Assessing Reflexes
Open Resources for Nursing (Open RN)
Assessment of reflexes is not typically performed by registered nurses as part of a routine nursing neurological assessment of adult patients, but it is used in nursing specialty units and in advanced practice. Spinal cord injuries, neuromuscular diseases, or diseases of the lower motor neuron tract can cause weak or absent reflexes. To perform deep reflex tendon testing, place the patient in a seated position. Use a reflex hammer in a quick striking motion by the wrist on various tendons to produce an involuntary response. Before classifying a reflex as absent or weak, the test should be repeated after the patient is encouraged to relax because voluntary tensing of the muscles can prevent an involuntary reflexive action.
Reflexes are graded from 0 to 4+, with “2+” considered normal:
- 0: Absent
- 1+: Hypoactive
- 2+: Normal
- 3+: Hyperactive without clonus
- 4+: Hyperactive with clonus (involuntary muscle contraction)
To observe assessment of deep tendon reflexes, view the following video.
View Stanford Medicine’s Assessment of Deep Tendon Reflexes video on YouTube.[1]
Brachioradialis Reflex
The brachioradialis reflex is used to assess the cervical spine nerves C5 and C6. Ask the patient to support their arm on their thigh or on your hand. Identify the insertion of the brachioradialis tendon on the radius and briskly tap it with the reflex hammer. The reflex consists of flexion and supination of the forearm. See Figure 6.37[2] for an image of obtaining the brachioradialis reflex.

Triceps Reflex
The triceps reflex assesses cervical spine nerves C6 and C7. Support the patient’s arm underneath their bicep to maintain a position midway between flexion and extension. Ask the patient to relax their arm and allow it to fully be supported by your hand. Identify the triceps tendon posteriorly just above its insertion on the olecranon. Tap briskly on the tendon with the reflex hammer. Note extension of the forearm. See Figure 6.38[3] for an image of the triceps reflex exam.

