth prior to every intervention. However, client safety is compromised when there are gaps in quality measures such as inadequate staff training, broken equipment, or an organizational culture that doesn’t support best practices.
The “Safety” competency is best addressed by organizations establishing a safety culture where every worker commits to keeping client safety at the center of decision-making. An organization that has a culture of safety encourages reporting of unusual incidents, process failures, or other issues that could cause client harm, allowing the organization to investigate the event and take action to prevent the event from occurring in the future. Improvements are made as a result of a culture that questions attitudes, actions, and decisions in client care and recognizes threats to safety. Read more about safety culture in the “Legal Implications” chapter.
Informatics
The Informatics QSEN competency focuses on using information and technology to communicate, manage knowledge, mitigate error, and support decision-making.[14] Health care is filled with various technologies used to promote a safe care environment, such as electronic medical records (EMRs), bedside medication administration devices, smart IV pumps, and medication distribution systems. These technologies provide safeguards and reminders to help prevent client harm, but the nurse must be knowledgeable in using technology, as well as understand how information obtained from technologies is used to improve client patient outcomes. As information related to technology continues to evolve, it is the responsibility of every nurse to participate in continued professional development related to informatics.
Media Attributions
- QSEN Competencies by Kim Ernstmeyer
- Evidence Based Practice by Kim Ernstmeyer
- “QSEN Competencies.png” by Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- QSEN. (n.d.). About. https://qsen.org/about-qsen/ ↵
- QSEN. (n.d.). About. https://qsen.org/about-qsen/ ↵
- Roseman, D., Osborne-Stafsnes, J., Amy, C. H., Boslaugh, S., & Slate-Miller, K. (2013). Early lessons from four 'aligning forces for quality' communities bolster the case for patient-centered care. Health Aff (Millwood), 32(2), 232-241. https://doi.org/10.1377/hlthaff.2012.1085 ↵
- QSEN. (n.d.). About. https://qsen.org/about-qsen/ ↵
- Burgener, A. M. (2020). Enhancing communication to improve patient safety and to increase patient satisfaction. The Health Care Manager, 39(3), 128-132. https://doi.org/10.1097/hcm.0000000000000298 ↵
- Enlow, M., Shanks, L., Guhde, J., & Perkins, M. (2010). Incorporating interprofessional communication skills (ISBARR) into an undergraduate nursing curriculum. Nurse Educator, 35(4), 176-180. https://doi.org/10.1097/nne.0b013e3181e339ac ↵
- American Nurses Association & American Organization of Nurses Executives. (n.d.). ANA/AONE principles for collaborative relationships between clinical nurses and nurse managers. https://www.nursingworld.org/~4af4f2/globalassets/docs/ana/ethics/principles-of-collaborative-relationships.pdf ↵
- QSEN. (n.d.). About. https://qsen.org/about-qsen/ ↵
- “Evidence-Based Practice.jpg” by Kim Ernstmeyer for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- QSEN. (n.d.). About. https://qsen.org/about-qsen/ ↵
- Cullen, L., Titler, M. G., & Rempel, G. (2011). An advanced educational program promoting evidence-based practice. Western Journal of Nursing Research, 33(3), 345-364. https://doi.org/10.1177/0193945910379218 ↵
- QSEN. (n.d.). About. https://qsen.org/about-qsen/ ↵
- QSEN. (n.d.). About. https://qsen.org/about-qsen/ ↵
Dosing considerations play an important role in understanding the effect that a medication may have on a client. During administration, the nurse must pay close attention to the desired effect and therapeutic response, as well as the safe dose range for any medication.
The nurse should have an understanding of medication efficacy in order to ensure its appropriateness. If a nurse is provided a variety of medication choices according to a provider's written protocol, the nurse should select the option with the anticipated desired therapeutic response.
Additionally, the nurse must be aware of the overall dose-response based on the dosage selected. Dose response is the dose of medication required to achieve the desired response to the medication. As the dose increases, the response of the drug may increase, as well as the potential for toxicity. This response helps determine the therapeutic index of a drug, or the effective dose range. The measured response and dose are often graphed perpendicular to each other, with the slope of the graph's curve representing therapeutic index (or overall dose-effect). It is important to note that some medications have a very small therapeutic window, and even small increases in dosages can result in toxic effects. See Figure 1.8[1] for an illustration of a dose-response graph.
Onset, Peak, and Duration
Three additional principles related to the effect a medication has on a client are onset, peak, and duration.
Onset of medication refers to when the medication first begins to take effect. Time of onset is affected by the route of administration. For example, a diuretic given intravenously will begin to take effect much faster than a diuretic administered orally because the intravenous route delivers the drug directly to the systemic circulation and avoids the first-pass effect.
Peak refers to the maximum concentration of medication in the body, and the client shows evidence of greatest therapeutic effect. For example, a client taking ibuprofen can anticipate maximum pain relief in one to two hours when the medication reaches peak serum levels.
Duration refers to the length of time the medication produces its desired therapeutic effect. For example, the duration of oral acetaminophen is four to six hours, at which time the client will likely require an additional dose for pain.
Duration, Dosing, and Steady State
Now let's consider the implication of duration and dosing. Remember the duration of medication is correlated with the elimination. Half-life is the amount of time that it takes for half of the drug to be eliminated from the body.
If a medication has a short half-life (and is therefore eliminated more quickly from the body), the therapeutic effect is shorter. These medications may require repeated dosing throughout the day in order to achieve steady blood levels of active free drug and a sustained therapeutic effect.
Other medications have a longer half-life (and therefore are eliminated more slowly from the body, resulting in longer therapeutic duration) and may only be administered once or twice per day. For example, oxycodone immediate release is prescribed every 4 to 6 hours for the therapeutic effect of immediate relief of severe pain, whereas oxycodone ER (extended release) is prescribed every 12 hours for the therapeutic effect of sustained relief of severe pain.
Steady state refers to the point at which the amount of drug entering the body is equal to the amount of drug being eliminated, resulting in a stable drug concentration.[2] When steady state is achieved, there is a state of equilibrium in the body and the concentration of the drug remains constant, resulting in optimal therapeutic effect.
Clinical Example
Consider this client care example and apply the principles of onset, peak, and duration: A 67-year-old female postoperative client rings the call light to request medication for pain related to the hip replacement procedure she had earlier that day. She notes her pain is "excruciating, a definite 9 out of 10." Her brow is furrowed, and she is grimacing in obvious discomfort. As the nurse providing care for the client, you examine her postoperative medication orders and consider the pain medication options available to you. In reviewing the various options, it is important to consider how quickly a medication will work (onset), when the medication will reach maximum effectiveness (peak), and how long the pain relief will last (duration). Understanding these principles is important in effectively relieving the client's pain and constructing an overall plan of care.
Critical Thinking Activity 1.9
- At 0500, your client who had a total knee replacement yesterday rates his pain while walking as 7 out of 10. Physical therapy is scheduled at 0900. The client has acetaminophen (Tylenol) 625 mg ordered every four hours as needed for discomfort. What should you consider in relation to the administration and timing of the client's pain medication?
- Your client is prescribed NPH insulin to be given at breakfast and supper. As a student nurse, you know that insulin is used to decrease blood sugar levels in clients with diabetes mellitus. During report, you hear that the client has been ill with GI upset during the night, and the nursing assistant just informed you he refused his breakfast tray. While reviewing this medication order, you consider the purpose of the medication and information related to the medication's onset, peak, and duration. When reviewing the drug reference, you find the NPH insulin has an onset of about 1 - 3 hours after medication administration. What should you consider in relation to the administration and timing of the client's insulin?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" section at the end of the book.
Dosing considerations play an important role in understanding the effect that a medication may have on a client. During administration, the nurse must pay close attention to the desired effect and therapeutic response, as well as the safe dose range for any medication.
The nurse should have an understanding of medication efficacy in order to ensure its appropriateness. If a nurse is provided a variety of medication choices according to a provider's written protocol, the nurse should select the option with the anticipated desired therapeutic response.
Additionally, the nurse must be aware of the overall dose-response based on the dosage selected. Dose response is the dose of medication required to achieve the desired response to the medication. As the dose increases, the response of the drug may increase, as well as the potential for toxicity. This response helps determine the therapeutic index of a drug, or the effective dose range. The measured response and dose are often graphed perpendicular to each other, with the slope of the graph's curve representing therapeutic index (or overall dose-effect). It is important to note that some medications have a very small therapeutic window, and even small increases in dosages can result in toxic effects. See Figure 1.8[3] for an illustration of a dose-response graph.