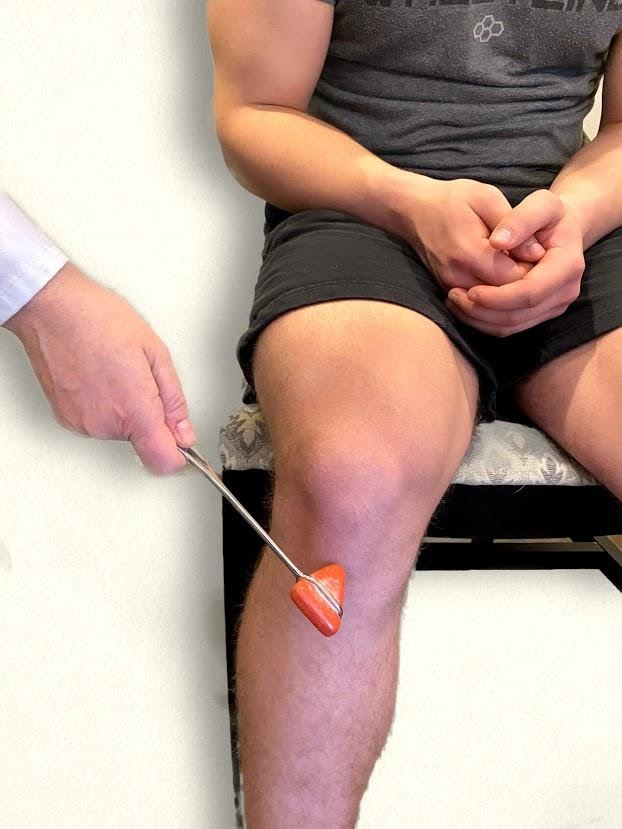
Patella (Knee Jerk) Reflex
The patellar reflex, commonly referred to as the knee jerk test, assesses lumbar spine nerves L2, L3, and L4. Ask the patient to relax the leg and allow it to swing freely at the knee. Tap the patella tendon briskly, looking for extension of the lower leg. See Figure 6.39[4] for an image of assessing a patellar reflex.
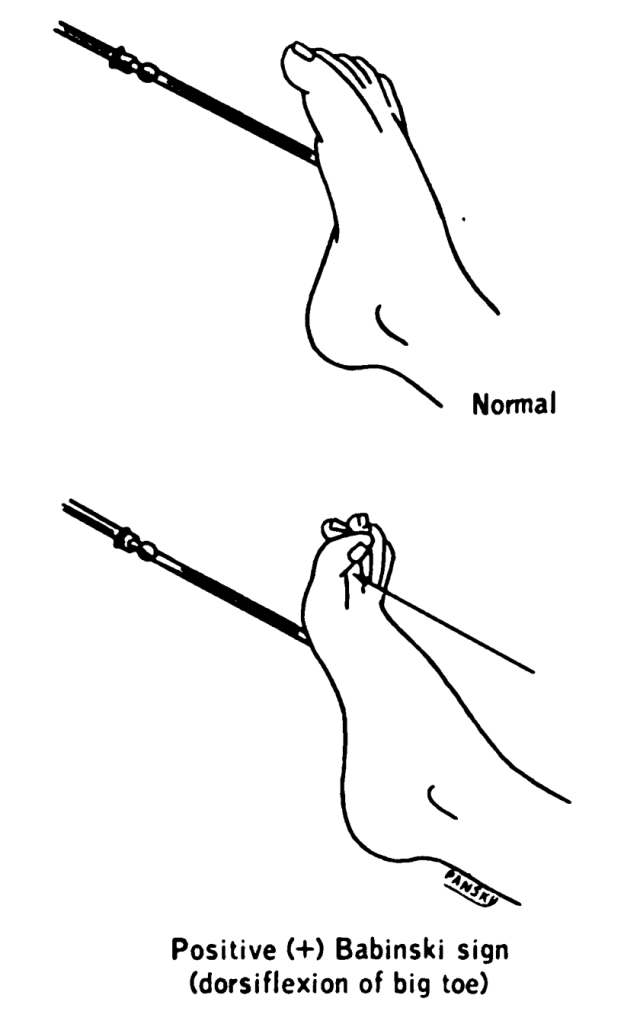
Plantar Reflex
The plantar reflex, or “Babinski reflex” assesses lumbar spine L5 and sacral spine S1. Ask the patient to extend their lower leg, and then stabilize their foot in the air with your hand. Slide the object along the lateral surface of the sole of the foot toward the toes. Many patients are ticklish and withdraw their foot, so it is sufficient to elicit the reflex by using your thumb to stroke lightly from the sole of the foot toward the toes. If there is no response, use a blunt object such as a key or pen. The expected reflex is flexion (i.e., bending) of the great toe. An abnormal response is toe extension (i.e., straightening), also known as the Babinski reflex. In a child younger than 2 years old, the big toe should bend up and backward toward the top of your foot while the other four toes fan out. This response is normal and doesn’t indicate any problems or abnormalities. In a child older than 2 years old or in a mature adult, the Babinski sign should be absent. All five toes should flex, or curl downward, as if they’re trying to grab something. If this test is conducted on a child older than 2 or an adult and the toes respond like those of a child under two years old, this can indicate an underlying neurological issue. See Figures 6.40 – 6.43[5],[6],[7],[8] for images of assessing the plantar reflex.



Newborn Reflexes
Newborn reflexes originate in the central nervous system and are exhibited by infants at birth but disappear as part of child development. Neurological disease or delayed development is indicated if these reflexes are not present at birth, do not spontaneously resolve, or reappear in adulthood. Common newborn reflexes include sucking, rooting, palmar grasp, plantar grasp, Babinski, Moro, and tonic neck reflexes.
Sucking Reflex
The sucking reflex is common to all mammals and is present at birth. It is linked with the rooting reflex and breastfeeding. It causes the child to instinctively suck anything that touches the roof of their mouth and simulates the way a child naturally eats. See Figure 6.44[11] for an image of the newborn sucking reflex.