Onset, Peak, and Duration
Three additional principles related to the effect a medication has on a client are onset, peak, and duration.
Onset of medication refers to when the medication first begins to take effect. Time of onset is affected by the route of administration. For example, a diuretic given intravenously will begin to take effect much faster than a diuretic administered orally because the intravenous route delivers the drug directly to the systemic circulation and avoids the first-pass effect.
Peak refers to the maximum concentration of medication in the body, and the client shows evidence of greatest therapeutic effect. For example, a client taking ibuprofen can anticipate maximum pain relief in one to two hours when the medication reaches peak serum levels.
Duration refers to the length of time the medication produces its desired therapeutic effect. For example, the duration of oral acetaminophen is four to six hours, at which time the client will likely require an additional dose for pain.
Duration, Dosing, and Steady State
Now let's consider the implication of duration and dosing. Remember the duration of medication is correlated with the elimination. Half-life is the amount of time that it takes for half of the drug to be eliminated from the body.
If a medication has a short half-life (and is therefore eliminated more quickly from the body), the therapeutic effect is shorter. These medications may require repeated dosing throughout the day in order to achieve steady blood levels of active free drug and a sustained therapeutic effect.
Other medications have a longer half-life (and therefore are eliminated more slowly from the body, resulting in longer therapeutic duration) and may only be administered once or twice per day. For example, oxycodone immediate release is prescribed every 4 to 6 hours for the therapeutic effect of immediate relief of severe pain, whereas oxycodone ER (extended release) is prescribed every 12 hours for the therapeutic effect of sustained relief of severe pain.
Steady state refers to the point at which the amount of drug entering the body is equal to the amount of drug being eliminated, resulting in a stable drug concentration.[4] When steady state is achieved, there is a state of equilibrium in the body and the concentration of the drug remains constant, resulting in optimal therapeutic effect.
Clinical Example
Consider this client care example and apply the principles of onset, peak, and duration: A 67-year-old female postoperative client rings the call light to request medication for pain related to the hip replacement procedure she had earlier that day. She notes her pain is "excruciating, a definite 9 out of 10." Her brow is furrowed, and she is grimacing in obvious discomfort. As the nurse providing care for the client, you examine her postoperative medication orders and consider the pain medication options available to you. In reviewing the various options, it is important to consider how quickly a medication will work (onset), when the medication will reach maximum effectiveness (peak), and how long the pain relief will last (duration). Understanding these principles is important in effectively relieving the client's pain and constructing an overall plan of care.
Critical Thinking Activity 1.9
- At 0500, your client who had a total knee replacement yesterday rates his pain while walking as 7 out of 10. Physical therapy is scheduled at 0900. The client has acetaminophen (Tylenol) 625 mg ordered every four hours as needed for discomfort. What should you consider in relation to the administration and timing of the client's pain medication?
- Your client is prescribed NPH insulin to be given at breakfast and supper. As a student nurse, you know that insulin is used to decrease blood sugar levels in clients with diabetes mellitus. During report, you hear that the client has been ill with GI upset during the night, and the nursing assistant just informed you he refused his breakfast tray. While reviewing this medication order, you consider the purpose of the medication and information related to the medication's onset, peak, and duration. When reviewing the drug reference, you find the NPH insulin has an onset of about 1 - 3 hours after medication administration. What should you consider in relation to the administration and timing of the client's insulin?
Note: Answers to the Critical Thinking activities can be found in the "Answer Key" section at the end of the book.
There are a variety of drugs and substances that clients may utilize for symptom management or to enhance their wellness. Nurses document clients' use of prescription medications, over-the-counter medications, herbal substances, and other supplements in the medical record. Some substances have a long half-life and have the potential to interact with new medications, so accuracy is vital. Ensuring an accurate medical record and knowledge of the different types of substances a client is taking is important for an effective nursing plan of care.
Prescription Medications
Drugs are prescribed by a licensed prescriber for a specific person's use and regulated through the United States Food and Drug Administration (FDA). More information about FDA approval of medications is described in the “Legal/Ethical” chapter. Prescription medications include brand-name medications and generic medications.[5]
Common Prefixes, Suffixes, And Roots For Classes Of Medication
Table 1.8 provides prefixes, suffixes, and roots associated with common prescription medications. As a nurse, familiarizing yourself with the content in the table can help you to quickly organize medications based on their name and recall their mechanism of action and identify potential interactions or side effects. This knowledge can improve your ability to safely administer medications and provide health teaching. Ultimately, this knowledge can lead to improved client outcomes, increased satisfaction, and a reduced risk of adverse events and medication errors.