Rooting Reflex
The rooting reflex assists in the act of breastfeeding. A newborn infant will turn its head toward anything that strokes its cheek or mouth, searching for the object by moving its head in steadily decreasing arcs until the object is found. See Figure 6.45[12] for an image of a newborn exhibiting the rooting reflex.

Palmar and Plantar Grasps
When an object is placed in an infant’s hand and the palm of the child is stroked, the fingers will close reflexively, referred to as the palmar grasp reflex. A similar reflexive action occurs if an object is placed on the plantar surface of an infant’s foot, referred to as the plantar grasp reflex. See Figure 6.46[13] for an image of the palmar grasp reflex.

Moro Reflex
The Moro reflex is present at birth and is often stimulated by a loud noise. The Moro reflex occurs when the legs and head of the infant extend while the arms jerk up and out with the palms up. See Figure 6.47[14] for an image of an infant exhibiting the Moro reflex.

Tonic Neck Reflex
The asymmetrical tonic neck reflex, also known as the “fencing posture,” occurs when the child’s head is turned to the side. The arm on the same side as the head is turned will straighten and the opposite arm will bend. See Figure 6.48[15] for an image of the tonic neck reflex.

Walking-Stepping Reflex
Although infants cannot support their own weight, when the soles of their feet touch a surface, it appears as if they are attempting to walk by placing one foot in front of the other foot.
Media Attributions
- Deep Reflex Exam image 4
- unnamed (46)
- unnamed41
- The Plantar Reflex
- Lawrence_1960_20.4
- BabinskiSign
- Babinski-newborn
- BabySuckingFingers
- download
- baby-428395_1920
- Moro_Reflex
- Asymmetrical_tonic_neck_reflex_(ATNR)_in_a_two-week-old_female
- Stanford Medicine 25. (2014, March 16). Deep tendon reflexes (Stanford medicine 25) [Video]. YouTube. All rights reserved. https://youtu.be/0sqCIzuotWo ↵
- “Deep Reflex Exam Image 4.png” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Deep Reflex Exam Image 2.png” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Deep Reflex Exam Image 3.jpg” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Neuro Exam Image 23.png” and “Neuro Exam Image 21.png” by Meredith Pomietlo for Chippewa Valley Technical College are licensed under CC BY 4.0 ↵
- “Lawrence 1960 20.4.png” by Earl Lawrence House & Ben Pansky is in the Public Domain. ↵
- “BabinskiSign.jpg” by Medicus of Borg is in the Public Domain. ↵
- “Babinski-newborn.jpg” by Medicus of Borg is licensed under CC BY-SA 3.0 ↵
- RegisteredNurseRN. (2016, April 1). Deep tendon reflex examination for nursing head to toe assessment of neuro system [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/eqOpNQH09pA ↵
- RegisteredNurseRN. (2016, March 29). Babinski reflex | Plantar reflex test | Nursing head to toe assessment [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/dcJgxuLtHdg ↵
- “BabySuckingFingers.jpg” by Florence Devouard (anthere) is licensed under CC BY-SA 3.0 ↵
- “Rooting Reflex” by Ashley Arbuckle is licensed under CC BY 2.0 ↵
- “baby-428395_960_720.jpg” by jarmoluk is licensed under CC0 ↵
- “Moro reflex.jpg” by tawamie is licensed under CC BY-SA 3.0 ↵
- “Asymmetrical tonic neck reflex (ATNR) in a two-week-old female.jpg” by Samuel Finlayson is licensed under CC BY-SA 4.0 ↵
A reflex demonstrated by the fanning of toes with the great toe pointed toward the back (dorsum) of the foot. In adults, the Babinski response is considered abnormal and an indication of motor neuron disease.