Table 1.8 Common Classes of Medications, Examples, Suffixes, and Roots
| Class of Medication | Example | Common Suffixes | Common Roots |
|---|---|---|---|
| Analgesics | lidocaine | -caine | -morph, -morphe, -morphic |
| Antacids | omeprazole | -azole | -tidine |
| Antibiotics | levofloxacin | -mycin, -floxacin | bacter-, vir-, -cidal |
| Anticoagulants | warfarin | -arin | coagul- |
| Antidepressants | fluoxetine | -oxetine, -ipramine | serotonin, norepinephrine |
| Antihistamines | diphenhydramine | -dine, -mine | hist- |
| Anti-inflammatory | cortisone | -one | -corti-, -flam-, -prost- |
| Antipsychotics | olanzapine | -azine, -apine | dopa-, sero-, -plegia |
| Beta-blockers | metoprolol | -olol | adrenergic, beta- |
| Bronchodilators | albuterol | -terol | bronch-, -pnea |
| Corticosteroids | prednisone | -sone or -solone | |
| Diuretics | furosemide | -semide, -thiazide | -uret-, -osm- |
| Hypoglycemics | glipizide | -ide | gluc-, insulin- |
| Statins | atorvastatin | -statin | cholesterol, lipid- |
Generic Medications
Generic medications can be safe and effective alternatives to their brand-name counterparts at a significantly reduced cost. By law, generic medications must have the same chemically active ingredient in the same dose as the brand name (i.e., they must be "bio-equivalent"). However, the excipients (the base substance that holds the active chemical ingredient into a pill form (such as talc) or the flavoring can be different. Some clients do not tolerate these differences in excipients very well. When prescribing a medication, the provider must indicate that a generic substitution is acceptable. Nurses are often pivotal in completing insurance paperwork on the client's behalf if the brand-name medication is more effective or better tolerated by that particular client.[6]
When studying medications in nursing school and preparing for the NCLEX, it is important to know medications by their generic name because the NCLEX does not include brand names in their questions.
Over-the-Counter Medications
Over-the-counter (OTC) medications do not require a prescription. They can be bought at a store and may be used by multiple individuals. OTC medications are also regulated through the FDA. Some prescription medications are available for purchase as OTC in smaller doses. For example, diphenhydramine (Benadryl) is commonly prescribed as 50 mg every 6 hours, and the prescription strength is 50 mg. However, it can also be purchased OTC in 25 mg doses (or less for children.)[7]
Herbals and Supplements
Herbs and supplements may include a wide variety of substances including vitamins, minerals, enzymes, and botanicals. Supplements such as “protein powders” are marketed to build muscle mass and can contain a variety of substances that may not be appropriate for all individuals. Herbals and supplements are often considered complementary and alternative medications (CAM). Complementary and alternative medications (CAM) are types of therapies that are commonly used in conjunction with or as an alternate to traditional medical therapies. These herbal and supplement substances are not regulated by the FDA, and most have not undergone rigorous scientific testing for safety for the public. While clients may be tempted to try these herbals and supplements, there is no guarantee that they contain the ingredients listed on the label. It is also important to remember that there is a potential for adverse effects or even overdose if the herbal or supplement contains some of the same drug that was also prescribed to a client.[8] By understanding the use of CAM therapies, nurses can help their clients make informed decisions and take a holistic approach to their care. Additionally, being knowledgeable about CAM therapies can help nurses to better educate their clients on the potential benefits and risks associated with these therapies, which can help improve client outcomes and satisfaction.
Read additional information on complementary and alternative medicine at the National Center for Complementary and Integrative Health (NCCIH) Database.
There are a variety of drugs and substances that clients may utilize for symptom management or to enhance their wellness. Nurses document clients' use of prescription medications, over-the-counter medications, herbal substances, and other supplements in the medical record. Some substances have a long half-life and have the potential to interact with new medications, so accuracy is vital. Ensuring an accurate medical record and knowledge of the different types of substances a client is taking is important for an effective nursing plan of care.
Prescription Medications
Drugs are prescribed by a licensed prescriber for a specific person's use and regulated through the United States Food and Drug Administration (FDA). More information about FDA approval of medications is described in the “Legal/Ethical” chapter. Prescription medications include brand-name medications and generic medications.[9]
Common Prefixes, Suffixes, And Roots For Classes Of Medication
Table 1.8 provides prefixes, suffixes, and roots associated with common prescription medications. As a nurse, familiarizing yourself with the content in the table can help you to quickly organize medications based on their name and recall their mechanism of action and identify potential interactions or side effects. This knowledge can improve your ability to safely administer medications and provide health teaching. Ultimately, this knowledge can lead to improved client outcomes, increased satisfaction, and a reduced risk of adverse events and medication errors.
Table 1.8 Common Classes of Medications, Examples, Suffixes, and Roots
| Class of Medication | Example | Common Suffixes | Common Roots |
|---|---|---|---|
| Analgesics | lidocaine | -caine | -morph, -morphe, -morphic |
| Antacids | omeprazole | -azole | -tidine |
| Antibiotics | levofloxacin | -mycin, -floxacin | bacter-, vir-, -cidal |
| Anticoagulants | warfarin | -arin | coagul- |
| Antidepressants | fluoxetine | -oxetine, -ipramine | serotonin, norepinephrine |
| Antihistamines | diphenhydramine | -dine, -mine | hist- |
| Anti-inflammatory | cortisone | -one | -corti-, -flam-, -prost- |
| Antipsychotics | olanzapine | -azine, -apine | dopa-, sero-, -plegia |
| Beta-blockers | metoprolol | -olol | adrenergic, beta- |
| Bronchodilators | albuterol | -terol | bronch-, -pnea |
| Corticosteroids | prednisone | -sone or -solone | |
| Diuretics | furosemide | -semide, -thiazide | -uret-, -osm- |
| Hypoglycemics | glipizide | -ide | gluc-, insulin- |
| Statins | atorvastatin | -statin | cholesterol, lipid- |
Generic Medications
Generic medications can be safe and effective alternatives to their brand-name counterparts at a significantly reduced cost. By law, generic medications must have the same chemically active ingredient in the same dose as the brand name (i.e., they must be "bio-equivalent"). However, the excipients (the base substance that holds the active chemical ingredient into a pill form (such as talc) or the flavoring can be different. Some clients do not tolerate these differences in excipients very well. When prescribing a medication, the provider must indicate that a generic substitution is acceptable. Nurses are often pivotal in completing insurance paperwork on the client's behalf if the brand-name medication is more effective or better tolerated by that particular client.[10]
When studying medications in nursing school and preparing for the NCLEX, it is important to know medications by their generic name because the NCLEX does not include brand names in their questions.
Over-the-Counter Medications
Over-the-counter (OTC) medications do not require a prescription. They can be bought at a store and may be used by multiple individuals. OTC medications are also regulated through the FDA. Some prescription medications are available for purchase as OTC in smaller doses. For example, diphenhydramine (Benadryl) is commonly prescribed as 50 mg every 6 hours, and the prescription strength is 50 mg. However, it can also be purchased OTC in 25 mg doses (or less for children.)[11]
Herbals and Supplements
Herbs and supplements may include a wide variety of substances including vitamins, minerals, enzymes, and botanicals. Supplements such as “protein powders” are marketed to build muscle mass and can contain a variety of substances that may not be appropriate for all individuals. Herbals and supplements are often considered complementary and alternative medications (CAM). Complementary and alternative medications (CAM) are types of therapies that are commonly used in conjunction with or as an alternate to traditional medical therapies. These herbal and supplement substances are not regulated by the FDA, and most have not undergone rigorous scientific testing for safety for the public. While clients may be tempted to try these herbals and supplements, there is no guarantee that they contain the ingredients listed on the label. It is also important to remember that there is a potential for adverse effects or even overdose if the herbal or supplement contains some of the same drug that was also prescribed to a client.[12] By understanding the use of CAM therapies, nurses can help their clients make informed decisions and take a holistic approach to their care. Additionally, being knowledgeable about CAM therapies can help nurses to better educate their clients on the potential benefits and risks associated with these therapies, which can help improve client outcomes and satisfaction.
Read additional information on complementary and alternative medicine at the National Center for Complementary and Integrative Health (NCCIH) Database.

